Abstract
Objective:
To determine whether sexual minority adolescents have earlier onset of suicidality and faster progressions from ideation to plan and attempt, than heterosexual adolescents.
Methods:
A population-based longitudinal cohort of 1771 adolescents participated in the NEXT Generation Health Study. Participants reported sexual minority status (defined by sexual attraction) in 2010/11, and retrospectively reported age of onset of suicidality in 2015/2016.
Results:
Sexual minority adolescents (5.8% of weighted sample) had higher lifetime risk of suicide ideation (26.1% vs. 13.0%), plan (16.6% vs. 5.4%), and attempt (12.0% vs. 5.4%) than heterosexual adolescents. Survival analyses adjusted for demographic characteristics and depressive symptoms revealed positive associations of sexual minority status with time to first onset of suicide ideation (Hazard Ratio [HR] = 1.77, 95% CI [1.03–3.06]) and plan (HR = 2.69, 95% CI [1.30–5.56]). The association between sexual minority status and age at onset of suicide attempt was stronger below age 15 (HR = 3.26, 95% CI [1.25–8.47]) than ≥ age 15 (HR = 0.59, 95% CI [0.21–1.66]). The association between sexual minority status and progression from ideation to plan was stronger in the same year of first ideation (HR = 2.01, 95% CI [1.07–3.77]) than ≥1 year after first ideation (HR = 1.33, 95% CI [0.26–6.77]).
Conclusions:
Sexual minority adolescents had earlier onset of suicidality and faster progression from suicide ideation to plan than heterosexual adolescents. The assessment of sexual minority status in routine pediatric care has the potential to inform suicide risk screening, management, and intervention efforts among early sexual minority adolescents.
Table of Contents Summary
In a nationally representative cohort study, sexual minority youth were found to have earlier onset of suicide ideation and behavior than heterosexual youth.
Suicide is the second leading cause of death among youth aged 15–24 in the United States.1 Between 12.1–24.0% of U.S. adolescents report lifetime suicide ideation and 3.1–8.8% of adolescents report one or more lifetime suicide attempts.2,3 Data from the National Comorbidity Survey Replication-Adolescent Supplement (NCS-A) show that suicide ideation is rare before age 10 and increases sharply between ages 12 and 17.3 Suicide plan and attempt often develop after ideation and risks of planning and attempting suicide tend to increase linearly from age 12 through late adolescence, leveling off in the 20s.3–6 Adolescents with suicide ideation are 12 times more likely to attempt suicide by age 307 and have poorer adult functioning across financial, health, risky/legal, and social domains.8 Thus, identification of risk factors for onset of suicidality could inform targeted and optimally timed suicide prevention efforts.
Sexual minority status, which has been variably defined in the literature based on sexual identity, behavior, and/or attraction and commonly used to refer to lesbian, gay, and bisexual individuals, is strongly associated with suicide ideation and behavior.4,9 Relative to their heterosexual peers, sexual minority adolescents report more depressive symptomatology and are more likely to experience suicide ideation, plan and attempt.10–12 The Youth Risk Behavior Survey (YRBS) is the principal data source used to study sexual orientation health disparities among U.S. adolescents.13–18 Recent YRBS studies show that the proportion of adolescents who identified as sexual minorities increased from 7.3% in 2009 to 14.3% in 201719 and that past-year prevalence of suicide ideation, plan, and attempt remained markedly high among sexual minority youth across the 23-year study period.20 In the 2015 YRBS, sexual minority adolescents were more likely than their heterosexual peers to consider suicide seriously (39.7% vs. 14.8%), make a suicide plan (34.9% vs. 11.9%), and attempt suicide (24.9% vs. 6.3%) in the past year.21 As data on age of onset of suicide ideation and behavior are unavailable in the YRBS,22 the examination of the timing of sexual orientation disparities in other recent, nationally representative datasets would be valuable.
According to minority stress theory, lesbian, gay, bisexual, and transgender (LGBT) populations are at elevated risk for mental health problems because they face a more hostile and stressful social environment characterized by stigma, prejudice, and discrimination.23 As a result, individuals who identify as sexual minorities tend to have higher prevalence and earlier onset of self-injurious thoughts and behaviors than heterosexual individuals.24 In a longitudinal study of sexual minority youth, earlier age of first same-sex attraction was correlated with increased likelihood of lifetime and recent suicide attempt, and depressive symptoms constituted a key mediator of the associations between family support and victimization due to being or perceived as LGBT with suicide attempt.25 Therefore, although recent meta-analyses suggest that depression alone may not be sufficient for predicting suicide ideation and behaviors,24,26 it has substantial relevance for suicide prevention among sexual minority youth considering sexual minority disparities in adolescent depressive symptoms.27,28
Effective screening practices in the pediatric primary care setting can help identify and refer at-risk youth to appropriate specialty treatment or services.29–31 Current recommendations from the U.S. Preventive Services Task Force (USPSTF) and the American Academy of Pediatrics (AAP) promote universal screening for depression after age 12.32,33 While there are unique challenges associated with the implementation of pediatric suicide risk screening,34 a growing number of brief screening tools have been developed to detect suicide risk in youth.35–37 Regardless of whether suicidality is detected within or outside the context of depression, improved understanding of the timing of sexual minority disparities in suicide ideation and behaviors could inform the appropriate age at which suicide risk screening procedures should incorporate an assessment of sexual orientation to enhance clinical care.38
Ideation-to-action theories of suicide outline typical progressions from suicide ideation to plan and from suicide plan to attempt.39 Using a data source other than the YRBS, we examined prevalence of lifetime suicide ideation, plan, and attempt among sexual minority and heterosexual youth, investigated whether sexual minority youth had earlier onset of suicide ideation and behavior than their heterosexual peers, and tested whether sexual minority youth had faster progressions from suicide ideation to plan and plan to attempt than their heterosexual peers while controlling for depressive symptoms.
Method
Sample
The NEXT Generation Health Study (NEXT) is a 7-year longitudinal study of 2,783 10th graders who were followed annually from 2009–2010 to 2015–2016. A three-stage stratified design was used to recruit a nationally representative sample of U.S. high school students. Self-report questionnaires were administered initially (Wave 1) in classrooms, with annual online follow-ups. Adolescents who participated at Wave 2, when sexual minority status was measured, and Wave 7, when lifetime history of suicide ideation and behaviors were assessed, were included in the current study (n = 1,771). Attrition analyses revealed that females were more likely than males to participate in Wave 7; participation in Wave 7 did not vary by sexual minority status, race/ethnicity, family affluence, or depressive symptoms at Wave 2. Parents provided written consent for adolescent participation; upon reaching age 18, participants provided consent. The study was approved by the Institutional Review Board of the Eunice Kennedy Shriver National Institute of Child Health and Human Development.
Measures
Sexual minority status (Wave 2).
Sexual minority status was determined using a single item querying sexual attraction, a core dimension of sexual orientation that adolescents find relevant and easy to answer.40–42 Participants were asked, “Which of the following best describes your sexual orientation?” Response options assessed: (1) attraction to opposite sex, (2) attraction to same sex, (3) attraction to both sexes, and (4) questioning. Adolescents who endorsed sexual attraction to the opposite sex only were coded as heterosexual adolescents, whereas the last three sexual minority subgroups were combined for analyses.
Suicide ideation and behavior (Wave 7).
Three separate questions adapted from the World Mental Health Survey Version of the World Health Organization Composite International Diagnostic Interview43 were asked of all respondents, assessing lifetime suicide ideation, plan, and attempt: “Have you ever seriously thought about committing suicide?” “Have you ever made a plan for committing suicide?” and “Have you ever attempted suicide?” Participants who endorsed lifetime suicide ideation, plan, and/or attempt were asked to report retrospectively the ages at which they first had suicide ideation, plan, and/or attempt.
Demographic covariates.
Demographic covariates included age, race/ethnicity, and family affluence. Race/ethnicity was categorized into four groups: White, African American, Hispanic and other. Participants’ family affluence was assessed using the Health Behaviour School-Aged Family Affluence Scale, which asked about number of family cars and computers, whether participants had their own bedroom, and frequency of family holidays.44
Depressive symptoms (Wave 2).
The 8-item pediatric Patient-Reported Outcomes Measurement Information System (PROMIS) scale,45 which does not include questions on suicidality, was used to measure depressive symptoms (α = .94). Sample items included, “I felt like I couldn’t do anything right,” “I feel sad,” and “I thought that my life was bad.” Response options ranged from 0 (never) to 4 (almost always) in the last 7 days. T-scores were assigned based on published norms.46
Analysis
Lifetime prevalence and mean age of first suicide ideation, plan, and attempt were computed for the overall analytic sample and by sexual minority status. Survival analyses were conducted to test associations of sexual minority status with ages at first suicide ideation, plan, and attempt, as well as progressions from ideation to plan and plan to attempt. The SAS LIFETEST procedure was utilized to generate Kaplan-Meier survival curves by sexual minority status. The SAS SURVEYPHREG procedure was used to fit Cox survival models of time-to-event outcomes adjusting for Wave 2 age, race/ethnicity, family affluence, and depressive symptoms. Survival models were extended to evaluate time-varying associations between sexual minority status and suicide ideation and behaviors (at ages <15 vs. ≥15 years, as the median of onset ages was around 15 years), and in progressions from suicide ideation to plan and from plan to attempt (in the same year vs. 1 or more years since first ideation or plan, as more than half of these transitions occurred in the same year). All analyses accounted for the complex survey design of NEXT; all proportions reported were weighted using the study’s sampling weight which accounted for selection probability into the study and attrition over the follow-up period.
Results
As shown in Table 1, the mean age of the adolescents was 17.2 years old at Wave 2 and 22.6 years old at Wave 7. The sample was 60.8% female and diverse with respect to race/ethnicity, with 5.8% sexual minority adolescents. The lifetime prevalences of suicide ideation, plan, and attempt in the overall sample were 13.8%, 6.0%, and 5.8%, respectively (Table 2). Sexual minority adolescents had higher lifetime prevalence of suicide ideation (26.1% vs. 13.0%), plan (16.6% vs. 5.4%), and attempt (12.0% vs. 5.4%) than heterosexual adolescents. Mean ages of first suicide ideation, plan, and attempt were generally younger among sexual minority than heterosexual adolescents. Though subgroup sizes were smaller, these patterns generally held across adolescents reporting that they were attracted to same sex, both sexes, and questioning (Supplemental Table 1) and among males and females (Supplemental Table 2).
Table 1.
Demographic characteristics of participants in the NEXT Generation Health Study included in the current study (n = 1771)
| Mean (SE) | Frequency | Weighted Percent | |
|---|---|---|---|
| Age at Wave 2 | 17.19 (0.01) | ||
| Age at Wave 7 | 22.63 (0.01) | ||
| Sex | |||
| Male | 717 | 39.2% | |
| Female | 1054 | 60.8% | |
| Race/Ethnicity | |||
| White | 721 | 58.9% | |
| African American | 440 | 19.5% | |
| Hispanic | 530 | 17.3% | |
| Other | 80 | 4.2% | |
| Family Affluence | |||
| Low | 560 | 22.2% | |
| Moderate | 826 | 50.1% | |
| High | 385 | 27.7% | |
| Family Structurea | |||
| Both biological | 874 | 54.8% | |
| Biological and step parent | 240 | 17.3% | |
| Single parent | 318 | 19.7% | |
| Other | 162 | 8.2% | |
| Parental Educationb | |||
| High school or less | 615 | 31.5% | |
| Some college | 614 | 40.5% | |
| Bachelor’s degree or more | 398 | 28.0% | |
| Sexual Minority Status at Wave 2 | |||
| Heterosexual | 1630 | 94.2% | |
| Sexual minority (combined) | 141 | 5.8% | |
| Attracted to the same sex | 33 | 1.5% | |
| Attracted to both males and females | 78 | 3.4% | |
| Questioning | 30 | 0.9% | |
| Depressive Symptoms at Wave 2 | 51.11 (0.28) |
Due to missing data among 177 participants, valid weighted percentages are presented.
Due to missing data among 144 participants, valid weighted percentages are presented.
Table 2.
Lifetime prevalence and age of first suicide ideation, suicide plan, and suicide attempt for the overall sample and by sexual minority status
| Overall (n = 1771) |
Heterosexual (n = 1630) |
Sexual Minority (n = 141) |
||||
|---|---|---|---|---|---|---|
| n | Weighted Percent | n | Weighted Percent | n | Weighted Percent | |
| Lifetime suicide ideation | ||||||
| No | 1563 | 86.2% | 1454 | 87.0% | 109 | 73.9% |
| Yes | 208 | 13.8% | 176 | 13.0% | 32 | 26.1% |
| Lifetime suicide plan | ||||||
| No | 1679 | 94.0% | 1559 | 94.6% | 120 | 83.4% |
| Yes | 92 | 6.0% | 71 | 5.4% | 21 | 16.6% |
| Lifetime suicide attempt | ||||||
| No | 1690 | 94.2% | 1567 | 94.6% | 123 | 88.0% |
| Yes | 81 | 5.8% | 63 | 5.4% | 18 | 12.0% |
| n | Mean (SE) | n | Mean (SE) | n | Mean (SE) | |
| Age of first suicide ideation | 208 | 15.16 (0.20) | 176 | 15.29 (0.22) | 32 | 14.11 (0.58) |
| Age of first suicide plan | 92 | 15.83 (0.35) | 71 | 16.10 (0.40) | 21 | 14.37 (0.56) |
| Age of first suicide attempt | 81 | 15.49 (0.34) | 63 | 15.69 (0.39) | 18 | 14.07 (0.59) |
Kaplan-Meier curves for time to first suicide ideation, plan, and attempt (constructed using ages retrospectively reported at Wave 7) in Figure 1 reveal marked differences between sexual minority and heterosexual participants beginning at age 10, the youngest age reportable on the survey. According to the Cox survival models (Table 3), sexual minority adolescents had earlier onsets of ideation, plan, and attempt than heterosexual peers. Model 1 revealed associations of sexual minority status with ages of first ideation (Hazard Ratio [HR] = 1.77 [95% Confidence Interval [CI], 1.03–3.06]) and plan (HR = 2.69 [95% CI, 1.30–5.56]) but not attempt. Model 2 examined these associations at ages <15 and ≥15 years. Sexual minority disparities in suicide ideation, plan, and attempt were largely phenomena of the youngest ages: hazard ratios were markedly larger below age 15 than at ages 15 or above, and the hazard ratio for suicide attempt at younger (HR = 3.26 [95% CI, 1.25–8.47]) was significantly different from the HR at older ages (HR = 0.59 [95% CI, 0.21–1.66]) (p = 0.02).
Figure 1.
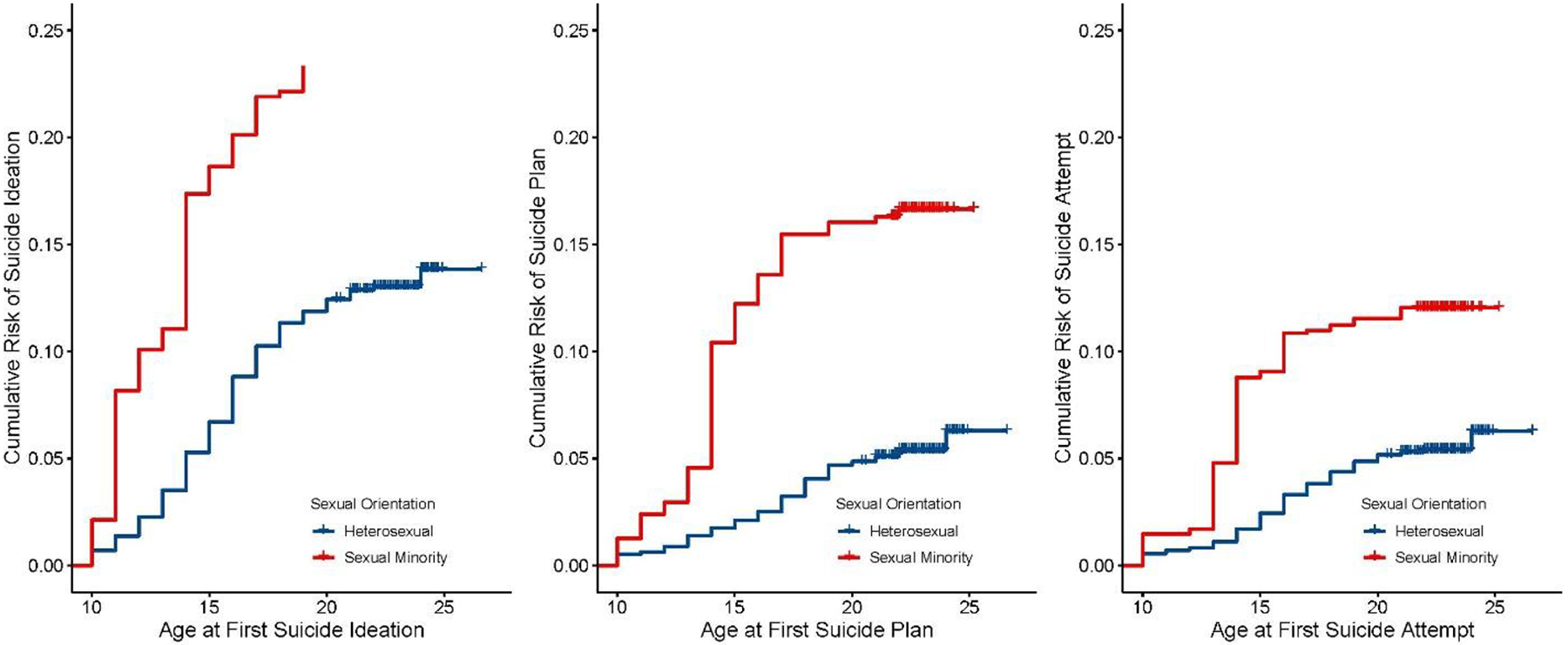
Sexual minority status and time to first age of suicide ideation, plan, and attempt
Kaplan-Meier survival curves showing a more rapid increase in the cumulative risk of suicide ideation, plan, and attempt before age 15 among sexual minority youth compared with heterosexual youth.
Table 3.
Results from survival analyses modeling the effect of sexual minority status on first age of suicide ideation and behavior and progressions from ideation to plan and from plan to attempt
| Model 1 | Model 2 | ||||||
|---|---|---|---|---|---|---|---|
| Full time period | Younger age (below age 15) | Older age (age 15 or above) | Time-varying effect | ||||
| Total | Event | Censored (Weighted %) | HR (95% CI) | HR (95% CI) | HR (95% CI) | p-value | |
| Time to first ideation | 1771 | 208 | 1563 (86.2%) | 1.77 (1.03–3.06) | 2.74 (1.25–6.02) | 1.04 (0.49–2.22) | 0.10 |
| Time to first plan | 1771 | 92 | 1679 (94.0%) | 2.69 (1.30–5.56) | 4.68 (1.81–12.07) | 1.58 (0.53–4.67) | 0.12 |
| Time to first attempt | 1771 | 81 | 1690 (94.2%) | 1.46 (0.66–3.22) | 3.26 (1.25–8.47) | 0.59 (0.21–1.66) | 0.02 |
| Model 1 | Model 2 | ||||||
| Full time period | Early progression (same year) | Late progression (1 or more years) | Time-varying effect | ||||
| Total | Event | Censored (Weighted %) | HR (95% CI) | HR (95% CI) | HR (95% CI) | p-value | |
| Progression from ideation to plan | 208 | 91 | 117 (57.5%) | 1.81 (0.90–3.67) | 2.01 (1.07–3.77) | 1.33 (0.26–6.77) | 0.60 |
| Progression from plan to attempt | 92 | 57 | 35 (36.2%) | 1.07 (0.55–2.07) | 1.08 (0.61–1.91) | 1.02 (0.18–5.85) | 0.10 |
Note. Two models were conducted for each suicide outcome. In Model 1, the time-invariant effect of sexual minority status on the suicide outcome was examined. In Model 2, the time-varying effect of sexual minority status on the suicide outcome was examined. All models adjusted for age, race/ethnicity, family affluence, and depressive symptoms. HR = Hazard Ratio; CI = Confidence Interval. Significant findings are highlighted in bold.
Kaplan-Meier curves for progressions from ideation to plan and plan to attempt also revealed pronounced differences between sexual minority and heterosexual youth (Figure 2). Of the 208 participants who reported suicide ideation, 42.5% (n = 91) progressed to developing suicide plan. Of the 92 participants who reported suicide plan, 63.8% (n = 57) progressed to suicide attempt. Progression from suicide ideation to attempt without any plan was observed in 19 participants (Supplemental Table 3); due to the low frequency, we did not conduct survival analyses of this progression. As shown in Table 3, survival analyses examining the time-varying effect of sexual minority status on progression from ideation to plan similarly revealed stronger association during the same year (HR = 2.01 [95% CI, 1.07–3.77]) than after 1 or more years (HR = 1.33 [95% CI, 0.26–6.77]), indicating that sexual minority adolescents had faster progression from ideation to plan than heterosexual adolescents. Sexual minority and heterosexual adolescents did not differ in the timing of progression from suicide plan to attempt.
Figure 2.
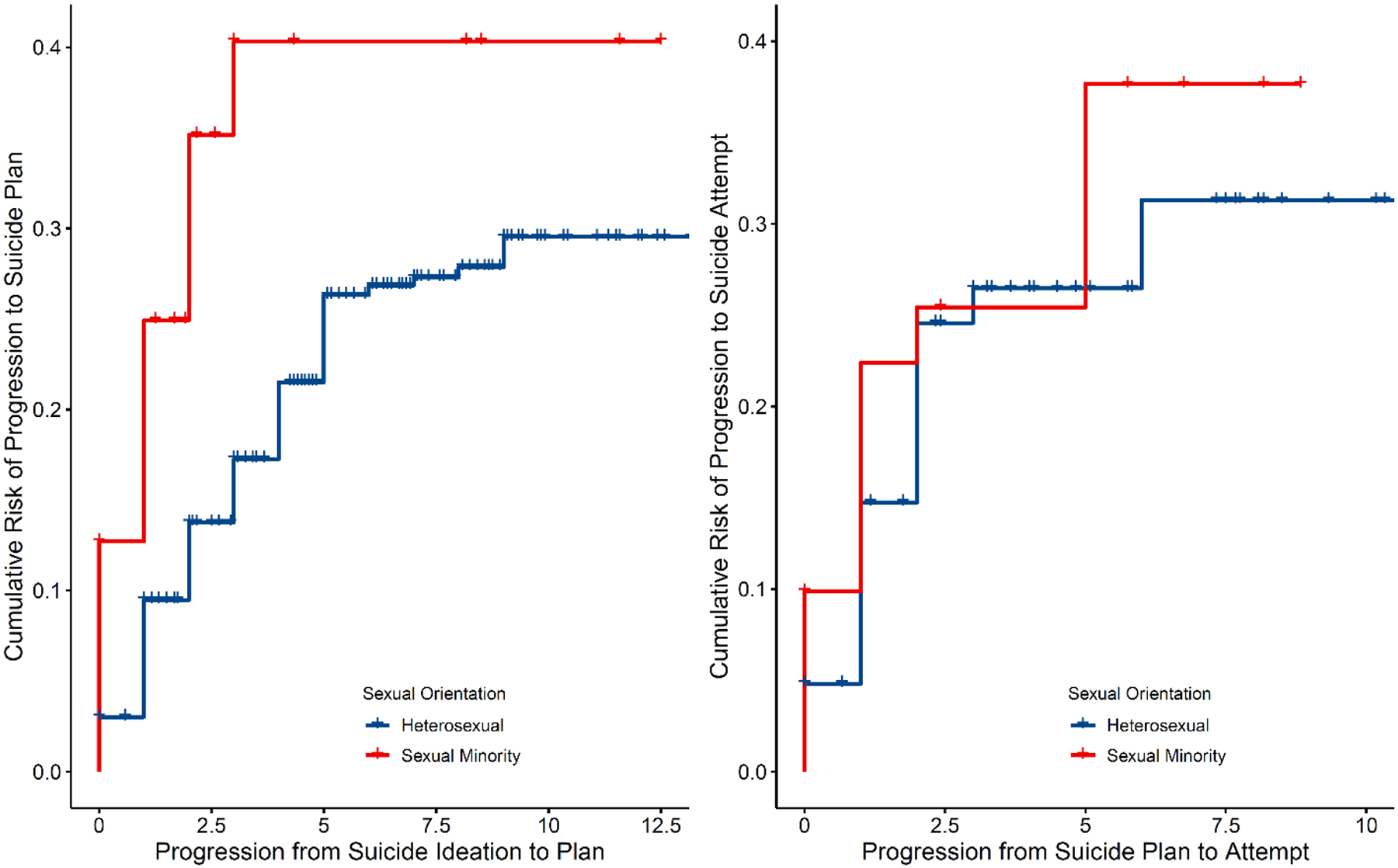
Sexual minority status and progressions from suicide ideation to plan and from suicide plan to attempt
Kaplan-Meier survival curves showing a more rapid increase in the cumulative risk of progression from suicide ideation to plan in the same year among sexual minority youth compared with heterosexual youth.
Discussion
The lifetime prevalences of suicide ideation, plan, and attempt in the NEXT sample (13.8%, 6.0%, and 5.8%, respectively) were comparable to those reported in the NCS-A sample (12.1%, 4.0%, and 4.1%).3 Consistent with prior meta-analyses,10–12 sexual minority adolescents were 2–3 times more likely to report lifetime suicide ideation (26.1% vs. 13.0%), plan (16.6% vs. 5.4%), and attempt (12.0% vs. 5.4%) than heterosexual peers. Because the YRBS assessed past year but not lifetime prevalence or ages of onset suicide ideation and behavior, direct comparisons of suicidality prevalences between NEXT and YRBS are not possible. Nonetheless, the magnitude of disparities in past-year prevalence of suicide attempt was notably greater in the YRBS (24.9% for sexual minority vs. 6.3% for heterosexual adolescents) than in NEXT.22 The higher prevalence of suicide attempt among sexual minorities in the YRBS may be due to concurrent measurement of sexual orientation and suicidality and/or measuring sexual identity rather than attraction. Coming out at an earlier age is a risk factor for suicide attempt.47,48 If adolescents who self-identify as sexual minority are more likely to come out than adolescents who have same-sex attraction,49 the resulting negative reactions from parents and friends may account for the more drastic sexual orientation disparity in YRBS.50–52
As age of onset of suicidality was assessed in NEXT but not in YRBS, our results complement YRBS-based studies13–18 and reveal earlier ages of onset of suicide ideation, plan and attempt among sexual minority adolescents compared to their heterosexual peers. Potential contributors to sexual minority disparities identified in previous studies include child psychopathology and family conflict,53 negative family and school environment,54,55 perceived burdensomeness and social rejection,56,57 and stress associated with the coming out process.49,51,52 Accordingly, it would be beneficial for interventions to address minority-status related risk (e.g., discrimination experiences) and promote protective factors (e.g., family acceptance58 and affirming and supportive school environments59). Furthermore, our results underscore the importance of intervention timing. Indeed, one explanation for the persistently large disparities in suicidality for sexual minority youth is the absence of developmentally timed interventions.60 Assessment of sexual orientation beginning in early- to mid-adolescence may facilitate early identification of sexual minority adolescents at elevated suicide risk, so that timely interventions can be provided.
Sexual minority adolescents also had faster progression from ideation to plan, but not from plan to attempt. The lack of association between sexual minority status and progression from plan to attempt may be due to fewer adolescents with suicide plans and higher clinical severity among suicide planners. In a recent study of adolescents admitted to inpatient psychiatric services, sexual minority adolescents reported higher levels of suicide ideation but not behavior, and no sexual orientation disparities were found in depression, clinical impairment, or life satisfaction.61 More research is needed to understand mental health and treatment related disparities among sexual minority youth in high-risk clinical samples. Conceptualized within the ideation-to-action theoretical framework,39,62 our findings highlight the importance of addressing sexual minority disparities before the onset of suicide ideation and before the progression from suicide ideation to plan.
Data from the NCS-A indicate that 66.4% of adolescents with suicide ideation received mental health specialty treatment in their lifetime, but only 39.6% were treated before the onset of suicide behavior.3 As sexual minority adolescents have earlier onset of suicide ideation and behaviors than heterosexual peers, there is an urgent need to develop and test psychosocial interventions tailored for sexual minority adolescents at earlier developmental stages.63 Sexual minority disparities in mental health symptoms including depression, anxiety and traumatic distress have been found in pediatric primary care,30 making it uniquely suited to identify at-risk sexual minority adolescents and connect them to appropriate resources and treatment.64,65 The AAP recommends providing culturally sensitive office-based care for sexual minority youth, which includes taking a confidential psychosocial history using a gender-neutral approach and following prevention and screening guidelines as outlined in Bright Futures.33,66 To successfully implement these screening procedures, a behavioral health workforce embedded in the primary care setting could increase the capacity for culturally sensitive care and referral to treatment. Greater sensitivity to confidentiality and privacy concerns related to sexual minority status, as well as an openness to discuss minority stressors can foster a supportive environment for sexual minority adolescents.67,68
Study limitations include the classification of sexual minority status based on a single item assessing sexual attraction at one timepoint. This item only categorized youth who experienced some same-sex attraction as sexual minority youth and did not capture asexual youth nor the full spectrum of gender identity. Such classification of sexual minority youth did not account for the multidimensionality of sexual orientation and excluded alternative definitions based on sexual identity and behavior. Second, the number of sexual minority adolescents in NEXT was not large enough to conduct analyses among males and females separately, limiting our ability to examine sex differences in suicide risk associated with sexual minority status. Likewise, small cell sizes for sexual minority subgroups precluded formal analyses to test which subgroup had the highest risk for suicide ideation and behaviors. Larger samples are needed to overcome these limitations. Third, single-item measures of suicide ideation and behavior could lead to under- or over-endorsement of these items.69 For instance, requiring suicide ideation to be “serious” may exclude adolescents with mild, transient, but clinically important ideation, whereas not requiring “intent to die” as part of the suicide attempt definition may lead to over-endorsement of this outcome.69,70 Fourth, the analytic sample consisted of 63.6% of the full NEXT cohort due to attrition and missing data on study variables. Lastly, retrospectively reported age of onset of suicidality could be prone to recall bias (e.g., influenced by current distress) and the timing of suicide ideation and behavior could have preceded the assessment of sexual minority status. Prospective research measuring multiple dimensions of sexual orientation and suicide-related behaviors should begin in early adolescence so as to enable modeling of fluidity of sexual orientation over time. Regional and state differences in acceptance, legal protection, and access to culturally sensitive health care for sexual minority youth should also be examined.
Sexual minority disparities in suicide risk emerge early in, and in some instances before, adolescence and are substantially independent from depressive symptoms. Our study highlights the importance of early identification of sexual minority adolescents who experience elevated suicidality. The inclusion of sexual orientation assessment, psychosocial support, education for families, appropriate treatment referral in pediatric primary care, and consideration of using tele-behavioral health approaches to reach underserved sexual minority youth could inform suicide prevention.31,67 Utilization of evidence-based interventions that are well-timed may help sexual minority adolescents navigate developmental, social, and psychological challenges. Clinical research is needed to evaluate if developmentally-timed interventions improve the effectiveness of suicide risk reduction efforts among sexual minority youth.60,63 Future studies that incorporate multiple levels of data to capture individual-level (e.g., perceived burdensomeness, access to lethal means) and state-level characteristics (e.g., legalization of same-sex marriage, anti-discrimination policies) can improve our understanding of risk and protective factors associated with suicidality among sexual minority youth.
Supplementary Material
What’s Known on This Subject.
Sexual minority youth have greater risk for suicide ideation and behavior than heterosexual youth, but less is known about the timing of first suicidality. A better understanding of the timing of disparities can inform targeted, optimally timed suicide risk screening.
What This Study Adds.
After controlling for depressive symptoms, sexual minority adolescents had earlier onset of suicide ideation, plan, and attempt than heterosexual adolescents. Sexual minority adolescents also progressed faster from suicide ideation to plan but not from plan to attempt, than heterosexual adolescents.
Acknowledgements
The authors would like to thank Gina Ma for her assistance in statistical programming.
Funding/Support:
This project (contract HHSN275201200001I) was supported in part by the Intramural Research Program of the Eunice Kennedy Shriver National Institute of Child Health and Human Development; the National Heart, Lung, and Blood Institute; the National Institute on Alcohol Abuse and Alcoholism; the National Institute on Drug Abuse; and the Maternal and Child Health Bureau of the Health Resources and Services Administration.
Abbreviations:
- AAP
American Academy of Pediatrics
- NEXT
NEXT Generation Health Study
- PROMIS
Patient-Reported Outcomes Measurement Information System
- YRBS
Youth Risk Behavior Survey
Footnotes
Conflict of Interest Disclosures: The authors have no conflict of interest and no financial relationships relevant to this article to disclose.
References
- 1.10 Leading Causes of Death by Age Group, United States - 2017. National Vital Statistics System, National Center for Health Statistics; 2019. https://www.cdc.gov/injury/wisqars/LeadingCauses.html. Accessed 3 January 2020. [Google Scholar]
- 2.Nock MK, Borges G, Bromet EJ, Cha CB, Kessler RC, Lee S. Suicide and suicidal behavior. Epidemiologic Reviews. 2008;30(1):133–154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Nock MK, Green JG, Hwang I, et al. Prevalence, correlates, and treatment of lifetime suicidal behavior among adolescents: results from the National Comorbidity Survey Replication Adolescent Supplement. JAMA Psychiatry. 2013;70(3):300–310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Cha CB, Franz PJ, M. Guzmán E, Glenn CR, Kleiman EM, Nock MK. Suicide among youth–epidemiology,(potential) etiology, and treatment. Journal of Child Psychology and psychiatry. 2018;59(4):460–482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Glenn CR, Lanzillo EC, Esposito EC, Santee AC, Nock MK, Auerbach RP. Examining the course of suicidal and nonsuicidal self-injurious thoughts and behaviors in outpatient and inpatient adolescents. Journal of Abnormal Child Psychology. 2017;45(5):971–983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Goldston DB, Daniel SS, Erkanli A, et al. Suicide attempts in a longitudinal sample of adolescents followed through adulthood: Evidence of escalation. Journal of Consulting and Clinical Psychology. 2015;83(2):253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Reinherz HZ, Tanner JL, Berger SR, Beardslee WR, Fitzmaurice GM. Adolescent suicidal ideation as predictive of psychopathology, suicidal behavior, and compromised functioning at age 30. American Journal of Psychiatry. 2006;163(7):1226–1232. [DOI] [PubMed] [Google Scholar]
- 8.Copeland WE, Goldston DB, Costello EJ. Adult associations of childhood suicidal thoughts and behaviors: A prospective, longitudinal analysis. Journal of the American Academy of Child & Adolescent Psychiatry. 2017;56(11):958–965. e954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Cash SJ, Bridge JA. Epidemiology of youth suicide and suicidal behavior. Current Opinion in Pediatrics. 2009;21(5):613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Marshal MP, Dietz LJ, Friedman MS, et al. Suicidality and depression disparities between sexual minority and heterosexual youth: A meta-analytic review. Journal of Adolescent Health. 2011;49(2):115–123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Di Giacomo E, Krausz M, Colmegna F, Aspesi F, Clerici M. Estimating the risk of attempted suicide among sexual minority youths: A systematic review and meta-analysis. JAMA pediatrics. 2018;172(12):1145–1152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hottes TS, Bogaert L, Rhodes AE, Brennan DJ, Gesink D. Lifetime prevalence of suicide attempts among sexual minority adults by study sampling strategies: A systematic review and meta-analysis. American Journal of Public Health. 2016;106(5):e1–e12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Bostwick WB, Meyer I, Aranda F, et al. Mental health and suicidality among racially/ethnically diverse sexual minority youths. American Journal of Public Health. 2014;104(6):1129–1136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Rosario M, Corliss HL, Everett BG, et al. Sexual orientation disparities in cancer-related risk behaviors of tobacco, alcohol, sexual behaviors, and diet and physical activity: pooled Youth Risk Behavior Surveys. American Journal of Public Health. 2014;104(2):245–254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Turpin RE, Rosario A, Wang MQ. Victimization, depression, and the suicide cascade in sexual minority youth. Journal of Mental Health. 2020:1–9. [DOI] [PubMed] [Google Scholar]
- 16.Bradford J, Mustanski B. Health disparities among sexual minority youth: The value of population data. American Journal of Public Health. 2014;104(2):197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Mustanski B, Van Wagenen A, Birkett M, Eyster S, Corliss HL. Identifying sexual orientation health disparities in adolescents: analysis of pooled data from the Youth Risk Behavior Survey, 2005 and 2007. American Journal of Public Health. 2014;104(2):211–217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Stone DM, Luo F, Ouyang L, Lippy C, Hertz MF, Crosby AE. Sexual orientation and suicide ideation, plans, attempts, and medically serious attempts: Evidence from local youth risk behavior surveys, 2001–2009. American Journal of Public Health. 2014;104(2):262–271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Raifman J, Charlton BM, Arrington-Sanders R, et al. Sexual orientation and suicide attempt disparities among US adolescents: 2009–2017. Pediatrics. 2020;145(3):e20191658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Liu RT, Walsh RF, Sheehan AE, Cheek SM, Carter SM. Suicidal ideation and behavior among sexual minority and heterosexual youth: 1995–2017. Pediatrics. 2020;145(3). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Caputi TL, Smith D, Ayers JW. Suicide risk behaviors among sexual minority adolescents in the United States, 2015. JAMA. 2017;318(23):2349–2351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kann L, McManus T, Harris WA, et al. Youth risk behavior surveillance—United States, 2015. Morbidity and Mortality Weekly Report: Surveillance Summaries. 2016;65(6):1–174. [DOI] [PubMed] [Google Scholar]
- 23.Meyer IH. Prejudice, social stress, and mental health in lesbian, gay, and bisexual populations: conceptual issues and research evidence. Psychol Bull. 2003;129(5):674–697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Fox KR, Hooley JM, Smith DMY, et al. Self-Injurious Thoughts and Behaviors May Be More Common and Severe Among People Identifying as a Sexual Minority. Behav Ther. 2018;49(5):768–780. [DOI] [PubMed] [Google Scholar]
- 25.Mustanski B, Liu RT. A longitudinal study of predictors of suicide attempts among lesbian, gay, bisexual, and transgender youth. Archives of Sexual Behavior. 2013;42(3):437–448. [DOI] [PubMed] [Google Scholar]
- 26.Franklin JC, Ribeiro JD, Fox KR, et al. Risk factors for suicidal thoughts and behaviors: A meta-analysis of 50 years of research. Psychol Bull. 2017;143(2):187–232. [DOI] [PubMed] [Google Scholar]
- 27.Luk JW, Gilman SE, Haynie DL, Simons-Morton BG. Sexual orientation and depressive symptoms in adolescents. Pediatrics. 2018;141(5):e20173309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Hatchel T, Ingram KM, Mintz S, et al. Predictors of Suicidal Ideation and Attempts among LGBTQ Adolescents: The Roles of Help-seeking Beliefs, Peer Victimization, Depressive Symptoms, and Drug Use. Journal of Child and Family Studies. 2019:1–13.33311964 [Google Scholar]
- 29.Luk JW, Parker EO, Richardson LP, McCarty CA. Sexual attraction and experiences in the primary care setting: Examining disparities in satisfaction with provider and health self-efficacy. Journal of Adolescence. 2020;81:96–100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Shearer A, Herres J, Kodish T, et al. Differences in mental health symptoms across lesbian, gay, bisexual, and questioning youth in primary care settings. Journal of Adolescent Health. 2016;59(1):38–43. [DOI] [PubMed] [Google Scholar]
- 31.Luk JW, Gilman SE, Haynie DL, Simons-Morton BG. Sexual orientation differences in adolescent health care access and health-promoting physician advice. Journal of Adolescent Health. 2017;61(5):555–561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Siu AL. Screening for Depression in Children and Adolescents: US Preventive Services Task Force Recommendation Statement. Pediatrics. 2016;137(3):e20154467. [DOI] [PubMed] [Google Scholar]
- 33.COMMITTEE ON PRACTICE AND AMBULATORY MEDICINE and BRIGHT FUTURES PERIODICITY SCHEDULE WORKGROUP. 2017 recommendations for preventive pediatric health care. Pediatrics. 2017;139(4). [DOI] [PubMed] [Google Scholar]
- 34.Cwik MF, O’Keefe VM, Haroz EE. Suicide in the pediatric population: screening, risk assessment and treatment. Int Rev Psychiatry. 2020;32(3):254–264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Milliman CC, Dwyer PA, Vessey JA. Pediatric Suicide Screening: A Review of the Evidence. J Pediatr Nurs. 2020;59:1–9. [DOI] [PubMed] [Google Scholar]
- 36.King CA, Brent D, Grupp-Phelan J, et al. Prospective Development and Validation of the Computerized Adaptive Screen for Suicidal Youth. JAMA Psychiatry. 2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Davis M, Rio V, Farley AM, Bush ML, Beidas RS, Young JF. Identifying Adolescent Suicide Risk via Depression Screening in Pediatric Primary Care: An Electronic Health Record Review. Psychiatr Serv. 2021;72(2):163–168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Arango A, Gipson PY, Votta JG, King CA. Saving Lives: Recognizing and Intervening with Youth at Risk for Suicide. Annu Rev Clin Psychol. 2021. [DOI] [PubMed] [Google Scholar]
- 39.Klonsky ED, Saffer BY, Bryan CJ. Ideation-to-action theories of suicide: A conceptual and empirical update. Current Opinion in Psychology. 2018;22:38–43. [DOI] [PubMed] [Google Scholar]
- 40.Saewyc EM. Research on adolescent sexual orientation: Development, health disparities, stigma, and resilience. Journal of Research on Adolescence. 2011;21(1):256–272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Saewyc EM, Bauer GR, Skay CL, et al. Measuring sexual orientation in adolescent health surveys: Evaluation of eight school-based surveys. Journal of Adolescent Health. 2004;35(4):345.e341–345.e315. [DOI] [PubMed] [Google Scholar]
- 42.Friedman MS, Silvestre AJ, Gold MA, et al. Adolescents define sexual orientation and suggest ways to measure it. Journal of Adolescence. 2004;27(3):303–317. [DOI] [PubMed] [Google Scholar]
- 43.Kessler RC, Üstün TB. The world mental health (WMH) survey initiative version of the world health organization (WHO) composite international diagnostic interview (CIDI). International Journal of Methods in Psychiatric Research. 2004;13(2):93–121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Currie C, Molcho M, Boyce W, Holstein B, Torsheim T, Richter M. Researching health inequalities in adolescents: the development of the Health Behaviour in School-Aged Children (HBSC) family affluence scale. Social Science & Medicine. 2008;66(6):1429–1436. [DOI] [PubMed] [Google Scholar]
- 45.Irwin DE, Stucky B, Langer MM, et al. An item response analysis of the pediatric PROMIS anxiety and depressive symptoms scales. Quality of Life Research. 2010;19(4):595–607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Liu H, Cella D, Gershon R, et al. Representativeness of the patient-reported outcomes measurement information system internet panel. Journal of Clinical Epidemiology. 2010;63(11):1169–1178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Gnan GH, Rahman Q, Ussher G, Baker D, West E, Rimes KA. General and LGBTQ-specific factors associated with mental health and suicide risk among LGBTQ students. Journal of Youth Studies. 2019;22(10):1393–1408. [Google Scholar]
- 48.Plöderl M, Sellmeier M, Fartacek C, Pichler E-M, Fartacek R, Kralovec K. Explaining the suicide risk of sexual minority individuals by contrasting the minority stress model with suicide models. Archives of Sexual Behavior. 2014;43(8):1559–1570. [DOI] [PubMed] [Google Scholar]
- 49.Rotheram-Borus MJ, Fernandez MI. Sexual orientation and developmental challenges experienced by gay and lesbian youths. Suicide and Life-Threatening Behavior. 1995;25:26–34. [PubMed] [Google Scholar]
- 50.D’amico E, Julien D, Tremblay N, Chartrand E. Gay, lesbian, and bisexual youths coming out to their parents: Parental reactions and youths’ outcomes. Journal of GLBT Family Studies. 2015;11(5):411–437. [Google Scholar]
- 51.Puckett JA, Horne SG, Surace F, et al. Predictors of sexual minority youth’s reported suicide attempts and mental health. Journal of Homosexuality. 2017;64(6):697–715. [DOI] [PubMed] [Google Scholar]
- 52.Puckett JA, Woodward EN, Mereish EH, Pantalone DW. Parental rejection following sexual orientation disclosure: Impact on internalized homophobia, social support, and mental health. LGBT health. 2015;2(3):265–269. [DOI] [PubMed] [Google Scholar]
- 53.Janiri D, Doucet GE, Pompili M, et al. Risk and protective factors for childhood suicidality: A US population-based study. Lancet Psychiatry. 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Fergusson DM, Woodward LJ, Horwood LJ. Risk factors and life processes associated with the onset of suicidal behaviour during adolescence and early adulthood. Psychological Medicine. 2000;30(1):23–39. [DOI] [PubMed] [Google Scholar]
- 55.Poštuvan V, Podlogar T, Šedivy NZ, De Leo D. Suicidal behaviour among sexual-minority youth: A review of the role of acceptance and support. The Lancet Child & Adolescent Health. 2019. [DOI] [PubMed] [Google Scholar]
- 56.Hill RM, Pettit JW. Suicidal ideation and sexual orientation in college students: The roles of perceived burdensomeness, thwarted belongingness, and perceived rejection due to sexual orientation. Suicide and Life-Threatening Behavior. 2012;42(5):567–579. [DOI] [PubMed] [Google Scholar]
- 57.Fulginiti A, Goldbach JT, Mamey MR, et al. Integrating minority stress theory and the interpersonal theory of suicide among sexual minority youth who engage crisis services. Suicide and Life-Threatening Behavior. 2020. [DOI] [PubMed] [Google Scholar]
- 58.Ryan C, Russell ST, Huebner D, Diaz R, Sanchez J. Family acceptance in adolescence and the health of LGBT young adults. J Child Adolesc Psychiatr Nurs. 2010;23(4):205–213. [DOI] [PubMed] [Google Scholar]
- 59.Russell ST, Fish JN. Mental Health in Lesbian, Gay, Bisexual, and Transgender (LGBT) Youth. Annu Rev Clin Psychol. 2016;12:465–487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Mustanski B, Espelage DL. Why are we not closing the gap in suicide disparities for sexual minority youth? Pediatrics. 2020;145(3):e20194002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Peters JR, Mereish EH, Krek MA, et al. Sexual orientation differences in non-suicidal self-injury, suicidality, and psychosocial factors among an inpatient psychiatric sample of adolescents. Psychiatry Research. 2020;284:112664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Klonsky ED, Qiu T, Saffer BY. Recent advances in differentiating suicide attempters from suicide ideators. Current Opinion in Psychiatry. 2017;30(1):15–20. [DOI] [PubMed] [Google Scholar]
- 63.Mustanski B. Future directions in research on sexual minority adolescent mental, behavioral, and sexual health. Journal of Clinical Child & Adolescent Psychology. 2015;44(1):204–219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Shain B. Suicide and suicide attempts in adolescents. Pediatrics. 2016;138(1):e20161420. [DOI] [PubMed] [Google Scholar]
- 65.Mehringer JE, Dowshen NL. Opportunities and challenges for previsit screening for sexual and gender identity among adolescents in primary care. Journal of Adolescent Health. 2020;66(2):133–134. [DOI] [PubMed] [Google Scholar]
- 66.Levine D. Committee on Adolescence. Office-based care for lesbian, gay, bisexual, transgender, and questioning youth. Pediatrics. 2013;132(1):e297–313. [DOI] [PubMed] [Google Scholar]
- 67.Fuzzell L, Fedesco HN, Alexander SC, Fortenberry JD, Shields CG. “I just think that doctors need to ask more questions”: Sexual minority and majority adolescents’ experiences talking about sexuality with healthcare providers. Patient Education and Counseling. 2016;99(9):1467–1472. [DOI] [PubMed] [Google Scholar]
- 68.Hubach RD. Disclosure matters: Enhancing patient-provider communication is necessary to improve the health of sexual minority adolescents. Journal of Adolescent Health. 2017;61:537–538. [DOI] [PubMed] [Google Scholar]
- 69.Millner AJ, Lee MD, Nock MK. Single-Item Measurement of Suicidal Behaviors: Validity and Consequences of Misclassification. PLoS One. 2015;10(10):e0141606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Nock MK, Kessler RC. Prevalence of and risk factors for suicide attempts versus suicide gestures: analysis of the National Comorbidity Survey. J Abnorm Psychol. 2006;115(3):616–623. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


