To the Editor:
Prone positioning (PP) is strongly recommended for the treatment of moderate-to-severe acute respiratory distress syndrome (ARDS) (1). However, before the coronavirus disease (COVID-19) pandemic, PP had been poorly adopted; a 2019 survey of Massachusetts hospitals found that fewer than half could routinely perform PP for patients who were intubated (2). Because the COVID-19 pandemic resulted in the rapid expansion of critical care delivery and adoption of novel practices (3), we resurveyed Massachusetts hospitals in 2021 to assess for changes in institutional PP availability for patients who were intubated as well as the adoption of PP in patients who were not intubated.
Methods
We emailed surveys to intensive care unit (ICU) nurse and physician leadership of all Massachusetts acute-care hospitals with ICUs between June and October 2021. If surveys remained incomplete after four follow-ups, we completed the survey by phone; one survey was completed per hospital. We administered the same multiple-choice questions as in our 2019 survey (hyperlinked), which asked, “Does your ICU have the ability to prone intubated patients?” (“Yes, routinely,” “Case-by-case,” or “No”) and inquired about institutional PP protocols/guidelines, presence of nurses trained in PP, and recent (6-month) use of PP in patients who were intubated. In addition, the survey asked five new questions regarding the role of the COVID-19 pandemic in motivating protocols or nurse training for intubated PP and institutional availability of nonintubated PP. Hospitals could submit comments as free text at the conclusion of the survey. We collected hospital data (hospital/ICU size (4), nonprofit status (5), teaching status (5), case-mix index (5), and Centers for Medicare and Medicaid Services star rating (6). Pairwise comparisons of 2019 and 2021 responses were tested for significance using McNemar’s (binary response) or Bowker’s tests (categorical response); significant associations between proning-related practices and hospital characteristics were assessed with chi-square tests. Statistical testing was two-tailed, with α = 0.05, using SAS 9.4 (SAS Institute). The Boston University Medical Campus institutional review board deemed this study not human subjects research.
Results
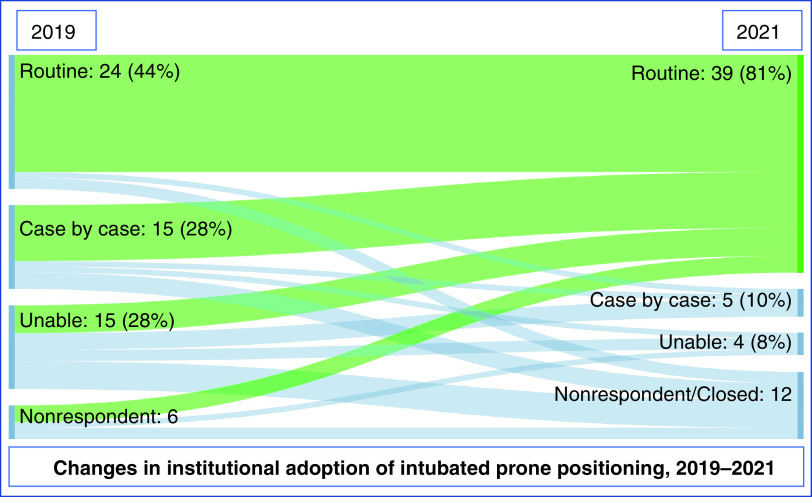
Of 57 acute care hospitals in Massachusetts with ICUs, 48 responded to the survey (84.2% response rate; 3 out of the 60 hospitals surveyed in 2019 had closed ICUs by 2021); 44 (77.2%) hospitals responded in both 2019 and 2021. By 2021, the number of hospitals able to routinely perform PP in patients who were intubated increased from 24 (44.4%) to 39 (81.3%) (P < 0.001); 18 hospitals increased PP ability, 2 hospitals decreased PP ability; and 24 hospitals did not change (Figure 1). Hospitals able to routinely perform PP accounted for 867 out of a total of 941 ICU beds in the state (92.1%), whereas hospitals unable to provide PP accounted for less than 1% of ICU beds (Table 1). The proportion of hospitals with a protocol/guideline for intubated PP and nurses trained in intubated PP also increased (P < 0.001 for both), whereas the number of hospitals reporting they had not recently proned any patients who were intubated decreased (P = 0.001). Among hospitals that reported new prone positioning practices, most reported that the COVID-19 pandemic motivated this change; 15/17 (88.2%) hospitals reporting new protocols and 11/12 (91.7%) hospitals reporting an increase in nurse staffing (i.e., no nurses trained in 2019 and some or all nurses trained in 2021) cited the pandemic. Respondents were given the opportunity to provide additional comments at the conclusion of the survey; four representative comments are shown in Table 1. Unlike in 2019, there was no association between the ability to perform PP and hospital size (P = 0.3) or teaching status (P = 0.1) (Table 2).
Figure 1.
Changes in institutional adoption of intubated prone positioning in Massachusetts intensive care units between 2019 and 2021. The number of hospitals (percentage of respondents), by category of ability to offer prone positioning to patients who were intubated, is shown. The width of the alluvial bands reflects the proportion of institutions that changed or maintained practices between 2019 and 2021.
Table 1.
Changes in institutional adoption of intubated prone positioning in Massachusetts intensive care units between 2019 and 2021
| 2019 | 2021 | P Value | |
|---|---|---|---|
| Hospitals, n (%) | n = 54 | n = 48 | |
| Institutional protocol/policy for intubated PP | 27 (50) | 43 (90) | <0.001 |
| Nurses trained in intubated PP (all or some) | 34 (63) | 45 (94) | <0.001 |
| Intubated PP not performed in the last 6 mo | 23 (43) | 6 (13) | 0.001 |
| ICU beds represented | n = 600 | n = 941 | |
| Ability to provide intubated PP, n (%) | — | — | <0.001 |
| Routine | 358 (59.7) | 867 (92.1) | — |
| Case-by-case | 121 (20.2) | 26 (2.7) | — |
| Unable | 74 (12.3) | 8 (0.9) | — |
| Nonrespondent/closed | 48 | 39 | — |
| Select quotes from free-text comments (2021) | |||
| • We had [a] protocol for PP before the pandemic but was rarely used, but COVID-19 really made it become implemented • We had a protocol for proning but with the Rotoprone bed. That was our ICU standard, but manual pronation was needed and a new protocol that was developed for the volume of proning with COVID-related ARDs. The staffing also was a challenge, but it did not hinder proning a patient. All staff were trained to assist. The organization also developed prone teams from other departments that we trained early in the pandemic. I feel this pushed us to a manual protocol and forced us to adapt. • Nurses were trained to prone by the OR staff proning teams, proning team would come and help ICU staff • The hospital is an orthopedic specialty hospital, so a lot of the "no" answers are because [we] do not typically have the patient population that requires these types of treatments/equipment. If [we] did have a patient that was very ill, they would be transferred to another facility for provision of care | |||
Definition of abbreviations: ARDS = acute respiratory distress syndrome; COVID-19 = coronavirus disease; ICU = intensive care unit; OR = operating room; PP = prone positioning.
The number (and proportion of respondents) of hospitals with various proning practices are shown, with McNemar’s test P values for statistically significant change between 2019 and 2021. Respondents were given the option to enter any additional comments at the end of the survey in free text; select representative comments from 2021 are shown. The number of ICU beds staffed within each hospital is derived from hospital staffing reports on Patient CareLink.
Table 2.
Characteristics associated with institutional ability to provide intubated prone positioning
| Hospital Characteristics | Prone-ready (n = 39) | PP Available on Case-by-Case Basis (n = 5) | PP Unavailable (n = 4) | Nonrespondent (n = 9) | P Value |
|---|---|---|---|---|---|
| Teaching hospital, n (%) | 13 (33.3) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0.1 |
| Total ICU beds, mean (SD) | 22.8 (25.9) | 6.6 (2.6) | 2.1 (1.0) | 4.8 (3.7) | 0.1 |
| Bed number, n (%) | — | — | — | — | 0.3 |
| Small (<250) | 22 (56.4) | 4 (80.0) | 4 (100.0) | 8 (88.9) | — |
| Medium (250–424) | 11 (28.2) | 1 (20.0) | 0 (0.0) | 1 (11.1) | — |
| Large (⩾425) | 6 (15.4) | 0 (0.0) | 0 (0.0) | 0 (0.0) | — |
| Nonprofit status, n (%) | 31 (79.5) | 4 (80.0) | 4 (100.0) | 8 (88.9) | 0.7 |
| High public payer hospital, n (%) | 15 (38.5) | 4 (80.0) | 3 (75.0) | 7 (77.8) | 0.1 |
| Case mix index,* mean (SD) | 1.1 (0.3) | 0.9 (0.1) | 1.0 (0.3) | 0.9 (0.1) | 0.1 |
| Centers for Medicare and Medicaid Services star rating, mean, (SD) | 3.5 (1.1) | 3.4 (1.3) | 4.3 (1.0) | 3.4 (0.9) | 0.6 |
Definition of abbreviations: ICU = intensive care unit; PP = prone positioning; SD = standard deviation.
In contrast to 2019, there was no association between hospital characteristics and the ability to provide prone positioning.
3M All Patient Refined grouper, version 30, reported through the Massachusetts Center for Health Information and Analysis.
In 2021, 43 (89.6%) respondents reported proning patients who were not intubated, 21 (48.8%) of whom had a protocol/guideline; 40 (93.0%) performed nonintubated PP in either ICU or floor, 1 (2.3%) in only the ICU, and 2 (4.7%) only on the floor. Nineteen (44.2%) of the hospitals that adopted nonintubated PP could not routinely provide intubated PP in 2019, and 6 (14.0%) could still not routinely provide intubated PP in 2021.
Discussion
Between 2019 and 2021, there was a substantial increase in the proportion of ICUs in Massachusetts that were able to routinely offer PP for patients who were intubated. Almost all hospitals with new protocols or nurse training attributed these changes to the COVID-19 pandemic. We also found high rates of adoption of nonintubated PP among Massachusetts acute-care hospitals.
Several factors may explain the rapid change in institutional adoption of intubated and nonintubated PP between 2019 and 2021. First, most of our survey respondents (either through multiple-choice responses or free-text comments) indicated that COVID-19 provided strong motivation for change, despite staffing challenges. While two hospitals did decrease their ability to provide intubated PP, far more hospitals increased or maintained their proning ability; we suspect that the anticipation of high rates of severe ARDS and limited ability to rely on transferring patients to higher-acuity institutions encouraged institutions to adopt new practices. In free text, hospitals indicated strategies used to overcome barriers, such as training by operating room proning teams. Second, in comparing our 2019 (2) and 2021 results, we observed the largest gains in PP ability in small, nonacademic hospitals, which are known to have unique challenges in incorporating evidence-based ICU practices (7). During COVID-19, multiple crossinstitutional (8) and international (9, 10) evidence reviews and guidelines for the care of patients with COVID-19, which clearly delineated intubated PP eligibility criteria and benefits, were disseminated early and broadly. This high amount of dissemination (even reaching lay news media (11) may have been more likely to reach smaller, nonacademic hospitals. Third, although randomized clinical trials examining the impact of nonintubated PP on intubation rates and mortality were not published until late 2021 and 2022 (12, 13), multiple early reports of nonintubated PP demonstrated improvements in hypoxemia (14–16) without major adverse effects. We suspect that, despite many uncertainties (e.g., the optimal duration of nonintubated PP [17] and risks of delaying intubation [18]), the perception of an overall favorable risk trade-off (“low-risk” intervention in a disease with high mortality) (19) helped drive the adoption of nonintubated PP.
Limitations
Our study has limitations. First, we surveyed only hospitals in Massachusetts, a state notable for having numerous academic hospitals in close proximity to one another, making generalizability to other states unclear. Second, with increased public awareness of PP during the COVID-19 pandemic (11), it is possible that our 2021 survey results have been affected by social desirability bias and may overestimate the increase in hospitals able to provide PP. Third, while many individuals responding on behalf of their hospital in 2021 were the same individuals that responded in 2019, many others were not, potentially leading to inconsistent answers. Fourth, prevalence estimates of nonintubated PP may be underestimated when ICU leadership alone is surveyed; further studies may wish to survey leadership from general hospital wards as well. Fifth, although we were able to provide rough estimates of the number of ICU beds in the state affected by the ability of each hospital to provide prone positioning, the actual number of eligible patients that a hospital can prone at a given time remains unknown; future studies are needed to understand the total number of ICU beds capable of intubated prone positioning at a given time. Sixth, given limits to the number of survey questions that could be feasibly completed by ICU leaders during a pandemic, further studies (e.g., qualitative interviews) may be useful to further understand the reasons why hospitals changed practices.
Conclusions
In conclusion, we found that hospitals in Massachusetts, most of which were unprepared to routinely provide PP for patients who were intubated at the start of the COVID-19 pandemic, rapidly developed the infrastructure (protocols and nurse training) to provide both intubated and nonintubated PP during the pandemic. Several factors unique to the pandemic, such as the broad dissemination of information and protocols, may have contributed to rapid institutional change.
Footnotes
Supported by the National Heart, Lung, and Blood Institute (NHLBI) of the National Institutes of Health (NIH) (T35HL139444 [X.A.]; 5F32GM133061 [N.A.B.]; 5R01HL151607, 5R01HL139751, and 5R01HL136660 [A.J.W.]; and K23HL153482 [A.C.L.]), Boston University School of Medicine Department of Medicine Career Investment Award (A.C.L.), and Doris Duke Charitable Foundation Fund to Retain Clinician Scientists (A.C.L.). The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH.
Author disclosures are available with the text of this letter at www.atsjournals.org.
References
- 1. Fan E, Del Sorbo L, Goligher EC, Hodgson CL, Munshi L, Walkey AJ, et al. American Thoracic Society, European Society of Intensive Care Medicine, and Society of Critical Care Medicine An official American Thoracic Society/European Society of Intensive Care Medicine/Society of Critical Care Medicine clinical practice guideline: mechanical ventilation in adult patients with acute respiratory distress syndrome. Am J Respir Crit Care Med . 2017;195:1253–1263. doi: 10.1164/rccm.201703-0548ST. [DOI] [PubMed] [Google Scholar]
- 2. Law AC, Forbath N, O’Donoghue S, Stevens JP, Walkey AJ. Hospital-level availability of prone positioning in Massachusetts ICUs. Am J Respir Crit Care Med . 2020;201:1006–1008. doi: 10.1164/rccm.201910-2097LE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Levin JM, Davis BS, Bukowski LA, Kahn JM. Willingness to treat with therapies of unknown effectiveness in severe COVID-19: a survey of intensivist physicians. Ann Am Thorac Soc . 2022;19:633–639. doi: 10.1513/AnnalsATS.202105-594OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Massachusetts Health and Hospital Association, Inc. PatientCareLink, 2022 plans. [accessed 2019 Aug 12]. Available from: http://patientcarelink.org/2022-plans/
- 5.Center for Health Information and Analysis, Commonwealth of Massachusetts. Massachusetts hospitals: hospital profiles; 2022. [accessed 2022 Mar 12]. Available from: http://www.chiamass.gov/massachusetts-hospitals/
- 6.Centers for Medicare & Medicaid Services. Hospital compare: a quality tool for adults, including people with medicare; 2022. [accessed 2022 Mar 15]. Available from: https://www.medicare.gov/care-compare/results?searchType=Hospital&page=5&state=MA&sort=alpha
- 7. Johnson EE, Sterba KR, Goodwin AJ, Warr EH, Beeks R, Zapka JM, et al. Implementation of an academic-to-community hospital intensive care unit quality improvement program. Qualitative analysis of multilevel facilitators and barriers. Ann Am Thorac Soc . 2019;16:877–885. doi: 10.1513/AnnalsATS.201810-735OC. [DOI] [PubMed] [Google Scholar]
- 8. Klaiman T, Silvestri JA, Srinivasan T, Szymanski S, Tran T, Oredeko F, et al. Improving prone positioning for severe acute respiratory distress syndrome during the COVID-19 pandemic. An implementation-mapping approach. Ann Am Thorac Soc . 2021;18:300–307. doi: 10.1513/AnnalsATS.202005-571OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Aziz S, Arabi YM, Alhazzani W, Evans L, Citerio G, Fischkoff K, et al. Managing ICU surge during the COVID-19 crisis: rapid guidelines. Intensive Care Med . 2020;46:1303–1325. doi: 10.1007/s00134-020-06092-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Coronavirus disease (COVID-19) technical guidance: patient management. World Health Organization; 2020. [accessed 2022 Jan 25]. Available from: https://www.who.int/emergencies/diseases/novel-coronavirus-2019/technical-guidance/patient-management [Google Scholar]
- 11.Belluck P. Low-tech way to help some covid patients: flip them over. The New York Times; 2020. [accessed 2022 Jan 21]. Available from: https://www.nytimes.com/2020/05/13/health/coronavirus-proning-lungs.html
- 12. Ibarra-Estrada M, Li J, Pavlov I, Perez Y, Roca O, Tavernier E, et al. Factors for success of awake prone positioning in patients with COVID-19-induced acute hypoxemic respiratory failure: analysis of a randomized controlled trial. Crit Care . 2022;26:84. doi: 10.1186/s13054-022-03950-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Ehrmann S, Li J, Ibarra-Estrada M, Perez Y, Pavlov I, McNicholas B, et al. Awake Prone Positioning Meta-Trial Group Awake prone positioning for COVID-19 acute hypoxaemic respiratory failure: a randomised, controlled, multinational, open-label meta-trial. Lancet Respir Med . 2021;9:1387–1395. doi: 10.1016/S2213-2600(21)00356-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Elharrar X, Trigui Y, Dols A-M, Touchon F, Martinez S, Prud’homme E, et al. Use of prone positioning in nonintubated patients with COVID-19 and hypoxemic acute respiratory failure. JAMA . 2020;323:2336–2338. doi: 10.1001/jama.2020.8255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Thompson AE, Ranard BL, Wei Y, Jelic S. Prone positioning in awake, nonintubated patients with COVID-19 hypoxemic respiratory failure. JAMA Intern Med . 2020;180:1537–1539. doi: 10.1001/jamainternmed.2020.3030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Damarla M, Zaeh S, Niedermeyer S, Merck S, Niranjan-Azadi A, Broderick B, et al. Prone positioning of nonintubated patients with COVID-19. Am J Respir Crit Care Med . 2020;202:604–606. doi: 10.1164/rccm.202004-1331LE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Koeckerling D, Barker J, Mudalige NL, Oyefeso O, Pan D, Pareek M, et al. Awake prone positioning in COVID-19. Thorax . 2020;75:833–834. doi: 10.1136/thoraxjnl-2020-215133. [DOI] [PubMed] [Google Scholar]
- 18. Gattinoni L, Chiumello D, Caironi P, Busana M, Romitti F, Brazzi L, et al. COVID-19 pneumonia: different respiratory treatments for different phenotypes? Intensive Care Med . 2020;46:1099–1102. doi: 10.1007/s00134-020-06033-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Maley JH, Law AC, Stevens JP. Evidence and our daily risk trade-offs in the care of critically ill patients. Am J Respir Crit Care Med . 2020;202:1493–1494. doi: 10.1164/rccm.202007-2898ED. [DOI] [PMC free article] [PubMed] [Google Scholar]