Abstract
Introduction
In order to better understand the pathophysiology of rhinosinusitis, several attempts have been made to create the disease in an animal model. Among the studied rodents each has its advantages and disadvantages. Rabbits are considered more appropriate for studies that require surgical manipulation or invasive procedures.
Objectives
To evaluate the most viable experimental model of rhinosinusitis in rabbits to be adopted in future studies.
Methods
An electronic search for studies with experimental models of rhinosinusitis in rabbits published in English and Portuguese between July of 1967 and January of 2013 was conducted in Medline, Pub Med, Cochrane, and CAPES databases, using the keywords “sinusitis”, “rabbits”, and “polyps”.
Results
A total of 256 studies were retrieved, but in accordance with the inclusion and exclusion criteria, only ten studies were selected. Many different methods of response assessment were used in these studies.
Conclusion
To date, there is no ideal experimental model for induction of acute or chronic rhinosinusitis in rabbits, but the rhinogenic model appears to be the most viable option for the continuity of studies of the disease.
Keywords: Sinusitis, Rabbits, Polyps
Resumo
Introdução
Como forma de tornar possível o entendimento da fisiopatologia da rinossinusite é fundamental a transposição da doença em animais. Os coelhos são, dentre os roedores estudados, os animais considerados mais adequados para o estudo que exija manipulação cirúrgica ou procedimentos invasivos. Cada modelo experimental tem seus pontos favoráveis e desfavoráveis.
Objetivo
Avaliar, em coelhos, o modelo experimental de rinossinusite mais viável a ser adotado em estudos futuros.
Método
Foi realizada busca eletrônica de estudos com modelos experimentais de rinossinusite em coelhos usando as palavras-chave (sinusite/coelhos/pólipos) em inglês e português nas principais bases de dados eletrônicas: Medline, PubMed, Cochrane e CAPES, publicados no período de julho de 1967 a janeiro de 2013.
Resultados
Foram encontrados 256 artigos, mas de acordo com os critérios de inclusão e exclusão apenas 10 foram selecionados. Muitos métodos distintos de avaliação de resposta foram utilizados nesses estudos.
Conclusão
Não existe, até o momento, um modelo experimental ideal para a indução de rinossinusite aguda ou crônica em coelhos, porém o modelo rinogênico parece ser a proposta mais viável para a continuidade dos estudos sobre a doença.
Palavras-chave: Sinusite, Coelhos, Pólipos
Introduction
Chronic rhinosinusitis (CRS) is one of the most common health problems in the world, with significant medical costs. According to Bhattacharyya, the cost of CRS/year per patient is around $1539 US, accounting for 4.8 days of absenteeism. In the United States, approximately 135 of every 1000 people, or 31 million individuals, are affected each year, with a total cost of $6 billion.1, 2, 3
The pathophysiology of CRS remains unclear to date, and the most accepted hypothesis is of a multifactorial chronic inflammatory disease, with probable genetic predisposition. Some related factors include: biofilms, osteitis, allergies, immune disorders, intrinsic upper airway factors, superantigens of Staphylococcus aureus, fungal colonization-induced eosinophilic inflammation, and metabolic disorders, such as hypersensitivity to acetylsalicylic acid.3 It is believed that several inflammatory patterns are involved, some of which can unfavorably influence postoperative prognosis.3, 4
In order to better understand the pathophysiology of acute and chronic rhinosinusitis, several attempts to create rhinosinusitis in animal models have been reported in the literature. Studies with rodents are the most frequent; the pathophysiology in these animals may be similar since both their anatomy and nasal physiology resemble that seen in humans.5
Among the studied rodents, rabbits, guinea pigs, and albino Wistar and Sprague-Dawley rats are the most frequent; the first is considered more suitable for studies involving surgery or other invasive procedures.5
Studies to induce an experimental model of CRS suggest maneuvers such as obliteration of nasal fossa and drainage of sinus ostia, instillation of inflammatory process mediators into the paranasal sinuses, and placement of materials that act as a culture medium in the nasal passages.6, 7 In addition to these aseptic methods, there are studies that use in vivo inoculation of infectious fungal, bacterial, and viral agents.6, 7
Each model has its favorable and unfavorable aspects. However, there is no consensus on what would be the ideal model to use in experimental studies.
This study aimed to identify the most viable experimental model of induced rhinosinusitis in rabbits to be recommended for future research on acute and chronic rhinosinusitis.
Materials and methods
Ethical considerations
This study was approved by the Ethics Committee on Animal Experimentation, Protocol No. 132/2010.
Literature search
An electronic search was conducted in major electronic databases (PubMed, Bireme, Cochrane, and CAPES) aiming to retrieve studies published from July of 1967 to January of 2013 in English and Portuguese with experimental models of induced acute and chronic rhinosinusitis, using a combination of keywords (“sinusitis”, “rabbits”, and “polyps”). The references cited in the selected studies, prior to 1967, were analyzed through active manual search.
Study selection
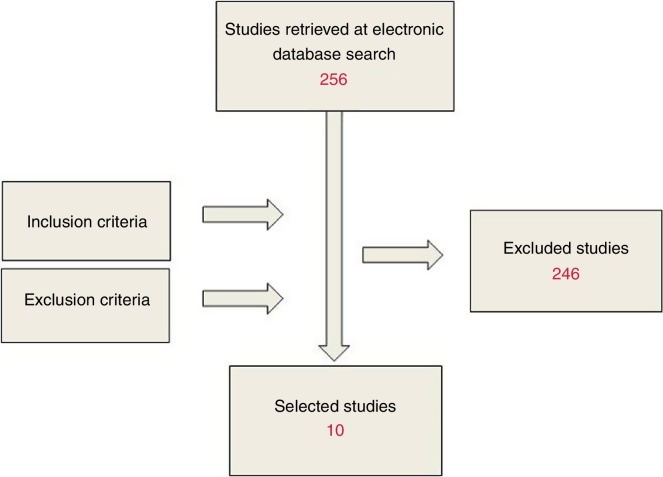
Prospective studies that included some experimental model for induction of acute or chronic rhinosinusitis with original methodology published in English and/or Portuguese were included. Publications in languages other than English or Portuguese were excluded. Studies with repeated methodologies in other publications were also excluded. A total of 256 articles were retrieved in the Medline/PudMed databases, and two were retrieved in the Lilacs database; according to the inclusion and exclusion criteria, ten studies were selected (Fig. 1).
Figure 1.
Flow chart of study selection.
Data collection
Materials and methods used in the induction of rhinosinusitis and the assessment of the response, as well as results, were analyzed and are shown below.
The selected studies assessed the response to several stimuli in the development of acute and chronic rhinosinusitis. Since the period during which the studies were published was long (1941–2010), many different methods for response assessment were found, including the macroscopic observation of the presence of secretions and/or inflammation, histological and microbiological analysis, analysis of blood flow in the tissue, and more modern techniques, such as optical and electron microscopy and endoscopy. The time period of evaluation before the development of signs of rhinosinusitis [RS (+) or absence of signs RS (−)] ranged from five days to 16 weeks.
Results
Hilding8 studied four groups, with three subjects each, and a control group, with six subjects. Group I was submitted to enlargement of the natural ostium in the maxillary sinus. In Group II, a window was created in the medial floor of the sinus; in Group III, a medial and upper window; and in Group IV, a window was created in the anterior recess of the maxillary sinus (Table 1).
Table 1.
Incidence of rhinosinusitis in the groups of the study by Hilding (1941).
| Group I: widening of natural ostium | 3 RS (+)/0 RS (−) |
| Group II: window in the medial sinus floor | 2 RS (+)/1 RS (−) |
| Group III: medial and upper window | 0 RS (+)/3 RS (−) |
| Group IV: window in the anterior recess | 0 RS (+)/3 RS (−) |
| Control | 0 RS (+)/6 RS (−) |
RS, rhinosinusitis.
Macroscopic parameters, such as patency of the created ostium and presence of secretion were analyzed. Through dissection, they sought to identify signs of mucosal inflammation and bone thickening. The windows created by enlargement of the natural ostium and near the sinus floor showed more significant inflammation than those created in the anterior and upper portions.
Maeyama9 evaluated two groups, both with 38 subjects. Group I received intradermal albumin and albumin with Staphylococcus aureus in the maxillary sinus. Group II received the same combination of Group I, but with the addition of proteolytic enzyme in the maxillary sinus (Table 2).
Table 2.
Incidence of rhinosinusites in the groups of the study by Maeyama (1981).
| Group I: albumin + Staphyloccocus aureus | RS (+) |
| Group II: albumin + Staphyloccocus aureus + proteolytic enzyme | RS (−) |
RS, rhinosinusitis.
In this report, macroscopic analysis was conducted after two weeks and, with the aid of optical microscopy, the presence of eosinophilic infiltration, goblet cells, and overall degree of epithelial degeneration were also assessed. Electron microscopy was used to analyze the degeneration of the ciliary layer.
According to the assessed parameters, there were signs of acute disease in the maxillary sinus samples from Group I, but the administration of proteolytic enzyme in Group II decreased macroscopic and cellular damage, suggesting that the greater the amount of proteolytic enzymes, the greater the damage reduction.
Drettner et al.10 analyzed the association between bacterial inoculation and occlusion of the natural ostium in the maxillary sinuses in four distinct groups. Group I (n = 17) received type 3 Pneumococcus and subsequently underwent maxillary sinus occlusion. Group II (n = 10) received type 3 Pneumococcus and Pseudomonas aeruginosa, and, subsequently, underwent maxillary sinus occlusion. Group III (n = 12) received type 3 Pneumococcus, without sinus occlusion, and Group IV (n = 25) underwent isolated sinus occlusion (Table 3).
Table 3.
Incidence of rhinosinusitis in the groups of the study by Drettner et al. (1987).
| Group I: pneumococcus type 3 and occlusion of maxillary sinus | RS (+) |
| Group II: pneumococcus type 3, Pseudomonas aeruginosa and sinus occlusion | RS (+) |
| Group III: pneumococcus type 3 without sinus occlusion | RS (−) |
| Group IV: isolated occlusion of the maxillary sinus | RS (+) |
RS, rhinosinusitis.
Macroscopic appearance, histology, and blood flow were evaluated five days after the initial procedures. Bacteria were found in all groups, even in Group IV, which was not inoculated with bacteria. Signs of sinus pathology were present in all samples that underwent sinus occlusion, but in none without the occlusion. Therefore, the association of inflammation with procedures that occluded the sinus ostium was higher than that of the non-occlusion procedure.
Hinnie et al.11 performed early assessment of the maxillary sinus after natural ostium occlusion. They compared the inoculation of bacteria and isotonic saline solution into the maxillary sinus. They used four groups with five subjects each. Group I was submitted to the introduction of isotonic saline prior to sinus occlusion, Group II was inoculated with Streptococcus pneumoniae, Group III with Haemophilus influenzae, and Group IV with P. aeruginosa.
Using electron microscopy they analyzed ciliary motion and hair cell destruction. Saline solution, even when associated with sinus occlusion, did not induce functional loss of ciliary motion or tissue injury as did the samples inoculated with bacteria.
Marks12 introduced a polyvinyl sponge impregnated with pathogenic bacteria (S. pneumoniae) in the nasal cavity of rabbits; a combination of macroscopic and bacteriological analysis was performed one to ten weeks after this procedure. Signs of inflammation in sinusal mucosa were found in 83% of histological samples and in over 50% of the cases, bacteria were identified after one week. The inflammatory response was greater in the first two weeks of the experiment, and the control group showed no significant alterations (Table 4).
Table 4.
Incidence of rhinosinusitis in the groups of the study by Marks (1997).
| Group I: polyvinyl sponge + S. pneumoniae | 83% RS (+) |
| Group II: control (no sponge) | RS (−) |
RS, rhinosinusitis.
Cetin et al.13 also used a model of polyvinyl introduction in the nasal cavity of rabbits, and employed five-inch long catheters of two different diameters (8 and 12 mm French). The authors studied two groups through macroscopic, histological, tomographic, and bacteriological analysis at one, two, and four weeks (Table 5).
Table 5.
Incidence of rhinosinusitis in the groups of the study by Cetin et al. (2002).
| Group I: catheter 12 Fr. | 8 RS (+)/1RS (−) |
| Group II: catheter 8 Fr. | 5 RS (+)/4 RS (−) |
RS, rhinosinusitis; Fr., French.
Escherichia coli was the most commonly found microorganism in the first week, but other pathogens, such as P. aeruginosa, Proteus sp., and Enterococcus sp., appeared in subsequent weeks. Macroscopic findings were correlated with computed tomography (CT) findings in all cases. High rates of a severe inflammatory response were observed with the rhinogenic model. The number of positive samples was greater with the larger diameter catheter.
Dufour et al.14 tried to induce the development of fungal sinusitis in the maxillary sinus, by the inoculation of Aspergillus fumigatus into three groups of animals. In Group I (n = 10), only the fungus was inoculated; in Group II (n = 10), mucosal damage was induced and the fungus was inoculated in the injured area; and in Group III (n = 17), the fungus was inoculated and the drainage ostium was occluded (Table 6).
Table 6.
Incidence of rhinosinusitis in the groups of the study by Dufour et al. (2005).
| Group I: A. fumigatus | RS (−) |
| Group II: A. fumigates + mucosal lesion | RS (+) 20% |
| Group III: A. fumigates + sinus occlusion | RS (+) 57% |
RS, rhinosinusitis.
The evaluation was performed through bacteriological, mycological, endoscopic, and histological analysis 30 days after the initial procedure. Samples inoculated with fungus alone did not show the same results of the inoculated samples that were submitted to mucosal injury or sinusal ostium occlusion, which showed positivity rates of 20% and 57%, respectively.
Costa et al.5 studied four groups of rabbits, each with five subjects. Procedures were performed to elicit an inflammatory response in one of the maxillary sinuses, and the contralateral sinus was used as a control. In Group I, a section of sponge bath was introduced into the nasal cavity; in Group II, cyanoacrylate was instilled in the infundibulum for occlusion of the maxillary sinus ostium; in Group III, the peripheral blood of the animal itself was percutaneously manipulated in the maxillary sinus; and in Group IV, a preparation of staphylococcal and streptococcal toxoid was used (Table 7).
Table 7.
Incidence of rhinosinusitis in the groups of the study by Costa et al. (2007).
| Group I: bath sponge | RS (+)/intense inflammation |
| Group II: cyanoacrylate | RS (+)/moderate inflammation |
| Group III: peripheral blood | RS (+)/slight inflammation |
| Group IV: toxoids | RS (+)/slight inflammation |
| Maxillary sinuses – controls | RS (−) |
RS, rhinosinusitis.
After 15 days, the presence of histological signs of inflammation was assessed. Significant results were observed in all groups, except the control, but the most intense inflammation was found in the samples submitted to sponge bath introduction into the nasal cavity.
Liang et al.15 introduced Merocel® sponge (Medtronic, Xomed) in one of the nasal cavities of two groups of rabbits for a period of two weeks. In Group I, Merocel® was introduced into one of the nasal cavities; the opposite side was left unaltered as a control. In Group II, the same protocol was performed after each nasal cavity had been treated with phorbol myristate acetate (PMA), a biologically active compound capable of activating protein kinase C and altering cell permeability. The authors used macroscopic, endoscopic, CTm and microbiological analysis at 12 and 16 weeks (Table 8).
Table 8.
Incidence of rhinosinusitis in the groups of the study by Liang et al. (2008).
| Group I: Merocel® | RS (+) 50% |
| Group II: Merocel® + PMA | RS (+) 60–70% |
| Control group: contralateral maxillary sinuses | RS (+) 16% |
PMA, phorbol myristate acetate.
The presence of Merocel® induced signs of an inflammatory response in 50% of samples that received no PMA and up to 70% of those that received it. Only 16% of the control paranasal sinuses showed an inflammatory response. Between the 12th and 16th weeks, the authors initiated treatment with intravenous ceftriaxone randomized to half of the rabbits showing signs of rhinosinusitis. Those that received treatment showed signs of resolution of the clinical picture compared to those that did not receive ceftriaxone (p = 0.00043), demonstrating treatment efficacy.
Sejima et al.16 evaluated four groups of animals and proposed a model for induction of eosinophilic polyps. Group A was a control group and consisted of four rabbits (n = 4), whereas Groups B–D had six rabbits each. In that study, the rabbits from Groups B–D were sensitized by subcutaneous injection of ovalbumin (OVA) on days 0 and 7; on day 14, they were submitted to a surgical procedure to occlude the drainage ostium of the maxillary sinus. Two weeks after obstruction of the ostium, they once more received ovalbumin directly into the maxillary sinuses, three times a week for two weeks, followed by injection of saline solution in Group B; saline with 40 μg/mL of valine-glycine-serine-glutamic acid (VGSG) was injected in Group C; and saline solution with poly-l-arginine (PLA) was injected in Group D, all three times a week for four weeks (Table 9).
Table 9.
Incidence of rhinosinusitis in the groups of the study by Sejima et al. (2010).
| Group A: control | Polyp 0% |
| Group B: sensitization (OVA) + saline solution | Polyp 0% |
| Group C: sensitization (OVA) + VGSG | Polyp 33% |
| Group D: sensitization (OVA) + PLA | Polyp 50% |
OVA, ovalbumin; VGSG, valine-glycine-serine-glutamic acid; PLA, poly-l-arginine.
Twenty-four hours after the last administration of polyp-inducing agents, the rabbits were euthanized for histopathological assessment of the left maxillary sinus mucosa using hematoxylin and eosin; the right maxillary sinus mucosa was subjected to genetic assessment. It was observed that Groups A and B did not exhibit polyp formation; large polyps were observed in two of the six rabbits in Group C, and middle-sized polyps were observed in three rabbits from Group D.
Groups C and D showed a significantly increased number of eosinophils in the mucosa with Group D exhibiting more eosinophils than Group C. A thickened lamina propria of the animals in Group D compared to Groups A and B was also noted, but it was not significantly different than that of the animals of Group C. Thus, the authors created an experimental model for induction of eosinophilic polyps that may be appropriate for the study of chronic rhinosinusitis in humans.
Discussion
The current difficulty in understanding the pathophysiology of chronic rhinosinusitis is evident. Potential pathological agents and several other causal factors are described in the literature every day, making the study of new therapeutic alternatives crucial. Studies on new drugs are extremely important and need reliable experimental models.
The analysis of some of the main studies on experimental models published over the years allowed us to make several observations. Perhaps due to the technical difficulties inherent in the long-term animals research, most of these studies present models of acute rhinosinusitis, and only the study by Sejima et al.16 for the induction of eosinophilic polyps in maxillary sinus of rabbits had a longer time frame. However, their methodology was extremely difficult and the authors used only a small number of animals in the groups that successfully induced polyp formation.
The analysis also discovered only two main alternatives to induce sinusitis in rabbits, each with its advantages and disadvantages. The first consisted of introducing cultures of bacteria, fungi, or other inducing agents in the paranasal sinuses by percutaneous injection, or through a surgical procedure with the opening and exposure of the mucosa and subsequent inoculation of infectious agents. In some cases, this procedure was associated with occlusion of the drainage ostium of the paranasal sinuses.
The occlusion of sinuses inoculated with bacteria or fungi was a superior method compared to the isolated pathogen inoculation,10, 12, 14 therefore confirming that alterations of the nasal fossa and its communication with the paranasal sinuses have a decisive role in the origin of rhinosinusitis.
The studies that performed early analyses, such as the study by Hinni,11 did not clearly demonstrate the superiority of a particular method of sinus occlusion. Perhaps the processes that characterize the development of rhinosinusitis in occluded sinuses require a longer time of exposure to the stimulus.
The second method, termed “rhinogenic rhinosinusitis”, is generated by the introduction of foreign bodies in the nasal cavities of rabbits. This method, as it routinely occurs with foreign bodies in the nasal cavities of children, was responsible for the appearance of abundant purulent rhinorrhea in most samples in the evaluated studies. Obstruction of the nasal cavity and formation of purulent secretion resulted in nasal sinus involvement.5, 12, 13, 15
Bath sponges, fragments of polyvinyl, cyanoacrylate, and even Merocel® catheters were among the materials used. They were positioned in many different ways, both with total occlusion of the nasal cavity, as well as placement restricted to the infundibular region. Foreign bodies were highly effective in inducing the onset of signs of inflammation and rhinosinusitis.
Both methods propose an intervention in sinonasal physiology of rabbits, but the rhinogenic model was shown to be more practical and easier to perform. The high response rates with intense inflammation5 suggest a high reproducibility of the method, a very desirable factor in experimental models.
Standardization of the technique to introduce the foreign material, as well as the dimensions and the exposure time, are the next steps to be taken in order to attain a reliable and easily reproducible experimental model; this will facilitate important advances in rhinosinusitis research and better comparison parameters between studies.
The removal of material from the rabbit maxillary sinus for post-study examination is a simple procedure, especially with the use of decalcification and paraffin-block embedding.16 The rhinogenic method reversibility procedure performed by Liang et al.15 presents the possibility of using it to study new drugs.
The model of pathogen introduction and complementary procedures, such as mucosal lesions or occlusion of drainage ostia, has the advantage of allowing the study of specific pathogens. However, the need for surgical violation of the sinuses to introduce the pathogens constitutes a major disadvantage, since it can influence inflammatory response-inducing factors. The rhinogenic models (introduction of foreign bodies into the nasal cavities) are less expensive, require less complex laboratory facilities, and do not depend on invasive procedures to be performed. Moreover, they are more easily implemented and are highly reproducible.
Conclusion
To date, there is no ideal experimental model to induce acute or chronic rhinosinusitis in rabbits, but the rhinogenic model appears to be the most viable proposal for the continuation of studies on the disease, based on our literature review.
Conflicts of interest
The authors declare no conflicts of interest.
Footnotes
Please cite this article as: Perez AC, Buzatto GP, Dantas IP, Dorgam JV, Valera FC, Tamashiro E, et al. Review of experimental models: sinusitis in rabbits. Braz J Otorhinolaryngol. 2014;80:435–40.
Institution: Faculdade de Medicina de Ribeirão Preto da Universidade de São Paulo, Ribeirão Preto, SP, Brazil.
References
- 1.Benninger M.S., Ferguson B.J., Hadley J.A., Hamilos D.L., Jacobs M., Kennedy D.W., et al. Adult chronic rhinosinusitis: definitions, diagnosis, epidemiology, and pathophysiology. Otolaryngol Head Neck Surg. 2003;129:S1–S32. doi: 10.1016/s0194-5998(03)01397-4. [DOI] [PubMed] [Google Scholar]
- 2.Bhattacharyya N. The economic burden and symptom manifestations of chronic rhinosinusitis. Am J Rhinol. 2003;17:27–32. [PubMed] [Google Scholar]
- 3.Fokkens W., Lund V., Mullol J., European Position Paper on Rhinosinusitis and Nasal Polyps group European position paper on rhinosinusitis and nasal polyps 2007. Rhinol Suppl. 2007;20:1–136. [PubMed] [Google Scholar]
- 4.Voegels R.L., de Melo Padua F.G. Expression of interleukins in patients with nasal polyposis. Otolaryngol Head Neck Surg. 2005;132:613–619. doi: 10.1016/j.otohns.2005.01.014. [DOI] [PubMed] [Google Scholar]
- 5.Costa H.O., Ruschi e Luchi G.E., Augusto A.G., Castro M., de Souza F.C. Comparative study of several sinusitis experimental modelling techniques in rabbits. Braz J Otorhinolaryngol. 2007;73:627–631. doi: 10.1016/S1808-8694(15)30122-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Schenkel E.P., Simões C.M.O., Mengue S.S., Mentz L.A., Irgang B.E., Stehmann J.R. O espaço das plantas medicinais e suas formas derivadas na medicina científica. Cad Farm. 1985;1:65–72. [Google Scholar]
- 7.Krouse J.H., Krouse H.J. Patient use of traditional and complementary therapies in treating rhinosinusitis before consulting an otolaryngologist. Laryngoscope. 1999;109:1223–1227. doi: 10.1097/00005537-199908000-00007. [DOI] [PubMed] [Google Scholar]
- 8.Hilding A.C. Experimental sinus surgery: effects of operative windows on normal sinuses. Ann Otol Rhinol Laryngol. 1941;50:379–392. [Google Scholar]
- 9.Maeyama T. A study of experimental sinusitis in rabbits. Auris Nasus Larynx. 1981;8:87–97. doi: 10.1016/s0385-8146(81)80005-3. [DOI] [PubMed] [Google Scholar]
- 10.Drettner B., Johansson P., Kumlien J. Experimental acute sinusitis in rabbit. A study of mucosal blood flow. Acta Otolaryngol. 1987;103:432–434. [PubMed] [Google Scholar]
- 11.Hinni M.L., McCaffrey T.V., Kasperbauer J.L. Early mucosal changes in experimental sinusitis. Otolaryngol Head Neck Surg. 1992;107:537–548. doi: 10.1177/019459989210700405. [DOI] [PubMed] [Google Scholar]
- 12.Marks S.C. Acute sinusitis in the rabbit: a new rhinogenic model. Laryngoscope. 1997;107:1579–1585. doi: 10.1097/00005537-199712000-00001. [DOI] [PubMed] [Google Scholar]
- 13.Cetin C.B., Kara C.O., Colakoglu N., Sengul M., Pinar H.S. Experimental sinusitis in nasally catheterised rabbits. Rhinology. 2002;40:154–158. [PubMed] [Google Scholar]
- 14.Dufour X., Kauffmann-Lacroix C., Goujon J.M., Grollier G., Rodier M.H., Klossek J.M. Experimental model of fungal sinusitis: a pilot study in rabbits. Ann Otol Rhinol Laryngol. 2005;114:167–172. doi: 10.1177/000348940511400215. [DOI] [PubMed] [Google Scholar]
- 15.Liang K.L., Jiang R.S., Wang J., Shiao J.Y., Su M.C., Hsin C.H., et al. Developing a rabbit model of rhinogenic chronic rhinosinusitis. Laryngoscope. 2008;118:1076–1081. doi: 10.1097/MLG.0b013e3181671b74. [DOI] [PubMed] [Google Scholar]
- 16.Sejima T., Kajiwara D., Kikuchi H., Imayoshi S., Yamauchi T., Ichimura K. Experimentally induced eosinophilic polyps in rabbit sinuses. Am J Rhinol Allergy. 2010;24:341–347. doi: 10.2500/ajra.2010.24.3519. [DOI] [PubMed] [Google Scholar]