Abstract
Background:
Open debridement (OD) of the extensor carpi radialis brevis tendon, both with and without repair to the lateral epicondyle, are effective treatments for recalcitrant lateral epicondylitis. However, few comparative studies exist within the literature.
Purpose:
To (1) compare the 5-year reoperation rates of patients who underwent OD alone versus OD with tendon repair (ODR) and (2) identify the 90-day adverse event rates, total same-day reimbursement amounts, and national usage trends for these 2 procedures from 2010 to 2019.
Study Design:
Cohort study; Level of evidence, 3.
Methods:
The PearlDiver MUExtr database was reviewed for patients diagnosed with lateral epicondylitis who underwent OD alone and ODR or reattachment between January 2010 and December 2019. These patients were stratified into 2 cohorts: the OD cohort and ODR cohort. The 5-year reoperation rates were assessed and compared, and the incidence of 90-day postoperative complications and risk factors were identified. The number of ODs and ODRs performed each year and the mean same-day reimbursement amounts (in US$) for both procedures were assessed.
Results:
Overall, 41,932 lateral epicondylitis patients who underwent debridement were identified, with 17,139 OD patients and 24,793 ODR patients. There were no significant changes in the proportion of OD versus ODR procedures performed during the study period (P = .18). A significantly higher incidence of hematoma was seen after OD compared with ODR (0.19% vs 0.12%; P = .04), but ODR had a significantly lower 5-year reoperation rate than OD (2.8% vs 3.9%; P = .006), with an absolute risk reduction of 1.1% and a number needed to treat of 91. Finally, ODR ($1683.17 ± $12.15) had a higher mean same-day reimbursement than OD ($1479.05 ± $15.78) (P = .001).
Conclusion:
Both OD and ODR had low complication rates. The 5-year reoperation rates were low for both procedures, but they were significantly higher for OD. Over the 10-year study period, there were no significant changes in the relative percentages of OD versus ODR performed. ODR had a significantly higher mean same-day reimbursement.
Keywords: lateral epicondylitis, open debridement, tendon repair, tennis elbow
Lateral epicondylitis, or tennis elbow, is a common overuse injury that results from degeneration of the extensor carpi radialis brevis (ECRB) tendon near its origin on the lateral epicondyle of the humerus. 4,5,6,15 Lateral epicondylitis is typically a self-limiting condition that resolves within a year without treatment. 4,5 Nonoperative treatments often consist of combinations of physical therapy, nonsteroidal anti-inflammatory drugs (NSAIDs), bracing, ultrasound, and therapeutic injections of corticosteroids, whole blood, or platelet rich-plasma. 1,5,8,27 Surgical intervention is typically reserved for those who exhibit recalcitrant symptoms with continued, quality of life-altering symptoms after 6 to 12 months of nonoperative management. 1,5,11,12,27,28 While different procedural treatment methods have been described, there is a lack of consensus regarding the optimal intervention for these patients.
For refractory lateral epicondylitis, excision of the diseased tissue (debridement) without reattachment to the lateral epicondyle has been the focus of many management plans with open, arthroscopic, and percutaneous methods demonstrating favorable long-term clinical outcomes. 7,9,20,24,30,34 Despite the overall success, long-term postoperative pain and loss of function have been reported, with up to 15% of cases experiencing criteria necessary to constitute failure (defined as poor outcomes score and/or reoperations) after isolated debridement. 26,32,34 As such, anatomic repair of the common extensor tendon to the lateral epicondyle, in addition to debridement, has been proposed to address the persistent pain and loss of function in these patients. 8,16,17,33 Excellent outcomes and significant increases in grip and pinch strength testing have been reported at 4 years after open debridement (OD) and concomitant tendon repair. 33 Although several case series have reported outcomes on OD alone or OD with repair (ODR) of lateral epicondylitis, there is a relative paucity of studies that have compared these 2 operative methods.
Reattachment or repair of the ECRB tendon with suture anchors after OD has been suggested to result in better short- and long-term functional outcomes as well as lower failure rates compared with OD alone. 16,17 However, these findings were in the setting of low-level evidence and comprised cohorts of limited size (ie, from 10 to 80 patients), which further limits the capacity to detect any mild or subtle difference in the complication profiles between these 2 approaches. 16,17 Large database studies may be better able to define the specific outcomes of OD alone compared with ODR.
The primary purpose of this study was to report and compare the 5-year reoperation rates of patients undergoing OD alone (OD cohort) versus ODR (ODR cohort). We hypothesized that the OD cohort would have a significantly higher 5-year reoperation rate compared with the ODR cohort. The secondary goals of this study were to identify the 90-day postoperative complications, total same-day reimbursements, and national usage trends from 2010 to 2019. Such comparative data may better inform surgical decision-making between the OD and ODR procedures.
Methods
Study Population
All data were acquired retrospectively from the PearlDiver upper extremity (MUExtr) database (PearlDiver Technologies), a commercially available administrative database containing 91 million patients within the United States. This is a deidentified and Health Insurance Portability and Accountability Act–compliant database. Given the deidentified nature of the data, our institutional review board granted exemption from approval for the conduction of this research.
The study period ranged from January 2010 to December 2019. Patients with an International Classification of Diseases, 9th Edition (ICD-9), or ICD-10 diagnosis code for “lateral epicondylitis” during this period were queried based on the following codes: ICD-9-D-72632, ICD-10-D-M7710, ICD-10-D-M7711, and ICD-10-D-M7712. The ICD-9/ICD-10 codes for lateral epicondylitis, only allowing for inclusion of patients diagnosed with lateral epicondylitis and exclusion of all other elbow diagnoses (ie, medial epicondylitis, rheumatoid arthritis, osteoarthritis, etc), were paired with the respective Current Procedural Terminology (CPT) codes for OD or ODR. 35 Cohorts of surgically treated patients were formed from pairing the ICD codes for lateral epicondylitis with the CPT code for “tenotomy, elbow, lateral or medial (eg, epicondylitis, tennis elbow, golfer’s elbow); debridement, soft tissue and/or bone, open” (CPT-24358) (for the OD cohort) or with the CPT code for “tenotomy, elbow, lateral or medial (eg, epicondylitis, tennis elbow, golfer’s elbow); and debridement, soft tissue and/or bone, open with tendon repair or reattachment” (CPT-24359) (for the ODR cohort).
Records were filtered based on first record of debridement and the presence of active records in the database for 90 days after index surgery. We excluded patients with certain concomitant procedures in addition to OD and ODR, including neuroplasty, radial tunnel release, cubital tunnel release, lateral collateral ligament reconstruction/repair, arthrotomy with synovectomy, arthroscopic synovectomy, and arthroscopic removal of loose bodies (CPT-64708, CPT-64722, ICD-9-D-3543, CPT-64718, CPT-64721, CPT-29848, CPT-24343, CPT-24344, CPT-24102, CPT-29835, CPT-29836, CPT-29834, respectively).
Adverse Events After 90 Days
The incidence of 90-day postoperative complications was assessed. Individual complications were assessed based on ICD codes for lateral epicondylitis after undergoing OD or ODR. Adverse events included acute kidney injury, deep vein thrombosis, hematoma formation, nerve injury, pulmonary embolism, sepsis, surgical-site infection, transfusion, and wound dehiscence. The designation “any adverse event” (AAE) was used if there was occurrence of at least 1 adverse event for a given patient within the 90-day time period. Demographic and comorbidity-based risk factors for 90-day AAEs were evaluated by multivariate analysis.
Reoperation Rates After 5 Years
The 5-year reoperation rates of the OD and ODR cohorts were investigated. Reoperation was defined by the presence of an ICD-10 code for lateral epicondylitis (ICD-10-D-M7711 or ICD-10-D-M7712) and CPT codes for any subsequent lateral epicondylitis procedure (open, arthroscopic, or percutaneous), including open elbow tenotomy with debridement (CPT-24358), debridement and tendon repair or reattachment (CPT-24359), percutaneous treatment (CPT-24357), or limited or extensive arthroscopic debridement (CPT-29837 or CPT-29838) within 5 years after index OD or ODR. Patients with ICD-9 codes were excluded from the reoperation analysis, as these codes do not include laterality. Only patients with ICD-10 codes that included documentation of laterality at the index procedure (right, ICD-10-D-M7711, or left, ICD-10-D-M7712) were included to calculate the reoperation rate, and any reoperations on the contralateral elbow (even for lateral epicondylitis) or the medial-sided ipsilateral elbow within the 5 years after index debridement were not counted as reoperations.
Kaplan-Meier curves were used to depict debridement durability in patients receiving index OD versus ODR. The Kaplan-Meier analysis of the PearlDiver software censored patients who were lost to follow-up before reaching the 5-year endpoint, thus yielding reoperation rates only for ICD-10 patients with complete records noting either reoperation or reoperation-free survivorship. Multivariate logistical regression analysis was used to control for any cofounding variables between OD versus ODR when calculating the reoperation rates.
Reimbursement
A cost analysis was performed to evaluate the difference in same-day total reimbursement amounts (in US$, currency rate averaged over the study period from 2010 to 2019) between OD (CPT-24358) and ODR (CPT-24359). These data represent all surgeon, facility, and prescription reimbursements associated with OD and ODR confined to the day of surgery. The mean reimbursement (±SE) for OD and ODR was compared.
Statistical Analysis
Patient demographic data were compared using an independent t test for continuous variables (age and Elixhauser Comorbidity Index [ECI] and Pearson chi-square test for categorical variables (sex, obesity, and tobacco use). Annual frequency of surgery for OD and ODR were assessed by comparison of the slopes of year-to-year trends in the 2 cohorts over the 5-year follow-up period.
Kaplan-Meier survival curves for 5-year reoperation rates in the OD and ODR cohorts were compared using a log-rank test. The ICD-10 codes for lateral epicondylitis (including elbow laterality) were paired with the relevant reoperation CPT codes. Multivariate logistic regression was also utilized to compare the 5-year reoperation risk between the OD and ODR cohorts, controlling for age, sex, tobacco use, and ECI score.
The risk of various postoperative complications for patients receiving OD versus ODR was assessed by multivariate logistic regression, controlling for age, sex, and ECI score. Adjusted odds ratios and 95% CIs were tabulated for risk of complications in patients who underwent OD relative to ODR. Multivariate logistic regression was also utilized to assess risk factors for any 90-day complications (90-day AAEs) in the overall (OD and ODR) cohort, controlling for sex, age, and various comorbidities, including asthma, chronic kidney disease (CKD), chronic obstructive pulmonary disease (COPD), congestive heart failure (CHF), coronary artery disease (CAD), diabetes, hypertension, obesity (defined by body mass index >30.0), and tobacco use.
Finally, the mean total reimbursements (±SE) for the day of surgery in the OD versus ODR cohort were compared via unpaired t test. All statistical analyses were performed using the PearlDiver software, Microsoft Excel, or GraphPad Prism, Version 9 (GraphPad Software). Significance was defined as P ≤ .05 for all analyses.
Results
Study Population
The study population consisted of 41,932 patients who underwent surgical treatment via OD (n = 17,139) or ODR (n = 24,793) for lateral epicondylitis from 2010 to 2019. Table 1 shows the patient characteristics by cohort. Compared with patients in the OD cohort, patients in the ODR cohort were significantly older (P = .05), more likely to be male (P = .003), and less likely to be tobacco users (P = .001) (Table 1).
Table 1.
Patient Demographics and Select Comorbidities by Study Group a
| OD Cohort (n = 17,139; 40.9%) |
ODR Cohort (24,793; 59.1%) |
P | |
|---|---|---|---|
| Age, y | 48.67 ± 8.49 | 49.11 ± 8.56 | .05 |
| Male sex | 7116 (41.5) | 10,658 (43.0) | .003 |
| Obesity | 4824 (28.1) | 6796 (27.4) | .10 |
| Tobacco use | 6716 (39.2) | 9104 (36.7) | <.001 |
| ECI score | 2.31 ± 2.50 | 2.34 ± 2.46 | .28 |
| ECI score grouping | |||
| 0 | 4607 (26.9) | 6304 (25.4) | |
| 1-3 | 8381 (48.9) | 12,458 (50.2) | |
| 4-5 | 2367 (13.8) | 3417 (13.8) | |
| >5 | 1784 (10.4) | 2614 (10.5) |
a Data are reported as mean ± SD or n (%). Boldface P values indicate statistically significant difference between groups (P ≤ .05). ECI, Elixhauser Comorbidity Index; OD, open debridement alone; ODR, open debridement with tendon repair.
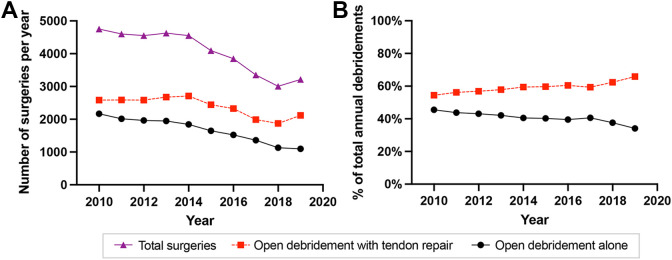
Between 2010 and 2019, there was an annual decrease in the number of procedures performed for both OD and ODR (with a slight increase in 2019 for ODR) (Figure 1A). Consequently, there was no significant change in the percentage of total surgeries via OD versus ODR each year (P = .18). While not statistically significant, there was a 6.5% increase in utilization of ODR relative to OD from 2017 to 2019. (Figure 1B).
Figure 1.
(A) Annual incidence (absolute number) of lateral epicondylitis debridements performed via OD versus ODR from 2010 to 2019 within the PearlDiver database. (B) Annual percentage of lateral epicondylitis debridements performed via OD versus an ODR approach as a percentage of the total surgeries performed annually (2010 to 2019) within the PearlDiver database. P = .18 for percentage trend over time. OD, open debridement alone; ODR, open debridement with tendon repair.
When stratified by age group, the patients who received the most lateral epicondyle debridement procedures were aged 40 to 44 years (n = 7404; 17.7% of total), 45 to 49 years (n = 10,014; 23.9% of total), and 50 to 54 years (n = 9166; 21.9% of total) years (Figure 2). These patients aged 40 to 54 years accounted for 63.4% of all debridements performed from 2010 to 2019.
Figure 2.
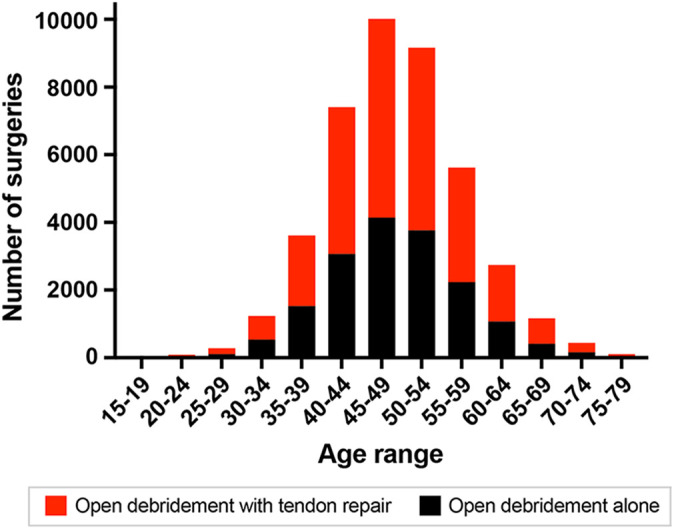
Age distribution of patients undergoing open debridement alone and open debridement with tendon repair for lateral epicondylitis from 2010 to 2019 within the PearlDiver database.
Adverse Events After 90 Days
The incidence of 90-day postoperative complications is depicted in Table 2. Logistic regression analysis revealed that patients who had ODR had fewer hematoma-related adverse events compared with patients who had OD (odds ratio, 0.58 [95% CI, 0.35-0.97]; P = .04).
Table 2.
Comparison of Adverse Events at 90 Days Postoperatively Between the OD and ODR Cohorts a
| Complication | OD Cohort (n = 17,139; 40.9%) |
ODR Cohort (n = 24,793; 59.1%)) |
Odds Ratio (95% CI) | P |
|---|---|---|---|---|
| 90-day AAEs | 190 (1.11) | 260 (1.05) | 0.99 (0.81-1.21) | .88 |
| Hematoma | 33 (0.19) | 30 (0.12) | 0.58 (0.35-0.97) | .04 |
| AKI | 33 (0.19) | 36 (0.15) | 0.76 (0.46-1.26) | .28 |
| SSI | 106 (0.62) | 118 (0.48) | 0.81 (0.61-1.07) | .14 |
| Transfusion | 5 (0.03) | 4 (0.02) | 0.82 (0.18-4.17) | .79 |
| Wound dehiscence | 33 (0.19) | 30 (0.12) | 0.98 (0.68-1.43) | .91 |
| Sepsis | 23 (0.13) | 30 (0.12) | 1.02 (0.57-1.90) | .94 |
| DVT | 33 (0.19) | 52 (0.21) | 1.02 (0.65-1.62) | .93 |
| Nerve injury | 15 (0.09) | 24 (0.10) | 1.41 (0.69-3.09) | .36 |
| PE | 18 (0.11) | 38 (0.15) | 1.52 (0.85-2.85) | .17 |
a Data are reported as n (%) unless otherwise indicated. Boldface P value indicates statistical significance (P ≤ .05). Each qualifying patient was only counted once regardless of the number of adverse events the patient experienced in that category. Comparisons were made using multivariate logistic regression, controlling for age, sex, tobacco use, and ECI. AAE, any adverse event; AKI, acute kidney injury; DVT, deep vein thrombosis; ECI, Elixhauser Comorbidity Index; OD, open debridement alone; ODR, open debridement with tendon repair; PE, pulmonary embolism; SSI, surgical site infection.
The incidence of 90-day AAEs was 1.11% for OD versus 1.05% for ODR (P = .88). By multivariate analysis, the ODR cohort had a significantly lower risk of hematoma formation compared with the OD cohort (0.12% vs 0.19%, respectively; odds ratio, 0.58; P = .04).
Assessing risk factors for complications, we found that asthma, CKD, COPD, CHF, CAD, diabetes, hypertension, obesity, and tobacco use were significant predictors of experiencing AAE in the 90 days after OD or ODR (P < .05 for each) (Table 3).
Table 3.
Risk Factors for 90-day AAEs in the Overall Cohort a
| Risk Factor | Odds Ratio (95% CI) | P |
|---|---|---|
| ODR | 1.03 (0.97-1.09) | .341 |
| Male sex | 1.04 (0.98-1.11) | .202 |
| Age >45 y | 1.01 (0.94-1.09) | .753 |
| Asthma | 1.18 (1.09-1.28) | <.001 |
| CKD | 3.83 (3.47-4.24) | <.001 |
| COPD | 1.62 (1.51-1.75) | <.001 |
| CHF | 2.06 (1.78-2.39) | <.001 |
| CAD | 1.41 (1.32-1.52) | <.001 |
| Diabetes | 1.50 (1.39-1.62) | <.001 |
| Hypertension | 1.35 (1.27-1.45) | <.001 |
| Obesity | 1.32 (1.24-1.41) | <.001 |
| Tobacco use | 1.53 (1.43-1.62) | <.001 |
a Comparisons were made using multivariate logistic regression. Boldface P values indicate statistical significance (P ≤ .05). AAE, any adverse event; CAD, coronary artery disease; CHF, congestive heart failure; CKD, chronic kidney disease; COPD, chronic obstructive pulmonary disease; ODR, open debridement with tendon repair.
Reoperation Rates After 5 Years
Kaplan-Meier analysis for the 5-year reoperation rates after OD and ODR can be seen in Figure 3. Overall, 15,105 patients (OD, 5663 and ODR, 9442) had 5-year follow-up data and ICD-10 laterality-specific diagnosis coding to be included in the reoperation analysis. Furthermore, OD had 162 reoperations (3.9%) and ODR had 195 reoperations (2.8%) at 5 years follow-up. ODR had a significantly lower reoperation rate than OD (2.8% vs 3.9%), with an absolute risk reduction of 1.1% and a number needed to treat of 91. Based on the log-rank test, the 5-year reoperation rate was significantly greater in the OD cohort relative to the ODR cohort (P = .006). Multivariate logistic regression analysis showed that the risk of reoperation was still significantly greater in the OD versus ODR cohort when controlling for age, sex, tobacco smoking, and ECI score (odds ratio = 1.67 [95% CI, 1.26-2.21]; P < .001).
Figure 3.
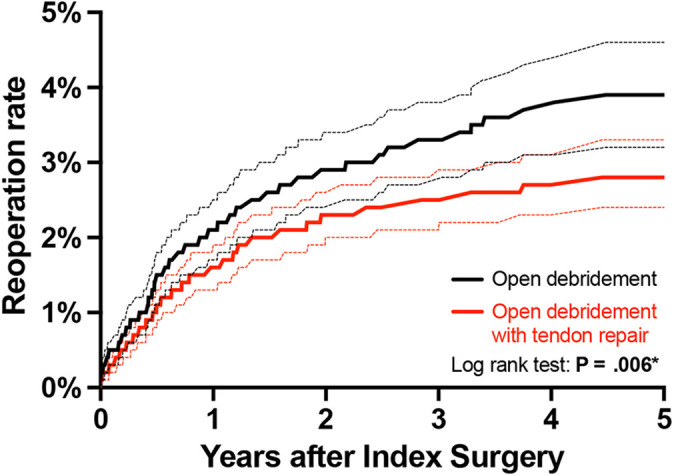
Five-year Kaplan-Meier curves depicting reoperation rates for lateral epicondylitis in patients undergoing index OD versus ODR. Curves were compared by log-rank test, with a cumulative 5-year reoperation rate of 3.9% for patients undergoing OD versus 2.8% for patients undergoing ODR (P = .006). OD, open debridement alone; ODR, open debridement with tendon repair. * is used to show the significant P-value.
Reimbursement
On average, there was a 13.8% increase in reimbursement for ODR compared with OD. The mean same-day total reimbursement for OD was $1479.05 ± $15.78, which was significantly lower compared with ODR of $1683.17 ± $12.15 (P < .001) (Figure 4).
Figure 4.
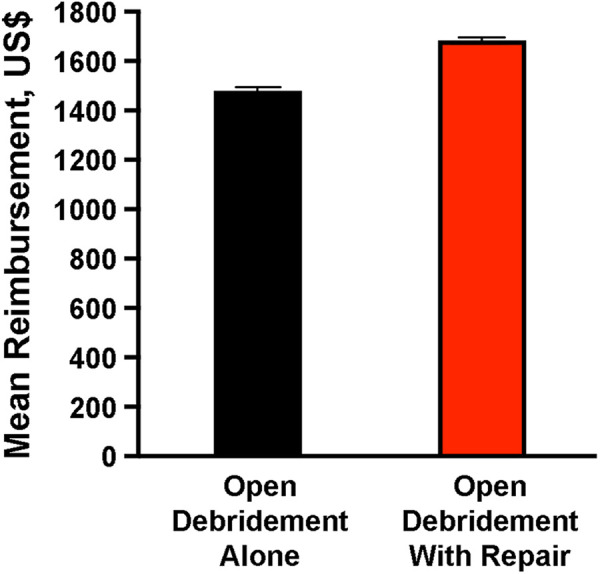
Mean total reimbursement for day of surgery treatment for OD versus ODR for lateral epicondylitis. Error bars represent SE. Mean reimbursement for OD was $1,479.05 ± $15.78, and mean reimbursement for ODR was $1,683.17 ± $12.15 (P < .001). OD, open debridement alone; ODR, open debridement with tendon repair.
Discussion
This study showed that the 5-year reoperation rate for patients undergoing open debridement, regardless of concomitant tendon repair, was low. However, OD (3.9%) had a slightly but statistically significantly higher reoperation rate than ODR (2.8%). These findings statistically confirmed our primary hypothesis of higher reoperation rates existing in patients undergoing OD versus those undergoing ODR; however, the clinical significance that pertains to this subtle difference needs to be further elucidated. In addition, this study found the incidence of 90-day complications was low for both OD and ODR, with no differences detected between the 2 cohorts apart from hematoma’s being slightly more common in the ODR cohort. We also identified asthma, CKD, COPD, CHF, CAD, diabetes, obesity, hypertension, and tobacco use as all being significant predictors of experiencing 90-day AAEs after OD or ODR. From 2010 to 2019, the total number of open debridements (alone and with repair) performed decreased, with no statistically significant changes in the percentage of OD versus ODR performed annually. Finally, ODR ($1683.17) had a mean 14% higher same-day total reimbursement rate compared with OD ($1479.05).
As described in the earlier studies involving Nirschl 9,19 as well as Nirschl and Pettrone, 20 debridement with primary repair of the ECRB tendon has demonstrated favorable and durable outcomes with high rates of satisfaction and return to full activity. In a case series of 16 patients, Thornton et al 33 reported less postoperative pain, superior grip and pinch strength, and no failures after debridement and repair of the ECRB tendon to the lateral epicondyle at minimum 2 years follow-up. Similarly, Li et al 16 reported significantly better outcomes for patients who underwent arthroscopic debridement with tendon repair (n = 19) compared with those who underwent arthroscopic debridement alone (n = 33), with no reported failures at minimum 1 year follow-up. In a randomized controlled trial, Monto 17 reported that OD and anatomic repair of the ECRB tendon resulted in clinically superior outcomes in all short-term and long-term scoring intervals compared with those treated with OD alone. Interestingly, there were zero failures in the repair group (defined as poor outcomes and/or reoperations), but 3 of 30 (10%) clinical failures in the OD alone group, with 2 of these failures undergoing subsequent conversion to anchored repairs with excellent clinical results. 17 However, the primary limitation cited by both Li et al and Monto pertained to the relatively small sample sizes used to report their comparative findings of operative failure. Therefore, with the 2008 implementation of more specific CPT codes and laterality-specific ICD-10 codes in 2015, the present study aimed to better define and differentiate the failure rates of OD versus ODR in a large cohort of patients. 35
In the present study, we analyzed 15,105 patients with both ICD-10 coded diagnoses and 5-year follow-up data who were initially treated with OD or ODR. We found that patients treated with OD (n = 162 reoperations; 3.9%) had higher reoperation rates than patients treated with ODR (n = 195 reoperations; 2.8%) at 5-year follow-up. While previous systematic reviews have not differentiated between OD and ODR, these failure rates are in agreement and within the range of the reported failure rate (2% to 5%) for open procedures. 3,13,18,21,25,29,36 Furthermore, previous studies have suggested that common extensor tendon repair to the lateral epicondyle after debridement may enhance the biomechanical healing at the origin of tendon compared with an unrepaired tendon. 14,16,17,23,33 Previous studies have used this as an explanation for the reported improved outcomes and lower failure rates compared with those treated without repair. 16,17 Similarly, this may be the reason for the slightly but significantly lower reoperation rates seen in our ODR cohort. In addition, the present study found that 91 patients would need to be treated with ODR to prevent 1 reoperation compared with OD. It is important to note that, although the difference in failure rates is statistically significant, there was an overall small difference in reoperation rates between the procedures. To our knowledge, these failure rates, defined by the presence of a secondary lateral epicondylitis surgery, have not been reported using large cohorts, and the clinical and biomechanical significance of these findings need to be further investigated.
The 90-day adverse events for OD and ODR have not previously been well-defined. The most common complication for OD and ODR in the present study was surgical-site infection (0.6%). This finding is in agreement with Pomerantz, 22 who analyzed the complication rates from 67 articles and reported an overall infection rate of 0.5% in open procedures of lateral epicondylitis. In addition, hematoma formation has been reported in multiple cases after open treatment for lateral epicondylitis. 2,22,24,31,37 Although rare, we found that OD had a significantly higher incidence of hematoma (n = 33; 0.19%) formation than ODR (n = 30; 0.12%) (P = .04). This discrepancy, although significant, could be the result of the adequate power of this study to detect a subtle difference, differences in patient selection, or greater percentage of tobacco smokers undergoing OD, but the possibility remains that it could also be the attributed to the increased dead space available for hematoma formation at the extensor origin when the tendon is not repaired. Nevertheless, the 90-day adverse events reported from our large cohort suggests that OD and ODR can be performed safely, with similar rates between the 2 methods.
In addition to the complication rates for OD and ODR, we found that asthma, CKD, COPD, CHF, CAD, diabetes, hypertension, obesity, and tobacco use were significant predictors of experiencing 90-day postoperative adverse events after OD and ODR. Similarly, Guillou et al 10 analyzed the prognostic factors for surgically treated lateral epicondylitis and found that tobacco use was associated with poor outcomes. Few studies have defined specific risk factors for 90-day adverse events after OD or ODR of lateral epicondylitis. 10 While there were minimal differences in 90-day adverse events between the cohorts, surgeons should be aware of these potential risk factors as we work toward improving patient outcomes and mitigating procedure-associated risks.
Finally, from 2010 to 2019, the overall number of ODs (alone and with repair) performed decreased. These results are in agreement with Wang et al, 35 who reported a decrease in incidence for open procedures of lateral epicondylitis. We found that there were no significant changes in the percentage of OD versus ODR performed annually. While not statistically significant, there was a 6.5% increase in utilization of ODR relative to OD from 2017 to 2019. In addition, the same-day total reimbursement rate for ODR was 14% higher ($1683.17 ± $12.15) on average and significantly greater than that of OD ($1479.05 ± $15.78). The higher surgeon reimbursement rates for ODR reported in this study may be explained by the longer operative time and increased amount of labor when performing concomitant repair. 17,27,36 While these secondary outcomes are less important for choosing between OD and ODR, reimbursement rates provide important information on health care spending considerations. This study uses a large number of patients to compare OD versus ODR for lateral epicondylitis, and these findings may be the first step in developing more focused randomized controlled trials to assess these 2 operative methods.
Strengths and Limitations
The present study has some notable strengths. First, advantages of the PearlDiver database include its diverse, nationally representative patient population, which covers the nation geographically and also with respect to insurance plan types, including commercial insurance, Medicare, Medicaid, and self-pay. Next, the large number of patients included in this study allows for adequate power to compare rare events, such as reoperations and complications, in patients undergoing OD alone or OD with common extensor tendon repair for lateral epicondylitis.
There are several well-documented limitations inherent to large national databases such as PearlDiver and the retrospective nature of this study. The use of ICD codes allowed us to include patients that were diagnosed only with lateral epicondylitis and exclude any other diagnoses (eg, medial epicondylitis, rheumatoid arthritis, osteoarthritis, etc) when paired with specific post-2008 CPT codes. However, whenever such coding is used, the accuracy of the data is a reflection of the accuracy of coding performed by physicians and billers.
Second, as data available from this national administrative database are based on claims data, variables outside those already present in the database are not available. Therefore, we were unable to assess factors such as extent of lateral epicondyle disease, strength, activity differences, anticoagulant use, NSAID use, or workers’ compensation status between treatment groups. However, we sought to eliminate common limitations associated with reporting reoperation rates from a large database like PearlDiver. First, the 5-year operation rate included only patients with a documented ICD-10 diagnosis code for lateral epicondylitis and excluded any patient with ICD-9 codes (ambiguous laterality). In addition, the ICD-10 codes for lateral epicondylitis indicate laterality (right or left elbow) of the index and (if relevant) revision procedures and thus can track ipsilateral reoperations for only the treatment of lateral epicondylitis during the 5-year follow-up period. As such, we were able to exclude any reoperations on the ipsilateral elbow that were not related to the initial lateral epicondylitis (ie, medial epicondylitis, rheumatoid arthritis, osteoarthritis, or any other diagnoses) and any operations on the contralateral elbow (even for lateral epicondylitis) that would have otherwise been counted as a reoperation. We also used multivariate logistical regression to control for potential cofounders. Cumulatively, we believe the use of ICD-10 diagnosis code for lateral epicondylitis, laterality-specific codes for the index and revision procedures, and use of multivariate logistical regression to control for potential confounders, eliminated many of the previously reported PearlDiver database limitations when using unspecific coding and ambiguous laterality.
A third limitation was that, as a result of our cohorts for OD and ODR deriving from CPT-code based claims data, we were unable to characterize the specific surgical approaches used for ECRB tendon repair (eg, direct suture anchor repair/reattachment vs side-to-side repair) within our ODR cohort and particular indication for OD versus ODR. Based on experience in our institution, surgeon preference frequently influences the decision to pursue OD versus ODR. ODR has also been proven to be particularly effective for chronic, recalcitrant lateral epicondylitis with regard to strength, return to previous activities, and pain relief and to produce more consistent outcomes. 33 However, lack of randomization with regard to whether tendon repair was performed could affect our results. Fourth, our cost data derived from day-of-surgery reimbursements to the surgeon and the facility and for prescription medications. The PearlDiver database prevents us from analyzing the total cost of the surgeries to the health care system (which also includes cost of implants for anchor repairs)–-a metric that would further aid assessment of the cost versus benefit of ODR versus OD alone for lateral epicondylitis. Finally, although we did not use a Bonferroni correction, which has been debated in the literature, we acknowledge that this may have computed insignificant findings for hematoma formation and reoperation rates. In light of this, we favored reporting these results but focused the discussion on the clinical application given the small difference in magnitude but statistically significant difference. Given the large cohort and power used to report the findings in this study, the clinical significance and differences between the 2 procedures need to be clinically correlated in future studies.
Conclusion
For recalcitrant lateral epicondylitis, OD and ODR had very low complication rates. While the 5-year reoperation rate was low in patients treated with both methods, it was significantly higher in those treated with OD. Over the 10-year period, there were no significant changes in the relative percentages of OD versus ODR performed. ODR had a significantly higher mean same-day surgeon reimbursement.
Footnotes
Final revision submitted May 21, 2022; accepted June 6, 2022.
One or more of the authors has declared the following potential conflict of interest or source of funding: A.E.J. has received education payments from Medwest. R.V. has received education payments from Mid-Atlantic Surgical Systems. A.D.N. has received grant support from Arthrex. T.A.B. has received consulting fees from Catalyst OrthoScience, Stryker, Wright Medical, and Zimmer Biomet; speaking fees from Wright Medical; and hospitality payments from Arthrex. D.W.A. has received consulting fees and royalties from Stryker and hospitality payments from Arthrex. L.V.G. has received education payments from Gotham Surgical; consulting fees from DePuy/Medical Device Business Services, Exactech, and Zimmer Biomet; speaking fees from Smith & Nephew; and royalties from Exactech. J.S.D. has received consulting fees from Arthrex, Merck Sharp & Dohme, and Trice Medical; nonconsulting fees from Arthrex; and royalties from Arthrex and Linvatec. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
Ethical approval was not sought for the present study.
References
- 1. Allander E. Prevalence, incidence, and remission rates of some common rheumatic diseases or syndromes. Scand J Rheumatol. 1974;3(3):145–153. [DOI] [PubMed] [Google Scholar]
- 2. Barth J, Mahieu P, Hollevoet N. Extensor tendon and fascia sectioning of extensors at the musculotendinous unit in lateral epicondylitis. Acta Orthop Belg. 2013;79(3):266–270. [PubMed] [Google Scholar]
- 3. Burn MB, Mitchell RJ, Liberman SR, et al. Open, Arthroscopic, and percutaneous surgical treatment of lateral epicondylitis: a systematic review. Hand (N Y). 2018;13(3):264–274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Calfee RP, Patel A, DaSilva MF, Akelman E. Management of lateral epicondylitis: current concepts. J Am Acad Orthop Surg. 2008;16(1):19–29. [DOI] [PubMed] [Google Scholar]
- 5. Clark T, McRae S, Leiter J, et al. Arthroscopic versus open lateral release for the treatment of lateral epicondylitis: a prospective randomized controlled trial. Arthroscopy. 2018;34(12):3177–3184. [DOI] [PubMed] [Google Scholar]
- 6. Coonrad RW, Hooper WR. Tennis elbow: its course, natural history, conservative and surgical management. J Bone Joint Surg Am. 1973;55(6):1177–1182. [PubMed] [Google Scholar]
- 7. Das D, Maffulli N. Surgical management of tennis elbow. J Sports Med Phys Fitness. 2002;42(2):190–197. [PubMed] [Google Scholar]
- 8. Donaldson CT, Finley ZJ, O’Brien MJ. Lateral epicondylitis debridement and repair using knotless suture anchor. Arthrosc Tech. 2019;8(7):e775–e779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Dunn JH, Kim JJ, Davis L, Nirschl RP. Ten- to 14-year follow-up of the Nirschl surgical technique for lateral epicondylitis. Am J Sports Med. 2008;36(2):261–266. [DOI] [PubMed] [Google Scholar]
- 10. Guillou J, Pougès C, Limousin M, Strouck G, Fontaine C. Arthroscopic treatment of work-related lateral epicondylitis–-prognostic factors. Hand Surg Rehabil. 2019;38(1):24–27. [DOI] [PubMed] [Google Scholar]
- 11. Hamilton PG. The prevalence of humeral epicondylitis: a survey in general practice. J R Coll Gen Pract. 1986;36(291):464–465. [PMC free article] [PubMed] [Google Scholar]
- 12. Hume PA, Reid D, Edwards T. Epicondylar injury in sport: epidemiology, type, mechanisms, assessment, management and prevention. Sports Med. 2006;36(2):151–170. [DOI] [PubMed] [Google Scholar]
- 13. Ikonen J, Lähdeoja T, Ardern CL, et al. Persistent tennis elbow symptoms have little prognostic value: a systematic review and meta-analysis. Clin Orthop Relat Res. 2021;480(4):647–770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Khashaba A. Nirschl tennis elbow release with or without drilling. Br J Sports Med. 2001;35(3):200–201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Kraushaar BS, Nirschl RP. Tendinosis of the elbow (tennis elbow). Clinical features and findings of histological, immunohistochemical, and electron microscopy studies. J Bone Joint Surg Am. 1999;81(2):259–278. [PubMed] [Google Scholar]
- 16. Li X, Zheng T, Li Y, Zhang H, Lu Y. A retrospective comparative study on arthroscopic suture anchors repair and tendon debridement. Ther Adv Chronic Dis. 2021;12:20406223211005596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Monto RR. Tennis elbow repair with or without suture anchors. Tech Shoulder Elbow Surg. 2014;15(3):92–97. [Google Scholar]
- 18. Moradi A, Pasdar P, Mehrad-Majd H, Ebrahimzadeh MH. Clinical outcomes of open versus arthroscopic surgery for lateral epicondylitis, evidence from a systematic review. Arch Bone Jt Surg. 2019;7(2):91–104. [PMC free article] [PubMed] [Google Scholar]
- 19. Nirschl RP. Lateral extensor release for tennis elbow. J Bone Joint Surg Am. 1994;76(6):951. [DOI] [PubMed] [Google Scholar]
- 20. Nirschl RP, Pettrone FA. Tennis elbow. The surgical treatment of lateral epicondylitis. J Bone Joint Surg Am. 1979;61(6A):832–839. [PubMed] [Google Scholar]
- 21. Pierce TP, Issa K, Gilbert BT, et al. A systematic review of tennis elbow surgery: open versus arthroscopic versus percutaneous release of the common extensor origin. Arthroscopy. 2017;33(6):1260–1268.e1262. [DOI] [PubMed] [Google Scholar]
- 22. Pomerantz ML. Complications of lateral epicondylar release. Orthop Clin North Am. 2016;47(2):445–469. [DOI] [PubMed] [Google Scholar]
- 23. Pruzansky ME, Gantsoudes GD, Watters N. Late surgical results of reattachment to bone in repair of chronic lateral epicondylitis. Am J Orthop (Belle Mead NJ). 2009;38(6):295–299. [PubMed] [Google Scholar]
- 24. Rayan GM, Coray SA. V-Y slide of the common extensor origin for lateral elbow tendonopathy. J Hand Surg Am. 2001;26(6):1138–1145. [DOI] [PubMed] [Google Scholar]
- 25. Riff AJ, Saltzman BM, Cvetanovich G, et al. Open vs percutaneous vs arthroscopic surgical treatment of lateral epicondylitis: an updated systematic review. Am J Orthop (Belle Mead NJ). 2018;47(6):10.12788/ajo.2018.0043. [DOI] [PubMed] [Google Scholar]
- 26. Rosenberg N, Henderson I. Surgical treatment of resistant lateral epicondylitis: follow-up study of 19 patients after excision, release and repair of proximal common extensor tendon origin. Arch Orthop Trauma Surg. 2002;122(9-10):514–517. [DOI] [PubMed] [Google Scholar]
- 27. Sanders TL, Maradit Kremers H, Bryan AJ, et al. The epidemiology and health care burden of tennis elbow: a population-based study. Am J Sports Med. 2015;43(5):1066–1071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Shiri R, Viikari-Juntura E. Lateral and medial epicondylitis: role of occupational factors. Best Pract Res Clin Rheumatol. 2011;25(1):43–57. [DOI] [PubMed] [Google Scholar]
- 29. Smidt N, Assendelft WJ, van der Windt DA, et al. Corticosteroid injections for lateral epicondylitis: a systematic review. Pain. 2002;96(1-2):23–40. [DOI] [PubMed] [Google Scholar]
- 30. Solheim E, Hegna J, Øyen J. Arthroscopic versus open tennis elbow release: 3- to 6-year results of a case-control series of 305 elbows. Arthroscopy. 2013;29(5):854–859. [DOI] [PubMed] [Google Scholar]
- 31. Solheim E, Hegna J, Øyen J. Extensor tendon release in tennis elbow: results and prognostic factors in 80 elbows. Knee Surg Sports Traumatol Arthrosc. 2011;19(6):1023–1027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Szabo SJ, Savoie FH, Field LD, Ramsey JR, Hosemann CD. Tendinosis of the extensor carpi radialis brevis: an evaluation of three methods of operative treatment. J Shoulder Elbow Surg. 2006;15(6):721–727. [DOI] [PubMed] [Google Scholar]
- 33. Thornton SJ, Rogers JR, Prickett WD, et al. Treatment of recalcitrant lateral epicondylitis with suture anchor repair. Am J Sports Med. 2005;33(10):1558–1564. [DOI] [PubMed] [Google Scholar]
- 34. Verhaar J, Walenkamp G, Kester A, van Mameren H, van der Linden T. Lateral extensor release for tennis elbow. A prospective long-term follow-up study. J Bone Joint Surg Am. 1993;75(7):1034–1043. [DOI] [PubMed] [Google Scholar]
- 35. Wang D, Degen RM, Camp CL, et al. Trends in surgical practices for lateral epicondylitis among newly trained orthopaedic surgeons. Orthop J Sports Med. 2017;5(10):2325967117730570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Wang W, Chen J, Lou J, Shentu G, Xu G. Comparison of arthroscopic debridement and open debridement in the management of lateral epicondylitis: a systematic review and meta-analysis. Medicine (Baltimore). 2019;98(44):e17668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Zingg PO, Schneeberger AG. Debridement of extensors and drilling of the lateral epicondyle for tennis elbow: a retrospective follow-up study. J Shoulder Elbow Surg. 2006;15(3):347–350. [DOI] [PubMed] [Google Scholar]