Abstract
Monitoring the spatial and temporal course of opioid-related drug overdose mortality is a key public health determinant. Despite previous studies exploring the evolution of drug-related fatalities following the stay-at-home mandates during the COVID-19 pandemic, little is known about the spatiotemporal dynamics that mitigation efforts had on overdose deaths. The purpose of this study was to describe the spatial and temporal dynamics of overdose death relative risk using a 4-week interval over a span of 5 months following the implementation of the COVID-19 lockdown in the city of Chicago, IL. A Bayesian space–time model was used to produce posterior risk estimates and exceedance probabilities of opioid-related overdose deaths controlling for measures of area-level deprivation and stay-at-home mandates. We found that area-level temporal risk and inequalities in drug overdose mortality increased significantly in the initial months of the pandemic. We further found that a change in the area-level deprivation from the first to the fourth quintile increased the relative risk of a drug overdose risk by 44.5%. The social distancing index measuring the proportion of persons who stayed at home in each census block group was not associated with drug overdose mortality. We conclude by highlighting the importance of contextualizing the spatial and temporal risk in overdose mortality for implementing effective and safe harm reduction strategies during a global pandemic.
Supplementary Information
The online version contains supplementary material available at 10.1007/s11524-022-00675-x.
Keywords: Bayesian spatiotemporal model, Opioid overdose mortality, Area deprivation, Social distancing
Introduction
Over the past decade, drug overdose fatalities began increasing at an alarming rate in the USA [1]. Beginning in March 2020, the synergy created by the syndemic of COVID-19 and opioid-related drug overdose deaths has resulted in a massive public health crisis both in the USA and abroad. During the COVID-19 pandemic, for example, fatal opioid-related overdoses in Cook County, IL, where the present study was conducted, increased by as much as 23.7% following the implementation of a stay-at-home order on March 20, 2020 [2]. The mechanisms linking COVID-19 to increases in drug overdose mortality are associated with the exacerbation of pre-existing social and economic conditions in the wake of the pandemic that has affected individuals (e.g., depression, anxiety, boredom) [3], relationships (e.g., physical and social isolation), and communities (e.g., job loss, unemployment, food, and housing insecurity). As a result, socio-economic inequalities in health, and specifically deaths attributable to drug use, have been magnified. Containment efforts used to control the spread of transmission during COVID-19 and other pandemics have resulted in a number of unintended consequences that have been shown to compromise mental and emotional health [4] despite their effectiveness in curbing disease transmission. For example, past research demonstrates the detrimental psychological effects of mandatory lockdowns associated with loss of income and social connections [4, 5]. Those who are unable to work remotely and/or are living in overcrowded, low-income neighborhoods continue to be disproportionately impacted by the COVID-19 pandemic [6–10].
Drug overdose is one of the leading causes of death and poses a significant public health threat on its own. A substantial body of research shows that drug overdoses have increased steadily from year to year even before the onset of COVID-19. For example, between 2000 and 2014, the opioid-related death rate increased by 200% in the USA [11]. Almost 47,000 persons in the USA died of a drug overdose involving opioids in 2018, which is nine times higher than the number of deaths attributed to opioids in 1999 [12, 13]. Nevertheless, research conducted in the early months of the COVID-19 pandemic has demonstrated that drug use patterns and, ultimately, overdose rates shifted, creating what some have called, the “co-occurrence of two public health crises” [14]. Research conducted at both national and state levels has shown increases in overdose deaths during the early months of the pandemic [15–18] attributing the increases, in part, to the COVID-19 lockdown [19]. According to preliminary data from the Center for Disease Control, from October 2019 to September 2020, there was a 28.8% increase in overdose deaths in the USA. In Illinois, this number was even more pronounced at 32.6% [20, 21]. One study of opioid-related fatalities in Cook County during the period spanning January 1, 2018–October 6, 2020, found that average overdose deaths per week were relatively stable prior to the pandemic but that there was a marked increase during the 11-week stay-at-home order followed by a substantial decline [2]. An examination of N = 470 adults who died of a drug overdose in the State of Rhode Island and found that, compared to the same time frame the previous year, mortality rates were higher among men, non-Hispanic Whites, unmarried individuals, individuals using synthetic opioids, and in residential settings [12]. In San Francisco, researchers found an increased risk of drug-related harms, including death, during the implementation of social distancing regulations among individuals requiring an emergency room visit following an opioid-related injury [17]. The authors speculated that the increase was due to the lack of timely reversal treatment measures, such as naloxone, the isolation of social distancing, and/or less visibility of public drug use or decreased home visitation because of reduced foot traffic. Demographic differences in drug overdose have also been noted. Studies comparing overdose deaths before and during COVID-19 have found an increase for African Americans and males [14] but not Whites [22]. This is supported by data from the Philadelphia Department of Public Health (2021) which shows Black residents dying of overdose at higher rates than Whites as of June 2020. This disparity runs parallel to COVID-19 infection and hospitalization rates in susceptible neighborhoods [22].
The opioid overdose epidemic has complex social, biological, and behavioral causes including but not limited to the proliferation of opioid prescribing to treat chronic pain, changes in the heroin and illegally manufactured opioid synthetics markets, deindustrialization, and concentrated poverty [13]. Lockdown measures implemented during COVID-19 have only added to this complexity by posing additional challenges to an already over-burdened healthcare system. Consequently, the drug using population has become more susceptible to drug relapse and overdose [14]. Due mostly to data limitations, previous studies have assumed, but not tested, that the onset of extreme social distancing measures such as the stay-at-home mandate contributed to observed increases in substance abuse and addiction. Whereas existing research has played a critical role in revealing the public health consequences of the COVID-19 policy response and their differential effects on individuals who use drugs, the assumption that people were abiding by the stay-at-home mandates and/or that human mobility is homogenous is untenable, infeasible, and does not hold empirically. Instead, several individual- and community-based factors have been found to play an important role in effectuating compliance [23, 24]. Some studies have found that lack of compliance is associated with being unemployed [25], single motherhood, and being a member of a minoritized group [26]. A recent review of research examining barriers to the implementation of social distancing measures implemented during COVID-19 uncovered two categories of barriers: individual-psychological/psychosocial and sociological phenomena, and shortcomings in governmental action or communication. Specific psychological and psychosocial barriers revealed include avoiding stigma, feelings of solidarity, perceived threat and value of the intervention, and alignment of messaging and lived experience, accounting for life circumstances and addressing social norms [27]. Government factors included providing support for people to adhere to social distancing mandates and trust in government, and involving the community in both the pandemic’s planning and response phase [27]. The factors that are associated with either the inability or unwillingness to comply with stay-at-home mandates seem more closely related to socioeconomic marginalization (SEM). SEM is defined as a set of conditions that contributes to exclusion from social and economic opportunities including labor market conditions, inadequate income and poverty, social stigma, and isolation and housing insecurity [28]. A recent systematic review found that the very conditions contributing to SEM have been linked to drug overdose risk in the majority of studies under consideration [28].
Previous research has revealed spatial and temporal variation in population-level opioid-related overdose fatalities during COVID-19 [29–31] but no study to date has incorporated existing indices of social distancing behavior in communities and its association with drug overdose fatalities. Rather, research has merely documented increases in drug overdoses in the months following the implementation of stay-at-home mandates without considering geographic differences or differences in community-level compliance. Given past research demonstrating variability in compliance with stay-at-home mandates, even during the initial months of the pandemic, the goals of the present study were to explore the spatiotemporal trends in drug overdose deaths at the census block group level and the relationship between area deprivation, percentages of people staying at home, and drug overdose fatality. More specifically, we address the following questions: (1) what areas in Chicago experienced the highest risk for an opioid-related drug overdose fatality during the initial months (April 2020–August 2020) of the COVID-19 pandemic following the implementation of the stay-at-home order on March 20, 2020? (2) What was the temporal trend in overdose fatalities following the implementation of the stay-at-home order? (3) What was the magnitude of drug overdose inequality across the city, and did it change over time? And (4) how does area-level deprivation and sheltering in place alter the spatial risk of a drug overdose? Given previous research examining the enablers of adherence to social distancing measures at both the individual and community level (i.e., socio-economic status, lack of community preparedness, and lower levels of trust in government), we expect that areas with less compliance of social distancing mandates will have higher overdose rates after controlling for area-level deprivation. Additionally, we expect to find a positive association between social and economic deprivation, or SEM, and drug overdose mortality rates after controlling for neighborhood compliance with social distancing mandates. Our expectation in this regard was developed based on previous research showing that SEM, which includes neighborhood deprivation and economic inequality, is a structural inequity associated with drug overdose risk through cumulative life course disadvantage that has resulted in differential access to health promoting services [28].
Methods
Data on all fatal opioid-related overdoses among individuals who died in Cook County, IL, during the time frame spanning March 24–Aug 11, 2020 (a 140-day period), was downloaded from the Medical Examiner Case Archives for Cook County, IL [32]. The data contains information about all deaths that occurred in Cook County that were under the Medical Examiner’s jurisdiction. The Medical Examiner’s office investigates any death that is attributable to an adverse reaction due to drugs or alcohol including deaths that occur in an Emergency Department and/or any death that does not occur in the presence of a practicing licensed physician. For this study, we examined deaths that were categorized as “accident,” “natural,” “suicide,” and “undetermined.” Opioid-related overdose deaths (i.e., deaths due to any opioid, heroin, and/or an opioid analgesic) are considered a subset of drug overdose deaths in which any opioid drug was reported as a contributing cause of death (ICD-10 codes T40.0, T40.1, T40.2, T40.3, T40.4, and T40.6). Opioid analgesics include natural (e.g., morphine and codeine) and semi-synthetic opioid analgesics (e.g., oxycodone, hydrocodone, hydromorphone, oxymorphone), methadone, and synthetic opioid analgesics other than methadone (e.g., fentanyl and tramadol). All overdose fatalities included the location of the decedent making it possible to aggregate the count of overdose deaths to the census block group (CBG). Any individual that did not have a valid address was excluded from the present study (41 addresses were deemed invalid in the present study). Among those cases that contained an invalid address, the average age was 46.27 (SD = 15.25), 82.9% were male, 55% were non-Hispanic Black, 30% were non-Hispanic White, and 15% were Hispanic/Latinx.
As part of their COVID-19 response, SafeGraph, Inc. [33], released aggregated mobile device GPS data at the CBG level to facilitate understanding of people’s compliance to the stay-at-home orders. The data is aggregated from GPS pings of tens of millions of mobile devices. The R function read_distancing() available from the SafeGraphR (v 0.4.4; https://safegraphinc.github.io/SafeGraphR/index.html) package in R was used to read and aggregate the social distancing files (v2) over the study period (i.e., 140 days of mobility) and filtered to Cook County. SafeGraph defines the proportion of devices near homes as the number of devices detected in their home census block group (destination CBG = origin census block group) divided by the number of devices associated with the CBG (device count). To estimate the number of people who stay at home each day, the number of mobile devices that were completely at home was divided by the total number of devices in each CBG (i.e., completely home device count divided by the device count) [32]. The data collected by SafeGraph does not capture devices that are out of service, not moving, lack a tracking app, have opted out of location services and/or are not linked to a home CBG [34]. However, although the data only includes a subset of the total population, the data has been subjected to an exhaustive 6-step process designed to guarantee its reliability, accuracy, and external validity (see, e.g., [35–39]). During the final stages of processing, the hb_shrink function was used to perform hierarchical Bayesian shrinkage on the county-to-CBG level to improve the reliability of the estimates. SafeGraph’s stay-at-home index has been used in many studies in order to analyze the impact of mobility patterns and physical distancing after the implementation of shelter-in-place policies in the USA [35–37, 40].
The Area Deprivation Index [41] is a validated, multidimensional indicator of socioeconomic status available from the University of Wisconsin Medical School (https://www.neighborhoodatlas.medicine.wisc.edu/). The Area Deprivation Index (ADI) is comprised of 15 variables taken from the 2019 American Community Survey (ACS) 5-year estimates and includes measures such as median family income, income disparity, occupational composition, unemployment rate, family poverty rate, percentage of the population below 150% of the poverty rate, single-parent household rate, home ownership rate, median home value, median gross rent, median monthly mortgage, and household crowding. The variables were initially selected based on empirical research to approximate the material and social conditions of a community and inform health delivery and policy for disadvantaged neighborhoods [41] (see Supp Table 1). The index was constructed from factor loadings for the CBGs and factor score coefficients are used to weight the 15 indicators comprising the index [41]. The factor scale was then transformed into a standardized index with mean = 100 and standard deviation = 20. Previous research has shown that area deprivation measures are reliable and valid and perform better than individual social class in describing the extent of inequalities [41]. The ADI was downloaded at the block group level for Cook County, IL, using the R function get_adi from the sociome package (https://github.com/NikKrieger/sociome). Higher values of the ADI are indicative of more area deprivation. We included arguments to download the block group geometry and all indicators for the ADIs for Cook County (state = “IL”) for the 5-year 2019 ACS clipped the county-level data to the city of Chicago. Supplementary Table 1 provides the list of measures used in the analysis along with the median and IQR for the least (Q1 = 1st quintile) and most deprived (Q5 = 5st quintile) areas as well as the factor loadings for each variable.
Statistical Analysis
To address the research questions presented above, data summarizing fatal drug overdoses were spatially and temporally aggregated into k = 1, … K = 2526 non-overlapping areal units (i.e., CBGs). The time period of this study began at month 1 (beginning March 24, 2020, and ending on April 24, 2020) and included n = 1, … N = 5 consecutive months starting 4 days after the implementation of the stay-at-home order in the state of Illinois (which began on March 20, 2020). We considered the month as the basic time unit due to the presence of excess zeros which may provide less reliable estimates. We aggregated the total number of opioid-related overdose deaths in each census block group over the monthly period and across 5 age groups (0 to 14, 15 to 24, 25 to 44, 45 to 64 and 65 +). Population estimates were downloaded using the get_acs function of the tidycensus package using 2019 ACS 5-year estimates. The final dataset was comprised of a 12,630 (2526 × 5) rows of age standardized overdose counts aggregated to the census block group level and merged by CBG with the ADI and SafeGraph’s social distancing index.
The standardized mortality ratio (SMR) was used to measure the association between drug overdose mortality, area deprivation, and social distancing. The SMR was defined, for each CBG, as the ratio between the observed number of overdose deaths, , and the number of overdose deaths that would be expected given the age-adjusted population counts in each CBG. The expected counts were then included as an offset in our models. Moran’s I statistic was used to assess residual spatial autocorrelation and a permutation test was conducted using 20,000 random permutations of the data [42]. Next, a log-linear conditional autoregressive model was used to estimate the association between ADI and social distancing while controlling for over-dispersion, temporal autocorrelation, and spatial autocorrelation.1 Once spatial autocorrelation was established, we proceeded to our Bayesian spatiotemporal modeling. In this scenario, we assume that the observed number of overdose deaths in each CBG is a Poisson random variable and that:
where represents the random effect for CBG k and time t. Consistent with standard practice, the regression parameters were assigned independent and weakly informative priors Since the goal of the present study is to quantify the evolution of the spatial pattern in overdose risk over time, a spatially autocorrelated first-order, AR(1), autoregressive process was used for the spatio-temporal structure of the random effects [42]. In the model, both temporal and spatial autocorrelation is controlled by the mean function , and the covariance structure of , respectively [42]. Random errors in the covariance structure are modeled as spatially autocorrelated when in the adjacency matrix. The precision matrix, , corresponds to the conditional autoregressive (CAR) prior [42, 43]. We used the default prior specification for the process variance, assuming an inverse-gamma distribution for .
The modeling strategy followed a step-wise approach. First, as a baseline measure, a Poisson model that did not account for spatial heterogeneity was fit to the data. The model was then extended to include the ADI and the social distancing index separately before both variables were included in the model simultaneously. The final linear model consisted of an intercept, the area deprivation index, the social distancing index, a spatially structured CAR term, and a first order random walk-correlated time variable. Model selection was based on the lowest values of the models’ Deviance Information Criteria (DIC) and number of effective parameters. The model was implemented using the ST.CARar function available in the CARBayesST package in R [42, 44]. Following suggested approaches [42], the model was run three times to generate MCMC samples from 3 independent Markov chains. Each chain was run for 700,000 samples of which 10,000 were removed as the burnin period and the remaining were thinned by 1000. Model convergence was assessed using a variety of methods. Trace plots were examined for all three chains simultaneously. The Gelman-Rubin diagnostic was also used to quantify the multivariate potential scale reduction factor (PSRF) [45]. The PSRF takes into account the covariance structure of the parameter space and provides a single summary measure across all parameters [46]. A multivariate PSRF < 1.05 is an indication that the model converged. Finally, Geweke diagnostic values between − 2 and 2 were taken to indicate model convergence.
The average risk and posterior distribution of spatial averages were computed for each CBG and month along with the 95% credible interval (CrI). We computed a change in the mean of Y for a relative change in the ADI by multiplying the ADI coefficient by a factor q using the formula where q is the ratio of the highest to lowest quintile [47]. Finally, the posterior median risk () and exceedance probabilities associated with a drug overdose risk > 4 given the data were computed. The exceedance probability quantifies a risk that is quadruple the average risk across the city of Chicago over the 5-month period. We chose a threshold of 4 based on two considerations: (1) our initial exploratory analyses of different thresholds indicated that a big enough fraction (i.e., 69 CBGs) of the posterior distribution had thresholds above 4 and therefore indicated areas of elevated risk; and (2) to ascertain small areas that are in greatest need of intervention. To capture inequality, we computed the variation in overdose disease risk across the city as the difference in the interquartile range of overdose risk for each month.
Results
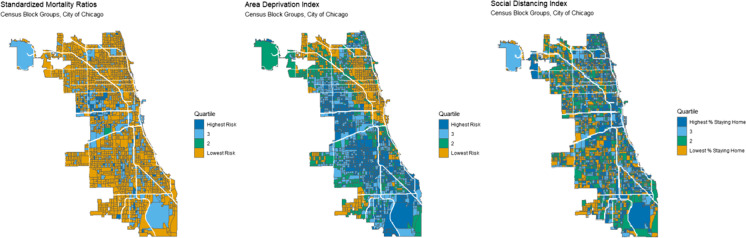
The data showed 853 opioid-related drug overdose deaths between March 24, 2020, and August 24, 2020, an average of 5.58 deaths per day. For comparison, between March 24 and April 24, 2020, drug overdoses in Chicago increased by more than 97% compared to the same time period the previous year. Table 1 shows descriptive features of key study variables. The average proportion of persons staying at home in each CBG was 0.306 (SD = 0.084) with substantial range (minimum = 0.099, maximum = 0.813). The ADI also showed significant variability across CBGs with the mean score = 104.99 (SD = 20.382). On average, the SMR was 1.189; however, more than half of CBGs had no overdose fatalities over the period. The spatial distribution of SMRs, the ADI, and the social distancing index is shown in Fig. 1. The maps demonstrate the clustering of both SMRs and ADI, as well as substantial areal overlap between the two measures. On the other hand, the social distancing index reveals a large amount of variation in the percentages of people staying at home across the time frame (see Supp Fig. 2 for a temporal distribution of the social distancing index). Figure 2 shows the bivariate distribution of overdose relative risk across quartiles of social distancing and area deprivation indices, which are on the Y and X axes, respectively. The map shows that the relative risk is highest for the most deprived CBGs regardless of the social distancing index level.
Table 1.
Descriptive characteristics of key study variables
| Population | Social distancing index | ADI | SMR | |
|---|---|---|---|---|
| Mean | 1317.783 | 0.306 | 104.989 | 1.189 |
| Median | 1141 | 0.302 | 105.621 | 0 |
| St. Dev | 834.8108 | 0.084 | 20.382 | 8.423 |
| Min | 25 | 0.099 | 43.893 | 0 |
| Max | 17,648 | 0.813 | 158.212 | 147.487 |
Population data was downloaded using the tidycensus package in R for the 2019 ACS using summary variable B01001_001 and the geography flag corresponding to the census block group (CBG). The social distancing index was downloaded from SafeGraph, Inc., and read into R using the SafeGraphR package. The Area Deprivation Index (ADI) was downloaded using the sociome package in R (function get_adi) for census block groups. The SMR is calculated as the observed number of opioid-related overdose deaths divided by the age-adjusted expected counts and aggregated to the CBG
Fig. 1.
Spatial distribution of standardized mortality ratios (SMRs), Area Deprivation Index (ADI), and the Social Distancing Index for the city of Chicago, IL. The map shows quartiles of risk for SMR and ADI variables (4 = 100th percentile, 1 = 25th percentile) and quartiles associated with the highest and lowest percentages of persons staying at home from March 24 to August 24, 2020
Fig. 2.
Conditional map of SMRs by social distancing and ADI quantiles
An overdispersed aspatial Poisson model was estimated using the observed number of overdose deaths in each CBG and the expected counts as an offset. The Moran’s I test performed on the aspatial model demonstrated significant residual spatial autocorrelation for the first 4 months (week 1: Moran’s I = 0.053, p-value < 0.001; week 2: Moran’s I = 0.029, p-value < 0.012; week 3: Moran’s I = 0.074, p-value < 0.001; week 4: Moran’s I = 0.0602, p-value < 0.001; week 5: Moran’s I = 0.016, p-value = 0.088) thereby justifying the implementation of the Bayesian spatiotemporal model.
Regarding model convergence, we examined trace plots for all three chains simultaneously, the PSRF statistic and Geweke diagnostics. The plots showed no trend in their mean or variance (see Supp. Fig. 1), the PSRF was lower than the recommended threshold of 1.05 (PSRF = 1), and all Geweke diagnostic values were within range (− 1 and 1). On this basis, a determination was made that the model achieved adequate convergence. The parameter estimates from the model (posterior median point estimate, 95% CrIs) are shown in Table 2. As shown by the table, the ADI was significantly related to drug overdose mortality risk , CrI = (0.019, 0.0363), as expected. Using the first and fourth quintiles of ADI ( and , we let q = 1.427 and calculated an increase (i.e., 1.33-fold increase) in the ADI, The result suggests that a change in ADI from quintile 4 to quintile 1 was associated with a 44.54% increase in the relative risk of an opioid-related overdose fatality. Contrary to our expectations, however, the stay-at-home index was not significantly related to overdose relative risk. Two additional findings are worth noting. First, the social distancing index was not significant in any of the models we estimated, and its inclusion did not result in significantly more of the variance in overdose mortality explained above and beyond area deprivation. Second, once the ADI and stay-at-home measures were included in the model, the residuals were no longer spatially autocorrelated (Moran’s I = − 0.02101, p = 0.9665).
Table 2.
Latent structure model — autoregressive order 1 CAR model. Posterior quantities for selected parameters and DIC
| Median | 2.5% CrI | 97.5% CrI | Geweke diagnostic | |
|---|---|---|---|---|
| Intercept | − 4.038 | − 5.175 | − 2.89 | − 0.4 |
| ADI | 0.027 | 0.019 | 0.036 | 0.7 |
| Stay-at-home | 0.683 | − 0.663 | 2.107 | 0.2 |
| 1.257 | 0.828 | 1.995 | 0.0 | |
| 0.987 | 0.962 | 0.997 | − 0.4 | |
| 0.932 | 0.795 | 0.996 | 0.0 | |
| Model diagnostics DIC = 2763.142; p.d = 210.6138; LMPL = − 1408.14 | ||||
Results from the Bayesian spatiotemporal conditional autoregressive (CAR) model of relative risk for a fatal opioid-related overdose. ADI, Area Deprivation Index; , process variance parameter; , spatial autocorrelation; , temporal autocorrelation; CrI, credible interval; DIC, Deviance Information Criterion; p.d., estimated effective number of parameters; LMPL, log marginal predictive likelihood
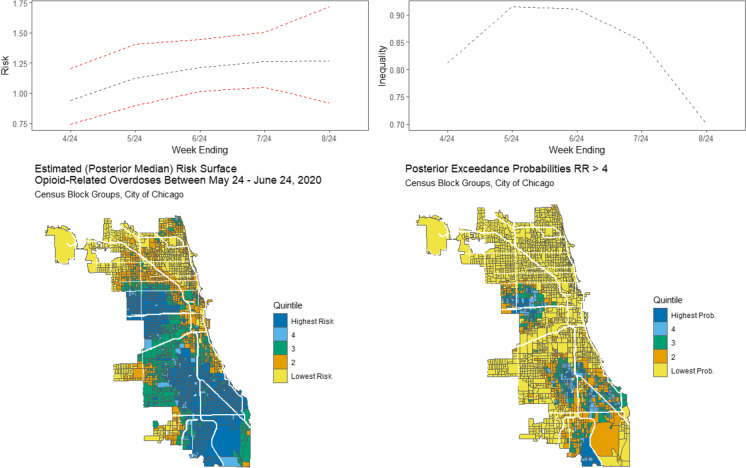
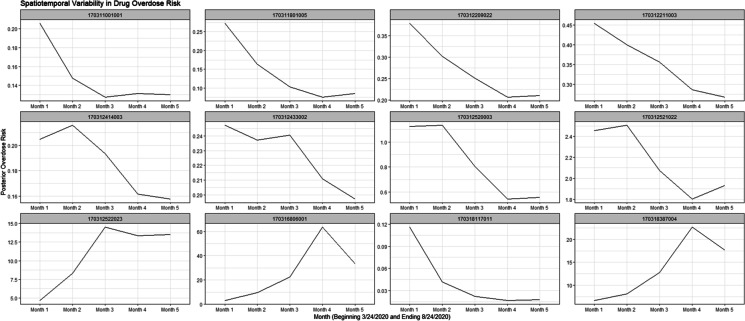
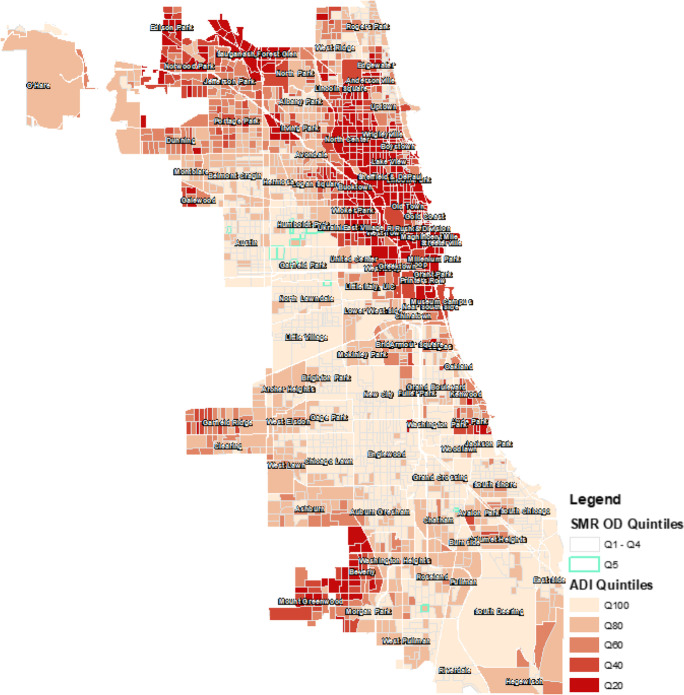
Results from the Bayesian space–time model are visually displayed in Fig. 3, panels A–D. Panel A shows a clear upward trend in drug overdose mortality risk in the 5-month period following the stay-at-home mandate. However, the trend plotted for each CBG separately shows a much different pattern, as shown by Fig. 4. Figure 4 plots the temporal trend for 12 randomly selected CBGs. Overall, the analysis demonstrated that some CBGs had a trend consistent with the overall increasing trend (increasing gradually from baseline to month 4, ending July 24, 2020) whereas some CBGs had a decreasing trend or a flat trend across the period. Regarding the temporal trend between IQR of overdose risks for each month, panel B shows that inequalities in drug overdoses increased in April, May, and June 2020 before decreasing substantially between July and August. Panel C shows the spatial risks derived from the model. About twenty-eight percent (28.7%) of census block groups had relative risks classified in the highest quintile (80th percentile). The posterior probability > 0.80 that the relative risk is at least four (4) times the whole city is shown by the map in panel D. Just over 3% of CBGs had a relative risk greater than four times the city with probability 0.80, all of which were characterized as areas of high deprivation (see Fig. 1). Figure 5 overlays the neighborhood boundaries onto the ADI quintiles and highlights the areas of highest risk. As shown by the figure, the neighborhoods with the greatest spatial and temporal increases in overdose risk included Humboldt Park, Garfield Park, Austin, North Lawndale, and Avalon Park. In these areas, the mean ADI score was 128.22 (SD = 12.75); about 31.1% of persons were staying at home on average (SD = 0.061). In contrast, in areas associated with stable risks, the mean ADI was significantly lower at 102.59 (SD = 19.80) and the average social distancing index indicated about 30.6% (SD = 0.085) of persons were staying-at-home during the 5-month period we analyzed. The spatial () and temporal ) dependence parameters indicate the strength of spatial and temporal autocorrelations (see Table 2). The spatial and temporal dependence parameters show high values ( = 0.9868; = 0.9318), indicating neighboring CBGs have a similar spatial and temporal trend in opioid-related overdoses compared to areas that are further away.
Fig. 3.
Panel A (top left): posterior median and 95% CrI for the temporal trend in opioid-related overdose fatality risk following the implementation of the stay-at-home order on March 20, 2020. Panel B (top right): estimated monthly trend in inequality in opioid-related overdose mortality risk measured by spatial interquartile range. Panel C (bottom left): estimated posterior median risk surface for month spanning May, 24, 2020–June 24, 2020, shown by quintiles (lowest risk = 20th percentile, highest risk = 80th percentile). Panel D (bottom right): estimated posterior exceedance probabilities that the risk in greater than quadruple the average risk for the whole city of Chicago. The probabilities are mapped in quintiles (lowest risk = probability < = 0.20, highest risk = probability > 0.80)
Fig. 4.
Temporal risk across 12 randomly selected CBGs. Figures illustrate differential time trends for selected CBGs. Month 1 = March 24, 2020–April 24, 2020 and month 5 = July 24, 2020–August 24, 2020
Fig. 5.
Standardized mortality ratios and Area Deprivation Index quintiles by census block group in the city of Chicago. The CBGs that are outlined in green correspond to the highest SMR quintile (Q5) or the area with the greatest risk of a fatal drug overdose. The lighter reddish-brown shading corresponds to the most deprived CBGs. The neighborhood boundaries are overlaid onto the map. The map shows that the areas associated with the highest opioid-related fatality risk are in areas of highest deprivation
Discussion
The present study is the first to explore the impact of area deprivation and social distancing on fatal drug-related overdose deaths in the city of Chicago at the neighborhood level (i.e., CBGs) during the initial months following the COVID-19 outbreak. Unlike much of the existing research on drug overdose mortality, which focuses on individual characteristics of users [48–52], our study explored the broader socio-economic context and policy environment in which overdoses occur, along with the chronosystemic element of change over time. In this regard, the present set of findings add to the current literature by examining the impact of both socio-economic disparities and COVID-19 policy responses (i.e., stay at home mandates) on drug overdose mortality controlling for area-level deprivation.
The mortality data showed 853 opioid-related drug overdose deaths between March 24, 2020, and Aug 24, 2020, an average of 5.58 deaths per day. For the sake of comparison, during the 4-week period spanning March 24–April 24, 2020, 4 days following the stay-at-home mandate, drug overdoses increased by more than 97% compared to the same time the previous year (authors’ calculations). Drug overdose inequality, which measures the variation in mortality risk across the city, increased by about 10% from baseline before decreasing to pre-pandemic levels in August 2020. This suggests that disparities in drug overdose mortality risk increased in the initial months of the pandemic before evening out in later months [42]. Our analysis also uncovered substantial spatial heterogeneity, with drug overdose deaths concentrated into the most susceptible parts of the city. Prior literature demonstrates the widely dynamic impact of socioeconomic factors on regional and temporal heterogeneity in drug overdose fatalities across both urban and rural landscapes [10, 48, 53]. Similarly, our multidimensional measure of area deprivation was strongly associated with the relative risk of a drug overdose death even after controlling for the percentage of people staying-at-home in each CBG. The CBGs with the highest relative risk overlapped substantially with areas of high deprivation (5th quintile) which comprised 464 census block groups across the city. Our results are consistent with research showing that opioid-related drug overdose deaths tend to cluster in economically stressed areas, including those with lower socioeconomic status, wealth, education, and median household income [54–57]. Importantly, however, this pattern was not observed for all opioid-related drug overdoses; rather, we observed some areas of low deprivation where drug overdose counts were higher than expected. This suggests that preventive interventions should consider how opioid overdose deaths overlap with significant inequities in social opportunity and economic inequality, as we saw in this study. For example, it may be that some overdose deaths are attributable to analgesics and/or other types of opioids including fentanyl that may be more common in highly vulnerable areas. Since this is beyond the scope of our study, it is left as a question for future research.
While it is difficult to know the reasons for the significant increase in drug overdose fatalities during COVID-19 as well as their spatial distribution across the county, the increases do coincide with policies aimed at minimizing the spread of disease. These findings, while consistent with previous reports, must be contextualized by two additional findings. First, we found no association between our CBG stay-at-home index and drug overdose risk. Nevertheless, consistent with previous research, we did find that the largest increases in drug overdoses took place between March and May 2020 which are also the months with the largest percentages of people staying-at-home. Our results caution against the assumption that stay-at-home mandates, in and of itself, fuel increases in drug fatalities, at least directly, however. Rather, our findings are more consistent with the assertion that economic hardship and inequality, lower socioeconomic status, and housing insecurity (i.e., multiple measures of marginalization and area-level deprivation) may have contributed to overdose risk and, consequently, more fatalities in the city of Chicago. Second, whereas overdose mortality trends increased in the wake of the pandemic, the increases were highly concentrated across time and space. For example, 28% of CBGs were in the highest risk quintile for drug overdose mortality and 3% of CBGs had a probability > 0.80 of experiencing an overdose relative risk that was at least four times as high as the city overall. It is important to note that many CBGs experienced no change or a decreasing trend during the months under consideration in this study. Taken together, our results suggest implementing sensitive and effective surveillance systems that promote harm reduction strategies in areas of high deprivation and/or where access may not be readily accessible or accepted. Minimizing drug overdose fatalities in such areas requires services that can reach marginalized populations, especially populations that were further ostracized during the pandemic. Future research should continue to explore the impact, if any, of COVID-19 policy prescriptions using publicly accessible and novel foot traffic data in other geographic areas and time periods. This is particularly important given that as of June 11, 2022, the pandemic continues to pose significant risk around the world.
Despite the novelty of the present study, it is not without limitation. First, our findings are limited to one city and are based on medical examiner reports, which may be incomplete. Nevertheless, the spatial and temporal characterization of these data is consistent with other studies showing similar increases during the initial months of COVID-19 while demonstrating spatial heterogeneity in the temporal trends. The medical examiner data provides the additional benefit of aggregation to the CBG level making it possible to merge it with other data such as SafeGraph’s social distancing index. Because the social distancing index does not include all devices, however, it is possible that the people whose cell phones are being tracked may not match those who are most at risk of overdose. On this basis, our failure to demonstrate an association between the stay-at-home index and opioid-related fatalities may be the result of a mismatch between the expectations of the data quality from both the index and the medical examiner reports. Nevertheless, SafeGraph’s mobility data has “tremendous potential to inform public health decision-making” and can be used to test the effectiveness of policies focused on controlling activities [45, p. 14] such as in the present study. Finally, although the ADI includes a set of comprehensive measures tapping economic hardship and inequality, socioeconomic status, and housing insecurity, our model may have omitted variables that would tend to explain more of the variance in overdose fatality risk including population density [57] and racial/ethnic heterogeneity [48]. Future research would benefit from including these indicators in models such as ours designed to assess spatiotemporal risk and exceedance probabilities in fatal drug overdoses.
Our study confirmed that overdoses are patterned by area-level deprivation, particularly economic hardship and inequality, housing insecurity, and socio-economic susceptibility rather than social distancing proxies. In this regard, our results have substantial implications for preventive interventions by suggesting that that neighborhood structural disadvantage is a long-enduring persistent predictor of drug overdose mortality and that temporary changes in population mobility as direct influences are weak. Future research should focus, as we did in the present study, on exploring the costs of policy interventions using similar data analytic and geospatial techniques to identify potential vulnerability to unintended consequences of policy interventions at local levels and assess the disparities of these impacts across racial and socioeconomic divides.
Supplementary Information
Below is the link to the electronic supplementary material.
Acknowledgements
This research was funded by a grant from the National Science Foundation 2032465.
Footnotes
For an excellent tutorial on the methods used in this paper, see Lee, D. (40). A tutorial on spatio-temporal disease risk modelling in R using Markov chain Monte Carlo simulation and the CARBayesST package. Spatial and Spatio-temporal Epidemiology, 34, 100,353.
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Paulozzi LJ. Prescription drug overdoses: a review. J Safety Res. 2012;43(4):283–289. doi: 10.1016/j.jsr.2012.08.009. [DOI] [PubMed] [Google Scholar]
- 2.Mason M, Welch SB, Arunkumar P, Post LA, Feinglass JM. Notes from the field: opioid overdose deaths before, during, and after an 11-week COVID-19 stay-at-home order—Cook County, Illinois, January 1, 2018–October 6, 2020. Morb Mortal Wkly Rep. 2021;70(10):362. 10.15585/mmwr.mm7010a3. [DOI] [PMC free article] [PubMed]
- 3.Ornell F, Moura HF, Scherer JN, Pechansky F, Kessler FHP, von Diemen L. The COVID-19 pandemic and its impact on substance use: implications for prevention and treatment. Psychiatry Res. 2020;289:113096. doi: 10.1016/j.psychres.2020.113096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Razai MS, Oakeshott P, Kankam H, Galea S, Stokes-Lampard H. Mitigating the psychological effects of social isolation during the covid-19 pandemic. BMJ. 2020;369:m1904. doi: 10.1136/bmj.m1904. [DOI] [PubMed] [Google Scholar]
- 5.Sprang G, Silman M. Posttraumatic stress disorder in parents and youth after health-related disasters. Disaster Med Public Health Prep. 2013;7(1):105–110. doi: 10.1017/dmp.2013.22. [DOI] [PubMed] [Google Scholar]
- 6.Antonio-Villa NE, Fernandez-Chirino L, Pisanty-Alatorre J, Mancilla-Galindo J, Kammar-García A, Vargas-Vázquez A, et al. Comprehensive evaluation of the impact of sociodemographic inequalities on adverse outcomes and excess mortality during the coronavirus disease 2019 (COVID-19) pandemic in Mexico City. Clin Infect Dis. 2022;74(5):785–792. 10.1093/cid/ciab577. [DOI] [PubMed]
- 7.Clark E, Fredricks K, Woc-Colburn L, Bottazzi ME, Weatherhead J. Disproportionate impact of the COVID-19 pandemic on immigrant communities in the United States. PLoS Negl Trop Dis. 2020;14(7):e0008484. doi: 10.1371/journal.pntd.0008484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Thakur N, Lovinsky-Desir S, Bime C, Wisnivesky JP, Celedón JC. The structural and social determinants of the racial/ethnic disparities in the U.S. COVID-19 pandemic. What’s our role? Am J Respir Crit Care Med. 2020;202(7):943–949. doi: 10.1164/rccm.202005-1523PP. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Alonzo D, Popescu M, Zubaroglu Ioannides P. Mental health impact of the COVID-19 pandemic on parents in high-risk, low income communities. Int J Soc Psychiatry. 2022;68(3):575–581. doi: 10.1177/0020764021991896. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Barboza GE. A spatiotemporal analysis of heroin-related calls for emergency medical services and community-health centers in Boston, Massachusetts. Appl Spat Anal Policy. 2020;13(2):507–525. doi: 10.1007/s12061-019-09315-5. [DOI] [Google Scholar]
- 11.Rudd RA, Aleshire N, Zibbell JE, Gladden RM. Increases in drug and opioid overdose deaths—United States, 2000–2014. Morb Mortal Wkly Rep. 2016;64(50 & 51):1378–1382. [DOI] [PubMed]
- 12.Macmadu A, et al. Comparison of characteristics of deaths from drug overdose before vs during the COVID-19 pandemic in Rhode Island. JAMA Netw Open. 2021;4(9):e2125538. doi: 10.1001/jamanetworkopen.2021.25538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Cerdá M, Krawczyk N, Hamilton L, Rudolph KE, Friedman SR, Keyes KM. A critical review of the social and behavioral contributions to the overdose epidemic. Annu Rev Public Health. 2021;42(1):27. doi: 10.1146/annurev-publhealth-090419-102727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Shreffler J, Shoff H, Thomas JJ, Huecker M. Brief Report: the impact of COVID-19 on emergency department overdose diagnoses and county overdose deaths. Am J Addict. 2021;30(4):330–333. doi: 10.1111/ajad.13148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.DiGennaro C, Garcia G-GP, Stringfellow EJ, Wakeman S, Jalali MS. Changes in characteristics of drug overdose death trends during the COVID-19 pandemic. Int J Drug Policy. 2021;98:103392. doi: 10.1016/j.drugpo.2021.103392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Friedman J, Akre S. COVID-19 and the drug overdose crisis: uncovering the deadliest months in the United States, January-July 2020. Am J Public Health. 2021;111(7):1284–1291. doi: 10.2105/ajph.2021.306256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Rodda LN, West KL, LeSaint KT. Opioid overdose–related emergency department visits and accidental deaths during the COVID-19 pandemic. J Urban Health. 2020;97(6):808–813. doi: 10.1007/s11524-020-00486-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Slavova S, Rock P, Bush HM, Quesinberry D, Walsh SL. Signal of increased opioid overdose during COVID-19 from emergency medical services data. Drug Alcohol Depend. 2020;214:108176. doi: 10.1016/j.drugalcdep.2020.108176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Glober N, et al. Impact of COVID-19 pandemic on drug overdoses in Indianapolis. J Urban Health Bull NY Acad Med. 2020;97(6):802–807. doi: 10.1007/s11524-020-00484-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Rossen LM, Branum AM, Ahmad FB, Sutton PD, Anderson RN. “Notes from the field: update on excess deaths associated with the COVID-19 pandemic - United States, January 26, 2020-February 27, 2021. MMWR Morb Mortal Wkly Rep. 2021;70(15):570–571. doi: 10.15585/mmwr.mm7015a4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ahmad FB, Escobedo LA, Rossen LM, Spencer MR, Warner M, Sutton P. Provisional drug overdose death counts National Center for Health Statistics. 2019. Statistics, Centers for Disease Control and Prevention (CDC)(Ed.). CDC. 2019. [Google Scholar].
- 22.Khatri UG, et al. Racial/ethnic disparities in unintentional fatal and nonfatal emergency medical services–attended opioid overdoses during the COVID-19 pandemic in Philadelphia. JAMA Netw Open. 2021;4(1):e2034878–e2034878. doi: 10.1001/jamanetworkopen.2020.34878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hou X, et al. Intracounty modeling of COVID-19 infection with human mobility: assessing spatial heterogeneity with business traffic, age, and race. Proc Natl Acad Sci. 2021;118(24):e2020524118. doi: 10.1073/pnas.2020524118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Wright AL, Sonin K, Driscoll J, Wilson J. Poverty and economic dislocation reduce compliance with COVID-19 shelter-in-place protocols. J Econ Behav Organ. 2020;180:544–554. doi: 10.1016/j.jebo.2020.10.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Fu X, Zhai W. Examining the spatial and temporal relationship between social vulnerability and stay-at-home behaviors in New York City during the COVID-19 pandemic. Sustain Cities Soc. 2021;67:102757. doi: 10.1016/j.scs.2021.102757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Block Jr R, Berg A, Lennon RP, Miller EL, Nunez-Smith M. African American adherence to COVID-19 public health recommendations. HLRP: Health Literacy Research and Practice. 2020;4(3):e166–e170. [DOI] [PMC free article] [PubMed]
- 27.Sadjadi M, Mörschel KS, Petticrew M. Social distancing measures: barriers to their implementation and how they can be overcome – a systematic review. Eur J Public Health. 2021;31(6):1249–1258. doi: 10.1093/eurpub/ckab103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Van Draanen J, Tsang C, Mitra S, Karamouzian M, Richardson L. Socioeconomic marginalization and opioid-related overdose: a systematic review. Drug Alcohol Depend. 2020;214:108127. doi: 10.1016/j.drugalcdep.2020.108127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Ghose R, Forati AM, Mantsch JR. Impact of the COVID-19 pandemic on opioid overdose deaths: a spatiotemporal analysis. J Urban Health. 2022;99(2):316–327. doi: 10.1007/s11524-022-00610-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kiang MV, et al. Sociodemographic and geographic disparities in excess fatal drug overdoses during the COVID-19 pandemic in California: a population-based study. Lancet Reg Health - Am. 2022;11:100237. doi: 10.1016/j.lana.2022.100237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Acharya A, Izquierdo A, Gonçalves S, Bates R, Taxman F, Rangwala H, et al. Exploring County-level Spatio-temporal Patterns in Opioid Overdose related Emergency Department Visits. medRxiv. 2022. [DOI] [PMC free article] [PubMed]
- 32.Cook County Medical Examiners Office. “Medical Examiner Case Archive.” Cook County Government Open Data. https://datacatalog.cookcountyil.gov/Public-Safety/Medical-Examiner-Case-Archive/cjeq-bs86. Accessed 25 Apr 2022.
- 33.Safegraph. Safegraph Social Distancing Metrics. 2020. https://www.safegraph.com/covid-19-data-consortium.
- 34.Klise K, Beyeler W, Finley P, Makvandi M. Analysis of mobility data to build contact networks for COVID-19. PLoS ONE. 2021;16(4):e0249726. doi: 10.1371/journal.pone.0249726. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Brzezinski A, Kecht V, Van Dijcke D, Wright AL. Belief in science influences physical distancing in response to covid-19 lockdown policies. University of Chicago, Becker Friedman Institute for Economics Working Paper. 2020;56(10.2139).
- 36.Kang Y, Gao S, Liang Y, Li M, Rao J, Kruse J. Multiscale dynamic human mobility flow dataset in the US during the COVID-19 epidemic. Sci Data. 2020;7(1):390. doi: 10.1038/s41597-020-00734-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Wang J, McDonald N, Cochran AL, Oluyede L, Wolfe M, Prunkl L. Health care visits during the COVID-19 pandemic: a spatial and temporal analysis of mobile device data. Health Place. 2021;72:102679. doi: 10.1016/j.healthplace.2021.102679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Guo J. The Impact of Statewide Stay-at-Home Orders: Estimating the Heterogeneous Effects Using GPS Data from Mobile Devices. Center for Research on the Wisconsin Economy, UW-Madison. 2020.
- 39.Squire RF. What about bias in the SafeGraph dataset. Safegraph. com. 2019. https://www.safegraph.com/blog/what-about-bias-in-the-safegraph-dataset. Accessed 12 Jun 2022.
- 40.Levin R, Chao DL, Wenger EA, Proctor JL. Cell phone mobility data and manifold learning: Insights into population behavior during the COVID-19 pandemic. medRxiv. 2020. [DOI] [PMC free article] [PubMed]
- 41.Singh GK. Area deprivation and widening inequalities in US mortality, 1969–1998. Am J Public Health. 2003;93(7):1137–1143. [DOI] [PMC free article] [PubMed]
- 42.Lee D. A tutorial on spatio-temporal disease risk modelling in R using Markov chain Monte Carlo simulation and the CARBayesST package. Spat Spatio-Temporal Epidemiol. 2020;34:100353. doi: 10.1016/j.sste.2020.100353. [DOI] [PubMed] [Google Scholar]
- 43.Leroux BG, Lei X, Breslow N. Estimation of disease rates in small areas: a new mixed model for spatial dependence. In Statistical models in epidemiology, the environment, and clinical trials. Springer, New York. 2000, pp. 179–191.
- 44.Lee D, Rushworth A, Napier G. Spatio-temporal areal unit modeling in R with conditional autoregressive priors using the CARBayesST package. J. Stat. Softw. 2018;84:1–39. doi: 10.18637/jss.v084.i09. [DOI] [Google Scholar]
- 45.Brooks SP, Gelman A. General methods for monitoring convergence of iterative simulations. J Comput Graph Stat. 1998;7(4):434–455. doi: 10.2307/1390675. [DOI] [Google Scholar]
- 46.Spannaus A, Papamarkou T, Erwin S, Christian JB. Bayesian state space modelling for COVID-19: with Tennessee and New York case studies. arXiv preprint arXiv:2012.15306. 2020.
- 47.Barrera-Gómez J, Basagaña X. Models with transformed variables: interpretation and software. Epidemiol Camb Mass. 2015;26(2):e16–17. doi: 10.1097/EDE.0000000000000247. [DOI] [PubMed] [Google Scholar]
- 48.Barboza GE, Angulski K. A descriptive study of racial and ethnic differences of drug overdoses and naloxone administration in Pennsylvania. Int J Drug Policy. 2020;78:102718. doi: 10.1016/j.drugpo.2020.102718. [DOI] [PubMed] [Google Scholar]
- 49.Pabayo R, Alcantara C, Kawachi I, Wood E, Kerr T. The role of depression and social support in non-fatal drug overdose among a cohort of injection drug users in a Canadian setting. Drug Alcohol Depend. 2013;132(3):603–609. doi: 10.1016/j.drugalcdep.2013.04.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Richer I, Bertrand K, Vandermeerschen J, Roy É. A prospective cohort study of non-fatal accidental overdose among street youth: the link with suicidal ideation. Drug Alcohol Rev. 2013;32(4):398–404. doi: 10.1111/dar.12003. [DOI] [PubMed] [Google Scholar]
- 51.Sherman SG, Cheng Y, Kral AH. Prevalence and correlates of opiate overdose among young injection drug users in a large U.S. city. Drug Alcohol Depend. 2007;88(2–3):182–187. doi: 10.1016/j.drugalcdep.2006.10.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Tobin KE, Latkin CA. The relationship between depressive symptoms and nonfatal overdose among a sample of drug users in Baltimore, Maryland. J Urban Health Bull NY Acad Med. 2003;80(2):220–229. doi: 10.1093/jurban/jtg025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Keyes KM, Cerdá M, Brady JE, Havens JR, Galea S. Understanding the rural–urban differences in nonmedical prescription opioid use and abuse in the United States. Am J Public Health. 2014;104(2):e52–e59. doi: 10.2105/AJPH.2013.301709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Grol-Prokopczyk H. Use and opinions of prescription opioids among Older American adults: sociodemographic predictors. J Gerontol Ser B. 2019;74(6):1009–1019. doi: 10.1093/geronb/gby093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Palombi L, Hawthorne AN, Irish A, Becher E, Bowen E. ‘One out of ten ain’t going to make it’: an analysis of recovery capital in the Rural Upper Midwest. J Drug Issues. 2019;49(4):680–702. doi: 10.1177/0022042619859309. [DOI] [Google Scholar]
- 56.Visconti AJ, Santos G-M, Lemos NP, Burke C, Coffin PO. Opioid overdose deaths in the city and county of San Francisco: prevalence, distribution, and disparities. J Urban Health Bull NY Acad Med. 2015;92(4):758–772. doi: 10.1007/s11524-015-9967-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Maroko AR, Nash D, Pavilonis BT. COVID-19 and inequity: a comparative spatial analysis of New York City and Chicago hot spots. J Urban Health. 2020;97(4):461–470. doi: 10.1007/s11524-020-00468-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.