Abstract
Background:
We aimed to investigate the effect of preoperative administration of oral tizanidine on postoperative pain intensity after bimaxillary orthognathic surgery.
Methods:
All healthy skeletal class III patients who were candidates for bimaxillary orthognathic surgery were enrolled in this triple-blind randomized clinical trial. The study was carried out in the Maxillofacial Surgery Department of Qaem Hospital, Mashhad, Iran; from January 2021 to November 2021. The consecutive patients were randomly divided into tizanidine and placebo groups. One hour prior to anesthesia induction, the tizanidine group received 4 mg Tizanidine dissolved in 10 ml apple juice, whereas the placebo group received an identical glass of plain apple juice. All operations were performed by the same surgical team, under the same general anesthesia protocol. Postoperative pain was measured using the Visual Analogue Scale (VAS) at 3, 6, 12, 18, and 24 hours. For statistical analysis; the significance level was set at 0.05 using SPSS 23.
Results:
A total of 60 consecutive patients, consisting of 36 females (60%) and 24 males (40%) with an average age of 25.4 ± 6.0 were recruited. An increasing trend was noticed in the amount of perceived postoperative pain from the 3rd till 12th hour, and then decreased afterward. Nevertheless, the average amount of pain was significantly lower in the tizanidine compared to the placebo group, in all the evaluated time intervals (P<0.001). Moreover, there was a significantly higher requirement for postoperative opioid analgesics in the placebo compared to the tizanidine group (P=0.011).
Conclusion:
The addition of oral tizanidine was effective in reducing postoperative pain following bimaxillary orthognathic surgery. Further studies are necessary for more relevancy.
Key Words: Tizanidine, Postoperative pain, Bimaxillary Orthognathic surgery
INTRODUCTION
Orthognathic surgery is a widely performed surgical procedure with increasing popularity over the past few decades 1-5. The state of the art is used to correct severe jaw deformities and maintain a stable dentoskeletal relationship 1-6.
Adequate and efficient acute pain control after surgery is a crucial component for inpatient care and renders uncomplicated recovery and hospital discharge 1, 2, 7, 8. Stabilizing intraoperative and postoperative hemodynamic responses, as well as satisfactory pain alleviation is considered an essential measure during the immediate postoperative period after orthognathic surgeries 1, 2, 4, 5.
Adopting an appropriate postoperative pain management protocol after orthognathic surgeries can attenuate postoperative complications, lead to a shorter hospitalization period and finally enhance overall patient satisfaction 1, 2, 4, 5, 7, 9. Administration of opioids and non-steroidal anti-inflammatory drugs (NSAIDs) are usually the first-line options for postoperative pain relief measures 1, 2, 7, 9, 10. However, opioids are among the listed risk factors for postoperative vomiting and nausea (POVN) 7, 8, 11. Since patients who have undergone orthognathic surgery receive intermaxillary fixation (IMF) with either wires or elastics for a 7-14 day period postoperatively, PONV can possibly cause aspiration of gastric contents and be extremely life-threatening 1, 2, 5, 8.
Tizanidine is a centrally active α2-agonist, which has proven clinically efficacious in managing muscle spasticity 12-14. This medication is structurally similar to clonidine and also has sedative, anti-anxiety, and analgesic properties 12-17. Nevertheless, side-effects such as hypotension and bradycardia seem to be less severe when tizanidine is prescribed instead of clonidine 5, 12-17. Tizanidine reduces the need for opioids, benzodiazepine, and anesthesia medications during and after patient intubation in the operating room 12-18. In general, α2-adrenergic receptor antagonists yield hemodynamic stability during induction of anesthesia and tracheal intubation and can also minimize the chances of postoperative shivering or myocardial infarction (MI) 5, 12-17.
The effect of tizanidine in alleviating postoperative pain after laparoscopic cholecystectomy, thyroid, anorectal, and hernia repair surgeries has been investigated in previously conducted studies 12-15, 19. On the other hand, the effect of tizanidine on the pain in the field of oral and maxillofacial surgery has only been assessed in regards to myofacial and third molar surgery pain 20-22.
To the best of our knowledge, no study has to date been devoted to evaluating this matter among patients undergoing orthognathic surgery 12-15, 19-22. Hence, the purpose of the present study was to determine the effect of preoperative administration of oral tizanidine on postoperative pain intensity following bimaxillary orthognathic surgery. Due to its promising results in treating myofacial and neuropathic pain 21, 22, the authors hypothesized that preoperative tizanidine may be effective in postoperative pain management after bimaxillary orthognathic surgery.
MATERIALS AND METHODS
The protocol of this randomized clinical trial was approved by the Research and Ethics Committee of Mashhad University of Medical Sciences (IR.MUMS.DENTISTRY.REC.1399.080) and was registered in IRCT under the code 20150613022697N10. Guidelines of the declaration of Helsinki and Consort statement were followed in this research. Patients were only recruited after obtaining fully informed written consent.
Healthy adults with an American Society of Anesthesiologists (ASA) status I or II, between the ages 17 and 45, and BMI less than 30 kg/m2 (non-obese) were included in this study. Participating patients had skeletal class III deformity and were candidates for bimaxillary orthognathic surgery in the Maxillofacial Surgery Department of Qaem Hospital, Mashhad, Iran; from January 2021 to November 2021. Patients with an identified history of drug abuse, chronic pain, hypotension, bradycardia, mental problems, renal disease, long-term use of NSAIDs as well as those allergic to tizanidine; were all excluded from the study. In cases where either an intraoperative blood transfusion or postoperative ICU admission was required; the patient was also to be dropped out from the study.
Patients who finally met the above-listed inclusion criteria were enrolled and then randomly allocated into the placebo and tizanidine groups; this was accomplished by using the block randomization technique and Random Allocation Software. Allocation concealment was performed using sequentially opaque sealed envelopes. All the packages were labeled and numbered randomly and the codes were kept in a secure location until the end of the study. Although the randomization codes were concealed from the patient, treating maxillofacial surgeon, as well as data assessor nurse (triple-blind, randomized clinical trial); the oral and maxillofacial resident and anesthesiologist were aware of which group the patient had been assigned to. The resident was in charge of documenting the patients’ age, gender, BMI, amount of jaw deformity in a corresponding checklist.
Patients were kept NPO (Nil Per Os) for 8 hours preoperatively. One hour prior to being transferred to the operating room, a glass containing 4mg of tizanidine (Tehran Daru, Iran) dissolved in 10 ml apple juice was given to the tizanidine group, whereas a glass of plain apple juice was given to the placebo group; therefor patients were blinded to group allocation. It was assured that dissolving the capsule in apple juice did not affect its pharmacokinetic properties and also consuming this minor amount of juice while the patient is kept NPO will not cause any problems during the surgical procedure 13, 14.
All operations were performed by the same surgical team and the same general anesthesia protocol was applied to all patients. Bimaxillary orthognathic surgeries included a standard LeFort I osteotomy for maxillary advancement ± impaction and adjunct mandibular setback through a bilateral sagittal split osteotomy (BSSO). The duration of the surgical procedure was also recorded. During the surgical procedure, patients were carefully monitored by pulse oximetry, electrocardiogram, thermal probe, and capnography. The heart rate and mean atrial pressure (MAP) were constantly checked throughout the operation to detect any possible chances of bradycardia or severe hypotension status. In order to minimize the risk for PONV, volatile anesthetics and opioids were avoided in all cases. Consecutive patients were pre-medicated with intravenous midazolam (0.1μgr/kg) and sufentanil (10 µg). Neuromuscular relaxation was achieved using 0.5 mg/kg IV atracurium. Anesthesia was induced with 2µg/kg hypotonic intravenous propofol and then maintained with propofol at 50 μgr/kg/min and fentanyl at 0.1μgr/kg/min. At the end of the surgery, 0.004 mgr/kg intravenous neostigmine and 0.02 mg/kg intravenous atropine were applied to antagonize the effect of the muscle relaxant.
After the patients fully recovered from anesthesia, they were transferred to the surgical ward. Pharmacological postoperative management was applied identically for all patients, regardless of which study group they were allocated to. In aims of abating postoperative pain and edema, 8 mg intravenous dexamethasone (1hour preoperatively, every 4 hours intraoperatively, and every 8 hours postoperatively) was administered. 1gr intravenous apotel (every 6 hours) and 100 mg diclofenac suppository (every 12 hours) were used to achieve postoperative analgesia. In order to minimize the risk for surgical site infection, intravenous cephazolin (1gr, every 6 hours postoperatively) was administered. It was ensured that none of these medications have any recognized drug interactions with tizanidine 13, 14.
Postoperative pain intensity was evaluated using visual analogue scale (VAS) at 3, 6, 12, 18, and 24 hours postoperatively. Pain intensity was graded as follows: VAS 0-3, mild pain; 3-7, moderate pain and greater than 7, demonstrating severe pain. Pain scores were recorded by a specially trained nurse who was blinded to the assigned groups. For cases that were experiencing intolerable severe postoperative pain, intravenous morphine (5 mg) was prescribed as a rescue analgesic drug. Patients were eligible to be safely discharged from the hospital after returning to a medically stable state with stable vital signs; which was in fact during the second day after surgery.
All obtained data were collected and sent for statistical analysis. The sample size was determined 30 patients per group. Shapiro–Wilk test used to determine the normal distribution of our sample data. Chi-square test, Man-Whitney test, Fischer’s exact, and Friedman test (nonparametric repeated measure analysis of variance by ranks) were incorporated in the statistical analysis process. Simple linear regression analysis was also employed. As for descriptive analysis, appropriate charts and tables were used to display the central tendency and dispersion indexes. The significance level was set at 0.05 using SPSS 23 (SPSS Inc, IBM corp, Armonk, NY).
RESULTS
A total of 60 patients, consisting of 36 females (60%) and 24 males (40%) with a mean age of 25.4±6.0 years and an age range of 17 to 45 years; were randomly allocated into tizanidine (9 males, 21 females) and placebo (15 males, 15 females) groups. The mean age of the patients was reported to be 25.8±8.3 years in the tizanidine and 25.1±2.2 years in the placebo groups.
Shapiro–Wilk test showed that our sample data had no normal distribution. Chi-square test. Chi-square and Man-Whitney test showed that there was no statistically significant difference between the groups in respect to demographic data (P=0.114 for gender and P=0.364 for age, respectively). Patients were evaluated regarding their BMI, duration of surgery, amount of jaw deformity, opioid consumption, and pain intensity at the 3rd, 6th, 12th, 18th, and 24th hour postoperatively. Patients’ BMI ranged from 18-25 kg/m2 and displayed an average of 22.3±2.2 kg/m2. Table 1 demonstrats the comparison of age, BMI, jaw discrepancy, and surgical duration between the study groups in greater detail. The differences were not statistically significant (P>0.05 for all variables).
Table 1.
Comparison of Age, BMI, Jaw Discrepancy, and Surgery Duration between the study groups
| Variable | Group | Number | Mean± Standard Deviation | Min-Max | P -value |
|---|---|---|---|---|---|
| Age (yr) |
Placebo | 30 | 25.1±2.2 | 21 - 29 | 0.364 |
| Tizanidine | 30 | 25.8±8.3 | 17 - 45 | ||
| BMI (kg/m2) |
Placebo | 30 | 22.3±2.2 | 20 - 28 | 0.817 |
| Tizanidine | 30 | 22.2±2.1 | 20 - 29 | ||
| Jaw Discrepancy (mm) | Placebo | 30 | 5.8±1.2 | 4 - 8 | 0.499 |
| Tizanidine | 30 | 5.5±1.6 | 2 - 9 | ||
| Surgery Duration (Minutes) | Placebo | 30 | 163.3±43.1 | 75 - 240 | 0.377 |
| Tizanidine | 30 | 151.5±42.7 | 75 - 210 |
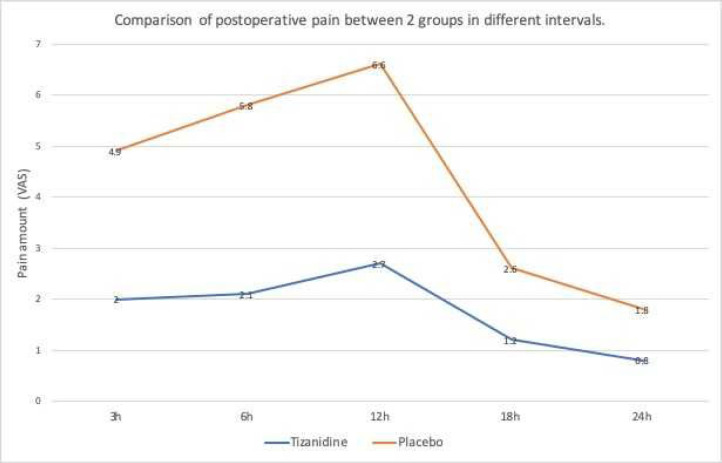
The highest and lowest recorded VAS score in all time frames was 0 and 9, respectively; while the average amount of pain was its highest at the 12th hour (4.3±2.7) and its least at the 24th hour (1.3±1.1) postoperatively. The average amount of perceived postoperative pain was 3.4±1.9 at the 3rd hour, 4.2±2.1 at the 6th hour, and finally 1.8±1.3 at the 18th hour. The average amount of pain exhibited an increasing trend until the 12th hour and then decreased thereafter.
The pain intensity was mild to moderate among the Tizanidine group, therefore none of the patients required rescue analgesics, whereas 7 (23.3%) of patients in the placebo group experienced severe pain and were in need of opioid analgesics. According to Fischer’s exact test, significantly lower opioid analgesic requirement was found in the tizanidine group compared to the placebo group (P=0.11).
Table 2 displays the average, maximum and minimum amount of postoperative pain during different time frames and intervals, in both groups. We discovered that the average amount of pain was always significantly lower in the tizanidine group in comparison to the placebo group (P<0.001 for all). We also realized that the average amount of pain intensified from the 3 to 12h and then significantly decreased afterward. Moreover, Friedman test revealed that for each group the average amount of pain was significantly different during different postoperative hours (P=0.001 for each group). This finding is illustrated in Table 3 and Figure 1.
Table 2.
Comparison of the average amount of pain between study groups
| Variable | Group | Number | Mean± Standard Deviation | Min-Max | P -value |
|---|---|---|---|---|---|
| Pain at 3h | Placebo | 30 | 4.9±1.2 | 3 - 8 | <0.001 |
| Tizanidine | 30 | 2.0±1.3 | 0 - 4 | ||
| Pain at 6h | Placebo | 30 | 5.8±1.2 | 4 - 8 | <0.001 |
| Tizanidine | 30 | 2.1±1.5 | 0 - 5 | ||
| Pain at 12h | Placebo | 30 | 6.6±1.1 | 4 - 9 | <0.001 |
| Tizanidine | 30 | 2.7±1.6 | 0 - 5 | ||
| Pain at 18h | Placebo | 30 | 2.6±1.1 | 1 - 5 | <0.001 |
| Tizanidine | 30 | 1.2±1.1 | 0 - 5 | ||
| Pain at 24h | Placebo | 30 | 1.8±1.0 | 0 - 4 | <0.001 |
| Tizanidine | 30 | 0.8±1.0 | 0 - 4 |
Table 3.
Comparison of the average amount of pain at different time intervals in both study groups
| Group | Variable | Number | Mean± Standard Deviation | Min-Max | P -value |
|---|---|---|---|---|---|
| Tizanidine | Pain at 3h | 30 | 2.0±1.3 | 0 - 4 | <0.001 |
| Pain at 6h | 30 | 2.1±1.5 | 0 - 5 | ||
| Pain at 12h | 30 | 2.7±1.6 | 0 - 5 | ||
| Pain at 18h | 30 | 1.2±1.1 | 0 - 5 | ||
| Pain at 24h | 30 | 0.8±1.0 | 0 - 4 | ||
| Placebo | Pain at 3h | 30 | 4.9±1.2 | 3 - 8 | <0.001 |
| Pain at 6h | 30 | 5.8±1.2 | 4 - 8 | ||
| Pain at 12h | 30 | 6.6±1.1 | 4 - 9 | ||
| Pain at 18h | 30 | 2.6±1.1 | 1 - 5 | ||
| Pain at 24h | 30 | 1.8±1.0 | 0 - 4 |
Figure 1.
Average amount of pain at different time intervals in placebo and tizanidine groups
As depicted in Table 4, only the amount of jaw discrepancy and duration of surgery were directly correlated to the amount of postoperative pain, in contrast to the patients’ age and BMI which were not associated with postoperative pain intensity.
Table 4.
Relationship between pain intensity and age, BMI, jaw Discrepancy, and surgery duration in each group, using Spearman correlation coefficient
| Group | Variable | Pain at 3h | Pain at 6h | Pain at 12h | Pain at 18h | Pain at 24h | |
|---|---|---|---|---|---|---|---|
| Placebo (Number=30) | Age | Spearman’s rank correlation coefficient | 0.297 | 0.193 | 0.204 | 0.188 | 0.195 |
| P-value | 0.111 | 0.31 | 0.28 | 0.32 | 0.303 | ||
| BMI | Spearman’s rank correlation coefficient | 0.361 | 0.289 | 0.169 | 0.168 | -0.183 | |
| P-value | 0.05 | 0.122 | 0.373 | 0.375 | 0.337 | ||
| Jaw Discrepancy (mm) | Spearman’s rank correlation coefficient | 0.082* | 0.149* | 0.147* | 0.087* | 0.207* | |
| P-value | 0.666 | 0.433 | 0.437 | 0.646 | 0.273 | ||
| Surgery Duration (Minutes) | Spearman’s rank correlation coefficient | 0.055* | 0.103* | 0.075* | 0.141* | 0.322* | |
| P-value | 0.044 | 0.050 | 0.030 | 0.045 | 0.083 | ||
| Tizanidine (Number=30) | Age | Spearman’s rank correlation coefficient | -0.177 | -0.249 | -0.141 | -0.302 | -0.071 |
| P-value | 0.35 | 0.185 | 0.458 | 0.105 | 0.71 | ||
| BMI | Spearman’s rank correlation coefficient | 0.345 | 0.419 | -0.016 | 0.019 | 0.108 | |
| P-value | 0.062 | 0.221 | 0.933 | 0.921 | 0.569 | ||
| Jaw Discrepancy (mm) | Spearman’s rank correlation coefficient | 0.414* | 0.392* | 0.291* | 0.414* | 0.231* | |
| P-value | 0.023 | 0.032 | 0.018 | 0.023 | 0.022 | ||
| Surgery Duration (Minutes) | Spearman’s rank correlation coefficient | 0.376* | 0.314* | 0.556* | 0.448* | 0.459* | |
| P-value | 0.041 | 0.009 | 0.001 | 0.013 | 0.011 | ||
*: significant relation.
Since the amount of postoperative pain reached its peak at 12h, the simultaneous effect of gender, age, BMI, jaw discrepancy, surgery duration, and preoperative administration of tizanidine on pain intensity were evaluated during this time. Simple linear regression analysis showed that the amount of jaw discrepancy, administration of tizanidine, and surgery duration were the only variables that were significantly related to pain intensity. Furthermore, pain intensity increased by 0.010 units in the tizanidine and 4.5 units in the placebo group, per each minute of extended surgery; and also increased by 0.07 units per each mm of greater jaw discrepancy.
Finally, we did not notice any drug-related side effects for tizanidine in any of the participating patients.
DISCUSSION
This triple-blinded randomized clinical trial was conducted in order to investigate the effect of preoperative oral tizanidine on postoperative pain in class III patients undergoing bimaxillary orthognathic surgery.
The results of the present study demonstrated that the average postoperative pain scores, as well as the need for opioid consumption, were significantly lower at all times in the tizanidine group compared to the placebo group.
Orthognathic surgery is accompanied by tissue manipulation, muscle stripping, and multiple osteotomies; resulting in subsequent mild to moderate postoperative pain which is typically controlled by pertinent pharmacologic interventions 1, 2, 4, 5, 7, 8, 23.
In patients subjected to orthognathic surgery without premedication; the chances for postoperative nausea (PON) and postoperative vomiting (POV) were reported to be %67 and %27, respectively 2, 8, 23. Taking into account the chances for PONV after opioid consumption and its proceeding complications; averting and minimizing the administration of opioid analgesics especially for patients who have undergone orthognathic surgery and are under IMF is of utmost importance 2, 8, 23.
Alpha2-agonists have long been prescribed for treating patients with hypertension 5, 13, 14. These medications have recently gained popularity for managing neuropathic pain, headaches, premedication for general anesthesia, and hemostasis during surgical procedures 13-16. Tizanidine is an imidazoline derivative of clonidine with less severe side-effect and is widely incorporated in treating muscle spasticity and also as a prophylaxis modality for chronic headaches 12-16, 19.
Oral preoperative administration of tizanidine is proven to reduce the induction dose of midazolam, the maintenance dose of propofol, the minimum alveolar concentration of sevoflurane; as well as prolong spinal anesthesia, and also regulate hypotensive responses during laryngoscopy 12-16, 19. Tizanidine side effects include drowsiness, headache, and fatigue, but are usually tolerated. However, it should be noted that this medication is contraindicated in patients with renal disease 12, 19. Therefore, the authors excluded the patients with renal disease in this study.
Tizanidine is easily absorbed in the gastrointestinal system, reaching its peak plasma concentration 2 hours after oral intake. It has a half-life of 2–4 hours 12-14, 19.
In this study, we administered preoperative oral 4mg tizanidine and used slow-release capsules. Delayed release of tizanidine from the capsule without having plasma peaks sustains the therapeutic plasma concentrations up to 24 h and has a softer pharmacokinetic profile 19.
Tizanidine’s side effects are mainly dose-dependent 12-14, 19. General tolerability was found in 44–100% of patients receiving a dose lower than 36 mg/day. The most common side effects were dry mouth (57%) and somnolence (48%) 12-14, 19. In the current study since we only administered a dose of 4mg of tizanidine, no drug-related side effects were identified in any of the participating patients.
Regarding the literature, no study has to date evaluated the effect of Tizanidine on postoperative pain among patients undergoing bimaxillary orthognathic surgery 12-15, 19-22. However, the effect of Tizanidine on myofacial pain and postoperative pain third molar surgery; have been studied 20-22.
Kirmeier et.al assessed the preemptive effect of oral tizanidine on pain intensity, trismus, and edema after third molar surgery 20. They realized that although the amount of postoperative pain and edema was lower in the tizanidine group compared to the control group, this difference was not significant; as a pose to maximum mouth opening which was significantly higher at days 1 and 3 after surgery in patients who took a preoperative dose of tizanidine 20.
In our study, the average amount of pain was significantly lower in the tizanidine compared to the Placebo group, in all the evaluated time intervals (P<0.001).
Ahiskalioglu et.al evaluated the analgesic effect of combined use of bilateral superficial cervical plexus block (BSPCB) with a single dose of oral tizanidine, after thyroid surgery in 60 patients 19. It was established that adjunct oral tizanidine administration abated posterior neck pain, occipital headache, and early postoperative opioid requirements 19.
Yazıcıoglu et.al studied the role of oral tizanidine in postoperative pain management 12. Patients undergoing inguinal hernia repair surgery were divided into tizanidine and placebo groups. The patients in the tizanidine group were to take a 4mg tizanidine pill, 1 hour prior to surgery and twice a day during their first postoperative week. The same treatment was given to the control group with an oral placebo instead of tizanidine. It was concluded that tizanidine was capable of decreasing postoperative pain intensity as well as analgesic consumption and facilitated the return to normal life 12. This was in accordance with the results of the present study.
The preemptive effect of tizanidine on postoperative pain following laparoscopic cholecystectomy was investigated by Talakoub et.al 13. A total of 70 consecutive patients were randomly allocated into tizanidine and placebo groups. Thirty patients took 4 mg of oral tizanidine with 50 cc water and the remaining subjects took plain water, 90 minutes before induction of anesthesia. It was determined that premedication with oral tizanidine prior to undergoing laparoscopic cholecystectomy, was helpful in subsiding postoperative pain, reducing additional analgesic consumption, and shortening the duration of stay in the recovery room 13. This was similar to the findings of our clinical trial.
Tabari et.al study evaluated the effect of oral tizanidine on hemodynamic responses throughout operations under general anesthesia 14. In total, 70 patients who were candidates for elective abdominal surgery under general anesthesia participated in this study. Half of the participants received 4 mg oral tizanidine 90 minutes prior to induction of anesthesia, while the other half received an oral placebo. It was concluded that oral tizanidine provided stability in blood pressure and heart rate during the surgical procedure and also reduced the required propofol dosage for maintenance of anesthesia 14. This was in accordance with the results of the present study.
A total of 60 patients with skeletal class 3 malocclusion met the inclusion criteria and were enrolled in this study. The number of consecutive patients was similar to studies conducted by Ahiskalioglu et.al 19, Yazıcıoglu et.al 12, which included 60 patients who underwent thyroidectomy, herniorrhaphy surgeries; but was larger than the number of recruited patients in Imanaga et.al study 15.
As like the studies conducted earlier, pain intensity after orthognathic surgery was evaluated during the first 24 hours postoperatively in this research, which is usually a more crucial period for patients 2, 4, 24, 25.
Time intervals for patient evaluation were set at 3, 6, 12, 18 and 24 h postoperatively which was similar previous studies 1, 2, 12, 26. Due to the fact that patients may still be disoriented one hour after full emergence from anesthesia 6, 9; therefore we decided to not assess pain intensity at 1h postoperatively. Postoperative pain intensity was evaluated subjectively through VAS; this method was also employed earlier1, 2, 13.
The administrative dose of preoperative oral tizanidine, 4mg, was similar to studies conducted earlier 13, 14. Determining the effective dose of dexamethasone, cephazoline, diclofenac, apotel, and rescue analgesic morphine was similar to what was prescribed for the patients already 2, 5, 27.
As previously mentioned, patients in the tizanidine and placebo groups were similar in respect to age, gender, BMI, jaw discrepancy and duration of surgery. Thus the net effect of our intervention is much more reliable. Similar to Samieirad et.al and Ansari et.al study, in this clinical trial postoperative pain was never significantly associated with patients’ age or BMI 1, 2.
Regardless of the study groups, average postoperative pain intensity demonstrated an increasing pattern up till 12h and then started to decrease thereafter. This finding was also observed already 1, 2, 7.
In both tizanidine and placebo groups, the amount of postoperative pain was significantly related to the duration of surgery and the amount of jaw discrepancy. This finding was also confirmed in studies conducted earlier 1, 2, 4, 7. This is attributable to the fact that severe discrepancy and prolonged surgery lead to extensive tissue trauma and therefore greater amounts of postoperative pain and edema 1, 2, 4, 7.
Table 5.
Simultaneous effect of administered drug, age, gender, BMI, jaw discrepancy, and surgery duration on pain intensity
| Variable | Regression coefficient | Standard Error | T | P -value |
|---|---|---|---|---|
| Type of Drug | 4.502 | 0.346 | 13.002 | <0 .001 |
| Age | -0.040 | 0.029 | -1.414 | 0.163 |
| Gender | 0.134 | 0.378 | 0.355 | 0.724 |
| BMI | 0.031 | 0.085 | 0.357 | 0.722 |
| Jaw Discrepancy | 0.075 | 0.137 | 0.543 | 0.005 |
| Surgery Duration | 0.010 | 0.004 | 2.187 | 0.033 |
SUGGESTIONS AND LIMITATIONS
While the results of this randomized clinical trial are encouraging, they are not without limitations. Since this study was carried out through a small population, it would be best if similar studies with a multicenter population were conducted across the country. In the present study the effect of tizanidine was assessed during the first 24 hours postoperatively; evaluating this preemptive effect over a longer period of time, and after administering higher and multiple doses of tizanidine is recommended, but it should be taken into consideration that repetitive doses in the postoperative period could improve the analgesic effect but could also lead to more frequent side effects.
CONCLUSION
Administration of oral tizanidine, 60 minutes prior to bimaxillary orthognathic surgery is effective in reducing postoperative pain, analgesic consumption, and therefore chances for PONV in candidate patients. Further studies are necessary for more relevancy.
FUNDING
None. This study was self-funded.
CONFLICTS OF INTEREST
The authors have no conflict of interest to disclose.
ACKNOWLEDGEMENTS
The authors appreciate the continued support of the research counselor of Mashhad University of Medical Sciences. We also thank Abdollah Rashid Javan for his contribution in the statistical analysis. The results of the present study were extracted from a postgraduate thesis (research project no. 990492) in Mashhad dental school, Mashhad, Iran.
References
- 1.Ansari AH, Shooshtari Z, Alipour M, Abrishami MH, Shirzadeh A, Samieirad S. What Is the Effect of Pre-Emptive Oral Montelukast on Postoperative Pain Following Bimaxillary Orthognathic Surgery? A Triple-Blind Randomized Clinical Trial. J Oral Maxillofac Surg .2022;80(2):240–247. doi: 10.1016/j.joms.2021.08.151. [DOI] [PubMed] [Google Scholar]
- 2.Samieirad S, Sharifian-Attar A, Eshghpour M, et al. Comparison of Ondansetron versus Clonidine efficacy for prevention of postoperative pain, nausea and vomiting after orthognathic surgeries: A triple blind randomized controlled trial. Med Oral Patol Oral Cir Bucal. 2018 Nov;23(6):e767–e76. doi: 10.4317/medoral.22493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Naran S, Steinbacher DM, Taylor JA. Current Concepts in Orthognathic Surgery. Plast Reconstr Surg. 2018 Jun;141(6):925e–36e. doi: 10.1097/PRS.0000000000004438. [DOI] [PubMed] [Google Scholar]
- 4.Eshghpour M, Mianbandi V, Samieirad S. Intra-and postoperative complications of Le Fort I maxillary osteotomy. J Craniofac Surg. 2018;29(8):e797–e803. doi: 10.1097/SCS.0000000000004828. [DOI] [PubMed] [Google Scholar]
- 5.Mohammadi F, Marashi M, Tavakoli I, Khakbaz O. Effects of oral clonidine premedication on hemodynamic status in bimaxillary orthognathic surgery: A double-blind randomized clinical trial. J Craniomaxillofac Surg. 2016 Apr;44(4):436–9. doi: 10.1016/j.jcms.2016.01.004. [DOI] [PubMed] [Google Scholar]
- 6.Khechoyan DY. Orthognathic surgery: general considerations. Semin Plast Surg. 2013 Aug;27(3):133–6. doi: 10.1055/s-0033-1357109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Mobini A, Mehra P, Chigurupati R. Postoperative Pain and Opioid Analgesic Requirements After Orthognathic Surgery. J Oral Maxillofac Surg. 2018 Nov;76(11):2285–95. doi: 10.1016/j.joms.2018.05.014. [DOI] [PubMed] [Google Scholar]
- 8.Panula K, Finne K, Oikarinen K. Incidence of complications and problems related to orthognathic surgery: a review of 655 patients. J Oral Maxillofac Surg. 2001;59(10):1128–36. doi: 10.1053/joms.2001.26704. [DOI] [PubMed] [Google Scholar]
- 9.Agbaje J, Luyten J, Politis C. Pain Complaints in Patients Undergoing Orthognathic Surgery. Pain Res Manag. 2018;2018:4235025. doi: 10.1155/2018/4235025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Fletcher MC, Spera JF. Management of acute postoperative pain after oral surgery. Dent Clin North Am. 2012 Jan;56(1):95–111, viii. doi: 10.1016/j.cden.2011.09.001. [DOI] [PubMed] [Google Scholar]
- 11.Shaikh SI, Nagarekha D, Hegade G, Marutheesh M. Postoperative nausea and vomiting: A simple yet complex problem. Anesth Essays Res. 2016 Sep-Dec;10(3):388–96. doi: 10.4103/0259-1162.179310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Yazicioglu D, Caparlar C, Akkaya T, Mercan U, Kulaçoglu H. Tizanidine for the management of acute postoperative pain after inguinal hernia repair: A placebo-controlled double-blind trial. Eur J Anaesthesiol. 2016;33(3):215–22. doi: 10.1097/EJA.0000000000000371. [DOI] [PubMed] [Google Scholar]
- 13.Talakoub R, Abbasi S, Maghami E, Zavareh SMHT. The effect of oral tizanidine on postoperative pain relief after elective laparoscopic cholecystectomy. Adv Biomed Res. 2016;5:19. doi: 10.4103/2277-9175.175905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Tabari M, Alipour M, Esalati H. Evaluation of oral tiazinidine effects on [intraoperative] hemodynamic responses during direct laryngoscopy under general anesthesia. Iran Red Cresc Med J. 2013;15(7) doi: 10.5812/ircmj.11540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Imanaga K, Wajima Zi, Inoue T, Ogawa R. Effect of oral tizanidine on local-anesthetic infiltration pain during epidural catheterization. J Nippon Med School. 2004;71(2):105–10. doi: 10.1272/jnms.71.105. [DOI] [PubMed] [Google Scholar]
- 16.Wajima Zi, Yoshikawa T, Ogura A, et al. Oral tizanidine, an α2-adrenoceptor agonist, reduces the minimum alveolar concentration of sevoflurane in human adults. Anesth Analg. 2002;95(2):393–6. doi: 10.1097/00000539-200208000-00028. [DOI] [PubMed] [Google Scholar]
- 17.Hord AH, Denson DD, Azevedo MI. Systemic Tizanidine Hydrochloride (Zanaflex™) Partially Decreases Experimental Postoperative Pain in Rats. Anesth Analg. 2001;93(5):1307–9. doi: 10.1097/00000539-200111000-00056. [DOI] [PubMed] [Google Scholar]
- 18.Manfredini D, Romagnoli M, Bosco M. Efficacyof tizanidine hydrochloride in the treatment of myofascial face pain. Minerva Med 2004Apr. 2004;95(2):165–71. [PubMed] [Google Scholar]
- 19.Ahiskalioglu A, Yayik AM, Ahiskalioglu EO, et al. Ultrasound-guided bilateral superficial cervical block and preemptive single-dose oral tizanidine for post-thyroidectomy pain: a randomized-controlled double-blind study. J Anesth. 2018;32(2):219–26. doi: 10.1007/s00540-018-2468-x. [DOI] [PubMed] [Google Scholar]
- 20.Kirmeier R, Truschnegg A, Payer M, Acham S, Schulz K, Jakse N. Evaluation of a muscle relaxant on sequelae of third molar surgery: a pilot study. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2007;104(3):e8–e14. doi: 10.1016/j.tripleo.2007.02.024. [DOI] [PubMed] [Google Scholar]
- 21.Malanga GA, Gwynn MW, Smith R, Miller D. Tizanidine is effective in the treatment of myofascial pain syndrome. Pain Physician. 2002;5(4):422–32. [PubMed] [Google Scholar]
- 22.Pal US, Kumar L, Mehta G, et al. Trends in management of myofacial pain. Natl J Maxillofac Surg. 2014;5(2):109. doi: 10.4103/0975-5950.154810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kim S-G, Park S-S. Incidence of complications and problems related to orthognathic surgery. J Oral Maxillofac Surg. 2007;65(12):2438–44. doi: 10.1016/j.joms.2007.05.030. [DOI] [PubMed] [Google Scholar]
- 24.Alizadeh R, Mireskandari S-M, Azarshahin M, et al. Oral clonidine premedication reduces nausea and vomiting in children after appendectomy. Iran J Pediatr. 2012;22(3):399. [PMC free article] [PubMed] [Google Scholar]
- 25.Wadood F, Muhammad R, Jamil M, un Nisa W. Efficacy of ondansetron alone and ondansetron plus dexamethasone in preventing nausea and vomiting after middle ear surgery. Ayub Med Coll Abbottabad . 2014;26(1):80–3. [PubMed] [Google Scholar]
- 26.Shilpa SN, Shailaja S, Hilda SS. Comparison of Efficacy of Clonidine versus Ondansetron for Prevention of Nausea and Vomiting Post Thyroidectomy: A Double Blind Randomized Controlled Trial. J Clin Diagn Res. 2015 May;9(5):Uc01–3. doi: 10.7860/JCDR/2015/12721.5866. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Tabrizi R, Eftekharian H, Pourdanesh F, Khaghaninejad MS. Does oral clonidine premedication decrease bleeding during open rhinoplasty? J Craniofac Surg. 2014 May;25(3):1101–3. doi: 10.1097/SCS.0000000000000660. [DOI] [PubMed] [Google Scholar]