Abstract
Background
The impact of the COVID‐19 pandemic on out‐of‐hospital cardiac arrest (OHCA) burden of disease in the United States is unknown. We sought to estimate and compare disability‐adjusted life years (DALYs) lost because of OHCA during the COVID‐19 pandemic to prepandemic values.
Methods
DALY were calculated as the sum of years of life lost (YLL) and years lived with disability (YLD). Adult non‐traumatic emergency medical services‐treated OHCA from the Cardiac Arrest Registry to Enhance Survival database for 2016 to 2020 were used to estimate YLL. Cerebral performance category score disability weights were used to estimate YLD. The calculated DALY for the study population was extrapolated to a national level to estimate total US DALY. Data were reported as DALY total and rate. Data for 2020 (pandemic) were compared prepandemic years (2016–2019) via the chi‐square test or t‐test, as appropriate.
Results
A total of 440,438 OHCA met study inclusion criteria. Total OHCA DALY in the United States increased from 4,468,155 (YLL = 4,463,988; YLD = 4167) in 2019 to 5,379,660 (YLL = 5,375,464; YLD = 4197) in 2020. The DALY rate increased from 1357 per 100,000 individuals in 2019 to 1630 per 100,000 individuals in 2020. Bystander cardiopulmonary resuscitation (CPR) rates did not significantly change (47.96% in 2016–2019 vs. 47.89% in 2020; p = 0.157).
Conclusion
The overall burden of disease because of adult OHCA increased significantly during the COVID‐19 pandemic. We observed no change in the willingness of layperson bystanders to perform CPR on a national level in the United States.
Keywords: burden of disease, COVID‐19, out‐of‐hospital cardiac arrest
1. INTRODUCTION
1.1. Background
Sudden out‐of‐hospital cardiac arrest (OHCA) is a leading cause of morbidity and mortality in the United States. 1 , 2 , 3 Recent reports have indicated that the incidence of OHCA has increased, and outcomes have worsened since the emergence of the COVID‐19 pandemic. 4 However, the overall impact of COVID‐19 on OHCA disease burden remains poorly understood, and has not been described using common public health metrics such as disability‐adjusted life years (DALYs).
1.2. Importance
The DALY combines morbidity and mortality into a single value and are commonly used to estimate the public health impact of a disease. DALYs are the sum of years of life lost (YLL) and years lived with disability (YLD). 5 One DALY is equal to 1 year of healthy life lost. We have previously published methodology to consistently estimate DALY for OHCA using data from the Cardiac Arrest Registry to Enhance Survival (CARES), and found adult OHCA to be a leading cause of annual DALY lost in the United States. 2 , 3 The impact of the COVID‐19 pandemic on OHCA DALY is currently unknown.
1.3. Goals of this investigation
In an effort to fill this knowledge gap, we estimated and compared the DALY lost because of OHCA in the United States during 2020 to prepandemic values (2016 to 2019). We hypothesized that OHCA DALY would increase in 2020 compared to previous years and that bystander interventions including cardiopulmonary resuscitation (CPR) would decrease owing to responder hesitancy and concern for possible transmission of infection. 6 The overall goals were to (1) inform clinicians, educators, and the public of potential changes in the health burden associated with OHCA; and (2) assess trends in bystander response during the COVID‐19 pandemic.
2. METHODS
2.1. Study aim, design, and population
The primary aim was to estimate DALY values because of OHCA in 2020 and to compare them to DALY values from prepandemic years (2016–2019). Our secondary aim was to evaluate the impact of bystander‐CPR (B‐CPR) participation, pre‐ and postpandemic, on DALY values. To do so, we performed a retrospective analysis of all adult non‐traumatic emergency medical services (EMS)‐treated OHCA from the national CARES database from 2016 to 2020. The University of Alabama at Birmingham Institutional Review Board determined the analysis to be “not human subjects research.”
The Bottom Line.
The COVID‐19 pandemic affected both care processes and outcomes for out‐of‐hospital cardiac arrest (OHCA), but the impact on burden of disease in the United States was unknown. Using a large, national OHCA registry, the authors described in over 440,000 OHCA cases that the total disability‐adjusted life years increased during the COVID‐19 pandemic despite no difference in bystander cardiopulmonary resuscitation rates. Future studies should examine which health care system changes contributed to this change.
Inclusion criteria for this evaluation included all adult (age 18 to 100 years old) non‐traumatic EMS‐treated OHCA in the CARES data set for 2016 to 2020, the most recent year of CARES data available at the time of the analysis. The CARES database does not capture data on cases where resuscitative efforts are not attempted; thus only EMS‐treated OHCA were available for analysis. Excluded from this analysis were records with missing data for age, gender, mortality disposition, or cerebral performance category (CPC) scores, and those above 100 years of age. Records for non‐binary or transgender individuals were also excluded as life expectancy estimates for these populations were not available in the National Vital Statistics Reports 7 , 8 , 9 , 10 and are required for the DALY calculation. Pediatric and traumatic OHCA were also excluded owing to the lack of established disability weights for these populations.
2.2. Cardiac Arrest Registry to Enhance Survival (CARES)
The CARES database was developed in 2004 as a collaborative effort between Emory University and the Centers for Disease Control and Prevention to serve as a central repository for cardiac arrest data from EMS systems throughout the United States. 11 The registry uses the Utstein style of OHCA reporting and includes variables from prehospital care through hospital discharge. 12 The program currently includes 27 state‐based registries and the District of Columbia with community sites in 14 additional states. CARES represents a catchment area of more than 162 million people or approximately 49% of the US population, with more than 2000 EMS agencies, and 2500 participating hospitals. Further details of CARES development, design, and data elements have been previously published. 11
2.3. Disability‐Adjusted Life Years (DALY)
The DALY were defined as the sum of YLL and YLD (ie, DALY = YLL + YLD). 2 , 3 , 5 Annual US population estimates for 2016 to 2020 were used to extrapolate the results to a national level. 13 The estimated CARES population coverage increased substantially from 88,673,688 in 2016 to 143,450,892 in 2020 (Raba Al‐Araji, MPH, unpublished data, 2021).
2.4. Years of Life Lost (YLL)
The YLL were calculated by multiplying the number of deaths due to OHCA (N) by the remaining standard life expectancy at the age of death (L) (ie, YLL = N × L). 2 , 3 , 5 The annual number of deaths due to OHCA were obtained from the national CARES database for 2016 to 2020. Standard life expectancy at the age of death, based on gender and race, were obtained from the National Vital Statistics Report for each corresponding year of CARES data. 7 , 8 , 9 , 10
2.5. Years Lived with Disability (YLD)
The YLD were calculated by multiplying the annual prevalence (P) of OHCA from the CARES database among survivors by a disability weight (DW) associated with the CPC score at time of hospital discharge (ie, YLDyear = P × DW) where prevalence is the number of cases alive for the year with each CPC score. 2 , 3 , 14
2.6. Disability Weights (DWs)
The DWs were used in the calculation of YLD to account for severity of disease and disability. 15 They range from 0 (perfect health) to 1 (worst possible health state). 5 Similar to our previous work, 2 , 3 and based on the findings of Ginsberg et al., 16 the following DWs were assigned to survivors according to CPC score at the time of hospital discharge: CPC 1 = 0.049, CPC 2 = 0.138, CPC 3 = 0.425, and CPC 4 = 0.673. The DW for a CPC 1 was based on the average DW for the 77 survivors with a CPC of 1. 16 To our knowledge, no other DWs have been described within the cardiac arrest literature. Our previously published sensitivity analyses showed a negligible effect on DALY when a uniform distribution of DWs was used in the CARES population. 2 , 3
2.7. Bystander interventions
The analysis for B‐CPR was limited to bystander‐witnessed events and excluded all EMS‐witnessed OHCA and nursing home/health care facility events. The bystander automated external defibrillator (B‐AED) analysis was further limited to OHCA events in a public location (public/commercial building, street/highway, place of recreation, industrial place, transport center, and other) and additionally excluded events where the first responder was the first person to use the AED (ie, only layperson).
2.8. Statistical methods
Continuous variables were summarized as means and SDs and categorical variables were summarized as counts and percentages. We compared variables by year (2016 to 2019 vs. 2020) using the Student's t‐test for continuous variables and the chi‐square test for categorical variables. P values <0.05 were considered to be statistically significant. Because the sample size was anticipated to be quite large (making differences between years statistically significant but not necessarily clinically significant), we further derived standardized differences using the method of Yang and Dalton. 17 We note that often standardized differences >0.1 are considered to be clinically significant. 18 All analyses were done using Stata/MP 15.1 for Windows 19 (StataCorp LLC, College Station, Texas, USA).
3. RESULTS
There were a total of 453,822 OHCA records available in the CARES database for the study period. A total of 12,028 (2.7%) pediatric (age <18 years) and advanced age adults (age >100 years) were excluded, along with 1463 (0.3%) cases with missing data, resulting in a final sample size of 440,438 (97.0%) records with complete data (Table 1). Demographics, cardiac arrest characteristics, and outcomes for the study population are in Table 2. The overall proportion of patients surviving with good neurologic outcome (CPC 1 or 2) decreased in 2020 compared to the prepandemic period: 7.06% versus 8.51%; p < 0.001. Overall mortality increased in 2020 (91.08%) compared to the prepandemic period (89.51%), p < 0.001. Notably, the percentage of patients dying in the field was much higher in 2020 compared to the prepandemic period: 36.04% versus 43.10%, p < 0.001 and standardized difference = 0.14.
TABLE 1.
Exclusion criteria and derivation of study population
| Exclusion criteria | Total number with this exclusion criterion (not including prior criteria) | Exclude an additional X number of patients | N = 453,822; The initial sample size |
|---|---|---|---|
| Missing gender or non‐binary/transgender | 26 | 26 | 453,796 |
| Missing age | 179 | 177 | 453,619 |
| Age <18 years or Age >100 years | 12,028 | 12,023 | 441,596 |
| Missing hospital outcome | 871 | 797 | 440,799 |
| Missing discharge location for survivors | 13 | 13 | 440,786 |
| Missing CPC score for survivors | 370 | 344 | 440,442 |
| Missing event location | 4 | 4 | Final sample size = 440,438 |
Abbreviation: CPC, cerebral performance category.
TABLE 2.
Patient characteristics stratified by year
| Variable | Years 2016 to 2019 N = 316,309 | Year 2020 N = 124,129 | p value | Standardized difference |
|---|---|---|---|---|
| Age (mean, SD) | 63.8 (16.9) | 63.6 (17.0) | <0.001 | 0.01 |
| % female | 119,720 (37.85%) | 46,918 (37.80%) | 0.752 | <0.01 |
| Race or ethnicity | ||||
| White | 158,675 (50.156%) | 63,809 (51.41%) | ||
| Black | 71,113 (22.48%) | 28,514 (22.97%) | ||
| Hispanic | 18,625 (5.89%) | 9826 (7.92%) | <0.001 | 0.13 |
| Asian | 9252 (2.92%) | 3888 (3.13%) | ||
| Other/unknown | 58,644 (18.53%) | 18,092 (14.57%) | ||
| Location category | ||||
| Home/residence | 219,832 (69.50%) | 91,815 (73.97%) | ||
| Nursing home/health care facility | 47,628 (15.06%) | 17,745 (14.30%) | <0.001 | 0.12 |
| Public | 48,849 (15.44%) | 14,569 (11.74%) | ||
| Arrest witnessed status | ||||
| Unwitnessed | 157,295 (49.73%) | 61,679 (49.69%) | ||
| Witnessed by 911 responder | 39,933 (12.62%) | 16,119 (12.99%) | 0.007 | 0.01 |
| Witnessed by bystander | 119,070 (37.64%) | 46,325 (37.32%) | ||
| Missing | 11 (0.00%) | 6 (0.00%) | ||
| Presumed cardiac arrest etiology | ||||
| Cardiac (presumed) | 262,743 (83.07%) | 101,210 (81.54%) | ||
| Respiratory/asphyxia | 28,458 (9.00%) | 11,492 (9.26%) | ||
| Drug overdose | 15,336 (4.85%) | 7991 (6.44%) | <0.001 | 0.08 |
| Exsanguination or hemorrhage | 1911 (0.60%) | 996 (0.80%) | ||
| Drowning/submersion | 1619 (0.51%) | 560 (0.45%) | ||
| Electrocution | 202 (0.06%) | 101 (0.08%) | ||
| Other | 6040 (1.91%) | 1779 (1.43%) | ||
| Who first performed CPR* | ||||
| Bystander | 91,981 (39.45%) | 36,691 (39.98%) | ||
| EMS | 62,084 (26.63%) | 24,009 (26.16%) | 0.002 | <0.01 |
| First responder | 79,059 (33.91%) | 31,047 (33.83%) | ||
| Unknown | 43 (0.02%) | 29 (0.03%) | ||
| Bystander CPR (*Bystander witnessed OHCA events only also excluding EMS‐witnessed and nursing home/health care facility events) | ||||
| All locations | 49,431 (47.96%); N = 103,058 | 19,482 (47.89%); N = 40,682 | 0.153 | <0.01 |
| Public location only | 13,964 (55.97%); N = 24,948 | 3702 (53.85%); N = 6875 | 0.007 | 0.04 |
| Home location only | 35,467 (45.41%); N = 78,110 | 15,780 (46.68%); N = 33,807 | <0.001 | 0.03 |
| Was an AED applied before EMS? | ||||
| No | 224,138 (70.86%) | 90,886 (73.22%) | ||
| Yes, with defibrillation | 23,103 (7.30%) | 7458 (6.01%) | <0.001 | 0.05 |
| Yes, without defibrillation | 69,056 (21.83%) | 25,783 (20.77%) | ||
| Was bystander AED applied before EMS in a public location? | ||||
| No | 38,048 (88.11%) | 11,700 (91.02%) | ||
| Yes | 5134 (11.89%) | 1154 (8.98%) | <0.001 | 0.10 |
| First documented rhythm category | ||||
| Asystole | 155,848 (49.27%) | 65,608(52.85%) | ||
| Idioventricular/PEA | 69,664 (22.02%) | 27,677 (22.30%) | ||
| Unknown unshockable | 30,449 (9.63%) | 10,126 (8.16%) | ||
| Ventricular fibrillation | 43,024 (13.60%) | 14,871 (11.98%) | <0.001 | 0.09 |
| Ventricular tachycardia | 4073 (1.29%) | 1562 (1.26%) | ||
| Unknown shockable | 13,215 (4.18%) | 4273 (3.44%) | ||
| Missing | 36 (0.01%) | 12 (0.01%) | ||
| Survived to hospital admission | ||||
| No | 226,800 (71.70%) | 94,340 (76.00%) | <0.001 | 0.10 |
| Yes | 89,509 (28.30%) | 29,789 (24.00%) | ||
| Died in the field (Yes) | 113,986 (36.04%) | 53,496 (43.10%) | <0.001 | 0.14 |
| Final outcome | ||||
| CPC = 1 | 21,064 (6.66%) | 7131 (5.74%) | ||
| CPC = 2 | 5861 (1.85%) | 1643 (1.32%) | ||
| CPC = 3 | 3467 (1.10%) | 1203 (0.97%) | <0.001 | 0.06 |
| CPC = 4 | 2776 (0.88%) | 1096 (0.88%) | ||
| Died | 283,141 (89.51%) | 113,056 (91.08%) | ||
| Discharge location | ||||
| Home/residence | 20,887 (6.60%) | 7215 (5.81%) | ||
| Rehabilitation facility | 5387 (1.70%) | 1563 (1.26%) | <0.001 | 0.06 |
| Skilled nursing facility | 6894 (2.18%) | 2295 (1.85%) | ||
Abbreviations: AED, automated external defibrillator; CPC, cerebral performance category; CPR, cardiopulmonary resuscitation; EMS, emergency medical services; OHCA; out‐of‐hospital cardiac arrest; PEA, pulseless electrical activity.
The proportion of OHCA in a home/private residence increased from 69.5% prepandemic to 73.9% in 2020, p < 0.001. Accordingly, a decrease in OHCA in a public location was observed from 15.4% prepandemic to 11.7% in 2020, p < 0.001 (Figure 1). Layperson B‐CPR rates remained stable (47.96% in 2016–2019 vs. 47.89% in 2020 p = 0.153). However, there were modest decreases in B‐CPR in public locations and increases in B‐CPR in home locations in 2020 compared to the prepandemic years (see Table 2). B‐AED application before EMS arrival in a public location decreased significantly in 2020 compared to the prepandemic years: 11.89% versus 8.98%, p < 0.001 and standardized difference = 0.10.
FIGURE 1.
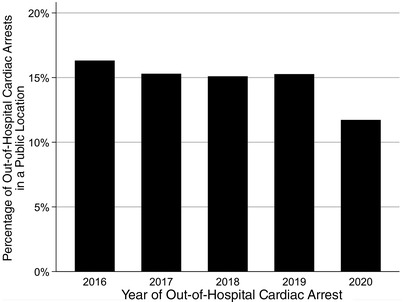
Percentage of out‐of‐hospital cardiac arrests in a public location by year
At the patient level, the mean (SD) DALY per OHCA increased from 18.2 (13.4) in 2019 to 18.8 (13.5) in 2020 (Table 3). The total DALY for the study population increased from 1,790,554 (YLL = 1,788,884; YLD = 1670) in 2019 to 2,339,405 (YLL = 2,337,580; YLD = 1825) in 2020. Total US OHCA DALY increased from 4,468,155 (YLL = 4,463,988; YLD = 4167) in 2019 to 5,379,660 (YLL = 5,375,464; YLD = 4197) in 2020. The DALY rate increased from 1357 per 100,000 individuals in 2019 to 1630 per 100,000 individuals in 2020. When mean DALY scores were plotted by month stratified by year, the DALY values were consistently higher in 2020 starting in April (see Figure 2).
TABLE 3.
Annual disability‐adjusted life years lost for study population and US population stratified by year
| 2016 | 2017 | 2018 | 2019 | 2020 | |
|---|---|---|---|---|---|
| Study population | |||||
| Total DALY | 1,092,961 | 1,368,624 | 1,456,499 | 1,790,554 | 2,339,405 |
| YLL | 1,092,037 | 1,367,430 | 1,455,215 | 1,788,884 | 2,337,580 |
| YLD | 923.6 | 1,194.50 | 1283.8 | 1670 | 1825 |
| Mean DALY (SD) | 18.3 (13.5) | 18.5 (13.7) | 18.4 (13.5) | 18.2 (13.4) | 18.8 (13.5) |
| US population | |||||
| Total DALY | 3,982,065 | 4,335,949 | 4,326,745 | 4,468,155 | 5,379,660 |
| YLL | 3,978,698 | 4,332,166 | 4,322,931 | 4,463,988 | 5,375,464 |
| YLD | 3365 | 3784 | 3814 | 4167 | 4197 |
| DALY rate (per 100,000 individuals) | 1232.6 | 1333.5 | 1322.4 | 1357.4 | 1630.8 |
Abbreviations: DALY, disability‐adjusted life years; YLL, years of life lost; YLD, years lived with disability.
FIGURE 2.
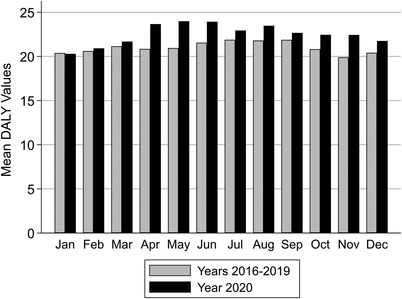
Mean DALY values by month for years 2016 to 2019 versus 2020. Abbreviation: DALY, disability‐adjusted life‐year.
4. DISCUSSION
DALY have been used as a key public health monitoring metric for the past 2 decades. 20 Our analysis of over 440,000 records from the national CARES database is the first to evaluate DALY for OHCA since the emergence of the COVID‐19 pandemic. Our most striking finding was that the public health impact of adult non‐traumatic EMS‐treated OHCA significantly increased during the COVID‐19 pandemic compared to prepandemic years. Total DALY lost because of OHCA in the United States increased from 4,468,155 in 2019 to 5,379,660 in 2020.
A number of factors contributed to the increase in DALY we observed. As we have previously described, DALY values for OHCA are driven by an overwhelming contribution of YLL because most patients do not survive the event. 2 , 3 When comparing 2020 to 2016–2019, overall mortality increased significantly from 89.51% to 91.08%, an increase of approximately 1.8%. However, the proportion of patients declared deceased by EMS in the field increased much more dramatically (approximately a 14.0% increase) going from 36.04% to 43.10%; p < 0.001. Furthermore, those who survived were less likely to experience a favorable neurologic outcome 7.06% in 2020 versus 8.51% in 2016–2019; p <0.001. Finally, changes in age, sex, and race are known to affect DALY values because life expectancy varies by these factors in the National Vital Statistics estimates. Comparing 2020 to 2016–2019, a significant increase in Hispanic population was observed (7.9% vs. 5.9% p < 0.001), with a reduction in cases with race documented as “other/unknown” (14.57% vs. 18.53% p = < 0.001).
We have previously attributed increases in OHCA DALY to the expansion of the CARES database, likely resulting in a more nationally representative sample. 3 This was because of observation that increases in the ratio of OHCA cases per catchment population have corresponded to growth in the CARES database. 3 For example, from 2013 to 2017, OHCA DALY increased from 950 per 100,000 to 1333 per 100,000, which coincided with 40% growth in the CARES population catchment (from 61.4 to 102.6 million). 3 For this period, the ratio of cases per population catchment increased by 34% (from 0.00056 to 0.00074). 3 However, in recent years this ratio of cases per population catchment has remained relatively flat despite continued expansion of CARES. For example, from 2017 to 2019, CARES population catchment increased by 22% (from 102.6 to 131.9 million), yet the ratio of cases per population catchment barely increased (0.00074 to 0.00076). For 2020, during the COVID‐19 pandemic, the CARES population catchment increased by 8% (from 131.9 to 143.4 million), whereas the ratio of OHCA cases per population catchment increased significantly, from 0.00076 to 0.00088. Although we cannot quantify the exact amount, we believe these data support the notion that OHCA burden of disease increased in 2020, at least in part, because of OHCA becoming more common and deadly during the COVID‐19 pandemic.
Finally, we hypothesized that the willingness of bystanders to perform CPR would decrease during the COVID‐19 pandemic owing to the public's concern for infection transmission 6 and reports from regions within the United States and Europe describing reduced B‐CPR rates since the emergence of COVID‐19. 21 , 22 , 23 , 24 , 25 However, we found no change in the proportion of bystander‐witnessed OHCA events receiving layperson CPR (47.96% in 2016–2019 vs. 47.89% in 2020; p = 0.153) though there was some evidence that the location of B‐CPR changed modestly during the pandemic (more home than public locations). Because the proportion of OHCA in a home/private residence increased by 4.5%, the overall layperson CPR rates may be influenced by an increase in family members witnessing the OHCA and performing CPR. Overall, our data suggest there has been no change in a willingness of laypersons to perform B‐CPR on a national level which is reassuring.
4.1. Limitations
Participation in CARES is voluntary and our results may be less generalizable to patient populations that are underrepresented in the CARES database or outside of the CARES database due to inherent selection bias. However, the DALY estimate was based on records from the national CARES database, which represents the largest, most robust, OHCA data set available. Our DALY calculation does not include pediatrics, traumatic cardiac arrest, in‐hospital cardiac arrest, or individuals experiencing OHCA where no resuscitative efforts were attempted and thus underestimates the total health burden of cardiac arrest. Additionally, the provision of B‐CPR may be a component of individual EMS protocols for termination of resuscitation, which may bias our finding of an increase in patients declared deceased by EMS in the field during the pandemic period.
The etiology of OHCA can be broad and often overlap with other disease categories. However, overlap between disease categories is common within the Global Burden of Disease study, which is the “gold standard” for DALY assessment (ie, chronic obstructive pulmonary disease and lung cancer; diabetes, stroke, and ischemic heart disease). DWs specific to cardiac arrest victims in the United States are not currently available. The DWs used were prospectively derived in OHCA survivors in Jerusalem, and morbidity after OHCA in the United States may be different, and subsequently require unique DWs. However, our previously published sensitivity analyses showed a negligible effect on DALY when a uniform distribution of DWs was used in the CARES population. 2 , 3 Additionally, patient comorbidities may contribute to overall disability beyond the CPC score at the time of hospital discharge. Unfortunately, comorbidity data are not routinely captured in the CARES database and were subsequently not included in the analysis. Finally, it is unknown how similar the results of 2020 are to 2021 (and beyond) where COVID‐19 is still a public health problem though future analyses of the CARES database would be able to determine this.
5. CONCLUSION
The public health impact of adult non‐traumatic OHCA increased significantly after the emergence of the COVID‐19 pandemic. Modest but statistically significant decreases in survival with good neurological outcome in 2020 were observed and were coupled with more dramatic changes in the number of OHCA patients dying in the field. We observed no significant change in layperson CPR rates on a national level though there was evidence that where B‐CPR is performed (home vs. public locations) has changed during the pandemic. These results should help inform the public, policy makers, and funding agencies of the recent changes in OHCA burden of disease in the United States.
CONFLICTS OF INTEREST
Ryan A. Coute: Society for Academic Emergency Medicine (SAEM) resident research grant, Emergency Medicine Foundation Research Grant, National Institutes of Health Loan Repayment Award, National Heart, Lung, and Blood Institute; Brian H. Nathanson: UAB paid his company, OptiStatim, LLC a consulting fee for statistical services related to the manuscript; Michael C. Kurz, and Timothy J. Mader has no conflicts of interest. CARES receives funding from the American Red Cross and the American Heart Association.
AUTHOR CONTRIBUTIONS
Ryan A. Coute and Timothy J. Mader designed the study, analyzed the data, and wrote the manuscript. Brian H. Nathanson performed the statistical analysis and participated in manuscript writing. Michael C. Kurz participated in manuscript writing and editing. All authors have read and approved of the manuscript.
ACKNOWLEDGMENTS
CARES participating sites can be located at: https://mycares.net/sitepages/map.jsp. This project was funded by a Society for Academic Emergency Medicine Resident Research Grant awarded to Dr. Coute (RF2018‐005).
Biography
Ryan Coute, DO, is an Assistant Professor of Emergency Medicine at the University of Alabama at Birmingham in Birmingham, Alabama. His primary interest is resuscitation science research with a focus on cardiac arrest treatment and outcome disparities, burden of disease estimation, and healthcare policy.
Coute RA, Nathanson BH, Kurz MC, Mader TJ. Estimating the impact of the COVID‐19 pandemic on out‐of‐hospital cardiac arrest burden of disease in the United States. JACEP Open. 2022;3:e12811. 10.1002/emp2.12811
Supervising Editor: Nicholas Johnson, MD.
REFERENCES
- 1. Taniguchi D, Baernstein A, Nichol G. Cardiac arrest: a public health perspective. Emerg Med Clin North Am. 2012;30:1‐12. [DOI] [PubMed] [Google Scholar]
- 2. Coute RA, Nathanson BH, Panchal AR, et al. Disability‐adjusted life years following adult out‐of‐hospital cardiac arrest in the United States. Circ Cardiovasc Qual Outcomes. 2019;12:e004677. [DOI] [PubMed] [Google Scholar]
- 3. Coute RA, Nathanson BH, Mader TJ, McNally B, Kurz MC. Trend analysis of disability‐adjusted life years following adult out‐of‐hospital cardiac arrest in the United States: A study from the CARES Surveillance Group. Resuscitation. 2021;163:124‐129. [DOI] [PubMed] [Google Scholar]
- 4. Teoh SE, Masuda Y, Tan DJH, et al. Impact of the COVID‐19 pandemic on the epidemiology of out‐of‐hospital cardiac arrest: a systematic review and meta‐analysis. Ann Intensive Care. 2021;11:169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Devleesschauwer B, Havelaar AH, Maertens de Noordhout C, et al. Calculating disability‐adjusted life years to quantify burden of disease. Int J Public Health. 2014;59:565‐569. [DOI] [PubMed] [Google Scholar]
- 6. Grunau B, Bal J, Scheuermeyer F, et al. Bystanders are less willing to resuscitate out‐of‐hospital cardiac arrest victims during the COVID‐19 pandemic. Resusc Plus. 2020;4:100034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Arias E. United States life tables, 2017. Natl Vital Stat Rep. 2019;68:1‐66. [PubMed] [Google Scholar]
- 8. Arias E, Xu J. United States life tables, 2018. Natl Vital Stat Rep. 2020;69:1‐45. [PubMed] [Google Scholar]
- 9. Arias E, Xu J, Kochanek KD. United States life tables, 2016. Natl Vital Stat Rep. 2019;68:1‐66. [PubMed] [Google Scholar]
- 10. Arias E, Xu J, Tejada‐Vera B, Bastian B.. U.S. State life tables, 2019. Natl Vital Stat Rep. 2021;70:1‐18. [PubMed] [Google Scholar]
- 11. McNally B, Stokes A, Crouch A, Kellermann AL; CARES Surveillance Group . CARES: Cardiac Arrest Registry to Enhance Survival. Ann Emerg Med. 2009;54:674‐683. e672. [DOI] [PubMed] [Google Scholar]
- 12. Cummins RO, Chamberlain DA, Abramson NS, et al. Recommended guidelines for uniform reporting of data from out‐of‐hospital cardiac arrest: the Utstein Style. A statement for health professionals from a task force of the American Heart Association, the European Resuscitation Council, the Heart and Stroke Foundation of Canada, and the Australian Resuscitation Council. Circulation. 1991;84:960‐975. [DOI] [PubMed] [Google Scholar]
- 13. United States Census Bureau . Monthly Population Estimates for the United States: April 1, 2010‐December 1, 2020. United States Census Bureau; 2022; https://www.census.gov/data/tables/time‐series/demo/popest/2010s‐national‐total.html Accessed February 9, 2022 [Google Scholar]
- 14. Murray CJ, Vos T, Lozano R, et al. Disability‐adjusted life years (DALYs) for 291 diseases and injuries in 21 regions, 1990–2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012;380:2197‐2223. [DOI] [PubMed] [Google Scholar]
- 15. Murray CJL, Lopez AD. Measuring global health: motivation and evolution of the Global Burden of Disease Study. Lancet. 2017;390:1460‐1464. [DOI] [PubMed] [Google Scholar]
- 16. Ginsberg GM, Kark JD, Einav S. Cost‐utility analysis of treating out of hospital cardiac arrests in Jerusalem. Resuscitation. 2015;86:54‐61. [DOI] [PubMed] [Google Scholar]
- 17. Yang DS, Dalton JE. A Unified Approach to Measuring the Effect Size Between Two Groups Using SAS. SAS Global Forum 2012. Paper 335. https://support.sas.com/resources/papers/proceedings12/335-2012.pdf
- 18. Austin PC. Balance diagnostics for comparing the distribution of baseline covariates between treatment groups in propensity‐score matched samples. Stat Med. 2009;28:3083‐3107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Cardiac Arrest Registry to Enhance Survival. Data Sharing Policy. https://mycares.net/sitepages/datasharepolicy.jsp Accessed January 10, 2022 [Google Scholar]
- 20. GBD 2016 DALYs and HALE Collaborators . Global, regional, and national disability‐adjusted life‐years (DALYs) for 333 diseases and injuries and healthy life expectancy (HALE) for 195 countries and territories, 1990–2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet. 2017;390:1260‐1344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Baldi E, Sechi GM, Mare C, et al. Out‐of‐hospital cardiac arrest during the Covid‐19 outbreak in Italy. N Engl J Med. 2020;383:496‐498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Baldi E, Sechi GM, Mare C, et al. COVID‐19 kills at home: the close relationship between the epidemic and the increase of out‐of‐hospital cardiac arrests. Eur Heart J. 2020;41:3045‐3054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Holland M, Burke J, Hulac S, et al. Excess cardiac arrest in the community during the COVID‐19 pandemic. JACC Cardiovasc Interv. 2020;13:1968‐1969. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Marijon E, Karam N, Jost D, et al. Out‐of‐hospital cardiac arrest during the COVID‐19 pandemic in Paris, France: a population‐based, observational study. Lancet Public Health. 2020;5:e437‐e443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Rosell Ortiz F, Fernandez Del Valle P, Knox EC, et al. Influence of the Covid‐19 pandemic on out‐of‐hospital cardiac arrest. A Spanish nationwide prospective cohort study. Resuscitation. 2020;157:230‐240. [DOI] [PMC free article] [PubMed] [Google Scholar]


