Abstract
Objective
The present study aimed to understand what factors can lead to late HIV diagnosis of illegal gold miners at French Guiana’s border with Brazil.
Design
An exploratory qualitative study with in-depth interviews and observations was conducted between November 2019 and February 2020.
Setting
The study was conducted in the main medical healthcare service and two non-governmental organisation premises in the Oyapock border region, which is a supply area for illegal gold mining sites.
Participants
Fifteen people living with HIV diagnosed with CD4 count <350 cells 106/L were interviewed. Seven women and eight men participated; they were between 31 and 79 years old, and the median time since HIV diagnosis was 6 years. Eight had links to illegal gold mining.
Findings
Three key themes for late HIV diagnosis emerged: (1) the presence of economic and political structural factors which constitute risks for this illegal activity, specifically the repression of gold mining sites by French Armed Forces and the distance from healthcare facilities; (2) representations of the body and health, related to the living conditions of this population; prioritisation of health emergencies and long-term self-medication; and (3) gender roles shaping masculinity and heterosexuality contributing to a perception of not being at risk of HIV and delaying testing.
Conclusion
This study highlights structural, group-based and individual factors that reduce access to HIV testing and healthcare in general for a population of migrant workers in an illegal gold mining area. Faced with harsh living conditions and state repression, these workers develop a vision of health which prioritises the functionality of the body. Associated with gender roles which are partly shaped both by the mining activity and its geographical location, this vision can lead to late HIV diagnosis.
Keywords: HIV & AIDS, Public health, Epidemiology
Strengths and limitations of this study
This is the first qualitative study on late diagnosis of HIV in illegal gold miners in Amazonia at the French Guiana–Brazil border.
It documents a specific HIV context with few existing data.
The study shows how structural, individual and group-based factors overlap to lead to late HIV diagnosis.
An anthropological approach was used to study representations of health and HIV in the gold miner population.
Study participants were not directly observed/interviewed at gold mining camps.
Introduction
French Guiana is the region of France most impacted by HIV with a prevalence of 1.25% in the general population.1 Located in continental America, it is 7000 km from Paris. The Amazonian forest represents 97% of its territory. The ethnic background of the region’s approximately 270 0002 inhabitants reflects its colonial history: Creoles, indigenous peoples, Bushinengues, persons from mainland France, as well as recent immigrants seeking a better life, mostly from Surinam, Brazil and Haiti.3 The presence of the French state in this area is mainly visible through the school system, the health system and the presence of the army, which carries out training and operations.4 Compared with mainland France, the health system is under-resourced, with inequalities between the coastal and inland areas.5 6
With one of the highest unemployment rates in France, and a large number of people living below the poverty line, social inequalities accumulate in French Guiana, facilitating the spread of HIV.5 It has been shown that social, economic, racial and gender inequalities make people more vulnerable to HIV. Daily difficulties with housing, food, transport and immigration status all impact both condom negotiation and access to prevention and care.7
The HIV epidemic particularly affects migrant populations.8 9 Contrary to the claims by some that HIV-positive migrants are already infected when they arrive, it would appear that most become infected after their arrival.9 10 Despite both France and Brazil having HIV ‘test and treat’ policies, access to healthcare in the isolated Amazonian areas of French Guiana is impacted by territorial inequalities, and the epidemic continues to grow there (eg, incidence in 2010–2015 increased from 32.09 to 42.35 per 10 000).6 Among Brazilian immigrants, HIV diagnosis occurs approximately 3.7 years later than in other population groups.11 HIV incidence is also increasing in the neighbouring Brazilian state of Amapá (+21.2% in 2009–2019).12
The border between the two countries represents a typical marginalised border area13 with asymmetric wealth, poor living conditions, little access to education, temporary population mobility and a flourishing sex trade which is often linked to nearby illegal gold mining in French Guiana.14 15 Geographically distant from decision-making centres, this area remains economically and politically neglected by both France and Brazil.16–18
The border towns of Saint Georges (French Guiana, approximately 5000 inhabitants) and Oiapoque (Brazil, approximately 25 000 inhabitants) are located on opposite sides of the Oyapock River. Oiapoque is a support base for the illegal gold mining industry located deep in the forests of French Guiana. It is a primary point of arrival and departure for Brazilian gold miners. Populations here are very exposed to health vulnerability,19 20 HIV treatment being available in Oiapoque only since 2019.
Approximately 10 000 gold miners work in the estimated 600 gold mining sites in French Guiana.21 The region has mostly small-scale and medium-scale artisanal mining operations, the majority of which are illegal (called garimpos), with workforces comprising mainly Brazilian miners (called garimpeiros).22–25 The social organisation of the garimpo is governed by norms, constraints and sanctions that exist outside of state mediation.26 The garimpeiros associate with donos (bosses) through very detailed oral contracts that formalise the work and the type of remuneration, mainly by percentage.23 26 Besides work-based hazards, the garimpos are subject to campaigns to eradicate illegal gold mining by the ongoing French military Operation Harpie.27 These campaigns accentuate the temporary and improvised nature of this activity.
The complex sociopolitical contexts of illegal mining camps means that they are hard to document from a scientific perspective as physical access is difficult for researchers.23 28 In the limited literature available in French Guiana, medical surveys found that gold miners’ working and living conditions led to poor health, a high prevalence of infectious and non-infectious diseases including HIV and limited access to healthcare.29 30 In 2013, primary healthcare centres located at French Guiana’s border with Brazil observed an increase in HIV seropositivity. Brazilian patients involved in gold mining were the most exposed. A third of the cases were diagnosed late (ie, defined as CD4 count <350 cells 106/L/).31 Understanding the reasons for late HIV diagnosis in this socially deprived migratory population who know little about HIV testing or prevention tools14 32 33 is essential to improve healthcare.
In this peripheral multilingual geographical context, using an exploratory anthropological research approach, the present study aimed to bring new evidence to the currently scarce data on factors leading to late HIV diagnosis. More specifically, it aimed to study how structural, individual and group-based social constructions can lead to late HIV diagnosis by gathering and analysing data on the experiences of patients living with HIV who are diagnosed late.
Methods
Patient and public involvement
No person living with HIV (PLHIV) was directly involved in the design of the study. The original research question emerged from physicians working in the border region. The interview guide and data collection methods were revised and validated by community health workers involved in PLHIV medical follow-up. We had planned to present the results to participants but this was delayed because of the COVID-19 border restrictions.
Study design
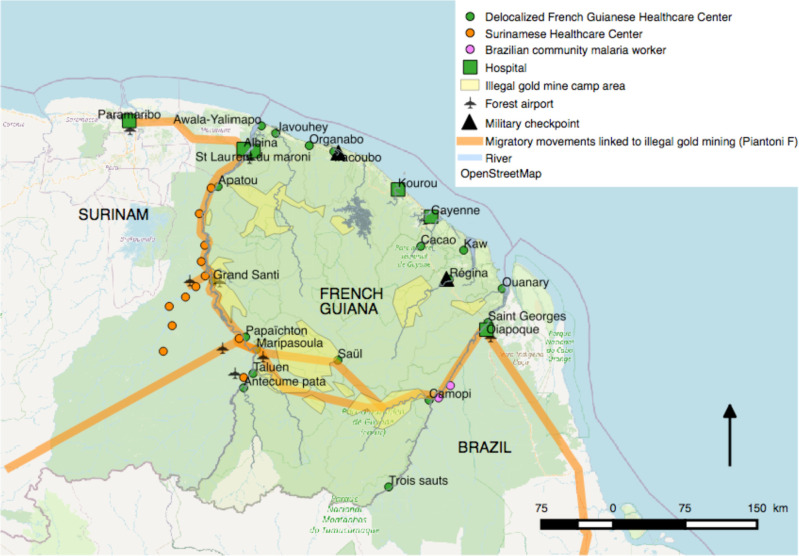
Between November 2019 and February 2020, an ethnographic anthropological research study was conducted combining observations in a medical healthcare service and two non-governmental organisation (NGO) premises with in-depth individual interviews at the border area between French Guiana and Brazil (figure 1).
Figure 1.
Map of healthcare centres, gold mine area and migratory movements linked to illegal gold mining in French Guiana which were previously reported by Piantoni F.54 Map was created by using QGIS Geographic Information System. Open Source Geospatial Foundation Project. http://qgis.osgeo.org
Data collection
Of the 55 PLHIV who frequented the primary health centre for follow-up at least once in the year preceding the study period, a panel of 21 patients with late diagnosis were identified by the referring infectious diseases physician. Late HIV diagnosis was defined as CD4 count <350 cells 106/L at diagnosis. The maximum time between diagnosis and study inclusion was 21 years, with a median of 6 years. Patients were then contacted by the healthcare mediator in charge of their medical follow-up. Study participation was proposed during medical consultation or by phone. Fifteen of the 21 patients agreed to participate and constituted the study sample. Of these, eight had either formerly worked in illegal gold mines in French Guiana and/or elsewhere or were/had been married to a gold miner. Before the interview and before written consent was obtained, the study was explained to the participants, and patient confidentiality and data privacy issues were clarified. The ethical permissions granted by the Cayenne Hospital Ethical Committee (UF6000/27.b) and the French National Commission on Informatics and Liberty (2215827) allowed us to retrieve specific data (CD4 count at diagnosis and low CD4 nadir)—with patient consent—from their medical records.
Interviews lasted between 60 and 90 min. They were conducted in French (n=2) and/or Portuguese (n=13) and translated simultaneously into French by an HIV community health mediator. The following themes were discussed during the interviews: life and migration trajectory, experience of gold mining, HIV risk perceptions, HIV screening and diagnosis history, seeking care and treatment, social life and everyday experience with HIV. In addition, ethnographic observations of both medical consultations and NGO HIV prevention activities were performed. An inductive method was used for both study dimensions, whereby the interview and observation guides could be adapted to new themes that emerged during data collection, and whereby initial protocol-defined data collection and categorisation techniques could be modified.34
The study was implemented in collaboration with Oyapock Coopération Santé, a French-Brazilian project to improve access to HIV care and sexual health at the border between the two countries.35
Analysis
Audio recordings of interviews and notes taken during observations were transcribed, coded manually and anonymised. The exploration and production of various sources (interviews, observations and written materials) enabled us to triangulate the data.36 Transcript analysis was performed following thematic classification. This made it possible to identify specific subthemes through occurrences and recurrences and analysis of correlations. The analysis focused on data in both French and Portuguese. The linguistic skills in Portuguese acquired by the interviewer/researcher during fieldwork enabled her to subsequently make a transversal analysis of the materials collected.
Results
Participant characteristics
Seven women and eight men living with HIV participated, aged between 31 and 79 years (table 1). One of the 15 self-defined as homosexual. During the analysis of sharing experiences and trajectories, a gold miner-related subgroup clearly emerged. Three men and three women were former workers in the gold mines while two women had never worked in the industry but were/had been married to a miner. The present analysis focuses on these eight people. The heterogeneity of the rest of the participants prevented us from being able to make a comparison with persons connected to gold mining and those who were not.
Table 1.
Summary of study participant characteristics (n=15)
| Pseudonym | Sex | Age range | Number of years diagnosed as HIV positive | CD4+* count at diagnosis | Low CD4+* nadir | Gold mining-related activity | |
| 1 | Aline | F | Late 30s | 3 | 302 | 104 | Married to a gold miner |
| 2 | Anderson | M | Late 30s | 6 | 15 | 15 | Former gold miner |
| 3 | André | M | Mid-40s | 1 | No | ||
| 4 | Felipe | M | Early 40s | 4 | 200 | 199 | No |
| 5 | Ana | F | Early 40s | 4 | 233 | 233 | Former gold miner |
| 6 | Janaina | F | Early 60s | 5 | 136 | 136 | Married to a gold miner |
| 7 | João | M | Mid-40s | 6 | 281 | 105 | No |
| 8 | Julia | F | Mid-40s | 6 | 56 | 56 | No |
| 9 | Juliano | M | Early 30s | 11 | <350 (Amapá, Brazil) |
<350 (Amapá, Brazil) |
No |
| 10 | Oscar | M | Mid-40s | 21 | Unknown at diagnosis | Unknown at diagnosis | No |
| 11 | Patricia | F | Late 40s | 5 | 196 | 196 | No |
| 12 | Rosa | F | Mid-40s | 6 | Unknown at diagnosis | Unknown at diagnosis | Former gold miner |
| 13 | Sizinho | M | Late 70s | 9 | 103 | 103 | Former gold miner |
| 14 | Teresa | F | Mid-40s | 7 | <350 (Amapá, Brazil) |
<350 (Amapá, Brazil) | Former gold miner |
| 15 | Walter | M | Mid-40s | 5 | 164 | 164 | Former gold miner |
*CD4+ in cells 106/L.
Nine topics emerged from the analysis of the individual interviews and observations (box 1).
Box 1. Main topics discussed during interviews with patients positive for HIV.
Life trajectory (childhood, professional activity, migration).
Gold mines, access to healthcare at gold mine sites.
Context of HIV diagnosis (pregnancy, HIV-positive partner, opportunistic disease).
Access to healthcare (HIV and other) in Brazil and French Guiana.
Prediagnosis representations and knowledge of HIV.
Sexuality (sex life, conjugality, gender role).
Representation of body and health.
Experience of living with HIV (acceptance, discrimination, status disclosure).
Police and administrative problems.
Illegal small-scale gold mining: a specific context
Illegal small-scale gold mining in French Guiana involves migration from poor regions of north and northeast Brazil and mobility from mining camps to support bases. Oiapoque, where most of the participants lived at the time of this study, is one such base. According to the HIV community health mediator: ‘Oiapoque in its entirety was built with gold’. Despite the destruction of illegal gold mining camps in the forest by the French government (see Operation Harpie above), Brazilian garimpeiros continue to build new ones. This is because compared with other types of jobs available in the Brazilian Amazon regions, illegal small-scale gold mining in French Guiana provides the garimpeiros with a lot of freedom (choice of employer, informal contract, etc) and the chance to make more money. This explains why, despite the dangerousness of the work, the hazards of production and repressive policies, gold mining still attracts many people in search for a better life.
I thought that there was the possibility of earning more money there; everyone was talking about it. I went through that experience, I ‘went in’ and I worked there. (Anderson, late 30s, male, bricklayer, former gold miner)
In remote areas of the Amazon rainforest, gold mining camps form microsocieties for places of work, social and economic exchange and daily life. Because of the setting of the activity, working in an illegal mine involves a time commitment from several months to years.
When I went, I didn’t get out. I did go out [for short periods] around 10 times because I stayed there for such a long time: 10 years. (Sizinho, late 70s, male, former gold miner)
The six garimpeiros interviewed had experienced government-based repression in their mining camps; some were arrested and then released. The complete destruction of a gold mining camp is the most common technique used by the police and the French Army. For the garimpeiros, this means fleeing into the forest for several days with the consequent risks (getting lost, no water, etc).
When they arrive, you run; if you have time you untie your hammock, if you don’t, you leave everything behind and run; you save your skin. (Walter, mid-40s, male, tree pruner, former gold miner)
The long periods of stay in the forest, moving in and out of the sites and facing camp destruction all represent a specific lifestyle with its own temporality. The socioeconomic environment in these sites, their geographical isolation and the illegality of the working practices all accentuate problems accessing HIV prevention/testing tools and services as well as treatment.
Gender roles and emotional and sexual relationships at the garimpo
The gold mining industry—whether practised legally or not—impacts gender roles, sexuality and conjugality. More specifically, the work environment and geographical distance from their homes affect garimpeiros’ sexual life in the camps and when they go back to their families in Brazil. Gender roles also shape relationships in the camps. The construction of masculinity around virility is justified by the physically demanding work of extraction.
With regard to prostitution, Sizinho (Late 70s, male, former gold miner) said:
There are many of them; at night there are the brothels that are open; it’s a woman’s work. You drink, you dance and do your business […] We spent a lot too: alcohol, partying, women, all night, all night, all night long.
In addition to promoting virility, the physical and dangerous element of the work shapes relationships with self-risk. Compared with the daily risks of mining and repression, miners put the less visible risks into perspective, such as HIV contamination. Most of the men interviewed, whether married or not, came on their own to the gold mining camps and saw their families between once a month and once a year. This has an impact on sexuality, as men develop several types of relationships including paying for sexual services and ‘second home’-type relationships.
Despite the very masculine environment—garimpeiros are almost exclusively men—women are also present in the camps. They mostly work as cooks and sex workers; some own gold extraction machines. Their roles and the types of work they do also have gender-specific constraints. Three of the women in this study were involved directly in the gold economy.
Some women go there to work in the kitchen; some women go there to work in prostitution. There are women who aren’t prostitutes, who don’t go to work in prostitution, but on the other hand they can pay for a lift [by canoe] by prostituting themselves. Everyone does business with the person that suits them. It’s very, very dangerous for a woman there, but once you’ve made acquaintances, once you see who can help you, who’s strong, who can defend you, you do business with that person. (Rosa, mid-40s, female, manicurist, former gold miner)
In the case of women who come to the garimpo alone, developing intimate relationships within the camp is a strategy for survival. Apart from prostitution, sexuality is a way to obtain services (eg, ride to the nearest town), and represents a protection strategy in an environment regulated by the threat of violence.
In terms of risk prevention, although wearing a condom can quite easily be negotiated in transactional sex, this becomes more difficult when sexuality is part of an intimate relationship. Couples at the camps are formed and are related to the context. For example, Walter had ‘uma namorada’, a girlfriend, in the camp where he had spent the most time; Rosa and Anderson met each other in a camp. Couples created in camps can exist in parallel with and/or in competition with marital relationships. Janaina discovered that her husband had an affair in the garimpo and this led to their separation. During their marriage, the couple had not used any form of contraception:
No, I wasn’t using anything; I also thought he wasn’t with anyone there; it was a marriage, wasn’t it? (Janaina, early 60s, female, farmer)
Outside the garimpo, heterosexual couples—where power relations are unequal and for which social expectations on fidelity are strong—therefore constitute a context for disease transmission. When a married man comes home from the garimpo, the monogamous contract, together with economic and emotional dependence, means hoping that the other person (whether the husband or wife) has been faithful during the absence. This leads to a perception of being safe from potential sexually transmissible infections.
Having a functional body: perceiving health as the absence of symptoms
Brazilians who migrate to the illegal gold mines in French Guiana in search for a better life are often uneducated. However, they have other types of knowledge and skills. As gold mining requires physical strength and endurance, health and illness are fundamental issues. Garimpeiros perceive that being in good health is mainly related to the proper functioning of the body. They fear disabling illnesses most and tend to minimise the importance of aches and pains. In our study, ‘Tudo bem’ (‘everything’s fine’ in Portuguese) was the most common answer to questions about health during the interviews. For garimpeiros, less contact with doctors is greater evidence of good health. Access to outside care and medical treatment are not matters for complaint or discussion.
Malaria is the most frequent disease in gold mining sites. When fever and influenza-like symptoms occur, the miners self-diagnose, assume it is malaria and self-medicate to reduce seizures. In gold mining sites, the individual is responsible for their own disease management, the latter depending on what medicine is available:
It’s a bit risky yes; some people bring their medicines with them; they have malaria drugs because there’s a lot of malaria there. Sometimes people come with some anti-inflammatory drugs; there’s also other people who work selling medicines, all kinds of medicines. There’s no professional, no doctor there. (Rosa, mid-40s, female, manicurist, former gold miner)
Medications and condoms are bought in gold, and prices fluctuate. This constitutes a heavy financial burden for the workers, effectively creating a barrier to disease prevention.
When the symptoms do not pass, the gold-diggers leave the camp to seek treatment, often when their health has already greatly deteriorated. For very serious cases, this is often difficult as the distance to the closest healthcare structure is long. Often, it is necessary to take a canoe, which further delays treatment, consequently lengthening the time spent self-medicating. Travel to hospitals only takes place ‘em caso da vida o morte’ (‘when it’s a matter of life or death’), as one participant, Rosa, put it.
When study participants described the HIV symptoms they experienced, they often mentioned energy loss, weight loss, fever, diarrhoea and chills. These symptoms can be mistaken for signs of other types of pathologies, such as malaria or dengue fever.
I’d already heard about it [HIV] before but I’d no idea what the symptoms were. If I’d known those were the symptoms, I’d have gone earlier; I’d have gone to a doctor sooner, but because I didn’t know, I kept taking medicines for one thing or another… (Walter, mid-40s, male, pruner, former gold miner)
Gold miners apply the general belief that humans hide both the fact that they are mortal and the fundamental worry that comes with this, and live their lives as if the present will last forever.37 Illness, including HIV seropositivity, can jeopardise the possibility to continue their gold extraction work:
Because when I got sick, I came here [Oiapoque]; everything was there [the Garimpo], I had to come back here. And I came here with what? With two backpacks and a child, and still sick. It is what it is. (Rosa, mid-40s, female, manicurist, former gold miner)
Like the other study participants, HIV diagnosis was the main reason why Rosa stopped working in the camp. Like them, her financial situation was very difficult when interviewed.
Social backgrounds and working conditions influence gold miner’s health-seeking behaviours. Other types of structural relationships also affect garimpeiros’ relationships to health and illness, including poor access to health services, repression of the camps by the French Armed Forces, threats of expulsion and other administrative difficulties.
Circumstances of HIV diagnosis
Patients in our study discovered they were HIV positive in three different circumstances: opportunistic disease, during pregnancy and having an HIV-positive partner. Gender influenced the circumstances of the discovery of their positive HIV status and their approach to seeking healthcare.
Opportunistic disease
The three male garimpeiros discovered they were HIV positive because long-term symptoms led them to be hospitalised. Walter was sick for 3 months at the garimpo and went to look for care because his fever did not go away:
When I went to St. Laurent, I did all kinds of tests, and nothing, nothing [no positive test results]. When a nurse asked me if I wanted to be tested for HIV, I said ‘Do it!’. (Walter, mid-40s, male, pruner, former gold miner)
Sizinho was also diagnosed with HIV after seeking treatment for a fever. In both cases, the medical staff did not immediately perform an HIV test. Only later, when the other test results proved inconclusive, did they propose this test and in an apologetic fashion. ‘Don’t take this the wrong way,’ the nurse said to Sizinho when inviting him to do the test. This illustrates how medical care providers in this context may still see heterosexual men as a non-risk category for HIV.
Despite discovering his wife was HIV positive during her pregnancy, Anderson never wanted to get tested. He finally went to the hospital to get medical care when he was already in a serious condition. Like Aline’s husband, Anderson did not want to believe that his wife was infected:
What made me not believe [that my wife was HIV positive], it’s because I believe—honestly—that I wanted to continue not believing, that is to say, because I didn’t want treatment. I was traumatized by doctors you see. I didn’t like doctors because I thought doctors were doing things to us, like to lab rats, right? Laughter. I didn’t like it, so I didn’t want to know. I thought that through the faith I had in God, I could heal myself, if possible, I believed that. (Anderson, mid-30s, male, bricklayer, former gold miner)
For these three participants, in addition to the mine being located far from any medical facility, having doubts about their infection, the very existence of the disease (Anderson) and a confrontational relationship with doctors were all factors which prevented them from getting tested despite knowing that their wives were HIV positive.
HIV-positive partners and pregnancy
Teresa was previously a cook in different garimpos. While she was resting at her family’s house in Oiapoque, she received a call from the regional hospital in French Guiana. Her companion, a gold miner, had been hospitalised in a serious condition for an opportunistic disease. When she arrived at his bedside, she was invited to have an HIV test. Only then did she discover she was seropositive.
Rosa and Aline discovered they were HIV positive during prenatal care, and indicated that this was very destabilising for them as future mothers. Pregnant women have more frequent contacts with medical institutions and our study highlights that women seem to be more likely to take up an offer to have a test and to receive care. For our participants, discovering their seropositivity, whether during routine check-ups (eg, pregnancy) or during hospitalisation for opportunistic diseases, was unexpected as none thought they could be infected by HIV.
Discussion
The illegal gold mining industry in the deep Amazonian forests of French Guiana represents one means to finding a better life for many socially deprived people living along the French Guiana–Brazil border. Living conditions (months spent on remote sites, the threat of repression23) and the social organisation of the camps (paid sexual services, self-diagnosis and medication) increase the likelihood of HIV infection in this population. Furthermore, access to HIV testing is difficult.38 Our results suggest that even when the garimpeiros return to a supply area, they do not take advantage of free HIV testing, as they do not perceive they are at risk, and prefer to forget about possible at-risk behaviours they practise during their time in gold mine sites.
At the garimpo, gender roles determine the functions allocated to each person. Masculinity is valorised through a specific relationship combining risk, alcohol and sexuality.39 40 The mining activity creates a specific organisation of sexuality where geographical distances influence conjugality. Women’s sexuality can be a currency for exchange41 and intimate relationships a strategy for safety. The risk of HIV infection is managed through social identity.42–44 It is most likely that the women in our study were infected during their stable relationship, as this has been reported in other contexts where female non-sex workers had the highest HIV prevalence in informal small-scale gold mines.45 Despite the fact that advances in treatment have transformed HIV into a controlled chronic disease, being diagnosed with HIV represented a clear biographical disruption46 for the ex-garimpeiros interviewed.
The physical extraction of gold requires physical strength and endurance, which produces a particular relationship with the body. Although garimpeiros arrive at the mining sites in good health, the harsh working conditions there negatively impact their health.29 Representations of the self, health and body all play an important role in the decision to seek (or not) medical care.47 Disease diagnosis and treatment depend on several factors including the geographical location of the camps. Garimpeiros often self-medicate, sometimes for long periods.48 When they consult a doctor, it is only for serious issues, often requiring hospitalisation.49
In the present study, the participants said that they were surprised when they tested HIV positive.42 None had ever thought of spontaneously doing a test. Not frequently seeking healthcare,50 mistrust of the medical profession and not perceiving risks can all lead to late HIV diagnosis. The latter can also occur when medical staff do not consider heterosexual patients as at-risk population.51 52 In our study, what emerges from the doctors and the majority of the patients is that most of the people invited to test agreed to do so. It would appear that preparing the person for a potential positive HIV diagnosis by first clearly explaining the disease itself, the test and current treatments is fundamental, especially for pregnant women.
Using a comprehensive approach, this study shows the overlapping of structural, individual and group-based factors in relation to HIV infection and its diagnosis, and provides a gendered perspective of the target population’s delay in seeking healthcare.53 Furthermore, it validates the impact of illegal gold mining on this delay and health issues in general. Indeed, in a context where research on health issues in French Guiana is scarce, this study is the first in over 20 years to use an ethnographic approach to investigate PLHIV in the French Amazon from a cross-border perspective.47
One limitation of our study is that the fieldwork could not be performed directly with current miners at the illegal camps due to their inaccessibility to researchers for obvious reasons. However, the experiences of former miners and other persons previously connected to this industry in French Guiana means that this survey—the first of its kind—provides excellent evidence for the situation of gold workers there. A second limitation is potential selection bias, as participants were recruited by medical and other healthcare staff. Furthermore, it would have been interesting to include PLHIV living in other parts of the French Guyanese territory.
Repressive policies applied to those on the margins of society in French Guiana create a situation where seeking healthcare becomes difficult. Garimpeiros’ attitudes towards health and HIV need to be understood in a context where vulnerability to infection could jeopardise their livelihood. Advocating for a global, not pathology-driven approach to healthcare is essential for this particularly vulnerable population. Actions to fight HIV have been implemented over the last few years, particularly at the French Guiana–Brazil border area. The Oyapock Coopération Santé project increased the number of tests offered and bettered the access to 'antiretroviral treatment at a transnational level.35 This community-based approach by health mediators who are familiar with the issues involved reinforces these efforts and enables gold miners to access these services when they leave the garimpo.
Ongoing studies, particularly on malaria (Malakit),30 show that when tests are offered on-site, or combined with other services, people readily agree to them. Continued efforts to provide access to health and prevention, and to integrate HIV into routine check-ups, could reduce the time between infection and diagnosis and help reduce the HIV epidemic. These actions, which have already borne fruits,30 35 should be perpetuated and funded in the long term. Furthermore, providing free HIV testing, self-tests and pre-exposure prophylaxis directly in camps could also be beneficial. Outreach focusing on educating garimpeiros and their partners on health and safety, especially regarding HIV symptoms and prevention, could promote community empowerment on health issues.
This study is exploratory. In-depth studies are needed to better understand the determinants of delay in testing and treating this migrant population, which is at particular risk of HIV infection.
Conclusion
Illegal gold mining in French Guiana involves the mobility of migrant Brazilian workers living in social deprivation, living in deep forests, experiencing repression by the French state and possible eviction. These conditions generate a relationship to the body and negatively impact health and healthcare-seeking behaviours. Garimpeiros perceive that less contact with doctors is evidence of their good health. Social constructions of both gender—especially masculinity—and HIV risk categories still impact the access to HIV testing, leading to deteriorating health and late HIV diagnosis. Taking into account the specific difficulties garimpeiros face when proposing healthcare options for them, including HIV screening mobile units, would improve access to healthcare and overall health, and would reduce the HIV burden in this vulnerable population.
Supplementary Material
Acknowledgments
We would like to thank the study participants who were interviewed in the town of Saint Georges de l'Oyapock in French Guiana. Our thanks also to the cultural mediators from the NGOs DAAC and DEPAC, as well as Dr Céline Michaud, Dr Bastien Bidaud, Dr Damien Davy, Sophie Rhodes, Capucine Dao and Dr Mélanie Gaillet for providing crucial support throughout this study. We would especially like to thank Jonailde Couadou who contributed to the data collection. Finally, our thanks to Jude Sweeney (Milan, Italy) for the English revision and copyediting of this manuscript.
Footnotes
Twitter: @FloeCharlotte
Deceased: Sandrine Musso passed away on August 7, 2021. She was a deeply committed health anthropologist. She co-directed and greatly influenced this research and we miss her every day. Here is the list of her work: https://journals.openedition.org/anthropologiesante/11725
Contributors: CF, SM and EM designed and implemented the study. CF is the guarantor and wrote the first draft of the manuscript. AE, GG, MD, BS, LS-T and MCP contributed to subsequent drafts, and reviewed and agreed on the content of the final manuscript. This article is based on research conducted during an MSc at Ecole des Hautes Etudes en Sciences Sociales.
Funding: This work was supported by the French National Agency for Research on AIDS and Viral Hepatitis (ANRS) (grant number: AO 2018-1CSS5), Regional Health Agency of French Guiana (ARS de la Guyane), l’Observatoire Hommes-Milieux/CNRS (APR 2019) and Le Réseau Français d’Études Brésiliennes.
Map disclaimer: The inclusion of any map (including the depiction of any boundaries therein), or of any geographical or locational reference, does not imply the expression of any opinion whatsoever on the part of BMJ concerning the legal status of any country, territory, jurisdiction or area or of its authorities. Any such expression remains solely that of the relevant source and is not endorsed by BMJ. Maps are provided without any warranty of any kind, either express or implied.
Competing interests: None declared.
Patient and public involvement: Patients and/or the public were not involved in the design, or conduct, or reporting, or dissemination plans of this research.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data availability statement
Data available on request due to privacy/ethical restrictions. The data that support the findings of this study are available on request from the corresponding author, [CF]. The data are not publicly available due to CNIL restrictions because they contain information that could compromise the privacy of research participants.
Ethics statements
Patient consent for publication
Not applicable.
Ethics approval
Biological results were retrieved anonymously from computerised medical charts. The retrospective use of anonymous patient files located in patient care services was authorised by the Cayenne Hospital Ethical Committee (UF6000/27.b) and the French National Commission on Informatics and Liberty (CNIL; 2215827). All the data collected retrospectively were anonymised in a standardised case report form. Both ethics approval and consent from the participants were obtained for the interviews. This study involves human participants and was conducted in accordance with the French national public health code and in compliance with the General Data Protection Regulation (EU 2016/679), which is the strictest regulation in the world governing the protection of patients’ rights and the use of health data. In accordance with French regulations, this study was conducted without the need for consent from an ethics committee. Moreover, it was conducted according to the principle of the reference methodologies of CNIL. A privacy impact study was also conducted. Participants gave informed consent to participate in the study before taking part.
References
- 1.Nacher M, Adriouch L, Huber F, et al. Modeling of the HIV epidemic and continuum of care in French Guiana. PLoS One 2018;13:e0197990. 10.1371/journal.pone.0197990 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.INSEE . Available: https://www.insee.fr/fr/statistiques/5005684 [Accessed Conculted:29/07/2021].
- 3.Mam-Lam-Fouck S. Histoire générale de la Guyane française: des débuts de la colonisation la fin du XXe siècle ; les grands problème guyanais. Nouv. éd. 2002 revue et complétée. Matoury: Ibis Rouge Éd 2002. [Google Scholar]
- 4.Noucher M. Atlas critique de la Guyane. CRNS éditions., 2020. [Google Scholar]
- 5.Bressy J. Avis et recommandations sur La Prévention et La prise en charge des IST en Guyane et dans les Antilles françaises. Conseil national Du SidA et des hépatites virales, rapport, 2018. Available: https://cns.sante.fr/rapports-et-avis/avis-outre-mer-2018/ [Accessed 25 Nov 2020].
- 6.Mosnier E, Epelboin L, Guiraud N, et al. Spatial dynamics and epidemiology for AIDS in remote areas in French Guiana. AIDS Care 2019;31:498–504. 10.1080/09540121.2018.1524111 [DOI] [PubMed] [Google Scholar]
- 7.UNAIDS . Unaids global AIDS update — confronting inequalities — lessons for pandemic responses from 40 years of AIDS. UNAIDS 2021;2021. [Google Scholar]
- 8.Desgrées du Loû A, Lert F, Delfraissy J-F. Parcours: parcours de vie et santé des Africains immigrés en France. Paris: la Découverte 2017. [Google Scholar]
- 9.Nacher M, Adriouch L, Van Melle A, Melle AV, et al. Country of infection among HIV-infected patients born abroad living in French Guiana. PLoS One 2018;13:e0192564. 10.1371/journal.pone.0192564 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Divino F, de Lima Guerra Corado A, Gomes Naveca F, et al. High prevalence and onward transmission of Non-Pandemic HIV-1 subtype B clades in northern and northeastern Brazilian regions. PLoS One 2016;11:e0162112. 10.1371/journal.pone.0162112 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Nacher M, Adenis A, Huber F, et al. Estimation of the duration between HIV seroconversion and HIV diagnosis in different population groups in French Guiana: strategic information to reduce the proportion of undiagnosed infections. PLoS One 2018;13:e0199267. 10.1371/journal.pone.0199267 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Da SAÚDE. Boletim Epidemiológico de HIV/AIDS 2019. Available: http://www.aids.gov.br/pt-br/pub/2019/boletim-epidemiologico-de-hivaids-2019MINISTÉRIO [Accessed 24 July 2020].
- 13.Fassin D. Deepening divides: how territorial borders and social boundaries delineate our world. PLUTO Press, 2019. [Google Scholar]
- 14.Parriault M-C, van Melle A, Basurko C, et al. Hiv-Testing among female sex workers on the border between Brazil and French Guiana: the need for targeted interventions. Cad Saude Publica 2015;31:1615–22. 10.1590/0102-311X00138514 [DOI] [PubMed] [Google Scholar]
- 15.Mosnier Émilie. [Border: problem or ressource in health for immigrants ? The exemple of French Guiana]. Rev Prat 2019;69:679–82. [PubMed] [Google Scholar]
- 16.Almeida C, Oiapoque RA. aqui começa o Brasil: a fronteira em construção e os desafios do Desenvolvimento Regional / Oiapoque, the city where it begins Brazil: the frontier in construction and Regional Development’s challenges. Redes 2016;22:474. [Google Scholar]
- 17.d’Hautefeuille MB. La frontière franco-brésilienne (Guyane/Amapá), un modèle hybride entre mise en marge et mise en interface. Confins Revue franco-brésilienne de géographie / Revista franco-brasilera de geografia 2013;17. [Google Scholar]
- 18.Grenand F. Enjeux de territoires sur une frontière méconnue. Entre la France et le Brésil : le fleuve Oyapock. Confins Revue franco-brésilienne de géographie / Revista franco-brasilera de geografia 2012;4. [Google Scholar]
- 19.Peiter PC, Franco V, Van-Gastel B. Villes Frontalières entre le Brésil et la Guyane Française: un contexte de vulnérabilité sanitaire. In: Ville, Habitat, Habiter. Granada: Editorial Universidad de Granada, 2018: 317–32. [Google Scholar]
- 20.Jolivet A, Cadot E, Florence S, et al. Migrant health in French Guiana: are undocumented immigrants more vulnerable? BMC Public Health 2012;12:53. 10.1186/1471-2458-12-53 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.WWF . Lutte contre l’orpaillage en Guyane: orientation pour une efficacité renforcée. Rapport 2018. [Google Scholar]
- 22.Douine M, Musset L, Corlin F, et al. Prevalence of Plasmodium spp. in illegal gold miners in French Guiana in 2015: a hidden but critical malaria reservoir. Malar J 2016;15:315. 10.1186/s12936-016-1367-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Le Tourneau FM. Chercheurs d’or: l’orpaillage clandestin en Guyane française. Paris: CNRS, 2020. [Google Scholar]
- 24.MacDonald K. The Geopolitics of gold in northern Amazonia. The Extractive Industries and Society 2016;3:659–68. [Google Scholar]
- 25.Cremers L, Kolen J, de TM. Small-scale gold mining in the Amazon: the cases of Bolivia, Brazil, Colombia, Perú and Suriname. Amsterdam: CEDLA, 2013. [Google Scholar]
- 26.Moullet D, Saffache P, Transler A-L. L’orpaillage en Guyane française : synthèse des connaissances. Études caribéennes, 2006. [Google Scholar]
- 27.. Available: https://www.defense.gouv.fr/operations/territoire-national/forces-de-souverainete/guyane/harpie/fag-bilan-harpie-2020 [Accessed consulted:16/03/2021].
- 28.Grégoire E, Gagnol L. Ruées vers l’or au Sahara : l’orpaillage dans le désert du Ténéré et le massif de l’Aïr (Niger). EchoGéo 2017. 10.4000/echogeo.14933 [DOI] [Google Scholar]
- 29.Douine M, Mosnier E, Le Hingrat Q. Illegal gold miners in French Guiana: a neglected population with poor health. BMC Public Health;2017:1––10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Parent AA. Maliqua, rapport, 2019. [Google Scholar]
- 31.Mosnier E, Guiraud N, Huber F. Diagnostic et prise en charge des PVVIH en zones isolées et frontalières en Guyane. Bulletin de veille sanitaire 2015;11:10. [Google Scholar]
- 32.Klingelschmidt J, Parriault M-C, Van Melle A, et al. Transactional sex among men who have sex with men in the French Antilles and French Guiana: frequency and associated factors. AIDS Care 2017;29:689–95. 10.1080/09540121.2016.1234680 [DOI] [PubMed] [Google Scholar]
- 33.Mosnier E, Nacher M, Parriault MC, et al. Knowledge, attitudes, practices about HIV and implications in risk and stigma prevention among French Guianese and Brazilian border inhabitants : Beliefs about HIV among border inhabitants. BMC Public Health 2019;19:1633. 10.1186/s12889-019-7997-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Beaud S, Weber F. Guide de l’enquête de terrain: produire et analyser des données ethnographiques. Paris, France: La Découverte, 2010. [Google Scholar]
- 35.Boser AS, Bidaud B, Maues S, et al. Addressing HIV on the French Guianese-Brazilian border: no choice but collaboration! AIDS 2018;32:539. 10.1097/QAD.0000000000001727 [DOI] [PubMed] [Google Scholar]
- 36.Olivier de Sardan J-P. La rigueur du qualitatif: les contraintes empiriques de l’interprétation socio-anthropologique. Academia-Bruylant: Louvain-La-Neuve, 2008. [Google Scholar]
- 37.Good B. Medicine, rationality, and experience: an anthropological perspective. Cambridge, UK; New York: Cambridge University Press, 2008: 127. [Google Scholar]
- 38.Guillemaut F. Travail Du sexe et mobilité en Guyane. des défis pour la luttecontre le VIH/sida rapport 2011. [Google Scholar]
- 39.Cros M, Mégret Q. D’un idéal de virilité l’autre ? Autrepart 2009;49:137–54. [Google Scholar]
- 40.Fassin D. Quand les corps se souviennent: expériences et politiques du sida en Afrique du Sud. Paris: La Découverte, 2006. [Google Scholar]
- 41.Tabet P. La grande arnaque: sexualité des femmes et échange économico-sexuel. France 2004. [Google Scholar]
- 42.Knauth DR, Hentges B, de MJL. O diagnóstico do HIV/AIDS em homens heterossexuais: a surpresa permanece mesmo após MAIS de 30 anos de epidemia. Cadernos de Saúde Pública 2020;36. [DOI] [PubMed] [Google Scholar]
- 43.Pollak M, Schiltz M-A. Identité sociale et gestion d’un risque de santé. Actes de la Recherche en Sciences Sociales 1987;68:77–102. [Google Scholar]
- 44.Mulot S. Comment les représentations des rapports de sexe influencent-elles la prévention du sida ?L’exemple des multipartenariats sexuels antillais. Revue française de sociologie 2009;50:63–89. [Google Scholar]
- 45.Sagaon-Teyssier L, Balique H, Diallo F, et al. Prevalence of HIV at the Kokoyo informal gold mining site: what lies behind the glitter of gold with regard to HIV epidemics in Mali? a community-based approach (the ANRS-12339 Sanu Gundo cross-sectional survey). BMJ Open 2017;7:e016558. 10.1136/bmjopen-2017-016558 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Bury M. Chronic illness as biographical disruption. Sociol Health Illn 1982;4:167–82. 10.1111/1467-9566.ep11339939 [DOI] [PubMed] [Google Scholar]
- 47.Bourdier F. Migration et sida en Amazonie française et brésilienne. Matoury. Guyane française: Ibis Rouge, 2004. [Google Scholar]
- 48.Benoist J. Soigner au pluriel: essais sur le pluralisme médical. Paris: Karthala, 1996. [Google Scholar]
- 49.Adam P, Herzlich C. Sociologie de la maladie et de la médecine. Malakoff, France: Armand Colin, 2017. [Google Scholar]
- 50.Bila B, Egrot M. Accès au traitement du sida au Burkina Faso : les hommes vulnérables ? Science et technique 2008:85–92. [Google Scholar]
- 51.Patton C, AIDS G. NED-New edition. University of Minnesota Press, 2002. [Google Scholar]
- 52.Gelly M. Le classement des publics aux guichets de la santé : raisons pratiques et travail discrétionnaire. Sociologie du travail 2018;60. [Google Scholar]
- 53.Musso S. Façonnements sociaux des “vulnérabiltés” du corps des femmes, retour sur l’histoire et les leçons de l’épidémie de sida. In: Femmes, enfants et santé Madagascar: approches anthropologiques comparées. Paris: L’Harmattan, 2018: 247–60. [Google Scholar]
- 54. Piantoni F . L’enjeu migratoire en Guyane française: une géographie politique. Matoury (Guyane): Ibis rouge éd. 2009
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Data available on request due to privacy/ethical restrictions. The data that support the findings of this study are available on request from the corresponding author, [CF]. The data are not publicly available due to CNIL restrictions because they contain information that could compromise the privacy of research participants.