Objectives
The present study applied the Integrated Behavior Change Model to investigate how behavioral decisions are predicted, namely, intention, planning, and habits, with respect to physical activity. Methods: Participants were older adults (ages 65+) residing in the U.S. (N = 667) who completed online measures of behavioral determinants (autonomous motivation, perceived behavioral control, subjective norms, attitudes, intention, habit, and consistency), in addition to past behavior. Results: A structural equation model revealed that intention was predicted by past behavior and social-cognitive determinants. Social cognitive determinants mediated between past behavior and habit, as well as between autonomous motivation and habit. Intention mediated between past behavior and planning. Discussion: This study highlights the importance of multiple processes (social cognitive, habit/automatic, and post-intentional/planning) that formulate physical activity intentions. Mediation pathways revealed the importance of autonomous motivation for establishing intentions and habit. Facilitating these processes among older adults could be effective for promoting physical activity.
Keywords: habit, integrated behavior change model, older adults, physical activity
Introduction
Engaging in regular physical activity has been shown to reduce the risk of developing common chronic conditions and disease among older adults, such as cognitive decline, major mobility disability, and osteoporosis (Barnes et al., 2003; McMillan et al., 2017; Pahor et al., 2014). Further, participating in regular physical activity in middle age or older adulthood is associated with improvements in physical and cognitive health (Falck et al., 2019; Lautenschlager et al., 2008; Sabia et al., 2012). Despite the documented benefits and awareness of these benefits among older adults (Goggin & Morrow, 2001), physical activity participation has been shown to decline with age (Hallal et al., 2012). This is a great concern given that older adults are being recognized as the fastest growing age group globally (United Nations, Department of Economic and Social Affairs, Population Division, 2019). Older adults may encounter unique challenges in the uptake of physical activity and its maintenance such as changes to mobility and functioning, fear of injury or pain, and the complexity of program contents (Chase, 2013; Fleig et al., 2016). Thus, identifying decisional determinants (i.e., individual and environmental factors that influence the decision to adopt a behavior) of physical activity is critical to successfully promote this behavior among this demographic.
Theoretical Approaches to Physical Activity Behavior
A variety of theoretical models and concepts have been utilized to explain the adoption of health behaviors such as physical activity (de Vries et al., 2018). Nonetheless, interventions focused on promoting physical activity in older adults vary considerably in their use of theoretical models (Stolte et al., 2017; Webb et al., 2010), and the proposed relationships between theoretical components and behavioral outcomes are often inadequately described (Chase, 2015; Senkowski et al., 2019). In studies that have applied theoretical frameworks to the topic, primarily social-cognitive models have been used to describe physical activity (e.g., the Theory of Planned Behavior; Ajzen, 1991) (Gourlan et al., 2016; McEwan et al., 2019; White et al., 2012). These studies were formative in identifying relevant social-cognitive predictors of physical activity; however, the application of theories specifically developed for physical activity may be more suitable to better understand the mechanisms behind this behavior. Currently, the multitude of determinants of behavior (change) is reduced to a limited number of theoretical elements (de Vries, 2017). Thus, the integration and critical testing of further decisional predictors of physical activity, such as automatic and self-regulatory skills (e.g., habit formation and planning), may allow for a more accurate depiction of the relation and interplay of variables (e.g., psychosocial factors, automatic processes, and motivational factors) (de Vries, 2017). To describe and study complex health behaviors (such as physical activity), the use and integration of multiple theoretical frameworks can increase the predictive validity (Kosma et al., 2006). Such a multi-theoretical approach can in turn support the development of tailored programs to encourage older adults with various degrees of physical activity engagement (Grodesky et al., 2006). A contemporary model that integrates hypotheses from various theories is the Integrated Behavior Change Model (IBC; Hagger & Chatzisarantis, 2014).
The Integrated Behavior Change Model
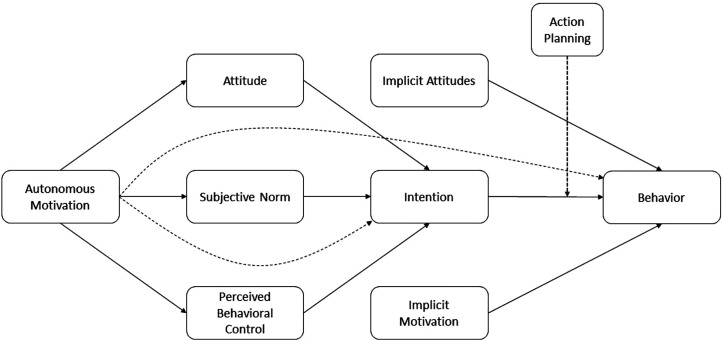
The IBC was designed to understand physical activity behavior by including evidence from reviews and meta-analyses (Chatzisarantis & Hagger, 2009; Hagger & Chatzisarantis, 2009; Sniehotta et al., 2005). As displayed in Figure 1, the model carries forward relevant social-cognitive constructs identified from the Theory of Planned Behavior (TPB; Ajzen, 1991), action planning theories (Hagger & Luszczynska, 2014), Self-Determination Theory (Deci & Ryan, 1985), in addition to non-conscious (Strack & Deutsch, 2004; Zhang et al., 2019) and post-intention processes such as planning (Schwarzer & Luszczynska, 2008). Predictive validity for the IBC model has previously been demonstrated (Hagger et al., 2017; Hamilton et al., 2017; Kaushal, Keith, et al., 2020). Based on the TPB, the IBC includes beliefs-based constructs about the participation in the respective health behavior, including attitudes toward the target behavior (i.e., perceived advantages and disadvantages of engaging in the behavior), perceived behavioral control (PBC), and subjective norms (Hagger et al., 2019). While subjective norms describe beliefs about the influence of a person’s social environment, PBC regards beliefs of personal capacities to engage in the respective behavior. According to the TPB, these belief constructs predict intention, which is considered the most proximal predictor of behavior (Hagger et al., 2019). The IBC model also includes autonomous motivation (Deci & Ryan, 2008) as the core pillar that facilitates the development of conscious motivational processes. Autonomous motivation refers to the degree to which individuals perceive that their actions stem from free choice and reflect their true self. In the IBC, autonomous motivation is theorized to predict attitudes, PBC, and subjective norms (Hagger et al., 2006). Further, autonomous motivation is proposed to predict intention via total indirect effects of determinants of intention as supported by findings in a meta-analysis (Hagger & Chatzisarantis, 2009). In light of the complexity of physical activity behavior (Nelson et al., 2007), the necessity of planning for translating intention into behavior has been well documented (Bélanger-Gravel et al., 2013; Carraro & Gaudreau, 2013; Norman et al., 2019; Pfeffer & Strobach, 2019).
Figure 1.
Schematic of the Integrated Behavior Change (IBC) model for physical activity, following Hagger & Chatzisarantis, 2014.
Finally, the IBC model accounts for automatic processes, which have been acknowledged as relevant determinants for predicting health behaviors such as physical activity (Gardner, 2015; Rebar et al., 2016). In the context of physical activity, habit has been shown to demonstrate validity for predicting behavior (Gardner et al., 2012; Hagger, 2019). Habit is defined as an automatic component that is established from repeatedly associating context with behavior, which eventually allows behavior to become cued or guided from associated contexts (Gardner et al., 2012; Wood & Rünger, 2016). An antecedent of physical activity habit is consistency (Kaushal et al., 2017; Kaushal & Rhodes, 2015). The familiarity of the context allows a portion of the behavior to be carried out automatically, while the behavior is still guided by conscious intention. This functionality is recognized as a dual process approach (Evans, 2008). As such, habit is an additional psychological variable with distinct characteristics from past behavioral frequency (van Bree et al., 2015). Whereas the role of habits in physical activity has been recognized across general population samples, its examination among older adults is limited (Rebar et al., 2016). This is problematic, because sustained activity is known to benefit cognitive and physical functioning (Denkinger et al., 2012; de Vries et al., 2012). Habits that promote a physically active lifestyle are desired in this target group as they may ease behavioral performance by lowering demands on cognitive resources (e.g., memory and attention; Danner et al., 2007; Fleig et al., 2016; Wood & Rünger, 2016).
Emerging evidence supports the importance of habit strength in older adults. For example, Peng et al. (2021) reported that long-term users of activity trackers aged 65+ used consistent temporal, locational, and contextual cues to facilitate habitual tracker use. Similarly, findings from a feasibility study for encouraging older adults to embed activities into daily life suggest the importance of activity and object-based cues for establishing action and behavioral automaticity (Fleig et al., 2016). Past research has also found habits to mediate between prior and later physical activity behavior within the frameworks of theoretical models for behavior change (Kaushal, Preissner, et al., 2020; van Bree et al., 2015). This construct may thus be valuable for physical activity promotion among older adults (van Bree et al., 2015). The IBC incorporates the dual process approach by placing habit as a proximal predictor of behavior, parallel to intention.
The Present Study
The present study aimed to examine the role of belief-based and automaticity-related variables in the prediction of older adults’ intention to engage in physical activity using the IBC model. Our extended model includes non-conscious decision-making (habit) and its antecedent (consistency). In alignment with the TPB, we first hypothesized that intention would be predicted by attitudes, PBC, and subjective norms (H1). Secondly, we expected that TPB constructs (attitudes, subjective norms, and PBC) would mediate the relationship between autonomous motivation and intention (H2). Because past behavior may affect decision making and model habitual effects (Hagger, 2019), we included previous engagement in physical activity as a predictor in the present model. We expected social-cognitive constructs to mediate between past physical activity behavior and intention (H3). Further, in light of findings that support the importance of planning for engaging in physical activity, we also expected that past intention and behavior would predict the planning of future subsequent behavior (H4). To investigate the role of automaticity, we hypothesized that the degree of habit formation would be predicted by consistency, past behavior, and the aforementioned social-cognitive constructs (H5).
Methods
In the following, a summary of the study methodology relevant for the present aims and hypotheses is provided. The full study methodology has been previously described (Kaushal, Preissner, et al., 2020).
Study Design and Setting
Older adults were recruited through the online research platform Prime Panels (CloudResearch, formerly TurkPrime) that enables researchers to sample individuals according to specific characteristics (Chandler et al., 2019; Davidai, 2018). For the present study, individuals were recruited solely based on their age group. Currently, 75% of adults aged 65+ are suggested to use the Internet (Perrin & Atske, 2021), with differences in demographic characteristics and health-related knowledge between users and non-users (Arcury et al., 2020). Though concerns prevail about the demographic representativeness of older adult samples obtained via online crowdsourcing (Follmer et al., 2017; McRobert et al., 2018), it is unclear whether the potential sampling bias also extends to behavioral outcomes (Ogletree & Katz, 2021). For the present research, we chose online crowdsourcing to recruit a large sample of older adults with varying degrees of automaticity in their physical activity.
Participants
Participants were older adults (M = 70.36, SD = 4.70, range = 65–92 years, females: 56.7%) living in the United States. Individuals were mostly retired, Caucasian, and had attained a bachelor’s degree. Table 1 provides a detailed overview of the demographic characteristics of the sample. In addition to being over the age of 65, participants were required to have proficiency in English as well as basic computer literacy to answer the survey. Participants provided informed consent and were redirected to the online questionnaire. To ensure a high data quality, we excluded responses associated with non-U.S. Internet protocol (IP) addresses, improbable reading or completion speed, and individuals who provided non-matching basic demographic data on an implemented control item. In total, 667 met the criteria for inclusion.
Table 1.
Summary of Respondents’ (N = 667) Sociodemographic Characteristics.
| Variable | Total Sample (N = 667) |
|---|---|
| Age | |
| Min–Max | 65–92 |
| Mean ± SD | 70.36 ± 4.70 |
| Gender (n, %) | |
| Male | 281 (42.2) |
| Female | 378 (56.7) |
| Other | 8 (1.1) |
| Ethnicity (n, %) | |
| Caucasian | 596 (89.4) |
| Black | 41 (6.1) |
| Asian | 8 (1.2) |
| Hispanic | 9 (1.3) |
| First Nations | 2 (0.3) |
| Mixed | 7 (1.0) |
| Other | 4 (0.5) |
| Weight (lbs.) | |
| N (N missing) | 658 (9) |
| Min–Max | 77–428 |
| Mean ± SD | 182.64 ± 45.73 |
| BMI | |
| N (N missing) | 653 (14) |
| Min–Max | 16.06–60.55 |
| Mean ± SD | 28.91 ± 6.46 |
| Household income (n, %) | |
| 35,000 or less | 255 (38.2) |
| 35,001–50,000 | 129 (19.3) |
| 50,001–75,000 | 143 (21.4) |
| 75,001–100,000 | 58 (8.7) |
| 100,001–150,000 | 56 (8.4) |
| 150,001–200,000 | 14 (2.1) |
| More than 200,000 | 9 (1.3) |
| Missing | 3 (0.4) |
| Marital status (n, %) | |
| Never married | 82 (12.3) |
| Married/common law marriage | 334 (50.1) |
| Separated/divorced/widowed | 244 (36.6) |
| Missing | 7 (1.0) |
| Occupation (n, %) | |
| Full-time employment | 45 (5.4) |
| Part-time employment | 57 (8.4) |
| Unemployed | 13 (3.0) |
| Retired | 528 (81.3) |
| Other | 24 (3.5) |
| Education (n, %) | |
| Less than high school | 2 (0.3) |
| High school diploma | 155 (23.2) |
| Bachelor’s or college degree | 413 (61.9) |
| Masters’ degree | 82 (12.3) |
| Obtained a PhD | 13 (1.9) |
| Missing | 2 (0.3) |
Measures
The following measures were used to assess the constructs of interest and control variables in this study. Prior to answering to physical activity-related items, participants were provided with a definition of what is defined as regular physical activity (in line with Nelson et al., 2007). Descriptive information for all relevant variables can be found in Tables 1 and 2.
Table 2.
Means, Ranges (Minimum, Maximum), Cronbach’s Alphas, and Standard Deviations (SD) of Variables Included in the Structural Equation Model for N = 667.
| Variables | Means (SD) | Minimum | Maximum | Internal Consistencies (Cronbach’s Alpha) |
|---|---|---|---|---|
| Attitude | 5.30 (1.29) | 1 | 7 | .89 |
| Consistency | 3.23 (1.32) | 1 | 5 | .91 |
| Habit | 3.20 (1.13) | 1 | 5 | .93 |
| Intention | 5.08 (1.78) | 1 | 7 | .98 |
| Perceived behavioral control | 5.73 (1.51) | 1 | 7 | .81 |
| Planning | 3.11 (1.10) | 1 | 5 | .87 |
| Physical activity behavior | 128.00 (73.69) | 0 | 511 | - |
| Subjective norm | 4.85 (1.39) | 1 | 7 | .69 |
| Autonomous motivation | 5.84 (4.39) | −4.25 | 18 | .72 (external), .69 (introjected), .95 (identified), and .88 (intrinsic) |
Note. Dashes signify “not applicable.”
Demographics
Demographic information collected included age, gender, ethnicity, height, weight, marital status, annual household income, level of education, and employment status.
Intention
Intention to engage in physical activity was measured using a scale developed in line with Ajzen (2002) and Arnautovska et al. (2017). Three items were scored on a 7-point Likert-type scale, ranging from 1 (strongly disagree) to 7 (strongly agree).
Habit strength
Habit strength within the context of physical activity was assessed using the four-item Self-Report Habit Index (SRHI; Gardner et al., 2012). The measure indicates the perceived extent to which physical activity is experienced as automatic and performed without thought. Answers are scored on a 5-point Likert-type scale from 1 (totally disagree) to 5 (totally agree). The SRHI has previously been used to assess habit strength in older adults (van Bree et al., 2017).
Planning
Planning for physical activity was assessed using a multi-item measure in line with Sniehotta et al. (2005). Three items assessed whether participants made specific plans for when and where to be physically active, and whether they set short-term goals for their activity behavior. Items were scored on a 5-point Likert-type scale ranging from 1 (strongly disagree) to 5 (strongly agree).
Consistency
Consistency in physical activity was assessed using a multi-item scale in line with Kaushal and Rhodes (2015) and Kaushal et al. (2017). Three items measured the perceived consistency in location, time and performance consistency using a 5-point Likert-type scale from 1 (not consistently) to 5 (very consistently).
Social cognition constructs
Attitude, subjective norms, and PBC regarding physical activity were assessed using multi-item measures developed in line with prior recommendations (Ajzen, 2002; Armitage et al., 1999; Fishbein & Ajzen, 1980; Rhodes et al., 2006). All items were scored using a 7-point Likert-type rating scale. Attitude was measured by six items, asking participants to indicate how, for example, enjoyable/unenjoyable or beneficial/harmful they perceived moderate physical activity over the next week to be. Injunctive and descriptive components of subjective norms were assessed using four items, assessing whether participants perceived important individuals in their social environment to want them to engage in physical activity and whether they will also engage in the behavior. PBC was measured using three items, asking individuals to rate the extent to which they believed themselves to have control over regular physical exercise.
Motivation
Self-regulatory styles regarding physical activity were assessed using the Self-Regulation Questionnaire (Ryan & Connell, 1989). Each of the four motivational regulation styles from the Self-Determination Theory were addressed by four specific subscales made up of four items within the overall 16-item scale: external regulation, intrinsic or internal regulation, introjected regulation, and identified regulation. Participants’ responses on these subscales were scored according to the Relative Autonomy Index (RAI) formula to form a total score of relative autonomous motivation (Nurmi et al., 2016), with higher and positive scores indicating greater relative autonomous motivation, while negative scores indicated less relative autonomous motivation. The Self-Regulation Questionnaire for physical activity has previously demonstrated adequate construct validity in a study by Nurmi et al. (2016).
Physical activity behavior
Physical activity behavior was assessed using the Physical Activity Scale for the Elderly (PASE; Washburn et al., 1993). The PASE is composed of questions about household activities, recreational activities, and occupational or work-related activities. Response options correspond to weekly frequencies (never, 1–2 days, 3–4 days, and 5–7 days) and daily frequencies (less than 1 hr, 1 but less than 2 hr, 2–4 hr, and more than 4 hr). Based on the PASE scoring manual (Washburn et al., 1993), frequencies were multiplied by a weight specific to the type of physical activity. Responses from activity type were added to form a total PASE score, with higher scores indicating greater levels of physical activity.
Health status
The Medical Outcome Study (MOS) 12-item Short Form Health Survey (SF-12 version 1) was used to measure physical and mental health status among participants. This questionnaire presents participants with questions about their general health, how their physical or mental health interferes with their work or other daily activities as well as questions regarding bodily pain and energy levels. The scores on these questions were then used to calculate the overall physical component summary score (PCS) and mental component summary score (MCS) which were used as a control variable in the present model. Responses from this questionnaire were scored according to scoring instructions provided by Ware et al. (1998) and entered as control variables.
Analysis Plan
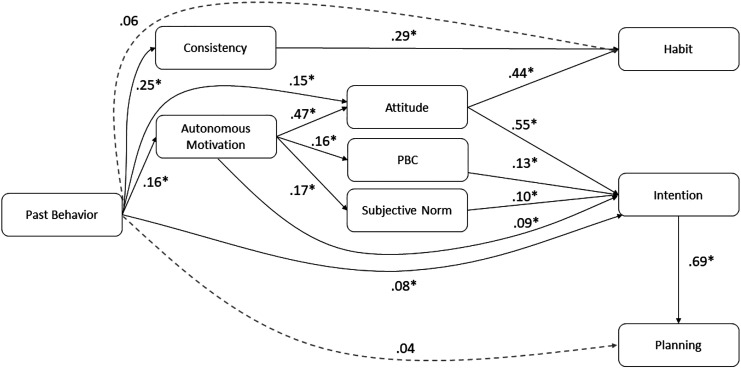
Demographics were calculated using SPSS v. 24.0 (IBM, 2016). The number of missing values was below 1% for all measures. In light of the distinct weights associated with the combination of a weekly and daily frequency in the PASE, missing values (<1%) on PASE subscales were not replaced, and the respective subscales not included in participants’ total score. To test the proposed model (Figure 2), structural equation modeling in AMOS was employed by using a maximum-likelihood estimation method (Enders, 2011). We followed Wolf et al.’s (2013) estimation criteria to confirm that the sample size was sufficient for conducting the structural equation model. Goodness of fit was assessed using cut off indices specified by Hu and Bentler’s (1999) Two-Index Presentation strategy for the Comparative Fit Index (CFI) (equal to or greater than 0.90) and other specifications for the root mean square error of approximation (RMSEA) (less than or equal to 0.08 with a 95% confidence interval), and TLI (greater than or equal to 0.90) reported in AMOS (Bentler, 1990). In the following, we present standardized regression coefficients as effect-size indices. Lastly, we expected the effects from the predictive model to hold after accounting for participants’ health status.
Figure 2.
Structural equation model predicting older adults’ (N = 667) physical activity habit, intention, and planning to be physically active. Note. Control variables and indirect effects have been omitted for clarity. Dashed lines indicate hypothesized pathways that were found to be statistically insignificant. *p < .01.
Results
Model Effects
Latent correlations found all constructs to significantly correlate with each other (see Table 3). Model fit indices were found to fall within an acceptable range (χ2 = 1220.988, df = 245, p = .000, RMSEA = .077, 90% CI (.073, .082), CFI = .927, TLI = .910). Descriptive statistics and factor loadings for all model constructs can be found in Tables 2 and 4.
Table 3.
Latent Correlations for Model Constructs (N = 667).
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | |
|---|---|---|---|---|---|---|---|---|---|
| Intention (1) | ___ | ||||||||
| RAI (2) | .44* | ___ | |||||||
| Attitude (3) | .42* | .41* | ___ | ||||||
| Subjective norm (4) | .60* | .20* | .31* | ___ | |||||
| PBC (5) | .39* | .29* | .22* | .29* | ___ | ||||
| Consistency (6) | .55* | .39* | .36* | .54* | .33* | ___ | |||
| Habit (7) | .54* | .36* | .42* | .41* | .40* | .46* | ___ | ||
| Planning (8) | .46* | .22* | .39* | .41* | .26* | .45* | .47* | ___ | |
| Past behavior (9) | .31* | .22* | .20* | .20* | .24* | .26* | .35* | .24* | ___ |
Note. RAI = Relative Autonomy Index; PBC = Perceived Behavioral Control.
*p < 0.01.
Table 4.
Factor Loadings of Constructs Included in the Structural Equation Model (N = 667).
| Indicator | Factor Loadings |
|---|---|
| Attitude | - |
| Attitude01 | .95 |
| Attitude02 | .88 |
| Attitude03 | .80 |
| Habit | - |
| Habit01 | .89 |
| Habit02 | .92 |
| Habit03 | .92 |
| Habit04 | .73 |
| Perceived behavioral control (PBC) | - |
| PBC01 | .77 |
| PBC02 | .91 |
| PBC03 | .67 |
| Consistency | - |
| Consistency01 | .84 |
| Consistency02 | .81 |
| Consistency03 | .95 |
| Subjective norm | - |
| Norm01 | .80 |
| Norm02 | .77 |
| Planning | - |
| Planning01 | .88 |
| Planning02 | .80 |
| Planning03 | .82 |
| Intention | - |
| Intention01 | .95 |
| Intention02 | .97 |
| Intention03 | .98 |
Note. Dashes signify “not applicable”; factor loadings for all latent variables were found to be significant at p < .05.
Hypotheses Tests
Predictors of intention
As can be seen from Figure 2, intention was predicted by attitudes, PBC, and subjective norm. Autonomous motivation was found to predict intention via direct and indirect effects from attitudes, PBC, and subjective norms at a higher magnitude (β = .30, p = .013, CI 95%, .25 to .35). Similar patterns were observed with past behavior having a direct effect on intention, and a larger effect via TPB constructs (β = .15, p = .012, CI 95%, .09 to .19).
Predictors of TPB constructs
Autonomous motivation proximally predicted attitudes, PBC, and subjective norms. Past behavior predicted autonomous motivation and attitudes (see Figure 2).
Predictors of habit
Habit was directly predicted by consistency and attitude. Further, past behavior directly predicted consistency but not habit. Attitude and autonomous motivation also mediated between past behavior and habit (β = .17, p = .004, CI 95%, .14 to .22). Similarly, attitude mediated between autonomous motivation and habit (β = .20, p = .006, CI 95%, .17 to .26).
Predictors of planning
Planning was directly predicted by intention but not past behavior. Intention mediated between past behavior and planning (β = .16, p = .007, CI 95%, .11 to .20)
Discussion
The present study investigated decisional determinants of physical activity, namely, intentions, planning, and habit among older adults. We utilized the IBC model, a multi-theoretical approach, that included past behavior to test decisional determinants to enact in future PA. Congruent with TPB theorizing, results showed that attitudes, subjective norms, and PBC positively predicted physical activity intentions (H1). Among these determinants, attitude was found to explain the most variance of intention. These findings suggest that it may be beneficial for health practitioners to build on existing awareness of the benefits of physical activity and reframe perceived negative outcomes. In this regard, behavior change techniques such as self-reevaluation (i.e., assessment of one’s identity as an active vs. sedentary person; Prochaska et al., 2015) may be relevant strategies to address attitudes toward physical activity in older adults (Bartholomew Eldredge et al., 2016). Subjective norms and PBC also demonstrated significant effects on intentions, implying that skill and ability to execute behavior, in addition to facilitating positive group-based interventions may likely facilitate physical activity intentions.
In support of one of the novel hypotheses specific to IBC, social cognitive constructs (attitudes, PBC, and subjective norms) were found to mediate the relationship between autonomous motivation and intention (H2). These results corroborate findings of behavioral, control-related as well as normative beliefs being of importance in the formation of exercise intentions (Hagger & Chatzisarantis, 2009). Our findings show that an individual’s motivational orientation plays a key role in the formation of attitudes and perceptions about PBC and the significance of the behavior of others. Individuals with greater autonomous motivation perceived greater benefits from physical activity, which in turn affected their intentions to engage in physical activity. Thus, fostering positive perceptions about physical activity, one’s control over behavioral enactment, and the perception of the importance of others may be achieved more efficiently through a previously identified importance of physical activity for one’s person or health. These findings are in line with previous meta-analytic findings on the predictive effects of autonomous motivation on TPB variables (Hagger & Chatzisarantis, 2009).
In addition to identifying the predictive role of autonomous motivation, this study examined the extent to which belief-based constructs of the TPB, autonomous motivation, as well as subsequent intention are a function of past behavior. In this regard, we found that the included TPB constructs mediate between past behavior and intention. This finding provides detailed insight into the psychological mechanisms by which past behavior affects intention formation via perceived barriers and beliefs (Hagger et al., 2018; Kaushal, Keith, et al., 2020; Ouellette & Wood, 1998). Past behavior also significantly predicted autonomous motivation to engage in physical activity (Hagger & Chatzisarantis, 2009), indicating that an individual’s activity status should be taken into consideration when developing interventions to foster the identified importance of physical activity and the subsequent intention to engage in physical activity. Thus, our results support the theoretical integration of autonomous motivation from Self-Determination Theory among other determinants, as this construct was shown to be a significant antecedent of belief-based constructs and intention for behavioral enactment. Inclusion of this construct can provide greater insight into the psychological mechanisms by which intentions are formed or changed, also on the basis of past behavior.
Regarding the role of planning, our study illustrates the role of past behavior because we found that past behavior predicted action planning via intention (H4). Given the identified relationship between planning and intention, older adults may benefit from tailored interventions that are based on their previous levels of PA engagement so that they can develop (more) effective action plans. This may subsequently assist in the translation from intention to behavior. Previous research examining the role of planning has been mixed; some studies found planning to function as a mediator and others have found planning to function as a moderator (Rhodes & Dickau, 2013; Rhodes & Pfaeffli, 2010). In a study among older adults, Arnautovska et al. (2017) showed that planning mediated between physical activity intentions and behavior, thereby adding support for the role for action planning as a mechanism to bridge the gap between intentions and behavior (Schwarzer & Luszczynska, 2008; Sniehotta et al., 2005). In this regard, studying an individual’s goals may provide more detailed insight into mechanisms related to planning, intention, and behavior (Amireault et al., 2013). Further research on these different populations might add clarity to the role of planning as a post-intention construct.
Last, our model examined the automatic process of habits, in parallel to intention. The present model extended the automatic processes proposed in the IBC framework by including consistency as a further antecedent of habit. Consistency can also represent a regular physical activity environment, and hence, the present study also assessed environmental, along with temporal consistency. These measures were included to reflect contextual support for habit formation (Hagger, 2019; Wood & Rünger, 2016). The present findings support previous work that found temporal consistency to facilitate habit formation among general adults (Kaushal & Rhodes, 2015; Kaushal et al., 2017). These findings are novel for older population groups, emphasizing the importance of having a regular, anticipated time and environment to engage in physical activity. Previous empirical work demonstrated feasibility of incorporating consistency among general adults to facilitate their habit formation and taking current findings into consideration encourages future interventions to test feasibility of implementing this construct among older adults.
To examine the predictive role of past behavior in the formation of habits, we included previous physical activity engagement into the model. Specifically, attitudes and autonomous motivation were found to mediate the relationship between past behavior and habit. Conforming to previous work (Kaushal, Keith, et al., 2020; Radel et al., 2017), our results suggest that autonomously motivated individuals are more likely to indicate to habitually engage in physical activity. In line with Self-Determination Theory (Deci & Ryan, 1985), being autonomously motivated may be associated with habit formation as the target behavior is perceived to satisfy one’s psychological needs. As a result, autonomously motivated individuals may be more likely to continuously seek engagement in the behavior, usually in similar environments or contexts (Kaushal, Keith, et al., 2020). Perceiving the performance of a behavior as highly rewarding in addition to consistency in context and behavior may in turn encourage the formation of habits (Gardner & Lally, 2013; Lally & Gardner, 2013). Consistent with the literature, the present results showed past behavior to predict habits via consistency. This corroborates findings regarding the need of stable contexts over a greater timeframe for the development of habits (Hagger, 2019; Kaushal & Rhodes, 2015).
In summary, the present study exemplified the importance of employing a multi-process approach (involving conscious and non-conscious processes) to predict complex behaviors such as physical activity. Though the proposed effects need to ultimately be established through randomized controlled trials, identifying patterns and effects while controlling for other determinants in a structural equation modeling test can help setting the groundwork for further refinement of health behavior theories as well as more tailored intervention designs.
Strengths and Limitations
Though consistency has been found to be one of the strongest predictors of exercise habit formation (Kaushal et al., 2017), this study is among the first to extend previous findings and demonstrate predictive validity of this construct among older adults. These results provide formative notes for designing physical activity interventions for older adults, at least in the context of primary prevention. In addition, investigations of physical activity determinants using contemporary models, that were specifically designed to predict the target behavior, are sparse; this is especially the case for research on older adults. The present study contributes novel findings based on the described, updated theoretical approach. Nonetheless, we recognize that the observed relationships in this study are limited to the cross-sectional design, as causation cannot be inferred. Further, the inclusion of an objective measure of physical activity may have provided more detailed insight into the physical activity habits in the present sample. Regarding the generalizability of our findings, the sample included participants of higher education compared with the national average. This discrepancy is not uncommon when recruiting older adults from crowdsourcing platforms (Ogletree & Katz, 2021). As physical activity is correlated with education (Zhao et al., 2011) and the online advertisement appeared to sample a higher educated older adult demographic, we acknowledge that the present sample may differ on behavioral, cognitive, or affective outcomes. We thus recommend that future studies explore decisional determinants of physical activity in a variety of older adult subpopulations via direct community recruitment methods. We also recognize that the sampling method could result in, for example, increased sedentary time and in turn increase the prevalence of high BMI scores. However, our sample shows great similarity in BMI to older adults from national reports who were recruited through other channels (Fryar et al., 2018). Similar online recruitment methods have previously been used regarding habit strength and physical activity in older adults (see Mullan et al., 2021).
In sum, this study extended previous investigations of older adults’ activity intentions by including deliberative processes (social cognitive variables, planning, and motivational orientation) in addition to testing non-conscious (habit) processes. Specifically, older adults’ physical activity adoption could benefit from facilitating these constructs. However, it is likely that this demographic may require adaptive methods to develop the constructs that were found to be effective in their younger counterparts.
Conclusion
In conclusion, this study highlights the importance of multiple processes (social cognitive, habit/automatic, and post-intentional/planning) that formulate physical activity intentions among older adults. Further, mediation pathways revealed the importance of autonomous motivation for establishing proximal behavioral determinants (intentions and habit). Facilitating these processes among older adults could be effective for promoting physical activity. Future research should further explore the major identified determinants of physical activity among older adults as a basis for interventions by using randomized controlled trials that test their long-term effects on establishing the maintenance of physical activity behavior.
Footnotes
Author Note: Christian E. Preissner is now at the Faculty of Health, Medicine and Life Sciences, Maastricht University, The Netherlands.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This work was supported by funds from James McGill Professorship to B.K.
ORCID iDs
Christian E. Preissner https://orcid.org/0000-0001-5704-2234
Navin Kaushal https://orcid.org/0000-0002-4511-7902
References
- Ajzen I. (1991). The theory of planned behavior. Organizational Behavior and Human Decision Processes, 50(2), 179-211. [Google Scholar]
- Ajzen I. (2002). Constructing a TPB questionnaire: Conceptual and methodological considerations. http://people.umass.edu/∼aizen/pdf/tpb.measurement.pdf.
- Amireault S., Godin G., Vézina-Im L.-A. (2013). Determinants of physical activity maintenance: A systematic review and meta-analyses. Health Psychology Review, 7(1), 55-91. DOI: 10.1080/17437199.2012.701060 10.1080/17437199.2012.701060. [DOI] [Google Scholar]
- Arcury T. A., Sandberg J. C., Melius K. P., Quandt S. A., Leng X., Latulipe C., Miller D. P., Jr., Alden Smith D., Bertoni A. G. (2020). Older adult internet use and eHealth literacy. Journal of Applied Gerontology, 39(2), 141-150. https://doi.org/10.1177%2F0733464818807468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Armitage C. J., Conner M., Loach J., Willetts D. (1999). Different perceptions of control: Applying an extended Theory of Planned Behavior to legal and illegal drug use. Basic and Applied Social Psychology, 21(4), 301-316. DOI: 10.1207/S15324834BASP2104_4 10.1207/S15324834BASP2104_4. [DOI] [Google Scholar]
- Arnautovska U., Fleig L., O’Callaghan F., Hamilton K. (2017). A longitudinal investigation of older adults’ physical activity: Testing an integrated dual-process model. Psychology & Health, 32(2), 166-185. DOI: 10.1080/08870446.2016.1250273 10.1080/08870446.2016.1250273. [DOI] [PubMed] [Google Scholar]
- Barnes D. E., Yaffe K., Satariano W. A., Tager I. B. (2003). A longitudinal study of cardiorespiratory fitness and cognitive function in healthy older adults. Journal of the American Geriatrics Society, 51(4), 459-465. DOI: 10.1046/j.1532-5415.2003.51153.x 10.1046/j.1532-5415.2003.51153.x. [DOI] [PubMed] [Google Scholar]
- Bartholomew Eldredge L. K., Markham C. M., Ruiter R. A., Fernandez M. E., Kok G., Parcel G. S. (2016). Planning health promotion programs: An intervention mapping approach. Jossey-Bass Inc. [Google Scholar]
- Bélanger-Gravel A., Godin G., Amireault S. (2013). A meta-analytic review of the effect of implementation intentions on physical activity. Health Psychology Review, 7(1), 23-54. DOI: 10.1080/17437199.2011.560095 10.1080/17437199.2011.560095. [DOI] [PubMed] [Google Scholar]
- Bentler P. M. (1990). Comparative fit indexes in structural models. Psychological Bulletin, 107(2), 238. [DOI] [PubMed] [Google Scholar]
- Carraro N., Gaudreau P. (2013). Spontaneous and experimentally induced action planning and coping planning for physical activity: A meta-analysis. Psychology of Sport and Exercise, 14(2), 228-248. DOI: 10.1016/j.psychsport.2012.10.004 10.1016/j.psychsport.2012.10.004. [DOI] [Google Scholar]
- Chandler J., Rosenzweig C., Moss A. J., Robinson J., Litman L. (2019). Online panels in social science research: Expanding sampling methods beyond Mechanical Turk. Behavior Research Methods, 51(5), 2022-2038. DOI: 10.3758/s13428-019-01273-7 10.3758/s13428-019-01273-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chase J. A. D. (2013). Methodological challenges in physical activity research with older adults. Western Journal of Nursing Research, 35(1), 76-97. https://doi.org/10.1177%2F0193945911416829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chase J. A. D. (2015). Interventions to increase physical activity among older adults: A meta-analysis. The Gerontologist, 55(4), 706-718. DOI: 10.1093/geront/gnu090 10.1093/geront/gnu090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chatzisarantis N. L. D., Hagger M. S. (2009). Effects of an intervention based on self-determination theory on self-reported leisure-time physical activity participation. Psychology & Health, 24(1), 29-48. DOI: 10.1080/08870440701809533 10.1080/08870440701809533. [DOI] [PubMed] [Google Scholar]
- Danner U. N., Aarts H., de Vries N. K. (2007). Habit formation and multiple means to goal attainment: Repeated retrieval of target means causes inhibited access to competitors. Personality & Social Psychology Bulletin, 33(10), 1367-1379. https://doi.org/10.1177%2F0146167207303948. [DOI] [PubMed] [Google Scholar]
- Davidai S. (2018). Why do Americans believe in economic mobility? Economic inequality, external attributions of wealth and poverty, and the belief in economic mobility. Journal of Experimental Social Psychology, 79, 138-148. DOI: 10.1016/j.jesp.2018.07.012 10.1016/j.jesp.2018.07.012. [DOI] [Google Scholar]
- de Vries H. (2017). An integrated approach for understanding health behavior; the I-Change Model as an example. Psychology and Behavioral Science International Journal, 2(2). DOI: 10.19080/PBSIJ.2017.02.555585 10.19080/PBSIJ.2017.02.555585. [DOI] [Google Scholar]
- de Vries H., Kremers S. P. J., Lippke S. (2018). Health education and health promotion: Key concepts and exemplary evidence to support them. In Fisher E. B., Cameron L. D., Christensen A. J., Ehlert U., Guo Y., Oldenburg B., Snoek F. J. (Eds.), Principles and concepts of behavioral medicine (pp. 489-532). Springer. [Google Scholar]
- de Vries N. M., Van Ravensberg C. D., Hobbelen J. S. M., Rikkert M. O., Staal J. B., Nijhuis-van der Sanden M. W. G. (2012). Effects of physical exercise therapy on mobility, physical functioning, physical activity and quality of life in community-dwelling older adults with impaired mobility, physical disability and/or multi-morbidity: A meta-analysis. Ageing Research Reviews, 11(1), 136-149. DOI: 10.1016/j.arr.2011.11.002 10.1016/j.arr.2011.11.002. [DOI] [PubMed] [Google Scholar]
- Deci E. L., Ryan R. M. (1985). Intrinsic motivation and self-determination in human behavior. Plenum Press. [Google Scholar]
- Deci E. L., Ryan R. M. (2008). Self-determination theory: A macrotheory of human motivation, development, and health. Canadian Psychology/Psychologie Canadienne, 49(3), 182-185. DOI: 10.1037/a0012801 10.1037/a0012801. [DOI] [Google Scholar]
- Denkinger M. D., Nikolaus T., Denkinger C., Lukas A. (2012). Physical activity for the prevention of cognitive decline. Zeitschrift für Gerontologie und Geriatrie, 45(1), 11-16. DOI: 10.1007/s00391-011-0262-6 10.1007/s00391-011-0262-6. [DOI] [PubMed] [Google Scholar]
- Enders C. K. (2011). Analyzing longitudinal data with missing values. Rehabilitation Psychology, 56(4), 267-288. DOI: 10.1037/a0025579 10.1037/a0025579. [DOI] [PubMed] [Google Scholar]
- Evans J. B. T. (2008). Dual-processing accounts of reasoning, judgment, and social cognition. Annual Review of Psychology, 59(1), 255-278. DOI: 10.1146/annurev.psych.59.103006.093629 10.1146/annurev.psych.59.103006.093629. [DOI] [PubMed] [Google Scholar]
- Falck R. S., Davis J. C., Best J. R., Crockett R. A., Liu-Ambrose T. (2019). Impact of exercise training on physical and cognitive function among older adults: A systematic review and meta-analysis. Neurobiology of Aging, 79, 119-130. DOI: 10.1016/j.neurobiolaging.2019.03.007 10.1016/j.neurobiolaging.2019.03.007. [DOI] [PubMed] [Google Scholar]
- Fishbein M., Ajzen I. (1980). Understanding attitudes and predicting social behavior. Prentice-Hall. [Google Scholar]
- Fleig L., McAllister M. M., Chen P., Iverson J., Milne K., McKay H. A., Ashe M. C. (2016). Health behaviour change theory meets falls prevention: Feasibility of a habit-based balance and strength exercise intervention for older adults. Psychology of Sport and Exercise, 22, 114-122. DOI: 10.1016/j.psychsport.2015.07.002 10.1016/j.psychsport.2015.07.002. [DOI] [Google Scholar]
- Follmer D. J., Sperling R. A., Suen H. K. (2017). The role of MTurk in education research: Advantages, issues, and future directions. Educational Researcher, 46(6), 329-334. https://doi.org/10.3102%2F0013189X17725519. [Google Scholar]
- Fryar C. D., Kruszan-Moran D., Gu Q., Ogden C. L. (2018). Mean body weight, weight, waist circumference, and body mass index among adults: United States, 1999–2000 through 2015–2016. National Health Statistics Reports, (122). National Center for Health Statistics. https://www.cdc.gov/nchs/data/nhsr/nhsr122-508.pdf. [PubMed] [Google Scholar]
- Gardner B. (2015). A review and analysis of the use of ‘habit’ in understanding, predicting and influencing health-related behaviour. Health Psychology Review, 9(3), 277-295. DOI: 10.1080/17437199.2013.876238 10.1080/17437199.2013.876238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gardner B., Abraham C., Lally P., de Bruijn G.-J. (2012). Towards parsimony in habit measurement: Testing the convergent and predictive validity of an automaticity subscale of the Self-Report Habit Index. International Journal of Behavioral Nutrition and Physical Activity, 9(1), 102. DOI: 10.1186/1479-5868-9-102 10.1186/1479-5868-9-102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gardner B., Lally P. (2013). Does intrinsic motivation strengthen physical activity habit? Modeling relationships between self-determination, past behaviour, and habit strength. Journal of Behavioral Medicine, 36(5), 488-497. DOI: 10.1007/s10865-012-9442-0 10.1007/s10865-012-9442-0. [DOI] [PubMed] [Google Scholar]
- Goggin N. L., Morrow J. R. (2001). Physical activity behaviors of older adults. Journal of Aging and Physical Activity, 9(1), 58-66. DOI: 10.1123/japa.9.1.58 10.1123/japa.9.1.58. [DOI] [Google Scholar]
- Gourlan M., Bernard P., Bortolon C., Romain A. J., Lareyre O., Carayol M., Ninot G., Boiché J. (2016). Efficacy of theory-based interventions to promote physical activity. A meta-analysis of randomised controlled trials. Health Psychology Review, 10(1), 50-66. DOI: 10.1080/17437199.2014.981777 10.1080/17437199.2014.981777. [DOI] [PubMed] [Google Scholar]
- Grodesky J. M., Kosma M., Solmon M. A. (2006). Understanding older adults’ physical activity behavior: A multi-theoretical approach. Quest, 58(3), 310-329. DOI: 10.1080/00336297.2006.10491885 10.1080/00336297.2006.10491885. [DOI] [Google Scholar]
- Hagger M. S. (2019). Habit and physical activity: Theoretical advances, practical implications, and agenda for future research. Psychology of Sport and Exercise, 42, 118-129. DOI: 10.1016/j.psychsport.2018.12.007 10.1016/j.psychsport.2018.12.007. [DOI] [Google Scholar]
- Hagger M. S., Chatzisarantis N. L. D. (2009). Integrating the theory of planned behaviour and self-determination theory in health behaviour: A meta-analysis. British Journal of Health Psychology, 14(2), 275-302. DOI: 10.1348/135910708X373959 10.1348/135910708X373959. [DOI] [PubMed] [Google Scholar]
- Hagger M. S., Chatzisarantis N. L. D. (2014). An Integrated Behavior Change model for physical activity. Exercise and Sport Sciences Reviews, 42(2), 62-69. DOI: 10.1249/JES.0000000000000008 10.1249/JES.0000000000000008. [DOI] [PubMed] [Google Scholar]
- Hagger M. S., Chatzisarantis N. L. D., Harris J. (2006). The process by which relative autonomous motivation affects intentional behavior: Comparing effects across dieting and exercise behaviors. Motivation and Emotion, 30(4), 306. DOI: 10.1007/s11031-006-9046-5 10.1007/s11031-006-9046-5. [DOI] [Google Scholar]
- Hagger M. S., Hamilton K., Hardcastle S. J., Hu M., Kwok S., Lin J., Nawawi H. M., Pang J., Santos R. D., Soran H., Su T.-C., Tomlinson B., Watts G. F. (2019). Predicting intention to participate in self-management behaviors in patients with Familial Hypercholesterolemia: A cross-national study. Social Science & Medicine, 242, 112591. 10.1016/j.socscimed.2019.112591. [DOI] [PubMed]
- Hagger M. S., Luszczynska A. (2014). Planning interventions for behaviour change: A protocol for establishing best practice through consensus. 16(5), 206-213. https://ehps.net/ehp/index.php/contents/article/view/ehp.v16.i5.p206. [Google Scholar]
- Hagger M. S., Polet J., Lintunen T. (2018). The reasoned action approach applied to health behavior: Role of past behavior and tests of some key moderators using meta-analytic structural equation modeling. Social Science & Medicine, 213, 85-94. DOI: 10.1016/j.socscimed.2018.07.038 10.1016/j.socscimed.2018.07.038. [DOI] [PubMed] [Google Scholar]
- Hagger M. S., Trost N., Keech J. J., Chan D. K. C., Hamilton K. (2017). Predicting sugar consumption: Application of an integrated dual-process, dual-phase model. Appetite, 116, 147-156. DOI: 10.1016/j.appet.2017.04.032 10.1016/j.appet.2017.04.032. [DOI] [PubMed] [Google Scholar]
- Hallal P. C., Andersen L. B., Bull F. C., Guthold R., Haskell W., Ekelund U. (2012). Global physical activity levels: Surveillance progress, pitfalls, and prospects. Lancet, 380(9838), 247-257. DOI: 10.1016/S0140-6736(12)60646-1 10.1016/S0140-6736(12)60646-1. [DOI] [PubMed] [Google Scholar]
- Hamilton K., Kirkpatrick A., Rebar A., Hagger M. S. (2017). Child sun safety: Application of an Integrated Behavior Change model. Health Psychology, 36(9), 916-926. DOI: 10.1037/hea0000533 10.1037/hea0000533. [DOI] [PubMed] [Google Scholar]
- Hu L., Bentler P. M. (1999). Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Structural Equation Modeling: A Multidisciplinary Journal, 6(1), 1-55. DOI: 10.1080/10705519909540118 10.1080/10705519909540118. [DOI] [Google Scholar]
- Kaushal N., Keith N., Aguiñaga S., Hagger M. S. (2020. a). Social cognition and socioecological predictors of home-based physical activity intentions, planning, and habits during the COVID-19 pandemic. Behavioral Sciences, 10(9), 133. DOI: 10.3390/bs10090133 10.3390/bs10090133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaushal N., Preissner C., Charles K., Knäuper B. (2020. b). Differences and similarities of physical activity determinants between older adults who have and have not experienced a fall: Testing an extended health belief model. Archives of Gerontology and Geriatrics, 92, e104247. DOI: 10.1016/j.archger.2020.104247 10.1016/j.archger.2020.104247. [DOI] [PubMed] [Google Scholar]
- Kaushal N., Rhodes R. E. (2015). Exercise habit formation in new gym members: A longitudinal study. Journal of Behavioral Medicine, 38(4), 652-663. DOI: 10.1007/s10865-015-9640-7 10.1007/s10865-015-9640-7. [DOI] [PubMed] [Google Scholar]
- Kaushal N., Rhodes R. E., Meldrum J. T., Spence J. C. (2017). The role of habit in different phases of exercise. British Journal of Health Psychology, 22(3), 429-448. DOI: 10.1111/bjhp.12237 10.1111/bjhp.12237. [DOI] [PubMed] [Google Scholar]
- Kosma M., Gardner R. E., Cardinal B. J., Bauer J. J., McCubbin J. A. (2006). Psychosocial determinants of stages of change and physical activity among adults with physical disabilities. Adapted Physical Activity Quarterly, 23(1), 49-64. DOI: 10.1123/apaq.23.1.49 10.1123/apaq.23.1.49. [DOI] [Google Scholar]
- Lally P., Gardner B. (2013). Promoting habit formation. Health Psychology Review, 7(1), 137-158. DOI: 10.1080/17437199.2011.603640 10.1080/17437199.2011.603640. [DOI] [Google Scholar]
- Lautenschlager N. T., Cox K. L., Flicker L., Foster J. K., van Bockxmeer F. M., Xiao J., Greenop K. R., Almeida O. P. (2008). Effect of physical activity on cognitive function in older adults at risk for Alzheimer Disease: A randomized trial. Journal of the American Medical Association, 300(9), 1027-1037. DOI: 10.1001/jama.300.9.1027 10.1001/jama.300.9.1027. [DOI] [PubMed] [Google Scholar]
- McEwan D., Beauchamp M. R., Kouvousis C., Ray C. M., Wyrough A., Rhodes R. E. (2019). Examining the active ingredients of physical activity interventions underpinned by theory versus no stated theory: A meta-analysis. Health Psychology Review, 13(1), 1-17. DOI: 10.1080/17437199.2018.1547120 10.1080/17437199.2018.1547120. [DOI] [PubMed] [Google Scholar]
- McMillan L. B., Zengin A., Ebeling P. R., Scott D. (2017). Prescribing physical activity for the prevention and treatment of osteoporosis in older adults. Healthcare, 5, 85. DOI: 10.3390/healthcare5040085 10.3390/healthcare5040085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McRobert C. J., Hill J. C., Smale T., Hay E. M., van der Windt D. A. (2018). A multi-modal recruitment strategy using social media and internet-mediated methods to recruit a multidisciplinary, international sample of clinicians to an online research study. Plos One, 13(7), e0200184. DOI: 10.1371/journal.pone.0200184 10.1371/journal.pone.0200184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mullan B., Olivier C., Thøgersen‐Ntoumani C. (2021). Mind the gap: Habit and self‐determined motivation predict health behaviours in middle‐aged and older adults. British Journal of Health Psychology. DOI: 10.1111/bjhp.12522 10.1111/bjhp.12522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nelson M., Rejeski W., Blair S., Duncan P., Judge J., King A., Macera C., Castaneda-Sceppa C. (2007). Physical activity and public health in older adults: Recommendation from the American College of Sports Medicine and the American Heart Association. Circulation, 116(9), 1094-1105. https://scholarcommons.sc.edu/sph_epidemiology_biostatistics_facpub/380. [DOI] [PubMed] [Google Scholar]
- Norman P., Webb T. L., Millings A. (2019). Using the theory of planned behaviour and implementation intentions to reduce binge drinking in new university students. Psychology & Health, 34(4), 478-496. DOI: 10.1080/08870446.2018.1544369 10.1080/08870446.2018.1544369. [DOI] [PubMed] [Google Scholar]
- Nurmi J., Hagger M. S., Haukkala A., Araújo-Soares V., Hankonen N. (2016). Relations between autonomous motivation and leisure-time physical activity participation: The mediating role of self-regulation techniques. Journal of Sport and Exercise Psychology, 38(2), 128-137. DOI: 10.1123/jsep.2015-0222 10.1123/jsep.2015-0222. [DOI] [PubMed] [Google Scholar]
- Ogletree A. M., Katz B. (2021). How do older adults recruited using MTurk differ from those in a national probability sample? International Journal of Aging & Human Development, 93(2), 700-721. DOI: 10.1177/0091415020940197 10.1177/0091415020940197. [DOI] [PubMed] [Google Scholar]
- Ouellette J. A., Wood W. (1998). Habit and intention in everyday life: The multiple processes by which past behavior predicts future behavior. Psychological Bulletin, 124(1), 54-74. DOI: 10.1037/0033-2909.124.1.54 10.1037/0033-2909.124.1.54. [DOI] [Google Scholar]
- Pahor M., Guralnik J. M., Ambrosius W. T., Blair S., Bonds D. E., Church T. S., Espeland M. A., Fielding R. A., Gill T. M., Groessl E. J., King A. C., Kritchevsky S. B., Manini T. M., McDermott M. M., Miller M. E., Newman A. B., Rejeski W. J., Sink K. M., Williamson J. D. (2014). Effect of structured physical activity on prevention of major mobility disability in older adults: The LIFE study randomized clinical trial. Journal of the American Medical Association, 311(23), 2387-2396. DOI: 10.1001/jama.2014.5616 10.1001/jama.2014.5616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peng W., Li L., Kononova A., Cotten S., Kamp K., Bowen M. (2021). Habit formation in wearable activity tracker use among older adults: Qualitative study. JMIR Mhealth and Uhealth, 9(1), e22488. DOI: 10.2196/22488 10.2196/22488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Perrin A., Atske S. (2021). 7% of Americans don’t use the internet. Who are they? (April 2). Pew Research Center. https://www.pewresearch.org/fact-tank/2021/04/02/7-of-americans-dont-use-the-internet-who-are-they/. [Google Scholar]
- Pfeffer I., Strobach T. (2019). Effects of a planning intervention on physical activity behavior in an RCT: Intention strength as moderator and action planning, coping planning, and coping self-efficacy as mediators. Sport, Exercise, and Performance Psychology, 8(2), 192-209. DOI: 10.1037/spy0000137 10.1037/spy0000137. [DOI] [Google Scholar]
- Prochaska J. O., Redding C. A., Evers K. E. (2015). The transtheoretical model of stages of change. In Glanz K., Rimer B. K., Viswanath K. (Eds.), Health behavior: Theory, research, and practice (5th ed., pp. 168-222). Jossey-Bass. [Google Scholar]
- Radel R., Pelletier L., Pjevac D., Cheval B. (2017). The links between self-determined motivations and behavioral automaticity in a variety of real-life behaviors. Motivation and Emotion, 41(4), 443-454. DOI: 10.1007/s11031-017-9618-6 10.1007/s11031-017-9618-6. [DOI] [Google Scholar]
- Rebar A. L., Dimmock J. A., Jackson B., Rhodes R. E., Kates A., Starling J., Vandelanotte C. (2016). A systematic review of the effects of non-conscious regulatory processes in physical activity. Health Psychology Review, 10(4), 395-407. DOI: 10.1080/17437199.2016.1183505 10.1080/17437199.2016.1183505. [DOI] [PubMed] [Google Scholar]
- Rhodes R. E., Blanchard C. M., Matheson D. H. (2006). A multicomponent model of the theory of planned behaviour. British Journal of Health Psychology, 11(1), 119-137. DOI: 10.1348/135910705X52633 10.1348/135910705X52633. [DOI] [PubMed] [Google Scholar]
- Rhodes R. E., Dickau L. (2013). Moderators of the intention-behaviour relationship in the physical activity domain: A systematic review. British Journal of Sports Medicine, 47(4), 215-225. DOI: 10.1136/bjsports-2011-090411 10.1136/bjsports-2011-090411. [DOI] [PubMed] [Google Scholar]
- Rhodes R. E., Pfaeffli L. A. (2010). Mediators of physical activity behaviour change among adult non-clinical populations: A review update. International Journal of Behavioral Nutrition and Physical Activity, 7(1), 37. DOI: 10.1186/1479-5868-7-37 10.1186/1479-5868-7-37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ryan R. M., Connell J. P. (1989). Perceived locus of causality and internalization: Examining reasons for acting in two domains. Journal of Personality and Social Psychology, 57(5), 749-761. DOI: 10.1037/0022-3514.57.5.749 10.1037/0022-3514.57.5.749. [DOI] [PubMed] [Google Scholar]
- Sabia S., Singh-Manoux A., Hagger-Johnson G., Cambois E., Brunner E. J., Kivimaki M. (2012). Influence of individual and combined healthy behaviours on successful aging. Canadian Medical Journal Association, 184(18), 1985-1992. DOI: 10.1503/cmaj.121080 10.1503/cmaj.121080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schwarzer R., Luszczynska A. (2008). How to overcome health-compromising behaviors: The health action process approach. European Psychologist, 13(2), 141-151. 10.1027/1016-9040.13.2.141. [DOI] [Google Scholar]
- Senkowski V., Gannon C., Branscum P. (2019). Behavior change techniques used in Theory of Planned Behavior physical activity interventions amongst older adults: A systematic review. Journal of Aging and Physical Activity, 27(5), 746-754. 10.1123/japa.2018-0103. [DOI] [PubMed] [Google Scholar]
- Sniehotta F. F., Schwarzer R., Scholz U., Schüz B. (2005). Action planning and coping planning for long-term lifestyle change: Theory and assessment. European Journal of Social Psychology, 35(4), 565-576. DOI: 10.1002/ejsp.258 10.1002/ejsp.258. [DOI] [Google Scholar]
- Stolte E., Hopman-Rock M., Aartsen M. J., van Tilburg T. G., Chorus A. (2017). The theory of planned behavior and physical activity change: Outcomes of the aging well and healthily intervention program for older adults. Journal of Aging and Physical Activity, 25(3), 438-445. 10.1123/japa.2016-0182 [DOI] [PubMed] [Google Scholar]
- Strack F., Deutsch R. (2004). Reflective and impulsive determinants of social behavior. Personality and Social Psychology Review, 8(3), 220-247. [DOI] [PubMed] [Google Scholar]
- United Nations, Department of Economic and Social Affairs, Population Division . (2019). World population prospects 2019: Highlights. https://population.un.org/wpp/Publications/Files/WPP2019_Highlights.pdf.
- van Bree R. J., Bolman C., Mudde A. N., van Stralen M. M., Peels D. A., de Vries H., Lechner L. (2017). Modeling longitudinal relationships between habit and physical activity: Two cross-lagged panel design studies in older adults. Journal of Aging and Physical Activity, 25(3), 464-473. DOI: 10.1123/japa.2016-0212 10.1123/japa.2016-0212. [DOI] [PubMed] [Google Scholar]
- van Bree R. J., van Stralen M. M., Mudde A. N., Bolman C., de Vries H., Lechner L. (2015). Habit as mediator of the relationship between prior and later physical activity: A longitudinal study in older adults. Psychology of Sport and Exercise, 19, 95-102. DOI: 10.1016/j.psychsport.2015.03.006 10.1016/j.psychsport.2015.03.006. [DOI] [Google Scholar]
- Ware J. E., Kosinski M., Keller S. D. (1998). SF-12: How to score the SF-12 physical and mental health summary scales . Health Institute, New England Medical Center. [Google Scholar]
- Washburn R. A., Smith K. W., Jette A. M., Janney C. A. (1993). The Physical Activity Scale for the Elderly (PASE): Development and evaluation. Journal of Clinical Epidemiology, 46(2), 153-162. [DOI] [PubMed] [Google Scholar]
- Webb T., Joseph J., Yardley L., Michie S. (2010). Using the internet to promote health behavior change: A systematic review and meta-analysis of the impact of theoretical basis, use of behavior change techniques, and mode of delivery on efficacy. Journal of Medical Internet Research, 12(1), e4. DOI: 10.2196/jmir.1376 10.2196/jmir.1376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- White S. M., Wójcicki T. R., McAuley E. (2012). Social cognitive influences on physical activity behavior in middle-aged and older adults. The Journals of Gerontology: Series B, 67B(1), 18-26. DOI: 10.1093/geronb/gbr064 10.1093/geronb/gbr064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wolf E. J., Harrington K. M., Clark S. L., Miller M. W. (2013). Sample size requirements for structural equation models: An evaluation of power, bias, and solution propriety. Educational and Psychological Measurement. 76(6), 913-934. DOI: 10.1177/0013164413495237 10.1177/0013164413495237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wood W., Rünger D. (2016). Psychology of habit. Annual Review of Psychology, 67(1), 289-314. DOI: 10.1146/annurev-psych-122414-033417 10.1146/annurev-psych-122414-033417. [DOI] [PubMed] [Google Scholar]
- Zhang C.-Q., Zhang R., Schwarzer R., Hagger M. S. (2019). A meta-analysis of the health action process approach. Health Psychology, 38(7), 623-637. DOI: 10.1037/hea0000728 10.1037/hea0000728. [DOI] [PubMed] [Google Scholar]
- Zhao G., Ford E. S., Li C., Balluz L. S. (2011). Physical activity in US older adults with diabetes mellitus: Prevalence and correlates of meeting physical activity recommendations. Journal of the American Geriatrics Society, 59(1), 132-137. DOI: 10.1111/j.1532-5415.2010.03236.x 10.1111/j.1532-5415.2010.03236.x. [DOI] [PubMed] [Google Scholar]