Abstract
Background: Coronavirus Disease (COVID-19) pandemic can affect mental health. Heads of the household are at higher risk of this effect because of their financial and social responsibilities. This study aimed to assess the psychological well-being and its associated factors during the COVID-19 pandemic among heads of households in Pakistan.
Methods: We conducted an online survey in May 2020. A convenience sampling strategy was used to enroll the heads of the households from all regions of Pakistan. A validated English and Urdu version of the WHO-5 well-being scale was used to assess well-being. The prevalence of poor well-being and its associated factors among heads of the households was measured using logistic regression.
Results: A total of 509 heads of households participated in the survey. About 35% of the participants were dependent on financial sources other than salary. The news was considered a source of fear as 70% assumed that avoiding such news may reduce the fear. The most common coping strategies used during lockdown were; spending quality time with family, eating healthy foods, adequate sleep and talking to friends on the phone. The prevalence of poor well-being was found to be 41% (95% CI: 36.62-45.51). Individuals with any chronic illness were at a higher risk of poor wellbeing adjusted odds ratio of 1.64 (95% CI: 1.04–2.59). Worriedness was also found to be associated with a higher risk of poor wellbeing adjusted OR 1.13 (95% CI: 1.06–1.19). Reading books showed a protective association with poor mental wellbeing adjusted OR 0.64 (95% CI: 0.42–0.98).
Conclusion: There was a high prevalence of poor mental wellbeing among heads of households in Pakistan. Worriedness related to the pandemic and having chronic illness were significant predictors of poor psychological wellbeing. Actions are required in the form of targeted mass psychological support systems for the heads of the families to improve their mental health during the COVID-19 crises.
Keywords: COVID-19, Mental Health, Psychological, Well-Being, Head of Household, Pakistan
Introduction
↑What is “already known” in this topic:
• COVID-19 pandemic has led to social and economic crises across the globe
• Mental health of front-line health care workers is severely affected by the pandemic
• There are widespread fears related to COVID-19 disease itself and preventive measures such as lockdowns on the general population.
→What this article adds:
• There is a high prevalence of poor mental well-being among the heads of the households
• Fears and worries related to COVID-19 are widely prevalent, and spending time with family is the most common coping strategy
• Worriedness and having the chronic disease are significant predictors of poor mental well-being among heads of households.
Coronavirus Disease (COVID-19) has been declared as a global pandemic (1). COVID-19 is not only detrimental to the physical health of the people but also poses a serious risk to the psychological state of the general population (2). Psychological and mental health refers to the state of people in which they realize their own ability to cope with life stressors (3).The drastic increase in mortality rate, high virulence and rapid transmission during a pandemic creates havoc. This may lead to fear, anxiety, depression, Post-Traumatic Stress Disorder, adjustment disorder or any other active psychiatric disorders in the general population (4).
This novel coronavirus has affected almost all the territories globally, and millions of people have suffered from the disease (5). The general population was advised by the experts to stay in self-isolation and quarantine, practice social distancing, limit their mobility and stay at home (6). Pakistan was in a state of high alert after the first case was reported on February 26, 2020 (7). Given the rapid increase in the number of cases and local transmission of COVID-19 in Pakistan, a nationwide lockdown was announced by the government of Pakistan which started on 22nd and 23rd March in Gilgit Baltistan and Khayber Pakhtunkhua respectively and on 24th March in the rest of the provinces. This complete lockdown continued till mid of May 2020, after which ‘Smart lockdown’, a partial type of lockdown, was implemented in high-risk cities and localities.
These necessary restrictions can create both short and potentially long-term but inevitable and serious effects on the psychological state of suspected, diseased, at-risk and healthy individuals (8). A high number of cases, economic shutdown and mobility restrictions created worries about the health care provision and food availability (9). For many countries, the situation is difficult to deal with, despite having the resources to deal with financial and social crises. Pakistan, a developing country with half of the population living below the poverty line, is facing the pressure of this outbreak. This situation led to frustration, anger, depression, anxiety, and several other active psychiatric complaints (10).United Nations (UN) defined Heads of households as “ that person in the household who is acknowledged as such by the other members” (11), he/she is an individual in one family setting who earns, lead the family and takes the decision on family matters (12). Social and economic circumstances resulting from these control measures may put heads of households under additional stress and affect their capabilities. This in turn, can affect the whole family (13). WHO’s Department of Mental Health and Substance Use on March 18th, 2020, developed an outline addressing considerations for general and various targeted populations. It aimed to support the mental health and psychosocial wellbeing of patients and the general population. It also added to the understanding of the possible effect of COVID-19 and assisting the population in dealing with the newest threat in the most effective ways (14).
Most of the research coverage is given to understand the mental health and behavioral changes in the health care professionals and the general population. A study from Pakistan reported the prevalence of mental disorders to be 52% (15). Other studies from Indian (16), Bangladesh (17), and Iran (18) have shown a high prevalence of mental disorders during the COVID-19 pandemic in the general population. However, literature on the mental health status of heads of a house is scarce. The research currently available has assessed the overall impact of COVID-19 on households and its relationship with the characteristics of heads of the household (19,20). This study focuses on the psychological impact, coping strategies, fears and worries of the pandemic on the heads of families as they seem to be the most vulnerable individuals.
Methods
An online survey was conducted among the heads of families in the general population of Pakistan. There are four provinces in Pakistan; Punjab, Sindh, Baluchistan and Khyber Pakhtunkhwa, two autonomous territories-Azad Kashmir and Gilgit-Baltistan, and one federal capital territory- Islamabad. The total population of Pakistan is 207 million, as per the Population Census of 2017 (21). The average household size in Pakistan is 6.6 persons, the adult literacy rate is 50% and 70% for females and males respectively. Internet usage is low with only 28% of the male and 12% of women using the internet. Common occupation include; manual skilled (female 34%, male 20.3%), agriculture (female 31.5%, male 20.7%), services and sales (female 14.1%, male 21.7%) and professionals (female 12%, male 12.5%) (22).
Data were collected from 5th - 25th May 2020. We opted for an online survey and used all possible means to contact the heads of households in the general population as it was not possible to conduct face-to-face interviews in the community due to strict lockdown all over the country. We used convenience and snowball sampling strategy strategies to include the families. Data were collected from heads of the households by a web-based self-administered questionnaire formulated on a google form. The detailed flowchart of this study is shown in Figure 1. Access link to the survey was sent to the household heads through email addresses and social networks like Facebook, WhatsApp, and Instagram.
Fig. 1.
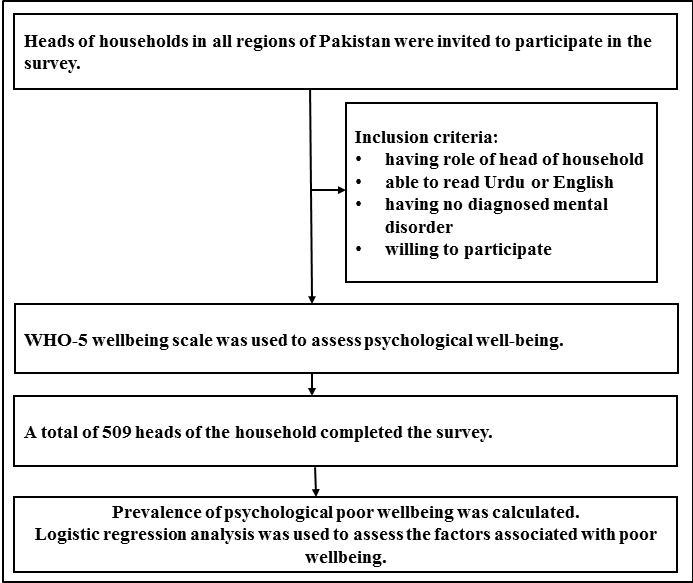
Flow chart of subjects’ enrollment
Sample size calculation
Sample size was calculated using an open epi sample size calculator (23). We assumed a proportion of 50% population to have poor wellbeing. This proportion of 50% would provide maximum variance and sample size. At 95% confidence level and 5% absolute precision, the sample size calculated was 384 participants. We further inflated our sample by 20% to account for incomplete and missing data so the final sample size required was 461 participants.
Data collection instruments, measures, and variables
The questionnaire form was available in both English and national language Urdu. It consisted of 27 questions divided into four sections. The willingness of the participants and choice of language was taken into consideration before the demographic information. Section I was based on socio-demographic information. It included gender, age, city, education, marital status, employment status, family type, disease status and financial support.
Section II was based on the attitude of Pakistani heads of the households related to COVID-19. The assessment was regarding the following aspects: belief in successful control of COVID-19, believing that Pakistan can win the battle against COVID-19, stopping oneself from watching the news will help in decreasing the fear and that the unverified information spreading through forwarded messages is increasing panic about COVID-19. The 5-point Likert scale was modified into a 3-point response. The response of strongly disagree and disagree was merged into one response as disagree; strongly agree and agree were merged as agree; and a middle category included was neither agree nor disagree.
Section III was based on five questions about nervousness regarding COVID-19. Following questions were asked: worry about contracting the disease even with preventive measures; get infected worried about the inability to survive COVID-19, the passage of infection to the family and fear among participants about contracting the disease. The responses were ‘not worried at all’, ‘mildly worried’, and ‘somewhat worried’, ‘moderately worried and extremely worried’. The total worriedness score was calculated by summing up the first four questions on the scale.
The WHO-5 Well-Being Index
Section IV of the survey was based on the 5-item World Health organization Well–Being index. (WHO-5) is among the most commonly used questionnaires assessing subjective psychological well-being (24). It is a short form of WHO-10 item and 28 item rating scale (25). This WHO-5 can be used as a screening tool for depressive symptoms, monitoring emotional well-being and psychological well-being (26). The WHO-5 items were; I have felt cheerful and in good spirits, I have felt calm and relaxed, I have felt active and vigorous, I woke up feeling fresh and rested and my daily life has been filled with things that interest me. The response alternatives were ‘all of the time = 5’, ‘most of the time = 4’, ‘more than half of the time = 3’, ‘less than half of the time = 2’, ‘some of the time = 1’ or ‘at no time =0. The respondents were asked to rate how well each of the 5 statements applies to them when considering the last 14 days. Each of the 5 items was scored from 5 all of the time) to 0 (none of the time). The raw score therefore theoretically ranges from 0 (absence of well-being) to 25 (maximal well-being). The raw score ranging from 0 to 25 was multiplied by 4 to give the final score from 0 representing the worst imaginable possible well-being to 100 representing the best imaginable well-being. We used the official Urdu version of the WHO-5 well-being scale (27). Reliability of the Urdu version of the WHO-5 well-being scale inferred by Cronbach’s Alpha was 0.795; Gutman Split Half Coefficient was 0.761 and test-retest reliability was 0.782. These findings showed good psychometric properties of the Urdu version of the WHO-5 well-being scale (28).
Statistical analysis
Data were downloaded as a Microsoft Excel sheet and then imported to IBM SPSS for Windows v. 22.0 (IBM Corp., Armonk, USA) for analysis. Quantitative variables such as age were reported as mean and standard deviation. Categorical variables such as gender, marital status, education, employment status, family type, region, financial support during lockdown and disease status were expressed as frequencies and percentages. The proportion for the attitudes, worriedness and coping strategies used by the participants at the time of lock-down was determined by using frequencies of individual questions. Prevalence of poor wellbeing was determined using a cut-off of ≤50 scores on 100 point WHO-5 well-being scale. Univariate and multivariate logistic regression models were developed to explore the factors associated with poor well-being among the heads of households. Variables were included in the multivariate model based on contribution in the overall model assessed by -2 log likelihood ratios. Crude and adjusted odds ratio (aOR) along with associated 95% confidence intervals (CI) were calculated. A P-value of ≤0.05 was considered statistically significant.
Results
A total of 509 heads of families participated in the survey. The mean age of the participants was 42.6 (12.1) (range: 19-89) years, and the majority (82.9%) was male. More than half (60.2%) had post-graduation/professional degrees. About three-fourths of the participants were employed, while only 5.5% and 4.9% were unemployed and students, respectively. Among the employed, majority (46%) had a private job. The highest proportion of participants was from Sindh 39.6% followed by Khyber Pakhtunkhwa (KPK) 22.3%. The most common financial support during lockdown was salary (65.2%), followed by savings (11.8%). The most common chronic disease was hypertension (19.8%) while the prevalence of any chronic illness was 36.5% (Table 1).
Table 1. Socio-demographic characteristics of the Pakistani heads of households (n=509) .
| Characteristic | n (%) |
| Age (n=506) | |
| Mean (SD) | 42.6 (12.1) |
| Gender (n=504) | |
| Male | 418 (82.9) |
| Female | 86 (17.1) |
| Marital Status (n=509) | |
| Ever married | 461 (90.6) |
| Single | 48 (9.4) |
| Education (n=507) | |
| Postgraduate | 305 (60.2) |
| Graduate | 125 (24.7) |
| Intermediate | 52 (10.3) |
| Others | 25 (4.9) |
| Employment Status (n=509) | |
| Employed | 391 (76.8) |
| Student | 25 (4.9) |
| Housewife | 36 (7.1) |
| Retired | 29 (5.7) |
| Unemployed | 28 (5.5) |
| Type of employment (n=352) | |
| Private job | 162 (46.0) |
| Government job | 134 (38.1) |
| Business | 41 (11.6) |
| Small business/Vendor | 11 (3.1) |
| Laborer | 3 (0.9) |
| Part time work | 1 (0.3) |
| Family Type (n=509) | |
| Nuclear | 263 (51.7) |
| Joint | 246 (48.3) |
| Region (n=503) | |
| Punjab | 96 (19.1) |
| Sindh | 199 (39.6) |
| Khyber Pakhtunkhwa | 112 (22.3) |
| Baluchistan | 19 (3.8) |
| Islamabad Capital Territory | 55 (10.9) |
| Others | 22 (4.4) |
| Financial support during lockdown (n=508) | |
| Salary | 331 (65.2) |
| Savings | 60 (11.8) |
| Business earning | 59 (11.6) |
| Support from friends and family | 12 (2.4) |
| No source | 15 (3.0) |
| Loan | 11 (2.2) |
| Pension | 20 (3.9) |
| Disease Status (n=509) | |
| Any chronic illness | 186 (36.5) |
| Cardiac disease | 44 (8.6) |
| Hypertension | 101 (19.8) |
| Diabetes | 69 (13.6) |
| Others | 63 (12.4) |
Table 2 presents the attitude and worries related to COVID-19 among Pakistani heads of households. About 67.6% and 69% of participants believed that COVID-19 would be controlled globally and in Pakistan respectively. Seventy percent assumed that avoiding news may help reduce the fears of COVID-19. A high proportion (87.4%) believed that unauthentic information through social media is adding to the panic about COVID-19. About two-third (68.9%) of the participants were mild to moderately worried about contracting the disease even with preventive measures. About 7.6% were extremely worried that after contracting COVID-19, drugs and treatment would have no effects on them. About one-third of the participants (34%) were extremely worried about transmitting the infection to family members.
Table 2. Attitudes and worriedness of Pakistani heads of households related to COVID-19 (n=509) .
| Variable | n (%) |
| Attitudes | |
| COVID-19 will be controlled (n=509) | |
| Agree | 344 (67.6) |
| Don’t know | 79 (15.5) |
| Disagree | 86 (16.9) |
| Pakistan will be able to control the CVOID-19 (n=509) | |
| Agree | 351 (69.0) |
| Don’t know | 84 (16.5) |
| Disagree | 74 (14.5) |
| Stopping yourself from watching news will help in decreasing the fear (n=509) | |
| Agree | 359 (70.5) |
| Don’t know | 43 (8.4) |
| Disagree | 107 (21.0) |
| Unauthentic information through social media is increasing panic about COVID-19 (n=508) | |
| Agree | 444 (87.4) |
| Don’t know | 31 (6.1) |
| Disagree | 33 (6.5) |
| Social distancing will become the new norm and we will not be able to meet people in future like we did before (n=508) | |
| Agree | 179 (35.2) |
| Don’t know | 64 (12.6) |
| Disagree | 265 (52.1) |
| Worries | |
| I will eventually contract COVID-19 despite preventive measures (n=508) | |
| Not worried at all | 137 (27.0) |
| Mildly worried | 142 (28.0) |
| Somewhat worried | 145 (28.5) |
| Moderately worried | 63 (12.4) |
| Extremely worried | 21 (4.1) |
| I will not be able to survive by COVID-19, if I contract the infection (n=508) | |
| Not worried at all | 186 (36.6) |
| Mildly worried | 149 (29.3) |
| Somewhat worried | 93 (18.3) |
| Moderately worried | 46 (9.1) |
| Extremely worried | 38 (7.5) |
| Drugs/treatment will have no effect on me (n=497) | |
| Not worried at all | 185 (37.2) |
| Mildly worried | 135 (27.2) |
| Somewhat worried | 95 (18.7) |
| Moderately worried | 44 (8.9) |
| Extremely worried | 38 (7.6) |
| I am ______ if I get the infection, I will pass to my family (n=507) | |
| Not worried at all | 53 (10.5) |
| Mildly worried | 106 (20.9) |
| Somewhat worried | 100 (19.7) |
| Moderately worried | 73 (14.4) |
| Extremely worried | 175 (34.5) |
| I am ______ about contracting it because I am old and have lived my life the best way I could (n=488) | |
| Not worried at all | 28 (26.4) |
| Mildly worried | 28 (26.4) |
| Somewhat worried | 26 (24.5) |
| Moderately worried | 14 (13.2) |
| Extremely worried | 10 (9.4) |
Most common coping strategies to counter the effects of lockdown and home confinement adopted by the participants included; spending quality time with family (80.7%), eating healthy foods (71.3%), adequate sleep (70.1%) and talking to friends on the phone (67.4%). Other strategies included; seeking spiritual support, watching TV/movies, reading and contributing in social welfare work (Table 3).
Table 3. Coping strategies used by Pakistani heads of households .
| Strategy | n (%) |
| Spending quality time with my family | 411 (80.7) |
| Eating Healthy Food | 363 (71.3) |
| Adequate Sleep | 357 (70.1) |
| Talking to friends on phone | 343 (67.4) |
| Seeking Spiritual support | 304 (59.7) |
| Watching TV/movies | 271 (53.2) |
| Reading | 242 (47.5) |
| Contributing in social welfare work | 221 (43.4) |
| Working on Hobbies | 203 (39.9) |
| Relaxing by meditation / yoga/ exercise | 194 (38.1) |
| Playing video Games | 119 (23.4) |
The mean score of well-being as measured by the WHO-5 wellbeing scale was 56.2 (24.0) out of a total of 100 points. The prevalence of poor wellbeing was 41% (95% CI: 36.62-45.51). Detailed results of individual items of WHO-5 are presented in Supplementary Table 1.
In univariate analysis, we found that being female, having no financial support, having any chronic illness and increasing worriedness score were significantly associated with poor wellbeing. While all coping strategies except spending time with family, playing video games and watching TV/movies were associated with a lower risk of poor mental wellbeing. When adjusted for confounding effects of other variables in the multivariate model, we found that individuals with any chronic illness were at higher risk of poor wellbeing aOR 1.64 (95% CI: 1.04– 2.59). Worriedness was positively associated with poor mental wellbeing aOR 1.13 (95% CI: 1.06 – 1.19). Other factors such as; age, marital status, education status, family type, region and employment status did not show any significant association with wellbeing. Among the coping strategies, reading books was associated with a lower risk of poor mental wellbeing aOR 0.64 (95% CI: 0.42 – 0.98) while others did not show any association with mental wellbeing (Table 4).
Table 4. Factors associated with poor well-being among Pakistani heads of households during COVID-19 pandemic .
| Characteristic | Univariate analysis | Multivariate analysis | ||
| Crude OR (95% CI) | p-value | Adjustedα OR (95% CI) | p-value | |
| Age© | 0.48 (0.98 – 1.01) | 0.485 | 0.98 (0.96 – 1.00) | 0.059 |
| Gender | ||||
| Male | 1 | 1 | ||
| Female | 1.93 (1.20 – 3.10) | 0.007 | 1.45 (0.84 – 2.50 | 0.183 |
| Marital Status | ||||
| Single | 1 | -- | -- | |
| Ever married | 0.70 (0.38 – 1.30) | 0.262 | -- | -- |
| Education Status | ||||
| Postgraduate | 1 | |||
| Graduate | 1.00 (0.65 – 1.55) | 0.990 | -- | -- |
| Intermediate | 1.39 (0.76 – 2.53) | 0.285 | -- | -- |
| Matric and lower | 1.39 (0.61 – 3.15) | 0.432 | -- | -- |
| Employment status | ||||
| Employed | 1 | |||
| Student | 2.01 (0.89 – 4.54) | 0.094 | -- | -- |
| Housewife | 1.49 (0.74 – 2.98) | 0.260 | -- | -- |
| Retired | 0.88 (0.39 – 1.95) | 0.747 | -- | -- |
| Unemployed | 1.82 (0.84 – 3.94) | 0.128 | -- | -- |
| Family Type | ||||
| Joint | 1 | |||
| Nuclear | 1.08 (0.75 – 1.54) | 0.688 | -- | -- |
| Financial support | ||||
| Yes | 1 | 1 | ||
| No | 3.73 (1.15 – 12.06) | 0.028 | 5.11 (0.96 -27.24) | 0.056 |
| Region | ||||
| Punjab | 1 | 1 | ||
| Sindh | 1.50 (0.90 – 2.50) | 0.116 | -- | -- |
| Khyber Pakhtunkhwa | 1.31 (0.74 – 2.32) | 0.350 | -- | -- |
| Baluchistan | 1.11 (0.40 – 3.10) | 0.837 | -- | -- |
| Islamabad Capital Territory | 1.46 (0.74 – 2.91) | 0.277 | -- | -- |
| Other | 1.56 (0.59 – 4.15) | 0.371 | -- | -- |
| Any chronic illness | ||||
| No | 1 | 1 | ||
| Yes | 1.64 (1.13 – 2.37) | 0.009 | 1.64 (1.04 – 2.59 | 0.033 |
| Worriedness© | 1.14 (1.08 – 1.20) | <0.001 | 1.13 (1.06 – 1.19) | <0.001 |
| Coping strategies | ||||
| Spending quality time with my family | 0.67 (0.43 – 1.06) | 0.089 | 1.27 (0.72 – 2.25) | 0.345 |
| Eating healthy food | 0.41 (0.28 – 0.62) | <0.001 | 0.79 (0.45 – 1.39) | 0.414 |
| Adequate sleep | 0.46 (0.31 – 0.68) | <0.001 | 0.73 (0.43 – 1.23) | 0.234 |
| Talking to friends on phone | 0.47 (0.32 – 0.69) | <0.001 | 0.62 (0.39 - 1.01) | 0.056 |
| Seeking spiritual (religious) support | 0.56 (0.39 – 0.80) | 0.002 | -- | -- |
| Watching TV/movies | 0.74 (0.52 – 1.06) | 0.105 | -- | -- |
| Reading books and magazines | 0.49 (0.32 – 0.71) | <0.001 | 0.64 (0.42 – 0.98) | 0.042 |
| Contributing in social welfare work | 0.43 (0.30 – 0.63) | <0.001 | 0.67 (0.42 – 1.05) | 0.079 |
| Working on hobbies | 0.50 (0.34 – 0.73) | 0.105 | 0.76 (0.47 – 1.21) | 0.249 |
| Relaxing by meditation / yoga /exercise | 0.51 (0.35 – 0.75) | <0.001 | 0.81 (0.52 – 1.25) | 0.345 |
| Playing video games | 1.05 (0.68 – 1.60) | 0.827 | 1.37 (0.83 – 2.26) | 0.219 |
α Mutually adjusted for each other, © Continuous variable, a¬¬¬ Those who have masters or higher education, b Having a bachelor degree, c Education up to 12 grades, d Includ-ed education lower than 12 grades and informal education in religious schools, e Nuclear Family: A two-generation family consisting of a father and mother and children or a single, possibly widow, parent and his/her children, f Joint Family: Three or more generation lived together with both vertical and lateral extension having a single line of authority, either patrilineal or matrilineal, g Included; Gilgit Baltistan, and Federally Administered Tribal Areas (FATA), --Not included in the multivariate model
Discussion
To the best of our knowledge, this is the first study of its kind to assess the psychological well-being of heads of the households amid the COVID-19 pandemic. Besides direct morbidity and mortality associated with the pandemic, there are psychological effects of the population due to lockdowns and quarantine (29). Head of households is vulnerable to psychological shocks due to events that may affect him/herself or the other family members. Economic and social lockdown to control the spread of COVID-19 may add to the risks for the mental health of heads of households (30,31).
COVID-19 pandemic has affected the global economy and may lead to household economic shocks (32).In our study, about 65% of the heads relied upon salary as the source of income during this period. The remaining one-third (35%) was dependent on other sources of income which could be badly affected by the lockdowns. This may lead to impoverishment and food insecurity of the affected households. This calls for short-term income and food support programs for such vulnerable households to avoid additional morbidity and mortality resulting from poverty and malnutrition (33,34).
We found that about two-thirds (68%) of the heads believed that COVID-19 would be controlled globally and a similar proportion (69%) agreed that Pakistan would be able to control the disease. This is lower than the report from China, where 91% of the general population believed that the pandemic would be controlled (35). During crises such as COVID-19, misinformation plays a key role in creating panic and further deterioration of the mental health of the population (36). In our study, about 70% of the heads of households believed that stopping oneself from watching the news may help reduce fear. Even higher proportion 87%, believed that unauthentic information through social media adds to the panic about COVID-19. This finding is consistent with the results of a study from Karachi, Pakistan, where about 84% of the respondents believed that fake news about COVID-19 on social media is adding to the panic (37). This is an important finding and needs intervention by the governments to control the spread of misinformation and strengthen uniform communication channels to disseminate required information to the masses.
Pandemics and intensive measures to control the spread of disease may lead to fears and worries among the populations. In this study, we found that about three-fourths (73%) of the participants were worried about contracting the disease despite adopting preventive measures. This proportion is higher than in China where about 54% were worried about getting an infection (38).This higher level of worry in our study could be due to the fact that there has been poor compliance among the population about social distancing and preventive measures. Worry about survival after disease and effectiveness of treatment was also higher in our study compared to China (38). This may have negative implications on the actual practices of the participants as people may perceive preventive measures to be ineffective. Nonetheless, these negative attitudes need to be addressed as these may lead to avoiding seeking care in case of disease which may worsen the outcome and increase the spread of disease in the community.
To avoid the negative consequences of the COVID-19 pandemic and associated social and economic lockdown, people adopt various coping mechanism to maintain optimum mental well-being. In our study, we found that the most common coping mechanisms were; spending time with family, eating healthy foods, adequate sleep, talking to friends, and seeking spiritual support. A previous study from Karachi Pakistan, showed that spiritual and religious activities are common coping strategies in the population (39). Another study from Italy showed that using digital devices during bedtimes was increased during the COVID-19 pandemic (40).
We found that the prevalence of poor wellbeing was 41%. However, no pre-pandemic national-level studies were conducted in Pakistan to assess the psychological wellbeing or mental health. A study conducted in five major cities of Pakistan in 2018 showed a prevalence of mental disorders to be 27% (41). Another study from Karachi Pakistan reported the prevalence of psychological distress to be 17% (42). An old systematic review that included studies before 2003 found the prevalence of anxiety and depression to be 34% (43). This may indicate a possible impact of COVID-19 on the mental health of the heads of the households. Our estimate is also higher than reported from China, where about 35% of the participants experienced psychological stress during this pandemic (44). On the other hand, studies from Malaysia and Egypt have shown higher levels of anxiety and stress among the population compared to our study (45,46).A number of reasons can be attributed to these differences across countries. The prevalence of mental disorders and substance abuse has been reported to be higher than in China and lower than in Malaysia and Egypt (47). Genetic factors and ethnicity have also been associated with mental disorders (48,49). Additionally, these differences in the finding across studies could be due to the different nature of tools used for the assessment of mental health. Another reason could be differences in context in which studies were carried out, for example, over all infrastructure of health care delivery system, the response of the country to the pandemic and economic situation of the country. Therefore, these comparisons are arbitrary and should be interpreted cautiously.
We also explored the factors associated with poor wellbeing and found that having a chronic illness and being worried were independently associated with poor wellbeing of the heads of households while reading books was protective against poor mental wellbeing. Females are prone to various psycho-social stresses which may affect their mental health and higher risk of psychiatric disorders (50,51). A previous study from Pakistan had reported low quality of life among female heads of the household compared to male heads (52). During the COVID-19 pandemic studies from different countries have shown a significant association of female gender with anxiety, depression and stress (44,53,54). However, we did not find any significant associationof gender with mental wellbeing. We found having a chronic illness was associated with a higher risk of poor wellbeing. This finding is consistent with the results of a study from Spain where a history of chronic illness was associated with a higher risk of Impact of Event Scale-Revised (IES-R) scores, indicating poor mental wellbeing. Therefore, people with chronic diseases need psychological counseling along with usual care during the COVID-19 pandemic. Coping strategies have been reported in the literature which has a positive impact on mental health. We also found a protective effect of reading on mental wellbeing. It is important to help people identify activities that help them relax and release mental stress to ensure mental wellbeing.
Study Limitations
This study used a standardized and validated tool for the assessment of the mental wellbeing of heads of households from all the regions of the country. There are some limitations that need to be considered while interpreting the results of this study. This was an online survey that might have excluded those heads of households who are not using smartphones and social media especially in the rural areas where the proportion of the illiterate population is high. This is also evident from the higher proportion of postgraduate and graduates in our sample. This may affect the generalizability of our study to this segment of the population. Secondly, there was low participation from the Punjab province which is the largest in terms of population. This may have led to under or over-representation of one or more regions. Nonetheless, our study is the first of its kind to assess the mental wellbeing of heads of the household during the COVID-19 pandemic.
Conclusion
We found a high prevalence of poor mental wellbeing among heads of households in Pakistan. We also found that having any chronic illness and being worried were significant predictors of poor psychological wellbeing while reading books was protective against poor mental wellbeing. We, therefore, recommend further research to explore further the mental health of heads of households and immediate interventions to reduce the psychological impact of COVID-19 to prevent long-term effects on mental health. It is imperative to develop evidence-based support systems and initiatives to support this highly important sub-group of our population. It may include counseling services and the provision of behavioral support programs focusing on heads of the households. Furthermore, self-relaxation training, regular exercise and a healthy lifestyle should also be emphasized. The findings of our study provide a foundation for further research and information for policymakers to develop and implement interventions for mental wellbeing and to assess the impact of these interventions besides other preventive measures for COVID-19.
Acknowledgments
We thank the participants for their cooperation.
Ethical confirmation
The ethical approval of the study was sought from the Ethics Review Committee of Women Medical College, Abbottabad (20204-2 CMD-ERC-20). The first page of the online form described the purpose of the study and consent was taken on that page from all the participants.
Conflict of Interests
The authors declare that they have no competing interests.
Supplementary Table 1
Supplementary Table 1. Wellbeing of Pakistani heads of households during COVID-19 pandemic (n=509).
| Variable | n (%) |
| I have felt cheerful and in good spirit (n=500) | |
| At no time | 32 (6.4) |
| Some of the time | 115 (23.0) |
| Less than half of the time | 55 (11.0) |
| More than half of the time | 97 (19.4) |
| Most of the times | 157 (31.4) |
| All of the time | 44 (8.8) |
| I have felt calm and relaxed (n=504) | |
| At no time | 33 (6.5) |
| Some of the time | 90 (17.9) |
| Less than half of the time | 59 (11.7) |
| More than half of the time | 97 (19.2) |
| Most of the times | 182 (36.1) |
| All of the time | 43 (8.5) |
| I have felt active and vigorous (n = 503) | |
| At no time | 31 (6.2) |
| Some of the time | 103 (20.5) |
| Less than half of the time | 88 (17.5) |
| More than half of the time | 86 (17.1) |
| Most of the times | 147 (29.2) |
| All of the time | 48 (9.5) |
| I woke up feeling fresh and rested (n=504) | |
| At no time | 25 (5.0) |
| Some of the time | 82 (16.3) |
| Less than half of the time | 71 (14.1) |
| More than half of the time | 89 (17.7) |
| Most of the times | 188 (37.3) |
| All of the time | 49 (9.7) |
| My life is filled with things which interest me (n=500) | |
| At no time | 29 (5.8) |
| Some of the time | 114 (22.8) |
| Less than half of the time | 62 (12.4) |
| More than half of the time | 77 (15.4) |
| Most of the times | 165 (33.0) |
| All of the time | 53 (10.6 |
Cite this article as: Rabbani U, Ahmed Khan A, Saqib Lodhi F, Arshad S, Irum S, Marwat NU. Psychological Well-Being and Coping Strategies among Pakistani Heads of Households during COVID-19 Pandemic: An Online Survey. Med J Islam Repub Iran. 2022 (14 May);36:49. https://doi.org/10.47176/mjiri.36.49
References
- 1. WHO Director-General's opening remarks at the media briefing on COVID-19, 11 March 2020. https://www.who.int/dg/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19---11-march-2020.
- 2.Xiao C. A novel approach of consultation on 2019 novel coronavirus (COVID-19)-related psychological and mental problems: structured letter therapy. Psychiatry Investig. 2020 Feb;17(2):175. doi: 10.30773/pi.2020.0047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. World Health Organization. Promoting mental health: concepts, emerging evidence, practice: a report of the World Health Organization, Department of Mental Health and Substance Abuse in collaboration with the Victorian Health Promotion Foundation and the University of Melbourne. World Health Organization; 2005.
- 4.Mak IW, Chu CM, Pan PC, et al. Long-term psychiatric morbidities among SARS survivors. Gen Hosp Psychiatry. 2009 Jul;31(4):318–26. doi: 10.1016/j.genhosppsych.2009.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. World Health Organization, Corona Virus disease pandemic. Corona Virus disease COVID 19 situation. WHO https://www.who.int/emergencies/diseases/novel-coronavirus-2019.
- 6.S S. Mental health and psychological aspects of coronavirus outbreak in Pakistan: Psychological intervention for public health crisis. Asian J Psychiatr. 2020;51:102069. doi: 10.1016/j.ajp.2020.102069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Government of Pakistan Official portal for Corona Virus disease. Pakistan cases detail, COVID 19 statistics. http://covid.gov.pk/stats/pakistan.
- 8. Coronavirus disease (COVID-19) advice for the public. (2020). Accessed: March 21, 2020. https://www.who.int/emergencies/diseases/novel-coronavirus-2019/advice-for-public.
- 9.Rubin GJ, Wessely S. The psychological effects of quarantining a city. Bmj. 2020 Jan;28:368. doi: 10.1136/bmj.m313. [DOI] [PubMed] [Google Scholar]
- 10.Hamza Shuja K, Aqeel M, Jaffar A, et al. COVID-19 Pandemic and Impending Global Mental Health Implications. Psychiatr Danub. 2020 Apr;32(1):32–5. doi: 10.24869/psyd.2020.32. [DOI] [PubMed] [Google Scholar]
- 11. United nations: principles and Recommendations for population and Housing Cenuses. United Nations, New York; 1998.
- 12.Buvinic M, Gupta GR. Female headed households and female-maintained families: are they worth targeting to reduce poverty in developing countries? Econ Dev Cult. 1997;45(2):259–280. [Google Scholar]
- 13. Sen A, Nussbaum M. Capability and well-being. The quality of life. Nussbaum, Sen, A(Eds), Oxford, Clarendon; 1993.
- 14. World Health Organization. Mental health and psychosocial considerations during the COVID-19 outbreak, 18 March 2020. World Health Organization; 2020.
- 15.Riaz M, Abid M, Bano Z. Psychological problems in general population during covid-19 pandemic in Pakistan: role of cognitive emotion regulation. Ann Med. 2021;53(1):189–96. doi: 10.1080/07853890.2020.1853216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Reddy V, Karri SR, Jezreel T, Afeen S, Khairkar P. Psychosocial Impact of COVID-19 Lockdown on Mental Wellbeing among 11 States of India: A Markov Modeling Approach. J Psychiatry Psychiatr Disord. 2020;4(4):158–74. [Google Scholar]
- 17. Mamun MA, Sakib N, Gozal D, Bhuiyan AI, Hossain S, Bodrud-Doza M, et al. The COVID-19 pandemic and serious psychological consequences in Bangladesh: A population-based nationwide study. J Affect Disord 2021; 279, pp.462-472. [DOI] [PMC free article] [PubMed]
- 18.Mani A, Estedlal AR, Kamali M, Ghaemi SZ, Zarei L, Shokrpour N, Heydari ST, Lankarani KB. Mental health status during COVID-19 pandemic in Fars Province, Iran: timely measures. BMC Public Health. 2020 Dec;20(1):1–1. doi: 10.1186/s12889-020-09928-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. The Impact of COVID-19 on Households in Nepal mVAM Household Livelihoods, Food Security and Vulnerability Survey. 2020. https://docs.wfp.org/api/documents/WFP-0000116728/download/.
- 20. The Disproportionate Effects of COVID-19 on Households with Children. 2020. https://libertystreeteconomics.newyorkfed.org/2020/08/the-disproportionate-effects-of-covid-19-on-households-with-children.html.
- 21. Pakistan Bureau of Statistics, Government of Pakistan. Province wise results of the Census, Population census 2017.
- 22. National Institute of Population Studies, Pakistan. Pakistan demographic and health survey 2017-18. Pakistan demographic and health survey 2017–18. 2019.
- 23. Dean A, Sullivan K, Soe M. OpenEpi: Open Source Epidemiologic Statistics for Public Health, Version 2013 [updated April 06, 2013; cited April 15, 2020]. Available from: www.OpenEpi.com.
- 24.Bech P, Gudex C, Johansen KS. The WHO (Ten) well-being index: validation in diabetes. Psychother Psychosom. 1996;65(4):183–90. doi: 10.1159/000289073. [DOI] [PubMed] [Google Scholar]
- 25.Krieger T, Zimmermann J, Huffziger S, Ubl B, Diener C, Kuehner C, et al. Measuring depression with a well-being index: further evidence for the validity of the WHO Well-Being Index (WHO-5) as a measure of the severity of depression. J Affect Disord. 2014;156:240–4. doi: 10.1016/j.jad.2013.12.015. [DOI] [PubMed] [Google Scholar]
- 26.Schneider CB, Pilhatsch M, Rifati M, Jost WH, Wodarz F, Ebersbach G, et al. Utility of the WHO‐five well‐being index as a screening tool for depression in Parkinson's disease. Mov Disord. 2010;25(6):777–83. doi: 10.1002/mds.22985. [DOI] [PubMed] [Google Scholar]
- 27. World Health Organization. WHO-5 Questionnaires: Urdu version [cited April 14, 2020]. Available from: https://www.psykiatri-regionh.dk/who-5/Documents/WHO5_Urdu.pdf.
- 28.Shahzad S, Jones HE, Begum N, Zia A. Urdu translation and psychometric properties of WHO-Five Wellbeing Index among male patients with substance use disorders in Pakistan. J Subst Use. 2021 Nov 22:1–5. [Google Scholar]
- 29.Brooks SK, Webster RK, Smith LE, Woodland L, Wessely S, Greenberg N, et al. The psychological impact of quarantine and how to reduce it: rapid review of the evidence. Lancet. 2020;395(10227):912–20. doi: 10.1016/S0140-6736(20)30460-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Kazmi SS, Hasan K, Talib S, Saxena S. COVID-19 and lockdwon: a study on the impact on mental health. Available at SSRN 3577515. 2020 Apr 15.
- 31.Heanoy EZ, Shi L, Brown NR. Assessing the Transitional Impact and Mental Health Consequences of the COVID-19 Pandemic Onset. Front Psychol. 2020;11:3715. doi: 10.3389/fpsyg.2020.607976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Hanspal T, Weber A, Wohlfart J. Exposure to the COVID-19 Stock Market Crash and its Effect on Household Expectations University of Copenhagen Department of Economics The Center for Economic Behavior and Inequality (CEBI) 2020; CEBI Working Paper Series, No. 13/20.
- 33.Dunn CG, Kenney E, Fleischhacker SE, et al. Feeding low-income children during the Covid-19 pandemic. N Engl J Med. 2020;382(18):e40. doi: 10.1056/NEJMp2005638. [DOI] [PubMed] [Google Scholar]
- 34. Mogaji E. Financial Vulnerability during a Pandemic: Insights for Coronavirus Disease (COVID-19). Mogaji, E 2020:57-63.
- 35.Zhong BL, Luo W, Li HM, Zhang QQ, Liu XG, Li WT, et al. Knowledge, attitudes, and practices towards COVID-19 among Chinese residents during the rapid rise period of the COVID-19 outbreak: a quick online cross-sectional survey. Int J Biol Sci. 2020;16(10):1745. doi: 10.7150/ijbs.45221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.BSD RP, Wilder-Smith A. The pandemic of social media panic travels faster than the COVID-19 outbreak. J Travel Med. 2020;27(3) doi: 10.1093/jtm/taaa031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Balkhi F, Nasir A, Zehra A, Riaz R. Psychological and Behavioral Response to the Coronavirus (COVID-19) Pandemic. Cureus. 2020;12(5):e7923. doi: 10.7759/cureus.7923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Wang C, Pan R, Wan X, Tan Y, Xu L, Ho CS, et al. Immediate psychological responses and associated factors during the initial stage of the 2019 coronavirus disease (COVID-19) epidemic among the general population in China. Int J Environ Res. 2020;17(5):1729. doi: 10.3390/ijerph17051729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Kasi PM, Naqvi HA, Afghan AK, Khawar T, Khan FH, Khan UZ, et al. Coping styles in patients with anxiety and depression. Int Sch Res Notices. 2012. [DOI] [PMC free article] [PubMed]
- 40.Cellini N, Canale N, Mioni G, Costa S. Changes in sleep pattern, sense of time, and digital media use during COVID-19 lockdown in Italy. J Sleep Res. 2020 May 15:e13074. doi: 10.1111/jsr.13074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Husain W. Prevalent tendencies for mental disorders in Pakistan. Clin Health. 2018 Feb 27;29(1):34–8. [Google Scholar]
- 42.Mirza I, Jenkins R. Risk factors, prevalence, and treatment of anxiety and depressive disorders in Pakistan: systematic review. Bmj. 2004 Apr 1;328(7443):794. doi: 10.1136/bmj.328.7443.794. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Kidwai R. Demographic factors, social problems and material amenities as predictors of psychological distress: a cross-sectional study in Karachi, Pakistan. Soc Psychiatry Psychiatr Epidemiol. 2014 Jan 1;49(1):27–39. doi: 10.1007/s00127-013-0692-0. [DOI] [PubMed] [Google Scholar]
- 44.Qiu J, Shen B, Zhao M, Wang Z, Xie B, Xu Y. A nationwide survey of psychological distress among Chinese people in the COVID-19 epidemic: implications and policy recommendations. Gen Psychiatry. 2020;33(2):e100213. doi: 10.1136/gpsych-2020-100213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Magdy DM, Metwally A, Magdy O. Assessment of community psycho-behavioral responses during the outbreak of novel coronavirus (2019-nCoV): a cross-sectional study. AIMS Public Health. 2022;9(1):26. doi: 10.3934/publichealth.2022003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Wong LP, Alias H. Temporal changes in psychobehavioural responses during the early phase of the COVID-19 pandemic in Malaysia. J Behav Med 2021. Feb;44(1):18–28. doi: 10.1007/s10865-020-00172-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Dattani S, Ritchie H, Roser M. Mental Health. 2021. Published online at Our WorldInData.org. Retrieved from: https://ourworldindata.org/mental-health' [Online Resource].
- 48.Dnlop DD, Song J, Lyons JS, Manheim LM, Chang RW. Racial/ethnic differences in rates of depression among preretirement adults. Am J Public Health. 2003 Nov;93(11):1945–52. doi: 10.2105/ajph.93.11.1945. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Bailey RK, Mokonogho J, Kumar A. Racial and ethnic differences in depression: current perspectives. Neuropsychiatr Dis Treat. 2019;15:603. doi: 10.2147/NDT.S128584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Kuehner C. Why is depression more common among women than among men? Lancet Psychiatry. 2017;4(2):146–58. doi: 10.1016/S2215-0366(16)30263-2. [DOI] [PubMed] [Google Scholar]
- 51. Pappa S, Ntella V, Giannakas T.et al. Prevalence of depression, anxiety, and insomnia among healthcare workers during the COVID-19 pandemic: A systematic review and meta-analysis. Brain Behav Immun. 2020 May 8. [DOI] [PMC free article] [PubMed]
- 52.Lodhi FS, Rabbani U, Khan AA, Irum S, Holakouie-Naieni K. Quality of life and its predictors among Pakistani head of household in district Abbottabad, Pakistan. Qual Quant. 2020 Aug;54(4):1129–43. [Google Scholar]
- 53. González-Sanguino C, Ausín B, Castellanos MÁ, Saiz J, López-Gómez A, Ugidos C, et al. Mental Health Consequences during the Initial Stage of the 2020 Coronavirus Pandemic (COVID-19) in Spain. Brain BehavImmun. 2020 May 13. [DOI] [PMC free article] [PubMed]
- 54.Othman N. Depression, Anxiety, and Stress In The Time of COVID-19 Pandemic In Kurdistan Region, Iraq. Kurd J Appl Res. 2020;5:37–44. [Google Scholar]


