ABSTRACT
Down syndrome (DS) is a neurodevelopmental disorder of known genetic cause, with a wide array of oral and systemic manifestations. The aim of the present study is to determine the level of oral hygiene status and practice of a group of individuals with DS in Benghazi/Libya. In this cross–sectional study 124 individuals were recruited from The Rehabilitation Centre of Special Needs in the city of Benghazi, Libya. Questionnaires were distributed among the attendees, covering oral health aspects and diet habits. Oral examination was conducted to evaluate oral health status among individuals with DS. The data were analysed descriptively and inferentially (including Chi-square test and Fisher’s exact test) using the Statistical Package for Social Science version 20 (SPSS). Most of DS individuals brush their teeth once daily (62%), spending less than one minute in brushing (44%). For diet habits, more than half (55%) eat sweet snacks between meals. For the dental status, 47% of the subject had zero DMFT, followed by score 2 in 21%. The highest percentage in Oral hygiene Index (OHI) was scored 1 by 46% of participants. The zero CPITN score was seen in 54.5%. Our results have shown a weaker tendency of DS towards oral hygiene. This should strengthen our goal of guiding and encouraging parents of individuals with DS to be more cautious in providing help and supervision of their individuals’ practice of oral health care.
KEYWORDS: Down syndrome, oral health, questionnaire, Libya
1. Introduction
Down syndrome (DS) is the most common neurodevelopmental disorder of known genetic cause, with an incidence of between 1:750 and 1:1000 live births. DS has usually been described simply as arising from an extra copy of chromosome 21 [1].
Down’s syndrome is characterized by certain physical, mental, and medical features. A number of these features, such as learning disability, cardiac anomalies and an altered immune system can have a profound effect on oral health and the delivery of oral care [2]. In DS, systemic dysfunction manifested by immunological deficiencies predispose the individual to oral infections, which in turn aggravate systemic diseases [2–5].
Many of the studies assessing the oral health status of individuals with DS reveal that they have midfacial abnormality, narrow palate, macroglossia as well as delayed teeth eruption, missing and malformation in tooth morphology. In addition, such individuals with oro-facial disorders may have high risk of developing oral health problems such as periodontal disease, malocclusion, and dental caries [6–10].
Normal development of the oral structures is altered (decreased tooth size, altered crown shape, delayed eruption and hypodontia) and function is impaired leading to compromised development of suckling, swallowing, chewing, mastication and speech difficulties [11]. Systemic dysfunction (i.e. immunological deficiencies) that affects individuals with Down syndrome may also predispose them to oral diseases and disorders that may in turn aggravate systemic diseases.
Periodontal disease in DS is a considerably more common and serious problem than caries, where it has been demonstrated in as many as 90% of this specific population [9].
Scientific evidence of susceptibility to dental caries in the population with DS is limited and conflicting, making it difficult to establish firm conclusions [11,12].
On the other hand, a smaller number of studies have highlighted an equivalent or higher prevalence of caries in individuals with DS. According to these studies, some local factors acting as determinants of caries (difficulty of access to dental care, poor dietary habits, use of drugs for severe infections of the upper airways, reduced manual dexterity, poor oral hygiene, parental neglect) override ‘protective factors’ (such as the buffer capacity of saliva, bruxism, diastema, agenesis and microdontia) [3,13–15].
Many of the medical and physiological characteristics of DS have direct connection to the oral health of subjects affected, which in turn have indirect consequences towards their quality of life and care [16].
Although the link between oral health and individuals’ wellbeing and quality of life (QoL) [17,18] is well established, research focusing specifically on individuals with Down syndrome is limited [19,20]. However, some studies investigated the relation of oral disorders with oral symptoms (such as pain, discomfort, or difficulty chewing and mastication) along with systemic impacts on nutrition and digestion, which can have broader effects on QoL including social interactions, speech difficulties and emotional status [20–22].
Evidence has showed that poor oral health status can be affected by improper ways of practice. In this regard, oral hygiene practices are voluntary physical activities that have at least two requirements: motivation and manual dexterity [23]. Thus, poor oral hygiene tends to be more prevalent among people with special needs compared to normal individuals. This is apparently due to their deficient oral hygiene practice, medication side effects and lack of cooperation in dental treatments [24].
Therefore, the caregiver of DS individuals should have a proper awareness of oral hygiene practice for taking care of their individuals’ teeth, thus improving their oral health status [25].
It seems necessary to address the oral health problems of DS individuals and their oral health-care practices, thereby assessing the individual needs of preparing dental health education programs for them as a step to improve their oral health status.
The aim of this study is to assess the oral health-care practices and oral health problems among individuals with DS in Benghazi, Libya, since no such study has, up to the best of our knowledge, been conducted before in this country.
2. Materials and methods
The target group was selected from special needs institution (Rehabilitation Centre) in the city of Benghazi, Libya.
The review board of Faculty of Dentistry, Benghazi University, has approved the study. The purpose and objectives of the study were explained to administration staff of the institution, thereby securing their approval for conducting the study. The aim of the study was explained to the caregivers and guardians of the individuals with DS, stressing on the confidentiality of the provided information for this research.
3. Sample selection
All individuals with DS were selected from the institution. The guardians were asked to participate in the study by filling a questionnaire distributed by the principals of the institutions. Consent and permission for examination were obtained from guardians and from the institutions to collect the demographic data and oral health status.
At the time of conducting this study, a total of 124 individuals diagnosed with Down syndrome (ages range between 6 and 30 years) (Table 1) were selected as study participants.
Table 1.
Ages of DS participants.
| Age group | percentage |
|---|---|
| 6 − 12 | 59.8% |
| 13–18 | 20.8% |
| ≥19 | 19.4% |
Behavior management was not a problem as DS individuals tend to be warm and well behaved. For those who were stubborn or uncooperative, they were given a little extra time and attention to feel comfortable.
4. Design of the study
The study is cross-sectional and descriptive nature. A pilot study was done to ensure the clearance, reliability, and validity of the questionnaires.
The first section included a questionnaire which covered the following areas: socio-demographic information such as age and gender of the individual with DS; mothers’ age, educational level, and occupational status (Table 2). It also included questions regarding the oral health-care practices, such as use of tooth brushing (frequency and type); dietary habits such as the type of snacks between meals; and the frequency of sweets intake. It also asked about their dental visit, for example, last time of visit, frequency, and barriers of dental visit.
Table 2.
DS mothers’ educational level and employment.
| Variable | Number | Percentage (%) |
|---|---|---|
|
||
| low | 16 | 12.9 |
| Undergraduate | 53 | 42.7 |
| Graduate | 55 | 44.4 |
|
||
| Working | 58 | 54.8 |
| Non-working | 68 | 45.2 |
The second section included intra-oral examination to evaluate oral health status among individuals with DS. Two dentists (first and second authors of this manuscript) who had been previously trained and calibrated (kappa = 0.9) conducted dental examinations under natural lighting conditions, with the aid of a dental mirror, CPITN periodontal probe and a 5 cm × 5 cm gauze square. All participants were examined following a standardized dental examination format.
For dental caries, WHO criteria were used to assess all teeth for the presence of caries. Both visual and tactile criteria were used, and the teeth scored as sound, decayed, or filled WHO [26]. The periodontal health was evaluated using CPITN.
Oral hygiene of individuals with DS was evaluated using the Simplified Oral Hygiene Index (OHI-S) by Greene and Vermillion. This index has two components: the debris index (DI-S) and the calculus index (CI-S), and both indices were measured on four posterior teeth and two anterior teeth. The DI-S and CI-S assessed for the OHI-S were examined on the labial surfaces of 11, 16, 26, and 31, and the lingual surfaces of 36 and 46. The OHI-S was assessed using disposable instruments, a periodontal probe, and artificial light. The criteria for classifying debris are 0 = no debris on the tooth surface; 1 = soft debris covering not more than one-third of the tooth surface or presence of extrinsic stain without debris in the tooth surface; 2 = soft debris covering more than one-third, but not more than two-thirds of the tooth surface; and 3 = soft debris covering more than two-thirds of the tooth surface. The debris scores are summed up and divided by the number of teeth scored to obtain the DI-S. At least two of the six teeth must be examined to calculate the score. The same methods are used to obtain the CI-S. The DI-S and the CI-S are summed up to obtain the OHI – S
Abnormalities of teeth, including developmental defects affecting size, eruption, shape, number, structure, and color of the tooth were noted. Occlusion abnormalities such as cross bite, open bite, rotation, and crowding were also observed. Any acquired abnormalities affecting tooth was also given consideration during the examination.
5. Statistical analysis
The distributions of selected questionnaire-based variables were studied and described. The association of tooth brushing frequency and mother’s educational levels along with occupational status were examined using chi-square test. If the assumptions for such significance were confirmed, such associations would be further evaluated with Fisher’s exact test. The level of statistical significance was p < 0.05. The statistical analysis was dine using SPSS statistical software version 23.0 (SPSS. Inc., Chicago, IL, USA).
6. Results
The results of this study can be categorized into two main levels: questionnaire-based and oral examination-based. The participants were classified according to their age into three age groups; Group I (6 − 12 years: 59.8%); group II (13–18 years: 20.8%) and group III (≥19 years: 19.4%). Males were more than females (58% vs. 42%). The most common systemic disease was congenital heart defects seen in 24%. Less than half of the subjects’ mothers were university graduates (44%) and more than half are working (55%). The great majority of subjects (91%) brush their teeth at least once a day (62%), with the brushing as the only cleansing method (65%) (Table 3).
Table 3.
DS dental brushing habit.
| Variable | Percentage (%) |
|---|---|
|
|
| Yes | 91.1 |
| No | 8.9 |
|
|
| Child | 49.6 |
| Older sibling | 19.4 |
| Parent | 31.0 |
|
|
| Yes | 92.9 |
| No | 7.1 |
|
|
| Fluoridated | 33.6 |
| Non-fluoridated | 8.0 |
| Don’t know | 58.4 |
|
|
| Once a day | 62.8 |
| 2 times a day | 24.8 |
| 3 times | 3.5 |
| Don’t know | 8.8 |
|
|
| Hard-bristled | 1.8 |
| Medium-bristled | 46 |
| Soft-bristled | 31 |
| Don’t know | 21.2 |
|
|
| Interdental cleaning aids such as dental floss | 1.6 |
| Water only | 64.8 |
| Gauze | 1.6 |
| Meswak | 5.7 |
| Don’t know | 26.2 |
For the diet habits, more than half (55%) eat sweet snacks between meals, and not much less than this (45%) consume sweet drinks a least one time daily. About 83% of the subjects visit a dentist, and of those more than half do the visit once in more than a year (58%), in other words 44% of DS subjects attend a dental care. Toothache was the main driving factor for urging the subjects to seek dental care (47%). The main reason from the subjects’ perspective of avoiding of dental care is fear of needle and drill (31%).
Oral examination revealed that 47% of the subjects had zero DMFT, followed by score 2 in 21% (Figure 1). The mean and STD of DMFT was 2.02 ± 2.9. For primary teeth dmft, 62.3% of children did not have any finding, that is, score zero, followed by score 4 in 9.8% (Figure 2).
Figure 1.
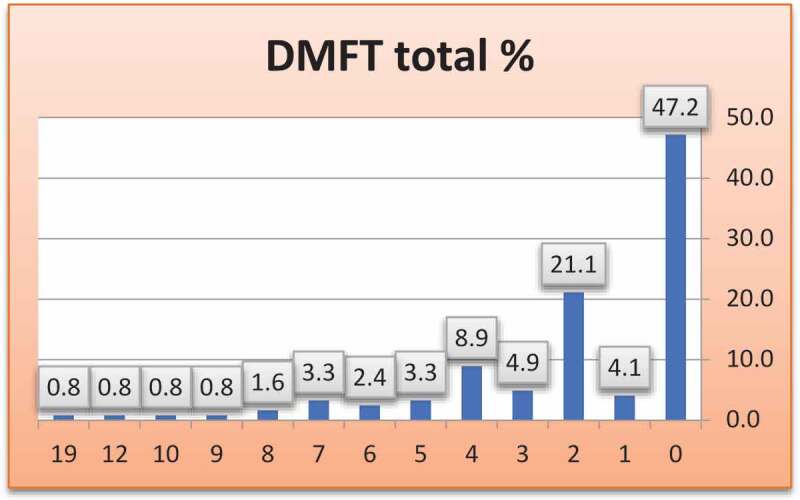
DMFT index among the study participants.
Figure 2.
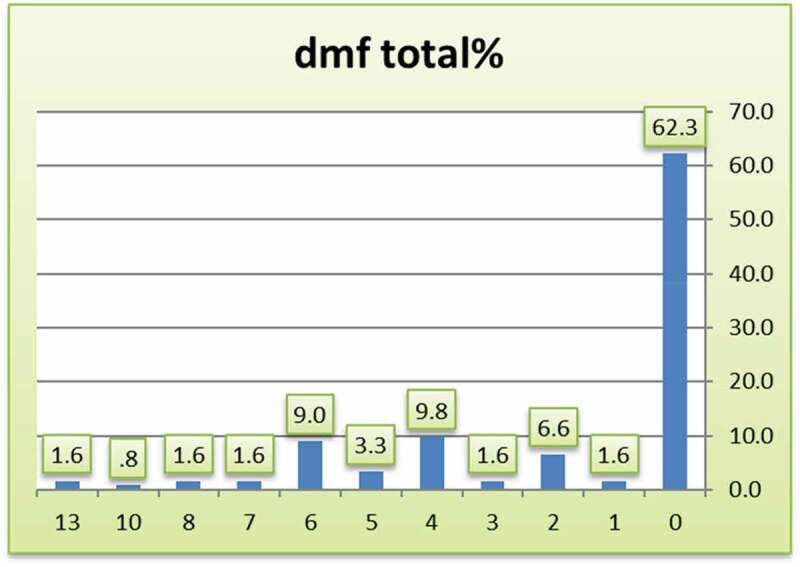
Dmft index of primary teeth in DS children.
The highest percentage in OHI-S was score 1 by 46% of participants (Figure 3), with a mean of 1.6 ± 0.9. For CPITN more than half of the group had a zero level (54%), mean of 0.8 ± 1.1.
Figure 3.

Oral hygiene index (OHI) among the participants.
In terms of oral pathological findings, most of the subjects (more than 80%) did not show any oral lesions, neither in dental structures nor in soft tissues. No statistical significance was found in the association of mothers’ education with frequency of toothbrushing.
7. Discussion
The study investigated the oral hygiene status and practice of a group of individuals with DS in the city of Benghazi, Libya. A few articles about DS in Libya are found in the literature. DS arises due to an extra copy of chromosome 21, which can lead to characteristic abnormal features in the facial region such as macroglossia, low muscle tone beside short stature and intellectual incapacity [1]. Oral health issues are of special concern and represent a major problem for these individuals compared to the general population. High rates of periodontal disease, dental caries, missing teeth, prolonged retention of primary teeth, supernumerary teeth, and malocclusion are all indicators of reduced oral health in this population [27]. Therefore, assessment of oral hygiene status and practice of this group is a basic requirement in preparing dental health education programs for such patients to improve their oral health status.
The American Dental Association (ADA) states that using of toothbrush is an important aspect in the maintenance of oral health and recommends the habit of brushing at least twice daily to clean the teeth and prevent dental caries [28]. In this regard, our study showed that over than half of the participants (62.8%) brushed their teeth once a day. This rate higher than the findings reported in Saudi Arabia [24], where they reported that about 28.3% of them use toothbrush once daily. Such low rate in the brushing frequency can be attributed to insufficient awareness of caregivers of the tooth brushing importance inn dental cleaning and controlling of plaque formation.
In our study, about 31% of the individuals received parental help in brushing their teeth, obviously less than the rate reported by Al-hussyeen and Al-sadhan, which was 60% [24]. The difference in the reported rates might reflect negative attitudes and less awareness of parents towards improving oral hygiene of their DS individuals.
The prevalence of caries in our sample represented by DMFT index showed that about half of the sample have caries-free dentition, which is lower than in many reported figures, for example, in Yemen 93.8% of DS individuals had dental caries [29]. Our findings are consistent with a meta-analysis showing that DS people tend to have lower levels of dental caries [30], which can be explained by the high percentage of practicing tooth brushing and frequent dental visits. The awareness of oral hygiene is essential in maintaining healthy dentition and that was reasonably better in our study compared to the findings of caries index study conducted two decades ago from the same city [31].
Besides the systemic problems, DS individuals have reduced manual dexterity which could lead to impairment in conducting their routine of oral hygiene practice, therefore; they often need assistance from caregivers, for example, parents, or siblings.
Despite the intellectual and physical obstacles in conducting the routine measures of oral hygiene of DS people, a high percentage of DS subjects brush their teeth (91%), which is considerably higher than what has been reported in some previous studies, for example, 59.4% in Yemen [32], 77.7% in Jordan [33], while it was similar to those in Australia (90%) [34].
In the developing world examination visits of DS individuals are often tedious due to many reasons, for example, lack of sufficient education of parents about the importance of oral hygiene, fewer number of dental clinics offering free treatments for DS individuals. People with DS and those with any type of mental or physical restraints have the right to full access to dental treatment in the same way as normal people have [35]. In our study, the number of these individuals is high, probably reflecting the relatively high number of educated parents especially mothers. In this regard, the study by Al-Sufyani et al., only 2% of their DS individuals were regular attenders of dental clinic, although they did not specify how often this ‘regularity’ is. According to Descamps I, 66% of DS individuals had a dental visit during the previous six months [36].
DS people are known to suffer from more severe periodontal diseases compared with normal people, owing to the unique composition of their subgingival plaque and higher bacterial profile of periodontopathic bacteria [37]. Beside the microbial role, an altered immune response of higher production of destructive enzymes, for example, matrix metalloproteinases contribute to the degradation of the periodontium [38].
In this regard, the OHI was scored 1 by about third of the participants, relatively lower than what was found in India (2.24) [39], or Croatia where the lower range of OHI was 3.8 [40].
To conclude, our study has shown a reasonable level of oral hygiene status in DS subjects, apparently not as poor as reported in other studies. Nevertheless, such findings dictate the necessity to pay more attention to the need of this minority of people in terms of supervising their oral health habits and providing dental care.
Funding Statement
The author(s) reported there is no funding associated with the work featured in this article.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Clinical relevance
Scientific rationale for study: People with DS express less mental and physical abilities in terms of taking care of their oral hygiene.
Principal findings: Our inclusion of mothers’ education and diet habits sheds some light on the roles of such important parameters in developing a clinical strategy to evaluate and improve the oral hygiene status of DS people’s.
Practical implications: The findings of our study should formulate a preventive program whereby proper toothbrushing and dental flossing are demonstrated to this small group of population.
References
- [1].Karmiloff-Smith A, Al-Janabi T, D’Souza H, et al. The importance of understanding individual differences in Down syndrome. F1000Res. 2016;5:389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Fiske J, Shafik HH.. Down’s syndrome and oral care. Dent Update. 2001;28(3):148–7. [DOI] [PubMed] [Google Scholar]
- [3].Hennequin M, Faulks D, Veyrune J-L, et al. Significance of oral health in persons with Down syndrome: a literature review. Dev Med Child Neurol. 1999;41(4):275–283. [DOI] [PubMed] [Google Scholar]
- [4].Bosch JJ. Health maintenance throughout the life span for individuals with Down syndrome. J Am Acad Nurse Pract. 2003;15(1):5–17. [DOI] [PubMed] [Google Scholar]
- [5].Van-Trotsenburg AS, Heymans HS, Tijssen JG, et al. Comorbidity, hospitalization, and medication use and their influence on mental and motor development of young infants with Down syndrome. Pediatrics. 2006;118(4):1633–1639. [DOI] [PubMed] [Google Scholar]
- [6].Desai SS, Fayetteville NY. Down syndrome: a review of the literature. Oral Surg, Oral Med, Oral Pathol, Oral Radiol, Endodontol. 1997;84(3):279–285 [DOI] [PubMed] [Google Scholar]
- [7].Macho V, Palha M, Macedo AP, et al. Comparative study between dental caries prevalence of Down syndrome children and their siblings. Spec Care Dentist. 2013;33(1):2–7. [DOI] [PubMed] [Google Scholar]
- [8].Macho V, Coelho A, Areias C, et al. Craniofacial features and spe‐ cific oral characteristics of Down syndrome children. Oral health dental manage‐ ment. 2014;13(2):408–411. [PubMed] [Google Scholar]
- [9].Cichon P, Crawford L, Grimm WD. Early-onset periodontitis associated with Down’s syndrome–clinical interventional study. Ann Periodontol. 1998;3(1):1633–1639. [DOI] [PubMed] [Google Scholar]
- [10].Almas K, Bulman JS, Newman HN. Assessment of periodontal status with CPITN and conventional periodontal indices. J Clin Periodontol. 1991;18(9):654–659. [DOI] [PubMed] [Google Scholar]
- [11].Allison PJ, Hennequin M, Faulks D. Dental care access among individuals with Down syndrome in France. Spec Care Dentist. 2000;20(1):28–34. [DOI] [PubMed] [Google Scholar]
- [12].Fung K, Lawrence H, Allison P. A paired analysis of correlates of dental restorative care in siblings with and without Down syndrome. Spec Care Dentist. 2008;28(3):85–91. [DOI] [PubMed] [Google Scholar]
- [13].Cornejo LS, Zak GA, Dorronsoro de Cattoni ST, et al. Bucodental health condition in patients with Down syndrome of Cordoba City, Argentina. Acta Odontol Latinoam. 1996;9(2):65–79. [PubMed] [Google Scholar]
- [14].Oredugba FA. Oral health condition and treatment needs of a group of Nigerian individuals with Down syndrome. Downs Syndr Res Pract. 2007;12(1):72–76. [DOI] [PubMed] [Google Scholar]
- [15].Asokan S, Muthu MS, Sivakumar N. Dental caries prevalence and treatment needs of Down syndrome children in Chennai, India. Indian J Dent Res. 2008;19(3):224–229. [DOI] [PubMed] [Google Scholar]
- [16].Shapira J, Stabholz A. A comprehensive 30-month preventive dental health program in a pre-adolescent population with Down’s syndrome: a longitudinal study. Spec Care Dentist. 1996;16(1):33–37. [DOI] [PubMed] [Google Scholar]
- [17].Sheiham A. Oral health, general health and quality of life. Bull World Health Organ. 2005;83(9):644. [PMC free article] [PubMed] [Google Scholar]
- [18].Benyamini Y, Leventhal H, Leventhal EA. Self-rated oral health as an independent predictor of self-rated general health, self-esteem and life satisfaction. Soc Sci Med. 2004;59(5):1109–1116. [DOI] [PubMed] [Google Scholar]
- [19].AlJameel AHM. The Development and testing of an oral health-related quality of life measure for children/adolescents with down syndrome (OH-QOLADS). Unpublished. Ph.D. Thesis, University College London, London UK, 2016 [Google Scholar]
- [20].AlJameel AH, Watt RG, Tsakos G, et al. Down syndrome and oral health: mothers’ perception on their children’s oral health and its impact. J Patient-Rep Outcomes. 2020;4(1):1–8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Oliveira AC, Pordeus IA, Luz CL, et al. Mothers’ perceptions concerning oral health of children and adolescents with Down syndrome: a qualitative approach. Eur J Paediatr Dent. 2010;11(1):27–30. [PubMed] [Google Scholar]
- [22].Amaral-Loureiro AC, Oliveira Costa F, Eustáquio da Costa J. The impact of periodontal disease on the quality of life of individuals with Down syndrome. Downs Syndr Res Pract. 2007;12(1):50–54 [DOI] [PubMed] [Google Scholar]
- [23].Tesini DA. Age, degree of mental retardation, institutionalization, and socioeconomic status as determinants in the oral hygiene status of mentally retarded individuals. Community Dent Oral Epidemiol. 1980;8(7):355–359. [DOI] [PubMed] [Google Scholar]
- [24].Al-hussyeen A, Al-sadhan S. Oral hygiene practices and dietary habits among children with Down’s syndrome in Riyadh, Saudi Arabia. Saudi Dental J. 2006;18(3):141–142. [Google Scholar]
- [25].Sheiham A, Watt RG. The common risk factor approach: a rational basis for promoting oral health. Community Dent Oral Epidemiol. 2000;28(6):399–406. [DOI] [PubMed] [Google Scholar]
- [26].WHO . Targets for health for all. Copenhagen: World Health Organisation Regional Office for Europe; 1986. [Google Scholar]
- [27].Sandeepa NC, Al Hagbani SA, Alhammad FA, et al. Oral health status of Down’s syndrome patients in Aseer, Saudi Arabia. J Pharm Bioall Sci. 2021;13(5):656–659 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [28].ADA recommendations for toothbrushes . Prepared by Department of Scientific Information, Evidence Synthesis & Translation Research, ADA Science & Research Institute, LLC. 2019. [Google Scholar]
- [29].Al-Maweri S, Al-Sufyani G. Dental caries and treatment needs of Yemeni children with down syndrome. Dent Res J (Isfahan). 2014;11(6):631–635. [PMC free article] [PubMed] [Google Scholar]
- [30].Deps TD, Angelo, GL, Martins, CC, Paiva, SM, Pordeus, IA, Borges-Oliveira, AC. Association between dental caries and Down syndrome: a systematic review and meta-analysis. PLoS One. 2015;10(6):e0127484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [31].al-Sharbati MM, Meidan TM, Sudani O. Oral health practices and dental caries among Libyan pupils, Benghazi (1993-94). East Mediterr Health J. 2000;6(5–6):997–1004. [PubMed] [Google Scholar]
- [32].Al-Sufyani, Ghada A, Al-Maweri, SA, Al-Ghashm, AA, Al-Soneidar, WA. Oral hygiene and gingival health status of children with Down syndrome in Yemen: a cross-sectional study. J Int Soc Prev Community Dent. 2014;4(2):275–283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [33].Al Habashneh R, Al-Jundi, S, Khader, Y, Nofel, N . Oral health status and reasons for not attending dental care among 12- to 16-year-old children with Down syndrome in special needs centres in Jordan. Int J Dent Hyg. 2012;10(4):259–264. [DOI] [PubMed] [Google Scholar]
- [34].Randell DM, Harth S, Seow WK. Preventive dental health practices of non-institutionalized Down syndrome children: a controlled study. J Clin Pediatr Dent. 1992;16(3):225–229. [PubMed] [Google Scholar]
- [35].Abdul Rahim FS, Mohamed AM, Marizan Nor M, et al. Dental care access among individuals with Down syndrome: a Malaysian scenario. Acta Odontol Scand. 2014;72(8):999–1004. [DOI] [PubMed] [Google Scholar]
- [36].Descamps I, Marks LA. Oral health in children with Down syndrome: parents’ views on dental care in Flanders (Belgium). Eur J Paediatr Dent. 2015;16(2):143–148. [PubMed] [Google Scholar]
- [37].Sakellari D, Arapostathis K, Konstantinidis A. Periodontal conditions and subgingival microflora in Down syndrome patients. A case-control study. J Clin Periodontol. 2005;32(6):684–690. [DOI] [PubMed] [Google Scholar]
- [38].Tsilingaridis G, Yucel-Lindberg, T, Quezada, HC, Modéer, T . The relationship between matrix metalloproteinases (MMP-3, −8, −9) in serum and peripheral lymphocytes (CD8 +, CD56 +) in Down syndrome children with gingivitis. J Periodontal Res. 2014;49(6):143–148. [DOI] [PubMed] [Google Scholar]
- [39].Makkar A, Indushekar KR, Saraf BG, et al. A cross sectional study to evaluate the oral health status of children with intellectual disabilities in the National Capital Region of India (Delhi-NCR). J Intellect Disabil Res. 2019;63(1):31–39. [DOI] [PubMed] [Google Scholar]
- [40].Ivancic Jokic N, Majstorović M, Bakarcić D, et al. Dental caries in disabled children. Coll Antropol. 2007;31(1):321–324. [PubMed] [Google Scholar]


