Abstract
Background
Total Knee Arthroplasty (TKA) is a common orthopaedic surgery to treat advanced knee arthritis. Post-operative complications can be affected by obesity, defined as a body mass index of 30 kg/m2 or higher. We examine the rates of specific complications, revision rates, and costs of care following TKA and compare them between multifactor matched obese and non-obese patients. We hypothesize these outcomes will be worse in obese patients than in non-obese patients.
Methods
This retrospective study of the PearlDiver database queries for patients who underwent TKA under Current Procedural Terminology (CPT) and International Statistical Classification of Diseases (ICD-9) codes between January 2011 and January 2020. Patients were matched based on age, gender, and comorbidity indices, and various complications, revision rates, and costs were compared between the matched obese and non-obese patient groups.
Results
Obesity was associated with higher rates of surgical complications, such as wound complications, surgical site infections, need for revision, and higher total cost of care one year after TKA, and medical complications such as, acute kidney injury, deep vein thrombosis, urinary tract infection, and narcotics use, but significantly lower rates of anemia, arrhythmia, cardiac arrest, pneumonia, and transfusion. Obese patients also experienced significantly lower drug costs of care.
Conclusion
Outcomes were not definitively worse in obese patients when compared to matched non-obese patients. Nevertheless, understanding the complications that can arise following TKA will assist in educating patients about potential risks from surgery and guide surgeons in caring for their patients as obesity is predicted to continue increasing in prevalence. As such, future studies should examine underlying mechanisms that cause these complications to develop potential therapies.
Keywords: Obesity, Complications, Total knee arthroplasty, Comparison, Retrospective database
1. Background
Total Knee Arthroplasty (TKA) is projected to increase to almost 1.3 million arthroplasties done in 2025 in the United States alone, a 110% growth compared to 2014.1 While TKA has a high success rate, complications can create a larger burden on the healthcare system, perhaps even requiring a revision.2,3 Obesity, defined as a body mass index (BMI) of 30 kg/m2 or higher, has globally increased by 27.5% in adults over the last 30 years.4 As obesity continues to increase, there will be a substantial need for safe, effective TKA with minimal complications and associated cost. Obesity will cause damage to bones and surrounding soft tissues both biochemically and biomechanically.11 While obesity is a risk factor for osteoarthritis specifically,5 it can also have extensive impacts on kidney to cardiovascular health.6 Because of these widespread effects, the specific function obesity has in post-operative outcomes and complication rates after TKA is controversial and requires further investigation.12 We theorize obese patients will have higher rates of complications and higher costs, thereby having worse outcomes, following TKA.
To the best of our knowledge, no TKA study has examined as extensive of a list of post-operative complications in a large, multicenter, matched cohort of patients with and without obesity. We aimed to investigate specific post-operative complications, along with revision rate and treatment costs between these two groups. We hypothesize that patients with obesity would have worse outcomes than patients without obesity.
2. Materials and methods
2.1. Data source and study population
This retrospective study queried the PearlDiver Patient Records Database (www.pearldiverinc.com, Colorado Springs, CO, USA) for all patients who underwent a TKA using Current Procedural Terminology (CPT) and International Statistical Classification of Diseases (ICD-9) codes between January 2011 and January 2020. The PearlDiver database contains hospital and physician billing, and prescription medication records for more than 91 million distinct patients from all U.S. states and territories and from a broad range of payer types, such as commercial insurance, Medicare, Medicaid, self-pay, and other databases like the National Inpatient Sample. Patient information from all sources is de-identified and compliant with the Health Insurance Portability and Affordability Act (HIPAA). As such, the study did not require review by our institutional review board (IRB).
We included patients who underwent TKA during the period specified above, based on CPT-27447 and ICD-9-P-8154 codes, both coding for TKA, who also maintained at least one year of post-operative follow up in the PearlDiver database. Patients with no medical records at least one year prior and one year following TKA were excluded from the study. Patients were then further divided based on whether they were also diagnosed with obesity.
2.2. Patient characteristics
Patients were studied based on the following characteristics: age, gender, Charlson Comorbidity Index (CCI), Elixhauser Comorbidity Index (ECI), and length of stay. Both CCI and ECI are reliable, frequently used predictors of long-term prognosis and survival, estimating the risk of death from comorbidities.7 It has been reported that ECI is more appropriate for predicting death after orthopaedic surgery in in-patient settings.8 Due to the fact that these comorbidities increase the risk for peri- and post-operative complications, we sought to compare our two groups with the CCI and ECI.
Bellwether-PearlDiver was used to generate propensity-matched populations from both obese and non-obese patients based on age, gender, CCI, and ECI. The software randomly selected patients to be included into each group while maintaining that the groups had the same age, gender, CCI, and ECI distributions. This resulted in each group having the same number of patients with similar age, gender, CCI, and ECI distributions (n = 118382 for each group) based on CPT-27447. Additionally, data on length of stay and total and drug costs of care were calculated using ICD-9 codes and not CPT codes. A similarly matched but smaller group (n = 60887 for each group) based on ICD-9-P-8154 was examined. As demonstrated in Table 1, the mean age, percentage of males and comorbidity indices were very similar between CPT and ICD-9 codes.
Table 1.
TKA patient characteristics.
| Obesity | Non-obesity | |
|---|---|---|
| CPT codes | ||
| Age (y), mean (SD) | 66.27 (8.31) | 66.49 (8.35) |
| Male, N (%) | 45259 (38.23) | 45259 (38.23) |
| CCI, mean (SD) | 1.51 (1.84) | 1.50 (1.83) |
| ECI, mean (SD) | 4.30 (2.74) | 4.27 (2.74) |
| ICD-9 codes | ||
| Age (y), mean (SD) | 66.31 (8.01) | 66. 53 (8.08) |
| Male, N (%) | 23161 (38.03) | 23161 (38.03) |
| CCI, mean (SD) | 1.55 (1.82) | 1.54 (1.81) |
| ECI, mean (SD) | 4.21 (2.50) | 4.18 (2.49) |
| length of stay (d), mean (SD) | 3.02 (1.4) | 3.08 (2.08) |
2.3. Post-operative complications
The following post-operative complications were assessed between the two groups over the time spans of 30 days, 90 days, and one year: dislocation, surgical site infection (SSI), myocardial infarction (MI), anemia, arrhythmia, congestive heart failure (CHF), acute kidney injury (AKI), cardiac arrest, deep venous thrombosis (DVT), wound complication (WC), hematoma, pneumonia, pulmonary embolism (PE), blood transfusion, urinary tract infection (UTI), and opioid prescription. These complications were chosen to be examined before data collection began. The odds ratio of complications for each group were calculated and compared, along with the 95% confidence intervals and p value for each complication.
2.4. Total and drug costs of care
Both the total and drug costs of care were calculated over the time spans of 30 days, 90 days, and one year. The means and standard deviations of the total cost and drug cost of both groups were then calculated and compared, along with the 95% confidence intervals and p value for the difference between the two groups for each span of time.
2.5. Statistical methods
Patient characteristics were described using mean (standard deviation) for continuous variables and frequency (proportion) for categorical variables where appropriate. Two-independent sample t-test for unequal variances (continuous variables) and test of significance was used to identify any differences between the two groups. Rates of complication in the obese group were compared with those in the non-obese group. Statistical analyses were performed using MedCalc's Odds Ratio Calculator and MedCalc's Comparison of Means Calculator.9,10 Statistical significance was defined as p < .05.
3. Results
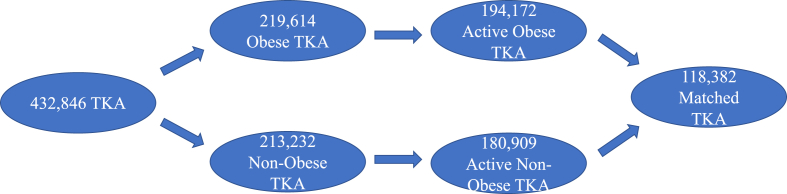
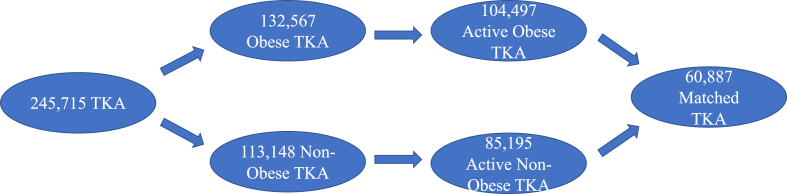
432,846 patients underwent TKA during this nine-year period based on CPT codes and 219,614 (51%) had a comorbidity of obesity. However, only 194,172 (obese) and 180,909 (non-obese) had records with a minimum of one year prior and following TKA. These two patient populations were matched to have 118,382 patients in each group, with the remaining patients from both groups excluded from the study [Fig. 1]. As demonstrated in Table 1, the mean age was 66 years, 38% of the patients were male, the mean CCI was 1.5, and the mean ECI was 4.3. When using ICD-9 codes, 245,715 patients underwent TKA during this 9-year period 132,567 (54%) had a comorbidity of obesity. However, only 104,497 (obese) and 85,195 (non-obese) had records a minimum of one year prior and after TKA. Then those two patient populations were group matched to have 60,887 patients in each group, with the remaining patients from both groups excluded from the study [Fig. 2]. Between the matched groups, the mean age was 66 years, 38% of the patients were male, the mean CCI was 1.5, the mean ECI was 4.2, and the length of stay was 3.02 and 3.08 days for obese and non-obese patients, respectively [Table 1].
Fig. 1.
Patient selection schematic based on CPT-27447.
Fig. 2.
Patient selection schematic based on ICD-9-P-8154.
During the first 30 postoperative days, obese patients experienced significantly higher rates of SSI, AKI, DVT, WC, hematoma, UTI, and narcotics use compared to non-obese patients. The rates of cardiac arrest, pneumonia, and transfusion, however, were significantly lower for obese than non-obese patients after 30 days. In the first 90 days after TKA, obese patients still had significantly higher odds of experiencing SSI, AKI, DVT, WC, UTI, and narcotics use. Anemia, arrhythmia, cardiac arrest, pneumonia, and transfusion were significantly decreased in obese patients. One year following TKA, obese patients continued to have a significantly higher odds of experiencing SSI, AKI, DVT, WC, UTI, and narcotics use, but also significantly higher chance of MI and hematoma. Finally, anemia, arrhythmia, cardiac arrest, pneumonia, and transfusions were all significantly lower in obese patients than in non-obese patients [Table 2].
Table 2.
Odds ratio of complications after TKA.
| Obesity | Non-obesity | Odds ratio | Lower CI | Upper CI | P value | |
|---|---|---|---|---|---|---|
| 30 days after TKA | ||||||
| Dislocation N (%) | 43 (0) | 31 (0) | 1.387 | 0.874 | 2.202 | 0.1648 |
| SSI N (%) | 982 (0.008) | 861 (0.007) | 1.142 | 1.042 | 1.252 | 0.0047 |
| MI N (%) | 963 (0.008) | 893 (0.008) | 1.079 | 0.985 | 1.182 | 0.1029 |
| Anemia N (%) | 1195 (0.01) | 1286 (0.011) | 0.929 | 0.858 | 1.005 | 0.0663 |
| Arrhythmia N (%) | 7024 (0.059) | 7246 (0.061) | 0.967 | 0.935 | 1.001 | 0.0552 |
| CHF N (%) | 1245 (0.011) | 1292 (0.011) | 0.963 | 0.891 | 1.042 | 0.3482 |
| AKI N (%) | 2061 (0.017) | 1577 (0.013) | 1.312 | 1.228 | 1.402 | < 0.0001 |
| Cardiac arrest N (%) | 63 (0.001) | 102 (0.001) | 0.617 | 0.451 | 0.845 | 0.0026 |
| DVT N (%) | 495 (0.004) | 392 (0.003) | 1.264 | 1.107 | 1.443 | 0.0005 |
| WC N (%) | 763 (0.006) | 556 (0.005) | 1.375 | 1.232 | 1.534 | < 0.0001 |
| Hematoma N (%) | 559 (0.005) | 486 (0.004) | 1.151 | 1.019 | 1.3 | 0.0237 |
| Pneumonia N (%) | 907 (0.008) | 1066 (0.009) | 0.850 | 0.777 | 0.929 | 0.0003 |
| PE N (%) | 616 (0.005) | 587 (0.005) | 1.050 | 0.937 | 1.176 | 0.4019 |
| Transfusion N (%) | 2135 (0.018) | 2799 (0.024) | 0.758 | 0.717 | 0.803 | < 0.0001 |
| UTI N (%) | 2767 (0.023) | 2492 (0.021) | 1.113 | 1.054 | 1.176 | 0.0001 |
| Narcotics Use N (%) | 84015 (0.71) | 82493 (0.697) | 1.064 | 1.045 | 1.083 | < 0.0001 |
| 90 days after TKA | ||||||
| Dislocation N (%) | 78 (0.001) | 88 (0.001) | 0.886 | 0.653 | 1.202 | 0.4378 |
| SSI N (%) | 1516 (0.013) | 1352 (0.011) | 1.123 | 1.043 | 1.209 | 0.0021 |
| MI N (%) | 1473 (0.012) | 1410 (0.012) | 1.045 | 0.971 | 1.125 | 0.2378 |
| Anemia N (%) | 1506 (0.013) | 1617 (0.014) | 0.930 | 0.867 | 0.999 | 0.0456 |
| Arrhythmia N (%) | 9140 (0.077) | 9825 (0.083) | 0.924 | 0.897 | 0.952 | < 0.0001 |
| CHF N (%) | 1790 (0.015) | 1861 (0.016) | 0.961 | 0.9 | 1.026 | 0.2364 |
| AKI N (%) | 2610 (0.022) | 2122 (0.018) | 1.235 | 1.166 | 1.309 | < 0.0001 |
| Cardiac arrest N (%) | 104 (0.001) | 157 (0.001) | 0.662 | 0.517 | 0.848 | 0.0011 |
| DVT N (%) | 683 (0.006) | 533 (0.008) | 1.283 | 1.145 | 1.437 | < 0.0001 |
| WC N (%) | 1314 (0.011) | 988 (0.008) | 1.334 | 1.228 | 1.449 | < 0.0001 |
| Hematoma N (%) | 653 (0.006) | 594 (0.005) | 1.100 | 0.984 | 1.23 | 0.094 |
| Pneumonia N (%) | 1370 (0.012) | 1642 (0.014) | 0.832 | 0.774 | 0.895 | < 0.0001 |
| PE N (%) | 809 (0.007) | 749 (0.006) | 1.081 | 0.978 | 1.194 | 0.1273 |
| Transfusion N (%) | 2271 (0.019) | 2918 (0.025) | 0.774 | 0.732 | 0.818 | < 0.0001 |
| UTI N (%) | 5081 (0.043) | 4710 (0.04) | 1.082 | 1.039 | 1.127 | 0.0001 |
| Narcotics Use N (%) | 89265 (0.754) | 87657 (0.74) | 1.075 | 1.055 | 1.095 | < 0.0001 |
| One year after TKA | ||||||
| Dislocation N (%) | 282 (0.002) | 276 (0.002) | 1.022 | 0.865 | 1.207 | 0.7993 |
| SSI N (%) | 2193 (0.019) | 1954 (0.017) | 1.125 | 1.058 | 1.196 | 0.0002 |
| MI N (%) | 3117 (0.026) | 2925 (0.025) | 1.067 | 1.014 | 1.123 | 0.0124 |
| Anemia N (%) | 2098 (0.018) | 2278 (0.019) | 0.920 | 0.866 | 0.976 | 0.006 |
| Arrhythmia N (%) | 13752 (0.116) | 14729 (0.124) | 0.925 | 0.902 | 0.948 | < 0.0001 |
| CHF N (%) | 3180 (0.027) | 3182 (0.027) | 0.999 | 0.921 | 1.05 | 0.9797 |
| AKI N (%) | 4306 (0.036) | 3722 (0.031) | 1.163 | 1.112 | 1.216 | < 0.0001 |
| Cardiac arrest N (%) | 235 (0.002) | 339 (0.003) | 0.693 | 0.586 | 0.818 | < 0.0001 |
| DVT N (%) | 1092 (0.009) | 814 (0.007) | 1.345 | 1.228 | 1.473 | < 0.0001 |
| WC N (%) | 1641 (0.014) | 1249 (0.011) | 1.318 | 1.224 | 1.42 | < 0.0001 |
| Hematoma N (%) | 929 (0.008) | 806 (0.007) | 1.154 | 1.05 | 1.268 | 0.0031 |
| Pneumonia N (%) | 3410 (0.029) | 3592 (0.03) | 0.948 | 0.904 | 0.994 | 0.0273 |
| PE N (%) | 1125 (0.01) | 1037 (0.009) | 1.086 | 0.997 | 1.182 | 0.0573 |
| Transfusion N (%) | 2639 (0.022) | 3296 (0.028) | 0.796 | 0.756 | 0.839 | < 0.0001 |
| UTI N (%) | 10411 (0.088) | 9771 (0.083) | 1.072 | 1.041 | 1.103 | < 0.0001 |
| Narcotics Use N (%) | 93180 (0.787) | 91568 (0.773) | 1.083 | 1.062 | 1.104 | < 0.0001 |
•Significant differences are highlighted in bold.
Across all time points, obese patients had a significantly higher revision rate than non-obese patients [Table 3].
Table 3.
Odds ratio of TKA revision 2, 5, and 10 years after primary.
| Obesity | Non-obesity | Odds ratio | Lower CI | Upper CI | P value | |
|---|---|---|---|---|---|---|
| 2 years N (%) | 2443 (0.021) | 2068 (0.017) | 1.185 | 1.117 | 1.257 | < 0.0001 |
| 5 years N (%) | 3238 (0.027) | 2662 (0.022) | 1.222 | 1.161 | 1.288 | < 0.0001 |
| 10 years N (%) | 3465 (0.029) | 2786 (0.024) | 1.251 | 1.189 | 1.316 | < 0.0001 |
•Significant differences are highlighted in bold.
The data shows that obese patients experienced significant albeit slightly higher total costs of care compared to non-obese counterparts at one year. Although the differences at 30 and 90 days were not significant, there was strong trend that obese patients had lower costs at 30 days compared to non-obese patients (p = .0524). The data also shows that obese patients experienced significantly lower drug costs of care compared to non-obese counterparts at all time points [Table 4].
Table 4.
Costs of care between Obese and Non-obese patients.
| Obesity | Non-obesity | Comparison | P value | |
|---|---|---|---|---|
| Total cost | ||||
| 30 days mean (SD) | 25908.2 (14073) | 26065.19 (14168.58) | 0.994 | 0.0524 |
| 90 days mean (SD) | 27964.71 (16554.3) | 27966.07 (17062.39) | 1.000 | 0.9887 |
| 1 year mean (SD) | 36010.99 (26468.2) | 35469.54 (28310.12) | 1.015 | 0.0006 |
| Drug cost | ||||
| 30 days mean (SD) | 284.32 (641.71) | 298.4 (767.33) | 0.953 | 0.0005 |
| 90 days mean (SD) | 674.55 (1582.06) | 715.67 (2152.99) | 0.943 | 0.0001 |
| 1 year mean (SD) | 2453.7 (5888.43) | 2604.14 (8046.89) | 0.942 | 0.0002 |
•Significant differences are highlighted in bold.
4. Discussion
In every examined time frame, we found obese patients experienced significantly higher rates of SSI, AKI, WC, UTI, and narcotics use, consistent with previous studies.5,6,11, 12, 13, 14, 15, 16, 17 We also found obese patients had a significantly higher risk of developing hematomas and DVT following TKA, both of which show conflicting results in existing literature.18, 19, 20, 21, 22 Recent articles discussing complications after TKA in obese patients are summarized in Table 5.12,14,21, 22, 23, 24, 25, 26, 27,35,37,38,45
Table 5.
Previous studies discussing complications following TKA in obese patients.
| Study | Year | Findings |
|---|---|---|
| Mantilla CB, Horlocker TT, Schroeder DR, Berry DJ, Brown DL | 2003 | Increased BMI (P = .031; odds ratio = 1.5 for each 5-kg/m2 increase) was found to independently increase the likelihood of pulmonary embolism or deep venous thrombosis. |
| Järvenpää J, Kettunen J, Kröger H, Miettinen H. | 2010 | Five complications (2 forms of wound infections, phlebitis, nerve injury, and massive edema) were found in obese patients compared with no complications found in non-obese patients (p = .028). |
| Kerkhoffs GM, Servien E, Dunn W, Dahm D, Bramer JA, Haverkamp D | 2012 | Infection, deep infection, and revision occurred more often in obese patients, with an odds ratio of 1.90, 2.38, and 1.30, respectively. |
| Suleiman LI, Ortega G, Ong'uti SK, Gonzalez DO, Tran DD, Onyike A, Turner PL, Fullum TM | 2012 | No differences existed in the rates of infection (P = .368), respiratory (P = .073), cardiac (P = .381), renal (P = .558), and systemic (P = .216) complications between BMI stratifications. |
| McElroy MJ, Pivec R, Issa K, Harwin SF, Mont MA | 2013 | Complication rates for non-obese, obese, and morbidly obese patients were 9, 15, and 22%, respectively, all of which were significantly different. |
| Issa K, Pivec R, Kapadia BH, Shah T, Harwin SF, Delanois RE, Mont MA | 2013 | There were no significant differences in the overall septic and aseptic implant survivorship (98.8 vs. 98.6%) between obese and non-obese patients. Obese patients had significantly higher complication rates (10.5 vs. 3.8%), however, there were no differences in the length of hospital stay for the two cohorts. |
| Frisch N, Wessell NM, Charters M, Peterson E, Cann B, Greenstein A, Silverton CD | 2016 | Transfusion rates were 17.3%, 11.4%, and 8.3% for normal, overweight, and obese patients, respectively (P = .002). This same cohort also loses a significantly decreased percentage of estimated blood volume. No trends were identified for a relationship between BMI and deep venous thrombosis, pulmonary embolism, myocardial infarction, discharge location, length of stay, 30-day readmission rate, and preoperative hemoglobin level. |
| Martin JR, Jennings JM, Dennis DA | 2017 | Postoperative issues for obese patients include tibial loosening, wound complications, cardiovascular events, and respiratory complications. |
| George J, Piuzzi NS, Ng M, Sodhi N, Khlopas AA, Mont MA. | 2018 | Obese patients were at increased risk of pulmonary embolism (PE) (P < .001), while morbidly obese patients were at increased risk of readmission (P < .001), reoperation (P < .001), superficial infection (P < .001), periprosthetic joint infection (P < .001), wound dehiscence (P < .001), PE (P < .001), urinary tract infection (P = .003), reintubation (P = .004), and renal insufficiency (P < .001). Transfusion was lower in overweight (P < .001), obese (P < .001), and morbidly obese (P < .001) patients. |
| Roche M, Law TY, Kurowicki J, Rosas S, Rush AJ 3rd | 2018 | The cost of treating obese patients rises as BMI deviates from normal, as does the incidence of revision surgery. |
| Sloan M, Sheth N, Lee GC | 2019 | Patients undergoing primary and revision TKA with World Health Organization classification as underweight (BMI <18.5 kg/m2), overweight (BMI 25–29.9 kg/m2), Class I obese (BMI 30–34.9 kg/m2), Class II obese (BMI 35–39.9 kg/m2), or Class III obese (BMI ≥40 kg/m2) did not demonstrate an association with increased risk of DVT compared with patients classified as normal weight (BMI 18.5–25 kg/m2). However, compared with patients classified as normal weight, the risk of PE was elevated in patients classified as overweight (OR, 1.56; 95% CI, 1.03–2.36; p = .035) and all heavier categories. |
| Boyce L, Prasad A, Barrett M, Dawson-Bowling S, Millington S, Hanna SA, Achan P. | 2019 | Overall complication rates, including infection, were higher in morbidly obese patients. Morbidly obese patients had a revision rate of 7% compared to and 2% (p < .001) in non-obese patients. |
| Abdulla I, Mahdavi S, Khong H, Gill R, Powell J, Johnston KD, Sharma R | 2020 | Patients with increased BMI had an increased number of in-hospital medical events, had an increased rate of deep infection, were less likely to be discharged home (p < .001) and had decreased transfusion requirements (p < .001) than patients whose weight was in the normal range. Increased BMI increased the rate of 30-day readmission and length of stay in the THA cohort but not in the TKA cohort. Increased BMI had no effect on acute postoperative dislocation or periprosthetic fractures. In the TKA cohort, patients with a BMI of 30 kg/m2 or greater required a TKA 2.7 years earlier than patients whose weight was in the normal range, patients with a BMI of 35 kg/m2 or greater required a TKA 4.6 years earlier, and patients whose BMI was 40 kg/m2 or greater required a TKA 7.6 years earlier. |
Curiously, we found significantly decreased risks of anemia, arrhythmia, cardiac arrest, pneumonia, and transfusion in obese patients. While this seems contradictory, other studies have found this same phenomenon called the “obesity paradox”, where BMI and mortality are inversely related, and this could explain the decrease in odds of cardiac arrest and arrhythmia.28,29 Even this paradox is controversial, however, because it could be due to retrospective data with obese patients being diagnosed earlier or due to a lack of proper adjustments for cardiorespiratory fitness as a high BMI due to fat and due to muscle are different.30 Furthermore, patients in the non-obese group could have been obese previously, but then experienced illness related weight loss.31
Previous studies have found that obesity has been linked to a decreased mortality with pneumonia,32,33 perhaps as an extension of the “obesity paradox”. Moreover, consistent with previous studies, obese patients had lower rates of transfusion.34 Finally, we found obese patients to have lower rates of anemia, however the precise relationship between obesity and anemia remains to be elucidated.35
After examining rates of post-operative complications, we investigated the difference in revision rates between obese and non-obese patients. Using two, five, and 10 years as time points to quantify how many patients underwent a revision, we found that obese patients had significantly more revisions across all time points, consistent with past studies.36,37 Revisions can be caused by various complications, however the most common is periprosthetic joint infection.38 The PearlDiver database does not allow for investigating the specific causes of revision in either the obese or non-obese group. However, we did find SSI as of the most common complications among obese patients undergoing TKA, supporting the association between obesity and increased revision rate due to SSI. Post-operative complications exacerbate the amount of medical treatment a patient requires, resulting in greater healthcare cost. Obese patients had a significantly higher total cost of care at one year, but surprisingly, obese patients had significantly lower drug costs at all time frames. Perhaps this is due to higher rates of anemia, arrhythmia, cardiac arrest, pneumonia, and transfusion in non-obese patients or other confounding variables.
Recent studies have investigated how adipose tissue and altered lipid metabolism present in obesity then lead to advanced arthritis. In obesity, pro-inflammatory cytokines, including TNF-α and IL-6, are released from adipose tissue, both of which upregulate matrix metalloproteinases (MMPs) that destroy cartilage.13 Adipokines, such as leptin and resistin, that further increase cartilage destruction are also upregulated. Moreover, oxidized low density lipoproteins cause arthritis and cartilage destruction, which can then be worsened by serum free fatty acids. All these microscopic proteins lead to a low-level, chronic inflammation that interferes with the immune system's proper surveillance by impairing immune chemotaxis and altering macrophage differentiation,39 thereby explaining the greater, macroscopic risk of SSI in obese patients.
Wound healing complications were also significantly higher in obese patients. Adipose tissue is largely avascular, leading to indirect revascularization following injury and causing substantial delay and reduced oxygen and nutrient perfusion.40 From this poor perfusion comes oxidative stress and reduced collagen production by fibroblasts, along with further chronic inflammation, all of which coalesce to prevent proper wound healing. The skin folds created with obesity could also prevent effective surgical prep and allowing some skin near the surgical site to avoid sterilization. Adipose tissue could also form pockets where fluid could accumulate and infection could prevent proper surgical closure. Furthermore, this chronic inflammation stimulates clot formation in vascular cells through TNF-alpha and IL-6 cytokines, and subsequent reduction in fibrinolysis,41 allowing for aberrant clots formation in pulmonary, renal, and lower extremities vasculature. There are contradictions in the literature as some studies have found a reduced risk of DVT in obese patients following TKA22 while other studies have found obesity to be a risk factor for symptomatic limb disease, including DVT.20,42 Therefore, further research must be done to determine the precise relationship between obesity and DVT risk.
With hypercoagulability, a reduced risk of hematoma would be expected, corresponding with the increased risk of DVT. However, our study found the risk of hematoma was increased across all time frames, significantly at 30 days and one year. The literature also has contradictory results: supporting the procoagulative tendency of obesity,18 but also arguing this increased hemostasis may be countered by other aspects of obesity.19 More investigation must be done to better understand obesity's effect on hemostasis. Finally, the relationships of cardiac arrest, arrhythmias, and pneumonia in obese patients are not yet fully understood and require further investigation.
Narcotics use was significantly higher in obese patients, and some authors theorize obesity is associated with increased postoperative pain.43 The cause of this pain is not fully understood as it could be due to chronic inflammation or biomechanical burden placed on the body from obesity. With this higher use of narcotics, obese patients would be expected to have higher costs of care.
However, we found that obese patients only experienced significantly higher total costs of care at one year and significantly lower drug costs at all three time points examined. Obesity's relationship with such a broad range of post-operative complications, however, has been correlated with both high total and high drug costs of care.44,45 Even so, this correlation is not easily explained as there are confounding variables difficult to match for, such as differences in economic status, access to healthcare, payment plans, or other social determinants of health.46 In our study, we matched for age, gender, CCI, and ECI. Though these factors reduce confounding variables, they are not all-encompassing and could still allow for interference with calculating obesity's true effect on costs. Furthermore, the “obesity paradox” could artificially lower the billed costs of care during the early post-operative period. Also, there could have been healthy patients placed under the category of obese, due to having an increased BMI from muscle tissue as opposed to adipose tissue or due to differences in age, sex, or height.47 Other simple, perhaps more accurate, practices of measuring BMI could be measuring the waist to hip ratio, waist circumference, skin fold thickness, or bioelectrical impedance analysis, while more sensitive methods could be advanced imaging, such as computed tomography or magnetic resonance.47 Obese patients had higher revision rates yet were only found to have significantly higher total costs of care than non-obese patients after one year. This is not surprising, however, because revision surgery is often performed years after the index procedure and our study only captured that cost from within a one-year time frame. According to one study, the average time between primary and revision TKA was 6.2 years on average.39 Therefore, the substantial cost of a revision would likely not be included in 30- and 90-day time frames, artificially lowering those total costs of care. The significantly lower drug costs are not easily explained and could be due to any limitation of this study, such as the lack of standardization in care due to being a multicenter retrospective study. Furthermore, some of the complications that were higher in the non-obese group, such as perhaps cardiac arrest, can be highly complex and require more medical and pharmacological intervention, resulting in higher costs for the non-obese group.48
We acknowledge several limitations in this study. Being a retrospective study with data gathered from various institutions and centers of practice, there were likely differences in surgical technique, equipment, and postoperative protocols. Furthermore, we could not determine if any procedures were done before the index TKA. Another limitation could stem from increasing BMIs past 30 kg/m2, between which the PearlDiver database did not differentiate. Those levels have been shown to affect post-operative outcomes37 and could skew the results of this study. Matching with CCI and ECI could include healthier obese patients that have comorbidity indices like that of non-obese patients, perhaps explaining the paradoxical results seen in the obese patient group. Retrospective studies rely on the accuracy of data that was previously entered. Consequently, any errors or discrepancies in data entry due to non-standardized and subjective criteria could have affected our results. Also, the PearlDiver Database records data based on CPT and ICD-9 codes, potentially limiting the data retrieval.
Even with these limitations, we sought to minimize the number of confounding variables by matching patients based on age, gender, CCI, and ECI and limit non-responder bias by only including patients who had records a year prior to and after their index TKA. This study also benefits from a high predictive power due to the large number of patients from the PearlDiver Database, with the matching protocol minimizing the potential for confounding variables. All the complications that were examined were decided before data collection began, thereby strengthening the credibility of our results. Moreover, none of the authors of this study matched the patients nor performed the surgeries, thereby further limiting the amount of selection bias.
As our population gets older and obesity becomes more common, the need for primary and revision TKA will likely increase. Obese patients did not have definitively worse outcomes than non-obese patients. Nonetheless, a robust understanding of the post-operative complications associated with obesity will promote educating patients and families about the potential risks of surgery. Not only will this improve patient ownership of their care but will also strengthen patient-physician rapport as surgeons can use the results of this study to work with patients in decision making in total knee arthroplasty.
5. Conclusion
With obesity on the rise, the ability to explain post-operative risks of complications due to obesity following TKA becomes ever more important. Our large, matched patient population study found significantly higher rates of SSI, AKI, DVT, WC, UTI, narcotics use, and revision surgery in obese patients. At the same time there were significantly lower rates of anemia, arrhythmias, cardiac arrest, pneumonia, transfusion, and drug costs of care in obese patients. Outcomes were not conclusively worse in obese patients, therefore further research should investigate the mechanisms that lead to these complications and understand the relationships between various other complications, diagnoses, or costs and total knee arthroplasty in obese patients.
Ethical approval
This is an observational study. The UTSW Institutional Review Board has confirmed that no ethical approval is required.
Consent to participate
Not applicable.
Consent to publish
Not applicable.
Authors contributions
All authors contributed to the study conception and design. Data collection and analysis were performed by Vikram Aggarwal. The first draft of the manuscript was written by Vikram Aggarwal and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Funding
The authors declare that no funds, grants, or other support were received during the preparation of this manuscript.
Competing interests
The authors have no relevant financial or non-financial interests to disclose.
Availability of data and materials
All data comes from the PearlDiver database.
Declaration of competing interest
None.
References
- 1.Singh J.A., Yu S., Chen L., Cleveland J.D. Rates of total joint replacement in the United States: future projections to 2020-2040 using the national inpatient sample. J Rheumatol. 2019 Sep;46(9):1134–1140. doi: 10.3899/jrheum.170990. Epub 2019 Apr 15. PMID: 30988126. [DOI] [PubMed] [Google Scholar]
- 2.Canovas F., Dagneaux L. Quality of life after total knee arthroplasty. Orthop Traumatol Surg Res. 2018 Feb;104(1S):S41–S46. doi: 10.1016/j.otsr.2017.04.017. Epub 2017 Nov 26. PMID: 29183821. [DOI] [PubMed] [Google Scholar]
- 3.Delanois R.E., Mistry J.B., Gwam C.U., Mohamed N.S., Choksi U.S., Mont M.A. Current epidemiology of revision total knee arthroplasty in the United States. J Arthroplasty. 2017 Sep;32(9):2663–2668. doi: 10.1016/j.arth.2017.03.066. Epub 2017 Apr 6. PMID: 28456561. [DOI] [PubMed] [Google Scholar]
- 4.Apovian C.M. Obesity: definition, comorbidities, causes, and burden. Am J Manag Care. 2016 Jun;22(7 Suppl):s176–s185. PMID: 27356115. [PubMed] [Google Scholar]
- 5.Kulkarni K., Karssiens T., Kumar V., Pandit H. Obesity and osteoarthritis. Maturitas. 2016 Jul;89:22–28. doi: 10.1016/j.maturitas.2016.04.006. Epub 2016 Apr 11. PMID: 27180156. [DOI] [PubMed] [Google Scholar]
- 6.Hennrikus M., Hennrikus W.P., Lehman E., Skolka M., Hennrikus E. The obesity paradox and orthopedic surgery. Medicine (Baltim) 2021 Aug 20;100(33) doi: 10.1097/MD.0000000000026936. PMID: 34414951; PMCID: PMC8376337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Austin S.R., Wong Y.N., Uzzo R.G., Beck J.R., Egleston B.L. Why summary comorbidity measures such as the Charlson comorbidity index and elixhauser score work. Med Care. 2015 Sep;53(9):e65. doi: 10.1097/MLR.0b013e318297429c. 72. PMID: 23703645; PMCID: PMC3818341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Menendez M.E., Neuhaus V., van Dijk C.N., Ring D. The Elixhauser comorbidity method outperforms the Charlson index in predicting inpatient death after orthopaedic surgery. Clin Orthop Relat Res. 2014 Sep;472(9):2878–2886. doi: 10.1007/s11999-014-3686-7. Epub 2014 May 28. PMID: 24867450; PMCID: PMC4117875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.MedCalc Software Ltd Odds ratio calculator. https://www.medcalc.org/calc/odds_ratio.php (Version 20.019
- 10.MedCalc Software Ltd Comparison of means calculator. https://www.medcalc.org/calc/comparison_of_means.php (Version 20.019
- 11.Gkastaris K., Goulis D.G., Potoupnis M., Anastasilakis A.D., Kapetanos G. Obesity, osteoporosis and bone metabolism. J Musculoskelet Neuronal Interact. 2020 Sep 1;20(3):372–381. PMID: 32877973; PMCID: PMC7493444. [PMC free article] [PubMed] [Google Scholar]
- 12.Martin J.R., Jennings J.M., Dennis D.A. Morbid obesity and total knee arthroplasty: a growing problem. J Am Acad Orthop Surg. 2017 Mar;25(3):188–194. doi: 10.5435/JAAOS-D-15-00684. PMID: 28146438. [DOI] [PubMed] [Google Scholar]
- 13.Thijssen Eva, Arjan van Caam, Peter M., van der Kraan. Obesity and osteoarthritis, more than just wear and tear: pivotal roles for inflamed adipose tissue and dyslipidaemia in obesity-induced osteoarthritis. Rheumatology. April 2015;54(4):588–600. doi: 10.1093/rheumatology/keu464. [DOI] [PubMed] [Google Scholar]
- 14.George J., Piuzzi N.S., Ng M., Sodhi N., Khlopas A.A., Mont M.A. Association between body mass index and thirty-day complications after total knee arthroplasty. J Arthroplasty. 2018 Mar;33(3):865–871. doi: 10.1016/j.arth.2017.09.038. Epub 2017 Oct 6. PMID: 29107493. [DOI] [PubMed] [Google Scholar]
- 15.Rodriguez-Merchan E.C. Review article: outcome of total knee arthroplasty in obese patients. J Orthop Surg. 2015 Apr;23(1):107–110. doi: 10.1177/230949901502300124. [DOI] [PubMed] [Google Scholar]
- 16.Stokes A., Lundberg D.J., Sheridan B., et al. Association of obesity with prescription opioids for painful conditions in patients seeking primary care in the US. JAMA Netw Open. 2020 Apr 1;3(4) doi: 10.1001/jamanetworkopen.2020.2012. PMID: 32239222; PMCID: PMC7118518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Stokes A., Berry K.M., Collins J.M., et al. The contribution of obesity to prescription opioid use in the United States. Pain. 2019 Oct;160(10):2255–2262. doi: 10.1097/j.pain.0000000000001612. PMID: 31149978; PMCID: PMC6756256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lee K.T., Lee H., Jeon B.J., Mun G.H., Bang S.I., Pyon J.K. Impact of overweight/obesity on the development of hematoma following tissue expander-based breast reconstruction. J Plast Reconstr Aesthetic Surg. 2020 Sep 19:S1748. doi: 10.1016/j.bjps.2020.08.105. 6815(20)30434-4. Epub ahead of print. PMID: 34756415. [DOI] [PubMed] [Google Scholar]
- 19.Braekkan S.K., van der Graaf Y., Visseren F.L., Algra A. Obesity and risk of bleeding: the SMART study. J Thromb Haemostasis. 2016 Jan;14(1):65–72. doi: 10.1111/jth.13184. Epub 2016 Jan 4. PMID: 26514237. [DOI] [PubMed] [Google Scholar]
- 20.Guss Daniel MD., Bhattacharyya Timothy MD. Perioperative management of the obese orthopaedic patient. J Am Acad Orthop Surg. July 2006;14(7):425–432. doi: 10.5435/00124635-200607000-00005. [DOI] [PubMed] [Google Scholar]
- 21.Mantilla Carlos B., Horlocker Terese T., Darrell R., Schroeder Daniel, Berry J., Brown David L. Risk factors for clinically relevant pulmonary embolism and deep venous thrombosis in patients undergoing primary hip or knee arthroplasty. Anesthesiology. 2003;99:552–560. doi: 10.1097/00000542-200309000-00009. [DOI] [PubMed] [Google Scholar]
- 22.Sloan M., Sheth N., Lee G.C. Is obesity associated with increased risk of deep vein thrombosis or pulmonary embolism after hip and knee arthroplasty? A large database study. Clin Orthop Relat Res. 2019 Mar;477(3):523–532. doi: 10.1097/CORR.0000000000000615. PMID: 30624321; PMCID: PMC6382191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Järvenpää J., Kettunen J., Kröger H., Miettinen H. Obesity may impair the early outcome of total knee arthroplasty. Scand J Surg. 2010;99(1):45–49. doi: 10.1177/145749691009900110. [DOI] [PubMed] [Google Scholar]
- 24.Kerkhoffs G.M., Servien E., Dunn W., Dahm D., Bramer J.A., Haverkamp D. The influence of obesity on the complication rate and outcome of total knee arthroplasty: a meta-analysis and systematic literature review. J Bone Joint Surg Am. 2012 Oct 17;94(20):1839–1844. doi: 10.2106/JBJS.K.00820. PMID: 23079875; PMCID: PMC3489068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Suleiman L.I., Ortega G., Ong'uti S.K., et al. Does BMI affect perioperative complications following total knee and hip arthroplasty? J Surg Res. 2012 May 1;174(1):7–11. doi: 10.1016/j.jss.2011.05.057. Epub 2011 Jun 25. PMID: 21816426. [DOI] [PubMed] [Google Scholar]
- 26.McElroy M.J., Pivec R., Issa K., Harwin S.F., Mont M.A. The effects of obesity and morbid obesity on outcomes in TKA. J Knee Surg. 2013 Apr;26(2):83–88. doi: 10.1055/s-0033-1341407. Epub 2013 Mar 11. PMID: 23479424. [DOI] [PubMed] [Google Scholar]
- 27.Issa K., Pivec R., Kapadia B.H., et al. Does obesity affect the outcomes of primary total knee arthroplasty? J Knee Surg. 2013 Apr;26(2):89–94. doi: 10.1055/s-0033-1341408. Epub 2013 Mar 15. PMID: 23504647. [DOI] [PubMed] [Google Scholar]
- 28.Kunju S.U., Badarudeen S., Schwarz E.R. Impact of obesity in patients with congestive heart failure. Rev Cardiovasc Med. 2009 Summer;10(3):142–151. doi: 10.3909/ricm0463. PMID: 19898291. [DOI] [PubMed] [Google Scholar]
- 29.Pouwels S., Topal B., Knook M.T., et al. Interaction of obesity and atrial fibrillation: an overview of pathophysiology and clinical management. Expert Rev Cardiovasc Ther. 2019 Mar;17(3):209–223. doi: 10.1080/14779072.2019.1581064. Epub 2019 Feb 20. PMID: 30757925. [DOI] [PubMed] [Google Scholar]
- 30.Ades P.A., Savage P.D. The obesity paradox: perception vs knowledge. Mayo Clin Proc. 2010 Feb;85(2):112–114. doi: 10.4065/mcp.2009.0777. PMID: 20118385; PMCID: PMC2813817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Flegal K.M., Graubard B.I., Williamson D.F., Cooper R.S. Reverse causation and illness-related weight loss in observational studies of body weight and mortality. Am J Epidemiol. 2011 Jan 1;173(1):1–9. doi: 10.1093/aje/kwq341. Epub 2010 Nov 8. PMID: 21059807. [DOI] [PubMed] [Google Scholar]
- 32.King Phoebe, Mortensen Eric M., Bollinger Mary, et al. Impact of obesity on outcomes for patients hospitalised with pneumonia Polly Hitchcock Noël. Eur Respir J. Apr 2013;41(4):929–934. doi: 10.1183/09031936.00185211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Kahlon S., Eurich D.T., Padwal R.S., et al. Obesity and outcomes in patients hospitalized with pneumonia. Clin Microbiol Infect. 2013 Aug;19(8):709–716. doi: 10.1111/j.1469-0691.2012.04003.x. Epub 2012 Sep 11. PMID: 22963453; PMCID: PMC3594436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Frisch N., Wessell N.M., Charters M., et al. Effect of body mass index on blood transfusion in total hip and knee arthroplasty. Orthopedics. 2016 Sep 1;39(5):e844–e849. doi: 10.3928/01477447-20160509-04. Epub 2016 May 13. PMID: 27172370. [DOI] [PubMed] [Google Scholar]
- 35.Purdy J.C., Shatzel J.J. The hematologic consequences of obesity. Eur J Haematol. 2021 Mar;106(3):306–319. doi: 10.1111/ejh.13560. Epub 2020 Dec 13. PMID: 33270290; PMCID: PMC8086364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Abdulla I., Mahdavi S., Khong H., et al. Does body mass index affect the rate of adverse outcomes in total hip and knee arthroplasty? A retrospective review of a total joint replacement database. Can J Surg. 2020 Mar 27;63(2):E142–E149. doi: 10.1503/cjs.006719. PMID: 32216250; PMCID: PMC7828962. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Boyce L., Prasad A., Barrett M., et al. The outcomes of total knee arthroplasty in morbidly obese patients: a systematic review of the literature. Arch Orthop Trauma Surg. 2019 Apr;139(4):553–560. doi: 10.1007/s00402-019-03127-5. Epub 2019 Feb 16. PMID: 30778723; PMCID: PMC6420900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Postler A., Lützner C., Beyer F., Tille E., Lützner J. Analysis of total knee arthroplasty revision causes. BMC Muscoskel Disord. 2018 Feb 14;19(1):55. doi: 10.1186/s12891-018-1977-y. PMID: 29444666; PMCID: PMC5813428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Huttunen R., Syrjänen J. Obesity and the risk and outcome of infection. Int J Obes. 2013;37:333–340. doi: 10.1038/ijo.2012.62. [DOI] [PubMed] [Google Scholar]
- 40.Pierpont Y.N., Dinh T.P., Salas R.E., et al. Obesity and surgical wound healing: a current review. ISRN Obes. 2014 Feb 20;2014 doi: 10.1155/2014/638936. PMID: 24701367; PMCID: PMC3950544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Blokhin I.O., Lentz S.R. Mechanisms of thrombosis in obesity. Curr Opin Hematol. 2013 Sep;20(5):437–444. doi: 10.1097/MOH.0b013e3283634443. PMID: 23817170; PMCID: PMC4445633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Davies H.O., Popplewell M., Singhal R., Smith N., Bradbury A.W. Obesity and lower limb venous disease - the epidemic of phlebesity. Phlebology. 2017 May;32(4):227–233. doi: 10.1177/0268355516649333. PMID: 27178403. [DOI] [PubMed] [Google Scholar]
- 43.Okifuji A., Hare B.D. The association between chronic pain and obesity. J Pain Res. 2015 Jul 14;8:399–408. doi: 10.2147/JPR.S55598. PMID: 26203274; PMCID: PMC4508090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Roche M., Law T.Y., Kurowicki J., Rosas S., Rush A.J., 3rd Effect of obesity on total knee arthroplasty costs and revision rate. J Knee Surg. 2018 Jan;31(1):38–42. doi: 10.1055/s-0037-1608933. Epub 2017 Dec 7. PMID: 29216676; PMCID: PMC6427916. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Narbro K., Agren G., Jonsson E., Näslund I., Sjöström L., Peltonen M., Swedish Obese Subjects Intervention Study Pharmaceutical costs in obese individuals: comparison with a randomly selected population sample and long-term changes after conventional and surgical treatment: the SOS intervention study. Arch Intern Med. 2002 Oct 14;162(18):2061–2069. doi: 10.1001/archinte.162.18.2061. PMID: 12374514. [DOI] [PubMed] [Google Scholar]
- 46.Biener A., Cawley J., Meyerhoefer C. The high and rising costs of obesity to the US health care system. J Gen Intern Med. 2017 Apr;32(Suppl 1):6–8. doi: 10.1007/s11606-016-3968-8. PMID: 28271429; PMCID: PMC5359159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Gurunathan U., Myles P.S. Limitations of body mass index as an obesity measure of perioperative risk. Br J Anaesth. 2016 Mar;116(3):319–321. doi: 10.1093/bja/aev541. PMID: 26865129. [DOI] [PubMed] [Google Scholar]
- 48.Selby L.V., Gennarelli R.L., Schnorr G.C., et al. Association of hospital costs with complications following total gastrectomy for gastric adenocarcinoma. JAMA Surg. 2017 Oct 1;152(10):953–958. doi: 10.1001/jamasurg.2017.1718. PMID: 28658485; PMCID: PMC5710284. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All data comes from the PearlDiver database.