Abstract
Background
Postoperative delirium (POD) is a common complication among elderly patients after surgery. It is unclear whether the systemic immune-inflammation index (SII) can be a predictor of POD. We explored the prognostic value of the SII in predicting POD in elderly patients undergoing non-neurosurgery and non-cardiac surgery in a large retrospective cohort.
Methods
We enrolled elderly patients undergoing non-neurosurgery and non-cardiac surgery between January 2014 and August 2019. Univariate and multivariate logistic regression analyses were performed to explore the correlation between POD and the SII value as both a continuous and categorical variable. Then, propensity score matching (PSM) analysis was applied to eliminate the confounding effect of covariates and prove our results. Subgroup analyses were then performed to discover the association between the SII and POD in different subgroups.
Results
A total of 29,608 patients with a median age of 70 years (IQR: 67–74) were enrolled in the retrospective cohort. The cut-off value of the SII was 650, which was determined by the receiver operating characteristic (ROC) curve. The ORs of an SII value > 650 was 2.709 (95% CI:2.373–3.092, P < 0.001), 1.615 (95% CI:1.384–1.882, P < 0.001), 1.855 (95% CI:1.602–2.146, P < 0.001), and 1.302 (95% CI:1.106–1.531, P = 0.001) for prediction of POD in univariate model and three multivariate regression models. After PSM, the OR of an SII value > 650 was 1.301 (95% CI: 1.062–1.598, P = 0.011). The subgroup analysis indicated that the SII indicates a significantly increased risk of POD in patients with Hb < 130 g/L, 4*109/L < WBC ≤ 10*109/L, albumin < 39 g/L, or duration of MAP < 60 mmHg ≥ 5 min. The SII was found to be a useful prognostic predictor of POD for patients of different ages, sexes, and ASA classifications.
Conclusions
The SII had a predictive value for POD in patients undergoing non-neurosurgery and non-cardiac surgery. As an index generated from routine blood tests, the SII has advantages regarding cost and time. After further validation, the SII may provide a new option for POD prediction.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12877-022-03418-4.
Keywords: Systemic-immune-inflammation (SII), Postoperative Delirium (POD), Inflammation, Elderly Patients, Biomarker
Background
Postoperative delirium (POD) is a common complication of elderly patients after surgery and is defined as a reversible disturbance in attention, awareness, and cognition. Its incidence is 3 to 50% for different surgeries [1, 2]. Loss of independence, increased morbidity and mortality, and high health costs are common adverse effects of POD [2, 3]. Thirty percent of patients with delirium can benefit from multifactorial preventive measures and treatments if they can be identified before POD occurs [4]. Therefore, identifying and managing high-risk POD patients is critical in improving the outcomes of elderly patients after surgery.
Inflammation plays a critical role in the pathophysiology of POD [5, 6]. Several inflammatory biomarkers in serum or cerebrospinal fluid are associated with POD after different surgeries [7–10]. Compared with IL-6, IL-8, C-reactive protein, and S-100β, white-cell derived inflammatory biomarkers, namely, the neutrophil–lymphocyte ratio (NLR), platelet-to-lymphocyte ratio (PLR), platelet-to-white cell ratio (PWR), and systemic immune inflammation index (SII, platelet × neutrophil/lymphocyte), can be obtained for a lower cost and require less time. Some studies have shown the potential value of the NLR, PLR, and PWR in predicting POD after lower limb, head and neck free-flap reconstruction, total hip arthroplasty, abdominal surgery, oesophagectomy carotid endarterectomy, and cardiac surgery [11–15]. As a white-cell derived inflammatory biomarker, systemic immune inflammation index (SII) has been used to predict ischemic stroke, delayed vasospasm, microvascular dysfunction, and acute kidney injury [16–19]. However, the SII has not been applied to predict POD in elderly patients after surgery.
In this study, we explored the prognostic value of the SII in predicting POD in elderly patients after non-neurosurgery and non-cardiac surgery in a large retrospective cohort. The hypothesis is that an elevated SII value before surgery may indicate an increased risk of POD.
Method
Study design and patients
This study was a retrospective cohort study. All the perioperative data were obtained from patients at the first medical center of the Chinese PLA General Hospital from January 2014 to April 2019. Inclusion criteria: 1) patients ≥ 65 years and 2) patients undergoing non-neurosurgery and non-cardiac surgery with anesthesia. The exclusion criteria were as follows: 1) patients undergoing digestive endoscopy; 2) missing data on white cell count, neutrophils, lymphocytes, and platelets; and 3) missing data for over 50% of all variables. The study was conducted following the Declaration of Helsinki. The study was approved by the Ethics Committee Board of the First Medical Center of Chinese PLA General Hospital (No. S2019-311–03). Patient consent was waived because the study was retrospective, and all data were anonymized before analysis.
Data collection
The dataset was established from the medical record system. For more accurate and broader clinical use of the models, we included both preoperative and intraoperative parameters of the models, which might be closely associated with POD, including the following aspects:
We collected the relevant patient demographics, including age; sex; body mass index (BMI); smoking; alcohol consumption; a combination of hypertension, diabetes, cardiovascular diseases and chronic obstructive pulmonary disease (COPD); chronic kidney disease (CKD); cerebrovascular disease; depression and anxiety; non-independent functional status; American Society of Anesthesiologists physical score (ASA); and days in the hospital before surgery.
The medication prescribed before surgery included nonsteroidal anti-inflammatory drugs (loxoprofen, acetaminophen, ibuprofen, celecoxib, meloxicam, diclofenac, etoricoxib, nimesulide), anticholinergic drugs (atropine, penehyclidine hydrochloride, scopolamine), benzodiazepines (midazolam, estazolam, diazepam, lorazepam, alprazolam, zolpidem, zopiclone), and antipsychotic drugs (quetiapine, olanzapine, droperidol, haloperidol, risperidone).
Laboratory tests (the most recent before surgery) were hemoglobin (Hb), WBC count, neutrophils, lymphocytes, monocytes, platelets, glucose (Glu), serum albumin, serum creatinine (Cre), alanine aminotransferase (ALT), aspartate aminotransferase (AST), total bilirubin, and prothrombin time (PT). SII = platelet × neutrophil/lymphocyte.
The intraoperative data included type of surgery, type of anesthesia, emergency status, duration of surgery and anesthesia, urine, blood loss, crystalloid, colloid, blood transfusion (red blood cells, whole blood, plasma, platelet, and cryoprecipitate, autologous blood, fibrinogen, albumin), use of glucocorticoids (dexamethasone, methylprednisolone), use of dexmedetomidine, duration of systolic blood pressure > 140 mmHg, and duration of MAP < 60 mmHg.
Definitions of outcomes
The primary outcome was the incidence of POD within seven days postoperatively. It was captured through descriptive words documented in the medical records and confirmed by the neurologist. The inclusion criteria were as follows: 1) the postoperative medical records contained "mental status change", "confusion", "disorientation", "agitation", "delirium", "inappropriate behaviour", "inattention", "hallucinations", and "combative behaviour" [20] and 2) the postoperative drug regimen contained "quetiapine", "olanzapine", "haloperidol", "haloperidol", and "risperidone". The exclusion criteria were 1) preoperative medical records containing the “symptoms” mentioned above and 2) a preoperative drug regimen containing the “drugs” mentioned above. Neurologists rechecked all the delirium patients’ medical records diagnosing the POD using Diagnostic and Statistical Manual of Mental Disorders, fourth edition (DSM-IV) criteria [13].
Correlation between the SII and POD
We divided the SII into multiple categories (using quartiles). The receiver operating characteristic (ROC) curve was also calculated to discover the optimal cut-off value of the SII in predicting POD. Then, we performed univariate and multivariate logistic analyses to explore the correlation between POD and the SII as continuous and categorical variables (with quartiles and optimal cut-off value). In multivariate logistic regression analysis, model 1 included the baseline characteristics (age, sex, BMI, smoking, alcohol consumption, hypertension, diabetes, cardiovascular disease, COPD, cerebrovascular disease, CKD, depression and anxiety, non-independent functional status, ASA), preoperative medications (anticholinergic drugs, NSAIDs, benzodiazepines, antipsychotic drugs), and preoperative laboratory tests (hemoglobin, WBC count, Glu, albumin, Cre, AST, ALT, PT). Model 1 adjusted for age, sex, BMI, ASA, alcohol, cerebrovascular disease, COPD, depression and anxiety, antipsychotic drugs, benzodiazepines, hemoglobin, WBC count, albumin, AST, ALT, PT, types of surgery, and anesthesia methods. Model 2 included intraoperative variables (emergency surgery, types of surgery, anesthesia methods, duration of surgery and anesthesia, blood loss, urine, crystalloid, colloid, blood transfusion, duration of SBP > 140 mmHg, duration of MAP < 60 mmHg) and intraoperative medication. Emergency surgery, duration of anesthesia, colloid, blood transfusion, duration of SBP > 140 mmHg, and MAP < 60 mmHg were adjusted in model 2. Model 3 included baseline characteristics, preoperative medications, preoperative laboratory tests, intraoperative variables, and intraoperative medication and adjusted for variables adjusted in model 1 and model 2.
Propensity score-matching analysis and adjustment
Propensity scores are an alternative method for estimating the effect of receiving treatment when the random assignment of treatments to subjects is not feasible. Propensity score matching (PSM) refers to the pairing of treatment and control subjects with similar values on the propensity score and possibly other covariates and discarding all unmatched subjects [21]. The propensity score was computed based on the probability of patients having different levels of the SII and derived from synthesized baseline parameters using the multivariate logistic regression model. After propensity score generation, patients with different categorical SII values were randomly matched at a 1:1 ratio using the greedy nearest neighbor matching approach (maximum calliper width, 0.1). Kernel density plots of the propensity scores were applied to examine the equivalence between the matched patients. The standardized mean difference (SMD) was reported and used to evaluate the baseline differences between the two groups, where a value < 0.1 indicated minor differences.
Subgroup analyses
After logistic regression analysis of different models and PSM analysis, subgroup analysis was conducted to explore the correlation between the SII and POD in different ages, sexes, ASA classification, hemoglobin, WBC count, albumin, duration of MAP < 60 mmHg subgroups. A forest plot was used to summarize the prediction of POD by the SII in subgroups.
Statistical analysis
Normally distributed continuous variables are expressed as the mean (SD) and were compared using Student’s t test. If the continuous data are not normally distributed, they are shown as the median and interquartile range (IQR) and were compared with the Mann–Whitney test. Categorical variables are expressed as frequencies or percentages and were compared using the χ2 test or Fisher’s exact test. Statistical significance was accepted at the 0.05 level, and all tests were two-tailed. The logistic regression model was performed using R 4.0.1 (R Foundation for Statistical Computing, Vienna, Austria).
Results
Patient characteristics
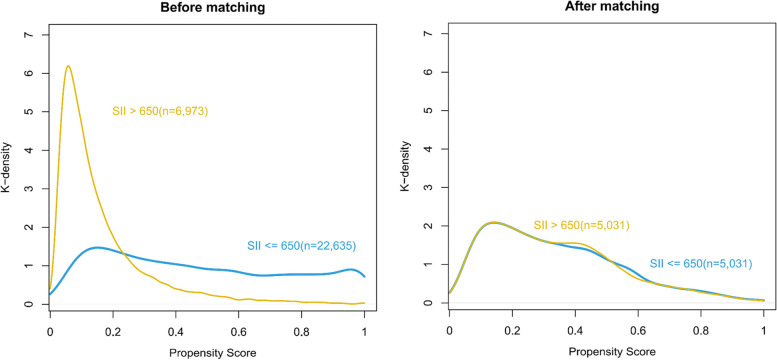
The medical records of 31,066 patients over 65 years old after non-neurosurgery and non-cardiac surgery from January 2014 to August 2019 at the First Medical Center of Chinese PLA General Hospital were retrospectively analyzed. After excluding 1116 patients for digestive endoscopy, 610 patients for missing variables, and 29 patients for ASA V, 29,608 patients were enrolled in the final analysis (Fig. 1). The median age was 70 years (IQR: 67, 74), and 50.9% of the enrolled patients (15,066/29608) were male. The median levels of hemoglobin, WBC count, and albumin were 130 (IQR: 119–141) g/L, 5.93 (IQR: 4.95–7.17) × 109, and 39.8 (IQR: 37.3–42.3) g/L, respectively. The incidence of POD was 3.1% (927/29608) in the overall cohort.
Fig. 1.
The enrolment flow chart of patients. ASA, American Society of Anesthesiologists classification; WBC, white blood cell
The median SII value was 416 (IQR: 289–630) × 109. The ROC curve showed that the optimal cut-off value of the SII in predicting POD was 650 × 109, with an area under the ROC curve (AUC) of 0.63 (Additional file Figure A1). The baseline characteristics of the patients and the preoperative and intraoperative variables are shown according to SII ≤ 650 (n = 22,635) and SII > 650 (n = 6973). Of the baseline characteristics, except for cardiovascular disease, depression and anxiety, and the use of NSAIDs, all variables differed between the two groups. The patients in the SII > 650 group had more comorbidities (hypertension, diabetes, cerebrovascular disease, CKD, COPD) and longer stays in the hospital before surgery than those in the SII ≤ 650 group. The preoperative hemoglobin, WBC count, Glu, albumin, Cre, and PT also differed between the two groups. The difference was also shown in the intraoperative variables, such as type and duration of surgery and anesthesia, and fluid balance (blood loss, urine, blood transfusion, colloid, and crystalloid) (Table 1).
Table 1.
The characteristics of patients before and after PSM
| Characteristic | Before PSM (n = 29,608) | After PSM (1:1) (n = 10,062) | ||||
|---|---|---|---|---|---|---|
| SII ≤ 650 (n = 22,635) | SII > 650 (n = 6973) | SMD | SII ≤ 650 (n = 5031) | SII > 650 (n = 5031) | SMD | |
| Age, years | 70(67,74) | 71(67,76) | 0.238 | 71.0 (67.0, 76.0) | 71.0 (67.0, 75.0) | 0.04 |
| Sex (male), n (%) | 11,208(49.5) | 3858(55.3) | 0.117 | 2716 (54.0) | 2725 (54.2) | 0.004 |
| BMI, kg·m,2 | 24.62(22.45,26.94) | 23.72(21.34,26.16) | 0.261 | 24.0 (21.8, 26.4) | 23.9 (21.6, 26.4) | 0.024 |
| Smoking, n (%) | 5134(22.7) | 1763(25.3) | 0.061 | 1253 (24.9) | 1268 (25.2) | 0.007 |
| Alcohol consumption, n (%) | 4806(21.2) | 1624(23.3) | 0.049 | 1141 (22.7) | 1185 (23.6) | 0.021 |
| Hypertension, n (%) | 10,762(47.5) | 3474(49.8) | 0.046 | 2388 (47.5) | 2499 (49.7) | 0.044 |
| Diabetes, n (%) | 5245(23.2) | 1761(25.3) | 0.049 | 1283 (25.5) | 1231 (24.5) | 0.024 |
| Cardiovascular diseases, n (%) | 2209(9.8) | 674(9.7) | 0.003 | 517 (10.3) | 473 (9.4) | 0.029 |
| COPD, n (%) | 803(3.5) | 382(5.5) | 0.093 | 229 (4.6) | 257 (5.1) | 0.026 |
| Cerebrovascular disease, n (%) | 2114(9.3) | 783(11.2) | 0.062 | 506 (10.1) | 542 (10.8) | 0.023 |
| CKD, n (%) | 220(1) | 142(2) | 0.088 | 76 (1.5) | 70 (1.4) | 0.01 |
| Depression and anxiety, n (%) | 115(0.5) | 46(0.7) | 0.02 | 33 (0.7) | 36 (0.7) | 0.007c |
| Non-independent functional status, n (%) | 5630(24.9) | 3147(45.1) | 0.435 | 2005 (39.9) | 1867 (37.1) | 0.056 |
| ASA, n (%) | 0.29 | 0.096 | ||||
| I | 298(1.3) | 59(0.8) | 49 (1.0) | 48 (1.0) | ||
| II | 18,466(81.6) | 4963(71.2) | 3862 (76.8) | 3729 (74.1) | ||
| III | 3802(16.8) | 1801(25.8) | 1088 (21.6) | 1179 (23.4) | ||
| IV | 69(0.3) | 150(2.2) | 32 (0.6) | 75 (1.5) | ||
| Emergency surgery, n (%) | 348(1.5) | 454(6.5) | 0.255 | 147 (2.9) | 193 (3.8) | 0.051 |
| Hemoglobin, g·L−1 | 132(122,142) | 123(109,137) | 0.5 | 127.0 (115.0, 137.0) | 126.0 (113.0, 139.0) | 0.014 |
| WBC count, *109/L | 5.63(4.75,6.62) | 7.4(6.08,9) | 0.843 | 6.8 (5.7, 8.0) | 6.7 (5.7, 7.9) | 0.009 |
| Monocytes, *109/L | 0.07(0.06,0.08) | 0.06(0.05,0.08) | 0.066 | |||
| Glu, mmol/L | 5.05(4.63,5.73) | 5.46(4.82,6.61) | 0.339 | 5.2 (4.7, 6.2) | 5.3 (4.8, 6.3) | 0.017 |
| Albumin, g/L | 40.2(37.9,42.5) | 38.1(34.7,41.3) | 0.519 | 39.0 (36.4, 41.6) | 38.9 (35.8, 42.0) | 0.018 |
| Cre, μmol/L | 70.9(60.7,82.6) | 70.1(58.8,83.6) | 0.048 | 72.0 (61.1, 84.4) | 70.40 (59.3, 83.0) | 0.076 |
| Total bilirubin, μmol/L | 11(8.5,14.3) | 10.8(7.9,15.7) | 0.262 | 10.50 (8.0, 14.3) | 10.70 (7.8, 14.9) | 0.06 |
| AST, U/L | 14.7(11,21.1) | 14.8(10.3,24.8) | 0.174 | 14.9 (10.7, 22.3) | 14.20(10.2, 23.1) | 0.019 |
| ALT, U/L | 16.8(14.1,20.9) | 16.7(13.4,23.3) | 0.167 | 16.8 (13.9, 21.9) | 16.4 (13.4, 21.8) | 0.006 |
| PT, s | 13.2(12.7,13.7) | 13.4(12.9,14.1) | 0.237 | 13.3 (12.8, 13.9) | 13.3 (12.8, 13.9) | 0.035 |
| Preoperative medication, n (%) | ||||||
| Anticholinergic drug | 13,292 (58.7) | 3632 (52.1) | 0.134 | 2807 (55.8) | 2809 (55.8) | 0.001 |
| NSAIDs | 1509 (6.7) | 506 (7.3) | 0.023 | 358 (7.1) | 331 (6.6) | 0.021 |
| Benzodiazepines | 5144 (22.7) | 1493 (21.4) | 0.032 | 1126 (22.4) | 1051 (20.9) | 0.036 |
| Antipsychotic drugs | 60 (0.3) | 47 (0.7) | 0.06 | 20 (0.4) | 27 (0.5) | 0.02 |
| Type of surgery, n (%) | 0.261 | 0.16 | ||||
| Hepatopancreatobiliary and gastrointestinal surgery | 7265(32.1) | 2849(40.9) | 1932 (38.4) | 2199 (43.7) | ||
| Orthopedic surgery | 6466(28.6) | 2183(31.3) | 1594 (31.7) | 1367 (27.2) | ||
| Urinary surgery | 2238(9.9) | 437(6.3) | 352 (7.0) | 308 (6.1) | ||
| Thoracic surgery | 1723(7.6) | 415(6) | 341 (6.8) | 291 (5.8) | ||
| E.N.T | 1181(5.2) | 301(4.3) | 201 (4.0) | 289 (5.7) | ||
| Gynecology | 839(3.7) | 163(2.3) | 134 (2.7) | 157 (3.1) | ||
| Vascular surgery | 952(4.2) | 229(3.3) | 163 (3.2) | 131 (2.6) | ||
| Others | 1971(8.7) | 396(5.7) | 314 (6.2) | 289 (5.7) | ||
| Anesthesia method, n (%) | 0.134 | 0.056 | ||||
| Basal anesthesia | 255(1.1) | 121(1.7) | 58 (1.2) | 73 (1.5) | ||
| Epidural anesthesia | 426(1.9) | 114(1.6) | 94 (1.9) | 63 (1.3) | ||
| Nerve blocks | 418(1.8) | 205(2.9) | 116 (2.3) | 117 (2.3) | ||
| General anesthesia | 19,006(84) | 5540(79.4) | 4163 (82.7) | 4169 (82.9) | ||
| General anesthesia combined with other anesthesia | 2530(11.2) | 993(14.2) | 600 (11.9) | 609 (12.1) | ||
| Duration of surgery, min | 130.0(85.0,190.0) | 140.0(95.0,210.0) | 0.164 | 10.00 (0.00, 30.00) | 10.00 (0.00, 30.00) | 0.022 |
| Duration of anesthesia, min | 178.0(127.0,240.0) | 190.0(140.0,260.0) | 0.169 | 5.00 (0.00, 15.00) | 5.00 (0.00, 15.00) | 0.007 |
| Blood loss, ml | 100.0(30.0,200.0) | 100.0(50.0,200.0) | 0.113 | 100.0 (50.0, 200.0) | 100.0 (50.0, 200.0) | 0.033 |
| Urine, ml | 200.0(100.0,500.0) | 250.0(100.0,500.0) | 0.047 | 300.0 (100.0,600.0) | 250.0 (100.0, 500.0) | 0.063 |
| Crystalloid, ml | 1300.0(1100.0,2100.0) | 1600.0(1100.0,2100.0) | 0.153 | 1600.0 (1100.0, 2100.0) | 1600.0 (1100.0, 2100.0) | 0.055 |
| Colloid, ml | 500.0(0,500.0) | 500.0(0,500.0) | 0.163 | 500.0 (0, 500.0) | 500.0 (0.0, 500.0) | 0.063 |
| Blood transfusion, n | 2763 (12.2) | 1420 (20.4) | 0.222 | 821 (16.3) | 949 (18.9) | 0.067 |
| Duration of SBP > 140 mmHg, min | 5.0(0,25.0) | 10.0(0,30.0) | 0.141 | 10.0 (0, 30.0) | 10.0 (0.0, 30.0) | 0.022 |
| Duration of MAP < 60 mmHg, min | 5.0(0,10.0) | 5.0(0,15.0) | 0.104 | 5.0 (0, 15.0) | 5.0 (0.0, 15.0) | 0.007 |
| Intraoperative medication, n (%) | ||||||
| Glucocorticoid | 14,303 (63.2) | 4324 (62.0) | 0.024 | 3155 (62.7) | 3251 (64.6) | 0.04 |
| Dexmedetomidine | 2262 (10.0) | 692 (9.9) | 0.002 | 532 (10.6) | 442 (8.8) | 0.061 |
| POD, n (%) | 514 (2.3) | 413 (5.9) | 0.185 | 170 (3.4) | 219 (4.4) | 0.051 |
Abbreviations: SII Systemic-immune-inflammation index, SMD Standardized mean difference, PSM Propensity Score Matching, BMI Body mass index, COPD Chronic obstructive pulmonary disease, CKD Chronic kidney disease, ASA American Society of Anesthesiologists physical status classification system, E.N.T Otolaryngology head, and neck surgery, SBP Systolic blood pressure, MAP Mean arterial pressure, WBC White blood cell, ESR Erythrocyte sedimentation rate, Glu Glucose, Cre Creatinine, AST Aspartate aminotransferase, ALT Alanine aminotransferase, NSAIDs Non-steroidal anti-inflammatory drugs
Correlation between the SII and POD
To investigate the correlation between the SII and POD, we performed four logistic regression models. As a continuous variable, the SII was associated with POD in the unadjusted regression model with an odds ratio (OR) of 1.0004 (95 CI: 1.0003–1.0004), P < 0.001. In the multivariate logistic regression models, the ORs of SII were 1.0001 (model 1), 1.0002 (model 2), and 1.0001(model 3). So, the SII was an independent risk factor of POD (All P < 0.01, Additional file Table. A1).
The SII was divided into four categories using quartiles (SII ≤ 289, 289 < SII ≤ 416, 416 < SII ≤ 630, SII > 630). An elevated SII value was also associated with an increased risk of POD in all models. In the univariate analysis, the patients in the 416 < SII ≤ 630 and SII > 630 groups had a significantly higher risk of POD than those in the SII ≤ 289 group (P < 0.05). After adjusting for a series of variables (model 3), SII > 630 group still showed a significantly higher risk than SII ≤ 289(OR = 1.26, P = 0.038). All the detailed results are shown in Table A2 in the additional file.
The ROC of SII showed the optimal cut-off value for predicting POD is 650 (Figure A1 in the additional file). So, the SII was divided into two groups with a cut-off value of 650. The OR of SII > 650 group was 2.71 (95% CI: 2.37–3.09, P < 0.001) in the univariate analysis. In the multivariate logistic regression models, the OR of an SII value > 650 ranged from 1.32 to 1.86, and the P values were ≤ 0.001 for all models (Table 2). The overall univariate and multivariate logistic regression results are shown in Table A3 of additional file.
Table 2.
Association between SII and POD with logistic regression models and PSM analysis
| Model | ORa | 95%CI | P |
|---|---|---|---|
| Unadjusted model | 2.709 | 2.373–3.092 | < 0.001 |
| Model 1 (adjusted for preoperative variables)b | 1.615 | 1.384–1.882 | < 0.001 |
| Model 2 (adjusted for intraoperative variables)c | 1.855 | 1.602–2.146 | < 0.001 |
| Model 3 (adjusted all the variables)d | 1.302 | 1.106–1.531 | 0.001 |
| Model PSM (n = 10,062)e | 1.301 | 1.062–1.598 | 0.011 |
SII Systemic-immune-inflammation index, POD Postoperative delirium, OR Odds ratio, CI Confidence interval, PSM Propensity score matching
aThe ORs of SII > 650
bModel 1 adjusted for age, sex, BMI, ASA, alcohol, cerebrovascular disease, COPD, depression and anxiety, antipsychotic drugs, benzodiazepines, hemoglobin, WBC count, albumin, AST, ALT, PT, types of surgery, and anesthesia methods
cModel 2 adjusted for emergency surgery, duration of anesthesia, colloid, blood transfusion, duration of SBP > 140 mmHg, and MAP < 60 mmHg
dModel 3 adjusted for model 1 plus model 2
eModel PSM was a univariate regression model
Propensity score matching analysis and adjustment
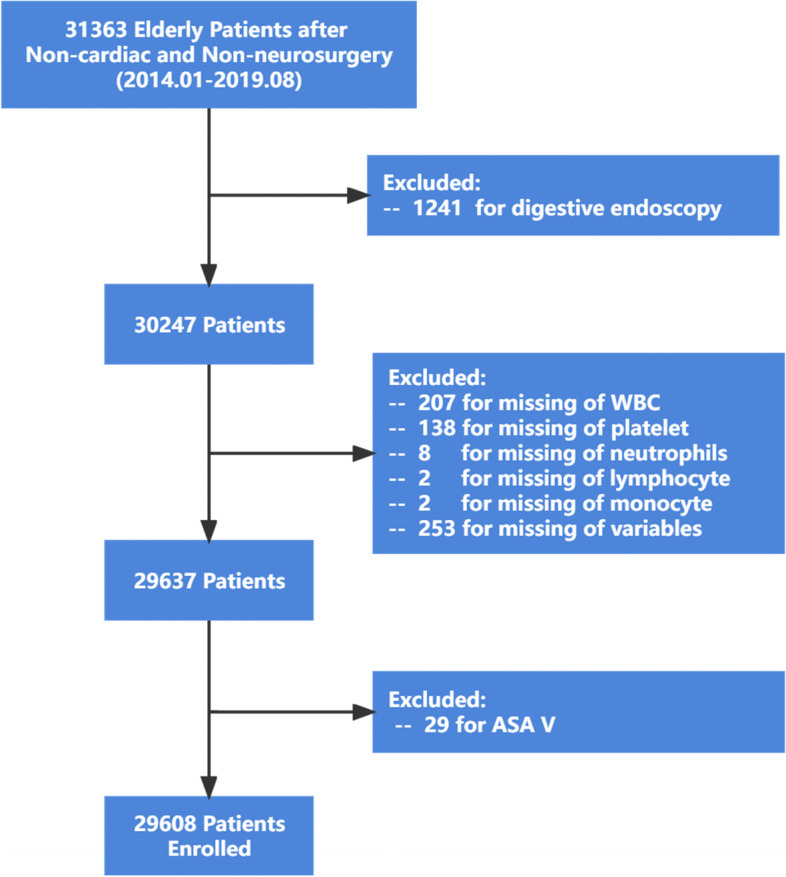
Then, PSM analysis was performed as planned. The 14 variables (sex, age, albumin, emergency, type of surgery, WBC, Glu, Hb, BMI, total bilirubin, non-independent functional status, diabetes, type of surgery, duration of anesthesia) were matched in constructing PSM cohort. A total of 5031 patients in the SII ≤ 650 group were matched with 5031 patients in the SII > 650 group. The distribution of propensity scores of the patients before and after PSM is displayed in Fig. 2. The baseline characteristics and variables were balanced between the two groups (SMD < 0.1 except for the type of surgery) (Table 1). In the logistic regression performed after PSM, the SII was still an independent predictor of POD, with an OR of 1.301 (95% CI: 1.062–1.598, P = 0.011) (Table 2). The univariate logistic regression results are shown in Table A4 of additional file.
Fig. 2.
Distribution of propensity scores before and after matching. SII, systemic-immune-inflammation
Subgroup analyses
Additional subgroup analyses showed that the OR of the SII was significant for age, sex, and ASA classification in each subgroup (all P < 0.05, Fig. 3). The crude ORs of the SII generated in each subgroup showed that the associations between the SII and POD were stronger when albumin was < 39 g/L, the duration of a MAP < 60 mmHg was > 5 min, and hemoglobin was < 130 g/L (Fig. 3). In the three subgroups of WBC count, the OR of the SII was significant only in the 4 < WBC < 10 group (Fig. 3).
Fig. 3.
Subgroup analyses of the association between SII and perioperative ischemic stroke. SII, systemic-immune-inflammation; POD, postoperative delirium; OR, odds ratio; CI, Confidence interval; ASA, American Society of Anesthesiologists classification; Hb, hemoglobin; WBC, white blood cell count; MAP, mean arterial pressure
Discussion
We evaluated the association between the SII and POD in 29,608 elderly patients who underwent nonneurosurgery and non-cardiac surgery with anaesthesia within our retrospective database. We found that the SII was an excellent predictor of POD after multivariate logistic regression and PSM.
The ability of SII as a continuous variable in predicting POD showed statistically significant in the univariate and 3 different multivariate models(P < 0.001). When the SII was divided into four categories with quartiles, it had an increasing trend of POD incidence as the SII grew in all models(P < 0.05). Then we explored the relationship between POD and SII as a categorical variable with a cut-off value of 650. In the univariate logistic regression, the SII > 650 showed a significant prediction for POD (OR 2.709, 95% CI 2.373–3.092, P < 0.001). Next, the association between the SII and POD was evaluated in 3 multivariate logistic regression models, including preoperative, intraoperative, and all variables. The results showed that the SII > 650 was still an independent risk factor for POD in elderly patients (P ≤ 0.001). To eliminate the confounding effect of covariates, we performed the PSM analysis further to test the relationship between the SII and POD. After all the covariates were used to estimate the propensity score, 5031 pairs of patients were matched. The results showed that the SII could be a powerful predictor of POD in the new cohort. The subgroup analysis indicated that an SII > 650 was associated with a significantly increased risk of POD in patients with an Hb level < 130 g/L, albumin level < 39 g/L, or a duration of MAP < 60 mmHg ≥ 5 min. In the 4 < WBC ≤ 10 group, patients with an SII ≥ 650 had an increased risk of POD (P < 0.001). The SII was found to be a valuable prognostic predictor for POD in patients of different ages, sexes, and ASA classifications.
Several possible mechanisms may account for the association between the preoperative SII and POD. First, Increased neutrophil levels, decreased lymphocyte levels, and decreased platelet levels are often nonspecific response to injury by trauma, surgery, and anesthesia [22, 23]. This change in peripheral circulation may involve disrupting the blood–brain-barrier and microglia, which activates and releases cerebral cytokines, resulting in POD [22, 24]. Second, many studies have found that white-cell derived inflammatory markers, such as the NLR, PLR, and PWR, are associated with delirium [11–15]. As one of the white-cell derived inflammatory markers, the SII was also calculated using neutrophil, lymphocyte, and platelet counts. Therefore, an elevated SII value indicated more severe immune-mediated and inflammation-mediated brain damage, which plays a critical role in the pathogenesis of POD [5, 22]. Moreover, many studies have indicated that the SII is associated with different cancers [25–27], ischaemic stroke [18, 28], and cerebral small vessel disease [16, 29, 30]. Individuals suffering from small vessel disease have more fragile brains, in which areas of vascular dysfunction can be more susceptible to acute impairment following systemic inflammatory insults [31, 32]. Neuroinflammation in areas of existing brain disease contributes to delirium [33]. As mentioned above, the SII may have good predictive power for POD.
To our knowledge, no study has explored the association between the SII and POD. Our analysis gave strong evidence to support that the SII can be a useful predictor of POD. As the incidence of POD differed among surgeries, we assessed the predictive ability of the SII for POD in an extensive retrospective cohort of 29,608 non-neurosurgery and non-cardiac surgery patients. Many statistical methods were used to confirm the conclusion. In addition to the multivariable logistic regression method, we also used PSM and subgroup analysis to reconfirm the conclusion. All the evidence proved that the SII was an independent predictor of POD in elderly patients undergoing non-neurosurgery and non-cardiac surgery.
However, our study also had some limitations. First, it is a retrospective study. The patients with POD were identified based on medical and nursing records but not assessment tools. The nurses may miss delirium for a lack of knowledge of POD assessment [34]. A gap existed between physicians’ perceptions and performance of delirium assessments in China. The actual prevalence of delirium assessment was suboptimal [35]. Before the evaluation of delirium becomes a routine postoperative evaluation item, only a retrospective dataset could provide such a large sample size. Nevertheless, only the recorded hyperactive and mixed POD patients needed urgent intervention. Therefore, predicting POD in these patients with the SII is also meaningful. We currently conduct a multicentre prospective study identifying POD patients with the Confusion Assessment Method (CAM) and 3D-CAM. Second, we only found an association between the SII and POD after a series of statistical analyses. The mechanism and validation of the association remain to be further studied. Thirdly, we only collected part of preoperative drugs and didn’t consider the effects of polypharmacy. Polypharmacy is also associated with delirium incidence and persistence [36]. In the future, we will try to collect all the preoperative drugs and fully consider polypharmacy.
Conclusion
The SII was found to have a predictive value for POD in patients undergoing non-neurosurgery and non-cardiac surgery. As an index generated from routine blood tests, the SII has advantages in terms of cost and time required. After further validation, the SII may provide a new option for POD prediction.
Supplementary Information
Additional file 1: Figure A1. The receiver operating characteristics (ROC) curve of SII for POD. Table A1. Association between SII as continuous variable and POD in different models. Table A2. Association between SII as categories variables used quartiles and POD in different models. Table A3. Association between SII as categories variables with a cut-off value of 650 and POD in different models. Table A4. Univariate logistic regression analyses for POD in the Model PSM.
Acknowledgements
We would like to thank Tongyan Sun and Wei Wei of Hangzhou Le9 Healthcare Technology Co., Ltd., for help in the clinical data collection of this study.
Abbreviations
- OR
Odds ratio
- CI
Confidence interval
- SII
Systemic-immune-inflammation index
- SMD
Standardized mean difference
- PSM
Propensity Score Matching
- BMI
Body mass index
- COPD
Chronic obstructive pulmonary disease
- CKD
Chronic kidney disease
- ASA
American Society of Anaesthesiologists classification system
- E.N.T
Otolaryngology head, and neck surgery
- SBP
Systolic blood pressure
- MAP
Mean arterial pressure
- WBC
White blood cell
- ESR
Erythrocyte sedimentation rate
- Glu
Glucose
- Cre
Creatinine
- AST
Aspartate aminotransferase
- ALT
Alanine aminotransferase
- NSAIDs
Non-steroidal anti-inflammatory drugs
- CAM
Confusion assessment method
Authors’ contributions
JC and WM conceptualized and designed the study. WM obtained funding. YS, YL, and FZ collected and interpreted the data. YS, YM, JL and HL analysed data, prepared and reviewed figures. YS wrote the original draft. YL and JC provided critical revisions of the manuscript. All authors read and approved the final manuscript.
Funding
This work was supported by the National Key Research and Development Program of China (2018YFC2001901).
Availability of data and materials
The datasets generated and/or analysed during the current study are not publicly available as individual privacy could be compromised but are available from the corresponding author on reasonable request.
Declarations
Ethics approval and consent to participate
The study was conducted following the Declaration of Helsinki. The study was approved by the Ethics Committee Board of the First Medical Center of Chinese PLA General Hospital (No. S2019-311–03). Patient consent was waived because the study was retrospective, and all data were anonymized before analysis.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Yuxiang Song and Yungen Luo contributed equally to this work.
Contributor Information
Weidong Mi, Email: wwdd1962@aliyun.com.
Jiangbei Cao, Email: caojiangbei@301hospital.com.cn.
References
- 1.Jin Z, Hu J, Ma D. Postoperative delirium: perioperative assessment, risk reduction, and management. Br J Anaesth. 2020;125(4):492–504. doi: 10.1016/j.bja.2020.06.063. [DOI] [PubMed] [Google Scholar]
- 2.Oh ES, Fong TG, Hshieh TT, Inouye SK. Delirium in older persons: advances in diagnosis and treatment. JAMA. 2017;318(12):1161–1174. doi: 10.1001/jama.2017.12067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Marcantonio ER. Delirium in hospitalized older adults. N Engl J Med. 2017;377(15):1456–1466. doi: 10.1056/NEJMcp1605501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Milisen K, Steeman E, Foreman MD. Early detection and prevention of delirium in older patients with cancer. Eur J Cancer Care. 2004;13(5):494–500. doi: 10.1111/j.1365-2354.2004.00545.x. [DOI] [PubMed] [Google Scholar]
- 5.Subramaniyan S, Terrando N. Neuroinflammation and perioperative neurocognitive disorders. Anesth Analg. 2019;128(4):781–788. doi: 10.1213/ANE.0000000000004053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Yang T, Velagapudi R, Terrando N. Neuroinflammation after surgery: from mechanisms to therapeutic targets. Nat Immunol. 2020;21(11):1319–1326. doi: 10.1038/s41590-020-00812-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Brattinga B, Plas M, Spikman JM, Rutgers A, de Haan JJ, Absalom AR, van der Wal-Huisman H, de Bock GH, van Leeuwen BL. The association between the inflammatory response following surgery and post-operative delirium in older oncological patients: a prospective cohort study. Age Ageing. 2022;51(2):afab237. [DOI] [PMC free article] [PubMed]
- 8.Song Y, Wang X, Hou A, Li H, Lou J, Liu Y, Cao J, Mi W. Integrative analysis of lncRNA and mRNA and profiles in postoperative delirium patients. Front Aging Neurosci. 2021;13:665935. doi: 10.3389/fnagi.2021.665935. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Yamanashi T, Nagao T, Wahba NE, Marra PS, Crutchley KJ, Meyer AA, Andreasen AJ, Hellman MM, Jellison SS, Hughes CG, et al. DNA methylation in the inflammatory genes after neurosurgery and diagnostic ability of post-operative delirium. Transl Psychiatry. 2021;11(1):627. doi: 10.1038/s41398-021-01752-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.McKay TB, Qu J, Liang F, Mueller A, Wiener-Kronish J, Xie Z, Akeju O. Tau as a serum biomarker of delirium after major cardiac surgery: a single centre case-control study. Br J Anaesth. 2022;129(1):e13–e16. [DOI] [PMC free article] [PubMed]
- 11.Li X, Wang G, He Y, Wang Z, Zhang M. White-cell derived inflammatory biomarkers in prediction of postoperative delirium in elderly patients undergoing surgery for lower limb fracture under non-general anaesthesia. Clin Interv Aging. 2022;17:383–392. doi: 10.2147/CIA.S346954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.He R, Wang F, Shen H, Zeng Y, Zhang L. Association between increased neutrophil-to-lymphocyte ratio and postoperative delirium in elderly patients with total hip arthroplasty for hip fracture. BMC Psychiatry. 2020;20(1):496. doi: 10.1186/s12888-12020-02908-12882. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kinoshita H, Saito J, Takekawa D, Ohyama T, Kushikata T, Hirota K. Availability of preoperative neutrophil-lymphocyte ratio to predict postoperative delirium after head and neck free-flap reconstruction: a retrospective study. PLoS One. 2021;16(7):e0254654. doi: 10.1371/journal.pone.0254654. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kotfis K, Slozowska J, Safranow K, Szylinska A, Listewnik M. The practical use of white cell inflammatory biomarkers in prediction of postoperative delirium after cardiac surgery. Brain Sci. 2019;9(11):308. doi: 10.3390/brainsci9110308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Oyama T, Kinoshita H, Takekawa D, Saito J, Kushikata T, Hirota K. Higher neutrophil-to-lymphocyte ratio, mean platelet volume, and platelet distribution width are associated with postoperative delirium in patients undergoing esophagectomy: a retrospective observational study. J Anesth. 2022;36(1):58–67. doi: 10.1007/s00540-00021-03007-00546. [DOI] [PubMed] [Google Scholar]
- 16.Yaşar E, Bayramoğlu A. Systemic Immune-Inflammation Index as a Predictor of Microvascular Dysfunction in Patients With Cardiac Syndrome X. Angiology. 2022;73(7):615–621. doi: 10.1177/00033197221087777. [DOI] [PubMed] [Google Scholar]
- 17.Geraghty JR, Lung TJ, Hirsch Y, Katz EA, Cheng T, Saini NS, Pandey DK, Testai FD. Systemic immune-inflammation index predicts delayed cerebral vasospasm after aneurysmal subarachnoid hemorrhage. Neurosurgery. 2021;89(6):1071–1079. doi: 10.1093/neuros/nyab354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Zhang F, Niu M, Wang L, Liu Y, Shi L, Cao J, Mi W, Ma Y, Liu J. Systemic-Immune-Inflammation Index as a Promising Biomarker for Predicting Perioperative Ischemic Stroke in Older Patients Who Underwent Non-cardiac Surgery. Front Aging Neurosci. 2022;14:865244. doi: 10.3389/fnagi.2022.865244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Jia L, Li C, Bi X, Wei F, Meng J, Sun G, Yu H, Dong H, Li B, Cao Y, et al. Prognostic Value of Systemic Immune-Inflammation Index among Critically Ill Patients with Acute Kidney Injury: A Retrospective Cohort Study. J Clin Med. 2022;11(14):3978. doi: 10.3390/jcm11143978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hornor MA, Ma M, Zhou L, Cohen ME, Rosenthal RA, Russell MM, Ko CY. Enhancing the American College of Surgeons NSQIP Surgical Risk Calculator to Predict Geriatric Outcomes. J Am Coll Surg. 2020;230(1):88–100.e101. doi: 10.1016/j.jamcollsurg.2019.09.017. [DOI] [PubMed] [Google Scholar]
- 21.Austin PC, Mamdani MM. A comparison of propensity score methods: a case-study estimating the effectiveness of post-AMI statin use. Stat Med. 2006;25(12):2084–2106. doi: 10.1002/sim.2328. [DOI] [PubMed] [Google Scholar]
- 22.Murray C, Sanderson DJ, Barkus C, Deacon RM, Rawlins JN, Bannerman DM, Cunningham C. Systemic inflammation induces acute working memory deficits in the primed brain: relevance for delirium. Neurobiol Aging. 2012;33(3):603–616.e603. doi: 10.1016/j.neurobiolaging.2010.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Alam A, Hana Z, Jin Z, Suen KC, Ma D. Surgery, neuroinflammation and cognitive impairment. EBioMedicine. 2018;37:547–556. doi: 10.1016/j.ebiom.2018.10.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hughes CG, Patel MB, Pandharipande PP. Pathophysiology of acute brain dysfunction: what's the cause of all this confusion? Curr Opin Crit Care. 2012;18(5):518–526. doi: 10.1097/MCC.0b013e328357effa. [DOI] [PubMed] [Google Scholar]
- 25.Tian T, Lu J, Zhao W, Wang Z, Xu H, Ding Y, Guo W, Qin P, Zhu W, Song C, et al. Associations of systemic inflammation markers with identification of pulmonary nodule and incident lung cancer in Chinese population. Cancer medicine. 2022;11(12):2482–2491. doi: 10.1002/cam4.4606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Han R, Tian Z, Jiang Y, Guan G, Sun X, Yu Y, Zhang L, Zhou J, Jing X. Prognostic significance of systemic immune-inflammation index and platelet-albumin-bilirubin grade in patients with pancreatic cancer undergoing radical surgery. Gland Surg. 2022;11(3):576–587. doi: 10.21037/gs-22-117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kubota K, Ito R, Narita N, Tanaka Y, Furudate K, Akiyama N, Chih CH, Komatsu S, Kobayashi W. Utility of prognostic nutritional index and systemic immune-inflammation index in oral cancer treatment. BMC Cancer. 2022;22(1):368. doi: 10.1186/s12885-022-09439-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Zhou YX, Li WC, Xia SH, Xiang T, Tang C, Luo JL, Lin MJ, Xia XW, Wang WB. Predictive Value of the Systemic Immune Inflammation Index for Adverse Outcomes in Patients With Acute Ischemic Stroke. Front Neurol. 2022;13:836595. doi: 10.3389/fneur.2022.836595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Nam KW, Kwon HM, Jeong HY, Park JH, Kwon H. Systemic immune-inflammation index is associated with white matter hyperintensity volume. Sci Rep. 2022;12(1):7379. doi: 10.1038/s41598-022-11575-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Jiang L, Cai X, Yao D, Jing J, Mei L, Yang Y, Li S, Jin A, Meng X, Li H, et al. Association of inflammatory markers with cerebral small vessel disease in community-based population. J Neuroinflammation. 2022;19(1):106. doi: 10.1186/s12974-022-02468-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Lu W, Zhang K, Chang X, Yu X, Bian J. The Association Between Systemic Immune-Inflammation Index and Postoperative Cognitive Decline in Elderly Patients. Clin Interv Aging. 2022;17:699–705. doi: 10.2147/CIA.S357319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Ding J, Song B, Xie X, Li X, Chen Z, Wang Z, Pan L, Lan D, Meng R. Inflammation in cerebral venous thrombosis. Front Immunol. 2022;13:833490. doi: 10.3389/fimmu.2022.833490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Clancy U, Gilmartin D, Jochems ACC, Knox L, Doubal FN, Wardlaw JM. Neuropsychiatric symptoms associated with cerebral small vessel disease: a systematic review and meta-analysis. The lancet Psychiatry. 2021;8(3):225–236. doi: 10.1016/S2215-0366(20)30431-4. [DOI] [PubMed] [Google Scholar]
- 34.Inouye SK, Foreman MD, Mion LC, Katz KH, Cooney LM., Jr Nurses' recognition of delirium and its symptoms: comparison of nurse and researcher ratings. Arch Intern Med. 2001;161(20):2467–2473. doi: 10.1001/archinte.161.20.2467. [DOI] [PubMed] [Google Scholar]
- 35.Chen K, Yang YL, Li HL, Xiao D, Wang Y, Zhang L, Zhou JX. A gap existed between physicians' perceptions and performance of pain, agitation-sedation and delirium assessments in Chinese intensive care units. BMC Anesthesiol. 2021;21(1):61. doi: 10.1186/s12871-021-01286-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Kurisu K, Miyabe D, Furukawa Y, Shibayama O, Yoshiuchi K. Association between polypharmacy and the persistence of delirium: a retrospective cohort study. BioPsychoSocial Med. 2020;14:25. doi: 10.1186/s13030-020-00199-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Additional file 1: Figure A1. The receiver operating characteristics (ROC) curve of SII for POD. Table A1. Association between SII as continuous variable and POD in different models. Table A2. Association between SII as categories variables used quartiles and POD in different models. Table A3. Association between SII as categories variables with a cut-off value of 650 and POD in different models. Table A4. Univariate logistic regression analyses for POD in the Model PSM.
Data Availability Statement
The datasets generated and/or analysed during the current study are not publicly available as individual privacy could be compromised but are available from the corresponding author on reasonable request.