Abstract
Background:
To examine the feasibility and acceptability of integrating a tele-mentoring component into the identification of oral lesions at the dental clinics of a Federally Qualified Health Center network.
Design and Methods:
General Practice Residency faculty and residents completed research ethics courses and trained dentists to use intra-oral cameras at chairside to photograph oral lesions of patients at routine dental visits. These images were then uploaded into the patient electronic health records (EHRs) with attendant descriptions and an oral surgeon was notified, who reviewed the charts, placed his observations in the EHR, and communicated his findings via secure e-mail to the involved residents, who in turn contacted their patients regarding follow-up actions. Feasibility was assessed via checklists completed by provider participants and semi-structured interviews. Acceptability was assessed via brief exit interviews completed by patient participants.
Results:
All 12 of the dentist participants reported that they had successfully provided the tele-mentoring intervention, and that the process (from EHR data entry to interaction with the oral surgeon over findings to patient referral) was clear and straightforward. Of 39 patient participants, most strongly agreed or agreed that the use of an intra-oral camera by their dentists helped them to better understand oral cancer screening (94.9%) and that dentists answered their questions about oral cancer and were able to provide them with resources (94.8%).
Conclusions:
Findings support further implementation research into adapting tele-mentoring using intra-oral cameras for training dental residents to detect and identify oral lesions and educating patients about oral cancer across settings.
Keywords: Telemedicine, early detection of cancer, preventive dentistry, vaccine preventable diseases, electronic health records
Introduction
According to the Annual Report to the Nation on the Status of Cancer, age-standardized oral and oropharyngeal cancer incidence rates increased for the period 2001–2018, with average annual percentage increases of 0.9% for men and 0.5% for women. 1 Age-standardized oral and oropharyngeal mortality rates also increased for men, with an average annual percentage increase of 0.5%, but dropped slightly for women (−0.1%). 1 The increasing incidence trends are limited to cancers in subsites with a strong association with human papillomavirus (HPV) infection, such as oropharynx and tonsils, likely due to changes in sexual practices, whereas rates are declining in other subsites, perhaps due to lower smoking prevalence.2,3
Strategies to decrease the incidence and mortality of oral and oropharyngeal cancers include evidence-based prevention strategies such as motivational interviewing (MI) to improve oral health education 4 and HPV vaccination to prevent infections and cancers of oropharynx, tonsils, and base of the tongue in both women and men.5–7 Visual and tactile screening by dentists at chairside during routine examinations for the discovery of pre- and cancerous lesions or other conditions that may benefit from treatment or close follow-up is also recommended.8,9
While not a new concept, the pace of telehealth technologies and methodologies to deliver oral health services has accelerated due to the ongoing COVID-19 pandemic. 10 The asynchronous (store and forward) technique captures electronic patient information such as photographs and then stores and forwards this information through a secure electronic communications system such as an electronic health record (EHR) to a treating dental provider for evaluation outside of a real-time or live interaction. 10
Low-cost intra-oral cameras may facilitate the detection and recording of carious, non-malignant, pre-malignant, and malignant lesions in the patient EHR11,12 and enhance both synchronous (live video) and asynchronous teledentistry modalities. 10 With the arrival of COVID-19, dental faculty were forced to implement remote learning and find meaningful clinical experiences for students and residents.13,14 While debate exists regarding whether or not dental schools ought to adopt teledentistry into their curricula, 15 already dental practices and programs are embracing teledentistry as a new service line, rather than merely a pandemic safety intervention. 16
The aim of this pilot study is to assess the feasibility and acceptability of integrating a tele-mentoring component using intra-oral cameras into the detection and identification of oral lesions at the dental clinics of Family Health Centers at NYU Langone, a Federally Qualified Health Center (FQHC) network in Brooklyn, NY. The General Practice Residency (GPR) program director, faculty, and residents collaborated with NYU Langone Health oral surgeons, dentists, administrators, research staff, biostatisticians, and technology experts to design, implement, and evaluate this pilot study.
Design and methods
Ethical safeguards
This research was performed in accordance with the Declaration of Helsinki. The NYU Grossman School of Medicine Institutional Review Board (IRB) reviewed and approved all study procedures on October 30, 2019 (protocol s19-01268). All Health Insurance Portability and Accountability Act (HIPAA) safeguards were followed. Written consent was obtained from each participant in accordance with the IRB-approved protocol, an abbreviated version of which was published that includes the study instruments as three appendices. 17
Study design
A mixed methods approach was used, guided by the Consolidated Framework for Implementation Research (CFIR) 18 and the Implementation Outcomes Framework (IOF). 19 Feasibility was assessed using two methods. First, surveys were administered to dentist participants that consisted of a checklist of 10 “essential components” of the tele-mentoring process who then endorsed each of the items that were met. The a priori feasibility criterion of the intervention was the endorsement of 8 of the 10 checklist items (80%) by the dentist participants. Second, semi-structured interviews were conducted with dental resident participants at the completion of the study to assess specific barriers to sustaining the intervention and strategies for addressing these barriers to facilitate integration of the intervention into the routine workflow of the dental clinics.
Acceptability was assessed using patient exit interviews 20 consisting of five statements about the oral cancer prevention and screening intervention they just underwent and asking the patient participants to indicate on a Likert scale whether they strongly disagree, disagree, neither disagree nor agree, agree, or strongly agree with each statement. The a priori acceptability criterion of the intervention was that 80% or more of patient participants would rate all five administered acceptability questions as agree or strongly agree.
Study device
The SOPROCARE® intra-oral camera that was used in this pilot study is intended for the practice of general dentistry to aid in the diagnosis of pit and fissure caries, visualize anatomical details that are invisible to the naked eye or with a mirror, and highlight dental plaque and gingival inflammation. 21 The magnification capability of the intra-oral camera was hypothesized to improve the detection and subsequent identification of oral lesions. Photographs captured by dental residents at chairside and stored in the Dexis imaging software within the Dentrix EHR provided the necessary technological advances to practice minimally invasive dentistry, which became increasingly important with the onset of the COVID-19 pandemic and concerns about viral transmission in dental settings.
Study procedures for training dentists and conducting the intervention
The tele-mentoring procedure involved training the NYU Langone Health General Practice Residency (GPR) Program dental faculty members and residents to use intra-oral cameras to take photographs of oral lesions with patients who had already been diagnosed at their recall visits. This research was conducted in July–November 2021 in Brooklyn, NY, before COVID-19 vaccines were available, following New York State interim guidance for dentistry to minimize viral spread once elective dental procedures were permitted to resume. 22 Note that no participants were recruited during the research pause at NYU Langone Health that was instituted on March 9, 2020 and titled, Policy on Human Subjects Research During COVID-19 (Pause Criteria).
Participant recruitment for the feasibility and acceptability study began in July 2020 once the research pause was lifted. Given dental provider furloughs and limited dental clinic operations at that time, a new oral surgeon expert was recruited to mentor the dental residents and only three of the six Family Health Centers at NYU Langone dental clinics were used as research sites. Further adaptations to the protocol were necessary to comply with stricter precautions instituted at the health center to protect providers, staff, and patients against COVID-19.
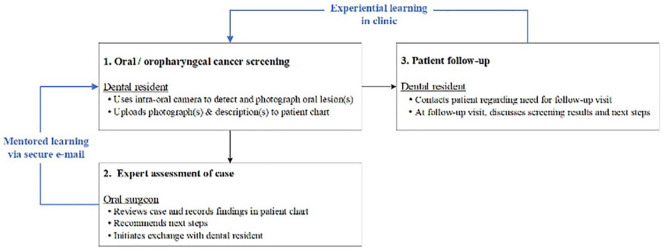
Figure 1 provides the general workflow for the tele-mentoring intervention.
Figure 1.
This graphic is derived from Figure 1 titled, Workflow for the tele-mentoring pilot study to detect and identify oral lesions at chairside by dental faculty and residents that was published as part of the protocol article for this pilot study. 17 The focus in this simplified schematic is on the mentored and experiential learning of the dental residents as part of the tele-mentoring intervention.
At routine dental visits for patients aged 18 years and older, GPR dental residents trained in the use of intra-oral cameras took photographs of any oral lesions detected and uploaded them to the Dentrix EHR using Dentris software as part of the standard noninvasive intra-oral and extra-oral visual and tactile examination in all adult patients recommended at initial and recall appointments.23,24 This information was then sent via the Dentrix EHR to the study oral surgeon, and an initial dummy code entry was placed in the Dentrix EHR. For each patient with a detected lesion, the oral surgeon then reviewed the Dentrix EHR chart that included the uploaded photograph(s) of the lesion(s) found and placed his observations in the Dentrix EHR. As part of the tele-mentoring process, the oral surgeon discussed his findings with the dental resident participants via secure NYU Langone Health e-mail, who in turn entered an apt comment in the Dentrix EHR using the following template: “Reviewed entry and contacted patient. Follow-up appointment needed/not needed (along with the date of patient contact) for an appointment on (date).” A second dummy code entry was then placed in the patient record in the Dentrix EHR. Once a week, the oral surgeon received a Dentrix EHR report with the two affiliated dummy codes for the pilot study, and assured that entries for both codes were completed, thus closing the loop on the process. 17
Data analysis
The short survey data collected from the dental provider checklists and the patient exit interviews were analyzed by the study data analyst who was supervised by the study biostatistician using the statistical software R version 4.1.0. 25 To obtain descriptive statistics, continuous variables were summarized with means and standard deviations (SDs) and categorical variables were summarized with counts and percentages.
The semi-structured interviews with the dental residents were digitally recorded and transcribed for analysis. Thematic content analysis26,27 was then used to understand more about the perceived benefits of the tele-mentoring intervention and suggestions for improving the process. To enhance the validity of the coding scheme, two members of the study team began the data analysis by each independently reading the transcribed key informant interviews to identify the topics discussed. To isolate the text in which participants discussed sub-themes related to perceived benefits and suggestions for improving the intervention, a senior member of the study team scrutinized the transcripts and extracted relevant sections of the text. Next, pertinent quotes were organized to characterize the specific views described by the study participants. Opinions that were expressed by multiple dental resident participants are presented in this article. Quotes were first grouped by major theme (perceived benefits of the intervention and suggestions for improving the intervention) and further organized by sub-themes that best represent the perceptions described by the dental resident participants.
Results
All 12 dentist participants were GPR dental residents with a mean age of 26.7 years (SD = 1.4). Most of the dentist participants were female (83.3%) and non-Hispanic Asian (66.7%). These demographic results are publicly available in the ClinicalTrials.gov record for this pilot study (see the CLINICAL TRIALS REGISTRATION section of this article for the pertinent details).
The patient participant demographic characteristics are presented in Table 1.
Table 1.
Patient demographic characteristics (n = 39).
| Continuous characteristic | Mean (SD) |
|---|---|
| Age (in years) | 40.9 (20.6) |
| Categorical characteristic | n a (%) |
| Gender | |
| Female | 20 (51.3) |
| Male | 19 (48.7) |
| Race/ethnicity | |
| Hispanic | 25 (65.8) |
| Non-Hispanic White | 6 (15.8) |
| Non-Hispanic Black | 1 (2.6) |
| Non-Hispanic Unspecified Race | 6 (15.8) |
| Dental clinic site | |
| Sunset Park | 18 (46.2) |
| Park Ridge | 12 (30.8) |
| Sunset Terrace | 9 (23.1) |
| Preferred language | |
| English | 19 (48.7) |
| Spanish | 20 (51.3) |
| Marital status | |
| Divorced | 1 (2.6) |
| Married | 15 (38.5) |
| Never married | 20 (51.3) |
| Separated | 2 (5.1) |
| Other | 1 (2.6) |
Numbers within characteristics may vary due to missing values.
The 39 patient participants had a mean age of 40.9 years (SD = 20.6). Most of the patient participants were female (51.3%), Hispanic (65.8%), spoke Spanish as their preferred language (51.3%), and were never married (51.3%). Almost half (46.2%) visited the Sunset Park dental clinic for their dental care and to participate in this study, which is the main dental clinic and hospital site at Family Health Centers at NYU Langone.
The patient exit interview results are presented in Table 2.
Table 2.
Patient exit interview results (n = 39).
| Statement | n a (% b ) |
|---|---|
| Dentists should discuss with me ways to prevent and screen for oral cancer. | |
| Agree | 21 (53.8) |
| Strongly agree | 18 (46.2) |
| The use of an intra-oral camera by my dentist helped me to better understand oral cancer screening. | |
| Neutral | 2 (5.1) |
| Agree | 19 (48.7) |
| Strongly agree | 18 (46.2) |
| The content of the educational material I received from my dentist was useful/helpful. | |
| Neutral | 7 (18.4) |
| Agree | 17 (44.7) |
| Strongly agree | 14 (36.8) |
| My dentist was able to answer my questions about oral cancer and was able to provide me with resources during our conversation. | |
| Neutral | 2 (5.1) |
| Agree | 21 (53.8) |
| Strongly agree | 16 (41.0) |
| After the conversation with my dentist about oral cancer prevention and screening, I would feel comfortable to reach out to my dentist/dental office if I had more questions about oral cancer. | |
| Neutral | 1 (2.7) |
| Agree | 18 (48.6) |
| Strongly agree | 18 (48.6) |
Numbers within statements may vary due to missing values.
Totals may not sum to 100% due to rounding.
The acceptability criterion was met, as 80% or more of the patient participants rated all five administered acceptability questions as agree or strongly agree. For instance, all 39 patient participants (100%) agreed or strongly agreed that dentists should discuss ways to prevent and screen for oral cancer with them, while fewer (31 patient participants or 81.5%) agreed or strongly agreed that the educational material they received from their dentist was useful/helpful.
The dentist participant “essential items” checklist results are presented in Table 3.
Table 3.
Provider “essential items” checklist results (n = 12).
| Intervention element | n a (%) Marking “Item Met” |
|---|---|
| Time allocation. Sufficient time was set aside at the beginning of the patient’s appointment for consenting and explaining the intervention. | 4 (33.3) |
| Appropriate target. Successfully provided the tele-mentoring intervention to the target population (education, screening with intra-oral camera). | 12 (100.0) |
| Content: What is oral cancer? Clearly communicated and presented all content in the “What is oral cancer?” section of the pamphlet. | 4 (36.4) |
|
Content: What are HPV vaccines? Clearly communicated and presented all content in the “What are HPV vaccines?” section of the pamphlet. |
2 (16.7) |
| Content: Why is screening for oral cancer necessary? Clearly communicated and presented all content in the “Why is screening for oral cancer necessary?” section of the pamphlet. | 2 (16.7) |
| Process: Dentrix b data entry. The dedicated tele-mentoring screens were clear and straightforward to complete / upload photographs of lesions. | 12 (100.0) |
| Process: Interaction with oral [surgeon] expert over findings. The oral [surgeon] expert clearly communicated his findings via secure e-mail and dedicated Dentrix b entry screen. | 12 (100.0) |
| Referral. (If applicable) Procedure for requesting a follow-up appointment was clear and straightforward to complete in Dentrix b . | 12 (100.0) |
| Time for questions. Provided time and space for patient to ask questions during and/or after the educational/intra-oral camera intervention. | 2 (16.7) |
| Additional resources. (If applicable) Provided additional information and resources related to oral cancer, when requested by the patient. | 2 (25.0) |
Intervension element (abbreviated in bold text).
Numbers within intervention elements may vary due to missing values.
Dentrix was the electronic health record system in use in the dental clinics at the time this pilot study was conducted.
The feasibility criterion was not met, as fewer than 8 of the 10 checklist items (80%) were endorsed by the 12 dentist participants. Note that only four (33.3%) of the checklist items were endorsed by all 12 dentist participants, namely: (1) successfully provided the tele-mentoring intervention to the target population; (2) the dedicated tele-mentoring screens were clear and straightforward to complete; (3) the oral [surgeon] expert clearly communicated his findings via secure e-mail and dedicated Dentrix entry screen; and (4) the procedure for requesting a follow-up appointment was clear and straightforward to complete.
The semi-structured interviews with the dental resident participants provide depth and context regarding the quantitative “essential checklist” feasibility results. First, the key informant interview findings related to perceived benefits of the intervention are presented in Table 4, which highlight various implementation, service, and client outcomes from the IOF. 19
Table 4.
Key informant interview findings related to perceived benefits of the intervention.
| Sub-theme | Representative quote(s) from dental resident participants |
|---|---|
| Reduces wait times and number of visits (efficiency a ) | From what we’ve seen, all the patients were very open to it. I think they understood it as a way to save them time, save them from having to make another appointment or wait for a long time before an appointment was available, so they were able to get answers to their questions sooner this way. |
| [T]his intervention is helpful because if you can reduce that wait time or if you can have a more direct line of communication with the pathologist, then it reduces all the back and forth. | |
| Improves equity a and patient-centeredness a | Things have an outlook here . . . that everyone deserves to have—regardless of their background or socioeconomic standing—deserves to get the best treatment possible. I think we approach every patient with that in mind. Just because someone doesn’t have as much money or something than someone else doesn’t mean that we should overlook stuff that should—treatment that should be done. |
| I believe the intervention allows us [to] be thorough, that we can be efficient and keeping our patients’ needs at heart. | |
| For me, the reward would be just knowing that I did what I could to make sure that this patient was [taken] care of in a timely manner, that we did the best that we could to ensure their oral health. | |
| Enhances documentation of lesions (effectiveness a ) | I think it will be helpful to the patients just to have—we can [have] documentation of the lesion. Sometimes, we’ll see something during an exam, and by the time the patient comes back for a follow-up, 2 week has gone by. They’re seeing a different provider who either doesn’t see the lesion or it doesn’t look the same. Just to have evidence that it was here and that it existed. The whole dental team can be on the same page regarding what was seen at the initial visit will definitely be helpful to the patient. |
| Improves patient compliance (satisfaction b ) | I feel like it would be very beneficial for our patients because when they have lesions that they’re unaware of, it’s pretty concerning. The fact that you can take a picture, show them where the lesion is, show them what it looks like, it brings light to the importance of their oral health. I also just feel like it lends to patient compliance. |
| Engenders staff and organizational support (penetration, c uptake c ) | [T]he general assistants, they know what’s going on too. They’ve been working with clinicians for a good time now, so they have an idea of what steps need to be taken. . . . That’s something I always appreciated from our staff, that they were open to sharing. |
| When I had a question, I was able to come to Dr. B or S. S is excellent with the hands-on stuff. He was available in person quite often, and then if not, we were able to reach [him] on the cell phone for support. I don’t think there was ever a time where we felt like we were on our own to figure it out. |
The perceived benefits of the intervention most often expressed by the dental resident participants are captured in the following five sub-themes, which are consistent with implementation, service, and client outcomes that are explicated in the IOF 19 and bolded below for emphasis: (1) reduces wait times and number of visits (efficiency); (2) improves equity and patient-centeredness; (3) enhances documentation of lesions (effectiveness); (4) improves patient compliance (satisfaction); and (5) engenders staff and organizational support (penetration, uptake). The finding that the dental resident participants believed that the intervention reduces wait times and number of visits for patients was heartening. In the words of one dental resident: “From what we’ve seen, all the patients were very open to it. I think they understood it as a way to save them time, save them from having to make another appointment or wait for a long time before an appointment was available, so they were able to get answers to their questions sooner this way.” The commitment of the GPR program dental residents to the health and well-being of their patients was evident by their remarks regarding patient-centeredness, including the following comment: “For me, the reward would be just knowing that I did what I could to make sure that this patient was [taken] care of in a timely manner, that we did the best that we could to ensure their oral health.”
Next, the key informant findings related to suggestions for improving the intervention are presented in Table 5, that map onto identified constructs which fall within several domains of the CFIR. 18
Table 5.
Key informant interview findings related to suggestions for improving the intervention.
| Sub-theme | Representative quote(s) from dental resident participants |
|---|---|
| Allot time for training and practice (available resources a ) | We were having a little difficulty figuring out how to exactly save the images on our system so that we could access it at a later time. We were fortunate enough that we had the patient for enough time, and they were willing to retake pictures, and they were pretty cooperative with us. |
| In a setting like ours, where we have 30 min for an appointment, sometimes there may not be time to take the pictures, and sometimes we may have to reschedule if we would like the pictures. | |
| Streamline the protocol (complexity b ) | But as of right now, because it’s so new, and there’s no streamlined protocol quite yet for it, I believe it would increase wait times. But I do believe it would improve access to services in that it would raise patient awareness that they need these kind of things. |
| Schedule a separate visit/allot more time for the intervention (structural characteristics c ) | I think one thing I found during this study is it worked better when the patient had a specific appointment for the intervention. While it does only take 5 min, sometimes, if the patient was here thinking that they were having a filling or some other work done, they were a little less likely to be interested. Even after we explained the need, they were sort of just, “I’m here for this, and that’s what I wanna do.” It did work better when we specifically called them or gave them an appointment just for the intervention. |
| [O]ur clinic is very busy. We see a lot of patients for a lot of different procedures such as restorative work. It’s a procedure-heavy clinic where sometimes there may not be the most—a lot of time left over. The focus may not be shifted toward taking the photo. If the patient came in for a separate appointment specific for the photos then I think that’d be a lot more manageable. | |
| Improve patient education (patient needs and resources d ) | I think with more education or if it is implemented where we are taking the images more often, it would raise in priority. |
| As long as the provider does a good job [of explaining] why we’re doing the screening and what the possible outcomes can be or what we expect to find—as long as we’re clear about that—make it clear to the patient, and I think that the intervention itself is very stress-free. |
Inner setting construct under readiness for implementation (Consolidated Framework for Implementation Research 18 ).
Intervention characteristics construct (Consolidated Framework for Implementation Research 18 ).
Inner setting construct (Consolidated Framework for Implementation Research 18 ).
Outer setting construct (Consolidated Framework for Implementation Research 18 ).
The suggestions for improving the intervention most often expressed by the dental resident participants are conveyed in the following four sub-themes, which are also captured as constructs in the CFIR 18 and bolded below for emphasis: (1) allot time for training and practice (available resources); (2) streamline the protocol (complexity); (3) schedule a separate visit / allot more time for the intervention (structural characteristics); and (4) improve patient education (patient needs and resources). One dental resident participant recognized the need to allot time for training and practice by stating: “In a setting like ours, where we have 30 min for an appointment, sometimes there may not be time to take the pictures, and sometimes we may have to reschedule if we would like the pictures.” Another dental resident emphasized the need for improving patient education in these terms: “As long as the provider does a good job [of explaining] why we’re doing the screening and what the possible outcomes can be or what we expect to find—as long as we’re clear about that—make it clear to the patient, and I think that the intervention itself is very stress-free.”
Conclusions
The primary outcome of this pilot study was met, in that 80% or more of the patient participants rated all five administered acceptability questions as agree or strongly agree for this tele-mentoring intervention that encompassed consultation with an oral surgeon after using intra-oral cameras at chairside to detect and identify oral lesions. This finding holds promise, in that a significantly higher proportion of racial/ethnic minority and socioeconomically disadvantaged patients versus their White and more advantaged counterparts reported not receiving an oral cancer examination despite a recent dental visit in a US national survey. 28
On the other hand, the feasibility criterion was not met, since fewer than 8 of the 10 checklist items (80%) were endorsed by the dentist participants. It was nonetheless encouraging that all 12 of the dentist participants believed that the tele-mentoring intervention was appropriately provided to the targeted population and that the process, 18 including referral to an oral surgeon, was clearly communicated and straightforward to complete. This is a credit to the formally appointed internal implementation leaders 18 and project champions 18 for the pilot study, as reflected in the qualitative findings.
The limitations of this pilot study include that it was conducted in three dental clinics within a single FQHC during a public health emergency, when novel personal protective equipment (PPE) and environmental precautions had recently been instituted, and providers and staff had been furloughed due to economic constraints imposed by minimal dental operations and revenue during an initial and profound SARS-CoV-2 surge. These conditions exacerbated the press on time of the remaining providers and staff once routine dental visits resumed and research was permitted to proceed. Nonetheless, the involved dental leaders, residents, and staff rallied to support one another in the implementation and evaluation of this tele-mentoring intervention, which proved to be acceptable to adult patients in this low-resource setting, most of whom were Hispanic and spoke English as their preferred language. An unexpected finding is that the dental resident participants endorsed the service outcome of equity, 19 as per the following comment: “Things have an outlook here . . . that everyone deserves to have—regardless of their background or socioeconomic standing—deserves to get the best treatment possible. I think we approach every patient with that in mind. Just because someone doesn’t have as much money or something than someone else doesn’t mean that we should overlook stuff that should—treatment that should be done.”
While the a priori feasibility criterion was not met, the quantitative and qualitative results point to several paths forward. For the quantitative results, the two items on time allocation and time for questions, and the four items related to the content of the oral cancer education provided and the availability additional resources garnered only two or four endorsements each. Using the CFIR 18 to guide interpretation of the qualitative evaluation results, the constructs that mapped to suggestions for improvement were at multiple levels, including the inner setting of the dental clinic (available resources, structural characteristics) and the outer setting of the local community (patient needs and resources) as well as intervention characteristics themselves (complexity). With external funding support from a new Health Resources and Services Administration (HRSA) postdoctoral training grant, a pilot project is underway to screen children, adolescents, and young adults for HPV vaccination at chairside and refer eligible patients to on-site primary care providers to improve HPV vaccine uptake and series completion. Further, the study team plans to develop, test, and translate educational materials targeted to low health literacy patients to emphasize the key take-home messages, including “HPV vaccination is cancer prevention.” 6 Finally, these pilot study results have been discussed with the leadership within the Department of Dental Medicine toward improving the training of dental residents and the quality of care that patients receive, including by creating apt quality indicators in the newly implemented Epic with Wisdom EHR implemented in Fall 2021.
The use of technology to improve oral cancer screening services has an inherent appeal for application in underserved and remote areas. 29 Asynchronous mobile phone applications have recently been developed and piloted in India using community health workers, 30 in Malaysia using dentists and medical officers, 31 and in Brazil using an examiner with experience in oral pathology and an assistant to take photographs and record videos, 32 all of which hold promise in facilitating the identification of high-risk lesions for early management. Nonetheless, there are no other studies in the extant literature other than the protocol for the current one 17 that used intra-oral cameras at chairside to upload photographs of oral lesions into patient charts for consultation with an oral surgeon to improve early detection and identification of pre- and cancerous lesions.
Hence, this feasibility and acceptability study contributes to the growing body of knowledge supporting teledentistry 33 and tele-mentoring 15 as efficient and effective means to remotely access the expertise of oral surgeons,30–32 provide distance learning to dental residents, 34 increase the empathy of dental providers for their socioeconomically disadvantaged patients, 35 and assess dental student satisfaction with home-based simulation learning. 14 Future implementation studies should include diverse dental settings to test the adaptability of the tele-mentoring intervention. Further, MI training for dental faculty and residents toward communicating effectively with their patients regarding behavior change, development and testing of culturally appropriate educational materials in low health literacy populations regarding the benefits of oral and oropharyngeal cancer prevention, early detection of pre- and cancerous lesions through intra-oral and extra-oral screening, and referral to available evidence-based treatment options are ongoing at Family Health Centers at NYU Langone.
The use of tele-mentoring and teledentistry to train dental residents in FQHCs and other low-resource settings that predominantly serve socioeconomically disadvantaged populations has historically been limited due to challenges as disparate as access to the requisite technology and broadband connectivity, the technical skills of patients and providers, security and confidentiality concerns, legislative and regulatory processes, reimbursement policies and mechanisms, and computer and health literacy. 10 Recent technological advances and increased broadband connectivity 36 have lowered both the cost of and simplified the use of videoconferencing, asynchronous imaging, streaming media, and web cameras.15,37 Through greater use of tele-mentoring and teledentistry enhancements, increased numbers of remote dental providers, residents, and students may one day gain access to the expertise of distant oral surgeons through technology-enabled collaborative learning and capacity building models that enable the detection, identification, diagnosis, monitoring, and treatment of pre- and cancerous oral lesions.37–40
Footnotes
Author contributions: MEN designed the research component of the study, oversaw the qualitative data analyses, and drafted the text of the article. KFW contributed research to the Discussion section and designed Figure 1. SSS oversaw the data collection aspects of the study and contributed to the qualitative data analyses. AT contributed oral pathology expertise to the study. NMF devised the clinical protocol for the study and gained the buy-in of the involved dental faculty and staff. SG conceived of the Dentris/Dentrix electronic health record (EHR) process for the study, advised on the intra-oral cameras to purchase, and installed all the hardware and software for use in the study in the three dental clinic sites. EG ensured all fiscal components of the study were carried out with integrity and created the virtual forum for continuing the study during the COVID-19 pandemic. TCL led the regulatory compliance process for the study and ensured that all investigators and staff completed the necessary research ethics training and disclosure of potential conflict of interest (COI) documents. ABT drafted the analysis section of the study and contributed biostatistical expertise. YW conducted the statistical analyses for the study and provided interpretation of the quantitative data. PAT contributed to the conception and design of the study and provided security safeguard expertise and assurance. JW, KZ, PT, and BB conducted the training on the use of intra-oral cameras, collected all survey data, and contributed dental expertise, with BB providing clinical leadership. All authors contributed to the writing of this paper and approved it for publication.
Declaration of conflicting interests: The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The authors disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This project is supported by the Health Resources and Services Administration (HRSA) of the US Department of Health and Human Services (US DHHS) as part of award # T93HP30391 totaling $575,037 in Year 6 with 0% financed with non-governmental sources. The contents are those of the authors and do not necessarily represent the official views of nor an endorsement by HRSA, US DHHS, or the US Government. For more information, please visit HRSA.gov.
Funding sponsor:
PHS/Health Resources and Services Administration (HRSA), Program Contact: Jesse Ungard, 5600 Fishers Ln Rm 15N146C, Rockville, MD 20857, USA. Email: jungard@hrsa.gov. Phone: (301) 443-6249, Fax: (301) 443-3323.
Ethics approval and consent to participate: This research was performed in accordance with the Declaration of Helsinki. The NYU Grossman School of Medicine Institutional Review Board (IRB) reviewed and approved all study procedures on October 30, 2019 (protocol s19-01268). This approval includes the three dental clinics where the research transpired. All Health Insurance Portability and Accountability Act (HIPAA) safeguards were followed. Written consent was obtained from each subject in accordance with the informed consent procedure included in this protocol.
Significance for public health: The findings reported here support further implementation research into adapting tele-mentoring using intra-oral cameras for training dental residents and faculty to detect and identify oral lesions and educating patients about oral and oropharyngeal cancer across settings. Interest in teledentistry modalities to advance dental education had been building incrementally over time but gained urgency in the past 2 years due to the global COVID-19 pandemic. Dental practice closures along with the pivot to remote learning for dental trainees has fostered new innovations that are likely to be sustained well beyond the current public health crisis. Next steps are to enhance the training of dental faculty and residents in the use of intra-oral cameras to detect a range of oral health conditions and monitor the success of treatments, while educating dental patients on the condition of their mouths toward enhancing their understanding of and contributions to promoting their oral and general health.
Clinical trial registration: ClinicalTrials.gov Identifier: NCT04166214. Title: Oral Pathology Asynchronous Tele-mentoring Pilot Study. Registered on November 15, 2019. Results submitted on October 1, 2021. At: https://clinicaltrials.gov/ct2/show/NCT04166214?term=NCT04166214&draw=2&rank=1. Accessed October 15, 2021.
Availability of data and materials: De-identified raw data and materials described in the manuscript are freely available from the corresponding author upon reasonable request.
References
- 1. Islami F, Ward EM, Sung H, et al. Annual Report to the nation on the status of cancer, Part 1: National Cancer Statistics. J Natl Cancer Inst 2021; 113: 1648–1669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Ellington TD, Henley SJ, Senkomago V, et al. Trends in incidence of cancers of the oral cavity and pharynx - United States 2007-2016. MMWR Morb Mortal Wkly Rep 2020; 69(15): 433–438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Deshmukh AA, Suk R, Shiels MS, et al. Recent trends in squamous cell carcinoma of the anus incidence and mortality in the United States, 2001-2015. J Natl Cancer Inst 2020; 112(8): 829–838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Tellez M, Myers Virtue S, Neckritz S, et al. Randomised clinical trial of a motivational interviewing intervention to improve oral health education amongst older adults in Philadelphia: 12-month evaluation of non-clinical outcomes. Gerodontology 2020; 37(3): 279–287. [DOI] [PubMed] [Google Scholar]
- 5. Dundar Y, Eldem I, Schwartz C, et al. Screening awareness of HPV-related oropharyngeal cancers and attitudes and concerns towards HPV vaccination among parents: HPV and oropharyngeal cancer. J Cancer Educ. Epub ahead of print 2021. DOI: 10.1007/s13187-020-01932-w. [DOI] [PubMed] [Google Scholar]
- 6. Centers for Disease Control and Prevention. Reasons to get HPV vaccine, https://www.cdc.gov/hpv/parents/vaccine/six-reasons.html (2021, accessed 30 September).
- 7. American Dental Association. ADA adopts policy on HPV vaccination for the prevention of oral HPV infection, https://www.prnewswire.com/news-releases/ada-adopts-policy-on-hpv-vaccination-for-the-prevention-of-oral-hpv-infection-300738140. (2018, accessed 5 August 2022).
- 8. Psoter WJ, Morse DE, Kerr AR, et al. Oral cancer examinations and lesion discovery as reported by U.S. General dentists: findings from the National Dental Practice-based Research Network. Prev Med 2019; 124: 117–123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. American Dental Association. Cancer (head and neck), https://www.ada.org/resources/research/science-and-research-institute/oral-health-topics/cancer-head-and-neck (2022, accessed 5 August 2022).
- 10. Teledentistry Learning Collaborative. Teledentistry user guide. Denver, CO: National Network for Oral Health Access, 2021. https://nnoha.org/new-resource-teledentistry-users-guide/ (accessed 30 September 2021). [Google Scholar]
- 11. Pretty IA, Ekstrand KR. Detection and monitoring of early caries lesions: a review. Eur Arch Paediatr Dent 2016; 17(1): 13–25. [DOI] [PubMed] [Google Scholar]
- 12. Pentapati KC, Mishra P, Damania M, et al. Reliability of intra-oral camera using teledentistry in screening of oral diseases - pilot study. Saudi Dent J 2017; 29(2): 74–77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Patel SA, Halpin RM, Olson GW, et al. Global pandemic and the rise of teledentistry. J Dent Educ 2020; 85(Suppl 1): 1158–1159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Tan SHX, Ansari A, Ali NMI, et al. Simulation design and students’ satisfaction with home-based simulation learning in oral health therapy. J Dent Educ 2021; 85(6): 847–855. [DOI] [PubMed] [Google Scholar]
- 15. Amin M, Lai JY, Lindauer PA, et al. Should dental schools adopt teledentistry in their curricula? Two viewpoints. J Dent Educ 2021; 85(7): 1238–1244. [DOI] [PubMed] [Google Scholar]
- 16. Danciu TE, Gagari E, DaSilva AF, et al. Teledentistry as a new service line-Not just a coping mechanism for the pandemic.. J Dent Educ 2021; 85 Suppl 3: 1986–1988. [DOI] [PubMed] [Google Scholar]
- 17. Northridge ME, Littlejohn T, Mohadjeri-Franck N, et al. Feasibility and acceptability of an oral pathology asynchronous tele-mentoring intervention: a protocol. J Public Health Res 2020; 9(1): 1777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Damschroder LJ, Aron DC, Keith RE, et al. Fostering implementation of health services research findings into practice: a consolidated framework for advancing implementation science. Implement Sci 2009; 4: 50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Proctor EK, Landsverk J, Aarons G, et al. Implementation research in mental health services: an emerging science with conceptual, methodological, and training challenges. Adm Policy Ment Health 2009; 36(1): 24–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Pbert L, Fletcher KE, Flint AJ, et al. Smoking prevention and cessation intervention delivery by pediatric providers, as assessed with patient exit interviews. Pediatrics 2006; 118(3): e810–e824. [DOI] [PubMed] [Google Scholar]
- 21. Aceton. Diagnostic Cameras. SOPROCARE®, https://www.acteongroup.com/us/products/imaging/diagnostic-cameras/soprocare (accessed 14 October 2021).
- 22. New York State Department of Health. Interim guidance for dentistry during the COVID-19 public health emergency, https://www.governor.ny.gov/sites/default/files/atoms/files/DentistryMasterGuidance.pdf (2021, accessed 14 October 2021).
- 23. Rethman MP, Carpenter W, Cohen EE, et al. American Dental Association Council on Scientific Affairs Expert Panel on screening for oral squamous cell carcinomas. Evidence-based clinical recommendations regarding screening for oral squamous cell carcinomas. J Am Dent Assoc 2010; 141(5): 509–520. [DOI] [PubMed] [Google Scholar]
- 24. Lingen MW, Abt E, Agrawal N, et al. Evidence-based clinical practice guideline for the evaluation of potentially malignant disorders in the oral cavity: a report of the American Dental Association. J Am Dent Assoc 2017; 148(10): 712–727.e10. [DOI] [PubMed] [Google Scholar]
- 25. The R Project for Statistical Computing. https://www.r-project.org/ (accessed 14 October 2021).
- 26. Boyatzis RE. Transforming qualitative information: thematic analysis and code development. Thousand Oaks, CA: SAGE, 1998. [Google Scholar]
- 27. Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol 2006; 3(2): 77–101. [Google Scholar]
- 28. Gupta A, Sonis S, Uppaluri R, et al. Disparities in oral cancer screening among dental professionals: NHANES 2011-2016. Am J Prev Med 2019; 57(4): 447–457. [DOI] [PubMed] [Google Scholar]
- 29. Warnakulasuriya S, Kerr AR. Oral cancer screening: past, present, and future. J Dent Res 2021; 100: 1313–1320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Birur N, Gurushanth K, Patrick S, et al. Role of community health worker in a mobile health program for early detection of oral cancer. Indian J Cancer 2019; 56(2): 107–113. [DOI] [PubMed] [Google Scholar]
- 31. Haron N, Rajendran S, Kallarakkal TG, et al. High referral accuracy for oral cancers and oral potentially malignant disorders using telemedicine. Oral Dis. Epub ahead of print 2021. DOI: 10.1111/odi.13892. [DOI] [PubMed] [Google Scholar]
- 32. Gomes MS, Bonan PR, Ferreira VY, et al. Development of a mobile application for oral cancer screening. Technol Health Care 2017; 25(2): 187–195. [DOI] [PubMed] [Google Scholar]
- 33. American Well. Telehealth index: 2019 consumer survey, https://static.americanwell.Com/app/uploads/2019/07/American-Well-Telehealth-Index-2019-Consumer-Survey-eBook2.pdf (2019, accessed 11 October 2021).
- 34. Kunin M, Julliard KN, Rodriguez TE. Comparing face-to-face, synchronous, and asynchronous learning: postgraduate dental resident preferences. J Dent Educ 2014; 78(6): 856–866. [PubMed] [Google Scholar]
- 35. Amini H, Gregory ME, Abrams MA, et al. Feasibility and usability study of a pilot immersive virtual reality-based empathy training for dental providers. J Dent Educ 2021; 85(6): 856–865. [DOI] [PubMed] [Google Scholar]
- 36. Cooper T. The decade in broadband: 2020 statistics & predictions, https://broadbandnow.com/research/broadband-2020 (2020, accessed 11 October 2021).
- 37. Office of the Assistant Secretary for Planning and Evaluation. Advances in telehealth.Washington, DC: U.S. Department of Health and Human Services, 2021. https://aspe.hhs.gov/topics/health-health-care/advances-telehealth (accessed 11 October 2021). [Google Scholar]
- 38. Abdelrahman H, Atteya S, Ihab M, et al. Dental practice closure during the first wave of COVID-19 and associated professional, practice and structural determinants: a multi-country survey. BMC Oral Health 2021; 21(1): 243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Wallace CK, Schofield CE, Burbridge LAL, et al. Role of teledentistry in paediatric dentistry. Br Dent J 2021; 25: 1–6. DOI: 10.1038/s41415-021-3015-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Kumar G, Gugnani N, Rabea D, et al. Severe acute respiratory syndrome coronavirus 2 and dentistry: a summative review of guidelines issued by national health authorities. J Indian Soc Pedod Prev Dent 2021; 39(2): 120–131. [DOI] [PubMed] [Google Scholar]