Abstract
Background and Objectives.
Experts hypothesized increased weight gain in children associated with the COVID-19 pandemic, potentially due to closures of schools and recreational facilities with consequent reduction of physical activity and dietary changes. Our objective was to evaluate whether the rate of change of child BMI increased during the COVID-19 pandemic compared to pre-pandemic years.
Methods.
The study population of 1996 children ages 2–19 years with at least one BMI measure before and during the COVID-19 pandemic was drawn from 38 pediatric cohorts across the US participating in the ECHO-wide Cohort Study. We modelled change in BMI using linear mixed models adjusting for age, sex, race, ethnicity, maternal education, income, baseline BMI category, and type of BMI measure. Data collection and analysis was approved by the local IRB of each institution or by the central ECHO IRB.
Results.
BMI increased during the COVID-19 pandemic compared to previous years (0.24 higher annual gain in BMI during the pandemic compared to previous years, 95% CI 0.02, 0.45). Children with BMI in the obese range compared to the healthy weight range were at higher risk for excess BMI gain during the pandemic, while children in higher-income households were at decreased risk of BMI gain.
Conclusions.
One effect of the COVID-19 pandemic is an increase in annual BMI gain during the COVID-19 pandemic compared with the three prior years among children in our national cohort. This increased risk among US children may worsen a critical threat to public health and health equity.
Article Summary:
This study evaluates whether the annual rate of change in child BMI was higher during the pandemic than in previous years.
INTRODUCTION
Childhood obesity is a serious problem with long-term health and quality of life concerns; nearly 1 in 5 US children were categorized as obese in 20181. Starting in March 2020, widespread closure of schools, recreation facilities, and recreational or sport activities due to the COVID-19 pandemic may have resulted in decreased physical activity and altered dietary habits in children, placing them at higher risk for excess weight gain2,3. Prior to the COVID-19 pandemic, higher rates of weight gain among school-aged children across the US were observed during the summer months, when children are out of school, particularly among children who are overweight or obese and among racial and ethnic groups at higher risk of obesity4–8. The Structured Days Hypothesis explains this weight gain as due to changes to or lack of structured opportunities for physical activity through school physical education classes, recess, or recreational sports activities, loss of regulated meal times and limits on amount and types of food, and more obesogenic screen time and sleep routines9; changes that were also present as the pandemic disrupted normal school and childcare routines. Such weight gain is problematic because it is maintained at least through the following school year5, and in general, weight gain in childhood is predictive of later overweight and obesity into adulthood10,11, with later health consequences. In this context, public health and obesity experts have expressed concern that a byproduct of the COVID-19 pandemic-related shutdowns will be excess weight gain among children12–15.
Two recently published US studies have suggested that these concerns are well-founded; using medical records data, Woolford et al. in Southern California and Lange et al. using data from children across the US, showed an accelerated rate of weight gain and increased BMI among children during the pandemic period16,17. A study of children who had a height and weight measured at school showed accelerated weight gain during the pandemic-year compared to pre-pandemic years18; in particular, accelerated weight gain was demonstrated among children in the healthy BMI category. Similar results have been reported internationally. A retrospective survey of 10,082 adolescents and young adults in China reported increases in BMI during the pandemic19. In another survey in Turkey, conducted after the start of the COVID-19 pandemic, 42% of parents reported that their child gained weight, compared to 55% reporting no change in weight, within a 3-week lock-down period20.
There are some limitations to current knowledge regarding excess weight gain in children during the COVID-19 pandemic. First, the US studies were done using medical records or in a school setting and had limited information available on child/household socioeconomic status (SES). Given the disproportionate impact of both the obesity epidemic as well as COVID-19 pandemic-related hardships on children from lower socioeconomic status levels, it is important to consider SES in examining changes in BMI21,22. Second, during the pandemic, many families had limited ability to attend a medical visit. Therefore, studies using solely medical records data may not fully reflect the experiences of the broader US population.
The Environmental Influences on Child Health Outcomes (ECHO) consortium brings together long-standing prospective child cohorts in the United States with the goal of investigating the effects of environmental exposures on child health outcomes23. Leveraging prospectively collected cohort study data, our objective in this analysis was to evaluate changes in children’s BMI from the pre-pandemic to the pandemic period. Specifically, we evaluated whether children exhibited accelerated weight gain during the COVID-19 pandemic (from March 2020 through May 2021), when many schools were closed and recreational activities curtailed, compared to the pre-pandemic years (October 2017 – February 2020).
METHODS
Study Population and Outcome
The study population was drawn from the ECHO-wide Cohort Study, a consortium of 69 pediatric cohort studies across the United States23,24. A central and cohort-specific institutional review boards monitored human subject activities at each cohort site and the centralized ECHO Data Analysis Center. All participants provided informed consent.
Children’s weight and height were obtained by each cohort from measurements taken at the cohort study visit, medical record abstraction, or self- or parent- reported measurements. Height and weight were used to calculate body mass index (BMI; kg/m2) and percentiles25,26. We use BMI as the outcome because it is considered most appropriate for the comparison of BMI changes as across time27–29. CDC cutoffs were used to determine implausible measures, which were excluded from analysis25. BMI category was defined according to CDC guidelines for defining childhood weight status based on BMI percentiles for age and sex: underweight (<5%); healthy weight (5 – <85%); overweight (85 – <95%); and obese (>=95%)30.
For this analysis, the COVID-19 “pandemic period” was defined as the 15-month period from March 1st, 2020, to May 31st, 2021 during which the COVID-19 pandemic caused many disruptions of daily routines. The baseline, or “pre-pandemic period” was between October 1st, 2017 to February 29th, 2020. A total of 1996 children from 38 cohorts, representing 53 recruitment sites across the US, who contributed at least one BMI in both the “pre-pandemic” and the “pandemic” study periods, comprised the primary analytic sample (Figure 1).
Figure 1. Map of Participating Enrollment Sites.
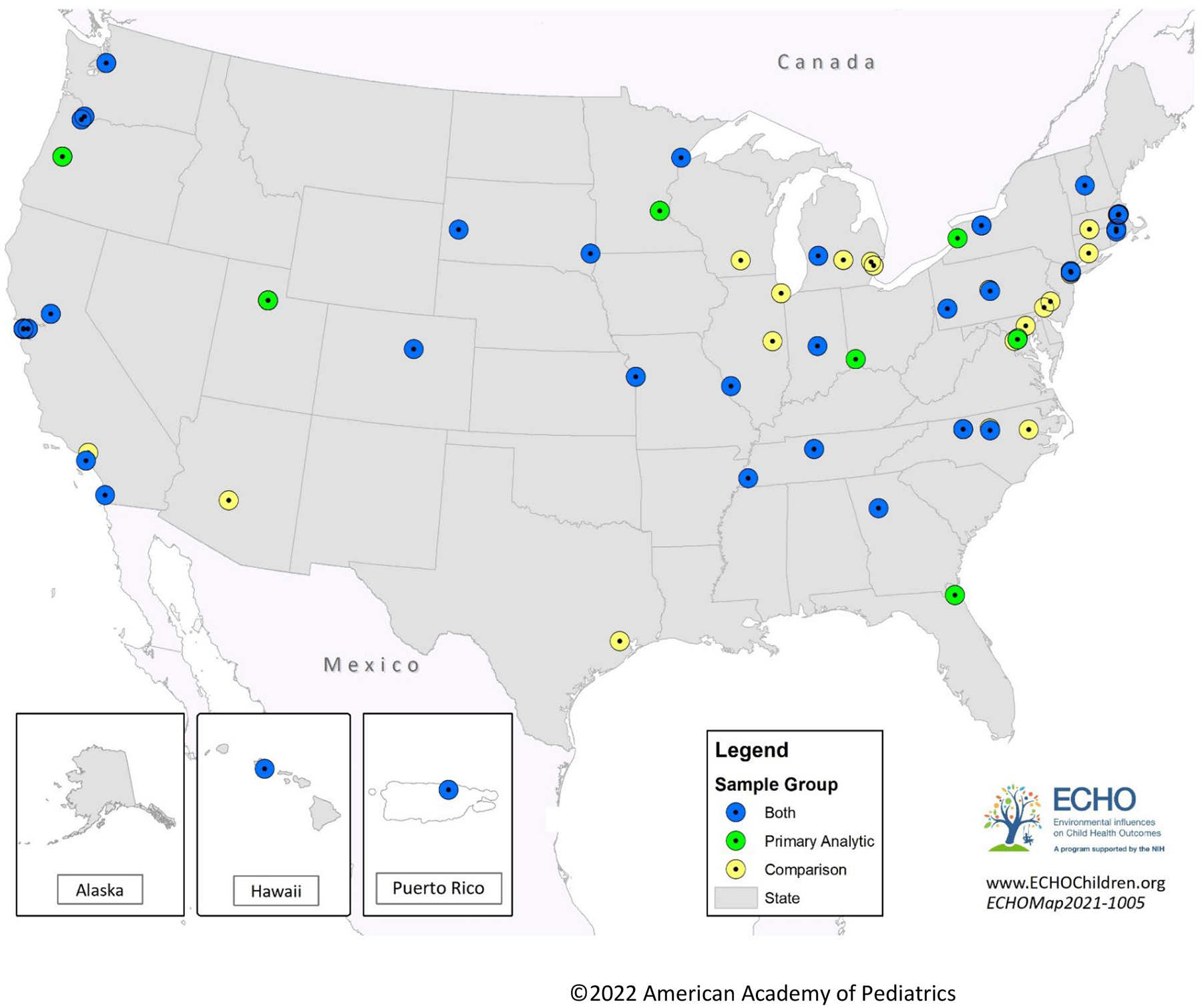
Figure 1 shows the data collection and enrollment sites from which the study population is drawn. Sites that only contributed participants to the primary study sample are in green, sites that only contributed to the comparison sample are shown in yellow, and sites that contributed participants to both samples are shown in blue.
Sociodemographic and other covariates
Child date of birth was collected at participant registration and age at assessment was recorded continuously in years. Categorical variables included child sex at birth (male, female); highest level of maternal education attained (less than high school; high school or GED equivalent; or at least some college or more), annual household income (less than or equal to $30,000; $30,000 – $49,999; $50,000 – $74,999; $75,000 or greater), and child race and ethnicity (reported by the parent or child as non-Hispanic white; non-Hispanic black; non-Hispanic other race; Hispanic), which we consider a proxy for exposure to structural racism that shapes a range of resources such as housing, education, and employment.31 All sociodemographic variables were collected via self-report or medical record abstraction. A binary “pandemic period” indicator was introduced to reflect whether a BMI measure was taken during the pandemic period (March 2020 through May 2021) or the pre-pandemic period (October 2017 through February 2020).
Statistical Analysis
We tabulated participant characteristics in the primary analytic sample for the baseline pre-pandemic period. For continuous variables (child age, BMI, change in BMI), means and standard deviations were calculated. Number of participants and percentages were reported for categorical variables (sex, race and ethnicity, maternal education level, household income level, type of BMI measure and BMI category).
To examine trends in BMI before and during the pandemic, we employed linear mixed effects models to compare the annual change in BMI between the pre-pandemic period and the pandemic period. All models included calendar year, child age, child sex, child race and ethnicity, maternal education, type of measurement (study measure, medical record, or self/parent report), baseline BMI category, household income level, and an indicator for pre-or post pandemic time period, with a random intercept for each child participant and for cohort. Missing data on income, race, and maternal education were imputed using the Multivariate Imputation by Chained Imputation (MICE) package in R, with all other variables from the analytic models included as predictors. Results were pooled after 10 iterations.32 Our key parameter of interest was an interaction term between the pandemic year indicator and calendar year, which represents the change in slope (rate of BMI change) between the COVID and pre-COVID time periods. To evaluate whether the rate of BMI change during the pandemic differed by key subgroups (race, Hispanic ethnicity, baseline BMI category, and household income), we employed interaction terms between the pandemic year indicator, calendar year, and the subgroup of interest.
All analyses were completed in R version 4.1.0 (2021-05-18). Mixed effects models were fit using the Fitting Linear Mixed-Effects Models (lme4) package.33
Sensitivity Analyses
We conducted three additional analyses to evaluate the robustness of our main findings to key assumptions. First, because our study inclusion criteria required completing an in-person or virtual cohort study visit during the pandemic period, we explored whether children who returned for a study visit had different sociodemographic attributes than those who were not seen during the COVID-19 pandemic. Second, we repeated our primary models using two time-periods that were both prior to the COVID-19 pandemic to evaluate whether the BMI changes we observed were due to the COVID-19 pandemic or instead to secular trends in BMI change. Last, we conducted our main analysis among children with study-measured anthropometric measures only, to determine whether changes to BMI ascertainment during the pandemic influenced our results. Additional details and results of these analyses are provided in the Online Supplement.
RESULTS
Of the 1996 children in the primary analytic sample, the mean baseline (pre-pandemic) age was 5.9 years (standard deviation (SD): 3.4 years) (Table 1). Half (N=975) were female, and 53% were non-Hispanic white, 15% non-Hispanic Black, and 16% of Hispanic ethnicity. The majority (85%) of mothers reported some college or higher level of education, and 49% reported a household income of $75,000 or more. Most children (70%) had a baseline BMI in the healthy weight range (5%−85%).
Table 1:
Sociodemographic Characteristics of Analytic Sample1 in the Pre-COVID-19 Pandemic Time Period
| Characteristic | N (%) |
|---|---|
| Children | 1996 |
| Child age in 2018, mean ±SD | 5.9 ± 3.4 |
| Sex at birth, Female | 975 (49%) |
| Race & Ethnicity | |
| Missing | 8 (0.4%) |
| Non-Hispanic white | 1067 (53%) |
| Non-Hispanic black | 299 (15%) |
| Non-Hispanic other | 294 (15%) |
| Hispanic, all races | 328 (16%) |
| Maternal Education | |
| Missing | 42 (2.1%) |
| Less than High School | 70 (3.5%) |
| High school degree, GED or equivalent | 178 (8.9%) |
| Some college and above2 | 1706 (85%) |
| Income | |
| Missing | 294 (15%) |
| <= $ 30,000 | 248 (12%) |
| $30,000 – $49,999 | 228 (11%) |
| $50,000 – $74,999 | 255 (13%) |
| $75,000 or more | 971 (49%) |
| BMI Category | |
| Underweight (<5th percentile) | 120 (6%) |
| Healthy weight (5–85th percentile) | 1400 (70%) |
| Overweight (85–95th percentile) | 244 (12%) |
| Obese(>=95th percentile) | 232 (12%) |
| BMI, mean ±SD, Pre-Pandemic | 17.05 ± 3.31 |
| BMI, mean ±SD, During Pandemic | 18.30 ± 4.68 |
| Change in BMI, Pre/During Pandemic, mean ±SD | 1.14 ± 2.79 |
| BMI Ascertainment Method Pre-Pandemic | |
| Self-report | 80 (2.6%) |
| Parent-report | 113 (3.7%) |
| Medical record | 423 (14%) |
| Study Measure | 2431 (80%) |
| BMI Ascertainment Method During-Pandemic | |
| Self-report | 591 (28%) |
| Parent-report | 433 (20%) |
| Medical record | 27 (1.3%) |
| Study Measure | 1092 (51%) |
Children are included in the primary analytic sample if they had at least one BMI in both the pre-pandemic period (October 2017 through February 2020) and the pandemic-period (March 2020 through May 2021).
Includes some college with no degree; Associate degrees (AA, AS); trade school, or higher levels of education.
Mean BMI in the pre-pandemic period was 17.05 (SD 3.3), and an average of 2.6 BMI measures per child were reported across the study period. Pre-pandemic, 80% of BMI measures were ascertained through study measurement compared to 51% of during-pandemic BMI measures. Pre-pandemic, 6.3% of BMI measures were parent or self-reported and 14% were by medical record abstraction, while during-pandemic, 48% were by parent or self-report and 1.3% were by medical record abstraction.
No annual increase in BMI was observed prior to the pandemic, after adjusting for age, sex, race, ethnicity, maternal education, household income, type of BMI measure, and baseline BMI category (−0.04 change in BMI per year, 95% CI: −0.15, 0.07). During the pandemic, the annual change in BMI was 0.24 higher than during the pre-pandemic period (95% CI 0.02, 0.45) (Table 2, Model A). Higher rates of BMI increase during the COVID-19 pandemic period were observed among obese, compared to healthy weight, children. The annual change in BMI during the pandemic, compared to pre-pandemic, among obese children was 1.12 (95% CI 0.47, 1.77) higher than among healthy weight children (Table 2, Model B). There was no observed increase in the rate of change in BMI during the pandemic for Black Children, Hispanic children, or overweight children (Table 2, Models D and B). Children in households with income of $75,000 or greater had decreases in rate of BMI change during the pandemic (−0.83 BMI, 95% CI −1.53, −0.14) (Table 2, Model C).
Table 2:
Longitudinal Associations with Change in BMI from October 2017 – May 2021 (n=1996 children)1
| Model A2 | Model B2 | Model C2 | Model D2 | |
|---|---|---|---|---|
| Change in BMI | ||||
| Pre-pandemic change in BMI per year | −0.04 (−0.15, 0.07) | −0.01 (−0.13, 0.12) | −0.1 (−0.42, 0.21) | −0.05 (−0.2, 0.1) |
| Excess change in BMI during pandemic | 0.24 (0.02, 0.45) | 0.16 (−0.09, 0.41) | 0.83 (0.2, 1.45) | 0.26 (−0.04, 0.56) |
| Excess change in BMI during pandemic among overweight children | −0.39 (−1.05, 0.27) | |||
| Excess change in BMI during pandemic among obese children | 1.12 (0.47, 1.77) | |||
| Excess change in BMI during pandemic among children in households with income of $30–50,000 | −0.01 (−0.95, 0.93) | |||
| Excess change in BMI during pandemic among children in households with income of $50–75,000 | −0.25 (−1.09, 0.58) | |||
| Excess change in BMI during pandemic among children in households with income of $75,000 | −0.83 (−1.53, −0.14) | |||
| Excess change in BMI during pandemic among Hispanic children | 0.09 (−0.5, 0.69) | |||
| Excess change in BMI during pandemic among Black children | 0.28 (−0.35, 0.92) | |||
| Baseline Characteristics | ||||
| Race/Ethnicity (REF: Non-Hispanic White) | ||||
| Non-Hispanic Black | 0.55 (0.23, 0.88) | 0.55 (0.22, 0.87) | 0.54 (0.22, 0.87) | 0.13 (−0.65, 0.91) |
| Non-Hispanic other race | 0.15 (−0.13, 0.43) | 0.15 (−0.13, 0.43) | 0.13 (−0.15, 0.41) | −0.03 (−0.79, 0.73) |
| Hispanic, all races | 0.13 (−0.16, 0.41) | 0.13 (−0.15, 0.41) | 0.12 (−0.17, 0.4) | 0.09 (−0.61, 0.78) |
| Income (REF: Less than $30,000) | ||||
| $30–50,000 | −0.26 (−0.65, 0.13) | −0.25 (−0.64, 0.13) | −0.39 (−1.42, 0.65) | −0.25 (−0.64, 0.14) |
| $50–75,000 | −0.29 (−0.69, 0.11) | −0.28 (−0.67, 0.11) | −0.28 (−1.32, 0.75) | −0.28 (−0.68, 0.12) |
| $75,000 or more | −0.68 (−1.04, −0.32) | −0.68 (−1.03, −0.32) | −0.21 (−1.08, 0.66) | −0.68 (−1.04, −0.32) |
| BMI Category at Baseline (REF: Healthy weight) | ||||
| Overweight | 2.87 (2.59, 3.16) | 2.71 (1.93, 3.49) | 2.88 (2.6, 3.16) | 2.88 (2.59, 3.16) |
| Obese | 6.93 (6.64, 7.23) | 7.19 (6.43, 7.95) | 6.94 (6.65, 7.24) | 6.93 (6.64, 7.23) |
| Intercept | 14.13 (13.42,14.84) | 14.11 (13.39,14.83) | 13.96 (12.99,14.93) | 14.27 (13.53,15.02) |
Children are included in the primary analytic sample if they had at least one BMI in both the pre-pandemic period (October 2017 through February 2020) and the pandemic-period (March 2020 through May 2021).
In addition to the factors shown above, all models adjusted for: age, sex, maternal education (less than high school; high school or GED equivalent; or at least some college or more), type of BMI measure (self-report, parent-report, medical record, or study measure), and an indicator for pre- or during COVID. Models B through D also include group-specific estimates of the pre-pandemic change in BMI.
Sensitivity Analyses
Completing a cohort study visit during the COVID-19 pandemic (whether in-person or by teleconference/telephone) was a burden that we hypothesized would be met by a population that would be sociodemographically different than the overall group of cohort enrollees. To test this hypothesis, we compared our primary analytic sample to the larger group of children enrolled in ECHO who had study visits during our pre-pandemic period but not during the COVID-19 pandemic period (Supplement Table 1). Our primary sample differed from our comparison sample in several important respects. The comparison sample had a higher proportion of Hispanic children (21% compared to 16% in the primary analytic sample) and a lower proportion of non-Hispanic white children (49% compared to 53%). The comparison sample had lower maternal education (81% with some college or more) and lower annual household income (38% with $75,000 or more).
In our second sensitivity analysis to determine if there were temporal trends in BMI change before the COVID-19 pandemic that may explain our main results, we observed no increase in BMI during the first half of the pre-pandemic period, and no statistically significant difference in slope in the final year of the pre-pandemic period (Supplement Table 2). In other words, the COVID-19 pandemic period appears to have a unique effect on trends in BMI among our study sample.
In our third sensitivity analysis, in the subsample of 1052 children who had study measured height and weight before and after the COVID-19 pandemic, similar results are observed as in our primary analytic sample (Supplement Table 2): there was a statistically significant increase in the change in BMI in the COVID-19 pandemic period as compared to previous years after restricting to children with a study measured height and weight only (Supplement Table 2: 0.42, 95% CI 0.1, 0.74).
DISCUSSION
Our study shows that one important effect of the COVID-19 pandemic is an increase in BMI during the COVID-19 pandemic period compared with the three prior years among children in our national cohort. Using populations combined from multiple prospective cohort studies, our findings underscore what other studies have shown both within16–18,34,35 and outside of the US13,36–38. We find that the COVID-19 pandemic period was associated with an excess increase in BMI of 0.24 kg/m2 per year more than in the previous pre-pandemic period, even when controlling for socioeconomic status, race and ethnicity, baseline BMI category, and type of BMI ascertainment. Our findings validate the predictions of many scholars that weight would increase among children due to the cumulative effects of anticipated decreases in physical activity and increases in sedentary behavior, screen time, and high-calorie diets among children during the pandemic12. Importantly, our study is the first to demonstrate this excess weight gain while controlling for individual SES, an important known predictor of obesity among children.
Alongside the COVID-19 pandemic, our data also highlight known risks of higher BMI among children reporting Black race, Hispanic ethnicity, and lower annual household income. Racial, ethnic, and socioeconomic disparities in obesity prevalence in the US have been well-documented, resulting in a disproportionate burden of physical and mental health consequences of obesity among vulnerable children and adults, reflecting exposure to structural racism and other social and economic determinants of health39. The COVID-19 pandemic has also disproportionately affected these same higher-risk groups in terms of both mortality and morbidity from COVID-19 infections in their families and communities40. Our study did not find widening disparities in BMI increase during the pandemic among Black or Hispanic children. It is important to note that these groups only comprised 15% and 16% of our sample size, respectively, so we may have been underpowered to detect differences among these subgroups. We encourage ongoing investigation of potential disparities among racial and ethnic minority children due to the pandemic. We observed increasing disparities due to socioeconomic position. Children living in households in the highest income category experienced decreases in BMI during this time, perhaps reflecting greater access to green space, nutritious foods, and other material conditions conducive to healthy growth. It will be important to collect more data on BMI change in children specifically among vulnerable subpopulations as the pandemic continues to alter children’s lives and use these data to inform evidenced-based interventions in order to reduce rather than augment health inequities.
The observed excess increase in BMI among children in our study during the COVID-19 pandemic will lead to a greater propensity for children to transition from a healthy BMI to one that is overweight/obese, which will only exacerbate the epidemic of obesity that is already a major public health concern across the US. Children with overweight and obesity are known to be at increased risk for poor physical and mental health outcomes41,42. Once weight is gained it is difficult to lose; thus much effort has been focused on primary prevention methods for avoiding excess weight gain and obesity during childhood43. Our study showed a more pronounced BMI increase during the COVID-19 pandemic among children categorized as obese in the baseline pre-pandemic period, putting this subgroup at further increased risk for adverse health outcomes.
We do note that our primary analytic sample is comprised of fewer children from higher-risk subgroups than our larger body of children enrolled in ECHO and therefore likely also when compared to the general US population. This is not surprising because the children in the primary analytic sample are those that were able to fulfill a cohort study visit during a global pandemic. We suspect that if we had BMI data during the COVID-19 year for our broader ECHO community, we would have witnessed an even greater increase in BMI during the widespread closures associated with the COVID-19 pandemic, as was observed in a recent publication of children living in the US16. We call for further research to quantify fully the impact of the pandemic on childhood obesity in the US.
Our analysis has several limitations. First, we bring together pediatric cohorts with different visit structures; therefore, the timing of measurements of child height and weight was not uniform. Second, the height and weight measurements were assessed differently through either self-report, medical record extraction, or direct measurement by trained study personnel, with and without repeated measurements per visit and/or adherence to ECHO measurement protocols. The method of ascertainment also differed pre- and during- pandemic. However, a sensitivity analysis of children with only study-measured height and weight mirrored our main findings. Of note, parent or self-reported weight often underestimates true weight44,45, and therefore findings of weight gain in this study that are partially informed by self-reported weight is likely an underestimation of the true weight gain, since a higher proportion of measures were self-report in the pandemic period.
CONCLUSION
This analysis documents an increase in BMI during the COVID-19 pandemic, in our national cohort of children. We highlight the need for targeted interventions to combat the physical and mental health consequences of the COVID-19 pandemic, particularly among higher-risk communities. Without more vigorous intervention, we can anticipate an exacerbation of the obesity epidemic among US children.
Supplementary Material
What’s known on this subject:
The COVID-19 pandemic may have increased the risk of excess weight gain for children, potentially due to closures of schools and recreational facilities with consequent reduction of physical activity and dietary changes.
What this study adds:
This analysis documents an increase in rate of BMI change during the COVID-19 pandemic compared to prior years, particularly among children who were obese at baseline. Higher household income appears to be protective of pandemic-related BMI increases.
Acknowledgments
The authors wish to thank our ECHO colleagues, the medical, nursing, and program staff, as well as the children and families participating in the ECHO cohorts. We also acknowledge the contribution of the following ECHO program collaborators:
Coordinating Center: Duke Clinical Research Institute, Durham, North Carolina: Smith PB, Newby KL, Benjamin DK; Data Analysis Center: Johns Hopkins University Bloomberg School of Public Health, Baltimore, Maryland: Jacobson LP; Research Triangle Institute, Durham, North Carolina: Parker CB; Northeastern University, Boston, Massachusetts: Alshawabkeh AN; Albert Einstein College of Medicine, Bronx, New York: Aschner JL; Massachusetts General Hospital, Boston: Camargo CA; University of Colorado Anschutz Medical Campus, Aurora, Colorado: Dabelea D; Memorial Hospital of Rhode Island, Pawtucket: Deoni S, D’Sa VA; Emory University, Atlanta, Georgia: Dunlop AL, Brennan PA, Corwin EJ; Avera McKennan Hospital and University Health Center, Sioux Falls, South Dakota: Elliott AJ; Kaiser Permanente, Oakland, California: Ferrara A, Croen LA; Vanderbilt University Medical Center, Nashville, Tennessee: Hartert T; Dartmouth College, Hanover, New Hampshire: Karagas MR; University of Washington, Seattle: Karr C, Sathyanarayana S; University of California, San Francisco: Lewinn KZ; Bush NR; University of Tennessee Health Sciences Center: Mason A; Women & Infants Hospital of Rhode Island, Providence: Lester B; University of Oregon, Eugene: Leve LD; Brigham & Women’s Hospital, Boston, Massachusetts: Litonjua AA, Weiss ST; Oregon Health & Science University, Portland, Oregon: McEvoy CT, Spindel ER; University of Rochester, New York: O’Connor TG, Buss C, Miller RK, Wadhwa PD; University of North Carolina, Chapel Hill: O’Shea M, Fry R; Columbia University, New York, New York: Perera FP, Herbstman JB; University of Illinois, Urbana: Schantz SL; University of Utah, Salt Lake City: Stanford JB, Clark EB, Porucznik C; Icahn School of Medicine at Mount Sinai, Boston, Massachusetts: Wright RJ, Wright RO.
Funding:
Research reported in this publication was supported by the Environmental influences on Child Health Outcomes (ECHO) program, Office of The Director, National Institutes of Health, under Award Numbers U2COD023375 (Coordinating Center), U24OD023382 (Data Analysis Center), U24OD023319 (PRO Core), UH3 OD023318 (Dunlop), UH3 OD023320 (Aschner), UH3 OD023249 (Stanford), UH3 OD023282 (Gern), UH3 OD023337 (Wright), UH3 OD023349 (O’Connor), UH3 OD023288 (McEvoy), UH3 OD023348 (O’Shea), UH3 OD023313 (Deoni), UH3 OD023275 (Karagas), UH3 OD023290 (Herbstman), UH3 OD023248 (Dabelea), UH3 OD023389 (Leve), UH3 OD023289 (Ferrara), UH3 OD023251 (Alshawabkeh), UH3 OD023287 (Breton), UH3 OD023279 (Elliott), and UH3 OD023253 (Camargo).
Role of funding agency
The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Abbreviations:
- BMI
Body mass index
Footnotes
Publisher's Disclaimer: This is a prepublication version of an article that has undergone peer review and been accepted for publication but is not the final version of record. This paper may be cited using the DOI and date of access. This paper may contain information that has errors in facts, figures, and statements, and will be corrected in the final published version. The journal is providing an early version of this article to expedite access to this information. The American Academy of Pediatrics, the editors, and authors are not responsible for inaccurate information and data described in this version.
All authors approved the final manuscript as submitted and agree to be accountable for all aspects of the work.
Conflict of Interest: The authors have no relevant conflicts of interest to disclose.
References
- 1.Fryar CD CM, Afful J. Prevalence of overweight, obesity, and severe obesity among children and adolescents aged 2–19 years: United States, 1963–1965 through 2017–2018. NCHS Health E-Stats. 2020. [Google Scholar]
- 2.Dunton GF, Do B, Wang SD. Early effects of the COVID-19 pandemic on physical activity and sedentary behavior in children living in the U.S. BMC public health. 2020;20(1):1351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bates LC, Zieff G, Stanford K, et al. COVID-19 Impact on Behaviors across the 24-Hour Day in Children and Adolescents: Physical Activity, Sedentary Behavior, and Sleep. Children (Basel, Switzerland). 2020;7(9). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.von Hippel P Paul T., Powell Brian, PhD, Downey Douglas B., PhD, and Rowland Nicholas J., MA. The Effect of School on Overweight in Childhood: Gain in Body Mass Index During the School Year and During Summer Vacation. American journal of public health. 2007;97(4):696–702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.von Hippel PT, Workman J. From Kindergarten Through Second Grade, U.S. Children’s Obesity Prevalence Grows Only During Summer Vacations. Obesity. 2016;24(11):2296–2300. [DOI] [PubMed] [Google Scholar]
- 6.Franckle R, Adler R, Davison K. Accelerated Weight Gain Among Children During Summer Versus School Year and Related Racial/Ethnic Disparities: A Systematic Review. Preventing chronic disease. 2014;11:E101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Moreno JP, Johnston CA, Woehler D. Changes in weight over the school year and summer vacation: results of a 5-year longitudinal study. The Journal of school health. 2013;83(7):473–477. [DOI] [PubMed] [Google Scholar]
- 8.Tanskey LA, Goldberg J, Chui K, Must A, Sacheck J. The State of the Summer: a Review of Child Summer Weight Gain and Efforts to Prevent It. Current obesity reports. 2018;7(2):112–121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Brazendale K, Beets MW, Weaver RG, et al. Understanding differences between summer vs. school obesogenic behaviors of children: the structured days hypothesis. International Journal of Behavioral Nutrition and Physical Activity. 2017;14(1):100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Whitaker RC, Pepe MS, Wright JA, Seidel KD, Dietz WH. Early adiposity rebound and the risk of adult obesity. Pediatrics. 1998;101(3):E5. [DOI] [PubMed] [Google Scholar]
- 11.Whitaker RC, Wright JA, Pepe MS, Seidel KD, Dietz WH. Predicting obesity in young adulthood from childhood and parental obesity. The New England journal of medicine. 1997;337(13):869–873. [DOI] [PubMed] [Google Scholar]
- 12.Rundle AG, Park Y, Herbstman JB, Kinsey EW, Wang YC. COVID-19-Related School Closings and Risk of Weight Gain Among Children. Obesity. 2020;28(6):1008–1009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Baysun Ş, Akar MN. WEIGHT GAIN IN CHILDREN DURING THE COVID-19 QUARANTINE PERIOD. Journal of paediatrics and child health. 2020;56(9):1487–1488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Workman J. How Much May COVID-19 School Closures Increase Childhood Obesity? Obesity. 2020;28(10):1787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Calcaterra V, Vandoni M, Pellino VC, Cena H. Special Attention to Diet and Physical Activity in Children and Adolescents With Obesity During the Coronavirus Disease-2019 Pandemic. Frontiers in pediatrics. 2020;8:407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lange SJ, Kompaniyets L, Freedman DS, et al. Longitudinal Trends in Body Mass Index Before and During the COVID-19 Pandemic Among Persons Aged 2–19 Years – United States, 2018–2020. MMWR Morbidity and mortality weekly report. 2021;70(37):1278–1283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Woolford SJ, Sidell M, Li X, et al. Changes in Body Mass Index Among Children and Adolescents During the COVID-19 Pandemic. Jama. 2021;326(14):1434–1436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Weaver RG, Hunt ET, Armstrong B, et al. COVID-19 Leads to Accelerated Increases in Children’s BMI z-Score Gain: An Interrupted Time-Series Study. American journal of preventive medicine. 2021;61(4):e161–e169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Yang S, Guo B, Ao L, et al. Obesity and activity patterns before and during COVID-19 lockdown among youths in China. Clinical obesity. 2020;10(6):e12416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Derya Adıbelli AS. The effect of the coronavirus (COVID-19)pandemic on health-related quality of life in children. Children and Youth Services Review. 2020;119(105595). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Vazquez CE, Cubbin C. Socioeconomic Status and Childhood Obesity: a Review of Literature from the Past Decade to Inform Intervention Research. Current obesity reports. 2020;9(4):562–570. [DOI] [PubMed] [Google Scholar]
- 22.Thomeer MB, Yahirun J, Colón-López A. How Families Matter for Health Inequality during the COVID-19 Pandemic. Journal of family theory & review. 2020;12(4):448–463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Gillman MW, Blaisdell CJ. Environmental influences on Child Health Outcomes, a Research Program of the National Institutes of Health. Current Opinion in Pediatrics. 2018;30(2):260–262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Romano ME, Buckley JP, Elliott AJ, Johnson CC, Paneth N. SPR Perspectives: scientific opportunities in the Environmental influences on Child Health Outcomes Program. Pediatric research. 2021:1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Centers for Disease Control and Prevention. A SAS Program for the 2000 CDC Growth Charts (ages 0 to <20 years). 2019; https://www.cdc.gov/nccdphp/dnpao/growthcharts/resources/sas.htm. Accessed December 9, 2020.
- 26.Department of Health and Human Services, Centers for Disease Control and Prevention, and National Center for Health Statistics. 2000. CDC Growth Charts for United States: Methods and Development. In. Vol Vital and Health Statistics. Hyattsville, Maryland: 2002. [Google Scholar]
- 27.von Hippel PT, Nahhas RW, Czerwinski SA. How much do children’s body mass indices change over intervals of 6–12 months? Statistics from before and during the obesity epidemic. Pediatr Obes. 2015;10(6):468–475. [DOI] [PubMed] [Google Scholar]
- 28.Cole TJ, Faith MS, Pietrobelli A, Heo M. What is the best measure of adiposity change in growing children: BMI, BMI %, BMI z-score or BMI centile? European journal of clinical nutrition. 2005;59(3):419–425. [DOI] [PubMed] [Google Scholar]
- 29.Berkey CS, Colditz GA. Adiposity in adolescents: change in actual BMI works better than change in BMI z score for longitudinal studies. Annals of epidemiology. 2007;17(1):44–50. [DOI] [PubMed] [Google Scholar]
- 30.Barlow SE. Expert committee recommendations regarding the prevention, assessment, and treatment of child and adolescent overweight and obesity: summary report. Pediatrics. 2007;120 Suppl 4:S164–192. [DOI] [PubMed] [Google Scholar]
- 31.Bailey ZD, Krieger N, Agénor M, Graves J, Linos N, Bassett MT. Structural racism and health inequities in the USA: evidence and interventions. The Lancet. 2017;389(10077):1453–1463. [DOI] [PubMed] [Google Scholar]
- 32.van Buuren S, Groothuis-Oudshoorn K. mice: Multivariate Imputation by Chained Equations in R. Journal of Statistical Software. 2011;45(3):1– 67. [Google Scholar]
- 33.Bates D, Mächler M, Bolker B, Walker S. Fitting Linear Mixed-Effects Models Using lme4. Journal of Statistical Software. 2015;67(1):1–48. [Google Scholar]
- 34.Brazendale K, Garcia J, Hunt ET, Blankenship M, Eisenstein D, Leon A. Preliminary Evidence of Children’s Weight Gain From 5 Months of Home Quarantine During the COVID-19 Pandemic. American Journal of Lifestyle Medicine. 0(0):15598276211006657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Mulugeta W, Hoque L. Impact of the COVID-19 lockdown on weight status and associated factors for obesity among children in Massachusetts. Obesity Medicine. 2021;22:100325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Vinker-Shuster M, Grossman ES, Yeshayahu Y. Increased Weight Gain of Children during the COVID-19 Lockdown. The Israel Medical Association journal : IMAJ. 2021;23(4):219–222. [PubMed] [Google Scholar]
- 37.Koletzko B, Holzapfel C, Schneider U, Hauner H. Lifestyle and Body Weight Consequences of the COVID-19 Pandemic in Children: Increasing Disparity. Annals of nutrition & metabolism. 2021;77(1):1–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Stavridou A, Kapsali E, Panagouli E, et al. Obesity in Children and Adolescents during COVID-19 Pandemic. Children (Basel, Switzerland). 2021;8(2):135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Wang Y, Beydoun MA, Min J, Xue H, Kaminsky LA, Cheskin LJ. Has the prevalence of overweight, obesity and central obesity levelled off in the United States? Trends, patterns, disparities, and future projections for the obesity epidemic. International journal of epidemiology. 2020;49(3):810–823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Moore JT, Ricaldi JN, Rose CE, et al. Disparities in Incidence of COVID-19 Among Underrepresented Racial/Ethnic Groups in Counties Identified as Hotspots During June 5–18, 2020 – 22 States, February-June 2020. MMWR Morbidity and mortality weekly report. 2020;69(33):1122–1126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Singh AS, Mulder C, Twisk JW, van Mechelen W, Chinapaw MJ. Tracking of childhood overweight into adulthood: a systematic review of the literature. Obesity reviews : an official journal of the International Association for the Study of Obesity. 2008;9(5):474–488. [DOI] [PubMed] [Google Scholar]
- 42.Daniels SR, Arnett DK, Eckel RH, et al. Overweight in children and adolescents: pathophysiology, consequences, prevention, and treatment. Circulation. 2005;111(15):1999–2012. [DOI] [PubMed] [Google Scholar]
- 43.Sanyaolu A, Okorie C, Qi X, Locke J, Rehman S. Childhood and Adolescent Obesity in the United States: A Public Health Concern. Glob Pediatr Health. 2019;6:2333794X19891305–12333794X19891305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Wright DR, Glanz K, Colburn T, Robson SM, Saelens BE. The accuracy of parent-reported height and weight for 6–12 year old U.S. children. BMC pediatrics. 2018;18(1):52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Sherry B, Jefferds ME, Grummer-Strawn LM. Accuracy of adolescent self-report of height and weight in assessing overweight status: a literature review. Archives of pediatrics & adolescent medicine. 2007;161(12):1154–1161. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


