Abstract
Objective
Epipericardial fat necrosis (EFN) has been considered to be a rare cause of acute chest pain, and especially important for emergency physicians. Chest computed tomography (CT) is often used for the diagnosis of EFN after excluding life-threatening states, such as acute coronary syndrome and pulmonary embolism. While the proportion of EFN patients who underwent chest CT in emergency departments is being clarified, little is still known about other departments in Japan. To investigate the proportion of EFN patients who underwent chest CT for acute chest pain in various departments.
Methods
Chest CT performed from January 2015 to July 2020 in Asahikawa Medical University Hospital in Japan was retrospectively analyzed in this study. All images were reviewed by two radiologists.
Results
There were 373 outpatients identified by a search using the word ‘chest pain’ who underwent chest CT. Eight patients satisfying the imaging criteria were diagnosed with EFN. The proportions of patients diagnosed with EFN were 10.7%, 4.8%, 2.8%, 0.9% and 0% in the departments of general medicine, cardiovascular surgery, emergency medicine, cardiovascular internal medicine and respiratory medicine, respectively. Only 12.5% of the patients were correctly diagnosed with EFN, and the other patients were treated for musculoskeletal symptoms, acute pericarditis or hypochondriasis.
Conclusion
EFN is not rare and is often overlooked in various departments. All physicians as well as emergency physicians should consider the possibility of EFN as the cause of pleuritic chest pain.
Keywords: pleuritic chest pain, epipericardial fat necrosis, chest CT, emergency medicine
Introduction
Epipericardial fat necrosis (EFN) is thought to be a very rare cause of chest pain. The first case of EFN was reported in 1957 by Jackson et al. (1) and to our knowledge, about 50 cases have been reported around the world.
Until early 2005, surgical removal was a common treatment, but it is now recommended that patients be followed without any invasive procedure, as EFN has a benign, self-limiting nature (2). Non-steroidal anti-inflammatory drugs are often used for the treatment of symptoms. Although the precise mechanisms remain unknown, bleeding from a fragile vessel due to increased pressure caused by Valsalva's maneuver, acute torsion of fat pedicle and structural anomalies of tissue, such as lipoma, may be involved in the pathogenesis of EFN (3).
Chest computed tomography (CT) should be performed for the diagnosis of EFN after life-threatening states, such as acute coronary syndrome and pulmonary embolism, have been excluded. The typical CT finding of EFN is a round, soft-tissue attenuation lesion with varying degrees of peripheral strands with or without a fatty center located in the epipericardial fat (4). Follow-up imaging after a few months is needed to exclude neoplastic diseases. With the development of image diagnostic technology, many cases of EFN have recently been reported by radiologists. The number of case reports in the field of emergency medicine has also recently been increasing because most patients with EFN visit an emergency department first (5). However, EFN is still not widely recognized and may therefore be frequently overlooked.
We herein report the proportion of EFN patients who underwent chest CT for acute chest pain in various departments to promote more awareness of the possibility of EFN in daily medical practice.
Materials and Methods
The present investigation was approved by the institutional ethics committee. Informed consent was obtained in the form of opt-out on a dedicated website. Instances of chest CT performed from January 2015 to July 2020 at Asahikawa Medical University Hospital, Japan were retrospectively analyzed in this study. All images were reviewed by two radiologists who were blinded to the clinical features.
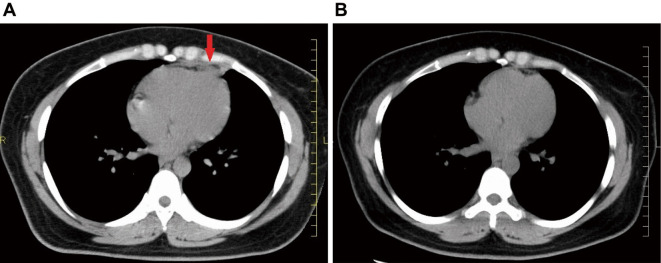
Lesions characterized as an ovoid lesion with total fat attenuation surrounded by intense stranding or an ovoid lesion with mixed fat-soft tissue attenuation with little stranding (6) (Fig. 1A) were diagnosed as EFN. Laboratory and physiological data, including data for white blood cell (WBC), creatine kinase (CK), CK-muscle brain (CK-MB), C-reactive protein (CRP), D-dimer and electrocardiograph (ECG), were obtained. Information on the departments the patients first visited (general medicine, cardiovascular surgery, cardiovascular internal medicine, respiratory medicine or emergency medicine) was also obtained.
Figure 1.
Chest CT diagnosed as EFN (patient No. 7). A: Chest CT shows an increased CT value of the epipericardial fat (red arrow) at the left cardiophrenic angle. B: Follow-up chest CT after two months showed drastic resolution in the necrotic area.
Results
There were 373 outpatients (192 men and 181 women) identified by a search using the word ‘chest pain’ who underwent chest CT during the period from January 2015 to July 2020. The mean age of the patients was 63.7±20.9 years old. Eight outpatients (4 men and 4 women) satisfying the imaging criteria were diagnosed with EFN. EFN tended to occur in young men, while it occurred at various ages in women (Table). EFN findings on CT performed for chest pain were detected in 4.8%, 2.8%, 0.9% and 0% of outpatients in the departments of cardiovascular surgery, emergency medicine, cardiovascular internal medicine and respiratory medicine, respectively, and there were EFN findings in 10.7% of outpatients in the Department of General Medicine (Fig. 2). As shown in Table, only 1 (12.5%) of the 8 patients was correctly diagnosed, and the other patients were diagnosed with musculoskeletal system pain (Patients 2, 4, 6 and 8), acute pericarditis (Patients 3 and 5) and hypochondriasis (Patient 1). All patients except for Patient 1 complained of pleuritic pain. Patient 1 had been suffering from dementia. Five of the eight patients showed inflammatory reactions on laboratory data. Elevation of D-dimer levels was observed in 57% of the patients. Although 25% of the patients showed a slight elevation of CK, the values of CK-MB were within the normal range in all patients. One patient showed ST-T elevation on an ECG but returned to a normal state after one month. Follow-up CT was performed in three patients. All of those patients showed the drastic resolution of the necrotic area, as shown in Fig. 1B.
Table.
Clinical and Laboratory Data of Patients with Epipericardial Fat Necrosis.
| Case No. | Gender (F/M) | Age (years) | Department of first contact | Sympton duration | Pain | Clinical course | WBC (/µL) | CRP (mg/dL) | CK (U/L) | CK-MB (U/L) | D-dimer (µg/mL) | ECG | Diagnosis |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Normal | 3,500-8,500 | 0.10< | 24-170 | 12< | 0-0.50 | ||||||||
| 1 | F | 87 | Emergency department | 1.5 h | Unknown Recurrent |
No treatment Unknown course |
5,840 | 61 | 3 | 1.6↑ | None | Hypochondriasis | |
| 2 | F | 31 | Cardiovascular internal medicine | Unknown | Pleuritic Recurrent |
No treatment Unknown course |
8,520↑ | 0.10< | 49 | 0.50< | None | Intercostal pain | |
| 3 | F | 53 | Emergency department | 4 h | Pleuritic Recurrent |
NSAIDs Improvement |
9,470↑ | 1.73↑ | 58 | 2 | 0.77↑ | None | Acute pericarditis |
| 4 | M | 16 | General medicine | 5 days | Pleuritic Recurrent |
No treatment Improvement |
6,100 | 0.10< | 235↑ | 3 | 0.58↑ | None | Costal cartilage pain |
| 5 | M | 25 | General medicine | 5 days | Pleuritic Recurrent |
Aspirin and colchicine Improvement |
8,780↑ | 13.7↑ | 23 | 1 | 1.1↑ | ST elevation | Acute pericarditis |
| 6 | M | 17 | Cardiovascular surgery | 2 days | Pleuritic Recurrent |
Acetaminophen Unknown course |
5,420 | 1.69↑ | 201↑ | 11 | 0.50< | None | Costal cartilage pain |
| 7 | F | 30 | General medicine | 24 h | Pleuritic Recurrent |
NSAIDs Improvement |
7,930 | 0.10< | 54 | 1 | None | EFN | |
| 8 | M | 22 | Emergency department | 8 h | Pleuritic Recurrent |
NSAIDs Improvement |
8,940↑ | 0.1 | 17 | 5< | 0.50< | None | Costal cartilage pain |
WBC: white blood cell, CRP: c-reactive protein, CK: creatine phosphokinase, CK-MB: creatine phosphokinase muscle brain type, ECG: electrocardiogram, EFN: epipericardial fat necrosiss, NSAID: non steroidal anti-inflammatory drug
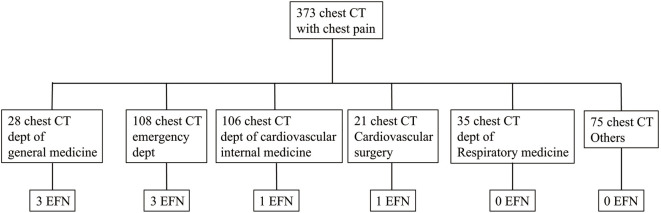
Figure 2.
The number of patients diagnosed with epipericardial fat necrosis in each department. Eight outpatients satisfying the imaging criteria were diagnosed with EFN. EFN findings were shown in three, three, one, one and no outpatients in the departments of general medicine, emergency medicine, cardiovascular internal medicine, cardiovascular surgery and respiratory medicine, respectively.
Discussion
This study was carried out to determine the clinical characteristic of EFN and to clarify the departments that EFN patients visited first and the frequency of misdiagnoses. The incidence of EFN in patients in whom chest CT was performed for chest pain in the emergency department was 2.8%, which is similar to that reported by Giassi et al. (4). While there were EFN findings on CT performed for chest pain in 4.8%, 0.9%, 0% and 0% of outpatients in the departments of cardiovascular surgery, cardiovascular internal medicine, respiratory medicine and other departments, respectively, there were EFN findings in 11% of outpatients who visited the Department of General Medicine (Fig. 2), which is much higher than that expected. It is notable that not all of the EFN patients complained of severe acute chest pain, that patients with pain of a manageable level tended to visit various departments and that only 35% of EFN patients visited the emergency department first. To our knowledge, this is the first study to evaluate the clinical characteristics of EFN patients with a focus on various departments in addition to the emergency department.
With regard to the age or sex of EFN patients, Giassi et al. reported their findings from an emergency department in Brasil. According to their report, 8 out of 11 EFN cases were men, and the age in 6 of those 8 men was 40-49 years old. The remained 2 men were 24 and 80 years old. In contrast, 3 cases in women were reported (23, 52 and 59 years old). The present study in Japan reported 4 men out of 8 EFN cases, with ages of 16, 17, 22 and 25 years old, suggesting EFN tends to be observed at much younger ages in men than in women. Thus, the age and sex distributions of EFN in this study were quite different from the findings in Brasil. This difference may be associated with race. To strengthen the limited information and further clarify the epidemiology of EFN in Japan, a large-scale study should be performed.
The values of laboratory tests are usually normal, but increases in the levels of D-dimer, CRP and/or WBC count are often found in EFN patients (7), as was seen in our patients. ECG findings are also usually normal, but non-specific ST-T wave changes have been reported (3), as were found in Patient 5 in our study.
The overlooked cases in our study were diagnosed with musculoskeletal symptoms, acute pericarditis or hypochondriasis, and only one case was diagnosed correctly due to the radiologist's comments. These results suggest that EFN is often overlooked, and there is a need for more awareness of the possibility of EFN in daily medical practice. Giassi et al. showed that disseminating knowledge on the clinical entity was able to increase the rate of EFN diagnoses (8).
Several limitations associated with the present study warrant mention. Because most cases were overlooked, we were only able to check follow-up CT findings in three of the eight EFN patients. Not all of the values of tests were obtained, since this study was a retrospective study. To strengthen the limited information and further clarify the epidemiology of EFN in Japan, a large-scale study should be performed. Accumulating evidence has shown that artificial intelligence (AI) may have marked power for diagnosing issues based on clinical imaging (9,10). We are looking forward to increasing the accuracy of EFN diagnoses using AI-assisted CT in the clinical setting in near future.
Conclusion
EFN is not very rare and is often overlooked in various departments. Therefore, all physicians as well as emergency physicians should consider the possibility of EFN as the cause of acute pleuritic chest pain.
The authors state that they have no Conflict of Interest (COI).
References
- 1.Jackson RC, Clagett OT, McDonald JR. Pericardial fat necrosis; report of three cases. J Thorac Surg 33: 723-729, 1957. [PubMed] [Google Scholar]
- 2.Pineda V, Caceres J, Andreu J, Vilar J, Domingo ML. Epipericardial fat necrosis: radiologic diagnosis and follow-up. AJR Am J Roentgenol 185: 1234-1236, 2005. [DOI] [PubMed] [Google Scholar]
- 3.Baig A, Campbell B, Russell M, Singh J, Borra S. Epicardial fat necrosis: an uncommon etiology of chest pain. Cardiol J 19: 424-428, 2012. [DOI] [PubMed] [Google Scholar]
- 4.Giassi K de S, Costa AN, Bachion GH, et al. Epipericardial fat necrosis: an underdiagnosed condition. Br J Radiol 87: 20140118, 2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Reich B, Edlow J. A 57-year-old man with right-sided chest pain. J Emerg Med 52: e167-e168, 2017. [DOI] [PubMed] [Google Scholar]
- 6.Giassi KS, Costa AN, Bachion GH, Kairalla RA, Filho JRP. Epipericardial fat necrosis: who should be a candidate? AJR Am J Roentgenol 207: 773-777, 2016. [DOI] [PubMed] [Google Scholar]
- 7.Mortensen SG, Buchmann P, Lappegard KT. Epipericardial fat necrosis: a case report and a review of the literature. Clin Med Insights Case Rep 13: 1179547620940769, 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Giassi KS, Costa AN, Kairalla RA, Parga Filho JR. Epipericardial fat necrosis: increasing the rate of diagnosis by disseminating knowledge within a single institution. Radiol Bras 51: 62-63, 2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Yen A, Pfeffer Y, Blumenfeld A, et al. Use of a dual artificial intelligence platform to detect unreported lung nodules. J Comput Assist Tomogr 45: 318-322, 2021. [DOI] [PubMed] [Google Scholar]
- 10.Ather S, Kadir T, Gleeson F. Artificial intelligence and radiomics in pulmonary nodule management: current status and future applications. Clin Radiol 75: 13-19, 2020. [DOI] [PubMed] [Google Scholar]