Abstract
Introduction
The average length of stay of a fast-track area of a large urban hospital was excessively long, which affected the patient experience and the rate at which patients left without being seen. One approach to reducing average length of stay is to create nurse standard work. Nurse standard work was a defined set of process and procedures that reduce variability within a nurse’s workflow.
Methods
Nurse standard work was created by a team of nurses assisted by management engineering using lean methodology and A3 problem solving. Data were gathered about average length of stay and left without being seen for patients in the emergency department fast-track area of an urban emergency department from October 2018 to June 2020. This period includes 5 months before the intervention start, 4 months during nurse standard work implementation, 9 months using nurse standard work before the unit was repurposed during COVID-19, and 3 months during COVID-19.
Results
Nurse standard work helped reduce average length of stay in the emergency department fast-track area from 205 minutes before project initiation to 150.4 minutes in the 7 months after implementing nurse standard work. The time spent walking for supplies was reduced from 422 and 272 seconds before nurse standard work to 25 and 30 seconds for the nurse technician and nurse, respectively, after nurse standard work. Left without being seen was decreased from 4.7% in October of 2018 to 0.7% by March of 2020.
Discussion
Nurse standard work reduced the amount of time that nurses spent performing support tasks and reduced delays in providing patient care, which then allowed more time for nurses to interact directly with patients. Nurse standard work provides a clear task sequence that eliminates delays in treating patients, but it also allows for fast identification of delays that do occur and simplifies problem solving to eliminate reoccurrence of delays. Therefore, nurse standard work is an essential component of efforts to reduce patient average length of stay in health care processes and reduce left without being seen to the national standard of less than 2%.
Key words: Nurses, Quality improvement, Emergency service, Problem solving, Standard work, Lean processes, Throughput improvement
Contribution to Emergency Nursing
-
•
This paper investigates how to create and maintain nurse standard work, which is essential to maintaining a lean value stream. Nurse standard work in the fast-track area of an emergency department helped to decrease the length of stay of fast-track patients. Management was able to maintain the use of nurse standard work through the use of daily audits of whether the staff were following the standard work procedures.
-
•
Recommendations are that nurses, who perform the care process, should be engaged in the creation and maintenance of nurse standard work.
Introduction
Overcrowding is an important issue in emergency departments across the United States1 due to more patients seeking medical care through the emergency department and hospitals operating close to capacity, which creates lengthy patient wait times.2 These long waits both negatively affect patient satisfaction and increase stress for staff,3 which previous research about fast-track areas serving low-acuity patients (ie, emergency severity index [ESI] 4 or 54) found decreases patient waiting and average length of stay (ALOS), which then decreases left without being seen (LWBS) and increases patient satisfaction.5 Creating a fast track is one of the most implemented approaches to increase ED capacity and reduce ED overcrowding.6
Problem Addressed
The fast-track area of the emergency department had a patient ALOS of 205 minutes in August 2018, which contributed to a crowded ED waiting room. Management created a “lean team” made up of project engineers (with previous lean experience) and ED leadership to implement lean in the fast-track area to reduce ALOS. After an initial investigation, this lean team determined that there was variance in how nursing tasks were performed, which contributed to patient waiting. The lean team then created a team of nurses whose charge was to establish standard work for the nurse’s workflow. The target goal was to achieve and maintain an average ALOS of 162 minutes. This target was set, because it allowed fast track to meet the average demand plus 1 standard deviation (SD).
Background
Standard work improves customer response time in several ways. Standard work helps to stabilize the system, which then allows managers to determine whether there is adequate capacity available to meet demand. Standard work also creates clear goals for employees and provides a baseline for further improvement.7 These characteristics of standard work make it a valuable tool to increase cost-effectiveness and productivity.8, 9, 10 Standard work is also valuable in health care,11, 12, 13, 14, 15, 16, 17 but although the need for standard work practices such as nurse standard work (NSW) is recognized,18 , 19 there has been no detailed explanation of how to achieve and, importantly, maintain NSW.13 , 20
Although standard work does not require that 1 patient at a time be processed, 1 tool of lean operations to improve patient flow is to ensure that each step of work is done for only 1 patient at a time, a batch size of 1.21 Organizing work into batches increases the average waiting time22 and creates spikes of work within the process that leads to further delays.23
NSW is not a clinical pathway, which is a standard set of clinical protocols for disease treatment,24 but it is a standard sequence of repeatable steps performed by nurses that facilitates patient flow and improves quality.25 In general, standard work for any process consists of 3 elements: (1) takt time, (2) sequence of tasks to be performed, and (3) standard inventory needed in the workplace that are then listed on a standard work sheet.26 , 27 Takt time is the time available to complete the work divided by patient demand (time available/[number of patients/hr]). Takt time states the amount of time within which the standard work needs to be completed. The task sequence is established by observing work as performed to determine the best task sequence to complete all tasks within takt time. To perform tasks within the takt time requires that all necessary supplies be available, so the third standard work component is a list of needed supplies. Standard work improves performance in 3 ways. First, takt time sets a baseline performance level required for the system to serve all the patients. Second, establishing a standard task sequence that can be performed within takt time ensures that the most efficient practice is known and is shared with all nurses. Third, identifying required supplies and setting par levels for them eliminates delays and interruptions when the nurse is doing their work. Hence, NSW can simplify nursing tasks by ensuring that the nursing tasks can actually be performed as designed so nurses are not constantly working around process problems,28 which reduces variability to ensure consistent care for all patients. NSW is effective, because it increases task performance predictability and allows staff to quickly recognize what tasks are done and undone. Eliminating the need to search for what to do next frees up staff cognitive resources29 and simplifies task performance, which allows time for nurses to respond flexibly to patients' heterogeneous needs.17
Purpose
The project’s goal was to create and then maintain NSW to support a lean improvement project in a large urban emergency department. The NSW project team used the A3 standard problem-solving approach as a guide to creating NSW to reduce patient ALOS. This report includes an explanation of how NSW was created using the A3 process and the importance of daily managerial audits of NSW compliance used to sustain the gains in ALOS. We also report about a secondary outcome of reduced LWBS rate.
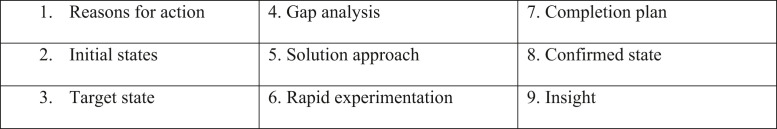
There are multiple standard problem-solving methods in use, but one characteristic they share is that they operationalize the scientific method by creating a set of steps for the team to follow. This team used the A3 problem-solving method, which divides the plan-do-study-act improvement method into smaller steps.30 The A3 9 block format used to establish NSW is shown in Figure 1 . The A3 directs the team to perform each of these steps in sequence and to focus its effort on tasks (e.g., the specified step in the template) that lead to problem solution. As standard procedure in A3 problem solving, the NSW team shared its progress with others weekly. It posted the updated A3 on a white board outside the ED nurse lunchroom.
Figure 1.
A3 Standard 9 Block Format.
Ethical Considerations
This research was determined to be exempt by the hospital institutional review board, because the research did not involve human subjects research. None of the participants had a conflict of interest.
Methods
This study was done in a large academic level I trauma center in the southeastern United States that treats more than 100,000 patients annually in the 102 beds in a pediatric and adult emergency department. Three nurses, a nursing assistant manager, a nurse educator, a nurse technician, and a project engineer comprised the group for the NSW project. The NSW project was part of a larger lean implementation that included multiple disciplines including physicians, ED leadership, pharmacy, radiology, and patient experience. This project began in December of 2018 and was completed by May 2019. NSW was maintained until the pandemic closed the unit in March of 2020.
Measures
ALOS (the time of patient arrival until discharge) and LWBS (the number of patients who leave before seeing a provider) were both measured for this project. The ALOS is a performance measure that is routinely gathered by the hospital. The primary goal of this intervention was to reduce ALOS. The ED lean team that sponsored this project investigated changes in the process weekly to determine whether this intervention was successful and whether the changes were cost effective.
Creating Nurse Standard Work
A nurse serving on the ED lean team was charged with creating and leading the NSW team and serving as the liaison between the lean and NSW teams to report weekly progress and barriers being encountered. The NSW team consisted of nursing staff who worked in the triage and fast-track areas. Gathering data was a lengthy part of the project taking 5 weeks as NSW team members spent only 2 hours each shift observing and recording the process steps as performed and did their clinical work for the remainder of their shift. The team was assisted by a lean facilitator experienced using the A3 problem-solving approach. The NSW team methods are explained step by step below using the 9 block A3 format given in Figure 1.
Blocks: 1. Reasons for Action and 2. Initial State of A3
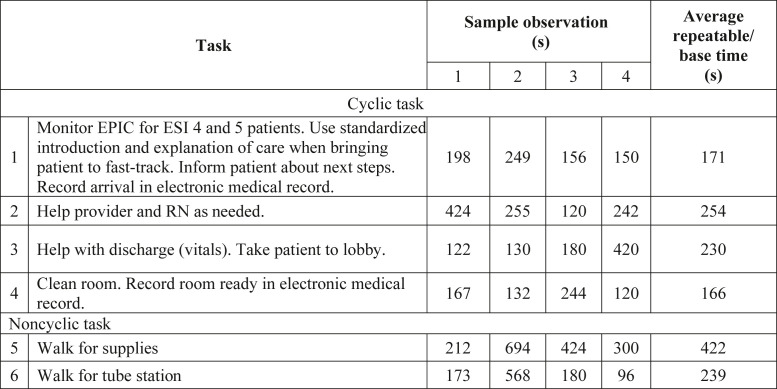
The NSW team was charged with creating NSW to create a stable process for providing patient care with a target ALOS of 162 minutes for the fast-track area. This target time allowed staff to meet takt time within the fast-track area and time for the processes before the fast-track area. The first step was to determine the initial baseline state from the patient’s perspective as they moved from arrival at security until they were discharged. The team observed, timed and documented all cyclical and noncyclic work elements during each process step similar to previous research.31 The NSW team used the same observation sheet to gather data about tasks performed by each of the 8 different staff roles patients interacted with during their ED visit until the observers saw convergence on the work elements performed and the time taken to do the work (eg, 1 role required 40 observations). Convergence meant that the team was not observing any new cyclic (ie, repeatable) or noncyclic work. Figure 2 shows a sample of 4 detailed observations of the nurse specialty technician (NST) role. Note that task 2 in Figure 2, labeled “2. Help provider and RN as needed,” shows high variance in task time (ie, 424-120 seconds) with an average of 254 seconds (see “Average repeatable/“Base time” column).
Figure 2.
Nurse specialty technician job element worksheet. ESI, emergency severity index; RN, registered nurse.
Blocks: 3. Target State and 4. Gap Analysis of A3
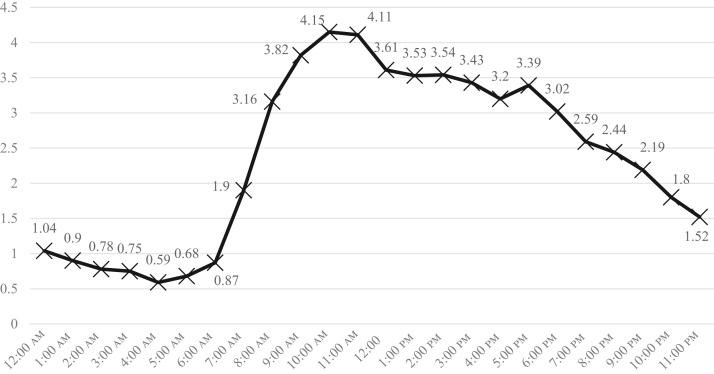
The target state was to develop NSW that allowed all tasks to be completed within takt time, and the gap was any difference between the takt and actual time. The first step in calculating takt time was to measure the SD and average demand per hour during the previous year. Demand for the next year was forecast to equal last year’s average demand per hour plus 1 SD as shown in Figure 3 . The annual demand for fast track was forecast to be 33,000 patients. The second step in calculating takt time was to determine the time available in minutes for the year. The fast-track area was scheduled for 20 hours per day, 7 days a week, which equals 438,000 minutes per year. The third step was to calculate takt time as (time available)/demand, so takt = (438,000 minutes)/(33,000 patients), or 13.27 minutes per patient room. Given that fast track has 6 rooms, each patient needs to have all tasks from arrival to discharge completed within 79.62 minutes (4772 seconds). Finally, each role interacting with the patient was assigned a portion of the takt time. Given that the fast-track registered nurse (RN) and NST needed the most time, they were each given the largest allocation of any of the 8 roles or 809 seconds.
Figure 3.
ESI 4 and ESI 5 patients average demand + 1 SD per hour. ESI, emergency severity index.
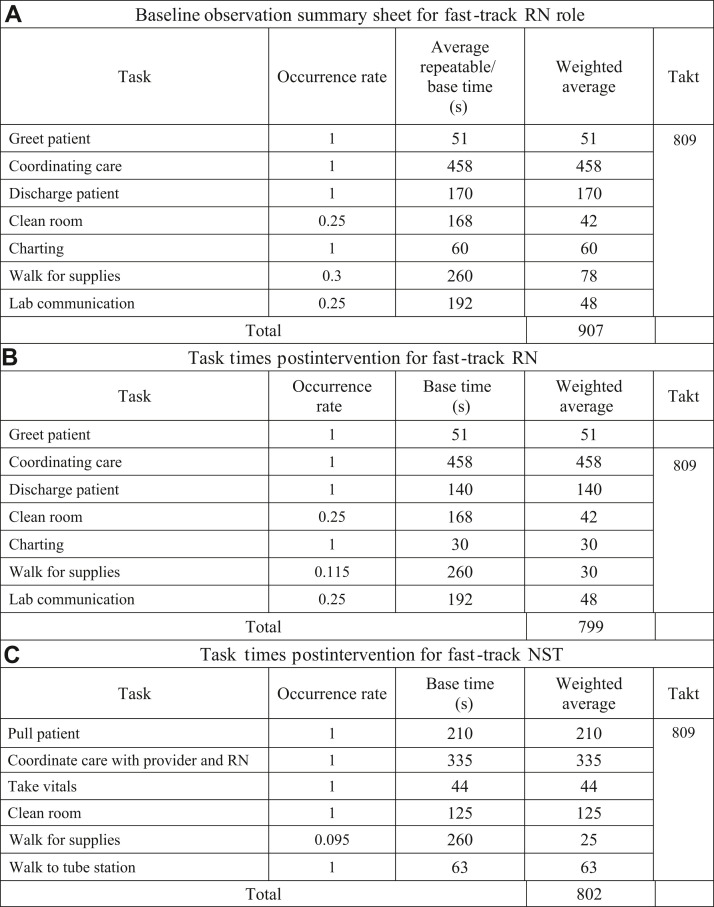
To analyze the gap, the average number of times the RN and the NST performed each task and the percent of times a task was observed (ie, occurrence rate) and the average repeatable/base time to perform that task (Figure 2) were placed into a baseline observation summary sheet for each role and then the weighted average time for each task was calculated (see Figure 4 A). The sum of the weighted averages was compared with the takt time for each role. Both the NST and RN tasks had longer weighted average baseline times than the takt time. Figure 4A shows that the RN baseline time was 907 seconds, which is 98 seconds longer than the 809 second takt time.
Figure 4.
(A) Baseline observation summary sheet for fast-track RN role. (B) Task times postintervention for fast-track RN. (C). Task times postintervention for fast-track NST. NST, nurse speciality technician; RN, registered nurse.
Blocks: 5. Solution approach and 6. Rapid Experimentation of A3
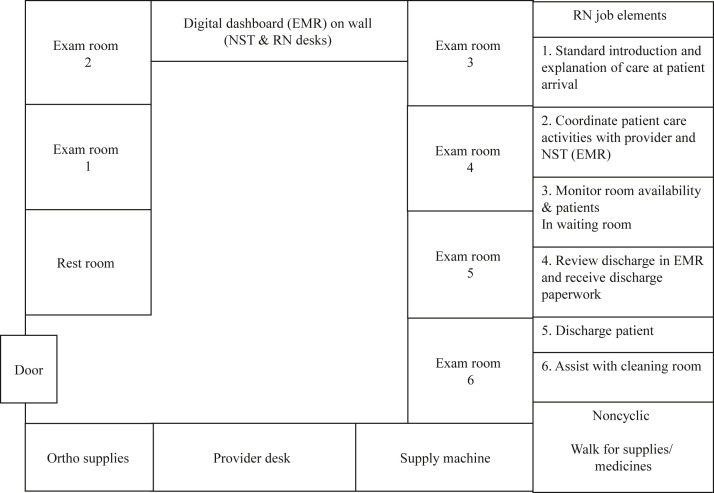
To eliminate the RN and NST workload gap (ie, difference between takt time target and actual time), the NSW team examined each task in detail for both the RN and NST. The team posted these tasks and times on a board in the conference room and then listed all the subelements of each task. For example, subelements to complete the RN’s “Charting” task included the following: (1) record disposition, (2) charge capture, (3) list all procedures or split/wound care provided, and (4) record any radiology ordered or provided. The team then identified all delays, interruptions, and walking that occurred when a task subelement was performed. For example, how much time did the RN spend searching for supplies or walking between locations to get supplies. To accurately measure walking, the NSW team first created a map of the fast-track area (see Figure 5 ) and then recorded all staff movements within and out of the area, creating a series of spaghetti diagrams (not shown, see previous examples32). The NSW team found that the RN and NST frequently left fast track to get orthopedic supplies and medicines and that almost three fourths of the medications and supplies needed were located outside the fast-track area. To eliminate these times, the NSW team cleaned and standardized the fast-track storeroom using the 5S technique.32 , 33 An essential step was to establish a standard set of medicines and supplies to be maintained at par level in the fast-track area. The NST was then charged to check that all fast-track supplies were at par level at the beginning of each day. The spaghetti diagrams also showed the NSW team that there was no standard procedure to bring patients from the waiting room to fast-track area when a room became available. This task was assigned to the NST as well as the task of monitoring the waiting room for arrival of ESI 4 and 5 patients using electronic health record screens.
Figure 5.
Fast-track layout with RN standard work. EMR, electronic medical record; NST, nurse specialty technician; RN, registered nurse.
Observations identified a delay in the RN patient discharge process that was caused by registration not starting patient discharge until the provider submitted discharge orders. This was addressed by creating standard work for registration that specified that registration was to be initiated as soon as feasible after the triage examination. Discussions to accomplish this led to registration and fast-track working together as a team with the common goal of expediting patient care. For example, if the RN was in the room performing a task such as starting an intravenous line, registration could enter and begin their process.
A significant improvement in patient flow was achieved by eliminating work batching. A common practice was for the provider to place orders for multiple patients at one time. The provider hopes that by batching this process step the average time of performing the step for each patient can be reduced. However, even if the task time is reduced, batching increases patient waiting and prevents other staff from starting their work. Batching at 1 step “starves” the next step and eventually overwhelms the next step when a batch of work suddenly arrives.34
Implementing these interventions required cooperation of multiple roles outside of nursing, so creating NSW also standardized other system work. These interventions eliminated delays and clarified task assignments and reduced the RN workload to 799 seconds (see Figure 4B) and the nurse technician workload to 802 seconds (see Figure 4C). These workloads were 10 and 7 seconds, respectively, less than their 809 second takt targets.
Blocks 7 Completion Plan and 8 Confirmed State of A3
Once NSW is created, it must become the way work is done. One technique to maintain NSW was to post the NSW tasks in the workplace. For example, the RN NSW was posted above the RN desk as shown in the right-hand side of Figure 5. The team added a standardized introduction and explanation of care to NSW, because it was a hospital-wide requirement for all nurse/patient contacts. Figure 5 shows the NSW noncyclic tasks (eg, walking for supplies and medicines) below the 6 repetitive NSW tasks.
A second step was to include training about NSW within the ED staff training procedures. A third and critical step to maintain NSW was to institute manager daily audits. Daily audits ensure that standard work is performed and demonstrate that management considers standard work to be important.35 The team developed an audit form (see Table 1 ) to check daily the extent to which NSW was used. The right-hand side of the Table shows the person responsible for the item being audited. Of the 21 standard NSW tasks, 13 were the responsibility of someone other than the RN or NST. For example, audit items 1, 2, and 3 were the responsibility of the charge nurse, but were required for the fast-track RN to maintain takt. The NSW audit was done at the beginning of each day by an emergency nurse manager. Having a manager conduct the audit is important for 2 reasons: (1) this signals that management cares about NSW. and (2) auditing NSW engages the manager in the standard work. On average this audit took 5 minutes or less each day. To do the audit, managers interviewed the RN in the fast-track area while looking at the digital dashboard (see “Digital Dashboard” in Figure 5). The auditor checked “Yes” or “No” for each of the 21 items in the form. A “Yes” was scored as 1 point and the points were totaled at the bottom. The audit was structured to avoid “blame” and to focus on problems performing NSW.
Table.
Form for audit of fast-track nurse standard work
| Score: yes = 1; no = 0 | Responsible | ||
|---|---|---|---|
| 1 | Is 1 RN assigned? | Charge nurse | |
| 2 | Is 1 NST assigned? | Charge nurse | |
| 3 | Are 2 advanced practice providers assigned? | Charge nurse | |
| 4 | Are supplies stocked to standards? (lac cart, IV cart, ortho room) | NST | |
| 5 | Are fast-track rooms full of appropriate patients (if available)? | NST | |
| 6 | Is the NST pulling patients? (see dashboard) | NST | |
| 7 | Are rooms cleaned and marked available within 5 min? | NST | |
| 8 | Is provider seeing patient within 5 min? (see dashboard) | Provider | |
| 9 | Is the provider seeing one patient and writing orders before seeing the next patient? (see dashboard) | Provider | |
| 10 | Is RN signing up for patients? (see dashboard) | RN | |
| 11 | Does the Pyxis have the needed medications? | Material services | |
| 12 | Are meds being administered within 15 min? (see chart) | RN | |
| 13 | Is patient ready to depart 15 min or less? (see dashboard) | RN | |
| 14 | Is discharge paperwork ready once discharge chosen? (ask RN) | Provider | |
| 15 | Are providers handing nurses discharge paperwork? (ask RN) | Provider | |
| 16 | Are all tests being processed appropriately? (ask RN) | Lab/Radiology | |
| 17 | Is RN taking proactive measures for any delayed testing? (ask RN) | RN | |
| 18 | Has housekeeping rounded on fast-track? (ask RN) | Housekeeping | |
| 19 | Is person assigned to job knowledgeable of standard work procedure? | Charge nurse | |
| 20 | Is registration complete before patient being ready for DC? (ask RN) | Registration | |
| 21 | Is the daily management system (computer screen) updated? | Information systems | |
| Total | |||
DC, discharge; IV, intravenous; lac cart, laceration cart; RN, registered nurse; NST, nurse specialty technician.
Results
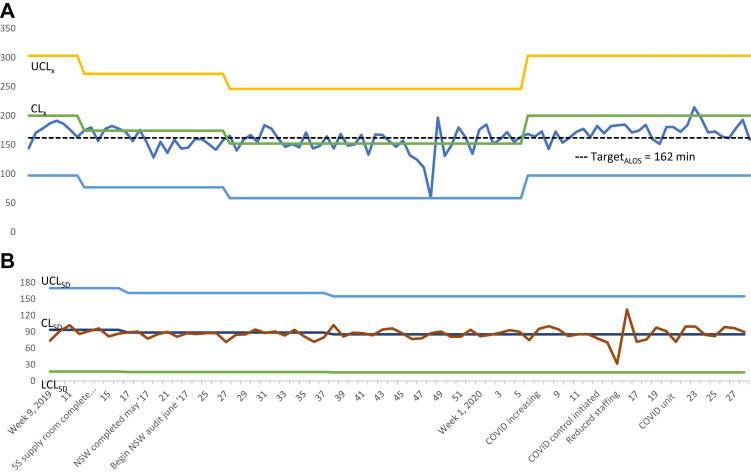
The primary analysis was a precomparison and postcomparison of ALOS performance using the Xbar and S control charts shown in Figure 6 A and 6B, respectively, to identify a significant change.36 Data from the first 8 weeks of 2019 were used to set the control limits for the Xbar and S chart. The control charts start with week 9, 2019 and extend through February 2021. The charts do not extend further, because the fast-track area was repurposed to manage the large number of COVID-19 patients arriving during the pandemic. Significant events in the creation and maintenance of NSW are shown on the horizontal axis; otherwise, the horizontal axis shows the week of the year. The control limits were updated when the charts indicated a significant change in the process (eg, the ALOS in Figure 6A remained below the centerline for more than 5 consecutive weeks). The NSW team ALOS goal was 162 minutes (see Figure 6A) and the initial centerline for ALOS was 200.2 minutes, which was reduced to 150 minutes as NSW was implemented; however, ALOS increased to 200 minutes when fast track transitioned to a COVID-19 unit. In week 15 of 2020, fast-track patients stayed away from the hospital (ie, there were only 17 ESI 4 and 5 patients for the week) as COVID-19 increased and ALOS was only 59 minutes.
Figure 6.
(A) ALOS (ALOS = x): week 9, 2019 to week 8, 2021 target ALOS = 162 minutes. (B) SD length of stay (s): week 9, 2019 to week 8, 2021. ALOS, average length of stay; CL, center line; LCL, lower control limit; UCL, upper control limit
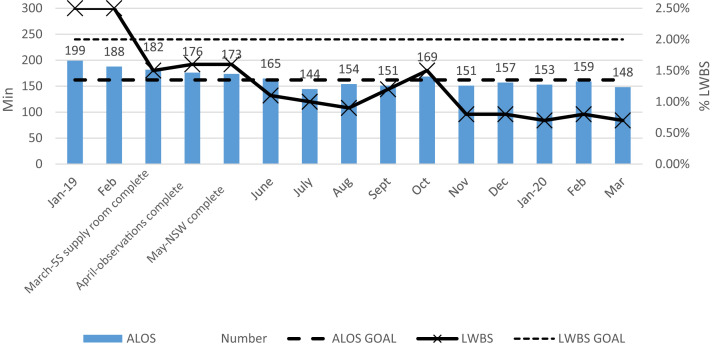
Figure 6B shows that the SD was small and moved randomly around the centerline and never approached its control limits. This means that the SD was within its control limits. Figure 7 gives the ALOS for each month from January 2019 to March 2020 when fast track was converted to treating COVID-19 patients. Figure 7 also includes the monthly LWBS. The horizontal axis shows the month when the NSW tasks were implemented. This shows a gradual drop in ALOS starting in January until in July when it was below 150 minutes. ALOS stayed close to 150 minutes the rest of the year, below the target of 162 minutes, whereas LWBS decreased below its target level of 2% and stayed there through March 2020.
Figure 7.
ALOS and LWBS. ALOS, average length of stay; LWBS, left without being seen; NSW, nurse standard work.
Discussion
This was a quality improvement study where preintervention performance was compared with postintervention performance. The team designing the changes included those who were actually doing the work, which can best be described as an action research methodology as the researchers not only tested an intervention, but they also simultaneously managed the practical realities, implementing it within the emergency department.37 Nursing standard work created here had 3 elements: (1) takt time, (2) task performance sequence, and (3) standard inventory. The NSW team formed the last week of February 2019 and met weekly until the work was completed in the third week of April 2019. The NSW team reported its progress completing its A3 to the larger lean team weekly. All process changes were implemented as they were developed, which was feasible because the NSW team included those actually performing the work. For example, the NST began to pull patients form the lobby the first week of March, the registration process changed the first week of April, and task assignments for the NST and RN were completed by the third week of April and formalized as standard work the first week of May 2019. The audit process was finalized in week 1 of June 2019. Implementing changes slowly allowed for staff to determine whether the change was beneficial to the project and allowed for focused education to be provided to the staff. Initially, the NSW team wanted to implement solutions as they discovered problems; however, taking time to work through the A3 methodology allowed for data-driven changes rather than based off of perceptions.
The NSW team used the A3 problem-solving method to identify and remove barriers to achieving NSW. This structured problem solving forced the NSW team to avoid quick fixes and to instead examine each individual process element. As described earlier, creating NSW was a process of making small changes to multiple job elements. Creating NSW was an example of evidence-based problem solving in health care. It required accurate measurements of patient demand and task performance times and observations of delays and performance barriers. However, creativity also was required for the NSW team to rethink how to perform required tasks to meet the takt time goal. Some creative solutions were to use 5S to address the lack of storage space for supplies. Finally, it required manager discipline via the NSW audit to maintain NSW and not to conduct a “blame”- audit, but rather a problemidentification audit.
The major changes to complete NSW within the takt time were that the NSW team identified excessive walking, delays, and interruptions it could eliminate by standardizing storeroom supplies using 5S and by standardizing the medicine storage in the fast-track area. The NSW team also recognized that assigning the NST the task of monitoring the track board and pulling patients from the waiting room quickly when a fast-track room became available eliminated service delays. The RN and NST shared the task of ensuring that patients going to radiology were properly dressed; this effort to coordinate care eliminated a process delay.
Daily audits by a nurse manager of NSW performance assisted compliance by reminding everyone that system performance depends on standard work, but also gave staff daily access to management when problems were encountered.38 The audit is feedback to both the manager and staff. It checks the unit compliance level and also provides a means for staff to notify management of operational failures when they occur.28 When staff can share process problems with managers as they occur, the manager has more information and can intervene to solve throughput problems in real time to enable patient care.38
Limitations
The generalizability of one case study of 1 fast-track area experience creating NSW is necessarily limited, but the approach taken here to identify repeatable tasks versus nonrepeatable tasks is applicable to all locations. A second limitation is that the outcome measures were gathered by the hospital, and patient satisfaction with the fast-track experience could not be measured. Third, the NSW team gathered data about task performance through task observation, which is time consuming, so the data gathering was limited. In addition, changes to the task elements, such as delegating tasks to the NST, are situation dependent and may not be applicable to other fast-track units. However, the process steps of implementing NSW and the NSW audit are generalizable to other environments.
Conclusion
NSW was an effective intervention that significantly reduced ALOS for fast-track patients in a large urban hospital. Sustainability depends on management follow-through, given that an essential step in this intervention is the management audit of standard work. There has been a lack of investigation in the health care literature about how to create and maintain standard work practices. A next, very important step is to investigate the effects of standard work in other ED units. After the COVID-19 pandemic, the fast-track area physically moved to another area to allow 2 additional beds, but all processes developed before this were duplicated in the new fast-track area. Hospital management found this process valuable, and other hospitals within the system are now implementing a similar process.
Author Disclosures
Conflicts of interest: The authors do not have any conflicts of interest to report.
Biographies
Dorothy Williams is a BSN, RN, Foothills ENA, Greenville, SC. ORCID identifier:https://orcid.org/0000-0003-3336-5244.
Lawrence D. Fredendall is a BS, MBA, PhD Professor Department of Management, Clemson University, Clemson, SC. ORCID identifier:https://orcid.org/0000-0002-7127-9737.
Gregory Hair is MS, BSN, RN, Greenville, SC. ORCID identifier:https://orcid.org/0000-0001-7069-128X.
Jim Kilton is a Project Facilitator, Greenville, SC.
Cassie Mueller is MSN, RN, Foothills ENA, Greenville, SC. ORCID identifier:https://orcid.org/0000-0002-9647-5048.
Joshua D. Gray is an MD, Greenville, SC. ORCID identifier:https://orcid.org/0000-0002-7341-7996.
Christian Graver is an MSN, RN, Greenville, SC.
Jaeyoung Kim is a PhD Candidate, Clemson, SC. ORCID identifier:https://orcid.org/0000-0003-3190-3184.
References
- 1.Wallingford G., Jr., Joshi N., Callagy P., Stone J., Brown I., Shen S. Introduction of a horizontal and vertical split flow model of emergency department patients as a response to overcrowding. J Emerg Nurs. 2018;44(4):345–352. doi: 10.1016/j.jen.2017.10.017. [DOI] [PubMed] [Google Scholar]
- 2.Bonalumi N.M., Bhattacharya A., Edwards C., et al. Impact of a planned workflow change: super track improves quality and service for low-acuity patients at an inner-city hospital. J Emerg Nurs. 2017;43(2):114–125. doi: 10.1016/j.jen.2016.03.029. [DOI] [PubMed] [Google Scholar]
- 3.Nash K., Zachariah B., Nitschmann J., Psencik B. Evaluation of the fast track unit of a university emergency department. J Emerg Nurs. 2007;33(1):14–20. doi: 10.1016/j.jen.2006.08.003. [DOI] [PubMed] [Google Scholar]
- 4.Gilboy N., Tanabe P., Travers D., Rosenau A.M. Version 4. Agency for Healthcare Research and Quality; 2012. Emergency Severity Index (ESI): A Triage Tool for Emergency Department Care. Accessed July 01, 2022. thepafp.org/website/wp-content/uploads/2017/05/2012-Emergency-Severity-Index-for-Triage.pdf. [Google Scholar]
- 5.Considine J., Kropman M., Kelly E., Winter C. Effect of emergency department fast track on emergency department length of stay: a case-control study. Emerg Med J. 2008;25(12):815–819. doi: 10.1136/emj.2008.057919. [DOI] [PubMed] [Google Scholar]
- 6.Liu S.W., Hamedani A.G., Brown D.F.M., Asplin B., Camargo C.A., Jr. Established and novel initiatives to reduce crowding in emergency departments. West J Emerg Med. 2013;14(2):85–89. doi: 10.5811/westjem.2012.11.12171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hino S. Productivity Press; 2006. Inside the Mind of Toyota: Management Principles for Enduring Growth. [Google Scholar]
- 8.Imai M. McGraw-Hill; 1997. Gemba Kaizen: A Commonsense, Low-Cost Approach to Management. [Google Scholar]
- 9.Liker J.K., Meier D. McGraw-Hill; 2006. The Toyota Way Fieldbook: A Practical Guide for Implementing Toyota’s 4Ps. [Google Scholar]
- 10.Ohno T. McGraw-Hill; 2013. Taiichi Ohno’s Workplace Management. [Google Scholar]
- 11.Ng D., Vail G., Thomas S., Schmidt N. Applying the Lean principles of the Toyota production system to reduce wait times in the emergency department. CJEM. 2010;12(1):50–57. doi: 10.1017/S1481803500012021. [DOI] [PubMed] [Google Scholar]
- 12.Bucci S., de Belvis A.G., Marventano S., et al. Emergency department crowding and hospital bed shortage: is Lean a smart answer? A systematic review. Eur Rev Med Pharmacol Sci. 2016;20(20):4209–4219. [PubMed] [Google Scholar]
- 13.Costa L.B.M., Filho M.G. Lean healthcare: review, classification and analysis of literature. Prod Plan Control. 2016;27(10):823–836. doi: 10.1080/09537287.2016.1143131. [DOI] [Google Scholar]
- 14.de Souza L.B. Trends and approaches in lean healthcare. Leadership in Health Services. 2009;22(2):121–139. doi: 10.1108/17511870910953788. [DOI] [Google Scholar]
- 15.Drotz E., Poksinska B. Lean in healthcare from employees’ perspectives. J Health Organ Manag. 2014;28(2):177–195. doi: 10.1108/JHOM-03-2013-0066. [DOI] [PubMed] [Google Scholar]
- 16.Holden R.J. Lean thinking in emergency departments: a critical review. Ann Emerg Med. 2011;57(3):265–278. doi: 10.1016/j.annemergmed.2010.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Mazzocato P., Holden R.J., Brommels M., et al. How does lean work in emergency care? A case study of a lean-inspired intervention at the Astrid Lindgren Children’s Hospital, Stockholm, Sweden. BMC Health Serv Res. 2012;12(1):1–13. doi: 10.1186/1472-6963-12-28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Alnajem M., Garza-Reyes J.A., Antony J. Lean readiness within emergency departments: a conceptual framework. Benchmarking. An International Journal. 2019;26(6):1874–1904. doi: 10.1108/BIJ-10-2018-0337. [DOI] [Google Scholar]
- 19.Hallam C.R.A., Contreras C. Lean healthcare: scale, scope and sustainability. Int J Health Care Qual Assur. 2018;31(7):684–696. doi: 10.1108/IJHCQA-02-2017-0023. [DOI] [PubMed] [Google Scholar]
- 20.Naik T., Duroseau Y., Zehtabachi S., et al. A structured approach to transforming a large public hospital emergency department via lean methodologies. J Healthc Qual. 2012;34(2):86–97. doi: 10.1111/j.1945-1474.2011.00181.x. [DOI] [PubMed] [Google Scholar]
- 21.Chalice R. Quality press; 2007. Improving Healthcare Using Toyota Lean Production Methods: 46 Steps for Improvement. [Google Scholar]
- 22.Kochevar B.J., Schumann M.D. In: Leading the Lean Healthcare Journey: Driving Culture Change to Increase Value. 1st ed. Wellman J., Jeffries H., Hagan P., editors. Productivity Press; 2010. Working hard to improve work flow in the lab; pp. 179–192. [Google Scholar]
- 23.Graban M., Toussaint J. 3rd ed. Productivity Press; 2018. Lean Hospitals: Improving Quality, Patient Safety, and Employee Engagement. [Google Scholar]
- 24.Eitel D.R., Rudkin S.E., Malvehy M.A., Killeen J.P., Pines J.M. Improving service quality by understanding emergency department flow: a white paper and position statement prepared for the American Academy of Emergency Medicine. J Emerg Med. 2010;38(1):70–79. doi: 10.1016/j.jemermed.2008.03.038. [DOI] [PubMed] [Google Scholar]
- 25.Radnor Z.J., Holweg M., Waring J. Lean in healthcare: the unfilled promise? Soc Sci Med. 2012;74(3):364–371. doi: 10.1016/j.socscimed.2011.02.011. [DOI] [PubMed] [Google Scholar]
- 26.Jackson T.L. CRC Press, Taylor and Francis Group; 2012. Standard Work for Lean Healthcare. [Google Scholar]
- 27.Robinson A.G. Productivity Press; 1991. Continuous Improvement in Operations: A Systematic Approach to Waste Reduction. [Google Scholar]
- 28.Tucker A.L. The impact of operational failures on hospital nurses and their patients. Journal of Operations Management. 2004;22(2):151–169. doi: 10.1016/j.jom.2003.12.006. [DOI] [Google Scholar]
- 29.Staats B.R., Brunner D.J., Upton D.M. Lean principles, learning, and knowledge work: evidence from a software services provider. Journal of Operations Management. 2011;29(5):376–390. doi: 10.1016/j.jom.2010.11.005. [DOI] [Google Scholar]
- 30.Chakravorty S.S. Process improvement: using Toyota’s A3 reports. Quality Management Journal. 2009;16(4):7–26. doi: 10.1080/10686967.2009.11918247. [DOI] [Google Scholar]
- 31.Dickson E.W., Anguelov Z., Vetterick D., Eller A., Singh S. Use of lean in the emergency department: a case series of 4 hospitals. Annals of Emergency Medicine. 2009;54(4):504–510. doi: 10.1016/j.annemergmed.2009.03.024. [DOI] [PubMed] [Google Scholar]
- 32.Labach E.J. Using standard work tools for process improvement. Journal of Business Case Studies. 2011;6(1):39–48. doi: 10.19030/jbcs.v6i1.855. [DOI] [Google Scholar]
- 33.Hirano H. 1st ed. PHP Institute of America; 1993. Putting 5s to Work: A Practical Step-by-Step Approach. [Google Scholar]
- 34.Simons J.V., Russell G.R. A case study of batching in a mass service operation. Journal Operations Management. 2002;20(5):577–592. doi: 10.1016/S0272-6963(02)00028-1. [DOI] [Google Scholar]
- 35.Mann D. 3rd ed. CRC Press Taylor and Francis Group; 2015. Creating a Lean Culture: Tools to Sustain Lean Conversions. [Google Scholar]
- 36.Reynolds M.S., Spencer S.P., Dunaway A., Buckingham D., Bartman T. Scientific approach to assess if change led to improvement—methods for statistical process control analysis in quality improvement. J Emerg Nurs. 2021;47(1):198–205. doi: 10.1016/j.jen.2020.09.002. [DOI] [PubMed] [Google Scholar]
- 37.Coughlan P., Coghlan D. Action research for operations management. International Journal of Operations and Production Management. 2002;22(2):220–240. doi: 10.1108/01443570210417515. [DOI] [Google Scholar]
- 38.Tucker A.L. The impact of workaround difficulty on frontline employees’ response to operational failures: a laboratory experiment on medication administration. Management Science. 2016;62(4):1124–1144. doi: 10.1287/mnsc.2015.2170. [DOI] [Google Scholar]