Goal:
The objective of this study was to evaluate the prevalence of burnout and professional fulfillment among healthcare administrative leaders and examine the association between burnout and professional fulfillment and personal and professional characteristics.
Methods:
Between June 7 and June 30, 2021, we performed a national survey of CEOs and other senior operational leaders to evaluate their personal work experience. Burnout and professional fulfillment—as well as a sleep-related impairment and self-valuation—were assessed using standardized instruments.
Principle Findings:
Of the 5,994 members of the American College of Healthcare Executives who were sent an invitation to participate, 1,269 (21.2%), including 279 CEOs, submitted usable responses. The mean overall burnout score was 2.71 (range: 0–10), and 33% of participants had burnout scores that fell in the high range (unfavorable). Mean professional fulfillment score was 7.29 (range: 0–10), with 56.6% scoring in the high range (favorable). Burnout and professional fulfillment scores varied by role. On multivariable analysis, sleep-related impairment (OR for each 1-point increase = 1.29, 95% CI [1.19–1.41]; p < .001) and self-valuation (OR for each 1-point increase = 0.63, 95% CI [0.57–0.68]; p < .001) were independently associated with burnout after adjusting for all other variables.
Applications to Practice:
Results of this study suggest that healthcare leaders had lower burnout and professional fulfillment scores than clinicians. Nonetheless, one third of healthcare leaders had burnout scores that fell in the high range. At the individual level, improved sleep health and self-valuation appear to reduce risk of burnout and promote professional fulfillment.
INTRODUCTION
The impact of clinician well-being and occupational distress on the U.S. healthcare delivery system has been rigorously studied over the past two decades. The high prevalence of occupational burnout among physicians (Shanafelt et al., 2012; Shanafelt, West, et al., 2019), nurses (Dyrbye, West, Johnson, et al., 2019; McHugh et al., 2011; Shah et al., 2021), and other healthcare professionals (Dyrbye, West, Halasy, et al., 2020; Dyrbye, West, Kelsey, et al., 2020; Skrupky et al., 2003), and its links to quality of care (Cimiotti et al., 2012; Shanafelt et al., 2010; Tawfik et al., 2019), staffing (Dyrbye, Major-Elechi, Thapa, et al., 2021; Shanafelt et al., 2016), turnover (Hamidi et al., 2018), cost of care (Dyrbye, West, Hunderfund, et al., 2020), and the economic viability of healthcare organizations (Han et al., 2019; Shanafelt, Goh, & Sinsky, 2017) are now well documented.
The COVID-19 pandemic has created new sources of distress for clinicians, forced rapid innovation and changes at work (Farrugia & Plutowski, 2020; Mann et al., 2020), and exacerbated previous challenges. In response to the impact of clinician distress on the U.S. healthcare delivery system, the triple aim for healthcare (improving population health, reducing the cost of care, and improving patient experience) was expanded to a quadruple aim that also incorporates clinician well-being (Bodenheimer & Sinsky, 2014). In parallel, a number of national organizations including the American Hospital Association, National Academy of Medicine, Association of American Medical Colleges, and The Joint Commission have turned their attention to this threat to the healthcare system (National Academies of Sciences, Engineering, and Medicine; National Academy of Medicine; & Committee on Systems Approaches to Improve Patient Care by Supporting Clinician Well-Being, 2019; Shanafelt, Stolz, et al., 2020; Shanafelt, Trockel, et al., 2019).
Although national efforts are important, interventions by care delivery systems and their operational leaders (both executives and managers) to improve the day-to-day environment in which clinicians practice are believed to be critical to address this issue (Shanafelt & Noseworthy, 2017). Evidence suggests that problems with organizational culture (Linzer et al., 2019; Shanafelt, Schein, et al., 2019), leadership behavior (Dyrbye, Major-Elechi, et al., 2020; Shanafelt et al., 2015; Shanafelt et al., 2021), suboptimal teamwork (Welp et al., 2016), inefficient workflows, staffing issues (Aiken et al., 2002) and a lack of support at the organization and work-unit level (Afonso et al., 2021; Aiken et al., 2002; McHugh et al., 2011; Shanafelt & Noseworthy, 2017; Swensen et al., 2016) are among the largest drivers of clinician distress. Evidence also suggests that organizational interventions to address these issues can effectively reduce clinician distress (DeChant et al., 2019; Melnyk et al., 2020; Panagioti et al., 2017; West et al., 2016).
Healthcare leaders have been asked to spearhead efforts to mitigate clinician distress, yet little is known about their own distress and work experience. Besides ensuring a sufficient, engaged, and adequately supported workforce, these operational leaders (both executives and managers) are tasked with extensive additional responsibilities. Specifically, they must set the strategy for their organization, safeguard the quality and safety of patient care, meet expectations of patients and their families, provide a safe and equitable workplace, respond to regulatory changes, work with payers so that patients have access to the healthcare system, manage the impact of reduced reimbursement for clinical care, position the organization in a competitive marketplace, and ensure the financial viability of the organization. In each of these dimensions, dynamic threats have arisen during the past 2 years to affect organizations in unique ways.
The COVID-19 pandemic has left a seismic impact on hospitals, requiring leaders to respond with unprecedented scale and speed—often with incomplete or conflicting information. Leaders have also faced difficult ethical decisions to protect the safety and well-being of their staff, patients, and communities in the face of severe resource shortages, especially in the early days of the pandemic. As of this writing, COVID-19 continues to present existential operational, financial, and staffing challenges.
Here, we report the results of a national survey of CEOs, other C-suite leaders (COOs, CFOs, CNOs, CMOs, CMIOs, CQOs, CHROs, CSOs), and other leaders. The survey was designed to evaluate burnout and professional fulfillment and examine any associations with personal and professional characteristics.
METHODS
Participants
From June 7 to 30, 2021, we surveyed members of the American College of Healthcare Executives (ACHE) to assess their work experience. Members who worked in healthcare provider organizations and were listed in the ACHE database as managers or above were included in the sample. Invitations to participate in the survey were sent via e-mail on June 7, with two reminder requests over the ensuing 2 weeks. Participation was voluntary; all responses were confidential. Retrospective analysis of an anonymous data set derived from this administratively collective data for research purposes was reviewed by the Stanford University institutional review board and deemed exempt.
Study Measures
Participants provided basic demographic information (e.g., age, gender, relationship status, whether they had children), as well as information on professional characteristics (e.g., position, type of organization they worked for, average weekly work hours). Burnout and professional fulfillment were assessed using the nonclinical versions of the Stanford Professional Fulfillment Index (Trockel et al., 2017). This scale measures both the interpersonal disengagement (six items) and the work exhaustion (four items) domains of burnout; scores on these two subscales are combined to derive an overall burnout score. The index also separately measures professional fulfillment (six items). Details on the index are available in prior publications (Brady et al., 2021; Trockel et al., 2017). Two additional items in this survey asked respondents to indicate whether they “liked their job” and whether they would “recommend a career in healthcare leadership as a field for young people” (response options for both items: strongly agree, agree, neither agree nor disagree, disagree, strongly disagree).
Based on evidence that sleep-related impairment contributes to the risk of burnout (Trockel et al., 2020), we also assessed sleep health using the four-item version of the National Institutes of Health PROMIS (Patient-Reported Outcomes Measurement Information System) Sleep-Related Impairment Scale. This instrument assesses alertness, sleepiness, and functional deficits related to inadequate sleep. National benchmarks are available for both general and clinical populations, with individuals scoring >9 on 4–20 scale considered to have sleep-related impairment (HealthMeasures, 2022).
Given the relationship between self-compassion and risk of burnout in healthcare clinicians (Trockel et al., 2019; Trockel et al., 2021), we assessed this domain in participating healthcare administrators using the Stanford Self-Valuation Scale. This instrument evaluates the combination of growth mindset (responding to personal imperfections with the desire to learn and improve rather than shame) and prioritization of self-care and personal well-being. As previously reported (Trockel et al., 2019; Trockel et al., 2021), the scale comprises four items in which respondents indicate their experience with indicators of low self-valuation over the preceding 2 weeks on a 5-point Likert Scale.
Once designed, the survey was pilot-tested on 69 healthcare administrators to obtain feedback and determine how long the survey took to be completed. This feedback prompted minor changes to the sequence of questions.
Statistical Analysis
Standard descriptive summary statistics were used to characterize the survey respondents. Scores from all scales were normalized to a 0–10 scale to facilitate ease of comparison, in keeping with work described in prior publications (Shanafelt, Makowski, et al., 2020; Shanafelt et al., 2021; Trockel et al., 2021). Associations between variables were evaluated using the χ2 test (categorical variables) or the Kruskal–Wallis test (continuous variables), as appropriate. All tests were two-sided with type 1 error rates of 0.05. Multivariable logistic regression was used to identify factors independently associated with burnout and professional fulfillment. All analyses were completed using R (Version 3.6.0).
RESULTS
A total of 5,994 members of ACHE were sent an invitation to participate; 1,301 responses were received (overall response rate = 21.7%). We excluded individuals who indicated that they were not currently employed (n = 1), were no longer in healthcare (n = 1), held staff or consultant roles (n = 16), or were not working for a healthcare delivery system, which left 1,269 individuals to be included in the analysis. To evaluate whether participants were representative of the overall sample, we compared the demographic, position, and work characteristics of all eligible individuals in the ACHE membership file with that of respondents (i.e., compared participants with the sampling frame; Johnson & Wislar, 2012). No significant differences were found between respondents and all eligible individuals in the ACHE membership file for position and work settings (χ2(3, N = 7,295) = 0.58, p = .90 and χ2(2, N = 7,295) = 2.80, p = .25, respectively). Respondents had a higher proportion in the 50–59 years age group and lower proportion aged <40 years than eligible individuals in the ACHE membership file (χ2(3, N = 7,295) = 10.03, p = .02). Next, we compared early respondents (responded in the first week of the survey window) with late respondents (responded in the survey's final 9 days), an established proxy for nonrespondents (Johnson & Wislar, 2012). No statistically significant difference was found in personal (age, gender, relationship status, children, age of children) or professional characteristics (position, hours worked per week, degree, work setting) between early respondents and late respondents. Collectively, these results suggest that participants were representative of all eligible ACHE members with the exception that they might be slightly older than eligible members overall.
The demographic characteristics of respondents are shown in Table 1. Roughly half were aged 50 years or older (473 [37.3%] 50–59; 137 [10.8%] ≥60) with a slight male predominance (47.1% female; 52.8% male). With respect to position, 279 (22.0%) respondents identified themselves as CEOs, 224 (17.7%) as other C-suite members (COO, CFO, CMO, CMIO, CQO, CNO, CHRO, CSO, and others), 222 (17.5%) as vice presidents, and 367 (28.9%) as department heads. With respect to education, a majority of the respondents had master's degrees in business administration (39.1%) or healthcare administration (44.6%). In all, 94.7% of those responding reported having master's, PhD, or clinical degrees.
TABLE 1. Personal and Professional Characteristics of Participants (N = 1,299).
| All Participants, N (%) N = 1,269 |
CEOs, N (%) N = 279 |
|
|---|---|---|
| Gender | ||
| Female | 595 (47.1) | 82 (29.5) |
| Male | 666 (52.8) | 196 (70.5) |
| Other | 1 (0.1) | 0 (0.0) |
| Missing | 7 | 1 |
| Age in years | ||
| <30 | 15 (1.2) | 0 (0.0) |
| 30–39 | 237 (18.7) | 27 (9.7) |
| 40–49 | 407 (32.1) | 69 (24.7) |
| 50–59 | 473 (37.3) | 132 (47.3) |
| ≥60 | 137 (10.8) | 51 (18.3) |
| Missing | 0 | 0 |
| Relationship status | ||
| Single | 142 (12.1) | 15 (5.7) |
| Married | 959 (82.0) | 236 (89.7) |
| Partnered | 59 (5.0) | 10 (3.8) |
| Widow, widower | 9 (0.8) | 2 (0.8) |
| Missing | 100 | 16 |
| Children | ||
| Yes | 937 (80.2) | 241 (91.6) |
| No | 231 (19.8) | 22 (8.4) |
| Missing | 101 | 16 |
| Age of youngest child (of those with children) in years | ||
| <5 | 135 (14.4) | 26 (10.8) |
| 5–12 | 217 (23.2) | 42 (17.4) |
| 13–18 | 221 (23.6) | 59 (24.5) |
| 19–22 | 126 (13.5) | 43 (17.8) |
| ≥23 | 236 (25.2) | 71 (29.5) |
| Missing | 334 | 38 |
| Position | ||
| CEO | 279 (22.0) | 279 (100) |
| COO | 108 (8.5) | – |
| CFO | 18 (1.4) | – |
| CIO | 10 (0.8) | – |
| CMO | 25 (2.0) | – |
| CNO | 41 (3.2) | – |
| CQO | 1 (0.1) | – |
| CHRO | 3 (0.2) | – |
| CSO | 4 (0.3) | – |
| Other C-suite role | 14 (1.1) | |
| Senior vice president | 47 (3.7) | – |
| Vice president | 222 (17.5) | – |
| Department head, director | 367 (28.9) | – |
| Manager | 126 (9.9) | – |
| Other | 4 (0.3) | – |
| Hours worked per week | ||
| Median (IQR) | 55 (50, 60) | 55 (50, 60) |
| <40 | 12 (1.2) | 3 (1.4) |
| 40–49.9 | 180 (18.1) | 20 (9.5) |
| 50–59.9 | 454 (45.8) | 95 (45.2) |
| 60–69.9 | 281 (28.3) | 75 (35.7) |
| 70–79.9 | 43 (4.3) | 14 (6.7) |
| ≥80 | 22 (2.2) | 3 (1.4) |
| Missing | 277 | 69 |
| Degreesa | ||
| Master of business administration | 461 (39.1) | 107 (40.5) |
| Master of health administration | 525 (44.6) | 148 (56.1) |
| Doctor of medicine or osteopathy | 77 (6.5) | 10 (3.8) |
| Nursing degree (baccalaureate or higher) | 191 (16.2) | 23 (8.7) |
| PhD or equivalent | 85 (7.2) | 18 (6.8) |
| Other clinical degree (e.g., pharmacy, radiology) | 153 (13.0) | 26 (9.8) |
| None of the above | 60 (5.1) | 12 (4.5) |
| Work setting | ||
| Academic medical center | 184 (14.6) | 9 (3.2) |
| Independent hospital, medical center | 232 (18.4) | 78 (28.1) |
| Member hospital of a nonfederal hospital system | 388 (30.7) | 96 (34.5) |
| Member hospital of a federal hospital system—military, VA, IHS | 91 (7.2) | 13 (4.7) |
| Corporate or regional headquarters of a healthcare system | 172 (13.6) | 20 (7.2) |
| Ambulatory care facility, group practice | 95 (7.5) | 30 (10.8) |
| Managed care, HMO, PPO | 8 (0.6) | 0 (0.0) |
| Postacute, chronic care | 36 (2.8) | 19 (6.8) |
| Public health, community health, mental health agency | 35 (2.8) | 10 (3.6) |
| Military—nonhospital, clinic setting | 15 (1.2) | 10 (3.6) |
| Hospital—unspecified | 5 (0.4) | 19 (6.8) |
| Other | 3 (0.2) | 0 (0.0) |
| Missing | 5 | 1 |
Note. HMO = health maintenance organization; IHS = Indian Health Service; IQR = interquartile range; PPO = preferred provider organization; VA = Veterans Administration.
aParticipants indicated degrees in multiple categories, so total adds to >100%.
Mean work exhaustion and interpersonal disengagement on the 0–10 scale (range 0–10, higher scores less favorable) were 3.30 and 2.32, respectively. Mean overall burnout score was 2.71 (higher scores less favorable), and 33% of participants had burnout scores that fell in the high range (unfavorable). Mean score for professional fulfillment (higher scores favorable) on the 0–10 scale was 7.29, with 56.6% scoring in the high range (favorable). Overall, 88.1% of participants agreed (39.6%) or strongly agreed (48.5%) with the statement “I like my job.” Similarly, 86.8% indicated that they agreed (42.8%) or strongly agreed (44.0%) that they would “recommend a career in healthcare leadership as a good field for young people” (Table 2).
TABLE 2. Measures of Personal and Professional Well-Being (N = 1,269).
| All Participants, N (%) N = 1,269 |
CEOs, N (%) N = 279 |
|
|---|---|---|
| Burnouta | ||
| Emotional exhaustion | ||
| Mean (SD)b | 3.30 (2.18) | 3.02 (2.08) |
| % high score | 540 (43.6%) | 107 (39.1%) |
| Missing | 30 | 5 |
| Interpersonal disengagement | ||
| Mean (SD)b | 2.32 (2.04) | 2.16 (1.95) |
| % high score | 380 (30.7%) | 80 (29.2%) |
| Missing | 30 | 5 |
| Burned out | ||
| Mean (SD)b | 2.71 (1.94) | 2.50 (1.86) |
| % high score | 409 (33.0%) | 79 (28.8%) |
| Missing | 30 | 5 |
| Professional fulfillment | ||
| Mean (SD)c | 7.29 (2.11) | 7.93 (1.88) |
| % high score | 717 (56.6%) | 197 (70.6%) |
| Missing | 2 | 0 |
| Sleep impairment scored | ||
| Mean (SD)b | 7.62 (3.49) | 7.49 (3.11) |
| % with sleep-related impairment | 288 (24.0%) | 65 (24.2%) |
| Missing | 67 | 10 |
| Self-valuation score | ||
| Mean (SD)c | 5.35 (2.31) | 5.45 (2.25) |
| Missing | 56 | 9 |
| Career satisfaction | ||
| “I like my job” | ||
| Strongly agree | 577 (48.5%) | 171 (64.0%) |
| Agree | 471 (39.6%) | 73 (27.3%) |
| Neutral | 78 (6.6%) | 11 (4.1%) |
| Disagree | 37 (3.1%) | 2 (0.7%) |
| Strongly disagree | 27 (2.3%) | 10 (3.7%) |
| Missing | 79 | 12 |
| “I would recommend healthcare leadership as a good field for young people” | ||
| Strongly agree | 550 (44.0%) | 140 (51.3%) |
| Agree | 535 (42.8%) | 93 (34.1%) |
| Neutral | 99 (7.9%) | 22 (8.1%) |
| Disagree | 38 (3.0%) | 9 (3.3%) |
| Strongly disagree | 28 (2.2%) | 9 (3.3%) |
| Missing | 19 | 6 |
aAssessed using the Stanford Professional Fulfillment Index.
bScores 0–10, higher score unfavorable.
cScores 0–10, higher score favorable.
dScores 4–20, higher score unfavorable.
The distribution of raw scores on the Sleep-Related Impairment and Self-Valuation scales is provided in the Appendix (see Supplemental Digital Content Figures 1 and 2, available at http://links.lww.com/JHM/A82). The mean score for sleep-related impairment on the 4–20 scale (higher scores less favorable) was 7.62, with 24.0% of participating administrative leaders scoring above the threshold for sleep-related impairment. Mean score for self-valuation on the 0–10 scale was 5.35 (higher scores favorable). Variation in sleep and self-valuation scores by age, gender, relationship status, and professional characteristics is shown in Table 3. Sleep-related impairment scores improved with age and were lowest among those working 40–49 hr per week. Self-valuation scores were more favorable for men relative to women and decreased incrementally as work hours increased.
TABLE 3. Personal/Professional Characteristics and Sleep/Self-Valuation Scores.
| Sleep Scorea | Self-Valuationb | |||
|---|---|---|---|---|
| M (SD) | p | M (SD) | p | |
| Gender | ||||
| Female | 7.58 (3.52) | .882 | 5.10 (2.33) | <.001 |
| Male | 7.61 (3.41) | 5.58 (2.26) | ||
| Age (years) | ||||
| <30 | 9.86 (3.80) | <.001 | 4.78 (3.15) | .063 |
| 30–39 | 8.33 (3.82) | 5.31 (2.25) | ||
| 40–49 | 7.84 (3.59) | 5.11 (2.41) | ||
| 50–59 | 7.33 (3.32) | 5.50 (2.23) | ||
| ≥60 | 6.60 (2.75) | 5.62 (2.25) | ||
| Relationship status | ||||
| Single | 7.87 (3.80) | .668 | 5.27 (2.52) | .551 |
| Married | 7.57 (3.37) | 5.37 (2.27) | ||
| Partnered | 7.81 (3.96) | 4.94 (2.62) | ||
| Widow, widower | 6.89 (3.41) | 5.56 (2.11) | ||
| Children | ||||
| No children | 7.85 (3.70) | .213 | 5.20 (2.49) | .317 |
| Aged <5 years | 7.68 (3.40) | 5.62 (2.20) | ||
| Aged 5–12 years | 7.47 (3.15) | 5.21 (2.37) | ||
| Aged 13–18 years | 7.75 (3.63) | 5.33 (2.19) | ||
| Aged 9–22 years | 8.00 (3.70) | 5.14 (2.28) | ||
| Aged ≥23 years | 7.18 (3.26) | 5.52 (2.29) | ||
| Position | ||||
| CEO | 7.49 (3.11) | .229 | 5.45 (2.25) | .088 |
| COO | 7.34 (3.39) | 5.58 (2.36) | ||
| CFO | 6.50 (3.08) | 5.74 (2.13) | ||
| CIO | 8.30 (3.68) | 4.00 (2.09) | ||
| CMO | 8.28 (4.25) | 4.80 (2.16) | ||
| CNO | 7.00 (3.08) | 4.84 (1.94) | ||
| Other C-suite role | 8.25 (4.24) | 4.69 (2.54) | ||
| Senior vice president | 7.29 (3.24) | 5.44 (2.31) | ||
| Vice president | 7.23 (3.29) | 5.13 (2.15) | ||
| Department head, director | 7.93 (3.80) | 5.31 (2.33) | ||
| Manager | 8.12 (3.67) | 5.76 (2.63) | ||
| Other | 8.25 (4.92) | 6.72 (3.36) | ||
| Position | ||||
| CEO | 7.49 (3.11) | .168 | 5.45 (2.25) | .197 |
| Member of C-suite (other than CEO) | 7.46 (3.53) | 5.21 (2.28) | ||
| Senior vice president | 7.29 (3.24) | 5.44 (2.31) | ||
| Vice president | 7.23 (3.29) | 5.13 (2.15) | ||
| Department head, director | 7.93 (3.80) | 5.31 (2.33) | ||
| Manager | 8.12 (3.67) | 5.76 (2.63) | ||
| Other | 8.25 (4.92) | 6.72 (3.36) | ||
| Hours worked per week | ||||
| <40 | 7.83 (2.82) | <.001 | 6.41 (2.34) | <.001 |
| 40–49.9 | 6.76 (3.00) | 6.28 (2.33) | ||
| 50–59.9 | 7.55 (3.34) | 5.44 (2.25) | ||
| 60–69.9 | 8.27 (3.83) | 4.69 (2.20) | ||
| 70–79.9 | 8.12 (3.33) | 3.90 (2.08) | ||
| ≥80 | 7.14 (4.17) | 4.12 (2.35) | ||
aScores 4–20, higher score unfavorable.
bScores 0–10, higher score favorable.
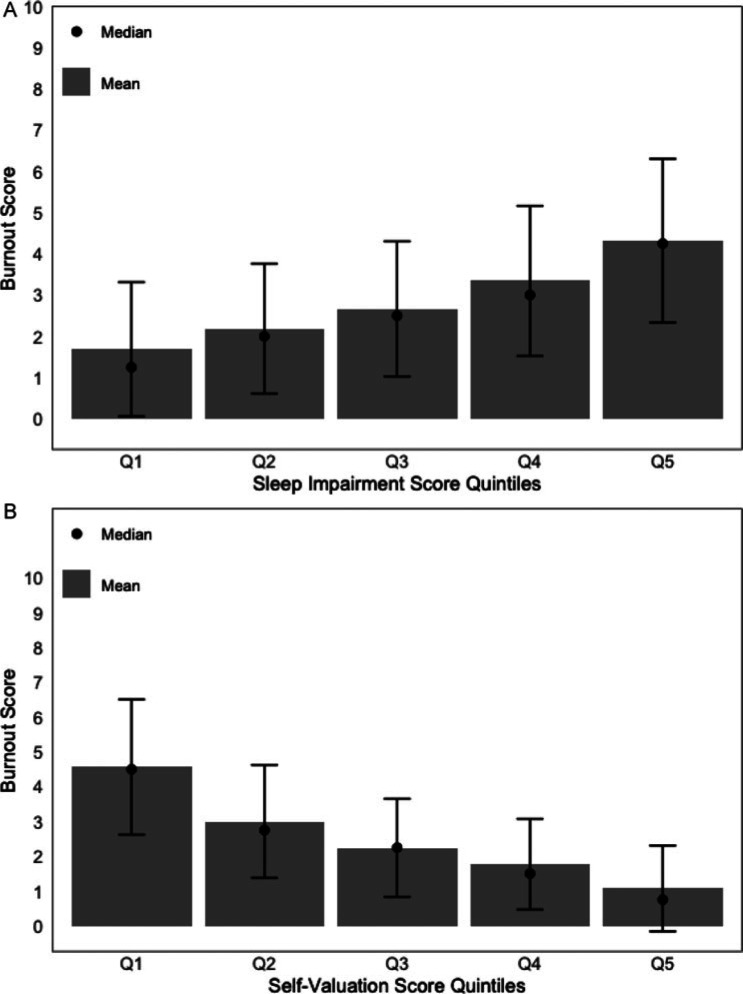
Variations in burnout and professional fulfillment by personal and professional characteristics are shown in Table 4. Mean burnout scores were more favorable as age increased and among those who were married or a widow or widower and those with children. Burnout scores varied by position, with the lowest scores among CFOs and CNOs and highest scores among CIOs. Higher sleep-related impairment scores were associated with higher burnout scores (Figure 1A); higher self-valuation scores were associated with lower burnout scores (Figure 1B).
TABLE 4. Personal/Professional Characteristics and Professional Well-Being.
| Burnouta | Professional Fulfillmentb | |||
|---|---|---|---|---|
| M (SD) | p | M (SD) | p | |
| Gender | ||||
| Female | 2.79 (1.93) | .127 | 7.20 (2.06) | .100 |
| Male | 2.62 (1.92) | 7.40 (2.13) | ||
| Age (years) | ||||
| <30 | 3.67 (2.39) | <.001 | 6.59 (1.88) | .162 |
| 30–39 | 3.01 (2.00) | 7.10 (1.99) | ||
| 40–49 | 2.91 (2.03) | 7.23 (2.31) | ||
| 50–59 | 2.53 (1.81) | 7.41 (2.01) | ||
| ≥60 | 2.14 (1.69) | 7.48 (2.01) | ||
| Relationship status | ||||
| Single | 3.05 (2.08) | .005 | 6.77 (2.26) | <.001 |
| Married | 2.62 (1.89) | 7.43 (2.07) | ||
| Partnered | 3.33 (2.29) | 6.79 (2.08) | ||
| Widow, widower | 2.36 (1.93) | 8.21 (1.49) | ||
| Children | ||||
| No children | 3.11 (2.19) | .003 | 6.87 (2.22) | .004 |
| Aged <5 years | 2.54 (1.76) | 7.51 (1.85) | ||
| Aged 5–12 years | 2.82 (1.97) | 7.21 (2.24) | ||
| Aged 13–18 years | 2.67 (1.88) | 7.39 (2.10) | ||
| Aged 19–22 years | 2.60 (1.90) | 7.45 (2.02) | ||
| Aged ≥23 years | 2.39 (1.83) | 7.62 (2.01) | ||
| Position | ||||
| CEO | 2.50 (1.86) | .010 | 7.93 (1.88) | <.001 |
| COO | 2.46 (1.66) | 7.65 (1.97) | ||
| CFO | 1.66 (1.35) | 7.59 (2.04) | ||
| CIO | 3.50 (1.63) | 6.83 (2.41) | ||
| CMO | 2.89 (2.40) | 6.92 (2.68) | ||
| CNO | 2.26 (1.66) | 8.01 (1.64) | ||
| Other C-suite role | 3.49 (2.35) | 7.12 (2.32) | ||
| Senior vice president | 2.41 (1.48) | 7.47 (1.44) | ||
| Vice president | 2.87 (1.89) | 7.15 (1.96) | ||
| Department head, director | 2.83 (2.02) | 6.94 (2.24) | ||
| Manager | 2.97 (2.15) | 6.59 (2.31) | ||
| Other | 1.62 (1.85) | 8.54 (1.42) | ||
| Position | ||||
| CEO | 2.50 (1.86) | .063 | 7.93 (1.88) | <.001 |
| Member of C-suite (other than CEO) | 2.56 (1.85) | 7.54 (2.07) | ||
| Senior vice president | 2.41 (1.48) | 7.47 (1.44) | ||
| Vice president | 2.87 (1.89) | 7.15 (1.96) | ||
| Department head, director | 2.83 (2.02) | 6.94 (2.24) | ||
| Manager | 2.97 (2.15) | 6.59 (2.31) | ||
| Other | 1.62 (1.85) | 8.54 (1.42) | ||
| Hours worked per week | ||||
| <40 | 2.56 (2.02) | <.001 | 6.35 (3.30) | .067 |
| 40–49.9 | 2.30 (1.80) | 7.34 (2.18) | ||
| 50–59.9 | 2.59 (1.88) | 7.41 (2.02) | ||
| 60–69.9 | 3.11 (2.03) | 7.21 (2.15) | ||
| 70–79.9 | 3.78 (2.02) | 6.52 (2.09) | ||
| ≥80 | 2.97 (2.22) | 7.46 (1.97) | ||
| Sleep impairment score | ||||
| Quintile 1 | 1.69 (1.63) | <.001 | 7.99 (1.96) | <.001 |
| Quintile 2 | 2.19 (1.57) | 7.69 (1.78) | ||
| Quintile 3 | 2.66 (1.64) | 7.30 (2.10) | ||
| Quintile 4 | 3.29 (1.80) | 6.91 (2.18) | ||
| Quintile 5 | 4.29 (2.00) | 6.32 (2.16) | ||
| Self-valuation score | ||||
| Quintile 1 | 4.57 (1.94) | <.001 | 5.92 (2.22) | <.001 |
| Quintile 2 | 3.00 (1.63) | 7.10 (1.91) | ||
| Quintile 3 | 2.24 (1.41) | 7.68 (1.79) | ||
| Quintile 4 | 1.77 (1.31) | 8.02 (1.69) | ||
| Quintile 5 | 1.07 (1.23) | 8.46 (1.99) | ||
aScores 0–10, higher score unfavorable.
bScores 0–10, higher score favorable.
FIGURE 1.
Relationship Among Burnout, Sleep-Related Impairment, and Self-Valuation. (A) Burnout Scores by Quintile of Sleep-Related Impairment (Lowest Quintile = Most Favorable). (B) Burnout Scores by Quintile of Self-Valuation (Highest Quintile = Most Favorable)
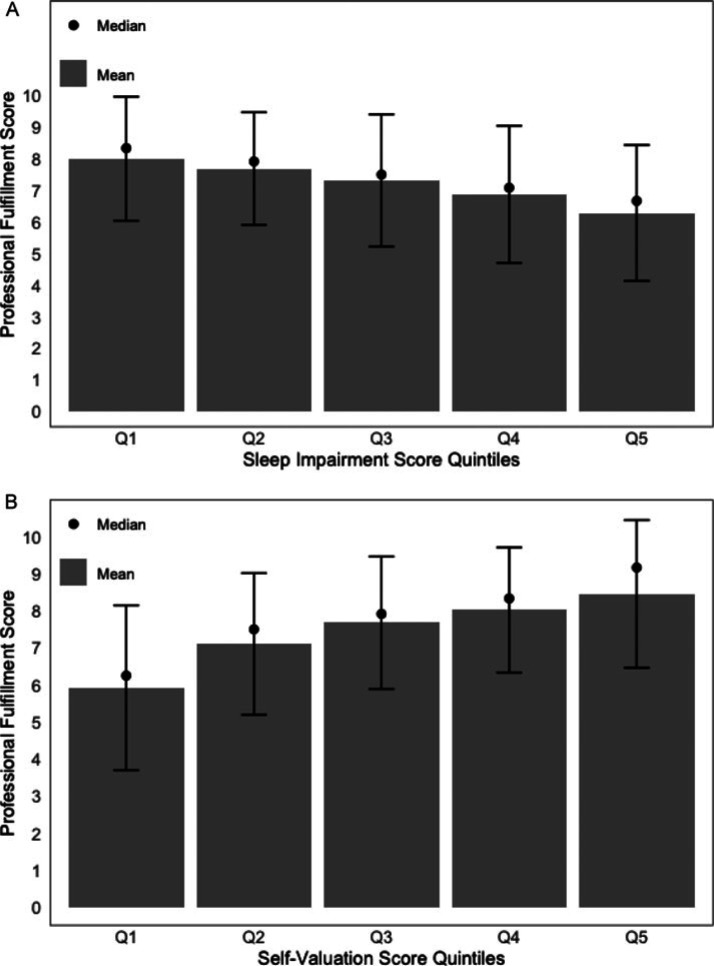
Mean professional fulfillment scores were highest for those who were married or a widow or widower and those with children. Professional fulfillment scores varied by role and were highest among CEOs and CNOs and lowest among CIOs and managers. Higher sleep-related impairment scores were associated with lower professional fulfillment scores (Figure 2A) whereas higher self-valuation scores were associated with higher professional fulfillment scores (Figure 2B).
FIGURE 2.
Relationship Among Professional Fulfillment, Sleep-Related Impairment, and Self-Valuation. (A) Professional Fulfillment Scores by Quintile of Sleep-Related Impairment (Lowest Quintile = Most Favorable). (B) Professional Fulfillment Scores by Quintile of Self-Valuation (Highest Quintile = Most Favorable)
Finally, we conducted a multivariable analysis to identify factors independently associated with burnout and professional fulfillment among administrative leaders. Sleep-related impairment (OR for each 1-point increase on a 0–10 scale = 1.29, 95% CI [1.19–1.41]; p < .001) and self-valuation (OR for each 1-point increase on a 0–10 scale = 0.63, 95% CI [0.57–0.68]; p < .001) were independently associated with burnout after adjusting for all other variables (age, gender, relationships status, children, hours worked per week, position). Notably, an increased risk of burnout among managers was the only other personal or professional characteristic that showed a statistically significant association after adjusting for sleep and self-valuation (see Supplemental Digital Content Table 1, available at http://links.lww.com/JHM/A82).
Sleep-related impairment (OR for each 1-point increase on a 0–10 scale = 0.88, 95% CI [0.82–0.95]; p = .001) and self-valuation (OR for each 1-point increase on a 0–10 scale = 1.43, 95% CI [1.32–1.54]; p < .001) were independently associated with professional fulfillment after adjusting for all other variables (age, gender, relationships status, children, hours worked per week, position). Notably, the only other personal or professional characteristic that showed a statistically significant association after adjusting for sleep and self-valuation was a higher likelihood of professional fulfillment among CEOs (see Supplemental Digital Content Table 2, available at http://links.lww.com/JHM/A82).
DISCUSSION
Although much is known about the experience of occupational distress in clinicians, little is known about the work experience of distress in healthcare administrators. We report here, to the best of our knowledge, the first large-scale assessment of burnout and professional fulfillment among healthcare leaders in the United States. The survey occurred in June 2021, roughly 15 months into the COVID-19 pandemic. The leaders had generally high professional fulfillment scores, with more than half scoring in the high range.
Mean scores for professional fulfillment for healthcare administrators in this study are higher than those reported in a previously published sample of U.S. physicians using the same instrument (Trockel et al., 2020; mean professional fulfillment score for healthcare leaders on a 0–10 scale = 7.29; mean score for physicians = 6.48). In this study, >85% of respondents indicated that they liked their job and would recommend a career in healthcare leadership to young people. Burnout scores were generally lower than have been observed in clinicians (Trockel et al., 2020; mean burnout score for healthcare leaders on a 0–10 scale = 2.71; mean score for physicians = 2.99). Nonetheless, roughly one third of healthcare leaders had burnout scores that fell in the high range. No statistically significant differences in burnout or professional fulfillment were observed by gender in either the univariate or multivariate analysis. With respect to role, burnout scores were highest among CIOs, operational managers, and CMOs; they were lowest among CFOs and CNOs. Professional fulfillment scores were highest among CNOs and CEOs and lowest among CIOs.
The large number of CEOs in the sample provides unique insights into the experience of these leaders. The CEOs in the sample were, on average, more likely than other workers to be men, older, married, and have children. On average, they worked more hours per week than those in other positions and had favorable sleep and self-valuation scores. The CEOs were more likely to have higher professional fulfillment scores than other senior leaders, after adjustments for other personal and professional characteristics. One may hypothesize that autonomy, respect, prestige, and compensation may account for some of this difference. Given the high rates of burnout and dissatisfaction among physicians and nurses, managers may have greater exposure to those struggling clinicians, which may contribute to their own distress. On the other hand, CEOs have ultimate responsibility for organizational performance and metrics and face an elevated level of pressure and accountability for organizational performance. Despite the high professional fulfillment scores, CEOs' risk of burnout was similar to that for other positions.
Our study also provides important insights into the critical impact of sleep health and self-compassion on the work experience of healthcare administrators. The distribution of sleep scores had a left-shifted distribution (toward more favorable scores), with less than one in four scoring above the cut point for sleep-related impairment, which is near 1 standard deviation above the PROMIS database mean. If similar to the PROMIS sample SRI data, about one in three would be above this cut point. Sleep health improved with age and was most favorable among those working 40–49 hr per week, with less favorable scores for those working above this threshold. In contrast, self-valuation scores showed a bell-shaped distribution. Self-valuation scores were higher among men than among women, a finding that has been observed in other survey populations (Trockel et al., 2019) and incrementally declined (unfavorable) as hours worked per week increased. Although causation and the potential direction of effect cannot be determined in this cross-sectional survey, one interpretation is that those who do not optimally value their personal needs are more likely to increase work hours and be consumed by work.
Notably, sleep-related impairment and self-valuation scores exhibited an apparent dose–response relationship with both burnout and professional fulfillment. Each 1 point more favorable sleep score or 1 point more favorable self-valuation score was associated with decreased burnout and increased professional fulfillment. Strikingly, in the multivariate analysis including all personal (age, gender, relationship status, children) and professional characteristics (role, work setting, hours worked per week), sleep and self-valuation scores were the dominant independent predictors of burnout and professional fulfillment. This observation has potentially significant implications for interventions to reduce occupational distress and improve professional fulfillment among healthcare executives. Specifically, it suggests that the ability of interventions to improve sleep health and self-valuation should be tested as a possible means to mitigate work-related distress and promote professional fulfillment.
Improvement in self-valuation and sleep health will likely require both individual- and system-based interventions. Professional coaching has been shown to be an effective approach to improve both sleep health and self-valuation on the individual level. However, wider interventions to create a culture that values sleep and attention to personal needs (time off, personal relationships, work–life integration) may have greater organizational impact (Dodson & Heng, 2021). A mindset of perfectionism and self-criticism can also be endemic in a healthcare organization (Dodson & Heng, 2021; Shanafelt, Schein, et al., 2019). Accordingly, interventions to replace a culture of perfectionism (unforgiving excellence) with commitment to excellence and growth mindset may be necessary (Dodson & Heng, 2021).
Recent evidence suggests that attending to the personal well-being, burnout (Shanafelt, Makowski, et al., 2020), and sleep health (Barnes, 2018) of leaders should be an institutional priority. Specifically, studies of physician leaders at Stanford Medicine demonstrated that the personal burnout, professional fulfillment, and sleep scores of each work unit leader correlated with their independently assessed leadership behavior score as evaluated by members of their team (Shanafelt, Makowski, et al., 2020). Other studies indicate that this same leader behavior score predicts burnout and professional fulfillment scores among the members of that leader's work unit (Dyrbye, Major-Elechi, et al., 2020; Dyrbye, Major-Elechi, et al., 2021; Shanafelt, Gorringe, et al., 2015). Leader behavior score also predicts whether members of the work unit believe that the values of their organization are aligned with their altruistic personal values (Shanafelt et al., 2021). These results illustrate the extent to which people experience their organization through the lens of their immediate supervisor as well as the impact that the behavior and effectiveness of that leader has on occupational burnout and professional fulfillment among members of their work unit. These findings also suggest that interventions to cultivate sleep health and personal well-being should be viewed as a component of leadership development rather than simply a dimension of self-care (Shanafelt, Makowski, et al., 2020). Such interventions may include defining these dimensions as important values for leaders, establishing new group norms, and offering individual (e.g., executive coaching), along with the group strategies to promote them.
Study Limitations
Our study has several important limitations. First, although the participation rate is typical of large national surveys, only one in four of those invited completed this survey. Two standard analyses to evaluate for response bias (comparing respondents with the sampling frame and comparison of early respondents with late respondents, an established proxy for nonrespondents [Johnson & Wislar, 2012]) suggest that respondents were representative of eligible ACHE members with the exception that they might be slightly older than members overall. It is unknown whether those with greater occupational distress are more likely to participate in such surveys out of interest in the topic or are less likely to do so because of apathy and disengagement. The available published data from studies of clinicians suggest that the burnout and professional fulfillment experiences of participants in such surveys are generally representative of the sample overall (Shanafelt, West, et al., 2019). Second, by design, the study focused on senior leaders. Although a limited number of managers were included, the extent to which the findings can be extrapolated to them is unknown. Third, we did not collect information on the geographic regions in which participants worked. It is possible that experience varies by geography, a dimension that should be explored in future studies. Finally, due to the cross-sectional nature of the data, a causal relationship between the variables evaluated and the potential direction of effect cannot be determined.
Future Research
Our study raises additional questions that merit future research, including the following:
What are the primary drivers of professional fulfillment in healthcare administrators?
Is there an association between a healthcare administrator's degree of burnout and the type of healthcare organization in which he or she works?
Are leaders who have high occupational well-being more likely to prioritize the importance of well-being in organizational strategy and decision-making?
How will burnout and professional fulfillment evolve as the challenges of the pandemic recede?
Will the growing advent of chief wellness officers and programs to prevent burnout have an effect on leaders' burnout and fulfillment?
How will diversity and inclusion efforts affect burnout and fulfillment?
CONCLUSION
The results of this study suggest that 15 months into the COVID-19 pandemic, healthcare leaders in the United States demonstrated high degrees of professional fulfillment and job satisfaction. Their burnout and occupational distress appeared lower than that documented in clinicians. Nonetheless, roughly one in three administrative leaders was experiencing professional burnout. Sleep health and self-compassion appeared to be critical drivers of both burnout and professional fulfillment. Attention to these domains may represent an actionable intervention for organizations to improve professional fulfillment. Given the evidence that personal health affects independently rated leadership effectiveness, these results suggest that organizations should prioritize the well-being of their leaders and support those who are experiencing burnout or other forms of occupational distress. Doing so may improve the health of the U.S. healthcare delivery system.
Supplementary Material
ACKNOWLEDGMENTS
The authors thank the healthcare leaders who responded to this survey for their time, consideration, and service to their profession and to healthcare leadership research.
Footnotes
Funding for this study was provided by the American College of Healthcare Executives and the Stanford WellMD Center.
The authors declare no conflicts of interest.
Supplemental digital content is available for this article. Direct URL citations appear in the printed text and are provided in the HTML and PDF versions of this article on the journal's Web site (www.jhmjournalonline.com).
Contributor Information
Tait Shanafelt, Stanford University, Palo Alto, California.
Mickey Trockel, Stanford University, Palo Alto, California.
Hanhan Wang, Stanford University, Palo Alto, California.
Thom Mayer, Duke University, Durham, North Carolina.
Leslie Athey, American College of Healthcare Executives, Chicago, Illinois.
REFERENCES
- Afonso A. M., Cadwell J. B., Staffa S. J., Zurakowski D., Vinson A. E. (2021). Burnout rate and risk factors among anesthesiologists in the United States. Anesthesiology, 134(5), 683–696. 10.1097/ALN.0000000000003722 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aiken L. H., Clarke S. P., Sloane D. M., Sochalski J., Silber J. H. (2002). Hospital nurse staffing and patient mortality, nurse burnout, and job dissatisfaction. JAMA, 288(16), 1987–1993. 10.1001/jama.288.16.1987 [DOI] [PubMed] [Google Scholar]
- Barnes C. (2018, September-October). Sleep well, lead better. Harvard Business Review, 140–143. https://hbr.org/2018/09/sleep-well-lead-better
- Bodenheimer T., Sinsky C. (2014). From triple to quadruple aim: Care of the patient requires care of the provider. Annals of Family Medicine, 12(6), 573–576. 10.1370/afm.1713 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brady K. J. S., Ni P., Carlasare L., Shanafelt T. D., Sinsky C. A., Linzer M., Stillman M., Trockel M. T. (2021). Establishing crosswalks between common measures of burnout in US physicians. Journal of General Internal Medicine, 37(4), 777–784. 10.1007/s11606-021-06661-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cimiotti J. P., Aiken L. H, Sloane D. M., Wu E. S. (2012). Nurse staffing, burnout, and health care-associated infection. American Journal of Infection Control, 40(6), 486–490. 10.1016/j.ajic.2012.02.029 [DOI] [PMC free article] [PubMed] [Google Scholar]
- DeChant P. F., Acs A., Rhee K. B., Boulanger T. S., Snowdon J. L., Tutty M. A., Sinsky C. A., Thomas Craig K. J. (2019). Effect of organization-directed workplace interventions on physician burnout: A systematic review. Mayo Clinic Proceedings Innovations, Quality & Outcomes, 3(4), 384–408. 10.1016/j.mayocpiqo.2019.07.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dodson S., Heng Y. (2021). Self-compassion in organizations: A review and future research agenda. Journal of Organizational Behavior, 43(2), 168–196. 10.1002/job.2556 [DOI] [Google Scholar]
- Dyrbye L. N., Major-Elechi B., Hays J. T., Fraser C. H., Buskirk S. J., West C. P. (2020). Relationship between organizational leadership and health care employee burnout and satisfaction. Mayo Clinic Proceedings, 95(4), 698–708. 10.1016/j.mayocp.2019.10.041 [DOI] [PubMed] [Google Scholar]
- Dyrbye L. N., Major-Elechi B., Hays J. T., Fraser C. H., Buskirk S. J., West C. P. (2021). Physicians' ratings of their supervisor's leadership behaviors and their subsequent burnout and satisfaction: A longitudinal study. Mayo Clinic Proceedings, 96(10), 2598–2605. 10.1016/j.mayocp.2021.01.035 [DOI] [PubMed] [Google Scholar]
- Dyrbye L. N., Major-Elechi B., Thapa P., Hays J. T., Fraser C. H., Buskirk S. J., West C. P. (2021). Characterization of nonphysician health care workers' burnout and subsequent changes in work effort. JAMA Network Open, 4(8), e2121435. 10.1001/jamanetworkopen.2021.21435 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dyrbye L. N., West C. P., Halasy M., O'Laughlin D. J., Satele D., Shanafelt T. (2020). Burnout and satisfaction with work–life integration among PAs relative to other workers. JAAPA, 33(5), 35–44. 10.1097/01.JAA.0000660156.17502.e6 [DOI] [PubMed] [Google Scholar]
- Dyrbye L. N., West C. P., Hunderfund A. L., Sinsky C., Trockel M., Tutty M., Carlasare L., Satele D., Shanafelt T. D. (2020). Relationship between burnout, professional behaviors, and cost-conscious attitudes among US physicians. Journal of General Internal Medicine, 35(5), 1465–1476. 10.1007/s11606-019-05376-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dyrbye L. N., West C. P., Johnson P. O., Cipriano P. F., Beatty D. E., Peterson C., Major-Elechi B., Shanafelt T. (2019). Burnout and satisfaction with work–life integration among nurses. Journal of Occupational and Environmental Medicine, 61(8), 689–698. 10.1097/JOM.0000000000001637 [DOI] [PubMed] [Google Scholar]
- Dyrbye L. N., West C. P., Kelsey E. A., Gossard A. A., Satele D., Shanafelt T. (2020). A national study of personal accomplishment, burnout, and satisfaction with work–life integration among advance practice nurses relative to other workers. Journal of the American Association of Nurse Practitioners, 33(11), 896–906. 10.1097/JXX.0000000000000517 [DOI] [PubMed] [Google Scholar]
- Farrugia G., Plutowski R. W. (2020). Innovation lessons from the COVID-19 pandemic. Mayo Clinic Proceedings, 95(8), 1574–1577. 10.1016/j.mayocp.2020.05.024 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hamidi M. S., Bohman B., Sandborg C., Smith-Coggins R., de Vries P., Albert M. S., Murphy M. L., Welle D., Trockel M. T. (2018). Estimating institutional physician turnover attributable to self-reported burnout and associated financial burden: A case study. BMC Health Services Research, 18(1), 851. 10.1186/s12913-018-3663-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Han S., Shanafelt T. D., Sinsky C. A., Awad K. M., Dyrbye L. N., Fiscus L. C., Trockel M., Goh J. (2019). Estimating the attributable cost of physician burnout in the United States. Annals of Internal Medicine, 170(11), 784–790. 10.7326/M18-1422 [DOI] [PubMed] [Google Scholar]
- HealthMeasures. (2022). PROMIS score cut points. https://www.healthmeasures.net/score-and-interpret/interpret-scores/promis/promis-score-cut-points
- Johnson T. P., Wislar J. S. (2012). Response rates and nonresponse errors in surveys. JAMA, 307(17), 1805–1806. 10.1001/jama.2012.3532 [DOI] [PubMed] [Google Scholar]
- Linzer M., Poplau S., Prasad K., Khullar D., Brown R., Varkey A., Yale S., Grossman E., Williams E., Sinsky C. (2019). Characteristics of health care organizations associated with clinician trust: Results from the healthy work place study. JAMA Network Open, 2(6), e196201. 10.1001/jamanetworkopen.2019.6201 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mann D. M., Chen J., Chunara R., Testa P. A., Nov O. (2020). COVID-19 transforms health care through telemedicine: Evidence from the field. Journal of the American Medical Informatics Association, 27(7), 1132–1135. 10.1093/jamia/ocaa072 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McHugh M. D., Kutney-Lee A., Cimiotti J. P., Sloane D. M, Aiken L. H. (2011). Nurses' widespread job dissatisfaction, burnout, and frustration with health benefits signal problems for patient care. Health Affairs (Millwood), 30(2), 202–210. 10.1377/hlthaff.2010.0100 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Melnyk B. M., Kelly S. A., Stephens J., Dhakal K., McGovern C., Tucker S., Hoying J., McRae K., Ault S., Spurlock E., Bird S. B. (2020). Interventions to improve mental health, well-being, physical health, and lifestyle behaviors in physicians and nurses: A systematic review. American Journal of Health Promotion, 34(8), 929–941. 10.1177/0890117120920451 [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Academies of Sciences, Engineering, and Medicine; National Academy of Medicine; & Committee on Systems Approaches to Improve Patient Care by Supporting Clinician Well-Being. (2019). Taking action against clinician burnout: A systems approach to professional well-being. The National Academies Press. 10.17226/25521 [DOI] [PubMed] [Google Scholar]
- Panagioti M., Panagopoulou E., Bower P., Lewith G., Kontopantelis E., Chew-Graham C., Dawson S., van Marwijk H., Geraghty K., Esmail A. (2017). Controlled interventions to reduce burnout in physicians: A systematic review and meta-analysis. JAMA Internal Medicine, 177(2), 195–205. 10.1001/jamainternmed.2016.7674 [DOI] [PubMed] [Google Scholar]
- Shah M. K., Gandrakota N., Cimiotti J. P., Ghose N., Moore M., Ali M. K. (2021). Prevalence of and factors associated with nurse burnout in the US. JAMA Network Open, 4(2), e2036469. 10.1001/jamanetworkopen.2020.36469 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shanafelt T. D., Balch C. M., Bechamps G., Russell T., Dyrbye L., Satele D., Collicott P., Novotny P. J., Sloan J., Freischlag J. (2010). Burnout and medical errors among American surgeons. Annals of Surgery, 251(6), 995–1000. 10.1097/SLA.0b013e3181bfdab3 [DOI] [PubMed] [Google Scholar]
- Shanafelt T. D., Boone S., Tan L., Dyrbye L. N., Sotile W., Satele D., West C. P., Sloan J., Oreskovich M. R. (2012). Burnout and satisfaction with work–life balance among US physicians relative to the general US population. Archives of Internal Medicine, 172(18), 1377–1385. 10.1001/archinternmed.2012.3199 [DOI] [PubMed] [Google Scholar]
- Shanafelt T., Goh J., Sinsky C. (2017). The business case for investing in physician well-being. JAMA Internal Medicine, 177(12), 1826–1832. 10.1001/jamainternmed.2017.4340 [DOI] [PubMed] [Google Scholar]
- Shanafelt T. D., Gorringe G., Menaker R., Storz K. A., Reeves D., Buskirk S. J., Sloan J. A., Swensen S. J. (2015). Impact of organizational leadership on physician burnout and satisfaction. Mayo Clinic Proceedings, 90(4), 432–440. 10.1016/j.mayocp.2015.01.012 [DOI] [PubMed] [Google Scholar]
- Shanafelt T. D., Makowski M. S., Wang H., Bohman B. D., Leonard M., Harrington R., Minor L. M., Trockel M. (2020). Association of burnout, professional fulfillment, and self-care practices of physician leaders with their independently rated leadership effectiveness. JAMA Network Open, 3(6), e207961. 10.1001/jamanetworkopen.2020.7961 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shanafelt T. D., Mungo M., Schmitgen J., Storz K. A., Reeves D., Hayes S. N., Sloan J. A., Swensen S. J., Buskirk S. J. (2016). Longitudinal study evaluating the association between physician burnout and changes in professional work-effort. Mayo Clinic Proceedings, 91(4), 422–431. 10.1016/j.mayocp.2016.02.001 [DOI] [PubMed] [Google Scholar]
- Shanafelt T. D., Noseworthy J. H. (2017). Executive leadership and physician well-being: Nine organizational strategies to promote engagement and reduce burnout. Mayo Clinic Proceedings, 92(1), 129–146. 10.1016/j.mayocp.2016.10.004 [DOI] [PubMed] [Google Scholar]
- Shanafelt T. D., Schein E., Minor L. B., Trockel M., Schein P., Kirch D. (2019). Healing the professional culture of medicine. Mayo Clinic Proceedings, 94(8), 1556–1566. 10.1016/j.mayocp.2019.03.026 [DOI] [PubMed] [Google Scholar]
- Shanafelt T. D., Stolz S., Springer J., Murphy D., Bohman B., Trockel M. A. (2020). Blueprint for organizational strategies to promote the well-being of health care professionals. NEJM Catalyst Innovations in Care Delivery, 1(6), 1–17. 10.1056/CAT.20.0266 [DOI] [Google Scholar]
- Shanafelt T. D., Trockel M., Ripp J., Murphy M. L., Sandborg C., Bohman B. (2019). Building a program on well-being: Key design considerations to meet the unique needs of each organization. Academic Medicine, 94(2), 156–161. 10.1097/ACM.0000000000002415 [DOI] [PubMed] [Google Scholar]
- Shanafelt T. D., Wang H., Leonard M., Hawn M., McKenna Q., Majzun R., Minor L., Trockel M. (2021). Assessment of the association of leadership behaviors of supervising physicians with personal-organizational values alignment among staff physicians. JAMA Network Open, 4(2), e2035622. 10.1001/jamanetworkopen.2020.35622 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shanafelt T. D., West C. P., Sinsky C., Satele D., Sloan J., West C. P. (2019). Changes in burnout and satisfaction with work–life integration in physicians and the general US working population between 2011 and 2017. Mayo Clinic Proceedings, 94(9), 1681–1694. 10.1016/j.mayocp.2015.08.023 [DOI] [PubMed] [Google Scholar]
- Skrupky L. P., West C. P., Shanafelt T., Satele D. V., Dyrbye L. N. (2003). Ability of the Well-Being Index to identify pharmacists in distress. Journal of the American Pharmacists Association, 60(6), 906–914.e2. 10.1016/j.japh.2020.06.015 [DOI] [PubMed] [Google Scholar]
- Swensen S., Kabcenell A., Shanafelt T. (2016). Physician–organization collaboration reduces physician burnout and promotes engagement: The Mayo Clinic experience. Journal of Healthcare Management, 61(2), 105–127. 10.1097/00115514-201603000-00008 [DOI] [PubMed] [Google Scholar]
- Tawfik D. S., Scheid A., Profit J., Shanafelt T., Trockel M., Adair K. C., Sexton J. B., Ioannidis J. P. A. (2019). Evidence relating health care provider burnout and quality of care: A systematic review and meta-analysis. Annals of Internal Medicine, 171(8), 555–567. 10.7326/M19-1152 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Trockel M., Bohman B., Lesure E., Hamidi M. S., Welle D., Roberts L., Shanafelt T. (2017). A brief instrument to assess both burnout and professional fulfillment in physicians: Reliability and validity, including correlation with self-reported medical errors, in a sample of resident and practicing physicians. Academic Psychiatry, 42, 11–24. 10.1007/s40596-017-0849-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Trockel M. T., Hamidi M. S., Menon N. K., Rowe S., Dudley J., Stewart M. T., Geisler C. Z., Bohman B. D., Shanafelt T. (2019). Self-valuation: Attending to the most important instrument in the practice of medicine. Mayo Clinical Proceedings, 94(10), 2022–2031. 10.1016/j.mayocp.2019.04.040 [DOI] [PubMed] [Google Scholar]
- Trockel M. T., Menon N. K., Rowe S. G., Stewart M. T., Smith R., Lu M., Kim P. K., Quinn M. A., Lawrence E., Marchalik D., Farley H., Normand P., Felder M., Dudley J. C., Shanafelt T. D. (2020). Assessment of physician sleep and wellness, burnout, and clinically significant medical errors. JAMA Network Open, 3(12), e2028111. 10.1001/jamanetworkopen.2020.28111 [DOI] [PubMed] [Google Scholar]
- Trockel M., Sinsky C., West C. P., Dyrbye L. N., Tutty M., Carlasare L., Wang H., Shanafelt T. D. (2021). Self-valuation challenges in the culture and practice of medicine and physician well-being. Mayo Clinic Proceedings, 96(8), 2123–2132. 10.1016/j.mayocp.2020.12.032 [DOI] [PubMed] [Google Scholar]
- Welp A., Meier L. L., Manser T. (2016). The interplay between teamwork, clinicians' emotional exhaustion, and clinician-rated patient safety: A longitudinal study. Critical Care, 20(1), 110. 10.1186/s13054-016-1282-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- West C. P., Dyrbye L. N., Erwin P. J., Shanafelt T. D. (2016). Interventions to prevent and reduce physician burnout: A systematic review and meta-analysis. Lancet, 388(10057), 2272–2281. 10.1016/S0140-6736(16)31279-X [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.