Abstract
Men’s low HPV vaccination uptake and HPV-related disease incidence are public health issues; gendered social–contextual factors likely play a role. In Study 1, college men (N = 130; Mage = 19.55; white = 58.1%) reported their social cognitions (male-referent descriptive norms and prototypes), self-reliance masculinity ideology, and vaccination intentions. In Study 2, college men (N = 106; Mage = 19.32; white = 61.3%) were randomly assigned to receive HPV vaccination information from a man or woman physician-avatar. Descriptive norms and favorable prototypes (bs ≥ .337; ps ≤ .016) were associated with higher HPV vaccination intentions. Men with higher self-reliance masculinity had higher HPV vaccination intentions with a man physician and when they perceived greater vaccination among men (ps ≤ .035). Men with higher self-reliance masculinity are more sensitive to gendered social–contextual effects in HPV vaccination decision-making. Gendered social–contextual factors should be integrated into public health interventions to increase college men’s HPV vaccination uptake.
Keywords: Prototype Willingness Model, Descriptive norms, Masculinity, HPV vaccine, Patient–physician interaction
Introduction
Human papillomavirus (HPV) is the most common STI in the United States (Center for Disease Control, CDC, 2020a; Kreisel et al., 2021). Transmitted through skin-to-skin contact, HPV infection causes serious health outcomes for men including genital warts and penile, anal, and oropharyngeal cancers (CDC, 2020a). HPV outcomes are on the rise among men; oral HPV infection is higher among men (10%) compared to women (3.6%; CDC, 2020b), and men’s HPV-related oropharyngeal cancer incidence now surpasses women’s HPV-related cervical cancer incidence in the U.S. (Berman & Schiller, 2017; CDC, 2020c). While barrier protection (e.g., condom, dental dam) reduces transmission risk, the HPV vaccine is the most effective way to protect men against the most common cancer-causing HPV strains (Giuliano et al., 2011) and has been approved for men and boys (ages 9–26) since 2015 (Daley et al., 2017).
Despite the efficacy and availability of the HPV vaccine, American boys and men have low HPV vaccination uptake (Elam-Evans, Yankey Singleton, et al., 2020; Nelson et al., 2020). College men are a particularly vulnerable population due to both high rates of risky sexual activity (Renfro et al., 2020) and low vaccination rates; only 49–50% of college men are vaccinated for HPV (American College Health Association, 2021; Lee et al., 2018). Even with these challenges, college is an opportune setting to intervene and increase men’s HPV vaccination (Ragan et al., 2018). For the approximately half of college men who arrive to college unvaccinated, those over 18 could consent to vaccination as they become more independent from parental influence and self-reliant in health decisions (DeLauer et al., 2020; Ragan et al., 2018). Theoretically-anchored research is needed to understand college men’s HPV vaccination decision-making and inform interventions.
Social–contextual influence on HPV vaccination and the Prototype Willingness Model
The Prototype Willingness Model is a health behavior theory that addresses social–contextual factors in novel health decision-making (Gibbons et al., 2015). The Prototype Willingness Model centers social cognitions, cognitions about people doing a behavior, as important behavioral drivers, expanding traditional expectancy/value theories which focus primarily on rational cognitions about behavioral consequences (e.g., perceived risk). Descriptive norms capture behavioral prevalence perceptions in social referent groups, and prototypes capture valanced attitudes toward the typical person who engages in the behavior (Gibbons et al., 2015). Descriptive norms and prototypes inform two decision-making cognitions: behavioral intentions and behavioral willingness. Behavioral intentions are predictive of vaccination uptake and reflect a more planful decision cognition. Behavioral willingness represents an openness to engage in a behavior given opportunity and is more predictive of risk behaviors and socially influenced behaviors (Gibbons et al., 2015). Meta-analyses demonstrate the Prototype Willingness Model’s predictive utility for multiple health behaviors across diverse populations (Gibbons et al., 2015; Todd et al., 2016; van Lettow et al., 2016), including sexual health behavior among college students (Blanton et al., 2001; Gebhardt et al., 2009; Gibbons et al., 1998). Additionally, the Prototype Willingness Model has been applied to interventions with college students; for example, oral sex informational interventions led to increased HPV vaccination likelihood and lower behavioral willingness to engage in HPV risk behavior (unprotected oral sex; Stock et al., 2013).
The Prototype Willingness Model provides an appropriate theoretical framework for exploring college men’s HPV-related decisions for several reasons. Among college men, inaccurate beliefs of the HPV vaccine as a female health intervention, peer influence, and physician influence all play a role in HPV vaccination decisions (Daley et al., 2017; Fontenot et al., 2014; Kasymova, 2020). These influences reflect social–contextual factors beyond what is typically captured in expectancy/value models of decision making (e.g., risk perception) and dovetail recent reviews that suggest vaccination decisions are socially informed (Brewer et al., 2017). Second, overestimation of the HPV vaccination as a women’s health intervention (i.e., feminization of HPV, Daley et al., 2017) means that college men’s pursuit of the HPV vaccine subverts typical gender norms, therefore, men’s decisions to pursue HPV vaccination may be influenced by gendered social–contextual factors such as male-referent descriptive norms and prototypes. Third, for unvaccinated college men, HPV vaccination is a new behavior, and social cognitions, rather than rational cognitions (e.g., perceived risk), are generally more predictive for novel behaviors (Gibbons et al., 2015; Pomery et al., 2009). No research has explored social cognitions from the Prototype Willingness Model in the context of college men’s HPV vaccination decisions, but existing research on descriptive norms and prototypes as individual constructs provides insight into possible relationships with decision making cognitions.
Descriptive norms
Descriptive norms capture prevalence perceptions of behavioral participation in social referent groups (e.g., Most of my male friends got the HPV vaccination.) and serve as an important behavioral guide during uncertain or new circumstances, like getting a new vaccine (Cialdini & Goldstein, 2004).1 Descriptive norms relate to behavioral intentions to perform cancer-prevention behaviors, and this relationship is stronger for cancer-prevention behaviors that are less established (Kim et al., 2015). Greater descriptive norms among friends (gender-unspecified) are associated with U.S. college men’s intentions to get the HPV vaccine (Gerend & Barley, 2009), greater girl/woman-referent descriptive norms are associated with HPV vaccination intention among Chinese and American emerging-adult women (Pan et al., 2020), and greater descriptive norms are associated with college students’ intention to get the coronavirus and influenza vaccination (Graupensperger et al., 2021). For men’s health-promotive behavior, descriptive norms of male referent groups are powerful behavioral correlates (Mahalik et al., 2007), and research is needed to determine whether descriptive male norms influence college men’s HPV vaccination decisions.
Prototypes
Prototypes are defined as images of a typical person who engages in a target behavior (e.g., The typical college man who gets the HPV vaccination is healthy and smart.) and predict both health-risk and health-promotive behavior (Gibbons et al., 2015). Favorable health-promotive prototypes (e.g., exercisers, healthy eaters, safe sun/tanning engagers) predict behavior predominantly through increases in behavioral intentions (e.g., COVID-19 prevention behavior; Peterson et al., 2021), but no research has explored the relationship between vaccinator prototypes and vaccination decisions (see van Lettow et al., 2016 for a prototype review). Research on separate variables from the present dataset showed that U.S. college men with more favorable prototypes of men who used male hormonal birth control were more willing to use male hormonal contraception (Peterson et al., 2019). Researchers have called for further investigation on how health-promotive prototype favorability influences health (Gibbons & Gerrard, 2016; van Lettow et al., 2016) and exploring vaccinator prototypes would be a meaningful next step for HPV-prevention.
Physician gender
In addition to social cognitions, gendered contextual factors may play a role in college men’s HPV vaccination decisions. One of the most common and desired sources for HPV information, as well as reasons for HPV vaccination, is physician recommendation (Barrera et al., 2021; Fontenot et al., 2014; Kasymova, 2020). College men may confront opportunities for vaccination in doctor’s offices, and persuasion literature suggests that messenger demographic similarity is an important reliability cue that leads to greater message efficacy in health domains (Kim et al., 2016). For example, gender messenger concordance is one of the most important factors in condom use intervention efficacy (for a review see Durantini et al., 2006). Among university students, those randomly assigned to receive a message encouraging fruit and vegetable consumption from a gender-concordant voice rated the messenger as more reliable (Elbert & Dijkstra, 2015). When the messenger is a physician, physician gender concordance may be particularly influential for college men’s HPV vaccination decisions due to gender stereotypes positioning men as superior for agentic occupations (Eagly et al., 2020).
Outside the lab, a review article of ten studies on dyadic physician–patient gender concordance revealed that men patients exhibit greater ease and discussion with men doctors compared to interactions with women doctors (Sandhu et al., 2009). However, research based on medical records demonstrates that general practitioners are more likely to deliver preventative care, including vaccinations, in appointments when the physician is a woman or the patient is a man (Delpech et al., 2020; Flocke & Gilchrist, 2005; Krähenmann-Müller et al., 2014). While lab and field research findings are somewhat mixed, further experimental research that isolates physician gender and holds dialogue constant would be useful to disentangle whether physician gender alone influences HPV prevention cognitions among college men. Men physicians may be particularly influential for college men’s intention to adhere to a feminized health intervention, like the HPV vaccine.
Masculinity as a moderator of gender contextual effects
Masculinity may moderate pathways between gendered social–contextual factors (i.e., male descriptive norms, male prototypes, men physician messengers) and HPV vaccination decisions. Generally, masculinity is negatively associated with a range of health-enhancing behaviors (Mahalik et al., 2007), including fewer annual physicals as boys transition from adolescence to emerging adulthood (Marcell et al., 2007) and less cancer protection, safe sex, and preventative medical appointments among college men (Mahalik et al., 2006). Among U.S. adult men, masculinity correlates with men physician preference, mostly due to the belief that men doctors are more competent than women doctors (Himmelstein & Sanchez, 2016). Masculinity is multidimensional and includes norms of masculinity ideology relevant to health decision-making such self-reliance masculinity; self-reliance masculinity reflects the normative ideology that independence is demonstrative of manhood (Levant & Richmond, 2007). The male role norm of self-reliance masculinity ideology, hereafter referred to as self-reliance masculinity, is relevant for vaccination decisions as past research shows that self-reliance masculinity is associated with healthcare and help-seeking avoidance (Courtenay, 2000; Wong et al., 2017).
While we are unaware of any research that directly examines whether masculinity moderates the influence of male descriptive norms or male prototypes, theoretical perspectives on men and masculinities (e.g., male reference group identity dependence, precarious manhood) suggest that men’s self-concept of gender is constructed through behavior and is dependent on interactions with and perceptions of other men’s behavior (Courtenay, 2000; Vandello & Bosson, 2013; Wade, 1998). Reference group norms (e.g., men friends/family members, male prototypes) may be especially influential for masculine men, as social constructionism posits that men’s societal pressures to conform to gender norms are restrictive and “fitting in” with the norms of men in salient referent groups is one way to adhere to masculinity (Addis, Reigeluth, & Schwab, 2016; Courtenay, 1998). Male prototypes may also interact with masculinity, and research on men’s help-seeking has called for further integration of masculinity and prototype research, arguing that male prototypes are part of the social construction of masculine behavior (Vogel & Heath, 2016). Thus, the influence of male referent descriptive norms and male prototypes may be stronger for masculine men, but empirical assessment is needed to directly explore theoretical application.
While we are unaware of research that has explored whether masculinity moderates physician gender effects for men’s health decision making, Italian men high in sexism were more tolerant of passively accepting physician recommendations when randomly assigned to an appointment vignette with a typically male (versus female) physician name (Monzani et al., 2020). Although sexism and masculinity are different, they may operate similarly in physician preference, such that men higher in self-reliance masculinity may be less likely to simply accept physician recommendations when their physician is a woman. For men who endorse self-reliance masculinity, gendered social–contextual factors (i.e., male descriptive norms, prototypes, and physicians) may be especially influential in shaping HPV prevention cognitions, but empirical work is needed to directly assess whether self-reliance masculinity moderates the influence of physician gender.
The present study
We examined the influence of gendered social–contextual factors (male descriptive norms, prototypes, and physicians) on unvaccinated college men’s HPV prevention cognitions across two studies. In Study 1, we cross-sectionally investigated whether social cognitions from the Prototype Willingness Model, male descriptive norms and male vaccinator prototypes, were associated with HPV vaccination decision cognitions. In Study 2, we experimentally examined whether HPV vaccination information delivered by a man or woman physician-avatar influenced HPV prevention cognitions. We hypothesized that higher descriptive norms, or perceptions of greater HPV vaccination prevalence among male referent groups, more positive male vaccinator prototypes (Study 1) and receiving HPV vaccination information from a man (versus woman) physician (Study 2) would relate to healthier HPV prevention cognitions. We conducted an exploratory assessment of whether relations between gendered social–contextual factors and HPV prevention cognitions would be stronger among men with higher self-reliance masculinity (Studies 1 and 2).2
Method: Study 1
Participants
Participants were a convenience sample of 171 undergraduate self-identified men recruited from introductory psychology courses via an online sign-up system at a mid-sized, urban, mid-Atlantic university. Participants who self-reported having been diagnosed with HPV (n = 13), already having received the HPV vaccine (n = 38), or as older than 26 (n = 3, above the recommended age for receiving the HPV vaccine), were not included in the analyses. The analytic sample included 130 college men (Mage = 19.55, SD = 2.55, range = 18–26) with diverse racial and ethnic identities (white n = 73 [58.1%]; Asian n = 24 [18.6%], other and/or multiracial n = 12 [9.3%], Latino and/or Hispanic n = 10 [7.8%], and Black and/or African American n = 8 [6.2%]; one participant did not report racial identity). Most men were straight (77.7%) and had had at least one sexual partner in the last three months (70.8%).
Procedure
After signing up, participants were provided a link to an online survey that opened with an informed consent. All students who consented to participate were then directed to the anonymous online survey (SurveyMonkey; Momentive, Inc.) and received one research course credit for participation in the survey, the standard at the University for research taking less than one hour. The survey covered questions on two health topics: HPV vaccination and male hormonal contraception. The present study focuses on the HPV questions; results of the male contraception questions are reported elsewhere (Peterson et al., 2019). To standardize participants’ basic knowledge, the survey began by giving participants brief, factual background information on HPV and the HPV vaccine. Participants then proceeded to respond to Prototype Willingness Model social cognitions (descriptive norms and prototypes) and decision cognitions (intentions and willingness), self-reliance masculinity, and demographic information. At the end of the survey, participants were provided with a link to the CDC website about the HPV vaccine and the university student health center’s phone number to follow up with any HPV questions. All procedures were approved by the university’s Institutional Review Board.
Measures
All Prototype Willingness Model constructs were constructed with fidelity to the validated model, adapted for the HPV vaccine (Gibbons et al., 2015).
Descriptive norms of men’s HPV vaccination
Participants were asked their perceived norms for HPV vaccination with the question “How many male undergraduate [redacted] University students have been vaccinated for HPV?” across five male referent groups that also included: of your male friends, male college students in the U.S., males 18–25 in Washington, DC, and males 18–25 in the U.S. (1 = none; 7 = almost all; Gibbons et al., 2015). The scale was reliable (α = .87), and five items were averaged to create a single descriptive norms construct with higher numbers representing perceptions of higher descriptive norms, or higher prevalence of vaccination in male referent groups.
Male HPV vaccinator prototype
Participants were asked to “Think about the type of guy your age who has received the HPV vaccination” and rated this individual on the following characteristics: attractive, confident, popular, and exciting (1 = not at all; 7 = very; Gibbons et al., 2015). The four items were reliable (a = .88) and were averaged together with higher numbers representing a more positive vaccinator prototype.
Self-reliance masculinity
Self-reliance masculinity was measured using the validated self-reliance subscale from the Male Role Norms Inventory—Revised, a scale that captures norms of traditional masculinity ideologies (Levant et al., 2010). The 7-item self-reliance subscale consisted of statements which included “A man should never doubt his own judgement” and “A man must be able to make his own way in the world” (1 = strongly disagree; 7 = strongly agree). The seven items were reliable (a = .84) and were averaged together to create the MRNI-R masculinity self-reliance scale, with higher scores representing greater self-reliance masculinity ideology.
Behavioral intention to receive the HPV vaccination
Behavioral intention to receive the HPV vaccination included the items: (1) “Do you intend to get the HPV vaccine in the next year?” (1 = I definitely will not; 7 = I definitely will) and (2) “How likely is it that you will get the HPV vaccine in the next year?” (1 = not at all likely; 7 = very likely; Gibbons et al., 2015). The two items were significantly correlated (r = .882, p < .0001) and averaged, with higher numbers representing greater intention.
Behavioral willingness to receive the HPV vaccination
Participants were asked to imagine a series of scenarios in which they were presented with different opportunities to receive the HPV vaccine, conditioned on it being free and available on campus: (1) “How willing would you be to a) Make an appointment to get the vaccine and b) Get the vaccine;” (2) “Suppose that there is a nurse practitioner or doctor at Student Health Services (the student health center on campus) who could administer the HPV vaccine for you at no cost. How willing would you be to a) Consider being vaccinated, b) Make an appointment to get vaccinated, c) Contact the nurse practitioner or doctor to ask more information, and d) Get vaccinated;” (3) “Suppose that tomorrow you receive an email from [redacted] University, listing the schedule to receive the HPV vaccine this month. How willing would you be to attend one of the scheduled vaccination clinics and get vaccinated?” (1 = not at all willing; 7 = very willing; Gibbons et al., 2015). The willingness scale was reliable (a = .96), and the seven items were averaged together to create a willingness construct, with higher numbers representing greater willingness to receive the HPV vaccine.
Demographic information and past behavior
Participants reported their age, race, and ethnicity. Sexual orientation was measured using the Kinsey scale (1 = totally straight; 4 = bisexual; 7 = totally homosexual; Diamond, 1993) and was recoded, such that 0 = totally straight; 1 = not totally straight. College men reported separately on the number of oral, vaginal, and anal sex partners they had in the past 3 months, responses were summed, and the item was recoded such that 0 = no sexual partners in the last 3 months and 1 = one or more sexual partners in the last 3 months. Participants also reported on their current relationship status (1 = no relationship; 7 = very strong commitment; 8 = married).
Results: Study 1
Preliminary bivariate associations
To determine putative covariates, bivariate associations between demographic variables and HPV vaccination intention and willingness were tested using Pearson and point-biserial correlations (Table 1); age, sexual orientation, recent sexual activity, and relationship status were not significantly associated with either HPV vaccination intention or willingness (ps ≥ .093; see Table 1). Race/ethnicity was examined using ANOVAs and neither intention nor willingness varied by race (ps ≥ .790; a two-category recoding of race/ethnicity and point-biserial correlations are included in Table 1). Thus, no covariates were included in the regression to examine Study 1 hypotheses.
Table 1.
Correlations, means, and standard deviations for HPV Prototype Willingness Model constructs, self-reliance masculinity, and demographics
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | Study 2 mean (SD) | Study 2 observed range | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1) Age | – | − .103 | − .239* | .178† | .306** | .074 | .104 | − .096 | .014 | 19.32 (1.299) | 18–25 | |||
| 2) Race and ethnicitya | − .134 | – | − .033 | .003 | .112 | − .052 | − .074 | − .015 | .092 | |||||
| 3) Sexual orientation | − .091 | .043 | – | − .040 | − .108 | .014 | − .447*** | .155 | − .181† | |||||
| 4) Past sexual partners | .167† | .072 | − .103 | – | .526*** | − .079 | .110 | − .060 | .169† | |||||
| 5) Relationship status | .226** | − .148† | − .008 | .381*** | – | − .110 | .020 | − .137 | .149 | 3.14 (2.400) | 1–7 | |||
| 6) HPV vaccination male-descriptive norms | − .127 | − .195* | .155† | − .059 | .007 | – | ||||||||
| 7) HPV male-vaccinator prototype | − .067 | − .095 | − .002 | .089 | .036 | .196* | – | |||||||
| 8) Physician gender—experimental condition | – | .072 | .098 | − .033 | ||||||||||
| 9) Self-reliance masculinity | .055 | − .106 | − .186* | .237** | .068 | .017 | .040 | – | − .117 | .211* | 4.31 (1.163) | 1–7 | ||
| 10) HPV vaccination behavioral intention | .028 | − .065 | .148† | − .047 | .018 | .259** | .327*** | − .055 | – | − .092 | 3.73 (1.616) | 1–7 | ||
| 11) HPV vaccination behavioral willingness | .089 | .019 | .031 | − .083 | − .100 | .090 | .298** | − .109 | .627*** | – | ||||
| 12) Unprotected sex behavior willingness | – | 3.76 (1.522) | 1–7 | |||||||||||
| Study 1 mean (SD) | 19.65 (1.584) | 2.86 (2.352) | 2.62 (1.030) | 4.17 (1.137) | 4.29 (1.206) | 3.32 (1.707) | 4.55 (1.644) | |||||||
| Study 1 observed range | 18–26 | 1–8 | 1–6 | 1–7 | 1–7 | 1–7 |
Study 1 (N = 130) is presented at the bottom left of the diagonal and Study 2 (N = 106) is presented at the top right of the diagonal
Sexual orientation 0 = straight, 1 = not straight; Past sexual partners 0 = no sexual partners in the past 3 months, 1 = one or more sexual partners in the past 3 months; Race and ethnicity 0 = Person of Color, 1 = white; Physician gender (experimental condition) 0 = woman physician, 1 = man physician
†p < .10, *p < .05, **p < .01, ***p < .0001
aRace and ethnicity analyses were run on 129 participants in Study 1
Prior to hypothesis testing, we examined bivariate relations of Prototype Willingness Model and self-reliance masculinity variables. Descriptive norms (r = .259, p = .001) and prototype favorability (r = .327, p < .0001) were associated with behavioral intention to receive the HPV vaccine, but only prototypes were associated with vaccination willingness (r = .298, p = .001; Table 1). Self-reliance masculinity was not significantly correlated with either Prototype Willingness Model social (norms and prototypes) or decision (intention and willingness) cognitions (ps ≥ .217; Table 1).
Hypothesis testing
A hierarchical linear regression was conducted to examine the main effect of descriptive norms, prototypes, and self-reliance masculinity on HPV vaccination decision cognitions and whether masculinity moderated the relation between social cognitions and HPV vaccination decision cognitions. To minimize multicollinearity, continuous variables were centered prior to analyses and included on the first step, the second step contained the cross-product interaction terms for centered versions of descriptive norms and prototypes by centered masculinity (Aiken & West, 1991; Fekedulegn, Colbert, Hicks, & Schuckers, 2002).
HPV vaccination behavioral intention
Similar to bivariate correlations, main effects emerged for descriptive norms and prototypes such that higher descriptive norms (b = .337, SE = .139, t = 2.431, p = .016) and more favorable prototypes (b = .435, SE = .126, t = 3.460, p = .001) were both significantly associated with higher HPV vaccination intention. Interaction analyses revealed a significant moderation of descriptive norms by self-reliance masculinity (p = .035; see Fig. 1), but not prototype (p = .705). No main effect emerged for self-reliance masculinity (p = .398). The overall model was significant F(5, 129) = 5.649, p < .0001, R2 = .186.
Fig. 1.
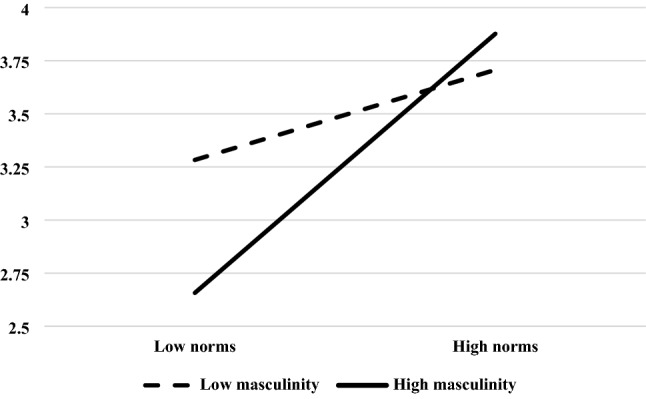
Study 1—Behavioral intention to receive the HPV vaccine as a function of descriptive norms of HPV vaccination in male referent groups and self-reliance masculinity. Overall interaction is significant (p = .035)
Probing the descriptive norms by self-reliance masculinity interaction
Follow-up Johnson–Neyman regions of significance moderation analyses were conducted in PROCESS v3.5 to investigate the descriptive norms by self-reliance masculinity interaction (Model 1, 95% confidence intervals, 5000 bootstrap samples, intention as Y, descriptive norms as X, self-reliance masculinity as W, vaccinator prototypes as covariate). Results indicate that self-reliance masculinity moderated the influence of descriptive norms on vaccination intentions at middle and higher values of self-reliance masculinity. Johnson–Neyman regions of significance results showed that the top 60.77% of self-reliance masculinity scores significantly moderated the effect of descriptive norms on intentions, such that higher descriptive norms were related to greater HPV vaccination intentions.
To further explore the interaction, we reversed the moderator and examined whether descriptive norms moderated the relationship between self-reliance masculinity and vaccination intention. Johnson–Neyman regions of significance results showed that the bottom 25.38% of descriptive norms scores significantly moderated the effect of self-reliance masculinity on intentions, such that higher self-reliance masculinity was related to lower vaccination intentions. Figure 1 shows a visualization of the interaction using 1 standard deviation above and below the mean. Taken together, these analyses indicate that men with higher self-reliance masculinity are more influenced by male descriptive norms.
HPV vaccination behavioral willingness
Like for behavioral intention, main effects emerged for prototypes such that more favorable prototypes were significantly associated with higher willingness to vaccinate for HPV (b = .428, SE = .124, t = 3.440, p = .001). However, the main effect for descriptive norms did not replicate, and no significant relationships emerged for self-reliance masculinity moderation or main effects (ps ≥ .109). The overall model was significant F(5, 129) = 3.225, p = .009, R2 = .115.
Method: Study 2
Participants
Participants in Study 2 were also a convenience sample of 154 college men drawn from a larger, parent study of college women and men recruited from undergraduate psychology courses at the same university.3 Replicating Study 1, men who self-reported being diagnosed with HPV (n = 13), having already received the HPV vaccine (n = 17), or over the age of 26 (n = 2) were excluded from the analyses. Additionally, participants who failed the manipulation check were also excluded from the analyses (i.e., reported the gender of the physician avatar at the end of the study inaccurately, n = 27). Applying the exclusion criteria resulted in a final analytic sample of 106 college men (Mage = 19.32 years, SD = 1.299, range = 18–25 years) of diverse racial and ethnic identities (white n = 65 [61.3%], Asian n = 12 [11.3%], other and/or multiracial n = 11 [10.4%], Latino and/or Hispanic n = 10 [9.4%], and Black and/or African American n = 8 [7.5%]). Most men were straight (77.4%) and had had at least one sexual partner in the last three months (66.0%).
Procedure and measures
Participants were invited to participate in a research study via an online sign-up system investigating the effects of physician–patient interactions and personal factors on healthcare decisions. The study was administered through an anonymous online survey which opened with an informed consent (SurveyMonkey; Momentive, Inc.). Participants received one research course credit for participation in the survey, the standard at the University for research that takes less than one hour. All participants who consented to participate were then directed to the survey which began with self-reliance masculinity, the potential moderator. Then participants were randomly assigned to receive identical HPV information from either a man or woman physician avatar, reported on dependent variables (intention to get the HPV vaccine and willingness to engage in sex without barrier protection), filled out past behavior and demographic information, and the survey concluded with manipulation checks.
Pre-manipulation measure: self-reliance masculinity
Participants first reported on self-reliance masculinity, which was replicated exactly from Study 1 using the self-reliance subscale from the Male Role Norms Inventory-Revised (Levant et al., 2010). The scale was again reliable (a = .79), and items were averaged together.
Stimuli development and experimental manipulation
After reporting on self-reliance masculinity, participants were randomly assigned to either a woman (n = 50; 47.2%) or man (n = 56; 52.8%) physician avatar photograph paired with identical, factual information about HPV risks and prevention behavior (risk of contracting HPV from sex without barrier protection and the availability of vaccination). To develop the stimuli, we recruited and photographed two volunteer models, a man and woman. To minimize differences other than gender, both models were white young adults with blonde/brown hair, dressed similarly in dark blue shirts, with neutral expressions in front of a white background. Images were edited using Microsoft Paint to be similar sizes and face frame (see Fig. 2 for example of physician stimuli).,4,5
Fig. 2.

Example physician avatar photos for woman (left) and man (right) avatar physicians
During the experiment, participants were prompted to envision that they were attending a doctor’s appointment and were presented with the randomly assigned physician avatar with identical physician comments:
The HPV vaccine is available for men and women; and I wanted to inform you of some of the key features of the vaccine as well as ways in which you can benefit from this vaccine.
HPV is a sexually transmitted disease; related to genital warts and cancer in both men and women. HPV is spread through sexual contact—oral, vaginal, anal—and is spread through skin-to-skin contact. Barrier protection, such as condoms, reduces risk but does not eliminate the risk of contracting HPV. I can provide you with the HPV vaccination today if you wish.
Post-manipulation measures
Following the experimental manipulation, participants reported on dependent variables related to their reception of the message derived from the validated Prototype Willingness Model (Gibbons et al., 2015), demographic information and past behavior questions, and manipulation checks.
Behavioral intention to receive the HPV vaccination
Behavioral intention to receive the HPV vaccination was assessed similarly to Study 1, but adapted slightly for the hypothetical scenario. Participants were asked about their immediate intentions to vaccinate (e.g., “Do you intend to get the HPV vaccine?”; Gibbons et al., 2015). In Study 2, the two items were significantly correlated (r = .829, p < .0001) and averaged together. Additionally, due the immediate nature of the experimental scenario, immediate intentions were relevant to the study, while willingness at future clinics was not; thus, HPV vaccination willingness was not assessed in Study 2.
Behavioral willingness to engage in sex without barrier protection
To examine whether physician avatars’ message regarding HPV-risk behaviors was influenced by physician gender, we measured participants' HPV risk willingness (unprotected sex willingness; Gibbons et al., 2015; Stock et al., 2013). Willingness to engage in unprotected sex was assessed by presenting participants with a scenario asking them to imagine they met someone at a party for the first time, and both the participant and the person they met want to have sex with each other, but neither have any available contraceptive (e.g., condom) of any kind. Participants were then asked how willing they would be to “Stay at his/her apartment and have sex;” “Go ahead but use a method like withdrawing the man’s penis before ejaculation;” and “Engage in oral sex without barrier protection” (1 = not at all willing; 7 = very willing). The three items were reliable (a = .73) and averaged together, with higher numbers signifying greater willingness for sex without barrier protection.
Demographic information and past behavior
Participants reported on their age, race and ethnicity, sexual orientation, relationship status, partners in the past three months, and HPV vaccination and diagnoses history, which were all measured and coded identically to Study 1.
Manipulation checks and stimuli assessment
As an attention and manipulation check, at the conclusion of the survey participants were asked to report whether the physician who provided them with the HPV message earlier in the study was a man or woman. Additionally, participants rated the attractiveness of the physician with the following item “Consider the image of the physician you saw when reviewing the information at the beginning of the survey about HPV—Please rate the attractiveness of this physician” (1 = not attractive; 7 = highly attractive).
Debrief
Upon completion of the survey, participants were informed that the purpose of the study was to explore whether aspects of physician appearance resulted in differences in health care perceptions and that the physician image may have been different for other study participants. Participants were then provided with a link to the CDC website about the HPV vaccine and the university student health center’s phone number to follow up with any HPV questions. All procedures were approved by the university’s Institutional Review Board.
Results: Study 2
Preliminary bivariate associations
As in Study 1, Table 1 presents the means, standard deviations, and Pearson and point-biserial correlation for the associations of all variables. To determine putative covariates, bivariate associations between demographic variables and HPV vaccination intention and unprotected sex willingness were examined; age, sexual orientation, recent sexual activity, and relationship status were not significantly associated with either vaccination intention or unprotected sex willingness (ps ≥ .064, see Table 1). Race/ethnicity was examined using ANOVAs and neither intention nor willingness varied by race (ps ≥ .584; a two-category recoding of race/ethnicity and point-biserial correlations are included in Table 1). Thus, no covariates were included in the regressions testing Study 2 hypotheses. No evidence of randomization effects emerged across physician gender condition for any demographic variables (ps ≥ .261, see Table 1, column 8) or self-reliance masculinity (p = .465, see Table 1, column 9, row 8).
To get a sense of overall patterns prior to hypothesis testing, we examined point-biserial and correlative relationships for the experimental condition, self-reliance masculinity, and vaccination intention and unprotected sex willingness. No bivariate associations emerged for physician gender condition on dependent variables (ps ≥ .319; Table 1). Self-reliance masculinity did not significantly associate with HPV vaccination intention (p = .230), but did associate with higher unprotected sex willingness (r = .211, p = .030; Table 1).
Hypothesis testing
A hierarchical linear regression was conducted to examine the main effect of physician gender (0 = woman physician; 1 = man physician) and self-reliance masculinity on HPV vaccination intentions and willingness to have sex without barrier protection and whether self-reliance masculinity moderated any physician gender effects. To minimize multicollinearity and build the interaction term, self-reliance masculinity was centered prior to analyses and included on the first step, the second step contained the cross-product physician gender by self-reliance masculinity term (Aiken & West, 1991; Fekedulegn, Colbert, Hicks, & Schuckers, 2002).
HPV vaccination behavioral intention
Main effects did not emerge for either physician gender or self-reliance masculinity (ps > .202), however there was a significant interaction between the two (p = .021; see Fig. 3) that paralleled self-reliance masculinity’s influence on descriptive norms in Study 1. The overall model was significant F(3, 105) = 2.770, p = .045, R2 = .075.6
Fig. 3.
Study 2—Behavioral intention to receive the HPV vaccine as a function of physician gender and self-reliance masculinity. Overall interaction is significant (p = .021)
Probing the physician gender by self-reliance masculinity interaction
Follow up Johnson–Neyman regions of significance moderation analyses were conducted in PROCESS v3.5 to probe the physician gender by self-reliance masculinity interaction (Model 1, 95% confidence intervals, 5000 bootstrap samples, intention as Y, physician gender as X, self-reliance masculinity as W). Results suggested that self-reliance masculinity moderated the influence of physician gender on intentions at higher values of self-reliance masculinity. Johnson–Neyman regions of significance results showed that the top 31.13% of self-reliance masculinity scores significantly moderated the effect of physician gender on intentions, such that the man physician condition was related to higher HPV vaccination intentions.
To explore the effect of self-reliance masculinity with each physician gender condition, we split the sample on condition and reran the regression dropping the physician gender condition and interaction term. Analyses within condition revealed that when men received information from a man physician, self-reliance masculinity was not significantly related to vaccination intention (p = .491), but when they received information from a woman physician, self-reliance masculinity was significantly related to vaccination intention such that higher self-reliance masculinity was associated with lower vaccination intentions (b = − .481, SE = .163, t = − 2.938, p = .005). Figure 1 shows a graph of the interaction using 1 standard deviation above and below the mean. Taken together, these analyses indicate that college men higher in self-reliance masculinity have lower HPV vaccination intention when they receive the vaccination recommendation from a woman physician; when college men receive the vaccination recommendation from a woman physician, higher self-reliance masculinity associates with lower vaccination intentions.
Sex without barrier protection behavioral willingness
No main effect of physician gender emerged for men’s willingness to engage in sex without barrier protection (p = .615) and self-reliance masculinity did not moderate the influence of physician gender (p = .759), but higher self-reliance masculinity was associated with greater willingness to have unprotected sex (b = .280, SE = 0.126, t = 2.219, p = .029). Overall, the model was not significant F(3, 105) = 1.699, p = .172, R2 = .048.,7
Discussion
The goal of the present research was to investigate whether gendered social–contextual factors—including descriptive norms, prototypes, and physician gender—associated with unvaccinated college men’s HPV prevention cognitions and to explore whether self-reliance masculinity moderated these effects. Results support the hypothesis that social cognitions, higher descriptive norms in male referent groups and more positive male vaccinator prototypes, are associated with HPV vaccination intentions. Positive HPV vaccinator prototypes related to greater HPV vaccination willingness and higher self-reliance masculinity related to greater unprotected sex willingness, but other findings did not replicate to behavioral willingness for either HPV vaccination or unprotected sex. No main effects emerged for physician gender. Self-reliance masculinity exacerbated social–contextual effects in similar patterns; higher self-reliance masculinity associated with higher HPV vaccination intention when men perceived that more men got the HPV vaccine (higher descriptive norms) and when a man (versus woman) physician recommended they get an HPV vaccine.
This is the first published study that we are aware of that applied the Prototype Willingness Model to vaccination decisions. Our results demonstrate that social cognitions from the Prototype Willingness Model associate with HPV vaccination intention among college men, expanding the application of the Prototype Willingness Model from college student condom and birth control use (Blanton et al., 2001; Gebhardt et al., 2009; Gibbons et al., 1998), demonstrating that vaccination intentions are also socially informed (Brewer et al., 2017). The findings that male-referent descriptive norms associate with HPV vaccination intentions parallel earlier research on college students demonstrating that descriptive norms of friends associate with HPV vaccination intention (Gerend & Barley, 2009) and coronavirus and influenza vaccination (Graupensperger et al., 2021) and that descriptive norms associate with health promotive intentions (McEachan et al., 2016). Descriptive norms of male referent groups are powerful health behavior correlates (Mahalik et al., 2007); the present results show that descriptive norms associate with behavioral intentions, and future longitudinal research could explore whether the influence of descriptive norms on men’s health behavior is mediated through planful intentions. Descriptive norms related to other men function as “social proof” (Cialdini & Goldstein, 2004), providing cues for demonstrating manhood (Courtenay, 2000; Vandello & Bosson, 2013; Wade, 1998), and inform men’s behavioral decision-making to align with their perceptions of the group. However, descriptive norms did not significantly relate to vaccination willingness. Given that vaccination willingness was captured in a more specified context (e.g., Student Health Center clinics) compared to intentions, future research could reexamine descriptive norms to determine whether situationally congruent descriptive norms (e.g., Most of my male classmates have gone to the HPV vaccination clinics at Student Health Services) are influential for willingness. Further research on college men’s vaccination and men’s participation in feminized health behavior should include male descriptive norms (Courtenay, 1998).
Favorable male prototypes also related to higher HPV vaccination decision cognitions. Results add to past meta-analyses that demonstrate the impact favorable health-promotive prototypes have on intentions (van Lettow et al., 2016), integrate male prototypes into masculinity research (Vogel & Heath, 2016), and address calls for increased research on prototypes and health promotion (Gibbons & Gerrard, 2016; van Lettow et al., 2016). College men may engage in a social comparison process by using perceptions of a confident and exciting male vaccinator prototype to inform a goal-state, thus integrating these characteristics into sense of self (van Lettow et al., 2016). Past research demonstrates stronger relations between health-promotive prototypes and behavioral intention (versus willingness; van Lettow et al., 2016), but the present findings mirror recent research on infectious disease, which demonstrates that prototypes contribute to both intention and willingness for COVID-19 prevention behaviors (Peterson et al., 2021). In sum, the influence of descriptive norms and prototypes suggest that the Prototype Willingness Model is a useful framework for exploring social influence on vaccination decision cognitions.
Results from Studies 1 and 2 demonstrate that self-reliance masculinity moderated social–contextual effects on HPV vaccination intention. Men higher in self-reliance masculinity were more sensitive to gendered social–contextual factors. Highly masculine men may be particularly attuned to demonstrating manhood through behavior and conform to behaviors in male reference groups (e.g., men friends/family members; Courtenay, 1998). These are the first results that we are aware of that experimentally examined the impact of physician gender on men’s acceptance of physician vaccination recommendations; our main effect hypothesis that men would have higher vaccination intention and lower HPV-risk sex willingness with men physicians was not supported, however the impact of physician gender was moderated by self-reliance masculinity.
Men with higher self-reliance masculinity had greater vaccination intentions when they received HPV vaccination information from a man physician. These results parallel past research demonstrating that more masculine and sexist men prefer men physicians (Himmelstein & Sanchez, 2016; Monzani et al., 2020) and suggest that messenger similarity effects (Durantini et al., 2006) may be particularly relevant for masculine men in sexual health domains. Research exploring a different health outcome, college men’s willingness to disclose symptoms in a medical appointment, showed the opposite, such that men higher in masculinity were more willing to disclose medical symptoms when randomly assigned to a woman (versus man) experimenter (Himmelstein & Sanchez, 2016). With man physicians, masculine men may want to appear more “tough” during symptom disclosure to preserve precarious manhood (a belief that masculinity can be “lost” through engaging in behaviors inconsistent with masculinity; Vandello & Bosson, 2013), but draw upon stereotyped beliefs and adhere to a man physician’s recommendations over a woman physician’s recommendations. Physician gender did not influence behavioral willingness for unprotected sex, rather more masculine men were more willing to engage in sex that would put them at-risk for HPV, consistent with former research on masculinity and risky sexual behavior (Mahalik et al., 2006; Pleck et al., 1993; Shearer et al., 2005). In sum, differing results for vaccination intention and risky sex willingness in Study 2 suggest that gender concordant medical interactions could lead self-reliant masculine men to greater adherence to medical recommendations, but masculinity may be a more important predictor for behavior that puts men at risk for HPV outside of the physician’s office.
Limitations
The present study has limitations in design and sample that warrant further discussion. First, Study 1 was cross-sectional and correlational, which limits directional and causal inference. Future research should examine whether the influence of descriptive norms and prototypes on behavioral cognitions follows through to vaccination uptake. Longitudinal research should be paired with experimental manipulations of descriptive norms (low versus high; Buunk et al., 2002; Hershey et al., 1994) and prototypes (unfavorable versus favorable; van Lettow et al., 2016) to enhance directional and causal inference. Second, while a benefit of Study 2 was an experimental design that isolated physician gender, ruling out potential confounds (e.g., voice tone, attractiveness), we did not capture stereotyped beliefs (e.g., ratings of the physician’s competence, agency, or warmth), which precludes direct examination of the mediating processes driving masculine men’s reduced intentions to adhere to medical recommendations from a woman physician (i.e., Jain, 2020). More research is needed to understand the mechanisms driving the masculinity-moderated physician gender effect.
Third, while we were specifically interested in college men’s experience, generalizability to the broader population of college men is limited. Data were collected from a PWI, and men identifying as African American and/or Black and Hispanic and/or Latino were underrepresented. Racial/ethnic differences did not emerge for HPV vaccination intention, but these findings should be interpreted with caution due to small group sizes and contrasting research demonstrating higher HPV vaccination rates among African American and/or Black college men (Kasymova, 2020). Fourth, we did not capture whether men identified as cisgender men or transgender men, which is an important direction for future research (Bednarczyk et al., 2017) as transgender men experience facilitators and barriers to HPV vaccination at the personal, provider, and systems level (Apaydin et al., 2018). Future research should examine rural, public, religious, community college, HBCU, and MSI institutions to ensure broader inclusion in research on social–contextual factors, masculinity, and college men’s HPV vaccination decision making (see Kasymova, 2020).
Future directions
Future research with a more diverse sample of college men and additional physician stimuli would expand the present analyses to encompass intersectional aspects of physician identity concordance. For example, among Latinas with lower earned trust in the medical system, ethnicity concordance is the most important physician factor over gender concordance when deciding to get the HPV vaccine (Hernandez et al., 2017). African American men randomly assigned to receive preventative care from an African American man doctor consented to greater preventative treatment (including flu vaccination) compared to men doctors of other races and ethnicities (Alsan et al., 2019). Together, these results illustrate the dimensionality of physician gender effects when applying an intersectional framework. Also, if physician gender effects in the field tend to be more strongly driven by the experience of physician communication, rather than gender identity alone, future research would benefit from immersive gender manipulations. To address both intersectionality and immersion, future research could harness Facial Image Manipulation (Sutherland et al., 2017), virtual reality physician manipulation (e.g., Persky et al., 2013), or in-person experimenter manipulations (e.g., Himmelstein & Sanchez, 2016) to capture the influence of both physician gender and race or ethnicity in health decision making contexts (see Jain, 2020).
In addition to expanding the findings on the physician-gender effects, research to understand the social forces that shape descriptive norms and prototypes is important. Social media is a source of norms messaging (Xiao & Borah, 2020). For example, college students' normative perceptions of the HPV vaccination uptake can be informed by bloggers (Lee & Su, 2020), and descriptive norms of female-referent social media users influence Chinese and American women’s HPV vaccination intentions (Pan et al., 2020). Health behavior prototypes are informed by culture, advertisements, and media representation/social media (Dal Cin et al., 2009; Gibbons et al., 2010; Litt & Stock, 2011), and male prototypes may be a particularly salient pathway through which cultural standards of masculinity inform individual behavioral masculinity construction (Vogel & Heath, 2016). Future studies should continue to investigate whether social media influences college men’s HPV vaccination decisions via masculinity, norms, and prototypes.
Applications
This study contributes to growing evidence that masculinity is an important contextual factor that influences college men’s sensitivity to experiences with healthcare providers (Himmelstein & Sanchez, 2016) and responsiveness to health interventions (Walsh & Stock, 2012), and findings should be integrated into public health initiatives. Messaging and physician-focused HPV vaccination interventions increased HPV vaccination uptake in a university system (Gerend et al., 2020a, 2020b) and low-cost text interventions enhanced HPV vaccination uptake among queer emerging-adult men (Gerend et al., 2020a, 2020b); these interventions could be adapted to address gender contextual-factors. While men higher in masculinity generally participate less in health prevention behavior (Mahalik et al., 2007), our results reveal that contextual effects (e.g., higher norms in male referent groups) associate with healthier vaccination cognitions for all college men, but are especially influential for men with greater self-reliance masculinity. Health messaging for college men and the HPV vaccine should harness social–contextual influence, such as highlighting men’s participation, promoting positive male prototypes, including messages with both men and women physicians, and positioning HPV vaccination as a form of self-reliance by taking charge of one’s health.
Conclusions
HPV persists as one of the most prevalent, yet preventable, sexual health risks in the U.S. (CDC, 2020a; Kreisel et al., 2021). The HPV vaccine is an outstanding medical achievement, being the first vaccine that prevents cancer, yet boys and men are under-vaccinated and increasingly at-risk for HPV-related cancers (Attia et al., 2018). The ongoing coronavirus pandemic has exacerbated low HPV vaccine uptake among adolescent boys, and there is an urgent need to get HPV vaccination “back on track” and increase vaccination catch-up efforts among emerging-adult men (Gilkey et al., 2020). Creative interventions are urgently needed to achieve the Healthy People 2030 target of 80% HPV vaccination coverage (Office of Disease Prevention & Health Promotion, 2021). Our research provides insight surrounding gendered social–contextual factors important to the most hesitant, yet promising, groups for intervention—college men. Addressing the gender disparity head on by harnessing social–contextual influence via descriptive norms, prototypes, and gender-diverse physicians has the potential to rectify HPV vaccination under-uptake, prevent cancer, and save men’s lives.
Acknowledgements
The authors thank Lauren Thomas and Drs. Caitlin Kennedy, Janine Beha, and Michelle Stock for their assistance with study development and Dr. Sarah DiMuccio for providing comments on the manuscript draft. This paper is dedicated to Jason Hartwig; his willingness to volunteer as stimuli led to a first date, falling in love, and marriage to the study’s primary author, who is available to attend to correspondence on this study.
Funding
There was no funding source for this project.
Data availability
Data are available from the corresponding author.
Declarations
Conflict of interest
We have no conflicts of interest to disclose.
Human and animal rights
All aspects of this research were approved by the George Washington University Institutional Review Board.
Informed consent
All participants provided informed consent.
Footnotes
Throughout the manuscript when we refer to descriptive norms the terms “higher/greater” or “lower” are meant to capture behavioral prevalence perceptions (e.g., “higher descriptive norms for HPV vaccination” represents higher perceived prevalence of HPV vaccination in a referent group).
Data collection for the two studies overlapped and analyses testing hypotheses occurred after data collection concluded for both studies. Study 1 hypotheses were analyzed first, followed by Study 2.
The larger, parent study explored the influence of physician characteristics for college students who identified as men and women (N = 460). The present study focused on questions specified for the men subsample, specifically how self-reliance masculinity may influence HPV vaccination cognitions and thus, the present study focuses exclusively on the subsample of college men (N = 154).
A second version of each physician stimuli were edited to slightly alter symmetry of facial features, creating two stimuli versions within each gender condition. The original purpose of manipulating facial features was to examine facial symmetry as an additional randomly assigned condition. No significant effects for physician facial symmetry emerged for either dependent variable (ps ≥ .220) and thus, the two versions of each physician gender stimuli were collapsed within their respective conditions and function as stimulus sampling in the present study (Wells & Windschitl, 1999). To further confirm that versions of the stimuli did not influence the results, analyses were repeated including stimuli symmetry version as a control variable, stimuli symmetry did not influence any results, and reports of each analysis are included in Results footnotes.
In the present analytic sample of college men, the woman physician was rated as more attractive than the man physician (p = .002), which is somewhat expected given that most of the sample was straight. In the larger, parent study of college men and women who passed the manipulation check, no significant differences emerged for attractiveness ratings between the man and woman stimuli (p = .385). To rule out the possibility that any significant physician gender effects were driven by attractiveness, analyses were repeated substituting attractiveness ratings for condition; no main effects or interactions emerged, and reports of each analysis are included in Results footnotes.
The analysis was repeated including physician facial stimuli as a control variable, functional results (i.e., direction and significance of the effects) were the same. The analysis was repeated substituting the continuous participant rating of physician attractiveness for physician gender condition. No significant effects emerged for either attractiveness or the attractiveness by masculinity interaction (ps ≥ .281).
The analysis was repeated including physician facial stimuli as a control variable, functional results (i.e., direction and significance of the effects) were the same. The analysis was repeated substituting the continuous participant rating of physician attractiveness for physician gender condition. No significant effects emerged for either attractiveness or the attractiveness by masculinity interaction (ps ≥ .298).
Study 1 participants responded to questions on a separate health topic and these findings are reported elsewhere (Peterson et al., 2019); the present data have not been previously reported beyond conference posters. Jennifer Orr and Sasha Rogelberg completed most of their work on this project while affiliated with Bryn Mawr College.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Jennifer A. Orr and Sasha D. Rogelberg contributed equally to this manuscript and their names are presented alphabetically as co-second authors.
References
- Addis, M. E., Reigeluth, C. R., & Schwab, J. R. (2016). Social norms, social constructionism, and the psychology of men and masculinity. In APA handbook of men and masculinities. (pp. 81–104). American Psychological Association.
- Aiken, L. S., & West, S. G. (1991). Multiple regression: Testing and interpreting interactions. Sage.
- Alsan M, Garrick O, Graziani G. Does diversity matter for health? Experimental evidence from Oakland. American Economic Review. 2019;109:4071–4111. doi: 10.1257/aer.20181446. [DOI] [Google Scholar]
- American College Health Association. (2021). American College Health Association-National College Health Assessment III: Undergraduate Student Reference Group Data Report Fall 2020. American College Health Association. https://www.acha.org/NCHA/ACHA-NCHA_Data/Publications_and_Reports/NCHA/Data/Reports_ACHA-NCHAIII.aspx
- Apaydin KZ, Fontenot HB, Shtasel D, Dale SK, Borba CPC, Lathan CS, Panther L, Mayer KH, Keuroghlian AS. Facilitators of and barriers to HPV vaccination among sexual and gender minority patients at a Boston community health center. Vaccine. 2018;36:3868–3875. doi: 10.1016/j.vaccine.2018.02.043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Attia AC, Wolf J, Núñez AE. On surmounting the barriers to HPV vaccination: We can do better. Annals of Medicine. 2018;50:209–225. doi: 10.1080/07853890.2018.1426875. [DOI] [PubMed] [Google Scholar]
- Barrera J, Greene S, Petyak E, Kenneson S, McGill E, Howell H, Billing D, Taylor S, Ewing A, Cull J. Reported rationales for HPV vaccination vs. Non-vaccination among undergraduate and medical students in South Carolina. Journal of American College Health. 2021;69:185–189. doi: 10.1080/07448481.2019.1659279. [DOI] [PubMed] [Google Scholar]
- Bednarczyk RA, Whitehead JL, Stephenson R. Moving beyond sex: Assessing the impact of gender identity on human papillomavirus vaccine recommendations and uptake among a national sample of rural-residing LGBT young adults. Papillomavirus Research. 2017;3:121–125. doi: 10.1016/j.pvr.2017.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berman TA, Schiller JT. Human papillomavirus in cervical cancer and oropharyngeal cancer: One cause, two diseases. Cancer. 2017;123:2219–2229. doi: 10.1002/cncr.30588. [DOI] [PubMed] [Google Scholar]
- Blanton H, VandenEijnden RJJM, Buunk BP, Gibbons FX, Gerrard M, Bakker A. Accentuate the negative: Social images in the prediction and promotion of condom use. Journal of Applied Social Psychology. 2001;31:274–295. doi: 10.1111/j.1559-1816.2001.tb00197.x. [DOI] [Google Scholar]
- Brewer NT, Chapman GB, Gibbons FX, Gerrard M, McCaul KD, Weinstein ND. Meta-analysis of the relationship between risk perception and health behavior: The example of vaccination. Health Psychology. 2007;26:136–145. doi: 10.1037/0278-6133.26.2.136. [DOI] [PubMed] [Google Scholar]
- Brewer NT, Chapman GB, Rothman AJ, Leask J, Kempe A. Increasing vaccination: Putting psychological science into action. Psychological Science in the Public Interest. 2017;18:149–207. doi: 10.1177/1529100618760521. [DOI] [PubMed] [Google Scholar]
- Buunk BP, Van Den Eijnden RJJM, Siero FW. The double-edged sword of providing information about the prevalence of safer sex. Journal of Applied Social Psychology. 2002;32:684–699. doi: 10.1111/j.1559-1816.2002.tb00237.x. [DOI] [Google Scholar]
- Center for Disease Control, CDC. (2020a). Basic information about HPV and cancer. Retrieved October 10, 2021, from https://www.cdc.gov/cancer/hpv/basic_info/index.htm.
- Center for Disease Control, CDC. (2020b). HPV and oropharyngeal cancer. Retrieved October 10, 2021, from https://www.cdc.gov/cancer/hpv/basic_info/hpv_oropharyngeal.htm
- Center for Disease Control, CDC. (2020c). How many cancers are linked with HPV each year? Retrieved October 10, 2021, from https://www.cdc.gov/cancer/hpv/statistics/cases.htm
- Cialdini RB, Goldstein NJ. Social influence: Compliance and conformity. Annual Review of Psychology. 2004;55:591–621. doi: 10.1146/annurev.psych.55.090902.142015. [DOI] [PubMed] [Google Scholar]
- Courtenay WH. College men’s health: An overview and a call to action. Journal of American College of Health. 1998;46:279–290. doi: 10.1080/07448489809596004. [DOI] [PubMed] [Google Scholar]
- Courtenay WH. Behavioral factors associated with disease, injury, and death among men: Evidence and implications for prevention. The Journal of Men’s Studies. 2000;9:81–142. doi: 10.3149/jms.0901.81. [DOI] [Google Scholar]
- Dal Cin S, Worth KA, Gerrard M, Gibbons FX, Stoolmiller M, Wills TA, Sargent JD. Watching and drinking: Expectancies, prototypes, and friends’ alcohol use mediate the effect of exposure to alcohol use in movies on adolescent drinking. Health Psychology. 2009;28:473–483. doi: 10.1037/a0014777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Daley EM, Vamos CA, Thompson EL, Zimet GD, Rosberger Z, Merrell L, Kline NS. The feminization of HPV: How science, politics, economics and gender norms shaped U.S. HPV Vaccine Implementation. Papillomavirus Research. 2017;3:142–148. doi: 10.1016/j.pvr.2017.04.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DeLauer V, McGill-O’Rourke A, Gordon C, Hamilton N, Desruisseaux R, DuarteCanela M, Heyer A, Macksoud K. Human papillomavirus and health decision-making: Perceptions and accountability in college. Health Education Journal. 2020;79:46–57. doi: 10.1177/0017896919862309. [DOI] [Google Scholar]
- Delpech R, Bloy G, Panjo H, Falcoff H, Ringa V, Rigal L. Physicians’ preventive practices: More frequently performed for male patients and by female physicians. BMC Health Services Research. 2020;20:331. doi: 10.1186/s12913-020-05136-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Diamond M. Homosexuality and bisexuality in different populations. Archives of Sexual Behavior. 1993;22:291–310. doi: 10.1007/BF01542119. [DOI] [PubMed] [Google Scholar]
- DiMuccio SH, Yost MR, Helweg-Larsen M. A qualitative analysis of perceptions of precarious manhood in U.S. and Danish men. Psychology of Men and Masculinity. 2017;18:331–340. doi: 10.1037/men0000062. [DOI] [Google Scholar]
- Durantini MR, Albarracín D, Mitchell AL, Earl AN, Gillette JC. Conceptualizing the influence of social agents of behavior change: A meta-analysis of the effectiveness of HIV-prevention interventionists for different groups. Psychological Bulletin. 2006;132:212–248. doi: 10.1037/0033-2909.132.2.212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eagly AH, Nater C, Miller DI, Kaufmann M, Sczesny S. Gender stereotypes have changed: A cross-temporal meta-analysis of U.S. public opinion polls from 1946 to 2018. American Psychologist. 2020;75:301–315. doi: 10.1037/amp0000494. [DOI] [PubMed] [Google Scholar]
- Elam-Evans LD, Yankey D, Singleton JA, et al. National, regional, state, and selected local area vaccination coverage among adolescents aged 13–17 years—United States, 2019. Morbidity and Mortality Weekly Report. 2020;69:1109–1116. doi: 10.15585/mmwr.mm6933a1externalicon. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elbert SP, Dijkstra A. Source reliability in auditory health persuasion: Its antecedents and consequences. Journal of Applied Biobehavioral Research. 2015;20:211–228. doi: 10.1111/jabr.12038. [DOI] [Google Scholar]
- Fekedulegn, B. D., Colbert, J. J., Hicks, J. R., & Schuckers, M. E. (2002). Coping with multicollinearity: An example on application of principal components regression in dendroecology (p. 43). U.S. Department of Agriculture, Forest Service, Northeastern Research Station.
- FitzGerald S, Cornally N, Hegarty J. Men’s perspectives on cancer prevention behaviors associated with HPV. Psycho-Oncology. 2018;27:484–491. doi: 10.1002/pon.4515. [DOI] [PubMed] [Google Scholar]
- Flocke SA, Gilchrist V. Physician and patient gender concordance and the delivery of comprehensive clinical preventive services. Medical Care. 2005;43:486–492. doi: 10.1097/01.mlr.0000160418.72625.1c. [DOI] [PubMed] [Google Scholar]
- Fontenot HB, Collins Fantasia H, Charyk A, Sutherland MA. Human papillomavirus (HPV) risk factors, vaccination patterns, and vaccine perceptions among a sample of male college students. Journal of American College of Health. 2014;62:186–192. doi: 10.1080/07448481.2013.872649. [DOI] [PubMed] [Google Scholar]
- Gebhardt WA, van Empelen P, van Beurden D. Predicting preparatory behaviours for condom use in female undergraduate students: A one-year follow-up study. International Journal of STD and AIDS. 2009;20:161–164. doi: 10.1258/ijsa.2008.008233. [DOI] [PubMed] [Google Scholar]
- Gerend MA, Barley J. Human papillomavirus vaccine acceptability among young adult men. Sexually Transmitted Diseases. 2009;36:58–62. doi: 10.1097/OLQ.0b013e31818606fc. [DOI] [PubMed] [Google Scholar]
- Gerend MA, Madkins K, Crosby S, Korpak AK, Phillips GL, Bass M, Houlberg M, Mustanski B. Evaluation of a text messaging-based Human Papillomavirus Vaccination intervention for young sexual minority men: Results from a pilot randomized controlled trial. Annals of Behavioral Medicine. 2020 doi: 10.1093/abm/kaaa056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gerend MA, Murdock C, Grove K. An intervention for increasing HPV vaccination on a university campus. Vaccine. 2020;38:725–729. doi: 10.1016/j.vaccine.2019.11.028. [DOI] [PubMed] [Google Scholar]
- Gibbons FX, Gerrard M. Reactions to the meta-analyses of the Prototype Willingness Model. Health Psychology Review. 2016;10:44–46. doi: 10.1080/17437199.2015.1116020. [DOI] [PubMed] [Google Scholar]
- Gibbons FX, Gerrard M, Blanton H, Russell DW. Reasoned action and social reaction: Willingness and intention as independent predictors of health risk. Journal of Personality and Social Psychology. 1998;74:1164–1180. doi: 10.1037//0022-3514.74.5.1164. [DOI] [PubMed] [Google Scholar]
- Gibbons, F. X., Gerrard, M., Stock, M. L., & Finneran, S. D. (2015). The Prototype/Willingness Model. In M. Connor & P. Norman (Eds.), Predicting health behavior: Research and practice with social cognition models (3rd ed., pp. 189–224). Cambridge University Press.
- Gibbons FX, Pomery EA, Gerrard M, Sargent JD, Weng C-Y, Wills TA, Kingsbury J, Dal Cin S, Worth KA, Stoolmiller M, Tanski SE, Yeh H-C. Media as social influence: Racial differences in the effects of peers and media on adolescent alcohol cognitions and consumption. Psychology of Addictive Behaviors. 2010;24:649–659. doi: 10.1037/a0020768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gilkey MB, Bednarczyk RA, Gerend MA, Kornides ML, Perkins RB, Saslow D, Sienko J, Zimet GD, Brewer NT. Getting Human Papillomavirus Vaccination back on track: Protecting our national investment in Human Papillomavirus Vaccination in the COVID-19 era. Journal of Adolescent Health. 2020;67:633–634. doi: 10.1016/j.jadohealth.2020.08.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Giuliano AR, Palefsky JM, Goldstone S, Moreira ED, Penny ME, Aranda C, Vardas E, Moi H, Jessen H, Hillman R, Chang Y-H, Ferris D, Rouleau D, Bryan J, Marshall JB, Vuocolo S, Barr E, Radley D, Haupt RM, Guris D. Efficacy of quadrivalent HPV vaccine against HPV infection and disease in males. The New England Journal of Medicine. 2011;364:401–411. doi: 10.1056/NEJMoa0909537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Graupensperger S, Abdallah DA, Lee CM. Social norms and vaccine uptake: College students’ COVID vaccination intentions, attitudes, and estimated peer norms and comparisons with influenza vaccine. Vaccine. 2021;39:2060–2067. doi: 10.1016/j.vaccine.2021.03.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hernandez ND, Daley EM, Young L, Kolar SK, Wheldon C, Vamos CA, Cooper D. HPV vaccine recommendations: Does a health care provider’s gender and ethnicity matter to unvaccinated Latina college women? Ethnicity and Health. 2017 doi: 10.1080/13557858.2017.1367761. [DOI] [PubMed] [Google Scholar]
- Hershey JC, Asch DA, Thumasathit T, Meszaros J, Waters VV. The roles of altruism, free riding, and bandwagoning in vaccination decisions. Organizational Behavior and Human Decision Processes. 1994;59:177–187. doi: 10.1006/obhd.1994.1055. [DOI] [Google Scholar]
- Himmelstein MS, Sanchez DT. Masculinity in the doctor’s office: Masculinity, gendered doctor preference and doctor–patient communication. Preventive Medicine. 2016;84:34–40. doi: 10.1016/j.ypmed.2015.12.008. [DOI] [PubMed] [Google Scholar]
- Jain P. The stereotype content model as an explanation of biased perceptions in a medical interaction: Implications for patient–provider relationship. Health Communication. 2020 doi: 10.1080/10410236.2020.1816311. [DOI] [PubMed] [Google Scholar]
- Johnson C, Ogletree R. Knowledge and behavioral intention related to HPV vaccination among male college students. American Journal of Health Education. 2017;48:320–330. doi: 10.1080/19325037.2017.1343159. [DOI] [Google Scholar]
- Kasymova S. Human papillomavirus (HPV) and HPV vaccine knowledge, the intention to vaccinate, and HPV vaccination uptake among male college students. Journal of American College Health. 2020 doi: 10.1080/07448481.2020.1785471. [DOI] [PubMed] [Google Scholar]
- Kim HK, Kim S, Niederdeppe J. Scientific uncertainty as a moderator of the relationship between descriptive norm and intentions to engage in cancer risk-reducing behaviors. Journal of Health Communication. 2015;20:387–395. doi: 10.1080/10810730.2014.977465. [DOI] [PubMed] [Google Scholar]
- Kim M, Shi R, Cappella JN. Effect of character–audience similarity on the perceived effectiveness of antismoking PSAs via engagement. Health Communication. 2016;31:1193–1204. doi: 10.1080/10410236.2015.1048421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krähenmann-Müller S, Virgini VS, Blum MR, da Costa BR, Collet T-H, Martin Y, Cornuz J, Zimmerli L, Gaspoz J-M, Bauer DC, Kerr EA, Aujesky D, Rodondi N. Patient and physician gender concordance in preventive care in university primary care settings. Preventive Medicine. 2014;67:242–247. doi: 10.1016/j.ypmed.2014.08.004. [DOI] [PubMed] [Google Scholar]
- Kreisel KM, Spicknall IH, Gargano JW, Lewis FMT, Lewis RM, Markowitz LE, Roberts H, Johnson AS, Song R, St. Cyr, S. B., Weston, E. J., Torrone, E. A., & Weinstock, H. S. Sexually transmitted infections among US women and men: Prevalence and incidence estimates, 2018. Sexually Transmitted Diseases. 2021;48:208–214. doi: 10.1097/OLQ.0000000000001355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee HY, Lust K, Vang S, Desai J. Male undergraduates’ HPV vaccination behavior: Implications for achieving HPV-associated cancer equity. Journal of Community Health. 2018;43:459–466. doi: 10.1007/s10900-018-0482-4. [DOI] [PubMed] [Google Scholar]
- Lee TK, Su LY-F. When a personal HPV story on a blog influences perceived social norms: The roles of personal experience, framing, perceived similarity, and social media metrics. Health Communication. 2020;35:438–446. doi: 10.1080/10410236.2019.1567440. [DOI] [PubMed] [Google Scholar]
- Levant RF, Rankin TJ, Williams CM, Hasan NT, Smalley KB. Evaluation of the factor structure and construct validity of scores on the Male Role Norms Inventory—Revised (MRNI-R) Psychology of Men and Masculinity. 2010;11:25–37. doi: 10.1037/a0017637. [DOI] [Google Scholar]
- Levant R, Richmond K. A review of research on masculinity ideologies using the Male Role Norms Inventory. The Journal of Men’s Studies. 2007;15:130–146. doi: 10.3149/jms.1502.130. [DOI] [Google Scholar]
- Litt DM, Stock ML. Adolescent alcohol-related risk cognitions: The roles of social norms and social networking sites. Psychology of Addictive Behaviors. 2011;25:708–713. doi: 10.1037/a0024226. [DOI] [PubMed] [Google Scholar]
- Mahalik JR, Burns SM, Syzdek M. Masculinity and perceived normative health behaviors as predictors of men’s health behaviors. Social Science and Medicine. 2007;64:2201–2209. doi: 10.1016/j.socscimed.2007.02.035. [DOI] [PubMed] [Google Scholar]
- Mahalik JR, Lagan HD, Morrison JA. Health behaviors and masculinity in Kenyan and US male college students. Psychology of Men and Masculinity. 2006;7:191–202. doi: 10.1037/1524-9220.7.4.191. [DOI] [Google Scholar]
- Marcell AV, Ford CA, Pleck JH, Sonenstein FL. Masculine beliefs, parental communication, and male adolescents’ health care use. Pediatrics. 2007;119:e966–e975. doi: 10.1542/peds.2006-1683. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McEachan R, Taylor N, Harrison R, Lawton R, Gardner P, Conner M. Meta-analysis of the reasoned action approach (RAA) to understanding health behaviors. Annals of Behavioral Medicine. 2016;50:592–612. doi: 10.1007/s12160-016-9798-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MicrosoftCorps. (n.d.). Microsoft Paint.
- Momentive, Inc. (n.d.). SurveyMonkey. https://www.surveymonkey.com/
- Monzani D, Vergani L, Pizzoli SFM, Marton G, Mazzocco K, Bailo L, Messori C, Pancani L, Cattelan M, Pravettoni G. Sexism interacts with patient–physician gender concordance in influencing patient control preferences: Findings from a vignette experimental design. Applied Psychology: Health and Well-Being. 2020;12:471–492. doi: 10.1111/aphw.12193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nelson NP, Weng MK, Hofmeister MG, Moore KL, Doshani M, Kamili S, Koneru A, Haber P, Hagan L, Romero JR, Schillie S, Harris AM. Prevention of Hepatitis A virus infection in the United States: Recommendations of the Advisory Committee on Immunization Practices, 2020. MMWR Recommendations and Reports. 2020;69:1–38. doi: 10.15585/mmwr.rr6905a1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Office of Disease Prevention and Health Promotion. (2021). Vaccination. In Healthy People 2030. U.S. Department of Health and Human Services. Retrieved October 10, 2021, from https://health.gov/healthypeople/objectives-and-data/browse-objectives/vaccination/increase-proportion-adolescents-who-get-recommended-doses-hpv-vaccine-iid-08
- Pan S, Zhang D, Zhang J. Caught in the crossfire: How contradictory information and norms on social media influence young women’s intentions to receive HPV vaccination in the United States and China. Frontiers in Psychology. 2020 doi: 10.3389/fpsyg.2020.548365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Persky S, Kaphingst KA, Allen VC, Senay I. Effects of patient–provider race concordance and smoking status on lung cancer risk perception accuracy among African-Americans. Annals of Behavioral Medicine. 2013;45:308–317. doi: 10.1007/s12160-013-9475-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peterson LM, Campbell MAT, Laky ZE. The next frontier for men’s contraceptive choice: College men’s willingness to pursue male hormonal contraception. Psychology of Men and Masculinities. 2019;20:226–237. doi: 10.1037/men0000174. [DOI] [Google Scholar]
- Peterson LM, Helweg-Larsen M, DiMuccio S. Descriptive norms and prototypes predict COVID-19 prevention cognitions and behaviors in the United States: Applying the Prototype Willingness Model to pandemic mitigation. Annals of Behavioral Medicine. 2021 doi: 10.1093/abm/kaab075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pleck JH, Sonenstein FL, Ku LC. Masculinity ideology: Its impact on adolescent males’ heterosexual relationships. Journal of Social Issues. 1993;49:11–29. doi: 10.1111/j.1540-4560.1993.tb01166.x. [DOI] [Google Scholar]
- Pomery EA, Gibbons FX, Reis-Bergan M, Gerrard M. From willingness to intention: Experience moderates the shift from reactive to reasoned behavior. Personality and Social Psychology Bulletin. 2009;35:894–908. doi: 10.1177/0146167209335166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ragan KR, Bednarczyk RA, Butler SM, Omer SB. Missed opportunities for catch-up human papillomavirus vaccination among university undergraduates: Identifying health decision-making behaviors and uptake barriers. Vaccine. 2018;36:331–341. doi: 10.1016/j.vaccine.2017.07.041. [DOI] [PubMed] [Google Scholar]
- Ratanasiripong NT. Factors related to Human Papillomavirus (HPV) vaccination in college men. Public Health Nursing. 2015;32:645–653. doi: 10.1111/phn.12198. [DOI] [PubMed] [Google Scholar]
- Renfro KJ, Haderxhanaj L, Coor A, Eastman-Mueller H, Oswalt S, Kachur R, Habel MA, Becasen JS, Dittus PJ. Sexual-risk and STI-testing behaviors of a national sample of non-students, two-year, and four-year college students. Journal of American College Health. 2020 doi: 10.1080/07448481.2020.1756830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sandhu H, Adams A, Singleton L, Clark-Carter D, Kidd J. The impact of gender dyads on doctor–patient communication: A systematic review. Patient Education and Counseling. 2009;76:348–355. doi: 10.1016/j.pec.2009.07.010. [DOI] [PubMed] [Google Scholar]
- Shearer CL, Hosterman SJ, Gillen MM, Lefkowitz ES. Are traditional gender role attitudes associated with risky sexual behavior and condom-related beliefs? Sex Roles. 2005;52:311–324. doi: 10.1007/s11199-005-2675-4. [DOI] [Google Scholar]
- Stock ML, Peterson LM, Houlihan AE, Walsh LA. Influence of oral sex and oral cancer information on young adults’ oral sexual-risk cognitions and likelihood of HPV vaccination. The Journal of Sex Research. 2013;50:95–102. doi: 10.1080/00224499.2011.642904. [DOI] [PubMed] [Google Scholar]
- Sutherland CAM, Rhodes G, Young AW. Facial image manipulation: A tool for investigating social perception. Social Psychological and Personality Science. 2017;8:538–551. doi: 10.1177/1948550617697176. [DOI] [Google Scholar]
- Todd J, Kothe E, Mullan B, Monds L. Reasoned versus reactive prediction of behaviour: A meta-analysis of the prototype willingness model. Health Psychology Review. 2016;10:1–24. doi: 10.1080/17437199.2014.922895. [DOI] [PubMed] [Google Scholar]
- van Lettow B, de Vries H, Burdorf A, van Empelen P. Quantifying the strength of the associations of prototype perceptions with behaviour, behavioural willingness and intentions: A meta-analysis. Health Psychology Review. 2016;10:25–43. doi: 10.1080/17437199.2014.941997. [DOI] [PubMed] [Google Scholar]
- Vandello JA, Bosson JK. Hard won and easily lost: A review and synthesis of theory and research on precarious manhood. Psychology of Men and Masculinity. 2013;14:101–113. doi: 10.1037/a0029826. [DOI] [Google Scholar]
- Vogel, D. L., & Heath, P. J. (2016). Men, masculinities, and help-seeking patterns. In APA handbook of men and masculinities (pp. 685–707). American Psychological Association.
- Wade JC. Male reference group identity dependence: A theory of male identity. The Counseling Psychologist. 1998;26:349–383. doi: 10.1177/0011000098263001. [DOI] [Google Scholar]
- Walsh LA, Stock ML. UV photography, masculinity, and college men’s sun protection cognitions. Journal of Behavioral Medicine. 2012;35:431–442. doi: 10.1007/s10865-011-9372-2. [DOI] [PubMed] [Google Scholar]
- Wells GL, Windschitl PD. Stimulus sampling and social psychological experimentation. Personality and Social Psychology Bulletin. 1999;25:1115–1125. doi: 10.1177/01461672992512005. [DOI] [Google Scholar]
- Wheldon CW, Daley EM, Walsh-Buhi ER, Baldwin JA, Nyitray AG, Giuliano AR. An integrative theoretical framework for HPV vaccine promotion among male sexual minorities. American Journal of Men’s Health. 2018;12:1409–1420. doi: 10.1177/1557988316652937. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wong YJ, Ho M-HR, Wang S-Y, Miller ISK. Meta-analyses of the relationship between conformity to masculine norms and mental health-related outcomes. Journal of Counseling Psychology. 2017;64:80–93. doi: 10.1037/cou0000176. [DOI] [PubMed] [Google Scholar]
- Xiao X, Borah P. Do norms matter? Examining norm-based messages in HPV vaccination promotion. Health Communication. 2020 doi: 10.1080/10410236.2020.1770506. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data are available from the corresponding author.



