Abstract
Objectives
COVID-19 vaccinations are highly efficacious in preventing severe illness that can lead to hospitalizations and death, but incidents of vaccine breakthrough (VBT) infections persist. We examined VBT infections within a congregate setting to help guide public health practices.
Study design
This is a retrospective cohort study of VBT infections identified via polymerase chain reaction (PCR) testing between 2/1/2021-11/1/2021.
Methods
A VBT infection was defined as the detection of SARS-CoV-2 collected from a person ≥14 days after all recommended doses of a COVID-19 vaccine. VBT infections were examined in five California psychiatric inpatient hospitals with a workforce of more than 10,000 hospital staff and approximately 5500 patients.
Results
415 VBT infections out of 14,101 fully vaccinated individuals within our system (2.9%) were identified. Days since final vaccine date ranged from 16 to 291 days. Kruskal-Wallis nonparametric test revealed a statistically significant difference in age between individuals with VBT infections versus all other vaccinated individuals [U = 6.47, p = .01]. A chi-square test of independence revealed no significant sex differences between individuals with VBT infections (58.8% male and 41.2% female) versus all other vaccinated individuals (59.6% male and 40.4% female; X2 (3, N = 14101) = 5.059, p = .167). Out of 415 VBT cases, 65.1% received the Moderna vaccine, 33.2% received Pfizer, and 1.7% received J&J; and 38.1% were asymptomatic at time of VBT infection, 24.1% were symptomatic, while 37.8% were missing symptom data.
Conclusions
Vaccination campaigns, including boosters and continued surveillance, are important complimentary strategies for reducing the proliferation of COVID-19 VBT cases and severity of symptoms associated with COVID-19.
1. Background
The ubiquitous impact of the global pandemic is complex and evolving, but in many ways is only beginning to be fully realized. In the United States alone, the novel coronavirus disease (COVID-19) caused by the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) has infected nearly 84 million people and has caused over 1,000,000 deaths [1]. In California alone, more than 8 million people have been infected and over 90,000 have lost their lives to COVID-19 [2]. New vaccine platform technology utilizing messenger RNA (mRNA) has greatly decreased the severity and transmissibility of SARS-CoV-2 [3]. Specifically, the Moderna mRNA-1273 and Pfizer/BioNtech BNT162b2 vaccines have reported very high efficacy (94.1% and 95%, respectively), including protecting against severe symptoms associated with COVID-19 (100% and 89%, respectively). Other vaccines using viral vector-based vaccines (e.g., Astra Zeneca, Johnson & Johnson, etc.) have also shown to have high efficacy against COVID-19 [4]. While vaccination campaigns have attenuated the transmission and symptom severity caused by SARS-CoV-2, there is lingering concern with waning efficacy of these vaccines against emerging virus variants. Mutations observed in the B.1.617.2 Delta variant, for example, is generating considerable concern as its high transmissibility is causing new outbreaks throughout the globe [5].
Vaccine breakthrough infections are defined as “the detection of SARS-CoV-2 RNA in a person ≥14 days after they have completed all recommended doses of a COVID-19 vaccine” [6]. Between January and April 30, 2021, a total of 10,262 SARS-CoV-2 vaccine breakthrough infections had been reported from 46 U.S. States and territories [7]. As of May 1, 2021, the CDC transitioned to only monitoring vaccine breakthrough cases that resulted in hospitalization or death. According to the CDC, these were some of the observed findings: 63% vaccine breakthrough infections occurred in females, the median age was 58 years (ranging from 40 to 74 years), 27% were asymptomatic, 10% were hospitalized and 2% of those patients died. Of the patients that were hospitalized, 29% were asymptomatic or hospitalized for a reason unrelated to COVID-19. Of those patients who died, the median age was 82 years (interquartile range = 71–89 years) with 18% of the decedents were asymptomatic or died from a cause unrelated to COVID-19. Thus, understanding the level of infectiousness of VBT infections remains a critical issue. Vasireddy and colleagues (2021) suggested that emerging variants resulted in increased transmissibility, morbidity and mortality, and exhibited decreased susceptibility to treatment [4]. Hacisuleyman and colleagues (2021) found that two individuals with VBT infections were symptomatic, while others report asymptomatic VBT infection [8]. It remains imperative to track vaccine breakthrough infections and identify common characteristics of these cases in order to reduce risk of transmission.
The California Department of State Hospitals (DSH) operates five inpatient psychiatric hospitals with a workforce of more than 10,000 hospital staff that includes healthcare and support services (e.g., custodial, correctional, and physical plant services) and houses approximately 5500 forensic psychiatric patients with severe mental illness. With 82% of hospital staff and 80% of patients vaccinated to date, this congregate setting which includes large dorm-style units with shared bathrooms and living spaces, allowed for examination of vaccine breakthroughs within a high-risk setting. The introduction of infection by hospital staff and widespread transmission throughout our system necessitated a clear need to better understand of the nature and severity of these VBT infections to help guide public health practices.
2. Methods
This study was approved by the California Health and Human Services Agency Committee for the Protection of Human Subjects (project number 2021-048).
DSH began vaccinating hospital staff December 21st, 2020 and patients in January 2021 in the Phase 1A of the national COVID-19 vaccination plan. All COVID-19 VBT infections identified between 2/1/2021-11/1/2021 via polymerase chain reaction (PCR) tests were analyzed. All samples were processed by the California Department of Public Health – Valencia Branch Laboratory.
3. Results
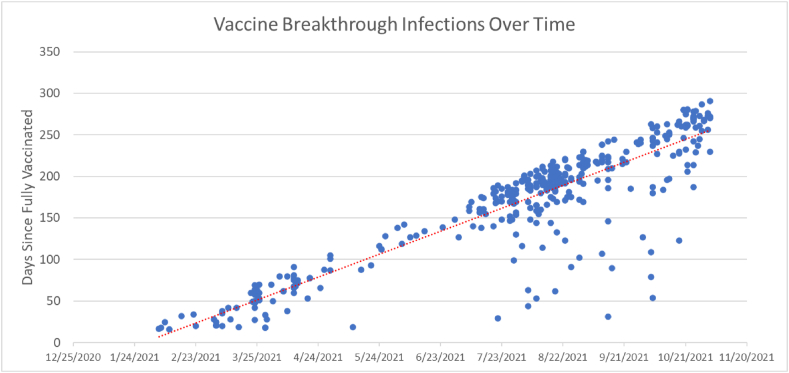
A total of 14,101 individuals received 2 doses of either the Moderna or Pfizer vaccine or 1 dose of the Johnson & Johnson vaccine and were considered fully vaccinated as of 10/15/2021. A total of 415 vaccine breakthrough infections were identified (2.9% of fully vaccinated individuals). Days post-vaccination ranged from 16 to 291 days (Fig. 1). Kruskal-Wallis nonparametric test revealed that there was a statistically significant difference in age between individuals with VBT infections [Median = 48.83 years] versus non-breakthrough vaccinated individuals [Median = 47.38 years; U = 6.47, p = .01]. A chi-square test of independence revealed that there were no significant sex differences between individuals with VBT infections (58.8% male and 41.2% female) versus non-breakthrough vaccinated individuals (59.6% male and 40.4% female; X2 (3, N = 14101) = 5.059, p = .167). Out of 415 VBT cases, 65.1% received the Moderna vaccine, 33.2% received Pfizer, and 1.7% received Jansen J&J vaccine; and 38.1% were asymptomatic at time of VBT infection, 24.1% were symptomatic, while 37.8% were missing symptom data. One hospitalization occurred and one death occurred among VBT cases.
Fig. 1.
Days post-final dose vaccination ranged from 16 to 291 days.
4. Conclusions
These findings hold important implications for similar institutions. First and foremost, increasing the number of vaccinations for both hospital staff and patients remains a critical goal in managing COVID-19 within large systems. As we have observed throughout the pandemic, congregate settings such as ours hold increased risk for greater spread of infections given the close contact of our patients and hospital staff. However, very few of the VBT infections in our institution resulted in hospitalization or death which is in line with other studies that have found that most breakthrough cases were mild or asymptomatic [9]. Notwithstanding, several important findings will be further discussed, especially with increasing concern about waning immunity as time from vaccination completion lengthens and more serious outbreaks may occur.
As the proliferation of COVID-19 variant strains arise and cause concern, we would predict that the number of VBT infections will increase similar to what is being observed throughout the United States and internationally [1]. Our results further suggest that older individuals remain at highest risk for breakthrough infections. It is important to note that our rigorous testing protocols (e.g., daily antigen testing and serial PCR testing for staff, response PCR testing for patients) likely allowed us to identify VBT infections that would have otherwise gone undetected within our hospitals if COVID-19 symptom presentation was the primary screening tool [10]. While our testing strategies may have increased the likelihood of our detecting VBT infections, it has likely also contributed to our ability to prevent transmission by asymptomatic individuals. Frequent testing of hospital staff and booster vaccinations can serve as a multi-pronged frontline defense to protect vulnerable populations, particularly older adults, in congregate settings and help reduce transmission of COVID-19.
The study has several limitations. Although the number of VBT infections is larger than most of what is currently being reported in the literature, the sample size is relatively small. Given that our data is preliminary, it may behoove other large congregate health care systems to continue COVID-19 screenings of all hospital staff regardless of vaccination status until a greater proportion of the population is vaccinated and infection rates decrease. Infection control measures such as the combination of rigorous testing protocols, unit quarantining, masking, social distancing, and vaccination may have contributed to the reduction in outbreaks within our congregate setting.
Vaccination campaigns, including the push to get boosters, and continued surveillance are important complimentary strategies for reducing both the proliferation of COVID-19 cases, as well as a reduction in severity of symptoms associated with COVID-19. These strategies are contributing to keeping COVID-19 outbreaks down and the severity of cases incredibly low in our system. The COVID-19 pandemic has proven to be a complex problem requiring a more nuanced and multidimensional response. We believe booster vaccinations are part of a complimentary, multi-dimensional response to an ever-changing virus.
Data sharing statement
Data requests must be submitted through the Department of State Hospitals Directors Office.
Declaration of competing interest
The authors have no conflicts of interest to report.
Acknowledgments
The findings and conclusions in this article are those of the author(s) and do not necessarily represent the views or opinions of the California Department of State Hospitals or the California Health and Human Services Agency.
References
- 1.https://coronavirus.jhu.edu/us-map
- 2.https://www.cdph.ca.gov/Programs/CID/DCDC/Pages/Immunization/nCOV2019.aspx
- 3.Funk C.D., Laferriere C., Ardakania A. Target product profile analysis of COVID-19 vaccines in phase III clinical trials and beyond: an early 2021 perspective. Viruses. 2021;13:418. doi: 10.3390/v13030418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Vasireddy, et al. Review of COVID-19 variants and COVID-19 vaccine efficacy: what the clinicians should know? J. Clin. Med. Res. 2021;13(6):317–325. doi: 10.14740/jocmr4518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.https://www.who.int/publications/m/item/global-consultation-on-a-decision-framework-for-assessing-the-impact-of-sars-cov-2-variants-of-concern-on-public-health-interventions
- 6.https://www.cdc.gov/coronavirus/2019-ncov/vaccines/effectiveness/why-measure-effectiveness/breakthrough-cases.html
- 7.https://www.cdc.gov/mmwr/volumes/70/wr/mm7021e3.htm
- 8.Hacisuleyman E., Hale C., Saito Y., Blachere N.E., Bergh M., Conlon E.G., et al. Vaccine breakthrough infections with SARS-CoV-2 variants. NEJM. 2021;384(23):2212–2218. doi: 10.1056/NEJMoa2105000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bergwerk M., Gonen T., Lustig Y., Amit S., Lipsithc M., Cohen C., et al. COVID-19 breakthrough infections in vaccinated health care workers. NEMJ. 2021;385(16):1474–1484. doi: 10.1056/NEJMoa2109072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ventura M.I., Delgado D., Velasquez S., Foote E., Jacobson K., Arguello J.C., Warburton K. Large-scale implementation of a daily rapid antigen testing program in California for detecting SARS-CoV-2. Am. J. Public Health. 2022;112(3):467–471. doi: 10.2105/AJPH.2021.306588. [DOI] [PMC free article] [PubMed] [Google Scholar]