Abstract
Background
Recurrent shoulder instability is an orthopedic problem with potentially long-term functional ramifications. Although arthroscopic stabilization has become increasingly utilized over open stabilization, optimal surgical intervention to minimize recurrent instability remains controversial.
Methods
The PearlDiver Mariner database was queried for all cases of open and arthroscopic shoulder stabilization from 2010 to 2019. Utilization trends were aggregated after identifying cohorts of 107,210 and 13,217 patients who respectively underwent arthroscopic or open stabilization using Current Procedural Terminology codes. Subsets from those cohorts with laterality-specific International Classification of Diseases, Tenth Revision codes for shoulder instability were used to evaluate 2-year rates of recurrent instability (presence of shoulder dislocation or revision open or arthroscopic stabilization). Linear regression and chi-squared analysis were used to analyze utilization trends and to compare recurrent instability.
Results
Arthroscopic stabilization comprised 90% of all stabilization procedures with annual utilization continuing to increase into 2019. Latarjet utilization increased from 15% to 42% of all open stabilization procedures while open Bankart repair utilization decreased from 56% to 35%. The rate of recurrent instability was 10.2% after arthroscopic stabilization and 12.3% after open stabilization (P = .01). Rates of redislocation (4.0% vs. 2.6%, P < .01), conversion to shoulder arthroplasty (1.2% vs. 0.4%, P < .01), and revision open stabilization (6.8% vs. 2.3%, P < .01) after index open stabilization were significantly higher than after index arthroscopic stabilization. There was no difference in revision stabilization or dislocation rates between open procedures.
Conclusion
Despite increasing utilization of coracoid transfer, arthroscopic stabilization is still the dominant modality used for surgical treatment of shoulder instability and in our analysis, showed lower 2-year rates of dislocation, revision open stabilization, and conversion to shoulder arthroplasty.
Keywords: Shoulder instability, Open shoulder stabilization, Arthroscopic shoulder stabilization, Revision shoulder stabilization, Shoulder stabilization trends, Latarjet procedure utilization
Shoulder instability is a common and challenging orthopedic problem with an estimated incidence of 23.9 per 100,000 persons.13,16,27,29 Symptomatic shoulder instability is increasingly managed with arthroscopic surgery, although the optimal surgical intervention remains controversial as there is concern of recurrent instability with arthroscopic-only procedures.1,17,18 For first-time dislocations nonsurgical treatment can be recommended; however, recurrent instability rates range from 70% to 100% in patients younger than 30 years old and present a challenging issue of which glenohumeral arthrosis is a potential debilitating long-term sequela.19 Commonly used techniques for surgical shoulder stabilization include arthroscopic procedures such as a capsulolabral (Bankart) repair as well as open procedures including Bankart repairs, Latarjet procedure, open capsular shift, and alternative bone block transfers.13,17 Arthroscopic stabilization is the predominant method for surgical stabilization with 84%-87% relative utilization compared to open stabilization procedures, an incidence that increased 8% between 2007 and 2015 in a recent analysis of nearly 6000 stabilization procedures.5,17
Despite these trends, optimal surgical intervention remains controversial.5,16,18 A matched prospective analysis of 186 patients who underwent arthroscopic Bankart repair compared to open Latarjet found a 2-fold increase in recurrent instability (10% vs. 22%) in patients who underwent arthroscopic Bankart repair though reoperation rates were similar.12 Although meaningful, few studies are able to compare the range of open procedures used to treat shoulder instability, a particular challenge given the relative infrequency with which these procedures are performed. Kowalski et al was the first study using a large database to look at postoperative complications from all open shoulder stabilization procedures.1 In their analysis from 2007 to 2010 they found that the overall complication rate from open stabilization surgery was 12.3% with posterior glenoid bone grafting having the highest complication rate (20.7%) though they did not do a comparative analysis with arthroscopic procedures.1
The goal of this study is to utilize a large nationwide administrative database to directly compare trends, complications, and need for revision stabilization surgery in arthroscopic stabilization as well as 4 separate open stabilization procedures to understand the relative differences in outcomes from these various procedures. We hypothesize that there will be significantly more arthroscopic procedures performed than open surgery and that this trend is continuing to increase. Additionally, we expect that the utilization of Latarjet will increase and we anticipate that soft tissue arthroscopic procedures will have higher rates of recurrent dislocation.
Materials and methods
This analysis was performed using the PearlDiver Mariner All-Payer Claims Database (Colorado Springs, CO, USA), a retrospective nationwide insurance billing database that provides deidentified and patient-specific claims including 144 million patients. The PearlDiver database that includes claims from patients of all age groups across the Unites States enrolled multiple private payer commercial insurances or Medicare advantage plans from 2010 through 2019 including populations across all payer types. Although deidentified and HIPAA compliant, this dataset is also capable of longitudinal research based on unique patient identifier codes. This database allows for searching of patients with any orthopedic International Classification of Diseases, Ninth Revision (ICD-9) or Current Procedural Terminology (CPT) code.28,29 It has been used in prior population-scale analyses both in shoulder instability analysis and other orthopedic surgery procedures.12,18,20,29
Inclusion criteria
All reported cases of open and arthroscopic shoulder stabilization procedures performed between 2010 and 2019 were queried from the database using CPT codes (Table I). The CPT code 29806 (arthroscopy, shoulder, surgical; capsulorrhaphy) was used to search the database for arthroscopic stabilizations. The CPT codes 23455 (capsulorrhaphy, anterior; with labral repair [i.e., Bankart procedure]), 23460 (capsulorrhaphy, anterior, any type; with bone block), 23462 (capsulorrhaphy, anterior, any type; with coracoid process transfer [i.e., Latarjet procedure], and 23466 (Capsulorrhaphy, glenohumeral joint, any type multidirectional instability [i.e., Capsular shift]) were used to search the database for open shoulder stabilizations. Demographics variables queried for trend analysis and to describe our cohort included year of surgery, sex, Charlson Comorbidity Index, obesity, patient-reported tobacco use, diabetes, and patient age at the time of surgery.
Table I.
CPT codes of stabilization surgeries, reoperations, and complications.
| Open stabilization | 23455: Capsulorrhaphy, anterior; with labral repair (i.e., Bankart procedure) |
| 23460: Capsulorrhaphy, anterior, any type; with bone block | |
| 23462: Capsulorrhaphy, anterior, any type; with coracoid process transfer (i.e., Latarjet procedure) | |
| 23466: Capsulorrhaphy, glenohumeral joint, any type multidirectional instability (i.e., Capsular shift) | |
| Arthroscopic stabilization | 29806: Arthroscopy, shoulder, surgical; Capsulorrhaphy |
| Dislocation: closed treatment | 23650: Closed treatment of shoulder dislocation, with manipulation; without anesthesia |
| 23655: Closed treatment of shoulder dislocation, with manipulation; requiring anesthesia | |
| Revision: open stabilization∗ | 23107: Arthrotomy, glenohumeral joint exploration with or without removal of loose or foreign body |
| 23331: Removal of foreign body, shoulder; deep (i.e., Neer hemiarthroplasty removal) | |
| 23465: Capsulorrhaphy, glenohumeral joint, posterior, with or without bone block | |
| 23660:- Open treatment of acute shoulder dislocation with fracture | |
| 23670:- Open treatment of shoulder dislocation, with fracture of greater humeral tuberosity | |
| 23470:- Arthroplasty, glenohumeral joint; hemiarthroplasty | |
| 23472: Arthroplasty, glenohumeral joint; total shoulder (glenoid and proximal humeral replacement) | |
| 23030: Incision and drainage, shoulder area; deep abscess or hematoma | |
| Revision: arthroscopic stabilization∗ | 29805: Arthroscopy, shoulder, diagnostic, with or without synovial biopsy (separate procedure) |
| 29807: Arthroscopy, shoulder, surgical; repair of SLAP lesion | |
| 29819: Arthroscopy, shoulder, surgical; with removal of loose body or foreign body | |
| 29820: Arthroscopy, shoulder, surgical; synovectomy, partial | |
| 29821: Arthroscopy, shoulder, surgical; synovectomy, complete | |
| 29822: Arthroscopy, shoulder, surgical; debridement, limited | |
| 29823: Arthroscopy, shoulder, surgical; debridement, extensive | |
| 29824: Arthroscopy, shoulder, surgical; distal claviculectomy including distal articular surface (Mumford procedure) | |
| 29825: Arthroscopy, shoulder, surgical; with lysis and resection of adhesions, with or without manipulation | |
| 29826: Arthroscopy, shoulder, surgical; decompression of subacromial space, acromioplasty | |
| 29827: Arthroscopy, shoulder, surgical; with rotator cuff repair |
CPT, Current Procedural Terminology.
Revision of open and arthroscopic stabilization groups also include the respective index stabilization CPT codes.
Revision analysis
For the 2-year revision surgery analysis, only patients with ICD-10 coding were analyzed. This subset of patients then were tracked for incidence of shoulder dislocation, conversion to shoulder arthroplasty, revision open stabilization, and revision arthroscopic stabilization using CPT codes listed in Table I for 24 months. ICD-10 coding allows for laterality-specific tracking to ensure that revision procedures were performed on the ipsilateral side as the index procedure. Overall recurrent instability was measured as presence of CPT code for revision procedure or dislocation treatment listed in Table I excluding arthroplasty procedural codes 23470 and 23472. As a proxy for ensuring patients were not lost to follow-up, “Active” tracking of these subsets was used to confirm that patients maintained insurance enrollment during our postoperative window of analysis.
Statistical analysis
All graphing and statistical analyses were performed using R statistical software (R Project for Statistical Computing, Vienna, Austria) integrated with PearlDiver and Microsoft Excel Version 16.46 (Microsoft Excel XLSTAT, New York, NY, USA) with significance defined as P < .05. Linear regression was used to analyze percent change in annual stabilization procedures performed open or arthroscopic. Chi-squared analysis was used to compare incidence of dislocation or revision procedures after index open and arthroscopic stabilization and among open stabilization procedures only.
Results
Between 2010 and 2019, we identified 120,427 patients who underwent shoulder stabilization, of which 89% (107,210) were arthroscopic and 11% (13,217) were open. Demographic variables to describe our cohorts are included in Table II. Patients who underwent shoulder stabilization were younger with 50% being between 10 and 30 years old. Approximately two-thirds of patients were male which was similar between open and arthroscopic stabilization as well as among open stabilization procedures with exception of open capsular shift whose population was divided evenly between genders.
Table II.
Patient demographics for open and arthroscopic shoulder stabilization.
| Demographics | Open stabilization (n = 13,217) | Arthroscopic stabilization (n = 107,210) | Open coracoid transfer (n = 4202) | Open capsulolabral repair (n = 5742) | Open capsular shift (n = 2398) | Open anterior glenoid bone graft (n = 875) |
|---|---|---|---|---|---|---|
| Age group | ||||||
| 10-19 | 18% | 25% | 15% | 21% | 24% | 12% |
| 20-29 | 32% | 24% | 40% | 26% | 25% | 33% |
| 30-39 | 20% | 17% | 24% | 18% | 19% | 21% |
| 40-49 | 12% | 15% | 11% | 13% | 9% | 11% |
| 50-59 | 9% | 11% | 6% | 11% | 8% | 10% |
| 60+ | 9% | 8% | 4% | 11% | 15% | 13% |
| Female | 33% | 35% | 25% | 32% | 49% | 32% |
| CCI (SD) | 0.84 (1.46) | 0.63 (1.17) | 0.77 (1.35) | 0.81 (1.43) | 0.96 (1.65) | 0.95 (1.51) |
| Obesity | 22% | 19% | 19% | 25% | 23% | 20% |
| Diabetes | 13% | 9% | 12% | 14% | 13% | 16% |
| Tobacco use | 26% | 17% | 28% | 23% | 28% | 35% |
CCI, Charlson Comorbidity Index; SD, standard deviation.
Trend analysis
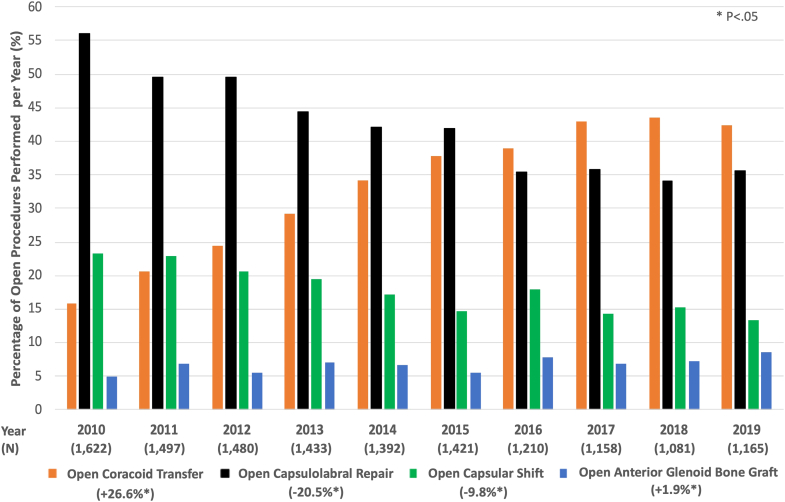
Arthroscopic stabilization accounted for 88% of all 12,598 shoulder stabilization procedures recorded in 2010 while only 12% of procedures were open stabilization. Over the course of the study period there was a slight but steady increase in the percent of procedures performed arthroscopically. In 2019, 90% of all 11,196 shoulder stabilization procedures were performed arthroscopically while only 10% were performed with open. With regard to utilization trends of open stabilization procedures (Fig. 1), we found that open coracoid transfer (Latarjet) utilization significantly (P < .01) increased from 15% to 42% of all open stabilization procedures performed while open capsulolabral repair (Bankart) and open capsular shift utilization respectively decreased from 56% to 35% (P < 1) and 23% to 13% (P < .01). Open anterior glenoid bone graft utilization showed a modest but statistically significant increase in percent utilization from 4.9% to 8.6% (P = .02).
Figure 1.
Percent of annual open stabilization procedures performed per procedure.
Revision stabilization analysis
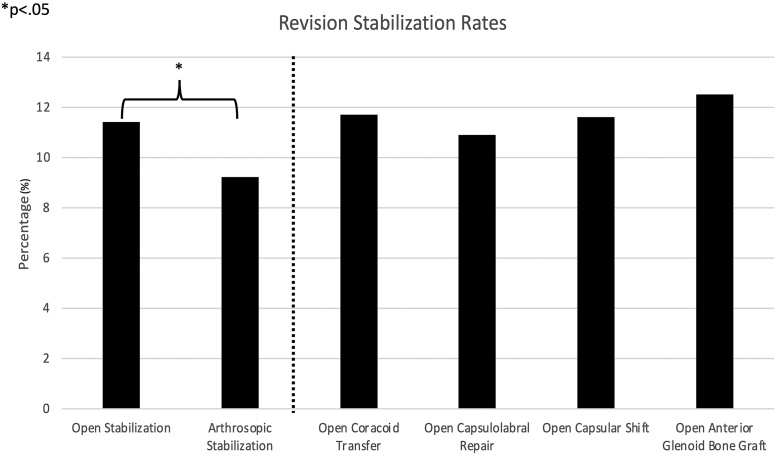
We identified a subset of 1733 open stabilization patients and 9558 arthroscopic stabilization patients as seen in Table III with same-day ICD-10 codes for shoulder instability linked to the CPT code for shoulder stabilization for our revision analysis. Of the 1733 open stabilization procedures in this subset, 777 were open coracoid transfer, 578 were open capsulolabral repairs, 250 were open capsular shift, and 128 were open anterior glenoid bone graft as seen in Table IV. From these cohorts, 2-year revision stabilization rates were analyzed. Within a 24-month postoperative period, the overall rate of recurrent instability was statistically lower after arthroscopic stabilization compared to open stabilization (10.2% vs. 12.3%, P = .01). About 11.5% of patients who underwent index open stabilization had revision open or arthroscopic stabilization compared to 9.2% of patients who underwent index arthroscopic stabilization (P < .01) (Fig. 2). Rates of redislocation (4.0% vs. 2.0%, P < .01), conversion to shoulder arthroplasty (1.2% vs. 0.4%, P < .01), and revision open stabilization (6.8% vs. 2.3%, P < .01) after index open stabilization were statistically higher compared to rates after index arthroscopic stabilization; however, rates of revision arthroscopic stabilization were not significantly different (Table III).
Table III.
Complication and revisions performed per index operation.
| Complication | Open stabilization (n = 1733) | Arthroscopic stabilization (n = 9558) | P value |
|---|---|---|---|
| Dislocation: closed treatment | 4.0% | 2.6% | <.01∗ |
| Conversion to shoulder arthroplasty | 1.2% | 0.4% | <.01∗ |
| Revision: open stabilization | 6.8% | 2.3% | <.01∗ |
| Revision: arthroscopic stabilization | 6.8% | 7.7% | .19 |
P < .05.
Table IV.
Complication and revisions performed per open index operation.
| Complication | Open coracoid transfer (n = 777) | Open capsulolabral repair (n = 578) | Open capsular shift (n = 250) | Open anterior glenoid bone graft (n = 128) | P value |
|---|---|---|---|---|---|
| Dislocation: closed treatment | 4.4% | 2.7% | 6.4% | 3.1% | .08 |
| Revision: open stabilization | 7.7% | 5.9% | 8.0% | 3.9% | .26 |
| Revision: arthroscopic stabilization | 6.2% | 6.7% | 7.6% | 8.6% | .70 |
Figure 2.
Two-year rates of revision stabilization after open or arthroscopic stabilization.
There were no significant differences in revision stabilization between the 4 different index open stabilization procedures (Fig. 2; open coracoid transfer 11.7%, open capsulolabral repair 10.9%, open capsular shift 11.6%, and open anterior glenoid bone graft 12.5%). There was also a nonsignificant trend (P = .08) toward higher dislocation rates after certain open stabilization procedures with open capsular shift (6.4%) having the largest 2-year dislocation rate followed by open coracoid transfer (4.4%), open anterior glenoid bone graft (3.1%), and open capsulolabral repair (2.7%) (Table IV). There was no difference in rates of revision open or arthroscopic stabilization between different index open stabilization procedures (Table IV).
Discussion
In this study, we utilized a population-size database to analyze recurrent shoulder instability after arthroscopic or open treatment with tracking of laterality-specific ICD-10 diagnostic codes previously unavailable before widespread implementation in 2015. We found that despite increasing utilization of open coracoid transfer compared to other open procedures, arthroscopic stabilization is still the dominant modality used with statistically lower rates of 2-year redislocation, revision open stabilization, and conversion to shoulder arthroplasty.
Open vs. arthroscopic stabilization
Although the rate of increasing use of arthroscopy has somewhat plateaued compared to analyses in prior decades, arthroscopy is still the main procedure used to manage shoulder instability.6,8,14,18,29 Bonazza et al,6 utilizing The MarketScan Database, similarly to our analysis found that 90% of shoulder stabilization procedures performed between 2008 and 2012 were performed arthroscopically. Reasons for these shifts are definitively multifactorial. Patient-level factors and the prevalence of these factors may play a role. In 2000, Burkhart and De Beer7 first reported a significantly higher recurrent instability rate in patients with significant glenoid bone deficiency treated with arthroscopic stabilization. They defined significant glenoid bone loss as >25% loss of the inferior glenoid diameter.26 Since then, multiple studies have demonstrated the need to identify the loss of and restore glenoid bone stock in treating shoulder instability which is done through an open approach.3,15,21,24 However, clinically significant glenoid bone loss after dislocation is relatively low with a retrospective analysis of the CT scans from 218 patients with single or recurrent shoulder dislocation showing only 6% had between 20-25% glenoid bone loss and 6% had >25% bone loss.9 Lower prevalence of injuries requiring open stabilization may contribute to lower utilization of open techniques.
Other risk factors for recurrent instability after arthroscopic stabilization include low age, competitive sport practice, and hyperlaxity.4 Specifically, competitive contact athletes have significantly higher risk of recurrent instability and postsurgical recurrent instability has been shown to be significantly associated with preoperative episodes of subluxation.23 Our analysis did demonstrate a greater risk of recurrent dislocation after open stabilization compared to arthroscopic stabilization though we suspect differences in preoperative severity of instability play a large role in that difference.
Patient-related factors may contribute to lower rates of open stabilization; however, whether arthroscopic or open stabilization leads to lower rates of recurrent instability is continuously debated. In this analysis, the overall rate of recurrent instability was lower (10.2%) after arthroscopic stabilization compared to open stabilization (12.3%). However, these differences may be due to the different indications for performing open vs. arthroscopic stabilization. As glenoid bone loss and higher number of dislocations may be indications for open stabilization, the open treatment cohort may inherently be at higher risk for recurrent instability. Harris et al10 in their systematic analysis of open vs. arthroscopic Bankart repair found that the rate of recurrent instability with arthroscopic repair was 11% which was similar to our current study. They documented a nonsignificantly different rate of recurrent instability for open Bankart of 8% which is lower than our reported value of 12.3%. However, it is important to note that our analysis included Latarjet and alternative bone block stabilization which have been reported in other analyses to have higher rates of recurrent instability.10,12 In addition, a recent randomized controlled trial comparing open and arthroscopic Bankart repair did not show any clinically relevant differences in patient-reported outcome scores between the 2 techniques.2 Bessière et al5 likewise demonstrated similar rates of recurrent instability between arthroscopic Bankart and open Latarjet, 6% and 7% respectively.
Subanalysis of only open stabilization procedures
Our study also demonstrated a continuation of the trend toward decreased open Bankart utilization seen in prior analyses6,18 and as of 2015, open coracoid transfer has become the dominant modality for open stabilization comprising nearly half of all open stabilization procedures in 2019. Riff et al18 similarly demonstrated this inflection point in 2015 with the 2 techniques being used in nearly the same number of cases in 2015 despite open Bankart repair being performed 6 times more frequently than Latarjet at the beginning of the study period in 2007. Reasons for this rise in use of Latarjet are most likely multifactorial and prior analyses have attributed it in part to increased international collaboration of European shoulder techniques and increased literature on the importance of patient selection and identifying glenoid bone loss.18 An international survey of European, American, and South African arthroscopy societies conducted in 2010 demonstrated that Latarjet was the preferred surgical technique for management of anterior glenohumeral instability by 72% of French surgeons compared to 9% for surgeons not from France.22
Despite the increase in utilization of Latarjet, clinical outcome studies between Latarjet and other open procedures have been mixed. A 2016 meta-analysis on Latarjet vs Bankart repair found increased risk of recurrent instability with open Bankart repair of 21.1% compared to 11.6%, although they did not find a difference in risk of revision surgery or dislocations.1 This is compared to Kowalski et al12 who demonstrated that open posterior glenoid bone graft stabilization had the highest 1-year complication rate (20.7%) followed by anterior glenoid bone graft stabilization (20.1), coracoid process transfer (16.8), and open Bankart repair (10.8%). In our study, we found no difference in rates of revision stabilization between open procedures with overall lower rates of revision stabilization after open anterior glenoid bone grafting (12.5%) and open coracoid transfer (11.7%) and a near identical rate after open Bankart repair (10.9%) compared to Kowalski et al.12 Jacobson et al11 in a meta-analysis of studies evaluating open capsular shift found a rate of recurrent instability of 11.7% comparable to our rate of revision stabilization after open capsular shift of 11.6%. As discussed previously presence of glenoid bone defects is increasingly recognized to contribute to anterior glenohumeral instability and as such patients with greater amounts of glenoid damage and risk of recurrent instability are more likely to undergo bone transfer procedures. However, specifically Latarjet procedure may have lower rates of revision stabilization among open procedures that involve bony defects due to the triple effect of anterior glenoid augmentation, capsular repair, and the sling effect of the conjoint tendon.26 According to a biomechanical study on 8 fresh-frozen cadavers, the sling effect contributes to 51%-76% of the stability of the glenohumeral joint after Latarjet fixation.25 This along with extension of the articular arc and patient selection may account for possible differences between open stabilization procedures.
Limitations
Although an advantage of this study is the nationwide patient population analyzed, there are limitations associated with analysis of an administrative database. There is limited granularity within a publicly available database and as such we were unable to evaluate patient-level factors for recurrent dislocation such as number of prior dislocations or glenoid bone loss which may point toward different indications for performing certain stabilization procedures. Along those lines, differences in indications of using open vs. arthroscopic stabilization for which we were not able to assess in this database may contribute to differences in revision rates. Additionally, use of an administrative database does not allow us to assess for lost to follow-up which may bias results; however, by using “Active” tracking of patients to ensure they maintained insurance enrollment for the duration of the analysis we sought to limit this effect. Additionally, our tracking of procedure codes was only for the first occurrence of a procedural code after an index procedure. It is possible that this index procedure was not their first operation and as such we may be counting a certain amount of revision procedures as index procedures which may bias toward worse outcomes for open stabilization procedures often done after failed arthroscopic surgery.
Conclusion
Despite increasing utilization of coracoid transfer, arthroscopic stabilization is still the dominant modality used for surgical treatment of shoulder instability and in our analysis, showed comparable yet lower 2-year rates of dislocation, revision open stabilization, and conversion to shoulder arthroplasty.
Disclaimers:
Funding: No funding was disclosed by the authors.
Conflicts of interest: The authors, their immediate families, and any research foundation with which they are affiliated have not received any financial payments or other benefits from any commercial entity related to the subject of this article.
Footnotes
Institutional review board approval was not required for this study.
Supplementary data to this article can be found online at https://doi.org/10.1016/j.jseint.2022.06.004.
Supplementary data
References
- 1.An V.V.G., Sivakumar B.S., Phan K., Trantalis J. A systematic review and meta-analysis of clinical and patient-reported outcomes following two procedures for recurrent traumatic anterior instability of the shoulder: Latarjet procedure vs. Bankart repair. J Shoulder Elbow Surg. 2016;25:853–863. doi: 10.1016/j.jse.2015.11.001. [DOI] [PubMed] [Google Scholar]
- 2.Archetti Netto N., Tamaoki M.J.S., Lenza M., dos Santos J.B.G., Matsumoto M.H., Faloppa F., et al. Treatment of Bankart lesions in traumatic anterior instability of the shoulder: a randomized controlled trial comparing arthroscopy and open techniques. Arthrosc J Arthrosc Relat Surg. 2012;28:900–908. doi: 10.1016/j.arthro.2011.11.032. [DOI] [PubMed] [Google Scholar]
- 3.Arciero R.A., Parrino A., Bernhardson A.S., Diaz-Doran V., Obopilwe E., Cote M.P., et al. The effect of a combined glenoid and Hill-Sachs defect on glenohumeral stability: a biomechanical cadaveric study using 3-dimensional modeling of 142 patients. Am J Sports Med. 2015;43:1422–1429. doi: 10.1177/0363546515574677. [DOI] [PubMed] [Google Scholar]
- 4.Balg F., Boileau P. The instability severity index score. A simple pre-operative score to select patients for arthroscopic or open shoulder stabilisation. J Bone Joint Surg. Br. 2007;89:1470–1477. doi: 10.1302/0301-620X.89B11.18962. [DOI] [PubMed] [Google Scholar]
- 5.Bessière C., Trojani C., Carles M., Mehta S.S., Boileau P. The open Latarjet procedure is more Reliable in terms of shoulder stability than arthroscopic bankart repair. Clin Orthop. 2014;472:2345–2351. doi: 10.1007/s11999-014-3550-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bonazza N.A., Liu G., Leslie D.L., Dhawan A. Trends in surgical management of shoulder instability. Orthop J Sports Med. 2017;5 doi: 10.1177/2325967117712476. :232596711771247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Burkhart S.S., De Beer J.F. Traumatic glenohumeral bone defects and their relationship to failure of arthroscopic Bankart repairs: significance of the inverted-pear glenoid and the humeral engaging Hill-Sachs lesion. Arthrosc J Arthrosc Relat Surg. 2000;16:677–694. doi: 10.1053/jars.2000.17715. [DOI] [PubMed] [Google Scholar]
- 8.Galvin J.W., Eichinger J.K., Cotter E.J., Greenhouse A.R., Parada S.A., Waterman B.R. Trends in surgical management of anterior shoulder instability: increased utilization of bone augmentation techniques†. Mil Med. 2018;183:e201–e206. doi: 10.1093/milmed/usx077. [DOI] [PubMed] [Google Scholar]
- 9.Griffith J.F., Antonio G.E., Yung P.S.H., Wong E.M.C., Yu A.B., Ahuja A.T., et al. Prevalence, pattern, and spectrum of glenoid bone loss in anterior shoulder dislocation: CT analysis of 218 patients. AJR Am J Roentgenol. 2008;190:1247–1254. doi: 10.2214/AJR.07.3009. [DOI] [PubMed] [Google Scholar]
- 10.Harris J.D., Gupta A.K., Mall N.A., Abrams G.D., McCormick F.M., Cole B.J., et al. Long-term outcomes after Bankart shoulder stabilization. Arthrosc J Arthrosc Relat Surg. 2013;29:920–933. doi: 10.1016/j.arthro.2012.11.010. [DOI] [PubMed] [Google Scholar]
- 11.Jacobson M.E., Riggenbach M., Wooldridge A.N., Bishop J.Y. Open capsular shift and arthroscopic capsular Plication for treatment of multidirectional instability. Arthrosc J Arthrosc Relat Surg. 2012;28:1010–1017. doi: 10.1016/j.arthro.2011.12.006. [DOI] [PubMed] [Google Scholar]
- 12.Kowalski T.J., Khan A.Z., Cohen J.R., Lord E.L., Ishmael C., Soohoo N.F., et al. Open shoulder stabilization: current trends and 1-year postoperative complications. JSES Open Access. 2017;1:72–78. doi: 10.1016/j.jses.2017.07.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kroner K., Lind T., Jensen J. The epidemiology of shoulder dislocations. Arch Orthop Trauma Surg. 1989;108:288–290. doi: 10.1007/BF00932317. [DOI] [PubMed] [Google Scholar]
- 14.Owens B.D., Harrast J.J., Hurwitz S.R., Thompson T.L., Wolf J.M. Surgical trends in Bankart repair: an analysis of Data from the American board of Orthopaedic surgery Certification Examination. Am J Sports Med. 2011;39:1865–1869. doi: 10.1177/0363546511406869. [DOI] [PubMed] [Google Scholar]
- 15.Park I., Oh M.-J., Shin S.-J. Effects of glenoid and humeral bone defects on recurrent anterior instability of the shoulder. Clin Orthop Surg. 2020;12:145–150. doi: 10.4055/cios19060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Petrera M., Patella V., Patella S., Theodoropoulos J. A meta-analysis of open versus arthroscopic Bankart repair using suture anchors. Knee Surg Sports Traumatol Arthrosc. 2010;18:1742–1747. doi: 10.1007/s00167-010-1093-5. [DOI] [PubMed] [Google Scholar]
- 17.Polyzois I., Dattani R., Gupta R., Levy O., Narvani A.A. Traumatic first time shoulder dislocation: surgery vs non-operative treatment. Arch Bone Joint Surg. 2016;4:104–108. [PMC free article] [PubMed] [Google Scholar]
- 18.Riff A.J., Frank R.M., Sumner S., Friel N., Bach B.R., Verma N.N., et al. Trends in shoulder stabilization techniques used in the United States based on a large private-payer database. Orthop J Sports Med. 2017;5 doi: 10.1177/2325967117745511. :232596711774551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Robinson C.M., Jenkins P.J., White T.O., Ker A., Will E. Primary arthroscopic stabilization for a first-time anterior dislocation of the shoulder: a randomized, Double-Blind trial. J Bone Joint Surg Am Vol. 2008;90:708–721. doi: 10.2106/JBJS.G.00679. [DOI] [PubMed] [Google Scholar]
- 20.Sherman W.F., Wu V.J., Ofa S.A., Ross B.J., Savage-Elliott I.D., Sanchez F.L. Increased rate of complications in myasthenia gravis patients following hip and knee arthroplasty: a nationwide database study in the PearlDiver Database on 257,707 patients. Acta Orthop. 2021;92:176–181. doi: 10.1080/17453674.2020.1865031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Streubel P.N., Krych A.J., Simone J.P., Dahm D.L., Sperling J.W., Steinmann S.P., et al. Anterior glenohumeral instability: a pathology-based surgical treatment strategy. J Am Acad Orthop Surg. 2014;22:283–294. doi: 10.5435/JAAOS-22-05-283. [DOI] [PubMed] [Google Scholar]
- 22.Thomazeau H., Courage O., Barth J., Pélégri C., Charousset C., Lespagnol F., et al. Can we improve the indication for Bankart arthroscopic repair? A preliminary clinical study using the ISIS score. Orthop Traumatol Surg Res OTSR. 2010;96:S77–S83. doi: 10.1016/j.otsr.2010.09.007. [DOI] [PubMed] [Google Scholar]
- 23.Uhorchak J.M., Arciero R.A., Huggard D., Taylor D.C. Recurrent shoulder instability after open reconstruction in athletes involved in collision and contact sports. Am J Sports Med. 2000;28:794–799. doi: 10.1177/03635465000280060501. [DOI] [PubMed] [Google Scholar]
- 24.Voos J.E., Livermore R.W., Feeley B.T., Altchek D.W., Williams R.J., Warren R.F., et al. Prospective evaluation of arthroscopic Bankart repairs for anterior instability. Am J Sports Med. 2010;38:302–307. doi: 10.1177/0363546509348049. [DOI] [PubMed] [Google Scholar]
- 25.Yamamoto N., Muraki T., An K.-N., Sperling J.W., Cofield R.H., Itoi E., et al. The stabilizing mechanism of the Latarjet procedure: a cadaveric study. J Bone Joint Surg Am. 2013;95:1390–1397. doi: 10.2106/JBJS.L.00777. [DOI] [PubMed] [Google Scholar]
- 26.Young A.A., Maia R., Berhouet J., Walch G. Open Latarjet procedure for management of bone loss in anterior instability of the glenohumeral joint. J Shoulder Elbow Surg. 2011;20:S61–S69. doi: 10.1016/j.jse.2010.07.022. [DOI] [PubMed] [Google Scholar]
- 27.Zacchilli M.A., Owens B.D. Epidemiology of shoulder dislocations presenting to Emergency Departments in the United States. J Bone Jt Surg Am Vol. 2010;92:542–549. doi: 10.2106/JBJS.I.00450. [DOI] [PubMed] [Google Scholar]
- 28.Zhang A.L., Montgomery S.R., Ngo S.S., Hame S.L., Wang J.C., Gamradt S.C. Analysis of rotator cuff repair trends in a large private insurance population. Arthrosc J Arthrosc Relat Surg. 2013;29:623–629. doi: 10.1016/j.arthro.2012.11.004. [DOI] [PubMed] [Google Scholar]
- 29.Zhang A.L., Montgomery S.R., Ngo S.S., Hame S.L., Wang J.C., Gamradt S.C. Arthroscopic versus open shoulder stabilization: current practice Patterns in the United States. Arthrosc J Arthrosc Relat Surg. 2014;30:436–443. doi: 10.1016/j.arthro.2013.12.013. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.