Abstract
Background
As one of the essential programs that have been developed for decades, childhood immunizations are mandatory to protect children from vaccine-preventable diseases. Despite its availability and accessibility, immunization coverage has not reached the intended goals. Vaccine hesitancy and COVID-19 pandemic may threaten immunization coverage in children. This study aimed to evaluate the tailored educational videos to reduce vaccine hesitancy and analyze the changes in childhood routine immunization status.
Methods
This was an interventional quasi-experimental study in three subdistricts of North Jakarta, Indonesia. Participants were allocated into educational videos exposures (intervention group, n = 116) or to the digital version of the maternal and child health handbook (control group, n = 104). We administered a pre- and post-intervention vaccine hesitancy survey using the Parent Attitudes about Childhood Vaccines (PACV) questionnaire with cut-off scores of 50.
Results
A total of 220 parents were recruited in this study from June 18, 2021, to December 10, 2021. The pre-intervention PACV survey showed that 19 (8.6%) parents were vaccine-hesitant from both groups: 12 (10.3%) and 7 (6.7%) of parents among intervention and control groups. After the interventions, there were 8 (6.9%) and 8 (7.7%) vaccine-hesitant parents in the intervention and control groups, respectively. We found a significant difference in the post-intervention PACV median score between the intervention and control groups (17 vs 23; p = 0.035). Around 25% of parents have not completed their children’s immunization status: 22.4% and 28.8% in the intervention and control groups, respectively. There was a significant difference between the proportion of PACV hesitancy on the immunization status within intervention and control groups (p = 0.001).
Conclusion
There was a reduction in vaccine hesitancy after interventions. Educational videos intervention distributed through WhatsApp group was associated with lower vaccine hesitancy and can be used as health education tools among Indonesian parents in the community.
Keywords: Health education, Health promotion, Indonesia, Vaccination, Vaccination hesitancy
1. Introduction
As one of the essential programs that have been developed for decades, childhood immunization aims to protect children from vaccine-preventable diseases (VPD). Vaccine hesitancy has been identified as one of the ten global health threats by the World Health Organization that can cause low vaccine intake and affect herd immunity [1], [2]. SAGE Working Group on Vaccine Hesitancy defines vaccine hesitancy as a “delay in acceptance or refusal of vaccination despite the availability of vaccination services” [3].
Regardless of being one of the most densely populated cities in Southeast Asia, some districts in Jakarta have not reached the immunization coverage of 95% as targeted through the comprehensive Multi-Year Plan (cMYP) for Universal Immunization Program [4]. This might be caused by the COVID-19 pandemic which had led to immunization service disruption, besides vaccine hesitancy. Poor herd immunity can cause an outbreak of VPD and threaten the future health of Indonesian children. The vaccine hesitancy movement in Indonesia in 2017 has warned us of its dangerous impact, resulting in measles and rubella outbreak—449 and 147 cases of measles and rubella, respectively, between January and July 2017 [5]. Furthermore, very low immunization coverage was found, even after the national campaign, where almost 10 million children were not immunized [6], [7]. Several strategies in overcoming vaccine hesitancy include involving religious and community leaders, mobilizing mass media, strengthening partnerships between private and public sectors, providing non-financial incentives, communication training in health care workers, and leveraging social media for online education [8], [9], [10].
The pandemic has also caused infodemic that may increase vaccine misconception and vaccine hesitancy, making it harder to achieve immunization goals and decreasing immunization coverage, even more, affected by risk perception [11]. Fortunately, as the internet became more widely used and accessible during the pandemic, distributing immunization information to parents may become more manageable. The latest publication also supported and encouraged social media use to improve parents' vaccine acceptance [12]. This study primarily aimed to evaluate educational videos as strategies to reduce vaccine hesitancy among Indonesian parents, compared to the maternal and child health (MCH) handbook digital version as a standard educational tool. We also analyzed the improvement in childhood routine immunization status after five weeks of intervention as a secondary outcome.
2. Methods
2.1. Participants
This was an interventional quasi-experimental study in three districts of North Jakarta: Cilincing, Koja, and Tanjung Priok. We included parents with children aged 10–18 months and had electronic devices that could play videos, such as smartphones or tablets, recruited through community health centers database. Participants were excluded if their children had contraindicated for immunization and dropped out if they did not finish the study. Our target population was parents with children aged 10–18 months in Jakarta. Participants were recruited both offline from parents who came to the community health centers and online through community health centers database. Eligible parents were selected using consecutive sampling, explained and asked to sign informed consent online, then allocated systematically into the intervention or control group.
2.2. Measurements and outcomes
Demographic data of parents and routine immunization status were obtained. Additionally, we conducted a short survey on parents’ attitude and practice towards childhood immunization during the COVID-19 pandemic (agree/disagree): (1) The government recommends routine immunization for your child, even during the pandemic; (2) I think immunization is important to prevent infectious diseases during the pandemic; (3) I will bring my child for immunization even during the pandemic.
2.3. Vaccine hesitancy assessments
We administered a pre- and post-intervention vaccine hesitancy survey regarding childhood immunizations using the Indonesian-translated Parent Attitudes about Childhood Vaccines (PACV) online questionnaire that has been validated, with cut-off scores of 50 out based on the original validation study and previous studies [13], [14]. A score of 15 questions on PACV was converted into 100 scales, where higher scores indicate hesitancy in vaccination [14].
2.4. Childhood routine immunization status
According to Indonesian Ministry of Health Decree no 12/2017, routine immunization is considered complete if children have received hepatitis B (HB)-0 vaccine at birth; one BCG vaccine; three doses of diphtheria, tetanus, and pertussis (DTP), HB, Haemophilus influenza type B (HiB) vaccine; four doses of oral polio vaccine (OPV) and one inactivated polio vaccine (IPV), or three doses of IPV; and one measles rubella (MR) vaccine. Routine immunization can be obtained freely from the community health centers, sponsored by the government, or out-of-pocket at the private clinics. Immunization status was obtained through records on MCH handbook. Increased immunization status were considered when children obtained at least one immunization after the intervention.
2.5. Intervention
The educational videos included five modules: (1) danger and prevention of VPD; (2) rationales of completing immunization; (3) immunization amid the COVID-19 pandemic; (4) vaccine misconception; and (5) adverse events following immunization and how to treat it. Each video was less than 2 min with clear and straightforward messages according to the National Institute of Health guideline for health education. Materials were distributed through WhatsApp groups and viewed for five weeks. Participants in the control group were given exposure to the digital version of the MCH handbook, 2020 edition, consisting of animated pictures and simple instructions [15].
2.6. Ethics
This study was approved by the Health Research Ethics Committee - the University of Indonesia, KET-1042/UN2.F1/ETIK/PPM.00.02/ 2020.
2.7. Statistical analysis
All data were processed using the Statistical Package for The Social Sciences (SPSS) version 25. Baseline characteristics were provided as proportion, and PACV scores were analyzed as a continuous and categorical variable. We analyzed the difference between pre- and post-intervention PACV scores between groups using the Mann-Whitney test. We also compared the immunization status using Fisher’s Exact test between groups and performed logistic regression analysis for the changes in childhood routine immunization status after five weeks of intervention as the secondary outcome, where children with complete or increased in at least one vaccination were compared to children with incomplete or no changes in immunization status. Adjustment for the logistic regression was done for potential confounders, including baseline PACV score, children’s age, maternal age, maternal education, and family income. Using data from previous studies,[14] the target sample size was 95 parents per group, which would provide 80% power to detect a difference in the proportion of 14% at a significance level of 5%.
3. Results
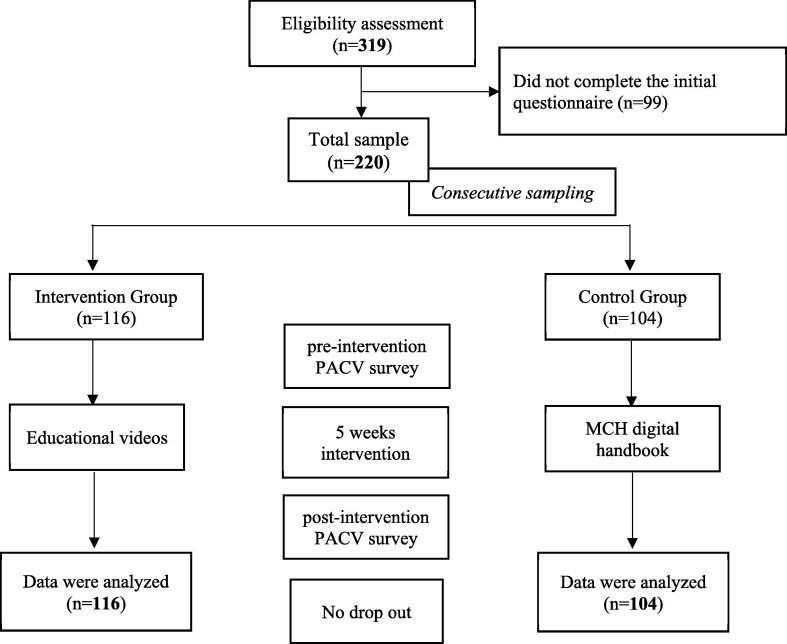
Out of 319 parents who went through the eligibility assessment, 99 parents did not complete the initial questionnaire. In the end, there were 116 parents in the intervention group, and 104 parents in the control group were recruited from June 18, 2021, to December 10, 2021 (Figure 1 ). We made 21 WhatsApp groups for sharing educational videos or MCH digital handbooks for participants. There were 11 groups for intervention parents and 10 groups for control parents, with 5–10 parents per group. No one was dropped out of this study.
Fig. 1.
Parents enrollment flow.
Table 1 shows the participants’ characteristics of each group. Most participants, both in intervention and control groups, were mothers in the 20–29 age group, senior high school graduates, and incomes of less than or equal to 280 USD (2021 Jakarta’s regional minimum wage). Around 25% of parents from both groups have not completed their children’s immunization status (Table 1). The pre-intervention PACV survey showed that 19 (8.6%) parents were vaccine-hesitant from both groups: 12 (10.3%) and 7 (6.7%) of parents among intervention and control groups, respectively. After the interventions, there were 16 (7.3%) vaccine-hesitant parents: 8 (6.9%) and 8 (7.7%) in the intervention and control groups, respectively. This number decreased by 3% (n = 4) in the intervention group while increasing by 1% (n = 1) in the control group.
Table 1.
Parents’ characteristics.
| Characteristics, n (%) | Intervention group n = 116 | Control group n = 104 | P* |
|---|---|---|---|
| Mothers, n (%) | 111 (95.7) | 104 (100) | 0.62 |
| Mother’s age-years, median (range) | 29 (22–45) | 27 (20–43) | 0.34 |
| Children’s age-months, median (range) | 14 (10–18) | 14 (10–18) | 0.00 |
| Age groups, n (%) | 0.94 | ||
| 20–29 years | 98 (84.5) | 89 (85.6) | |
| 30–39 years | 16 (13.8) | 13 (12.5) | |
| 40–49 years | 2 (1.7) | 2 (1.9) | |
| Education, n (%) | 0.15 | ||
| Elementary school | 6 (5.2) | 5 (4.8) | |
| Junior high school | 7 (6) | 15 (14.4) | |
| Senior high school | 69 (59.5) | 49 (47.1) | |
| Diploma | 7 (6) | 11 (10.6) | |
| University | 27 (23.3) | 24 (23.1) | |
| Income per month, n (%) | 0.26 | ||
| ≤4 million rupiahs | 79 (68.1) | 78 (75) | |
| >4 million rupiahs | 37 (31.9) | 26 (25) | |
| Complete immunization status, n (%) | 90 (77.6) | 74 (71.2) | 0.274 |
| Complete/increased after intervention, n (%) | 92 (79.3) | 75 (72.1) | |
| Vaccine hesitant (PACV ≥ 50), n (%) | 0.341 | ||
| Pre-intervention | 12 (10.3) | 7 (6.7) | |
| Post-intervention | 8 (6.9) | 8 (7.7) |
Note: *Chi-square, Fisher’s Exact, or Mann-Whitney U test between intervention and control groups; PACV: Parent Attitudes about Childhood Vaccines.
Our short survey on parents’ attitude and practice towards childhood immunization regarding the COVID-19 pandemic revealed: 1) 94% of parents agreed on government recommendations towards routine immunization; 2) 96% of parents think that immunization is important to prevent infectious diseases during the pandemic; 3) and 95% of parents will bring their children for immunization even during the pandemic.
As PACV scores were not distributed normally, the median score was used and compared for pre- and post-intervention (Table 2 ). There was a significant difference between post-intervention PACV median scores between the intervention and control groups. Additionally, we also ran a sub-analysis of PACV classification of immunization status. We found a significant difference between the proportion of PACV hesitancy on the immunization status within intervention and control groups (p = 0.001) (Table 3 ). Three confident parents (two from intervention group, one from control group) improved their children’s immunization status after the intervention. Table 4 shows unadjusted and adjusted regression analysis, showing insignificant higher odds (adjusted odds ratio of 1.9) of improved immunization status after five weeks of intervention in the intervention group.
Table 2.
PACV median scores of pre- and post-intervention.
| Intervention group n = 116 | Control group n = 104 | P-value* | |
|---|---|---|---|
| Median (range) | Median (range) | ||
| Pre-intervention score | 20 (11–33) | 27 (17–33) | 0.148 |
| Post-intervention score | 17 (10–33) | 23 (17–33) | 0.035 |
| Delta median score | 0 ((−4)−10) | 0 ((−6)−4) | 0.583 |
Mann-Whitney test.
Table 3.
Changes in immunization status on the intervention and control groups.
|
Intervention group*n = 116 |
Control group*n = 104 |
|||
|---|---|---|---|---|
| Confident | Hesitant | Confident | Hesitant | |
| Immunization status, n(%) | ||||
| Complete/increased | 90 (83.3) | 2 (25) | 75 (78.1) | 0 (0) |
| Incomplete/no change | 18 (16.7) | 6 (75) | 21 (21.9) | 8 (100) |
Fisher’s Exact test, p-value ≤ 0.001.
Table 4.
Odds ratio of changes in immunization status on the intervention and control groups.
| Intervention (n = 116) | Control (n = 104) | |
|---|---|---|
| Complete/increased immunization status | 92 (79.3%) | 75 (72.1%) |
| OR |
1.48 (95% CI: 0.80– 2.76) |
Ref |
| aOR |
1.87 (95% CI: 0.49–7.08) |
Ref |
OR: Odds Ratio.
aOR: Adjusted Odds Ratio for baseline PACV score, children’s age, mothers’ age, mother’s education, and family income.
4. Discussion
In this study, a total of 8.6% of parents were vaccine-hesitant. This number was lower than previous studies in Sumatra (15.9%) and Malaysia (11.6%) [14], [16]. This might be because we obtained samples from high immunization coverage (92%) in three community health centers in North Jakarta with different demographic and socioeconomic status.
We found a significant difference in post-intervention PACV median score between the intervention and the control group, indicating significantly lower vaccine-hesitant parents in the intervention group after learning from the educational videos distributed through WhatsApp groups. There was no significant difference in the median difference between PACV scores pre- and post-intervention, although it showed an improvement. A validation study by Opel et al.,[17] showed that a decrease in PACV scores was significantly associated with the age at which children received complete routine immunization.
A previous study by Williams et al [18] revealed a statistically significant decrease in the PACV scores of mothers who received education in the form of videos. Similarly, Klein et al [19] also reported statistically significant results for vaccine confidence after being given an educational pamphlet. Changes in attitudes and behavior towards immunization are the first step towards increasing vaccination adherence. However, in these two studies, the significant difference in the PACV scores of the intervention subjects was not followed by a significant change in children’s immunization status at the end of the study [18], [19].
There was a significant relationship between vaccine hesitancy and the child’s immunization status (p < 0.001). A previous study by Stoeckel et al [20] showed lower immunization rates in areas where vaccine hesitancy was more pronounced. Parents’ vaccine hesitancy can hinder the completeness of the childhood immunization status and may bring future harm to children and their surroundings. Therefore, pockets of low immunization coverage should be the priority areas as they are risk factors for future VPD outbreaks caused by vaccine-hesitant parents.
Besides socioeconomic status, vaccine hesitancy—a complex problem—has become one of the critical determinants of immunization status [21], [22]. Improving vaccine confidence among parents requires specific context and culturally appropriate messages and relevant to reasons behind vaccine hesitancy, as they might differ across countries [23]. Materials were carefully designed according to the “Clear and Simple” National Institute of Health guideline and adapted to the Indonesian culture. Our educational videos were carefully tailored and relevant to Indonesian parents. These materials contain positive persuasion, emphasizing optimism and motivating parents to vaccinate their children. For example, “We can build a healthy and prosperous young generation of Indonesia by having a complete immunization schedule!” This hopeful message is expected to “win ‘hearts and minds’” and create a sense of responsibility for a better future in the parents’ hands [24], [25]. These emotions can create a powerful drive and influence parents’ decision-making. Anticipating adverse events following immunization was also addressed to reduce parents’ anxiety. Furthermore, we tailored our materials to the current pandemic situation, such as what to do when bringing children to the vaccination centers, which may address parents’ concerns regarding COVID-19 transmission while vaccinating their children.
Vaccine hesitancy is associated with delayed and incomplete vaccination, and our goal for the immunization program should first make hesitant parents more compliant with vaccination practice to improve child health, reach herd immunity, and prevent future outbreaks, regardless of their attitude. We are certain that completing childhood immunization status, even in only one child, is clinically important. Studies regarding parents’ perception and decisions on children’s vaccination in China showed that a modified health belief model might help to understand the drivers and barriers to childhood vaccination. They found that worry, anxiety, and social norms are significant in parents’ decision-making [26]. Similar themes were also found in Australian parents who were highly concerned about vaccine safety, side effects, and vaccine schedule [27]. These issues, however, can also be tackled by analyzing the vaccine development report and post-marketing surveillance report on adverse events and debunking inappropriate vaccine safety profiles using the actual evidence [28].
A recent survey in Bangladesh showed that the theory of planned behavior contains psychological determinants of vaccine hesitancy and predicts better, particularly on the COVID-19 vaccine. This theory includes attitude toward vaccines, subjective norm, perceived behavioral control, and anticipated regret. In the latest research in Indonesia, Sinuraya et al [29] found that parents’ attitudes and knowledge were associated with the practice of childhood immunization during the pandemic. Though it may be different across cultures, such as doctor’s recommendation in India influenced parents’ decision making more than other factors [30]. Studying psychological determinants in the Indonesian context may be necessary for future studies to increase vaccine uptake, reduce hesitancy, and tailor educational materials and communication messages [31]. Our materials addressed these themes from the health belief model, such as the consequences for unvaccinated children (perceived severity), vaccine efficacy (perceived benefits), and simple practical steps in acquiring immunization (self-efficacy).
Our short survey results on parents’ attitudes and practices towards childhood immunization regarding the COVID-19 pandemic might indicate the possibility that the pandemic may be a contributing factor, but not the leading cause of vaccine hesitancy in the community. Additionally, the Indonesian Pediatric Society has urged parents not to delay childhood immunization to prevent future VPD outbreaks [32].
Further implementation of this study includes disseminating the potential materials to a larger scale, bringing community and religious leaders, engaging community health workers and primary health care professionals, and evaluating materials to ensure parents’ needs and motivations still fit the context [23]. Educational materials can also be broadcasted on the radio, TV, or social media and combined with messages/call reminder systems to increase uptake; and with motivational interviewing, which has been proven to reduce hesitancy [33], [34], [35]. Social media utilization, particularly Facebook and WhatsApp used for this study, has also been proven to effectively increase vaccine acceptance among parents in Italy, yielding greater vaccination coverage than the national coverage for the COVID-19 vaccine among children aged 5–11 years old [12].
There were several limitations to this study. First, educational videos in the intervention group were given online through WhatsApp groups, and subjects watched the videos independently at home. We did not collect data on how focused or how many times participants had watched the videos. Second, a quasi-experimental method without the data collection and analysis blinding may contribute to bias. Third, instead of probability sampling, we used a consecutive sampling method that may also play a role in selection bias.
Despite these shortcomings, this research was the first study to use educational materials in the form of videos through WhatsApp group to improve vaccine confidence. Furthermore, it can help health care workers educate parents about immunization, especially during a pandemic. This study used the internationally recognized PACV questionnaire to quantify vaccine hesitancy. The digital intervention also significantly provides fewer vaccine hesitancy in the intervention group compared to the control group. This study proves that immunization status is related to vaccine hesitancy.
5. Conclusions
Educational videos can reduce vaccine hesitancy in parents with children aged 10–18 months. Tailored educational video intervention shared through WhatsApp groups was associated with lower vaccine hesitancy (PACV median score) and can be used as health education tools that affect childhood immunization completion status among Indonesian parents in the community. This can be a starting point to promote national immunization programs in other provinces.
Ethical approval
We acquired written permission from Professor Douglas J. Opel, University of Washington, Seattle as the inventor of the PACV questionnaire to adapt and use the translated version. This study was approved by the Health Research Ethics Committee - the University of Indonesia, KET-1042/UN2.F1/ETIK/PPM.00.02/ 2020. Participants read the informed consent form and agreed before participating.
Author contributions
HG, ABP, TAL, H conceptualized this study. SS, HIS, and FSA were involved in the methodology process. TAL managed data collection. HG, ABP, TAL, H analyzed this study. TAL and HG drafted the initial manuscript. SS, HIS, and FSA revised the manuscript. All authors reviewed and finalized the manuscript.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgment
We would like to acknowledge all parents who participated in the study and community health centers in Koja, Cilincing, Tanjung Priuk for their support. We would also thank Jeslyn Tengkawan MD, MPH for her assistance in preparing the manuscript and statistical computation. The authors would like to thank Universitas Indonesia for funding this research (PUTI Grant No: NKB-1884/UN2.RST/HKP.05.00/2020).
References
- 1.Schuster M., Eskola J., Duclos P. SAGE Working Group on Vaccine Hesitancy. Review of vaccine hesitancy: Rationale, remit and methods. Vaccine. 2015;33(34):4157–4160. doi: 10.1016/j.vaccine.2015.04.035. [DOI] [PubMed] [Google Scholar]
- 2.World Health Organization. Ten threats to global health in 2019. Published 2019. Accessed January 28, 202https://www.who.int/news-room/spotlight/ten-threats-to-global-health-in-2019
- 3.MacDonald N.E. Vaccine hesitancy: definition, scope and determinants. Vaccine. 2015;33(34):4161–4164. doi: 10.1016/j.vaccine.2015.04.036. [DOI] [PubMed] [Google Scholar]
- 4.World Health Organization. Regional Office for South-East Asia. South-East Asia Regional Vaccine Action Plan 2016-2020. World Health Organization. Regional Office for South-East Asia; 2017. Accessed May 18, 2022. https://apps.who.int/iris/handle/10665/272397
- 5.Ministry of Health. Measles-Rubella Immunization Coverage. Sehat Negeriku. Published January 8, 2019. Accessed May 7, 2022. https://sehatnegeriku.kemkes.go.id/baca/umum/20190108/1529050/secara-makro-cakupan-imunisasi-campak-rubella-capai-87/
- 6.Pronyk P., Sugihantono A., Sitohang V., et al. Vaccine hesitancy in Indonesia. Lancet Planet Health. 2019;3(3):e114–e115. doi: 10.1016/S2542-5196(18)30287-0. [DOI] [PubMed] [Google Scholar]
- 7.Harapan H., Shields N., Kachoria A.G., Shotwell A., Wagner A.L. Religion and measles vaccination in Indonesia, 1991–2017. Am J Prev Med. 2021;60(1 Suppl 1):S44–S52. doi: 10.1016/j.amepre.2020.07.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Butler R., MacDonald N.E. SAGE Working Group on Vaccine Hesitancy. Diagnosing the determinants of vaccine hesitancy in specific subgroups: The Guide to Tailoring Immunization Programmes (TIP) Vaccine. 2015;33(34):4176–4179. doi: 10.1016/j.vaccine.2015.04.038. [DOI] [PubMed] [Google Scholar]
- 9.WHO SAGE working group dealing with vaccine hesitancy. Strategies for Addressing Vaccine Hesitancy – A Systematic Review. World Health Organization; 2014. https://www.who.int/immunization/sage/meetings/2014/october/3_SAGE_WG_Strategies_addressing_vaccine_hesitancy_2014.pdf
- 10.Tan T.Q., Gunardi H., Smith S., et al. Global immunization systems strengthening through pediatric societies: the promise of private–public partnerships in Indonesia. Hum Vaccines Immunother. 2019;16(5):1194–1201. doi: 10.1080/21645515.2019.1697108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.He K, Mack WJ, Neely M, Lewis L, Anand V. Parental Perspectives on Immunizations: Impact of the COVID-19 Pandemic on Childhood Vaccine Hesitancy. J Community Health. Published online July 23, 2021. doi: https://doi.org/10.1007/s10900-021-01017-9 [DOI] [PMC free article] [PubMed]
- 12.Di Mauro A, Di Mauro F, De Nitto S, et al. Social Media Interventions Strengthened COVID-19 Immunization Campaign. Front Pediatr. 2022;10. Accessed July 20, 2022. https://www.frontiersin.org/articles/10.3389/fped.2022.869893 [DOI] [PMC free article] [PubMed]
- 13.Opel D.J., Mangione-Smith R., Taylor J.A., et al. Development of a survey to identify vaccine-hesitant parents: the parent attitudes about childhood vaccines survey. Hum Vaccin. 2011;7(4):419–425. doi: 10.4161/hv.7.4.14120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Yufika A., Wagner A.L., Nawawi Y., et al. Parents’ hesitancy towards vaccination in Indonesia: A cross-sectional study in Indonesia. Vaccine. 2020;38(11):2592–2599. doi: 10.1016/j.vaccine.2020.01.072. [DOI] [PubMed] [Google Scholar]
- 15.Ministry of Health. Maternal and Child Health Handbook. Ministry of Health Indonesia; 2020. Accessed January 28, 2022. https://kesga.kemkes.go.id/assets/file/pedoman/BUKU%20KIA%20REVISI%202021%20LENGKAP.pdf
- 16.Mohd Azizi F.S., Kew Y., Moy F.M. Vaccine hesitancy among parents in a multi-ethnic country, Malaysia. Vaccine. 2017;35(22):2955–2961. doi: 10.1016/j.vaccine.2017.04.010. [DOI] [PubMed] [Google Scholar]
- 17.Opel D.J., Taylor J.A., Mangione-Smith R., et al. Validity and reliability of a survey to identify vaccine-hesitant parents. Vaccine. 2011;29(38):6598–6605. doi: 10.1016/j.vaccine.2011.06.115. [DOI] [PubMed] [Google Scholar]
- 18.Williams S.E., Rothman R.L., Offit P.A., Schaffner W., Sullivan M., Edwards K.M. A Randomized Trial to Increase Acceptance of Childhood Vaccines by Vaccine-Hesitant Parents: A Pilot Study. Acad Pediatr. 2013;13(5):475–480. doi: 10.1016/j.acap.2013.03.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Klein N.P., Kissner J., Aguirre A., et al. Differential maternal responses to a newly developed vaccine information pamphlet. Vaccine. 2009;28(2):323–328. doi: 10.1016/j.vaccine.2009.10.046. [DOI] [PubMed] [Google Scholar]
- 20.Stoeckel F., Carter C., Lyons B.A., Reifler J. Association of vaccine hesitancy and immunization coverage rates in the European Union. Vaccine. 2021;39(29):3935–3939. doi: 10.1016/j.vaccine.2021.05.062. [DOI] [PubMed] [Google Scholar]
- 21.Bedford H., Attwell K., Danchin M., Marshall H., Corben P., Leask J. Vaccine hesitancy, refusal and access barriers: The need for clarity in terminology. Vaccine. 2018;36(44):6556–6558. doi: 10.1016/j.vaccine.2017.08.004. [DOI] [PubMed] [Google Scholar]
- 22.Gunardi H., Strirartnaputri A., Saidah F., et al. Socioeconomic Determinants of Complete Immunization Status in Under-Five Children in Slum Inner Capital City. Indian J Public Health Res Dev. 2019;10(11) [Google Scholar]
- 23.Thomson A., Vallée-Tourangeau G., Suggs L.S. Strategies to increase vaccine acceptance and uptake: From behavioral insights to context-specific, culturally-appropriate, evidence-based communications and interventions. Vaccine. 2018;36(44):6457–6458. doi: 10.1016/j.vaccine.2018.08.031. [DOI] [PubMed] [Google Scholar]
- 24.Attwell K., Smith D.T. Hearts, minds, nudges and shoves: (How) can we mobilise communities for vaccination in a marketised society? Vaccine. 2018;36(44):6506–6508. doi: 10.1016/j.vaccine.2017.08.005. [DOI] [PubMed] [Google Scholar]
- 25.Enkel S.L., Attwell K., Snelling T.L., Christian H.E. ‘Hesitant compliers’: Qualitative analysis of concerned fully-vaccinating parents. Vaccine. 2018;36(44):6459–6463. doi: 10.1016/j.vaccine.2017.09.088. [DOI] [PubMed] [Google Scholar]
- 26.He L., Liao Q.Y., Huang Y.Q., Feng S., Zhuang X.M. Parents’ Perception and their Decision on their Children’s Vaccination Against Seasonal Influenza in Guangzhou. Chin Med J (Engl) 2015;128(3):327–341. doi: 10.4103/0366-6999.150099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Rozbroj T., Lyons A., Lucke J. Vaccine-Hesitant and Vaccine-Refusing Parents’ Reflections on the Way Parenthood Changed Their Attitudes to Vaccination. J Community Health. 2020;45(1):63–72. doi: 10.1007/s10900-019-00723-9. [DOI] [PubMed] [Google Scholar]
- 28.Stefanizzi P., De Nitto S., Patano F., et al. Post-marketing surveillance of adverse events following measles, mumps, rubella and varicella (MMRV) vaccine: retrospecive study in apulia region (ITALY) Hum Vaccines Immunother. 2009–2017.;16(8):1875–1883. doi: 10.1080/21645515.2019.1704124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Sinuraya R.K., Kusuma A.S., Pardoel Z.E., Postma M.J., Suwantika A.A. Parents’ Knowledge, Attitude, and Practice on Childhood Vaccination During the COVID-19 Pandemic in Indonesia. Patient Prefer Adherence. 2022;16:105–112. doi: 10.2147/PPA.S339876. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Ramprasad C., Zachariah R., Steinhoff M., Simon A. Parental attitudes towards influenza vaccination for children in South India. World J Pediatr. 2017;13(1):84–90. doi: 10.1007/s12519-016-0053-7. [DOI] [PubMed] [Google Scholar]
- 31.Hossain MB, Alam MdZ, Islam MdS, et al. Health Belief Model, Theory of Planned Behavior, or Psychological Antecedents: What Predicts COVID-19 Vaccine Hesitancy Better Among the Bangladeshi Adults? Front Public Health. 2021;9. Accessed February 2, 2022. https://www.frontiersin.org/article/10.3389/fpubh.2021.711066 [DOI] [PMC free article] [PubMed]
- 32.Pudjiadi AH, Putri ND, Sjakti HA, et al. Pediatric COVID-19: Report From Indonesian Pediatric Society Data Registry. Front Pediatr. 2021;9. Accessed February 10, 2022. https://www.frontiersin.org/article/10.3389/fped.2021.716898 [DOI] [PMC free article] [PubMed]
- 33.MacDonald N.E., Butler R., Dubé E. Addressing barriers to vaccine acceptance: an overview. Hum Vaccines Immunother. 2017;14(1):218–224. doi: 10.1080/21645515.2017.1394533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Atchison C., Zvoc M., Balakrishnan R. The Evaluation of a Standardized Call/Recall System for Childhood Immunizations in Wandsworth, England. J Community Health. 2013;38(3):581–587. doi: 10.1007/s10900-013-9654-4. [DOI] [PubMed] [Google Scholar]
- 35.Gagneur A., Gosselin V., Dubé È. Motivational interviewing: a promising tool to address vaccine hesitancy. Vaccine. 2018;36(44):6553–6555. doi: 10.1016/j.vaccine.2017.10.049. [DOI] [PubMed] [Google Scholar]