Abstract
Efforts to intervene with subgroups at particularly high risk for alcohol use require information on factors that differentiate drinking intensity levels. This paper summarizes existing research and provides new findings on sociodemographics and risk factors that differentiate high-intensity drinking (HID) to provide context for developing and delivering interventions for the highest-risk drinkers. Cross-sectional data were obtained in 2019 from participants who reported past 30-day alcohol use in 2018 as part of the nationally representative 12th grade Monitoring the Future (MTF) study. Among past 2-week drinkers in 2019 (N=601; modal age 19; 57.0% male; 67.4% non-Hispanic White), bivariate associations between drinking intensity (moderate drinking [1-4 drinks for women/1-5 drinks for men], binge-only drinking [4-7/5-9 drinks], and HID [8+/10+ drinks]) and a range of sociodemographic characteristics, risk factors, and alcohol-related consequences were examined. Results showed binge drinking norms, social and enhancement drinking motives, nicotine vaping, and use of limiting/stopping drinking and manner of drinking protective behavioral strategies differentiated all drinking intensity levels, lending support to HID and binge-only drinking having an overlapping risk profile. However, there were also risk factors uniquely associated with HID, including sex, college attendance, employment, HID norms, use of serious harm reduction protective behavioral strategies, family history of drinking problems, any cigarette or drug use other than marijuana, and depression symptoms. Therefore, risk factors differentiate young adult drinking intensity. These results can inform efforts to adapt interventions for young adults who report HID.
Keywords: high-intensity drinking, young adult, drinking motives, brief intervention, alcohol
Risk factors for high-intensity drinking and implications for intervention
Binge drinking (defined as 5+ drinks, or sex-specific 4+/5+ for women/men) is associated with acute and long-term risks and has been widely studied in the alcohol research field. However, binge drinking may reflect a relatively low intoxication level, such that an average-weight adult might have a blood alcohol concentration (BAC) of .08 or below (Pearson, Kirouac, & Witkiewitz, 2016). Furthermore, the average number of drinks during a young adult binge episode is 9.5 (Naimi, Nelson, & Brewer, 2010), or about twice the binge threshold. Therefore, a significant degree of existing heterogeneity is ignored when using only the binge threshold to demarcate risky drinking. A higher threshold is needed to identify individuals at greatest risk for negative alcohol use consequences (Patrick, 2016; Patrick & Azar, 2017; Patrick et al., 2013; Patrick, Terry-McElrath, Kloska, & Schulenberg, 2016), particularly for the purpose of tailoring interventions. While the field needs to find consensus on how many drinks define a higher threshold of concern, the starting point has been at least twice the quantity of alcohol in a binge episode. High-intensity drinking (National Institute on Alcohol Abuse and Alcoholism, 2018; also sometimes called “extreme binge drinking” [Patrick et al., 2013]) has been operationalized as 10+ drinks, or a sex-specific 8+/10+ for women/men (Patrick, 2016).
Research examining associations between high-intensity drinking (HID) and negative outcomes has highlighted intervention needs. Individuals who report HID also report drinking at binge levels below the HID threshold more frequently than those who do not engage in HID (Patrick, Terry-McElrath et al., 2016). Compared with drinking at binge levels below the HID threshold, HID is associated with a higher likelihood of alcohol use disorder (AUD) symptoms both cross-sectionally (Hingson, Zha, & White, 2017; Linden-Carmichael, Vasilenko, Lanza, & Maggs, 2017) and longitudinally (Patrick, Evans-Polce, Parks, & Terry-McElrath, in press). Cross-sectional research has also identified associations between HID and negative outcomes such as fights, injuries, and arrest (Hingson et al., 2017) and mental distress (Wang, 2020). Within-person research has found that on days when individuals report HID, they also are more likely to report both positive (Patrick, Cronce, Fairlie, Atkins, & Lee, 2016) and negative consequences (Linden-Carmichael, Calhoun, Patrick, & Maggs, 2018; Patrick, Cronce, et al., 2016; Patrick & Terry-McElrath, in press), including blackouts (Merrill, Boyle, Jackson, & Carey, 2019). Longitudinally, HID poses greater risk than binge drinking for traffic tickets/collisions (Evans-Polce, Patrick, O’Malley, 2017), poorer performance on some measures of learning and recall (Nguyen-Louie et al., 2016), and AUD symptoms (Patrick et al., in press).
Despite being at highest risk for binge drinking, young adults are unlikely to self-identify as having a problem with alcohol consumption (Monti, Trevyaw, & Borsari, 2004/2005). Thus, brief interventions that can proactively screen individuals in a wide range of locations have been recommended for addressing young adults’ risky drinking (Monti et al., 2004/2005; Samson & McHugh, 2019) in an effort to disrupt trajectories toward development of AUD. Efforts to intervene with subgroups at particularly high risk for HID should be informed by whether HID and binge drinking have the same general risk factors, or whether there are particular risks for HID that are different than the factors that predict binge drinking.
Identification of sociodemographic characteristics and other risk factors associated with HID will be key to designing effective programs and resources. One example of research yielding potential clues to guide intervention followed adolescents in a clinical treatment setting into young adulthood: Creswell and colleagues (2020) found that decreases in coping motives for drinking were associated with a lower likelihood of later HID, whereas continued high social and enhancement motives were associated with increased likelihood. Other examples may be found in looking at risk factors for AUD. AUD is highly comorbid with depression and anxiety (Grant et al., 2015; Helle, Trull, Watts, McDowell, & Sher, 2020; Kuntsche, Knibbe, Gmel, & Engels, 2005) and family history of alcohol problems is a significant risk factor for later alcohol problems (Knopik et al., 2004; Lieb, Merikangas, Höfler, Pfister, Isensee, & Wittchen, 2002), yet whether these constructs are also uniquely associated with HID has not yet been examined. In addition, social norms and protective behavioral strategies are often targeted in brief interventions as mediators that should decrease young adult alcohol consumption and consequences (e.g., Borsari & Carey, 2000; Carey, Henson, Carey, & Maisto, 2010; Larimer et al., 2007; Neighbors, Larimer, & Lewis, 2004; Neighbors, Lee, Lewis, Fossos, & Larimer, 2007). Again, associations between these constructs and HID are not well-characterized, so it is unclear whether these same mediators should also be targeted to decrease HID.
Most early research on drinking beyond a binge involved college students and high-risk events (e.g., Read, Beattie, Chamberlain, & Merrill, 2008; White, Anderson, Ray, & Mun, 2016; White, Kraus, & Swartzwelder, 2006), with little information available for other subgroups. Additional HID research among a wide range of populations and contexts is needed to inform effective interventions. Data on HID is now available through several national studies. One of the key studies used to investigate drinking beyond binge levels is the national Monitoring the Future (MTF) study, which has provided rich data on HID in the U.S. from mid-adolescence into adulthood via cross-sectional and longitudinal analyses. This paper aims to summarize existing HID research from MTF, as well as provide new findings on HID risk factors in a new follow-up MTF sample. Given the broad national representation of young people in MTF, reviewing these epidemiological findings provides context for further research.
High-intensity Drinking Research Based on Monitoring the Future Data
Sociodemographic characteristics
Age
HID prevalence peaks during early young adulthood (Schulenberg et al., 2020), with a slightly earlier peak for men (ages 21/22) than women (ages 25/26) (Patrick & Terry-McElrath, 2019). However, HID is not limited to older adolescence and adulthood. Approximately 1% of 8th and 3% of 10th grade students report past-year HID (Miech et al., 2019; Patrick, Terry-McElrath, Miech, O’Malley et al., 2017; Patrick & Terry-McElrath, 2019). More than 1 in 7 (16%) high school students evidence a long-term pattern of high-intensity drinking lasting into their mid-20s (Patrick, Terry-McElrath, Schulenberg, & Bray, 2017).
Age-related patterns in alcohol use include an increase in drinking during the transition out of high school; this increase is steeper for binge drinking than HID (Patrick & Terry-McElrath, 2019). In regards to age-related associations with HID frequency, individuals with lower HID frequency at the end of adolescence have been found to increase more quickly though ages 21/22; those reporting the strongest rates of increase from ages 18-21/22 were also those who reported the strongest rates of decrease from ages 21/22-25/26 (Patrick, Terry-McElrath et al., 2016). Different age groups have different historical trends in HID. Between 2005 and 2015, HID generally decreased for individuals in their early 20s, remained somewhat stable for individuals in their mid-20s, and increased for individuals at the end of young adulthood (ages 29/30) (Patrick, Terry-McElrath, Miech, Schulenberg, et al., 2017).
The age of consuming the first-ever drink and the speed at which individuals escalate from their first drink to first being intoxicated also are associated with HID. Among 12th grade students, faster escalation from first drink to first intoxication was associated with HID, such that HID was reported by 17.4% of those with same-grade escalation from first drink to intoxication, 15.8% of those with a 1-grade delay, and 12.6% of those with a 2+ grade delay (Patrick, Evans-Polce, & Terry-McElrath, 2019). The likelihood of reporting HID during the early- to mid-20s was higher among those who initiated alcohol use prior to high school, and decreased sharply among those who reported no alcohol use through 12th grade (Patrick & Terry-McElrath, 2017; Terry-McElrath & Patrick, 2016).
Sex
From early adolescence through young adulthood, men consistently report higher HID prevalence than women (Mehus & Patrick, 2020; Patrick & Terry-McElrath, 2019; Patrick, Terry-McElrath, Miech, O’Malley et al., 2017; Terry-McElrath & Patrick, 2016). About 1/4 to 1/3 of binge-drinking women engage in high-intensity drinking; closer to half of binge-drinking men do so (Patrick, Terry-McElrath, Miech, Schulenberg, et al., 2017). Men are more likely than women to engage in longer-term HID (Patrick, Terry-McElrath, Schulenberg, et al., 2017) and to have stronger increases in HID frequency across the transition into young adulthood (Patrick, Terry-McElrath et al., 2016). HID prevalence trends by age generally have been similar for men and women (Patrick, Terry-McElrath, Miech, Schulenberg, et al., 2017).
Race/ethnicity
During 8th and 10th grades, no HID prevalence differences have been observed by race/ethnicity (Patrick, Terry-McElrath, Miech, O’Malley, et al., 2017). By 12th grade, HID prevalence was highest for individuals who self-identified as White + Native Peoples (17%), followed by Native Peoples (13%) and White (12%) separately (Terry-McElrath & Patrick, 2020). In contrast, binge drinking prevalence was higher among students identifying as White than all other racial/ethnic groups (Terry-McElrath & Patrick, 2020). The lowest binge and HID prevalence levels were reported by students identifying as Asian American and African American (Terry-McElrath & Patrick, 2020). In both early- and mid-young adulthood, HID prevalence has been highest among respondents who identify as White (Patrick & Terry-McElrath, 2017; Terry-McElrath & Patrick, 2016), and self-identification as White is associated with longer-term HID participation (Patrick, Terry-McElrath, Schulenberg, et al., 2017).
Education and college attendance
We have investigated HID associations with parental education (a proxy for family-of-origin socioeconomic status) and participants’ own education. Having college-educated parents has been associated with a lower likelihood of extreme HID (15+ drinks per occasion) among 12th grade students (Patrick et al., 2013), but has not shown associations with prevalence or stability of drinking at the 10+ HID threshold (Mehus & Patrick, 2020; Patrick, Terry-McElrath, Miech, O’Malley et al., 2017; Patrick, Terry-McElrath, Schulenberg, et al., 2017; Patrick & Terry-McElrath, 2017; Terry-McElrath & Patrick, 2016).
College attendance is a key predictor of alcohol use. For example, young adults who attend college full-time engage in more frequent binge drinking than non-attenders (Schulenberg et al, 2020). There are signs of similar associations between HID and college attendance. Full-time 4-year college students were more likely to report HID than 2-year college students or non-attenders at age 19/20, and there was a particularly high risk for 4-year students who did not live with their parents (Patrick & Terry-McElrath, 2017). There was also a higher prevalence of HID among individuals in their mid-20s who had graduated from a 4-year college, compared to non-graduates (Terry-McElrath & Patrick, 2016). Looking at trajectories of change over time, HID frequency increased from ages 18 to 21/22 only among those attending a 4-year college full-time, but there was no change among other young adults (Patrick, Terry-McElrath, et al., 2016).
Relationship, parental, and employment status
At ages 25/26, HID prevalence was lower among those who were married (vs. not) or had children (vs. not), and higher among those who had paid work (vs. no paid work; Terry-McElrath & Patrick, 2016).
Risk factors
Drinking reasons and motives
HID was particularly likely among older adolescents who reported drinking for coping, compulsive use, and drug effect reasons; alcohol appears to serve more functions for those who report HID (Terry-McElrath, Stern, & Patrick, 2017). HID associations with drinking to get away from problems, to get high, to relax, and to sleep were stable across ages 18–26; association strength decreased for anger/frustration and to have a good time, and increased for boredom (Patrick, Evans-Polce, Kloska, Maggs, & Lanza, 2017). Each of the reasons noted above was more strongly associated with HID than binge drinking; however, drinking to have a good time and to relax did not distinguish HID from binge drinking (Patrick, Evans-Polce, et al., 2017).
Other substance use
During 8th and 10th grades, HID prevalence was higher among students who reported cigarette or marijuana use than among those who reported never using the substance (Patrick, Terry-McElrath, Miech, O’Malley, et al., 2017). In 12th grade, HID (vs. binge drinking) was associated with higher risk for simultaneous alcohol and marijuana use (Patrick, Veliz, & Terry-McElrath, 2017) and simultaneous alcohol and prescription drug use (McCabe, Veliz, & Patrick, 2017). Cigarette, marijuana, and other illicit drug use continued to be associated with higher HID prevalence at ages 25/26 (Terry-McElrath & Patrick, 2016).
The Current Study
The current study extends research using MTF by including information on normative perceptions of binge drinking and HID, multi-item empirically validated motives and protective behavioral strategy measures, family history, and mental health symptoms, and comparing three levels of alcohol intensity to each other: (1) less than binge; (2) binge, but not HID; and (3) HID. These three levels have been examined in a few papers, namely among 10th grade students (Mehus & Patrick, 2020) and among 12th graders with respect to other substance use (McCabe et al., 2017; Patrick, Veliz et al., 2017). A gap remains in existing research related to how risk factors, which could be important intervention targets, may differentiate alcohol use intensity levels among the high-risk young adult population. The current study focuses on how such measures differentiate HID from other alcohol use levels in young adulthood among a subsample of MTF respondents who reported current drinking as 12th grade students (modal age 18) and in the current study (at modal age 19). Specifically, we examine cross-sectional associations between drinking intensity and (1) sociodemographic characteristics (age, sex, race/ethnicity, college attendance) and social roles (relationship, parenting, employment statuses); (2) risk factors (perceived norms, drinking motives, protective behavioral strategies, family history, mental health symptoms, other substance use); and (3) alcohol-related consequences. Particularly for informing intervention, we focus on whether observed associations appear to indicate HID has a risk profile unique from binge-only drinking, or if HID and binge-only drinking share overlapping risk factors.
Method
The Young Adult Daily Life (YADL) Study is a longitudinal follow-up of a subsample of MTF participants who reported past 30-day alcohol use in 12th grade (Patrick & Terry-McElrath, in press). YADL is designed to examine predictors and consequences of binge and HID (Patrick & Terry-McElrath, in press). Although YADL is ongoing, the current study presents information from participants’ initial YADL survey, completed in 2019, one year after the 12th grade MTF survey.
Detailed information on MTF is available elsewhere (Miech et al., 2019). YADL participants were drawn from the 14,502 US nationally-representative 12th grade students who participated in the Spring 2018 MTF study; eligible participants had to report past 12th grade 30-day alcohol use. Past 30-day drinking was reported by 4,240 (29.2%) respondents; of these, 828 were excluded because they were randomly selected for MTF longitudinal study participation (Schulenberg et al., 2020) and 1,208 were excluded for not providing follow-up contact information, leaving 2,204 individuals eligible for the YADL study sample. Of the 2,204, 16 respondents (0.7%) refused participation; 911 (41.3%) provided written informed consent and completed the initial YADL online survey at modal age 19 in Spring 2019 (a $40 incentive was offered for completing the initial survey). Of the 911, 10 (1.1%) did not provide past 2-week drinking data, and 300 (32.9%) reported no past 2-week drinking, leaving 601 cases for analysis. Respondents were 57.0% male; 19.9% identified as Hispanic, 67.4% non-Hispanic White, and 12.7% other. Participants reported the following social roles: 40.6% were in a serious relationship, 62.7% attended college full-time, 25.1% worked full-time, and 51.3% worked part-time.
Measures
Drinking intensity.
In Spring 2019, respondents were asked, “During the last two weeks, what was the largest number of drinks that you had in a row? (Give your best estimate)” with response options from 0 to 20 or more. Drinking intensity was coded using sex-specific thresholds: no drinking (0 drinks), moderate drinking (1-4/1-5 drinks for women/men), binge but not HID (4-7/5-9 drinks for women/men; hereafter referred to as binge-only drinking), and HID (8+/10+ drinks for women/men; Patrick, 2016).
Sociodemographic characteristics.
Sex was reported as male or female. Race/ethnicity was coded as Hispanic, non-Hispanic White, or other (collapsed due to limited variation in the YADL sample of only respondents reporting 12th grade alcohol use). College attendance was coded as not attending, attending a 2-year/community college/trade or vocational school (referred to as 2-year/vo-tech), or attending a 4-year college/graduate/professional school. Relationship status was coded as serious (dating seriously/engaged/married/committed partner) or other; at modal age 19, few reported engaged/married/committed partner. Parental status was coded as having any or no children; employment status was coded as none, part-, or full-time.
Risk factors.
Perceived norms for binge drinking and HID were measured by asking, “How many times do you think the typical person your age has had [5 or more/10 or more] drinks in a row over the last two weeks?” with response options ranging from 0 occasions to 40 or more occasions. Drinking motives were measured using the Drinking Motives Questionnaire-R (Cooper, 1994; Grant, Stewart, O’Connor, Blackwell, & Conrod, 2007): social motives (5 items, α = 0.88; e.g., because it makes social gathering more fun), coping motives (5 items, α = 0.84; e.g., to forget your worries), enhancement motives (5 items, α = 0.86; e.g., because you like the feeling), and conformity motives (5 items α = 0.80; e.g., so you won’t feel left out). Response options ranged from 1=almost never or never to 5=almost always or always; the mean of relevant items was used for each scale. Protective behavioral strategies (Treloar, Martens, & McCarthy, 2015) were measured by asking, “Please indicate the degree to which you engage in the following behaviors when using alcohol or partying” followed by 20 items coded into three scales (each ranging 1-6): serious harm reduction (8 items [e.g., designated driver, taxi, or ride-sharing app], α = 0.75), limiting/stopping drinking (7 items [e.g., alternate alcoholic and nonalcoholic drinks], α = 0.81), and manner of drinking (5 items [e.g., avoid drinking games], α = 0.78). Family history of drinking problems was an any/none indicator of 1st degree biological relatives (parents/siblings) with significant drinking problems (Andersson, Johnsson, Berglund, & Öjehagen, 2007).
Past 2-week depression symptoms were measured using a continuous sum (range of 0-27; α = 0.91) from the Patient Health Questionnaire PHQ-9 (Kroenke, Spitzer, & Williams, 2001; Spitzer, Kroenke, & Williams, 1999). Scores of 5, 10, 15, and 20 indicate mild, moderate, moderately severe, and severe depression symptoms, respectively. Past 2-week anxiety symptoms were measured using a continuous sum (range of 0-21; α = 0.92) on the General Anxiety Disorder GAD-7 (Spitzer, Kroenke, Williams, & Löwe, 2006). Values of 0-4, 5-9, 10-14, and 15-21 indicate minimal, mild, moderate, and severe anxiety symptoms, respectively.
Substance use included past 30-day cigarette use (prevalence: any/none; quantity: 1=not at all, 2=<1/day, 3=1-5/day, 4=1/2 pack/day, 5=1 pack/day, 6=1½ packs/day, 7=2+ packs/day); past 30-day nicotine vaping (prevalence: any/none; frequency: 1=0 days, 2=1-2, 3=3-5, 4=6-9, 5=10-19, 6=20+ days); past 30-day marijuana use (prevalence: any/none; frequency: 1=0 occasions, 2=1-2, 3=3-5, 4=6-9, 5=10-19, 6=20-39, 7=40+ occasions); and past 12-month use of illicit drugs other than marijuana (not including prescription drug misuse), coded as any/none.
Consequences.
Respondents reported consequences experienced during or after alcohol use in the past month using the Brief Young Adult Consequences Questionnaire (Kahler, Hustad, & Barnett, 2008). A total of 24 consequences were listed; the number of total consequences endorsed were summed and treated as a continuous count measure.
Analysis
Analyses were conducted using SAS v.9.4. Frequencies and means were obtained using FREQ and MEANS procedures. Associations between sociodemographics and risk factors and drinking intensity were obtained from bivariate multinomial logistic regression models using the LOGISTIC procedure. First, moderate drinking was set as the referent class in order to obtain estimates comparing the likelihood of binge-only and HID versus moderate drinking. Second, binge-only drinking was set as the referent class to obtain estimates comparing the likelihood of HID versus binge-only drinking. Drinking intensity and consequence associations were estimated using negative binomial regression in the GENMOD procedure. All analyses were weighted to adjust for sampling and non-response (based on extensive information available from MTF 12th grade measures including sex, race/ethnicity, region, number of parents in the household, average parental education, religious commitment, average high school grades, truancy, college plans, and substance use).
Results
Risk factor associations with drinking intensity
In this sample of young adults who reported recent alcohol use at both ages 18 and 19, age 19 prevalence of past 2-week drinking was: 45.3% [SE 2.46] moderate drinking, 37.8% [2.31] binge-only drinking, and 16.9% [1.89] HID. Table 1 presents prevalence levels for categorical measures (e.g., the percentage of women reporting HID) and means for continuous measures by drinking intensity. Table 2 provides unadjusted odds ratios from multinomial logistic regression models.
Table 1.
Prevalence or mean differences in sociodemographics and risk factors by drinking intensity among US young adults reporting any past 2-week alcohol use, 2019
| Moderate | Binge-only | HID | ||||
|---|---|---|---|---|---|---|
| %/Mean | (95% CI) | %/Mean | (95% CI) | %/Mean | (95% CI) | |
|
|
||||||
| Sex (n=601) | ||||||
| Female | 43.0 | (37.7, 48.3) | 43.8 | (38.6, 49.1) | 13.2 | (9.4, 16.9) |
| Male | 47.1 | (39.7, 54.6) | 33.2 | (26.5, 40.0) | 19.6 | (13.8, 25.5) |
| Race/ethnicity (n=601) | ||||||
| Hispanic | 51.9 | (39.8, 63.9) | 37.0 | (25.7, 48.2) | 11.2 | (3.7, 18.7) |
| Non-Hispanic White | 40.9 | (35.2, 46.6) | 39.3 | (33.8, 44.8) | 19.9 | (15.1, 24.6) |
| Other | 58.8 | (46.9, 70.7) | 31.3 | (20.4, 42.3) | 9.9 | (2.4, 17.4) |
| College attendancea (n=601) | ||||||
| Not a student | 55.6 | (42.0, 69.1) | 27.8 | (15.9, 39.7) | 16.6 | (6.8, 26.4) |
| Attending 2-year/vo-tech | 51.2 | (39.0, 63.3) | 36.9 | (25.6, 48.1) | 12.0 | (4.8, 19.2) |
| Attending 4-year | 40.9 | (35.5, 46.3) | 40.8 | (35.5, 46.1) | 18.3 | (13.7, 22.9) |
| Relationship status (n=601) | ||||||
| Seriousb relationship | 52.8 | (45.2, 60.5) | 35.8 | (28.7, 43.0) | 11.4 | (6.5, 16.2) |
| Other | 40.2 | (34.1, 46.3) | 39.2 | (33.3, 45.0) | 20.6 | (15.4, 25.8) |
| Employment status (n=601) | ||||||
| None | 46.5 | (37.0, 56.0) | 35.0 | (26.0, 44.0) | 18.5 | (11.0, 26.0) |
| Part-time | 43.9 | (37.5, 50.2) | 42.6 | (36.5, 48.7) | 13.5 | (9.3, 17.7) |
| Full-time | 47.2 | (36.1, 58.4) | 30.7 | (21.0, 40.3) | 22.1 | (12.6, 31.7) |
| Perceived past 2-week drinking norms (n=599-600) | ||||||
| Binge drinking norm | 1.7 | (1.5, 1.9) | 1.9 | (1.8, 2.1) | 2.2 | (1.8, 2.6) |
| HID norm | 1.1 | (1.0, 1.3) | 1.2 | (1.0, 1.3) | 1.7 | (1.3, 2.2) |
| Drinking motives (n=592) | ||||||
| Social motives | 2.7 | (2.5, 2.8) | 3.2 | (3.1, 3.4) | 3.6 | (3.4, 3.8) |
| Coping motives | 1.8 | (1.6, 1.9) | 2.0 | (1.9, 2.2) | 2.1 | (1.8, 2.3) |
| Enhancement motives | 2.4 | (2.3, 2.6) | 2.8 | (2.7, 3.0) | 3.2 | (2.9, 3.4) |
| Conformity motives | 1.3 | (1.2, 1.4) | 1.4 | (1.3, 1.5) | 1.4 | (1.2, 1.5) |
| Protective behavioral strategies (n=585-587) | ||||||
| Serious harm reduction | 4.7 | (4.6, 4.9) | 4.8 | (4.6, 4.9) | 4.6 | (4.3, 4.8) |
| Limiting/stopping drinking | 3.3 | (3.1, 3.5) | 3.2 | (3.0, 3.3) | 2.7 | (2.5, 3.0) |
| Manner of drinking | 3.4 | (3.2, 3.6) | 3.0 | (2.9, 3.2) | 2.4 | (2.2, 2.6) |
| Family history of drinking problems (n=583) | ||||||
| No first degree relatives | 46.2 | (40.7, 51.8) | 39.5 | (34.2, 44.8) | 14.2 | (10.5, 18.0) |
| 1+ first degree relatives | 40.5 | (30.6, 50.4) | 32.6 | (23.8, 41.5) | 26.9 | (17.0, 36.7) |
| Mental health (n=574) | ||||||
| Depression symptomsc | 5.0 | (4.1, 5.8) | 5.6 | (4.7, 6.5) | 6.8 | (5.4, 8.2) |
| Anxiety symptomsd | 4.7 | (3.9, 5.5) | 4.8 | (4.0, 5.6) | 5.1 | (4.0, 6.3) |
| Past 30-day cigarette use (n=586) | ||||||
| None | 45.9 | (40.7, 51.1) | 38.0 | (33.1, 42.8) | 16.1 | (12.1, 20.2) |
| Any | 40.9 | (28.1, 53.6) | 36.4 | (24.0, 48.9) | 22.7 | (12.2, 33.2) |
| Quantity | 1.2 | (1.1, 1.3) | 1.3 | (1.1, 1.4) | 1.3 | (1.1, 1.4) |
| Past 30-day nicotine vaping (n=585) | ||||||
| None | 54.3 | (47.2, 61.3) | 32.2 | (25.9, 38.4) | 13.6 | (8.1, 19.1) |
| Any | 39.0 | (32.4, 45.5) | 41.2 | (34.9, 47.5) | 19.8 | (14.6, 25.0) |
| Frequency | 2.6 | (2.3, 3.0) | 3.1 | (2.8, 3.4) | 3.9 | (3.3, 4.4) |
| Past 30-day marijuana use (n=584) | ||||||
| None | 49.0 | (42.1, 55.9) | 36.1 | (29.6, 42.6) | 14.9 | (9.7, 20.1) |
| Any | 42.0 | (35.2, 48.8) | 38.8 | (32.5, 45.1) | 19.1 | (13.8, 24.5) |
| Frequency | 2.9 | (2.5, 3.3) | 3.0 | (2.7, 3.3) | 3.3 | (2.7, 3.8) |
| Past 12-month illicit drug usee (n=585) | ||||||
| None | 46.1 | (40.9, 51.3) | 38.4 | (33.5, 43.3) | 15.5 | (11.6, 19.4) |
| Any | 39.4 | (26.0, 52.9) | 34.6 | (22.9, 46.3) | 25.9 | (14.3, 37.6) |
Notes: Drinking intensity defined using the maximum number of drinks per occasion in the past 2 weeks: moderate = 1-3 drinks for women/1-4 drinks for men; binge-only = 4-7/5-9; high-intensity = 8+/10+.
College attendance categories (1) included not attending, (2) attending 2-year or community college, or trade or vocational school, (3) attending 4-year college or university, or graduate or professional school.
Serious relationship status includes dating seriously, engaged, married, committed partner.
Depression symptom scores from the Patient Health Questionnaire (PHQ-9).
Anxiety symptom scores measured using the General Anxiety Disorder (GAD-7).
Illicit drug use prevlance indicates any past 12-month use of illicit drugs other than marijuana.
Table 2.
Bivariate multinomial regression associations between sociodemographics and risk factors and drinking intensity among US young adults reporting any past 2-week alcohol use, 2019
| Binge-only (vs. Moderate) | HID (vs. Moderate) | HID (vs. Binge-only) | |||||||
|---|---|---|---|---|---|---|---|---|---|
| OR | (95% CI) | p | OR | (95% CI) | p | OR | (95% CI | p | |
|
|
|||||||||
| Sex | |||||||||
| Female | (ref) | (ref) | (ref) | ||||||
| Male | 0.69 | (0.55, 0.87) | 0.002 | 1.36 | (1.00, 1.85) | 0.050 | 1.96 | (1.44, 2.68) | <0.001 |
| Race/ethnicity | |||||||||
| Hispanic | 0.74 | (0.56, 0.99) | 0.039 | 0.44 | (0.29, 0.67) | <0.001 | 0.60 | (0.39, 0.92) | 0.019 |
| Non-Hispanic White | (ref) | (ref) | (ref) | ||||||
| Other | 0.55 | (0.39, 0.78) | 0.001 | 0.35 | (0.21, 0.58) | <0.001 | 0.63 | (0.36, 1.08) | 0.095 |
| College attendancea | |||||||||
| Not a student | (ref) | (ref) | (ref) | ||||||
| Attending 2-year/vo-tech | 1.44 | 0.98, 2.12 | 0.064 | 0.78 | 0.47, 1.31 | 0.350 | 0.54 | 0.31, 0.94 | 0.030 |
| Attending 4-year | 2.00 | 1.45, 2.74 | <0.001 | 1.49 | 1.02, 2.19 | 0.041 | 0.75 | 0.49, 1.14 | 0.175 |
| Relationship status | |||||||||
| Serious relationshipb | 0.70 | (0.55, 0.88) | 0.002 | 0.42 | (0.31, 0.58) | <0.001 | 0.60 | (0.43, 0.84) | 0.002 |
| Other | (ref) | (ref) | (ref) | ||||||
| Employment status | |||||||||
| None | 1.16 | (0.83, 1.62) | 0.386 | 0.85 | (0.57, 1.26) | 0.412 | 0.73 | (0.48, 1.11) | 0.142 |
| Part-time | 1.49 | (1.13, 1.98) | 0.005 | 0.66 | (0.47, 0.93) | 0.018 | 0.44 | (0.31, 0.63) | <0.001 |
| Full-time | (ref) | (ref) | (ref) | ||||||
| Perceived drinking norms | |||||||||
| Binge drinking norm | 1.16 | (1.06, 1.27) | 0.002 | 1.35 | (1.21, 1.51) | <0.001 | 1.17 | (1.05, 1.30) | 0.006 |
| HID norm | 1.04 | (0.94, 1.14) | 0.441 | 1.38 | (1.24, 1.53) | <0.001 | 1.33 | (1.19, 1.48) | <0.001 |
| Drinking motives | |||||||||
| Social | 1.69 | (1.50, 1.89) | <0.001 | 2.43 | (2.07, 2.86) | <0.001 | 1.44 | (1.23, 1.69) | <0.001 |
| Coping | 1.43 | (1.25, 1.63) | <0.001 | 1.45 | (1.23, 1.71) | <0.001 | 1.01 | (0.87, 1.19) | 0.857 |
| Enhancement | 1.51 | (1.35, 1.70) | <0.001 | 2.07 | (1.78, 2.41) | <0.001 | 1.37 | (1.18, 1.59) | <0.001 |
| Conformity | 1.40 | (1.15, 1.70 | 0.001 | 1.14 | (0.88, 1.48) | 0.314 | 0.82 | (0.64, 1.05) | 0.111 |
| Protective behavioral strategies | |||||||||
| Serious harm reduction | 1.01 | (0.89, 1.14) | 0.892 | 0.82 | (0.71, 0.95) | 0.009 | 0.82 | (0.70, 0.95) | 0.008 |
| Limiting/stopping drinking | 0.90 | (0.82, 0.99) | 0.036 | 0.64 | (0.56, 0.73) | <0.001 | 0.71 | (0.62, 0.81) | <0.001 |
| Manner of drinking | 0.78 | (0.71, 0.86) | <0.001 | 0.47 | (0.41, 0.54) | <0.001 | 0.60 | (0.52, 0.70) | <0.001 |
| Family history of drinking problems | |||||||||
| No first-degree relatives | (ref) | (ref) | (ref) | ||||||
| 1+ first-degree relatives | 0.94 | (0.71, 1.25) | 0.679 | 2.16 | (1.57, 2.96) | <0.001 | 2.29 | (1.64, 3.18) | <0.001 |
| Mental health | |||||||||
| Depression symptomsc | 1.02 | (1.00, 1.04) | 0.066 | 1.05 | (1.03, 1.08) | <0.001 | 1.03 | (1.01, 1.06) | 0.013 |
| Anxiety symptomsd | 1.00 | (0.98, 1.03) | 0.740 | 1.02 | (0.99, 1.05) | 0.283 | 1.01 | (0.98, 1.04) | 0.426 |
| Substance use Cigarette smoking (30-day) | |||||||||
| None | (ref) | (ref) | (ref) | ||||||
| Any | 1.08 | (0.79, 1.46) | 0.633 | 1.58 | (1.10, 2.27) | 0.013 | 1.47 | (1.02, 2.12) | 0.041 |
| Use quantity | 1.13 | (0.92, 1.39) | 0.243 | 1.17 | (0.91, 1.51) | 0.221 | 1.04 | (0.81, 1.33) | 0.780 |
| Nicotine vaping (30-day) | |||||||||
| None | (ref) | (ref) | (ref) | ||||||
| Any | 1.78 | (1.41, 2.26) | <0.001 | 2.03 | (1.49, 2.78) | <0.001 | 1.14 | (0.82, 1.58) | 0.433 |
| Use frequency | 1.13 | (1.06, 1.19) | <0.001 | 1.32 | (1.23, 1.42) | <0.001 | 1.17 | (1.09, 1.26) | <0.001 |
| Marijuana use (30-day) | |||||||||
| None | (ref) | (ref) | (ref) | ||||||
| Any | 1.25 | (0.99, 1.58) | 0.058 | 1.50 | (1.11, 2.03) | 0.009 | 1.20 | (0.87, 1.64) | 0.265 |
| Use frequency | 1.02 | (0.97, 1.08) | 0.457 | 1.08 | (1.01, 1.16) | 0.020 | 1.06 | (0.99, 1.14) | 0.091 |
| Illicit drug usee (12-month) | |||||||||
| None | (ref) | (ref) | (ref) | ||||||
| Any | 1.05 | (0.77, 1.44) | 0.753 | 1.95 | (1.37, 2.79) | <0.001 | 1.86 | (1.29, 2.68) | 0.001 |
Notes: n(unwtd)=574-601. Drinking intensity defined using the maximum number of drinks per occasion in the past 2 weeks: moderate = 1-3 drinks for women/1-4 drinks for men; binge-only = 4-7/5-9; high-intensity = 8+/10+. Bold font indicates associations significant at p<.05 or stronger.
College attendance categories (1) included not attending, (2) attending 2-year or community college, or trade or vocational school, (3) attending 4-year college or university, or graduate or professional school.
Serious relationship status includes dating seriously, engaged, married, committed partner.
Depression symptom scores from the Patient Health Questionnaire (PHQ-9).
Anxiety symptom scores measured using the General Anxiety Disorder (GAD-7).
Illicit drug use prevalence indicates any past 12-month use of illicit drugs other than marijuana.
Sociodemographic characteristics
Sex and race/ethnicity.
The likelihood of binge-only (vs. moderate) drinking was lower for men than women; in contrast, HID likelihood (vs. moderate and binge-only drinking) was higher for men than women. Binge-only (vs. moderate) drinking and HID (vs. moderate drinking) likelihoods were lower for Hispanic and other (vs. White) racial/ethnic identities; HID (vs. binge-only drinking) likelihood also was lower for Hispanic than White racial/ethnic identities. No difference in the likelihood of HID (vs. binge-only drinking) was observed between other and White racial/ethnic identities.
College attendance.
The likelihoods of binge-only (vs. moderate) drinking and HID (vs. moderate drinking) were higher for 4-year attenders than those not attending college. HID (vs. binge-only drinking) likelihood was lower for 2-year/vo-tech attenders than those not attending college.
Relationship and employment status.
Not being in a serious relationship was associated with higher likelihoods of binge-only (vs. moderate) drinking and HID (vs. moderate or binge-only drinking). No differences in drinking intensity likelihood were observed between full-time versus not employed young adults. Compared with full-time, part-time employment was associated with greater likelihood of binge-only (vs. moderate) drinking, but lower likelihood of HID (vs. moderate or binge-only).
Risk factors
Perceived drinking norms.
Higher binge drinking norms were associated with greater likelihoods of binge-only (vs. moderate) drinking and HID (vs. moderate or binge-only drinking). No significant differences by HID norms were observed for binge-only (vs. moderate) drinking, but higher HID norms were associated with greater likelihood of HID (vs. moderate or binge-only drinking).
Drinking motives.
Stronger social motives were associated with greater likelihoods of binge-only (vs. moderate) drinking and HID (vs. moderate or binge-only drinking) (see Figure 1). Stronger coping motives were associated with greater likelihoods of binge-only (vs. moderate) drinking and HID (vs. moderate drinking), but did not differentiate HID and binge-only drinking. Stronger enhancement motives were associated with greater likelihoods of binge-only (vs. moderate) drinking and HID (vs. moderate or binge-only drinking). Stronger conformity motives were associated with a greater likelihood of binge-only (vs. moderate) drinking, but not with HID (vs. moderate or binge-only drinking).
Figure 1. Drinking motives and drinking intensity among US young adults reporting any past 2-week alcohol use, 2019.
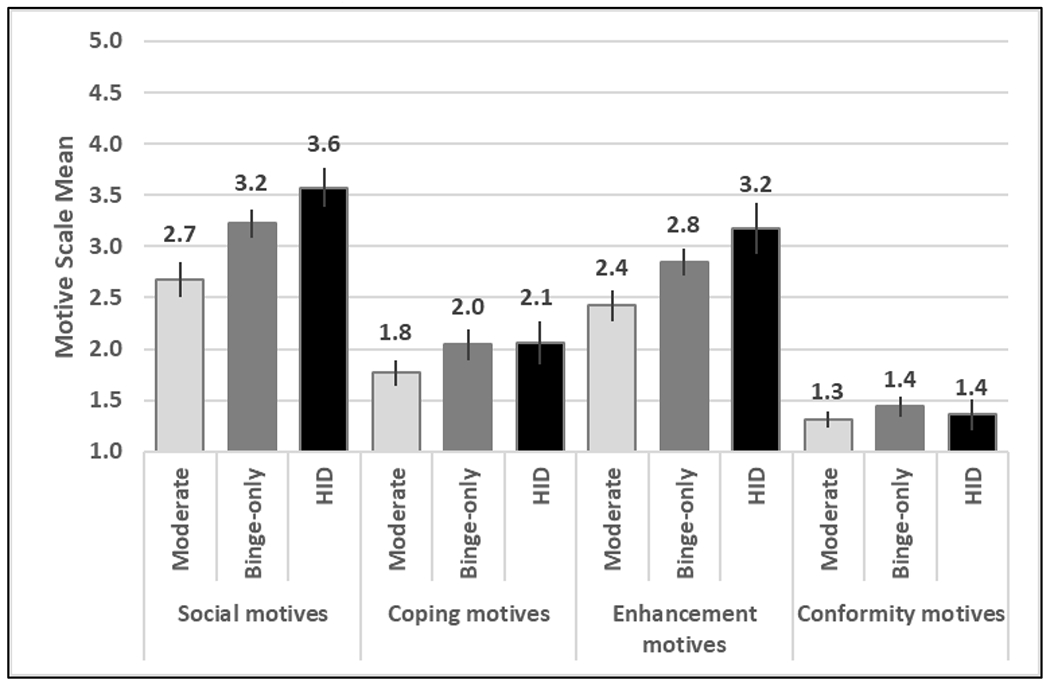
Notes: n(unwtd)=592. Drinking intensity coded using sex-specific thresholds of 1-3/1-4 drinks for women/men for moderate drinking, 4-7/5-9 for binge-only drinking; 8+/10+ for HID (high-intensity drinking).
Protective behavioral strategies.
More serious harm reduction strategies were not associated with binge-only (vs moderate) drinking, but were associated with lower odds of HID (vs. moderate or binge-only drinking) (see Figure 2). For both limiting/stopping drinking and manner of drinking, higher means were associated with lower likelihoods of binge-only (vs. moderate) drinking and HID (vs. moderate or binge-only drinking).
Figure 2. Protective behavioral strategies and drinking intensity among US young adults reporting any past 2-week alcohol use, 2019.
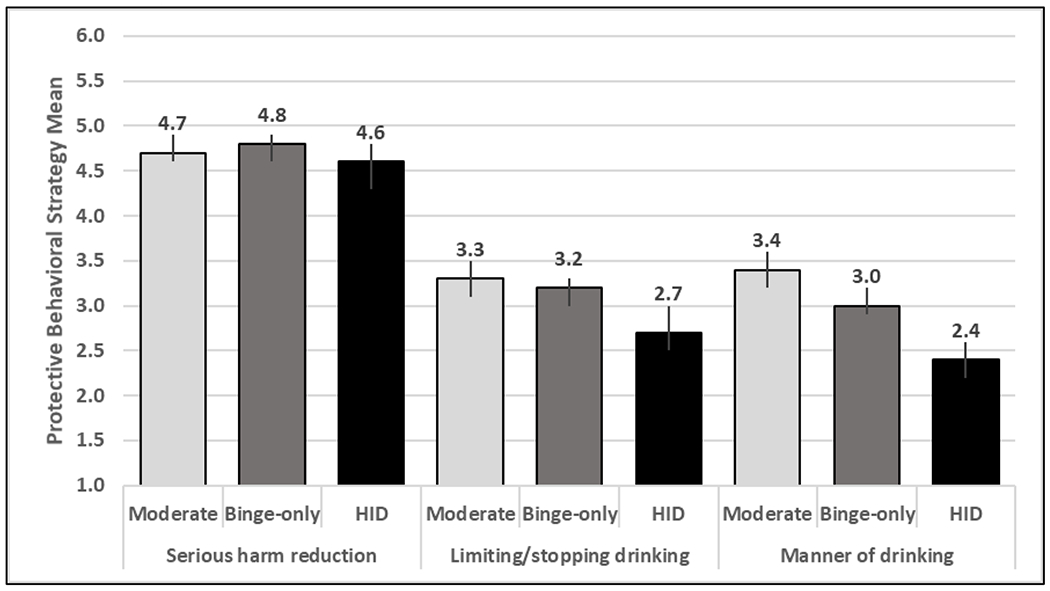
Notes: n(unwtd)=585-587. Drinking intensity coded using sex-specific thresholds of 1-3/1-4 drinks for women/men for moderate drinking, 4-7/5-9 for binge-only drinking; 8+/10+ for HID (high-intensity drinking).
Family history.
Reporting any first-degree biological relatives with drinking problems was not associated with binge-only (vs. moderate) drinking, but was associated with higher odds of HID (vs. moderate or binge-only drinking) (see Figure 3).
Figure 3. Family history of drinking problems and drinking intensity among US young adults reporting any past 2-week alcohol use, 2019.
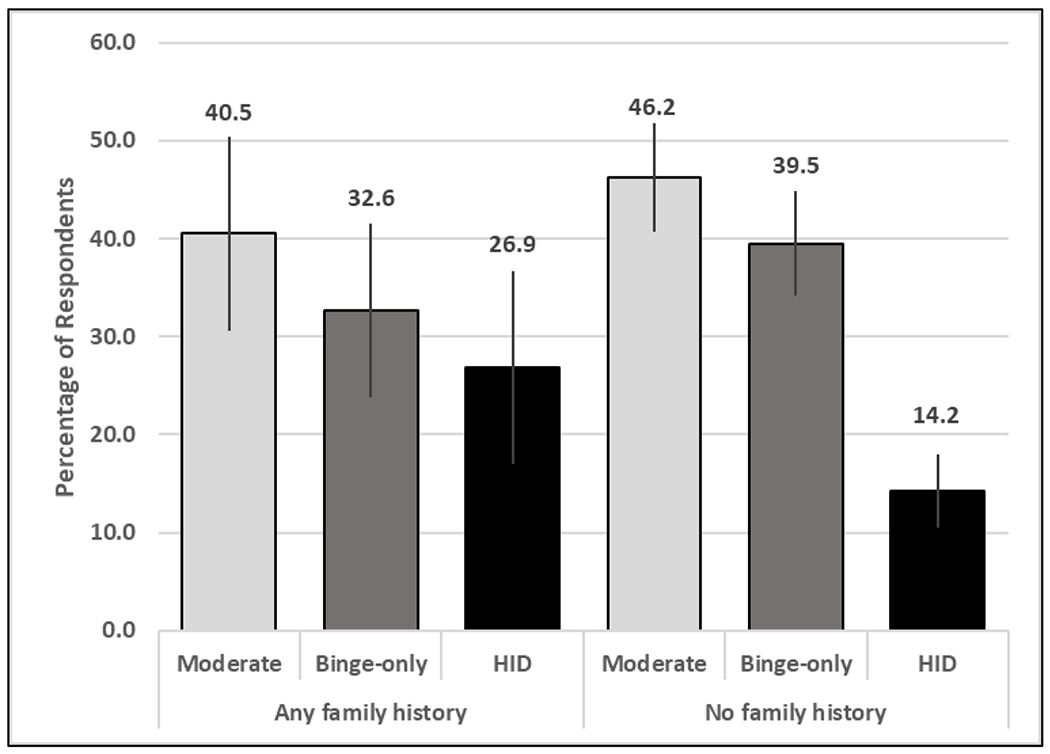
Notes: n(unwtd)=583. Drinking intensity coded using sex-specific thresholds of 1-3/1-4 drinks for women/men for moderate drinking, 4-7/5-9 for binge-only drinking; 8+/10+ for HID (high-intensity drinking).
Mental health.
Higher depression symptoms were not associated with the likelihood of binge-only (vs. moderate) drinking, but were associated with higher likelihoods of HID (vs. moderate or binge-only drinking) (see Figure 4). Anxiety symptoms were not associated with drinking intensity level.
Figure 4. Mental health and drinking intensity among US young adults reporting any past 2-week alcohol use, 2019.
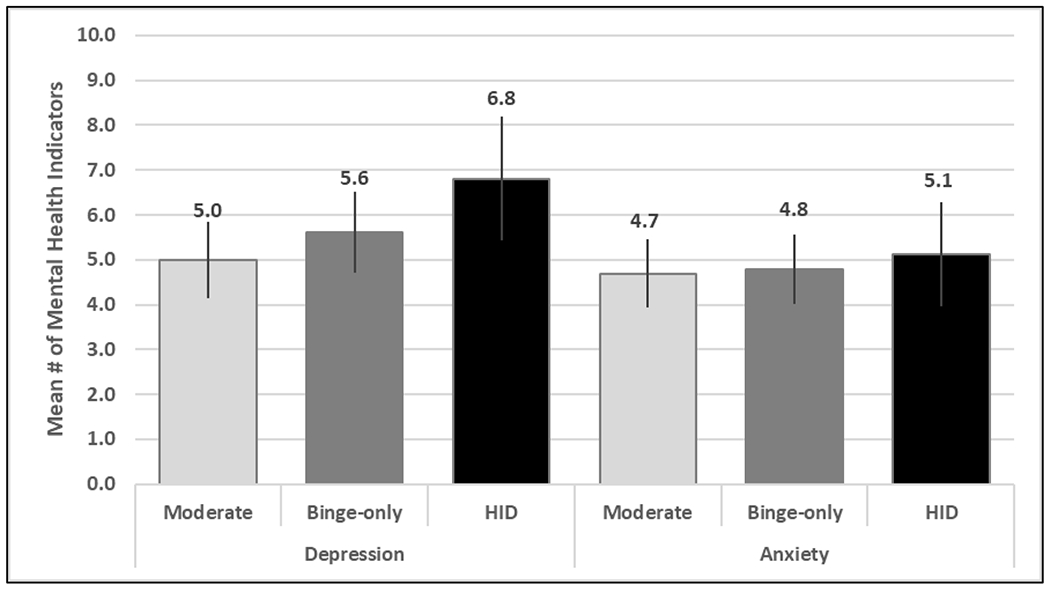
Notes: n(unwtd)=574. Drinking intensity coded using sex-specific thresholds of 1-3/1-4 drinks for women/men for moderate drinking, 4-7/5-9 for binge-only drinking; 8+/10+ for HID (high-intensity drinking).
Substance use.
Cigarette use was not associated with binge-only (vs. moderate) drinking, but cigarette use was associated with greater likelihoods of HID (vs. moderate or binge-only drinking). Mean cigarette quantity was not associated with drinking intensity.
Nicotine vaping was associated with greater likelihoods of binge-only (vs. moderate) drinking and HID (vs. moderate drinking), but did not differentiate HID from binge-only drinking. Higher vaping frequency was associated with greater likelihoods of binge-only (vs. moderate) drinking and HID (vs. moderate or binge-only drinking).
Neither marijuana prevalence nor frequency were associated with binge-only (vs. moderate) or HID (vs. binge-only drinking). However, marijuana prevalence and mean frequency were both associated with greater likelihood of HID (vs. moderate drinking).
Illicit drug use other than marijuana was not associated with binge-only (vs. moderate) drinking, but was associated with greater likelihoods of HID (vs. moderate or binge-only drinking).
Drinking intensity and consequences
The average number of past 30-day negative alcohol use consequences was 2.6 [95% CI 2.2, 3.1] for moderate drinking, 4.4 [3.9, 5.0] for binge-only drinking, and 6.4 [5.2, 7.6] for HID. Results from bivariate negative binomial regression models (not tabled) showed higher consequences were associated with binge-only versus moderate drinking (Est. 0.536 [SE 0.089], p<0.001); HID versus moderate drinking (Est. 0.915 [SE 0.110], p<0.001); and HID versus binge-only drinking (Est. 0.379 [0.108], p<0.001).
Discussion
The current study’s results study showed distinct risk factors among young adult drinkers based on drinking intensity (i.e., moderate, binge-only, or HID). This finding reflects a need to consider drinking intensity when developing and delivering brief alcohol interventions. Prevention research and interventions designed to reduce the negative outcomes of alcohol use among young people have largely focused on reducing binge drinking, a critical risk behavior associated with myriad negative consequences (Jennison, 2004; Kuntsche, Kuntsche, Thrul, & Gmel, 2017; Llerena, Arias-Loste, Puente, Cabezas, Crespo, & Fabrega, 2015; Piano, Mazzuco, Kang, & Phillips, 2017; Stephens & Duka, 2008). Research differentiating young adult moderate, binge-only, and HID drinking is sparse; however, the results of the current study, combined with prior work, underscore that young adults who engage in HID exhibit a more severe pattern of drinking and associated risks than those who binge drink only. Some covariate associations indicated HID has a risk profile unique from binge-only drinking, while other associations indicated a shared risk profile.
Rapid increases in HID prevalence from adolescence through the early- to mid-20s highlight the importance of prevention and intervention efforts targeting these populations (Patrick & Terry-McElrath, 2019). Despite associations between HID and alcohol use disorder (Linden-Carmichael, Lanza, Dziak, & Bray, 2017; Patrick et al., in press) and other consequences (Allen, Calhoun, & Maggs, 2020; Cox et al., 2019; Hingson et al., 2017; Patrick & Azar, 2017; White et al., 2016), fewer than 1% of young people seek or receive formal treatment for alcohol use (Substance Abuse and Mental Health Services Association, 2020). Thus, screening and brief intervention approaches may be beneficial, with more intensive interventions potentially indicated for those engaging HID given their greater severity and comorbidities and lack of treatment-seeking.
In the current study, compared to binge-only drinkers, young adults reporting HID were more likely to be male, identify as non-Hispanic White (vs. Hispanic), not be a student (vs. attend a 2-year/vo-tech school), not be in a serious relationship, work full-time (vs. part-time), have higher perceived drinking norms and social and enhancement drinking motives, report using fewer protective behavioral strategies, have a family history of drinking problems, smoke cigarettes, vape nicotine more frequently, use drugs other than marijuana, and have more depression symptoms. Some results reflected an increased likelihood with each level of drinking intensity: non-serious relationship status, Hispanic identity, higher binge drinking norms, stronger social and enhancement drinking motives, more frequent nicotine vaping, and lower use of limiting/stopping drinking and manner of drinking protective behavioral strategies. These findings lend support to HID and binge-only drinking having overlapping risk factors. In contrast, other results indicated some measures were associated with higher risk of HID, but did not differentiate binge-only from moderate drinking: no school attendance (vs. 2-year/vo-tech attendance), higher HID norms, lower use of serious harm reduction protective behavioral strategies, family history of drinking problems, any cigarette or illicit drug use other than marijuana, and depression symptoms. Still other covariates had different associations predicting binge-only drinking and HID, such that women were more likely to engage in binge-only than moderate drinking, while men were more likely to engage in HID than lower levels of drinking. Similarly, those working part-time (vs. full-time) were more likely to engage in binge-only than moderate drinking, but less likely to engage in HID than lower levels of drinking.
In sum, HID shared several risk factors with binge-only drinking, but unique risk factors also emerged. Particular risks associated with HID included family history of alcohol problems and symptoms of depression. These factors suggest that HID is more closely linked with potentially entrenched genetic risks and a more severe psychiatric profile, therefore underscoring the need for early interventions and addressing comorbid mental health issues to improve outcomes.
Attending a 4-year college did not differentiate binge-only and HID. College settings often are a well-justified location for brief interventions based on student binge drinking prevalence (Krieger, Young, Anthenien, & Neighbors, 2018). However, we found that 4-year college attendance (versus not attending college) was not associated with a greater prevalence of HID than binge-only. Non-attenders are at risk for HID. In fact, non-attenders have a higher risk of HID than 2-year college attenders. Additional research is needed to: (1) evaluate HID outcomes from currently available and supported college-based interventions; and (2) extend and adapt efficacious college interventions to reach young adults outside of the college setting, given that non-students are also at risk for HID and roughly half of young adults do not attend college (National Kids Count, 2020). In thinking beyond the college setting, we can also look to healthcare settings such as hospital emergency departments where young adults may be identified as heavy drinkers (Cunningham et al., 2015; Suffoletto et al., 2015). Other methods of identifying young adults at risk may involve social media to reach young adults in their daily lives (Bonar et al., 2020; Ramo et al., 2018).
The results from the current study suggest that brief interventions targeting HID likely need to incorporate content to address unique risk factors, including other substance use and depression, with potential referral options. These interventions should also consider genetic vulnerability such as family history of substance use problems to identify those in need of early interventions. Although negative affect regulation (i.e., coping motives) did not distinguish HID from binge-only drinking in this sample, motives related to increasing positive affect (i.e., social and enhancement motives) did. Interventions addressing depression symptoms in this group could be a logical next step to increasing positive affect in more adaptive ways than drinking, and promoting greater well-being and improved functional outcomes. Drinking motives may be another important intervention target given that motives distinguish HID drinking events. A study that pooled data across several trials found that among college students reporting HID, those who reduced their drinking over time reported reduced coping and enhancement motives (White et al., 2016). Constructs such as motivation and self-efficacy are important mechanisms in brief motivational alcohol interventions that can differentiate response (Davis et al., 2018; DiBello, Miller, & Carey, 2019; Walton et al., 2015), but little is known about how these mechanisms function in those reporting HID. HID is associated with more undesirable drinking consequences which could prompt greater motivation to change, in the face of perhaps lower self-efficacy to do so. Behavioral activation, a well-supported treatment for depression (Uphoff et al., 2020), with guidance toward events that are not drinking-centered (consistent with the substance-free activity session approach; Murphy et al., 2012, 2019) might reduce depression symptoms and increase positive affect. Given that the current study found HID was more likely among young adults reporting using drugs other than marijuana, and other studies have found similar associations between HID and nonmedical use of prescription drugs (McCabe et al., 2017), overdose risk reduction and provision of naloxone may be beneficial and lifesaving, although more data are needed to understand patterns of HID co-use with opioids, sedatives, and/or stimulants.
In addressing how, when, and with whom to intervene to address HID, several considerations point to the need to explore tailored and personalized approaches with critically relevant content and strategies. One example is using just-in-time adaptive intervention approaches given the episodic nature of drinking (Nahum-Shani, Heckler, & Spruijt-Metz, 2015). Data suggest event-specific drinking motives and protective behavioral strategies are associated with event-specific HID, as well as risk of specific negative outcomes. For example, on a given drinking day, reporting stronger enhancement and social drinking motives was associated with higher drinking intensity, and stronger enhancement and coping motives were associated with more negative consequences (Patrick & Terry-McElrath, in press). Further, Linden-Carmichael, Calhoun, Patrick, and Maggs (2019) found using manner of drinking strategies weakened associations between HID and passing out from drinking, and using serious harm reduction strategies weakened associations between HID and having no one sober enough to drive and experiencing regretted sexual behaviors. However, on days with HID, students were less likely to using manner of drinking strategies and were no more likely to use serious harm reduction strategies to protect themselves (Linden-Carmichael, Calhoun, Patrick, & Maggs, 2019). Interventions that center on drinking motives and use of relevant strategies closer to real time may help reduce HID and could also reinforce coping skills for depression given this particular comorbidity.
Limitations and future directions
The data examined in the current study were subject to limitations. The sample was based on high school students (alcohol use is higher among high school dropouts; Tice, Lipari, & Van Horn, 2017); due to sample size limitations, analyses were unable to examine HID for all race/ethnicity categories. Further, information was not available regarding over what time period drinking occurred. These limitations notwithstanding, the current study examined how risk factors differentiated drinking intensity level among early young adults in the U.S. The results, combined with existing research on young adult HID predictors and trends, can contribute to efforts to adapt interventions for young adults who show more extreme drinking levels. Adapting intervention approaches based on initial response is consistent with sequential, multiple assignment, randomized trial (i.e., SMART) designs that could be used to define and test decision rules within intervention trials in order to examine which interventions work equally well (or differently) at different drinking levels, including HID (e.g., Patrick et al., 2020).
Future research should investigate the extent to which interactions between risk factors (such as employment and college, or family history of alcohol problems and depression) may be differentially associated with binge and HID risk, including whether there are particular combinations of risk factors most associated with HID. Additional HID research is needed (Patrick, 2016), including HID risk factors and situations in which HID is most likely to occur, drinking intensity variation in outcome expectancies, and subjective evaluation of drinking consequences. Existing interventions should examine whether they effectively reduce HID. These findings should be used to develop, test, and refine interventions that will be most effective specifically for young adults who engage in HID and are most likely to experience negative alcohol-related consequences.
Public Health Significance Statements.
This study indicates that young adults who report high-intensity drinking have higher social and enhancement drinking motives than young adults who engage in drinking at binge levels below high-intensity drinking thresholds.
Young adults who report high-intensity drinking are more likely to have a family history of drinking problems and to report more depression symptoms than young adults who engage in drinking at binge or moderate intensity levels.
The results from the current study suggest that brief interventions targeting HID likely need to address unique risks, including other substance use, depression symptoms, fewer protective behavioral strategies, and negative alcohol consequences.
Acknowledgments
Data collection and manuscript preparation were supported research grants from the National Institute on Alcohol Abuse and Alcoholism (R01AA023504 to M. Patrick and R34AA027272 to E. Bonar) and the National Institute on Drug Abuse (R01DA001411 to R. Miech and R01DA016575 to J. Schulenberg). The study sponsors had no role in the study design, collection, analysis or interpretation of the data, writing of the manuscript, or the decision to submit the paper for publication. The content is solely the responsibility of the authors and does not necessarily represent the official views of the study sponsor.
References
- Allen HK, Calhoun BH, & Maggs JL (2020). High-risk alcohol use behavior and daily academic effort among college students. Journal of American College Health. doi: 10.1080/07448481.2020.1752697 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Andersson C, Johnsson KO, Berglund M, & Öjehagen A (2007). Alcohol involvement in Swedish university freshman related to gender, age, serious relationship and family history of alcohol problems. Alcohol and Alcoholism, 42, 448–455. 10.1093/alcalc/agm008 [DOI] [PubMed] [Google Scholar]
- Bonar EE, Schneeberger DM, Bourque C, Bauermeister JA, Young SD, Blow FC, …Walton MA (2020). Social media interventions for risky drinking among adolescents and emerging adults: protocol for a randomized controlled trial. JIMR Research Protocols, 9, e16688. doi: 10.2196/16688 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Borsari B, & Carey KB (2000). Effects of a brief motivational intervention with college student drinkers. Journal of Consulting and Clinical Psychology, 68, 728–733. doi: 10.1037/0022-006X.68.4.728 [DOI] [PubMed] [Google Scholar]
- Carey KB, Henson JM, Carey MP, & Maisto SA (2010). Perceived norms mediate effects of a brief motivational intervention for sanctioned college drinkers. Clinical Psychology: Science and Practice, 17, 58–71. doi: 10.1111/j.1468-2850.2009.01194.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cooper ML (1994). Motivations for alcohol use among adolescents: development and validation of a four-factor model. Psychological Assessment, 6, 117–128. doi: 10.1037/1040-3590.6.2.117 [DOI] [Google Scholar]
- Cox MJ, Egan KL, Suerken CK, Reboussin BA, Song EY, Wagoner KG, & Wolfson M (2019). Social and situational party characteristics associated with high-intensity alcohol use among youth and young adults. Alcoholism: Clinical and Experimental Research, 43, 1957–1966. doi: 10.1111/acer.14143 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Creswell KG, Chung T, Skrzynski CJ, Bachrach RL, Jackson KM, Clark DB, & Martin CS (2020). Drinking beyond the binge threshold in a clinical sample of adolescents. Addiction, 115, 1472–1481. doi: 10.1111/add.14979 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cunningham RM, Chermack ST, Ehrlich PF, Carter PM, Booth BM, Blow FC,… Walton MA (2015). Alcohol interventions among underage drinkers in the ED: a randomized controlled trial. Pediatrics, 136, e783–e793. doi: 10.1542/peds.2015-1260 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davis AK, Arterberry BJ, Bonar EE, Chermack ST, Blow FC, Cunningham RM, & Walton MA (2018). Predictors of positive drinking outcomes among youth receiving an alcohol brief intervention in the emergency department. Drug and Alcohol Dependence, 188, 102–108. doi: 10.1016/j.drugalcdep.2018.03.044 [DOI] [PMC free article] [PubMed] [Google Scholar]
- DiBello AM, Miller MB, & Carey KB (2019). Self-efficacy to limit drinking mediates the association between attitudes and alcohol-related outcomes. Substance Use and Misuse, 54, 2400–2408. doi: 10.1080/10826084.2019.1653322 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Evans-Polce RJ, Patrick ME, & O’Malley PM (2017). Prospective associations of 12th grade drinking intensity and age 19/20 driving-related consequences. Journal of Adolescent Health, 61, 389–391. doi: 10.1016/j.jadohealth.2017.04.016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grant GF, Goldstein RB, Saha TD, Chou SP, Jung J, Zhang H,…Hasin DS (2015). Epidemiology of DSM-5 alcohol use disorder: results from the National Epidemiologic Survey on Alcohol and Related Conditions III. JAMA Psychiatry, 72, 757–766. doi: 10.1001/jamapsychiatry.2015.0584 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grant VV, Stewart SH, O’Connor RM, Blackwell E, & Conrod PJ (2007). Psychometric evaluation of the five-factor Modified Drinking Motives Questionnaire-Revised in undergraduates. Addictive Behaviors, 32, 2611–2632. doi: 10.1016/j.addbeh.2007.07.004 [DOI] [PubMed] [Google Scholar]
- Helle AC, Trull TJ, Watts AL, McDowell Y, & Sher KJ (2020). Psychiatric comorbidity as a function of severity: DSM-5 alcohol use disorder and HiTOP classification of mental disorders. Alcoholism: Clinical and Experimental Research, 44, 632–644. doi: 10.1111/acer.14284 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hingson RW, Zha W, & White AM (2017). Drinking beyond the binge threshold: predictors, consequences, and changes in the U.S. American Journal of Preventive Medicine, 52, 717–727. doi: 10.1016/j.amepre.2017.02.014 [DOI] [PubMed] [Google Scholar]
- Jennison KM (2004). The short-term effects and unintended long-term consequences of binge drinking in college: a 10-year follow-up study. American Journal of Drug Alcohol Abuse, 30, 659–684. doi: 10.1081/ADA-200032331 [DOI] [PubMed] [Google Scholar]
- Kahler CW, Hustad J, Barnett NP (2008). Validation of the 30-day version of the Brief Young Adult Consequences Questionnaire for use in longitudinal studies. Journal of Studies on Alcohol and Drugs, 69, 611–615. doi: 10.15288/jsad.2008.69.611 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Knopik VS, Heath AC, Madden PAF, Bucholz KK, Slutske WS,…Martin NG (2004). Genetic effects on alcohol dependence risk: re-evaluating the importance of psychiatric and other heritable risk factors. Psychological Medicine, 34, 1519–1530. doi: 10.1017/s0033291704002922 [DOI] [PubMed] [Google Scholar]
- Krieger H, Young CM, Anthenien AM, & Neighbors C (2018). The epidemiology of binge drinking among college-age individuals in the United States. Alcohol Research: Current Reviews, 39, 23–30. https://pubmed.ncbi.nlm.nih.gov/30557145/ [PMC free article] [PubMed] [Google Scholar]
- Kroenke K, Spitzer RL, Williams JB (2001). The PHQ-9: Validity of a brief depression severity measure. Journal of General Internal Medicine, 16, 606–616. doi: 10.1046/j.1525-1497.2001.016009606.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kuntsche E, Knibbe R, Gmel G, & Engels R (2005). Why do young people drink? A review of drinking motives. Clinical Psychology Review, 25, 841–861. doi: 10.1016/j.cpr.2005.06.002 [DOI] [PubMed] [Google Scholar]
- Kuntsche E, Kuntsche S, Thrul J, & Gmel G (2017). Binge drinking: health impact, prevalence, correlates and interventions. Psychology and Health, 32, 976–1017. doi: 10.1080/08870446.2017.1325889 [DOI] [PubMed] [Google Scholar]
- Larimer ME, Lee CM, Kilmer JR, Fabiano PM, Stark CB, Geisner IM....Neighbors C (2007). Personalized mailed feedback for college drinking prevention: a randomized clinical trial. Journal of Consulting and Clinical Psychology, 75, 285–293. doi: 10.1037/0022-006X.75.2.285 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lieb R, Merikangas KR, Höfler M, Pfister H, Isensee B, & Wittchen HU (2002). Parental alcohol use disorders and alcohol use and disorders in offspring: a community study. Psychological Medicine, 32, 63–78. doi: 10.1017/s0033291701004883 [DOI] [PubMed] [Google Scholar]
- Linden-Carmichael AN, Calhoun BH, Patrick ME, & Maggs JL (2018). Are protective behavioral strategies associated with fewer negative consequences on high-intensity drinking days? Results from a measurement-burst design. Psychology of Addictive Behaviors, 32, 904–913. doi: 10.1037/adb0000421 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Linden-Carmichael AN, Calhoun BH, Patrick ME, & Maggs JL (2019). University students use fewer protective behavioural strategies on high-intensity drinking days. Drug and Alcohol Review, 38, 302–305. doi: 10.1111/dar.12913 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Linden-Carmichael AN, Lanza ST, Dziak JJ, & Bray BC (2017). Contemporary alcohol use patterns among a national sample of U.S. adult drinkers. Journal of Addictive Diseases, 36, 222–226. doi: 10.1080/10550887.2017.1338816 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Linden-Carmichael AN, Vasilenko SA, Lanza ST, Maggs JL (2017). High-intensity drinking versus heavy episodic drinking: prevalence rates and relative odds of alcohol use disorder across adulthood. Alcoholism: Clinical and Experimental Research, 41, 1754–1759. doi: 10.1111/acer.13475 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Llerena S, Arias-Loste MT, Puente A, Cabezas J, Crespo J, & Fábrega E (2015). Binge drinking: burden of liver disease and beyond. World Journal of Hepatology, 7, 2703–2715. doi: 10.4254/wjh.v7.i27.2703 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCabe SE, Veliz P, & Patrick ME (2017). High-intensity drinking and nonmedical use of prescription drugs: Results from a national survey of 12th grade students. Drug and Alcohol Dependence, 178, 372–379. doi: 10.1016/j.drugalcdep.2017.05.038 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mehus CJ, & Patrick ME (2020). Alcohol use among 10th-graders: distinguishing between high-intensity drinking and other levels of use. Journal of Adolescence, 83, 27–30. doi: 10.1016/j.adolescence.2020.07.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Merrill JE, Boyle HK, Jackson KM, & Carey KB (2019). Event-level correlates of drinking events characterized by alcohol-induced blackouts. Alcoholism: Clinical and Experimental Research, 43, 2599–2606. doi: 10.1111/acer.14204 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miech RA, Johnston LD, O’Malley PM, Bachman JG, Schulenberg JE, & Patrick ME (2019). Monitoring the Future national survey results on drug use, 1975-2018: Volume I, Secondary school students. Ann Arbor: Institute for Social Research, The University of Michigan. [Google Scholar]
- Monti PM, Tevyaw TO, & Borsari B (2004/2005). Drinking among young adults. Alcohol Research and Health, 28, 236–244. [Google Scholar]
- Murphy JG, Dennhardt AA, Martens MP, Borsari B, Witkiwitz K, Meshesha LZ (2019). A randomized clinical trial evaluating the efficacy of a brief alcohol intervention supplemented with a substance-free activity session or relaxation training. Journal of Consulting and Clinical Psychology, 87, 657–669. doi: 10.1037/ccp0000412 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murphy JG, Skidmore JR, Dennhardt AA, Martens MP, Borsari B, Barnett NP, & Colby SM (2012). A behavioral economic supplement to motivational interventions for college drinking. Addiction Research and Theory, 20, 456–465. doi: 10.3109/16066359.2012.665965 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nahum-Shani I, Hekler EB, & Spruijt-Metz D (2015). Building health behavior models to guide the development of just-in-time adaptive interventions: a pragmatic framework. Health Psychology, 34S, 1209–1219. doi: 10.1037/hea0000306 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Naimi TS, Nelson DE, & Brewer RD (2010). The intensity of binge alcohol consumption among U.S. adults. American Journal of Preventive Medicine, 38, 201–207. doi: 10.1016/j.amepre.2009.09.039 [DOI] [PubMed] [Google Scholar]
- National Kids Count. (2020). Young adults ages 18 to 24 who are enrolled in or have completed college in the United States. Annie E. Casey Foundation Kids Count Data Center. https://datacenter.kidscount.org/data/tables/77-young-adults-ages-18-to-24-who-are-enrolled-in-or-have-completed-college#detailed/1/any/false/37,871,870,573,869,36,868,867,133,38/any/388,389 [Google Scholar]
- NIAAA (National Institute on Alcohol Abuse and Alcoholism) (2018). High-intensity drinking working group meeting. Retrieved from https://www.niaaa.nih.gov/news-events/meetings-events-exhibits/high-intensity-drinking-working-group-meeting
- Neighbors C, Larimer ME, & Lewis MA (2004). Targeting misperceptions of descriptive drinking norms: efficacy of a computer-delivered personalized normative feedback intervention. Journal of Consulting and Clinical Psychology, 72, 434–447. doi: 10.1037/0022-006X.72.3.434 [DOI] [PubMed] [Google Scholar]
- Neighbors C, Lee CM, Lewis MA, Fossos N, & Larimer ME (2007). Are social norms the best predictor of outcomes among heavy-drinking college students? Journal of Studies on Alcohol and Drugs, 68, 556–565. doi: 10.15288/jsad.2007.68.556 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nguyen-Louie TT, Tracas A, Squeglia LM, Matt GE, Eberson-Shumate S, & Tapert SF (2016). Learning and memory in adolescent moderate, binge, and extreme-binge drinkers. Alcoholism: Clinical and Experimental Research, 40, 1895–1904. doi: 10.1111/acer.13160 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patrick ME (2016). A call for research on high-intensity alcohol use. Alcoholism: Clinical and Experimental Research, 40, 256–259. doi: 10.1111/acer.12945 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patrick ME, & Azar B (2017). High-intensity drinking. Alcohol Research: Current Reviews, 39, e1–e7. [PMC free article] [PubMed] [Google Scholar]
- Patrick ME, Boatman JA, Morrell N, Wagner AC, Lyden GR, Nahum-Shani I,… Almirall D (2020). A sequential multiple assignment randomized trial (SMART) protocol for empirically developing an adaptive preventive intervention for college student drinking reduction. Contemporary Clinical Trials, 96, 106089. doi: 10.1016/j.cct.2020.106089 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patrick ME, Cronce JM, Fairlie AM, Atkins DC, & Lee CM (2016). Day-to-day variations in high-intensity drinking, expectancies, and positive and negative alcohol-related consequences. Addictive Behaviors, 58, 110–116. doi: 10.1016/j.addbeh.2016.02.02 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patrick ME, Evans-Polce R, Kloska DD, Maggs JL, & Lanza ST (2017). Age-Related Changes in Associations Between Reasons for Alcohol Use and High-Intensity Drinking Across Young Adulthood. Journal of Studies on Alcohol and Drugs, 78, 558–570. doi: 10.15288/jsad.2017.78.558 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patrick ME, Evans-Polce RJ, Parks MJ, & Terry-McElrath YM (in press). Drinking intensity at age 29/30 as a predictor of alcohol use disorder symptoms at age 35 in a national sample. Journal of Studies on Alcohol and Drugs. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patrick ME, Evans-Polce R, & Terry-McElrath YM (2019). Faster escalation from first drink to first intoxication as a risk factor for binge and high-intensity drinking among adolescents. Addictive Behaviors, 92, 199–202. doi: 10.1016/j.addbeh.2019.01.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patrick ME, Schulenberg JE, Martz ME, Maggs JL, O’Malley PM, & Johnston LD (2013). Extreme Binge Drinking Among 12th-Grade Students in the United States Prevalence and Predictors JAMA Pediatrics, 167, 1019–1025. doi: 10.1001/jamapediatrics.2013.2392 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patrick ME, & Terry-McElrath YM (in press). Drinking motives, alcohol use, and dinking consequences across days among U.S. young adults: differences and similarities between moderate, binge, and high-intensity drinking. Alcoholism: Clinical and Experimental Research. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patrick ME, & Terry-McElrath YM (2017). High-intensity drinking by underage young adults in the United States. Addiction, 112, 82–93. doi: 10.1111/add.13556 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patrick ME, & Terry-McElrath YM (2019). Prevalence of high-intensity drinking from adolescence through young adulthood: national data from 2016-2017. Substance Abuse: Research and Treatment, 13, 1–5. doi: 10.1177/1178221818822976 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patrick ME, Terry-McElrath YM, Kloska DD, & Schulenberg JE (2016). High-intensity drinking among young adults in the United States: prevalence, frequency, and developmental change. Alcoholism: Clinical and Experimental Research, 40, 1905–1912. doi: 10.1111/acer.13164 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patrick ME, Terry-McElrath YM, Miech RA, O’Malley PM, Schulenberg JE, & Johnston LD (2017). Current high-intensity drinking among eighth and tenth grade students in the U.S. American Journal of Preventive Medicine, 53, 904–908. doi: 10.1016/j.amepre.2017.06.027 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patrick ME, Terry-McElrath YM, Miech RA, Schulenberg JE, O’Malley PM, & Johnston LD (2017). Age-specific prevalence of binge and high-intensity drinking among US young adults: changes from 2005 to 2015. Alcoholism: Clinical and Experimental Research, 47(7), 1319–1328. doi: 10.1111/acer.13413 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patrick ME, Terry-McElrath YM, Schulenberg JE, & Bray BC (2017). Patterns of high-intensity drinking among young adults in the United States: A repeated measures latent class analysis. Addictive Behaviors, 74, 134–139. doi: 10.1016/j.addbeh.2017.06.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patrick ME, Veliz PT, & Terry-McElrath YM (2017). High-intensity and simultaneous alcohol and marijuana use among high school seniors in the United States. Substance Abuse, 38, 498–503. doi: 10.1080/08897077.2017.1356421 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pearson MR, Kirouac M, & Witkiewitz K (2016). Questioning the Validity of the 4+/5+ Binge or Heavy Drinking Criterion in College and Clinical Populations. Addiction, 111, 1720–1726. doi: 10.1111/add.13210 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Piano MR, Mazzuco A, Kang M, & Phillips SA (2017). Cardiovascular consequences of binge drinking: an integrative review with implications for advocacy, policy, and research. Alcoholism: Clinical and Experimental Research, 41, 487–496. doi: 10.1111/acer.13329 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ramo DE, Kaur M, Corpuz ES, Satre DD, Delucchi K, Brown SA, & Prochaska JJ (2018). Using Facebook to address smoking and heavy drinking in young adults: protocol for a randomized, controlled trial. Contemporary Clinical Trials, 26, 52–60. doi: 10.1016/j.cct.2018.02.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Read JP, Beattie M, Chamberlain R, & Merrill JE (2008). Beyond the “binge” threshold: heaving drinking patterns and their association with alcohol involvement indices in college students. Addictive Behaviors, 33, 225–234. doi: 10.1016/j.addbeh.2007.09.001 [DOI] [PubMed] [Google Scholar]
- Samson JE, & McHugh RM (2019). Brief alcohol interventions for adolescents and young adults in emergency department settings: a descriptive review and meta-analysis. Adolescent Research Review, 4, 313–327. doi: 10.1007/s40894-018-0102-7 [DOI] [Google Scholar]
- Schulenberg JE, Johnston LD, O’Malley PM, Bachman JG, Miech RA, & Patrick ME (2020). Monitoring the Future national survey results on drug use, 1975-2019: Volume II, college students and adults ages 19-60. Ann Arbor: Institute for Social Research. [Google Scholar]
- Spitzer RL, Kroenke K, Williams JB, & Löwe B (2006). A brief measure for assessing generalized anxiety disorder: the GAD-7. Archives of Internal Medicine, 166, 1092–1097. doi: 10.1001/archinte.166.10.1092. [DOI] [PubMed] [Google Scholar]
- Spitzer RL, Kroenke K, Williams JB (1999). Validation and utility of a self-report version of PRIME-MD: The PHQ primary care study. Journal of the American Medical Association, 282, 1737–1744. doi: 10.1001/jama.282.18.1737 [DOI] [PubMed] [Google Scholar]
- Stephens DN, & Duka T (2008). Cognitive and emotional consequences of binge drinking: role of amygdala and prefrontal cortex. Philosophical Transactions of the Royal Society of London. Series B, Biological Sciences, 363, 3169–3179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Substance Abuse and Mental Health Services Association. (2020). 2019 NSDUH Detailed Tables. https://www.samhsa.gov/data/report/2019-nsduh-detailed-tables
- Suffoletto B, Kristan J, Chung T, Jeong K, Fabio A, Monti P, & Clark DB (2015). An interactive text message intervention to reduce binge drinking in young adults: a randomized controlled trial with 9-month outcomes. PLoS One, 10, e0142877. doi: 10.1371/journal.pone.0142877 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Terry-McElrath YM, & Patrick ME (2016). Intoxication and binge and high-intensity drinking among US young adults in their mid-20s. Substance Abuse, 37, 597–605. doi: 10.1080/08897077.2016.1178681 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Terry-McElrth YM, & Patrick ME (2020). U.S. adolescent alcohol use by race/ethnicity: consumption and perceived need to reduce/stop use. Journal of Ethnicity in Substance Abuse, 19, 3–27. doi: 10.1080/15332640.2018.1433094 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Terry-McElrath YM, Stern SA, & Patrick ME (2017). Do Alcohol Use Reasons and Contexts Differentiate Adolescent High-Intensity Drinking? Data from U.S. High School Seniors, 2005–2016. Psychology of Addictive Behaviors, 31, 775–785. doi: 10.1037/adb0000314 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tice P, Lipari RN, & Van Horn SL (2017). Substance use among 12th grade aged youths, by dropout status. The CBHSQ Report: August 15. Center for Behavioral Health Statistics and Quality, Substance Abuse and Mental Health Services Administration, Rockville, MD. [PubMed] [Google Scholar]
- Treloar H, Martens MP, & McCarthy DM (2015). The Protective Behavioral Strategies Scale-20: improved content validity of the serious harm reduction subscale. Psychological Assessment, 27, 340–346. doi: 10.1037/pas0000071 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Uphoff E, Ekers D, Robertson L, Dawson S, Sanger E, South E,…Churchill R (2020). Behavioural activation therapy for depression in adults. Cochrane Database of Systematic Reviews, 7, CD013305. doi: 10.1002/14651858.CD013305.pub2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walton MA, Chermack ST, Blow FC, Ehrlich PF, Barry KL, Booth BB, & Cunningham RM (2015). Components of brief alcohol interventions for youth in the emergency department. Substance Abuse, 36, 339–349. doi: 10.1080/08897077.2014.958607 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang Q (2020). High-intensity binge drinking is associated with cigarette smoking and e-cigarette use among US adults aged 40–64 years: Findings from the 2017 BRFSS survey. Tobacco Induced Diseases, 18, 54. doi: 10.18332/tid/122603 [DOI] [PMC free article] [PubMed] [Google Scholar]
- White HR, Anderson KG, Ray AE, & Mun E-Y. (2016). Do drinking motives distinguish extreme drinking college students from their peers? Addictive Behaviors, 60, 213–218. doi: 10.1016/j.addbeh.2016.04.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- White AM, Kraus CL, & Swartzwelder H (2006). Many college freshmen drink at levels far beyond the binge threshold. Alcoholism: Clinical and Experimental Reserch, 30, 1006–1010. doi: 10.1111/j.1530-0277.2006.00122.x. [DOI] [PubMed] [Google Scholar]


