Abstract
Exosomes, known as a type of extracellular vesicles (EVs), are lipid particles comprising heterogeneous contents such as nucleic acids, proteins, and DNA. These bi-layered particles are naturally released into the extracellular periphery by a variety of cells such as neoplastic cells. Given that exosomes have unique properties, they can be used as vectors and carriers of biological and medicinal particles like drugs for delivering to the desired areas. The proteins and RNAs being encompassed by the circulating exosomes in B-cell malignancies are deemed as the promising sources for diagnostic and prognostic biomarkers, as well as therapeutic agents. Exosomes can also provide a “snapshot” view of the tumor and metastatic landscape at any particular time. Further, clinical research has shown that exosomes are produced by immune cells such as dendritic cells can stimulate the immune system, so these exosomes can be used in antitumor vaccines. Despite the great potential of exosomes in the fields of diagnostic and treatment, further studies are in need for these purposes to reach a convergence notion. This review highlights the applications of exosomes in multiple immune-related diseases, including chronic lymphocytic leukemia, multiple sclerosis, and arthritis rheumatoid, as well as explaining sundry aspects of exosome therapy and the function of exosomes in diagnosing diseases.
Keywords: Exosome, Cancer, Chronic lymphocytic leukemia, Acute myeloid leukemia, Rheumatic arthritis, Multiple sclerosis
Introduction
B-cell disorders include a highly heterogeneous class of disease. While the proportion of patients shows no symptoms and remains stable without therapy, some others indicate rapid progression of disease and need urgent treatment [1]. Emerging evidence has uncovered that, in B-cell-related malignancies such as B-cell chronic lymphocytic leukemia (B-CLL), cancerous cells require to be interacted with the tumor microenvironment (TME) to survive and proliferate [2, 3]. Actually, the growth of a tumor cell in vivo is mainly affected by the TME which comprises immune cells and the extracellular matrix constituents like cytokines and stromal components [4, 5]. Recently, “remote” communication tools of CLL cells have been discovered that they engage in novel molecular structures, namely extracellular vesicles (EVs). These particles are categorized into four categories based on their size and on the mechanism of biogenesis, all of which are secreted by all types of cells [6, 7]. The first time when EVs were discovered, they were assumed to be a kind of “rubbish bin”, to remove the unusual materials coming from exterior cells. Later, a growing body of evidence indicated that the EVs serve as functional delivery envelopes released from parental cells to other tissues. At the present, they are regarded as new actors playing a crucial role in cellular cross talks at closed and long distances facilitating cellular communications in health and disease [8, 9].
Exosomes, as one of the EVs, are responsible for the functional transfer of biologically active molecules including lipids, proteins and ribonucleic acid species (including mRNAs, miRNAs and lncRNAs) [10]. Exosomes can be secreted and uptaken by most types of cells, including immune cells. Intracellular proteins and extracellular stimuli regulate the biogenesis, secretion, and uptake of exosomes derived from immune cells. Cancer progression and metastasis can be regulated with immune cell-derived exosomes that facilitate the interaction between innate and adaptive immunity [11]. Among the immune cells, B cells are becoming increasingly clear as a potential major source of exosomes in vivo [12].It has been revealed that B cell-derived exosomes can play a key role in disease pathogenesis such as cancer via suppressing anti-tumor T cell responses [13].
Exosomes are known as double-layered lipid membrane vesicles, abundant in lipids, particularly sphingomyelin, phosphatidylserine, glycolipid GM3, and phosphatidyl ethanolamines [14]. These molecules are originated from the parental cells through the time of the exocytosis process, whereby the exosomes are able to carry their cargos throughout the bloodstream and lymph vessels to the target cells, thus affecting metabolism and phenotype of target cells [15]. As a matter of fact, the number of exosomes and also the composition of cargos may be divergent in normal and tumor situations, which is an indicator of tumor heterogeneity [16]. The content of exosomes reflects the cell activation state and can be affected by pathological processes from the origin tissue. In fact, releasing exosomes is a type of cellular adaptation mechanism, and the biogenesis compositions of exosomes and secretion thereof are influenced by the cellular microenvironment. Due to the current progress in high-throughput transcriptome assessment methods, analyzing the trace amounts of biomaterials of whole exosomes has become feasible [17].
On the exosomes secreted from antigen-presenting cells, glycosyl phosphatidylinositol-anchored proteins and also CD55 and CD59 as the complement regulators are lipid markers specific for exosomes [18, 19]. Exosomes alone are unable to perform the synthesis of functional proteins but have the ability to alter functional proteins at the first time when the cargo of RNA is transferred to a recipient cell [20]. Persuasive evidence has divulged that the regulation of exosomal mRNAs is carried out via attaching miRNA [21]. Unlike proteins or miRNA, exosomal mRNAs have not grabbed scholars’ attention to be used as disease-related biomarkers. Besides a number of technical challenges, due to selective packaging of exosome contents, exosomal mRNAs do not really represent the state of the origin cells. Furthermore, exosomal mRNAs may be exposed to degradation machinery, while there is no internal RNA control that can be taken into consideration for varied exosome yields [22]. Additionally, it has been represented that exosomes have both mitochondrial (mtDNA) and genomic (gDNA) DNA. The first DNA was envisaged to consist of one chromosome and to be capable of coding specific proteins involved in particular metabolic pathways, whereas the latter DNA is organized on the standard 46 chromosomes. Exosomal mtDNA can be found in a large number of cell types, especially glioblastoma and astrocytes cells [23]. The gDNA, denoting the total genome, is abundant in exosomes. However, there is no adequate proof of exosomal DNA, as disease biomarker. Furthermore, unlike protein and RNA molecules, DNA can be detected selectively and cell-dependently inside some exosomes. Notwithstanding having been carried out valuable surveys on exosomal DNA, mRNAs, and lipids in Rheumatoid arthritis (RA), the data provided below describe the function of the exosomal protein, miRNAs, and lncRNAs in RA[22].
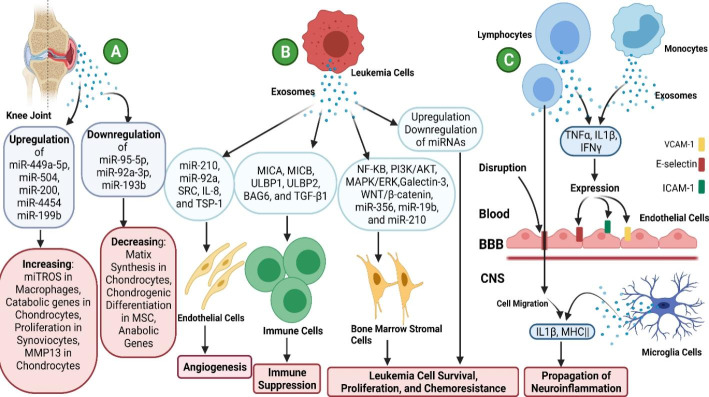
This review highlights exosome applications in different autoimmune diseases such as multiple sclerosis (MS), RA, as well as chronic and acute lymphocytic leukemia and discusses various aspects of exosome therapy as well as the continuous attempts in this field. (Fig. 1.)
Fig. 1.
Exosome Functions in B-cell Disorders: A) Chronic Lymphocytic Leukemia (AML), B)Multiple Sclerosis (MS), and C) Arthritis Rheumatoid (AR)
Exosome structure and function
Exosomes are spherical 40–150 nm nano-carriers generated from various cell types, encompassing cytoplasmic fractions without organelles. These type of vesicles are surrounded by double-layered lipid membranes in orientation to the original cells. Exosomes are rich in endosomal pathway proteins via CD9, CD81, and CD82, and their secretion into the extracellular space by various cells has been observed [24]. Exosomes eliminate excess debris within the cells or establish signaling networks between cells. The biogenesis of exosomes initiates within the endosomal system. Premature endosomes are capable of maturating to late endosomes, as well as to multi-vesicular bodies (MVBs) [25]. Throughout this process, late endosomes undergo the internal budding of the membrane, and intra-luminal vesicles (ILVs) are thus created inside the large MVBs [25], which contain large amounts of cholesterol and sphingolipid rafts and clathrin. However, the endosomal sorting complex required for the transport (ESCRT) components has more ability to form ILVs, which their large numbers are secreted as exosomes, while the amount remaining of which is degraded by autophagosome complexes and cellular lysosomes [26]. The small Rab GTPases, which comprise about 70 different proteins, are capable of controlling intracellular transportation and releasing exosomes from the plasma membrane. Rab11, Rab35, and Rab27 are among Rabs that can directly control the secretion of exosomes [27].
ESCRT is composed of about 30 protein members, which are assorted into five functional sub-complexes. ESCRT-0 – the first complex – identifies ubiquitous cargos (mostly proteins and rarely RNAs) via ALIX, Vps4, and Tsg101. The second, third, and fourth complexes, i.e. ESCRT-I, ESCRT-II, and ESCRT-III, manage the budding of ILV. Vps4 – the last and fifth complex – mediates not only ultimate membrane scission but also ESCRT recycling[28]. The sorting mechanism of RNA in the exosome is a subject that has thus far remained vague and less clear-cut. However, by distributing EXO-motif, exosomal RNAs facilitate their sorting into the exosomes. The exosome loading process is affected by cellular RNA abundance. There are also different mechanisms that contribute to the adsorption of cells such as comprising macro-pinocytosis, endocytosis, phagocytosis, clathrin-dependent, and clathrin-independent endocytosis, direct binding, and ligand-receptor interplay [29]. While transmembrane integrin arrangement on exosomes is a necessary marker for tissue-specific deliverance of these vesicles [29]. Exosomes, through their exterior or loaded macromolecules, trigger a variety of signaling pathways. During cellular stress, the secretion of exosomes enhances the preservation of cellular hemostasis and limits the innate immune response. Immoderate release of exosomes inhibits the cell-cycle and results in apoptosis induction. Within cell communication networks, exosomes are central mediators in varied physiological and pathological situations, such as autoimmune and infectious diseases, neurological disorders, cancers, clouding inflammation, regenerative medicine, and tissue repair [30]. The exosome-based delivery system has exceptional merits such as stability, specificity, and safety. For delivering cargos (i.e. interfering RNA or active pharmaceuticals) in a specific approach, exosomes can reach long-distance targets. Exosomes can also act as perfect vectors being able to escape from the degradation of lysosomes and phagocytosis. After being fused with the plasma membrane, exosomes effectively deliver their freights to the intended cells. In addition, exosomes are able to remain continuously in the blood circulation without notable induction of immune responses [31, 32].
Exosome and Cancer diagnosis
Biomarkers are defined as a “characteristic which is objectively assessed and analyzed as a marker in interventional therapy. These can be further classified as prognostic, predictive, and pharmacodynamics in the context of cancer. The normal course of cancer could be predicted by prognostic biomarkers. Response of patients to specific treatment might be assessed by using predictive biomarkers, and the efficacy of anti-tumor treatment can be measured by pharmacodynamic biomarkers [33, 34]. However, in order to be a useful clinical tool, a biomarker must have different criteria. Each cancer biomarker must represent the tumor’s characteristics, with a high degree of specificity and sensitivity, practical in usefulness, minimally invasive procedure, repeatable, and minimal cost [35]. Contents of exosomes represent the primary cells and reproduce the transcriptome and proteome of the original cell [36]. Therefore, the number of researches that study the possibility of exosomes as disease biomarkers has been increased significantly over the previous decade [37].
To summarize, exosomes are the realistic representation of the parental cell that produced them. Follow-up of circulating exosomes which carry proteins and RNAs in patients with B cell malignancy could represent a reliable source of biomarkers for prediction. Also, regular sampling could be possible because of the low invasiveness of their isolation. The progression of malignancies within patients can be tracked by assessing exosomes content, either before or after anti-cancer therapy, allowing physicians to choose the appropriate treatment option for each individual case [38]. Exosomes separated from the bloodstream of patients with head and neck cancer have protein signatures and oncogenic miRNA signatures [39]. In finding mutations in primary phase in non-small cell lung cancer (NSCLC), exosomes are more sensitive than Cell-free DNA (cfDNA) (25.7% compared to 14.2%, respectively) and more specific (96.6% and 91.7%, respectively) [40, 41]. Furthermore, a research conducted by Allenson et al., showed that a greater proportion of patients with pancreatic cancer in its early phases had more detectable kirsten rat sarcoma viral oncogene homologue (KRAS) mutations in exosomal DNA (exoDNA) than cfDNA [42].
The increase in exosome secretion by tumor cells could be due to specific mechanisms. Earlier research has demonstrated that hypoxia and stress in the TME are two reasons that could explain the increased secretions of exosome [43]. The Heparanase, p53 protein, and Rap GTPase proteins have all been found to modulate exosome production and secretion [44]. It is also been proposed that exosomes secreted by tumors in the first phase might be a possible means of early disease identification. Exosome-related protein marker was elevated in an in vivo model of pancreatic cancer before the tumor was identifiable by imaging methods [45]. By mediating biomacromolecule transfers, exosomes played a key role in mediating resistance to various therapies. Several studies in various cancers, such as breast cancer, colon cancer, and soft tissue sarcoma have shown that exosomes derived from drug-resistant cells can also make resistant in drug-sensitive cells by changing the drug-associated signaling pathways [46–49]. In short, these findings imply that tumor exosome biomarkers may have predictive and prognostic utility [50].
In cancer, exosomes are of specific interest as they are found all over the body and can be physiological or pathological bio-print. They can provide a “snapshot” view of the tumor and metastatic landscape at any particular time. The contents of exosomes, such as genetic material, are expected to be protected from degradation, enhancing the identification of clinically relevant alterations [51]. In the case of melanoma in humans, exosomes play a crucial role in modulating the antitumor immune response [52]. Zmigrodzka et al. showed by flow-cytometry that exosomes separated from plasma were higher in cancerous dogs than normal controls. This study included one melanoma-affected dog; however, it focused on exosomes released from platelets and leucocytes [53].
Exosome application in chronic lymphocytic leukemia (B-CLL)
B-CLL is considered the most frequent type of adult hematological malignancies worldwide. People over the age of 65 are prone to be afflicted by this disease, accounting for well over 40%. The average prevalence is nearly 5 in 100,000, annually and the incidence range rises with aging. CLL is diagnosed by clinical demonstrations, changes in the number and the ratio of lymphocytes in peripheral blood smear (PBS), physical examinations, microscopic examination of bone marrow smear, and finally flow cytometric characterization of the surface marker expression of leukemic B cells [54]. CLL-related single nucleotide polymorphisms (SNPs) have been found in highly expressed proteins such as lymphoid enhancer binding factor 1 (LEF1), B-cell lymphoma 2 (BCL2), and phorbol-12-myristate-13-acetate-induced protein 1 (PMAIP1) [55]. LEF1, which is expressed in pre-B and T cells, binds to the T-cell receptor-alpha (TCRA) enhancer and confers maximal enhancer activity, and also it controls the proliferation, survival, and differentiation of hematopoietic cells [56]. In addition, BCL2 family proteins play central roles in cell death regulation and can regulate diverse cell death mechanisms including apoptosis, necrosis and autophagy. They are the key regulators of the mitochondrial pathway of apoptosis. This pathway is required for normal embryonic development and for preventing cancer [57]. PMAIP1 also plays a role in the activation of apoptosis [58]. Dysregulation of miRNAs has been shown to be associated with the onset and progression of CLL. For instance, both the onset and progression of CLL are associated with the deregulation of miR-15a and miR-16-1[59]. As the expression levels of BCL2 and the zeta-chain-associated protein kinase 70 (ZAP70) – which turns on (activates) immune system cells called T cells – gene are suppressed by miR-15a and miR-16-1, decreased expression of these miRNAs can lead to increasing BCL2 and ZAP70, which are involved in inhibiting cell apoptosis [60]. A wide variety of procedures are used in treatment of CLL. For several decades, chloramphenicol is utilized as conventional standard therapy for CLL. The use of these drugs has been shown to be related to some restrictions such as adverse effects and risk of toxicity. Over the past decade, new targeted therapeutic approaches such as bruton’s tyrosine kinase (BTK) inhibitors and Bcl2 blockers as well as innovative therapies that modulate the immune response against cancer cells [61, 62]. Non-coding RNAs have been implicated in the development and progression of CLL in numerous studies. Some of these non-coding RNAs like microRNAs (miRNAs) and tRNA-derived small RNAs (tsRNAs) have been discovered to be important biomarkers that can be used to diagnose, monitor, and predict medication resistance, assisting clinicians in selecting treatment regimens that are suited to the patient’s needs [63].
Pathogenesis of CLL is related to the tumor-supporting environment. Lymphocytic cells are highly dependent on their environment for survival, so exosomes have emerged as the main mechanism of intercellular cross-talk which provide a promising environment for stimulating CLL progression [64]. The levels of CLL-derived exosomes were considerably higher, compared to healthy patients [65]. Exosomes protein carriers carrying CD markers have been shown to act as predictive biomarkers in patients with CLL at numerous stages of the disease. Elevated levels of HLA-DR, HLA-C, HLA-B, HLA-A, CD82,CD62L, CD55, CD44, CD31, CD19, and CD5 and low levels of CD63, CD49c, and CD21 were detected by using an antibody microarray profiling of the membrane protein which content of plasma exosomes, whereas none of these changes has been shown in exosomes derived from plasma of healthy individuals [66]. In particular, CD19 and CD37 from plasma exosomes were shown highly elevated in advanced clinical stages and were associated with a relatively high cancer burden [67]. The signaling pathway of B-cell receptor (BCR) plays a vital pathogenic role in CLL [68]. Mutations in the components of the BCR signaling that give rise to the continuous activation of downstream kinases are common [68]. Exosome secretion does not show a constructive mechanism in B cells, but it is triggered by external stimuli supported by several signaling interactions [69]. Inhibitors of these stimulants can be used to prevent or inhibit the secretion of exosomes by CLL cells to prevent contact with the tumor microenvironment and to prevent tumor progression [69, 70].
miRNAs exosomes in B-CLL
Dysregulated small non-coding RNAs are considered as major causatives of altered gene expression in cancer cells. This outstanding discovery paves the way for significant advances in the development of new and more efficient treatments for cancer. In B-CLL, the unbalanced miRNA profiles encouraged the development of anti-ROR1 antibodies and Bcl2 inhibitors [63].
Among the diverse range of molecules transported by exosomes, we will focus on miRNAs differentially expressed by CLL cells. MicroRNAs are short, highly conserved non-coding RNA molecules of about 20 nucleotides that post-transcriptionally interfere with protein expression by direct transcript degradation or translational repression. MicroRNA expression is not always fixed and depends on the source of cells and physiological or pathological situations. MiRNAs have grabbed the attention of many scientific researchers because they seem to be beneficial tools for interfering with mammalian RNA genes for in vitro studies to determine the target genes’ duty [71, 72]. The regulatory role of miRNAs on gene expression plays a key role in the initiation and progression of cancer. Tumor cells related microenvironment dictates the expression level of miRNAs to increase the expression of pro-survival genes and repress the anti-tumorigenic genes. For instance, the upregulated expression of c-Myc transacting factor in cancer is due to an increase in the expression level of a set of miRNAs that suppress their target tumor suppressor transcripts [73]. In addition, miRNAs can play as tumorigenic, so-called “oncomiRs”, while they suppress pro-apoptotic or anti-proliferative targets [74].
Several studies indicate the release of miRNAs in exosomes derived from CLL. Table 1 summarizes the most plentiful miRNAs observed in the CLL-derived exosomes and their potential roles.
Table 1.
Exosomal miRNAs in B-CLL
| mRNAs | Expression in CLL |
Target | Function | Oncogenic or Suppressive | Refs. |
|---|---|---|---|---|---|
| miR-202-3p | Upregulated | Sufu gene |
‘suppressing fused’ (Sufu) is targeted by gene of miR-202-3p increase, modulator of the Gli Hedgehog signaling pathway -During development, it is thought to be involved in pattern formation and cellular proliferation. - decreasing in the intracellular level of this miRNA causes an increase in the expression level of Sufu, which aids tumor cell survival and progression. |
Oncogene | [69, 71] |
| miR-146a/miR-451 | Upregulated | Kinases in Stromal cells | inducing the stromal cells activation by phosphorylation of several kinases | Oncogene | [69, 71, 75] |
| miR-150 | Upregulated | c-Myb | playing an important role in the process of hematopoiesis, particularly in the development of lymphoid lineage | Oncogene | [69, 71] |
| miR-19b | Upregulated | TP53 and MKI67 | TP53 downregulation and MKI67 upregulation as tumor cell proliferation, survival, and invasion mechanisms | Oncogene | [69, 76] |
| miR-155 | Upregulated | SHIP1 | In CLL, it has an oncogenic role; it promotes the BCR response by targeting SHIP1. | Oncogene | [69, 71] |
| miR-29 | Downregulated | TCL1 |
regulation of TCL1, MCL1 and DNA-methyltransferases |
Tumor suppressor function in aggressive CLLs (downregulated versus indolent CLL) |
[69, 71] |
| miR-223 | Downregulated | HSPs | HSP90B1 | Oncogene | [69, 77, 78] |
| Y RNA | Upregulated | it is overexpressed in tumors and is essential for cell proliferation | Oncogene | [69, 79] |
miRNAs are selected by CLL leukemic cells to be packed into the circulating exosomes to adjust the expression of their target genes in support of tumor cells’ proliferation and progression [69]. Exosomes originated from CLL cells have a high level of miR-202-3p [80, 81]. The other two miRNAs that are differentially upregulated in the CLL-derived exosomes are miR-146a and miR-451, which switch stromal cells to cancer-associated fibroblasts (CAFs) [82]. In fact, exosomes released from the CLL cells with a cargo of miR-146a and miR-451 by delivering their cargoes to stromal cells activate their target genes by phosphorylation of several kinase proteins. Furthermore, CAFs can also produce many inflammatory signals, such as cytokines and proangiogenic factors, thereby promoting tumor development and invasiveness [83]. The expression level of miRNAs (serum levels or intracellular levels) depends relatively on the phenotypic characteristics of invasive CLL. Among these miRNAs, miR-150 has a pivotal role in hematopoietic events, particularly in lymphoid lineage development and differentiation [84]. miR-150 functions are correlated with the ζ-chain-associated protein of ZAP-70 expression or the unmutated immunoglobulin heavy variable (IGHV) genes when the common molecular characteristics of poor prognosis are examined [85]. Despite the abundant upregulated expression of miR-150, either free or bound to the serum protein in circulation, CLL-derived exosomes can protect it from decomposing by RNAse, thus sustaining its pro-tumorigenic properties [86]. Interestingly, miR-155 and miR-150 expression in exosomes is positively correlated with BCR activation. miR-155 and miR-150 in serum exosomes could be valuable diagnostic biomarkers for patients with an activated BCR pathway who might take advantage of treatment with BCR-related kinase inhibitors. Moreover, serum EV-miR-155 could be a useful indicator of disease transformation from monoclonal B-cell lymphocytosis (MBL) to CLL. Ferrajoli et al. Plasma miR-155 levels of exosomes could be valuable biomarkers for the probability of transition from MBL to CLL [87].
miR-155 family is highly expressed in mature B and T cells and plays a key role in the differentiation of hematopoietic lineage, viral infections, inflammation, and cancer and immune system regulation [88]. Examination of exosomes originated from CLL shows that these vesicles have large amounts of miR-155 which can trigger and sustain the myeloid-derived suppressing cells (MDSCs) in a vitamin D-related stage [89]. The MDSCs are newly identified immature myeloid cells that are characterized by the ability to suppress immune responses and expand during cancer, infection, and inflammatory diseases [90].
A recent study has investigated circulating exosomes in CLL leukemic cells and found upregulated miR-19b as a predictor of the development of resistance to chemotherapy in CLL [91]. Yeh et al. investigated the entire collection of miRNAs that could be dysregulated in both CLL-derived exosomes and CLL cells. They discovered that miR-29 is expressed similarly in both CLL cells and normal B cells, but that CLL-obtained exosomes had elevated amounts of miR-29 than normal exosomes [68]. It seems that miR-29 plays a vital role in blood cancers by modulating T-cell leukemia/lymphoma protein 1 (TCL1), myeloid cell leukemia 1 (MCL1), and DNA-methyltransferase enzymes [92]. Some researches show that miR-223 has lowered expression in CLL-derived exosomes in comparison with healthy individuals. Moreover, miR-223 was shown to be downregulated in invasive stages of CLL and was linked with poor prognosis [93]. In vitro secreted exosomes, enriched with mt-circRNAs and upregulated mt-COX2, have been detected in a well-known CLL cell line MEC-1 [81]. The MEC1 and MEC2 are EBV-contaminated lines that were established earlier from blood-derived cells of a chronic lymphocytic leukemia (CLL) patient at different stages of progression towards prolymphocytoid transformation. In a number of ways, these lines are unique. By rearrangement of immunoglobulin genes, their common clonal origin was demonstrated. In vitro, the same indigenous strain of epstein-barr virus (EBV) caused the cells to proliferate. Their phenotypic differences are indicative of subsequent subclones emerging from the CLL population [94].
Apparently, mt-COX2 overexpression is linked to leukemogenesis and poor outcomes. This finding establishes the groundwork for the acceptance of mt-COX2 as a novel CLL prognostic biomarker [95].
Exosome application in other Leukemia
Exosome in chronic myeloid leukemia (CML)
Chronic myeloid leukemia (CML) is among the hematological malignancies affecting adults, with an expected prevalence of 1–2 cases per 100,000 [96, 97]. The significance of the microenvironment in leukemia development has been proven in recent years. Exosomes have been recognized as important intermediaries of communication in the midst of leukemia cells and the stromal microenvironment. Exosomes obtained from CML cells could be taken up by endothelial cells and boost endothelial cell tube formation [98]. It is worth mentioning that exosomes from K562 cell line, which are of the erythroleukemia type, can induce dasatinib-sensitive Src phosphorylation and activate downstream proteins in endothelial cells [99]. Furthermore, a study showed that premiR-92a, which originated from K562 exosomes, could decrease the expression of the target gene integrin a5 and then improve endothelial cell movement and tube formation [100]. miR-210 from CML exosomes has also been shown to interact with the target gene Ephrin-A3 and play a vital role in angiogenesis and vascular endothelial growth factor (VEGF) signaling [101].
These studies indicate how leukemia cells may transmit signals to the microenvironment and prove the curative potential of exosome-derived miRNAs in combination with presently accessible VEGF inhibitors [100, 101]. Furthermore, exosomes derived from CML can establish an autocrine loop with their parent cells via a ligand-receptor interaction. This kind of loop is mediated by exosome-associated transforming growth factor beta 1 (TGF-β1) and subsequent activation of the extracellular signal-regulated kinases (ERKs), protein kinase B (PKB), also known as AKT, and nuclear factor kappa B (NF-κB) signaling pathways, resulting in augmented CML cell expansion and survival [102].
These data show the importance of exosomes in cancer biology. In a co-culture of K562-derived exosomes with bone marrow mesenchymal stem cells (BM-MSCs) and macrophages, the expression of several genes including tumor necrosis factor alpha (TNF-α), Wnt family member 5 A (Wnt5a), interleukin-6 (IL-6), C-X-C motif chemokine 12 (CXCL12) and Dickkopf-related protein1 (DKK1) was altered. This led to increased production of nitric oxide (NO) and consequently the production of reactive oxygen species (ROS) which was reduced in a time- and dose-dependent fashion [103].
Exosomes derived from human umbilical cord mesenchymal stem cells (hUCMSC) could improve the sensitivity of K562 cells to imatinib (IM) by activating the caspase apoptotic pathway by increasing Bcl-2 associated X (Bax) expression and lowering Bcl-2 levels. Thus, a combination of IM with hUCMSC-derived exosomes may be a hopeful method to improve the efficiency of CML treatment [104]. Min QH showed that the level of miR365 was considerably higher in exosomes that come from drug-resistant CML cells in comparison with sensitive cells. In parallel, IM sensitive CML cells transfected with pre-miR365 exhibited lower chemo-sensitivity and apoptosis rate when it is compared with controls. Exosomal delivery of miR-365 may lead to drug resistance by preventing the production of pro-apoptosis proteins in non- resistant CML cells [105].
Moreover, a BCR-ABL transcript was discovered in exosomes derived from CML cell lines and CML patients sera, indicating the potential of exosomes as detection targets for BCR-ABL [106].
Exosomes in Acute myeloid leukemia
Acute myeloid leukemia (AML) is a type of hematological malignancy that manifests rapid cellular proliferation and poor prognosis. Compared to parental cells, the presence of miRNAs was known to be greater in exosomes derived from AML cells. Nine hematopoiesis/ leukemogenesis-related factors (i.e., c-Myc, myocyte enhancer factor 2 C (MEF2C) [20], CCAAT/enhancer-binding protein alpha and -beta (CEBP-α/-β), E2F transcription factor 1 (E2F1), inhibitor of DNA binding 1 (ID1), SH2-domain-containing inositol 5′-phosphatase 1 (SHIP1), forkhead box P3 (FOXP3), and GATA-binding factor 1 (GATA1)) and five specific biomarkers (i.e., insulin-like growth factor type 1 receptor (IGF-1R), matrix metalloproteinase-9 (MMP9), C-X-C chemokine receptor type 4 (CXCR4), fms related receptor tyrosine kinase 3 (FLT3), and nucleophosmin 1 (NPM1)) associated with the prediction of AML were discovered in the relating exosomes. Kaplan-Meier analysis similarly showed that an increased miR-125b level was related to higher accumulative relapse and total death rates [107]. These data recommend possibly strong regulation of AML development by exosomes. Furthermore, higher levels of miR-223, miR-191, miR-155, miR150, miR-99b, miR-9 and let-7a (ranging from 2- to 40-fold) have been found in AML cell-derived exosomes, compared to the parental cells [108]. For instance, among mature miRNAs existed in both cellular and exosomal samples, Hornick et al. identified a set of upregulated Serum exosomal miRNAs, such as miR-150, miR-155, and miR-1246, as minimally-Invasive early biomarker of AML [109] BM-MSCs are shown to be able to uptake the exosomes released by AML cells. In an experiment, expression of CXCR4 – a target of miR150 – was significantly declined in BM-MSCs after co-culture with AML cell-derived exosomes and the movement of AML cells toward the chemokine stromal cell-derived factor-1 (SDF-1) was markedly decreased [108].
Moreover, Zhang. L et al. investigated that AML is affected by miR-425-5p loaded in exosomes derived from BM-MSCs. They indicated that the expression of miR-425-5p, participating in different cancer types, decreased in CD34 + CD38-AML cells and exosomes of AML patients, as well as AML cell lines, compared to the bone marrow healthy cases or generally healthy cases. BM-MSCs-derived exosomal miR-425-5p significantly inhibited cell viability, invasion and migration, and induced apoptosis of AML cells via upregulation of cleaved poly (ADP-ribose) polymerase (PARP) and cleaved caspase3 and downregulation of wilms tumor 1-associated protein (WTAP) [110].
AML cell-derived exosomes have also been shown to suppress the residual hematopoietic functioning preceding widespread leukemic bone marrow metastasis directly or by mediating stromal elements. Exosomes that are derived from AML cells could downregulate critical retention factors (like C-X-C motif chemokine ligand 12 (CXCL12) and stem cell factor (SCF)) in stem cells, and lead to mobilization of hematopoietic stromal and progenitor cell (HSPC) from bone marrow. On the other hand, these exosomes directly modulate HSPCs by decreasing clonogenicity and declining expression of c-Kit, CXCR4, and other hematopoietic transcription factors (i.e., c-Myc). In addition, exosomes of leukemia blasts could indirectly prohibit hematopoietic progenitor cell (HPC) activities. This suppression occurs indirectly by stromal reprogramming of niche-retention factors and re-arranges the bone marrow niche into a microenvironment which allows leukemia progression [111]. AML-derived exosomes also, can inhibit the expression of the hematopoietic factor DKK1 inducing the downregulation of hematopoietic stem cell promoters in bone marrow stromal cells and creating a favorable microenvironment for the proliferation and survival of leukemia cells. Moreover, through overexpression miR-21 and miR-29, AML exosomes promote the survival of healthy hematopoietic stem cells and induce leukemia-like functional features in them [112, 113].
Chemoresistance is a regular rampant event that happens in AML cells. Exosomes have also been found to take part in the progress of drug resistance in myeloid neoplasms [111]. AML cells are shown to release exosomes that contain VEGF/VEGFR factors that cause glycolysis in hUVECs, leading to vascular re-arrangement and chemo-resistance [114]. AML-derived plasma exosomes mediate the intercellular transmission of regulatory proteins, such as MCL-1, BCL-2- like 1 isoform 1 (BCL-XL), and BCL-2. Accordingly, these exosomes were recognized as important causes of treatment resistance, that is, exosomes have been found to have impacts on the progress of drug resistance in myeloid neoplasms [114]. Liu et al. found that PI3K/AKT/ mTOR signaling and autophagic activity were enhanced markedly in the IM-resistant CML cell line K562 (K562RIMT). Moreover, mTOR-independent beclin-1/Vps34 signaling pathway was found to have participated in exosome release from the relating cells [115]. Dasatinib can boost apoptosis by interfering with AKT/mTOR function and also stopping exosome release and preventing autophagy through decreased expression of Vps34 and beclin-1 in K562RIMT cells. In another study, the bioactivities of leukemia stem cells (LSCs) were investigated via AML-derived miR-1246. The results indicated that AML derived miR-1246 is highly-expressed and directly-targeted the human leucine rich repeats and immunoglobulin like domains 1 (LRIG1), as a negatively regulator of receptor tyrosine kinase signaling, to activate the signal transducer and activator of transcription 3 (STAT3) pathway so that, by up-regulating LRIG1, miR-1246 inhibitor/EV-encapsulated miR-1246 inhibitor can suppress the viability and colony formation abilities but promote the apoptosis and differentiation of LSCs through inactivation of STAT3 pathway [116]. Exosomal miRNAs associating in CML and AML are illustrated in Table 2.
Table 2.
Exosomal miRNAs associating in CML and AML
| miRNA | Malignancy | Alteration mode | Function/description | Refs. |
|---|---|---|---|---|
| Pre-miR-92a | CML | Increased | Down-regulating the integrin a5 and improving endothelial the cell movement and tube formation. | [100] |
| miR-210 | CML | Increased | Interacting with Ephrin-A3 and playing a vital role in angiogenesis and VEGF signaling. | [101] |
| miR365 | CML | Increased | Drug resistance by preventing the production of pro-apoptosis proteins. | [105] |
| miR-150, miR-155 and miR-1246 | AML | Increased |
Their high serum levels lead to considering them as minimally-invasive early biomarker of AML. promoting the apoptosis and differentiation of LSCs through inactivation of STAT3 pathway. |
[109] |
| miR-425-5p | AML | Decreased | Inhibiting cell viability, invasion and migration via inducing apoptosis genes of AML cells such as cleaved PARP, cleaved caspase3 and Wilms tumor 1-associated protein (WTAP). | [110] |
| miR-21 and miR-29 | AML | Increased | Promoting the survival of healthy hematopoietic stem cells and inducing leukemia-like functional features in them | [112, 113] |
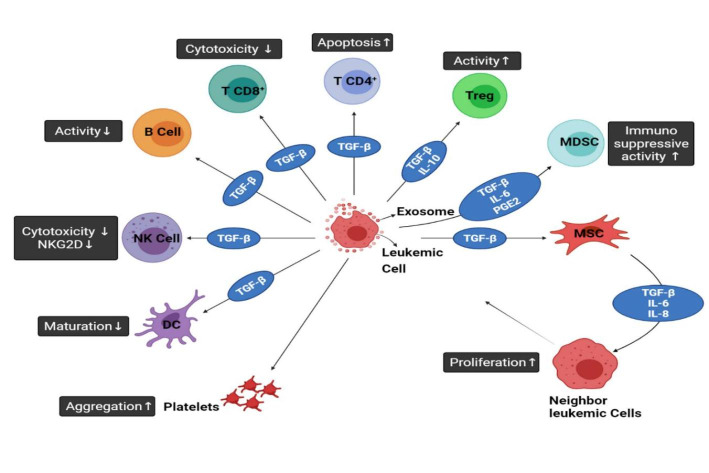
Szczepanski et al. [117] found that the exosomes derived from blasts in the sera of AML patients have large amounts of TGF-β1 protein and prevent the cytotoxicity of the NK cells. A potential function of exosomes in predicting response to therapy (like chemotherapy) was assayed in AML patients. It was evident that TGF-β1 levels were higher in AML exosomes. These values declined after induction chemotherapy, increased during consolidation chemotherapy, normalized during long-term and complete remission. Figure 2. shows various effects of exosomes originated from leukemic cells on immune system. As demonstrated in Fig. 2, one of the reasons for progression of leukemia is caused by the fusion of late endosomes with the cytoplasmic membrane and, subsequently, the production of exosomes by a leukemic cell. These exosomes are contained molecules such as TGF-β that promote leukemia. Exosomal TGF-β decreases cytotoxicity and activity and increases apoptosis in CD4+ and CD8+T cells. TGF-β has also similar effects on the activity of B cells. TGF-β shows its effect on natural killer cells (NK cells) by reducing the number of surface receptors NKG2D (C-type lectin-like receptors) and cytotoxicity. The presence of this receptor on NK cells and the presence of its ligand on cancer cells cause cancer cells to lysis. Therefore, lowering of NKG2D plays a critical role in escaping the immune system. TGF-β plays an important role in escaping of leukemic cells from the immune system by preventing of dendritic cells (DCs) cells from maturing. TGF-β affects regulatory T cells (Treg cells) by increasing their activity, and also it boosts the activity of MDSCs along with prostaglandin E2 (PGE2) and IL-6.
Fig. 2.
Different Effects of Exosomes Generated from Leukemic Cells on The Immune System. Furthermore, the influence of leukemia-derived exosomes and their cargoes on MSCs has been demonstrated
Correlation between Exosome and multiple sclerosis (MS)
Multiple sclerosis (MS) is an autoimmune disease, defined by chronic inflammation, demyelination, leading to neurological impairment [118, 119] The most common cause of neurologic dysfunction in young adults is MS [120]. Inflammation, demyelination and neuro-axonal injury are renowned features of MS that affect the central nervous system and cause long-term persistent disability [120]. Treatment choices for MS are limited and include common immunosuppressives, immunomodulatory agents, or compounds that inhibit lymphocyte infiltration into the CNS [121].
The raid of auto-reactive CD4+ T cells (especially Th17and Th1 cells) into the CNS, is a main immune-pathologic characteristic of multiple sclerosis, leading to neuro-axonal degeneration and disability. According to the literature, microRNAs also play crucial roles in the pathology of MS [74, 122, 123]. Since exosomes can cross the blood-brain barrier, it is likely that some circulating exosomes originated from affected CNS cells or the related inflammatory microenvironment be engaged in MS patients [124, 125]. Cells’ exosomes are major carriers of miRNAs into the circulation protecting them from degradation. Accordingly, exosomal miRNAs seem to be more stable than free miRNAs and leukocyte-derived exosomal miRNAs could provide useful information about MS pathogenesis [126–128]. Ebrahimkhani et al. assumed that physiological alterations linked to the initiation and progression of MS are reflected in a variety of exosomal miRNAs in serum. They revealed that serum exosomal miRNA profiles can accurately identify MS patients from healthy controls, as well as relapsing-remitting multiple sclerosis (RRMS) from progressive disease by next-generation sequencing (NGS) and integrative bioinformatics [129].
Additionally, the development of Th1 and Th17 inflammatory cells has been shown to be induced by miR-155 and mir-326. Du et al. indicated that mice lacking MicroRNA-155 are resistant to experimental autoimmune encephalomyelitis (EAE) [130]. Some miRNAs like miR-146a and miR-29, on the other hand, have been linked to the prevention of autoimmune disorders. MicroRNA-146a inhibits Th1 cell activity by activating regulatory T cells [122, 123]. Moreover, the production of gamma interferon (IFN-γ) is suppressed by miR-29 and miR-29 deficient cells produce significantly more IFN-γ compared to normal cells [131]. In addition, a dysregulated miRNA profile is evident in leukocytes of MS patients [132, 133]. Keller et al. demonstrated that among patients with RRMS, 165 miRNAs were substantially up- or down-regulated in comparison with healthy controls [134]. Similarly, miR-106b and miR-25, which can potentially regulate TGF-β signaling pathway, have lowered expression in regulatory T cells of MS patients [135]. Thus, the pathology of MS may be affected by the alteration of miRNA expression. A recent study by Azimi et al., found an altered abundance of miR-326 in exosomes derived from conventional T cells from MS patients [136]. It has been previously shown that miR-326 has a prominent role in the immunopathogenesis of MS via Th17 cells maturation and differentiation [130]. Consequently, exosomal miR-326 may be a clinical goal in the course of MS. Additionally, deregulation of this miRNA may be used as a diagnostic and prognostic biomarker [137].
Dendritic cells (DCs), the important modulators of adaptive immune reactions, have recently been known as scalable sources of exosomes in vitro in MS. Depending on the external factors and cell conditions, the composition of DC exosomes differs from one another. For instance, the profiles of exosomal miRNAs differ noticeably between mature and immature lipopolysaccharide-stimulated DCs [138].
Pusic et al. have found that phasic stimulation with low-level IFNγ could significantly improve myelination in cultured brain slices or following nasal administration to animals. Then, they used low-level IFNγ for primary DC cultures stimulation and assessed the miRNA affecting the function of exosomes [139]. Previous experiments have demonstrated that peripheral exosomes can possibly affect brain myelination through the delivery of miR-219 [139]. It was deduced that exosomes released by IFN-stimulated DCs (IFNγ-DC-Exos) can improve the myelination process and oxidative tolerance. Additionally, administration of IFNγ-DC-Exos in slice culture increased recovery from MS-like demyelination. It was endorsed that nasally administered IFNγ-DC-Exos can improve brain myelination in vivo. In vitro tracking studies indicated that oligodendrocytes and microglia (to a smaller degree) preferentially absorb IFN-DC-Exos. This is an elementary step in understanding the mechanisms of exosome-mediated myelin development, and the introduction of exosomes as therapeutic agents for re-myelination [140].
The understanding of miRNA’s role in MS has advanced remarkably over the last decade. In a pioneering study, miR-155 was recognized as the main regulator of inflammatory reactions. In mice, targeted deletion of this gene led to a decrease in cellular differentiation of Th1 and Th17 in both the CNS and peripheral lymphoid organs. Also, miR-155 deletion and pharmacological targeting both resulted in a delay in the course and severity of EAE [141]. In another investigation, miR-155-3p was discovered to cause the development of autoimmune demyelination by regulating heat shock protein (HSP) [142]. MiR-301a also was found to have a central role in the regulation of myelin-reactive T-helper type 17 cells, supporting the role of miRNAs as therapeutic agents for regulating autoimmune demyelination [143]. Beside their function in regulating the responses of effector inflammatory T cells, they also play role in modulating the Treg cells population which in normal counterbalances the former. Surprisingly, Treg formation and function have also been affected by miR-155, to such an extent that miR-155 is regulated by Foxp3 which is a characteristic transcription factor for this cell type [144]. The intricacy of the immune system’s regulatory networks is highlighted by the opposite functions of the same miRNA in different cells. While the regulating role of miRNA in pro-inflammatory responses during EAE was highlighted in the preceding cases, further research also revealed their main role in regulating myelination itself. For instance, myelin thickness has been increased in mice by overexpressing miR-23a, and also studies have shown that the synthesis of myelin and of oligodendrocyte differentiation are both increased by miR-23a in vivo [145].
Despite having been discovered many drug delivery systems such as chemical small-molecule drugs, protein drugs, or nucleotide drugs, exosomes have been demonstrated to have a lot of use in modern medicine [146]. It has been shown that exosomes are able to cross the blood brain barrier (BBB) and responsible for spreading brain antigens to the periphery. Microglia-derived exosomes were injected into the central nervous system (CNS) of EAE animals, which increased inflammation and exacerbated illness [147].
Mesenchymal stem cells (MSCs) stimulated by IFNγ produced exosomes have been demonstrated to have a noticeable effect on treating EAE. These findings showed that exosomes derived from MSCs can be employed as cell-free treatments for autoimmune and CNS illnesses [148]. Application of exosomes derived from overexpression of TGF-1 dendritic cells for the treatment of EAE leads to enhanced Treg production and suppressed Th1 and Th17 differentiation, resulting in a weakened intensity of EAE [149]. Casella G. et al. designed a mouse microglial cell line secreting high quantities of engineered exosomes carrying the anti-inflammatory cytokine IL-4. Following the administration of the mentioned exosomes, the clinical score of EAE was dramatically declined [150]. Also nasal administration of curcumin-loaded exosomes in mice with lipopolysaccharide (LPS)-induced encephalitis led to a reduction of neuroinflammation by targeting microglia [151]. Moreover, exosome-encapsulated curcumin exhibited improved anti-inflammatory effects in LPS-induced inflammatory demyelinating models [152].
Pusic et al. pointed out that exosomes generated by bone marrow-derived dendritic cells could be used as a therapeutic medium for oligodendrocyte maturation [125]. In vivo studies showed that the maturation of oligodendrocytes and recovery of myelin damage could be promoted by using these exosomes. Accordingly, exosomes may not only aggravate inflammation during EAE but also promote myelin regeneration [146].
New data on the use of miRNAs and other molecular cargos carried by circulating exosomes as biomarkers for a variety of diseases has attracted a great deal of interest in the significance of these microvesicles as a possible indicators of MS state and disease monitoring [153] (Table 3.). Interestingly, exosomes in the blood reveal the presence of CNS markers originated from the brain [154]. The analysis of these exosomes could provide an exclusive tool for understanding the status of the CNS and eliminate the need for biopsy [155]. Furthermore, exosomes could be a source of the BBB-crossing CNS antigens [154] that could provoke more investigations into exosome analysis for understanding CNS conditions and MS [156].
Table 3.
Exosomal mRNA as biomarkers in MS
| mRNA | Source of exosomes | Function | Refs. |
|---|---|---|---|
| miR-326 | Conventional T cells | differentiation and maturation of Th17 | [136] |
| let-7i | Plasma | inhibit the initiation of regulatory T cells | [157] |
| miR-15b-5p | Serum | Targets FGF-2 implicated in Demyelination and remyelination | [158] |
| miR-451a | Serum | Regulator of oxidative stress | [158] |
| miR-30b-5p | Serum | Neuro-axonal injury | [158] |
| miR-342-3p | Serum | Neuro-axonal injury | [158] |
| miR-122-5p,miR-196b-5p,miR-301a-3p,miR-532-5b | Serum | Targets STAT3 and AHR, differentiation and regulation of Th17 | [159] |
Exosome and rheumatic arthritis
Rheumatoid arthritis (RA) is an autoimmune inflammatory disease that involves 0.5-1% of the world’s adults [160]. Women are three times more vulnerable than men, and the highest frequency of this autoimmune disease is between the ages of 40–50. Rheumatoid arthritis usually causes joint damage as well as disability. Early diagnosis and treatment may prevent joint destruction and also achieve good results in the long term. Because most irreversible joint damage occurs in the first two years of illness, optimal disease management is essential in the first three to six months [161–164]. Therefore, a reliable biomarker is needed for the timely diagnosis of the disease and effective disease management. Some features of RA are infiltration of immune cells in the joints, joint pain, and bone erosions. Different auto-antibodies have been identified based on their antigen type in RA disease that the two most common types of these auto-antibodies are anti-citrullinated protein antibodies (ACPA) and rheumatoid factor (RF). Like other rheumatoid diseases, many factors are engaged in the pathogenesis of RA, including environment, genetic background, and serological elements. It has been found that the effect of genetics is about 50 to 60%, so genetic factors play an important role in the development of RA disease. Most of the genes that cause RA, which account for about 30 to 50% of the genetic factors involved in causing RA, belong to human leukocyte antigen (HLA) genes [164–167]. Multiple risk alleles associated with RA which are located in the HLA-DRB1 gene cause the production of a conserved amino acid sequence. Recent advances in genome wide association studies (GWAS) have enhanced our understanding of the influence of genetic factors on the development of RA, and also revealed that RA is a polygenetic disease. These studies have linked more than 100 genetic loci that enhance the risk of developing RA [165, 168–171]. One of these important genes that plays an important role, especially in Japanese populations, is the peptidyl arginine deiminase 4 (PADI4) gene. Also, an R620W mutation in PTPN22 is another missense risk variant in RA disease. PTPN22 encodes a protein tyrosine phosphatase in hematopoietic cells. In T and B cells, this enzyme works as a negative modulator of the antigen receptor signaling pathways. The R620W risk allele is a gain-of-function mutation that attenuates TCR and BCR signaling pathways in cells that carry this risk allele. The HLA locus has been linked to higher serum levels of antibodies against citrullinated protein and has been linked to seropositive RA [165, 168–171].
Moreover, there are some biological treatments for RA that target inflammatory factors like TNF-α. These antibodies and proteins are mostly sedative and cannot reverse the symptoms of RA. Recently, gene therapy has yielded encouraging preliminary outcomes; nonetheless, its different aspects are still under investigation [172]. Numerous studies have shown that vesicles can be good carriers of drugs due to their unique properties. Exosomes can deliver their drug cargoes to targets because of their ability to cross different biological membranes like synovial membranes [172]. In the blood stream, exosomal packed curcumin has a longer half-life than free curcumin. Therefore, encapsulation of the drugs in the exosomes increases the half-life of the drugs [173]. Thus, in inflammatory diseases and RA, exosomes seem to be promising transfer tools for a variety of drugs. For example, in collagen-induced arthritis (CIA) mice in which miR-146a/miR-155 was downregulated, the miR-146a/miR-155 transduced MSC-derived exosomes significantly altered the Treg cells levels of CIA mice cell and recovered their appropriate responses [174] A similar study was done on therapeutic effect of MSC–derived miR-150-5p exosomes (Exo-150) on collagen-induced arthritis mice. The results revealed that injection of Exo-150 reduced hind paw thickness and the clinical arthritic scores in modeled mice. Moreover, Exo-150 decreased migration and invasion in RA fibroblast like synoviocytes (FLS) and downregulated tube formation in HUVECs by targeting MMP14 and VEGF [175].
Exosomes can deliver anti-TNF-α and other anti-inflammatory drugs to their destination without being degraded by different enzymes. In this line, some features of exosomes, such as immunosuppressive and anti-inflammatory properties, have been identified in different diseases, such as CIA and inflammatory bowel disease (IBD) [176, 177].
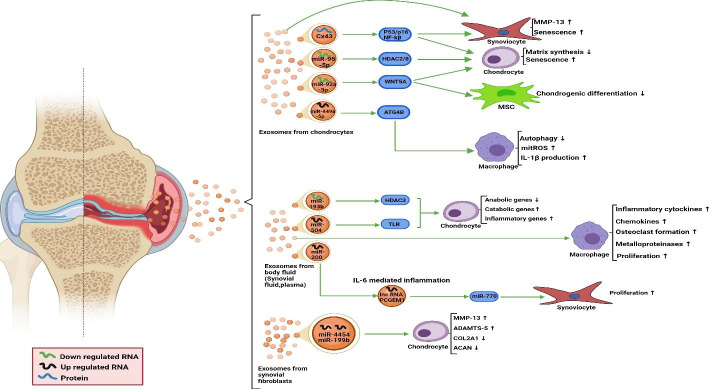
Numerous studies have shown that exosomes play effective roles in cell-cell communication (Fig. 3.).
Fig. 3.
Exosomes involved in pathology of RA
Furthermore, exosomes are involved in other activities such as the transfer of genetic information and signaling compounds, antigen presentation, and immune regulation. Exosomes transport receptors and ligands, as well as peptide-MHC complexes and antigenic material, so they play an effective role in regulating immune responses. It has shown that exosomes found in fluid are released by cells that have penetrated knee fluid. Different cells that infiltrated into the synovial joint release exosomes into the synovial fluid to injury the joint and sever the RA adverse symptoms. These exosomes can be contained different miRNAs, such as hsa-miR-151a-3p, hsa-miR-199a-5p, hsa-miR-370-3p, hsa-miR-589-5p, and hsa-miR-769-5p, to be connected with the common pathogenesis of RA [178].
Approximately, in the synovial fluid of people with inflammatory arthritis such as RA, the most common exosomes found are originated from platelets [179]. In addition, the presence of exosomes derived from neutrophils, monocytes, and granulocytes has been described. According to the literature, B and T cells could release exosomes in the synovial fluid, inasmuch as exosomes extricated from T cell are more abundant in the RA synovial fluid and have a significant correlation with rheumatoid factor serum levels [179].
human T lymphocytes also, can release exosomes containing numerous amounts of miR-204-5p which can be transferred into synovial fibroblasts and inhibit cell proliferation. Exosomal miR-204-5p expression is inversely correlated with disease parameters of RA patients, such as rheumatoid factor, erythrocyte sedimentation rate, and C-reactive protein [180].
In general, exosomes that have been derived from synoviocytes, in inflammatory diseases such as RA, promote adjacent cells to release inflammatory agents and cause cartilage damage. It has been revealed that dendritic cells treated with IL-10 can release exosomes which reduce the severity of RA. Exosomes derived from IL-1-stimulated fibroblast-like synoviocytes are shown to induce the osteoarthritic alterations in chondrocytes [181]. In RA models, exosomes have immunological activities such as motivating apoptosis, antigen-presenting to T cells, and extracellular damages [182]. This evidence confirms the use of synovial-derived exosomes as a RA biomarker to anticipate disease stages and to develop novel and more effective treatments. The pathogenesis of RA may be due to exosomes which establish cell-to-cell communication and participation thereof in many functions such as inflammation, delivery of miRNAs, destruction of extracellular matrix, antigen presentation, and formation of immune complexes [183]. It can be concluded that exosomes make a connection between synoviocytes, immune cells, chondrocytes, and endothelial cells, so they affect different processes of RA. Taken together, these findings identify the role of exosomes in the pathogenesis of RA and may be utilized to develop new therapeutic solutions [181, 184].
Exosomes could change the joint structure by various functions including antigen presentation, angiogenesis, regulation of inflammation, alteration in cell-to-cell communication, and extracellular matrix degradation [185]. Exosomes derived from RA FLS may induce CD4+ T cells by interfering with activation-induced cell death, fortified IL-2 and IFNγ release from the mentioned cells, increasing the activity of Akt and NF-κB, and preventing caspase 8 and caspase 3 degradation [181, 186]. RA FLS secrets exosomes that destroy cartilage and bone by autocrine activation of matrix metalloproteinase 1 (MMP-1) or direct activity of metalloproteinase. On the other hand, TNF activation of RA FLS increases the production of exosomal miR-221-3p, which in turn inhibits bone formation [187, 188]. In addition to exosome secretion, FLS can target exosomes secreted by other immune cells like monocytes and activated T cells. Under this condition, FLS might increase the releasing of MMPs, also chemokines and cytokines, like monocyte chemotactic protein 1 (MCP-1), MCP-2, IL-8, and IL-6. Moreover, transcription of CXCL6, CXCL5, CXCL3, CXCL2, and CXCL1 chemokine genes may be increased [184]. Exosomes derived from synovial fluid might act as receptors for activators of NF-κB and receptor activator of nuclear factor kappa-Β ligand (RANKL), which can activate the functioning of bone osteoclasts and resorption [189]. Exosomes derived from the plasma of RA patients with severe disease activity enhanced proinflammatory cytokines such as TNF, IL-17, and IL-1 generated by autologous peripheral blood mononuclear [181]. Furthermore, the increased amounts of C1q suggested that circulatory exosomes in RA expand the inflammation by transporting complement components. In the connection between inhabitant synoviocytes like FLS and immune cells in a joint with inflammation, exosomes are secreted into the synovial tissue and fluid. The increased amount of released proinflammatory cytokines will activate proliferation, immune cell infiltration, and angiogenesis. Thus, exosomes provide positive feedback throughout the inflammatory stage. Joint inflammation may enhance the infiltration of neutrophil-derived exosomes, which may reduce the additional degradation of cartilage in RA [190].
It had been shown that both adaptive and innate immunological responses are regulated by exosomes generated by DCs. Genetic alteration and reaction modulated by cytokine/cytokines inhibitors might lead to creating immunosuppressive and tolerogenic immature DCs. Efficacy of exosomes derived from genetically engineered immature DCs that overexpress Th2 cytokine (such as IL-4) has been found to be effective for CIA therapy model illness [191, 192]. Humoral immunity responses could be decreased effectively by these exosomes and when activated by an antigen and immune cells in the spleen become activated and result in a Th-2 dominant response [191].
DCs which express FasL are efficient at preventing collagen reactive T cell activation and decreasing CIA progression in mice. In the murine delayed-type hypersensitivity (DTH) model, exosomes released by these DCs are found to have anti-inflammatory properties. This kind of DTH response suppression is specific to the antigen and depends on class II MHC. Moreover, the efficacy of DC/FasL exosomes in the treatment of CIA murine models has been shown by systemic injection. During animal DTH and CIA treatment, it has been demonstrated that exosomes originated from immunosuppressive DCs have an equivalent or stronger effect compared to exosomes of the primary DCs, so they could potentially be utilized for the treatment of RA. In addition to the effectiveness of DCs ex vivo, exosomes produced by DCs are more stable throughout the isolation procedures and seem to be safer for in vivo delivery than autologous cells. Exosomes have a longer lifetime and due to their unique biologic properties, they are more detectable after injection in comparison with other cell types [177, 191]. Exosomes generated by immature DCs were studied for their effectiveness as a cell-free treatment for CIA in mice. It was discovered that immature DCs treated by IL-10 produced exosomes that inhibited inflammatory and autoimmune reactions through suppressing the pro-inflammatory cytokines IL-1 and TNF-α and decreased the levels of Hsp70. It was reported that DTH responses in contralateral joints were reduced by these exosomes via modulation of T cell responses [176]. In addition, exosomes from DCs treated with IL-10 could prevent the incursion of murine CIA and also reduce the severity of existing arthritis. Other research showed that inflammation and autoimmunity were suppressed by exosomes produced by DCs. This suppression is done through the regulation of both endogenous T cells and APCs activity, MHC class II-dependent, and an antigen-specific pathway. Exosomes generated from DCs had a similar or even stronger immunosuppressive impact in comparison with their original secreting cells [176, 193]. It has been revealed that the indoleamine-pyrrole 2, 3-dioxygenase (IDO) enzyme which degrades tryptophan, has an immunosuppressive capability in a variety of conditions, such as RA. Although the main mechanism of this effect has not been completely discovered, it has been proposed to be via preventing the CD8+ effector T cell response and induction of Treg cells, by either depriving them of essential tryptophan. Importantly, immunosuppressive exosomes with higher levels of stability and proper bioactivity for delivery could be released by DCs which express IDO [194]. On the other hand, there are other findings that demonstrated that exosomes may have a pro-inflammatory ability in RA, unlike the anti-inflammatory exosomes mentioned above. For instance, in a study by Lim. M et al. it was indicated that Has-miR-1915-3p and has-miR-6511b-5p were significantly higher in the serum exosomes of RA disease so that the level of serum C-reactive protein (CRP) was negatively correlated with them [195].
Conclusion
The emergence of exosomes and their different activities has undoubtedly been one of the most important discoveries in the fields of medical and biology sciences in recent years. Given that exosomes have unique biological characteristics, they have been noticed in the treatment and diagnosis of various disorders and diseases, in particular B-cell disorders such as Leukemia, Multiple Sclerosis, and Arthritis Rheumatoid. Some characteristics of exosomes include: unique physicochemical properties and structure, low toxicity and immunogenicity, efficient cellular entry, inherent targeting, innate ability to cross biological barriers, and high stability in blood circulation. Exosomes play important roles in the maintaining of normal physiological conditions as well as disease status. Therefore, the type of exosomes released in health conditions are different from ones secreted in disease states; this feature can be utilized as an advanced strategy in precise and personalized diagnosis and treatment of varied disorders such as B-cell disorders. Exosomes, owing to their unique properties, can be used as vectors and carriers of biological and medicinal particles like drugs for delivering to the desired areas. Clinical research has shown that extracellular vesicles produced by immune cells (such as dendritic cells) can stimulate the immune system, so these exosomes can be used in antitumor vaccines. Exosomes are closely related to the survival, proliferation, metastasis, and recurrence of tumors, and they play an important role in the diagnosis and pathological identification of tumors and provide new avenues for immunotherapy. Despite the great potential of exosomes in the fields of diagnostic and treatment, further researches are in need for these purposes, so complementary cooperation between physicians and biologists can shed further light on the basic functions of extracellular vesicles and their different applications.
Acknowledgements
The authors acknowledge Tabriz University of Medical Sciences.
Abbreviations
- B-CLL
B-cell Chronic Lymphocytic Leukemia.
- TME
Tumor Microenvironment.
- EVs
Extracellular Vesicles.
- mtDNA
Mitochondrial DNA.
- gDNA
Genomic DNA.
- RA
Rheumatoid Arthritis.
- MS
Multiple Sclerosis.
- AML
Chronic Lymphocytic Leukemia.
- MVBs
Multi-vesicular Bodies.
- ILVs
Intra-luminal Vesicles.
- ESCRT
Endosomal Sorting Complex Required for the Transport.
- NSCLC
Non-small Cell Lung Cancer.
- cfDNA
Cell-free DNA.
- KRAS
Kirsten Rat Sarcoma Viral Oncogene Homologue.
- exoDNA
Exosomal DNA.
- PBS
Peripheral Blood Smear.
- SNPs
Single Nucleotide Polymorphisms.
- LEF1
Lymphoid Enhancer Binding Factor 1.
- BCL2
B-cell Lymphoma 2.
- PMAIP1
Phorbol-12-myristate-13-acetate-induced Protein 1.
- TCRA
T-cell Receptor-alpha.
- ZAP70
Zeta-chain-associated Protein Kinase 70.
- BTK
Bruton’s Tyrosine Kinase.
- miRNAs
microRNAs.
- tsRNAs
tRNA-derived Small RNAs.
- BCR
B-cell Receptor.
- CAFs
Cancer-associated Fibroblasts.
- IGHV
Immunoglobulin Heavy Variable.
- MBL
B-cell Lymphocytosis.
- MDSCs
Myeloid-derived Suppressing Cells.
- TCL1
T-Cell Leukemia/Lymphoma 1.
- MCL1
Myeloid Cell Leukemia 1.
- CLL
Chronic Lymphocytic Leukemia.
- EBV
Epstein-Barr Virus.
- CML
Chronic Myeloid Leukemia.
- VEGF
Vascular Endothelial Growth Factor.
- TGF-β1
Transforming Growth Factor Beta 1.
- ERKs
Extracellular Signal-regulated Kinases.
- PKB
Protein Kinase B.
- NF-κB
Nuclear Factor Kappa B.
- BM-MSCs
Bone Marrow Mesenchymal Stem Cells.
- TNF-α
Tumor Necrosis Factor Alpha.
- Wnt5a
Wnt Family Member 5 A.
- IL-6
Interleukin-6.
- CXCL12
C-X-C Motif Chemokine 12.
- DKK1
Dickkopf-related Protein1.
- NO
Nitric Oxide.
- hUCMSC
Human Umbilical Cord Mesenchymal Stem Cells.
- IM
Imatinib.
- Bax
Bcl-2 Associated X.
- AML
Acute Myeloid Leukemia.
- MEF2C
Myocyte Enhancer Factor 2 C.
- CEBP-α/-β
CCAAT/Enhancer-binding Protein Alpha and -Beta.
- E2F1
E2F Transcription Factor 1.
- ID1
Inhibitor of DNA Binding 1.
- SHIP1
SH2-domain-Containing Inositol 5′-phosphatase 1.
- FOXP3
Forkhead Box P3.
- GATA1
GATA-binding Factor 1.
- IGF-1R
Insulin-like Growth Factor Type 1 Receptor.
- MMP9
Matrix Metalloproteinase-9.
- CXCR4
C-X-C Chemokine Receptor Type 4.
- FLT3
Fms Related Receptor Tyrosine Kinase 3.
- NPM1
Nucleophosmin 1.
- SDF-1
Stromal Cell-derived Factor-1.
- PARP
Poly (ADP-ribose) Polymerase.
- WTAP
Wilms Tumor 1-associated Protein.
- SCF
Stem Cell Factor.
- HSPC
Hematopoietic Stromal and Progenitor Cell.
- HPC
Hematopoietic Progenitor Cell.
- LSCs
Leukemia Stem Cells.
- LRIG1
Leucine Rich Repeats and Immunoglobulin Like Domains 1.
- STAT3
Signal Transducer and Activator of Transcription 3.
- NK cells
Natural Killer Cells.
- Treg cells
Regulatory T Cells.
- PGE2
Prostaglandin E2.
- MS
Multiple Sclerosis.
- RRMS
Relapsing-remitting Multiple Sclerosis.
- NGS
Next Generation Sequencing.
- EAE
Experimental Autoimmune Encephalomyelitis.
- IFN-γ
Gamma Interferon.
- DCs
Dendritic Cells.
- IFNγ-DC-Exos
Exosomes Released by IFN-stimulated DCs.
- HSP
Heat Shock Protein.
- BBB
Blood Brain Barrier.
- CNS
Central Nervous System.
- MSCs
Mesenchymal Stem Cells.
- LPS
Lipopolysaccharide.
- RA
Rheumatoid Arthritis.
- ACPA
Anti-citrullinated Protein Antibodies.
- RF
Rheumatoid Factor.
- HLA
Human Leukocyte Antigen.
- GWAS
Genome Wide Association Studies.
- PADI4
Peptidyl Arginine Deiminase 4.
- FLS
Fibroblast Like Synoviocytes.
- IBD
Inflammatory Bowel Disease.
- MMP-1
Matrix Metalloproteinase 1.
- MCP-1
Monocyte Chemotactic Protein 1.
- RANKL
Receptor Activator of Nuclear Factor Kappa-Β Ligand.
- DTH
Delayed-type Hypersensitivity.
- IDO
Indoleamine-pyrrole 2, 3-Dioxygenase.
- CRP
C-reactive Protein.
Authors’ contributions
DSh, E, MKF and NJ conceived and designed research. NJ, MAO, AA, AK, MNA and HZ wrote and edited the manuscript. MNA, HZ, ZP revised the manuscript. ZP, HZ, and DSh supervised the study. All authors read and approved the manuscript.
Funding
This study was review article so no need to funding.
Data Availability
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Declarations
Ethics approval and consent to participate
There is no involvement of human or animal in this study.
Consent for publication
All other authors declare no conflict of interest.
Competing interests
All other authors declare no conflict of interest.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Mohsen Karami Fath, Email: mkf9702@gmail.com.
Jalil Azami, Email: jalil.azami@yahoo.com.
Niloofar Jaafari, Email: Niloojaafari1376@gmail.com.
Mahsa Akbari Oryani, Email: akbarimh@mums.ac.ir, Email: mahsa.akbari.oryani@gmail.com.
Nafiseh Jafari, Email: Nafisejafari77@gmail.com.
Ali Azargoonjahromi, Email: aazargoonj@gmail.com.
Mohsen Nabi-Afjadi, Email: mohsennabi66@gmail.com.
Zahra Payandeh, Email: Zpayandeh58@yahoo.com.
Hamidreza Zalpoor, Email: hamidreza.zlpr1998@gmail.com.
Dariush Shanehbandi, Email: dariush_shanehbandi@yahoo.com.
References
- 1.Mertens D, Stilgenbauer S. Prognostic and predictive factors in patients with chronic lymphocytic leukemia: relevant in the era of novel treatment approaches? J Clin oncology: official J Am Soc Clin Oncol. 2014;32(9):869–72. doi: 10.1200/JCO.2013.53.8421. [DOI] [PubMed] [Google Scholar]
- 2.Herishanu Y, Katz B-Z, Lipsky A, Wiestner A. Biology of chronic lymphocytic leukemia in different microenvironments: clinical and therapeutic implications. Hematology/Oncology Clin. 2013;27(2):173–206. doi: 10.1016/j.hoc.2013.01.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Burger JA, Gribben JG, editors. The microenvironment in chronic lymphocytic leukemia (CLL) and other B cell malignancies: insight into disease biology and new targeted therapies. Seminars in cancer biology. Elsevier; 2014. [DOI] [PubMed]
- 4.Hanahan D, Coussens LM. Accessories to the crime: functions of cells recruited to the tumor microenvironment. Cancer Cell. 2012;21(3):309–22. doi: 10.1016/j.ccr.2012.02.022. [DOI] [PubMed] [Google Scholar]
- 5.Swartz MA, Iida N, Roberts EW, Sangaletti S, Wong MH, Yull FE, et al. Tumor microenvironment complexity: emerging roles in cancer therapy. AACR; 2012. [DOI] [PMC free article] [PubMed]
- 6.Colombo M, Raposo G, Théry C. Biogenesis, secretion, and intercellular interactions of exosomes and other extracellular vesicles. Annu Rev Cell Dev Biol. 2014;30:255–89. doi: 10.1146/annurev-cellbio-101512-122326. [DOI] [PubMed] [Google Scholar]
- 7.Raposo G, Stoorvogel W. Extracellular vesicles: exosomes, microvesicles, and friends. J Cell Biol. 2013;200(4):373–83. doi: 10.1083/jcb.201211138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Meldolesi J. Exosomes and ectosomes in intercellular communication. Curr Biol. 2018;28(8):R435-R44. doi: 10.1016/j.cub.2018.01.059. [DOI] [PubMed] [Google Scholar]
- 9.Wortzel I, Dror S, Kenific CM, Lyden D. Exosome-mediated metastasis: communication from a distance. Dev Cell. 2019;49(3):347–60. doi: 10.1016/j.devcel.2019.04.011. [DOI] [PubMed] [Google Scholar]
- 10.Matsuno Y, Kanke T, Maruyama N, Fujii W, Naito K, Sugiura K. Characterization of mRNA profiles of the exosome-like vesicles in porcine follicular fluid. PLoS ONE. 2019;14(6):e0217760. doi: 10.1371/journal.pone.0217760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Yan W, Jiang S. Immune cell-derived exosomes in the cancer-immunity cycle. Trends in cancer. 2020;6(6):506–17. doi: 10.1016/j.trecan.2020.02.013. [DOI] [PubMed] [Google Scholar]
- 12.McLellan A. Exosome release by primary B cells. Critical Reviews™ in Immunology. 2009;29(3). [DOI] [PubMed]
- 13.Vigano S, Alatzoglou D, Irving M, Ménétrier-Caux C, Caux C, Romero P, et al. Targeting adenosine in cancer immunotherapy to enhance T-cell function. Front Immunol. 2019;10:925. doi: 10.3389/fimmu.2019.00925. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Laulagnier K, Motta C, Hamdi S, Roy S, Fauvelle F, Pageaux J-F, et al. Mast cell-and dendritic cell-derived exosomes display a specific lipid composition and an unusual membrane organization. Biochem J. 2004;380(1):161–71. doi: 10.1042/bj20031594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Vidal M, Exosomes Revisiting their role as “garbage bags”. Traffic. 2019;20(11):815–28. doi: 10.1111/tra.12687. [DOI] [PubMed] [Google Scholar]
- 16.Khatun Z, Bhat A, Sharma S, Sharma A. Elucidating diversity of exosomes: biophysical and molecular characterization methods. Nanomedicine. 2016;11(17):2359–77. doi: 10.2217/nnm-2016-0192. [DOI] [PubMed] [Google Scholar]
- 17.Das S, Abdel-Mageed AB, Adamidi C, Adelson PD, Akat KM, Alsop E, et al. The extracellular RNA communication consortium: establishing foundational knowledge and technologies for extracellular RNA research. Cell. 2019;177(2):231–42. doi: 10.1016/j.cell.2019.03.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Clayton A, Harris CL, Court J, Mason MD, Morgan BP. Antigen-presenting cell exosomes are protected from complement‐mediated lysis by expression of CD55 and CD59. Eur J Immunol. 2003;33(2):522–31. doi: 10.1002/immu.200310028. [DOI] [PubMed] [Google Scholar]
- 19.Rabesandratana H, Toutant J-P, Reggio H, Vidal M. Decay-accelerating factor (CD55) and membrane inhibitor of reactive lysis (CD59) are released within exosomes during In vitro maturation of reticulocytes. Blood The Journal of the American Society of Hematology. 1998;91(7):2573–80. [PubMed] [Google Scholar]
- 20.Mittelbrunn M, Gutiérrez-Vázquez C, Villarroya-Beltri C, González S, Sánchez-Cabo F, González M, et al. Unidirectional transfer of microRNA-loaded exosomes from T cells to antigen-presenting cells. Nat Commun. 2011;2(1):1–10. doi: 10.1038/ncomms1285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Yuyama K, Sun H, Mitsutake S, Igarashi Y. Sphingolipid-modulated exosome secretion promotes clearance of amyloid-β by microglia. J Biol Chem. 2012;287(14):10977–89. doi: 10.1074/jbc.M111.324616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Zhang Y, Liu Y, Liu H, Tang WH. Exosomes: biogenesis, biologic function and clinical potential. Cell & bioscience. 2019;9(1):1–18. doi: 10.1186/s13578-018-0263-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Rajagopal C, Harikumar K. The origin and functions of exosomes in cancer. Front Oncol. 2018;8:66. doi: 10.3389/fonc.2018.00066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Wang W, Zhu N, Yan T, Shi Y-N, Chen J, Zhang C-J, et al. The crosstalk: exosomes and lipid metabolism. Cell Communication and Signaling. 2020;18(1):1–12. doi: 10.1186/s12964-019-0473-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Gurung S, Perocheau D, Touramanidou L, Baruteau J. The exosome journey: from biogenesis to uptake and intracellular signalling. Cell Communication and Signaling. 2021;19(1):1–19. doi: 10.1186/s12964-021-00730-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Lakkaraju A, Rodriguez-Boulan E. Itinerant exosomes: emerging roles in cell and tissue polarity. Trends Cell Biol. 2008;18(5):199–209. doi: 10.1016/j.tcb.2008.03.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Blanc L, Vidal M. New insights into the function of Rab GTPases in the context of exosomal secretion. Small GTPases. 2018;9(1–2):95–106. doi: 10.1080/21541248.2016.1264352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Schmidt O, Teis D. The ESCRT machinery. Curr Biol. 2012;22(4):R116-R20. doi: 10.1016/j.cub.2012.01.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.McKelvey KJ, Powell KL, Ashton AW, Morris JM, McCracken SA. Exosomes: mechanisms of uptake. J circulating biomarkers. 2015;4:7. doi: 10.5772/61186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Yáñez-Mó M, Siljander PR-M, Andreu Z, Bedina Zavec A, Borràs FE, Buzas EI, et al. Biological properties of extracellular vesicles and their physiological functions. J Extracell vesicles. 2015;4(1):27066. doi: 10.3402/jev.v4.27066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Antimisiaris SG, Mourtas S, Marazioti A. Exosomes and exosome-inspired vesicles for targeted drug delivery. Pharmaceutics. 2018;10(4):218. doi: 10.3390/pharmaceutics10040218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Li Q, Wang H, Peng H, Huyan T, Cacalano NA. Exosomes: Versatile nano mediators of immune regulation. Cancers. 2019;11(10):1557. doi: 10.3390/cancers11101557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Ludwig JA, Weinstein JN. Biomarkers in cancer staging, prognosis and treatment selection. Nat Rev Cancer. 2005;5(11):845–56. doi: 10.1038/nrc1739. [DOI] [PubMed] [Google Scholar]
- 34.Hosseini K, Ranjbar M, Pirpour Tazehkand A, Asgharian P, Montazersaheb S, Tarhriz V, et al. Evaluation of exosomal non-coding RNAs in cancer using high-throughput sequencing. J translational Med. 2022;20(1):1–15. doi: 10.1186/s12967-022-03231-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Wu L, Qu X. Cancer biomarker detection: recent achievements and challenges. Chem Soc Rev. 2015;44(10):2963–97. doi: 10.1039/C4CS00370E. [DOI] [PubMed] [Google Scholar]
- 36.Hurwitz SN, Rider MA, Bundy JL, Liu X, Singh RK, Meckes DG., Jr Proteomic profiling of NCI-60 extracellular vesicles uncovers common protein cargo and cancer type-specific biomarkers. Oncotarget. 2016;7(52):86999. doi: 10.18632/oncotarget.13569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Zhou B, Xu K, Zheng X, Chen T, Wang J, Song Y, et al. Application of exosomes as liquid biopsy in clinical diagnosis. Signal Transduct Target therapy. 2020;5(1):1–14. doi: 10.1038/s41392-019-0089-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Gargiulo E, Morande PE, Largeot A, Moussay E, Paggetti J. Diagnostic and therapeutic potential of extracellular vesicles in b-cell malignancies. Frontiers in oncology. 2020;10. [DOI] [PMC free article] [PubMed]
- 39.Momen-Heravi F, Saha B, Kodys K, Catalano D, Satishchandran A, Szabo G. Increased number of circulating exosomes and their microRNA cargos are potential novel biomarkers in alcoholic hepatitis. J translational Med. 2015;13(1):1–13. doi: 10.1186/s12967-015-0623-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Thakur BK, Zhang H, Becker A, Matei I, Huang Y, Costa-Silva B, et al. Double-stranded DNA in exosomes: a novel biomarker in cancer detection. Cell Res. 2014;24(6):766–9. doi: 10.1038/cr.2014.44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Soofiyani SR, Hosseini K, Soleimanian A, Abkhooei L, Hoseini AM, Tarhriz V, et al. An Overview on the Role of miR-451 in Lung Cancer: Diagnosis, Therapy, and Prognosis. MicroRNA. 2021;10(3):181–90. doi: 10.2174/2211536610666210910130828. [DOI] [PubMed] [Google Scholar]
- 42.Allenson K, Castillo J, San Lucas F, Scelo G, Kim D, Bernard V, et al. High prevalence of mutantKRAS in circulating exosome-derived DNA from early-stage pancreatic cancer patients. Ann Oncol. 2017;28(4):741–7. doi: 10.1093/annonc/mdx004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Szabo G, Momen-Heravi F. Extracellular vesicles in liver disease and potential as biomarkers and therapeutic targets. Nat reviews Gastroenterol Hepatol. 2017;14(8):455. doi: 10.1038/nrgastro.2017.71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Whiteside TL. Tumor-derived exosomes and their role in cancer progression. Adv Clin Chem. 2016;74:103–41. doi: 10.1016/bs.acc.2015.12.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Melo SA, Luecke LB, Kahlert C, Fernandez AF, Gammon ST, Kaye J, et al. Glypican-1 identifies cancer exosomes and detects early pancreatic cancer. Nature. 2015;523(7559):177–82. doi: 10.1038/nature14581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Ma X, Chen Z, Hua D, He D, Wang L, Zhang P, et al. Essential role for TrpC5-containing extracellular vesicles in breast cancer with chemotherapeutic resistance. Proceedings of the National Academy of Sciences. 2014;111(17):6389-94. [DOI] [PMC free article] [PubMed]
- 47.Wei Y, Lai X, Yu S, Chen S, Ma Y, Zhang Y, et al. Exosomal miR-221/222 enhances tamoxifen resistance in recipient ER-positive breast cancer cells. Breast Cancer Res Treat. 2014;147(2):423–31. doi: 10.1007/s10549-014-3037-0. [DOI] [PubMed] [Google Scholar]
- 48.Hornick NI, Doron B, Abdelhamed S, Huan J, Harrington CA, Shen R, et al. AML suppresses hematopoiesis by releasing exosomes that contain microRNAs targeting c-MYB. Sci Signal. 2016;9(444):ra88-ra. doi: 10.1126/scisignal.aaf2797. [DOI] [PubMed] [Google Scholar]
- 49.Fu F, Jiang W, Zhou L, Chen Z. Circulating exosomal miR-17-5p and miR-92a-3p predict pathologic stage and grade of colorectal cancer. Translational Oncol. 2018;11(2):221–32. doi: 10.1016/j.tranon.2017.12.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Mathew M, Zade M, Mezghani N, Patel R, Wang Y, Momen-Heravi F. Extracellular Vesicles as Biomarkers in Cancer Immunotherapy. Cancers. 2020;12(10):2825. doi: 10.3390/cancers12102825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Zocco D, Bernardi S, Novelli M, Astrua C, Fava P, Zarovni N, et al. Isolation of extracellular vesicles improves the detection of mutant DNA from plasma of metastatic melanoma patients. Sci Rep. 2020;10(1):1–12. doi: 10.1038/s41598-020-72834-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Hood JL. editor Natural melanoma-derived extracellular vesicles. Seminars in cancer biology. Elsevier; 2019. [DOI] [PubMed]
- 53.Żmigrodzka M, Witkowska-Piłaszewicz O, Rzepecka A, Cywińska A, Jagielski D, Winnicka A. Extracellular Vesicles in the Blood of Dogs with Cancer—A Preliminary Study. Animals. 2019;9(8):575. doi: 10.3390/ani9080575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Redaelli A, Laskin B, Stephens J, Botteman M, Pashos C. The clinical and epidemiological burden of chronic lymphocytic leukaemia. Eur J Cancer Care. 2004;13(3):279–87. doi: 10.1111/j.1365-2354.2004.00489.x. [DOI] [PubMed] [Google Scholar]
- 55.Butler T, Gribben J. Biologic and clinical significance of molecular profiling in Chronic Lymphocytic Leukemia. Blood Rev. 2010;24(3):135–41. doi: 10.1016/j.blre.2010.03.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Metzeler KH, Heilmeier B, Edmaier KE, Rawat VP, Dufour A, Döhner K, et al. High expression of lymphoid enhancer-binding factor-1 (LEF1) is a novel favorable prognostic factor in cytogenetically normal acute myeloid leukemia. Blood The Journal of the American Society of Hematology. 2012;120(10):2118–26. doi: 10.1182/blood-2012-02-411827. [DOI] [PubMed] [Google Scholar]
- 57.Hardwick JM, Soane L. Multiple functions of BCL-2 family proteins. Cold Spring Harb Perspect Biol. 2013;5(2):a008722. doi: 10.1101/cshperspect.a008722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Hagenbuchner J, Ausserlechner MJ, Porto V, David R, Meister B, Bodner M, et al. The anti-apoptotic protein BCL2L1/Bcl-xL is neutralized by pro-apoptotic PMAIP1/Noxa in neuroblastoma, thereby determining bortezomib sensitivity independent of prosurvival MCL1 expression. J Biol Chem. 2010;285(10):6904–12. doi: 10.1074/jbc.M109.038331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Yeh C-H, Moles R, Nicot C. Clinical significance of microRNAs in chronic and acute human leukemia. Mol Cancer. 2016;15(1):1–16. doi: 10.1186/s12943-016-0518-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Klasen C, Ohl K, Sternkopf M, Shachar I, Schmitz C, Heussen N, et al. MIF promotes B cell chemotaxis through the receptors CXCR4 and CD74 and ZAP-70 signaling. J Immunol. 2014;192(11):5273–84. doi: 10.4049/jimmunol.1302209. [DOI] [PubMed] [Google Scholar]
- 61.Eichhorst B, Robak T, Montserrat E, Ghia P, Hillmen P, Hallek M, et al. Chronic lymphocytic leukaemia: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann Oncol. 2015;26:v78–84. doi: 10.1093/annonc/mdv303. [DOI] [PubMed] [Google Scholar]
- 62.Payandeh Z, Rajabibazl M, Mortazavi Y, Rahimpour A, Taromchi AH, Dastmalchi S. Affinity maturation and characterization of the ofatumumab monoclonal antibody. J Cell Biochem. 2019;120(1):940–50. doi: 10.1002/jcb.27457. [DOI] [PubMed] [Google Scholar]
- 63.Pepe F, Balatti V. Role of non-coding RNAs in the development of targeted therapy and immunotherapy approaches for chronic lymphocytic leukemia. J Clin Med. 2020;9(2):593. doi: 10.3390/jcm9020593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Caivano A, La Rocca F, Laurenzana I, Trino S, De Luca L, Lamorte D, et al. Extracellular vesicles in hematological malignancies: from biology to therapy. Int J Mol Sci. 2017;18(6):1183. doi: 10.3390/ijms18061183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Ghosh AK, Secreto CR, Knox TR, Ding W, Mukhopadhyay D, Kay NE. Circulating microvesicles in B-cell chronic lymphocytic leukemia can stimulate marrow stromal cells: implications for disease progression. Blood. 2010;115(9):1755–64. doi: 10.1182/blood-2009-09-242719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Belov L, Matic KJ, Hallal S, Best OG, Mulligan SP, Christopherson RI. Extensive surface protein profiles of extracellular vesicles from cancer cells may provide diagnostic signatures from blood samples. J Extracell vesicles. 2016;5(1):25355. doi: 10.3402/jev.v5.25355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.De Luca L, D’Arena G, Simeon V, Trino S, Laurenzana I, Caivano A, et al. Characterization and prognostic relevance of circulating microvesicles in chronic lymphocytic leukemia. Leuk Lymphoma. 2017;58(6):1424–32. doi: 10.1080/10428194.2016.1243790. [DOI] [PubMed] [Google Scholar]
- 68.Yeh Y-Y, Ozer HG, Lehman AM, Maddocks K, Yu L, Johnson AJ, et al. Characterization of CLL exosomes reveals a distinct microRNA signature and enhanced secretion by activation of BCR signaling. Blood The Journal of the American Society of Hematology. 2015;125(21):3297–305. doi: 10.1182/blood-2014-12-618470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Nisticò N, Maisano D, Iaccino E, Vecchio E, Fiume G, Rotundo S, et al. Role of Chronic Lymphocytic Leukemia (CLL)-Derived Exosomes in Tumor Progression and Survival. Pharmaceuticals. 2020;13(9):244. doi: 10.3390/ph13090244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.DeNardo DG, Ruffell B. Macrophages as regulators of tumour immunity and immunotherapy. Nat Rev Immunol. 2019;19(6):369–82. doi: 10.1038/s41577-019-0127-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Javandoost E, Firoozi-Majd E, Rostamian H, Khakpoor-Koosheh M, Mirzaei HR. Role of microRNAs in chronic lymphocytic leukemia pathogenesis. Curr Med Chem. 2020;27(2):282–97. doi: 10.2174/0929867326666190911114842. [DOI] [PubMed] [Google Scholar]
- 72.Tarhriz V, Eyvazi S, Musavi M, Abasi M, Sharifi K, Ghanbarian H, et al. Transient induction of Cdk9 in the early stage of differentiation is critical for myogenesis. J Cell Biochem. 2019;120(11):18854–61. doi: 10.1002/jcb.29204. [DOI] [PubMed] [Google Scholar]
- 73.Chang T-C, Yu D, Lee Y-S, Wentzel EA, Arking DE, West KM, et al. Widespread microRNA repression by Myc contributes to tumorigenesis. Nat Genet. 2008;40(1):43–50. doi: 10.1038/ng.2007.30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Du B, Lin C, Bian Z, Xu B. An insight into anti-inflammatory effects of fungal beta-glucans. Trends Food Sci Technol. 2015;41(1):49–59. doi: 10.1016/j.tifs.2014.09.002. [DOI] [Google Scholar]
- 75.Farzadfard E, Kalantari T, Tamaddon G. Serum Expression of Seven MicroRNAs in Chronic Lymphocytic Leukemia Patients. J blood Med. 2020;11:97. doi: 10.2147/JBM.S230842. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Kuo G, Wu C-Y, Yang H-Y. MiR-17-92 cluster and immunity. J Formos Med Assoc. 2019;118(1):2–6. doi: 10.1016/j.jfma.2018.04.013. [DOI] [PubMed] [Google Scholar]
- 77.Mardani R, Jafari Najaf Abadi MH, Motieian M, Taghizadeh-Boroujeni S, Bayat A, Farsinezhad A, et al. MicroRNA in leukemia: Tumor suppressors and oncogenes with prognostic potential. J Cell Physiol. 2019;234(6):8465–86. doi: 10.1002/jcp.27776. [DOI] [PubMed] [Google Scholar]
- 78.Favero A, Segatto I, Perin T, Belletti B. The many facets of miR-223 in cancer: Oncosuppressor, oncogenic driver, therapeutic target, and biomarker of response. Wiley Interdisciplinary Reviews: RNA. 2021:e1659. [DOI] [PMC free article] [PubMed]
- 79.Driedonks TA. Circulating Y-RNAs in extracellular vesicles and ribonucleoprotein complexes; implications for the immune system. Front Immunol. 2019;9:3164. doi: 10.3389/fimmu.2018.03164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Hegde GV, Peterson KJ, Emanuel K, Mittal AK, Joshi AD, Dickinson JD, et al. Hedgehog-induced survival of B-cell chronic lymphocytic leukemia cells in a stromal cell microenvironment: a potential new therapeutic target. Mol Cancer Res. 2008;6(12):1928–36. doi: 10.1158/1541-7786.MCR-08-0142. [DOI] [PubMed] [Google Scholar]
- 81.Farahani M, Rubbi C, Liu L, Slupsky JR, Kalakonda N. CLL exosomes modulate the transcriptome and behaviour of recipient stromal cells and are selectively enriched in miR-202-3p. PLoS ONE. 2015;10(10):e0141429. doi: 10.1371/journal.pone.0141429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Paggetti J, Haderk F, Seiffert M, Janji B, Distler U, Ammerlaan W, et al. Exosomes released by chronic lymphocytic leukemia cells induce the transition of stromal cells into cancer-associated fibroblasts. Blood. 2015;126(9):1106–17. doi: 10.1182/blood-2014-12-618025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.El-Daly SM, Bayraktar R, Anfossi S, Calin GA. The Interplay between MicroRNAs and the Components of the Tumor Microenvironment in B-Cell Malignancies. Int J Mol Sci. 2020;21(9):3387. doi: 10.3390/ijms21093387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.He Y, Jiang X, Chen J. The role of miR-150 in normal and malignant hematopoiesis. Oncogene. 2014;33(30):3887–93. doi: 10.1038/onc.2013.346. [DOI] [PubMed] [Google Scholar]
- 85.Mraz M, Chen L, Rassenti LZ, Ghia EM, Li H, Jepsen K, et al. miR-150 influences B-cell receptor signaling in chronic lymphocytic leukemia by regulating expression of GAB1 and FOXP1. Blood. 2014;124(1):84–95. doi: 10.1182/blood-2013-09-527234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Stamatopoulos B, Van Damme M, Crompot E, Dessars B, El Housni H, Mineur P, et al. Opposite prognostic significance of cellular and serum circulating microRNA-150 in patients with chronic lymphocytic leukemia. Mol Med. 2015;21(1):123–33. doi: 10.2119/molmed.2014.00214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Ferrajoli A, Shanafelt TD, Ivan C, Shimizu M, Rabe KG, Nouraee N, et al. Prognostic value of miR-155 in individuals with monoclonal B-cell lymphocytosis and patients with B chronic lymphocytic leukemia. Blood. J Am Soc Hematol. 2013;122(11):1891–9. doi: 10.1182/blood-2013-01-478222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Elton TS, Selemon H, Elton SM, Parinandi NL. Regulation of the MIR155 host gene in physiological and pathological processes. Gene. 2013;532(1):1–12. doi: 10.1016/j.gene.2012.12.009. [DOI] [PubMed] [Google Scholar]
- 89.Bruns H, Böttcher M, Qorraj M, Fabri M, Jitschin S, Dindorf J, et al. CLL-cell-mediated MDSC induction by exosomal miR-155 transfer is disrupted by vitamin D. Leukemia. 2017;31(4):985–8. doi: 10.1038/leu.2016.378. [DOI] [PubMed] [Google Scholar]
- 90.Lv M, Wang K, Huang X. -j. Myeloid-derived suppressor cells in hematological malignancies: friends or foes. J Hematol Oncol. 2019;12(1):1–12. doi: 10.1186/s13045-018-0686-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Jurj A, Pop L, Petrushev B, Pasca S, Dima D, Frinc I, et al. Exosome-carried microRNA-based signature as a cellular trigger for the evolution of chronic lymphocytic leukemia into Richter syndrome. Crit Rev Clin Lab Sci. 2018;55(7):501–15. doi: 10.1080/10408363.2018.1499707. [DOI] [PubMed] [Google Scholar]
- 92.Kollinerova S, Vassanelli S, Modriansky M. The role of miR-29 family members in malignant hematopoiesis. Biomedical Papers. 2014;158(4):489–501. doi: 10.5507/bp.2014.029. [DOI] [PubMed] [Google Scholar]
- 93.Stamatopoulos B, Meuleman N, Haibe-Kains B, Saussoy P, Van Den Neste E, Michaux L, et al. microRNA-29c and microRNA-223 down-regulation has in vivo significance in chronic lymphocytic leukemia and improves disease risk stratification. Blood The Journal of the American Society of Hematology. 2009;113(21):5237–45. doi: 10.1182/blood-2008-11-189407. [DOI] [PubMed] [Google Scholar]
- 94.Rasul E, Salamon D, Nagy N, Leveau B, Banati F, Szenthe K, et al. The MEC1 and MEC2 lines represent two CLL subclones in different stages of progression towards prolymphocytic leukemia. PLoS ONE. 2014;9(8):e106008. doi: 10.1371/journal.pone.0106008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Haderk F, Schulz R, Iskar M, Cid LL, Worst T, Willmund KV, et al. Tumor-derived exosomes modulate PD-L1 expression in monocytes. Science immunology. 2017;2(13). [DOI] [PubMed]
- 96.Jafarzadeh N, Gholampour MA, Alivand M-R, Kavousi S, Arzi L, Rad F, et al. CML derived exosomes promote tumor favorable functional performance in T cells. BMC Cancer. 2021;21(1):1–11. doi: 10.1186/s12885-021-08734-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Hamidi AA, Khalili-Tanha G, Nasrpour Navaei Z, Moghbeli M. Long non-coding RNAs as the critical regulators of epithelial mesenchymal transition in colorectal tumor cells: an overview. Cancer Cell Int. 2022;22(1):1–15. doi: 10.1186/s12935-022-02501-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Ohyashiki JH, Umezu T, Ohyashiki K. Exosomes promote bone marrow angiogenesis in hematologic neoplasia: the role of hypoxia. Curr Opin Hematol. 2016;23(3):268–73. doi: 10.1097/MOH.0000000000000235. [DOI] [PubMed] [Google Scholar]
- 99.Mineo M, Garfield SH, Taverna S, Flugy A, De Leo G, Alessandro R, et al. Exosomes released by K562 chronic myeloid leukemia cells promote angiogenesis in a Src-dependent fashion. Angiogenesis. 2012;15(1):33–45. doi: 10.1007/s10456-011-9241-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Umezu T, Ohyashiki K, Kuroda M, Ohyashiki JH. Leukemia cell to endothelial cell communication via exosomal miRNAs. Oncogene. 2013;32(22):2747–55. doi: 10.1038/onc.2012.295. [DOI] [PubMed] [Google Scholar]
- 101.Tadokoro H, Umezu T, Ohyashiki K, Hirano T, Ohyashiki JH. Exosomes derived from hypoxic leukemia cells enhance tube formation in endothelial cells. J Biol Chem. 2013;288(48):34343–51. doi: 10.1074/jbc.M113.480822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Raimondo S, Saieva L, Corrado C, Fontana S, Flugy A, Rizzo A, et al. Chronic myeloid leukemia-derived exosomes promote tumor growth through an autocrine mechanism. Cell Communication and Signaling. 2015;13(1):1–12. doi: 10.1186/s12964-015-0086-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Jafarzadeh N, Safari Z, Pornour M, Amirizadeh N, Forouzandeh Moghadam M, Sadeghizadeh M. Alteration of cellular and immune-related properties of bone marrow mesenchymal stem cells and macrophages by K562 chronic myeloid leukemia cell derived exosomes. J Cell Physiol. 2019;234(4):3697–710. doi: 10.1002/jcp.27142. [DOI] [PubMed] [Google Scholar]
- 104.Liu Y, Song B, Wei Y, Chen F, Chi Y, Fan H, et al. Exosomes from mesenchymal stromal cells enhance imatinib-induced apoptosis in human leukemia cells via activation of caspase signaling pathway. Cytotherapy. 2018;20(2):181–8. doi: 10.1016/j.jcyt.2017.11.006. [DOI] [PubMed] [Google Scholar]
- 105.Min Q-H, Wang X-Z, Zhang J, Chen Q-G, Li S-Q, Liu X-Q, et al. Exosomes derived from imatinib-resistant chronic myeloid leukemia cells mediate a horizontal transfer of drug-resistant trait by delivering miR-365. Exp Cell Res. 2018;362(2):386–93. doi: 10.1016/j.yexcr.2017.12.001. [DOI] [PubMed] [Google Scholar]
- 106.Kang K-W, Jung J-H, Hur W, Park J, Shin H, Choi B, et al. The potential of exosomes derived from chronic myelogenous leukaemia cells as a biomarker. Anticancer Res. 2018;38(7):3935–42. doi: 10.21873/anticanres.12679. [DOI] [PubMed] [Google Scholar]
- 107.Jiang L, Deng T, Wang D, Xiao Y. Elevated serum exosomal miR-125b level as a potential marker for poor prognosis in intermediate-risk acute myeloid leukemia. Acta Haematol. 2018;140(3):183–92. doi: 10.1159/000491584. [DOI] [PubMed] [Google Scholar]
- 108.Huan J, Hornick NI, Shurtleff MJ, Skinner AM, Goloviznina NA, Roberts CT, et al. RNA trafficking by acute myelogenous leukemia exosomes. Cancer Res. 2013;73(2):918–29. doi: 10.1158/0008-5472.CAN-12-2184. [DOI] [PubMed] [Google Scholar]
- 109.Hornick NI, Huan J, Doron B, Goloviznina NA, Lapidus J, Chang BH, et al. Serum exosome microRNA as a minimally-invasive early biomarker of AML. Sci Rep. 2015;5(1):1–12. doi: 10.1038/srep11295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Zhang L, Khadka B, Wu J, Feng Y, Long B, Xiao R, et al. Bone Marrow Mesenchymal Stem Cells-Derived Exosomal miR-425-5p Inhibits Acute Myeloid Leukemia Cell Proliferation, Apoptosis, Invasion and Migration by Targeting WTAP. OncoTargets and therapy. 2021;14:4901. doi: 10.2147/OTT.S286326. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 111.Huan J, Hornick N, Goloviznina N, Kamimae-Lanning A, David L, Wilmarth P, et al. Coordinate regulation of residual bone marrow function by paracrine trafficking of AML exosomes. Leukemia. 2015;29(12):2285–95. doi: 10.1038/leu.2015.163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Kumar B, Garcia M, Weng L, Jung X, Murakami J, Hu X, et al. Acute myeloid leukemia transforms the bone marrow niche into a leukemia-permissive microenvironment through exosome secretion. Leukemia. 2018;32(3):575–87. doi: 10.1038/leu.2017.259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Szymczyk A, Macheta A, Podhorecka M. Abnormal microRNA expression in the course of hematological malignancies. Cancer Manage Res. 2018;10:4267. doi: 10.2147/CMAR.S174476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Le MT, Hamar P, Guo C, Basar E, Perdigão-Henriques R, Balaj L, et al. miR-200–containing extracellular vesicles promote breast cancer cell metastasis. J Clin Investig. 2014;124(12):5109–28. doi: 10.1172/JCI75695. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Pan M, Reid MA, Lowman XH, Kulkarni RP, Tran TQ, Liu X, et al. Regional glutamine deficiency in tumours promotes dedifferentiation through inhibition of histone demethylation. Nat Cell Biol. 2016;18(10):1090–101. doi: 10.1038/ncb3410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Chen L, Guo Z, Zhou Y, Ni J, Zhu J, Fan X, et al. microRNA-1246-containing extracellular vesicles from acute myeloid leukemia cells promote the survival of leukemia stem cells via the LRIG1-meditated STAT3 pathway. Aging. 2021;13(10):13644. doi: 10.18632/aging.202893. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Szczepanski MJ, Szajnik M, Welsh A, Whiteside TL, Boyiadzis M. Blast-derived microvesicles in sera from patients with acute myeloid leukemia suppress natural killer cell function via membrane-associated transforming growth factor-β1. Haematologica. 2011;96(9):1302. doi: 10.3324/haematol.2010.039743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Mirmosayyeb O, Naderi M, Raeisi S, Ebrahimi N, Ghaffary EM, Afshari-Safavi A, et al. Hearing loss among patients with multiple sclerosis (PwMS): A systematic review and meta-analysis. Multiple Sclerosis and Related Disorders. 2022:103754. [DOI] [PubMed]
- 119.Zalpoor H, Akbari A, Samei A, Forghaniesfidvajani R, Kamali M, Afzalnia A, et al. The roles of Eph receptors, neuropilin-1, P2 × 7, and CD147 in COVID-19-associated neurodegenerative diseases: inflammasome and JaK inhibitors as potential promising therapies. Cell Mol Biol Lett. 2022;27(1):1–21. doi: 10.1186/s11658-021-00301-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Nicholas R, Rashid W. Multiple sclerosis. Am Fam Physician. 2013;87(10):712–4. [PubMed] [Google Scholar]
- 121.Pusic AD, Pusic KM, Kraig RP. What are exosomes and how can they be used in multiple sclerosis therapy? Expert Rev Neurother. 2014;14(4):353–5. doi: 10.1586/14737175.2014.890893. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Yang L, Boldin MP, Yu Y, Liu CS, Ea C-K, Ramakrishnan P, et al. miR-146a controls the resolution of T cell responses in mice. J Exp Med. 2012;209(9):1655–70. doi: 10.1084/jem.20112218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Zhou S, Dong X, Zhang C, Chen X, Zhu J, Li W, et al. MicroRNAs are implicated in the suppression of CD4 + CD25 – conventional T cell proliferation by CD4 + CD25 + regulatory T cells. Mol Immunol. 2015;63(2):464–72. doi: 10.1016/j.molimm.2014.10.001. [DOI] [PubMed] [Google Scholar]
- 124.Alvarez-Erviti L, Seow Y, Yin H, Betts C, Lakhal S, Wood MJ. Delivery of siRNA to the mouse brain by systemic injection of targeted exosomes. Nat Biotechnol. 2011;29(4):341–5. doi: 10.1038/nbt.1807. [DOI] [PubMed] [Google Scholar]
- 125.Pusic AD, Pusic KM, Kraig RP. What are exosomes and how can they be used in multiple sclerosis therapy? Expert Rev Neurother. 2014;14(4):353–5. doi: 10.1586/14737175.2014.890893. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Gallo A, Tandon M, Alevizos I, Illei GG. The majority of microRNAs detectable in serum and saliva is concentrated in exosomes. PLoS ONE. 2012;7(3):e30679. doi: 10.1371/journal.pone.0030679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Okoye IS, Coomes SM, Pelly VS, Czieso S, Papayannopoulos V, Tolmachova T, et al. MicroRNA-containing T-regulatory-cell-derived exosomes suppress pathogenic T helper 1 cells. Immunity. 2014;41(1):89–103. doi: 10.1016/j.immuni.2014.05.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Ge Q, Zhou Y, Lu J, Bai Y, Xie X, Lu Z. miRNA in plasma exosome is stable under different storage conditions. Molecules. 2014;19(2):1568–75. doi: 10.3390/molecules19021568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Ebrahimkhani S, Vafaee F, Young PE, Hur SS, Hawke S, Devenney E, et al. Exosomal microRNA signatures in multiple sclerosis reflect disease status. Sci Rep. 2017;7(1):1–10. doi: 10.1038/s41598-017-14301-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Du C, Liu C, Kang J, Zhao G, Ye Z, Huang S, et al. MicroRNA miR-326 regulates T H-17 differentiation and is associated with the pathogenesis of multiple sclerosis. Nat Immunol. 2009;10(12):1252. doi: 10.1038/ni.1798. [DOI] [PubMed] [Google Scholar]
- 131.Jeker LT, Bluestone JA. MicroRNA regulation of T-cell differentiation and function. Immunol Rev. 2013;253(1):65–81. doi: 10.1111/imr.12061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Cox MB, Cairns MJ, Gandhi KS, Carroll AP, Moscovis S, Stewart GJ, et al. MicroRNAs miR-17 and miR-20a inhibit T cell activation genes and are under-expressed in MS whole blood. PLoS ONE. 2010;5(8):e12132. doi: 10.1371/journal.pone.0012132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Junker A, Hohlfeld R, Meinl E. The emerging role of microRNAs in multiple sclerosis. Nat Reviews Neurol. 2011;7(1):56–9. doi: 10.1038/nrneurol.2010.179. [DOI] [PubMed] [Google Scholar]
- 134.Keller A, Leidinger P, Lange J, Borries A, Schroers H, Scheffler M, et al. Multiple sclerosis: microRNA expression profiles accurately differentiate patients with relapsing-remitting disease from healthy controls. PLoS ONE. 2009;4(10):e7440. doi: 10.1371/journal.pone.0007440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.De Santis G, Ferracin M, Biondani A, Caniatti L, Tola MR, Castellazzi M, et al. Altered miRNA expression in T regulatory cells in course of multiple sclerosis. J Neuroimmunol. 2010;226(1–2):165–71. doi: 10.1016/j.jneuroim.2010.06.009. [DOI] [PubMed] [Google Scholar]
- 136.Azimi M, Ghabaee M, Moghadasi AN, Izad M. Altered expression of miR-326 in T cell-derived exosomes of patients with relapsing-remitting multiple sclerosis. Iranian Journal of Allergy, Asthma and Immunology. 2019. [PubMed]
- 137.Hartman ZC, Wei J, Glass OK, Guo H, Lei G, Yang X-Y, et al. Increasing vaccine potency through exosome antigen targeting. Vaccine. 2011;29(50):9361–7. doi: 10.1016/j.vaccine.2011.09.133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Yin W, Ouyang S, Li Y, Xiao B, Yang H. Immature dendritic cell-derived exosomes: a promise subcellular vaccine for autoimmunity. Inflammation. 2013;36(1):232–40. doi: 10.1007/s10753-012-9539-1. [DOI] [PubMed] [Google Scholar]
- 139.Pusic A, Kraig R, editors. Exosome-mediated mitigation of oxidative stress and demyelination. Soc Neurosci; 2012.
- 140.Pusic AD, Pusic KM, Clayton BL, Kraig RP. IFNγ-stimulated dendritic cell exosomes as a potential therapeutic for remyelination. J Neuroimmunol. 2014;266(1–2):12–23. doi: 10.1016/j.jneuroim.2013.10.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Murugaiyan G, Beynon V, Mittal A, Joller N, Weiner HL. Silencing microRNA-155 ameliorates experimental autoimmune encephalomyelitis. J Immunol. 2011;187(5):2213–21. doi: 10.4049/jimmunol.1003952. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Mycko MP, Cichalewska M, Cwiklinska H, Selmaj KW. miR-155-3p drives the development of autoimmune demyelination by regulation of heat shock protein 40. J Neurosci. 2015;35(50):16504–15. doi: 10.1523/JNEUROSCI.2830-15.2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Mycko MP, Cichalewska M, Machlanska A, Cwiklinska H, Mariasiewicz M, Selmaj KW. MicroRNA-301a regulation of a T-helper 17 immune response controls autoimmune demyelination. Proceedings of the National Academy of Sciences. 2012;109(20):E1248-E57. [DOI] [PMC free article] [PubMed]
- 144.Lu L-F, Thai T-H, Calado DP, Chaudhry A, Kubo M, Tanaka K, et al. Foxp3-dependent microRNA155 confers competitive fitness to regulatory T cells by targeting SOCS1 protein. Immunity. 2009;30(1):80–91. doi: 10.1016/j.immuni.2008.11.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Lin S-T, Huang Y, Zhang L, Heng MY, Ptáček LJ, Fu Y-H. MicroRNA-23a promotes myelination in the central nervous system. Proceedings of the national academy of sciences. 2013;110(43):17468-73. [DOI] [PMC free article] [PubMed]
- 146.Tian J, Casella G, Zhang Y, Rostami A, Li X. Potential roles of extracellular vesicles in the pathophysiology, diagnosis, and treatment of autoimmune diseases. Int J Biol Sci. 2020;16(4):620. doi: 10.7150/ijbs.39629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Selmaj I, Mycko MP, Raine CS, Selmaj KW. The role of exosomes in CNS inflammation and their involvement in multiple sclerosis. J Neuroimmunol. 2017;306:1–10. doi: 10.1016/j.jneuroim.2017.02.002. [DOI] [PubMed] [Google Scholar]
- 148.Riazifar M, Mohammadi MR, Pone EJ, Yeri A, Lasser C, Segaliny AI, et al. Stem cell-derived exosomes as nanotherapeutics for autoimmune and neurodegenerative disorders. ACS Nano. 2019;13(6):6670–88. doi: 10.1021/acsnano.9b01004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Yu L, Yang F, Jiang L, Chen Y, Wang K, Xu F, et al. Exosomes with membrane-associated TGF‐β1 from gene‐modified dendritic cells inhibit murine EAE independently of MHC restriction. Eur J Immunol. 2013;43(9):2461–72. doi: 10.1002/eji.201243295. [DOI] [PubMed] [Google Scholar]
- 150.Casella G, Colombo F, Finardi A, Descamps H, Ill-Raga G, Spinelli A, et al. Extracellular vesicles containing IL-4 modulate neuroinflammation in a mouse model of multiple sclerosis. Mol Ther. 2018;26(9):2107–18. doi: 10.1016/j.ymthe.2018.06.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Zhuang X, Xiang X, Grizzle W, Sun D, Zhang S, Axtell RC, et al. Treatment of brain inflammatory diseases by delivering exosome encapsulated anti-inflammatory drugs from the nasal region to the brain. Mol Ther. 2011;19(10):1769–79. doi: 10.1038/mt.2011.164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Sun D, Zhuang X, Xiang X, Liu Y, Zhang S, Liu C, et al. A novel nanoparticle drug delivery system: the anti-inflammatory activity of curcumin is enhanced when encapsulated in exosomes. Mol Ther. 2010;18(9):1606–14. doi: 10.1038/mt.2010.105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Sáenz-Cuesta M, Irizar H, Castillo-Triviño T, Muñoz-Culla M, Osorio-Querejeta I, Prada A, et al. Circulating microparticles reflect treatment effects and clinical status in multiple sclerosis. Biomark Med. 2014;8(5):653–61. doi: 10.2217/bmm.14.9. [DOI] [PubMed] [Google Scholar]
- 154.Galazka G, Mycko MP, Selmaj I, Raine CS, Selmaj KW. Multiple sclerosis: Serum-derived exosomes express myelin proteins. Multiple Scler J. 2018;24(4):449–58. doi: 10.1177/1352458517696597. [DOI] [PubMed] [Google Scholar]
- 155.Ramirez SH, Andrews AM, Paul D, Pachter JS. Extracellular vesicles: mediators and biomarkers of pathology along CNS barriers. Fluids and Barriers of the CNS. 2018;15(1):1–21. doi: 10.1186/s12987-018-0104-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Tian J, Casella G, Zhang Y, Rostami A, Li X. Potential roles of extracellular vesicles in the pathophysiology, diagnosis, and treatment of autoimmune diseases. Int J Biol Sci. 2020;16(4):620–32. doi: 10.7150/ijbs.39629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Kimura K, Hohjoh H, Fukuoka M, Sato W, Oki S, Tomi C, et al. Circulating exosomes suppress the induction of regulatory T cells via let-7i in multiple sclerosis. Nat Commun. 2018;9(1):1–14. doi: 10.1038/s41467-017-02088-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.Ebrahimkhani S, Vafaee F, Young PE, Hur SSJ, Hawke S, Devenney E, et al. Exosomal microRNA signatures in multiple sclerosis reflect disease status. Sci Rep. 2017;7(1):14293. doi: 10.1038/s41598-017-14301-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.Selmaj I, Cichalewska M, Namiecinska M, Galazka G, Horzelski W, Selmaj KW, et al. Global exosome transcriptome profiling reveals biomarkers for multiple sclerosis. Ann Neurol. 2017;81(5):703–17. doi: 10.1002/ana.24931. [DOI] [PubMed] [Google Scholar]
- 160.Liu L, Zuo Y, Xu Y, Zhang Z, Li Y, Pang J. MiR-613 inhibits proliferation and invasion and induces apoptosis of rheumatoid arthritis synovial fibroblasts by direct down-regulation of DKK1. Cell Mol Biol Lett. 2019;24(1):1–14. doi: 10.1186/s11658-018-0127-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.de Brito Rocha S, Baldo DC, Andrade LEC. Clinical and pathophysiologic relevance of autoantibodies in rheumatoid arthritis. Adv Rheumatol. 2019;59(1):1–13. doi: 10.1186/s42358-018-0042-8. [DOI] [PubMed] [Google Scholar]
- 162.Farid SS, Azizi G, Mirshafiey A. Anti-citrullinated protein antibodies and their clinical utility in rheumatoid arthritis. Int J Rheum Dis. 2013;16(4):379–86. doi: 10.1111/1756-185X.12129. [DOI] [PubMed] [Google Scholar]
- 163.Moeez S, John P, Bhatti A. Anti-citrullinated protein antibodies: role in pathogenesis of RA and potential as a diagnostic tool. Rheumatol Int. 2013;33(7):1669–73. doi: 10.1007/s00296-012-2635-6. [DOI] [PubMed] [Google Scholar]
- 164.Szodoray P, Szabó Z, Kapitány A, Gyetvai Á, Lakos G, Szántó S, et al. Anti-citrullinated protein/peptide autoantibodies in association with genetic and environmental factors as indicators of disease outcome in rheumatoid arthritis. Autoimmun rev. 2010;9(3):140–3. doi: 10.1016/j.autrev.2009.04.006. [DOI] [PubMed] [Google Scholar]
- 165.Imboden JB. The immunopathogenesis of rheumatoid arthritis. Annu Rev Pathol. 2009;4:417–34. doi: 10.1146/annurev.pathol.4.110807.092254. [DOI] [PubMed] [Google Scholar]
- 166.Klareskog L, Malmström V, Lundberg K, Padyukov L, Alfredsson L, editors. Smoking, citrullination and genetic variability in the immunopathogenesis of rheumatoid arthritis. Seminars in immunology. Elsevier; 2011. [DOI] [PubMed]
- 167.Verheul M, Fearon U, Trouw L, Veale D. Biomarkers for rheumatoid and psoriatic arthritis. Clin Immunol. 2015;161(1):2–10. doi: 10.1016/j.clim.2015.04.005. [DOI] [PubMed] [Google Scholar]
- 168.Vang T, Congia M, Macis MD, Musumeci L, Orrú V, Zavattari P, et al. Autoimmune-associated lymphoid tyrosine phosphatase is a gain-of-function variant. Nat Genet. 2005;37(12):1317–9. doi: 10.1038/ng1673. [DOI] [PubMed] [Google Scholar]
- 169.Kochi Y, Suzuki A, Yamada R, Yamamoto K. Genetics of rheumatoid arthritis: underlying evidence of ethnic differences. J Autoimmun. 2009;32(3–4):158–62. doi: 10.1016/j.jaut.2009.02.020. [DOI] [PubMed] [Google Scholar]
- 170.Stahl EA, Raychaudhuri S, Remmers EF, Xie G, Eyre S, Thomson BP, et al. Genome-wide association study meta-analysis identifies seven new rheumatoid arthritis risk loci. Nat Genet. 2010;42(6):508. doi: 10.1038/ng.582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 171.McAllister K, Eyre S, Orozco G. Genetics of rheumatoid arthritis: GWAS and beyond. Open Access Rheumatology: Research and Reviews. 2011;3:31. doi: 10.2147/OARRR.S14725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 172.Cloutier N, Paré A, Farndale RW, Schumacher HR, Nigrovic PA, Lacroix S, et al. Platelets can enhance vascular permeability. Blood The Journal of the American Society of Hematology. 2012;120(6):1334–43. doi: 10.1182/blood-2012-02-413047. [DOI] [PubMed] [Google Scholar]
- 173.Sun D, Zhuang X, Xiang X, Liu Y, Zhang S, Liu C, et al. A novel nanoparticle drug delivery system: the anti-inflammatory activity of curcumin is enhanced when encapsulated in exosomes. Mol Ther. 2010;18(9):1606–14. doi: 10.1038/mt.2010.105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 174.Tavasolian F, Hosseini AZ, Soudi S, Naderi M. miRNA-146a improves immunomodulatory effects of MSC-derived exosomes in rheumatoid arthritis. Curr Gene Ther. 2020;20(4):297–312. doi: 10.2174/1566523220666200916120708. [DOI] [PubMed] [Google Scholar]
- 175.Chen Z, Wang H, Xia Y, Yan F, Lu Y. Therapeutic potential of mesenchymal cell–derived miRNA-150-5p–expressing exosomes in rheumatoid arthritis mediated by the modulation of MMP14 and VEGF. J Immunol. 2018;201(8):2472–82. doi: 10.4049/jimmunol.1800304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 176.Kim S-H, Lechman ER, Bianco N, Menon R, Keravala A, Nash J, et al. Exosomes derived from IL-10-treated dendritic cells can suppress inflammation and collagen-induced arthritis. J Immunol. 2005;174(10):6440–8. doi: 10.4049/jimmunol.174.10.6440. [DOI] [PubMed] [Google Scholar]
- 177.Cai Z, Zhang W, Yang F, Yu L, Yu Z, Pan J, et al. Immunosuppressive exosomes from TGF-β1 gene-modified dendritic cells attenuate Th17-mediated inflammatory autoimmune disease by inducing regulatory T cells. Cell Res. 2012;22(3):607–10. doi: 10.1038/cr.2011.196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 178.Chen X-M, Zhao Y, Wu X-D, Wang M-J, Yu H, Lu J-J, et al. Novel findings from determination of common expressed plasma exosomal microRNAs in patients with psoriatic arthritis, psoriasis vulgaris, rheumatoid arthritis, and gouty arthritis. Discov Med. 2019;28(151):47–68. [PubMed] [Google Scholar]
- 179.Schioppo T, Ubiali T, Ingegnoli F, Bollati V, Caporali R. The role of extracellular vesicles in rheumatoid arthritis: a systematic review. Clinical Rheumatology. 2021:1–17. [DOI] [PMC free article] [PubMed]
- 180.Wu L-F, Zhang Q, Mo X-B, Lin J, Wu Y-L, Lu X, et al. Identification of novel rheumatoid arthritis-associated MiRNA-204-5p from plasma exosomes. Experimental & Molecular Medicine. 2022:1–12. [DOI] [PMC free article] [PubMed]
- 181.Withrow J, Murphy C, Liu Y, Hunter M, Fulzele S, Hamrick MW. Extracellular vesicles in the pathogenesis of rheumatoid arthritis and osteoarthritis. Arthritis Res therapy. 2016;18(1):1–12. doi: 10.1186/s13075-016-1178-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 182.Zhang H-G, Liu C, Su K, Yu S, Zhang L, Zhang S, et al. A membrane form of TNF-α presented by exosomes delays T cell activation-induced cell death. J Immunol. 2006;176(12):7385–93. doi: 10.4049/jimmunol.176.12.7385. [DOI] [PubMed] [Google Scholar]
- 183.Malda J, Boere J, Van De Lest CH, Van Weeren PR, Wauben MH. Extracellular vesicles—new tool for joint repair and regeneration. Nat Rev Rheumatol. 2016;12(4):243. doi: 10.1038/nrrheum.2015.170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 184.Fu H, Hu D, Zhang L, Tang P. Role of extracellular vesicles in rheumatoid arthritis. Mol Immunol. 2018;93:125–32. doi: 10.1016/j.molimm.2017.11.016. [DOI] [PubMed] [Google Scholar]
- 185.Buzas EI, György B, Nagy G, Falus A, Gay S. Emerging role of extracellular vesicles in inflammatory diseases. Nat Rev Rheumatol. 2014;10(6):356–64. doi: 10.1038/nrrheum.2014.19. [DOI] [PubMed] [Google Scholar]
- 186.Stanczyk J, Ospelt C, Karouzakis E, Filer A, Raza K, Kolling C, et al. Altered expression of microRNA-203 in rheumatoid arthritis synovial fibroblasts and its role in fibroblast activation. Arthr Rhuem. 2011;63(2):373–81. doi: 10.1002/art.30115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 187.Miller MC, Manning HB, Jain A, Troeberg L, Dudhia J, Essex D, et al. Membrane type 1 matrix metalloproteinase is a crucial promoter of synovial invasion in human rheumatoid arthritis. Arthritis & Rheumatism: Official Journal of the American College of Rheumatology. 2009;60(3):686–97. doi: 10.1002/art.24331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 188.Maeda Y, Farina NH, Matzelle MM, Fanning PJ, Lian JB, Gravallese EM. Synovium-derived microRNAs regulate bone pathways in rheumatoid arthritis. J Bone Miner Res. 2017;32(3):461–72. doi: 10.1002/jbmr.3005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 189.Xing L, Schwarz EM, Boyce BF. Osteoclast precursors, RANKL/RANK, and immunology. Immunol Rev. 2005;208(1):19–29. doi: 10.1111/j.0105-2896.2005.00336.x. [DOI] [PubMed] [Google Scholar]
- 190.Tran T-H, Mattheolabakis G, Aldawsari H, Amiji M. Exosomes as nanocarriers for immunotherapy of cancer and inflammatory diseases. Clin Immunol. 2015;160(1):46–58. doi: 10.1016/j.clim.2015.03.021. [DOI] [PubMed] [Google Scholar]
- 191.Kim SH, Bianco NR, Shufesky WJ, Morelli AE, Robbins PD. Effective treatment of inflammatory disease models with exosomes derived from dendritic cells genetically modified to express IL-4. J Immunol. 2007;179(4):2242–9. doi: 10.4049/jimmunol.179.4.2242. [DOI] [PubMed] [Google Scholar]
- 192.Yang C, Robbins PD. Immunosuppressive exosomes: a new approach for treating arthritis. International journal of rheumatology. 2012;2012. [DOI] [PMC free article] [PubMed]
- 193.Payandeh Z, Pirpour Tazehkand A, Azargoonjahromi A, Almasi F, Alagheband Bahrami A. The Role of Cell Organelles in Rheumatoid Arthritis with Focus on Exosomes. Biol Procedures Online. 2021;23(1):20. doi: 10.1186/s12575-021-00158-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 194.Bianco NR, Kim SH, Ruffner MA, Robbins PD. Therapeutic effect of exosomes from indoleamine 2, 3-dioxygenase–positive dendritic cells in collagen‐induced arthritis and delayed‐type hypersensitivity disease models. Arthritis & Rheumatism: Official Journal of the American College of Rheumatology. 2009;60(2):380–9. doi: 10.1002/art.24229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 195.Lim M-K, Yoo J, Sheen D-H, Ihm C, Lee SK, Kim SA. Serum exosomal miRNA-1915-3p is correlated with disease activity of Korean rheumatoid arthritis. in vivo. 2020;34(5):2941–5. doi: 10.21873/invivo.12124. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.