Abstract
Background
In the FULFIL trial, once-daily single-inhaler triple therapy with fluticasone furoate/umeclidinium/vilanterol (FF/UMEC/VI) resulted in reduced moderate/severe exacerbation rates and conferred significant improvements in lung function and health status in patients with chronic obstructive pulmonary disease (COPD) versus twice-daily budesonide/formoterol (BUD/FOR) dual therapy.
Methods
FULFIL was a Phase III, randomized, double-blind, double-dummy, parallel-group study. Patients ≥40 years of age with symptomatic COPD were randomized 1:1 to FF/UMEC/VI 100/62.5/25 mcg or BUD/FOR 400/12 mcg. In this post hoc analysis, patients were categorized by exacerbation history in the year prior to study entry (≥1 moderate/severe exacerbation [recent exacerbation] versus no recent exacerbation). Endpoints included annual rate of on-treatment moderate/severe exacerbations up to Week 24, annual rate of on-treatment severe exacerbations up to Week 24, change from baseline in trough forced expiratory volume in 1 second at Week 24, and change from baseline in health status as measured by St George’s respiratory questionnaire total score at Week 24.
Results
Of the 1810 patients in the intent-to-treat population, 1180 (65%) had one or more moderate/severe exacerbation in the year prior to entry, while 630 (35%) patients did not. FF/UMEC/VI versus BUD/FOR significantly reduced moderate/severe exacerbation rates in the recent exacerbation subgroup (mean annualized rate: 0.19 vs 0.29; rate ratio [95% confidence interval [CI]]: 0.64: [0.45, 0.91]; p=0.014) and numerically reduced moderate/severe exacerbation rates in the no recent exacerbation subgroup (mean annualized rate: 0.29 vs 0.43; rate ratio [95% CI]: 0.67 [0.43, 1.04]; p=0.073). Severe exacerbation rates were numerically reduced with FF/UMEC/VI versus BUD/FOR treatment across both subgroups. FF/UMEC/VI conferred significant improvements in lung function and health status versus BUD/FOR, regardless of recent exacerbation history.
Conclusion
FF/UMEC/VI reduced moderate/severe and severe exacerbation rates and improved lung function and health status versus BUD/FOR in patients with symptomatic COPD, regardless of recent exacerbation history.
Keywords: COPD, exacerbations, severe exacerbations, triple therapy, ICS/LABA
Introduction
Chronic obstructive pulmonary disease (COPD) is a preventable and treatable respiratory disease that is a leading cause of morbidity and mortality worldwide.1,2 COPD is characterized clinically by dyspnea, chronic cough and sputum production, and frequent exacerbations. Treatment strategies for COPD primarily focus on symptom management and exacerbation prevention.2
COPD exacerbations are defined as periods of worsening respiratory symptoms resulting in additional therapy.2 Exacerbations contribute to the overall disease burden experienced by patients with COPD and are associated with increased medical costs and healthcare resource utilization.3–6 In particular, severe exacerbations, defined as those requiring hospitalization, place a higher clinical and financial burden on patients and health-care systems than moderate exacerbations that do not require inpatient care.3,6 A history of an exacerbation in the prior year is a major risk factor for predicting future exacerbations.2,7,8 Recently, investigators examined the frequency and associations of exacerbations in the ECLIPSE trial over a 3-year period, and observed that the single best predictor of future exacerbations was having a recent history of exacerbations.7 In a subsequent analysis of risk factors for severe exacerbations within the ECLIPSE population, having a prior history of COPD exacerbations requiring hospital admission was associated with the highest risk of a new hospitalization for exacerbation.8
The FULFIL study evaluated once-daily fluticasone furoate/umeclidinium/vilanterol (FF/UMEC/VI) inhaled corticosteroid/long-acting muscarinic receptor antagonist/long-acting β2-agonist (ICS/LAMA/LABA) triple therapy versus twice-daily budesonide/formoterol (BUD/FOR) ICS/LABA dual therapy in patients with symptomatic COPD.9 The results indicated clinically meaningful and statistically significant improvements in lung function and health status, as well as reductions in moderate/severe exacerbation annualized rates in patients receiving FF/UMEC/VI versus those receiving BUD/FOR.9 FULFIL allowed the inclusion of a broad and generalizable patient population with COPD, including those with and without a history of exacerbations.9 In contrast, most clinical studies to date comparing triple versus dual therapies have been performed only in patient populations with a history of exacerbations.10–17 For example, patients from the TRIBUTE, TRILOGY, IMPACT and ETHOS trials were required to have a history of exacerbations in the year prior to study entry and as such were deemed at high risk of future exacerbations.12,14–16 However, similar to FULFIL, the recent KRONOS trial also included patients with and without a history of exacerbations.18,19
As history of exacerbations is one of the major risk factors for future exacerbations, we sought to investigate whether the effects of triple versus dual therapy on exacerbation outcomes in the FULFIL population were driven by patients with a recent history of exacerbations. Since severe exacerbations place a high clinical and financial burden on both patients and health-care systems, understanding treatment effects on severe exacerbation rates in the FULFIL population is of interest. Our post hoc analyses of FULFIL evaluated the efficacy of FF/UMEC/VI versus BUD/FOR on exacerbation outcomes, including severe exacerbations, in patients with and without a history of exacerbations in the year prior to study entry.
Materials and Methods
Study Design
The FULFIL trial (NCT02345161; GSK study CTT116853) was a phase III, randomized, double-blind, double-dummy, parallel-group, multicenter study comparing once-daily single-inhaler triple therapy with FF/UMEC/VI with twice daily dual therapy with BUD/FOR. The trial design has been described previously.9 Patients were randomized (1:1) to receive 24 weeks of treatment with either FF/UMEC/VI 100/62.5/25 mcg once daily via the ELLIPTA inhaler and twice-daily placebo using the Turbuhaler, or BUD/FOR 400/12 mcg twice daily via the Turbuhaler and once-daily placebo using the ELLIPTA inhaler. An extension subgroup remained on blinded treatment for up to 52 weeks.9
Study Population
Inclusion/exclusion criteria have been described previously.9 Briefly, eligible patients were ≥40 years of age with symptomatic COPD (COPD Assessment Test score ≥10) and had a forced expiratory volume in 1 second (FEV1) <50% of predicted normal values with or without a history of exacerbations in the prior year, or an FEV1 of ≥50–<80% of predicted normal values and ≥2 moderate exacerbations or ≥1 severe exacerbation in the prior year. Exclusion criteria included current diagnosis of asthma, and unresolved pneumonia or an unresolved severe COPD exacerbation within 14 days of screening. The study was conducted in accordance with Good Clinical Practice guidelines and the provisions of the Declaration of Helsinki and received approval from local institutional review boards and independent ethics committees.
Endpoints
The efficacy and safety endpoints of the FULFIL trial have been described previously.9 These post hoc analyses evaluated the following efficacy outcomes by treatment group (FF/UMEC/VI and BUD/FOR) and by exacerbation history subgroup in the year prior to study entry (≥1 moderate/severe exacerbation and no recent exacerbation): annual rate of on-treatment moderate/severe exacerbations up to Week 24, annual rate of on-treatment severe exacerbations up to Week 24, change from baseline in trough FEV1 at Week 24, and change from baseline in St George’s respiratory questionnaire (SGRQ) total score at Week 24. Moderate exacerbations were defined as those requiring treatment with antibiotics and/or oral/systemic corticosteroids, and severe exacerbations were defined as events resulting in hospitalization or death.
In the FULFIL trial, the safety endpoints included the incidence of on-treatment adverse events (AEs), serious AEs (SAEs) and AEs of special interest (AESIs) derived from Medical Dictionary for Regulatory Standardized Activity Queries. AESIs were defined a priori as AEs typically associated with the ICS, LAMA and LABA drug classes.
Statistical Analyses
The intent-to-treat (ITT) population comprised all randomized subjects, excluding those who were randomized in error. Subgroups based on exacerbation history in the year prior to study entry (ie, those with ≥1 moderate/severe exacerbation [referred to hereafter as the recent exacerbation subgroup] and those without a recent exacerbation history [referred to hereafter as the no recent exacerbation subgroup]) were derived from the ITT population.
The annualized rate of on-treatment severe exacerbations at Week 24 was evaluated using a generalized linear model assuming a negative binomial distribution. Covariates for the analysis of on-treatment severe exacerbations in the overall ITT population included treatment group, exacerbation history (0, 1, ≥2 moderate/severe exacerbations), smoking status at screening, geographical region and post bronchodilator percent predicted FEV1 on Day 1. Covariates for the analysis of on-treatment moderate/severe exacerbations and severe exacerbations by recent exacerbation subgroup included treatment group, smoking status at screening, geographical region and post bronchodilator percent predicted FEV1 on Day 1.
Change from baseline in trough FEV1 and SGRQ total score by recent exacerbation subgroup were analyzed using a repeated measures model with covariates of treatment group, smoking status at screening, geographical region, visit, baseline, baseline by visit and treatment by visit interactions.
All other analyses reported here (annualized rate of on-treatment moderate/severe exacerbations, change from baseline in trough FEV1 and change from baseline in SGRQ total score in the overall ITT population) were pre-specified and have been previously described in the original publication of the FULFIL trial results.9
Safety was summarized descriptively.
Results
Patients
The ITT population included 1810 patients (FF/UMEC/VI, N = 911; BUD/FOR, N = 899). While 1180 (65%) patients had ≥1 moderate/severe exacerbation in the year prior to study entry (FF/UMEC/VI, n = 598; BUD/FOR, n = 582), 630 (35%) patients did not (FF/UMEC/VI, n = 313; BUD/FOR, n = 317). Baseline characteristics were similar across treatment groups in the ITT population (Table 1). Baseline characteristics were also similar across treatment groups within each exacerbation history subgroup (Table 2).
Table 1.
Baseline Characteristics of the ITT Population
| Characteristics | FF/UMEC/VI (N=911) | BUD/FOR (N=899) | Total (N=1810) |
|---|---|---|---|
| Age, years, mean (SD) | 64.2 (8.6) | 63.7 (8.7) | 63.9 (8.6) |
| Female, n (%) | 233 (26) | 236 (26) | 469 (26) |
| BMI, kg/m2, mean (SD)a,b | 26.9 (5.2) | 27.0 (5.1) | 26.9 (5.1) |
| Current smokers, n (%)b | 400 (44) | 394 (44) | 794 (44) |
| Smoking history, pack-years, mean (SD) | 39.5 (21.9) | 39.2 (22.2) | 39.4 (22.0) |
| Moderate/severe exacerbations in past year, n (%) | |||
| 0 | 313 (34) | 317 (35) | 630 (35) |
| 1 | 252 (28) | 253 (28) | 505 (28) |
| ≥2 | 346 (38) | 329 (37) | 675 (37) |
| Severe exacerbations in past year, n (%) | |||
| 0 | 726 (80) | 699 (78) | 1425 (79) |
| 1 | 167 (18) | 177 (20) | 344 (19) |
| ≥2 | 18 (2) | 23 (3) | 41 (2) |
| Post-bronchodilator FEV1, % predicted, mean (SD)a | 45.5 (13.0) | 45.1 (13.6) | 45.3 (13.3) |
| SGRQ total score, mean (SD)c | 51.8 (16.3) | 50.8 (16.7) | N/A |
| Eosinophils, 109/L, mean (SD)b,d | 0.213 (0.191) | 0.213 (0.280) | N/A |
Notes: aFF/UMEC/VI n=908, BUD/FOR n=897, total n=1805. bAt screening. cFF/UMEC/VI n=904, BUD/FOR n=893. dFF/UMEC/VI n=887, BUD/FOR n=873, total n=1804.
Abbreviations: BUD, budesonide; FEV1, forced expiratory volume in 1 second; FF, fluticasone furoate; FOR, formoterol; N/A, not available; SD, standard deviation; SGRQ, St George’s respiratory questionnaire; UMEC, umeclidinium; VI, vilanterol.
Table 2.
Baseline Characteristics of the ITT Population by Recent Exacerbation Subgroup
| Characteristic | Recent Exacerbationa | No Recent Exacerbationa | ||||
|---|---|---|---|---|---|---|
| FF/UMEC/VI (n=598) | BUD/FOR (n=582) | Total (n=1180) | FF/UMEC/VI (n=313) | BUD/FOR (n=317) | Total (n=630) | |
| Age, years, mean (SD) | 64.0 (8.9) | 63.2 (9.3) | 63.6 (9.1) | 64.7 (7.9) | 64.5 (7.6) | 64.6 (7.7) |
| Female, n (%) | 170 (28) | 162 (28) | 332 (28) | 63 (20) | 74 (23) | 137 (22) |
| BMI, kg/m2, mean (SD)b,c | 27.3 (5.1) | 27.0 (4.9) | 27.2 (5.0) | 26.0 (5.2) | 26.9 (5.5) | 26.5 (5.4) |
| CAT score, mean (SD)b | 19.1 (5.1) | 19.2 (5.3) | 19.2 (5.2) | 19.3 (5.4) | 18.8 (5.1) | 19.0 (5.3) |
| Pre-bronchodilator FEV1, mL, mean (SD)d | 1373 (477) | 1353 (498) | 1364 (487) | 1044 (313) | 1032 (294) | 1038 (303) |
| Post-bronchodilator FEV1, % predicted, mean (SD)e | 49.5 (13.2) | 48.9 (14.6) | 49.2 (13.9) | 37.7 (8.2) | 38.1 (7.9) | 37.9 (8.0) |
| Eosinophil count, 109 cells/L, mean (SD)b,f | 0.212 (0.184) | 0.220 (0.333) | 0.216 (0.267) | 0.216 (0.202) | 0.199 (0.151) | 0.207 (0.178) |
Notes: aIn the year prior to study entry. bAt screening. cRecent exacerbation FF/UMEC/VI n=595, BUD/FOR n=580; total n=1175; no recent exacerbation FF/UMEC/VI n=313, BUD/FOR n=317, total n=630. dRecent exacerbation FF/UMEC/VI n=597, BUD/FOR n=582; total n=1179; no recent exacerbation FF/UMEC/VI n=312, BUD/FOR n=317, total n=629. eRecent exacerbation FF/UMEC/VI n=596, BUD/FOR n=581; total n=1177; no recent exacerbation FF/UMEC/VI n=312, BUD/FOR n=316, total n=628. fRecent exacerbation FF/UMEC/VI n=582, BUD/FOR n=560; total n=1142; no recent exacerbation FF/UMEC/VI n=305, BUD/FOR n=313, total n=618.
Abbreviations: BMI, body mass index; BUD, budesonide; CAT, COPD Assessment Test; COPD, chronic obstructive pulmonary disease; FEV1, forced expiratory volume in 1 second; FF, fluticasone furoate; FOR, formoterol; SD, standard deviation; UMEC, umeclidinium; VI, vilanterol.
Efficacy Endpoints
The number of patients experiencing on-treatment exacerbations in each exacerbation history subgroup is summarized in Table 3.
Table 3.
On-Treatment Moderate/Severe and Severe Exacerbations of the ITT Population by Recent Exacerbation Subgroup
| Recent Exacerbationa | No Recent Exacerbationa | |||||
|---|---|---|---|---|---|---|
| FF/UMEC/VI (n=598) | BUD/FOR (n=582) | Total (n=1180) | FF/UMEC/VI (n=313) | BUD/FOR (n=317) | Total (n=630) | |
| On-treatment moderate/severe exacerbations, n (%) | 58 (10) | 75 (13) | 133 (11) | 37 (12) | 51 (16) | 88 (14) |
| On-treatment severe exacerbations, n (%) | 7 (1) | 14 (2) | 21 (2) | 5 (2) | 8 (3) | 13 (4) |
Note: aIn the year prior to study entry.
Abbreviations: BUD, budesonide; FF, fluticasone furoate; FOR, formoterol; UMEC, umeclidinium; VI, vilanterol.
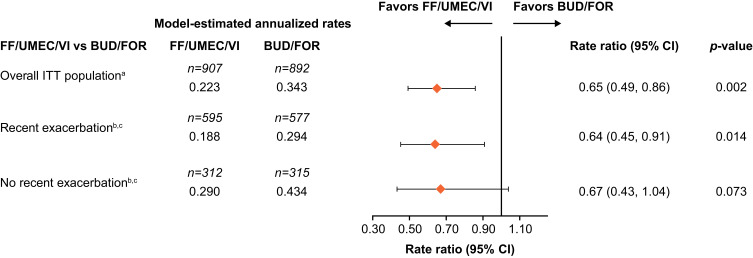
Treatment with FF/UMEC/VI significantly reduced the annualized rate of moderate/severe exacerbations up to Week 24 compared with BUD/FOR in the recent exacerbation subgroup (mean annualized rate: 0.19 vs 0.29; rate ratio: 0.64 [95% confidence interval [CI]: 0.45, 0.91]; p=0.014). There was a 33% reduction in moderate/severe exacerbation rate favoring FF/UMEC/VI over BUD/FOR in the no recent exacerbation subgroup, but this was not statistically significant (mean annualized rate: 0.29 vs 0.43; rate ratio: 0.67 [95% CI: 0.43, 1.04]; p=0.073; Figure 1).
Figure 1.
Rate of on-treatment moderate/severe exacerbations up to Week 24 by recent exacerbation subgroup. aPre-specified. bIn the year prior to study entry. cPost hoc.
Abbreviations: BUD, budesonide; CI, confidence interval; FF, fluticasone furoate; FOR, formoterol; ITT, intent-to-treat; UMEC, umeclidinium; VI, vilanterol.
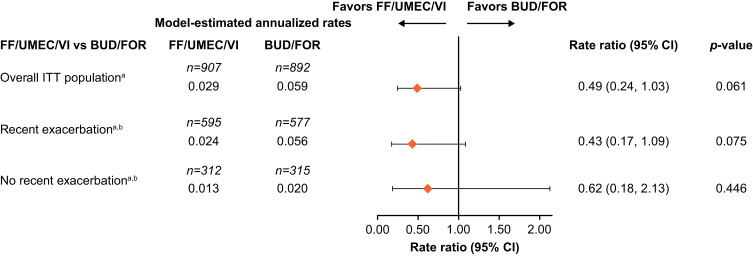
Patients receiving FF/UMEC/VI had numerically lower annualized rates of severe exacerbations in both the recent exacerbation subgroup (mean annualized rate: 0.02 vs 0.06; rate ratio: 0.43 [95% CI: 0.17, 1.09]; p=0.075) and in the no recent exacerbation subgroup (mean annualized rate: 0.01 vs 0.02; rate ratio: 0.62 [95% CI: 0.18, 2.13]; p=0.446) compared with BUD/FOR, but these differences were not statistically significant (Figure 2).
Figure 2.
Rate of on-treatment severe exacerbations up to Week 24 by recent exacerbation subgroup. aPost hoc. bIn the year prior to study entry.
Abbreviations: BUD, budesonide; CI, confidence interval; FF, fluticasone furoate; FOR, formoterol; ITT, intent-to-treat; UMEC, umeclidinium; VI, vilanterol.
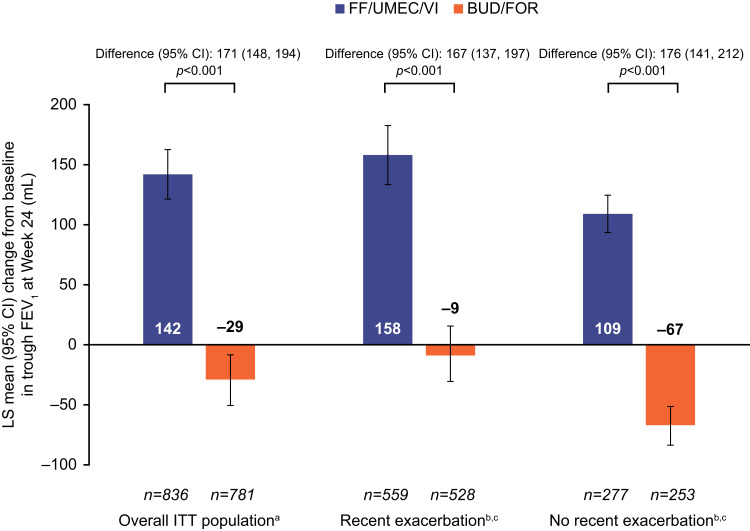
FF/UMEC/VI significantly increased trough FEV1 from baseline at Week 24 versus BUD/FOR regardless of recent exacerbation history (recent exacerbation subgroup: 167 mL [95% CI: 137, 197]; no recent exacerbation subgroup: 176 mL [95% CI: 141, 212]; p<0.001 for both comparisons; Figure 3).
Figure 3.
Change from baseline in trough FEV1 at Week 24 by recent exacerbation subgroup. aPre specified. bIn the year prior to study entry. cPost hoc.
Abbreviations: BUD, budesonide; CI, confidence interval; FEV1, forced expiratory volume in1 second; FF, fluticasone furoate; FOR, formoterol; ITT, intent-to-treat; LS, least-squares; UMEC, umeclidinium; VI, vilanterol.
SGRQ total score at Week 24 was significantly improved with FF/UMEC/VI compared with BUD/FOR in both the recent exacerbation subgroup (least squares [LS] mean change from baseline difference: −2.3 [95% CI: −3.9, −0.7]; p=0.005) and the no recent exacerbation subgroup (LS mean change from baseline difference: −2.1 [95% CI: −4.1, −0.2]; p=0.032).
Efficacy endpoints by recent exacerbation for the extension subgroup at Week 52 are presented in Supplementary Table S1.
Safety
The safety data from the FULFIL ITT population at Weeks 24 and 52 have been previously reported.9 Briefly, up to Week 24, the incidence rates of on-treatment AEs were 38.9% in the FF/UMEC/VI group and 37.7% in the BUD/FOR group. The incidence rates of on-treatment SAEs with FF/UMEC/VI and BUD/FOR were 5.4% and 5.7%, respectively. Up to Week 52, the incidence rates of on-treatment AEs were 47.6% in the FF/UMEC/VI group and 55.5% in the BUD/FOR group; the incidence of on-treatment SAEs with FF/UMEC/VI and BUD/FOR were 10.0% and 12.7%, respectively. For both time periods, the most common on-treatment AEs were nasopharyngitis and headache, and the most common on-treatment SAEs were COPD exacerbation and pneumonia. Cardiovascular effects AESIs were reported in 8.6% of patients receiving FF/UMEC/VI and 10.0% of patients receiving BUD/FOR. The reported rates of pneumonia AESIs in patients receiving FF/UMEC/VI and BUD/FOR were 2.2% and 0.8%, respectively, up to Week 24, and 1.9% and 1.8%, respectively, up to Week 52.
Discussion
This FULFIL post hoc analysis showed overall efficacy outcomes in the subgroup of patients with and without a recent exacerbation history were generally consistent with those reported in the overall ITT population.9 In the subgroup of patients with recent exacerbations, single-inhaler triple therapy with FF/UMEC/VI conferred significant improvements in moderate/severe exacerbations, lung function and health status, and numerical reductions in severe exacerbations, compared with BUD/FOR. In the subgroup of patients without recent exacerbations, FF/UMEC/VI numerically reduced the rate of moderate/severe and severe exacerbations, and significantly improved lung function and health status versus dual therapy with BUD/FOR.
The inclusion criteria of other trials comparing triple and dual therapies in patients with COPD such as TRIBUTE, TRILOGY, IMPACT and ETHOS all required patients to have a history of exacerbations in the year prior to study entry.12,14–16 Similar to the subgroup of patients with ≥1 moderate/severe exacerbation examined in this post hoc analysis of FULFIL, the populations of these studies were considered to be at high risk of future exacerbations as having a history of exacerbations in the previous 12 months has been shown to be a major risk factor for future exacerbations.2,7,8 In this analysis of the FULFIL trial, treatment with FF/UMEC/VI triple therapy compared with BUD/FOR dual therapy significantly reduced the annualized rate of moderate/severe exacerbations in patients with COPD who had ≥1 moderate/severe exacerbation in the year prior to study entry. This is consistent with the results of TRIBUTE, TRILOGY, IMPACT and ETHOS, in which significant reductions in the rates of moderate/severe exacerbations with ICS/LAMA/LABA triple therapy versus ICS/LABA and/or LAMA/LABA were observed in similar patient populations.12,14–16
In the subgroup of patients without recent exacerbations, numerical reductions of over 30% in the annualized rate of moderate/severe exacerbations were observed with FF/UMEC/VI versus BUD/FOR, suggesting that triple therapy may have a benefit in exacerbation prevention in this patient population. This reduction is most likely not statistically significant because this study was not powered to investigate any subgroups, and this particular subgroup is a relatively small sample. A formally powered study would be required to confirm this finding, although the point estimate suggests a meaningful clinical difference. The recent KRONOS study evaluated the efficacy and safety of the fixed-dose combination ICS/LAMA/LABA BUD/glycopyrrolate (GLY)/FOR versus LAMA/LABA GLY/FOR and ICS/LABA BUD/FOR.19 A post hoc analysis of KRONOS investigated whether exacerbation benefits were driven by the subset of patients who had ≥1 exacerbations in the year prior to study entry. That analysis showed that there was no difference in moderate/severe exacerbations with triple versus ICS/LABA dual therapy in the subgroup of patients without recent exacerbations (rate ratio: 0.98 [95% CI: 0.63, 1.54]; p=0.9384). However, a significant reduction in moderate/severe exacerbations with triple versus LAMA/LABA dual therapy was seen for this patient subgroup (rate ratio: 0.52 [95% CI: 0.37, 0.72]; p=0.0001). Taken together, these results suggest that the exacerbation reduction seen in the ITT population was not solely driven by patients at high risk of future exacerbations.18
Due to the high clinical and financial burden severe exacerbations place on patients and health-care systems, these analyses of FULFIL also assessed the impact of triple therapy versus ICS/LABA dual therapy on annualized rate of severe exacerbations. Numerical reductions in severe exacerbations in the range of 40% to 55% were observed with FF/UMEC/VI compared with BUD/FOR in the ITT population, and in both the with and without recent exacerbation subgroups. The post hoc analysis of the KRONOS trial also examined the effects of triple versus dual therapy on the rate of severe exacerbations in patients with and without recent exacerbations. The results showed that triple therapy did not reduce the annual rate of severe exacerbations versus ICS/LABA dual therapy in patients without recent exacerbations (rate ratio: 1.05 [95% CI: 0.36, 3.11]; p=0.9279); however, a 58% reduction in rate of severe exacerbations with triple versus LAMA/LABA dual therapy in this patient population was observed (rate ratio: 0.42 [95% CI: 0.19, 0.93]; p=0.0316).18 In KRONOS, the severe exacerbation event numbers were too small to conduct meaningful analyses in the subgroup of patients with recent exacerbations. While in FULFIL the effects of triple versus LAMA/LABA dual therapy could not be explored owing to the absence of a LAMA/LABA comparator, the findings from KRONOS18 suggest that patients without recent exacerbations may also benefit from treatment with FF/UMEC/VI triple therapy compared with dual bronchodilation therapy.
Consistent with the FULFIL ITT population, significant improvements in lung function and health status were observed with FF/UMEC/VI versus BUD/FOR, regardless of recent exacerbation status. This implies that the benefits observed in the ITT population were not solely driven by the subgroup of patients with recent exacerbations and indicates that patients without recent exacerbations also benefit from treatment with triple therapy. Similar results have also been observed in patient populations from other studies which included either patients with a recent history of exacerbations12,14,16 or with and without a history of exacerbations.18
Some limitations of these analyses should also be considered. The FULFIL trial was not specifically powered to detect a treatment difference in recent exacerbation history subgroups and these analyses were conducted post hoc. Additionally, a small number of exacerbation events were observed during the duration of the clinical trial. It would have been of interest to study whether prior medications affected the subgroups studied here. However, an analysis comprising a subgroup of subgroups would have led to small samples, potentially leading to unreliable results and therefore has not been conducted for this analysis. While differences in pre-study medication may exist between the two exacerbation subgroups, the split of prior medications at Screening and during run-in (period in which patients stayed on their pre-study medication before switching to their randomized treatment) was balanced between the two treatment groups in the primary study,9 which gives us confidence that prior medication was unlikely to have affected the treatment differences presented in this study. Nevertheless, the fact that FULFIL included patients without a history of exacerbations, who are often excluded from clinical trials investigating ICS/LAMA/LABA triple therapy, provides novel insights into this patient population. Additionally, the FULFIL population appears consistent with a real-world COPD population compared with other highly selected trial populations. A recent epidemiological study by Rothnie et al demonstrated that 26% of patients with COPD did not exacerbate during 10 years of follow-up, further indicating that patients without recent exacerbations are a sizeable proportion of the patient population in COPD.20
Conclusion
In these post hoc analyses of the FULFIL trial, FF/UMEC/VI reduced moderate/severe and severe exacerbation rates and improved lung function and health status compared with BUD/FOR in patients with symptomatic COPD, regardless of exacerbation history in the year prior to study entry. Our results highlight the potential benefits of once-daily single-inhaler FF/UMEC/VI triple therapy over twice-daily BUD/FOR dual therapy in reducing the clinical and economic burden caused by exacerbations in this patient population.
Acknowledgments
Editorial support (in the form of writing assistance, including preparation of the draft manuscript under the direction and guidance of the authors, collating and incorporating authors’ comments for each draft, assembling tables and figures, grammatical editing and referencing) was provided by Maria Guillermina Casabona, PhD, from Fishawack Indicia Ltd, part of Fishawack Health, UK, and was funded by GSK.
Funding Statement
This study was funded by GSK (CTT116853/NCT02345161). The funders of the study had a role in the study design, data analysis, data interpretation, and writing of the report.
Abbreviations
AE, adverse event; AESI, adverse event of special interest; BMI, body mass index; BUD, budesonide; CAT, COPD Assessment Test; CFB, change from baseline; CI, confidence interval; COPD, chronic obstructive pulmonary disease; FEV1, forced expiratory volume in 1 second; FF, fluticasone furoate; FOR, formoterol; GLY, glycopyrrolate; ICS, inhaled corticosteroid; ITT, intent-to-treat; LABA, long-acting β2-agonist; LAMA, long-acting muscarinic receptor antagonist; LS, least squares; SAE, serious adverse event; SD, standard deviation; SGRQ, St George’s respiratory questionnaire; UMEC, umeclidinium; VI, vilanterol.
Data Sharing Statement
Anonymized individual participant data and study documents can be requested for further research from www.clinicalstudydatarequest.com.
Ethics Approval and Informed Consent
All patients provided written informed consent. This study was conducted in accordance with the Declaration of Helsinki and Good Clinical Practice guidelines, and was approved by the relevant national, regional, or independent ethics committees or institutional review boards. A full list of the ethics committees and institutional review boards is provided in Supplementary Table S2.
Consent for Publication
All authors contributed to the writing and reviewing of the manuscript and have given final approval for the version to be published.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Disclosure
RA Panettieri has received research support from Novartis, AstraZeneca, Genentech, Optikira, Medimmune, Maven, Evelobio, Johnson & Johnson, RIFM, Equillium, Theravance, TEVA, Origo, ACTIV-1, Janssen and Vault Health; has received consulting fees from AstraZeneca, RIFM, Equillium, Bayer and TEVA; is part of the speaking bureau for Sanofi/Regeneron, AstraZeneca, Merck & Co and Genentech; and is a member of the advisory committee for AstraZeneca, Genentech, RIFM, Equillium and Theravance. CA Camargo is a member of the scientific advisory board for AstraZeneca. T Cheema is part of the speaking bureau for BI, GSK, Regeneron and AstraZeneca, and is a consultant for Noveome Biotherapeutics. S El Bayadi is a speaker for GSK, Grifols, Sanofi Genzyme Regeneron, Mylan Theravance, Janssen, Bayer, Mallinckrodt Pharmaceuticals. S Fiel is a member of Speakers Bureau Gilead. T Vila, RG Jain, D Midwinter, DA Lipson are GSK employees and hold stock/shares at GSK. B Thomashow has taken part in advisory boards for AstraZeneca, Boehringer Ingelheim and GSK and performed consulting work for GSK. A Ludwig-Sengpiel is KLB Gesundheitsforschung Lübeck GmbH managing director. ELLIPTA is owned by or licensed to the GSK group of companies. Turbuhaler is owned by or licensed to the AstraZeneca group of companies, and BUD/FOR 400/12 mcg twice-daily is not a US Food and Drug Administration-approved formulation. The authors report no other conflicts of interest in this work.
References
- 1.Foreman KJ, Marquez N, Dolgert A, et al. Forecasting life expectancy, years of life lost, and all-cause and cause-specific mortality for 250 causes of death: reference and alternative scenarios for 2016–40 for 195 countries and territories. Lancet. 2018;392(10159):2052–2090. doi: 10.1016/s0140-6736(18)31694-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Global Initiative for Chronic Obstructive Lung Disease. Global initiative for chronic obstructive lung disease. global strategy for the diagnosis, management and prevention of Chronic Obstructive Pulmonary Disease (2021 report); 2021. Available from: https://goldcopd.org/2021-gold-reports/. Accessed December 16, 2020.
- 3.Pasquale MK, Sun SX, Song F, Hartnett HJ, Stemkowski SA. Impact of exacerbations on health care cost and resource utilization in chronic obstructive pulmonary disease patients with chronic bronchitis from a predominantly Medicare population. Int J Chron Obstruct Pulmon Dis. 2012;7:757–764. doi: 10.2147/copd.s36997 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Halpin DM, Miravitlles M, Metzdorf N, Celli B. Impact and prevention of severe exacerbations of COPD: a review of the evidence. Int J Chron Obstruct Pulmon Dis. 2017;12:2891–2908. doi: 10.2147/copd.S139470 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Dhamane AD, Moretz C, Zhou Y, et al. COPD exacerbation frequency and its association with health care resource utilization and costs. Int J Chron Obstruct Pulmon Dis. 2015;10:2609–2618. doi: 10.2147/copd.s90148 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Iheanacho I, Zhang S, King D, Rizzo M, Ismaila AS. Economic burden of Chronic Obstructive Pulmonary Disease (COPD): a systematic literature review. Int J Chron Obstruct Pulmon Dis. 2020;15:439–460. doi: 10.2147/copd.s234942 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hurst JR, Vestbo J, Anzueto A, et al. Susceptibility to exacerbation in chronic obstructive pulmonary disease. N Engl J Med. 2010;363(12):1128–1138. doi: 10.1056/NEJMoa0909883 [DOI] [PubMed] [Google Scholar]
- 8.Müllerova H, Maselli DJ, Locantore N, et al. Hospitalized exacerbations of COPD: risk factors and outcomes in the ECLIPSE cohort. Chest. 2015;147(4):999–1007. doi: 10.1378/chest.14-0655 [DOI] [PubMed] [Google Scholar]
- 9.Lipson DA, Barnacle H, Birk R, et al. FULFIL trial: once-daily triple therapy for patients with Chronic Obstructive Pulmonary Disease. Am J Respir Crit Care Med. 2017;196(4):438–446. doi: 10.1164/rccm.201703-0449OC [DOI] [PubMed] [Google Scholar]
- 10.Aaron SD, Vandemheen KL, Fergusson D, et al. Tiotropium in combination with placebo, salmeterol, or fluticasone-salmeterol for treatment of chronic obstructive pulmonary disease: a randomized trial. Ann Intern Med. 2007;146(8):545–555. doi: 10.7326/0003-4819-146-8-200704170-00152 [DOI] [PubMed] [Google Scholar]
- 11.Lee SD, Xie CM, Yunus F, et al. Efficacy and tolerability of budesonide/formoterol added to tiotropium compared with tiotropium alone in patients with severe or very severe COPD: a randomized, multicentre study in East Asia. Respirology. 2016;21(1):119–127. doi: 10.1111/resp.12646 [DOI] [PubMed] [Google Scholar]
- 12.Lipson DA, Barnhart F, Brealey N, et al. Once-daily single-inhaler triple versus dual therapy in patients with COPD. N Engl J Med. 2018;378(18):1671–1680. doi: 10.1056/NEJMoa1713901 [DOI] [PubMed] [Google Scholar]
- 13.Magnussen H, Disse B, Rodriguez-Roisin R, et al. Withdrawal of inhaled glucocorticoids and exacerbations of COPD. N Engl J Med. 2014;371(14):1285–1294. doi: 10.1056/NEJMoa1407154 [DOI] [PubMed] [Google Scholar]
- 14.Papi A, Vestbo J, Fabbri L, et al. Extrafine inhaled triple therapy versus dual bronchodilator therapy in chronic obstructive pulmonary disease (TRIBUTE): a double-blind, parallel group, randomised controlled trial. Lancet. 2018;391(10125):1076–1084. doi: 10.1016/s0140-6736(18)30206-x [DOI] [PubMed] [Google Scholar]
- 15.Rabe KF, Martinez FJ, Ferguson GT, et al. Triple inhaled therapy at two glucocorticoid doses in moderate-to-very-severe COPD. N Engl J Med. 2020;383(1):35–48. doi: 10.1056/NEJMoa1916046 [DOI] [PubMed] [Google Scholar]
- 16.Singh D, Papi A, Corradi M, et al. Single inhaler triple therapy versus inhaled corticosteroid plus long-acting β2-agonist therapy for chronic obstructive pulmonary disease (TRILOGY): a double-blind, parallel group, randomised controlled trial. Lancet. 2016;388(10048)::963–973. doi: 10.1016/s0140-6736(16)31354-x [DOI] [PubMed] [Google Scholar]
- 17.Welte T, Miravitlles M, Hernandez P, et al. Efficacy and tolerability of budesonide/formoterol added to tiotropium in patients with chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2009;180(8):741–750. doi: 10.1164/rccm.200904-0492OC [DOI] [PubMed] [Google Scholar]
- 18.Martinez FJ, Ferguson GT, Bourne E, et al. Budesonide/Glycopyrrolate/Formoterol Fumarate Metered dose inhaler improves exacerbation outcomes in patients with COPD without a recent exacerbation history: a subgroup analysis of KRONOS. Int J Chron Obstruct Pulmon Dis. 2021;16:179–189. doi: 10.2147/copd.S286087 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ferguson GT, Rabe KF, Martinez FJ, et al. Triple therapy with budesonide/glycopyrrolate/formoterol fumarate with co-suspension delivery technology versus dual therapies in chronic obstructive pulmonary disease (KRONOS): a double-blind, parallel-group, multicentre, Phase 3 randomised controlled trial. Lancet Respir Med. 2018;6(10):747–758. doi: 10.1016/s2213-2600(18)30327-8 [DOI] [PubMed] [Google Scholar]
- 20.Rothnie KJ, Müllerová H, Smeeth L, Quint JK. Natural history of chronic obstructive pulmonary disease exacerbations in a general practice-based population with Chronic Obstructive Pulmonary Disease. Am J Respir Crit Care Med. 2018;198(4):464–471. doi: 10.1164/rccm.201710-2029OC [DOI] [PMC free article] [PubMed] [Google Scholar]