Key Points
Question
Among patients with type 2 diabetes in an integrated health care system with minimal medication cost-sharing, does prescription of sodium-glucose cotransporter-2 inhibitors (SGLT2i) and glucagon-like peptide-1 receptor agonists (GLP-1 RA) differ by race and ethnicity?
Findings
In this cross-sectional study that included 1 197 914 patients in the Veterans Health Administration system, the proportion of patients with an active prescription was 10.7% for SGLT2i and 7.7% for GLP-1 RA. Individuals of several different racial groups and those of Hispanic ethnicity had statistically significantly lower odds of receiving prescriptions for these medications compared with individuals of White race and non-Hispanic ethnicity.
Meaning
Among patients with type 2 diabetes in the Veterans Health Administration system, prescription of SGLT2i and GLP-1 RA was low overall, and there were differences in prescribing by race and ethnicity.
Abstract
Importance
Novel therapies for type 2 diabetes can reduce the risk of cardiovascular disease and chronic kidney disease progression. The equitability of these agents’ prescription across racial and ethnic groups has not been well-evaluated.
Objective
To investigate differences in the prescription of sodium-glucose cotransporter-2 inhibitors (SGLT2i) and glucagon-like peptide-1 receptor agonists (GLP-1 RA) among adult patients with type 2 diabetes by racial and ethnic groups.
Design, Setting, and Participants
Cross-sectional analysis of data from the US Veterans Health Administration’s Corporate Data Warehouse. The sample included adult patients with type 2 diabetes and at least 2 primary care clinic visits from January 1, 2019, to December 31, 2020.
Exposures
Self-identified race and self-identified ethnicity.
Main Outcomes and Measures
The primary outcomes were prevalent SGLT2i or GLP-1 RA prescription, defined as any active prescription during the study period.
Results
Among 1 197 914 patients (mean age, 68 years; 96% men; 1% American Indian or Alaska Native, 2% Asian, Native Hawaiian, or Other Pacific Islander, 20% Black or African American, 71% White, and 7% of Hispanic or Latino ethnicity), 10.7% and 7.7% were prescribed an SGLT2i or a GLP-1 RA, respectively. Prescription rates for SGLT2i and GLP-1 RA, respectively, were 11% and 8.4% among American Indian or Alaska Native patients; 11.8% and 8% among Asian, Native Hawaiian, or Other Pacific Islander patients; 8.8% and 6.1% among Black or African American patients; and 11.3% and 8.2% among White patients, respectively. Prescription rates for SGLT2i and GLP-1 RA, respectively, were 11% and 7.1% among Hispanic or Latino patients and 10.7% and 7.8% among non-Hispanic or Latino patients. After accounting for patient- and system-level factors, all racial groups had significantly lower odds of SGLT2i and GLP-1 RA prescription compared with White patients. Black patients had the lowest odds of prescription compared with White patients (adjusted odds ratio, 0.72 [95% CI, 0.71-0.74] for SGLT2i and 0.64 [95% CI, 0.63-0.66] for GLP-1 RA). Patients of Hispanic or Latino ethnicity had significantly lower odds of prescription (0.90 [95% CI, 0.88-0.93] for SGLT2i and 0.88 [95% CI, 0.85-0.91] for GLP-1 RA) compared with non-Hispanic or Latino patients.
Conclusions and Relevance
Among patients with type 2 diabetes in the Veterans Health Administration system during 2019 and 2020, prescription rates of SGLT2i and GLP-1 RA medications were low, and individuals of several different racial groups and those of Hispanic ethnicity had statistically significantly lower odds of receiving prescriptions for these medications compared with individuals of White race and non-Hispanic ethnicity. Further research is needed to understand the mechanisms underlying these differences in rates of prescribing and the potential relationship with differences in clinical outcomes.
This cross-sectional analysis of data from the US Veterans Health Administration investigates differences in the prescription of sodium-glucose cotransporter-2 inhibitors (SGLT2i) and glucagon-like peptide-1 receptor agonists (GLP-1 RA) among adult patients with type 2 diabetes by racial and ethnic groups.
Introduction
Achieving pharmacoequity is central to overcoming health care disparities that persist across race and ethnic groups.1 Racial and ethnic minority individuals have been less likely than White persons to be prescribed novel guideline-recommended therapies with proven effectiveness.1,2 These disparities may be particularly salient among patients with type 2 diabetes because Asian, Black, and Hispanic or Latino persons have a higher prevalence of diabetes and its complications than White patients.3,4,5 Therefore, evaluating whether health care disparities exist in the prescription of guideline-recommended therapies that could reduce the cardiovascular and kidney complications of diabetes is of public health importance.
The advent of sodium-glucose cotransporter-2 inhibitors (SGLT2i) and glucagon-like peptide-1 receptor agonists (GLP-1 RA) has changed the approach to the management of type 2 diabetes because both classes have cardiovascular and kidney protective effects. Rather than relying on a glucose-centric approach to diabetes management and control, current guidelines recommend inclusion of these therapies to lower the risks of cardiovascular disease and chronic kidney disease (CKD) progression.6,7 Recent research has shown that Black patients are less likely than White patients to be prescribed these therapies.8,9 However, prescription was strongly associated with income, which may have influenced the results given the high cost-sharing incurred by patients for these medications.10
The primary objective of this study was to evaluate prescription patterns of SGLT2i and GLP-1 RA across racial and ethnic groups in the Veterans Health Administration (VHA) system from January 1, 2019, to December 31, 2020. The VHA is the largest integrated health system in the US and provides uniform pharmacy access that offers discounted or free medications to patients, thereby minimizing the influence of medication costs.
Methods
This study was deemed minimal risk and was approved by the University of California, San Francisco institutional review board (19-29496). Participant informed consent was waived by the institutional review board.
Study Design, Setting, and Participants
We conducted a cross-sectional study to establish the prevalence of SGLT2i and GLP-1 RA prescription from January 1, 2019, to December 31, 2020, among patients with type 2 diabetes using the VHA Corporate Data Warehouse. It contains individual-level information on sociodemographic characteristics, outpatient and inpatient clinical encounters, medication prescriptions and fills, medical conditions, procedures, and laboratory results. It also organizes the 171 VHA medical centers and 1283 outpatient facilities into 130 distinct health care networks known as VHA stations. Patients were assigned to one of these stations based on where they received most of their health care within the VHA.
Type 2 diabetes was ascertained by adapting the Electronic Medical Records and Genomics Network algorithm for ascertainment of diabetes in electronic health records.11,12 It combines International Classification of Diseases (ICD) codes, hemoglobin A1C values, and diabetes medication use (eFigure 1 in the Supplement). We included all VHA patients with type 2 diabetes who had at least 2 primary care encounters during the study period (eFigure 2 in the Supplement).
Exposures
Race and ethnicity at the VHA are ascertained through a 2-question self-identified method included in the VHA Form 10-10EZ at the time of application for health benefits or at the time of inpatient or outpatient visits to a VHA facility.13,14 The first question asks patients to classify their ethnicity: Hispanic or Latino (yes or no; hereafter referred to as Hispanic) (eTable 1 in the Supplement). The second question asks patients to classify their race (>1 classification may be selected): American Indian or Alaska Native; Asian; Black or African American (hereafter referred to as Black); Native Hawaiian or Other Pacific Islander; White; and unknown race by patient or declined to answer. If self-identification of race and ethnicity is impossible, these categories may be assigned by a proxy or by a VHA enrollment coordinator/clerk. In this sample, more than 99% of the race and ethnicity categories were self-identified. Because relatively few patients self-identified as Native Hawaiian or Other Pacific Islander, we combined those individuals with the Asian group. We included those with unknown or declined to answer in an “unknown” race category. We also created a multiracial category for patients who marked more than 1 race category. Race and ethnicity groups were analyzed separately.
Covariates
Covariates were ascertained at baseline prior to January 1, 2019 (first day of the study period), with a look-back to October 1, 2015, when migration from ICD-9 to ICD-10 codes occurred. Exceptions were variables that denoted clinical care such as primary care, endocrinology, cardiology, or nephrology visits; patient residence; COVID-19 diagnoses; and all diabetes medication prescriptions, for which ascertainment was extended to December 31, 2020. Because the VHA does not collect individual-level information on socioeconomic characteristics, we used the median per capita income of residential zip code and the zip code–level Social Deprivation Index as proxies for socioeconomic status using data derived from the American Community Survey.15,16 We assessed rurality using Rural-Urban Commuting Area codes, which consider population density and closeness of a community’s socioeconomic linkage to large urban centers.17 We used the VHA service-connection disability information as proxies for medication cost-sharing.18 Patients do not have co-payments for their medications if they have more than 50% health coverage for service-connected conditions and those for whom diabetes is a service-connected condition.
For system-level characteristics, we used the VHA 4-tier facility complexity rating, which encompasses facility volume, intensive care availability, number of subspecialists per patient, and teaching/research capacity (eTable 2 in the Supplement). This rating is assigned to each station based on the classification of the parent facility within the station. To assess the geographic location of each VHA station, we used the Census Bureau classification of US Regions and Divisions. eTable 3 in the Supplement summarizes covariate descriptions.
Outcomes
Across each race and ethnicity category, we assessed the prevalence of SGLT2i and GLP-1 RA prescription, defined as any active prescription, including VHA formulary and nonformulary medications, from January 1, 2019, through December 31, 2020. For SGLT2i, ertugliflozin, canagliflozin, dapagliflozin, and empagliflozin were evaluated. For GLP-1 RA, semaglutide, liraglutide, albiglutide, and dulaglutide were evaluated because they have demonstrated protective cardiovascular effects. Only empagliflozin and semaglutide are included in the VHA national formulary; however, clinicians can prescribe nonformulary medications with prior authorization.
Statistical Analysis
The association of race and ethnicity categories with SGLT2i and GLP-1 RA prescription was examined using multilevel, multivariable mixed-effect models with VHA station–specific random intercepts. Adjusted odds ratios (ORs) were calculated from models that specified a binomial distribution with a logit link function and included station-specific random effects following previously published methods.19 The models were 2 level, with individual patients clustered within VHA stations. To estimate prescription prevalence, we fitted 4 sequential multilevel models separately for SGLT2i and GLP-1 RA prescription: (1) a model with only the VHA station random intercept; (2) a model that added patient-level demographic characteristics; (3) a model adding patient-level clinical characteristics; and (4) a final model adding VHA station–level characteristics: facility complexity rating and Census division.
Age-adjusted rates of SGLT2i and GLP-1 RA prescription across race and ethnicity groups were calculated using predicted probabilities from multilevel logistic models that included a random intercept with race and ethnicity categories as predictors.20 Absolute risk differences were calculated from the sequential multilevel logistic regression models with conditional predicted probabilities for each race and ethnicity group, age set to the mean value, and balanced levels for categorical covariates so that all levels within a given covariate were equal. The differences from those predicted probabilities (absolute risk differences) were calculated, comparing all other race groups with White patients and Hispanic patients with non-Hispanic patients. Overall model discrimination was assessed with C-statistic calculations for models that included random intercepts and patient-level characteristics and for models that added system-level characteristics.
Analyses comparing SGLT2i and GLP-1 RA prescription within each race category vs White race and among Hispanic vs non-Hispanic ethnicity were conducted, stratifying by patient- and system-level characteristics. For all models, adjusted ORs were obtained using multivariable logistic regression. Because of the potential for type I error from multiple comparisons, findings for these analyses should be interpreted as exploratory. Additional analyses calculated incident prescription rates (eAppendix in the Supplement) using regression models that adjusted for age, sex, race, ethnicity, and CKD status and specified a Poisson distribution with a log link function.
To assess the relative contribution of the VHA station–level characteristics to overall prescription, we calculated the median ORs and the intraclass correlation coefficient (ICC). The median OR allows for quantifying heterogeneity between clusters.19,21,22 It compares the prescription prevalences between individuals from VHA stations with different prescription prevalences but same patient-level covariate values. The ICC is the relative proportion of cluster variance to total variance (ie, higher ICC signifies larger variability attributable to VHA station differences). ICCs were first calculated for the null models to estimate the proportion of SGLT2i and GLP-1 RA prescription variation attributable to the VHA stations. Subsequently, we calculated ICCs for VHA stations in models that adjusted for patient-level characteristics.
When missing data were present, an indicator variable denoted as “unknown” was entered in the regression models. All primary and secondary analyses of the study outcomes used 2-sided testing and an α = .05. All statistical analyses were conducted using SAS software version 9.4.6 of the SAS system for Unix (SAS Institute Inc). Sensitivity analyses are described in the eAppendix in the Supplement. Tolerances for assessment of multicollinearity were greater than 0.1 and all variance inflation factors less than 2.2. The ratio of the Pearson χ2 was less than 1, indicating properly modeled variability.
Results
The study sample comprised 1 197 914 patients with type 2 diabetes, of whom 10.7% and 7.7% were prescribed an SGLT2i or a GLP-1 RA, respectively (eFigure 2 in the Supplement). The mean (SD) age of the sample was 68 (10) years, and 96% were male. Race and ethnicity categories were distributed as follows: 1% American Indian or Alaska Native; 2% Asian, Native Hawaiian, or Other Pacific Islander; 20% Black; 71% White; and 7% of Hispanic ethnicity (Table). The frequency of missing data was low (<5%) across most covariates, and missing data did not significantly differ between racial or ethnic categories.
Table. Demographic and Clinical Characteristics of Patients With Type 2 Diabetes in the Veterans Health Administration System From 2019 to 2020 by Race Categoriesa.
| Characteristic | No. (%) | |||||
|---|---|---|---|---|---|---|
| American Indian or Alaska Native (n = 10 127) | Asian, Native Hawaiian, or Other Pacific Islander (n = 24 663) | Black or African American (n = 234 932) | White (n = 850 648) | Multiracial (n = 9795) | Unknown race (n = 67 749)a | |
| Sociodemographic | ||||||
| Age, mean (SD), y | 65 (11) | 64 (12) | 63 (10) | 69 (10) | 65 (12) | 68 (11) |
| Sex | ||||||
| Female | 557 (6) | 1242 (5) | 18 187 (8) | 25 269 (3) | 617 (6) | 2543 (4) |
| Male | 9570 (94) | 23 421 (95) | 216 745 (92) | 825 379 (97) | 9178 (94) | 65 206 (96) |
| Hispanic or Latino ethnicity | 1349 (13) | 2040 (8) | 3584 (2) | 64 278 (8) | 939 (10) | 12 844 (19) |
| Service-connected disability >50%b | 5374 (53) | 15 563 (63) | 124 927 (53) | 358 836 (42) | 5239 (53) | 30 904 (46) |
| Diabetes service connectionb | 2662 (26) | 7318 (30) | 48 219 (21) | 224 174 (26) | 2333 (24) | 16 360 (24) |
| Lowest zip code median income quartile (income <$44 818) | 3264 (32) | 2885 (12) | 85 538 (36) | 186 233 (22) | 2328 (24) | 16 220 (24) |
| Highest Social Deprivation Index quartile (score >73) | 3391 (33) | 6102 (25) | 106 340 (45) | 150 468 (18) | 2614 (27) | 18 832 (28) |
| Rural or highly rural zip code | 5057 (50) | 3977 (16) | 44 644 (19) | 367 240 (43) | 3120 (32) | 23 505 (35) |
| Lifestyle | ||||||
| Unhealthy alcohol usec | 843 (8) | 1683 (7) | 18 746 (8) | 68 620 (8) | 688 (7) | 5724 (8) |
| Current smoking | 1985 (20) | 3406 (14) | 43 868 (19) | 143 093 (17) | 1865 (19) | 10 269 (15) |
| Diabetes management and control, HbA1c, % | ||||||
| ≤7 | 4700 (46) | 12 019 (49) | 126 258 (54) | 438 173 (52) | 5072 (52) | 33 371 (49) |
| >7-8 | 2134 (21) | 5403 (22) | 44 953 (19) | 200 231 (24) | 2100 (21) | 14 695 (22) |
| >8-9 | 1213 (12) | 2594 (11) | 22611 (10) | 90 275 (11) | 1062 (11) | 7008 (10) |
| >9 | 1406 (14) | 2739 (11) | 28917 (12) | 73 232 (9) | 1067 (11) | 6760 (10) |
| Unknown | 674 (7) | 1908 (8) | 12193 (5) | 48 737 (6) | 494 (5) | 5915 (9) |
| Lifetime maximum HbA1c level, % | ||||||
| Mean (SD) | 9.1 (2) | 8.7 (2) | 9.0 (3) | 8.6 (2) | 8.9 (2) | 8.7 (2) |
| Median (IQR) | 8.7 (7.2-10.6) | 8.2 (7.0-10.0) | 8.3 (6.9-10.6) | 8.2 (7.1-9.8) | 8.4 (7.1-10.3) | 8.2 (7.1-10.0) |
| Clinical characteristics | ||||||
| Hypertension | 8856 (87) | 21 433 (87) | 215 486 (92) | 766 377 (90) | 8891 (91) | 58 127 (78) |
| BMI ≥30 | 5926 (59) | 11 013 (45) | 133 893 (57) | 480 217 (56) | 5578 (57) | 36 748 (54) |
| CKD | 2583 (26) | 6411 (26) | 49 524 (21) | 251 752 (30) | 2571 (26) | 18 190 (27) |
| Unknown CKD | 2311 (23) | 6820 (28) | 67 993 (29) | 201 885 (24) | 2314 (24) | 18 373 (27) |
| ASCVD | 2324 (23) | 4589 (19) | 39 209 (17) | 243 897 (29) | 2276 (23) | 15 181 (22) |
| Heart failure | 577 (6) | 1092 (4) | 14 963 (6) | 58 994 (7) | 676 (7) | 3689 (5) |
| VHA station parent facility complexity leveld | ||||||
| 1a (Highest) | 3383 (33) | 12 405 (50) | 113 848 (48) | 347 922 (41) | 4083 (42) | 33 345 (49) |
| 1b (High) | 2164 (21) | 3805 (15) | 56 435 (24) | 121 167 (14) | 1807 (18) | 10 311 (15) |
| 1c (Mid-high) | 1235 (12) | 1823 (7) | 35 792 (15) | 139 034 (16) | 1327 (14) | 7933 (12) |
| 2 (Medium) | 1708 (17) | 1276 (5) | 18 501 (8) | 125 404 (15) | 1326 (14) | 8358 (12) |
| 3 (Low) | 1601 (16) | 4076 (17) | 9703 (4) | 114 057 (13) | 1209 (12) | 7631 (11) |
| Census region of VHA station | ||||||
| South | 3945 (39) | 6559 (27) | 156 987 (67) | 360 166 (42) | 4583 (47) | 27 662 (41) |
| West | 3826 (38) | 13 719 (53) | 22 645 (10) | 154 481 (18) | 2383 (24) | 21 275 (31) |
| Midwest | 1800 (18) | 1911 (8) | 33 787 (14) | 209 175 (25) | 1551 (16) | 12 919 (19) |
| Northeast | 514 (5) | 1049 (6) | 19 792 (8) | 112 807 (13) | 1155 (12) | 4893 (7) |
Abbreviations: ASCVD, atherosclerotic cardiovascular disease; BMI, body mass index (calculated as weight in kilograms divided by height in meters squared); CKD, chronic kidney disease; GLP-1 RA, glucagon-like peptide-1 receptor agonist; HbA1c, hemoglobin A1c; SGLT2i, sodium-glucose cotransporter 2 inhibitor; VHA, Veterans Health Administration.
The VHA collects race and ethnicity information based on a 2-question self-identified method. The first question asks patients to classify their ethnicity: Hispanic or Latino (yes or no). The second question asks patients to classify their race (>1 classification may be selected): American Indian or Alaska Native; Asian; Black or African American; Native Hawaiian or Other Pacific Islander; White; and unknown race by patient or declined to answer.
The VHA assigns a given disability (eg, diabetes) a rating to indicate the severity of their service-connected condition. Patients with a disability rating greater than 50% and those for whom diabetes is a service-connected condition do not have co-payments for their medications.
Alcohol Use Disorder Identification Test score of 3 or greater for women and 4 or greater for men.
VHA complexity rating is assigned to each VHA station based on the classification of the parent facility within the station encompassing facility volume, intensive care availability, number of subspecialists per patient, and teaching/research capacity.
Race and Ethnicity Differences in the Prescription of SGLT2i and GLP-1 RA
The crude proportions with prescription for SGLT2i and GLP-1 RA, respectively, were 11% and 8.4% among American Indian or Alaska Native patients; 11.8% and 8.0% among Asian, Native Hawaiian, or Other Pacific Islander patients; 8.8% and 6.1% among Black patients; 11.3% and 8.2% among White patients; 11.5% and 8.7% among multiracial patients; and 10% and 7% among patients with unknown race. Prescription rates for SGLT2i and GLP-1 RA, respectively, were 11% and 7.1% among Hispanic patients and 10.7% and 7.8% among non-Hispanic patients. In age-adjusted models, absolute prescription rates for SGLT2i and GLP-1 RA, respectively, were 8.3% (95% CI, 7.4%-9.2%) and 8.5% (95% CI, 7.4%-9.6%) among American Indian or Alaska Native patients; 8.6% (95% CI, 7.8%-9.5%) and 6.9% (95% CI, 6.1%-7.8%) among Asian, Native Hawaiian, or Other Pacific Islander patients; 6.8% (95% CI, 6.2%-7.5%) and 6.3% (95% CI, 5.6%-7.0%) among Black patients; 9.6% (95% CI, 8.7%-10.5%) and 9.5% (95% CI, 8.5%-10.5%) among White patients; 8.4% (95% CI, 7.5%-9.4%) and 8.7% (95% CI, 7.6%-9.8%) among multiracial patients; and 8.5% (95% CI, 7.7%-9.3%) and 7.9% (95% CI, 7.0%-8.8%) among patients of unknown race. In age-adjusted models, absolute prescription rates for SGLT2i and GLP-1 RA were 8.3% (95% CI, 7.5%-9.1%) and 7.7% (95% CI, 6.8%-8.5%) among Hispanic patients and 8.6% (95% CI, 7.8%-9.4%) and 8.1% (95% CI, 7.2%-8.9%) among non-Hispanic patients, respectively.
All racial groups had statistically significant lower odds and absolute risk differences of SGLT2i and GLP-1 RA prescription compared with White individuals after adjusting for patient- and system-level characteristics (Figure 1 and Figure 2; eFigures 3 and 4 in the Supplement). Compared with White patients, the odds of prescription for SGLT2i and GLP-1 RA, respectively, were 0.85 (95% CI, 0.80-0.92) and 0.89 (95% CI, 0.82-0.97) for American Indian or Alaska Native patients; 0.95 (95% CI, 0.91-1.0) and 0.80 (95% CI, 0.76-0.85) for Asian, Native Hawaiian, or Other Pacific Islander patients; 0.72 (95% CI, 0.71-0.74) and 0.64 (95% CI, 0.63-0.66) for Black patients; 0.88 (95% CI, 0.82-0.94) and 0.90 (95% CI, 0.83-0.97) for multiracial patients; and 0.92 (95% CI, 0.90-0.95) and 0.87 (95% CI, 0.84-0.91) for patients of unknown race. The absolute risk differences for SGLT2i and GLP-1 RA prescription, respectively, were −1.8% (95% CI, −2.5% to −1.0%) and −1.0% (95% CI, −1.7% to −0.3%) for American Indian or Alaska Native patients; −0.5% (95% CI, −1.1% to 0%) and −1.9% (95% CI, −2.4% to −1.3%) for Asian, Native Hawaiian, or Other Pacific Islander patients; −3.4% (95% CI, −3.9% to −2.9%) and −3.4% (95% CI, −4.1% to −2.8%) for Black patients; −1.5% (95% CI, −2.3% to −0.7%) and −0.9% (95% CI, −1.6% to −0.2%) for multiracial patients; and −0.9% (95% CI, −1.3% to −0.5%) and −1.2% (95% CI, −1.6% to −0.8%) for patients of unknown race. Compared with non-Hispanic ethnicity, the odds of prescription among Hispanic patients were 0.90 (95% CI, 0.88-0.93) for SGLT2i and 0.88 (95% CI, 0.85-0.91) for GLP-1 RA. Absolute risk differences were −1.1% (95% CI, −1.4% to −0.8%) for SGLT2i and −1.0% (95% CI, −1.3 to −0.7%) for GLP-1 RA.
Figure 1. Association Between Race and Ethnicity Groups and Sodium-Glucose Cotransporter-2 Inhibitor (SGLT2i) Prescription With Sequential Adjustment for Patient- and System-Level Characteristics.
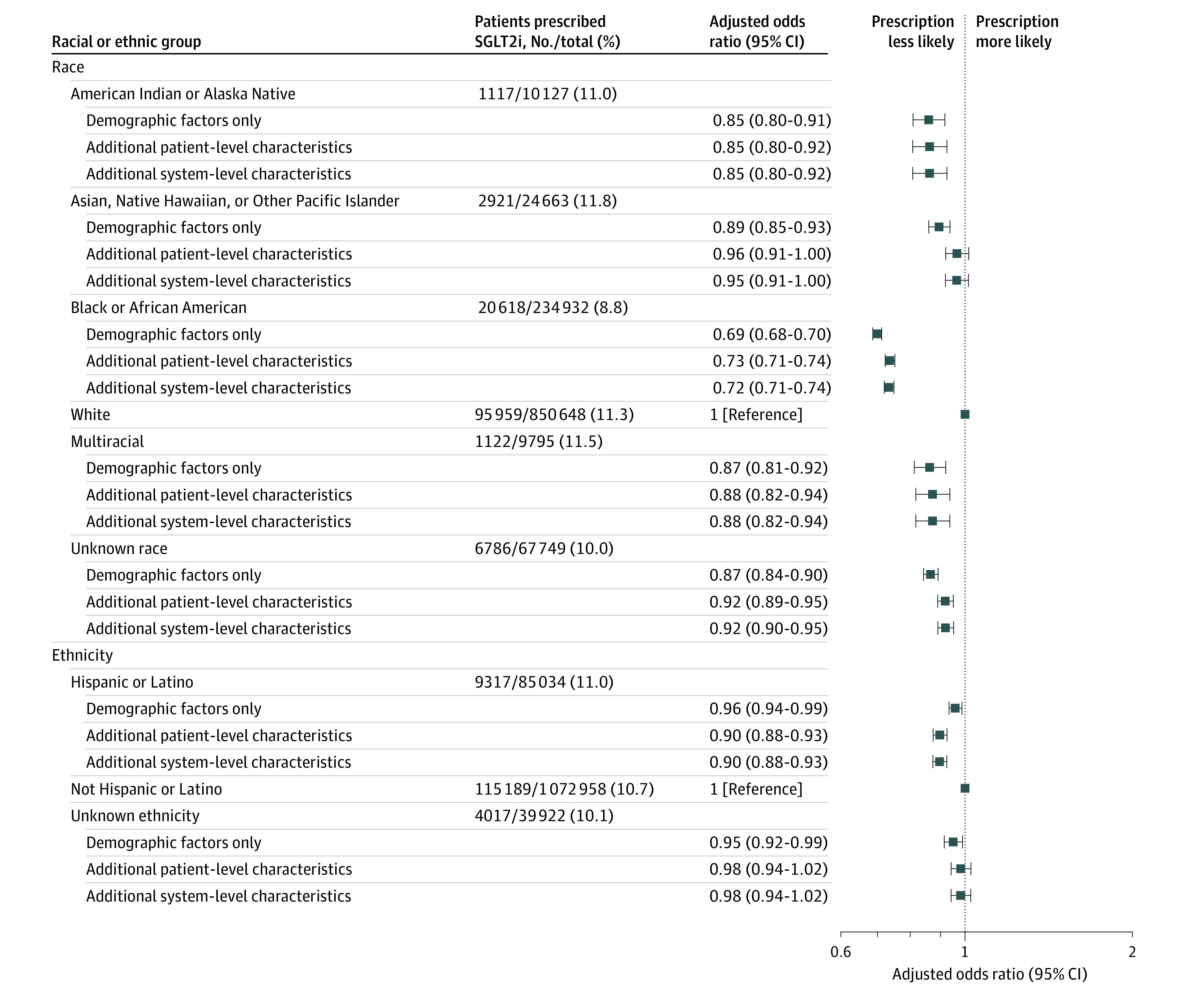
The demographic factors only model includes age, sex, and self-identified race and ethnicity. The additional patient-level characteristics model includes demographic factors and zip code median income; zip code Social Deprivation Index; Veterans Health Administration (VHA) diabetes and service connection; rurality; smoking status; unhealthy alcohol use; hemoglobin A1C level; other antidiabetic agents; hypertension; body mass index; mental health diagnosis; atherosclerotic cardiovascular disease; heart failure; no chronic kidney disease; chronic kidney disease: estimated glomerular filtration rate and albuminuria categories; number of primary care, cardiology, endocrinology, and nephrology visits; VHA frailty index; and COVID-19 diagnosis. The additional system-level characteristics model includes VHA station parent facility-complexity level and US Census division.
Figure 2. Association Between Race and Ethnicity Groups and Glucagon-like Peptide-1 Receptor Agonist (GLP-1 RA) Prescription With Sequential Adjustment for Patient- and System-Level Characteristics.
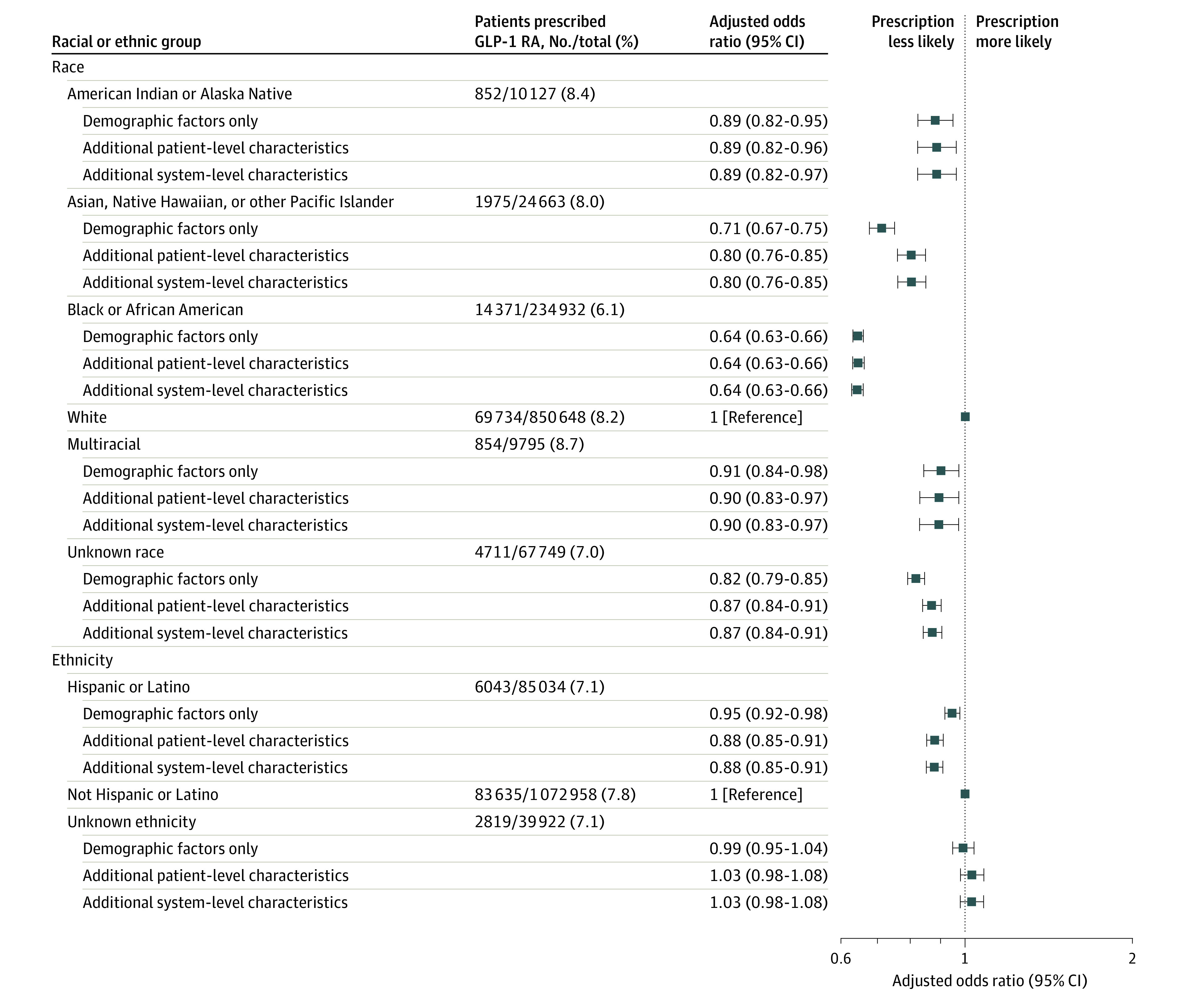
The demographic factors only model includes age, sex, and self-identified race and ethnicity. The additional patient-level characteristics model includes demographic factors and zip code median income; zip code Social Deprivation Index; Veterans Health Administration (VHA) diabetes and service connection; rurality; smoking status; unhealthy alcohol use; hemoglobin A1C level; other antidiabetic agents; hypertension; body mass index; mental health diagnosis; atherosclerotic cardiovascular disease; heart failure; no chronic kidney disease; chronic kidney disease: estimated glomerular filtration rate and albuminuria categories; number of primary care, cardiology, endocrinology, and nephrology visits; VHA frailty index; and COVID-19 diagnosis. The additional system-level characteristics model includes VHA station parent facility-complexity level, US Census division.
VHA System–Level Characteristics and SGLT2i and GLP-1 RA Prescription
Across VHA stations, the prescription prevalence ranged from 1.8% to 28.9% for SGLT2i and 1.1% to 20% for GLP-1 RA (eFigures 5 and 6 and eTable 4 in the Supplement for system-level characteristics). For a patient within a VHA station of higher vs lower likelihood for prescription of these medications, the adjusted median ORs were 1.72 (95% CI, 1.61-1.84) for SGLT2i and 1.95 (95% CI, 1.79-2.14) for GLP-1 RA. The between VHA variance in prescription was low (adjusted ICC, 8.9% [95% CI, 7.0%-1.0%] for SGLT2i and 12.9% [95% CI, 10.2%-16.3%] for GLP-1 RA).
Figure 3 and Figure 4 show stratified analyses by patient- and system-level characteristics for the comparison of prescriptions between Black vs White patients and between Hispanic vs non-Hispanic patients, respectively. Except among patients with concurrent diagnosis of heart failure, the results across these strata were qualitatively consistent with the overall findings; however, not all estimates reached statistical significance in the comparisons by ethnicity. eFigures 7, 8, 9, and 10 in the Supplement display the remaining comparisons.
Figure 3. Prescription of Sodium-Glucose Cotransporter-2 Inhibitor (SGLT2i) and Glucagon-like Peptide-1 Receptor Agonist (GLP-1 RA) Comparing Black vs White Patients Across Patient- and System-Level Characteristics.
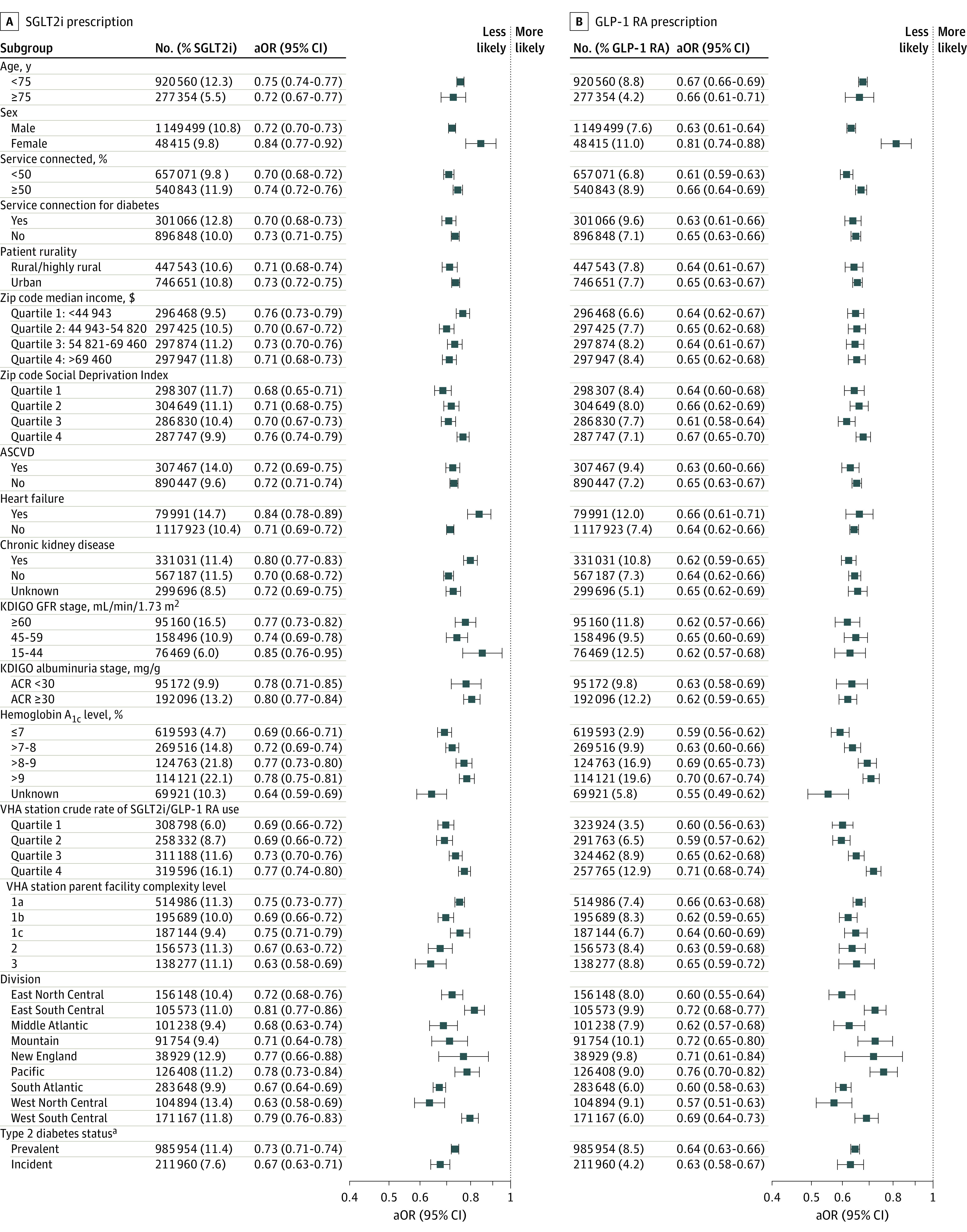
The variables adjusted for in the multivariable models are listed in the Figure 1 legend. Adjusted odds ratios (aORs) <1 indicate Black persons were less likely to receive medications than White persons.
aPrevalent type 2 diabetes includes a diagnosis of type 2 diabetes before January 1, 2019. Incident type 2 diabetes includes a diagnosis between January 1, 2019, and December 31, 2020.
Figure 4. Prescription of Sodium-Glucose Cotransporter-2 Inhibitor (SGLT2i) and Glucagon-like Peptide-1 Receptor Agonist (GLP-1 RA) Comparing Hispanic or Latino Ethnicity vs Not Hispanic or Latino Ethnicity Across Patient- and System-Level Characteristics.
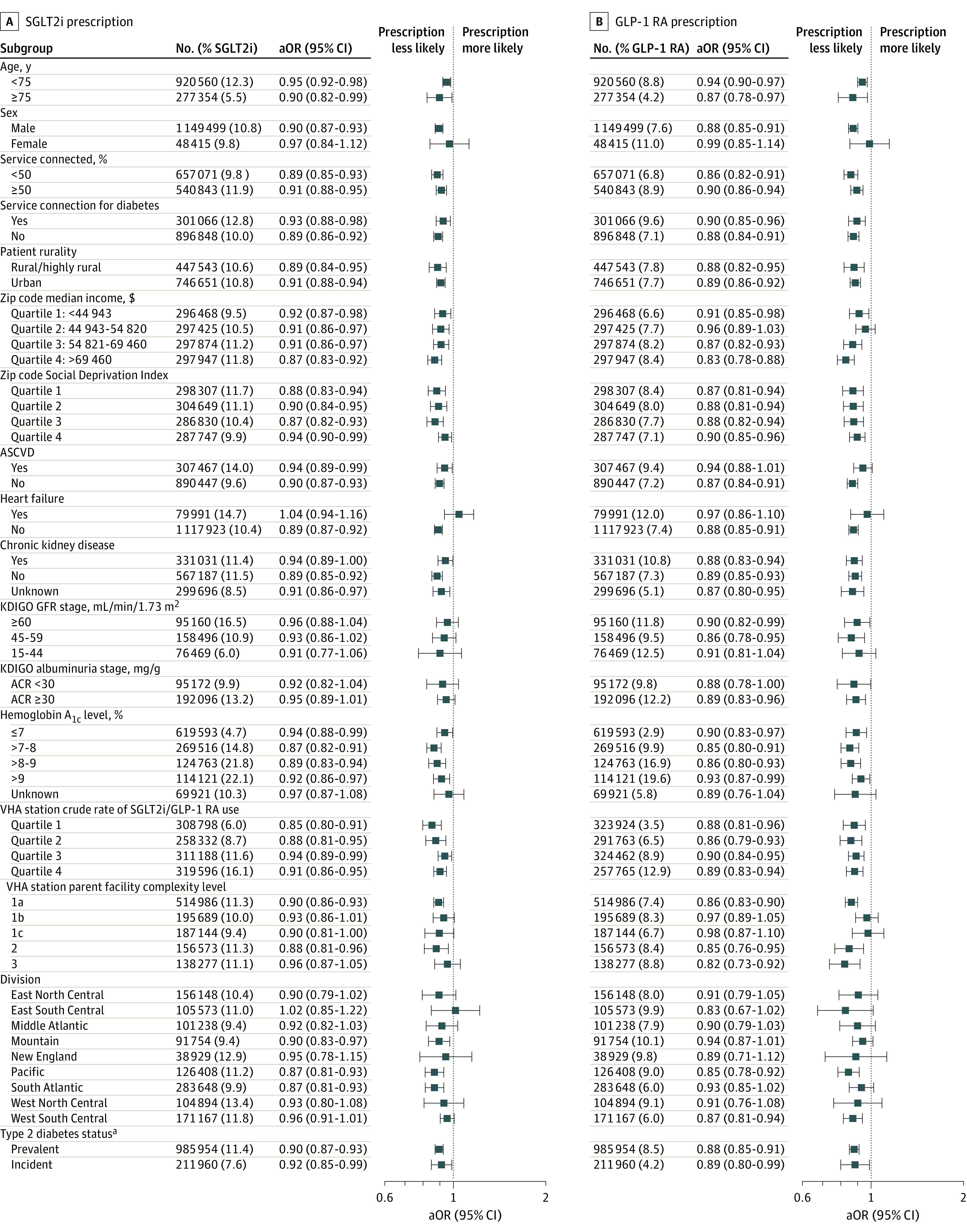
The variables adjusted for in the multivariable models are listed in the Figure 1 legend. Adjusted odds ratios (aORs) <1 indicate Hispanic persons were less likely to receive medications than non-Hispanic persons.
aPrevalent type 2 diabetes includes a diagnosis of type 2 diabetes before January 1, 2019. Incident type 2 diabetes includes a diagnosis between January 1, 2019, and December 31, 2020.
Results of sensitivity analyses were consistent with the main findings, including those stratified by patients’ site of primary care and distance to a VHA facility, those that defined the outcome as 2 prescriptions per year, and those that only assessed incident prescriptions (eTables 5, 6, 7, 8, and 9 and eFigures 11, 12, 13, and 14 in the Supplement). The results from these analyses are summarized in the eAppendix in the Supplement.
Discussion
In this cross-sectional analysis of SGLT2i and GLP-1 RA prescription among more than 1 million patients with type 2 diabetes, prescription rates were low across all racial and ethnic groups. Compared with White patients, those of all other racial groups had significantly lower odds of prescription of these medications. Patients of Hispanic ethnicity had significantly lower odds of these prescriptions compared with non-Hispanic patients, even after accounting for individual- and system-level factors.
These results are consistent with recent research that found low prescription rates of SGLT2i and GLP-1 RA among racial and ethnic minority groups in commercial and Medicare Advantage health plans.8,9 Given the high cost-sharing for these medications,10 this study extends these findings to the VHA where the financial constraints impeding medication access are minimized. Consistent with these analyses and other recent research,23,24 the absolute rates of prescription in this study were low even for patients with concomitant atherosclerotic cardiovascular disease (ASCVD), heart failure, or CKD, the 3 conditions for which guidelines recommend SGLT2i and/or GLP-1 RA prescription irrespective of glycemic control. These findings align with 2 recent VHA studies that found low prescription rates of GLP-1 RA among patients with established ASCVD and similar facility-level variability in SGLT2i and GLP-1 RA prescription.21,25
The observed lower prescription of SGLT2i and GLP-1 RA for all race and ethnic groups relative to White patients and non-Hispanic patients persisted even after accounting for a broad array of patient- and system-level characteristics. Differences in comorbidities, social determinants of health at the zip code level, and access to primary and specialty care did not appear to explain observed racial and ethnic differences in these prescriptions. Indeed, system-level variation was low relative to overall variability in the prescription of SGLT2i and GLP-1 RA.
Racial and ethnic disparities in health and health care are pervasive in the US.26 Although to a smaller magnitude, these disparities have been reproduced in the VHA,27 indicating that financial constraints do not solely account for the observed differences across race and ethnic groups.
Racism—a system of structuring opportunity and assigning value based on the social interpretation of how one looks28—and other implicit biases may be playing a role. Prior research has identified that clinician perceptions and attitudes of risk and treatment benefits frequently underlie differential prescription of guideline-recommended therapies.29,30 However, quantitative analyses can offer only a general overview of racial differences and cannot provide in-depth information about contextual determinants. For instance, clinician knowledge of these novel therapies, comfort with prescribing, and clinicians’ race and ethnicity were not assessed in this study. Therefore, qualitative explorations are needed to further understand and contextualize these findings. In addition, the low prescription rates observed across all race and ethnic groups may be due to the relative novelty of these medications. As quality improvement initiatives are established to overcome this treatment gap, these findings suggest that such initiatives must take a racial and ethnic equity lens so that improvements in care can extend benefits to all.
Limitations
This study has several limitations. First, racial and ethnic disparities in the VHA system are less pronounced than in other US health systems.31 Therefore, these results are not necessarily generalizable to other health systems. Second, there was low representation of women, which is inherent to the VHA. Third, the VHA does not retain individual-level information on socioeconomic characteristics; thus, unmeasured and residual confounding by individual-level socioeconomic characteristics may have partially accounted for these findings. Fourth, only 1 medication per class was available in the VHA national formulary, which may limit prescriptions. Fifth, the VHA facility complexity index does not necessarily indicate quality of care. Better indicators of facility-level quality might have demonstrated a larger contribution of facility characteristics to the observed findings. Sixth, this study includes all patients with type 2 diabetes and does not exclusively focus on patients with concomitant ASCVD, heart failure, and CKD, for whom SGLT2i and GLP-1 RA should be prioritized. Seventh, the cross-sectional design has limitations, which include prevalence-incidence bias and reverse causality. Eighth, this study did not assess the association of prescription and utilization of these medications with clinical outcomes.
Conclusions
Among patients with type 2 diabetes in the VHA system during 2019 and 2020, prescription rates of SGLT2i and GLP-1 RA medications were low, and individuals of several different racial groups and those of Hispanic ethnicity had statistically significantly lower odds of receiving prescriptions for these medications compared with individuals of White race and non-Hispanic ethnicity. Further research is needed to understand the mechanisms underlying these differences in rates of prescribing and the potential relationships with differences in clinical outcomes.
eTable 1. Demographic and Clinical Characteristics of Patients With Type 2 Diabetes in the Veterans Health Administration System From 2019 to 2020 by Ethnicity Categories
eTable 2. VHA Facility Complexity Level
eTable 3. Covariate Definition and Method of Ascertainment
eTable 4. System characteristics and SGLT2i and GLP-1 RA prescription
eTable 5. Type of VHA Facility and Driving Distance to Tertiary VHA Facility by Race Group
eTable 6. Association of Race and Ethnicity Categories With SGLT2i and GLP-1 RA Prescription With Further Adjustment for VHA Facility Type and Driving Time to Tertiary Care VHA Center
eTable 7. Association of Race and Ethnicity With SGLT2i and GLP-1 RA Prescription Restricting Study Sample to Patients With at Least Two Prescription Fills During in One Year
eTable 8. Incident Prescription Rates for SGLT2i From 2017 to 2021
eTable 9. Incident Prescription Rates for GLP-1 RA From 2017 to 2021
eFigure 1. Algorithm for Ascertainment of Type 2 Diabetes Cases in Electronic Health Records
eFigure 2. Identification of the Study Sample
eFigure 3. Association Between Race and Ethnicity Groups and SGLT2i Prescription With Sequential Adjustment for Patient and System-Level Characteristics
eFigure 4. Association Between Race and Ethnicity Groups and GLP-1 RA prescription With Sequential Adjustment for Patient and System-Level Characteristics
eFigure 5. Variability in SGLT2i Prescription Across VHA Stations
eFigure 6. Variability in GLP-1 RA Prescription Across VHA Stations
eFigure 7. Prescription of SGLT2i and GLP1-RA Comparing American Indian or Alaska Native Patients versus White Patients Across Patient- and System-Level Characteristics
eFigure 8. Prescription of SGLT2i and GLP1-RA Comparing Asian, Native Hawaiian or Other Pacific Islander Patients versus White Patients Across Patient- and System-Level Characteristics
eFigure 9. Prescription of SGLT2i and GLP1-RA Comparing Multiracial Patients versus White Patients Across Patient- and System-Level Characteristics
eFigure 10. Prescription of SGLT2i and GLP1-RA Comparing Patients With Unknown Race versus White Patients Across Patient- and System-Level Characteristics
eFigure 11. Incident Prescription Rates for SGLT2i From 2017 to 2021 Across Race Groups
eFigure 12. Incident Prescription Rates for SGLT2i From 2017 to 2021 Across Ethnicity Groups
eFigure 13. Incident Prescription Rates for GLP1-RA From 2017 to 2021 Across Race Groups
eFigure 14. Incident Prescription Rates for GLP1-RA From 2017 to 2021 Across Ethnicity Groups
eAppendix. Sensitivity Analyses
eReferences
References
- 1.Essien UR, Dusetzina SB, Gellad WF. A policy prescription for reducing health disparities: achieving pharmacoequity. JAMA. 2021;326(18):1793-1794. doi: 10.1001/jama.2021.17764 [DOI] [PubMed] [Google Scholar]
- 2.Essien UR, Kim N, Hausmann LRM, et al. Disparities in anticoagulant therapy initiation for incident atrial fibrillation by race/ethnicity among patients in the Veterans Health Administration system. JAMA Netw Open. 2021;4(7):e2114234. doi: 10.1001/jamanetworkopen.2021.14234 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Cheng YJ, Kanaya AM, Araneta MRG, et al. Prevalence of diabetes by race and ethnicity in the United States, 2011-2016. JAMA. 2019;322(24):2389-2398. doi: 10.1001/jama.2019.19365 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hsu CY, Lin F, Vittinghoff E, Shlipak MG. Racial differences in the progression from chronic renal insufficiency to end-stage renal disease in the United States. J Am Soc Nephrol. 2003;14(11):2902-2907. doi: 10.1097/01.ASN.0000091586.46532.B4 [DOI] [PubMed] [Google Scholar]
- 5.US Renal Data System. 2021 Annual data report. Accessed March 20, 2022. https://adr.usrds.org/2021
- 6.American Diabetes Association . 16, Diabetes Advocacy: Standards of Medical Care in Diabetes-2019. Diabetes Care. 2020;43(suppl 1):S203-S204. doi: 10.2337/dc20-S016 [DOI] [PubMed] [Google Scholar]
- 7.Eknoyan G, Lameire N, Eckardt K, et al. KDIGO 2012 clinical practice guideline for the evaluation and management of chronic kidney disease. Kidney Int. 2013;3(1):5-14. [DOI] [PubMed] [Google Scholar]
- 8.Eberly LA, Yang L, Eneanya ND, et al. Association of race/ethnicity, gender, and socioeconomic status with sodium-glucose cotransporter 2 inhibitor use among patients with diabetes in the US. JAMA Netw Open. 2021;4(4):e216139. doi: 10.1001/jamanetworkopen.2021.6139 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Eberly LA, Yang L, Essien UR, et al. Racial, ethnic, and socioeconomic inequities in glucagon-like peptide-1 receptor agonist use among patients with diabetes in the US. JAMA Health Forum. 2021;2(12):e214182-e214182. doi: 10.1001/jamahealthforum.2021.4182 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Tummalapalli SL, Montealegre JL, Warnock N, Green M, Ibrahim SA, Estrella MM. Coverage, formulary restrictions, and affordability of sodium-glucose cotransporter 2 inhibitors by US insurance plan types. JAMA Health Forum. 2021;2(12):e214205-e214205. doi: 10.1001/jamahealthforum.2021.4205 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Newton KM, Peissig PL, Kho AN, et al. Validation of electronic medical record-based phenotyping algorithms: results and lessons learned from the eMERGE network. J Am Med Inform Assoc. 2013;20(e1):e147-e154. doi: 10.1136/amiajnl-2012-000896 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kho AN, Hayes MG, Rasmussen-Torvik L, et al. Use of diverse electronic medical record systems to identify genetic risk for type 2 diabetes within a genome-wide association study. J Am Med Inform Assoc. 2012;19(2):212-218. doi: 10.1136/amiajnl-2011-000439 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Department of Veterans Affairs, Veterans Health Administration . VHA directive 1601A.01: registration and Enrollment. Published July 7, 2020. Accessed June 12, 2022. https://www.va.gov/vhapublications/ViewPublication.asp?pub_ID=8907
- 14.Department of Veterans Affairs . VA form 10-10EZ application for health benefits. Published July 2021. Accessed June 12, 2022. https://www.va.gov/Vaforms/medical/pdf/10-10EZ-fillable.pdf
- 15.Citro CF, Kalton G, eds; National Research Council; Division of Behavioral and Social Sciences and Education; Committee on National Statistics; Panel on the Functionality and Usability of Data from the American Community Survey . Using the American Community Survey: Benefits and Challenges. National Academies Press; 2007. [Google Scholar]
- 16.Butler DC, Petterson S, Phillips RL, Bazemore AW. Measures of social deprivation that predict health care access and need within a rational area of primary care service delivery. Health Serv Res. 2013;48(2, pt 1):539-559. doi: 10.1111/j.1475-6773.2012.01449.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hall SA, Kaufman JS, Ricketts TC. Defining urban and rural areas in US epidemiologic studies. J Urban Health. 2006;83(2):162-175. doi: 10.1007/s11524-005-9016-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.US Department of Veterans Affairs. About VHA disability ratings. Published February 4, 2022. Accessed June 14, 2022. https://www.va.gov/disability/about-disability-ratings/
- 19.Austin PC, Merlo J. Intermediate and advanced topics in multilevel logistic regression analysis. Stat Med. 2017;36(20):3257-3277. doi: 10.1002/sim.7336 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Muller CJ, MacLehose RF. Estimating predicted probabilities from logistic regression: different methods correspond to different target populations. Int J Epidemiol. 2014;43(3):962-970. doi: 10.1093/ije/dyu029 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Mahtta D, Ramsey DJ, Lee MT, et al. Utilization rates of SGLT2 inhibitors and GLP-1 receptor agonists and their facility-level variation among patients with atherosclerotic cardiovascular disease and type 2 diabetes: insights from the Department of Veterans Affairs. Diabetes Care. 2022;45(2):372-380. doi: 10.2337/dc21-1815 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Merlo J, Chaix B, Ohlsson H, et al. A brief conceptual tutorial of multilevel analysis in social epidemiology: using measures of clustering in multilevel logistic regression to investigate contextual phenomena. J Epidemiol Community Health. 2006;60(4):290-297. doi: 10.1136/jech.2004.029454 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Cai C, Woolhandler S, McCormick D, et al. Racial and ethnic inequities in diabetes pharmacotherapy: Black and Hispanic patients are less likely to receive SGLT2is and GLP1as. J Gen Intern Med. Published online February 9, 2022. doi: 10.1007/s11606-022-07428-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Zhuo M, Li J, Buckley LF, et al. Prescribing patterns of sodium-glucose cotransporter-2 inhibitors in patients with chronic kidney disease. Kidney360. 2022;3(3):455-464. doi: 10.34067/KID.0007862021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Al Rifai M, Vaughan EM, Abushamat LA, et al. Correlates of glucagon-like peptide-1 receptor agonist use among patients with atherosclerotic cardiovascular disease and type 2 diabetes mellitus (from the Department of Veterans Affairs). Am J Cardiol. 2022;172:7-10. doi: 10.1016/j.amjcard.2022.02.013 [DOI] [PubMed] [Google Scholar]
- 26.Churchwell K, Elkind MSV, Benjamin RM, et al. ; American Heart Association . Call to action: structural racism as a fundamental driver of health disparities: a presidential advisory from the American Heart Association. Circulation. 2020;142(24):e454-e468. doi: 10.1161/CIR.0000000000000936 [DOI] [PubMed] [Google Scholar]
- 27.Trivedi AN, Grebla RC, Wright SM, Washington DL. Despite improved quality of care in the Veterans Affairs health system, racial disparity persists for important clinical outcomes. Health Aff (Millwood). 2011;30(4):707-715. doi: 10.1377/hlthaff.2011.0074 [DOI] [PubMed] [Google Scholar]
- 28.Jones CP. Confronting institutionalized racism. Phylon. 2002;50(1/2):7-22. doi: 10.2307/4149999 [DOI] [Google Scholar]
- 29.Chapman EN, Kaatz A, Carnes M. Physicians and implicit bias: how doctors may unwittingly perpetuate health care disparities. J Gen Intern Med. 2013;28(11):1504-1510. doi: 10.1007/s11606-013-2441-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.van Ryn M, Fu SS. Paved with good intentions: do public health and human service providers contribute to racial/ethnic disparities in health? Am J Public Health. 2003;93(2):248-255. doi: 10.2105/AJPH.93.2.248 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Jha AK, Shlipak MG, Hosmer W, Frances CD, Browner WS. Racial differences in mortality among men hospitalized in the Veterans Affairs health care system. JAMA. 2001;285(3):297-303. doi: 10.1001/jama.285.3.297 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eTable 1. Demographic and Clinical Characteristics of Patients With Type 2 Diabetes in the Veterans Health Administration System From 2019 to 2020 by Ethnicity Categories
eTable 2. VHA Facility Complexity Level
eTable 3. Covariate Definition and Method of Ascertainment
eTable 4. System characteristics and SGLT2i and GLP-1 RA prescription
eTable 5. Type of VHA Facility and Driving Distance to Tertiary VHA Facility by Race Group
eTable 6. Association of Race and Ethnicity Categories With SGLT2i and GLP-1 RA Prescription With Further Adjustment for VHA Facility Type and Driving Time to Tertiary Care VHA Center
eTable 7. Association of Race and Ethnicity With SGLT2i and GLP-1 RA Prescription Restricting Study Sample to Patients With at Least Two Prescription Fills During in One Year
eTable 8. Incident Prescription Rates for SGLT2i From 2017 to 2021
eTable 9. Incident Prescription Rates for GLP-1 RA From 2017 to 2021
eFigure 1. Algorithm for Ascertainment of Type 2 Diabetes Cases in Electronic Health Records
eFigure 2. Identification of the Study Sample
eFigure 3. Association Between Race and Ethnicity Groups and SGLT2i Prescription With Sequential Adjustment for Patient and System-Level Characteristics
eFigure 4. Association Between Race and Ethnicity Groups and GLP-1 RA prescription With Sequential Adjustment for Patient and System-Level Characteristics
eFigure 5. Variability in SGLT2i Prescription Across VHA Stations
eFigure 6. Variability in GLP-1 RA Prescription Across VHA Stations
eFigure 7. Prescription of SGLT2i and GLP1-RA Comparing American Indian or Alaska Native Patients versus White Patients Across Patient- and System-Level Characteristics
eFigure 8. Prescription of SGLT2i and GLP1-RA Comparing Asian, Native Hawaiian or Other Pacific Islander Patients versus White Patients Across Patient- and System-Level Characteristics
eFigure 9. Prescription of SGLT2i and GLP1-RA Comparing Multiracial Patients versus White Patients Across Patient- and System-Level Characteristics
eFigure 10. Prescription of SGLT2i and GLP1-RA Comparing Patients With Unknown Race versus White Patients Across Patient- and System-Level Characteristics
eFigure 11. Incident Prescription Rates for SGLT2i From 2017 to 2021 Across Race Groups
eFigure 12. Incident Prescription Rates for SGLT2i From 2017 to 2021 Across Ethnicity Groups
eFigure 13. Incident Prescription Rates for GLP1-RA From 2017 to 2021 Across Race Groups
eFigure 14. Incident Prescription Rates for GLP1-RA From 2017 to 2021 Across Ethnicity Groups
eAppendix. Sensitivity Analyses
eReferences


