Abstract
Background:
Little is known about the benefits and outcomes of meniscal repair in patients older than 60 years.
Purpose:
To (1) report the clinical and radiographic outcomes of meniscal repair in patients aged ≥60 years and compare them with matched patients who underwent meniscectomy and (2) identify procedural failures.
Study Design:
Cohort study; Level of evidence, 2.
Methods:
We included 32 knees in 32 patients aged ≥60 years (20 female, 12 male; mean age, 64.5 ± 4.6 years) who underwent meniscal repair surgery at a single medical institution between 2010 and 2020. Patients were matched according to age, sex, body mass index, and meniscal tear type with a comparison cohort who underwent meniscectomy (n = 49 patients [49 knees]; 32 female, 17 male). For all patients, demographic information, clinical history, physical examination findings, treatment details, and radiographic images were reviewed and analyzed. At final follow-up (mean, 42.2 months; range, 13-128 months), patients completed the 2000 International Knee Documentation Committee (IKDC) Subjective Knee Evaluation Form, Knee injury and Osteoarthritis Outcome Score (KOOS), and Lysholm score. Clinical failure was defined as revision surgery and/or progression to total knee arthroplasty (TKA). A matched-pairs t test was used to analyze differences between the 2 treatment groups, and Kaplan-Meier analysis was used to determine the rates of knee osteoarthritis and progression to TKA.
Results:
The majority of patients had a medial meniscal tear (72.8%), whereas the lateral meniscus was torn in 27.2% of cases. Most tears were located in the meniscal root (56.8%), followed by the posterior horn (34.6%) and midbody (8.6%). At final follow-up, all outcome scores were higher in the repair group compared with the meniscectomy group (IKDC, 78.9 ± 13.4 vs 56.0 ± 15.4; KOOS, 86.6 ± 11.9 vs 61.7 ± 16.2; Lysholm, 88.3 ± 13.3 vs 68.7 ± 15.2, respectively; P < .001 for all). Clinical failure was observed in 22% of patients in the repair group.
Conclusion:
All clinical outcome scores were higher in the meniscal repair group compared with the matched meniscectomy group at final follow-up. The clinical failure rate of the repair group was 22%. These findings support meniscal repair in selected patients aged ≥60 years.
Keywords: meniscal tear, root tear, meniscal repair, meniscectomy, older patients
The menisci of the knee are crucial for maintaining the biological and biomechanical integrity of the joint. They absorb and transmit compressive loads, estimated to amount to 50% of the load carried during walking and 70% to 99% during other compressive moments. 33,35 Correlating with the high relevance of the meniscal structure to joint homeostasis, meniscal surgery is the most common type of orthopaedic surgery performed in the United States, with more than 500,000 meniscal tears treated annually. 13
Isolated meniscal tears are increasingly recognized as a cause of knee pain and early onset of knee osteoarthritis in young patients and are often addressed with surgical repair. 12 The success rates for meniscal repairs in the adult and athletic population have been well-documented and are generally favorable. 28,31 In older patients, however, surgeons were historically reluctant to repair these lesions because of concerns about healing potential or the presence of preexisting degenerative changes. 4 A proposed limiting factor of the success of the procedure is the sparse vasculature of the meniscus and therefore its limited healing potential. 2 In the course of aging, blood supply to the meniscus decreases even further, and degenerative changes in the knee joint increase. 32 Because of this biological degradation, meniscal repairs in older patients might be associated with higher failure rates, which have been documented in multiple studies. 3,30
Given these concerns, partial meniscectomy and nonoperative measures have traditionally been first-line treatment for older (usually >40 years) patients with meniscal pathology. However, because the average life expectancy continues to increase, and several studies revealed that total and partial meniscectomy significantly altered tibiofemoral biomechanics leading to deleterious effects on the knee, meniscal repair has gained popularity. 6,11,20,10 Meniscal repair has become the preferred technique when indicated because of its ability to preserve knee biomechanics and prevent or delay the progression of chondral degeneration associated with meniscal pathology. 16,22 Due to inherent benefits of meniscal repair and the notable downside to meniscectomy, there has been a significant increase in the number of meniscal repairs in relation to meniscectomies in the United States for all age groups. 1
Although the definition of “older patients” is usually ≥40 years, outcome data for meniscal repair surgery on patients aged ≥60 years are limited. 10 Studies describing patient-reported outcome measures (PROMs) in particular are scarce, despite their value as a metric of patient satisfaction and quality of life after a surgical intervention. To our knowledge, no data are readily available regarding outcomes of meniscal repair in a population aged ≥60 years. Therefore, the purpose was to (1) report the clinical and radiographic outcomes of meniscal repair procedures in this population and compare them with matched patients who were treated with meniscectomy and (2) identify procedural failures.
Methods
Study Population and Design
The study protocol was approved by our institutional review board. The study was retrospective in nature. We reviewed the records of all patients aged ≥60 years who underwent arthroscopic meniscal repair and meniscectomy at our institution between November 2010 and January 2020. Procedures were identified based on Current Procedural Terminology codes 29880, 29881, 29882, and 29883. The former 2 codes comprised the meniscectomy cohort, and the latter 2 comprised the meniscal repair cohort.
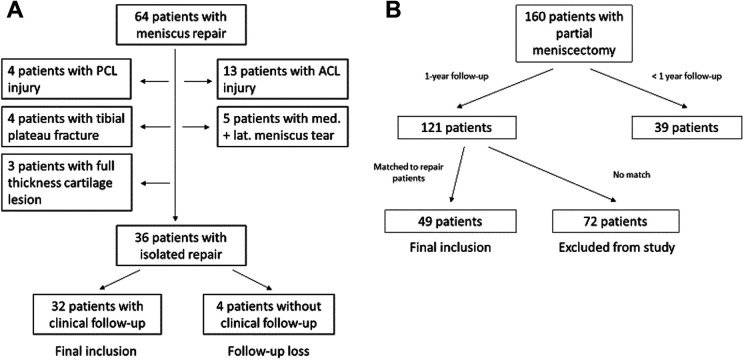
A total of 74 repaired meniscal tears in 64 patients were identified. A total of 36 consecutive isolated meniscal repairs (in 36 patients) remained after we applied exclusion criteria, which were concomitant anterior cruciate ligament tear and reconstruction, grade 2 or 3 posterior cruciate ligament (PCL) injury, medial collateral or lateral collateral ligament injury, full-thickness (grade 4) osteochondral lesion (as determined at the time of arthroscopy), periarticular fracture, combination injuries of both menisci in the same knee, and <1 year of follow-up. PROMs (2000 International Knee Documentation Committee [IKDC] Subjective Knee Evaluation Form, Knee injury and Osteoarthritis Outcome Score [KOOS], and Lysholm score) were exclusively collected for this study during routine visits to the clinic or by telephone interview at the time of final follow-up. Despite attempts to contact all patients, 4 patients did not have clinical follow-up (14%). Therefore, the repair group consisted of 32 meniscal repairs that were performed by 4 different surgeons in 32 patients, who were evaluated for at least 1 year or until known failure (Figure 1).
Figure 1.
Flowchart showing patient movement through the study for (A) the repair group and (B) the meniscectomy group. ACL, anterior cruciate ligament; PCL, posterior cruciate ligament.
The same exclusion criteria were applied to patients treated with partial meniscectomy (meniscectomy group). A total of 160 patients aged ≥60 years who underwent consecutive partial meniscectomy were identified. After exclusion criteria were applied, 121 patients with at least 1 year of follow-up remained. After matching to the patients in the repair group was performed based on age (±2.5 years), sex (male or female), body mass index (BMI) (±2.5 kg/m2), location of lesion (medial meniscus or lateral meniscus), and zone of lesion (body, posterior horn, or root), 49 meniscectomy patients remained and were included in the study. All patients in the meniscectomy group completed the same PROMs as those in the repair group. Meniscal repairs were matched in a 1:2 ratio where possible by a blinded statistician.
Surgical Indications
Our criteria for meniscal repair were the ability to technically stabilize and coaptate an unstable, full-thickness tear >1 cm in length and within 6 mm of the meniscosynovial junction. Indications for partial meniscectomy included but were not limited to degenerated, macerated tears and tears that could not be technically stabilized. The final decision regarding treatment type was at the discretion of the surgeon and was based on a patient’s chronological age, biological age, general health, comorbidities, athletic ambition, and preference. Contraindications for meniscal repair included stable tears <10 mm in length, partial-thickness tears (<50%), and radial tears (<3 mm). Patients were assessed, and all surgeries were performed, at a single institution. Treatment decisions were made by the surgeon, taking into account tear type and location, overall status of the knee, patient age and activity level, and patient preference.
The majority of repaired tears in our study cohort represented injuries of the meniscus root, which constitutes a special subsection of meniscal tears. They are generally classified into 2 clinical categories: (1) traumatic tears, which typically occur in younger patients and are often lateral and associated with concomitant ligamentous injury; and (2) degenerative tears, which are often found in older patients, affect the medial meniscus, and result from chronic, often low-energy attritional mechanisms. 26 Risk factors for posterior root tears are well-documented and include varus malalignment, older age, increased BMI, female sex, and increased Kellgren-Lawrence (K-L) grade. 19
Root tears result in total loss of meniscal function and have a biomechanical effect similar to a total meniscectomy if left untreated. Therefore, thorough understanding of diagnostic and therapeutic details is important to achieve the best possible clinical outcomes. In pursuit of this, the surgeon must discriminate between injuries that are approachable with a repair procedure and injuries that are best treated nonoperatively or with meniscectomy. Magnetic resonance imaging (MRI) has been considered the gold standard in preoperative diagnosis of meniscus root tears. MRI is used to assess 5 findings, crucial for diagnosis and treatment decision, which can best be analyzed using T2-weighted sequences: (1) meniscal extrusion; (2) missing meniscus near the PCL (commonly known as ghost sign); (3) a gap in the meniscus root, termed cleft sign; (4) a linear signal found at the fracture site, and (5) a bone marrow edema found due to contusion under the tear. 17
Meniscal extrusion is defined as a substantial (≥3 mm for medial tears) outward radial displacement of the meniscus from the tibial articular cartilage and has been reported to be strongly associated with meniscus root pathology and joint degeneration. 27 MRI evaluation of the meniscus roots must be viewed in light of certain limitations and should always be augmented by physical examination and patient history. 7 Krych et al 26 demonstrated that the rate of preoperatively identified posterior root tears on MRI scans read by fellowship-trained musculoskeletal radiologists was only 33%, with only 50% of missed tears clearly evident when retrospectively reviewing known tears.
In the presence of mechanical symptoms, such as catching or locking, nonoperative treatment of root tears is not advised. Contraindications for meniscus root repair include subchondral bone collapse, substantial malalignment (≥5°), unaddressed instability of the knee joint, chondral defects (grade ≥3; >2 cm2), and notable degenerative pathology of the affected knee (K-L grade >2). In addition, increased BMI (ie, >30 kg/m2) and milder forms of malalignment (<5°) serve as relative contraindications given the increased stress of the repair construct. 5 In these cases, meniscectomy poses a viable treatment option in order to eliminate mechanical symptoms. Clinical outcome, however, is not significantly improved by meniscectomy. Krych 24 demonstrated that patients undergoing partial meniscectomy for symptomatic medial meniscus posterior root tears demonstrated no substantial benefit in PROMs, and furthermore, 52% of meniscectomy patients progressed to arthroplasty at a mean of 4.5 years.
Surgical Technique
Medial or lateral meniscal tears were repaired using a routine arthroscopic setup for diagnostic purposes. Standard arthroscopic portals were used, and all tears underwent preparation, including rasping and anatomic reduction before fixation. The majority of meniscal repairs were performed in the setting of a root tear (n = 15; 52%) using a previously described transtibial suture technique. 18,40 All repairs were performed with the patient in the supine position. Standard anterolateral and anteromedial portals were established adjacent to the patellar tendon and proximal to the meniscus to allow for instrument passage to the posteromedial and posterolateral compartments. Diagnostic arthroscopy was completed, and the root tear was identified. A transtibial drill guide (Arthrex) was inserted through the anterior portal. The guide tip was positioned at the center of the posterior horn root footprint. A 3.5-mm wire was inserted through the tibia and then exchanged with a 6 mm–diameter Flip Cutter (Arthrex). The Flip Cutter was used to create a 5 mm–deep socket with exposed bleeding bone.
Three No. 0 Fiberlink (Arthrex), simple cinch (luggage tag) sutures were placed in the meniscus root using a self-retrieving device (Knee Scorpion; Arthrex). These sutures were then pulled through the tibia using a shuttling technique. The sutures were tensioned, and slack was removed by cycling the knee. The sutures were then fixed to the tibia with a knotless suture anchor (4.75-mm Swivelock anchor; Arthrex).
The remaining suture repairs were carried out with an all-inside technique using the FasT-Fix 360 device (Smith & Nephew Endoscopy), deploying a needle-insertion device in a vertical mattress configuration on the superior surface of the meniscus, 3 mm inside the meniscal cut. This device has 2 arrow-shaped polyether ether ketone anchors connected by a No. 2-0 braided, ultra-high-molecular-weight polyethylene suture with a pretied sliding locking knot (Smith & Nephew Endoscopy).
Rehabilitation
The postoperative rehabilitation after isolated meniscal repair included protected weightbearing (touch-down weightbearing) with crutches and range of motion limited to <90° for 3 to 4 weeks. Activities were slowly increased, but no squatting or pivoting was allowed for 4 months. Sports were permitted 4 to 6 months after surgery based on clinical progress.
Patients who underwent partial meniscectomy had no limitation in weightbearing and range of motion exercise when tolerable. In addition, continuous and progressive muscle-strengthening exercises were recommended within the tolerable range for each patient.
Evaluation Methods
All patients underwent routine preoperative and postoperative clinical evaluation as part of standard clinical care. During these visits, demographic data, patient-specific health data, and radiographic data were collected. A review of the extensive and detailed electronic medical records was performed to analyze historical data. Meniscal tears and concomitant injuries were described at the time of arthroscopy. Further, the articular cartilage condition was graded at the time of arthroscopy using the Outerbridge classification, distinguishing patellar chondral surface, femoral chondral surface, and tibial chondral surface. 36 Normal chondral joint surface is graded as 0, whereas grade 4 includes erosion of the articular cartilage that exposes subchondral bone.
Outcome Measures
Objective outcome parameters included reoperation of the repaired meniscus, progression to total knee arthroplasty (TKA), and K-L grade. Postoperative Lysholm, KOOS, and IKDC scores were used for the subjective knee evaluation. These evaluation forms were scored in the standard manner at final follow-up, which was completed for all study patients between May 3 and June 18, 2021.
Patients were considered to have a clinically successful repair if they had no mechanical signs or symptoms, including locking, catching, giving way, or significant swelling, and had no subsequent surgical procedures on the repaired meniscus. Progression to TKA in the period of follow-up was considered failure.
Radiographic assessment of knee arthritis was determined using the K-L grading system. 21 Weightbearing anteroposterior knee radiographs were evaluated, and arthritis was graded as none (grade 0), doubtful (grade 1), minimal (grade 2), moderate (grade 3), or severe (grade 4). All postoperative radiographs were obtained for clinical follow-up as part of standard clinical care and were reevaluated by a fellowship-trained orthopaedic surgeon (M.H.) for the purpose of this study.
Statistical Analysis
Rates of failure were estimated at specific follow-up times using the Kaplan-Meier method and were compared between groups using log-rank tests. The effect of continuous variables on risk of failure was assessed using Cox proportional hazards regression. Kaplan-Meier rates were reported with 95% CIs. Analysis was performed using SPSS software (Version 18.0 for Windows; IBM) and JMP Pro (Version 14.1.0; SAS Institute). Statistical significance was set at 5% (P < .05). The independent t test was used to compare continuous variables distributed normally between the groups as well as other numerical values. The Mann-Whitney test was used to compare nonnormally distributed variables between groups and other nonparametric values. The chi-square test was used to compare categorical data, and if >20% of the expected frequencies were >5, the Fisher exact test was used.
Results
The mean follow-up after surgery was 42.2 months (range, 13-128 months). The mean age at surgery was 64.5 years (range, 60-77 years). There were 29 men and 52 women in the total cohort. In total, 59 medial and 22 lateral menisci were treated. There were 45 right and 36 left knees involved. A total of 4 patients were lost to follow-up and were not included in the study. We found no significant difference in demographic characteristics, tear type, or tear location between the groups at baseline. The preoperative K-L grade was not significantly different between the groups (P = .52).
Demographic Characteristics
Baseline demographic characteristics are displayed in Table 1. Radiographical characteristics per study group can be found in Table 2. We found no statistically significant difference between the groups preoperatively and postoperatively regarding the K-L grade. Table 3 displays the meniscal tear characteristics of the groups, and Table 4 provides the mean Outerbridge scores at time of surgery.
Table 1.
Demographic Characteristics of the Groups a
| Characteristic | Repair Group (n = 32) |
Meniscectomy Group (n = 49) |
P |
|---|---|---|---|
| Sex, male/female, n | 12/20 | 17/32 | .82 b |
| Age, y | 64.5 ± 4.6 | 64.7 ± 4.3 | .71 c |
| Follow-up, mo | 39.4 ± 27.9 | 45 ± 19.2 | .52 d |
| Body mass index, kg/m2 | 28.9 ± 6.4 | 29.6 ± 6.6 | .65 c |
a Data are presented as mean ± SD unless otherwise indicated.
b Fisher exact test.
c Independent t test.
d Mann-Whitney test.
Table 2.
Radiographic Characteristics of the Groups a
| Kellgren-Lawrence Grade | Repair Group (n = 32) |
Meniscectomy Group (n = 49) |
P |
|---|---|---|---|
| Grades 0/1/2/3/4, preoperative | 2/12/12/6/0 | 5/24/12/7/0 | .52 b |
| Grade 0/1/2/3/4, postoperative | 2/4/6/8/2 | 1/4/15/11/2 | .63 b |
a Data are presented as No. of patients.
b Fisher exact test.
Table 3.
Meniscal Tear Characteristics of the Groups a
| Characteristic | Repair Group (n = 32) |
Meniscectomy Group (n = 49) |
P |
|---|---|---|---|
| Tear laterality | >.99 b | ||
| Medial | 23 | 36 | |
| Lateral | 9 | 13 | |
| Tear location | .89 b | ||
| Middle body | 2 | 5 | |
| Posterior horn | 11 | 17 | |
| Root | 19 | 27 |
a Data are presented as No. of patients.
b Fisher exact test.
Table 4.
Mean Outerbridge Grades of Chondral Surfaces at the Time of Arthroscopy
| Repair Group (n = 32) |
Meniscectomy Group (n = 49) |
P | |
|---|---|---|---|
| Patella | 1.7 | 1.9 | 0.2 a |
| Femoral condyle | 1.9 | 2.0 | 0.3 a |
| Tibial plateau | 1.3 | 1.5 | 0.2 a |
| Treated compartment | 1.5 | 1.7 | 0.3 a |
a Fisher exact test.
Clinical Success Rate
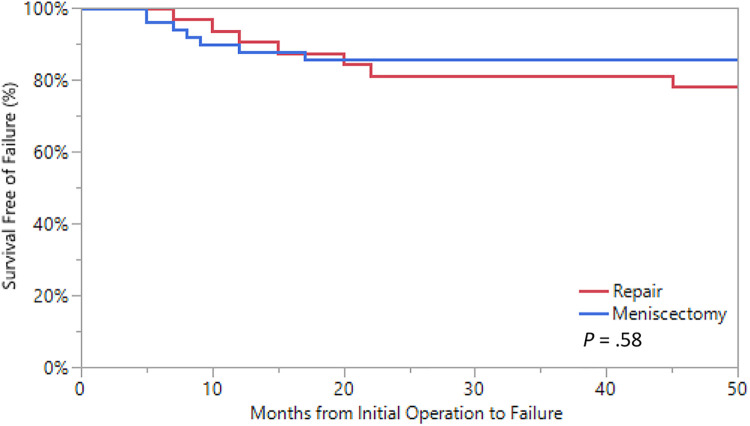
The clinical success rate of meniscal repair was 78% overall, with 100% in the patients with meniscal body tears, 82% in the patients with meniscus root tears, and 69% in the patients with posterior horn lesions. Of the 32 patients in the repair group, 7 patients (22%) had repaired menisci that failed after an average time of 19 months (range, 8-46 months). In total, 3 (9%) of the menisci that failed were treated with partial meniscectomy, and 4 (12.5%) progressed to TKA. One patient was reoperated with a partial meniscectomy and progressed to TKA 20 months afterward. Time point of failure was defined as the date of partial meniscectomy. Two of the failed initial repairs occurred in the first 12 months after repair. In the meniscectomy cohort, 9 patients (18%) progressed to TKA and were therefore considered to have experienced failure. A Kaplan-Meier plot with 95% CIs is presented in Figure 2.
Figure 2.
Kaplan-Meier survival analysis from failure of initial operative management resulting in either meniscectomy (repair cohort only) or total knee arthroplasty (repair and meniscectomy cohort).
Outcomes Based on Outerbridge Grade at Arthroscopy
We found no statistical outcome differences regarding clinical success rate between patients with Outerbridge grade 0 or 1 and those with Outerbridge grade 2 or 3 of the whole joint.
In a compartment-specific analysis including only the Outerbridge grade of the treated knee compartment, there were 2 clinical failures in patients of the repair group (n = 12) with an Outerbridge grade 0 or 1 at the time of index arthroscopy. Of the meniscectomy group (n = 9), 1 patient progressed to TKA. In patients of the repair group with Outerbridge grade 2 or 3 (n = 20), 4 clinical failures were recorded, whereas 3 of 40 patients of the meniscectomy group with Outerbridge grade 2 or 3 progressed to TKA.
Patient-Reported Outcomes
PROMs are displayed in Table 5 and Figure 3. At final follow-up, patients in the repair group reported significantly better outcomes with regard to IKDC, KOOS, and Lysholm scores (P < .001 for all). The most significant difference was observed in the KOOS, with a mean ± SD of 86.6 ± 11.9 for the repair group and 61.7 ± 16.2 for the meniscectomy group (P < .001). Of those menisci that clinically failed, PROM scores were 66.8 for IKDC, 74 for KOOS, and 76 for Lysholm. Spearman correlation coefficients were calculated to assess for correlation between PROMs, BMI, and age at procedure (Table 6). The only statistically significant correlation found was a negative correlation between BMI and Lysholm score (Figure 4).
Table 5.
Injury Traits and Patient-Reported Outcomes Postoperatively a
| Characteristic | Repair Group (n = 32) |
Meniscectomy Group (n = 49) |
P |
|---|---|---|---|
| Tear laterality | >.99 b | ||
| Medial | 23 | 36 | |
| Lateral | 9 | 13 | |
| Tear location | .89 b | ||
| Middle body | 2 | 5 | |
| Posterior horn | 11 | 17 | |
| Root | 19 | 27 | |
| IKDC score | 78.9 ± 13.4 | 56.0 ± 15.4 | <.001 |
| KOOS | 86.6 ± 11.9 | 61.7 ± 16.2 | <.001 |
| Lysholm score | 88.3 ± 13.3 | 68.7 ± 15.2 | <.001 |
a Data are presented as No. of patients or mean ± SD. Boldface P values indicate statistically significant difference between groups (P < .05). IKDC, International Knee Documentation Committee; KOOS, Knee injury and Osteoarthritis Outcome Score.
b Fisher exact test.
Figure 3.
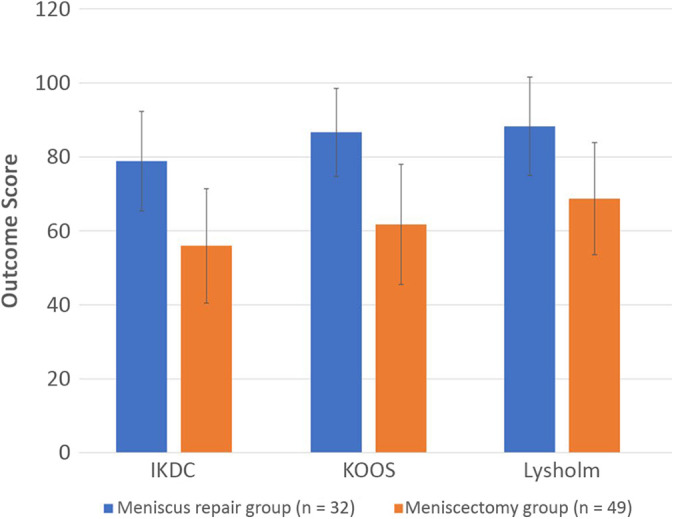
Postoperative patient-reported outcome scores. IKDC, International Knee Documentation Committee; KOOS, Knee injury and Osteoarthritis Outcome Score.
Table 6.
Spearman Rank Correlation Coefficient of Various Patient-Reported Scores and BMI or Age at Time of Procedure a
| BMI | Age at Procedure | |||
|---|---|---|---|---|
| Outcome Measure | r S | P | r S | P |
| IKDC | –0.344 | .054 | .066 | .719 |
| KOOS | –0.268 | .139 | .124 | .500 |
| Lysholm | –0.402 | .026 | .079 | .667 |
a Boldface P value indicates statistical significance (P < .05). BMI, body mass index; IKDC, International Knee Documentation Committee; KOOS, Knee injury and Osteoarthritis Outcome Score.
Figure 4.
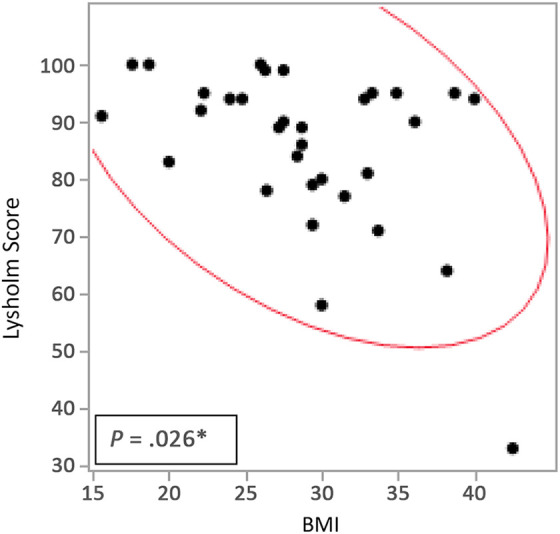
Scatter matrix of postoperative Lysholm score and body mass index (BMI).
Radiographic Outcomes
Knee radiographs at final follow-up were available in 55 patients and are displayed in Table 2. We found no statistical difference in preoperative rate of osteoarthritis between the groups. The follow-up radiographs showed no significant differences between the repair and meniscectomy groups. Two knees in the repair group progressed from K-L grade 2 preoperatively to grade 4 postoperatively and were treated with TKA.
Discussion
Prior studies have reported good results with meniscal repairs in patients aged ≥40 years. 8,10 However, no study has specifically addressed the outcome of isolated arthroscopic repairs in the age group of ≥60 years. In this study, we review our clinical experience of arthroscopic repair of isolated meniscal tears in patients ≥60 years and report an overall clinical success rate of 78% for the repair group and 82% for the meniscectomy group. In this context, the most important finding of this study was that the patient-reported outcomes in meniscal repair and meniscectomy cohorts at an average of 42.2 months of follow-up postoperatively differed significantly in favor of the repair group.
The literature provides sparse data regarding PROMs for an older patient cohort with meniscal pathology undergoing meniscal repair. Engler et al 10 compared IKDC scores between meniscal repair and partial meniscectomy in a cohort of patients aged ≥40 years with meniscal pathology. Those investigators reported no significant differences in IKDC scores between the 2 groups. Further, they found that the average IKDC score of their repair cohort was 78. These average IKDC scores were comparable with average IKDC scores of our meniscal repair cohort (78.9). However, our meniscectomy group reported notably worse outcomes. The Patient Acceptable Symptom State of the IKDC score for patients treated with meniscectomy (57.9) was well-exceeded by patients of the repair group (78.9) but not by patients of the meniscectomy group (56.0). 14 The difference in IKDC score for the meniscectomy patients might result from age difference and patient selection. Although Engler and coworkers reported a mean age of 52.8 years, our meniscectomy cohort had a mean age of 64.7 years and is more likely to have a lower IKDC score even without any form of treatment.
The Outerbridge grade of the knee joint at time of arthroscopy seemed to be not significantly correlated with the clinical success rate in this study. However, the sample size of our study was not large enough to eliminate confounders and bias in order to reach a statistically significant conclusion. Although less favorable outcomes are often seen with Outerbridge grade 4, these patients were not included in our study. 34 It can be assumed that a meniscal repair procedure is less likely to be performed in the presence of a full-thickness cartilage lesion with the exposure of subchondral bone.
The main biomechanical function of the menisci is to decrease contact pressure by distributing axial load and absorbing shock within the knee. To fulfill this function, the meniscus roots need to be intact and stable to prevent extrusion during compression. 11,26,39 Meniscus root tears drastically alter native tibiofemoral biomechanics and have similar biomechanical effects to meniscus-deficient knees. Similarly, partial meniscectomy for degenerative root tears significantly alters biomechanics and is associated with a high risk of TKA conversion. 25 Therefore, repair of the meniscus root pathology (n = 46 in the present study) with an aim to reestablish its biomechanical properties is integral to preservation of the native joint biomechanics and longevity of tibiofemoral joint function. 19,23 The present study demonstrated a significant improvement of clinical joint function in PROMs and a relatively low rate of progression to TKA (12.5% in the repair group and 18% in the meniscectomy group). The conversion rate in the present study was lower than most reported in the literature. However, this study’s follow-up time of 45 months for the meniscectomy group was relatively short.
We report a clinical success rate of 78% after initial arthroscopic repair, with most of the decline in the median survival occurring during the first 22 months (Figure 2). It should be noted, however, that the minimum time of follow-up was 12 months and that the mean time of follow-up was 39.4 months. This time frame is relatively short, and considering that the repair group was subject to postoperative weightbearing and activity limitations whereas the meniscectomy group was released to full activity postoperatively, there is a risk of bias due to different rehabilitation protocols between the groups. Previous studies that analyzed meniscal repair in ligament-stable knees reported a variable clinical success rate between 33% and 76%. 9,15,29,38 Although previous authors have used patient-reported outcomes to compare meniscectomy and meniscal repair, the current study is the first to our knowledge that specifically examined a patient population of ≥60 years. Xu and Zhao 41 conducted a meta-analysis comparing both treatments and found improved IKDC score, Lysholm score, and Tegner activity score. However, those investigators excluded publications with patients ≥45 years old, and the reported mean age of the included studies was 22 to 33 years. Dragoo et al 8 investigated the outcomes of arthroscopic all-inside repair versus observation in older patients with meniscus root tears. The study size was 48 patients (30 treated, 18 observed) with a mean age of 59.7 years, and the investigators reported improved functional outcomes compared with nonoperative treatment. This is consistent with our study, in which the KOOS for the repair group (86.6) was significantly higher compared with the meniscectomy group (61.7).
Limitations
We note the following limitations. First, this retrospective cohort contains a relatively small group of patients with mixed locations of the meniscal tears. Although the majority of patients in both groups were treated for root tears, the remaining patients were treated for more conventional tears of the meniscal body or posterior horn. However, the procedure of meniscal repair in patients ≥60 years of age remains relatively uncommon, and to our knowledge, this is one of the largest series of isolated tears in the older population to be reported in the literature. Second, no MRI or second-look arthroscopy was performed on asymptomatic patients to assess for clinically silent failures; thus, the failure rate in both groups may have been higher. Previous studies showed that half of asymptomatic patients can have failed repairs at the time of second-look arthroscopy. 37 Third, multiple surgeons performed the meniscal repairs and meniscectomies during a 10-year time period. Fourth, patients were matched by tear location but not by exact tear type, possibly resulting in a mismatch of patients and potentially reducing the comparability of matched pairs. Fifth, the minimum follow-up time in this study was 12 months, which is short compared with other clinical outcome studies. Due to this time frame, final follow-up was conducted in some patients of the repair group only 6 months after full release to activity, whereas it was 12 months after release for the matched patients of the meniscectomy group.
Conclusion
Meniscal repair led to significantly higher patient-reported outcome scores compared with partial meniscectomy in a cohort matched based on patient characteristics. Further studies are needed to help define the ideal treatment for patients with a meniscal tear based on their clinical, demographic, and radiographic characteristics.
Footnotes
Final revision submitted April 21, 2022; accepted May 24, 2022.
One or more of the authors has declared the following potential conflict of interest or source of funding: The authors acknowledge support from the Foderaro-Quattrone Musculoskeletal-Orthopaedic Surgery Research Innovation Fund. This study was partially funded by the Deutsche Forschungsgemeinschaft (grant No. 466023693 to M.H.) and the National Institute of Arthritis and Musculoskeletal and Skin Diseases for the Musculoskeletal Research Training Program (T32AR56950). N.I.K. has received hospitality payments from Encore Medical. M.J.S. has received research support from Stryker and consulting fees, nonconsulting fees, and royalties from Arthrex. A.J.K. has received grant support from DJO; consulting fees from Arthrex, the Joint Restoration Foundation, and Responsive Arthroscopy; speaking fees from Arthrex; royalties from Arthrex and Responsive Arthroscopy; and honoraria from Vericel and the Joint Restoration Foundation; he serves on the medical board of trustees for the Musculoskeletal Transplant Foundation. D.B.F.S. has received consulting fees from Smith & Nephew. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
Ethical approval for this study was obtained from Mayo Clinic (reference No. PR15-000601-06).
References
- 1. Abrams GD, Frank RM, Gupta AK, et al. Trends in meniscus repair and meniscectomy in the United States, 2005-2011. Am J Sports Med. 2013;41(10):2333–2339. [DOI] [PubMed] [Google Scholar]
- 2. Barber-Westin SD, Noyes FR. Clinical healing rates of meniscus repairs of tears in the central-third (red-white) zone. Arthroscopy. 2014;30(1):134–146. [DOI] [PubMed] [Google Scholar]
- 3. Barrett GR, Field MH, Treacy SH, Ruff CG. Clinical results of meniscus repair in patients 40 years and older. Arthroscopy. 1998;14(8):824–829. [DOI] [PubMed] [Google Scholar]
- 4. Bhatia S, LaPrade CM, Ellman MB, LaPrade RF. Meniscal root tears: significance, diagnosis, and treatment. Am J Sports Med. 2014;42(12):3016–3030. [DOI] [PubMed] [Google Scholar]
- 5. Brophy RH, Wojahn RD, Lillegraven O, Lamplot JD. Outcomes of arthroscopic posterior medial meniscus root repair: association with body mass index. J Am Acad Orthop Surg. 2019;27(3):104–111. [DOI] [PubMed] [Google Scholar]
- 6. Burks RT, Metcalf MH, Metcalf RW. Fifteen-year follow-up of arthroscopic partial meniscectomy. Arthroscopy. 1997;13(6):673–679. [DOI] [PubMed] [Google Scholar]
- 7. Cinque ME, Chahla J, Moatshe G, et al. Meniscal root tears: a silent epidemic. Br J Sports Med. 2018;52(13):872–876. [DOI] [PubMed] [Google Scholar]
- 8. Dragoo JL, Konopka JA, Guzman RA, et al. Outcomes of arthroscopic all-inside repair versus observation in older patients with meniscus root tears. Am J Sports Med. 2020;48(5):1127–1133. [DOI] [PubMed] [Google Scholar]
- 9. Eggli S, Wegmuller H, Kosina J, Huckell C, Jakob RP. Long-term results of arthroscopic meniscal repair: an analysis of isolated tears. Am J Sports Med. 1995;23(6):715–720. [DOI] [PubMed] [Google Scholar]
- 10. Engler ID, Moradian JR, Pockros BM, et al. Patient-reported outcomes of meniscal repair and meniscectomy in patients 40 years of age and older show similar good results. Knee Surg Sports Traumatol Arthrosc. 2021;29(9):2911–2917. [DOI] [PubMed] [Google Scholar]
- 11. Fairbank TJ. Knee joint changes after meniscectomy. J Bone Joint Surg Br. 1948;30B(4):664–670. [PubMed] [Google Scholar]
- 12. Faucett SC, Geisler BP, Chahla J, et al. Meniscus root repair vs meniscectomy or nonoperative management to prevent knee osteoarthritis after medial meniscus root tears: clinical and economic effectiveness. Am J Sports Med. 2019;47(3):762–769. [DOI] [PubMed] [Google Scholar]
- 13. Garrett WE, Jr, Swiontkowski MF, Weinstein JN, et al. American Board of Orthopaedic Surgery practice of the orthopaedic surgeon, part II: certification examination case mix. J Bone Joint Surg Am. 2006;88(3):660–667. [DOI] [PubMed] [Google Scholar]
- 14. Gowd AK, Lalehzarian SP, Liu JN, et al. Factors associated with clinically significant patient-reported outcomes after primary arthroscopic partial meniscectomy. Arthroscopy. 2019;35(5):1567–1575.e1563. [DOI] [PubMed] [Google Scholar]
- 15. Hagmeijer MH, Kennedy NI, Tagliero AJ, et al. Long-term results after repair of isolated meniscal tears among patients aged 18 years and younger: an 18-year follow-up study. Am J Sports Med. 2019;47(4):799–806. [DOI] [PubMed] [Google Scholar]
- 16. Han SB, Shetty GM, Lee DH, et al. Unfavorable results of partial meniscectomy for complete posterior medial meniscus root tear with early osteoarthritis: a 5- to 8-year follow-up study. Arthroscopy. 2010;26(10):1326–1332. [DOI] [PubMed] [Google Scholar]
- 17. Harper KW, Helms CA, Lambert HS III, Higgins LD. Radial meniscal tears: significance, incidence, and MR appearance. AJR Am J Roentgenol. 2005;185(6):1429–1434. [DOI] [PubMed] [Google Scholar]
- 18. Hevesi M, Stuart MJ, Krych AJ. Medial meniscus root repair: a transtibial pull-out surgical technique. Oper Techn Sport Med. 2018;26(3):205–209. [Google Scholar]
- 19. Hwang BY, Kim SJ, Lee SW, et al. Risk factors for medial meniscus posterior root tear. Am J Sports Med. 2012;40(7):1606–1610. [DOI] [PubMed] [Google Scholar]
- 20. Katz JN, Losina E. Surgery versus physical therapy for meniscal tear and osteoarthritis. N Engl J Med. 2013;369(7):677–678. [DOI] [PubMed] [Google Scholar]
- 21. Kellgren JH, Lawrence JS. Radiological assessment of osteo-arthrosis. Ann Rheum Dis. 1957;16(4):494–502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Kim C, Bin SI, Kim JM, Lee BS, Kim TH. Progression of radiographic osteoarthritis after partial meniscectomy in degenerative medial meniscal posterior root tears was greater in varus- than in neutral-aligned knees: a minimum 5-year follow-up. Knee Surg Sports Traumatol Arthrosc. 2020;28(11):3443–3449. [DOI] [PubMed] [Google Scholar]
- 23. Koenig JH, Ranawat AS, Umans HR, Difelice GS. Meniscal root tears: diagnosis and treatment. Arthroscopy. 2009;25(9):1025–1032. [DOI] [PubMed] [Google Scholar]
- 24. Krych AJ. Editorial commentary: knee medial meniscus root tears: “you may not have seen it, but it’s seen you.” Arthroscopy. 2018;34(2):536–537. [DOI] [PubMed] [Google Scholar]
- 25. Krych AJ, Johnson NR, Mohan R, et al. Partial meniscectomy provides no benefit for symptomatic degenerative medial meniscus posterior root tears. Knee Surg Sports Traumatol Arthrosc. 2018;26(4):1117–1122. [DOI] [PubMed] [Google Scholar]
- 26. Krych AJ, Nauert RF III, Song BM, et al. Association between transtibial meniscus root repair and rate of meniscal healing and extrusion on postoperative magnetic resonance imaging: a prospective multicenter study. Orthop J Sports Med. 2021;9(8):23259671211023774. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Lerer DB, Umans HR, Hu MX, Jones MH. The role of meniscal root pathology and radial meniscal tear in medial meniscal extrusion. Skeletal Radiol. 2004;33(10):569–574. [DOI] [PubMed] [Google Scholar]
- 28. Logan M, Watts M, Owen J, Myers P. Meniscal repair in the elite athlete: results of 45 repairs with a minimum 5-year follow-up. Am J Sports Med. 2009;37(6):1131–1134. [DOI] [PubMed] [Google Scholar]
- 29. Marigi EM, Keyt LK, LaPrade MD, et al. Surgical treatment of isolated meniscal tears in competitive male wrestlers: reoperations, outcomes, and return to sport. Orthop J Sports Med. 2021;9(1):2325967120969220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Noyes FR, Barber-Westin SD. Arthroscopic repair of meniscus tears extending into the avascular zone with or without anterior cruciate ligament reconstruction in patients 40 years of age and older. Arthroscopy. 2000;16(8):822–829. [DOI] [PubMed] [Google Scholar]
- 31. Noyes FR, Chen RC, Barber-Westin SD, Potter HG. Greater than 10-year results of red-white longitudinal meniscal repairs in patients 20 years of age or younger. Am J Sports Med. 2011;39(5):1008–1017. [DOI] [PubMed] [Google Scholar]
- 32. Petersen W, Tillmann B. Age-related blood and lymph supply of the knee menisci: a cadaver study. Acta Orthop Scand. 1995;66(4):308–312. [DOI] [PubMed] [Google Scholar]
- 33. Radin EL, de Lamotte F, Maquet P. Role of the menisci in the distribution of stress in the knee. Clin Orthop Relat Res. 1984;185:290–294. [PubMed] [Google Scholar]
- 34. Searle H, Asopa V, Coleman S, McDermott I. The results of meniscal allograft transplantation surgery: what is success? BMC Musculoskelet Disord. 2020;21(1):159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Seedhom BB. Loadbearing function of the menisci. Physiotherapy. 1976;62(7):223. [PubMed] [Google Scholar]
- 36. Slattery C, Kweon CY. Classifications in brief: Outerbridge classification of chondral lesions. Clin Orthop Relat Res. 2018;476(10):2101–2104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Tenuta JJ, Arciero RA. Arthroscopic evaluation of meniscal repairs: factors that effect healing. Am J Sports Med. 1994;22(6):797–802. [DOI] [PubMed] [Google Scholar]
- 38. Venkatachalam S, Godsiff SP, Harding ML. Review of the clinical results of arthroscopic meniscal repair. Knee. 2001;8(2):129–133. [DOI] [PubMed] [Google Scholar]
- 39. Vertullo CJ, Cadman J, Dabirrahmani D, Appleyard R. Biomechanical comparison of an all-inside meniscal repair device construct versus pullout sutures for arthroscopic transtibial repair of posterior medial meniscus root tears: a matched-pair cadaveric study. Orthop J Sports Med. 2021;9(4):23259671211000464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Woodmass JM, Mohan R, Stuart MJ, Krych AJ. Medial meniscus posterior root repair using a transtibial technique. Arthrosc Tech. 2017;6(3):e511–e516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Xu C, Zhao J. A meta-analysis comparing meniscal repair with meniscectomy in the treatment of meniscal tears: the more meniscus, the better outcome? Knee Surg Sports Traumatol Arthrosc. 2015;23(1):164–170. [DOI] [PubMed] [Google Scholar]