Abstract
Objective
The study aimed to understand multimorbidity among adults in a high-tech city in southern coastal China that has undergone rapid economic development and to investigate its relationship with lifestyle status.
Methods
A population-based survey was conducted among 24 community centers in the Nanshan District of Shenzhen from February to December of 2018. Participants were recruited using a stratified random sampling approach. A self-administered questionnaire on typical chronic diseases, lifestyle factors, body composition, and social demographics was used to collect data. Multimorbidity was defined as two or more chronic diseases coexisting in a single person. An algorithm on body mass index, physical activity, drinking, smoking, and sleep quality was used to calculate lifestyle scores (0–9), with higher scores predicting a healthier lifestyle.
Results
A total of 2,905 participants were included in the analysis, with men accounting for 52.4%, and single for 25%. The prevalence of multimorbidity was 4.8%, and the mean lifestyle score was 4.79 ± 1.55. People who were old, retired, married, and had less education were more likely to have multimorbidity (all P < .05). A higher prevalence of multimorbidity was found among those who were obese, less engaged in physical activity, consumed more alcohol, and had poorer sleep quality (all p < .05). After adjusting for age, employment, education, and marital status, one unit increase in lifestyle score was associated with 0.74 times lower to have multimorbidity (OR: 0.74; 95% CI: 0.63–0.87, p < .05).
Conclusion
The prevalence of multimorbidity was relatively low in economically developed Shenzhen. Keeping a healthy lifestyle was related to the lower possibility of suffering from multiple chronic diseases.
Keywords: Lifestyle, smoking, drinking, exercise, body mass index, sleep
Introduction
Multimorbidity refers to the coexistence of two or more chronic diseases in an individual. 1 As populations worldwide age, multimorbidity has increased in prevalence by more than 10% over the past two decades.2–5 Even among people of working age, the prevalence has reached 30%.6,7 Multimorbidity has become a major public health issue and is related to high healthcare costs and hospital admissions. Compared with the healthy population, the hospital admission rate of patients with multimorbidity was found to be 5.6 times higher, 8 which impose a heavy burden to the public health. Multimorbidity can also significantly affect individuals’ mental and physical well-being. 9
The evidence showed that lifestyle factors were associated with the occurrence of multimorbidity, such as physical inactivity, smoking, alcohol consumption, obesity, and inefficient sleep.10–12 A study conducted in Canada on a population of 10,000 showed that people who were physically inactive or obese were 1.06 times (95% CI: 1.01–1.11) and 1.37 times (95% CI: 1.32–1.43), respectively, more likely to have multimorbidity. 11 Lifestyles have changed with economic and social developments. Owing to the rapid urbanization rate, the lifestyle of Chinese people has changed drastically. 13 Shenzhen, located at the border with Hong Kong, is an example of a metropolis in China that has developed quickly. In 2020, Shenzhen ranked third in China in terms of gross domestic product (GDP), at approximately 2.77 trillion yuan (approximately 396.9 billion U.S. dollars).14 Eight Fortune 500 companies operate in the city, among which are Huawei, Tencent, and Da-Jiang Innovations (DJI). Every year, Shenzhen attracts domestic and foreign companies and talented people. With the announcement of the formation of the Greater Bay Area (Guangdong-Hong Kong-Macao), the rate of migration to Shenzhen surpassed even that of Beijing and Shanghai. 15
Owing to rapid urbanization, a diverse immigration population, new technologies, and a fast pace of life, people in Shenzhen tend to lead unhealthy lifestyles. Previous studies have revealed that 95.4% of migrant workers were not physically active enough, 16 and 25.4% experienced poor sleep quality. 17 The prevalence rates of smoking and obesity among adults aged 35 years and older were 19.97% nationally and 28.29% in Shenzhen, respectively. 18 What is the situation with multimorbidity and what is its association with lifestyle status in this city? No relevant study has focused on this population. Only one study conducted in a rural area of China investigated the relationship between socioeconomic and lifestyle factors with multimorbidity in older people. 19 It indicated that older people who are comfortably off (i.e., those who own a home and have medical coverage) were less likely to have multimorbidity. However, the findings could not be generalized to other Chinese populations owing to huge differences in lifestyle between rural and urban areas in China. Furthermore, most previous studies examined the association between individual lifestyle factors and multimorbidity. 20 An increasing body of evidence supported that multiple lifestyle factors played a more vital role in preventing and reducing the disease burden compared with individual factor. 21 Since personal lifestyles is a synthesis of various living habits and behaviors, unhealthy behavior tend to occur clustered and exert a synergistic impact on mortality. 22 In view of unclear relationship between combined lifestyle habits and occurrence of multimorbidity, we therefore conducted the present study with the aim to understand the relationship between lifestyle status and multimorbidity in a sample of adults living in high-tech city in southern coastal China that has undergone rapid social-economic transformation in the past decades.
Methods
Study design and setting
The data analyzed in this study were extracted from a larger-scale community-based survey implemented in 24 community health service centers in the Nanshan District of Shenzhen from February to December 2018. The purpose was to understand the typical health needs of the residents of the target community. The 24 participating community health service centers are managed by the Huazhong University of Science and Technology Union Shenzhen Hospital (HUSTUSH). The latter provides primary healthcare services and manages typical health problems in the community to fulfill the basic health demands of residents of the community. The main health services provided include vaccination, rehabilitation, health education, birth control, postpartum follow-ups, chronic disease management, mental health support, traditional medicine treatments, and cancer screening. The serviced populations are all residents of those areas and are typically women, children, older people, patients with chronic diseases, and people with disabilities.
Study population
Nanshan residents who visited one of the 24 community health service centers and met the criteria for eligibility to participate in this study were considered potential participants. The inclusion criteria were (1) aged 18 years and above, (2) able to read and write Chinese or able to speak Cantonese or Putonghua, and (3) currently residing in Nanshan. The exclusion criteria were (1) having lived in the Nanshan District for less than one year, (2) psychologically or physically unable to communicate, or (3) unable to provide informed consent.
Sample size, sampling, and recruitment procedure
Based on the government report, the size of the population (aged 18 or above) in the Nanshan District of Shenzhen at the end of 2016 was 1,356,307. Assuming that the overall prevalence of all chronic diseases was 30%, 2,800 participants would be needed to achieve a power of 80% for the study at the 0.05 level of significance. A stratified random sampling method was used to recruit the participants. First, the number of participants needed in each age group (18–44, 45–64, and 65+ years) was determined by referring to the age and sex distribution in the Nanshan population. 23 The HUSTUSH had a list of Nanshan residents who had registered at the community health service centers. These residents regularly visited the service centers for body checks or health consultations. The community nurses randomly invited subjects from the list to visit the service centers to take part in the study. Screening for eligibility was then conducted according to the inclusion and exclusion criteria. Subjects who provided written informed consent were considered eligible participants. Thereafter, the participants completed a self-administered questionnaire at the centers. Valid participation was defined as having no more than 10% of the data missing in any one part of the questionnaire.
Measures
Identification of chronic diseases and multimorbidity
Based on the leading causes of both death and non-communicable diseases in China, 24 information on the following eleven chronic diseases was collected: hypertension, diabetes, chronic obstructive lung disease, stroke, coronary heart disease or other heart disease, osteoarthritis, asthma, high cholesterol, hepatitis, cancer, and headache disorder. Furthermore, under the item “others,” the participants could write down the names of any other diseases that they were suffering from. All of the diseases reported by the participants were confirmed through their medical records. We then counted the number of chronic diseases that one person suffered. Multimorbidity was defined as two or more chronic diseases coexisting in a single person. 25
Lifestyle factors and anthropometrics
Physical Activity (PA). The present study used the short form of the International Physical Activity Questionnaire (IPAQ) to measure the physical activity of the participants during the last seven days. 26 The IPAQ short form is a self-administered questionnaire with seven items, covering activities in the areas of transportation, work, house and yard work, and even recreation. People were asked to recall the duration and frequency with which they engaged in vigorous-intensity, moderate-intensity, and walking activities. Then, the total metabolic equivalents (METs) were calculated in terms of the number of minutes/week that the individual engaged in each activity. Based on the results, the activity was categorized into three levels: low, moderate, and high. The intra-class correlation coefficient of the Chinese version of IPAQ was 0.79. 27
Sleep quality. Sleep quality was measured using the Chinese Pittsburg Sleep Quality Index (PSQI), a widely used nineteen-item scale that assesses the quality and patterns of sleep. 28 Each item was scored as a structured categorical value (from 0 to 3), from which seven components were generated to assess the specific feature of sleep. The seven components are as follows: subjective sleep quality, sleep latency, sleep duration, habitual sleep efficiency, sleep disturbances, the use of sleep medication, and daytime dysfunction. The global PSQI score is the sum of the scores of the seven components. It ranges from 0 to 21. Lower scores mean better sleep. The threshold for good sleep quality is 5. The reliability of the Chinese version of PSQI was 0.82. 29
Alcohol consumption. Alcohol consumption was surveyed by asking people whether they had ever drunk alcohol. The participants were grouped into three categories according to their drinking status: never drink alcohol, used to drink but have now quit, and currently drinking alcohol. If the participants are currently drinking, they would be asked about the frequency and amount that they drink and what kind of drink.
Smoking. Smoking was assessed by asking people whether they had ever smoked (non-smoker, ex-smoker, and smoker). In addition, participants were asked which of the following they would choose to smoke (cigarettes, cigar, self-rolling cigarettes, and e-cigarettes). Smokers were asked about the number of cigarettes they smoked per day and whether they had attempted to quit smoking in the past one year.
Body Mass Index (BMI). Participants were asked to stand on an ultrasonic sensor height and weight electronic scale (Brand SK) in their bare feet with light clothes when they came to the community center. The scale automatically provided data on height, weight, and BMI, which were recorded by the community nurses. Weight was recorded to the nearest 0.1 kg and height to the nearest 0.1 m. Each participant was measured twice, and the average value was calculated as that individual’s final BMI. BMI was derived from body weight (kg) divided by the square of the body height (m) (BMI = kg/m2). Subjects were classified as underweight (BMI < 18.5 kg/m2), normal weight (BMI 18.6–22.9 kg/m2), overweight (BMI 23–24.9 kg/m2), or obese (BMI ≥ 25 kg/m2) based on the World Health Organization’s standards for Asian populations. 30
Lifestyle score calculation
A total lifestyle score was calculated using an algorithm that summarized the sub-scores from physical activity, alcohol consumption, smoking, sleep quality, and BMI. 31 Each lifestyle factor was classified according to three levels: optimal (2 points), intermediate (1 point), and poor (0 point). Table 1 shows the classifications for the lifestyle score. BMI: less than 23 kg/m2 (optimal), 23–24.9 kg/m2 (intermediate), 25 kg/m2 or above (poor). Total amount of time spent on physical activity per week: 150 min or above (optimal), less than 150 min (intermediate), and 0 min (poor). 32 Alcohol consumption: 1–7 glasses/week for women and 1–14 glasses/week for men (optimal), no drink (intermediate), more than 7 glasses/week for women, and 14 glasses/week for men (poor).33–35 Smoking: never a smoker (optimal), former smoker (intermediate), and current smoker (poor). PSQI score: 5 or less (optimal), and larger than 5 (poor). 29 The sum of the above scores reflected the total score for lifestyle status, which could range from 0 (least healthy lifestyle) to 9 (most healthy lifestyle).
Table 1.
Construction and weighted score of lifestyle score.
| Construction | Score weighted | ||
|---|---|---|---|
| Optimal (2) | Intermediate (1) | Poor (0) | |
| BMI | <23 | 23–24.9 | ≥25 |
| Total Physical Activity | ≥150 min | <150 min | no |
| Alcohol consumption | 1–7 dose /wk for women | no | ≥8 dose /wk for women |
| 1–14 dose/wk for men | ≥15 dose/wk for men | ||
| Smoking status | Never | Former | Current smokers |
| Sleep quality | Optimal (1): < = 5 | Poor (0): >5 | |
| Total score | 0–9 a | ||
aLarger number means healthier lifestyle
Sociodemographic characteristics
Sociodemographic variables were assessed in the questionnaire, which included sex (male or female), age group (18–44 years, 45–64 years, ≥65 years), employment status (employed, retired, student, and unemployed), level of education (primary or lower, secondary school, college, master’s, and above), marital status (single and married/with partner), and total monthly family income (in RMB, conversion rate: 1 RMB = 0.154 US).
Data analysis
To describe the basic characteristics of the participants, mean and standard deviation (SD) were used for the continuous variables and counts and percentages for the categorical variables. Those who had been diagnosed with two or more chronic conditions were classified as “having multimorbidity.” The other participants were grouped under “no disease” and “one disease,” respectively. A Chi-square test, independent t-tests, and ANOVA were used to compare the differences in multimorbidity situation and lifestyle score between different socio-demographic groups where appropriate. Fisher’s exact test was also adopted in the study if small numbers of cases existed in some sub-groups. The binary logistic regression analysis was used to further analyze the association between multimorbidity and lifestyle. Several regression models were implemented, and the odds ratios (OR) were calculated. In Model 1, only lifestyle score was involved as independent variable. In Model 2, except lifestyle score, the demographic characteristics were also adjusted. In Model 3, the independent variables were the same as those in Model 2, while the dependent variable was categorized as the participants with multimorbidity vs. had no disease. In Model 4, the dependent variable was categorized as participants with one chronic disease vs. multimorbidity. SPSS version 23.0 (SPSS Institute) was used in all data analyses, and the level of significance was considered to be 0.05.
Results
Basic characteristics and the situation of multimorbidity in the study population
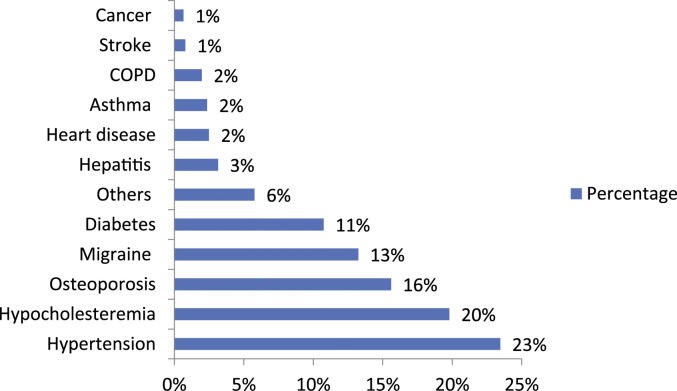
A total of 2,905 participants were involved in the analysis, with males accounting for 52.4%; the majority were young adults (73.8%), 85.8% were working, 25% were single, and 67.7% had a bachelor’s degree or a higher level of education. Approximately one fifth (19.8%) of the participants reported suffering from at least one chronic disease (Figure 1). The prevalence of multimorbidity among the participants was 4.8%. The most prevalent chronic disease was hypertension (6.2%), followed by hypercholesterolemia (5.2%), and osteoporosis (4.1%). No statistically significant differences were found between those of different sex and income levels. People who were old, retired, married, and had a lower level of education were more likely to have multimorbidity (all p < .05) (Table 2). The overall lifestyle score was 4.79 ± 1.55. Males had healthier lifestyles than females (p < .001). People who were young, employed, single, and had a higher level of education were more likely to have a healthier lifestyle (all p < .05) (Table 2).
Figure 1.
Percentage of comorbidity among participants.
Table 2.
Multimorbidity and lifestyle score according to demographical variables.
| Variables | N (%) | Multimorbidity, n (%) | p-value a | Lifestyle score(M±SD) | p-value a |
|---|---|---|---|---|---|
| Sex | .135 | <.001 | |||
| Male | 1522 (52.4%) | 80 (5.31%) | 5.02 ± 1.67 | ||
| Female | 1383 (47.6%) | 59 (4.35%) | 4.51 ± 1.34 | ||
| Age Group | <.001 | <.001 | |||
| Young Adult(18–44) | 2144 (73.8%) | 29 (1.4%) | 4.94 ± 1.53 | ||
| Middle Age (45–64) | 662 (22.8%) | 77 (11.70%) | 4.29 ± 1.54 | ||
| Elderly (≥65) | 94 (3.2%) | 33 (35.48%) | 4.07 ± 1.43 | ||
| Employment status | <.001 | <.001 | |||
| Employed | 2494 (85.8%) | 62 (2.52%) | 4.87 ± 1.54 | ||
| Student | 64 (2.2%) | 1 (1.6%) | 4.90 ± 1.22 | ||
| Retired | 189 (6.5%) | 57 (30.81%) | 3.87 ± 1.50 | ||
| Unemployed | 133 (4.6%) | 17 (12.87%) | 4.79 ± 1.52 | ||
| Marital status | <.001 | <.001 | |||
| Single | 730 (25.1%) | 11 (1.54%) | 5.08 ± 1.47 | ||
| Married/With partner | 2136 (73.5%) | 127 (6.00%) | 4.68 ± 1.57 | ||
| Educational Level | <.001 | <.001 | |||
| Primary Level or Lower | 73 (2.5%) | 17 (23.61%) | 4.12 ± 1.52 | ||
| Secondary School | 830 (28.6%) | 70 (8.62%) | 4.59 ± 1.73 | ||
| College | 1849 (63.6%) | 50 (2.73%) | 4.88 ± 1.48 | ||
| Master and above | 119 (4.1%) | 1 (0.85%) | 4.80 ± 1.34 | ||
| Family Monthly Income (CNY) | .388 | .268 | |||
| <10,000 | 422 (14.5%) | 16 (3.88%) | 4.9 ± 1.78 | ||
| 10,000–29,999 | 1233 (42.4%) | 61 (4.98%) | 4.77 ± 1.48 | ||
| 30,000–59,999 | 874 (30.1%) | 40 (4.66%) | 4.69 ± 1.43 | ||
| 60,000 or Above | 101 (3.5%) | 8 (7.92%) | 4.89 ± 1.89 |
aChi-Square, fish-exact test; ANOVA, Independent t-tests.
Associations between lifestyle factors and multimorbidity
A higher proportion of those overweight and obese had multimorbidity than those who were not obese (p < .001). A higher level of total PA was linked with a lower proportion of multimorbidity (p = .018). People engaged in more than 75 min of vigorous PA were more likely to have lower multimorbidity (p = .035), but no significant association was found between moderate PA and multimorbidity (p > .05). Alcohol consumption and amount of drinking were both linked to multimorbidity (p < .001). A lower proportion of multimorbidity was found among people who never drank alcohol than among those who had quit drinking or who were currently drinking alcohol (P < .05). No significant difference was found according to smoking status (p < .05), but a higher proportion of multimorbidity was observed among people who consumed more cigarettes daily (p = .013). Moreover, people who suffered with poor sleep quality were more likely to have multimorbidity (p < .001). The lifestyle score was higher among participants without multimorbidity than among those with multimorbidity (P < .001) (Table 3).
Table 3.
Associations between lifestyle factors and multimorbidity.
| Multimorbidity | p-value* | ||
|---|---|---|---|
| No | Yes | ||
| BMI | <.001 | ||
| Underweight (<18.5) | 151 (99.3%) | 1 (0.7%) | |
| Normal (18.5–23.9) | 1899 (96.4%) | 70 (3.6%) | |
| Overweight (24–27.9) | 558 (91.5%) | 52 (8.5%) | |
| Obesity (≥28) | 84 (84.8%) | 15 (15.2%) | |
| VPAWeekly | .035 | ||
| No VIPA | 1370 (94.9%) | 74 (5.1%) | |
| < 75 min | 189 (97.9%) | 4 (2.1%) | |
| ≥ 75 min | 512 (97.0%) | 16 (3.0%) | |
| MPAWeekly | |||
| No MIPA | 997 (96.0%) | 42 (4.0%) | .390 |
| < 150 min | 409 (94.5%) | 24 (5.5%) | |
| ≥ 150 min | 815 (95.0%) | 43 (5.0%) | |
| TOPAWeekly | .018 | ||
| No PA | 912 (95.9%) | 39 (4.1%) | |
| < 150 min | 249 (91.9%) | 22 (8.1%) | |
| ≥ 150 min | 1231 (95.6%) | 57 (4.4%) | |
| Alcohol consumption | |||
| Never | 1783 (96.5%) | 65 (3.5%) | <.001 |
| Quitted | 151 (88.3%) | 20 (11.7%) | |
| Yes | 686 (94.2%) | 42 (5.8%) | |
| Amount of drinking | 1.92 ± 1.12 | 2.73 ± 1.28 | <.001 |
| Smoking status | .119 | ||
| Never | 2202 (95.5%) | 104 (4.5%) | |
| Quitted | 117 (97.5%) | 3 (2.5%) | |
| Yes | 277 (93.3%) | 20 (6.7%) | |
| Amount of Cigarettes, daily | 9.68 ± 7.47 | 13.91 ± 9.95 | .013 |
| PSQI (mean score) | 4.42 ± 2.45 | 7.12 ± 3.10 | <.001 |
| PSQI score | <.001 | ||
| Optimal ≤5 | 1642 (97.9%) | 36 (2.1%) | |
| Poor>5 | 623 (89%) | 77 (11%) | |
| Lifestyle score | 4.84 ± 1.52 | 3.77 ± 1.66 | <.001 |
VPA: Vigorous physical activity; MPA: moderate physical activity; TOPA weekly: weekly total physical activity; PSQI: Pittsburg Sleep Quality Index.
Table 4 shows the logistic analysis results. In the simple regression model (Model 1), one unit increase in the lifestyle score was associated with 0.61 times decrease in the odds of having multimorbidity (crude OR: 0.6; 95% CI: 0.53–0.71). Four variables, including age, employment, education, and marital status, which showed significant associations with multimorbidity in the previous univariate analyses were entered into the regression models for further analysis (Model 2). After adjusting these variables, the association between lifestyle score and multimorbidity was strengthened (OR: 0.74, 96% CI: 0.63–0.87). The people with healthier lifestyles were observed to have low risk of multimorbidity. The results also showed that for younger people, the odds of developing multimorbidity was 0.09 times lower than for older adults (OR: 0.09; 95% CI: 0.03–0.22). The likelihood of multimorbidity among employment people was 0.31 times lower than among unemployed people (OR: 0.31; 95% CI: 0.17–0.55). When comparing the participants with multimorbidity and those without diseases (Model 3), healthier lifestyle was also less likely to have multimorbidity (OR: 0.75; 95% CI: 0.63–0.88). Those of a younger age (OR: 0.04; 95% CI: 0.01–0.10) and with employment (OR: 0.27; 95% CI: 0.15; 0.48) showed lower odds of developing multimorbidity. Similar results were found in Model 4 (comparing participants with multimorbidity vs. those with one chronic disease), where worse lifestyles (OR: 0.80; 95% CI: 0.68–0.95), older age (OR: 0.30; 95% CI: 0.11–0.79), and unemployment status (OR: 0.51; 95% CI: 0.26–0.99) all predicted high levels of multimorbidity. We also examined the association between multimorbidity and single lifestyle factor. The results are shown in the supplementary Table 1. It indicated that higher BMI and poorer sleep status were both related to a higher level of multimorbidity. No significant association was identified between multimorbidity and other individual factors.
Table 4.
Regression analyses of associations between lifestyle score and multimorbidity.
| Variable | Model 1 a | Model 2 b | Model 3 c | Model 4 d | ||||
|---|---|---|---|---|---|---|---|---|
| OR (95% CI) | p | OR (95% CI) | p | OR (95% CI) | p | OR (95% CI) | p | |
| Lifestyle score | 0.61 (0.53–0.71) | <0.001 | 0.74 (0.63–0.87) | <.001 | 0.75 (0.63–0.88) | .001 | 0.80 (0.68–0.95) | .011 |
| Age | ||||||||
| Young Adult(18–44) | 0.09 (0.03–0.22) | <.001 | 0.04 (0.01–0.10) | <.001 | 0.30 (0.11–0.79) | .01 | ||
| Middle Age (45–64) | 0.36 (0.18–0.73) | <.001 | 0.22 (0.10–0.48) | <.001 | 0.45 (0.21–0.97) | .04 | ||
| Elderly (≥65) | 1 (reference) | 1 (reference) | 1 (reference) | |||||
| Employment status | ||||||||
| Employed | 0.31 (0.17–0.55) | <.001 | 0.27 (0.15–0.48) | <.001 | 0.51 (0.26–0.99) | .05 | ||
| Unemployed | 1 (reference) | 1 (reference) | 1 (reference) | |||||
| Educational Level | ||||||||
| Primary Level or Lower | 2.38 (0.26–21.4) | .43 | 2.01 (0.20–20.25) | .55 | 2.27 (0.22–22.86) | .48 | ||
| Secondary School | 2.66 (0.34–20.79) | .34 | 3.27 (0.39–7.39) | .27 | 2.36 (0.26–21.04) | .43 | ||
| College | 1.75 (0.22–13.5) | .59 | 2.05 (0.24–17.02) | .5 | 1.80 (0.21–15.48) | .59 | ||
| Master and above | 1 (reference) | 1 (reference) | 1 (reference) | |||||
| Marital status | ||||||||
| Single | 0.59 (0.26–1.34) | .21 | 0.51 (0.22–1.16) | .11 | 0.92 (0.35–2.39) | .87 | ||
| Married/With partner | 1 (reference) | 1 (reference) | 1 (reference) | |||||
aModel 1 Simple logistic model, crude OR was obtained; independent variable (Y): participants with vs. without multimorbidity.
bModel 2 was adjusted for age, employment, education, and marital status; independent variable (Y): participants with vs. without multimorbidity.
cModel 3 was adjusted for age, employment, education and marital status; independent variable (Y): participants with multimorbidity vs. had no disease.
dModel 4 was adjusted for age, employment, education and marital status; independent variable (Y): participants with multimorbidity vs. have one disease.
Discussion
The current study found a relatively low prevalence of multimorbidity in a high-tech coastal city in China that had undergone rapid economic development. Among the sample participants, a healthier overall lifestyle score was associated with a lower level of multimorbidity. The most common chronic disease in the present study was hypertension. This result was consistent with that of a previous study conducted in Shenzhen (9.2%) 36 but was lower than the global prevalence of hypertension of 22%. 37 This finding could be due to the higher proportion of young residents in Shenzhen. According to the statistical yearbook, residents aged 60 or above accounted 6.99% of the total population in Shenzhen, which was lower than the national level of 13.34 percent points. 14 Thus, a low prevalence of hypertension was observed in our study. We selected the sample population from the Nanshan District, which is one of the ten administrative divisions of Shenzhen. Nanshan is the economic core of Shenzhen, where Fortune 500 companies operate such as Tencent, Da-Jiang Innovations, and more than 4,000 state-level high-tech enterprises. The sex ratio and age structure of population in Nanshan District are similar to the whole population in Shenzhen. The population sex ratio (male to female) in Shenzhen City is 113.1 and 110 in Nanshan District. The percentage of elderly people in Nanshan District is 3.67%, which is similar to the whole Shenzhen City. 38 Therefore, Nanshan is a representative district of Shenzhen City.
We generated an overall lifestyle score in our study to investigate the joint contribution of several typical lifestyle factors to variations in multimorbidity. This lifestyle score helped us quantify the composite effects of those lifestyle factors on the health status of the participants. Considering that life behavior is not an isolated issue, studying the impact of comprehensive lifestyle factors is more meaningful for policy makers and healthcare providers than focusing on individual factors. Previous studies have found that the overall lifestyle was associated with morbidity and mortality. Wakasugi’s study showed that one unit increase in lifestyle score was associated with 0.87 (95% CI: 0.81–0.94) times reduction in the odds of developing proteinuria among men. 39 Villegas’ and colleagues further confirmed the composite effects of protective lifestyle factors on the risk reduction of hypertension and dyslipidemia. 40 A large study (n = 71, 243) in China also demonstrated that healthier lifestyle contributes to lower mortality in women. 41 Contrarily, evidence suggested that people with multimorbidity are more likely to engage in negative lifestyle behaviors. For instance, a Scottish study showed that level of physical activity was lower in older people with multimorbidity than general older adults; only one third of them met the recommended amount of exercise.42,43 Another study among 22,684 Australian adults with chronic diseases found that 18% of the subjects experienced long-term risky drinking. 44 These pieces of evidence suggest that the relationship between multimorbidity and lifestyle could be reciprocal causation.
However, only a few Chinese people engaged in healthy amid the rapid social-economic transformation. One recent study showed that the prevalence of a healthy lifestyle among adults was very low, in which only 0.7% of participants followed a healthy lifestyle in all six aspects that were examined. 45 Previous studies indicated that people did not perceive healthy lifestyle behaviors to be important in the progression of an illness.46,47 In our study, we found that the people who had healthier lifestyles were more likely to have lower prevalence of multimorbidity. Using a simple and quantified way to educate people with or without multimorbidity the importance of modifying their lifestyle will benefit both individuals and the society. Using the composite lifestyle score to demonstrate the overall lifestyle status provides quantitative evidence for policymakers to advice people about adopting positive changes in lifestyle behaviors.
Our data supported the finding of a previous study that a higher BMI is associated with multimorbidity. 48 Urbanization and high technology use, such as ordering takeout food online (Jiang et al., 2019) and using a dishwasher and a sweeping robot (Jari Alshumrani, Yousef Alhazmi, Baloush, Aljohani, & Almutairi, 2020), may have contributed to an increase in obesity and a decrease in PA among the Shenzhen population. A review has shown that each increment of 2,000 steps per day up to 10,000 steps was associated with a 10% lower cardiovascular event rate. 49 A recent study showed that the prevalence of physical inactivity was 63.1% in Shenzhen. 50 A shortage of time and the lack of an appropriate environment may have contributed to such results. A promising approach to promoting PA in big cities is to build urban greenways. 51 Meanwhile, strengthening the use of electronic tools would be an optimal method. E-health plays a vital part in tailoring lifestyles to manage chronic disease using fitness trackers, remote monitors, and inventive strategies to prevent and delay the occurrence of comorbidity.52,53 Some comorbidities may prevent older people from engaging in more vigorous exercises. Therefore, light walking or trekking are types of physical activity that should be encouraged in this population. Sleep quality was another lifestyle factor linked with multimorbidity and was also shown in another Chinese study. 54 In our study, 700 participants reported poor sleep quality. Studies have shown that using electronic devices in the bedroom is linked to a later onset of sleep and can shorten sleep duration. Light exposure in a metropolis has also been linked to shorter sleep times and a later onset of sleep.55–57 Therefore, creating a positive environment to improve the sleep quality of people in big cities might be necessary in the future.
Smoking has also been consistently linked with the development of morbidity.19,48,58 Although the prevalence of smoking in Shenzhen was lower than the national level,59,60 efforts to reduce smoking in a metropolis such as Shenzhen should continue. Furthermore, electronic cigarettes are a new way of smoking that has increased over the past 5 years in China, especially among young adults. 61 As a young city, Shenzhen also needs to regulate electronic cigarettes to prevent chronic diseases.
Some demographic factors also contributed to the development of multimorbidity. Older age was a significant factor across studies.58,62,63 This finding indicates that additional years of life make people prone to developing other chronic conditions. 64 Our study also showed that the overall lifestyle score of older participants was lower than the score of younger participants. Therefore, promoting healthy living among old people is essential. Sex was not associated with multimorbidity in our sample, contradicting much of the literature, which found that females tend to have more comorbidities than men.19,65 A systematic review has shown that this finding was commonly reported across studies but is not consistent across studies. 64
Socioeconomic status is also key to the development of multimorbidities. Our study expressed this finding through the participants’ level of education, employment status, and family income. All of these factors have been linked to other comorbidities, particularly in the older population.62,66,67 In addition, our study found that people in the minimum family income group (less than 10,000 RMB monthly) follow a healthier lifestyle than the other groups. Those who do manual work tend to take public transportation. Both activities increased their level of physical activity compared with white-collar workers. By contrast, those in the median family income group tended to be white-collar workers who were more likely to drive a private car, which decreased their level of physical activity. Furthermore, long working hours and a high workload led to poor sleep quality for white-collar workers. These results suggest that health promotion messages should be targeted at older adults, retirees, middle-income people, and those with lower socioeconomic status (the unemployed and those with lower levels of education).
This study has some limitations. The cross-sectional design did not allow for assessing causality. Considering the high proportion of young people in this city, some sub-groups (i.e., the category of older people) had fewer participants. Caution is needed when interpreting the data. Nevertheless, the evidence from our study could provide useful information for health-related policy making and for the allocation of healthcare services in society. The findings could also serve as a reference for many similar cities in other countries.
Conclusions
The prevalence of multimorbidity was relatively low in Shenzhen, a city in south China. The typical chronic diseases in the sample population were hypertension, followed by hypocholesteremia, and osteoporosis. The findings may raise awareness among policymakers and healthcare providers regarding the importance of promoting an overall healthier lifestyle for residents, especially those with relatively weak lifestyle factors. Strengthening the management of chronic diseases in older and retired people in this city is essential. This study shows potential culturally appropriate targets for campaigns promoting a healthy lifestyle to minimize incidences of the premature development of non-communicable diseases and mortality.
Acknowledgements
We express our gratitude to the community nurses in Nanshan for their support.
Footnotes
Author Contribution: Conceptualization, YJX and A.M.; methodology, YJX and H.Y.; formal analysis, H.Y.; investigation, G.H.; data curation, M.W.; writing—original draft preparation, H.Y. and B.M.; writing—review and editing, YJX; supervision, YJX; project administration, A.M. All authors have read and agreed to the published version of the manuscript.
Declaration of conflicting interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This research was funded by the San-Ming Project in Nanshan District, Shenzhen.
Ethical approval: The study was conducted in accordance with the Declaration of Helsinki and approved by the Research Ethics Committee of the HUSTUSH and the Human Research Committee of the Hong Kong Polytechnic University (HSEARS20180521004 and July, 2017).
ORCID iDs
Hua-Lu Yang https://orcid.org/0000-0001-9029-7394
Yao Jie Xie https://orcid.org/0000-0001-9289-4985
References
- 1.Almirall J, Fortin M. The coexistence of terms to describe the presence of multiple concurrent diseases. J Comorb 2013; 3: 4–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Palladino R, Pennino F, Finbarr M, et al. Multimorbidity and health outcomes in older adults in ten European health systems, 2006-15. Health Aff (Millwood) 2019; 38(4): 613–623. [DOI] [PubMed] [Google Scholar]
- 3.Steffler M, Li Y, Weir S, et al. Trends in prevalence of chronic disease and multimorbidity in Ontario, Canada. Cmaj 2021; 193(8): E270–E277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Pati S, Swain S, Hussain MA, et al. Prevalence and outcomes of multimorbidity in South Asia: a systematic review. BMJ Open 2015; 5(10): e007235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Zhang L, Sun F, Li Y, et al. Multimorbidity in community-dwelling older adults in beijing: prevalence and trends, 2004-2017. J Nutr Health Aging 2021; 25(1): 116–119. [DOI] [PubMed] [Google Scholar]
- 6.Ferry FR, et al. Multimorbidity among persons aged 25-64 years: a population-based study of social determinants and all-cause mortality. J Public Health (Oxf) 2020; 7: 1–9. [DOI] [PubMed] [Google Scholar]
- 7.Sakib MN, Shooshtari S, St John P, et al. The prevalence of multimorbidity and associations with lifestyle factors among middle-aged Canadians: an analysis of Canadian longitudinal study on aging data. BMC Public Health 2019; 19(1): 243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bähler C., Huber CA, Brungger B, et al. Multimorbidity, health care utilization and costs in an elderly community-dwelling population: a claims data based observational study. BMC Health Serv Res 2015; 15: 23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Makovski TT, Schmitz S, Zeegers MP, et al. Multimorbidity and quality of life: systematic literature review and meta-analysis. Ageing Res Rev 2019; 53: 100903. [DOI] [PubMed] [Google Scholar]
- 10.Yadav UN, Ghimire S, Mistry SK, et al. Prevalence of non-communicable chronic conditions, multimorbidity and its correlates among older adults in rural Nepal: a cross-sectional study. BMJ Open 2021; 11(2): e041728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Geda NR, Janzen B, Pahwa P. Chronic disease multimorbidity among the Canadian population: prevalence and associated lifestyle factors. Arch Public Health 2021; 79(1): 60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Shao J, Wang X, Zou P, et al. Associating modifiable lifestyle factors with multimorbidity in community dwelling individuals from mainland China. Eur J Cardiovasc Nurs 2021; 20(6): 556–564. [DOI] [PubMed] [Google Scholar]
- 13.Hou B, Nazroo J, Banks J, et al. Are cities good for health? A study of the impacts of planned urbanization in China. Int J Epidemiol 2019; 48(4): 1083–1090. [DOI] [PubMed] [Google Scholar]
- 14.Statistics NBO . National bureau of statistics. 2020. http://www.stats.gov.cn/tjsj/ndsj/ [Google Scholar]
- 15.Yang M, Dijst M, Helbich M. Mental health among migrants in shenzhen, China: does it matter whether the migrant population is identified by hukou or birthplace? Int J Environ Res Public Health 2018; 15(12): 2671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Liu J, Cheng Y, Lau JTF, et al. The majority of the migrant factory workers of the light industry in Shenzhen, China may be physically inactive. PLoS One 2015; 10(8): e0131734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Yang X, You L, Jin D, et al. A community-based cross-sectional study of sleep quality among internal migrant workers in the service industry. Compr Psychiatry 2020; 97: 152154. [DOI] [PubMed] [Google Scholar]
- 18.Li X, Cai L, Cui Wl, et al. Association of socioeconomic and lifestyle factors with chronic non-communicable diseases and multimorbidity among the elderly in rural southwest China. J Public Health (Oxf) 2020; 42(2): 239–246. [DOI] [PubMed] [Google Scholar]
- 19.Fortin M, Haggerty J, Almirall J, et al. Lifestyle factors and multimorbidity: a cross sectional study. BMC Public Health 2014; 14: 686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.de Almeida MGN, Nascimento-Souza MA, Lima-Costa MF, et al. Lifestyle factors and multimorbidity among older adults (ELSI-Brazil). Eur J Ageing 2020; 17(4): 521–529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Krokstad S, Ding D, Grunseit AC, et al. Multiple lifestyle behaviours and mortality, findings from a large population-based norwegian cohort study - The HUNT study. BMC Public Health 2017; 17(1): 58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Zhang YB, Pan XF, Chen J, et al. Combined lifestyle factors, all-cause mortality and cardiovascular disease: a systematic review and meta-analysis of prospective cohort studies. J Epidemiol Community Health 2021; 75(1): 92–99. [DOI] [PubMed] [Google Scholar]
- 23.Municipality SBOS . Statistics bureau of shenzhen municipality, 2020. [Google Scholar]
- 24.Zhou M, Wang H, Zeng X, et al. Mortality, morbidity, and risk factors in China and its provinces, 1990-2017: a systematic analysis for the global burden of disease study 2017. Lancet 2019; 394(10204): 1145–1158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Claudia D, Klaus B, Bartels DBJJOG. The measurement of multiple chronic diseases--a systematic review on existing multimorbidity indices. Journals of Gerontology 2011; 66(3): 301–311. [DOI] [PubMed] [Google Scholar]
- 26.Bassett DR, Jr. International physical activity questionnaire: 12-country reliability and validity. Med Sci Sports Exerc 2003; 35(8): 1396. [DOI] [PubMed] [Google Scholar]
- 27.Macfarlane DJ, Lee CC, Ho EY, et al. Reliability and validity of the Chinese version of IPAQ (short, last 7 days). J Sci Med Sport 2007; 10(1): 45–51. [DOI] [PubMed] [Google Scholar]
- 28.Buysse DJ, Reynolds CF, Monk TH, et al. The pittsburgh sleep quality index: a new instrument for psychiatric practice and research. Psychiatry Res 1989; 28(2): 193–213. [DOI] [PubMed] [Google Scholar]
- 29.Tsai PS, Wang SY, Wang MY, et al. Psychometric evaluation of the Chinese version of the pittsburgh sleep quality index (CPSQI) in primary insomnia and control subjects. Qual Life Res 2005; 14(8): 1943–1952. [DOI] [PubMed] [Google Scholar]
- 30.Caterson ID, Inoue S, Zimmet PZJWIOA. The Asia-pacific perspective: redefining obesity and its treatment, 2000. [Google Scholar]
- 31.Nyberg ST, Singh-Manoux A, Pentti J, et al. Association of healthy lifestyle with years lived without major chronic diseases. JAMA Intern Med 2020; 180(5): 760–768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.DiPietro L, Al-Ansari SS, Biddle SJH, et al. Advancing the global physical activity agenda: recommendations for future research by the 2020 WHO physical activity and sedentary behavior guidelines development group. Int J Behav Nutr Phys Act 2020; 17(1): 143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Gordis EJA. National Institute on Alcohol Abuse and Alcoholism 2010; 83(5): 483–493. [DOI] [PubMed] [Google Scholar]
- 34.Goel S, Sharma A. AJCCR Garg. Effect of Alcohol Consumption on Cardiovascular Health 2018; 20(4): 19. [DOI] [PubMed] [Google Scholar]
- 35.Traversy G. Chaput JPJCOR. Alcohol Consumption and Obesity: An Update 2015; 4(1): 122–130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Luo B, Chen H, Dong J. The prevalence of hepertension and associated factors among middle-age adults in Shenzhen. Laboratory Medicine and Clinic 2014; 11: 19. [Google Scholar]
- 37.Alwan A. Global status report on noncommunicable diseases, 2014. [Google Scholar]
- 38.Shenzhen Statistical Yearbook . 2020; Available from: http://tjj.sz.gov.cn/zwgk/zfxxgkml/tjsj/tjnj/content/post_8386382.html
- 39.Wakasugi M, Kazama J, Narita I, et al. Association between overall lifestyle changes and the incidence of proteinuria: a population-based, cohort study. Intern Med 2017; 56(12): 1475–1484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Villegas R, Kearney PM, Perry IJ. The cumulative effect of core lifestyle behaviours on the prevalence of hypertension and dyslipidemia. BMC Public Health 2008; 8: 210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Nechuta SJ, Shu XO, Li HL, et al. Combined impact of lifestyle-related factors on total and cause-specific mortality among Chinese women: prospective cohort study. PLoS Med 2010; 7(9): e1000339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Salman A, Sellami M. Do older adults with multimorbidity meet the recommended levels of physical activity? An analysis of scottish health survey. Int J Environ Res Public Health 2019; 16(19): 3748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Sun F, Norman IJ, While AE. Physical activity in older people: a systematic review. BMC Public Health 2013; 13: 449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Pham TTL, Callinan S, Livingston M. Patterns of alcohol consumption among people with major chronic diseases. Aust J Prim Health 2019; 25(2): 163–167. [DOI] [PubMed] [Google Scholar]
- 45.Zhu NB, Zhou M, Yu CQ, et al. [Prevalence of ‘healthy lifestyle’ in Chinese adults]. Zhonghua Liu Xing Bing Xue Za Zhi 2019; 40(2): 136–141. [DOI] [PubMed] [Google Scholar]
- 46.De Bacquer D, Astin F, Kotseva K, et al. Poor adherence to lifestyle recommendations in patients with coronary heart disease: results from the EUROASPIRE surveys. Eur J Prev Cardiol 2021; 29: 383–395. [DOI] [PubMed] [Google Scholar]
- 47.Dolan HR, Alvarez AA, Freylersythe SJ, et al. Barriers and facilitators for adopting a healthy lifestyle among latina cancer survivors: a qualitative descriptive study. Support Care Cancer 2021; 30: 2649–2659. [DOI] [PubMed] [Google Scholar]
- 48.Katikireddi SV, Skivington K, Leyland AH, et al. The contribution of risk factors to socioeconomic inequalities in multimorbidity across the lifecourse: a longitudinal analysis of the Twenty-07 cohort. BMC Med 2017; 15(1): 152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Kraus WE, Powell KE, Haskell WL, et al. Physical activity, all-cause and cardiovascular mortality. And Cardiovascular Disease 2019; 51(6): 1270–1281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Zhou Y, Wu J, Zhang S, et al. Prevalence and risk factors of physical inactivity among middle-aged and older Chinese in Shenzhen: a cross-sectional study. BMJ Open 2018; 8(10): e019775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Frank LD, Hong A, Ngo VD. Causal evaluation of urban greenway retrofit: a longitudinal study on physical activity and sedentary behavior. Prev Med 2019; 123: 109–116. [DOI] [PubMed] [Google Scholar]
- 52.Jiménez-Muñoz L, Gutierrez-Rojas L, Porras-Segovia A, et al. Mobile applications for the management of chronic physical conditions: a systematic review. Intern Med J 2020; 52(1): 21–29. [DOI] [PubMed] [Google Scholar]
- 53.Omboni S, Panzeri E, Campolo L, E-Health. Hypertension management: an insight into the current and future role of blood pressure telemonitoring. Curr Hypertens Rep 2020; 22(6): 42. [DOI] [PubMed] [Google Scholar]
- 54.Wu W, Wang W, Dong Z, et al. Sleep quality and its associated factors among low-income adults in a rural area of China: a population-based study. Int J Environ Res Public Health 2018; 15(9): 2055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Martins AJ, Isherwood CM, Vasconcelos SP, et al. The effect of urbanization on sleep, sleep/wake routine, and metabolic health of residents in the amazon region of Brazil. Chronobiol Int 2020; 37(9–10): 1335–1343. [DOI] [PubMed] [Google Scholar]
- 56.Pilz LK, Levandovski R, Oliveira MAB, et al. Sleep and light exposure across different levels of urbanisation in Brazilian communities. Sci Rep 2018; 8(1): 11389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Cain SW, McGlashan EM, Vidafar P, et al. Evening home lighting adversely impacts the circadian system and sleep. Sci Rep 2020; 10(1): 19110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Singh PK, Singh L, Dubey R, et al. Socioeconomic determinants of chronic health diseases among older Indian adults: a nationally representative cross-sectional multilevel study. BMJ Open 2019; 9(9): e028426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Mou J, Fellmeth G, Griffiths S, et al. Tobacco smoking among migrant factory workers in Shenzhen, China. Nicotine Tob Res 2013; 15(1): 69–76. [DOI] [PubMed] [Google Scholar]
- 60.Li H, Yan X, Deng X, et al. Magnitude of and gender differences in cardiovascular risk profiles among community residents in Shenzhen, China. Public Health 2017; 147: 59–65. [DOI] [PubMed] [Google Scholar]
- 61.Xiao L, et al. Awareness and prevalence of e-cigarette use among Chinese adults: policy implications. Tob Control, 2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Barnett K, Mercer SW, Norbury M, et al. Epidemiology of multimorbidity and implications for health care, research, and medical education: a cross-sectional study. Lancet 2012; 380(9836): 37–43. [DOI] [PubMed] [Google Scholar]
- 63.Kingston A, Robinson L, Booth H, et al. Projections of multi-morbidity in the older population in England to 2035: estimates from the population ageing and care simulation (PACSim) model. Age Ageing 2018; 47(3): 374–380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Violan C, Foguet-Boreu Q, Flores-Mateo G, et al. Prevalence, determinants and patterns of multimorbidity in primary care: a systematic review of observational studies. PLoS One 2014; 9(7): e102149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.de Carvalho JN, de Camargo Cancela M, de Souza DLB. Lifestyle factors and high body mass index are associated with different multimorbidity clusters in the Brazilian population. PLoS One 2018; 13(11): e0207649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Marengoni A, Winblad B, Karp A, et al. Prevalence of chronic diseases and multimorbidity among the elderly population in Sweden. Am J Public Health 2008; 98(7): 1198–1200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Singer L, Green M, Rowe F, et al. Social determinants of multimorbidity and multiple functional limitations among the ageing population of England, 2002-2015. SSM Popul Health 2019; 8: 100413. [DOI] [PMC free article] [PubMed] [Google Scholar]