Resumo
Introdução
A avaliação de potenciais evocados auditivos de longa latência em criancas usuárias de implante coclear tem se mostrado um método eficaz para avaliar a maturação cortical após estimulação elétrica.
Objetivo
Analisar as modificações nos valores de latência do potencial evocado auditivo cortical antes e três meses após o uso do implante coclear.
Material e método
Estudo de caso-controle em um grupo de cinco criancas usuárias do implante coclear que aguardavam a ativação dos eletrodos, e um grupo controle constituído por cinco crianças ouvintes. A avaliação eletrófisiologica da audição foi realizada por meio do registro dos potenciais evocados auditivos corticais em duas diferentes etapas: anterior à ativação do implante coclear e após três meses de adaptação.
Resultados
Os resultados demonstraram diminuição significativa em relação ao tempo de latência do componente P1 no grupo estudo, cujos valores foram maiores daqueles do grupo controle. Quanto menor a idade na ativação, maior a redução no tempo de latência do componente P1.
Conclusão
Modificações nas características dos potenciais evocados auditivos corticais podem ser observadas em crianças que recebem o implante coclear e estas modificações têm uma relação com a idade de intervenção, sugerindo uma rápida maturação das vias auditivas apos estimulação elétrica.
© 2014 Associação Brasileira de Otorrinolaringologia e Cirurgia Cérvico-Facial. Publicado por Elsevier Editora Ltda. Todos os direitos reservados.
Keywords: PALAVRAS-CHAVE, Implante coclear, Eletrofisiologia, Audição, Plasticidade neuronal, Criança
Abstract
Introduction
: Evaluation of cortical auditory evoked potentials in children with cochlear implants has been proven to be an effective method for assessing cortical maturation after electrical stimulation.
Objective
: To analyze the changes in latency values of cortical auditory evoked potentials before and three months after cochlear implant use.
Material and methods
: This was a case-control study with a group of five children using cochlear implant awaiting activation of the electrodes, and a control group composed of five normal-hearing children. Auditory electrophysiological assessment was performed by the testing of the cortical auditory evoked potentials at two different periods: prior to cochlear implant activation and after three months of cochlear implant use.
Results
: A significant decrease in the latency time of the P1 component was observed after three months of stimulation via cochlear implant, whose values were higher than those from the control group. The younger the child was at electrode activation, the greater the reduction in latency of the P1 component.
Conclusion
: Changes in the characteristics of cortical auditory evoked potentials can be observed in children who receive cochlear implants; these changes are related to the age of intervention, suggesting a rapid maturation of the auditory pathways after electrical stimulation.
© 2014 Associação Brasileira de Otorrinolaringologia e Cirurgia Cérvico-Facial. Published by Elsevier Editora Ltda. All rights reserved.
KEYWORDS: Cochlear implants, Electrophysiology, Hearing, Neuronal plasticity, Child
Introduction
Hearing loss in early life can affect the communication development and interfere in several other aspects, such as cognitive, psychosocial, and academic, among others.1., 2. The consensus is that proper auditory stimulation from the beginning of life is necessary for the normal development of speech.3., 4., 5., 6.
The full reception of the acoustic signal by the auditory cortex allows it to constantly changes due to the phenomenon of neuronal plasticity. These changes and reorganizations enable the development of the ability to discriminate sounds that reach the central auditory nervous system (CANS), thus enabling the gradual learning of oral language.7., 8., 9.
Given the damage caused by bilateral severe-to-profound sensorineural hearing loss in children during the development of auditory skills and oral language, there is a need to provide the ability to know and recognize the sound world.
For hearing impaired children who did not experience significant benefits with the use of a hearing aid (HA), the cochlear implant (CI) has been shown to be an effective clinical resource for intervention. This electronic device aims to partially replace the function of the ear through direct stimulation of the auditory nerve fibers, improving the quality of life of adults and children.10., 11.
In order to provide maximum benefit to children - allowing for the development of auditory skills and oral language - it is important that CI stimulation is initiated within a sensitive period, preferably up to 3 years of age, so that the maturation of the CANS can properly occur.12., 13., 14. Some authors explain this phenomenon by arguing that although the deeper layers of the cortex undergo maturation processes even in the absence of stimulation, the most superficial layers of the cortex need stimulation to properly develop.15
After this sensitive period, appreciable alterations in relation to synaptic plasticity may occur, resulting in an abnormal connectivity among neuronal cells, functional disintegration and immaturity of auditory cortical areas, as well as the possibility that some auditory areas develop non-auditory functions, causing abnormalities of cognitive function restructuring.16
To verify the changes in the CANS throughout its development, objective techniques are currently capable of accurately demonstrating the benefits of effective use of CI in the process of cortical maturation. Cortical auditory evoked potentials (CAEP) have emerged as a procedure capable of objectively measuring the degree of development and limits of plasticity of the central auditory pathway through the analysis of changes in morphology and latency values of P1-N1-P2 components.13., 17.
The P1 wave of CAEP has been established as a biomarker to evaluate the maturation of the central auditory system in children. Thus, these measures can assist in verifying the effectiveness of auditory rehabilitation in children using HAs or CIs.17
Considering that the development and organization of central auditory pathways in children is closely related to an effective and appropriate auditory experience, the effective use of CAEP as a procedure capable of reflecting mainly the activity of thalamic and cortical regions appears to be potentially valid for determining the integrity of the auditory pathway and monitoring neurophysiological changes in the population with hearing loss after the intervention and auditory stimulation by CI.18., 19., 20., 21., 22.
Many studies combined the results of CAEP electrophysiological tests with behavioral assessments, which indicates that the decrease in latency time of P1 is correlated with the improvement of communicative behaviors (vocalization),4 speech perception,11 and also with speech and language skills of children.20
However, it is not clear how these changes occur in CANS. It is uncertain whether there are changes in latency time values of the P1 component after a short period of auditory stimulation via CI.
Objective
To assesss central auditory pathway maturation in children with hearing loss after three months of auditory stimulation via CI.
Methods
Study design and Ethical aspects
This investigation consisted of a case-control study with hearing impaired children who were CI users. The study group (SG) was composed of five children with bilateral sensorineural hearing loss who received surgical indication for the use of CI as an intervention in the process of auditory habilitation. The control group (CG) consisted of five normal hearing children age-matched to the children in the SG.
The study was approved by the ethics committee of the institution under the process No. 0319/11. The procedures were performed after the parents or tutors signed the informed consent.
Sample characteristics
Study group
The inclusion criteria established for SG were: maximum age of 4 years; severe/profound bilateral sensorineural hearing loss; without benefits from HA; included in the CI program; device properly functioning (according to mapping registration); full electrode insertion; daily use of the device for eight hours or longer; not using HA in the contralateral ear. Exclusion criteria were: children with neurological or cognitive impairment, or any other impairment that might compromise auditory or language development.
The SG comprised five children with cochlear implants (three males and two females) with a mean age at the time of CI activation of 2 years and 3 months (minimum 9 months and a maximum of 3 years and 6 months). The children were residents of São Paulo, Brazil, and all had bilateral severe-to-profound sensorineural hearing loss, and were awaiting activation of CI electrodes in the period between May and September of 2012.
Table 1 shows the characteristics and specifications of each participant of SG.
Table 1.
Sample characterization regarding gender, age, etiology, degree of hearing loss, duration of sensory deprivation, duration of hearing aid use, implanted side, and cochlear implant.
| Participant | Gender | Age at activation |
Etiology | Duration of sensory deprivation |
Duration of hearing aid use |
Implanted side |
|---|---|---|---|---|---|---|
| 1 | F | 21 m | Unknown | 12 m | 9 m | R |
| 2 | F | 31 m | Prematurity | 12 m | 18 m | R |
| 3 | M | 36 m | Meningitis | 24 m | 10 m | R |
| 4 | M | 9 m | Unknown | 3 m | 6 m | BE |
| 5 | M | 42 m | Unknown | 28 m | 13 m | L |
F, female; M, male; m, months; R, right; BE, both ears; L, left.
The children from SG were age-matched to those of CG, so that the results obtained after three months of CI use could be compared with those observed in normal hearing children at the same age range. The criteria used to pair children was a difference of 4 months of age between children of the study group and the control group.
Statistical analysis showed no difference for age and gender. The Mann-Whitney test indicated that there was no difference in age mean between groups (mean SG = 27.8 ± 13.03; mean CG = 27.8 ± 12.60; U = 12.0, z = − 0.104, p = 0.917). Fisher’s exact test indicated no difference on gender distribution between groups (p = 0.524), although there were more males in the SG (60%) and females in the CG (80%).
Control group
Inclusion criteria established for CG were: maximum age of 4 years; without hearing loss (tympanometric curve type A, present reflexes and auditory and speech reception thresholds less than or equal to 15 dB); and without impairments in neurological, motor, or language development.
The CG comprised five children (one male and four females) with a mean age of 2 years and 3 months (minimum 11 months and maximum of 3 years and 2 months). The participants of the CG are characterized in Table 2.
Table 2.
Characterization of the control group regarding gender and age.
| Participant | 1 | 2 | 3 | 4 | 5 |
|---|---|---|---|---|---|
| Gender | F | F | M | F | F |
| Age at first assessment |
19 m | 35 m | 37 m | 10 m | 38 m |
F, female; M, male; m, months.
Children of this group underwent hearing assessment prior to electrophysiological evaluation to discard any type of hearing impairment. This consisted of: pure tone audiometry, speech audiometry (speech reception threshold - SRT), as well as immittance measures with acoustic reflex research.
Procedures
Children were invited to participate in the study by an invitation letter delivered to their parents or guardians or by telephone.
An interview was conducted with the parents or guardians of the SG at the Audiology Clinic of the Department in order to obtain information on: age, education, side of implantation, HAs, etiology of hearing loss, and results of the last audiometry performed at the institution.
The evaluation of the CAEP was performed in an acoustically treated room with the child in an alert state, sitting comfortably in a reclining chair. They were instructed and encouraged to watch a puppet theater or movie with no sound during the procedure. Before starting the procedure, it was verified that the CI was functioning: battery, program, and microphone.
The Smart EP USB Jr Intelligent Hearing Systems (IHS 5020), a device that provides two channels of stimulation, was used. Channel A was intended to capture the CAEP in the right ear, and channel B, in the left ear. In both channels, the active electrode was placed at Cz connected to the input (+) of the pre-amplifier, and the reference electrode was placed on the earlobe of the CI side and connected to the input (−). The ground electrode was positioned at Fpz and connected to the ground position.
The electrodes were placed with conductive paste for electroencephalogram (EEG) from Tem 20TM after cleaning the skin with an EEG abrasive gel from NUPREP. The impedance level of electrodes that was accepted for the procedure was between 1 and 3 K ohms.
The acoustic stimulation was presented by a sound field system with speakers positioned at an angle of 90° azimuth and 40 cm away from the implanted side of children from the SG. The same procedure was used with children from CG; the stimuli presentation was performed on the side with better audiometric thresholds. For subjects with symmetric audiometric thresholds, stimuli was presented at the right side. Two samples were collected from each subject to confirm the results.
Regarding the parameters of stimulation, the CAEP were recorded with the speech stimulus of the syllable /ba/, presented with inter-stimulus intervals of 500 ms, at an intensity of 70 dBNA and a presentation rate of 1.9 stimuli per second. The parameters described below were also used during registration: bandpass filter from 1 to 30 Hz, gain of 100,000, averaging 512 stimuli, and response analysis window of 100 ms pre-stimulus and 500 ms post-stimulus.
Data analysis consisted of an assessment of the latency times of the P1 component, represented in milliseconds, before and after three months of CI use. The findings were compared to those obtained with children from the CG.
Results
Control group
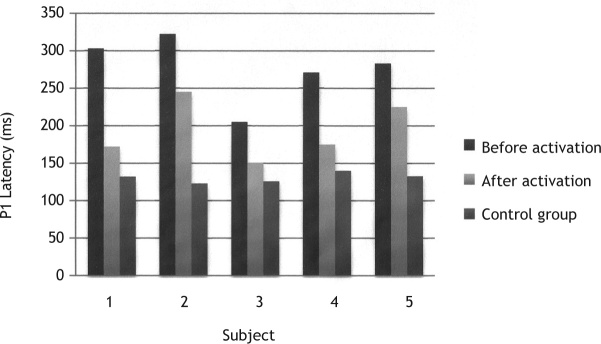
The values of the latency time of the P1 component from CG children ranged between 123 ms and 140 ms (children aged 35 months and 10 months, respectively) (Table 3 and Fig. 1).
Table 3.
Description of age and latency values obtained with cortical auditory evoked potential for the study group and control group.
| Participant | 1 | 2 | 3 | 4 | 5 | |
|---|---|---|---|---|---|---|
| SG | Age (m) | 21 | 31 | 36 | 9 | 42 |
| P1 latency (ms) | ||||||
| 1st assessment | 303 | 322 | 205 | 271 | 283 | |
| 2nd assessment | 172 | 245 | 151 | 175 | 225 | |
| CG | Age (m) | 19 | 35 | 37 | 10 | 38 |
| P1 latency (ms) | 132 | 123 | 126 | 140 | 133 |
SG, study group; CG, control group; m, months; ms, milliseconds.
Figure 1.
P1 component latency values before and after activation of cochlear implant electrodes of the study group compared to control group.
Study group
After three months of CI use, a reduction in latency of the CAEP in all participants from the SG was observed.
The first child assessed was diagnosed at 1 year of age and used bilateral HAs for nine months. Hearing thresholds obtained in free field with the device were 85 and 80 dB for frequencies between 250 and 500 Hz, respectively. Three months after surgery, the audiometric thresholds in the implanted ear ranged between 55 and 70 dB at frequencies from 0.25 to 2 KHz. In the CAEP record prior to activation, the P1 wave latency was observed at 303 ms. After three months of CI use, a decrease in P1 component latency was observed, which was registered at 172 ms.
The second child assessed was diagnosed at 3 months and received bilateral HAs at 1 year of age. Pre-surgical pure tone audiometry in free field with HAs revealed responses between 70 and 100 dB for frequencies from 0.25 to 2 KHz in the right ear. Three months after surgery, the audiological data showed responses in the implanted ear between 45 and 65 dB at frequencies from 0.25 to 4 kHz. At the evaluation of long latency potentials, there was a decrease in latency, with values of 322 and 245 ms in the pre- and post-activation periods, respectively.
The third child was diagnosed at 1 year and 8 months after meningitis at 11 months, and used bilateral HAs for 10 months. The audiometric results with the HA in the left ear showed responses of 80 and 90 dB for frequencies of 250 and 500 Hz, respectively. Three months after surgery, the patient detected speech sounds at average intensity. The data initially showed the CAEP P1 component at 205 ms. After stimulation via CI, this component was observed at 151 ms.
The fourth child was diagnosed at 1 month of age with unknown etiology. After using bilateral HAs for six months, the child underwent CI surgery at 9 months. The results of audiometry in free field with HAs were 80 dB for the frequency of 250 Hz bilaterally. After three months of CI use, these values were between 30 and 50 dB for frequencies from 500 to 4,000 Hz in the left ear. In the evaluation of long latency potential, there was a decrease in latency, with values of 271 and 175 ms in the pre- and post-activation period, respectively.
The last child was diagnosed at 2 years of age without defined etiology of hearing loss. This child had used HAs bilaterally for one year and one month when he underwent the surgery. The audiometric results with the HA in free field showed responses in the left ear from 55 to for frequencies from 0.25 to 1 KHz. Three months after surgery, responses were observed at 50 and 60 dB for frequencies 250 and 500 Hz, respectively. The CAEP records initially showed the P1 component at 283 ms. After three months of CI use, the latency of this component was observed at 225 ms.
A decrease in the latency values of the P1 component was observed in all participants of this study after three months of stimulation via CI. The P1 latency values were closer to values found in normal hearing children of the same age, as shown in Table 3 and Fig. 1. Children from the CG were also reassessed after an interval of three months from the first evaluation; however, there were no differences in latency between the two assessments.
Discussion
Considering the maturation of the CANS in children who receive CI, this study aimed to investigate the changes in latency values of the P1 component observed in CAEP before and three months after electrode activation.
The P1 component, a positive wave generated by thalamic cortical activity upon sound stimulation, is a measure capable of reflecting changes in the CANS arising from neuronal plasticity, an essential phenomenon for the development of auditory skills and language.16., 17., 18.
In children with CI, these changes can be observed, as the electrical stimulation provides better functionality of synaptic connections with gradual increase in the rate of synaptic neural transmission and synchronization. These cortical changes allow for a gradual decrease in the latency of P1 component - a phenomenon observed in this study - corroborating the findings described in the literature that evaluated children in similar conditions.5., 16., 19., 23.
There are several published studies that suggest a rapid change of this latency time, especially in children who are early-implanted. Some authors observed that these children reached the latency values of P1 component expected for their respective age three months after implantation;5., 23. others have reported these changes between three and six months;21 other studies have shown changes after four months of CI use;22 and still others have observed changes after six to eight months.16., 19. In the latter, the results demonstrated that children who receive CI early exhibit a rapid development of CANS, with changes in waveform morphology as well as in latency of P1 component: one week after implantation, the latency of P1 decreased approximately 100 ms, generating results similar to those of normal hearing newborns, and after six to eight months of use, this value reached the normal range for children at the same age. The results also demonstrated that children who are late-implanted present abnormal waveform morphology and slow decrease in latency time.19
This reduction in latency time of the P1 component in relation to age at activation is related to the existence of a sensitive period in which the auditory stimulation should be initiated for obtaining a higher degree of clinical effectiveness. Thus, as seen in the literature, children who receive stimulation via CI before three years and five months of age quickly reach the expected values of normality. Those who receive CI later present less development of the CANS than that observed in normal hearing children.11., 19., 23., 24.
In the present study, it was not possible to follow-up the modifications of the CANS for a period exceeding three months of CI use in a larger group of children. However, a longitudinal assessment for a period exceeding 12 months, with more subjects, would demonstrate how CANS structures are modified after a longer period of CI use. It would also be possible to verify the alignment of registry parameters of the CAEP found in implanted children compared to those observed in normal hearing children of the same age.
Considering that the analysis of this component appears to be related to the results of speech perception obtained after activation of CI, the use of these electrophysiological measures, associated with behavioral assessment of auditory skills, can contribute to a better understanding of intervention results. Several studies highlight the P1 component analysis as a biomarker, which can provide information about the evolutionary process of rehabilitation when associated with behavioral tests, and, consequently, suggest prognosis.5., 16., 20., 21., 22., 25.
In this sense, the longitudinal assessment of these children is fundamental, so that the changes in the CANS of children with CI can be assessed in the long term and compared to the development of the CANS of normal hearing children. Studies with larger sample sizes and with longer observation time are necessary for a better understanding of CANS changes.
Therefore, it was verified that CAEP may be used as a biomarker for the CANS, which is able to register changes caused by electric stimulation via CI after three months of its use.
Conclusion
The results of this case-control study indicated a decrease in the P1 latency values of CAEP in children under the age of 4 years after three months of CI activation.
The values of the latency time of the P1 component from children who have used a CI for more than three months are higher than those from normal hearing children.
Funding
This study was supported by Fundação de Amparo à Pesquisa do Estado de São Paulo (FAPESP).
Conflicts of interest
The authors declare no conflicts of interest.
Footnotes
Please cite this article as: Silva LAF, Couto MIV, Tsuji RK, Bento RF, Matas CG, Carvalho ACM. Auditory pathways’ maturation after cochlear implant via cortical auditory evoked potentials. Braz J Otorhinolaryngol. 2014;80:131-7.
Study conducted at work performed in the Departament of Phisotherapy, Phonoaudiology and Occupational Therapy and in Departament of Otorhinolaryngology, Faculdade de Medicina, Universidade de Sao Paulo (FM-USP), São Paulo, SP, Brasil.
References
- 1.Mendes B.C.A., Barzaghi L. In: Tratado de audio- logia. Bevilacqua M.C., et al., editors. Santos; São Paulo: 2011. Percepção e produção da fala e deficiência auditiva; pp. 653–669. [Google Scholar]
- 2.Bento R.F., Brito Neto R., Castilho A.M., Gómez V.G., Giorgi S.B., Guedes M.C. Resultados auditivos com o IC multicanal em pacientes submetidos a cirurgia no Hospital das Clinicas da Faculdade de Medicina da Universidade de São Paulo. Rev Bras Otorrinolarin- gol. 2004;70:632–637. [Google Scholar]
- 3.Maurer J., Collet L., Pelster H., Truy E., Gallégo S. Auditory late cortical response and speech recognition in digisonic cochlear implant users. Laryngoscope. 2002;112:2220–2224. doi: 10.1097/00005537-200212000-00017. [DOI] [PubMed] [Google Scholar]
- 4.Boéchat E.M. In: Tratado de fonoaudilogia. 2nd edition. Fernandes F.D.M., Mendes B.C.A., Nava A.L.P.G.P., editors. Roca; São Paulo: 2010. Plasticidade e amplificação; pp. 160–168. [Google Scholar]
- 5.Sharma A., Tobey E., Dorman M., Bharadwaj S., Martin K., Gilley P., et al. Central auditory maturation and babbling development in infants with cochlear implants. Arch Otolaryngol Head Neck Surg. 2004;130:511–516. doi: 10.1001/archotol.130.5.511. [DOI] [PubMed] [Google Scholar]
- 6.Thai-Van H., Veuillet E., Norena A., Guiraud J., Collet L. Plasticity of tonotopic maps in humans: influence of hearing loss, hearing aids and cochlear implants. Acta Oto-Laryngologica. 2010;130:333–337. doi: 10.3109/00016480903258024. [DOI] [PubMed] [Google Scholar]
- 7.Moret A.L.M., Bevilacqua M.C., Costa A.O. IC: audição e linguagem em crianças deficientes auditivas pré-linguais. Pro-Fono Rev Atual. Cient. 2007;19:295–304. doi: 10.1590/s0104-56872007000300008. [DOI] [PubMed] [Google Scholar]
- 8.Bevilacqua M.C., Costa A.O., Carvalho A.C.M., Moret A.L.M. In: Tratado de fonoaudilogia. 2nd edition. Fernandes F.D.M., Mendes B.C.A., Nava A.L.P.G.P., editors. São Paulo; Roca: 2010. pp. 220–231. IC. [Google Scholar]
- 9.Clark G.M. Springer; New York: 2003. Cochlear implants: fundamentals & applications; p. p. 830. [Google Scholar]
- 10.Sharma A., Dorman M. Central auditory development in children with cochlear implants: clinical implications. Møller A, ed. Cochlear and brainstem implants. Adv Otorhinolaryngol. 2006;64:66–88. doi: 10.1159/000094646. [DOI] [PubMed] [Google Scholar]
- 11.Sharma A., Nash A.A., Dorman M. Cortical development, plasticity and re-organization in children with cochlear implants. J Comm Disord. 2009;42:272–279. doi: 10.1016/j.jcomdis.2009.03.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Fallon J.B., Irvine D.R.F., Shepherd R.K. Neural prostheses and brain plasticity. J Neural Eng. 2009;6:065008. doi: 10.1088/1741-2560/6/6/065008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Eggermont J.J., Ponton C.W. Auditory-evoked potential studies of cortical maturation in normal hearing and implanted children: correlations with changes in structure and speech perception. Acta Otolaryngol. 2003;123:249–252. doi: 10.1080/0036554021000028098. [DOI] [PubMed] [Google Scholar]
- 14.Kral A., Sharma A. Developmental neuroplasticity after cochlear implantation. Trends Neurosci. 2012;35:111–122. doi: 10.1016/j.tins.2011.09.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Nash A., Sharma A., Martin K., Biever A. In: Seewald R., Bamford J., editors. 2007. Clinical applications of the p1 cortical auditory evoked potential (CAEP) biomarker; pp. 43–49. [Google Scholar]
- 16.Sharma A., Dorman M., Spahr J. Rapid development of cortical auditory evoked potentials after early cochlear implantation. NeuroReport. 2002;13:1365–1368. doi: 10.1097/00001756-200207190-00030. [DOI] [PubMed] [Google Scholar]
- 17.Jang J.H., Jang H.K., Kim S.E., Oh S.H., Chang S.O., Lee J.H. Analysis of P1 latency in normal hearing and profound sensorineural hearing loss. Clin Exp Otorhinolaryn. 2010;3:194–198. doi: 10.3342/ceo.2010.3.4.194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ventura L.M.P. Dissertação de mestrado. Bauru; Faculdade de Odontologia de Bauru, Universidade de São Paulo: 2008. Maturação do sistema auditivo em crianças ouvintes normais: potenciais evocados auditivos de longa latência. 2008. [Google Scholar]
- 19.Sharma A., Dorman M., Kral A. The influence of a sensitive period on central auditory development in children with unilateral and bilateral cochlear implants. Hear Res. 2005;203:134–143. doi: 10.1016/j.heares.2004.12.010. [DOI] [PubMed] [Google Scholar]
- 20.Sharma A., Martin K., Roland P., Bauer P., Sweeney M.H., Gilley P., et al. P1 latency as a biomarker for central auditory development in children with hearing impairment. J Am Acad Audiol. 2005;16:564–573. doi: 10.3766/jaaa.16.8.5. [DOI] [PubMed] [Google Scholar]
- 21.Bauer P.W., Sharma A., Martin K., Dorman M. Central auditory development in children with bilateral cochlear implants. Arch Otolaryngol Head Neck Surg. 2006;132:1133–1136. doi: 10.1001/archotol.132.10.1133. [DOI] [PubMed] [Google Scholar]
- 22.Dorman M.F., Sharma A., Gilley P.M., Martin K., Roland P. Central auditory development: evidence from CAEP measurements in children fit with cochlear implants. J Comm Disord. 2007;40:284–294. doi: 10.1016/j.jcomdis.2007.03.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Sharma A., Gilley P.M., Martin K., Roland P., Bauer P., Dorman M. Simultaneous versus sequential bilateral implantation in young children: effects on central auditory system development and plasticity. Audiol Med. 2007;5:218–223. [Google Scholar]
- 24.Gilley P.M., Sharma A., Dorman M.F. Cortical reorganization in children with cochlear implants. Brain Res. 2008;1239:56–65. doi: 10.1016/j.brainres.2008.08.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Dinces E., Chobot-Rhodd J., Sussman E. Behavioral and electro- physiological measures of auditory change detection in children following late cochlear implantation: a preliminary study. Int J Pediatr Otorhinolaryngol. 2009;73:843–851. doi: 10.1016/j.ijporl.2009.03.002. [DOI] [PMC free article] [PubMed] [Google Scholar]