Abstract
AIM:
Nurses use their smartphones during the work shift. The objective of this review is to investigate the presence of bacteria on mobile phones and the procedures to disinfect or decontaminate the smartphone and decrease the infection rate.
Method:
This systematic review was carried out through a search on the main scientific databases by following the Preferred Reporting Items for Systematic Reviews and Meta-Analyses guidelines. The research was conducted by considering articles published in the last ten years.
Results:
Of 502 initial articles, 489 were excluded and 12 articles were considered relevant. Twelve articles were included in the review. The analysis of the studies showed a high contamination of pathogenic microorganisms on the device’s surfaces, most of which appear to be antibiotic resistant. The use of smartphones during clinical practice increases the risk of contracting nosocomial infections. The presence of bacteria on mobile phones and their use favors the cross-transmission of microorganisms.
Conclusıon:
Onset prevention is a primary goal for the entire multidisciplinary team. There are no protocols concerning smartphones disinfection during clinical practice, but their implementation would reduce the incidence by improving nursing care.
Keywords: Bacterial contamination, infection, mobile communication, nosocomial infection, nosocomial pathogen, smartphone
Introduction
The introduction of the smartphone in humans lives has influenced and changed every aspect of daily life. Smartphones are a real extension of humans itselves, they move with us in every environment, and it is estimated that, on average, each person touches their mobile up to 200 times a day. It is important to know that telephone not only transmits phone calls, messages, and e-mails but also spreads a large number of bacteria; in fact, the heat generated by the phone and the residual microbial flora present on the hands create a perfect habitat for bacterial growth (Abdali et al., 2018). Nevertheless, the worry and the constant need to always stay interconnected have made these devices essential both in daily and working life. The hospital environment for its part has not remained inert; different studies have shown that the adoption of mobile devices from the staff is constantly increasing, accompanying and supporting care activities. Some healthcare companies, for example, provide mobile devices to medical personnel for internal use within hospital facilities, in order to improve communication and accessibility to documents and to support clinical diagnosis (Morvai & Szabó, 2015). The latest generation devices consist of a touch screen part in direct contact with the fingers, which inevitably becomes a potential reservoir for the bacterial flora present on the hands. In the healthcare sector, all of this only increases the spread of healthcare-associated infections, also known as hospital-acquired infections. Although technological evolution has brought significant advantages in all sectors, it is also necessary to consider the negative effects regarding the use of smartphones during clinical practice. The World Health Organization (WHO) (2011) has conducted research to examine the main clinical risks arising from the use of mobile technology, such as distraction, electromagnetic interference, and issues and risk of infection. According to a recent study, it has been shown that the bacterial count present on a mobile phone is greater than that on a toilet seat. The risk of cross-contamination is therefore a fundamental aspect to be taken into consideration and under control since nurses’ hands are to be considered the most powerful vehicle for infections (Tschopp et al., 2016). The uncontrolled use of mobile devices contributes to increasing the likelihood of contamination not only between nurses and patients but also among healthcare professionals themselves, consequently increasing the incidence of contracting a hospital infection and causing an increase in hospitalization time and costs. The widespread prevalence makes them the most serious and common adverse event of health care at global level. This condition requires careful monitoring, but still in Italy, there is no active national surveillance system with dedicated staff to assess the frequency of infections. In order to confirm the hypothesis of a possible cross-contamination mediated by the use of smartphones during the care practice, a literature review was conducted. The main objective is to investigate the presence of bacteria on mobile phones and the procedures to disinfect or decontaminate the smartphone and decrease the infection rate.
Method
Study Design
A systematic review of the literature was conducted according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses statement indications (Moher et al., 2009a).
Study Process
In order to formulate a valid search strategy, the research question, the characteristics, and the sample to be analyzed were identified using the Patient, Intervention, Outcome, Setting method (Table 1). The research question was: Are microorganisms present on smartphone surfaces? Are there a correlation between increased infections and smartphone use?
Table 1.
Research Question Identified Through PIOS Methodology
| Research Question Identified Through PIOS Methodology | ||
|---|---|---|
| P | Patient | Nurses or nursing students who use smartphones during care activities |
| I | Intervention | Evaluation of the relation between smartphone use during healthcare and increased infections |
| O | Outcome | Increase in the infections |
| S | Setting | All hospital care settings: intensive care, medicine and surgery unit, and first aid |
| Research question | Can the use of smartphones during clinical practice really increase the incidence of healthcare-related infections? | |
Note: PIOS = Patient, Intervention, Outcome, Setting.
To answer the research question, the main electronic databases of scientific nature were consulted, both generalist such as PubMed and Scopus and specialized such as CINAHL. To carry out the search, the main keywords were combined using the Boolean operators “AND” and “OR.” This search string has been used for the research in the PubMed database: (smartphone OR mobile communication OR cell phone OR personal communication device) AND (infection OR infections OR nosocomial infection OR nosocomial pathogen OR nosocomial pathogens OR bacterial contaminant OR bacterial infection OR bacterial infections OR hands infected) AND (nurs*).
Inclusion and Exclusion Criteria
Once the eligibility criteria were defined, all Italian and English articles from 2010 to 2020 were included. This choice was made by considering the last 10 years as most representative of smartphone use. In addition, observational studies and randomized control trials focused on nurses or nursing students working in any care setting were included (Table 1). Articles that met the following criteria were included: articles focusing on nurses or nursing students who use smartphones during care activities; focusing on evaluation of the relation between smartphone use during health care and increased infections; focusing on all hospital care settings: intensive care, medicine and surgery unit, and first aid.
Search Outcome
The results obtained from the search were imported into the Endnote® database, duplicates were eliminated, and only results in English and Italian were considered. Once the articles were found and appropriate duplicates removed, two independent authors (SDM and SD) reviewed each article. Articles were reviewed based on previously established eligibility criteria. The first phase of screening allowed articles to be eliminated by reading the title and abstract. In the second, eligibility phase, relevant studies were selected through full-text reading. Articles deemed questionable were evaluated by two additional authors (EDS and NG). Through full-text reading, it was possible to exclude articles that did not answer the research question, thus allowing further restriction of the field.
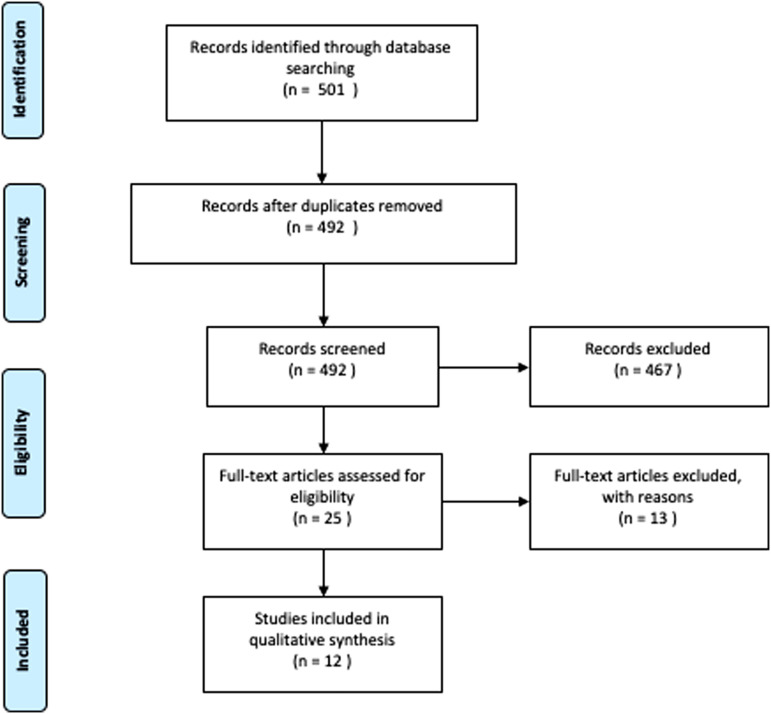
Five hundred one articles were initially identified, 25 of which were potentially eligible. The reading of the full texts led to the final inclusion of 12 articles. Figure 1 shows the selection process according to the PRISMA methodology (Moher et al., 2009b).
Figure 1.
PRISMA Flowchart. PRISMA = Preferred Reporting Items for Systematic Reviews and Meta-Analyses.
Quality Appraisal
All studies were independently examined for inclusion/exclusion criteria. A qualitative evaluation of the evidence related to the individual outcomes was conducted (GRADE Handbook) (Kavanagh, 2009). The only studies in line with the aim of the research were observational studies; therefore, the quality was low for most of the trials or very low due to important limitations. The numbering of the articles refers to the number of citation present in the bibliography (Table 3).
Table 3.
Quality Assessment
| Quality Assessment | |||||||
| No. of Study | Study Design | Risk of Bias | Inconsistency | Indirectness | Imprecision | Other Consideration | Quality |
| Outcome: | To assess the presence of bacterial contamination of healthcare workers’ smartphones | ||||||
| 10 | Prospective study | Not serious | Not serious | Not serious | Not serious | None | ⨁⨁◯◯Low |
| 11 | Case–control study | Not serious | Not serious | Not serious | Not serious | None | ⨁⨁◯◯Low |
| 13 | Prospective study | Not serious | Not serious | Not serious | Not serious | None | ⨁⨁◯◯Low |
| 14 | Prospective study | Not serious | Not serious | Not serious | Serious | None | ⨁◯◯◯Very low |
| 17 | Cross-sectional study | Not serious | Not serious | Not serious | Not serious | None | ⨁⨁◯◯Low |
| 18 | Cross-sectional study | Not serious | Not serious | Not serious | Not serious | None | ⨁⨁◯◯Low |
| Outcome: | To assess the frequency of bacterial contamination and antibiotic resistance | ||||||
| 8 | cross-sectional study | Not serious | Not serious | Not serious | Not serious | None | ⨁⨁◯◯Low |
| Outcome: | To assess the presence of bacterial flora on the hands and smartphones of healthcare workers | ||||||
| 12 | Prospective study | Not serious | Not serious | Not serious | Not serious | None | ⨁⨁◯◯Low |
| 7 | Cross-sectional study | Not serious | Not serious | Not serious | Serious | None | ⨁◯◯◯Very low |
| Outcome: | To compare the contamination of healthcare workers’ smartphones with non-healthcare workers’ smartphones | ||||||
| 9 | Case–control study | Not serious | Not serious | Not serious | Serious | None | ⨁◯◯◯Very low |
| Outcome: | To consider creating a cleaning protocol for operators’ smartphones to reduce bacterial transmission | ||||||
| 15 | Cross-sectional study | Not serious | Not serious | Not serious | Not serious | None | ⨁⨁◯◯Low |
| Outcome: | To evaluate the presence of RNA on the surface of smartphones | ||||||
| 16 | Prospective study | Not serious | Not serious | Not serious | Not serious | None | ⨁⨁◯◯Low |
Data Extraction
The following data were collected for each study: name and year of the first author, purpose and design of the study, study population, and summary of results. The following information was compiled into a data extraction table (Table 2).
Table 2.
Extraction Table
| No. | Authors and Years | Title | Study Design | Setting | Study Object | Sample Selected | Study Results |
|---|---|---|---|---|---|---|---|
| 1 | Qureshi et al. 2020 | Mobile phones in the orthopedic operating room: microbial colonization and antimicrobial resistance | Cross-sectional study | Pakistan | To investigate microbial colonization on the mobile phones of healthcare professionals in the orthopedic operating room | All orthopedic and anesthesia attendings, residents and technicians, and all nursing staff working in the orthopedic operating room |
Ninety-three of 100 mobile phones were contaminated. Species isolated were coagulase-negative Staphylococcus (62%), Micrococcus (41%), and Bacillus (26%). |
| 2 | Galazzi et al. 2019 | Microbiological colonization of healthcare workers’ mobile phones in a tertiary-level Italian intensive care unit | Prospective study | Italy | To evaluate the contamination rate of healthcare workers’ mobile phones in intensive care units before and after shifts. | 50 health workers including 28 nurses, 16 doctors, 6 assistants | 98% of the nurses’ smartphones were most contaminated with coagulase-negative Staphylococci, Bacillus spp., and MRSA. No patients in the ICU had positive infections with bacteria on their phones. Smartphones are colonized even before the shift. |
| 3 | Simmond et al. 2019 | Mobile phones as fomites for potential pathogens in hospitals: microbiome analysis reveals hidden contaminants. | Case - control study | UK | To analyze the amount and diversity of bacterial contamination of healthcare workers’ phones. Identify the potential pathogens prevalence and compare microbial communities of hospital staff and control group |
250 hospital staff smartphones, 191 control group participants. | Almost all 99.2% of hospital staff’s smartphones were contaminated with potential pathogens, with a significantly higher rate than the control rate. The results revealed MRSA, vancomycin-resistant Enterococci. |
| 4 | Shah et al. 2019 | Microorganism isolated from mobile phones and hands of healthcare workers in a tertiary care hospital of Ahmedabad, Gujarat, India | Prospective study | India | To verify the bacterial flora on hands and smartphones and the bacterial correlation between the dominant hand and the phone | 300 samples were collected from phones and dominant hand of nurses, doctors, support staff working in TIN, TI, and DEA | 150 smartphones and 150 dominant hands have been analyzed. High contamination rate was found on doctors’ phones (32.66%), support staff (32%), and finally nurses (31.33%). The most isolated microorganism was coagulase-negative Staphylococcus with 52% prevalence. The bacterial isolates recovered from the hands of 47 nurses showed 27 types of microorganisms identical to those isolated on smartphones. |
| 5 | Khashei et al. 2018 | The occurrence of nosocomial pathogens on cell phones of healthcare workers in an Iranian tertiary care hospital | Cross-sectional study | Iran | To analyze healthcare workers’ cell phones to determine the frequency of bacterial contamination and antibiotic resistance | 25 healthcare workers’ mobile and 75 medicine students | 139 potentially pathogenic bacterial colonies were isolated (Staphylococcus most prevalent, of which 40.9% were methicillin-resistant bacteria). The cell phone contamination rate decreased significantly after disinfection from 88% to 52%. Disinfection has been associated with reduced methicillin-resistant isolates colonization. |
| 6 | Dorost et al. 2018 | Microbial contamination data of keypad and touchscreen of cell phones among hospital and non-hospital staff—A case study: Iran | Cross-sectional study | Iran | To compare mobile phone, keyboard, and touchscreen microbial contamination of healthcare and non-healthcare workers | 456 smartphones, including 240 healthcare professionals and 216 non-healthcare professionals | Bacterial contamination is significantly lower on touch screens than on keyboards. Nurses’ phones have been more contaminated. The bacteria most present were Enterococci, Gram-positive bacilli, Staphylococcus coagulase negative. |
| 7 | Kanayama et al. 2017 | Staphylococcus aureus surface contamination of mobile phones and the presence of genetically identical strains on the hands of nursing personnel | Cross-sectional study | Japan | To prove the correlation between bacteria found on phones and those on the healthcare workers’ hands. | Analyze the hands and smartphones of 221 nurses in 23 general care units | Of the 221 smartphones used, 16 (7.2%) have been contaminated with S. aureus, of which 5 (2.3%) had MRSA. S. aureus has been isolated from 55 hands. The highest rate of isolation has been found in Unit F, where 4 out of the 5 MRSA-positive nurses worked, cell phones and hospitalized patients also tested positive. |
| 8 | Murgier et al 2016. | Microbial flora on cell phones in an orthopedic surgery room before and after decontamination. | Prospective study | France | To examine the bacterial colonies present on the phone surfaces introduced into the orthopedic surgical room and evaluate the decontamination effectiveness | 52 participants (29 men and 23 women aged 22-52) including nurses, surgeons, anesthetists | Before decontamination, the average number of colony units was 258 per cell phone. After cleaning, the number significantly reduced to 127. Mobile phones were bacteria carriers. |
| 9 | Kotris et al. 2016 | Identification of microorganisms on mobile phones of intensive care unit healthcare workers and medical students in the tertiary hospital. | Prospective study | Croatia | To identify the microorganism difference in the intensive care unit on the mobile phones of nurses, doctors, and students | 50 health care workers’ mobile phone swabs who work in intensive care unit and 60 medical student swabs | Of 110 processed smartphones, 25 (22.7%) devices were free of contamination. No significant difference between health workers and students in bacteria terms had been revealed. The bacteria isolated common to both groups was S. aureus. |
| 10 | Kirkby et al 2016 | Cell Phones in the Neonatal Intensive Care Unit: How to Eliminate Unwanted Germs. | Cross-sectional study. | USA | To affirm that mobile phones are a reservoir of potentially harmful microorganisms and implement a disinfection protocol for them. | 18 participants including family members and nurses, doctors, technicians in the neonatal intensive care unit | All smartphones tested positive for bacterial colonization, the prevalence rate after decontamination has been significantly lower. |
| 11 | Pillet et al. 2015 | Contamination of healthcare workers’ mobile phones by epidemic viruses. | Prospective study | France |
To investigate RNA from epidemic viruses including rotavirus, flu, respirators on healthcare workers’ smartphones | 114 health workers (35 doctors, 32 nurses, 30 residents, 27 OSS) in adult or pediatric units | The medical staff used the smartphone more frequently than the nurses. More use has been in adult wards than in pediatric wards. RNA virus has been isolated from 42 of the 109 mobile phones collected. The rotavirus has been found on 39 devices, respiratory syncytial virus on 3, and metapneumovirus on 1. |
| 12 | Ustun & Cihangiroglu, 2012 | Healthcare workers’ mobile phones: a potential cause of microbial cross-contamination between hospitals and community | Transversal study | Turkey | To determine pathogenic microorganisms on health care workers’ cell surfaces | 183 mobile phones; 94 (51.4%) from nurses, 32 (17.5%) from laboratory workers, and 57 (31.1%) from healthcare personnel | 179 cells tested positive for culture, of which 17 MRSA, 20 Escherichia coli were capable of causing nosocomial infections. A significant difference emerged between E. coli contamination in intensive and non-intensive care wards. |
Note: MRSA = methicillin-resistant Staphylococci.
Data Synthesis
The results of this review reveal a high contamination of pathogenic microorganisms on smartphones surfaces which constitutes a potential vector for cross-transmission. The studies included varied in terms of aims, methods, outcome measures, results, limitations, and implications for practice.
Results
Overall, the data from the individual studies confirmed the initial assumption: smartphones are a vehicle for the spread of potential pathogens capable of causing nosocomial infections. The results of this review reveal a high contamination of pathogenic microorganisms on smartphones surfaces which constitutes a potential vector for cross-transmission.
The Microbial Colonization on the Mobile Phone
The bacteria isolated on nurses’ smartphones surfaces are: Enterobacteriaceae and Bacilli spp. Galazzi et al. (2019) analyzed 50 smartphones of healthcare professionals. The aim of the study was to evaluate the contamination rate on the devices at the beginning and at the end of the work shift. The results from the swab tampons reported no significant difference in contamination; the devices appeared to be contaminated even before the work shift. Simmond et al. (2019), through a case–control study, confronted the diversity of microorganisms present on smartphones of healthcare workers compared to the control group. The most common bacteria included coagulase-negative Staphylococcus (CoNS), Staphylococcus aureus, and Enterococcus spp. Hospital workers’ smartphones turned out to be more contaminated than the control group, but no difference in microorganisms was found between the two subjects participating in the study. Shah et al. (2019) assessed the frequency of contamination on a sample of 300 healthcare professionals and it was found that the category of nurses showed the least contamination on phones’ surfaces. The bacteria identified on nurses’ smartphones were CoNS, methicillin-sensitive Bacillus spp., S. aureus, Klebsiella pneumonie.
The study by Kotris et al. (2017) analyzed the difference in microorganisms present on the surfaces of the phones of healthcare workers and medical students in the intensive care unit (ICU). No substantial difference in bacteria was found between health workers and students, the major organism isolated was CoNS followed by S. aureus. The study group looked for the presence of RNA viruses (metapneumovirus, syncytial virus, rotavirus, norovirus). Rotavirus followed by syncytial virus were the two most isolated viral agents. Ustun et al. (2012) evaluated contamination on smartphone surfaces. One hundred seventy-nine culture-positive samples for methicillin-resistant Staphylococcus and Escherichia Coli, capable of transmitting nosocomial infections, were isolated.
Qureshi et al. (2020) investigated microbial colonization on the mobile phone of health care professionals in operating room. Ninety-three of 100 mobile phones were contaminated. Different species isolated were CoNS, Micrococcus, and Bacillus.
Microbial Colonization on Smartphone and Disinfection Technique
The research conducted in Japan has in fact analyzed the genetic relation between the Staphylococcus present on the hands compared to that present on smartphones (Kanayama et al., 2017). The obtained results confirm the genetic sameness of the isolated bacteria and therefore confirm the influence of hands and smartphones for the transmission of bacteria responsible for hospital infections. Khashei et al. (2019) evaluated the frequency of bacterial contamination before and after disinfection through a cross-sectional study. It was found that the pre- and post-disinfection contamination rate was significantly reduced from 88% to 52% and of the 139 isolated colonies, 99 were potentially pathogenic (Staphylococci, Streptococci, and Pseudomonas). The study by Dorost et al. (2018) compared the contamination of keyboard and touch devices between nurses and non-hospital staff.
In this regard, Murgier et al. (2016) conducted research aimed at analyzing bacterial colonies present on the surfaces of telephones in the operating room and verifying the effectiveness of decontamination methods. Around 33% of healthcare workers claimed to systematically answer the phone in the operating room and 34% to disinfect it regularly. It turned out that the contamination rate of the devices was 94% and was significantly reduced by disinfection with Surfanios (often used in operating room cleaning).
Kirkby et al. (2016) analyzed the contamination rate of cell phones in neonatal intensive care and proposed a device disinfection protocol to reduce the transmission of germs in the neonatal environment. Pre- and post-disinfection swab samples were collected using hospital-grade wipes on the front surface of the smartphones and commercial antibacterial wipes on the rear surface. No difference was reported between the two disinfection methods. From the obtained results, it was decided to implement a process of cleaning the smartphones of healthcare workers and families. Pillet et al. (2016) examined the presence and type of viruses on smartphones.
Discussion
The results from the articles included in the review showed consistent results with the research objective, which is to demonstrate that the smartphone is a reservoir of different species of microorganisms that can cause nosocomial infections. The hands of nurses and more generally of health workers are the major cause of contamination and the uncontrolled use of them, during care, favors the spread of microbes from one patient to another.
The correlation between increased infections and smartphone use was verified by Kanayama et al. (2017) and Shah et al. (2019), whose studies have shown the presence of a high number of genetically identical bacterial strains on nurses’ hands and cell phones. In fact, both studies found that the main microorganism present is microorganism is Staphylococcus. This finding is also confirmed in the study by Ustun et al. (2012) where the major microorganisms isolated were methicillin-resistant Staphylococci (MRSA) and methicillin-sensitive Staphylococci (MSSA), those responsible for most nosocomial infections.
In the study by Qureshi et al. (2020), the microorganisms isolated were CoNS, Micrococcus, and Bacillus. The presence of MRSA on surfaces is a cause for concern, especially when it comes to high-risk wards such as intensive care and pediatrics. The results of the study by Galazzi et al. (2019) conducted in an Italian ICU not only confirmed the presence of MRSA but also showed that there was little or almost no difference between the bacteria isolated before and after the work shift. Nevertheless, bacteria are not the only microorganisms present on cell phone surfaces, in fact, unlike bacterial contamination, which is widely discussed in many articles, data on viral contamination are lacking. Epidemic viruses can contaminate inert surfaces and medical devices in the vicinity of patients and can also survive for several weeks. In this regard, Pillet et al. (2016) analyzed the presence of viruses (rotavirus, norovirus, metapneumovirus, and syncytial virus) on smartphones. Most of the studies included in this review showed high contamination of cell phones not only from healthcare workers but also from relatives of hospitalized patients. Two studies compared the type of microorganisms present on the hands of healthcare workers and control (non-healthcare) groups (Dorost et al., 2018; Simmonds et al., 2020). The research did not reveal any significant difference in the type of bacteria, but the percentage of microorganisms was higher on staff smartphones. All of the articles examined in this review stressed the importance of hygiene measures demonstrated an important reduction in bacterial contamination after smartphone disinfection (Khashei et al., 2019; Kirkby et al., 2016; Kotris et al., 2017; Murgier et al., 2016). Currently, the only interventions that can reduce the possibility of cross-transmission are hand washing, respect for the five moments, and education of nurses, doctors, hospital staff, and family members to comply with hygiene rules. This systematic review is not without its limitations. In fact, it represents a preliminary study to analyze the phenomenon of interest. The main objective was in fact to identify the presence of bacteria on mobile phones and whether their use during clinical practice increases the risk of infection. The results obtained suggest that in order to determine this risk, it would be appropriate to do experimental studies.
Patient safety is a priority of all healthcare systems and services, such as the prevention of medication errors and the control of healthcare-associated infections (Giannetta et al., 2020; Márquez-Hernández et al., 2019). On this topic, the use of smartphones in nursing practice can affect patient safety also due to distraction (Di Muzio et al., 2019).
The review significantly shows how smartphones represent a reservoir of both pathogenic and non-pathogenic microorganisms. The implementation of guidelines on the cleaning and disinfection of smartphones within the various care settings, and further studies in this regard, would allow us to further investigate the field of study. The need to strengthen and follow the guidelines for the control and prevention of the spread of healthcare-related infections is evident (Khashei et al., 2019; Kirkby et al., 2016; Kotris et al., 2017; Murgier et al., 2016). All staff involved in patient care must be aware of the damage that an infection could cause. It is therefore important to respect hand hygiene as suggested by the WHO guidelines (WHO, 2020). The high rate of isolated MRSA, the consequent difficulty in treating infections caused by antibiotic-resistant microorganisms, makes it necessary to implement interventions in order to prevent them. In some Italian hospitals, policies have already been applied to restrict the use of smartphones during the work shift (Fiorinelli et al., 2021). This intervention stems from the responsibility that their use in the workplace can interfere both with the quality of service and with the transmission of nosocomial infections. This limitation not only applies to health professionals but has also been extended to parents and family members. The data concerning the effects that the use of mobile devices produce on the quality of care suggest the need to promote information and training programs in order to sensitize nurses and the whole team on the potential harmful effects and to promote a better clinical use. Future studies should aim at obtaining consistent data on the use of telephones during nursing care since the nurse is the one who is in direct contact with patients.
Conclusion and Recommendations
By carrying out numerous procedures every day, the risk of carrying pathogens and thus causing the patient to contract a nosocomial infection is certainly higher than for any other healthcare professional. It is therefore important to focus on this aspect in the near future so that it is possible to develop new best practices, implement existing ones in order to support good nursing practices, and minimize the incidence of care-related infections caused by incorrect handling of mobile devices. Smartphones and new technologies have made and can still make significant improvements in assistance. Their use should not be prohibited but rather a regulation on their use and good disinfection practices to be followed would ensure excellent quality care.
Author Contributions:
Concept – S.D.M., N.G.; Design – S.D., S.D.M.; Supervision – M.D.M., N.G.; Resources – S.D.M., G.L.; Materials – C.C., E.D.S.; Data Collection and/or Processing – S.D.M, G.L.; Analysis and/or Interpretation – S.D.M, G.L.; Literature Search – S.D.M, G.L.; Writing Manuscript – N.G., S.D.; Critical Review – M.D.M., N.G.
Footnotes
Ethics Committee Approval: This study was not approved by Ethics committee because it is a systematic review.
Informed Consent: N/A.
Peer Review: Externally peer-reviewed.
Declaration of Interests: The authors have no conflicts of interest to declare.
Funding: The authors declared that this study has received no financial support.
References
- Abdali N., Younas F., Mafakheri S., Pothula K. R., Kleinekathöfer U., Tauch A., Benz R. (2018). Identification and characterization of smallest pore-forming protein in the cell wall of pathogenic Corynebacterium urealyticum DSM 7109. BMC Biochemistry, 19(1), 3. 10.1186/s12858-018-0093-9) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Di Muzio M., Napoli C., Fiorinelli M., Orsi G. B. (2019). Nurses distracted by smartphone use during clinical practice: Italian validation of the “Nurses’ use of Personal Communication Devices (PCD) questionnaire”. Applied Nursing Research, 49, 23–28. 10.1016/j.apnr.2019.07.008) [DOI] [PubMed] [Google Scholar]
- Dorost A., Safari Y., Akhlaghi M., Soleimani M., Yoosefpour N. (2018). Microbial contamination data of keypad and touch screen of cell phones among hospital and non-hospital staffs – A case study: Iran. Data in Brief, 20, 80–84. 10.1016/j.dib.2018.07.041) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fiorinelli M., Di Mario S., Surace A., Mattei M., Russo C., Villa G., Dionisi S., Di Simone E., Giannetta N., Di Muzio M. (2021). Smartphone distraction during nursing care: Systematic literature review. Applied Nursing Research, 58, 151405. 10.1016/j.apnr.2021.151405) [DOI] [PubMed] [Google Scholar]
- Galazzi A., Panigada M., Broggi E., Grancini A., Adamini I., Binda F., Mauri T., Pesenti A., Laquintana D., Grasselli G., Pesenti A., Laquintana D., Grasselli G. (2019). Microbiological colonization of healthcare workers’ mobile phones in a tertiary-level Italian intensive care unit. Intensive and Critical Care Nursing, 52, 17–21. 10.1016/j.iccn.2019.01.005) [DOI] [PubMed] [Google Scholar]
- Giannetta N., Dionisi S., Cassar M., Trapani J., Renzi E., Di Simone E., Di Muzio M. (2020). Measuring knowledge, attitudes and behavior of nurses in medication management: Cross-cultural comparisons in Italy and Malta. European Review for Medical and Pharmacological Sciences, 24(9), 5167–5175. 10.26355/eurrev_202005_21212) [DOI] [PubMed] [Google Scholar]
- Kanayama A. K., Takahashi H., Yoshizawa S., Tateda K., Kaneko A., Kobayashi I. (2017). Staphylococcus aureus surface contamination of mobile phones and presence of genetically identical strains on the hands of nursing personnel. American Journal of Infection Control, 45(8), 929–931. 10.1016/j.ajic.2017.02.011) [DOI] [PubMed] [Google Scholar]
- Kavanagh B. P. 2009). The GRADE system for rating clinical guidelines. PLoS Medicine, 6(9), e1000094. 10.1371/journal.pmed.1000094) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khashei R., Ebrahim-Saraie H. S., Hadadi M., Ghayem M., Shahraki H. R. (2019). The occurrence of nosocomial pathogens on cell phones of healthcare workers in an Iranian tertiary care hospital. Infectious Disorders Drug Targets, 19(3), 327–333. 10.2174/1871526518666180830165732) [DOI] [PubMed] [Google Scholar]
- Kirkby S., Biggs C., Ikuta L., Zukowsky K. (2016). Cell phones in the neonatal intensive care unit: How to Eliminate Unwanted Germs. Advances in Neonatal Care, 16(6), 404–409. 10.1097/ANC.0000000000000328) [DOI] [PubMed] [Google Scholar]
- Kotris I., Drenjančević D., Talapko J., Bukovski S. (2017). Identification of microorganisms on mobile phones of intensive care unit health care workers and medical students in the tertiary hospital. Medicinski Glasnik, 14(1), 85–90. 10.17392/878-16) [DOI] [PubMed] [Google Scholar]
- Márquez-Hernández V. V., Fuentes-Colmenero A. L., Cañadas-Núñez F., Di Muzio M., Giannetta N., Gutiérrez-Puertas L. (2019). Factors related to medication errors in the preparation and administration of intravenous medication in the hospital environment. PLoS One, 14(7), e0220001. 10.1371/journal.pone.0220001) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moher D., Liberati A., Tetzlaff J., Altman D. G. (2009. a). Linee guida per il reporting di revisioni sistematiche e meta-analisi: Il PRISMA statement. Evidence, 7(6), e1000114. [Google Scholar]
- Moher D., Liberati A., Tetzlaff J., Altman D. G., & Prisma Group. (2009. b). Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA statement. PLoS Medicine, 6(7), e1000097. 10.1371/journal.pmed.1000097) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morvai J., Szabó R. (2015). The role of mobile communication devices in the spread of infections. Orvosi Hetilap, 156(20), 802–807. 10.1556/650.2015.30147) [DOI] [PubMed] [Google Scholar]
- Murgier J., Coste J. F., Cavaignac E., Bayle-Iniguez X., Chiron P., Bonnevialle P., Laffosse J. M. (2016). Microbial flora on cell-phones in an orthopedic surgery room before and after decontamination. Orthopaedics and Traumatology, Surgery and Research, 102(8), 1093–1096. 10.1016/j.otsr.2016.09.014) [DOI] [PubMed] [Google Scholar]
- Pillet S., Berthelot P., Gagneux-Brunon A., Mory O., Gay C., Viallon A., Lucht F., Pozzetto B., Botelho-Nevers E., Pozzetto B., Botelho-Nevers E. (2016). Contamination of healthcare workers’ mobile phones by epidemic viruses. Clinical Microbiology and Infection, 22(5), 456.e1–456.e6. 10.1016/j.cmi.2015.12.008) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Qureshi N. Q., Mufarrih S. H., Irfan S., Rashid R. H., Zubairi A. J., Sadruddin A., Ahmed I., Noordin S., Noordin S. (2020). Mobile phones in the orthopedic operating room: Microbial colonization and antimicrobial resistance. World Journal of Orthopedics, 11(5), 252–264. 10.5312/wjo.v11.i5.252) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shah P. D., Shaikh N. M., Dholaria K. V. (2019). Microorganisms isolated from mobile phones and hands of health-care workers in a tertiary care hospital of Ahmedabad, Gujarat, India. Indian Journal of Public Health, 63(2), 147–150. 10.4103/ijph.IJPH_179_18) [DOI] [PubMed] [Google Scholar]
- Simmonds R., Lee D., Hayhurst E. (2020). Mobile phones as fomites for potential pathogens in hospitals: Microbiome analysis reveals hidden contaminants. Journal of Hospital Infection, 104(2), 207–213. 10.1016/j.jhin.2019.09.010) [DOI] [PubMed] [Google Scholar]
- Tschopp C., Schneider A., Longtin Y., Renzi G., Schrenzel J., Pittet D. (2016). Predictors of heavy stethoscope contamination following a physical examination. Infection Control and Hospital Epidemiology, 37(6), 673–679. 10.1017/ice.2016.40) [DOI] [PubMed] [Google Scholar]
- Ustun C., Cihangiroglu M. (2012). Health care workers’ mobile phones: A potential cause of microbial cross-contamination between hospitals and community. Journal of Occupational and Environmental Hygiene, 9(9), 538–542. 10.1080/15459624.2012.697419) [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization (WHO). (2011). WHO mHealth: New horizons for health through mobile technologies: Second global survey on eHealth [ISBN 972-92-4-156425-0]. [Google Scholar]
- World Health Organization (WHO). (2020). WHO guidelines on hand hygiene in health care. Retrieved from http://apps.who.int/iris/bitstream/10665/44102/1/9789241597906_eng.pdf. [Google Scholar]



 Content of this journal is licensed under a
Content of this journal is licensed under a