Abstract
Background: With the advent of coronavirus-2019 (COVID-19), telemedicine services have played an essential role in reducing the transmission of this virus between patients and health care providers. Nevertheless, financial and reimbursement barriers are the biggest challenge in adopting these technologies. It seems necessary to determine the successful reimbursement methods in different countries. The purpose of this study was to identify methods of reimbursing telemedicine services.
Methods: A search without time limitation was conducted on the PubMed, Web of Science, and Scopus databases in December 2020 and updated in January 2022. Articles were identified using predefined inclusion and exclusion criteria. Two researchers independently evaluated the titles, abstracts, and full text of the articles.
Results: Out of 4946 identified articles, 28 articles were included. In these studies, the most used insurances were Medicare (n = 17), and Medicaid (n = 15). The majority of services included telepsychiatry (n = 7), telehealth (n = 7), and telemedicine (n = 7). There was no difference between the reimbursements in telemedicine services and face-to-face visits in 18 studies.
Conclusion: Various government, state, and private insurance reimbursed telemedicine services. In most studies, there was no difference between reimbursing telemedicine services and in-person visits. Differences in the type and number of reimbursements may be due to the year of publication of the articles, changes in covered service policies, and state laws. Because of the COVID-19 pandemic, it is crucial to develop and update the guidelines and regulations for telemedicine reimbursement. Future studies can examine the telemedicine reimbursement methods in developed and developing countries before and after the COVID-19 pandemic.
Keywords: Telehealth, Telemedicine, Reimbursement, COVID-19
Introduction
↑What is “already known” in this topic:
Telemedicine can lower health care costs and provide your patients with better access to health care services. Many barriers can prevent the widespread implementation and utilization of telemedicine services. The financial and reimbursable barriers to telemedicine services are the first and foremost challenge of adopting this technology.
→What this article adds:
Various government, state, and private insurance reimburse telemedicine services. It is necessary to develop and update telemedicine reimbursement guidelines and regulations, especially in the COVID-19 pandemic.
The use of information and communication technology to access health services has introduced a concept called telehealth (1). Telehealth means transmitting medical information and providing and supporting clinical care from one place to another through electronic communication methods (2,3). One of the subsets of telehealth is telemedicine (4). Telemedicine is used in different ways and offers a wide range of simple services—such as telephone consultations between physicians and patients and complicated services, including robotic surgery through video conferencing equipment between providers in health care institutions in 2 different countries (2,3,5). The goal of all telemedicine is to improve patient care and accessibility of health care services in rural and disadvantaged areas, facilitating automated examinations for physicians and reducing costs (eg, medical care, patient transfer, and patient accommodation in the medical center). Other goals include providing medical care services in a wide geographical area, reducing patient transfer to medical centers, and creating a managed care atmosphere in hospitals and medical centers (6,7). These benefits and capabilities advocated telemedicine in various areas of health. Hence, modern health care services such as teleconsultation, tele-education, teleradiology, telepathology, telecardiology, tele-home care, telemedicine in emergencies, and telesurgery have emerged (2,3,6).
Despite the many benefits and applications of telemedicine, this technology has been used sparingly in some countries in areas such as communicating radiology reports and telephone or televised visits (7). Many barriers and challenges can prevent the widespread implementation and utilization of telemedicine services. Studies have shown that financial, technical, and technology integration barriers (such as lack of proper infrastructure, software, and hardware), patient mistrust, and negative attitudes toward health care providers are among the telemedicine implementation challenges (8-12). However, from the perspective of health care providers, the financial and reimbursable barrier to telemedicine services is the first and foremost challenge of adopting this technology (13). In many, often developed countries, telemedicine services are reimbursed by public or private institutions (7,13-17). For example, Browm, in a review study, reported that in the United States, telemedicine reimbursement is covered by the Medicaid program and private payers (14). Bursell et al also showed that in Australia, telemedicine services, such as audio or video consultation, are reimbursed somewhat by Medicare (15). However, some payers and states do not reimburse the cost of telemedicine services or reimburse it at a lower rate compared with face-to-face services (18). On the other hand, average reimbursements and charges for diagnoses and procedures for telemedicine services were examined by clinical classification systems and terminologies (18).
The New coronavirus 2019 (COVID-19) is currently spreading rapidly worldwide, thus, the World Health Organization declared it a global pandemic on March 11, 2020 (19). With the advent of COVID-19, telemedicine services have played an essential role in reducing the prevalence and transmission of COVID-19 among patients, families, and health care providers (20). Also, during COVID-19, telemedicine has provided the possibility of preserving valuable personal protective equipment and palliative care for vulnerable people and patients with serious illnesses (20). Therefore, determining the successful reimbursement methods, coverage of these services by insurance organizations in different countries, and terminologies and clinical classification systems used for reimbursing are necessary to expand telemedicine. Hence, the present scoping review was conducted to answer the following questions:
What are the methods for reimbursing telemedicine services in different countries?
Which telemedicine services arde remotely covered by insurance and payers?
What clinical classification systems are used for telemedicine reimbursement services?
The results of this study can help health policymakers and insurance organizations revise or develop guidelines and rules for telemedicine reimbursement.
Methods
Search Strategy
The present scoping review was conducted in December 2020 (31/12/2020) to review payment methods of telemedicine services based on thePreferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) extension for scoping reviews (PRISMA-ScR) (21). Then, this study was updated in January 2022 (21/1/2022). For this purpose, 2 researchers searched PubMed, Web of Science, and Scopus to identify related articles without time limitation. The search strategy included searching for titles, abstracts, and keywords of relevant studies in the PubMed, Scopus, and Web of Science databases. The first group of keywords was related to reimbursement methods and related insurances. The second group consisted of keywords related to telemedicine services. The synonym words were combined with the OR operator within these 2 groups. Then, these 2 groups of keywords were combined using the AND operator (Appendix 1).
The limitations applied to the 3 databases were (1) articles published in English and (2) articles only.
Eligibility Criteria
The following were the inclusion criteria for the relevant articles: (1) focusing on telemedicine systems and their various varieties, (2) addressing payment, reimbursement, or insurance methods, (3) being relevant to telemedicine payment methods, and (4) written in English.
Descriptive articles, review studies, case reports, commentaries, conference papers, and letters to the editor were excluded because these studies could not provide sufficient detail to achieve results relevant to the purpose of the study.
Study Selection and Data Extraction
After searching the databases, the extracted articles were imported into Endnote Version X8.0.1, and the duplications were removed. The titles and abstracts of all articles were reviewed independently by 2 researchers. The results were then discussed at a group meeting. The full texts of abstracts of all publications that met all the inclusion criteria were then selected for reading, and the study’s findings were discussed in meetings between the 2 researchers. In this study, the third researcher reviewed the articles in case of disagreement between the 2 researchers. The reference lists of the final selected studies were reviewed to avoid missing possible related studies. Finally, the information of the final studies was recorded in the data collection table. This table consisted of the following items: author, year of publication, place of implementation, study type, study population, type of telemedicine system, type of reimbursement method, coding system, and primary outcomes results. The third researcher also judged disagreements in data extraction. The PRISMA-ScR checklist (21) was used for drawing the flow diagram.
Results
Study Characteristics
The PRISMA-ScR flow diagram based on the search results is shown in Figure 1. In total, 4946 articles were identified from 3 databases and reference lists of selected studies. Of these articles, 1877 were duplicate studies. After screening the studies based on their titles and abstracts, 2876 articles were irrelevant, and only 193 articles were selected for a more detailed review of abstracts. Among the studies selected for the review of abstracts, 123 studies were selected for full-text review, of which 42 studies could not be accessed free of charge. Among the 81 articles with free full texts, 53 studies were excluded from the final review phase for various reasons, such as the type of study (letter to the editor, reports, and review), descriptive and qualitative presentation of information concerning telemedicine and reimbursement methods, and missing the role of the payment methods and insurance institutions in the reimbursement of telemedicine services. Finally, 28 articles met all the inclusion criteria (4,16,18,22-46) (Fig. 1). The quality assessment of studies was not performed due to the type of review, which was scoping review (21).
Fig. 1.
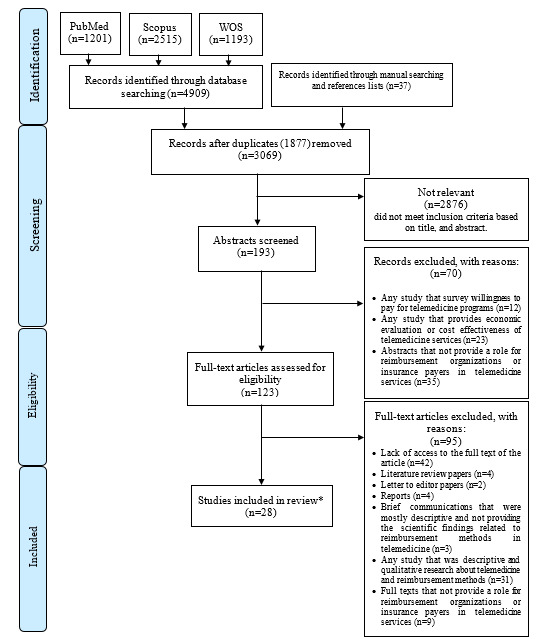
PRISMA-ScR flow diagram of study selection
*no articles were included from manual reference searching as inclusion criteria were not met.
Features of the Selected Articles
Details of the selected studies are shown in Table 1. The year of publication of the selected studies (n = 28) was between 2001 and 2022, most of which were published in 2017 and 2020 (Table 1). Of the 27 studies, the highest number (n = 24) were conducted in the United States. Most of the selected studies were retrospective (n = 12), and cross-sectional (n = 5). The use of data related to claims and reimbursement of various insurances made up the study population in most studies (n = 16).
Table 1. Summary of study characteristics and extracted data .
| No | Author/year of publication | Country | Type of telemedicine services | Classification systems | Type of payment or insurance | Reimbursement rate (telemedicine services vs. face-to-face visits a,b) |
||||
| Medicaid | Medicare | Private payer | Combined payers | Other | ||||||
| 1 | Skinner et al., (2022) (22) | USA | Telehealth | CPT | * | * | TELEMED = F2F | |||
| 2 | Murray et al., (2021) (23) | USA | Telehealth | CPT | * | TELEMED < F2F | ||||
| 3 | Andino et al., 2021 (24) | USA | Telehealth | E&M, CPT | * | TELEMED = F2F | ||||
| 4 | Miller et al., 2020 (25) | USA | Tele-dermatology Tele-otolaryngology Tele-psychiatry |
HCPCS | * | TELEMED = F2F | ||||
| 5 | Mehta et al., 2020 (4) | USA | Tele-homecare | E&M | * | * | * | * | TELEMED = F2F | |
| 6 | Lin et al., 2020 (26) | USA | Tele-cardiology | NM c | * | * | * | * | TELEMED = F2F | |
| 7 | Wilson et al., 2020 (27) | Australia | Tele-psychiatry | NM | * | TELEMED < F2F | ||||
| 8 | Ehlert et al., 2019 (28) | German | Tele-cardiology | Social insurance code book five, ICD | * | TELEMED < F2F | ||||
| 9 | Yu et al., 2018 (29) | USA | Telemedicine | CPT | * | * | * | * | TELEMED = F2F | |
| 10 | Crane et al., 2018 (30) | USA | Tele-toxicology | E&M, CPT | * | * | * | * | TELEMED = F2F | |
| 11 | Wilson et al., 2017 (18) | USA | Tele-psychiatry | CPT, HCPCS, ICD-9-CM | * | TELEMED < F2F | ||||
| 12 | Wilson et al., 2017 (31) | USA | Tele-psychiatry | CPT, ICD-9-CM |
* | TELEMED < F2F | ||||
| 13 | Trout et al., 2017 (32) | USA | Telehealth | NM | * | TELEMED = F2F | ||||
| 14 | Douglas et al., 2017 (33) | USA | Tele-psychiatry | CPT, HCPCS, ICD-9 | * | TELEMED = F2F | ||||
| 15 | Schmeida et al., 2016 (34) | USA | Telemedicine | NM | * | TELEMED < F2F | ||||
| 16 | Neufeld et al., 2016 (35) | USA | Telemedicine | NM | * | * | * | * | TELEMED = F2F | |
| 17 | Neufeld et al., 2015 (36) | USA | Telemedicine | HCPCS, CPT | * | TELEMED < F2F | ||||
| 18 | Guedon-Moreau et al., 2014 (37) | France | Tele-cardiology | NM | * | TELEMED < F2F | ||||
| 19 | Antoniotti et al., 2014 (38) | USA | Telehealth | CPT | * | * | * | * | TELEMED = F2F | |
| 20 | Adler-Milstein et al., 2014 (39) | USA | Telehealth | NM | * | * | * | * | TELEMED = F2F | |
| 21 | Gilman et al. 2013 (40) | USA | Telehealth | NM | * | TELEMED < F2F | ||||
| 22 | Smith et al., 2012 (41) | Australia | Tele-psychiatry | NM | * | TELEMED < F2F | ||||
| 23 | Palmas et al., 2010 (16) | USA | Remote patient monitoring for diabetes | NM | * | TELEMED = F2F | ||||
| 24 | Hilty et al., 2008(42) | USA | Tele-psychiatry | CPT | * | * | * | * | TELEMED = F2F | |
| 25 | Whitten et al., 2007 (43) | USA | Telemedicine | CPT | * | TELEMED = F2F | ||||
| 26 | Gray et al., 2006 (44) | USA | Telemedicine | CPT, HCPCS | * | TELEMED = F2F | ||||
| 27 | Palsbo, 2004 (45) | USA | Tele-rehabilitation | CPT | * | TELEMED = F2F | ||||
| 28 | Barker et al., 2001 (46) | USA | Telemedicine | CPT | * | * | * | * | TELEMED = F2F | |
a TELEMED: Telemedicine services, and F2F: Face-to-Face visits,
bThe “equals sign” indicates that the reimbursement of telemedicine services was equivalent to the face-to-face visits. Also, the “less than sign” indicates that the reimbursement for telemedicine services was lower than the face-to-face visits.
cNM: Not Mentioned
USA= United States, HCPCS= Healthcare Common Procedure Coding System, CAGR= Compound Annual Growth Rate, HTH= Home telehealth, E&M= Evaluation and Management, HAP= Health Alliance Plan, HMO= Health Maintenance Organization, CHF= Chronic Heart Failure, ICD= International Classification of Diseases, CPT= Current Procedural Terminology, ICD-9-CM= International Classification of Diseases, Clinical Modification, RPM= Remote Patient Monitoring, ADD= attention deficit disorder, ADHD= attention deficit hyperactivity disorder, RM= remote monitoring, ICD= implantable cardioverter defibrillators, MBS= Medicare Benefits Schedule
Reimbursement Methods, Telemedicine Services, and Classification Systems
In most studies, the insurances used to reimburse telemedicine services included Medicare (n = 17), Medicaid (n = 15), and private insurances (n = 13) (Table 1). In 9 studies, a combination of Medicare, Medicaid, and private insurances (combined payers) were used to reimburse telemedicine services. Only 2 studies used public insurance from the same country, such as German health insurance and the French national insurance reimbursement system (28,37).
Services provided in these studies include telepsychiatry (n = 7), telemedicine (n = 7), telehealth (n = 7), telecardiology (n = 3), telehomecare (n = 1), remote patient monitoring for diabetes (n = 1), teledermatology and teleotolaryngology (n = 1), teletoxicology (n = 1), and telerehabilitation (n = 1) (Table 1).
In 18 studies (4,16,22,24,25,26,29,30,32,33,35,38,39,42,43,44,45,46) various insurances did not differentiate between the reimbursement of telemedicine services and face-to-face (traditional) visits. Also, among the studies related to the reimbursement of telemedicine services by private insurances (n = 13), only in 4 studies the rate of reimbursement of private insurances for telemedicine services was higher compared with other insurances (38,39,43,46). In 10 studies, the reimbursement rate of telemedicine services was lower compared with face-to-face services (18,23,27,28,31,34,36,37,40,41).
In the reviewed studies, the current procedural terminology (CPT) classification system was used in 15 studies and the Healthcare Common Procedure Coding System classification system in 5 studies to code and reimburse telemedicine procedures (Table 1). In 10 studies, the type of telemedicine classification system was not mentioned (Table 1).
Discussion
The present scoping review identified and examined the reimbursement methods and insurances used for telemedicine services in previous studies. In these studies, government, federal, private, and commercial insurances were used to reimburse telemedicine services. In most of these studies, part of the telemedicine services was reimbursed by various insurances. In more than half of the studies, Medicare insurance was used to reimburse telemedicine services (4,16,22,23,25,26,27,29,30,35,36,38-42,46). Medicare is funded by the government and regulated at the federal level (47). Medicare health insurance consists of 3 parts: A (hospital insurance), B (medical insurance), and D (prescription drug coverage). In Section B of this insurance, a certain part of telehealth services is reimbursed. According to the latest policy, covered patients only have to pay 20% of the costs related to receiving telehealth services, and the rest is covered by Medicare insurance (48). In a study by Miller et al (25), between 2010 and 2018, Medicare insurance had paid the costs of $57488, $121182, and $45984763 for teleotolaryngology, teledermatology, and telepsychiatry, respectively. Wilson et al (27) also showed that 1 year after introducing the video conferencing consultation reimbursement program in Australia (2018), approximately 4141 videoconferencing consultations were reimbursed by Medicare. In the study by Palmas et al (16), the average Medicare reimbursement for telemedicine services in diabetes management ($ 9669) was almost the same compared with the traditional and face-to-face methods ($ 9040). Skinner et al (22) did not find significant differences in insurance payment between face-to-face visits and telehealth. However, in their study, a total of 8 of 90 (8.9%) visit claims were not paid by insurance, including 6 face-to-face visits (10.3%), and 2 telehealth visits (6.3%) (p = 0.43). In the study by Murray et al (23), a total of 30 encounters were billed to Medicare Part B; the average payment from them was $165.11, which is on the lower end of the range of those received from insurers. Unlike other studies, Gilman et al (40) showed that in 2009, health care providers’ acceptance and use of telemedicine services was low, based on data from Medicare insurance claims. The difference in this result may be due to the difference in the year of conducting these studies. Over time, Medicare insurance regulations and policies for reimbursement and coverage of telemedicine services have changed. This change has led to the acceptance and use of telemedicine services by health care providers and patients. Today, telemedicine services covered by Medicare insurance include all medical visits, psychotherapy, and consultations provided by an interactive 2-way telecommunications system (such as real-time audio and video) (48). Also, in 2019, Medicare insurance has provided the possibility of receiving telemedicine services such as early diagnosis and treatment of stroke, substance use disorders, and mental health disorders at home (48). At present, due to the COVID-19 pandemic, Medicare has changed its policies for telemedicine services and reimbursements (47,48). To this end, Medicare has expanded the list of eligible services, providers, geographical locations, and methods of providing telemedicine services; so that it can even cover telemedicine audio communications (47). From March 6, 2020, physicians and other health care providers will be able to provide telemedicine services to treat patients with COVID-19 and other medical purposes from offices, hospitals, and residential areas (such as homes and elderly homes). These services are reimbursed by Medicare, coinsurance, and tax deduction (48). Also, under this policy, people covered by Medicare do not pay for COVID-19 testing (48).
According to the results, Medicaid insurance was another common insurance for reimbursement of telemedicine services (4, 22, 26, 29, 30, 32-35, 38, 39, 42, 44-46). States regulate Medicaid insurance by the United States federal regulations (49). Trout et al (32) showed that according to the Center for Connected Health Policy (CCHP) reports in 2014 and 2015 in the United States, Medicaid insurance has reimbursed live video streaming services (47 states), store-and-forward services (37 states), and telemonitoring (20 states). According to their study, in only 13 states Medicaid reimbursement for live video services was similar to face-to-face services. Gray et al (44) showed that in 2003 Medicaid insurance reimbursed teleconsultation services in all US states. In another study in 2002, Medicaid reimbursed management, evaluation, and consulting services in 12 US states. This reimbursement was done for telepsychiatry in 7 states and tele speech, language pathology, physiotherapy, and occupational therapy in 4 states (45). Douglas et al (33) also showed that 95% of Medicaid insurance claims were related to the reimbursement of mental health services. The difference in telemedicine reimbursements by Medicaid in the reviewed studies could be because of the changes in policies, new federal and state annual laws to address some barriers to telemedicine use, and state-specific conditions (29,34,50). According to the CCHP report in the fall of 2020, Medicaid insurance will pay for live video conferencing services in 50 states and Washington, DC, for store and forward services in 18 states, and telemonitoring of patients in 21 states. Schmeida et al (34) have also shown that the specific conditions of the states can be an influential factor so that the states with higher internet access rates and more rural health clinics are likely to pass more comprehensive Medicaid telemedicine reimbursement laws. Today, Washington DC and all 50 states covered by Medicaid insurance offer remote access to health services to their stakeholders to reduce the risk of COVID-19. To this end, states may provide access to telehealth services concerning behavioral health, child services, reproductive and maternal services, care for people with COVID-19, dental services, speech therapy, physiotherapy, and occupational therapy for individuals covered by Medicaid insurance (51). Also, during the COVID-19 pandemic, Medicaid insurance provided reimbursement only for voice communications of telemedicine (52).
Based on the results, in some studies, only private insurance was used to reimburse telemedicine services (18,24,31,43). In the study by Wilson et al (18), the average reimbursement of private insurance for telemedicine claims per clinical diagnosis ($42) was 36% lower than conventional and nontelemedicine services ($67). In another study by Wilson et al (31), there was a declining trend in average private insurance reimbursements for telemedicine services (from $54.61 in 2009 to $43.28 in 2013). In contrast to these 2 studies, in the other 2 studies (24,43), private insurance reimbursed telemedicine services similar to traditional and conventional services and did not differentiate between these 2 health care providing methods. Differences in the results of these studies may be due to the type of reimbursement claims. For example, in 2 studies by Wilson et al (18,31), most of the claims were related to telepsychiatry services, while in the study by Whitten et al (43), the claims covered a diverse range of telemedicine services. In the present study, several reviewed studies examined the impact of private insurance on the reimbursement of telemedicine services along with other insurances such as Medicare and Medicaid (4,26,29,30,35,38,39,42,46). In the study of Lin et al (24), the 2 private insurance HAP (HAP and HAP Medicare Advantage) had the highest reimbursement for telehealth services compared with other insurances (31.3% and 60.7%, respectively). In the study by Antoniotti et al (38), telemedicine services were also routinely reimbursed through private payers. The top private insurance companies in their study were Blue Cross Blue Shield, Aetna, United Health Care, Cigna, and Humana, respectively. Barker et al (46) also found in a study that telemedicine services in Arizona were reimbursed by private insurance (29%), state plans and Medicaid (24%), Indian Health Service (17%), Medicare (13%), Self-Pay (9%), and Department of Corrections (8%), respectively. Contrary to the previous studies (26,38,46), in the study by Mehta et al (4), private payers, and federal and state insurances did not differentiate between the reimbursement of telehealth services and face-to-face visits and reimbursed an average of 94% to 107% of telehealth services at home. Differences in the results of these studies could be due to the policies and conditions of different states and the impact of different insurances on each other (35,39,42). The acceptance of telehealth services leads to the development of policies related to the reimbursement of telehealth services by private insurance (39). Neufeld et al (35) have also shown in a study that the approval of different insurances affects each other. The use of telemedicine by individuals covered by Medicare has increased dramatically with changes in the state Medicaid and private insurance policies. In a study by Hilty et al (42), the type of insurance also affected the reimbursement of telepsychiatry services. Compared with other insurances, psychiatrists visited more patients covered only by Medi-Cal (California’s Medicaid Program) or Medicare. Private insurance policies, like other state and federal insurance policies, are currently affected by the COVID-19 pandemic. In this regard, the US federal government has asked private payers to cover telehealth services for COVID-19 to minimize the spread of the virus in the community and clinics (53). Policies of private payers during the COVID-19 pandemic include increasing access to telephone and voice-only visits, increasing coverage of preventive services, providing required tests and treats, and exempting some costs of telehealth services for eligible individuals (54,55).
In the present study, the CPT and HCPCS classification systems were used in insurance claims and data reviewed by most studies (18,22-25,29-31,33,35,36,38,42-46). CPT codes and modifiers represent a claim for professional services, and HCPCS codes represent a claim for the facility fees and are considered by various public, federal, and private insurances (35). In general, common telemedicine services in Medicare insurance can include codes 99201-99215, G0425-G0427, and G0406-G0408 from the CPT and HCPCS classification systems (56). In Medicaid insurance, states can also choose between different HCPCS codes (T1014 and Q3014) and CPT codes and modifiers (GT, U1-UD) to identify, track and reimburse telehealth services (57). However, the coverage of billing codes for online video conferencing visits and nonvideo and asynchronous services by different private insurance is different (58). For example, the virtual check-in code is covered by private insurance Aetna, Cigna, Humana, and United Healthcare, but is not covered by all BlueCross plans (58). This difference has left some providers unsure about how to bill for telemedicine services (38). Providers also do not know how much private payers will reimburse if the bill is done correctly (38). Therefore, public, federal, and private insurances must develop and approve clear coding guidelines and policies appropriate to the type of service provided and state requirements to provide similar coverage for telehealth services. For example, with the outbreak of COVID-19 and the change in the conditions for providing face-to-face services, the public, federal, and some private insurances (such as United Healthcare) have covered more billing codes for the reimbursement of telehealth services (47,58).
In general, the present scoping review examined the reimbursement methods and insurances used in telemedicine services. In previous studies, various Medicare, Medicaid, and private insurances had been used to reimburse telemedicine services. The insurances used in most studies (especially Medicare and Medicaid) only cover a specific group of Americans (4,16,18,22-26,29-36,38-40,42-46) or Australians (27,41). So that Medicare insurance covers people aged 65 and over, young people with specific disabilities, and people with end-stage renal disease (59). On the other hand, Medicaid insurance covers low-income adults, children, pregnant women, the elderly, and disabled people (49). Since face-to-face visits to hospitals and medical centers can increase the risk of COVID-19 outbreaks, the physical presence of all individuals, either covered by insurance or not, is dangerous (60). Telemedicine services are a viable alternative to face-to-face visits during the COVID-19 pandemic and require changes to existing policies and guidelines for widespread use. One way to accept and use telemedicine services widely can be a temporary change in the policies concerning the insureds to help a wider range of people receive health care services outside of health care institutions during COVID-19. Therefore, health policymakers and managers are advised to develop and approve new policies and guidelines tailored to the conditions of communities for the reimbursement of telemedicine services. Based on the results of the present study, all studies were conducted in the developed country (eg, the United States, Australia, Germany, and France). Therefore, developing countries should adopt policies concerning the use of telemedicine services and their reimbursement by the insurance to be able to take full advantage of these technologies, especially during the COVID-19 pandemic.
Limitations of the Study
The present study had 2 limitations. First, out of 123 articles eligible for the full-text review, 42 articles were excluded from the study due to a lack of access to their full texts. Of these 42 omitted studies, 33 were published from 1995 to 2009. This issue might be the reason for the inaccessibility of these articles. Out of the remaining 81 articles eligible for full-text review, only 28 articles met all inclusion criteria. On the other hand, the same reimbursement methods for telemedicine services were used in most articles. Therefore, the omission of 42 without full-text studies does not seem to affect the results of this scoping review. However, future studies can consider this issue. Future studies can also conduct a systematic review of all relevant studies and perform a quality assessment stage (risk of bias) on included studies. Second, the present study excluded articles that were not published in English. Excluding these studies may lead to language bias. However, the current scoping review used a comprehensive search strategy and an additional search based on a list of study references. It seems that using this method has reduced the possibility of losing relevant articles.
Conclusion
The results of this scoping review showed that telemedicine services are reimbursed by various public, federal, state, and private insurance. In most studies, the rate of reimbursement for telemedicine services was similar to that of face-to-face services, but in some, private insurances paid more. Differences in the number of refunds in different studies may be due to the publication year of the articles, changes and updates of policies and guidelines related to covered services, and state laws’ conditions. Therefore, because of the COVID-19 pandemic, it is important to develop and update guidelines and regulations for telemedicine reimbursement by the requirements of each community. Future studies could examine methods of telemedicine reimbursement in developed and developing countries before and after the COVID-19 pandemic.
Acknowledgment
The authors are grateful to the Medical Informatics Research Center of Kerman University of Medical Sciences.
Ethical Approval
The study was approved by the Research Ethics Committee of Kerman University of Medical Sciences (Code of Ethics: IR.KMU.REC.1399.532).
Conflict of Interests
The authors declare that they have no competing interests.
Appendix
Appendix 1. Search strategy in each database .
| Name | Search strategy |
| PubMed | (Telemedicine[Title/Abstract] OR Telehealth[Title/Abstract] OR Telecare[Title/Abstract] OR Teleconsultation[Title/Abstract] OR Telemonitoring[Title/Abstract]) AND (reimbursement[Title/Abstract] OR Pay*[Title/Abstract] OR Refund*[Title/Abstract] OR insurance[Title/Abstract] OR Repay*[Title/Abstract]) Filters: English |
| Scopus | TITLE-ABS-KEY ( reimbursement OR pay* OR refund* OR insurance OR repay* ) ) AND ( TITLE-ABS-KEY ( telemedicine OR telehealth OR telecare OR teleconsultation OR telemonitoring ) ) AND ( LIMIT-TO ( DOCTYPE, “ar” ) ) AND ( LIMIT-TO ( LANGUAGE, “English” ) ) |
| Web of Sciences |
# 1 (TS=(reimbursement OR Pay* OR Refund* OR insurance OR Repay*)) AND LANGUAGE: (English) AND DOCUMENT TYPES: (Article) Indexes=SCI-EXPANDED, SSCI, A&HCI, CPCI-S, CPCI-SSH, BKCI-S, BKCI-SSH, ESCI, CCR-EXPANDED, IC Timespan=All years # 2 (TS=(Telemedicine OR Telehealth OR Telecare OR Teleconsultation OR Telemonitoring)) AND LANGUAGE: (English) AND DOCUMENT TYPES: (Article) Indexes=SCI-EXPANDED, SSCI, A&HCI, CPCI-S, CPCI-SSH, BKCI-S, BKCI-SSH, ESCI, CCR-EXPANDED, IC Timespan=All years # 3 #2 AND #1 Indexes=SCI-EXPANDED, SSCI, A&HCI, CPCI-S, CPCI-SSH, BKCI-S, BKCI-SSH, ESCI, CCR-EXPANDED, IC Timespan=All years |
Cite this article as: Salmanizadeh F, Ameri A, Bahaadinbeigy K. Methods of Reimbursement for Telemedicine Services: A Scoping Review. Med J Islam Repub Iran. 2022 (22 Jun);36:68. https://doi.org/10.47176/mjiri.36.68
References
- 1.Achenbach SJ. Telemedicine: benefits, challenges, and its great potential. Health L & Pol’y Brief. 2020;14(1):1–14. [Google Scholar]
- 2.Rogers H, Madathil KC, Agnisarman S, Narasimha S, Ashok A, Nair A, et al. A systematic review of the implementation challenges of telemedicine systems in ambulances. Telemed J E Health. 2017;23(9):707–17. doi: 10.1089/tmj.2016.0248. [DOI] [PubMed] [Google Scholar]
- 3.Kane-Gill SL, Rincon F. Expansion of telemedicine services: telepharmacy, telestroke, teledialysis, tele–emergency medicine. Crit Care Clin. 2019;35(3):519–33. doi: 10.1016/j.ccc.2019.02.007. [DOI] [PubMed] [Google Scholar]
- 4.Mehta P, Braskett M, Tam JS, Espinoza J. Reimbursement patterns and user experiences in pediatric allergy home telehealth. Ann Allergy Asthma Immunol. 2020;125:693–8. doi: 10.1016/j.anai.2020.06.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Saliba V, Legido-Quigley H, Hallik R, Aaviksoo A, Car J, McKee M. Telemedicine across borders: a systematic review of factors that hinder or support implementation. Int J Med Inform. 2012;81(12):793–809. doi: 10.1016/j.ijmedinf.2012.08.003. [DOI] [PubMed] [Google Scholar]
- 6.Gamus A, Chodick G. Costs and benefits of telemedicine compared to face-to-face treatment in patients with lower extremity ulcers. Adv Wound Care. 2019:1–31. doi: 10.1089/wound.2018.0906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Rudin RS, Auerbach DI, Zaydman M, Mehrotra A. Paying for telemedicine. Am J Manag Care. 2014;20(12):983–5. [PubMed] [Google Scholar]
- 8.Weinstein RS, Lopez AM, Joseph BA, Erps KA, Holcomb M, Barker GP, et al. Telemedicine, telehealth, and mobile health applications that work: opportunities and barriers. Am J Med. 2014;127(3):183–7. doi: 10.1016/j.amjmed.2013.09.032. [DOI] [PubMed] [Google Scholar]
- 9.Scott Kruse C, Karem P, Shifflett K, Vegi L, Ravi K, Brooks M. Evaluating barriers to adopting telemedicine worldwide: A systematic review. J Telemed Telecare. 2018;24(1):4–12. doi: 10.1177/1357633X16674087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ghani MK, Jaber MM, Suryana N. Barriers faces telemedicine implementation in the developing countries: toward building Iraqi telemedicine framework. ARPN J Eng Appl Sci. 2015;10(4):1562–7. [Google Scholar]
- 11.Rogove HJ, McArthur D, Demaerschalk BM, Vespa PM. Barriers to telemedicine: survey of current users in acute care units. Telemed J E Health. 2012;18(1):48–53. doi: 10.1089/tmj.2011.0071. [DOI] [PubMed] [Google Scholar]
- 12.Driessen J, Castle NG, Handler SM. Perceived benefits, barriers, and drivers of telemedicine from the perspective of skilled nursing facility administrative staff stakeholders. J Appl Gerontol. 2018;37(1):110–20. doi: 10.1177/0733464816651884. [DOI] [PubMed] [Google Scholar]
- 13.Lin JC, Kavousi Y, Sullivan B, Stevens C. Analysis of outpatient telemedicine reimbursement in an integrated healthcare system. Ann Vasc Surg. 2020;65:100–6. doi: 10.1016/j.avsg.2019.10.069. [DOI] [PubMed] [Google Scholar]
- 14.Brown NA. State Medicaid and private payer reimbursement for telemedicine: An overview. J Telemed Telecare. 2006;12(2_suppl):32–9. doi: 10.1258/135763306778393108. [DOI] [PubMed] [Google Scholar]
- 15.Bursell SE, Zang S, Keech AC, Jenkins AJ. Evolving telehealth reimbursement in Australia. Intern Med J. 2016;46(8):977–81. doi: 10.1111/imj.13150. [DOI] [PubMed] [Google Scholar]
- 16.Palmas W, Shea S, Starren J, Teresi JA, Ganz ML, Burton TM, et al. Medicare payments, healthcare service use, and telemedicine implementation costs in a randomized trial comparing telemedicine case management with usual care in medically underserved participants with diabetes mellitus (IDEATel) J Am Med Inform Assoc. 2010;17(2):196–202. doi: 10.1136/jamia.2009.002592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Frilling S. Medicare telehealth services and nephrology: policies for eligibility and payment. Adv Chronic Kidney Dis. 2017;24(1):46–50. doi: 10.1053/j.ackd.2016.11.003. [DOI] [PubMed] [Google Scholar]
- 18.Wilson FA, Rampa S, Trout KE, Stimpson JP. Reimbursements for telehealth services are likely to be lower than non-telehealth services in the United States. J Telemed Telecare. 2017;23(4):497–500. doi: 10.1177/1357633X16652288. [DOI] [PubMed] [Google Scholar]
- 19. World Health Organization. WHO Director-General’s opening remarks at the media briefing on COVID-19. [cited 2021 Jan 20]. Available from: https://www.who. int/dg/speeches/detail/who-director-general-s-opening-remarks-at-the-mediabriefing-on-covid-19.
- 20.Calton B, Abedini N, Fratkin M. Telemedicine in the time of coronavirus. J Pain Symptom Manage. 2020;60(1):e12–e14. doi: 10.1016/j.jpainsymman.2020.03.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Tricco AC, Lillie E, Zarin W, O’Brien KK, Colquhoun H, Levac D, et al. PRISMA extension for scoping reviews (PRISMA-ScR): Checklist and explanation. Ann Intern Med. 2018;169:467–73. doi: 10.7326/M18-0850. [DOI] [PubMed] [Google Scholar]
- 22.Skinner HJ, Casares M, Wombles C, Brooks K, Hussain A, Seo JH, et al. Comparison of care accessibility, costs, and quality with face-to-face and telehealth epilepsy clinic visits. Epilepsy Behav. 2022;127(108510):1–5. doi: 10.1016/j.yebeh.2021.108510. [DOI] [PubMed] [Google Scholar]
- 23.Murray BP, Watson A. Reimbursement for Clinical Services Provided by Ambulatory Care Pharmacists via Telehealth. J Am Coll Clin Pharm. 2021;4:959–963. [Google Scholar]
- 24.Andino JJ, Castaneda PR, Shah PK, Ellimoottil C. The impact of video visits on measures of clinical efficiency and reimbursement. Urol Pract. 2021;8:53–57. doi: 10.1097/upj.0000000000000149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Miller LE, Rathi VK, Kozin ED, Naunheim MR, Xiao R, Gray ST. Telemedicine services provided to medicare beneficiaries by otolaryngologists between 2010 and 2018. JAMA Otolaryngol Head Neck Surg. 2020;146(9):816–21. doi: 10.1001/jamaoto.2020.1911. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Lin JC, Kavousi Y, Sullivan B, Stevens C. Analysis of outpatient telemedicine reimbursement in an integrated healthcare system. Ann Vasc Surg. 2020;65:100–6. doi: 10.1016/j.avsg.2019.10.069. [DOI] [PubMed] [Google Scholar]
- 27.Wilson A, Moretto N, Langbecker D, Snoswell CL. Use of reimbursed Psychology Videoconference Services in Australia after their introduction: An investigation using administrative data. Value Health Reg Issues. 2020;21:69–73. doi: 10.1016/j.vhri.2019.07.007. [DOI] [PubMed] [Google Scholar]
- 28.Ehlert A, Oberschachtsiek D. Can telehealth reduce health care expenditure? A lesson from German health insurance data. Int J Health Plann Manage. 2019;34(4):1121–32. doi: 10.1002/hpm.2764. [DOI] [PubMed] [Google Scholar]
- 29.Yu J, Mink PJ, Huckfeldt PJ, Gildemeister S, Abraham JM. Population-level estimates of telemedicine service provision using an all-payer claims database. Health Aff. 2018;37(12):1931–9. doi: 10.1377/hlthaff.2018.05116. [DOI] [PubMed] [Google Scholar]
- 30.Crane PW, Wiegand TJ, Kamali M, Reif M, Wratni R, Montante R, et al. Telemedicine Delivery and Successful Reimbursement in Toxicology. J Med Toxicol. 2018;14(3):242–7. doi: 10.1007/s13181-018-0665-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Wilson FA, Rampa S, Trout KE, Stimpson JP. Telehealth delivery of mental health services: an analysis of private insurance claims data in the United States. Psychiatr Serv. 2017;68(12):1303–6. doi: 10.1176/appi.ps.201700017. [DOI] [PubMed] [Google Scholar]
- 32.Trout KE, Rampa S, Wilson FA, Stimpson JP. Legal mapping analysis of state telehealth reimbursement policies. Telemed J E Health. 2017;23(10):805–14. doi: 10.1089/tmj.2017.0016. [DOI] [PubMed] [Google Scholar]
- 33.Douglas MD, Xu J, Heggs A, Wrenn G, Mack DH, Rust G. Assessing telemedicine utilization by using Medicaid claims data. Psychiatr Serv. 2017;68(2):173–8. doi: 10.1176/appi.ps.201500518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Schmeida M, McNeal R. State policy action on Medicaid telemedicine reimbursement laws. Health Policy Technol. 2016;5(1):32–9. [Google Scholar]
- 35.Neufeld JD, Doarn CR, Aly R. State policies influence medicare telemedicine utilization. Telemed J E Health. 2016;22(1):70–4. doi: 10.1089/tmj.2015.0044. [DOI] [PubMed] [Google Scholar]
- 36.Neufeld JD, Doarn CR. Telemedicine spending by Medicare: a snapshot from 2012. Telemed J E Health. 2015;21(8):686–93. doi: 10.1089/tmj.2014.0185. [DOI] [PubMed] [Google Scholar]
- 37.Guédon-Moreau L, Lacroix D, Sadoul N, Clémenty J, Kouakam C, Hermida JS, et al. Costs of remote monitoring vs ambulatory follow-ups of implanted cardioverter defibrillators in the randomized ECOST study. Europace. 2014;16(8):1181–8. doi: 10.1093/europace/euu012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Antoniotti NM, Drude KP, Rowe N. Private payer telehealth reimbursement in the United States. Telemed J E Health. 2014;20(6):539–43. doi: 10.1089/tmj.2013.0256. [DOI] [PubMed] [Google Scholar]
- 39.Adler-Milstein J, Kvedar J, Bates DW. Telehealth among US hospitals: several factors, including state reimbursement and licensure policies, influence adoption. Health Aff. 2014;33(2):207–15. doi: 10.1377/hlthaff.2013.1054. [DOI] [PubMed] [Google Scholar]
- 40.Gilman M, Stensland J. Telehealth and Medicare: payment policy, current use, and prospects for growth. Medicare Medicaid Res Rev. 2013;3(4):E1–E14. doi: 10.5600/mmrr.003.04.a04. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Smith AC, Armfield NR, Croll J, Gray LC. A review of Medicare expenditure in Australia for psychiatric consultations delivered in person and via videoconference. J Telemed Telecare. 2012;18(3):169–71. doi: 10.1258/jtt.2012.SFT111. [DOI] [PubMed] [Google Scholar]
- 42.Hilty DM, Cobb HC, Neufeld JD, Bourgeois JA, Yellowlees PM. Telepsychiatry reduces geographic physician disparity in rural settings, but is it financially feasible because of reimbursement? Psychiatr Clin N Am. 2008;31(1):85–94. doi: 10.1016/j.psc.2007.11.010. [DOI] [PubMed] [Google Scholar]
- 43.Whitten P, Buis L. Private payer reimbursement for telemedicine services in the United States. Telemed J E Health. 2007;13(1):15–24. doi: 10.1089/tmj.2006.0028. [DOI] [PubMed] [Google Scholar]
- 44.Gray GA, Stamm BH, Toevs S, Reischl U, Yarrington D. Study of participating and nonparticipating states’ telemedicine Medicaid reimbursement status: Its impact on Idaho’s policymaking process. Telemed J E Health. 2006;12(6):681–90. doi: 10.1089/tmj.2006.12.681. [DOI] [PubMed] [Google Scholar]
- 45.Palsbo SE. Medicaid payment for telerehabilitation. Arch Phys Med Rehabil. 2004;85(7):1188–91. doi: 10.1016/j.apmr.2003.09.008. [DOI] [PubMed] [Google Scholar]
- 46.Barker G, Krupinski EA, Laursen T, Erps K, Weinstein RS. Pay per view: the Arizona telemedicine program’s billing results. Telemed J E Health. 2001;7(4):287–91. doi: 10.1089/15305620152814692. [DOI] [PubMed] [Google Scholar]
- 47.Kircher SM, Mulcahy M, Kalyan A, Weldon CB, Trosman JR, Benson AB. Telemedicine in oncology and reimbursement policy during covid-19 and beyond. J Natl Compr Canc Netw. 2020;1(aop):1–7. doi: 10.6004/jnccn.2020.7639. [DOI] [PubMed] [Google Scholar]
- 48. Medicare.gov. Telehealth. [cited 2021 Jan 20]. Available from: https://www.medicare.gov/coverage/telehealth.
- 49. Medicaid.gov. Medicaid. [cited 2021 Jan 20]. Available from: https://www.medicaid.gov/medicaid/index.html.
- 50. Center for Connected Health Policy. Telehealth Medicaid and state policy. [cited 2021 Jan 20]. Available from: https://www.cchpca.org/telehealth-policy/telehealth-medicaid-and-state-policy.
- 51. Guth M, Hinton E. State Efforts to Expand Medicaid Coverage & Access to Telehealth in Response to COVID-19. [cited 2021 Jan 20]. Available from: https://www.kff.org/coronavirus-covid-19/issue-brief/state-efforts-to-expand-medicaid-coverage-access-to-telehealth-in-response-to-covid-19/.
- 52. Centers for Medicare & Medicaid Services. State Medicaid & CHIP Telehealth Toolkit, Policy Considerations for States Expanding Use of Telehealth. [cited 2021 Jan 20]. Available from: https://www.medicaid.gov/medicaid/benefits/downloads/medicaid-chip-telehealth-toolkit.pdf.
- 53. American College of Physicians. COVID-19 State and Private Payer Policies. [cited 2021 Jan 20]. Available from: https://www.acponline.org/practice-resources/covid-19-practice-management-resources/covid-19-state-and-private-payer-policies.
- 54. American College of Physicians. Private payer coverage during Covid-19. [cited 2021 Jan 20]. Available from: https://www.acponline.org/system/files/documents/clinical_information/resources/covid19/payer_chart-_covid-19.pdf.
- 55. AHIP. Health Insurance Providers Respond to Coronavirus (COVID-19). [cited 2021 Jan 20]. Available from: https://www.ahip.org/health-insurance-providers-respond-to-coronavirus-covid-19/.
- 56. CMS.gov. Medicare telemedicine health care provider fact sheet. [cited 2021 Jan 20]. Available from: https://www.cms.gov/newsroom/fact-sheets/medicare-telemedicine-health-care-provider-fact-sheet.
- 57. Medicaid.gov. Telemedicine. [cited 2021 Jan 20]. From: https://www.medicaid.gov/medicaid/benefits/telemedicine/index.html.
- 58.Bajowala SS, Milosch J, Bansal C. Telemedicine pays: billing and coding update. Curr Allergy Asthma Rep. 2020;20(10):1–9. doi: 10.1007/s11882-020-00956-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Medicare.gov. What’s Medicare?. [cited 2021 Jan 20]. Available from: https://www.medicare.gov/what-medicare-covers/your-medicare-coverage-choices/whats-medicare.
- 60.Lee IK, Wang CC, Lin MC, Kung CT, Lan KC, Lee CT. Effective strategies to prevent coronavirus disease-2019 (COVID-19) outbreak in hospital. J Hosp Infect. 2020;105(1):102–103. doi: 10.1016/j.jhin.2020.02.022. [DOI] [PMC free article] [PubMed] [Google Scholar]


