Abstract
Introduction
When there is a change in the physiological pattern of nasal breathing, mouth breathing may already be present. The diagnosis of mouth breathing is related to nasal patency. One way to access nasal patency is by acoustic rhinometry.
Objective
To systematically review the effectiveness of acoustic rhinometry for the diagnosis of patients with mouth breathing.
Methods
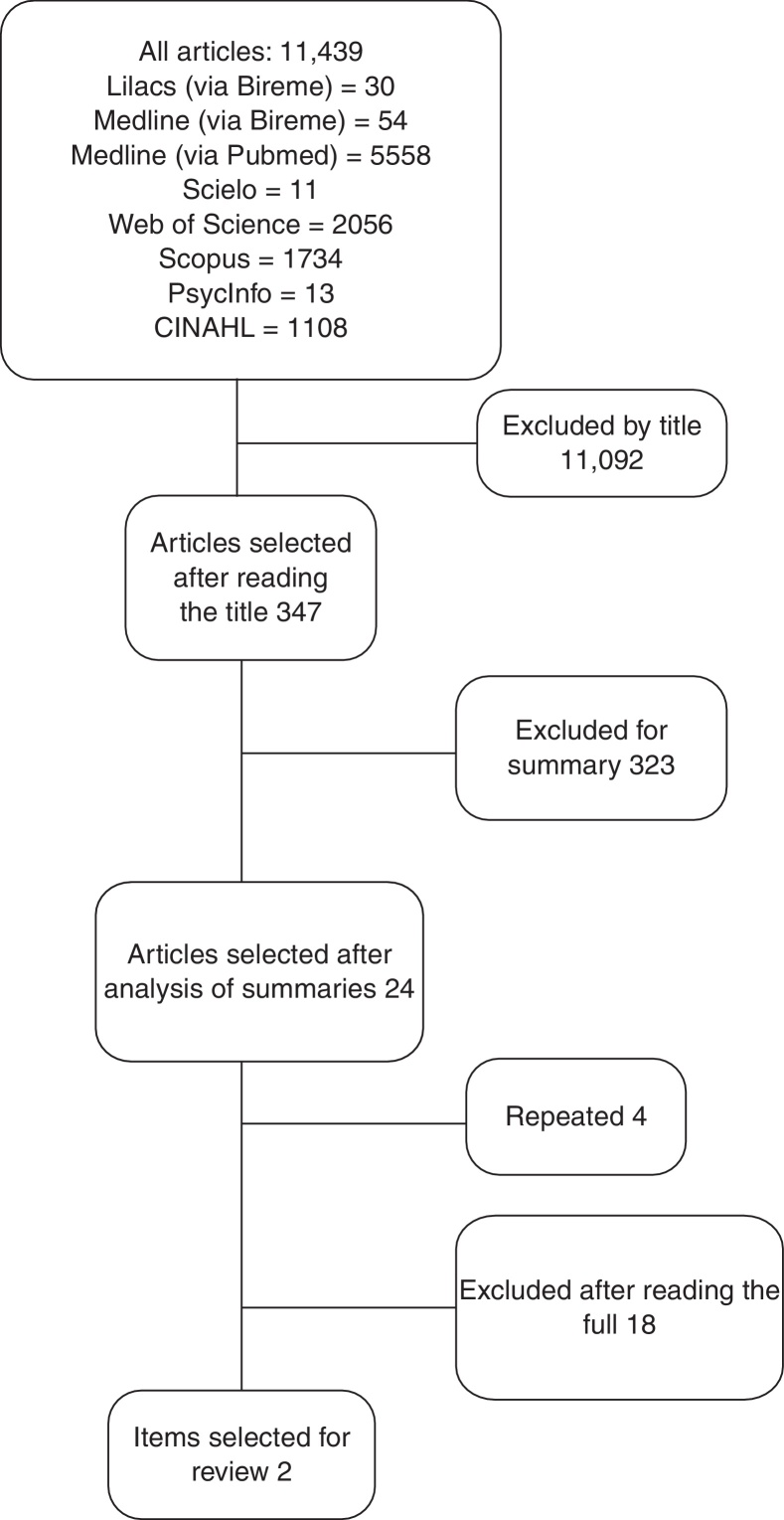
Electronic databases LILACS, MEDLINE via PubMed and Bireme, SciELO, Web of Science, Scopus, PsycInfo, CINAHL, and Science Direct, from August to December 2013, were consulted. 11,439 articles were found: 30 from LILACS, 54 from MEDLINE via Bireme, 5558 from MEDLINE via PubMed, 11 from SciELO, 2056 from Web of Science, 1734 from Scopus, 13 from PsycInfo, 1108 from CINAHL, and 875 from Science Direct. Of these, two articles were selected.
Results
The heterogeneity in the use of equipment and materials for the assessment of respiratory mode in these studies reveals that there is not yet consensus in the assessment and diagnosis of patients with mouth breathing.
Conclusion
According to the articles, acoustic rhinometry has been used for almost twenty years, but controlled studies attesting to the efficacy of measuring the geometry of nasal cavities for complementary diagnosis of respiratory mode are warranted.
Keywords: Acoustic rhinometry, Mouth breathing, Diagnosis, Nasal cavity
Resumo
Introdução
Quando há alteração no padrão respiratório nasal fisiológico, a respiração oral de suplência já pode estar presente. O diagnóstico da respiração oral vincula-se à permeabilidade nasal. Uma das possibilidades para avaliação da permeabilidade nasal é a rinometria acústica.
Objetivo
Revisar, de forma sistemática, a eficácia da rinometria acústica no auxílio diagnóstico de pacientes com respiração oral.
Método
Foram consultadas as bases de dados eletrônicas LILACS, MEDLINE via Bireme e via PUBMED, SciELO, Web of Science, Scopus, PsycInfo, CINAHL e Science Direct, de agosto a dezembro de 2013. Foram encontrados 11.439 artigos, sendo 30 da LILACS, 54 da MEDLINE via Bireme, 5.558 da MEDLINE via Pubmed, 11 da Scielo, 2.056 da Web of Science, 1.734 da Scopus, 13 da PyscInfo, 1.108 da CINAHL e 875 Science Direct. Desses, foram selecionados dois artigos.
Resultados
A heterogeneidade no uso dos equipamentos e materiais utilizados para a avaliação do modo respiratório nesses estudos mostra que ainda não há um consenso na avaliação e diagnóstico de indivíduos com respiração oral.
Conclusão
De acordo com os artigos, a rinometria acústica é utilizada há quase vinte anos, porém são necessários estudos controlados que atestem a eficácia da mensuração da geometria das cavidades nasais como auxílio diagnóstico do modo respiratório.
Palavras-chave: Rinometria acústica, Respiração bucal, Diagnóstico, Cavidade nasal
Introduction
Nasal breathing plays an important role in vital body functions, such as air filtration, heating and humidification of inspired air, a first defense barrier against inhaled allergens, and protection of the paranasal sinuses, ear cavities and lower airways; as its primary function, nasal breathing prepares the air for its optimal utilization in the lungs.1, 2, 3 When a person is unable to use his/her nasal airways, changes in physiological nasal breathing pattern will occur and, thereafter, mouth breathing ensues.4
However, the literature exhibits conflict in defining what is considered normal breathing through the nose, as well as in objectively identifying nasal obstruction.5, 6 Moreover, although the diagnosis of mouth breathing is related to nasal obstruction, this situation is not always the case, especially when oral breathing mode has become chronic.
For decades, specific tests for evaluation of nasal permeability have been used in order to quantify the subjective symptom of nasal obstruction.5
The Altman graph mirror, for example, is one of the instruments used in clinical practice to assess nasal patency. Its metal plate has a smooth side, and the other side shows millimeter markings, allowing for a precise measurement of the area marked by the nasal exhalation,7 comparing the condensation area between the nasal cavities.8
However, acoustic rhinometry is one of the newest methods for statically measuring different segments of the nasal cavity, from the nostrils to the choanae, quickly and non-invasively, and ‘requiring little patient cooperation.9, 10 The technique is based on the analysis of the nasal cavity's reflected sound from incident sound waves, taking into account the properties of this sound in relation to the intensity and arrival time of the echo.9 Therefore, this technique enables the measurement of the distances corresponding to the cross-sectional areas, usually of the nasal valve area and the front and rear areas of the conchae, and the calculation of nasal volumes, allowing the identification of the loci of constrictions that contribute to nasal resistance11, 12 thus providing topographical information on the individual profile of the nasal and nasopharyngeal airways.13
Its reproducibility and accuracy were confirmed by several authors,14, 15, 16, 17, 18 the procedures are standardized and shown to be reliable,11, 19, 20, 21, 22 and research on reference values in adults and children have also been reported.12, 23, 24, 25, 26, 27
The technique is also used by several authors to estimate nasal airway obstruction in different etiologies, as well as the effect of distinct pathologies and surgical and orthopedic procedures on nasal and nasopharyngeal cavities in pediatric and adult populations.18, 28, 29, 30, 31, 32, 33, 34, 35, 36, 37
The clinical value of acoustic rhinometry rests in its ability to measure nasal geometry, thus being an important tool for the clinical rhinological follow-up,9, 38, 39 allowing for the discrimination between mucosal functional effects and structural changes related to nasal obstruction, when used in tests before and after treatment with a vasoconstrictor.39
Although the test does not provide an etiological diagnosis of nasal obstruction, it quantifies the magnitude of the obstructive symptom at any given time, and is therefore considered a specific test in the investigation of nasal patency,5, 21, 40 complementary to clinical examination.
Given the importance of nasal patency for the establishment of a physiological nasal breathing and the negative impact of nasal obstruction on stomatognathic system functions,41 including speech/articulation, this article aims to systematically review the effectiveness of acoustic rhinometry as a complementary procedure to the diagnosis of mouth breathers.
Methods
A systematic literature review was performed from the following databases: LILACS via MEDLINE, MEDLINE via Bireme, MEDLINE via PubMed, SciELO, Web of Science, Scopus, PsycInfo, CINAHL, and Science Direct. The data search occurred from August to December 2013. To this investigation, descriptors and crossings used are shown in Table 1.
Table 1.
Search strategies for database (MeSH and MeSH) survey.
| Crossings in English | Crossings in Spanish | Crossings in Portuguese |
|---|---|---|
| “Acoustic rhinometry” and “mouth breathing” | “Rinometría acústica” and “Respiración por la boca” | “Rinometria acústica” and “Respiração bucal” |
| “Acoustic rhinometry” and “diagnosis” | “Rinometría acústica” and “Diagnóstico” | “Rinometria acústica” and “Diagnóstico” |
| “Diagnosis” and “mouth breathing” | “Diagnóstico” and “Respiración por la boca” | “Diagnóstico” and “Respiração bucal” |
| “Nasal cavity” and “mouth breathing” | “Cavidad nasal” and “Respiración por la boca” | “Cavidade nasal” and “Respiração bucal” |
| “Nasal cavity” and “diagnosis” | “Cavidad nasal” and “Diagnóstico” | “Cavidade nasal” and “Diagnóstico” |
| “Nasal cavity” and “acoustic rhinometry” | “Cavidad nasal” and “Rinometría acústica” | “Cavidade nasal” and Rinometria acústica” |
The search was conducted by two researchers independently, following criteria of inclusion and exclusion. As inclusion criteria, original articles (whose manuscripts were published in any language) addressing the effectiveness of the instrument of acoustic rhinometry in the evaluation of oral breathing were selected.
Literature review articles and editorials were excluded, as well as those papers with no words referring to the subject discussed in this review, those that did not use the instrument of acoustic rhinometry as a complementary diagnostic, and studies on animals.
The methodological characteristics of articles were addressed according to inclusion criteria, statistical analysis and statistical comparison between selected groups (Table 2).
Table 2.
Methodological classification of selected articles.
| Articles and criteria | Zavras et al. (1994) | Fensterseifer et al. (2013) |
|---|---|---|
| 1. Specified inclusion criteria | Yes | Yes |
| 2. Control group | Yes | Yes |
| 3. Random allocation | No | No |
| 4. Confidentiality in allocation | No | No |
| 5. “Blind” subjects | No | No |
| 6. “Blind” therapists | No | No |
| 7. Statistical analysis | Yes | Yes |
| 8. Statistical comparison between groups | Yes | Yes |
Results
We can observe in the flow chart the number of items found and selected after applying our inclusion and exclusion criteria, according to descriptors and databases (Fig. 1).
Figure 1.
Flow chart: number of articles found.
To better present the results and to cover the proposed objectives, it was decided to consider the following variables of the selected articles: author/year, location, type of study, sample, equipment/methods used and results (Table 3).
Table 3.
Study variables.
| Author/year | Local | Study type | Sample | Equipment/methods used | Results |
|---|---|---|---|---|---|
| Zavras, White, Rich, Jackson/1994 | Boston, USA | Quantitative descriptive analytical study | 20 children: 10 predominantly mouth breathers; 10 nose breathers. | Breathing mode noted by the pediatric dentist. | In relation to the total volume of both nostrils, it was found that the values of the group of nose breathers (17.7 + 4.9 mL) were significantly higher than those of the group of mouth breathers (12.0 + 4.1 mL). |
| Mean ages of the groups with oral and nasal breathing were 10.1 and 10.2 years, respectively. | Application of a questionnaire for the child's parents and/or guardians for obtaining information about medical/dental history and breathing mode. | No significant difference was observed between minimum cross-section areas. | |||
| Evaluation of nasal cavities with acoustic rhinometry equipment (EK Electronics, Aarhus, Denmark). | |||||
| Fensterseifer, Carpes, Weckx, Martha/2013 | Porto Alegre, RS, Brazil | Case control study | 48 children: 24 with nasal obstruction and learning difficulty. 24 children without learning difficulty, with and without nasal obstruction. | Evaluation of nasal breathing according to the “Protocol for the evaluation of children with learning disabilities.” | In comparing the two groups, nasal obstruction (p = 0.14) shows a trend to be higher in the group with learning difficulties. |
| Ages between 8–12 years, with an average of 9.1 years. | Oroscopy, anterior rhinoscopy and cavum X-ray carried out. | Highly consistent relationship between learning disability and pharyngeal tonsil hypertrophy (p < 0.001). | |||
| Acoustic rhinometry. | Size of nasal cavities; this association was not consistent (p = 0.75). | ||||
Discussion
In the twentieth XIX, specifically in 1977, Jackson et al. developed studies on the acoustic reflex technique with the aim to calculate cross-sectional areas of trachea, pharynx and supraglottic region.42 Only in 1989, Hilberg et al.9 introduced the method of rhinometry as an acoustic reflection method, adapted to nasal cavities. Such a method can be defined as an objective assessment of nasal patency (or permeability), based on the reflection of a sound wave and offering information on the dimensions and geometry of nasal cavity.11, 12, 27, 43
The use of this technique in the evaluation of mouth breathers has been maturing over the last twenty years. In this investigation, we found two articles that addressed the proposed theme and perceived heterogeneity between these papers, with respect to the authors and publication periods. In the manuscripts included in our study, the beginning of the use of acoustic reflection technique for breathing-mode evaluation and characterization was observed, following an interval of almost two decades to the applicability of this same technique. From the paper published in 1994 to the year 2013,44, 45 no studies depicting the use of acoustic rhinometry as a complementary procedure for the diagnosis of mouth breathing were published.
The objective assessment of nasal permeability in patients with nasal obstruction has been developed with the use of the acoustic reflection method, through investigations in populations with allergic rhinitis, hypertrophy of palatine tonsils and recurrent respiratory infections.1, 46, 47, 48 Mouth breathing has been underlined in publications using acoustic rhinometry, as a consequence of nasal obstruction. Due to this fact, we found large gaps between the studies here evaluated.
With respect to the origin, the manuscripts included in this review are from North America (Boston, United States) and South America (Porto Alegre, Brazil).44, 45 However, the last US publication on the proposed issue occurred in 1994, showing that the use of acoustic rhinometry equipment in Brazil continues in its update process in a wide range of populations, including the assessment and diagnosis of oral breathing. In the included manuscripts, we observe similarities regarding the type of study, in which they present specified inclusion criteria, presence of a control group, statistical analysis and statistical comparison between groups. These manuscripts are characterized as quantitative, descriptive analytical study,43 and as case control study.45
The sampling procedure is a relevant aspect underlined in the manuscripts, and revealed a similarity in the small number of subjects in the first article (20; 10 in each group)44 versus a slightly more than twice (48; 24 in each group) the number of subjects in the second article.45 It is assumed that the small numbers of individuals presented in these studies may compromise the reproducibility of the findings for the general population. In the manuscripts, the participants’ age is also similar: children between eight and 12 years with an approximate means of 9.145 and 10.1 years.44 This is in line with other studies using the same technique with pediatric populations, both for mean age and number of participants.31, 48, 49
In studies evaluating surgical procedures for nasal obstruction, acoustic rhinometry is used to quantify the success of these surgeries. Considering that this is a method available which provides the geometric measure of the nasal cavity by means of a reflected acoustic signal, its result is a wave called rhinogram, which has the typical form of a “W”. Thus, this method provides some parameters, such as the minimum cross-sectional area (region of higher resistance to air flow) and volume at specific segments.31, 49, 50
Another important aspect is how the sample is divided. In both articles included in this review there is a division of two sample groups: a group of mouth breathers and another predominantly with nose breathers. The statistical comparison between groups44, 45 shows the homogeneity of these variables in our selected studies. This is consistent with studies using the same methodology to compare groups, with predominance of publications studying allergic rhinitis populations and control groups.41, 48
In both manuscripts included in this review, the method of acoustic rhinometry to evaluate oral breathing was used. Zavras et al.44 used an EK Electronics (Aarhus, Denmark) acoustic rhinometer. This was an observational clinical evaluation of respiratory mode by a pediatric dentist, followed by a questionnaire given to relatives/carers. On the other hand, the Fenterseifer et al.45 did not specify which rhinometric equipment was used; on the other hand, these authors performed ENT tests of oroscopy, anterior rhinoscopy and cavum X-ray, in addition to the clinical evaluation of respiratory mode through the Protocol for the Assessment of Children with Learning Disabilities.
Differences in the use of equipment and in materials for breathing mode evaluation between studies were observed, showing that there has not yet been consensus on the assessment and diagnosis of mouth breathers. Moreover, our analysis shows the limited number of publications demonstrating the use of a device that aims to measure the nasal cavity area – a very important resource as a complementary procedure for the diagnosis of patients’ respiratory mode.
The articles in this review were statistically analyzed using the same statistical test for independent samples. In the study published in 1994,44 a data analysis was carried out with the paired t-test for independent samples; with this test, in the analysis of the total volume of both nostrils, it was found that the values of group B – predominantly with nasal breathers (17.7 + 4.9 mL) – were significantly higher than those obtained for Group A – with mouth breathers (12.0 + 4.1 mL). On the other hand, the Spearman correlation test used for the analysis between nasal cavities showed significant correlations between minimum area of each nostril and the corresponding volume of the nostril being analyzed. However, the study published in 201345 reported that in the evaluation of nasal cavity volume by acoustic rhinometry, the results showed no consistent relationship in the comparison between the two groups studied with respect to the sum of the mean volume of nasal cavities (p = 0.75). In general, the selected studies show that a decrease in nasal geometry occurs in mouth breathing children. We can infer that the absence of more significant statistic data could be related to the small number of subjects in these studies.
Despite not being directed to oral breathing, a study of 101 subjects demonstrated significant differences in nasal geometry, volume and minimal cross-sectional area between groups with different degrees (mild, moderate and severe) of nasal obstruction.47 This finding shows that the study of a greater number of subjects results in better significant differences.
These results indicate the need for more detailed studies in the population of mouth breathers, with investments in objective and quantitative methods, as well as in standardized tests.
Conclusion
In this review, the included studies attest to the use of acoustic rhinometry in the population of mouth breathers. Although there may be a theoretical consensus regarding geometry and volume decreases of nasal cavities in mouth breathers, it has not yet been possible to demonstrate scientifically and clinically this decrease, compared to nose breathers. According to the articles investigated, this technique has already been applied for almost twenty years, but controlled studies attesting to the efficacy of measuring the area of nasal cavities for complementary diagnosis of respiratory mode are needed.
Conflicts of interest
The authors declare no conflicts of interest.
Footnotes
Please cite this article as: de Melo AC, Gomes AO, Cavalcanti AS, da Silva HJ. Acoustic rhinometry in mouth breathing patients: a systematic review. Braz J Otorhinolaryngol. 2015;81:212–8.
Institution: Universidade Federal de Pernambuco (UFPE), Recife, PE, Brazil.
References
- 1.Trindade I.E.K., Conegliam P.C.P., Trindade S.H.K., Dias N.H., Sampaio-Teixeira A.C.M. Internal nasal dimensions of adults with nasal obstruction. Braz J Otorhinolaryngol. 2013;79:575–581. doi: 10.5935/1808-8694.20130103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ferreira M.L. A incidência de respiradores bucais em indivíduos com oclusão classe II. J Bras Ortodon Ortop Facial. 1999;4:223–240. [Google Scholar]
- 3.Di Francesco R.C. Respirador bucal: a visão do otorrinolaringologista. J Bras Ortodon Ortop Facial. 1999;4:241–247. [Google Scholar]
- 4.Cópio F.C. Faculdade de Medicina da Universidade Federal de Minas Gerais; Belo Horizonte, MG: 2008. A capacidade funcional da criança respiradora oral avaliada pelo teste de caminhada de seis minutos. [dissertação] [Google Scholar]
- 5.Roithmann R. Testes específicos da permeabilidade nasal. Braz J Otorhinolaryngol. 2007;73:2. doi: 10.1016/S1808-8694(15)31114-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Baraniuk J. Subjective nasal fullness and objective congestion. Proc Am Thorac Soc. 2011;8:62–69. doi: 10.1513/pats.201006-042RN. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Cunha D.A., Silva H.J., Moraes K.J.R., Cunha R.A., Régis R.M.F.L., Silva E.G.F. Aeração nasal em crianças asmáticas. Rev CEFAC. 2011;13:783–789. [Google Scholar]
- 8.Brecvovici S., Roithmann R. A reprodutibilidade do espelho de glatzel modificado na aferição da permeabilidade nasal. Braz J Otorhinolaryngol. 2008;74:215–222. doi: 10.1016/S1808-8694(15)31091-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hilberg O., Jackson A.C., Swift D.L., Pedersen O.F. Acoustic rhinometry: evaluation of nasal cavity geometry by acoustic reflection. J Appl Phycol. 1989;66:295–303. doi: 10.1152/jappl.1989.66.1.295. [DOI] [PubMed] [Google Scholar]
- 10.Djupesland P., Pedersen O.F. Acoustic rhinometry in infants and children. Rhinol Suppl. 2000;16:52–58. [PubMed] [Google Scholar]
- 11.Hilberg O. Objective measurement of nasal airway dimensions using acoustic rhinometry: methodological and clinical aspects. Allergy. 2002;57(Suppl. 70):5–39. doi: 10.1046/j.0908-665x.2001.all.doc.x. [DOI] [PubMed] [Google Scholar]
- 12.Trindade I.E.K., Gomes A.O.C., Sampaio-Teixeira A.C.M., Trindade S.H.K. Adult nasal volumes assessed by acoustic rhinometry. Braz J Otorhinolaryngol (Engl Ed) 2007;73:32–39. doi: 10.1016/S1808-8694(15)31119-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kunkel M., Wahlmann U., Wagner W. Nasal airway in cleft-palate patients: acoustic rhinometric data. J Cranio-Max Fac Surg. 1997;25:270–274. doi: 10.1016/s1010-5182(97)80065-0. [DOI] [PubMed] [Google Scholar]
- 14.Wilson A.M., Fowler S.J., Martin S.W., White P.S., Gardiner Q., Lipworth B.J. Evaluation of the importance of head and probe stabilisation in acoustic rhinometry. Rhinology. 2001;39:93–97. [PubMed] [Google Scholar]
- 15.Fonseca M.J., Goto E.Y., Nigro C.E.N., Rocha F.M., Mello Junior J.F., Voegels R.L. Reprodutibilidade e repetibilidade da rinometria acústica. Arq Otorrinolaringol. 2003;7:213–218. [Google Scholar]
- 16.Ouriques D.M., Carlini D., Fujita R., Pignatari S.S.N.P., Weckx L.L.M. Correlation between fiberoptic nasal endoscopy and acoustic rhinometry in adults without nasal complaints. Am J Rhinol. 2006;20:375–378. doi: 10.2500/ajr.2006.20.2874. [DOI] [PubMed] [Google Scholar]
- 17.Castano R., Thériaoult G., Gautrin D., Ghezzo H., Trudeau C., Malo J. Reproducibility of acoustic rhinometry in the investigation of occupational rhinitis. Am J Rhinol. 2007;21:474–477. doi: 10.2500/ajr.2007.21.3039. [DOI] [PubMed] [Google Scholar]
- 18.Doruk C., Söcükü O., Biçakçi A.A., Yilmaz U., Tas F. Comparison of nasal volume changes during rapid maxillary expansion using acoustic rhinometry and computed tomography. Eur J Orthod. 2007;29:251–255. doi: 10.1093/ejo/cjl069. [DOI] [PubMed] [Google Scholar]
- 19.Hilberg O., Pedersen O.F. Acoustic rhinometry: recommendations for technical specifications and standard operating procedures. Rhinol Suppl. 2000;16:3–17. [PubMed] [Google Scholar]
- 20.Clement P.A.R., Gordts F. Consensus report on acoustic rhinometry and rhinomanometry. Rhinology. 2005;43:169–179. [PubMed] [Google Scholar]
- 21.Corey J.P. Acoustic rhinometry: should we be using it? Curr Opin Otolaryngol Head Neck Surg. 2006;14:29–34. doi: 10.1097/01.moo.0000193166.57129.80. [DOI] [PubMed] [Google Scholar]
- 22.Clement P.A., Halewyck S., Gordts F., Michel O. Critical evaluation of different objective techniques of nasal airway assessment: a clinical review. Eur Arch Otorhinolaryngol. 2014 doi: 10.1007/s00405-013-2870-9. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 23.Zancanella E., Anselmo-Lima W.T. Uso da rinometria acústica como método diagnóstico. Braz J Otorhinolaryngol. 2004;70:500–503. [Google Scholar]
- 24.Millqvist E., Bende M. Two-year follow-up with acoustic rhinometry in children. Am J Rhinol. 2006;20:203–205. [PubMed] [Google Scholar]
- 25.Qian W., Chen W., Chen J.M., Haight J. Acoustic rhinometry in preschool children. Otolaryngol Head Neck Surg. 2007;137:39–42. doi: 10.1016/j.otohns.2007.02.007. [DOI] [PubMed] [Google Scholar]
- 26.Samolinski B.K., Grzanka A., Gotlib T. Changes in nasal cavity dimensions in children and adults by gender and age. Laryngoscope. 2007;117:1429–1433. doi: 10.1097/MLG.0b013e318064e837. [DOI] [PubMed] [Google Scholar]
- 27.Gomes A.O.C., Sampaio-Teixeira A.C., Trindade S.H., Trindade I.E. Nasal cavity geometry of healthy adults assessed using acoustic rhinometry. Braz J Otorhinolaryngol. 2008;74:746–754. doi: 10.1016/S1808-8694(15)31386-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Mamikoglu B., Houser S.M., Akbar I.N.G.B., Corey J.P. Acoustic rhinometry and computed tomography scans for the diagnosis of nasal septal deviation, with clinical correlation. Otolaryngol Head Neck Surg. 2000;123:61–68. doi: 10.1067/mhn.2000.105255. [DOI] [PubMed] [Google Scholar]
- 29.Mamikoglu B., Houser S.M., Corey J.P. An interpretation method for objective assessment of nasal congestion with acoustic rhinometry. Laryngoscope. 2002;112:926–929. doi: 10.1097/00005537-200205000-00027. [DOI] [PubMed] [Google Scholar]
- 30.Carlini D., Ouriques D.M., Weckx L.L.M., Fujitaet R.R. Modified method of acoustic rhinometry. Acta Otolaryngol. 2002;122:298–301. doi: 10.1080/000164802753648196. [DOI] [PubMed] [Google Scholar]
- 31.Nigro C.E.N., Goto E., Nigro J.F.A., Junior J.M., Mion O., Voegels R.L. Acoustic rhinometry evaluation of nasal cavity and nasopharynx before and after adenoidectomy. Braz J Otorhinolaryngol. 2003;69:333–336. [Google Scholar]
- 32.Marques V.C., Anselmo-Lima W.T. Pre and postoperative evaluation by acoustic rhinometry of children submitted to adenoidectomy or adenotonsillectomy. Int J Pediatr Otorhinolaryngol. 2004;68:311–316. doi: 10.1016/j.ijporl.2003.10.017. [DOI] [PubMed] [Google Scholar]
- 33.Can I.H., Ceylan K., Bayiz U., Olmez A., Samim E. Acoustic rhinometry in the objective evaluation of childhood septoplasties. Int J Pediatr Otorhinolaryngol. 2005;69:445–448. doi: 10.1016/j.ijporl.2004.09.013. [DOI] [PubMed] [Google Scholar]
- 34.Trindade I.E.K., Castilho R.L., Sampaio-Texeira A.C.M., Suedam-Trindade I.K., Silva Filho O.G. Effects of orthopedic rapid maxillary expansion on internal nasal dimensions in children with cleft lip and palate assessed by acoustic rhinometry. J Craniofac Surg. 2010;21:306–311. doi: 10.1097/SCS.0b013e3181cf5f5f. [DOI] [PubMed] [Google Scholar]
- 35.Compadretti G.C., Tasca T., Alessandri-Bonetti Peri S., D́Addario A. Acoustic rhinometric measurements in children undergoing rapid maxillary expansion. Int J Pediatr Otorhinolaryngol. 2006;70:27–34. doi: 10.1016/j.ijporl.2005.05.004. [DOI] [PubMed] [Google Scholar]
- 36.Enoki C., Valera F.C., Lessa F.C., Elias A.M., Matsumoto M.A., Anselmo-Lima W.T. Effect of rapid maxillary expansion on the dimension of the nasal cavity and on nasal air resistance. Int J Pediatr Otorhinolaryngol. 2006;70:1225–1230. doi: 10.1016/j.ijporl.2005.12.019. [DOI] [PubMed] [Google Scholar]
- 37.Trindade I.E.K., Prado P.C., Trindade S.H.K., Dias N.H., Sampaio-Texeira A.C.M. Internal nasal measurements of adults with nasal obstruction. Braz J Otorhinolaryngol. 2013;79:1–7. doi: 10.5935/1808-8694.20130103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Grymer L.F. Clinical applications of acoustic rhinometry. Rhinol Suppl. 2000;16:35–43. [PubMed] [Google Scholar]
- 39.Gomes AOC . Tese, HRAC-USP; 2007. Dimensões internas nasais de crianças com fissuras de lábio e palato unilateral aferidas por rinometria acústica. Bauru. [Google Scholar]
- 40.Lal D., Corey J.P. Acoustic rhinometry and its uses in rhinology and diagnosis of nasal obstruction. Facial Plast Surg Clin North Am. 2004;12:397–405. doi: 10.1016/j.fsc.2004.04.002. [DOI] [PubMed] [Google Scholar]
- 41.Lemos C.M., Wilhelmsen N.S.W., Mion O.G., Júnior J.F.M. Alterações funcionais do sistema estomatognático em pacientes com rinite alérgica: estudo caso-controle. Braz J Otorhinolaryngol. 2009;75:268–274. doi: 10.1016/S1808-8694(15)30789-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Connell J.T. Rhinometry: measurement of nasal patency. Ann Allergy. 1982;49:179–185. [PubMed] [Google Scholar]
- 43.Grymer L.F., Hilberg O., Pedersen O.F. Prediction of nasal obstruction based on clinical examination and acoustic rhinometry. Rhinology. 1997;35:53–57. [PubMed] [Google Scholar]
- 44.Zavras G.E., White A., Rich I., Jackson A.C. Acoustic rhinometry n the evaluation of children with nasal or oral respiration. J Clin Pediatr Dent. 1994;18:203–210. [PubMed] [Google Scholar]
- 45.Fensterseifer G.S., Carpes O., Weckx L.L.M., Martha V.F. Mouth breathing in children with learning disorders. Braz J Otorhinolaryngol. 2013;79:620–624. doi: 10.5935/1808-8694.20130111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Mendes A.I., Wandalsen G.F., Solé D. Objective, subjective assessments of nasal obstruction in children and adolescents with allergic rhinitis. J Pediatr. 2012;88:389–395. doi: 10.2223/JPED.2213. [DOI] [PubMed] [Google Scholar]
- 47.Teik-Ying N.G., Chen Y.F., Tsai M.H., Huang K.H., Tai C.J. Objective measurements differ for perception of left and right nasal obstruction. Auris Nasus Larynx. 2012;40:81–84. doi: 10.1016/j.anl.2012.03.001. [DOI] [PubMed] [Google Scholar]
- 48.Wandalsen G.F., Mendes A.I., Solé D. Correlation between nasal resistance and different acoustic rhinometry parameters in children and adolescents with and without allergic rhinitis. Braz J Otorhinolaryngol. 2012;78:81–86. doi: 10.5935/1808-8694.20120038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Voegels R.L., Goto E.Y., Lessa M.M., Romano F.R., Neves M.C., Tavares R., et al. Avaliação Pré e Pós-operatória por Rinometria Acústica de Pacientes Submetidos à Cirurgia de Septo Nasal e Conchas Inferiores. Int Arch Otorhinolaryngol. 2002;6:172. [Google Scholar]
- 50.Paiva J.B., Freire-Maia A.V., Neto J.R., Di Francesco R.C., Voegels R.L. Evaluation of children nasal geometry, employing accoustic rhinometry. Braz J Otorhinolaryngol. 2010;76:355–362. doi: 10.1590/S1808-86942010000300014. [DOI] [PMC free article] [PubMed] [Google Scholar]