Abstract
Introduction:
Chinese Americans with limited English proficiency have higher mental health needs than English speakers but are more likely to be undiagnosed and undertreated for depression. Increasing anti-Asian hate crimes during the COVID-19 pandemic has increased the urgency to accurately detect depressive symptoms in this community. This systematic review examines the validity of the Patient Health Questionnaire (PHQ)-2/9 for depression screening in Chinese-speaking populations.
Methods:
We queried PubMed, Web of Science, Embase, and PsycINFO databases, examining studies through September 2021. Studies were included if they evaluated the Chinese language PHQ-2 or PHQ-9 and diagnosed depression using a clinical interview. Two investigators independently extracted study data and assessed quality using the QUADAS-2. Study sensitivities and specificities were combined in random effects meta-analyses.
Results:
Of 513 articles, 20 met inclusion criteria. All examined the PHQ-9; seven also examined the PHQ-2. Studies were conducted in Mainland China (17), Hong Kong (1), Taiwan (1), and the United States (1). Fourteen studies were published in English; six in Chinese. Studies were diverse in setting, participant age, and comorbidities. For the Chinese language PHQ-9, Cronbach's alpha ranged from 0.765 to 0.938 for included studies (optimal cutoff scores ranged from 6 to 11). For the PHQ-2, Cronbach's alpha ranged from 0.727 to 0.785 (optimal cutoff scores 1–3). Overall, the PHQ-9 pooled sensitivity was 0.88 (95% CI 0.86–0.90), and pooled specificity was 0.87 (95% CI 0.83–0.91). Similarly, the pooled PHQ-2 sensitivity was 0.84 (95% CI 0.80–0.87), and pooled specificity was 0.87 (95% CI 0.78–0.93). The overall risk of bias was low (12 studies) or indeterminate (8 studies).
Discussion:
While limited by missing study information, the Chinese language PHQ-9 appears to be a valid depression screening tool among Chinese-speaking populations across geographic and clinical settings. Further research should explore optimal cutoff scores for this population for routine depression screening and the validity of the tool to measure response to depression treatment.
Keywords: depressive symptoms, Chinese, depression screening, language barriers, psychometrics
Introduction
Depression is a major public health concern, which affects 19.4 million adults in the United States1 and 280 million people worldwide.2 Depression leads to poor quality of life,3 worse health outcomes with increased morbidity and mortality,4,5 and increased health care costs.6 While patients with limited English proficiency (LEP) are more likely to present with more severe depressive symptoms compared with English-only speakers,7–9 clinicians are less likely to diagnose these patients with depression.10 This exacerbates existing disparities in access to mental health care among individuals with LEP.11–13
Almost 3 million U.S. residents speak Chinese at home, making it the third most spoken language in the nation.14 Past studies have found that Chinese Americans with LEP have high mental health burden, with the prevalence of depressive symptoms among Chinese monolingual primary care patients in the United States as high as 20%; however, Asian patients in the United States face disparities in mental health care access and have lower odds of receiving needed services than patients from other ethnic groups.13,15
Furthermore, Asian patients with LEP who are able to access the health care system may find that their symptoms go unrecognized compared with their English-proficient counterparts.16–19 In fact, one study of English, Spanish, and Chinese-speaking primary care patients found that physicians were least likely to diagnose depressive symptoms in Chinese-speaking patients.10 Thus, one pathway to improving access to depression treatment and specialty mental health services for Chinese patients with LEP is ensuring that physicians are using evidence-based tools to better identify patients with depressive symptoms.
Of particular note, the heightened anti-Asian racism throughout the COVID-19 pandemic has been associated with an increase in depression and anxiety in the Asian American community, further highlighting the need for physicians to screen effectively for mental health symptoms in this population.20
The Patient Health Questionnaire (PHQ)-9 has long been recognized as an effective screening instrument for depression among English-proficient adults.21 It is commonly used in primary care settings as a first-line measure for detecting depressive symptoms in adults,22 as recommended by the U.S. Preventive Services Task Force.23 The PHQ-2 is a briefer version of the PHQ-9 with similar sensitivity but higher specificity when paired with the PHQ-9 to follow up on positive screens,24 which is commonly used due to its efficiency. While the original PHQ-9 was developed and validated in English, it has since been translated and used in many other languages, including Chinese.25 However, given that the presentation of depression can vary across cultures and languages,26,27(p.1) we must determine the validity of the PHQ-2 and PHQ-9 in Chinese languages.
Two systematic reviews of Chinese language depression screening tools have been previously conducted but both had limitations that affect generalizability to our population of interest. These reviews28,29 focused on a variety of screening tools, with fewer studies specifically evaluating the PHQ-9 (a maximum of four studies in one review). Additionally, both research teams excluded studies conducted outside of China, limiting their applicability to Chinese-speaking immigrants in the United States. Both reviews included studies that compared the PHQ-9 with a variety of different instruments, including more widely used research tools such as Center for Epidemiologic Studies Depression Scale; neither conducted a clinical interview as the gold standard for diagnosis of depression. Furthermore, the systematic review by Sun et al, which concluded that the PHQ-9 was “acceptable,” was published in Chinese only, and thus remains inaccessible to English-speaking clinicians who may wish to apply this evidence to their practice.
Chiu and Chin concluded that the PHQ-9 was sensitive and “highly effective” for screening for depression in Chinese primary care; however, they only looked at articles published in English, with only four studies included in final review. Since these reviews were conducted in 2016, multiple studies evaluating the PHQ-2 and PHQ-9 have been published, warranting re-evaluation of the evidence.
We conducted a systematic review of the current literature evaluating the validity of both the Chinese language PHQ-2 and PHQ-9 for depression screening, specifically in comparison to a clinical interview as the gold standard for diagnosing depression, across geographic and practice settings.
Methods
Publication search
To find relevant articles, we performed comprehensive searches in PubMed, Web of Science, Embase, and PsycINFO databases with a university librarian (author P.T.). Searches were developed around these concepts: the PHQ-2 and PHQ-9, screening for depression and depressive disorders, and the validity and efficacy of the questionnaires, with a focus on the tool in Chinese languages. We chose to include multiple spoken Chinese languages (Mandarin, Cantonese, etc.) as written traditional/simplified Chinese does not distinguish between them and the PHQs are usually administered in written form. We used multiple synonyms for the different concepts to create sensitive searches that would not miss any eligible articles. We used both index terms (Mesh, Emtree) and keywords to develop the searches, and limited the search in PsycINFO to peer-reviewed articles (because this database includes non-peer-reviewed sources such as news articles and dissertations).
The full search strategies for each database can be found in the search appendix (Appendix A1). The initial searches were performed in December 2020, and a search update was performed in September 2021 to capture any relevant studies in the interval period. We also searched reference lists of retrieved articles and systematic reviews for relevant articles.
Study selection
Studies that met all of the following criteria were included in this systematic review: (1) participants were 16 years of age or older; (2) participants were primarily Chinese speakers of any language or dialect; (3) studies specifically examined either the PHQ-2 or PHQ-9; (4) questionnaire validity was studied for the purpose of screening specifically for major depression; (5) the questionnaire(s) studied were validated against a clinical interview as the gold standard for diagnosing depression; and (6) outcomes included biometric properties of the questionnaire(s).
We chose criterion five following best practices of diagnostic research, wherein validity studies should utilize the gold standard for comparison if one exists; in the field of psychiatry, the gold standard for depression diagnosis is the clinical interview, structured or semistructured, performed by a trained health professional or researcher. Examples include the Structured Clinical Interview for DSM (SCID), Mini-International Neuropsychiatric Interview (MINI), Composite International Diagnostic Interview (CIDI), or Schedules for Clinical Assessment in Neuropsychiatry (SCAN).30–32
We excluded studies on the basis of one or more of the following: (1) inappropriate population (e.g., children, English- or other non-Chinese language spoken); (2) studies conducting factor analysis alone; (3) inappropriate gold standard (i.e., studies evaluating the PHQ-2 or PHQ-9 against another clinical scale or questionnaire only); (4) studies examining other versions of the PHQ (e.g., PHQ-15 or PHQ-8); and (5) studies examining diagnosis or screening for disorders other than major depression, such as postpartum depression.
Two investigators (L.Y. and H.P.) reviewed the titles and abstracts for all citations to identify studies that met inclusion criteria. If the reviewers could not determine from the abstract whether a particular study met inclusion criteria, the article advanced to a full-text review. Articles that were selected for inclusion based on the title and abstract also advanced to full-text review.
Data extraction
Three investigators (L.Y., S.T., and R.L.) independently used a standardized data extraction form to collect the following: first author name, publication year, country and setting (community, outpatient clinics, inpatient), participant characteristics (age, study inclusion criteria), sample size, study design, years of study, depression screening tool (PHQ-2 and/or PHQ-9), gold standard comparison, screening tool and gold standard administration protocol (e.g., timing and blinding procedures), outcome measures, and main results (with a focus on biometric properties and internal consistency). For any missing data, if valid author contact information was available, we reached out directly to request information, allowing for a response time of 2 months. Data from articles published only in Chinese were abstracted by two bilingual investigators (L.Y. and R.L.).
Biometrics and meta-analysis
Sensitivity and specificity from the studies were combined in random effects meta-analyses separated by PHQ-9 and PHQ-2. Subgroups within these groups were analyzed by the ideal cutoff for the questionnaires (a cutoff of 10 for PHQ-9 and a cutoff of 3 for PHQ-2). Results are presented in forest plots with the random pooled effect size (sensitivity or specificity) and 95% confidence bounds. As studies did not provide complete sets of their original data, a meta-analysis could not be performed on the Cronbach's alpha or area under the curve (AUC). We, therefore, present a range of Cronbach's alpha and AUCs for the PHQ-9 and PHQ-2 for all included studies, as well as test/retest reliability for those studies with this information.
Quality assessment
Two investigators (L.Y. and S.T.) independently assessed the methodological quality of the studies using the QUADAS-2, a tool specifically developed to assess the quality of diagnostic accuracy studies included in systematic reviews. The tool investigates potential for bias in four domains: (1) patient selection, (2) index test, (3) reference standard (including blinding), and (4) flow and timing. As recommended by the tool development team,34 we made several modifications according to relevance to our research question, and classified each study as overall low, high, or indeterminate risk for bias after taking all four domains into consideration. For the full version of our modified QUADAS-2, please see Appendix A2. This systematic review is considered exempt by the University of California, San Francisco IRB criteria.
Results
Study characteristics
Our search strategy yielded 513 articles, of which 20 were included (see Fig. 1 for PRISMA flow diagram). Table 1 summarizes the characteristics of the included studies. As we were looking specifically for screening tool validation studies, all included studies had a cross-sectional design. Six studies35–39 were available only in Chinese; data were abstracted and translated by our team (L.Y., R.L.) for analysis. Seventeen studies were set in mainland China, one in Hong Kong, one in Taiwan, and one in the United States.
FIG. 1.
PRISMA flow diagram of study selection.
Table 1.
Description and Results of Included Studies
| Study | Administration | Gold standard | Setting | Participants | Biometric properties | Cronbach's αa | Blindingb/limitations | Risk of bias |
|---|---|---|---|---|---|---|---|---|
| PHQ-9 | ||||||||
| Wang et al. (2014)49 | Self | MINI; within 2 weeks | Mainland China; urban community; 2011–2012 | 1045; adults 16 and over | Ideal cutoff value: 7 Sensitivity: 0.86 Specificity: 0.86 AUCb: 0.92 [0.86–0.97] Test/retest correlation coefficient (2 weeks): 0.86c |
0.86 | Blinding is unknown. | L |
| Yuan (2019)43 | Self | MINI | Mainland China; hospital; 2013–2015 | 782; adult patients in the coronary care unit with diagnosis of Acute Coronary Syndrome | Ideal cutoff value: 10 Sensitivity: 0.869 Specificity: 0.847 AUC: 0.842 [0.806–0.894] Test/retest correlation coefficient: not reported |
0.837 | Blinded. Administration of gold standard relative to index is unknown. |
I |
| Yeung et al. (2008)25 | Self | bCB-SCID-I/P; within 4 weeks | United States; Urban outpatient clinics; 2004–2005 | 1940; adults 18 and over; Chinese Americans | Preset cutoff value: 15 Sensitivity: 0.81 Specificity: 0.98 AUC: 0.97 Test/retest correlation coefficient: Not reported |
0.91 | Not blinded. | L |
| Zhang et al. (2013)42 | Self | MINI | Hong Kong; outpatient; 2010–2011 | 586; Chinese patients between 25 and 75 years of age with type 2 diabetes | Ideal cutoff value: 7 Sensitivity: 0.826 Specificity: 0.737 AUC: 0.85 [0.76–0.94] Test/retest correlation coefficient (2–4 weeks): 0.70d |
0.86 | Blinding is unknown. Administration of gold standard relative to index is unknown. |
L |
| Ye et al. (2020)44 | Self, with personnel guidance if needed | American DSM-V; immediately | Mainland China; outpatient and inpatient; 2018 | 148; patients with psoriasis | Ideal cutoff value: 9 Sensitivity: 0.98 Specificity: 0.908 AUC: 0.979 [0.968–0.991] Test/retest correlation coefficient (1 week): 0.955c |
0.938 | Blinding is unknown. Exclusion criteria are unclear. |
I |
| Chen et al. (2013)46 | Self | SCID; within 2 weeks | Mainland China; primary care clinics; 2009–2010 | 2639; adult patients 18 and over | Ideal cutoff value: 10 Sensitivity: 0.87 Specificity: 0.81 AUC: 0.91 [0.87–0.94] Test/retest correlation coefficient (2 weeks): 0.76c |
0.89 | Blinded. 7% dropout rate. |
L |
| Du et al. (2017)48 | Self (online) | MINI; within 48 h | Mainland China; university | 230; adult university students 18 and over | Ideal cutoff value: 10 Sensitivity: 0.74 Specificity: 0.85 AUC: 0.897 [0.823–0.970] Test/retest correlation coefficient (2 weeks): 0.78e |
0.80 | Blinded. | L |
| Peng et al. (2020)45 | Self | SCID | Mainland China; outpatient; 2019 | 258; adults with acne between ages 18 and 24 | Preset cutoff value: 9 Sensitivity: 0.957 Specificity: 0.886 AUC: 0.973 [0.956–0.990] Test/retest correlation coefficient (1 week): 0.824c |
0.851 | Blinding is unknown. Administration of gold standard relative to index is unknown. 8% dropout rate. |
I |
| PHQ-2 and PHQ-9 | ||||||||
| Liu et al. (2016)40 | By postgraduate students and psychiatrists | SCID-I; immediately | Mainland China; rural community; 2010–2011 | 839; adults 60 and over | Ideal cutoff value for PHQ-9: 8 Sensitivity: 0.97 Specificity: 0.89 AUC: 0.97 [0.96–0.98] Test/retest correlation coefficient for PHQ-9: Not reported Ideal cutoff value for PHQ-2: 3 Sensitivity: 0.90 Specificity: 0.90 AUC: 0.94 [0.90–0.97] Test/retest correlation coefficient for PHQ-2: Not reported |
PHQ-9: 0.82 PHQ-2: 0.76 |
Not blinded. | L |
| Xiong (2015)47 | Self | MINI | Mainland China; outpatient clinics; 2011–2012 | 491; adults 18 and over with multiple somatic symptoms | Ideal cutoff value for PHQ-9: 10 Sensitivity: 0.77 Specificity: 0.76 AUC: 0.82 [0.77–0.86] Test/retest correlation coefficient for PHQ-9: not reported Ideal cutoff value for PHQ-2: 3 Sensitivity: 0.77 Specificity: 0.74 AUC: 0.81 [0.77–0.86] Test/retest correlation coefficient for PHQ-2: not reported |
0.90 | Blinding is unknown. Administration of gold standard relative to index is unknown. |
I |
| Zhang et al. (2013)50 | Self | SCID; within 2 weeks | Mainland China; University | 959; Chinese college students | Ideal cutoff value for PHQ-9: 11 Sensitivity: 0.89 Specificity: 0.97 AUC: 0.977 [0.966–0.988] Test/retest correlation coefficient (4 weeks) for PHQ-9: 0.873f Ideal cutoff value for PHQ-2: 3 Sensitivity: 0.81 Specificity: 0.96 AUC: 0.939 [0.911–0.967] Test/retest correlation coefficient (4 weeks) for PHQ-2: 0.829c |
PHQ-9: 0.854 PHQ-2: 0.727 |
Blinded. 13.8% dropout rate. |
L |
| Xia (2019)51 | Self | MINI; within 1 day | Mainland China; outpatient, 2018 | 213; Chinese adult patients with epilepsy | Ideal cutoff value for PHQ-9: 7 Sensitivity: 0.8286 Specificity: 0.8427 AUC: 0.888 [0.838–0.927] Test/retest correlation coefficient for PHQ-9: Not reported Ideal cutoff value for PHQ-2: 2 Sensitivity: 0.7714 Specificity: 0.7528 AUC: 0.802 [0.742–0.853] Test/retest correlation coefficient for PHQ-2: not reported |
PHQ-9: 0.86 | Blinded. | L |
| Chen (2010)53 | Self, with assistance from nurse as needed | SCID | Mainland China; primary care clinics; 2008 | 364; adult patients 60 and over | Ideal cutoff value for PHQ-9: 9 Sensitivity: 0.86 Specificity: 0.85 AUC: 0.92 [0.88–0.96] Test/retest correlation coefficient for PHQ-9: not reported Ideal cutoff value for PHQ-2: 3 Sensitivity: 0.84 Specificity: 0.90 AUC: 0.92 [0.87–0.97] Test/retest correlation coefficient for PHQ-2: not reported |
PHQ-9: 0.91 | Blinded. Administration of gold standard relative to index is unknown. 20% dropout rate. |
L |
| Liu et al. (2011)41 | Self | SCAN | Taiwan; community-based primary care clinics; 2007–2008 | 1954; adult patients 18 and over | Ideal cutoff value for PHQ-9: 10 Sensitivity: 0.86 Specificity: 0.939 AUC: 0.96 [0.93–0.98] Test/retest correlation coefficient (2 weeks): 0.87g Ideal cutoff value for PHQ-2: 2 Sensitivity: 0.88 Specificity: 0.82 AUC: 0.90 [0.85–0.95] Test/retest correlation coefficient for PHQ-2: not reported |
PHQ-9: 0.80 | Blinded. Administration of gold standard relative to index is unknown. 21.6% dropout rate. |
L |
| Studies published in Chinese language journals | ||||||||
|---|---|---|---|---|---|---|---|---|
| PHQ-9 | ||||||||
| Jin et al. (2011)39 |
Self |
SCID |
Mainland China; community |
1275; adult patients 60 and over |
Preset cutoff value: 10 Sensitivity: 0.8831 Specificity: 0.825 AUC: not reported Test/retest correlation coefficient: not reported |
0.767 |
Blinding is unknown. Administration of gold standard relative to index is unknown. |
I |
| Xu et al. (2007)38 |
Self, with guidance from family or research staff if illiterate |
SCID; within 1 week |
Mainland China; community |
622; adult patients 60 and over |
Preset cutoff value: 15 Sensitivity: 0.88 Specificity: 0.99 AUC: not reported Test/retest correlation coefficient for PHQ-9 (1 week): 0.934 |
0.8325 |
Blinding is unknown. |
I |
| Yang et al. (2015)37 |
Self |
SCID |
Mainland China; outpatient |
258; psychosomatic outpatients between 16 and 65 |
Preset cutoff value: 10 Sensitivity: 0.98 Specificity: 0.67 AUC: not reported Test/retest correlation coefficient: not reported |
Not reported |
Blinded. Administration of gold standard relative to index is unknown. |
L |
| Zhi et al. (2013)36 |
Self |
MINI; immediately |
Mainland China; outpatient |
2009; adult patients between 18 and 65 |
Ideal cutoff value: 8 Sensitivity: 0.856 Specificity: 0.802 AUC: 0.903 [0.869–0.937] Test/retest correlation coefficient: not reported |
0.855 |
Blinding is unknown. 0.6% dropout rate. |
L |
| Chen et al. (2015)35 |
Self, with personnel guidance if needed |
MINI; immediately |
Mainland China; outpatients Department of Psychiatry; 2012–2013 |
319; adult patients 18 and over |
Cutoff values reported: 6 (mild); 12 (moderate); 15 (severe) Sensitivity: not reported for mild depression; 0.94; 0.83 Specificity: not reported for mild depression; 0.82; 0.90 AUC: 0.94 Test/retest correlation coefficient: not reported |
0.89 |
Blinding is unknown. |
L |
| PHQ-2 and PHQ-9 | ||||||||
| Wang et al. (2015)33 | Self | CIDI; immediately | Mainland China; outpatients from Psycho-cardiological Department; 2013–2014 | 201; Adult patients 18 and over | Ideal cutoff value for PHQ-9: 10 Sensitivity: 0.871 Specificity: 0.835 AUC: 0.877 Test/retest correlation coefficient for PHQ-9 (1 week): 0.882h Ideal cutoff value for PHQ-2: 2 Sensitivity: 0.857 Specificity: 0.692 AUC: 0.806 Test/retest correlation coefficient for PHQ-2 (1 week): 0.813e |
PHQ-9: 0.809 PHQ-2: 0.785 |
Blinded | L |
As a measurement of internal consistency.
“Blinded” refers to the interviewers not knowing the PHQ-2 and PHQ-9 scores before conducting the clinical interview.
Conducted after 2 weeks.
Conducted after 2 weeks on 6.82% of the participants (40/586).
Conducted after 2 weeks on 65.2% of the participants (150/230).
Conducted after 4 weeks on 10% of the participants (121/959).
Conducted after 2 weeks on 13.1% of the participants (256/1954).
Conducted after 1 week on 24.9% of the participants (50/201).
ACS, Acute Coronary Syndrome; AUC, area under the curve; bCB, Chinese Bilingual version of the PHQ-9; CIDI, Composite International Diagnostic Interview; DSM-V, American Diagnostic and Statistical Manual of Mental Disorders, fifth edition; I, indeterminate; L, low; MINI, Mini International Neuropsychiatric Interview; PHQ, Patient Health Questionnaire; SCAN, Schedule for Clinical Assessments in Neuropsychiatry; SCID, Structured Clinical Interview for Diagnostic and Statistical Manual Disorders.
Across studies, we observed a wide range in sample size (n=148–2639) as well as clinical setting (primary care vs. specialty outpatient care vs. hospital inpatients). Samples ranged from patients with specific medical conditions such as cardiac disease or psoriasis, to general primary care patients, to individuals in the community. All samples consisted of patients who were Chinese speaking only, except for the study set in the United States. That study stated that the majority of their patient population were “less acculturated Chinese immigrants,” although they did not identify the proportion of their sample that truly had LEP.25
All 20 included studies examined the PHQ-9. Of these, Yeung et al utilized a bilingual (English and Chinese) PHQ-9, which the investigator team translated themselves.25 All other teams examined only the Chinese language PHQ-9; Liu et al40 utilized the Chinese portion of Yeung et al questionnaire, Liu et al41 used their own translation, Zhang et al reported that they used a translation available on the Hong Kong government website,42 and the remaining studies did not specify the version of the Chinese PHQ-9 used.
For their gold standard, nine of our included studies used the SCID, eight used the MINI, one used the SCAN, one used the CIDI, and one diagnosed subjects according to the American Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition criteria (unclear if they relied on SCID).44 For all studies, except one, the PHQ-9 was completed before the gold standard (therefore blinded to the results of the clinical interview); the remaining article, Chen et al,35 did not specify the details of the study protocol and we could not confirm the details by reaching out to the investigators. For 13 studies, we were able to identify the intervals between conducting the PHQ-9 and the gold standard, which ranged from immediate to four weeks. We were able to confirm that investigators conducting the gold standard were blinded to PHQ-9 results for 10 studies. For eight studies, only a select subset of the study sample (selected a priori) was asked to complete the gold standard for comparison.
Biometrics and meta-analysis
For the Chinese language PHQ-9, internal consistency varied across studies, with the Cronbach's alpha ranging from 0.765 to 0.938. Five studies preset a cutoff value and calculated the Chinese language PHQ-9 sensitivity/specificity using that cutoff value—two studies chose 10 as the cutoff,37,39 two studies chose 15,25,38 and one study chose 9.45 Studies that did not use a preset cutoff value and conducted receiver operating characteristic (ROC) curve analyses found that the area under the ROC curve ranged from 0.78 to 0.977. These studies identified ideal cutoff values ranging from 6 to 11, with 10 being the most common (6/15 studies).
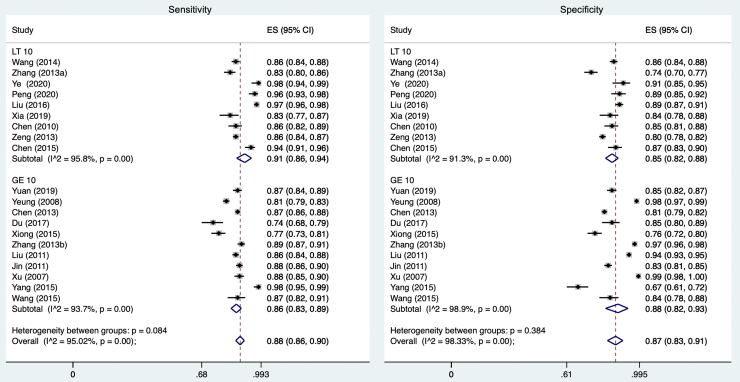
For the nine studies that identified or preset a cutoff value of less than 10, the meta-analysis demonstrated a pooled sensitivity of 0.91 (95% CI 0.86–0.94) and a pooled specificity of 0.85 (95% CI 0.82–0.88; see Fig. 2). For the eleven studies that identified or preset a cutoff value of greater than or equal to 10, the pooled sensitivity was 0.86 (95% CI 0.83–0.89) and the pooled specificity was 0.88 (95% CI 0.82–0.93). Overall, the pooled sensitivity of studies evaluating the Chinese language PHQ-9 was 0.88 (95% CI 0.86–0.90), and the pooled specificity was 0.87 (95% CI 0.83–0.91).
FIG. 2.
Meta-analyses of sensitivity (left) and specificity (right) of PHQ-9 by cutoff score. ES, effect size; LT, less than; GE, greater than or equal to; I^2=variation in effect size attributable to heterogeneity. PHQ, Patient Health Questionnaire.
Ten studies additionally analyzed the test/retest reliability for the Chinese language PHQ-9. Of these, four retested their patients after an interval of 1 week, resulting in coefficients ranging from 0.824 to 0.95538,44,45; five retested their patients after 2 weeks, resulting in coefficients ranging from 0.70 to 0.8741,42,46,48,49; and one study retested their patients after 4 weeks, resulting in a coefficient of 0.873.50
Patient health questionnaire-2
Seven of our included studies used a subset of their data to examine the Chinese language PHQ-2. Cronbach's alpha ranged from 0.727 to 0.785. The area under the ROC curve (AUC) ranged from 0.802 to 0.94. Five studies identified 3 as the ideal cutoff score; at this cutoff, the pooled sensitivity was 0.84 (95% CI 0.79–0.88) and the pooled specificity was 0.89 (95% CI 0.81–0.96; Fig. 3). For the two remaining studies that identified the ideal cutoff value as 2, the pooled sensitivity was 0.87 (95% CI 0.85–0.88) and the pooled specificity was 0.81 (95% CI 0.79–0.83). Overall, the pooled sensitivity of studies evaluating the Chinese language PHQ-2 was 0.84 (95% CI 0.80–0.87), and the pooled specificity was 0.87 (95% CI 0.78–0.93).
FIG. 3.
Meta-analyses of sensitivity (left) and specificity (right) of PHQ-2 by cutoff score.
Only two studies evaluated the test/retest reliability for the Chinese language PHQ-2. One study evaluated the reliability after 1week, resulting in a coefficient of 0.813; another study evaluated the reliability after 4 weeks, resulting in a coefficient of 0.829.42
Quality assessment
After assessment with our modified QUADAS-2 tool, none of the included studies had a high risk of bias (Table 2). Twelve included studies had a low risk of bias, while eight studies had an indeterminate risk of bias, attributed to missing key information, including whether study team members conducted the PHQ while blinded to the gold standard results or vice versa. In particular, Ye et al44 did not describe their exclusion criteria when enrolling patients; this limited our ability to evaluate, for example, how much of their sample had pre-existing psychiatric illness that would invoke bias when studying the efficacy of a depression screening tool.
Table 2.
Quality Assessment Details of Included Studies
| Question | Wang et al. (2014)49 | Yuan (2019)43 | Yeung et al. (2008)25 | Zhang et al. (2013)50 | Ye et al. (2020)44 | Chen et al. (2013)46 | Du et al. (2017)48 |
|---|---|---|---|---|---|---|---|
| Overall risk of bias | Low | Indeterminate: unknown interval between test and reference standard | Low | Low | Indeterminate: no description of exclusion criteria, unknown blinding protocol | Low | Low |
| Was a consecutive or random sample of patients enrolled? | Yes: probability proportionate to size sampling and simple random sampling | Yes: consecutive | Yes: consecutive | Yes: consecutive | Yes: consecutive | Yes: random | University student email list—unclear if truly random |
| Was a case/control design avoided? | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Did the study avoid inappropriate exclusions? | Yes | Yes: illness preventing completion, previous history of mental illness or psychotherapy, unwilling | Yes | Yes: disabling disease or reduced life expectancy, difficulty communicating | Information not found | Yes: patients with psychotic disorders | Yes |
| Were the index testa results interpreted without knowledge of the results of the reference standardb? | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Are the specificity and sensitivity recorded for multiple cutoff scores? | Yes | Yes | No: only one (15) | Yes | Yes | Yes | Yes |
| Was the index test administered in a standardized fashion? | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Was an appropriate version of the index test used? | Information not found | Information not found | Yes: translated by investigators | Yes: translation on Hong Kong government website | Information not found | Information not found | Information not found |
| Is the reference standard likely to correctly classify the target condition? | Yes: MINI | Yes: MINI | Yes: SCID | Yes: MINI | Yes: DSM-V | Yes: SCID | Yes: MINI |
| Were the reference standard results interpreted without knowledge of the results of the index test? | Information not found | Yes | No: SCID conducted for all patients with PHQ-9≥15 and 8% of patients with PHQ-9<15 | Yes | Information not found | Yes | Yes |
| Was the reference standard administered in a standardized fashion? | Yes: one interviewer | Yes: standardized training | Yes: one interviewer | Yes | Yes: one interviewer | Yes: two psychiatrists with interrater reliability 0.81 | Yes: two psychiatrists |
| Was there an appropriate interval between index tests and reference standard? | Yes: <2 weeks | Information not found | No: “about 4 weeks” | No: “within 2–4 weeks” | Yes: immediate | Yes: 2 weeks | Yes: within 48 h |
| Did all patients receive a reference standard? | Yes | Yes | No: subsample analysis | No: subsample analysis | Yes | No: subsample analysis | No: subsample analysis |
| Did patients receive the same reference standard? | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Were all patients included in the analysis without a significant percentage of dropouts? | Yes: 0% dropout rate (1045/1045) | Yes: 0% dropout rate (782/782) | Yes: 0% dropout rate (1940/1940) | Yes: 0% dropout rate (586/586) | Yes: 0% dropout rate (148/148) | Yes: 7% dropout rate (280/300) | Yes: 0% dropout rate (230/230) |
| Question | Peng et al. (2020)45 | Liu et al. (2016)40 | Xiong (2015)47 | Zhang et al. (2013)50 | Xia (2019)51 | Chen (2010)53 | Liu et al. (2011)41 |
|---|---|---|---|---|---|---|---|
| Overall risk of bias |
Indeterminate: unknown blinding protocol, interval between test and reference standard |
Low |
Indeterminate: unknown blinding protocol, interval between test and reference standard |
Low |
Low |
Low |
Low |
| Was a consecutive or random sample of patients enrolled? |
Yes: consecutive |
Yes: study province → random towns → random villages → all individuals |
Yes: on randomly assigned days, patients consecutively invited |
Yes |
Yes: consecutive |
Yes: consecutive |
Yes: consecutive |
| Was a case/control design avoided? |
Yes |
Yes |
Yes |
Yes |
Yes |
Yes |
Yes |
| Did the study avoid inappropriate exclusions? |
Yes: patients with pre-existing mental illness, severe physical illness |
Yes: if not in area during study period or difficulty with communication due to illness |
Yes: wrong language, limited writing skills, cognitive impairment, psychosis, acute suicidality |
Yes |
Yes: severe psychiatric disorders or antisocial, schizotypal personality disorders |
Yes |
Yes |
| Were the index testa results interpreted without knowledge of the results of the reference standardb? |
Yes |
Yes |
Yes |
Yes |
Yes |
Yes |
Yes |
| Are the specificity and sensitivity recorded for multiple cutoff scores? |
No: only one (9) |
Yes |
Yes |
Yes |
Yes |
Yes |
Yes |
| Was the index test administered in a standardized fashion? |
Yes |
Yes |
Yes |
Yes |
Yes |
Yes |
Yes |
| Was an appropriate version of the index test used? |
Information not found |
Yes: cited Yeung et al. 2008 |
Information not found |
Information not found |
Information not found |
Information not found |
Yes: study team translated and back translated |
| Is the reference standard likely to correctly classify the target condition? |
Yes: SCID |
Yes: SCID |
Yes: MINI |
Yes: SCID |
Yes: MINI |
Yes: SCID |
Yes: SCAN |
| Were the reference standard results interpreted without knowledge of the results of the index test? |
Information not found |
No: SCID conducted immediately after PHQ-9 by same interviewer |
Information not found |
Yes |
Yes |
Yes |
Yes |
| Was the reference standard administered in a standardized fashion? |
Yes: two psychiatrists |
Yes: standardized interview training |
Yes |
Yes: standardized training |
Yes: one interviewer |
Yes: two psychiatrists |
Yes: trained staff with 0.88 interrater reliability |
| Was there an appropriate interval between index tests and reference standard? |
Information not found |
Yes: immediate |
Information not found |
Yes: <2 weeks |
Yes: <24h |
Information not found |
Information not found |
| Did all patients receive a reference standard? |
Yes |
Yes |
Yes |
Yes |
Yes |
No: subsample analysis |
Yes |
| Did patients receive the same reference standard? |
Yes |
Yes |
Yes |
Yes |
Yes |
Yes |
Yes |
| Were all patients included in the analysis without a significant percentage of dropouts? | Yes: 8% dropout rate (275/300) | Yes: 0.7% dropout rate (839/845) | Yes: 0% dropout rate (491/491) | Significant: 13.8% dropout rate (959/1112) | Yes: 0% dropout rate (213/213) | Significant: 20% dropout rate (77/96) for subsample chosen to undergo reference standard | Significant: 21.6% dropout rate, however, sample was large (1532/1954) |
| Question | Jin et al. (2011)39,c | Xu et al. (2007)38,c | Yang et al. (2015)37,c | Zhi et al. (2013)36,c | Chen (2015)35,c | Wang et al. (2015)33,c | |
|---|---|---|---|---|---|---|---|
| Overall risk of bias |
Indeterminate: unknown blinding protocol, interval between test and reference standard |
Low |
Low |
Low |
Low |
Low |
|
| Was a consecutive or random sample of patients enrolled? |
Yes: random |
Yes: random |
Yes: consecutive |
Yes: consecutive |
Yes |
Yes: consecutive |
|
| Was a case/control design avoided? |
Yes |
Yes |
Yes |
Yes |
Yes |
Yes |
|
| Did the study avoid inappropriate exclusions? |
Yes: dementia or physically incapable of completing questionnaire |
Yes |
Yes: incapable of understanding and responding to questionnaire, severe mental health symptoms or physical disability, substance use disorders, currently receiving medication or therapy treatment for mental illness |
Yes: physically incapable of completing questionnaire, severe physical or mental illness |
Yes: those incapable of completing study or consent due to language or hearing |
Yes |
|
| Were the index test results interpreted without knowledge of the results of the reference standard? |
Yes |
Yes |
Yes |
Yes |
Information not found |
Yes |
|
| Are the specificity and sensitivity recorded for multiple cutoff scores? |
No: only one (10) |
No: only one (15) |
No: only one (10) |
Yes |
Yes |
Yes |
|
| Was the index test administered in a standardized fashion? |
Yes |
Yes |
Yes |
Yes |
Yes |
Yes |
|
| Was an appropriate version of the index test used? |
Information not found |
Information not found |
Information not found |
Information not found |
Information not found |
Yes: cited Liu 2011's translation |
|
| Is the reference standard likely to correctly classify the target condition? |
Yes: SCID |
Yes: SCID |
Yes: SCID |
Yes: MINI |
Yes: MINI |
Yes: CIDI |
|
| Were the reference standard results interpreted without knowledge of the results of the index test? |
Information not found |
Information not found |
Yes |
Information not found |
Information not found |
Yes |
|
| Was the reference standard administered in a standardized fashion? |
Yes: standardized training |
Yes: two psychiatrists |
Yes: standardized training |
Yes: standardized training |
Yes |
Yes: one interviewer |
|
| Was there an appropriate interval between index tests and reference standard? |
Information not found |
Yes: 1 week |
Information not found |
Yes: immediate |
Yes: immediate |
Yes: immediate |
|
| Did all patients receive a reference standard? |
No: subsample analysis |
No: subsample analysis |
No: subsample analysis |
Yes |
Yes |
Yes |
|
| Did patients receive the same reference standards? |
Yes |
Yes |
Yes |
Yes |
Yes |
Yes |
|
| Were all patients included in the analysis without a significant percentage of dropouts? | Yes: 0% dropout rate (117/117) | Yes: 0% dropout rate (195/195) | Yes: 0% dropout rate (97/97) | 0.6% dropout rate (1997/2009) | Yes: 0% dropout rate (319/319) | Yes: 0% dropout rate (201/201) | |
Index test=PHQ.
Reference standard=old standard clinical interview used by the particular study.
Study published in Chinese.
Discussion
In this systematic review, we found that the available literature supports the use/validity of the Chinese PHQ-9 and PHQ-2 as a tool for screening for depression in monolingual Chinese patients. We found high sensitivity and specificity for depression for both the PHQ-2 and PHQ-9 among individuals who spoke Chinese languages, across a variety of clinical settings and with a range of clinical comorbidities. Our findings are consistent with the two previous systematic reviews that have been conducted in this area. Our review has unique strengths, including a greater number of studies, comparison to gold standard clinical interviews as an inclusion criterion, studies encompassing broad geographic settings and patient populations and, therefore, better generalizability, and examination of both English- and Chinese-language articles.
The studies included in our review that evaluated the validity of the Chinese PHQ-9 at multiple cutoff scores identified different ideal cutoffs, ranging from 6 to 11, with 10 identified as the optimal cutoff score in 6 of 15 studies. This is consistent with how the PHQ-9 is currently used in primary care settings, with a score of 10 as the cutoff for a positive screen across languages.21 Notably, it is also comparable to the English language PHQ-9 at this cutoff.52 However, not all studies in our review agreed on this cutoff, with many identifying lower scores as the optimal cutoff for diagnosing depression. This points to the need for further investigation to ensure that we are not missing depression in Chinese patients with LEP, who are already at high risk of depression under-recognition and undertreatment.
Additionally, the English language PHQ-9 can also be used to evaluate symptom severity, with scores of 5, 10, 15, and 20 indicating mild, moderate, moderately severe, and severe depression, respectively.21 Of the studies we found, only Chen et al identified score cutoffs for different levels of symptom severity: 6, 12, and 15 for mild, moderate, and severe depression.34 Yeung et al indirectly acknowledged this by setting the cutoff for a positive screen at the higher score of 15 instead of 10, to identify subjects whose depression was significant enough to warrant treatment; Xu et al also set their cutoff at 15 and did not state their justification, but presumably had similar reasoning.25,38 Although our review did not explicitly address this question, for providers who wish to use the PHQ-9 to monitor response to treatment, further research could help confirm ideal cutoffs for depression symptom severity.
Less than half the articles we found evaluated the PHQ-2 in addition to the PHQ-9; all seven of these articles validated the PHQ-2 as a screening tool, with four out of seven studies agreeing on 3 as the best cutoff value for screening positive for depression, as is used for the English language PHQ-2.
We recognize several limitations to our systematic review. First, despite a rigorous search for relevant articles, it is possible that some were missed; in particular, although we were able to include six Chinese language studies that were identified through our search, we did not specifically examine the Chinese language literature or databases and may have missed studies that were published only in Chinese. However, as our purpose is to apply these findings to monolingual Chinese speakers in the United States, we felt it was appropriate to limit to Chinese language articles in English language databases for this review.
Second, we did not target any specific practice setting for our search; our ability to make strong recommendations for clinicians may thus be limited by the variability in patient comorbidities or countries of residence among the included studies. However, the broad range of populations represented in our review improves generalizability for the PHQ-2/9 as a broad screening tool. Third, although our search was internationally targeted, most studies that fit our inclusion criteria were conducted in mainland China.
Although a single study was conducted in the United States, Yeung et al, similarly found high sensitivity and specificity, the dearth of studies around the use of the Chinese PHQ in settings with patient/provider language discordance points to the need for more research in this direction. In the United States, while Asian Americans account for 5.7% of the population, less than 1% of National Institutes of Health funding goes to research on Asian American health.54 Additionally, for immigrant populations, the preferred language is frequently used as a measure of acculturation55; U.S. patients preferring the Chinese language PHQ are therefore more likely to be recent immigrants and/or less acculturated to the United States, implying some crossapplicability to research conducted with nondiasporic Chinese patients. Fourth, the quality of the diagnoses made through clinical interviews may vary depending on the individual investigator and the specific clinical interview used, which could affect the internal validity of our included studies.
Fifth, as the PHQ-2 and PHQ-9 are usually given as written questionnaires, we did not choose to distinguish between the various dialects of spoken Chinese (as all literate speakers read the same written form). However, in studies where some questionnaires were verbally administered by a research assistant, variation between the spoken dialects may have impacted tool validity. Finally, although we contacted study authors when possible to inquire about missing information, in several cases, we were unable to ascertain the exact translation of the Chinese PHQ-9 or PHQ-2 used, whether the studies appropriately excluded patients with pre-existing psychiatric illness, or whether the investigators were double blinded to the PHQ and gold standard results. This particularly impacted our evaluation of the six studies published only in Chinese, which did not provide contact information for the study authors.
Conclusion
Chinese patients with LEP and depression are more likely to be underdiagnosed and undertreated, leading to worse health outcomes and quality of life. As the mental health burden for the Asian American community has increased during the COVID-19 pandemic with the rise in racism and violence, it is more urgent than ever for us to ensure we are using the right tools to identify patients with depression. Despite the limitations of our review, we found strong evidence supporting the accuracy of Chinese language versions of the PHQ-9 and PHQ-2 for screening for depression across practice settings. However, studies reported a wide range of cutoff scores for the PHQ-9, with many demonstrating high sensitivity and specificity at lower cutoff scores, alluding to the possibility that the ideal cutoff score for Chinese monolingual patients may differ from the score used for English speakers. If so, the PHQ-9 as currently used in practice may miss depressive symptoms in some Chinese monolingual patients.
To effectively address mental health disparities for patients with LEP in the United States, more research is necessary to investigate this possibility specifically among Chinese monolingual patients living in the United States and to establish the validity of depression screening tools in other commonly spoken non-English languages. Finally, once the research is robust, medical institutions and professional bodies must standardize the uptake of evidence-based depression screening tools and interventions to truly impact patient care.
Acknowledgment
The authors wish to thank Dr. Isabel Elaine Allen for conducting the meta-analyses.
Abbreviations Used
- SCID
Structured Clinical Interview for DSM
- MINI
Mini-International Neuropsychiatric Interview
- CIDI
Composite International Diagnostic Interview
- SCAN
Schedules for Clinical Assessment in Neuropsychiatry
- AUC
area under the curve
- DSM-V
American Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition
- ROC
receiver operating characteristic
- PHQ
Patient Health Questionnaire
- LEP
limited English proficiency
Appendix
Appendix A1.
PHQ-9 PHQ-2 Questionnaire Chinese: Search Appendix
| DATABASE | SEARCH STRATEGY |
|---|---|
| PubMed | (“PHQ-9” OR “PHQ-2” OR “patient health questionnaire-9” OR “patient health questionnaire-2” OR “Patient Health Questionnaire”[Mesh]) AND (“Depression/diagnosis”[Mesh] OR depression screening OR depression assessment OR “Depressive Disorder/diagnosis”[Mesh] OR depressive disorder screening OR depressive disorder assessment) AND (efficacy OR reliability OR validity OR utility OR “Validation Studies as Topic”[Mesh]) AND (Cantonese OR Mandarin OR Vietnamese OR Chinese OR China OR “China”[Mesh] OR Taiwan OR “Taiwan”[Mesh] OR Vietnam OR “Vietnam”[Mesh]) |
| Web of Science | (“PHQ-9” OR “PHQ-2” OR “patient health questionnaire-9” OR “patient health questionnaire-2”) AND (“Depression diagnosis” OR depression screening OR depression assessment OR depressive disorder screening OR depressive disorder assessment) AND (efficacy OR reliability OR validity OR utility) AND (Cantonese OR Mandarin OR Vietnamese OR Chinese OR China OR Taiwan OR Vietnam) |
| Embase | (‘patient health questionnaire 2′/exp OR ‘patient health questionnaire 2′ OR ‘patient health questionnaire 9′/exp OR ‘patient health questionnaire 9′) AND (‘depression’/exp/dm_di OR ‘depression assessment’ OR ‘depression screening’) AND (‘efficacy parameters’/exp OR ‘efficacy parameters' OR ‘efficacy’/exp OR efficacy OR ‘validity’/exp OR validity OR ‘reliability’/exp OR reliability OR utility) AND (‘chinese’/exp OR chinese OR ‘cantonese language’/exp OR ‘cantonese language’ OR ‘cantonese’/exp OR cantonese OR ‘mandarin’/exp OR mandarin OR ‘mandarin language’/exp OR ‘mandarin language’ OR ‘vietnamese’/exp OR Vietnamese OR ‘china’/exp OR china OR ‘viet nam’/exp OR ‘viet nam’ OR ‘taiwan’/exp OR taiwan) |
| PsycINFO | (“PHQ-9” OR “PHQ-2” OR “patient health questionnaire-9” OR “patient health questionnaire-2”) AND (“Depression diagnosis” OR depression screening OR depression assessment OR depressive disorder screening OR depressive disorder assessment) AND (efficacy OR reliability OR validity OR utility) AND (Cantonese OR Mandarin OR Vietnamese OR Chinese OR China OR Taiwan OR Vietnam) |
Appendix A2. QUADAS 2 Tool
Modified by Leena Yin & Dr. Maria Garcia
This tool is a modified version of the QUADAS 2 (https://www.bristol.ac.uk/population-health-sciences/projects/quadas/quadas-2/), developed by a team led by the University of Bristol as a method of assessing quality and risk of bias in systematic reviews. Major modifications for our review included the following:
-The original QUADAS 2 included two parts under each domain: part 1 addressing internal validity, and part B addressing external validity. As we have selected our studies carefully based on applicability to our study population as part of the search criteria, we felt it reasonable to remove part 2 from this portion of the analysis. Considerations for external validity will be included in the discussion.
-Three questions were added, and one was modified, based on applicability to our review.
-Taking each of the four domains into consideration, we classified each study as overall low, high, or unclear risk for bias.
For all main questions, respond with low/high/unclear risk
For all subquestions, respond with yes/no/unclear
Domain 1: Patient Selection
Could the selection of patients have introduced bias?
-
A.
Was a consecutive or random sample of patients enrolled?
-
B.
Was a case-control design avoided?
-
C.
Did the study avoid inappropriate exclusions?
Domain 2: Index Tests
Could the conduct or interpretation of the index test have introduced bias?
-
A.
Were the index test results interpreted without knowledge of the results of the reference standard? (may need to ask the authors)
-
B.
(modified) Are the specificity and sensitivity recorded for multiple cutoff scores?
-
C.
(new) Was the index test administered in a standardized fashion?
-
D.
(new) Was an appropriate version of the index test used?
Domain 3: Reference Standard
Could the reference standard, its conduct, or its interpretation have introduced bias?
-
A.
Is the reference standard likely to correctly classify the target condition?
-
B.
Were the reference standard results interpreted without knowledge of the results of the index test?
-
C.
(new) Was the reference standard administered in a standardized fashion?
Domain 4: Flow and Timing
Could the patient flow have introduced bias?
-
A.
Was there an appropriate interval between index tests and reference standard (<1 month)?
-
B.
Did all patients receive a reference standard?
-
C.
Did patients receive the same reference standard?
-
D.
Were all patients included in the analysis?
Authors' Contributions
L.Y,: Conceptualization, investigation, visualization, and writing—original draft preparation. S.T.: Investigation and visualization. H.P.: Investigation. R.L.: Investigation. P.T.: Methodology and writing—reviewing and editing. M.G.: Supervision, Conceptualization, depression-screening tools and Writing—Reviewing and Editing.
Author Disclosure Statement
No competing financial interests exist.
Funding Information
Dr. Garcia received support through a National Institute on Minority Health and Health Disparities (NIMHD) K23MD015115; the content does not necessarily represent the official views of the NIMHD or the National Institutes of Health (NIH).
Cite this article as: Yin L, Teklu S, Pham H, Li R, Tahir P, Garcia ME (2022) Validity of the Chinese-language patient health questionnaire 2 and 9: a systematic review, Health Equity 6:1, 574–594, DOI: 10.1089/heq.2022.0030.
References
- 1. NIMH Information Resource Center. Major Depression. National Institute of Mental Health; 2021. Available from: https://www.nimh.nih.gov/health/statistics/major-depression#part_2562 [Last accessed: December 10, 2021].
- 2. World Health Organization. Depression. World Health Organization; 2021. Available from: https://www.who.int/news-room/fact-sheets/detail/depression [Last accessed: December 10, 2021].
- 3. Vos T, Flaxman AD, Naghavi M, et al. Years lived with disability (YLDs) for 1160 sequelae of 289 diseases and injuries 1990–2010: A systematic analysis for the global burden of disease study 2010. Lancet 2012;380(9859):2163–2196; doi: 10.1016/S0140-6736(12)61729-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. de Groot M, Anderson R, Freedland KE, et al. Association of depression and diabetes complications: A meta-analysis. Psychosom Med 2001;63(4):619–630; doi: 10.1097/00006842-200107000-00015. [DOI] [PubMed] [Google Scholar]
- 5. Hofmann M, Köhler B, Leichsenring F, et al. Depression as a risk factor for mortality in individuals with diabetes: A meta-analysis of prospective studies. PLoS One 2013;8(11):e79809; doi: 10.1371/journal.pone.0079809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Egede LE, Zheng D, Simpson K. Comorbid depression is associated with increased health care use and expenditures in individuals with diabetes. Diabetes Care 2002;25(3):464–470; doi: 10.2337/diacare.25.3.464. [DOI] [PubMed] [Google Scholar]
- 7. Jang Y, Yoon H, Park NS, et al. Health vulnerability of immigrants with limited English proficiency: A study of older Korean Americans. J Am Geriatr Soc 2016;64(7):1498–1502; doi: 10.1111/jgs.14199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Ponce NA, Hays RD, Cunningham WE. Linguistic disparities in health care access and health status among older adults. J Gen Intern Med 2006;21(7):786–791; doi: 10.1111/j.1525-1497.2006.00491.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Kim G, Kim M, Park S, et al. Limited English proficiency and trajectories of depressive symptoms among Mexican American older adults. Gerontologist 2019;59(5):856–864; doi: 10.1093/geront/gny032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Leng JCF, Changrani J, Tseng CH, et al. Detection of depression with different interpreting methods among Chinese and Latino primary care patients: A randomized controlled trial. J Immigr Minor Health 2010;12(2):234–241; doi: 10.1007/s10903-009-9254-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Sentell T, Shumway M, Snowden L. Access to mental health treatment by English language proficiency and race/ethnicity. J Gen Intern Med 2007;22(Suppl 2):289–293; doi: 10.1007/s11606-007-0345-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Bauer AM, Chen CN, Alegría M. English language proficiency and mental health service use among Latino and Asian Americans with mental disorders. Med Care 2010;48(12):1097–1104; doi: 10.1097/MLR.0b013e3181f80749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Abe-Kim J, Takeuchi DT, Hong S, et al. Use of mental health–related services among Immigrant and US-Born Asian Americans: Results From the National Latino and Asian American Study. Am J Public Health 2007;97(1):91–98; doi: 10.2105/AJPH.2006.098541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Ryan C. Language Use in the United States: 2011. United States Census Bureau; 2010. Available from: https://www.census.gov/library/publications/2013/acs/acs-22.html [Last accessed: December 11, 2021].
- 15. Cook BL, Trinh NH, Li Z, et al. Trends in racial-ethnic disparities in access to mental health care, 2004–2012. Psychiatr Serv 2017;68(1):9–16; doi: 10.1176/appi.ps.201500453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Garcia ME, Hinton L, Gregorich SE, et al. Unmet mental health need among chinese and latino primary care patients: Intersection of ethnicity, gender, and english proficiency. J Gen Intern Med 2020;35(4):1245–1251; doi: 10.1007/s11606-019-05483-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Yeung A, Chan R, Mischoulon D, et al. Prevalence of major depressive disorder among Chinese-Americans in primary care. Gen Hosp Psychiatry 2004;26(1):24–30; doi: 10.1016/j.genhosppsych.2003.08.006. [DOI] [PubMed] [Google Scholar]
- 18. Chung H, Teresi J, Guarnaccia P, et al. Depressive symptoms and psychiatric distress in low income Asian and Latino primary care patients: Prevalence and recognition. Community Ment Health J 2003;39(1):33–46; doi: 10.1023/a:1021221806912. [DOI] [PubMed] [Google Scholar]
- 19. Garcia ME, Hinton L, Gregorich SE, et al. Primary care physician recognition and documentation of depressive symptoms among Chinese and Latinx patients during routine visits: A cross-sectional study. Health Equity 2021;5(1):236–244; doi: 10.1089/heq.2020.0104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Zhou S, Banawa R, Oh H. The Mental Health Impact of COVID-19 racial and ethnic discrimination against Asian American and Pacific Islanders. Front Psychiatry 2021;12:708426; doi: 10.3389/fpsyt.2021.708426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Kroenke K, Spitzer RL, Williams JB. The PHQ-9: Validity of a brief depression severity measure. J Gen Intern Med 2001;16(9):606–613; doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Maurer DM, Raymond TJ, Davis BN. Depression: Screening and diagnosis. Am Fam Physician 2018;98(8):508–515. [PubMed] [Google Scholar]
- 23. Siu AL, and the US Preventive Services Task Force (USPSTF). Screening for depression in adults: US preventive services task force recommendation statement. JAMA 2016;315(4):380–387; doi: 10.1001/jama.2015.18392. [DOI] [PubMed] [Google Scholar]
- 24. Levis B, Sun Y, He C, et al. Accuracy of the PHQ-2 alone and in combination with the PHQ-9 for screening to detect major depression. JAMA 2020;323(22):2290–2300; doi: 10.1001/jama.2020.6504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Yeung A, Fung F, Yu SC, et al. Validation of the patient health questionnaire-9 for Depression Screening Among Chinese Americans. Compr Psychiatry 2008;49(2):211–217; doi: 10.1016/j.comppsych.2006.06.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Goodmann DR, Daouk S, Sullivan M, et al. Factor analysis of depression symptoms across five broad cultural groups. J Affect Disord 2021;282:227–235; doi: 10.1016/j.jad.2020.12.159. [DOI] [PubMed] [Google Scholar]
- 27. Dere J, Sun J, Zhao Y, et al. Beyond “somatization” and “psychologization”: Symptom-level variation in depressed Han Chinese and Euro-Canadian outpatients. Front Psychol 2013;4:377; doi: 10.3389/fpsyg.2013.00377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Sun X, Li Y, Yu C, et al. Reliability and validity of depression scales of Chinese version: A systematic review. Chin J Endemiol 2017;38(1):110–116; doi: 10.3760/cma.j.issn.0254-6450.2017.01.021. [DOI] [PubMed] [Google Scholar]
- 29. Chiu CFB, Chin WY. Systematic review and meta-analysis on the patient health questionnare-9 (PHQ-9) for depression screening in Chinese primary care patients. Fam Med Care 2018;1(1); doi: 10.15761/FMC.1000105. [DOI] [Google Scholar]
- 30. Sheehan DV, Lecrubier Y, Sheehan KH, et al. The mini-international neuropsychiatric interview (M.I.N.I.): The development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. J Clin Psychiatry 1998;59 Suppl 20:22–33; quiz 34–57. [PubMed] [Google Scholar]
- 31. Gelenberg AJ. Using assessment tools to screen for, diagnose, and treat major depressive disorder in clinical practice. J Clin Psychiatry 2010;71(suppl E1):26567; doi: 10.4088/JCP.9058se1c.01gry. [DOI] [PubMed] [Google Scholar]
- 32. Cheng ATA, Tien AY, Chang CJ, et al. Cross-cultural implementation of a Chinese version of the schedules for clinical assessment in Neuropsychiatry (SCAN) in Taiwan. Br J Psychiat 2001;178(6):567–572; doi: 10.1192/bjp.178.6.567. [DOI] [PubMed] [Google Scholar]
- 33. Wang L, Lu K, Li J, Sheng L, Ding R, Hu D. [Value of patient health questionnaires (PHQ)-9 and PHQ-2 for screening depression disorders in cardiovascular outpatients]. Zhonghua Xin Xue Guan Bing Za Zhi. 2015. May;43(5):428–431. Chinese. [PubMed] [Google Scholar]
- 34. QUADAS-2: A revised tool for the quality assessment of diagnostic accuracy studies. Annals of Internal Medicine. Accessed February 19, 2022. Available from: https://www.acpjournals.org/doi/10.7326/0003-4819-155-8-201110180-00009 [Last accessed: February 19, 2021]. [DOI] [PubMed]
- 35. Chen MM, Sheng L, Qu S. Diagnostic test of screening depressive disorders in general hospital with the patient health questionnaire. Chin Mental Health J 2015;(4):241–245. [Google Scholar]
- 36. Zhi ZQ, Liu H, Ming MJ, et al. Screening value of the patient health questionnaire depression scale in outpatients from traditional Chinese internal department. J Clin Psychiatry 2013;23(4):229–232. [Google Scholar]
- 37. Yang H, Yan D, Li X, et al. Application of patient health questionnaire-9 in psychosomatic disease outpatients in a general hospital. Chin J Behav Med Brain Sci 2015;24(5):473–476. [Google Scholar]
- 38. Xu Y, Wu H, Xu Y. The reliability and validity of patient health questionnaire depression module (PHQ-9) in Chinese elderly. Shanghai Arch Psychiatry 2007;19(5):257–276. [Google Scholar]
- 39. Jin T, Chen S lin, Shen Y. The reliability and validity of the patient health questionnaire depression scale (PHQ-9) in the elderly population in community. Zhejiang Yufang Yixue 2011;6(23):27–29. [Google Scholar]
- 40. Liu Z wei, Yu Y, Hu M, et al. PHQ-9 and PHQ-2 for screening depression in Chinese rural elderly. PLoS One 2016;11(3):e0151042; doi: 10.1371/journal.pone.0151042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Liu SI, Yeh ZT, Huang HC, et al. Validation of patient health questionnaire for depression screening among primary care patients in Taiwan. Compr Psychiatry 2011;52(1):96–101; doi: 10.1016/j.comppsych.2010.04.013. [DOI] [PubMed] [Google Scholar]
- 42. Zhang Y, Ting R, Lam M, et al. Measuring depressive symptoms using the patient health questionnaire-9 in Hong Kong Chinese subjects with type 2 diabetes. J Affect Disord 2013;151(2):660–666; doi: 10.1016/j.jad.2013.07.014. [DOI] [PubMed] [Google Scholar]
- 43. Yuan J, Ding R, Wang L, Sheng L, Li J, Hu D. Screening for depression in acute coronary syndrome patients: A comparison of Patient Health Questionnaire-9 versus Hospital Anxiety and Depression Scale-Depression. J Psychosom Res. 2019. Jun;121:24–28. doi: 10.1016/j.jpsychores.2019.03.018. Epub 2019 Mar 19. PMID: . [DOI] [PubMed] [Google Scholar]
- 44. Ye X, Shu HL, Feng X, et al. Reliability and validity of the Chinese version of the patient health questionnaire-9 (C-PHQ-9) in patients with psoriasis: A cross-sectional study. BMJ Open 2020;10(7):e033211; doi: 10.1136/bmjopen-2019-033211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Peng T, Li Z ming, Liu J, et al. Evaluation of reliability and validity of the patient health questionnaire-9 in patients with acne. Dermatol Ther 2020;33(4):e13584; doi: 10.1111/dth.13584. [DOI] [PubMed] [Google Scholar]
- 46. Chen S, Fang Y, Chiu H, et al. Validation of the nine-item patient health questionnaire to screen for major depression in a Chinese primary care population. Asia Pac Psychiatry 2013;5(2):61–68; doi: 10.1111/appy.12063. [DOI] [PubMed] [Google Scholar]
- 47. Xiong N, Fritzsche K, Wei J, Hong X, Leonhart R, Zhao X, Zhang L, Zhu L, Tian G, Nolte S, Fischer F. Validation of patient health questionnaire (PHQ) for major depression in Chinese outpatients with multiple somatic symptoms: a multicenter cross-sectional study. J Affect Disord. 2015 Mar 15;174:636–43. doi: 10.1016/j.jad.2014.12.042. Epub 2014 Dec 25. [DOI] [PubMed] [Google Scholar]
- 48. Du N, Yu K, Ye Y, et al. The validity study of patient health questionnaire-9 items for internet screening in depression among Chinese University students. Asia Pac Psychiatry 2017;9(3): 10.1111/appy.12266; doi: 10.1111/appy.12266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Wang W, Bian Q, Zhao Y, et al. Reliability and validity of the Chinese version of the patient health questionnaire (PHQ-9) in the general population. Gen Hosp Psychiatry 2014;36(5):539–544; doi: 10.1016/j.genhosppsych.2014.05.021. [DOI] [PubMed] [Google Scholar]
- 50. Zhang YL, Liang W, Chen ZM, et al. Validity and reliability of patient health questionnaire-9 and patient health questionnaire-2 to screen for depression among college students in China. Asia Pac Psychiatry 2013;5(4):268–275; doi: 10.1111/appy.12103. [DOI] [PubMed] [Google Scholar]
- 51. Xia NG, Lin JH, Ding SQ, Dong FR, Shen JZ, Du YR, Wang XS, Chen YY, Zhu ZG, Zheng RY, Xu HQ. Reliability and validity of the Chinese version of the Patient Health Questionnaire 9 (C-PHQ-9) in patients with epilepsy. Epilepsy Behav. 2019. Jun;95:65–69. doi: 10.1016/j.yebeh.2019.03.049. Epub 2019 Apr 24. PMID: . [DOI] [PubMed] [Google Scholar]
- 52. Wu Y, Levis B, Riehm KE, et al. Equivalency of the diagnostic accuracy of the PHQ-8 and PHQ-9: A systematic review and individual participant data meta-analysis. Psychol Med 2020;50(8):1368–1380; doi: 10.1017/S0033291719001314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Chen S, Chiu H, Xu B, Ma Y, Jin T, Wu M, Conwell Y. Reliability and validity of the PHQ-9 for screening late-life depression in Chinese primary care. Int J Geriatr Psychiatry. 2010. Nov;25(11):1127–33. doi: 10.1002/gps.2442. [DOI] [PubMed] [Google Scholar]
- 54. Đoàn LN, Takata Y, Sakuma KLK, et al. Trends in clinical research including Asian American, Native Hawaiian, and Pacific Islander participants funded by the US National Institutes of Health, 1992 to 2018. JAMA Netw Open 2019;2(7):e197432; doi: 10.1001/jamanetworkopen.2019.7432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Salant T, Lauderdale DS. Measuring culture: A critical review of acculturation and health in Asian immigrant populations. Soc Sci Med 2003;57(1):71–90; doi: 10.1016/S0277-9536(02)00300-3. [DOI] [PubMed] [Google Scholar]