Abstract
People living with (PLWH) and at risk for HIV and people who use drugs (PWUD) are at heightened risk for health consequences of COVID-19 because of compromised immunity and high comorbidities. We studied their use of COVID-19 testing during the first year of the COVID-19 pandemic. Eight NIDA funded cohorts across North America in the Collaborating Consortium of Cohorts Producing NIDA Opportunities (C3PNO) administered multiple waves of a COVID-19 survey. Respondents were at least 18 years of age, half PLWH, and many active substance users. Wave one of the COVID-19 survey was May-November, 2020 and wave two October 2020-April 2021. Associations of COVID-19 testing with demographics, socio-demographics, substance use, and HIV-status were assessed. Of the 3762 responses from 2331 individuals, half reported ever COVID-19 testing (49.1 %), with 4.3 % reporting a positive test (163/3762 surveys=4.3 %) and 41.5 % of people reporting current symptoms reported having been tested. In multivariable analysis adjusting for age, sex, and cohort type associations with COVID-19 testing included African American/Black identification compared to Caucasian/white (adjusted odds ratio (AOR)= 0.68; 95 % confidence interval (CI) 0.53, 0.88); being unemployed (AOR=0.61; 95 % CI 0.51, 0.73), and living with HIV (AOR=0.76; 95 % CI0.65, 0.90). Findings from these C3PNO COVID-19 modules suggests that in the first year of the pandemic COVID-19 testing was not broadly accessed by these marginalized populations including PLWH and those unemployed. Factors associated with not testing may also parallel those for vaccination and identify populations needing better access to COVID-19 prevention.
Keywords: COVID-19 testing, People living with HIV, People who use substances, COVID-19 pandemic
1. Introduction
The COVID-19 pandemic, caused by the SARS-CoV-2 virus, took the world by surprise in early 2020 and resulted in unprecedented disruptions to normal life throughout the world as measures were put in place to control the spread of the deadly virus (Das et al., 2022, Guide, 2020). Across North America, COVID-19 swept across the United States and Canada overwhelming health services and health infrastructure as cases exploded, hospitalizations exceeded capacity, and businesses and public programs like schools were forced to shut their doors, go online, or on hiatus (Johns Hopkins Coronavirus Resource Center, 2020). The physical and social impact was enormous – death rates grew exponentially and the healthcare system was pushed to exceed capacity in the face of enormous caseloads and a virus that spread rapidly (Emanuel et al., 2020, Reese et al., 2020). As schools, clinics, social venues, and otherwise non-essential businesses shut their doors, the most vulnerable in our society including those marginally housed, those experiencing substance use and/or those with mental health issues) were even further marginalized as a result of lost services and support (Tomar et al., 2021, Rozanova et al., 2020, Usher et al., 2020, Shiau et al., 2020, Czeisler, 2020, Taylor et al., 2021, Hochstatter et al., 2021a, Green et al., 2020). Early in the pandemic, signs of increases in substance use (Czeisler, 2020) raised concerns that substance use would skyrocket (Das et al., 2022). Overdoses and particularly overdose deaths hit unprecedented levels (Haley and Saitz, 2020) and partially because of the reduced availability of emergency medical services (Slavova et al., 2020). People living with HIV (PLWH) and particularly those who are not virally suppressed, were considered to be at heightened risk for COVID-19 serious consequences because of being immunocompromised and experiencing high prevalence of comorbidities (Shoptaw et al., 2020, Mitchell et al., 2021, Karmen-Tuohy et al., 2020, Lesko and Bengtson, 2021). Among such individuals are people who use drugs (PWUD) and those with mental health problems (Taylor et al., 2021, Hochstatter et al., 2021a, Winwood et al., 2021). Therefore, understanding patterns of who did not obtain COVID-19 testing among PWUD and PLWH provides insight into how those with intersectional challenges may have experienced systematic exclusion from public health initiatives during the COVID-19 pandemic. This may shed light on strategies that may help us enhance access to testing among marginalized populations who experience health inequities in a future public health crisis.
To assess the impact of the COVID-19 pandemic among those confronting multiple challenges such as substance use and HIV, a consortium of NIDA funded cohorts entitled the Collaborating Consortium of Cohorts Producing NIDA Opportunities (C3PNO) launched a specially designed survey administered three times during the pandemic. The C3PNO COVID-19 survey module contained specific measures for PWUD and PLWH. These data provide insight into the compelling questions of change in the levels of substance use among those enrolled in the cohorts many of whom have been using long term, been in substance use treatment, and have heavy use (Starks et al., 2020, Hochstatter et al., 2021b). Moreover, the results may demonstrate the extent to which critical COVID-19 public health interventions such as testing for the virus reached PWUD and PLWH. The C3PNO consortium was uniquely positioned to identify impacts of the COVID-19 pandemic on PWUD and PLWH as its cohorts following large numbers of such individuals across North America. The analyses described herein focus on the prevalence and factors associated with COVID-19 testing among PWUD and PLWH who participated in the first two rounds of the C3PNO COVID-19 module.
2. Material and methods
2.1. Study setting and population
C3PNO was established in 2017 by the National Institute on Drug Abuse (NIDA) to enhance data sharing opportunities and mechanisms to facilitate collaborative research efforts among NIDA-supported cohorts that examine HIV/AIDS in the context of substance misuse. Details of the participating cohorts and other methodology have been previously described (Gorbach et al., 2021) but in sum, the C3PNO consortium is comprised of nine NIDA cohorts located in major cities throughout North America (Baltimore, Chicago, Los Angeles, Miami, and Vancouver) with a combined sample size of up to 12,000 active participants. Some cohorts had initial enrollment criteria that participants be people who inject drugs (PWID) while other cohorts are young men who have sex with men. The consortium links a wide range of behavioral, clinical, and biological data from diverse individuals at high-risk for HIV or living with HIV participating in the cohorts. Starting in May 2020, the consortium launched a survey to examine patterns of substance use, substance use disorder treatment, and utilization of HIV prevention and care services in the midst of the COVID-19 pandemic. Specific domains collected as part of the survey included overall impact of the COVID-19 pandemic and related governmental/societal restrictions on day-to-day life, adoption of COVID-19 prevention practices, COVID-19 testing and symptomatology, changes in substance use behaviors as well as reports of pandemic impact on access, quality, and pricing of illicit substances. The survey also included various measures of mental health including anxiety as well as access to medical care and substance use treatment. At the time of this study COVID-19 testing was available and recommended mostly for those with symptoms defined by the CDC at the time as the most predictive of COVID-19 infection including: fever, feeling feverish, chills, repeated shaking with chills, muscle aches or pain, runny nose, sore throat, new or worsening cough, shortness of breath, nausea or vomiting, headache, abdominal pain, diarrhea, and sudden loss of taste or smell. In the survey module current symptom reports were collected. Eight of the nine C3PNO cohorts participated in both of the first rounds of data collection but one was unable to share its data – all nine cohorts joined for later rounds.
Each participating cohort contacted a minimum of 200 of their cohort members to participate in the survey eligible if they: (1) were previously enrolled in one of the eight participating C3PNO cohorts; (2) participated in a recent study visit (within the preceding 12 months prior to the emergence of COVID-19); (3) were English and/or Spanish speaking; and (4) willing and able to complete the survey remotely. Cohort investigators were encouraged to enroll participants who had a recent history of substance use as determined by self-report at their most previous visit. The survey was either self-administered through a web based survey for participants that had computer and internet access or interviewer administered by telephone for those participants without online access. The survey took approximately 20 min to complete and participants were remunerated for their time. The study was approved by the institutional review boards of the consortium cohorts and each participant provided informed consent for their study participation.
There were 4035 responses to the survey across all eight cohorts that participated in both of the first two rounds and collected fully analyzable data; 3762 were available for this analysis because the Canadian cohorts confronted restrictions with sending data and were not able to be included. The analyzed data for this manuscript includes data from 2331 individuals who completed one or both of the first two rounds of the C3PNO COVID-19 module. Participants were offered participation in each round of the survey regardless of participation in first round. This resulted in 1431 (38 % of all surveys) from individuals responding to both rounds. The first round was conducted from May-November 2020 and the second round from October 2020 through April 2021. Median time between surveys for participants who completed both rounds of the survey was 4.1 months (range: 3.5–5.1 months; 5 % completed a second survey > 6 months later). The time to implement the survey was a window period starting from when the programmed survey was made available for each round (May 2020 for round 1 and October 2020 for round 2). Intervals are overlapping because some cohorts had not finished their first round when the first cohorts to implement started their second round. The survey was implemented in a very challenging time of research administration with entire components of universities shut down for months delaying aspects of survey conduct such as reviews of research and procedures for compensation. Therefore, the cohort research teams did the best they could to administer the survey when available and to reach the requested minimum number of participants and there was a range in time as to how long it took them to be able to collect data. Moreover, the implementation of the survey resulted in different timeframes required by cohort research teams to complete the data collection. Those that sent links to web-based questionnaires and had participants who were responsive to these completed the rounds relatively quickly (1–2 months). Other cohorts had many older participants who had to be interviewed by telephone (previous to COVID utilizing face to face in person interviews). These teams required much more time to reach participants and conduct the interviews. We implemented and conducted this research in a unique and challenging time in history that required some flexibility and innovations in data collection. This means because of the geographic range captured in these surveys, participants in different cities responded during different phases of the pandemic. Finally, given the burdens on the cohort staff to implement this study in addition to their other work, systematic data on refusal rates were not able to be collected.
2.2. Analytic strategy
The main outcome variable for these analyses was COVID-19 testing and was assessed via self-report. Specifically, participants were asked if they were tested for COVID-19 and if yes, if they have ever tested positive. Participants were also asked if they had symptoms of COVID-19. Participants were considered to have recent substance use if they reported using any of the following substances in the past month: methamphetamine, cocaine, heroin, fentanyl, or misused prescription opioids. Alcohol, tobacco, and cannabis use were also assessed but are not the focus of these analyses. Univariate analyses provided descriptive statistics for the sample overall and by COVID-19 testing status. Comparisons of demographics, substance use and frequency of use, as well as HIV-status by COVID-19 testing status were based on t-tests, chi-square methods, and other non-parametric tests as appropriate while adjusting for the effect of the subject (i.e., repeated measures). Factors associated with the outcome of interest were assessed using regression analysis with generalized estimating equations (GEE) in order to account for the within-subject correlations.
3. Results
Overall the C3PNO COVID-19 module achieved a sample made up of half respondents from cohorts of those who had enrolled as people who inject drugs (PWID) (n = 1196 individuals and n = 1962 surveys) and half respondents from cohorts of young men who have sex with men (MSM) (n = 1135 individuals; n = 1800 surveys). Among unique participants completing the survey (n = 2331), the median age was 39 years (interquartile range: 26–56 years) with more male (79 %) and over half identifying as Black (55 %), 25 % Hispanic/Latino, and 13 % White/Caucasian ( Table 1). Nearly half of respondents were living with HIV (42 %), 66 % reported being unemployed 5 % unstably housed, and over one third (38 %) reported food insecurity.
Table 1.
Numbers of Individuals and Surveys from Each C3PNO Cohort Completing the C3PNO COVID-19 Module and Type of Cohort (PWID or YMSM) a.
| Individuals |
Surveys |
|||
|---|---|---|---|---|
| (n = 2331) |
(n = 3762) |
|||
| n | % | N | % | |
| Cohort | ||||
| ACCESS2 | 0 | 0.0 | 0 | 0.0 |
| ALIVE | 492 | 21.1 | 748 | 19.9 |
| HEART | 147 | 6.3 | 147 | 3.9 |
| HYM | 344 | 14.8 | 586 | 15.6 |
| JHHCC | 227 | 9.7 | 427 | 11.4 |
| MASH | 330 | 14.2 | 640 | 17.0 |
| MSTUDY | 334 | 14.3 | 558 | 14.8 |
| RADAR | 457 | 19.6 | 656 | 17.4 |
| V-DUS2 | 0 | 0.0 | 0 | 0.0 |
| Cohort Typea | ||||
| YMSM | 1135 | 48.7 | 1800 | 47.8 |
| PWID | 1196 | 51.3 | 1962 | 52.2 |
*Data shared with the C3PNO Consortium from the first 2 of 3 rounds completed by the cohorts. Data was not ready for analysis from Round 3 at the time this manuscript was prepared and the Vancouver cohorts were not able to share data
YMSM = young men who have sex with men (HYM, MSTUDY, RADAR); PWID = people who inject drugs (HEART, ALIVE, JHHCC, MASH)
Substance use as defined by self-reported use of methamphetamine, cocaine, heroin, fentanyl, or misuse of prescription opioids in the past month was reported in 16 % of surveys. The most commonly reported substance was cocaine (8.6 %) followed by methamphetamine (7.2 %) (Table 1). Among those reporting substance use, 23 % (138/605) reported daily use, with the remainder using at least once, but less than daily in the preceding month (i.e., intermittent use) ( Table 2). Overall 19.4 % of participants reported participation in treatment including those reporting receiving some treatment for substance use, participating in a 12-step program, or on methadone. Missing data regarding the 12 step program participation (n = 317) suggests a potential underestimate of those in treatment and may partially help to explain low reports of substance use. Substance use treatment and methadone was reported by (13.0 %) individuals (n = 297) in 13.3 % of surveys (n = 491) which was very close to those reporting only methadone treatment. Moreover, among those who reported being in substance use treatment (n = 297), 75 % reported no substance use in the past month, with others potentially using substances at a reduced rate.
Table 2.
Substance Use Reported in the Past Month by Cohort across surveys (n = 3762 surveys).
| ALIVE | HEART | HYM | JHHCC | MASH | MSTUDY | RADAR | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| (n = 748) | (n = 147) | (n = 586) | (n = 427) | (n = 640) | (n = 558) | (n = 656) | ||||||||
| n | % | n | % | n | % | n | % | n | % | n | % | n | % | |
| Methamphetaminea | 0 | 0.0 | 39 | 6.7 | 3 | 0.7 | 5 | 0.8 | 166 | 29.7 | 24 | 3.7 | ||
| Cocaine | 40 | 5.3 | 8 | 5.4 | 52 | 8.9 | 27 | 6.3 | 77 | 12.0 | 78 | 14.0 | 40 | 6.1 |
| Heroin | 77 | 10.3 | 2 | 1.4 | 6 | 1.0 | 10 | 2.3 | 1 | 0.2 | 17 | 3.0 | 4 | 0.6 |
| Fentanyl | 25 | 3.3 | 2 | 1.4 | 3 | 0.5 | 2 | 0.5 | 3 | 0.5 | 19 | 3.4 | 3 | 0.5 |
| RX Opioids | 14 | 1.9 | 2 | 1.4 | 9 | 1.5 | 1 | 0.2 | 26 | 4.1 | 38 | 6.8 | 11 | 1.7 |
| Cannabis | 134 | 17.9 | 30 | 20.4 | 353 | 60.2 | 131 | 30.7 | 147 | 23.0 | 320 | 57.3 | 386 | 58.8 |
| Binge Drinking | 45 | 6.0 | 17 | 11.6 | 280 | 47.8 | 15 | 3.5 | 124 | 19.4 | 182 | 32.6 | 278 | 42.4 |
| Tobacco | 494 | 66.0 | 73 | 49.7 | 128 | 21.8 | 172 | 40.3 | 307 | 48.0 | 200 | 35.8 | 175 | 26.7 |
methamphetamine use not available for ALIVE
Of the 3762 responses, just under half reported being tested for COVID-19 (49.1 %). The majority reported nasal swab testing (92 %), with 19 % (n = 354) reporting an antibody blood test (among this group 230 also reported a nasal swab test). Of 2331 individuals, 448 (19 %) reported having some kind of COVID-19 test at both surveys. Testing positive for COVID − 19 (swab, antibody, or other) was reported at 163 surveys (163 / 3762 surveys = 4.3 %). COVID-19 hospitalization was reported at 24 surveys (24 / 3762 surveys = 0.64 %) that represents 6.0 % of all those who reported testing positive (data not shown). Among those completing both rounds of the survey, in the first round 36.7 % (n = 525) reported ever testing for COVID and for the second round 52.7 % (n = 448) with 28 % (n = 402) reporting testing only in the second round. Finally, across surveys, among participants with current symptoms 41.5 % report having been tested and 58.5 % report having not been tested ( Table 3). As shown in Table 2 this represents 35 % of all those surveys completed with reports by those with symptoms of COVID-19 having been tested.
Table 3.
Characteristics of Individuals who participated in COVID-19 Survey.
| Individuals |
Surveys |
|||
|---|---|---|---|---|
| (n = 2331)a |
(n = 3762)a,b |
|||
| n | % | n | % | |
| Socio-Demographics | ||||
| Age, Median(IQR) | 39 | (26–56) | 42 | (26–57) |
| Male Sex at Birth | 1678 | 79.8 | 2780 | 78.7 |
| Race/Ethnicity | ||||
| Black, non-Hispanic | 1166 | 55.7 | 1988 | 56.5 |
| Hispanic/Latinx | 522 | 24.9 | 880 | 25.0 |
| Other | 136 | 6.5 | 214 | 6.1 |
| White, non-Hispanic | 270 | 12.9 | 435 | 12.4 |
| Unemployedb | 1526 | 66.1 | 2453 | 65.8 |
| Unstable Housingc | 111 | 4.9 | 177 | 4.8 |
| Food Insecurity | 847 | 37.6 | 1334 | 36.6 |
| HIV-positive | 983 | 42.2 | 1639 | 43.6 |
| Substance Used, past month | ||||
| Methamphetamine | 147 | 8.0 | 237 | 7.2 |
| Cocaine | 190 | 8.2 | 322 | 8.6 |
| Heroin | 82 | 3.5 | 117 | 3.1 |
| Fentanyl | 38 | 1.6 | 57 | 1.5 |
| RX Opioids | 61 | 2.6 | 101 | 2.7 |
| Cannabis | 953 | 41.5 | 1501 | 40.4 |
| Binge Drinkingd | 605 | 26.0 | 941 | 25.0 |
| Tobaccoe | 985 | 42.3 | 1549 | 41.2 |
| Treatment for substance usef | 381 | 19.3 | 657 | 19.4 |
| COVID-19 | ||||
| Ever testedg | 998 | 42.8 | 1848 | 49.1 |
| Current symptomsh | 978 | 42.0 | 1328 | 35.3 |
| Ever tested positiveg | 89 | 3.8 | 163 | 4.3 |
| Ever hospitalized | 20 | 0.9 | 24 | 0.6 |
bfor those with multiple visits, socio-demographics and substance use were taken from round 1
sum may not equal due to missing data
unemployed defined as not working, no formal employment, furloughed from employment
unstable housing defined as living in shelter, transitional housing, street, vehicle, abandoned building, or group home
binge drinking defined as ≥ 4 drinks on at least one occasion if assigned female at birth, ≥ 5 drinks on at least one occasion if assigned male at birth
tobacco use defined as smoking tobacco cigarettes or vaping e-cigarettes
substance use treatment defined as receiving treatment for substance use, participating in a 12-step program and/or being on methadone or other medications for treatment of opioid use disorder
defined as a swab test for active infection, antibody test to check for previous infection, or a test other than an antibody or swab test.
defined as at least one of the following: fever, feeling feverish, chills, repeated shaking with chills, muscle aches or pain, runny nose, sore throat, new or worsening cough, shortness of breath, nausea or vomiting, headache abdominal pain, diarrhea, sudden loss of taste or smell.
Across study surveys, among PLWH fewer were tested than not tested (43 % vs. 57 %; p value<0.01). Among unemployed fewer reported testing (44 % tested v s 56 % not tested; p value<0.01) and among those reporting drug use fewer tested than not tested (46 % vs 54 %; p value=0.07). There was no difference by housing (Table 3).
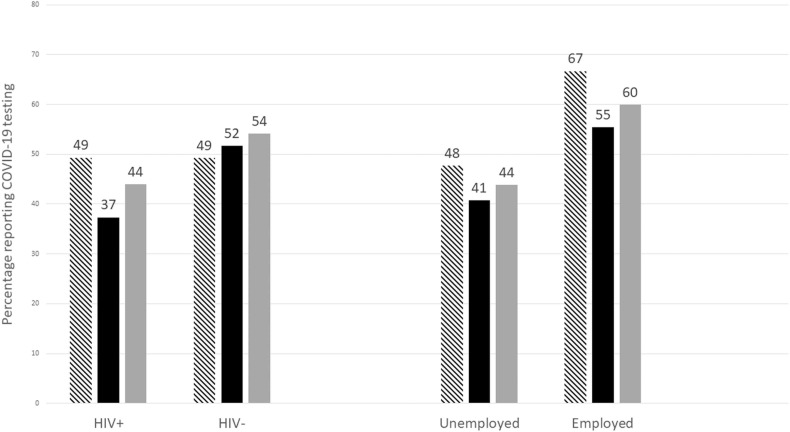
Of key interest was substance use and a greater percentage of those who were not tested for COVID-19 reported substance use in the past month (17 vs. 15 %; p value=0.09) with differences noted by frequency of substance use (p value=0.03). Specifically, while no differences in daily substance use was noted among COVID-19 testers and non-testers, the prevalence of intermittent substance use was higher among those who were not tested for COVID-19 (14 % vs. 11 %; p value=0.05). The prevalence of COVID-19 testing was significantly lower among those reporting heroin use and methamphetamine use and higher among those reporting Rx Opioid use than those not using these substances (Table 3). When substance use frequency was examined within variables significantly associated with COVID testing (HIV status and employment), the fewest tested were those who were HIV positive and unemployed who reported using substances intermittently ( Fig. 1).
Fig. 1.
COVID-19 Testing by Substance Use Frequency Across 8 C3PNO Cohorts, N = 3762 visits, Legend:  .
.
Based on multivariable analysis, after adjusting for age, sex, and cohort type the following were independently associated with COVID-19 testing: African American/Black identity had a reduced odds of COVID-19 testing as compared to those who identified as Caucasian/White (adjusted odds ratio (AOR)= 0.68; 95 % confidence interval (CI) 0.53, 0.87); those who were unemployed also had lower odds of testing (AOR=0.61; 95 % CI 0.51, 0.73) and those who were HIV-positive (AOR=0.76; 95 % CI0.65, 0.90( Table 4)). Substance use was not associated with COVID-19 testing in these models (neither frequency of use or any recent use). Interactions between HIV status and substance use and unemployment by substance use were examined and found not significant. Table 5.
Table 4.
Comparison of Substance Use and COVID-19 Testing (n = 3762 surveys)a.
| COVID-19 Test |
|||||
|---|---|---|---|---|---|
| Yes |
No |
||||
| (n = 1848) |
(n = 1914) |
||||
| n | Row % | n | Row % | P value | |
| Substance | |||||
| Methamphetamine | 108 | 45.6 | 129 | 54.4 | 0.07 |
| Cocaine | 153 | 47.5 | 169 | 52.5 | 0.44 |
| Heroin | 46 | 39.3 | 71 | 60.7 | 0.04 |
| Fentanyl | 26 | 45.6 | 31 | 54.4 | 0.51 |
| RX Opioids | 61 | 60.4 | 40 | 39.6 | 0.02 |
| Any Substance Useb | 277 | 45.8 | 328 | 54.2 | 0.07 |
| Substance Use Frequencyc | |||||
| Daily | 68 | 49.3 | 70 | 50.7 | 0.13 |
| Intermittentd | 209 | 44.8 | 258 | 55.2 | |
| Never | 1571 | 49.8 | 1586 | 50.2 | |
| Change in Substance Use Frequencyc | |||||
| Increased | 61 | 43.9 | 78 | 56.1 | 0.56 |
| Same or Less | 215 | 46.4 | 248 | 53.6 | |
| HIV-Positive | 709 | 43.3 | 930 | 56.7 | < 0.01 |
| Unemployede | 1069 | 43.6 | 1384 | 56.4 | < 0.01 |
| Unstable Housingf | 96 | 54.2 | 81 | 45.8 | 0.18 |
| Current COVID-19 symptomsg | 551 | 41.5 | 777 | 58.5 | < 0.01 |
| Ever hospitalized for COVID-19h | 24 | 100.0 | 0 | 0.0 | – |
sum may not equal due to missing data
reported use of methamphetamine, cocaine, heroin, fentanyl, and/or prescription opioids
among participants who reported using methamphetamine, cocaine, heroin, fentanyl, and/or prescription opioids (n = 602 visits)
intermittent substance use defined as weekly, less than weekly, or once in the past month
unemployed defined as not working, no formal employment, furloughed from employment
unstable housing defined as living in shelter, transitional housing, street, vehicle, abandoned building, or group home
defined as at least one of the following: fever, feeling feverish, chills, repeated shaking with chills, muscle aches or pain, runny nose, sore throat, new or worsening cough, shortness of breath, nausea or vomiting, headache abdominal pain, diarrhea, sudden loss of taste or smell.
among those reporting having been tested
Table 5.
Association of substance use and COVID-19 Testing across surveys.
| COVID-19 Test |
Bivariate Association |
Multivariable Modela |
||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Yes |
No |
OR | 95 % CI | P | aOR | 95 % CI | P | |||
| (n = 1848) |
(n = 1914) |
|||||||||
| n | Row % | n | Row % | |||||||
| Substance use frequencyb | ||||||||||
| Daily | 68 | 49.3 | 70 | 50.7 | 0.98 | (0.68, 1.42) | 0.92 | |||
| Intermittentc | 209 | 44.8 | 258 | 55.2 | 0.82 | (0.67, 1.00) | 0.05 | |||
| Never | 1571 | 49.8 | 1586 | 50.2 | 1.00 | |||||
| Any substance use (yes/no)b | 277 | 45.8 | 328 | 54.2 | 0.85 | (0.71, 1.03) | 0.09 | 0.93 | (0.76, 1.14) | 0.48 |
| Male sex at birth | 1379 | 49.6 | 1401 | 50.4 | 1.38 | (1.14, 1.67) | < 0.01 | 1.03 | (0.82, 1.29) | 0.82 |
| Age at visit (mean,sd) | 39.6 | 47.2 | 44.3 | 52.8 | 0.98 | (0.98, 0.99) | < 0.01 | 1.00 | (0.99, 1.01) | 0.51 |
| Race/Ethnicity | ||||||||||
| Black, non-Hispanic | 825 | 41.5 | 1163 | 58.5 | 0.53 | (0.42, 0.67) | < 0.01 | 0.68 | (0.53, 0.87) | < 0.01 |
| Hispanic/Latinx | 493 | 56.0 | 387 | 44.0 | 0.95 | (0.74, 1.23) | 0.7 | 0.91 | (0.70, 1.19) | 0.49 |
| Other | 119 | 55.6 | 95 | 44.4 | 0.94 | (0.65, 1.34) | 0.72 | 0.96 | (0.66, 1.41) | 0.85 |
| White, non-Hispanic | 249 | 57.2 | 186 | 42.8 | 1.00 | 1.00 | ||||
| Unemployedd | 1069 | 43.6 | 1384 | 56.4 | 0.53 | (0.45, 0.61) | < 0.01 | 0.61 | (0.51, 0.73) | < 0.01 |
| Unstable Housinge | 96 | 54.2 | 81 | 45.8 | 1.23 | (0.91, 1.68) | 0.18 | 1.37 | (0.98, 1.91) | 0.07 |
| HIV-positive | 709 | 43.3 | 930 | 56.7 | 0.66 | (0.57, 0.76) | < 0.01 | 0.76 | (0.65, 0.90) | < 0.01 |
| Cohort Type | ||||||||||
| YMSM | 992 | 55.1 | 808 | 44.9 | 1.59 | (1.37, 1.83) | < 0.01 | 0.99 | (0.70, 1.39) | 0.94 |
| PWID | 856 | 43.6 | 1106 | 56.4 | 1.00 | 1.00 | ||||
multivariable model includes any substance use, male sex at birth, age at visit, race/ethnicity, unemployed, unstable housing, HIV-positive, and cohort type
substances include methamphetamine, cocaine, heroin, fentanyl, and/or prescription opioids
Intermittent substance use defined as weekly, less than weekly, or once in the past month
unemployed defined as not working, no formal employment, furloughed from employment
Unstable housing defined as living in shelter, transitional housing, street, vehicle, abandoned building, or group home
4. Discussion
This large survey of COVID-19 testing experience among cohorts that follow people living with HIV and people who use drugs across North America provides a snapshot of how the COVID-19 pandemic in its first year may have impacted those who live on the margins of society. This sample included those among the most socially vulnerable in North America - over half were unemployed before the pandemic, about one third food insecure, many people of color almost half of whom were living with HIV. Many of these individuals are not in the formal economy that may partially explain why only half of them were tested for COVID-19 – the entry point into COVID-19 prevention (Lieberman-Cribbin et al., 2020, Martino et al., 2021, Woolhandler and Himmelstein, 2020). It is also of concern that across surveys those reporting having COVID-19 symptoms did not have higher testing rates than those who didn’t report symptoms, although the recommendation and priority for COVID-19 was testing of those symptomatic early in the pandemic when testing was limited by supply of tests. Testing continues to be a pillar of COVID-19 control; especially before vaccine availability when these surveys were implemented (Manabe et al., 2020).
Our findings show that lack of COVID-19 testing was associated with markers of social marginalization such as unemployment. As many workplaces began offering testing to their employees, this can explain why unemployed had less opportunity for testing. Fewer Black participants reported testing, and this parallels what has been seen in studies of the more general population (Lieberman-Cribbin et al., 2020, Bilal et al., 2020, Dalva-Baird et al., 2021, Rentsch et al., 2020, Muñoz-Price et al., 2020). This may be related to historical mistrust with the healthcare system and negative experiences of Black individuals with public health interventions that have previously exploited or misled them (Bogart et al., 2021).
Another key finding was that fewer PLWH reported COVID-19 testing than people HIV negative in these cohorts. That may be because our PLWH were older, more were Black, and more reported frequent substance use representing intersectional marginalization that may have kept them from accessing a COVID-19 test (Nydegger and Hill, 2020). The finding that fewer PLWH accessed COVID-19 testing suggests that COVID-19 services may have been less available in places they mostly access care such as their HIV treatment clinics because early in the pandemic there was less in-person HIV care. Moreover, it is possible that because PLWH have weakened immune systems they may been aware of their heightened vulnerability so vigilantly practiced masking and social distancing) (Waterfield et al., 2021, Mitchell et al., 2020, Iversen et al., 2020).
While the substance use reported in the month before the survey does not seem high (16 %) among cohorts of people who use drugs, it must be clarified that our study defined substance use by use of highly addictive, i.e. “hard” or street drugs such as methamphetamine, heroin, cocaine, fentanyl and prescription opioids. Use only of alcohol, tobacco and cannabis were not included in this analysis as the focus was on how the pandemic affected those who use highly addictive illicit substances that usually becomes a dominant part of their lives. Moreover, many of those who participated in this survey (13 %) reported being on treatment including methadone, and given high rates of relapse of substance use among those in treatment this suggests many in our survey were at high risk of substance use. When critical services that helped PWUD survive overdose and keep their use under control such as group therapy and MOUD became only virtual during the pandemic, the use of such services declined (Green et al., 2020, Shoptaw et al., 2020, Diaz-Martinez et al., 2021). Virtual access to care may be particularly challenging for individuals who are unemployed and older as fewer may own and have access to the technology needed for this than younger and employed people. What should also be noted is that fewest of those reporting intermittent use of substances were tested for COVID-19, with more of the daily users getting tested. This may be because reduced social interaction during the pandemic may have lessened situations in which some people use drugs (Winwood et al., 2021, Rogers et al., 2021) particularly affecting those who used at bars or parties and thereby had less exposure to COVID-19. Some substances are often use for social enhancement particularly by YMSM, and the less social opportunities the less they may have felt like or had opportunities to use drugs reflected in their COVID testing rates. The reduction in social use of substances may also reflect the high rates of overdose that were noted during the pandemic as more people may have used drugs alone without someone to help them or call for help if they did overdose (Slavova et al., 2020, Genberg et al., 2021, Appa et al., 2021). Higher testing by those reporting daily use may be because these individuals may access services such as needle exchange or MOUD and may have been offered testing through these services.5
5. Limitations
The C3PNO COVID-19 module accessed a sub-set of each cohort and likely missed those who were the most vulnerable who did not have telephones or email addresses and possibly the most drug engaged. Therefore, the sample may be biased towards those more connected with the general population. Overall 38 % of all responses were individuals who responded to both rounds of the survey. This may have been due to the timing of the surveys or the ability of the study staff to reach respondents. Additionally, because of differential access to the internet or a cell phone, not all surveys were administered in the same format. Some of the older users of opioids were those with the least ability to complete the survey as self-administered and so if they could be reached were done so for a telephone interview and that may result in systematic under reporting of substance use and other behaviors considered socially unacceptable such as not practicing COVID-19 protective behavior. While later versions of the module assess number of times tested, the first and second versions of this survey only asked about ever testing because early in the pandemic access to and availability of tests were limited. The assessment of use of COVID-19 testing was also limited because the surveys questions were about current symptoms and testing about ever use.
6. Conclusions
This C3PNO COVID-19 survey module provides insight into how during the early part of the pandemic some of the most socially vulnerable in public systems were not adequately tested for COVID-19 even if they had symptoms. Because less than half of cohort participants had been COVID-19 tested, this also suggests there is not an accurate assessment of the prevalence of COVID-19 in marginalized communities as many of them will never be counted as having COVID-19 and may subsequently perceive lower risk of acquiring it. As the most critical public health prevention for COVID-19 vaccination became available just after the second round of this survey was completed, it will be important to understand if the same factors kept PWUD and PLWH from vaccinating kept them from getting tested for COVID-19.
Funding
This work was supported by the following NIDA grants: U24DA044554; 5U01DA021525-15; U01DA036297-09; 5U01DA040325-06; 5U01DA036926-07; 5U01DA038886-07; 5U01DA040381-05; 5U01DA036267-09; 3U01DA036939-07S2; 5U01DA036935-07.
CRediT authorship contribution statement
All authors reviewed and edited the Manuscript. The following also contributed data from their studies and serve as principle investigator on them: Richard Moore, Steven Shoptaw, Brian Mustanski, Shruti H. Mehta, Gregory D. Kirk, Marianna K. Baum, M-J Milloy, Kanna Hayashi, Kora DeBeck, Michele Kipke, and Shenghan Lai). The authors Allison Rosen and Marjan Javanbakht contributed to data management, conducted the analyses, created tables and figures, and edited the manuscript, the following author was involved in the data acquisition and management: Suzanne Siminski. All authors have approved the final article.
Role of funding source
Nothing declared.
Contributors
Should always state something when more than one author.
Conflict of Interest
No conflict declared.
Acknowledgements
Optional.
References
- Appa A., Rodda L.N., Cawley C., Zevin B., Coffin P.O., Gandhi M., et al. Drug overdose deaths before and after shelter-in-place orders during the COVID-19 pandemic in San Francisco. JAMA Netw. Open. 2021;4 doi: 10.1001/jamanetworkopen.2021.10452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bilal U., Tabb L.P., Barber S., Roux A.V.D. Spatial Inequities in COVID-19 Testing, Positivity, Confirmed Cases and Mortality in 3 US Cities: an Ecological Study. Epidemiology; 2020. [DOI] [PMC free article] [PubMed]
- Bogart L.M., Ojikutu B.O., Tyagi K., Klein D.J., Mutchler M.G., Dong L., et al. COVID-19 related medical mistrust, health impacts, and potential vaccine hesitancy among black americans living with HIV. J. Acquir Immune Defic. Syndr. 2021;86:200–207. doi: 10.1097/QAI.0000000000002570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Czeisler M.É. Mental health, substance use, and suicidal ideation during the COVID-19 pandemic — United States, June 24–30, 2020. MMWR Morb. Mortal. Wkly Rep. 2020;69 doi: 10.15585/mmwr.mm6932a1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dalva-Baird N.P., Alobuia W.M., Bendavid E., Bhattacharya J. Racial and ethnic inequities in the early distribution of U.S. COVID-19 testing sites and mortality. Eur. J. Clin. Investig. 2021;51 doi: 10.1111/eci.13669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Das A., Singh P., Bruckner T.A. State lockdown policies, mental health symptoms, and using substances. Addict. Behav. 2022;124 doi: 10.1016/j.addbeh.2021.107084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Diaz-Martinez J., Tamargo J.A., Delgado-Enciso I., Liu Q., Acuña L., Laverde E., et al. Resilience, anxiety, stress, and substance use patterns during COVID-19 pandemic in the Miami adult studies on HIV (MASH) Cohort. AIDS Behav. 2021 doi: 10.1007/s10461-021-03292-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Emanuel E.J., Persad G., Upshur R., Thome B., Parker M., Glickman A., et al. Fair allocation of scarce medical resources in the time of covid-19. N. Engl. J. Med. 2020 doi: 10.1056/NEJMsb2005114. [DOI] [PubMed] [Google Scholar]
- Genberg B.L., Astemborski J., Piggott D.A., Woodson-Adu T., Kirk G.D., Mehta S.H. The health and social consequences during the initial period of the COVID-19 pandemic among current and former people who inject drugs: a rapid phone survey in Baltimore, Maryland. Drug Alcohol Depend. 2021;221 doi: 10.1016/j.drugalcdep.2021.108584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gorbach P.M., Siminski S., Ragsdale A. C3PNO investigators. Cohort profile: the collaborating consortium of cohorts producing NIDA opportunities (C3PNO) Int J. Epidemiol. 2021;50:31–40. doi: 10.1093/ije/dyaa163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Green T.C., Bratberg J., Finnell D.S. Opioid use disorder and the COVID 19 pandemic: a call to sustain regulatory easements and further expand access to treatment. Subst. Abus. 2020;41:147–149. doi: 10.1080/08897077.2020.1752351. [DOI] [PubMed] [Google Scholar]
- A. Guide to State Coronavirus Lockdowns. The Wall Street Journal 2020.
- Haley D.F., Saitz R. The opioid epidemic during the COVID-19 pandemic. JAMA. 2020;324:1615–1617. doi: 10.1001/jama.2020.18543. [DOI] [PubMed] [Google Scholar]
- Hochstatter K.R., Akhtar W.Z., Dietz S., Pe-Romashko K., Gustafson D.H., Shah D.V., et al. Potential influences of the COVID-19 pandemic on drug use and HIV care among people living with HIV and substance use disorders: experience from a pilot mHealth intervention. AIDS Behav. 2021;25:354–359. doi: 10.1007/s10461-020-02976-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hochstatter K.R., Akhtar W.Z., Dietz S., Pe-Romashko K., Gustafson D.H., Shah D.V., et al. Potential influences of the COVID-19 pandemic on drug use and HIV care among people living with HIV and substance use disorders: experience from a pilot mHealth intervention. AIDS Behav. 2021;25:354–359. doi: 10.1007/s10461-020-02976-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Iversen J., Sabin K., Chang J., Morgan Thomas R., Prestage G., Strathdee S.A., et al. COVID-19, HIV and key populations: cross-cutting issues and the need for population-specific responses. J. Int AIDS Soc. 2020;23 doi: 10.1002/jia2.25632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johns Hopkins Coronavirus Resource Center. Johns Hopkins Coronavirus Resource Center. n.d. URL: 〈https://coronavirus.jhu.edu/〉 (Accessed 24 March 2020).
- Karmen-Tuohy S., Carlucci P.M., Zervou F.N., Zacharioudakis I.M., Rebick G., Klein E., et al. Outcomes among HIV-positive patients hospitalized with COVID-19. J. Acquir Immune Defic. Syndr. 2020 doi: 10.1097/QAI.0000000000002423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lesko C.R., Bengtson A.M. HIV and COVID-19: intersecting epidemics with many unknowns. Am. J. Epidemiol. 2021;190:10–16. doi: 10.1093/aje/kwaa158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lieberman-Cribbin W., Tuminello S., Flores R.M., Taioli E. Disparities in COVID-19 testing and positivity in New York City. Am. J. Prev. Med. 2020;59:326–332. doi: 10.1016/j.amepre.2020.06.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Manabe Y.C., Sharfstein J.S., Armstrong K. The need for more and better testing for COVID-19. JAMA. 2020;324:2153–2154. doi: 10.1001/jama.2020.21694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martino R.J., Krause K.D., Griffin M., LoSchiavo C., Comer-Carruthers C., Karr A.G., et al. A nationwide survey of COVID-19 testing in LGBTQ+ populations in the United States. Public Health Rep. 2021;136:493–507. doi: 10.1177/00333549211018190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mitchell K.M., Dimitrov D., Silhol R., Geidelberg L., Moore M., Liu A., et al. Estimating the potential impact of COVID-19-related disruptions on HIV incidence and mortality among men who have sex with men in the United States: a modelling study. MedRxiv 2020:2020.10.30.20222893. https://doi.org/10.1101/2020.10.30.20222893.
- Mitchell K.M., Dimitrov D., Silhol R., Geidelberg L., Moore M., Liu A., et al. The potential effect of COVID-19-related disruptions on HIV incidence and HIV-related mortality among men who have sex with men in the USA: a modelling study. Lancet HIV. 2021;8:e206–e215. doi: 10.1016/S2352-3018(21)00022-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muñoz-Price L.S., Nattinger A.B., Rivera F., Hanson R., Gmehlin C.G., Perez A., et al. Racial disparities in incidence and outcomes among patients with COVID-19. JAMA Netw. Open. 2020;3 doi: 10.1001/jamanetworkopen.2020.21892. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nydegger L.A., Hill M.J. Examining COVID-19 and HIV: the impact of intersectional stigma on short- and long-term health outcomes among African Americans. Int. Soc. Work. 2020;63:655–659. doi: 10.1177/0020872820940017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reese H., Iuliano A.D., Patel N.N., Garg S., Kim L., Silk B.J., et al. Estimated Incidence of Coronavirus Disease 2019 (COVID-19) Illness and Hospitalization—United States, February–September 2020. Clinical Infectious Diseases 2020. https://doi.org/10.1093/cid/ciaa1780. [DOI] [PMC free article] [PubMed]
- Rentsch C.T., Kidwai-Khan F., Tate J.P., Park L.S., JTK, Skanderson M., et al. Patterns of COVID-19 testing and mortality by race and ethnicity among United States veterans: a nationwide cohort study. PLOS Med. 2020;17 doi: 10.1371/journal.pmed.1003379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rogers B.G., Tao J., Darveau S.C., Maynard M., Almonte A., Napoleon S., et al. The Impact of COVID-19 on Sexual Behavior and Psychosocial Functioning in a Clinical Sample of Men who have Sex with Men Using HIV Pre-exposure Prophylaxis. AIDS Behav 2021. https://doi.org/10.1007/s10461–021-03334–5. [DOI] [PMC free article] [PubMed]
- Rozanova J., Shenoi S., Zaviryukha I., Zeziulin O., Kiriazova T., Rich K., et al. Social support is key to retention in care during covid-19 pandemic among older people with HIV and substance use disorders in Ukraine. Subst. Use Misuse. 2020;55:1902–1904. doi: 10.1080/10826084.2020.1791183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shiau S., Krause K.D., Valera P., Swaminathan S., Halkitis P.N. The burden of COVID-19 in people living with HIV: a syndemic perspective. AIDS Behav. 2020 doi: 10.1007/s10461-020-02871-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shoptaw S., Goodman-Meza D., Landovitz R.J. Collective call to action for HIV/AIDS community-based collaborative science in the era of COVID-19. AIDS Behav. 2020;24:2013–2016. doi: 10.1007/s10461-020-02860-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Slavova S., Rock P., Bush H.M., Quesinberry D., Walsh S.L. Signal of increased opioid overdose during COVID-19 from emergency medical services data. Drug Alcohol Depend. 2020;214 doi: 10.1016/j.drugalcdep.2020.108176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Starks T.J., Jones S.S., Sauermilch D., Benedict M., Adebayo T., Cain D., et al. Evaluating the impact of COVID-19: a cohort comparison study of drug use and risky sexual behavior among sexual minority men in the U.S.A. Drug Alcohol Depend. 2020;216 doi: 10.1016/j.drugalcdep.2020.108260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taylor J.L., Ruiz-Mercado G., Sperring H., Bazzi A.R. A collision of crises: addressing an HIV outbreak among people who inject drugs in the midst of COVID-19. J. Subst. Abus. Treat. 2021;124 doi: 10.1016/j.jsat.2021.108280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tomar A., Spadine M.N., Graves-Boswell T., Wigfall L.T. COVID-19 among LGBTQ+ individuals living with HIV/AIDS: psycho-social challenges and care options. AIMS Public Health. 2021;8:303–308. doi: 10.3934/publichealth.2021023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Usher K., Bhullar N., Jackson D. Life in the pandemic: social isolation and mental health. J. Clin. Nurs. 2020 doi: 10.1111/jocn.15290. [DOI] [PubMed] [Google Scholar]
- Waterfield K.C., Shah G.H., Etheredge G.D., Ikhile O. Consequences of COVID-19 crisis for persons with HIV: the impact of social determinants of health. BMC Public Health. 2021;21:299. doi: 10.1186/s12889-021-10296-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Winwood J.J., Fitzgerald L., Gardiner B., Hannan K., Howard C., Mutch A. Exploring the Social Impacts of the COVID-19 Pandemic on People Living with HIV (PLHIV): A Scoping Review. AIDS Behav 2021. https://doi.org/10.1007/s10461–021-03300–1. [DOI] [PMC free article] [PubMed]
- Woolhandler S., Himmelstein D.U. Intersecting U.S. epidemics: COVID-19 and lack of health insurance. Ann. Intern Med. 2020;173:63–64. doi: 10.7326/M20-1491. [DOI] [PMC free article] [PubMed] [Google Scholar]