Abstract
Background
Degenerative arthritis is a major indication for both anatomic and reverse total shoulder arthroplasty (TSA). Degenerative arthritis is an age-related process that can be secondary to mechanical wear or inflammatory or autoimmune diseases, such as rheumatoid arthritis or systemic lupus erythematosus. Management of these diseases can include chronic corticosteroid for their anti-inflammatory and immunosuppressive effects. Given the well-known complications of chronic steroid use on other surgical procedures, investigation into postoperative complications specific to TSA will assist physicians in risk stratification and preoperative planning. The purpose of this study was to investigate the association between chronic preoperative steroid use and postoperative complications following TSA.
Methods
The American College of Surgeons National Surgical Quality Improvement database was queried for all patients who underwent TSA between 2015 and 2020. Patient demographics, comorbidities, surgical characteristics, and 30-day postoperative complication data were collected. Multivariate logistic regression was used to identify postoperative complications associated with chronic preoperative steroid use. Reasons and risk factors for readmission among chronic steroid users were subsequently identified, as well.
Results
A total of 26,669 patients were included in this study: 25,376 (95.2%) were included in the nonsteroid cohort and 1293 (4.8%) were included in the chronic steroid cohort. The postoperative complications that were significantly associated with chronic preoperative steroid use were septic shock (P = .007), urinary tract infection (P = .016), myocardial infarction (P = .022), ventilator >48 hours (P = .028), readmission (P < .001), nonhome discharge (P < .001), and mortality (P = .007). The only postoperative complication independently associated with chronic preoperative steroid use was readmission (odds ratio, 1.36; 95% confidence interval, 1.04-1.79; P = .027).
Conclusion
Preoperative chronic steroid use is an independent predictor for readmission following TSA. As procedural improvement increases surgical volume for TSA, a better understanding of preoperative risk factors can improve perioperative risk stratification and help to minimize adverse outcomes.
Keywords: Total shoulder arthroplasty, Reverse shoulder arthroplasty, Corticosteroids, Osteoarthritis, Readmission
Total shoulder arthroplasty (TSA) is an effective surgical treatment for degenerative diseases of the shoulder. Anatomic TSA provides favorable outcomes to patients with osteoarthritis or inflammatory arthropathy of the glenohumeral joint. Reverse TSA was initially introduced as an option for patients with rotator cuff tear arthropathy. However, indications for reverse TSA have since expanded to include degenerative glenohumeral arthritis, proximal humerus fractures, and revision surgery for failed open reduction and internal fixation.22 Procedural improvements in TSA have led to significant increases in surgical volume over the past two decades, with a concomitant decrease in the use of hemiarthroplasty.3 From 2011 to 2017, the volume of TSA performed each year went from 57,179 to 109,734.27 Additionally, rising life expectancy has allowed for a growing number of elderly patients to become candidates for TSA.20 The increased use of TSA in older patients, with a potentially higher incidence of chronic comorbidities, necessitates higher quality preoperative risk stratification to minimize adverse outcomes.
Degenerative arthritis is a major indication for both anatomic and reverse TSA. Degenerative arthritis is an age-related process that can be secondary to mechanical wear or inflammatory or autoimmune diseases, such as rheumatoid arthritis or systemic lupus erythematosus.25 Management of these diseases can include chronic corticosteroids for their anti-inflammatory and immunosuppressive effects.15 However, corticosteroid use is associated with delayed wound healing and increased rates of superficial and deep surgical site infections after surgery.14,28
In the realm of orthopedic surgery, the association between chronic steroid use and postoperative complications has been investigated for many common procedures such as spinal fusion, hip arthroplasty, and knee arthroplasty. For all three procedures, chronic preoperative steroid use has been found to be an independent risk factor for superficial and deep surgical site infections, wound dehiscence, urinary tract infection, pneumonia, and 30-day readmission.15,18 Reported investigations of chronic steroid use in conjunction with shoulder surgery are limited to studies of open and arthroscopic rotator cuff repairs and shoulder stabilization.1 To our knowledge, the effects of chronic steroid use on TSA has not been studied. Given the well-known complications of chronic steroid use on other surgical procedures, investigation into postoperative complications specific to TSA will assist physicians in risk stratification and preoperative planning.
The purpose of this study was to investigate the association between chronic preoperative steroid use and postoperative complications following TSA. We hypothesized that chronic steroid use is associated with higher rates of surgical site infection, wound dehiscence, and readmission following TSA.
Methods
The American College of Surgeons National Surgical Quality Improvement (NSQIP) database was queried for all patients who underwent TSA between 2015 and 2020. The NSQIP database is fully deidentified, therefore rendering this study exempt from approval by our University’s Institutional Review Board. Data in the NSQIP database are obtained from over 600 hospitals in the United States and is collected by trained surgical clinical reviewers. The data are periodically audited to maintain high fidelity.24
Current Procedural Terminology code 23472 was used to identify patients who underwent TSA, both anatomic and reverse, from 2015 to 2020. Cases for patients younger than 18 years of age or TSA performed for trauma were excluded. Cases were also excluded if any of the following variables had missing information: age, height, weight, functional status, smoking status, and perioperative steroid use.
Variables collected in this study included patient demographics, comorbidities, surgical characteristics, preoperative laboratory values, and 30-day postoperative complication data. Patient demographics included gender, body mass index, age, smoking status, functional status, American Society of Anesthesiologists (ASA) classification, and perioperative steroid use. Notable preoperative comorbidities included insulin-dependent and non-insulin–dependent diabetes, severe chronic obstructive pulmonary disease (COPD), congestive heart failure, acute renal failure, hypertension, recent unintentional weight loss, bleeding disorder, transfusion, previous sepsis, disseminated cancer, and open wound/wound infection. Both major and minor complications that occurred within 30 days postoperatively were included in the analysis. Major complications included cardiac arrest requiring cardiopulmonary resuscitation, myocardial infarction, deep vein thrombosis requiring therapy, cerebrovascular accident, stroke, unplanned intubation, pulmonary embolism, ventilator >48 hours, acute renal failure, sepsis, septic shock, reoperation, readmission, mortality, deep incisional surgical site infection (SSI), and organ/space SSI. Minor complications included progressive renal insufficiency, urinary tract infection, transfusions within 72 hours after surgery, pneumonia, and superficial incisional SSI. Reasons for readmission were collected and identified using the corresponding International Classification of Diseases, Ninth Revision (ICD-9) and International Classification of Diseases, Tenth Revision (ICD-10) codes.
The initial pool of patients was divided into two cohorts: chronic steroid and nonsteroid. The chronic steroid cohort consisted of patients who required regular administration of parenteral or oral corticosteroid medication and received such medication within the 30-day preoperative period. Patients who received short-term steroids over the span of 10 days or less during the 30-day preoperative period were not considered chronic steroid users and were thus allocated to the nonsteroid cohort. Additionally, patients who received corticosteroids dermally, rectally, or via inhalation were not considered steroid users and were also classified as nonsteroid users.
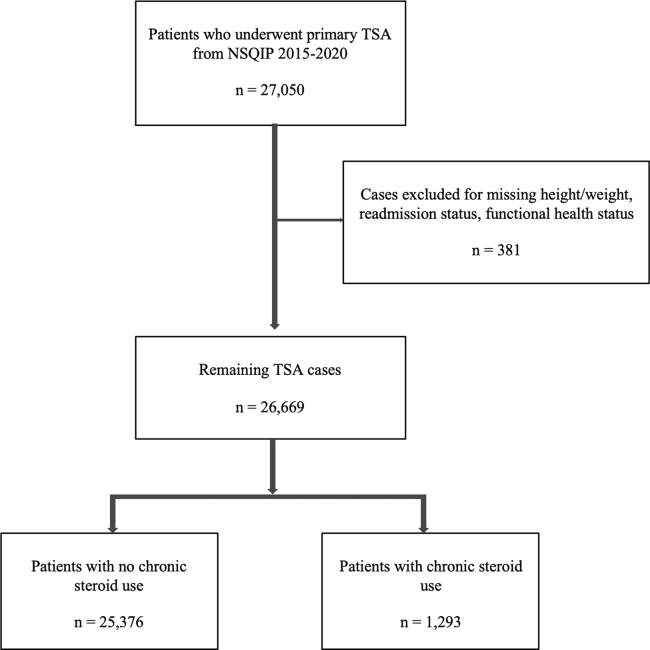
A total of 27,050 patients underwent primary TSA in NSQIP from 2015 to 2020. Cases were excluded as follows: 152 for missing height/weight, 2 for missing readmission status, 227 for missing functional health status prior to surgery. Of the 26,669 patients remaining after exclusion criteria, 25,376 (95.2%) patients were included in the nonsteroid cohort and 1293 (4.8%) patients were included in the chronic steroid cohort (Fig. 1).
Figure 1.
Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) diagram with inclusion and exclusion criteria. TSA, total shoulder arthroplasty; NSQIP, National Surgical Quality Improvement Program
All statistical analyses were conducted using SPSS Software version 26.0 (IBM Corp., Armonk, NY, USA). Patient demographics and comorbidities were compared between cohorts using bivariate analysis.
Multivariate logistic regression, adjusted for all significantly associated patient demographics and comorbidities, was used to identify associations between preoperative chronic steroid use and postoperative complications.
Multivariate logistic regression was also used to identify significant associations between patient variables of chronic steroid users and readmission. This was performed in the following manner: 1) patient demographics and comorbidities that were significantly associated with chronic steroid use were all initially included in the analysis, 2) variables were eliminated one by one in a stepwise fashion, with the highest P value being eliminated first, and 3) variables were eliminated until only statistically significant variables associated with readmission remained. Odds ratios (ORs) were reported with 95% confidence intervals (CIs). The level of statistical significance was set at P < .05.
Results
Patient demographics and comorbidities that were significantly associated with chronic steroid use were female gender (P < .001), dependent functional status (P < .001), ASA classification ≥3 (P < .001), COPD (P < .001), bleeding disorders (P < .0001), open wound/wound infection (P < .001), and disseminated cancer (P < .001) (Table I).
Table I.
Patient demographics/comorbidities for patients with and without chronic steroid use. Bold P-values indicate statistical significance with P < .05.
| Characteristic | Non steroid |
Chronic steroid |
P value | ||
|---|---|---|---|---|---|
| Number | Percent | Number | Percent | ||
| Total | 25,376 | 100.0 | 1293 | 100.0 | |
| Age | .133 | ||||
| 18-39 | 121 | 0.5 | 23 | 1.8 | |
| 40-64 | 6978 | 27.5 | 357 | 27.6 | |
| 65-74 | 10,591 | 41.7 | 552 | 42.7 | |
| ≥75 | 7686 | 30.3 | 361 | 27.9 | |
| Body mass index (kg/m2) | .188 | ||||
| <18.5 | 174 | 0.7 | 22 | 1.7 | |
| 18.5-29.9 | 12,057 | 47.5 | 670 | 51.8 | |
| 30-34.9 | 6806 | 26.8 | 311 | 24.1 | |
| 35-39.9 | 3638 | 14.3 | 158 | 12.2 | |
| ≥40 | 2701 | 10.6 | 132 | 10.2 | |
| Gender | <.001 | ||||
| Female | 13,975 | 55.1 | 879 | 68.0 | |
| Male | 11,401 | 44.9 | 414 | 32.0 | |
| Functional status prior to surgery | <.001 | ||||
| Independent | 24,859 | 98.0 | 1242 | 96.1 | |
| Dependent | 517 | 2.0 | 51 | 3.9 | |
| ASA classification | <.001 | ||||
| 1-2 | 10,982 | 43.3 | 315 | 24.4 | |
| ≥3 | 14,394 | 56.7 | 978 | 75.6 | |
| Smoker | .546 | ||||
| No | 22,757 | 89.7 | 1153 | 89.2 | |
| Yes | 2619 | 10.3 | 140 | 10.8 | |
| Diabetes mellitus | .234 | ||||
| No diabetes | 20,777 | 81.9 | 1071 | 82.8 | |
| Non-insulin dependent | 3281 | 12.9 | 148 | 11.4 | |
| Insulin dependent | 1318 | 5.2 | 74 | 5.7 | |
| Hypertension | .334 | ||||
| No | 8525 | 33.6 | 417 | 32.3 | |
| Yes | 16,851 | 66.4 | 876 | 67.7 | |
| COPD | <.001 | ||||
| No | 23,769 | 93.7 | 1126 | 87.1 | |
| Yes | 1607 | 6.3 | 167 | 12.9 | |
| Bleeding disorders | <.001 | ||||
| No | 24,768 | 97.6 | 1230 | 95.1 | |
| Yes | 608 | 2.4 | 63 | 4.9 | |
| Open wound/wound infection | <.001 | ||||
| No | 25,295 | 99.7 | 1278 | 98.8 | |
| Yes | 81 | 0.3 | 15 | 1.2 | |
| Disseminated cancer | <.001 | ||||
| No | 25,328 | 99.8 | 1279 | 98.9 | |
| Yes | 48 | 0.2 | 14 | 1.1 | |
| Acute renal failure | .449 | ||||
| No | 25,365 | 100.0 | 1292 | 99.9 | |
| Yes | 11 | 0.0 | 1 | 0.1 | |
ASA, American Society of Anesthesiologists; COPD, chronic obstructive pulmonary disease.
Bivariate analysis was used to determine postoperative complications associated with chronic preoperative steroid use vs nonsteroid use (Table II). The postoperative complications that were significantly associated with chronic preoperative steroid use were septic shock (P = .007), urinary tract infection (P = .016), myocardial infarction (P = .022), ventilator > 48 hours (P = .028), readmission (P < .001), nonhome discharge (P < .001), and mortality (P = .007).
Table II.
Bivariate analysis of 30-day postoperative complications in patients with and without chronic steroid use.
| Postoperative complication | Non steroid (n = 25,376) |
Chronic steroid (n = 1293) |
P value | ||
|---|---|---|---|---|---|
| Number | Percent | Number | Percent | ||
| Sepsis | 39 | 0.15 | 0 | 0.00 | .998 |
| Septic shock | 10 | 0.04 | 3 | 0.23 | .007 |
| Pneumonia | 119 | 0.47 | 9 | 0.70 | .252 |
| Reintubation | 49 | 0.19 | 2 | 0.15 | .919 |
| Urinary tract infection | 168 | 0.66 | 16 | 1.24 | .016 |
| Stroke | 21 | 0.08 | 1 | 0.08 | .947 |
| Cardiac arrest | 15 | 0.06 | 0 | 0.00 | .999 |
| Myocardial infarction | 66 | 0.26 | 7 | 0.54 | .022 |
| Bleeding transfusions | 442 | 1.74 | 32 | 2.47 | .053 |
| Deep vein thrombosis | 78 | 0.31 | 5 | 0.39 | .642 |
| Pulmonary embolism | 67 | 0.26 | 7 | 0.54 | .080 |
| Failure to wean off ventilator | 24 | 0.09 | 4 | 0.31 | .028 |
| Deep incisional SSI | 17 | 0.07 | 0 | 0.00 | .999 |
| Superficial incisional SSI | 63 | 0.25 | 6 | 0.46 | .143 |
| Organ/space SSI | 58 | 0.23 | 0 | 0.00 | .999 |
| Wound dehiscence | 17 | 0.07 | 0 | 0.00 | .999 |
| Readmission | 716 | 2.82 | 61 | 4.72 | <.001 |
| Reoperation | 349 | 1.38 | 21 | 1.62 | .456 |
| Nonhome discharge | 2106 | 8.30 | 155 | 11.99 | <.001 |
| Mortality | 36 | 0.14 | 6 | 0.46 | .007 |
Bold P-values indicate statistical significance with P < .05.
SSI, surgical site infection.
After adjusting for the patient variables significantly associated with chronic steroid use identified in paragraph 1 of our results, multivariate logistic regression identified readmission (OR 1.36; 95% CI, 1.04-1.79; P = .027) as the only postoperative complication independently associated with chronic preoperative steroid use. The other postoperative complications with significance in bivariate analysis were no longer significant after adjustment (Table III).
Table III.
Multivariate analysis of 30-day postoperative complications in patients with chronic steroid use, adjusted for significantly associated patient demographics/comorbidities.
| Postoperative complication | Odds ratio | 95% CI | P value |
|---|---|---|---|
| Septic shock | 3.65 | 0.94-14.14 | .061 |
| Urinary tract infection | 1.38 | 0.82-2.33 | .227 |
| Myocardial infarction | 1.80 | 0.87-3.76 | .116 |
| Failure to wean off ventilator | 2.43 | 0.82-7.22 | .111 |
| Readmission | 1.36 | 1.04-1.79 | .027 |
| Nonhome discharge | 1.03 | 0.85-1.23 | .786 |
| Mortality | 2.30 | 0.94-5.62 | .067 |
Bold P-values indicate statistical significance with P < .05.
CI, confidence interval.
Given the significant association between chronic steroid use and readmission following TSA, multivariate logistic regression was used to identify the patient variables of chronic steroid users associated with readmission (Table IV). After using a backward stepwise approach, the regression identified COPD (OR, 2.45, 95% CI 1.33-4.52; P = .004) and disseminated cancer (OR, 6.78; 95% CI, 1.83-25.19; P = .004) as significant predictors for readmission in chronic steroid users. As shown in Table II, 61 (4.72%) patients of the chronic steroid cohort were readmitted.
Table IV.
Significant predictors for 30-day readmission in patients prescribed steroids for a chronic condition.
| Characteristic | Odds ratio | 95% CI | P value |
|---|---|---|---|
| COPD | .004 | ||
| No | Reference | -- | |
| Yes | 2.45 | 1.33-4.52 | |
| Disseminated cancer | .004 | ||
| No | Reference | -- | |
| Yes | 6.78 | 1.83-25.19 |
CI, confidence interval; COPD, chronic obstructive pulmonary disease.
The reasons for readmission among the chronic steroid cohort are summarized in Table V. The most common reason for readmission among the chronic steroid cohort was pulmonary complication (n = 10), which accounted for 16% of readmissions. Pulmonary complications included pneumonia (n = 5), COPD with acute exacerbation (n = 2), acute respiratory failure with hypoxia (n = 2), and shortness of breath (n = 1). The second most common reason for readmission among the chronic steroid cohort was thromboembolic complication (n = 6). Thromboembolic complications included pulmonary embolism (n = 4), vein thrombosis requiring therapy (n = 1), and occlusion of vessel (n = 1). Among surgical site-related reasons for readmission, pain (n = 4) and dislocation of prosthesis (n = 3) were the most common.
Table V.
Reasons for 30-day readmission in patients with chronic steroid use after total shoulder arthroplasty.
| Reason | Number | Percent |
|---|---|---|
| Total | 61 | 100 |
| Nonsurgical site related | ||
| Pulmonary complications | 10 | 16 |
| Thromboembolic complications | 6 | 10 |
| Renal complications | 5 | 8 |
| Unrelated orthopedic complications | 5 | 8 |
| Bleeding complications | 4 | 7 |
| Cardiovascular complications | 3 | 5 |
| Gastrointestinal complications | 3 | 5 |
| Neurological complications | 2 | 3 |
| Septic shock | 2 | 3 |
| Metabolic complications | 2 | 3 |
| Infectious complications | 2 | 3 |
| Weakness | 2 | 3 |
| Rheumatoid arthritis | 1 | 2 |
| Hypotension | 1 | 2 |
| Surgical site related | ||
| Pain | 4 | 7 |
| Dislocation of prosthesis | 3 | 5 |
| Wound complications | 2 | 3 |
| Other complications/Unspecified | 4 | 7 |
Discussion
In this study, we reported on 30-day postoperative complications associated with chronic steroid use in patients who underwent TSA from 2015 to 2020 using a large national database. Our analysis included 26,669 patients, of which 1293 (4.8%) patients were prescribed steroids for a chronic condition. Through bivariate analysis, we identified chronic steroid use as a risk factor for septic shock, urinary tract infection, myocardial infarction, ventilator >48 hours, readmission, non-home discharge, and mortality. After controlling for significantly associated patient demographics and comorbidities, we identified chronic steroid use as an independent predictor for readmission following TSA. Among chronic steroid users, the clinically significant risk factors for readmission were COPD and disseminated cancer.
Corticosteroids are commonly used in the treatment of many inflammatory and autoimmune diseases due to their anti-inflammatory and immunosuppressive effects. In chronic inflammatory diseases, genes responsible for the expression of cyclooxygenase-2, nitric oxide synthase, and pro-inflammatory cytokines are activated.29 Steroids reduce inflammation by inhibiting these inflammatory genes through reversing histone acetylation.2 Additionally, steroids inhibit phospholipase A2 to ultimately decrease the production of inflammatory mediators such as prostaglandins and leukotrienes.10 These anti-inflammatory mechanisms allow steroids to be highly effective in the management of diseases such as rheumatoid arthritis and systemic lupus erythematous.7,13
Despite the effectiveness of corticosteroids, long-term corticosteroid use has an extensive profile of adverse effects. Common adverse effects include infection, osteoporosis, aseptic necrosis, weight gain, and diabetes.6,21 With respect to surgery, long-term steroid use has been associated with poor wound healing and worse long-term outcomes.14
TSA is an effective and increasingly popular surgical treatment for degenerative diseases of the shoulder. Indications for TSA include osteoarthritis, inflammatory arthropathy, rotator cuff arthropathy, and proximal humerus fractures.22 The incidence of TSA has substantially increased in recent years, with the greatest increase being in reverse TSA. From 2012 to 2017, the incidence of reverse TSA in the United States increased from 22,835 to 62,705 procedures, representing almost a three-fold increase.3 As the surgical volume of TSA continues to increase, preoperative risk stratification is increasingly valuable to minimizing adverse outcomes.
Chronic steroid use is an important patient characteristic to consider during the preoperative planning for TSA. As previously mentioned, steroids are commonly used to treat rheumatoid arthritis, which can predispose patients to developing secondary osteoarthritis due to avascular necrosis.11 Additionally, the adverse effects of chronic steroid use, such as weight gain and diabetes, can also lead to secondary osteoarthritis or progression of pre-existing degenerative joint disease.19 Finally, patients with steroid-induced osteoporosis may also be predisposed to require TSA, as proximal humerus fractures are a common site for osteoporotic fractures.26
In the realm of orthopedic surgery, significant associations between chronic steroid use and postoperative complications have been investigated for hip arthroplasty, knee arthroplasty, and spinal fusion. A study by Kittle et al found that patients with chronic steroid use undergoing total hip or knee arthroplasty were at increased risk for surgical site infections, wound dehiscence, wound infection, pneumonia, reintubation, urinary tract infection, and readmission.15 Another study that focused specifically on patients with chronic steroid use undergoing total hip arthroplasty found that these patients were at increased risk of urinary tract infection, surgical site infection, readmission, and sepsis.4 In cases of posterior lumbar fusion, patients with chronic steroid use were identified to be at increased risk of surgical site infections, wound dehiscence, urinary tract infection, pulmonary embolism, nonhome discharge, and readmission.18 The postoperative complications associated with chronic steroid use that were consistent across all three studies were surgical site infections, urinary tract infection, and readmission.
Other reports have investigated the association between arthroplasty in patients with chronic inflammatory diseases including rheumatoid arthritis, systemic lupus erythematous, and juvenile idiopathic arthritis. These reports found that patients with chronic inflammatory disease were at higher risk of periprosthetic joint infection, sepsis, genitourinary complication, bleeding complication, reduced long-term implant survival, increased length of stay, non-home discharge, and death.5,9,12,17
More specific to shoulder surgery, a study by Aziz et al investigated the associations of chronic steroid use in shoulder stabilization and arthroscopic and open rotator cuff repair. This study found that patients with chronic steroid use had increased odds of minor, major, and infection complications following shoulder surgery.1
Our study identified chronic steroid use to be a significant risk factor for septic shock, urinary tract infection, myocardial infarction, ventilator dependence, readmission, nonhome discharge, and mortality following TSA. The increased risks for urinary tract infection and readmission associated with steroid use are consistent with the aforementioned studies regarding hip and knee arthroplasty.4,15 However, our study did not find steroid use to be a significant risk factor for surgical site infections, as reported in those studies. Similar to the various studies investigating arthroplasty in patients with chronic inflammatory disease, the significant postoperative complications also identified in our study were nonhome discharge and mortality.5,9,12,17
Our study also identified chronic steroid use to be an independent predictor for readmission following TSA. We further identified that among patients with chronic steroid use, those with COPD and disseminated cancer had an even higher risk for 30-day readmission following TSA. There have been no prior studies that investigated patient risk factors associated with readmission in patients with chronic steroid use undergoing TSA. Among the patients in our study with chronic steroid use, most of the readmissions were due to nonsurgical reasons. Pulmonary complications were the most common reasons overall for readmission in this cohort. The most common surgical site-related reason for readmission in this cohort was pain. These results differ from a study investigating overall readmission rates after primary TSA, which identified osteoarthritis and infection as the most common nonsurgical and surgical site-related reasons for readmission, respectively.23 This suggests that patients with chronic steroid use are readmitted for different reasons from the overall patient population receiving TSA.
The findings of our study should not be used to discourage the use of TSA in patients with chronic steroid use. Rather, they suggest that patients with chronic steroid use may require more extensive preoperative planning. Given that chronic steroid use is a significant risk factor for myocardial infarction and ventilator dependence, patients with preexisting cardiac and pulmonary diseases may necessitate further preoperative testing. In particular, pulmonary testing may be important because pulmonary complication is the most likely cause for readmission in chronic steroid users. More specifically, pneumonia and pulmonary embolism were the most common reasons for readmission in chronic steroid users. Additionally, chronic steroid users with COPD are at greatly increased risk for readmission.
Patients can also be counseled on their chronic steroid use as being risk factors for readmission and nonhome discharge. In terms of readmission, surgeons and hospitals have a financial incentive to limit the number of readmissions following arthroplasty. The Patient Protection and Affordable Care Act of 2010 contains provisions that preclude payment of hospital costs associated with readmission within 30 days of discharge following joint arthroplasty.16 A study analyzing costs associated with TSA found that readmitted patients incurred hospital costs of $82,348, compared to $16,621 for nonreadmitted patients.8
Our study was limited to the information available on the NSQIP database. Due to inherent characteristics of the database, we could not account for operative variables such as experience of the surgeon, institution where the procedure was performed, and postoperative rehabilitation. Additionally, postoperative complications in NSQIP are only considered within a 30-day postoperative period. Therefore, we were unable to account for long-term complications following TSA, such as instability, loosening, and periprosthetic fracture. NSQIP also does not distinguish between anatomic and reverse TSA. Although we found pulmonary embolism to be a common reason for readmission, we were unable to account for differences in deep vein thrombosis prophylaxis between cohorts. Finally, the disease process for which chronic steroids were prescribed was not a variable available in the database. Regardless of these limitations, we used a large national database to investigate postoperative complications associated with chronic preoperative steroid use in patients undergoing TSA. Moreover, this is the first study to investigate the association of significant patient comorbidities associated with chronic steroid use and readmission in patients undergoing TSA.
Conclusion
Preoperative chronic steroid use is an independent predictor for readmission following TSA. Among chronic steroid users, COPD and disseminated cancer are significant risk factors for readmission following TSA, with pneumonia and pulmonary embolism being the most common reasons for readmission. Chronic steroid use is also significantly associated with septic shock, urinary tract infection, myocardial infarction, ventilator >48 hours, nonhome discharge, and mortality following TSA. As procedural improvement increases surgical volume for TSA, a better understanding of preoperative risk factors can improve perioperative risk stratification and help to minimize adverse outcomes.
Disclaimers
Funding: No funding was disclosed by the authors.
Conflicts of interest: The authors, their immediate families, and any research foundation with which they are affiliated have not received any financial payments or other benefits from any commercial entity related to the subject of this article.
Footnotes
Institutional review board approval was not required for this study.
References
- 1.Aziz K.T., Best M.J., Ren M., Nayar S.K., Timothy Kreulen R., Gupta H.O., et al. The impact of chronic steroid use on early postoperative complications in shoulder surgery. Phys Sportsmed. 2021;49:223–228. doi: 10.1080/00913847.2020.1811616. [DOI] [PubMed] [Google Scholar]
- 2.Barnes P.J. How corticosteroids control inflammation: quintiles prize Lecture 2005. Br J Pharmacol. 2006;148:245–254. doi: 10.1038/sj.bjp.0706736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Best M.J., Aziz K.T., Wilckens J.H., McFarland E.G., Srikumaran U. Increasing incidence of primary reverse and anatomic total shoulder arthroplasty in the United States. J Shoulder Elbow Surg. 2021;30:1159–1166. doi: 10.1016/j.jse.2020.08.010. [DOI] [PubMed] [Google Scholar]
- 4.Boddapati V., Fu M.C., Su E.P., Sculco P.K., Bini S.A., Mayman D.J. Preoperative corticosteroid use for medical conditions is associated with increased postoperative infectious complications and readmissions after total hip arthroplasty: a Propensity-Matched study. Am J Orthop (Belle Mead NJ) 2018;47 doi: 10.12788/ajo.2018.0104. [DOI] [PubMed] [Google Scholar]
- 5.Bongartz T., Halligan C.S., Osmon D.R., Reinalda M.S., Bamlet W.R., Crowson C.S., et al. Incidence and risk factors of prosthetic joint infection after total hip or knee replacement in patients with rheumatoid arthritis. Arthritis Rheum. 2008;59:1713–1720. doi: 10.1002/art.24060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Buchman A.L. Side effects of corticosteroid therapy. J Clin Gastroenterol. 2001;33:289–294. doi: 10.1097/00004836-200110000-00006. [DOI] [PubMed] [Google Scholar]
- 7.Chatham W.W., Kimberly R.P. Treatment of lupus with corticosteroids. Lupus. 2001;10:140–147. doi: 10.1191/096120301675075008. [DOI] [PubMed] [Google Scholar]
- 8.Chung A.S., Makovicka J.L., Hydrick T., Scott K.L., Arvind V., Hattrup S.J. Analysis of 90-day readmissions after total shoulder arthroplasty. Orthop J Sports Med. 2019;7 doi: 10.1177/2325967119868964. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Cordtz R.L., Zobbe K., Højgaard P., Kristensen L.E., Overgaard S., Odgaard A., et al. Predictors of revision, prosthetic joint infection and mortality following total hip or total knee arthroplasty in patients with rheumatoid arthritis: a nationwide cohort study using Danish healthcare registers. Ann Rheum Dis. 2018;77:281–288. doi: 10.1136/annrheumdis-2017-212339. [DOI] [PubMed] [Google Scholar]
- 10.Ericson-Neilsen W., Kaye A.D. Steroids: pharmacology, complications, and practice delivery issues. Ochsner J. 2014;14:203–207. [PMC free article] [PubMed] [Google Scholar]
- 11.Figueiredo C.P., Simon D., Englbrecht M., Haschka J., Kleyer A., Bayat S., et al. Quantification and impact of secondary osteoarthritis in patients with anti-Citrullinated Protein Antibody-Positive rheumatoid arthritis. Arthritis Rheumatol. 2016;68:2114–2121. doi: 10.1002/art.39698. [DOI] [PubMed] [Google Scholar]
- 12.Gholson J.J., Wilkinson B.G., Brown T.S., Gao Y., Dowdle S.B., Callaghan J.J. Systemic lupus erythematosus is a risk factor for complications in total joint arthroplasty. Iowa Orthop J. 2018;38:183–190. [PMC free article] [PubMed] [Google Scholar]
- 13.Hua C., Buttgereit F., Combe B. Glucocorticoids in rheumatoid arthritis: current status and future studies. RMD Open. 2020;6:e000536. doi: 10.1136/rmdopen-2017-000536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ismael H., Horst M., Farooq M., Jordon J., Patton J.H., Rubinfeld I.S. Adverse effects of preoperative steroid use on surgical outcomes. Am J Surg. 2011;201:305–308. doi: 10.1016/j.amjsurg.2010.09.018. [discussion 308-9] [DOI] [PubMed] [Google Scholar]
- 15.Kittle H., Ormseth A., Patetta M.J., Sood A., Gonzalez M.H. Chronic corticosteroid use as a risk factor for perioperative complications in patients undergoing total joint arthroplasty. J Am Acad Orthop Surg Glob Res Rev. 2020;4:e20.00001. doi: 10.5435/JAAOSGlobal-D-20-00001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Mahoney A., Bosco J.A., 3rd, Zuckerman J.D. Readmission after shoulder arthroplasty. J Shoulder Elbow Surg. 2014;23:377–381. doi: 10.1016/j.jse.2013.08.007. [DOI] [PubMed] [Google Scholar]
- 17.Malviya A., Walker L.C., Avery P., Osborne S., Weir D.J., Foster H.E., et al. The long-term outcome of hip replacement in adults with juvenile idiopathic arthritis: the influence of steroids and methotrexate. J Bone Joint Surg Br. 2011;93:443–448. doi: 10.1302/0301-620x.93b4.26078. [DOI] [PubMed] [Google Scholar]
- 18.Ranson W.A., White S.J.W., Cheung Z.B., Mikhail C., Ye I., Kim J.S., et al. The effects of chronic preoperative steroid therapy on perioperative complications following elective posterior lumbar fusion. Glob Spine J. 2018;8:834–841. doi: 10.1177/2192568218775960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Rechardt M., Shiri R., Karppinen J., Jula A., Heliövaara M., Viikari-Juntura E. Lifestyle and metabolic factors in relation to shoulder pain and rotator cuff tendinitis: a population-based study. BMC Musculoskelet Disord. 2010;11:165. doi: 10.1186/1471-2474-11-165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ricchetti E.T., Abboud J.A., Kuntz A.F., Ramsey M.L., Glaser D.L., Williams G.R., Jr. Total shoulder arthroplasty in older patients: increased perioperative morbidity? Clin Orthop Relat Res. 2011;469:1042–1049. doi: 10.1007/s11999-010-1582-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Rice J.B., White A.G., Scarpati L.M., Wan G., Nelson W.W. Long-term systemic corticosteroid Exposure: a Systematic Literature review. Clin Ther. 2017;39:2216–2229. doi: 10.1016/j.clinthera.2017.09.011. [DOI] [PubMed] [Google Scholar]
- 22.Sanchez-Sotelo J. Total shoulder arthroplasty. Open Orthopaedics J. 2011;5:106–114. doi: 10.2174/1874325001105010106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Schairer W.W., Zhang A.L., Feeley B.T. Hospital readmissions after primary shoulder arthroplasty. J Shoulder Elbow Surg. 2014;23:1349–1355. doi: 10.1016/j.jse.2013.12.004. [DOI] [PubMed] [Google Scholar]
- 24.Sebastian A.S., Polites S.F., Glasgow A.E., Habermann E.B., Cima R.R., Kakar S. Current quality measurement tools are insufficient to assess complications in orthopedic surgery. J Hand Surg Am. 2017;42:10–15.e1. doi: 10.1016/j.jhsa.2016.09.014. [DOI] [PubMed] [Google Scholar]
- 25.Shane Anderson A., Loeser R.F. Why is osteoarthritis an age-related disease? Best Pract Res Clin Rheumatol. 2010;24:15–26. doi: 10.1016/j.berh.2009.08.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Taskesen A., Göçer A., Uzel K., Yaradılmış Y.U. Effect of osteoporosis on proximal humerus fractures. Geriatr Orthop Surg Rehabil. 2020;11 doi: 10.1177/2151459320985399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Wagner E.R., Farley K.X., Higgins I., Wilson J.M., Daly C.A., Gottschalk M.B. The incidence of shoulder arthroplasty: rise and future projections compared with hip and knee arthroplasty. J Shoulder Elbow Surg. 2020;29:2601–2609. doi: 10.1016/j.jse.2020.03.049. [DOI] [PubMed] [Google Scholar]
- 28.Wang A.S., Armstrong E.J., Armstrong A.W. Corticosteroids and wound healing: clinical considerations in the perioperative period. Am J Surg. 2013;206:410–417. doi: 10.1016/j.amjsurg.2012.11.018. [DOI] [PubMed] [Google Scholar]
- 29.Williams D.M. Clinical pharmacology of corticosteroids. Respir Care. 2018;63:655–670. doi: 10.4187/respcare.06314. [DOI] [PubMed] [Google Scholar]