Abstract
Introduction
The capacity of a healthy individual to estimate the true vertical in relation to the Earth when a fluorescent line is aligned in a completely dark room is called the subjective visual vertical.
Objective
To evaluate subjective visual vertical using the bucket method in healthy Brazilian individuals.
Methods
Binocular subjective visual vertical was measured in 100 healthy volunteers, 50 females and 50 males. The volunteers indicated the estimated position in which a fluorescent line inside a bucket reached the vertical position. A total of ten repetitions were performed, five clockwise and five counterclockwise. Data were tabulated and analyzed statistically.
Results
It was observed that the highest concentration of absolute values of vertical deviation was present up to 3°, regardless of gender, and the vertical deviation did not increase with age. The analysis of the mean of the absolute values of deviations from the vertical of 90% of the sample showed a maximum value of 2.6°, and at the analysis of 95%, the maximum value was 3.4° deviation from the vertical.
Conclusion
The bucket method is easy to perform and interpret when assessing the deviation of the subjective visual vertical in relation to the true vertical in healthy Brazilian individuals.
Keywords: Ear, Postural balance, Otolithic membrane
Resumo
Introdução
A capacidade que um indivíduo hígido tem em estimar a vertical verdadeira em relação à Terra, quando alinha uma linha fluorescente em uma sala completamente escura é denominada de Vertical Visual Subjetiva (VVS).
Objetivo
Avaliar a VVS com o método do balde em indivíduos brasileiros hígidos.
Método
A VVS binocular foi medida em 100 voluntários hígidos, 50 do gênero feminino e 50 do masculino. Os voluntários indicaram a posição estimada em que uma linha fluorescente no interior de um balde alcançou a posição vertical. Foram realizadas 10 repetições, cinco no sentido horário e cinco no anti-horário. Os dados foram tabulados e submetidos à análise estatística.
Resultados
Observou-se que a maior concentração dos valores absolutos dos desvios da vertical esteve presente até 3°, independente do gênero e o desvio da vertical não aumentou conforme a idade. À análise da média dos valores absolutos dos desvios da vertical de 90% da amostra, foi encontrado o valor máximo de 2,6° e à análise de 95% o valor máximo foi de 3,4° de desvio da vertical.
Conclusão
O método do balde é fácil de realizar e de interpretar na avaliação do desvio da vertical visual subjetiva em relação à vertical verdadeira de indivíduos brasileiros hígidos.
Palavras-chave: Orelha, Equilíbrio postural, Membrana otolítica
Introduction
The inner ear, also called the labyrinth, can be divided into anterior labyrinth, which contains the hearing organ (cochlea) and posterior labyrinth, comprising the three semicircular canals (lateral, superior, and posterior) and the vestibular system, which includes the utricle and the saccule.1 The inner ear vestibular system receptors consist of two types of structures: one cupula-endolymphatic system in the three semicircular canals, sensitive to angular accelerations, and an amalgam of otoliths within a viscoelastic membrane at the level of the utricular and saccular macula, sensitive to linear accelerations.1 Concomitant with information from the visual and proprioceptive systems, the cortical otolith afferents also participate in spatial orientation, motion perception, the mental representation of the body in space,1 and the perception of verticality.2, 3
The ability to judge whether the objects are in the vertical position is called subjective visual vertical (SVV).
In a healthy individual, the otolith organs alone can construct the SVV, even in cases of deprivation of visual and proprioceptive stimuli; in unilateral vestibular dysfunction, the recovery of SVV seems to be associated with the possibility of effectively using proprioceptive and exteroceptive information, particularly those of the plantar surface.4
The bucket method, the object of our research, was initially designed5 and then compared6 with the sophisticated and standardized hemispheric dome method,7 showing that the distribution of SVV values was similar for the two methods, thus demonstrating that the bucket method can become part of routine clinical examinations, as it is inexpensive and easy to perform.
In the dome method, a hemispheric dome covered with colored dots and a linear target is rotated randomly and the individual is instructed to align the target through a video game control, making it as vertical as possible; in the bucket method, a bucket is rotated and the individual indicates when a fluorescent straight line displayed in the inferior and inner part of the bucket reaches a vertical position.6 In the bucket method, the range of absolute deviations of the SVV values in relation to the true vertical in healthy subjects was 0.9 ± 0.7° (mean ± standard deviation); no significant effect of age or gender was identified.6
Another study indicated that the bucket method is useful to describe spatial deficits in patients with proven vestibular disorder, but not as a screening test. In 50 healthy subjects, the mean (standard deviation, minimum/maximum) of the absolute values of vertical deviation was 1.2° (0.7; 0°/3.2°) for females; and 1.0° (0.8; 0°/2.7°) for males.8
In Brazil, SVV was evaluated in 30 healthy Brazilian individuals by adjusting a virtual line in the vertical position with a computer mouse, projected on a white screen. The mean deviation of SVV was −0.372° ± 1.21; representing six repetitions.9
Another study with of 160 healthy Brazilian individuals determined the SVV using a 24-cm portable stick with fluorescent light, positioned in front of the individuals and at the level of their eyes. The assessed individuals wore glasses with light-filtering lenses that made any other visual afferent information impossible, with the exception of the fluorescent light, perceived as a green line. Ten SVV adjustments were made, one for each side, totaling five in the clockwise and five in the counterclockwise direction. The angular inclinations of the vertical position were measured in degrees and defined as positive for clockwise and negative for the counterclockwise deviations, in relation to the patient. The results of SVV showed the mean values of ten adjustments, ranging between −2.0° and +2.4° (mean = 0.18, SD = 0.77).10
Several studies have shown the importance of vestibular assessment by SVV with different methods, and also with the bucket method. However, to apply this method in Brazil, it is important to know the behavior of healthy Brazilian individuals, for subsequent comparison with patients who have vestibular disorders. Considering the semiological value of the SVV assessment and the scarcity of national studies using the bucket method, which is inexpensive and easy to apply, it was decided to perform this investigation.
The objective of this study was to assess the SVV using the bucket method in healthy Brazilian individuals.
Methods
This study was performed after approval by the Research Ethics Committee of the institution under protocol No. 51439/12.
The sample of this cross-sectional study consisted of 100 healthy adult volunteer individuals from the community, 50 females and 50 males, with no complaints of vestibular disorders and/or hearing loss; individuals with cognitive impairment, severe visual acuity alteration, and history of neurological disease were excluded.
The SVV evaluation was performed using a bucket, as well as inexpensive and easily acquired materials: an opaque plastic bucket, with a border larger than 25 cm, cardboard, string, fluorescent tape, weights (screw nuts), and adhesive tape. A piece of fluorescent tape, placed vertically on the inner side of the bottom of the bucket, was perfectly aligned with the zero mark of a protractor positioned on the external and inferior part of the bucket, and both were aligned with the true vertical in relation to the Earth11 (Figure 1, Figure 2).
Figure 1.

View of the fluorescent tape on the bottom of the inside of the bucket.
Figure 2.

View of the outside and bottom of the bucket.
The SVV was measured binocularly. The healthy volunteers were asked to look at a fluorescent line inside the bucket, in the sitting position, with their heads up6 (Fig. 3). In some cases, when it was impossible for the visual field to be completely inside the bucket, the volunteer's head and the bucket were covered with a dark cloth to prevent visual cues (Fig. 4).
Figure 3.

Applying the bucket method.
Figure 4.

Applying the bucket method using a dark cloth.
To measure the SVV, the bucket was randomly rotated by the examiner, to exclude possible tactile cues, in the clockwise or counter-clockwise directions, to a final position around 15°, and then slowly rotated toward the zero degree position. The volunteers indicated the estimated position where the fluorescent line had reached the vertical position, asking the examiner to stop moving the bucket, by saying “stop”. Ten repetitions of the procedure were performed, five in the clockwise and five in the anti-clockwise direction; the identified values were recorded in the degree scale on the outside of the bucket. The angular inclinations of the vertical position were measured in degrees and defined as positive deviations in the clockwise and negative in the anti-clockwise direction, in relation to the volunteer. The procedure was repeated when the examiner moved the bucket too fast, without giving the patient enough time for the response.
The findings were recorded, tabulated, and submitted to descriptive statistical analysis using mean, median, standard deviation, and maximum and minimum values of the mean of absolute values of deviations from true vertical in ten repetitions of the procedure, regardless of the movement direction. The joint distribution of the angular deviation from the vertical and age was illustrated by a two-dimensional scatter plot graph and the 50%, 90%, and 95% percentiles. The Mann–Whitney test was used to compare the genders regarding the mean of absolute values of deviations from the vertical. The level of significance was 5% (α = 0.05) and SPSS v. 19 for Windows and Office Excel 2007 were used in the statistical analysis.
Results
A total of 100 healthy volunteers was evaluated, 50 females and 50 males, aged between 18 and 59 years, with no complaints of vestibular disorders and/or hearing loss.
Table 1 shows the mean, median, standard deviation, and minimum and maximum values of the mean of the absolute values of deviations from the vertical of ten repetitions in the 50 female and male volunteers.
Table 1.
Measurements – summary of absolute values of deviations from the vertical, according to gender and statistical comparison.
| Deviations from vertical | Female gender | Male gender |
|---|---|---|
| n | 50 | 50 |
| Mean | 2.02 | 1.66 |
| Median | 2.00° | 1.65 |
| Minimum value | 0.4 | 0.6 |
| Maximum value | 4.1 | 3.4 |
| Standard deviation | 0.8042 | 0.6386 |
| pa | 0.026 | |
Mann–Whitney test.
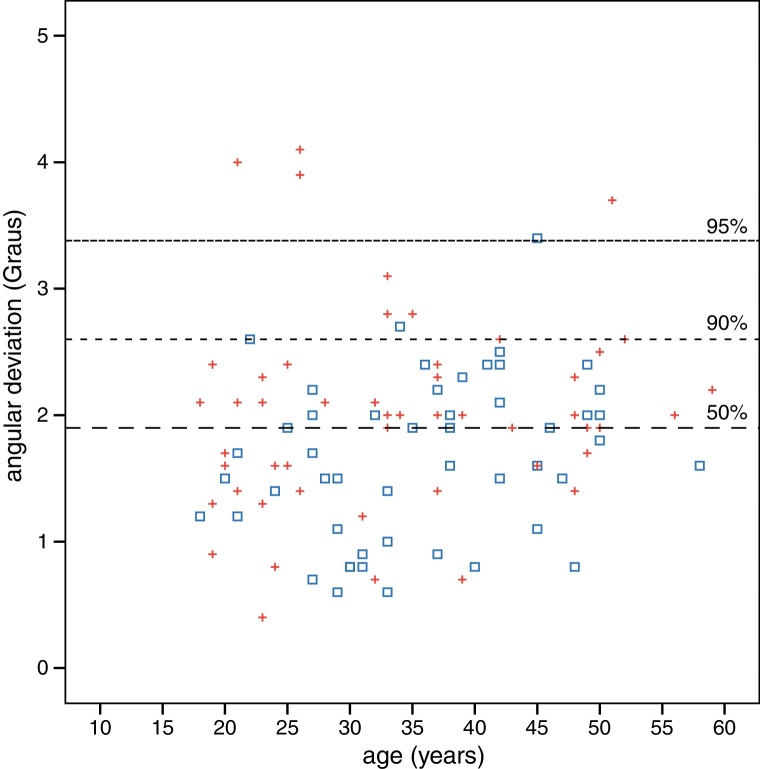
Fig. 5 represents the mean of the absolute values of deviations from the vertical regarding age and gender. It can be observed that the highest concentration of values can be found up to 3° of vertical deviation, regardless of gender, and that the vertical deviation does not increase with age. The analysis of the mean of the absolute values of deviations from the vertical of 90% of the sample showed a maximum value of 2.6° and the 95% analysis found a maximum value of 3.4° of deviation from vertical.
Figure 5.
Two-dimensional scatter plot and the 50%, 90%, and 95% percentiles of the mean of the absolute values of deviations from the vertical (degrees) and the age (years) according to gender (+ female/male).
Discussion
SVV assessment is a simple technique to study otolith function, as the inclination of the fluorescent line beyond the values considered to be normal is the most sensitive sign of vestibular system dysfunction; the bucket test is inexpensive and easy to perform; the analysis of the results is simple, the test is fast and reliable, and it can be applied anywhere, warranting its broad use.6
In this study, the SVV assessment in 100 individuals without vestibular and/or hearing complaints showed a significant difference between the mean of the absolute values of deviations from the vertical in female and male volunteers, similar to previous reports in the literature.8
The original study using the bucket method did not identify an effect of gender and age on the deviation from the vertical.6 However, according to the two-dimensional scatter plot graph, the sample can be considered homogenous regarding gender and age, and when 90% of the sample was analyzed, the values were found up to 2.6°, or approximately 3°, as the bucket method identifies angular deviation values in whole numbers. The value of 2.6° is similar to the value of 2.3° found in the original study using the bucket method.6 Another study,12 assessing the performance of healthy elderly individuals, adopted a deviation of 3° as the normal limit, similar to that of the present study, also making an approximation of the standard values used as reference.6
The SVV was evaluated in healthy Brazilian individuals through other methods that identified values similar to that found in this study; the mean deviation from SVV was −0.372 ± 1.21° with the method that used a computer mouse to adjust a virtual line in the vertical position projected on a white screen,9 and it ranged between −2.0° and +2.4° in another study that used a portable stick with fluorescent light.10
As previously noted,6, 13 the authors also believe that an easy-to-perform and easy-to-interpret SVV evaluation should be included in routine clinical vestibular tests, as it can provide information on the otolith organ function and also can monitor changes and responses to treatment in patients with central or peripheral vestibular disorders.
The aim of this study was to evaluate SVV using the bucket method in healthy Brazilian individuals with no auditory and vestibular complaints. It is hoped that these findings utilizing this method may be useful in clinical practice and in future studies, in order to help characterize vestibular system dysfunction in patients with body balance disorders.
Conclusion
The bucket method is easy to perform and interpret when evaluating the deviation of the SVV in relation to true vertical in healthy Brazilian individuals.
Conflicts of interest
The authors declare no conflicts of interest.
Footnotes
Please cite this article as: Ferreira MM, Cunha F, Ganança CF, Ganança MM, Caovilla HH. Subjective visual vertical with the bucket method in Brazilian healthy individuals. Braz J Otorhinolaryngol. 2016;82:442–6.
References
- 1.Maia F.C.Z. 2nd ed. Revinter; Rio de Janeiro: 2011. Elementos práticos em otoneurologia. [Google Scholar]
- 2.Anastasopoulos D., Bronstein A.M. A case of thalamic syndrome: somatosensory influences on visual orientation. J Neurol Neurosurg Psychiatry. 1999;67:390–394. doi: 10.1136/jnnp.67.3.390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Schwarz U. Neuroophthalmology: a brief Vademecum. Eur J Radiol. 2004;49:31–63. doi: 10.1016/j.ejrad.2003.09.006. [DOI] [PubMed] [Google Scholar]
- 4.Faralli M., Longari F., Ricci G., Ibba M.C., Frenguelli A. Influence of extero and proprioceptive afferents of the plantar surface in determining subjective visual vertical in patients with unilateral vestibular dysfunction. Acta Otorhinolaryngol Ital. 2009;29:245–250. [PMC free article] [PubMed] [Google Scholar]
- 5.Frisén L. Practical estimation of ocular torsion and subjective vertical. Neuro-ophthalmology. 2000;23:195. [Google Scholar]
- 6.Zwergal A., Rettinger N., Frenzel C., Dieterich M., Brandt T., Strupp M. A bucket of static vestibular function. Neurology. 2009;72:1689–1692. doi: 10.1212/WNL.0b013e3181a55ecf. [DOI] [PubMed] [Google Scholar]
- 7.Dieterich M., Brandt T. Ocular torsion and tilt of subjective visual vertical are sensitive brainstem signs. Ann Neurol. 1993;33:292–299. doi: 10.1002/ana.410330311. [DOI] [PubMed] [Google Scholar]
- 8.Cohen H.S., Sangi-Haghpeykar H. Subjective visual vertical in vestibular disorders measured with the bucket test. Acta Otolaryngol. 2012;132:850–854. doi: 10.3109/00016489.2012.668710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Pavan T.Z., Funabashi M., Carneiro J.A., Pontelli T.E., Tedeschi W., Colafêmina J.F., et al. Software for subjective visual vertical assessment: an observational cross-sectional study. Braz J Otorhinolaryngol. 2012;78:51–58. doi: 10.5935/1808-8694.20120008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kanashiro A.M.K., Pereira C.B., Maia F.M., Scaff M., Barbosa E.R. Avaliação da vertical visual subjetiva em indivíduos brasileiros normais. Arq Neuropsiquiatr. 2007;65:472–475. doi: 10.1590/s0004-282x2007000300021. [DOI] [PubMed] [Google Scholar]
- 11.Cook J. SVV Bucket construction (last edited 2010-05-05 09:14:00 by James Cook), University of Pittsburgh.
- 12.Davalos-Bichara M., Agrawal Y. Normative results of healthy older adults on standard clinical vestibular tests. Otol Neurotol. 2014;35:297–300. doi: 10.1097/MAO.0b013e3182a09ca8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Cal R. In: Otoneurologia atual. Zuma e Maia F.C., Mangabeira Albernaz P.L., Carmona S., editors. Revinter; Rio de Janeiro: 2014. Visual vertical subjetiva (VVS) pp. 141–146. [Google Scholar]