Abstract
Gliomas are the most common malignant brain tumors. High-grade gliomas, represented by glioblastoma multiforme (GBM), have a poor prognosis and are prone to recurrence. The standard treatment strategy is tumor removal combined with radiotherapy and chemotherapy, such as temozolomide (TMZ). However, even after conventional treatment, they still have a high recurrence rate, resulting in an increasing demand for effective anti-glioma drugs. Drug repurposing is a method of reusing drugs that have already been widely approved for new indication. It has the advantages of reduced research cost, safety, and increased efficiency. Disulfiram (DSF), originally approved for alcohol dependence, has been repurposed for adjuvant chemotherapy in glioma. This article reviews the drug repurposing method and the progress of research on disulfiram reuse for glioma treatment.
Keywords: gliomas, glioblastoma multiforme, disulfiram, drug repurposing, temozolomide
1 Introduction
Glioma is a central nervous system (CNS) tumor and is one of the most common malignant brain tumors (Özcan et al., 2021), accounting for approximately 80% of all brain-related malignancies (Ostrom et al., 2019). According to the World Health Organization (WHO) classification, gliomas are divided into four grades based on their malignancy. Grades I–II are low-grade gliomas (LGGs), whereas grades III–IV are called high-grade gliomas (HGGs) (Özcan et al., 2021). Glioblastomas (GBMs) are WHO grade IV tumors with a high degree of malignancy and a median overall survival of approximately 15–26 months (Seliger and Hau, 2018).
Conventional treatment only modestly prolongs survival (Jakola et al., 2018). The growing demand for effective anticancer drugs has led researchers to search for Food and Drug Administration (FDA)-approved drugs that can be reused as chemotherapeutic agents (McMahon et al., 2020). Drug repurposing, also known as drug repositioning, drug reprofiling, drug redirecting, drug rediscovery, and others (Langedijk et al., 2015), is a promising treatment strategy for reusing drugs with known formulations, pharmacokinetics, toxicity, clinical trials, and post-marketing surveillance safety data that offer increased scope for use (Ashburn and Thor, 2004; Turanli et al., 2021).
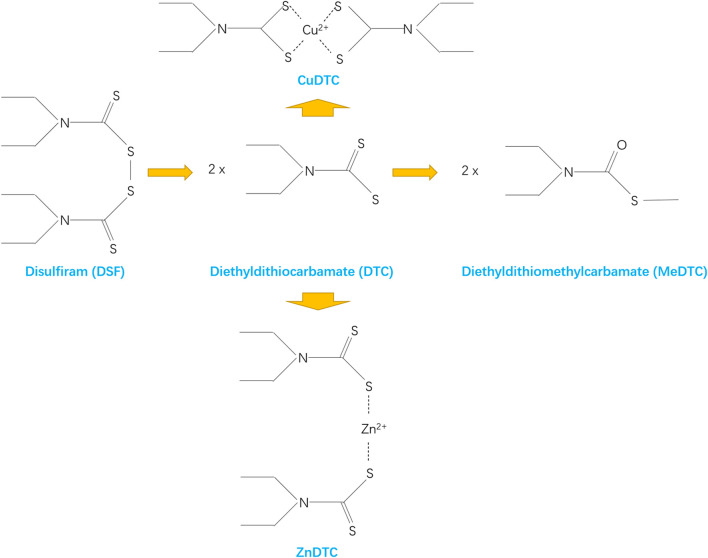
Disulfiram (DSF), also known as antabuse, is an FDA-approved acetaldehyde dehydrogenase inhibitor (Shirley et al., 2021; Turanli et al., 2021). Figure 1 shows the molecular structure of DSF. It has been used for treating alcohol dependence for the past 70 years with good pharmacokinetic properties, safety, and tolerability owing to the flu-like symptoms that patients experience when consuming alcohol (Seliger and Hau, 2018; Shirley et al., 2021). Preclinical and clinical studies have shown that DSF exhibits broad-spectrum anticancer activity against a variety of cancer types when administered with copper (Cu)-containing supplements (McMahon et al., 2020). Therefore, this review describes the drug repurposing of DSF in gliomas.
FIGURE 1.
Molecular structure of DSF.
2 Chemotherapy for glioma
The standard initial treatment for GBM is extensive neurosurgical resection, followed by postoperative segmental radiotherapy, temozolomide (TMZ) chemotherapy, and combined adjuvant therapy (Jakola et al., 2018; Stylli, 2020). The therapy using some natural and synthetic anti-glioma agents, such as medicinal cannabis or cannabinoids, bipolaris setariae fungi, oncolytic viruses, neurostatin, and fatty acid synthase (FAS) inhibitors, can also help combat gliomas (Anjum et al., 2017). Despite comprehensive strategies, residual GBM cells can develop treatment resistance (TR), resulting in GBM recurrence within a median time of approximately 7 months (Louis et al., 2016; Liu C. C. et al., 2021).
TMZ is a chemotherapeutic agent specifically used for brain cancer and was approved for recurrent mesenchymal astrocytoma in the United States in 1999 and recurrent mesenchymal astrocytoma and glioblastoma in Europe in 2000 (Mutter and Stupp, 2006). However, mitozolomide, the essential compound of TMZ, entered the clinic in 1983 (Newlands et al., 1997) and a phase I trial was completed in 1985 (Newlands et al., 1985), indicating that TMZ was developed over 16 years. A randomized clinical study conducted by Stupp in 2005 showed that adding TMZ to radiotherapy improved the 2-year survival rate of patients with GBM from 10.9% to 27.2% with minimal toxicity (Stupp et al., 2005). Since then, TMZ has been used as the first-line chemotherapeutic agent for gliomas (Stylli, 2020).
However, it is estimated that at least 50% of patients treated with TMZ do not respond to it, exhibiting innate or acquired chemoresistance, which ultimately leads to tumor recurrence (Lee, 2016). Presumably, during the window of chemotherapy with TMZ, most tumor cells are vulnerable and killed and may not have acquired full resistance (Osuka and Van Meir, 2017). Eventually, tumor cells resistant to multiple therapies persist in the brain parenchyma surrounding the tumor cavity and become the basis of tumor regeneration and recurrence (Osuka and Van Meir, 2017).
Given the slow and costly development of new therapies, drug repurposing has become an attractive strategy (Stylli, 2020). For example, a trial on metformin for GBM in 2015 showed that metformin prolonged the survival of patients with glioblastoma and diabetes (Adeberg et al., 2015). However, a pooled analysis questioned this finding and showed that metformin did not prolong survival in patients with GBM (Seliger et al., 2020). Similarly, celecoxib, as an adjuvant to TMZ chemotherapy, has shown good tolerability, but its efficacy in terms of survival benefits for patients remains uncertain (Stockhammer et al., 2010). The classical antimalarial drug, chloroquine, has been found to kill various cancer types, including GBM, through drug repurposing (Weyerhäuser et al., 2018). However, its concentration threshold for killing tumor cells under laboratory conditions is much higher than the clinically tolerable dose; therefore, its clinical value remains unclear (Weyerhäuser et al., 2018).
TMZ has shown great therapeutic value; however, the rate of drug resistance and recurrence of glioma remains reasonably high. Drug repurposing has contributed to the discovery of new therapies, but clinical application remains slow. Thus, there is an urgent need for developing new adjuvant chemotherapeutic agents.
3 Drug repurposing
3.1 Significance of drug repurposing
Drug repurposing can shorten development times by 5–7 years, reduce research investment costs by accounting for less than 10% of new compounds, and avoid risks such as a constant weight of generics (Cha et al., 2018). Moreover, a strict and burdensome regulatory process for new drugs forces developers to explore novel therapeutic uses for existing drugs (Turanli et al., 2021). Drug repurposing provides sufficient assurance regarding the safety, efficacy, and administration route of existing drugs (Parvathaneni et al., 2019; Juárez-López and Schcolnik-Cabrera, 2021; Turanli et al., 2021). Studies have shown that the cost and time to develop DSF as an anticancer drug are reduced by over 40% with an estimated annual cost of approximately $550 with DSF 500 mg per day (Cvek, 2012).
Drug repurposing facilitates the passage of projects and improves development efficiency. Only a minority of drug development projects can obtain FDA approval among newly developed drugs, compared with over 65% of drug repurposing projects (Masoudi-Sobhanzadeh et al., 2019). Recently, drug repurposing projects have accounted for approximately 30% of all newly approved drugs by the FDA (Parvathaneni et al., 2019). Additionally, drug repurposing can allow the revaluation of drugs that failed in the development phase for other uses and the change of application settings for better use (Masoudi-Sobhanzadeh et al., 2019).
3.2 Methods of drug repurposing
As high-throughput screening and computational biology methods advance, accumulated data lay the foundation for new approaches to rational drug repurposing (Turanli et al., 2021). Currently, numerous drug repurposing databases are available, allowing easy access to drug repurposing research, and systematic analysis is now accessible on platforms or screening systems dedicated to identifying repurposable drug candidates (Juárez-López and Schcolnik-Cabrera, 2021).
There are multiple information-gathering methods for drug repurposing. Electronic drug repurposing involves using various public databases to gather information from research, clinical trials, utilization reports, and other published data, and then to identify drug targets and networks of drug-drug interactions with the help of bioinformatics tools and artificial intelligence (Kumar et al., 2019). Text mining methods are used to discover new information by extracting aggregated new information from multiple published resources with the help of a computer, and by obtaining a large amount of data on conceptual relationships in biology from publications (Kumar et al., 2019). Clustering methods are applied to display and discover new drug targets or drug-disease relationships through various modules, groups, or subnetworks using clustering algorithms (Kumar et al., 2019). Propagation methods are based on information transmission from the source node to the network nodes and individual subnetwork nodes to determine the relationship between disease genes and target diseases (Emig et al., 2013). Semantic approaches seek biological entity relationships from medical databases, build semantic networks based on existing ontology networks, develop algorithms to discover the relationships, and extract medical information and image resources for drug reuse (Xue et al., 2018). Biological approaches include using systems and network biology to develop various models for drug reutilization studies that mimic the physiological environment of the target protein and modulate the outcome of its action, particularly targeting multifactorial complex diseases (Pujol et al., 2010). Knowledge-based empirical approaches are methods based on the knowledge of researchers and physicians and their ability, experience, and skills to interpret observations, with the opportunity for the serendipitous discovery of new drug utilization pathways (Kumar et al., 2019). Experimental methods include target screening, cellular analysis, animal models, and clinical trials (Kumar et al., 2019). These various methods of drug repurposing have been developed to evaluate the clinical efficacy for glioma treatment.
3.3 Database for drug repurposing
Advances in biotechnology, bioinformatics, and histological techniques (proteomics, genomics, metabolomics, etc.) have facilitated the development of several databases in biology, chemistry, medicine, and pharmacology (Kumar et al., 2019).
Basic databases for drug repurposing, such as DrugBank (Wishart et al., 2018), DGIdb (Cotto et al., 2018), and KEGG (Kanehisa et al., 2017), can provide information on drugs, targets, and pathways (Masoudi-Sobhanzadeh et al., 2019; Turanli et al., 2021). Recently, the newly developed DrugR + database based on DrugBank and KEGG provides a new source of information for the single application and reuse of drugs (Masoudi-Sobhanzadeh et al., 2019). The DrugR + database supports not only specialist users with structured query language (SQL) query functions, but also nonspecialist users with different options for targeted functions (Masoudi-Sobhanzadeh et al., 2019). The DrugR + database can also be readjusted to include drug use and provide a list of potential drugs for certain uses (Masoudi-Sobhanzadeh et al., 2019). The DrugR + database has several advantages, such as 1) providing a suitable and simple way to search for and obtain information about drugs with no technical problems, 2) providing information on the reusability of drugs, 3) allowing the selection of different types of research targets to obtain lists of drugs for diseases, and 4) providing up-to-date information on new drugs and the latest research (Masoudi-Sobhanzadeh et al., 2019).
Drug repurposing databases contain news, articles, and results obtained from drug repurposing studies (Masoudi-Sobhanzadeh et al., 2019), such as RepoDB (Brown and Patel, 2017b), Excelra (Arora et al., 2017), Drug Repurposing Hub (DRH) (Corsello et al., 2017), and TTD (Yang et al., 2016). Databases such as PREDICT (Gottlieb et al., 2011) and RepurposeDB (Shameer et al., 2018) summarize similarities between one drug or target and another (Masoudi-Sobhanzadeh et al., 2019). ChemMapper and iDrug Target are databases that assess ligand similarity (Sam and Athri, 2019). Drug target-based databases, such as DMAP (Huang et al., 2015), DrugSig (Wu et al., 2017), DDW (Holland, 2016), PDID, and idTarget (Sam and Athri, 2019), summarize drugs and their various targets, based on which new drug application pathways is proposed (Masoudi-Sobhanzadeh et al., 2019).
There are other databases such as ConnectivityMap (Lamb et al., 2006) for drug-induced gene expression studies, LINCS (Koleti et al., 2018) and GEO (Barrett et al., 2013) for transcriptomic characterization of tumor tissue from patients with cancer, CSNAP (Gaulton et al., 2012) and STITCH (Kuhn et al., 2012) for biological networks, RE:fine drugs (Moosavinasab et al., 2016) and MeSHDD (Brown and Patel, 2017a) linking drugs to disease databases, and PubChem (Wang et al., 2017) for comprehensive chemical and structural information on active ingredient components.
These databases cover an amount of information on drug targets, pathways, characteristics, and recent advances, allowing for exploring potentially efficient drugs.
4 History of drug repurposing of disulfiram
The urgent need for glioma treatment and the application of DSF to cancer through drug repurposing has led to a steady stream of studies in recent years that have shown good results in treating glioma (Huang J. et al., 2016; Huang et al., 2018; Huang et al., 2019; Halatsch et al., 2021). Table 1 shows the information on DSF in the drug repurposing database.
TABLE 1.
The information on DSF in the drug repurposing database.
| Drug repurposing database | Website | Id number | Disease area | Drug repurposing area |
|---|---|---|---|---|
| RepoDB | http://apps.chiragjpgroup.org/repoDB/ | None | Alcoholic Intoxication, Chronic (CUI: C0001973) | GBM/glioma |
| DRH | www.broadinstitute.org/repurposing | BRD-K32744045 | Abstinence from alcohol (neurology/psychiatry) | None |
| DrugBank | www.drugbank.ca | DB00822 | Chronic Alcoholism | GBM/glioma |
| DGIdb | www.dgidb.org | NSC-25953 | Alcohol Deterrents | Cocaine abuse |
| KEGG | http://www.kegg.jp | D00131 | Management of selected chronic alcohol patients | Antiparasitic |
| LINCS | http://lincsportal.ccs.miami.edu/ | LSM-5467 | Alcohol dependence | Melanoma |
| DrugSig | http://biotechlab.fudan.edu.cn/database/drugsig/ | BCTD00137 | Chronic alcoholism | None |
| PubChem | https://pubchem.ncbi.nlm.nih.gov | 3117 | Alcoholism | GBM |
In 1937, factory workers who were regularly exposed to DSF developed flu-like symptoms when they ingested alcohol (Triscott et al., 2015). DSF has been used to treat alcohol dependence since 1947 (Chick, 1999).
In the last 40 years, the anticancer effects of DSF have been discovered in vitro and in cancer xenografts (Conticello et al., 2012; Paranjpe et al., 2014). In 2003, Wang et al. suggested the possible clinical use of DSF in rectal cancer using cellular assays (Wang et al., 2003). In 2006, Chen et al. demonstrated through animal testing that DSF promotes selective apoptosis of tumor cells by inhibiting proteasome activity (Chen et al., 2006). In 2009, Iljin et al. systematically investigated the efficacy of most drugs and drug-like molecules already on the market against prostate cancer cells, and ultimately showed that DSF reduced tumor growth, induced metallothionein expression, and reduced DNA replication in vivo, indicating its potential as a therapeutic agent for prostate cancer (Iljin et al., 2009).
In 2009, Richard et al. speculated that DSF should be studied as an adjuvant to chemotherapy for glioblastoma based on its effect on acetaldehyde dehydrogenase (ALDH) in glioma (Kast and Belda-Iniesta, 2009), and since then the value of DSF in glioma has been focused. In 2012, Joanna et al. used the database approach for drug repurposing and selected DSF from numerous drugs that inhibit tumor-initiating cells using the Prestwick database (Triscott et al., 2012). They found that DSF inhibited PLK1 expression in GBM cells, suggesting that DSF could be repurposed for the treatment of refractory GBM (Triscott et al., 2012). In 2015, high ALDH1A1 expression was found to be associated with highly aggressive tumor cells and high-grade gliomas (Chen et al., 2006). ALDH1A1 promoted glioma progression, invasion, and proliferation, and led to poor prognosis (Chen et al., 2006). This finding brought the anti-glioma effects of DSF as an ALDH inhibitor back into the spotlight (Chen et al., 2006). In 2016, Huang et al. conducted the first phase I clinical trial using DSF in combination with TMZ for GBM treatment (Huang J. et al., 2016). In 2017, Karamanakos et al. combined DSF with standard treatment modalities to treat a patient with GBM and ultimately improved his prognosis, thereby confirming the clinical value of DSF (Karamanakos et al., 2017). In 2019, DSF was first reported to preferentially enhance radiosensitivity in GBM cells, particularly in radioresistant cells (Koh et al., 2019). In 2021, Meier et al. demonstrated the therapeutic value of DSF as a repurposed drug for treating gliomas in children (Meier et al., 2021). To date, relevant clinical trials are ongoing (NCT03363659, NCT03151772, NCT02715609, etc.).
5 Clinical practice for disulfiram in glioma
Huang et al. (2016) conducted a phase I clinical trial. Twelve patients newly diagnosed with supratentorial primary GBM were studied using concomitant adjuvant DSF and TMZ chemotherapy after radiotherapy. Patients were divided into two groups and received 500 mg/day or 1000 mg/day of DSF in combination with TMZ chemotherapy. The results showed that the maximum tolerated dose of DSF was 500 mg/day. Although some associated adverse effects, such as fatigue, delirium, ataxia, dizziness, and peripheral motor/sensory neuropathy, existed, these adverse reactions were self-limiting and resolved within 30 days after DSF discontinuation (Huang J. et al., 2016).
In 2018, Huang et al. updated data from a phase I clinical trial. The study population comprised 18 patients newly diagnosed with GBM after standard radiotherapy. DSF was also administered during the chemotherapy phase of TMZ. Seven patients received DSF at 500 mg/day, five patients received DSF at 1000 mg/day, and six patients received DSF/Cu at 500 mg/day. The results showed that a maximum dose of 500 mg/day of DSF was well tolerated with or without combined Cu, while 1000 mg/day was poorly tolerated. Of the patients receiving 500 mg DSF with a combination of Cu per day, one patient suffered from nausea and diarrhea in the first 30 days, which was relieved after the reduction of DSF to 250 mg per day. Additionally, without the combination of Cu, one patient developed delirium after 1.6 months and one developed motor neuropathy after 2.6 months. All adverse reactions resolved rapidly after dose reduction or DSF discontinuation. Notably, a 40-year-old woman in the study who received 500 mg DSF per day discontinued DSF therapy after 2.6 months of treatment due to motor neuropathy. At 33 months after DSF treatment, the patient survived in good health with no signs of tumor recurrence (Huang et al., 2018).
Based on a previous study, Huang et al. conducted a phase II clinical trial in 2019. Twenty-three patients with recurrent TMZ-resistant GBM were enrolled in the study. DSF (80 mg) and Cu gluconate (1.5 mg) were administered orally thrice daily at approximately 4–8 hourly intervals in conjunction with TMZ chemotherapy. The results showed that 14% of the patients achieved clinical benefit over a stabilization period of over 6 months. The most common adverse effects were nausea and vomiting in 17% of patients, followed by dizziness (Huang et al., 2019).
In 2021, Marc et al. conducted a phase Ib/IIa clinical trial using a CUSP9 treatment regimen in combination with TMZ. Ten patients with GBM were included in this study. CUSP9 was gradually added at increasing doses during uninterrupted TMZ chemotherapy. When all drugs reached the target dose, the drug was maintained until side effects or tumor progression occurred. The results showed that the regimen was safe under clinical, laboratory, and electrocardiographic monitoring and that the side effects were mild and disappeared after discontinuation (Halatsch et al., 2021).
Since 2016, there have been updates on clinical trials using DSF as an adjuvant in the treatment of glioma. Evidence suggests that DSF has great therapeutic potential but with mild side effects; however, clinical studies are still inadequate.
6 Pharmacological mechanism of disulfiram
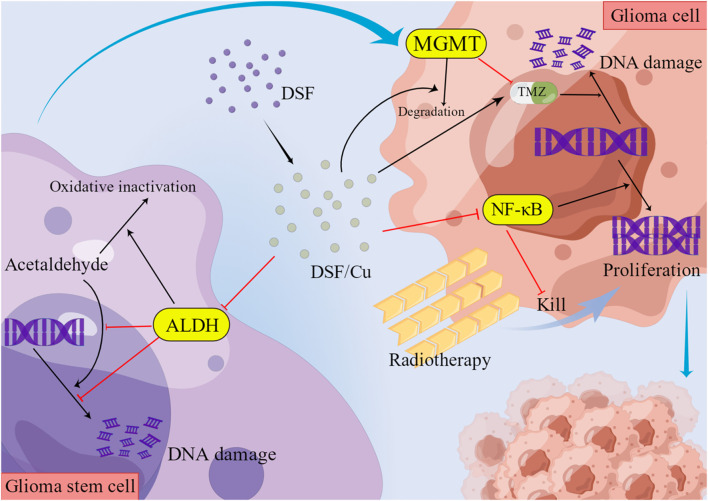
DSF can act as an anticancer agent through various Cu- and zinc-dependent processes, including the inhibition of nuclear factor kappa B (NF-κB), NPL4, and phosphoglycerol dehydrogenase (Spillier et al., 2019). DSF produces oxidative stress by inhibiting NF-κB activation and superoxide dismutase (SOD) and inducing an increased ratio of oxidized glutathione to its reduced form (Tesson et al., 2017). DSF cytotoxicity is dependent on Cu (Ye et al., 2011). Cu plays a key role in redox reactions and triggers the generation of reactive oxygen species (ROS) in human cells (Liu et al., 2012). Many cancer types, including GBM, have significantly higher intracellular Cu levels than normal tissues, and DSF penetrates and chelates Cu intracellularly (Liu et al., 2012). As DSF cytotoxicity appears to be Cu-dependent, high Cu concentrations in cancer cells produce cytotoxicity through oxidative stress generated by the Fenton reaction (production of Cu ions and hydroxyl radicals) or through inhibiting enzymes that bind Cu to peptide bonds, allowing DSF to specifically target cancer cells and preserve normal tissue (Liu et al., 2012; Tesson et al., 2017).
Approximately 80–95% of the orally administered DSF is absorbed and the unabsorbed portion is excreted (Shirley et al., 2021). In the body, DSF is rapidly metabolized to DTC acid and then rapidly formed as diethylthiocarbamic acid methyl ester (diethyldithiomethylcarbamate, MeDTC) or broken down into carbon disulphide and dimethylamine (Shirley et al., 2021). MeDTC inhibits ALDH and is a strong metal chelate that can form complexes with metal ions (Shirley et al., 2021). DSF is also reduced to DTC in the stomach and forms metal-ion complexes in the gastrointestinal tract (Shirley et al., 2021). DTC metal complexes have a relatively long half-life, are widely distributed throughout the body, and penetrate the blood-brain barrier (BBM) (Shirley et al., 2021). This pharmacological mechanism makes it possible for DSF to kill glioma cells specifically. During DSF treatment, alcohol ingestion leads to acetaldehyde accumulation due to ALDH inhibition, causing the DSF-ethanol reaction (Jørgensen et al., 2011). This reaction manifests as tachypnea, tachycardia, facial flushing, nausea, vomiting, hypotension, and even cardiovascular collapse (Jørgensen et al., 2011).
7 Molecular mechanism of disulfiram against tumor stem cells
7.1 Inhibition of ALDH
DSF has a symmetric structure, and its first metabolic step is reducing the disulfide bond at the center of the molecule to produce two diethyldithiocarbamate (DTC) fractions (Lipsky et al., 2001a). DTC is further converted to its methyl ester and other metabolites (Lipsky et al., 2001a). DTC is a potent ALDH inhibitor, which forms a mixed disulfide bond with the key cysteine near the active site (Lipsky et al., 2001a). DSF significantly alters alcohol metabolism and treats chronic alcohol dependence by irreversibly inhibiting ALDH and causing acetaldehyde accumulation (Jørgensen et al., 2011). ALDH belongs to a family of metabolic enzymes that catalyze the oxidation of aldehydes, a toxic alcohol metabolism product (Lipsky et al., 2001b). ALDH promotes cell survival by protecting DNA from genotoxic damage and providing resistance to a wide range of anticancer drugs (Hothi et al., 2012). Therefore, ALDH inhibition is an effective way to sensitize resistant cell populations to the cytotoxic effects of chemotherapeutic drugs (Hothi et al., 2012). The strong expression of ALDH is a prominent feature of normal and cancer stem cells, including the stem cell subpopulation of glioblastoma (Kast and Belda-Iniesta, 2009). In GBM and other cancers, increased ALDH expression is observed in a small subpopulation of tumor cells with stem cell properties (Rappa et al., 2013). ALDH expression is associated with the anti-apoptotic capacity of glioma stem cells (GSCs) and the protection of DNA against damage by ROS and aldehydes (Kast and Belda-Iniesta, 2009). DSF and its metabolites form mixed disulfide bonds with key cysteines (Cys302) near the active site of ALDH to inactivate it (Paranjpe et al., 2014). With ALDH inhibition, the division of stem cells into non-stem daughter cells is blocked (Kast and Belda-Iniesta, 2009). However, such inhibitory effect of DSF on ALDH does not affect normal neural stem cells or fibroblasts (Choi et al., 2015).
7.2 Induced degradation of mixed lineage leukemia
MLL1 and MLL2 are human homologs of the Drosophila epigenetic regulator Trithorax (Trx) (Schuettengruber et al., 2017). MLL1 promotes tumor stem cell characteristics, cell growth, and tumorigenicity in adult glioblastomas (Meier et al., 2021). MLL2 mutations are found in 14% of patients with medulloblastoma (Parsons et al., 2011). Studies have shown that DSF can effectively kill both childhood glioma stem cells at low concentrations and glioma cell lines at slightly higher concentrations by inducing MLL degradation (Meier et al., 2021).
7.3 Mediation of increased intracellular ROS production
DSF-mediated cytotoxicity is partially due to increased ROS production. Elevated ROS levels are the major mode of DSF-mediated cell death (Kast et al., 2014). DSF/Cu induces ROS in GBM cell lines, which activates the JNK and p38 pathways, and inhibits NF-κB activity (Liu et al., 2012). DSF/Cu eliminates stem cell-like cell populations in GBM cell lines by modulating the Bcl2 family to trigger the intrinsic apoptotic pathway (Liu et al., 2012). DSF rapidly inhibits superoxide dismutase 1 (SOD1) in murine microglia to induce neurotoxic microglia activation (Dimayuga et al., 2007). ROS production by activated microglia directs redox-sensitive inflammatory signaling and initiates neurotoxic inflammation (Dimayuga et al., 2007). The inhibition of activated microglia might lower the neurological side effects of DSF during the treatment.
8 Molecular mechanism of disulfiram against glioma cells
8.1 Inhibition of MGMT activity
O6-methylguanine-DNA methyltransferase (MGMT) is a DNA repair protein and chemotherapeutic target that is highly expressed in approximately 80% of brain tumors and other cancers (Gerson, 2002). MGMT, as an anti-mutagenic DNA repair protein, can remove mutagenic O6-alkyl groups from guanine and interfere with the cytotoxic effects of alkylating agents to make tumors resistant (Gerson, 2002). The survival of patients with GBM depends on the MGMT promoter methylation status (Koh et al., 2019). Those with methylated MGMT promoter (MGMT meth) had a higher survival rate than those with the wild-type (MGMT wt) (Paranjpe et al., 2014; Koh et al., 2019). Thus, MGMT has become a central determinant of tumor resistance to alkylating agents (Paranjpe et al., 2014). DSF causes MGMT degradation (Srivenugopal et al., 2016) and synergistically inhibits the growth and renewal of TMZ-resistant GBM cells (Triscott et al., 2012). Compared to normal astrocytes, DSF induces a preferential increase in radiosensitivity in GBM cells, causing increased apoptosis and delayed DNA damage repair (Koh et al., 2019). DSF-induced radiosensitization is more pronounced in radioresistant cells, especially drug-resistant GBM cells with wild-type non-methylated MGMT promoters (Koh et al., 2019). In brain tumor cell lines, DSF reduced MGMT activity in a rapid and dose-dependent manner (Paranjpe et al., 2014). Of these, DSF/Cu was approximately five times more potent than DSF in inhibiting MGMT activity in cultured brain tumor cells (Paranjpe et al., 2014). There are no reports about adverse effects on normal neuronal cells caused by this mechanism.
8.2 Inhibition of NF-κB
NF-κB promotes disease progression by increasing tumor cell proliferation, inducing the transcription of anti-apoptotic genes and genes involved in the DNA damage response, and promoting angiogenesis (Voorhees and Orlowski, 2006). NF-κB activation is associated with radioresistance, particularly through inducing anti-apoptotic and antioxidant gene expression (Tesson et al., 2017). DSF is an NF-κB inhibitor, which interferes with TGF-β-induced epithelial-mesenchymal transition in cancer (Han et al., 2015). The blockade of NF-κB activation by DSF reduces tumor volume and cell invasion (Westhoff et al., 2013). The aggressiveness of GBM is associated with the secretion and processing of fibronectin by GBM cells via fibrinogen and matrix metallopeptidases (Mettang et al., 2018). GBM causes reduced intercellular interactions by creating this new extracellular matrix (ECM)-based microenvironment, and generating a stress response that triggers NF-κB activation and enhances cell-matrix adhesion of GBM (Mettang et al., 2018). DSF blockade of NF-κB activation inhibits cell-matrix adhesion between GBM and the brain tissue microenvironment, and reduces tumor volume and cell invasion (Mettang et al., 2018). Other drugs that modulate fibrinogen, metallopeptidases, and fibronectin in the microenvironment of glioma cells might synergistically enhance the anti-invasive effects of DSF.
8.3 Inhibition of proteasome activation
Proteasome activity promotes tumorigenesis by enhancing tumor cell proliferation, down-regulating apoptosis, and promoting angiogenesis (Voorhees and Orlowski, 2006). Therefore, the ubiquitin-proteasome pathway is an important target for cancer therapy (Voorhees and Orlowski, 2006). DSF inhibits proteasome activation (Voorhees and Orlowski, 2006), leading to the accumulation of misfolded proteins and potentially toxic protein aggregates (Hothi et al., 2012), subsequently inducing tumor cell death (Hothi et al., 2012). The DSF activity depends on the presence of Cu ions, and Cu thiocarbamate complexes act as proteasome inhibitors (Hothi et al., 2012). As a potent proteasome inhibitor, DSF/Cu can functionally impair the DNA repair pathways and enhance the effects of DNA alkylating agents and radiation (Lun et al., 2016). DSF/Cu inhibits the chymotrypsin-like proteasome activity in cultured glioma stem cells (GSC), consistent with the inactivation of the ubiquitin-proteasome pathway and subsequent tumor cell death induction (Hothi et al., 2012).
8.4 Downregulation of PLK1 expression
Polo-like kinase 1 (PLK1), which is highly expressed in tumor cells, is a key serine/threonine kinase involved in many important cell cycle functions such as mitotic entry, centrosome maturation, cell cycle progression, and cytoplasmic division (Triscott et al., 2012). As GBM tumors with higher levels of PLK1 expression have a higher incidence and poorer prognosis, PLK1 could be a promising therapeutic target for brain tumors (Triscott et al., 2012). DSF leads to downregulation of cell cycle kinase PLK1 in GBM cells (Triscott et al., 2012).
DSF is involved in the regulation of complicated molecular mechanisms. These molecular mechanisms of DSF are shown in Figure 2 .
FIGURE 2.
Molecular mechanisms of DSF.
9 DSF delivery route
The standard dosage following FDA-approved indications for managing chronic alcohol use is 250 mg/day orally, with a maximum dose of 500 mg/day (Ekinci et al., 2019). Additionally, the nasal-brain pathway is considered a safe and effective alternative for direct drug delivery to the CNS (Landis et al., 2012). Administration via the nasal cavity to the CNS bypasses the blood-brain barrier and avoids hepatic first-pass effects (Qu et al., 2021). The clinical application of DSF as an anticancer drug is limited by its poor oral bioavailability and rapid metabolism in vivo (Shergill et al., 2016). It has been shown that DSF encapsulation in hydroxypropyl-β-cyclodextrin (HP-β-CD) produces a DSF complex with enhanced solubility (Qu et al., 2021). In vitro anti-GBM activity and safety (DSF/HP-β-CD/Cu) can increase the aqueous solubility of DSF by approximately 2,450-fold and may be a promising intranasal agent to treat (Qu et al., 2021). Animal studies have shown that DSF/HP-β-CD/Cu significantly inhibited tumor growth and migration, promoted tumor apoptosis, and prolonged the median survival time in male glioma rats in the intranasal administration group (Qu et al., 2021). Besides oral and nasal-brain access, 1,2-distearoyl-sn-glycero-3-phosphocholine (DSPC)/cholesterol liposomes to prepare DSF as an injectable Cu(DDC)2 formulation are also therapeutically active (Wehbe et al., 2017).
10 Combination therapy of disulfiram
Combinations of two or more drugs with different mechanisms of action, also referred to as combination therapy, is an alternative strategy for improving the success of drug repurposing (Masoudi-Sobhanzadeh et al., 2019). Compared with single-drug therapy, it reduces the incidence/emergence of resistance mechanisms, doses of drugs, and adverse effects, and improves the synergistic effects and success of treatment modalities (Masoudi-Sobhanzadeh et al., 2019). Combination therapy allows simultaneous targeting of multiple therapeutic genes, and is currently the most effective treatment for aggressive tumors, such as GBM (Ghosh et al., 2018). Combination therapy of DSF with other modalities holds great promise.
10.1 Disulfiram in combination with metal supplements
Preclinical and clinical studies have shown that DSF has broad-spectrum anticancer activity against a variety of cancer types when combined with Cu-containing supplements, such as Cu gluconate (McMahon et al., 2020). The combination regimen comprised 500 mg of DSF daily plus 50 mg of zinc gluconate or 2 mg of Cu gluconate three times daily (Ekinci et al., 2019). It has been shown that DSF/Cu sulphide (CuS) nanocomplexes (Tf-DSF/CuS) modified with transferrin (Tf) exhibit high cytotoxic effects in vitro (Lan et al., 2021). The CuS nanoparticles enable them to accumulate specifically and within tumor tissue by enhancing the permeability and retention (EPR) effect of the tumor tissue (Lan et al., 2021). The metallic nature of the nanoparticles enhanced the drug-loading capacity by forming Cu complexes on the CuS surface (Lan et al., 2021). Additionally, the use of a long-wavelength laser in the near-infrared (700–1000 nm) region activated the photothermal effect of the nanoparticles, resulting in minimal damage to normal tissue from tumor ablation (Lan et al., 2021). Besides Cu, DSF can act through zinc chelation to inhibit the activities of MMP-2 and MMP-9 (Kast and Halatsch, 2012).
10.2 Disulfiram in combination with standard chemotherapy drugs
In vitro cytotoxicity is enhanced by the addition of DSF to standard chemotherapeutic agents (Rappa et al., 2013) such as cisplatin (O'Brien et al., 2012), TMZ (Triscott et al., 2012), paclitaxel (Yip et al., 2011), gemcitabine (Cunningham and Chaiton, 2018), doxorubicin (Budman and Calabro, 2002), cyclophosphamide (Moreb et al., 2012), 5-fluorouracil (Wang et al., 2003), and adriamycin (Xu et al., 2011). The combination regimens for DSF against gliomas are described below.
10.2.1 Disulfiram in combination with temozolomide
The 5-year survival rate of patients with GBM treated with radiation alone was 1.9%, and TMZ, in conjunction with radiation therapy, only increased the rate to 9.8% (Triscott et al., 2015). Additionally, TMZ toxicity is often not well tolerated by patients, and other modalities of TMZ resistance, such as MGMT expression, make it complicated (Triscott et al., 2015).
DSF is highly effective in cases where cells develop TMZ resistance (Triscott et al., 2012). DSF has synergistic activity when combined with TMZ, which is highly effective against TMZ-resistant cells (Lun et al., 2016). In the presence of low Cu doses, DSF significantly enhanced TMZ activity in vitro (Lun et al., 2016). In vivo studies have confirmed that DSF and Cu have synergistic effects with TMZ and improve survival in mice with in situ GBM tumors (Lun et al., 2016).
DSF can be safely used in combination with TMZ, although it causes reversible neurotoxicity (Huang J. et al., 2016). At a maximum tolerated dose (MTD) of 500 mg/day of DSF with TMZ without concomitant Cu administration, slight proteasomal inhibition of peripheral blood cells was observed after 4 weeks, with an average reduction of approximately 5% (Huang J. et al., 2016). A dose-response trend appeared with doubling proteasome inhibition at a dose of 1000 mg/day (Huang J. et al., 2016). The results of a phase II clinical study in 23 patients showed that adding DSF/Cu to TMZ was safe and well tolerated in TMZ-resistant IDH wild-type GBM (Huang et al., 2019).
10.2.2 Disulfiram in combination with cisplatin
DSF enhances cisplatin-induced cytotoxicity by directly damaging DNA (O'Brien et al., 2012). Activating transcription factor 3 (ATF3) exerts a pro-apoptotic effect in response to cisplatin by directly binding to and activating vascular endothelial cells (O'Brien et al., 2012). It has been shown that the combination of cisplatin and DSF plays a synergistic role in inducing ATF3 protein expression and promoting tumor cell death (O'Brien et al., 2012). Adding DSF to the combination regimen of cisplatin and vincristine is well tolerated in antitumor therapy (Nechushtan et al., 2015). A dose of 40 mg DSF, with a half-life of approximately 7 hours, can be administered three times daily to improve its therapeutic effect with minimal side effects (Nechushtan et al., 2015). Significant neurotoxicity has not been reported with this combination therapy, besides fatigue (Nechushtan et al., 2015).
DSF may assist cisplatin in enhancing cytotoxic effects. This strategy appears to be safe, but the in vivo efficacy in glioma patients remains unclear.
10.2.3 Disulfiram in combination with auranofin
A study of glioma stem cells in children found that DSF killed glioma stem cells at low concentrations and killed cell lines at slightly higher concentrations (Meier et al., 2021). The addition of auranofin increased DSF efficiency, and the synergistic effect was more pronounced in differentiated cells than in undifferentiated cells (Meier et al., 2021). Auranofin was also used in combination with DSF in the CUSP9 treatment program (Skaga et al., 2019).
10.2.4 Combination with coordinated undermining of survival paths
DSF with aprepitant, auranofin, captopril, celecoxib, itraconazole, minocycline, quetiapine, and sertraline constituted a CUSP9 regimen that was used in combination with TMZ to synergistically disrupt the active survival pathway in GBM, block multiple signaling pathways, and make GBM vulnerable to the cytotoxic effects of TMZ (Skaga et al., 2019). A study of patient-derived glioblastoma stem cell (GSC) cultures from 15 patients with GBM showed that combining CUSP9 with TMZ produced a synergistic effect compared to the single drug (Skaga et al., 2019). CUSP9, combined with TMZ, was more effective than TMZ monotherapy in terms of the clinical plasma concentrations (Skaga et al., 2019). The CUSP9* regimen was generated based on the CUSP9 regimen, comprising DSF in combination with aprepitant, artesunate, auranofin, captopril, celecoxib, itraconazole, sertraline, and ritonavir (Kast et al., 2014). All nine drugs in the CUSP9* regimen were FDA-approved, each inhibiting one or more of the important GBM growth pathways (Kast et al., 2014).
DSF and auranofin have synergistic effect even without the other components of a CUSP9 regimen. All these might be the powerful adjuncts to TMZ chemotherapy. However, the side effects of CUSP9 or CUSP9* regimens combined with multiple agents deserve further clinical study.
10.2.5 Disulfiram in combination with gemcitabine
Gemcitabine (2,2′-difluorodeoxycytidine, dFdC) is a deoxyribonucleic acid analogue that can be used as a single agent or combined with other anticancer drugs (Metro et al., 2010). Gemcitabine is active against a wide range of hematological and solid cancers. It is one of the few classical anticancer drugs that can pass through the BBB, penetrate the tumor mass, and be effectively converted to its active form in GBM tissue (Metro et al., 2010). However, its use in GBM chemotherapy is limited by the high resistance of GBM cells to dFdCs (Liu et al., 2012). Therefore, it is currently used mainly in combination with radiotherapy as a radiosensitizer for GBM treatment (Liu et al., 2012). DSF can synergistically enhance gemcitabine cytotoxicity and reverse gemcitabine resistance in cancer cell lines through ROS induction and inhibition of the ALDH and NF-κB pathways (Liu et al., 2012; O'Brien et al., 2012). In preclinical studies, DSF and its derivative pyrrolidine dithiocarbamate have been successfully used to enhance gemcitabine efficacy, particularly through NF-κB inhibition and oxidative stress generation (Iljin et al., 2009; Tesson et al., 2017). Increased oxidative stress due to DSF/Cu interactions with glutathione sensitizes cancer cells to gemcitabine treatment (Iljin et al., 2009; Tesson et al., 2017).
10.2.6 Disulfiram in combination with carbenoxolone
Carbenoxolone is mainly used to treat gastric ulcers and other types of inflammation (Connors, 2012) and can play a role in inhibiting tumor cell growth by interfering with intracellular signaling through inhibiting ligand proteins (Zhang et al., 2003). DSF and carbenoxolone inhibit distinct interactions of GBM with the brain tissue microenvironment and stress-induced GBM cell-matrix adhesion with gap junction-mediated intercellular communication (Mettang et al., 2018). Animal experiments have shown that the combined use of DSF, carbenoxolone, and TMZ reduces tumor size in an in situ mouse model (Mettang et al., 2018). Tumor-initiating and adherent differentiated cells form gap junctions, and carbenoxolone can block adherent differentiated cells and affect intercellular communication (Mettang et al., 2018). Adherent differentiated cells are more sensitive to DSF treatment, and DSF interferes with cell-matrix adhesion by modulating NF-κB signaling (Mettang et al., 2018).
Table 2 shows the candidate chemicals used in combination with DSF for cancer treatment.
TABLE 2.
The candidate chemicals used in combination with DSF for anticancer therapy.
| Combination of drugs | Tumor type | Evidence type | Year and References |
|---|---|---|---|
| Temozolomide (TMZ) | Glioblastoma (GBM) | Clinical trials | Huang et al. (2019) |
| Glioblastoma stem cells (GSCs) | Cells | Zirjacks et al. (2021) | |
| Cisplatin | Ovarian Cancer | Animals | Bai et al. (2021) |
| Head and neck squamous cell carcinoma (HNSCC) | Cells | Yao et al. (2021) | |
| Mammary cancer | Cells | Yang et al. (2019) | |
| Prostate adenocarcinoma | Cells | O'Brien et al. (2012) | |
| Atypical teratoid/rhabdoid tumor (AT/RT) | Animals | Jangra et al. (2020) | |
| Bladder cancer | Cells | Kita et al. (2019) | |
| Testicular germ cell tumors | Animals | Schmidtova et al. (2019) | |
| Esophageal squamous cell carcinoma | Animals | Jivan et al. (2018) | |
| Metastatic non-small cell lung cancer | Clinical trials | Nechushtan et al. (2015) | |
| Nasopharyngeal carcinoma (NPC) | Animals | Li et al. (2020) | |
| Auranofin | Pediatric glioma | Cells | Meier et al. (2021) |
| Hepatoma | Cells/Animals | Huang et al. (2016a) | |
| Ovarian cancer | Cells | Papaioannou et al. (2014) | |
| Gemcitabine (dFdC) | Glioblastoma (GBM) | Cells | Tesson et al. (2017) |
| Mammary cancer | Animals | Liu et al. (2021a) | |
| Pancreatic ductal adenocarcinoma (PDAC) | Cells/Animals | Kim et al. (2013) | |
| Colon cancer | Cells | Guo et al. (2010) | |
| Regorafenib | Glioblastoma (GBM) | Animals | Zhao et al. (2018) |
| Carbenoxolone | Glioblastoma (GBM) | Animals | Mettang et al. (2018) |
| CUSP9/ Temozolomide (TMZ) | Glioblastoma stem cells (GSCs) | Cells | Skaga et al. (2019) |
| Paclitaxel | Mammary cancer | Cells | Liu et al. (2013) |
| Lung adenocarcinoma | Animals | Mohammad et al. (2019) | |
| Docetaxel | Mammary cancer | Cells | Swetha et al. (2020) |
| Doxorubicin | Osteosarcoma | Cells | Mandell et al. (2022) |
| Mammary cancer | Cells | Rolle et al. (2020) | |
| Acute myeloid leukemia (AML) | Cells | Xu et al. (2011) | |
| 5-Fluorouracil (5-Fu) | Cervical carcinoma | Cells | Abidin et al. (2020) |
| Pancreatic ductal Adenocarcinoma (PDAC) | Animals | Cong et al. (2017) | |
| Colorectal cancer (CRC) | Cells | Wang et al. (2003) | |
| Arsenic trioxide (ATO) | Pancreatic cancer | Animals | Dinnen et al. (2013) |
All references listed in the table are the latest research progress.
10.3 Disulfiram in combination with radiotherapy
DSF has a radiosensitizing effect on GBM cells (Koh et al., 2019) and enhances the radiosensitivity of AT/RT cell lines by increasing DNA damage, apoptosis, and autophagy (Lee et al., 2017). Combining DSF and Cu enhanced radiosensitivity by inducing cell death or interfering with DNA repair (Liu C. C. et al., 2021).
Thus, the efficacy of both chemotherapy and radiotherapy might be enhanced by DSF.
11 Adverse effects of disulfiram
DSF is a safe and well-tolerated drug, with mild side effects (Shirley et al., 2021). With chronic lymphocytic leukemia and normal lymphocytes (Wickström et al., 2007), invasive cancer and normal endothelial cells (Shian et al., 2003), and glioblastoma and normal astrocytes (Hothi et al., 2012), DSF is selectively toxic and kills human cancer cells (Paranjpe et al., 2014). The ability of different organs to resist endogenous and environmentally derived alkylating agents may be compromised, and this unrepaired DNA damage, particularly in regulatory oncogenes, may manifest as deleterious mutations and promote genomic instability (Paranjpe et al., 2014). DSF combined with Cu has an enhanced role in killing cancer cells; however, Cu-mediated cytotoxicity is also significantly increased in normal cells (Choi et al., 2015). The combined use of Cu and Zn in therapy is potentially dangerous because they are teratogenic and may lead to developmental defects (Choi et al., 2015). High DSF doses are hepatotoxic (Triscott et al., 2015), and rare cases of severe atopic hepatitis may occur, along with a risk of neuropathy; however, these symptoms are reversible after discontinuation (Huang J. et al., 2016). The mechanisms of neurological side effects of DSF remain unclear and may involve free acid radicals, inhibition of certain enzymes, calcium-induced neuronal toxicity, synergistic activity of neurotoxic drugs/chemicals, and other mechanisms (Kulkarni et al., 2013). If ethanol is ingested during DSF treatment, the large amounts of acetaldehyde produced from ethanol can cause severe nausea, headache, vomiting, flushing, and physical discomfort (Kast and Belda-Iniesta, 2009).
DSF is considered a relatively safe treatment since most of its adverse effects resolve after discontinuation. The mechanism of neuropathy caused by DSF still requires further research.
12 Conclusion
Malignant gliomas have a poor prognosis and high recurrence rate, posing a major threat to global public health. Current conventional treatment modalities hardly eradicate gliomas; therefore, new therapeutic approaches are urgently needed. Drug repurposing approaches have provided new research ideas for glioma treatment. This can help the pharmaceutical industry and researchers identify new uses for existing drugs. The expanding research on gliomas through drug repurposing approaches has made DSF a potential adjuvant for glioma treatment. DSF has a good safety profile and is an economical drug that is expected to play a broader role in the future treatment of gliomas. Further epidemiological studies should be performed to investigate the relationship between DSF and the risk to or survival of patients with gliomas. More clinical trials are needed to further refine treatment options for DSF. However, drug repurposing may not yet reach its full potential in the field of glioma, and new therapeutic agents through drug repurposing deserve further exploration.
Author contributions
Conceptualization, YB and SZ; methodology, SZ; critical revision of the manuscript for important intellectual content, YB, YW, and SL; analysis and interpretation of data, XZ and SL; investigation, XS, GL, KL, XZ, LL, LR, ST, QZ, BZ, WS, ZY, and QX; reference collection and data acquisition, SZ and SL; original draft preparation, SZ; review and editing, SZ, YB, and YW; visualization, SZ; supervision, YB and YW; project administration, SZ, SL, YB, and YW; funding acquisition, YB and XS. All authors have read and agreed to the published version of the manuscript.
Funding
This study was funded by Liaoning Provincial Natural Science Foundation (2020-MS-155), China Medical University novel coronavirus pneumonia prevention and control research project (2020-12-11), Shenyang Planning Foundation for Science and Technology (21-173-9-38), the first batch of medical education scientific research project of China Medical University for the 14th Five-Year Plan (YDJK2021011), the Scientific Research Funding Project of Education Department of Liaoning Province (JCZR2020010), National Science Foundation of China (72074104), Immersion Technology and Evaluation Shandong Engineering Research Center (2022), and Immersion Technology and Evaluation Shandong Engineering Research Center (2022). The researchers are grateful for the support of several organizations.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors, and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
- Abidin I. Z., Rezoagli E., Simonassi-Paiva B., Fehrenbach G. W., Masterson K., Pogue R., et al. (2020). A bilayer vaginal tablet for the localized delivery of disulfiram and 5-fluorouracil to the cervix. Pharmaceutics 12, E1185. 10.3390/pharmaceutics12121185 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Adeberg S., Bernhardt D., Ben Harrabi S., Bostel T., Mohr A., Koelsche C., et al. (2015). Metformin influences progression in diabetic glioblastoma patients. Strahlenther. Onkol. 191, 928–935. 10.1007/s00066-015-0884-5 [DOI] [PubMed] [Google Scholar]
- Anjum K., Shagufta B. I., Abbas S. Q., Patel S., Khan I., Shah S. A. A., et al. (2017). Current status and future therapeutic perspectives of glioblastoma multiforme (GBM) therapy: A review. Biomed. Pharmacother. 92, 681–689. 10.1016/j.biopha.2017.05.125 [DOI] [PubMed] [Google Scholar]
- Arora N., Kacker P. K. M., Kacker P. (2017). Translational research in drug discovery and development. Translational Bioinformatics and its Application. [Google Scholar]
- Ashburn T. T., Thor K. B. (2004). Drug repositioning: Identifying and developing new uses for existing drugs. Nat. Rev. Drug Discov. 3, 673–683. 10.1038/nrd1468 [DOI] [PubMed] [Google Scholar]
- Bai M. Y., Yu M. H., Wang T. T., Chen S. H., Wang Y. C. (2021). Plate-like alginate microparticles with disulfiram-SPIO-coencapsulation: An in vivo study for combined therapy on ovarian cancer. Pharmaceutics 13, 1348. 10.3390/pharmaceutics13091348 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barrett T., Wilhite S. E., Ledoux P., Evangelista C., Kim I. F., Tomashevsky M., et al. (2013). NCBI GEO: Archive for functional genomics data sets--update. Nucleic Acids Res. 41, D991–D995. 10.1093/nar/gks1193 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown A. S., Patel C. J. (2017b). A standard database for drug repositioning. Sci. Data 4, 170029. 10.1038/sdata.2017.29 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown A. S., Patel C. J. (2017a). MeSHDD: Literature-based drug-drug similarity for drug repositioning. J. Am. Med. Inf. Assoc. 24, 614–618. 10.1093/jamia/ocw142 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Budman D. R., Calabro A. (2002). In vitro search for synergy and antagonism: Evaluation of docetaxel combinations in breast cancer cell lines. Breast Cancer Res. Treat. 74, 41–46. 10.1023/a:1016070230538 [DOI] [PubMed] [Google Scholar]
- Cha Y., Erez T., Reynolds I. J., Kumar D., Ross J., Koytiger G., et al. (2018). Drug repurposing from the perspective of pharmaceutical companies. Br. J. Pharmacol. 175, 168–180. 10.1111/bph.13798 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen D., Cui Q. C., Yang H., Dou Q. P. (2006). Disulfiram, a clinically used anti-alcoholism drug and copper-binding agent, induces apoptotic cell death in breast cancer cultures and xenografts via inhibition of the proteasome activity. Cancer Res. 66, 10425–10433. 10.1158/0008-5472.Can-06-2126 [DOI] [PubMed] [Google Scholar]
- Chick J. (1999). Safety issues concerning the use of disulfiram in treating alcohol dependence. Drug Saf. 20, 427–435. 10.2165/00002018-199920050-00003 [DOI] [PubMed] [Google Scholar]
- Choi S. A., Choi J. W., Wang K. C., Phi J. H., Lee J. Y., Park K. D., et al. (2015). Disulfiram modulates stemness and metabolism of brain tumor initiating cells in atypical teratoid/rhabdoid tumors. Neuro. Oncol. 17, 810–821. 10.1093/neuonc/nou305 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cong J., Wang Y., Zhang X., Zhang N., Liu L., Soukup K., et al. (2017). A novel chemoradiation targeting stem and nonstem pancreatic cancer cells by repurposing disulfiram. Cancer Lett. 409, 9–19. 10.1016/j.canlet.2017.08.028 [DOI] [PubMed] [Google Scholar]
- Connors B. W. (2012). Tales of a dirty drug: Carbenoxolone, gap junctions, and seizures. Epilepsy Curr. 12, 66–68. 10.5698/1535-7511-12.2.66 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Conticello C., Martinetti D., Adamo L., Buccheri S., Giuffrida R., Parrinello N., et al. (2012). Disulfiram, an old drug with new potential therapeutic uses for human hematological malignancies. Int. J. Cancer 131, 2197–2203. 10.1002/ijc.27482 [DOI] [PubMed] [Google Scholar]
- Corsello S. M., Bittker J. A., Liu Z., Gould J., Mccarren P., Hirschman J. E., et al. (2017). The drug repurposing hub: A next-generation drug library and information resource. Nat. Med. 23, 405–408. 10.1038/nm.4306 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cotto K. C., Wagner A. H., Feng Y. Y., Kiwala S., Coffman A. C., Spies G., et al. (2018). DGIdb 3.0: A redesign and expansion of the drug-gene interaction database. Nucleic Acids Res. 46, D1068-D1073–d1073. 10.1093/nar/gkx1143 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cunningham J. A., Chaiton M. (2018). Has there been an increase in the frequency with which people who drink in a risky fashion receive advice to cut down on their drinking from 1998 to 2015? Subst. Abus. 39, 449–451. 10.1080/08897077.2018.1449048 [DOI] [PubMed] [Google Scholar]
- Cvek B. (2012). Nonprofit drugs as the salvation of the world's healthcare systems: The case of antabuse (disulfiram). Drug Discov. Today 17, 409–412. 10.1016/j.drudis.2011.12.010 [DOI] [PubMed] [Google Scholar]
- Dimayuga F. O., Wang C., Clark J. M., Dimayuga E. R., Dimayuga V. M., Bruce-Keller A. J. (2007). SOD1 overexpression alters ROS production and reduces neurotoxic inflammatory signaling in microglial cells. J. Neuroimmunol. 182, 89–99. 10.1016/j.jneuroim.2006.10.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dinnen R. D., Mao Y., Qiu W., Cassai N., Slavkovich V. N., Nichols G., et al. (2013). Redirecting apoptosis to aponecrosis induces selective cytotoxicity to pancreatic cancer cells through increased ROS, decline in ATP levels, and VDAC. Mol. Cancer Ther. 12, 2792–2803. 10.1158/1535-7163.Mct-13-0234 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ekinci E., Rohondia S., Khan R., Dou Q. P. (2019). Repurposing disulfiram as an anti-cancer agent: Updated review on literature and patents. Recent Pat. anticancer. Drug Discov. 14, 113–132. 10.2174/1574892814666190514104035 [DOI] [PubMed] [Google Scholar]
- Emig D., Ivliev A., Pustovalova O., Lancashire L., Bureeva S., Nikolsky Y., et al. (2013). Drug target prediction and repositioning using an integrated network-based approach. PLoS One 8, e60618. 10.1371/journal.pone.0060618 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gaulton A., Bellis L. J., Bento A. P., Chambers J., Davies M., Hersey A., et al. (2012). ChEMBL: A large-scale bioactivity database for drug discovery. Nucleic Acids Res. 40, D1100–D1107. 10.1093/nar/gkr777 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gerson S. L. (2002). Clinical relevance of MGMT in the treatment of cancer. J. Clin. Oncol. 20, 2388–2399. 10.1200/jco.2002.06.110 [DOI] [PubMed] [Google Scholar]
- Ghosh D., Nandi S., Bhattacharjee S. (2018). Combination therapy to checkmate glioblastoma: Clinical challenges and advances. Clin. Transl. Med. 7, 33. 10.1186/s40169-018-0211-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gottlieb A., Stein G. Y., Ruppin E., Sharan R. (2011). Predict: A method for inferring novel drug indications with application to personalized medicine. Mol. Syst. Biol. 7, 496. 10.1038/msb.2011.26 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guo X., Xu B., Pandey S., Goessl E., Brown J., Armesilla A. L., et al. (2010). Disulfiram/copper complex inhibiting NFkappaB activity and potentiating cytotoxic effect of gemcitabine on colon and breast cancer cell lines. Cancer Lett. 290, 104–113. 10.1016/j.canlet.2009.09.002 [DOI] [PubMed] [Google Scholar]
- Halatsch M. E., Kast R. E., Karpel-Massler G., Mayer B., Zolk O., Schmitz B., et al. (2021). A phase ib/IIa trial of 9 repurposed drugs combined with temozolomide for the treatment of recurrent glioblastoma: CUSP9v3. Neurooncol. Adv. 3, vdab075. vdab075. 10.1093/noajnl/vdab075 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Han D., Wu G., Chang C., Zhu F., Xiao Y., Li Q., et al. (2015). Disulfiram inhibits TGF-β-induced epithelial-mesenchymal transition and stem-like features in breast cancer via ERK/NF-κB/Snail pathway. Oncotarget 6, 40907–40919. 10.18632/oncotarget.5723 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holland R. (2016). Drug discovery world, drug discovery and development news. Drug Discov. [Google Scholar]
- Hothi P., Martins T. J., Chen L., Deleyrolle L., Yoon J. G., Reynolds B., et al. (2012). High-throughput chemical screens identify disulfiram as an inhibitor of human glioblastoma stem cells. Oncotarget 3, 1124–1136. 10.18632/oncotarget.707 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huang H., Liao Y., Liu N., Hua X., Cai J., Yang C., et al. (2016a). Two clinical drugs deubiquitinase inhibitor auranofin and aldehyde dehydrogenase inhibitor disulfiram trigger synergistic anti-tumor effects in vitro and in vivo . Oncotarget 7, 2796–2808. 10.18632/oncotarget.6425 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huang H., Nguyen T., Ibrahim S., Shantharam S., Yue Z., Chen J. Y. (2015). Dmap: A connectivity map database to enable identification of novel drug repositioning candidates. BMC Bioinforma. 16 (13), S4. 10.1186/1471-2105-16-s13-s4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huang J., Campian J. L., Gujar A. D., Tran D. D., Lockhart A. C., Dewees T. A., et al. (2016b). A phase I study to repurpose disulfiram in combination with temozolomide to treat newly diagnosed glioblastoma after chemoradiotherapy. J. Neurooncol. 128, 259–266. 10.1007/s11060-016-2104-2 [DOI] [PubMed] [Google Scholar]
- Huang J., Campian J. L., Gujar A. D., Tsien C., Ansstas G., Tran D. D., et al. (2018). Final results of a phase I dose-escalation, dose-expansion study of adding disulfiram with or without copper to adjuvant temozolomide for newly diagnosed glioblastoma. J. Neurooncol. 138, 105–111. 10.1007/s11060-018-2775-y [DOI] [PubMed] [Google Scholar]
- Huang J., Chaudhary R., Cohen A. L., Fink K., Goldlust S., Boockvar J., et al. (2019). A multicenter phase II study of temozolomide plus disulfiram and copper for recurrent temozolomide-resistant glioblastoma. J. Neurooncol. 142, 537–544. 10.1007/s11060-019-03125-y [DOI] [PubMed] [Google Scholar]
- Iljin K., Ketola K., Vainio P., Halonen P., Kohonen P., Fey V., et al. (2009). High-throughput cell-based screening of 4910 known drugs and drug-like small molecules identifies disulfiram as an inhibitor of prostate cancer cell growth. Clin. Cancer Res. 15, 6070–6078. 10.1158/1078-0432.Ccr-09-1035 [DOI] [PubMed] [Google Scholar]
- Jakola A. S., Werlenius K., Mudaisi M., Hylin S., Kinhult S., Bartek J., JR., et al. (2018). Disulfiram repurposing combined with nutritional copper supplement as add-on to chemotherapy in recurrent glioblastoma (DIRECT): Study protocol for a randomized controlled trial. F1000Res. 7, 1797. 10.12688/f1000research.16786.1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jangra A., Choi S. A., Yang J., Koh E. J., Phi J. H., Lee J. Y., et al. (2020). Disulfiram potentiates the anticancer effect of cisplatin in atypical teratoid/rhabdoid tumors (AT/RT). Cancer Lett. 486, 38–45. 10.1016/j.canlet.2020.05.006 [DOI] [PubMed] [Google Scholar]
- Jivan R., Peres J., Damelin L. H., Wadee R., Veale R. B., Prince S., et al. (2018). Disulfiram with or without metformin inhibits oesophageal squamous cell carcinoma in vivo . Cancer Lett. 417, 1–10. 10.1016/j.canlet.2017.12.026 [DOI] [PubMed] [Google Scholar]
- Jørgensen C. H., Pedersen B., TøNNESEN H. (2011). The efficacy of disulfiram for the treatment of alcohol use disorder. Alcohol. Clin. Exp. Res. 35, 1749–1758. 10.1111/j.1530-0277.2011.01523.x [DOI] [PubMed] [Google Scholar]
- Juárez-López D., Schcolnik-Cabrera A. (2021). Drug repurposing: Considerations to surpass while Re-directing old compounds for new treatments. Arch. Med. Res. 52, 243–251. 10.1016/j.arcmed.2020.10.021 [DOI] [PubMed] [Google Scholar]
- Kanehisa M., Furumichi M., Tanabe M., Sato Y., Morishima K. (2017). Kegg: New perspectives on genomes, pathways, diseases and drugs. Nucleic Acids Res. 45, D353-D361–d361. 10.1093/nar/gkw1092 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Karamanakos P. N., Trafalis D. T., Papachristou D. J., Panteli E. S., Papavasilopoulou M., Karatzas A., et al. (2017). Evidence for the efficacy of disulfiram and copper combination in glioblastoma multiforme - a propos of a case. J. buon 22, 1227–1232. [PubMed] [Google Scholar]
- Kast R. E., Belda-Iniesta C. (2009). Suppressing glioblastoma stem cell function by aldehyde dehydrogenase inhibition with chloramphenicol or disulfiram as a new treatment adjunct: An hypothesis. Curr. Stem Cell. Res. Ther. 4, 314–317. 10.2174/157488809789649241 [DOI] [PubMed] [Google Scholar]
- Kast R. E., Halatsch M. E. (2012). Matrix metalloproteinase-2 and -9 in glioblastoma: A trio of old drugs-captopril, disulfiram and nelfinavir-are inhibitors with potential as adjunctive treatments in glioblastoma. Arch. Med. Res. 43, 243–247. 10.1016/j.arcmed.2012.04.005 [DOI] [PubMed] [Google Scholar]
- Kast R. E., Karpel-Massler G., Halatsch M. E. (2014). CUSP9* treatment protocol for recurrent glioblastoma: Aprepitant, artesunate, auranofin, captopril, celecoxib, disulfiram, itraconazole, ritonavir, sertraline augmenting continuous low dose temozolomide. Oncotarget 5, 8052–8082. 10.18632/oncotarget.2408 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim S. K., Kim H., Lee D. H., Kim T. S., Kim T., Chung C., et al. (2013). Reversing the intractable nature of pancreatic cancer by selectively targeting ALDH-high, therapy-resistant cancer cells. PLoS One 8, e78130. 10.1371/journal.pone.0078130 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kita Y., Hamada A., Saito R., Teramoto Y., Tanaka R., Takano K., et al. (2019). Systematic chemical screening identifies disulfiram as a repurposed drug that enhances sensitivity to cisplatin in bladder cancer: A summary of preclinical studies. Br. J. Cancer 121, 1027–1038. 10.1038/s41416-019-0609-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koh H. K., Seo S. Y., Kim J. H., Kim H. J., Chie E. K., Kim S. K., et al. (2019). Disulfiram, a Re-positioned aldehyde dehydrogenase inhibitor, enhances radiosensitivity of human glioblastoma cells in vitro . Cancer Res. Treat. 51, 696–705. 10.4143/crt.2018.249 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koleti A., Terryn R., Stathias V., Chung C., Cooper D. J., Turner J. P., et al. (2018). Data portal for the library of integrated network-based cellular signatures (LINCS) program: Integrated access to diverse large-scale cellular perturbation response data. Nucleic Acids Res. 46, D558-D566–d566. 10.1093/nar/gkx1063 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kuhn M., Szklarczyk D., Franceschini A., von Mering C., Jensen L. J., Bork P. (2012). Stitch 3: Zooming in on protein-chemical interactions. Nucleic Acids Res. 40, D876–D880. 10.1093/nar/gkr1011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kulkarni R. R., Pradeep A. V., Bairy B. K. (2013). Disulfiram-induced combined irreversible anterior ischemic optic neuropathy and reversible peripheral neuropathy: A prospective case report and review of the literature. J. Neuropsychiatry Clin. Neurosci. 25, 339–342. 10.1176/appi.neuropsych.12120410 [DOI] [PubMed] [Google Scholar]
- Kumar R., Harilal S., Gupta S. V., Jose J., Thomas Parambi D. G., Uddin M. S., et al. (2019). Exploring the new horizons of drug repurposing: A vital tool for turning hard work into smart work. Eur. J. Med. Chem. 182, 111602. 10.1016/j.ejmech.2019.111602 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lamb J., Crawford E. D., Peck D., Modell J. W., Blat I. C., Wrobel M. J., et al. (2006). The connectivity map: Using gene-expression signatures to connect small molecules, genes, and disease. Science 313, 1929–1935. 10.1126/science.1132939 [DOI] [PubMed] [Google Scholar]
- Lan Q. H., du C. C., Yu R. J., Zhai J., Shi Y., Kou L., et al. (2021). Disulfiram-loaded copper sulfide nanoparticles for potential anti-glioma therapy. Int. J. Pharm. 607, 120978. 10.1016/j.ijpharm.2021.120978 [DOI] [PubMed] [Google Scholar]
- Landis M. S., Boyden T., Pegg S. (2012). Nasal-to-CNS drug delivery: Where are we now and where are we heading? An industrial perspective. Ther. Deliv. 3, 195–208. 10.4155/tde.11.149 [DOI] [PubMed] [Google Scholar]
- Langedijk J., Mantel-Teeuwisse A. K., Slijkerman D. S., Schutjens M. H. (2015). Drug repositioning and repurposing: Terminology and definitions in literature. Drug Discov. Today 20, 1027–1034. 10.1016/j.drudis.2015.05.001 [DOI] [PubMed] [Google Scholar]
- Lee S. Y. (2016). Temozolomide resistance in glioblastoma multiforme. Genes. Dis. 3, 198–210. 10.1016/j.gendis.2016.04.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee Y. E., Choi S. A., Kwack P. A., Kim H. J., Kim I. H., Wang K. C., et al. (2017). Repositioning disulfiram as a radiosensitizer against atypical teratoid/rhabdoid tumor. Neuro. Oncol. 19, 1079–1087. 10.1093/neuonc/now300 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li Y., Chen F., Chen J., Chan S., He Y., Liu W., et al. (2020). Disulfiram/copper induces antitumor activity against both nasopharyngeal cancer cells and cancer-associated fibroblasts through ROS/MAPK and ferroptosis pathways. Cancers (Basel) 12, E138. 10.3390/cancers12010138 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lipsky J. J., Shen M. L., Naylor S. (2001a). In vivo inhibition of aldehyde dehydrogenase by disulfiram. Chem. Biol. Interact. 130-132, 93–102. 10.1016/s0009-2797(00)00225-8 [DOI] [PubMed] [Google Scholar]
- Lipsky J. J., Shen M. L., Naylor S. (2001b). Overview--in vitro inhibition of aldehyde dehydrogenase by disulfiram and metabolites. Chem. Biol. Interact. 130-132, 81–91. 10.1016/s0009-2797(00)00224-6 [DOI] [PubMed] [Google Scholar]
- Liu C. C., Wu C. L., Lin M. X., Sze C. I., Gean P. W. (2021b). Disulfiram sensitizes a therapeutic-resistant glioblastoma to the TGF-β receptor inhibitor. Int. J. Mol. Sci. 22, 10496. 10.3390/ijms221910496 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu C., Qiang J., Deng Q., Xia J., Deng L., Zhou L., et al. (2021a). ALDH1A1 activity in tumor-initiating cells remodels myeloid-derived suppressor cells to promote breast cancer progression. Cancer Res. 81, 5919–5934. 10.1158/0008-5472.Can-21-1337 [DOI] [PubMed] [Google Scholar]
- Liu P., Brown S., Goktug T., Channathodiyil P., Kannappan V., Hugnot J. P., et al. (2012). Cytotoxic effect of disulfiram/copper on human glioblastoma cell lines and ALDH-positive cancer-stem-like cells. Br. J. Cancer 107, 1488–1497. 10.1038/bjc.2012.442 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu P., Kumar I. S., Brown S., Kannappan V., Tawari P. E., Tang J. Z., et al. (2013). Disulfiram targets cancer stem-like cells and reverses resistance and cross-resistance in acquired paclitaxel-resistant triple-negative breast cancer cells. Br. J. Cancer 109, 1876–1885. 10.1038/bjc.2013.534 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Louis D. N., Perry A., Reifenberger G., von Deimling A., Figarella-Branger D., Cavenee W. K., et al. (2016). The 2016 world health organization classification of tumors of the central nervous system: A summary. Acta Neuropathol. 131, 803–820. 10.1007/s00401-016-1545-1 [DOI] [PubMed] [Google Scholar]
- Lun X., Wells J. C., Grinshtein N., King J. C., Hao X., Dang N. H., et al. (2016). Disulfiram when combined with copper enhances the therapeutic effects of temozolomide for the treatment of glioblastoma. Clin. Cancer Res. 22, 3860–3875. 10.1158/1078-0432.Ccr-15-1798 [DOI] [PubMed] [Google Scholar]
- Mandell J. B., Douglas N., Ukani V., Beumer J. H., Guo J., Payne J., et al. (2022). ALDH1A1 gene expression and cellular copper levels between low and highly metastatic osteosarcoma provide a case for novel repurposing with disulfiram and copper. Sarcoma 2022, 7157507. 10.1155/2022/7157507 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Masoudi-Sobhanzadeh Y., Omidi Y., Amanlou M., Masoudi-Nejad A. (2019). DrugR+: A comprehensive relational database for drug repurposing, combination therapy, and replacement therapy. Comput. Biol. Med. 109, 254–262. 10.1016/j.compbiomed.2019.05.006 [DOI] [PubMed] [Google Scholar]
- Mcmahon A., Chen W., Li F. (2020). Old wine in new bottles: Advanced drug delivery systems for disulfiram-based cancer therapy. J. Control. Release 319, 352–359. 10.1016/j.jconrel.2020.01.001 [DOI] [PubMed] [Google Scholar]
- Meier S., Cantilena S., Niklison Chirou M. V., Anderson J., Hargrave D., Salomoni P., et al. (2021). Alcohol-abuse drug disulfiram targets pediatric glioma via MLL degradation. Cell. Death Dis. 12, 785. 10.1038/s41419-021-04078-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Metro G., Fabi A., Mirri M. A., Vidiri A., Pace A., Carosi M., et al. (2010). Phase II study of fixed dose rate gemcitabine as radiosensitizer for newly diagnosed glioblastoma multiforme. Cancer Chemother. Pharmacol. 65, 391–397. 10.1007/s00280-009-1155-x [DOI] [PubMed] [Google Scholar]
- Mettang M., Meyer-Pannwitt V., Karpel-Massler G., Zhou S., Carragher N. O., FöHR K. J., et al. (2018). Blocking distinct interactions between glioblastoma cells and their tissue microenvironment: A novel multi-targeted therapeutic approach. Sci. Rep. 8, 5527. 10.1038/s41598-018-23592-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mohammad I. S., Teng C., Chaurasiya B., Yin L., Wu C., He W. (2019). Drug-delivering-drug approach-based codelivery of paclitaxel and disulfiram for treating multidrug-resistant cancer. Int. J. Pharm. 557, 304–313. 10.1016/j.ijpharm.2018.12.067 [DOI] [PubMed] [Google Scholar]
- Moosavinasab S., Patterson J., Strouse R., Rastegar-Mojarad M., Regan K., Payne P. R., et al. (2016). 'RE:fine drugs': An interactive dashboard to access drug repurposing opportunities. Oxford): Database. 10.1093/database/baw083 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moreb J. S., Ucar D., Han S., Amory J. K., Goldstein A. S., Ostmark B., et al. (2012). The enzymatic activity of human aldehyde dehydrogenases 1A2 and 2 (ALDH1A2 and ALDH2) is detected by Aldefluor, inhibited by diethylaminobenzaldehyde and has significant effects on cell proliferation and drug resistance. Chem. Biol. Interact. 195, 52–60. 10.1016/j.cbi.2011.10.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mutter N., Stupp R. (2006). Temozolomide: A milestone in neuro-oncology and beyond? Expert Rev. Anticancer Ther. 6, 1187–1204. 10.1586/14737140.6.8.1187 [DOI] [PubMed] [Google Scholar]
- Nechushtan H., Hamamreh Y., Nidal S., Gotfried M., Baron A., Shalev Y. I., et al. (2015). A phase IIb trial assessing the addition of disulfiram to chemotherapy for the treatment of metastatic non-small cell lung cancer. Oncologist 20, 366–367. 10.1634/theoncologist.2014-0424 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Newlands E. S., Blackledge G., Slack J. A., Goddard C., Brindley C. J., Holden L., et al. (1985). Phase I clinical trial of mitozolomide. Cancer Treat. Rep. 69, 801–805. [PubMed] [Google Scholar]
- Newlands E. S., Stevens M. F., Wedge S. R., Wheelhouse R. T., Brock C. (1997). Temozolomide: A review of its discovery, chemical properties, pre-clinical development and clinical trials. Cancer Treat. Rev. 23, 35–61. 10.1016/s0305-7372(97)90019-0 [DOI] [PubMed] [Google Scholar]
- O'brien A., Barber J. E., Reid S., Niknejad N., Dimitroulakos J. (2012). Enhancement of cisplatin cytotoxicity by disulfiram involves activating transcription factor 3. Anticancer Res. 32, 2679–2688. [PubMed] [Google Scholar]
- Ostrom Q. T., Cioffi G., Gittleman H., Patil N., Waite K., Kruchko C., et al. (2019). CBTRUS statistical report: Primary brain and other central nervous system tumors diagnosed in the United States in 2012-2016. Neuro. Oncol. 21, v1–v100. 10.1093/neuonc/noz150 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Osuka S., Van Meir E. G. (2017). Overcoming therapeutic resistance in glioblastoma: The way forward. J. Clin. Investig. 127, 415–426. 10.1172/jci89587 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Özcan H., Emiroğlu B. G., Sabuncuoğlu H., Özdoğan S., Soyer A., SAYGı T. (2021). A comparative study for glioma classification using deep convolutional neural networks. Math. Biosci. Eng. 18, 1550–1572. 10.3934/mbe.2021080 [DOI] [PubMed] [Google Scholar]
- Papaioannou M., Mylonas I., Kast R. E., BRüNING A. (2014). Disulfiram/copper causes redox-related proteotoxicity and concomitant heat shock response in ovarian cancer cells that is augmented by auranofin-mediated thioredoxin inhibition. Oncoscience 1, 21–29. 10.18632/oncoscience.5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Paranjpe A., Zhang R., Ali-Osman F., Bobustuc G. C., Srivenugopal K. S. (2014). Disulfiram is a direct and potent inhibitor of human O6-methylguanine-DNA methyltransferase (MGMT) in brain tumor cells and mouse brain and markedly increases the alkylating DNA damage. Carcinogenesis 35, 692–702. 10.1093/carcin/bgt366 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parsons D. W., Li M., Zhang X., Jones S., Leary R. J., Lin J. C., et al. (2011). The genetic landscape of the childhood cancer medulloblastoma. Science 331, 435–439. 10.1126/science.1198056 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parvathaneni V., Kulkarni N. S., Muth A., Gupta V. (2019). Drug repurposing: A promising tool to accelerate the drug discovery process. Drug Discov. Today 24, 2076–2085. 10.1016/j.drudis.2019.06.014 [DOI] [PubMed] [Google Scholar]
- Pujol A., Mosca R., FARRéS J., Aloy P. (2010). Unveiling the role of network and systems biology in drug discovery. Trends Pharmacol. Sci. 31, 115–123. 10.1016/j.tips.2009.11.006 [DOI] [PubMed] [Google Scholar]
- Qu Y., Sun X., Ma L., Li C., Xu Z., Ma W., et al. (2021). Therapeutic effect of disulfiram inclusion complex embedded in hydroxypropyl-β-cyclodextrin on intracranial glioma-bearing male rats via intranasal route. Eur. J. Pharm. Sci. 156, 105590. 10.1016/j.ejps.2020.105590 [DOI] [PubMed] [Google Scholar]
- Rappa F., Cappello F., Halatsch M. E., Scheuerle A., Kast R. E. (2013). Aldehyde dehydrogenase and HSP90 co-localize in human glioblastoma biopsy cells. Biochimie 95, 782–786. 10.1016/j.biochi.2012.11.007 [DOI] [PubMed] [Google Scholar]
- Rolle F., Bincoletto V., Gazzano E., Rolando B., Lollo G., Stella B., et al. (2020). Coencapsulation of disulfiram and doxorubicin in liposomes strongly reverses multidrug resistance in breast cancer cells. Int. J. Pharm. 580, 119191. 10.1016/j.ijpharm.2020.119191 [DOI] [PubMed] [Google Scholar]
- Sam E., Athri P. (2019). Web-based drug repurposing tools: A survey. Brief. Bioinform. 20, 299–316. 10.1093/bib/bbx125 [DOI] [PubMed] [Google Scholar]
- Schmidtova S., Kalavska K., Gercakova K., Cierna Z., Miklikova S., Smolkova B., et al. (2019). Disulfiram Overcomes Cisplatin Resistance in Human Embryonal Carcinoma Cells, 11. 10.3390/cancers11091224 Cancers (Basel) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schuettengruber B., Bourbon H. M., di Croce L., Cavalli G. (2017). Genome regulation by polycomb and Trithorax: 70 Years and counting. Cell. 171, 34–57. 10.1016/j.cell.2017.08.002 [DOI] [PubMed] [Google Scholar]
- Seliger C., Genbrugge E., Gorlia T., Chinot O., Stupp R., Nabors B., et al. (2020). Use of metformin and outcome of patients with newly diagnosed glioblastoma: Pooled analysis. Int. J. Cancer 146, 803–809. 10.1002/ijc.32337 [DOI] [PubMed] [Google Scholar]
- Seliger C., Hau P. (2018). Drug repurposing of metabolic agents in malignant glioma. Int. J. Mol. Sci. 19, E2768. 10.3390/ijms19092768 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shameer K., Glicksberg B. S., Hodos R., Johnson K. W., Badgeley M. A., Readhead B., et al. (2018). Systematic analyses of drugs and disease indications in RepurposeDB reveal pharmacological, biological and epidemiological factors influencing drug repositioning. Brief. Bioinform. 19, 656–678. 10.1093/bib/bbw136 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shergill M., Patel M., Khan S., Bashir A., Mcconville C. (2016). Development and characterisation of sustained release solid dispersion oral tablets containing the poorly water soluble drug disulfiram. Int. J. Pharm. 497, 3–11. 10.1016/j.ijpharm.2015.11.029 [DOI] [PubMed] [Google Scholar]
- Shian S. G., Kao Y. R., Wu F. Y., Wu C. W. (2003). Inhibition of invasion and angiogenesis by zinc-chelating agent disulfiram. Mol. Pharmacol. 64, 1076–1084. 10.1124/mol.64.5.1076 [DOI] [PubMed] [Google Scholar]
- Shirley D. A., Sharma I., Warren C. A., Moonah S. (2021). Drug repurposing of the alcohol abuse medication disulfiram as an anti-parasitic agent. Front. Cell. Infect. Microbiol. 11, 633194. 10.3389/fcimb.2021.633194 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Skaga E., Skaga I., Grieg Z., Sandberg C. J., Langmoen I. A., Vik-Mo E. O. (2019). The efficacy of a coordinated pharmacological blockade in glioblastoma stem cells with nine repurposed drugs using the CUSP9 strategy. J. Cancer Res. Clin. Oncol. 145, 1495–1507. 10.1007/s00432-019-02920-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spillier Q., Vertommen D., Ravez S., Marteau R., THéMANS Q., Corbet C., et al. (2019). Anti-alcohol abuse drug disulfiram inhibits human PHGDH via disruption of its active tetrameric form through a specific cysteine oxidation. Sci. Rep. 9, 4737. 10.1038/s41598-019-41187-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Srivenugopal K. S., Rawat A., Niture S. K., Paranjpe A., Velu C., Venugopal S. N., et al. (2016). Posttranslational regulation of O(6)-methylguanine-DNA methyltransferase (MGMT) and new opportunities for treatment of brain cancers. Mini Rev. Med. Chem. 16, 455–464. 10.2174/1389557515666150722101046 [DOI] [PubMed] [Google Scholar]
- Stockhammer F., Misch M., Koch A., Czabanka M., Plotkin M., Blechschmidt C., et al. (2010). Continuous low-dose temozolomide and celecoxib in recurrent glioblastoma. J. Neurooncol. 100, 407–415. 10.1007/s11060-010-0192-y [DOI] [PubMed] [Google Scholar]
- Stupp R., Mason W. P., van Den Bent M. J., Weller M., Fisher B., Taphoorn M. J., et al. (2005). Radiotherapy plus concomitant and adjuvant temozolomide for glioblastoma. N. Engl. J. Med. 352, 987–996. 10.1056/NEJMoa043330 [DOI] [PubMed] [Google Scholar]
- Stylli S. S. (2020). Novel treatment strategies for glioblastoma. Cancers (Basel) 12, E2883. 10.3390/cancers12102883 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Swetha K. L., Sharma S., Chowdhury R., Roy A. (2020). Disulfiram potentiates docetaxel cytotoxicity in breast cancer cells through enhanced ROS and autophagy. Pharmacol. Rep. 72, 1749–1765. 10.1007/s43440-020-00122-1 [DOI] [PubMed] [Google Scholar]
- Tesson M., Anselmi G., Bell C., Mairs R. (2017). Cell cycle specific radiosensitisation by the disulfiram and copper complex. Oncotarget 8, 65900–65916. 10.18632/oncotarget.19539 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Triscott J., Lee C., Hu K., Fotovati A., Berns R., Pambid M., et al. (2012). Disulfiram, a drug widely used to control alcoholism, suppresses the self-renewal of glioblastoma and over-rides resistance to temozolomide. Oncotarget 3, 1112–1123. 10.18632/oncotarget.604 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Triscott J., Rose Pambid M., Dunn S. E. (2015). Concise review: Bullseye: Targeting cancer stem cells to improve the treatment of gliomas by repurposing disulfiram. Stem Cells 33, 1042–1046. 10.1002/stem.1956 [DOI] [PubMed] [Google Scholar]
- Turanli B., Altay O., BORéN J., Turkez H., Nielsen J., Uhlen M., et al. (2021). Systems biology based drug repositioning for development of cancer therapy. Semin. Cancer Biol. 68, 47–58. 10.1016/j.semcancer.2019.09.020 [DOI] [PubMed] [Google Scholar]
- Voorhees P. M., Orlowski R. Z. (2006). The proteasome and proteasome inhibitors in cancer therapy. Annu. Rev. Pharmacol. Toxicol. 46, 189–213. 10.1146/annurev.pharmtox.46.120604.141300 [DOI] [PubMed] [Google Scholar]
- Wang W., Mcleod H. L., Cassidy J. (2003). Disulfiram-mediated inhibition of NF-kappaB activity enhances cytotoxicity of 5-fluorouracil in human colorectal cancer cell lines. Int. J. Cancer 104, 504–511. 10.1002/ijc.10972 [DOI] [PubMed] [Google Scholar]
- Wang Y., Bryant S. H., Cheng T., Wang J., Gindulyte A., Shoemaker B. A., et al. (2017). PubChem BioAssay: 2017 update. Nucleic Acids Res. 45, D955-D963–d963. 10.1093/nar/gkw1118 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wehbe M., Anantha M., Shi M., Leung A. W., Dragowska W. H., Sanche L., et al. (2017). Development and optimization of an injectable formulation of copper diethyldithiocarbamate, an active anticancer agent. Int. J. Nanomedicine 12, 4129–4146. 10.2147/ijn.S137347 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Westhoff M. A., Zhou S., Nonnenmacher L., Karpel-Massler G., Jennewein C., Schneider M., et al. (2013). Inhibition of NF-κB signaling ablates the invasive phenotype of glioblastoma. Mol. Cancer Res. 11, 1611–1623. 10.1158/1541-7786.Mcr-13-0435-t [DOI] [PubMed] [Google Scholar]
- Weyerhäuser P., Kantelhardt S. R., Kim E. L. (2018). Re-Purposing chloroquine for glioblastoma: Potential merits and confounding variables. Front. Oncol. 8, 335. 10.3389/fonc.2018.00335 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wickström M., Danielsson K., Rickardson L., Gullbo J., Nygren P., Isaksson A., et al. (2007). Pharmacological profiling of disulfiram using human tumor cell lines and human tumor cells from patients. Biochem. Pharmacol. 73, 25–33. 10.1016/j.bcp.2006.08.016 [DOI] [PubMed] [Google Scholar]
- Wishart D. S., Feunang Y. D., Guo A. C., Lo E. J., Marcu A., Grant J. R., et al. (2018). DrugBank 5.0: A major update to the DrugBank database for 2018. Nucleic Acids Res. 46, D1074-D1082–d1082. 10.1093/nar/gkx1037 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu H., Huang J., Zhong Y., Huang Q. (2017). DrugSig: A resource for computational drug repositioning utilizing gene expression signatures. PLoS One 12, e0177743. 10.1371/journal.pone.0177743 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xu B., Shi P., Fombon I. S., Zhang Y., Huang F., Wang W., et al. (2011). Disulfiram/copper complex activated JNK/c-jun pathway and sensitized cytotoxicity of doxorubicin in doxorubicin resistant leukemia HL60 cells. Blood Cells Mol. Dis. 47, 264–269. 10.1016/j.bcmd.2011.08.004 [DOI] [PubMed] [Google Scholar]
- Xue H., Li J., Xie H., Wang Y. (2018). Review of drug repositioning approaches and resources. Int. J. Biol. Sci. 14, 1232–1244. 10.7150/ijbs.24612 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang H., Qin C., Li Y. H., Tao L., Zhou J., Yu C. Y., et al. (2016). Therapeutic target database update 2016: Enriched resource for bench to clinical drug target and targeted pathway information. Nucleic Acids Res. 44, D1069–D1074. 10.1093/nar/gkv1230 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang Z., Guo F., Albers A. E., Sehouli J., Kaufmann A. M. (2019). Disulfiram modulates ROS accumulation and overcomes synergistically cisplatin resistance in breast cancer cell lines. Biomed. Pharmacother. 113, 108727. 10.1016/j.biopha.2019.108727 [DOI] [PubMed] [Google Scholar]
- Yao W., Qian X., Ochsenreither S., Soldano F., Deleo A. B., Sudhoff H., et al. (2021). Disulfiram acts as a potent radio-chemo sensitizer in head and neck squamous cell carcinoma cell lines and transplanted xenografts. Cells 10, 517. 10.3390/cells10030517 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ye X. Q., Li Q., Wang G. H., Sun F. F., Huang G. J., Bian X. W., et al. (2011). Mitochondrial and energy metabolism-related properties as novel indicators of lung cancer stem cells. Int. J. Cancer 129, 820–831. 10.1002/ijc.25944 [DOI] [PubMed] [Google Scholar]
- Yip N. C., Fombon I. S., Liu P., Brown S., Kannappan V., Armesilla A. L., et al. (2011). Disulfiram modulated ROS-MAPK and NFκB pathways and targeted breast cancer cells with cancer stem cell-like properties. Br. J. Cancer 104, 1564–1574. 10.1038/bjc.2011.126 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang Y. W., Kaneda M., Morita I. (2003). The gap junction-independent tumor-suppressing effect of connexin 43. J. Biol. Chem. 278, 44852–44856. 10.1074/jbc.M305072200 [DOI] [PubMed] [Google Scholar]
- Zhao P., Wang Y., Kang X., Wu A., Yin W., Tang Y., et al. (2018). Dual-targeting biomimetic delivery for anti-glioma activity via remodeling the tumor microenvironment and directing macrophage-mediated immunotherapy. Chem. Sci. 9, 2674–2689. 10.1039/c7sc04853j [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zirjacks L., Stransky N., Klumpp L., Prause L., Eckert F., Zips D., et al. (2021). Repurposing disulfiram for targeting of glioblastoma stem cells: An in vitro study. Biomolecules 11, 1561. 10.3390/biom11111561 [DOI] [PMC free article] [PubMed] [Google Scholar]