Abstract
Experiences of racism and racial discrimination are associated with poorer mental and physical health outcomes for people from minoritised ethnic groups. One mechanism by which racism leads to poor health is through reduced socio-economic resources, but the evidence documenting the direct and indirect effects of racism on health via socio-economic inequality over time is under-developed. The central aims of this paper are to better understand how racism affects health over time, by age, and via the key mechanism of socio-economic inequality. This paper analyses large-scale, nationally representative data from the UK Household Longitudinal Study (Understanding Society) 2009–2019. Findings from longitudinal structural equation models clearly indicate the enduring effects of racism on health, which operate over time both directly and indirectly through lower income and poorer prior health. Repeated exposure to racism severely and negatively impacts the health of people from minoritised ethnic groups. These findings make an important contribution to the existing evidence base, demonstrating the enduring effects of racism on health over time and across age groups.
Highlights
-
•
We examine the role of racism as a key driver of ethnic inequalities in health.
-
•
We examine the direct and indirect effects of racism on mental and physical health.
-
•
Racism severely and negatively impacts health over time and across the life course.
-
•
Repeated exposure to racism leads to accumulation of disadvantage and poorer health.
-
•
Policy and academic debates must focus on the fundamental role of racism on health.
1. Introduction
Racism is a system of oppression which unjustly disadvantages people from minoritised ethnic groups, and unfairly advantages people from White ‘majority’ groups (Jones, 2000). Racism leads to negative prejudice, stereotyping, and discrimination (Williams & Mohammed, 2013), and operates at structural, institutional, and interpersonal levels (Nazroo et al., 2020). Structural racism is reflected in disadvantaged access to physical, economic, and social resources, resulting in, for example, deep and persistent socio-economic inequalities. Institutional racism is reflected in routine processes and procedures within institutional settings that translate into actions that negatively shape the experiences of people from minoritised ethnic groups. Interpersonal racism refers to the everyday encounters of racism for people from minoritised ethnic groups, ranging from everyday slights to verbal or physical abuse (Jones, 2000).
International studies have documented the adverse effects of racism and racial discrimination on health outcomes (Paradies, 2006; Paradies et al., 2015; Williams et al., 2019; Williams & Mohammed, 2013). Experiences of racism and racial discrimination are negatively associated with health outcomes including hypertension (Dolezsar et al., 2014; Karlsen & Nazroo, 2002b; Williams & Neighbors, 2001), cardiovascular disease (Lewis et al., 2014), risky health behaviours (Pascoe & Smart Richman, 2009), and self-reported health (Harris et al., 2006; Karlsen & Nazroo, 2002a, 2002b; Paradies, 2006; Paradies et al., 2015). Experiences of racism and racial discrimination are associated with negative mental health outcomes, such as psychological distress or depressive symptoms (Bécares & Zhang, 2018; Nandi et al., 2016; Wallace et al., 2016), and psychosis or severe mental illness (Karlsen & Nazroo, 2002b; Karlsen et al., 2005; Nazroo et al., 2020). Experiences of racism are also negatively associated with positive mental health outcomes, such self-esteem or life satisfaction (see Schmitt et al., 2014). The effects of racism on health operate both directly (for example, through stress pathways), and indirectly (for example, through socio-economic inequalities) (Hudson et al., 2013; Karlsen & Nazroo, 2002b, 2004; Wallace et al., 2016; Williams & Mohammed, 2013). Importantly, racism and racial discrimination have negative effects on the health of people who experience it themselves or vicariously through the experiences of others, which can be understood from a linked lives perspective (Bécares et al., 2015a; Gee et al., 2012).
Racism and racial discrimination also lead to entrenched ethnic inequalities across socio-economic position. For example, evidence from the UK shows that compared with the White majority, people from minoritised ethnic groups tend to live in more disadvantaged areas (Jivraj & Khan, 2015); have poorer housing or insecure tenures (Finney & Harries, 2013; Shankley & Finney, 2020); have higher rates of unemployment (Clark & Shankley, 2020; Kapadia et al., 2015); and work in less advantaged, lower paid occupations (Brynin & Longhi, 2015). Overall, the evidence shows that socio-economic inequalities make a substantial contribution to ethnic inequalities in health (Nazroo, 2001). However, most academic and policy discourses on ethnic inequalities rarely make explicit that the underlying cause of socio-economic disadvantage is racism and discrimination (see Nazroo & Bécares, 2020; Torres, 2020).
Life course exposure to racism and racial discrimination leads to poorer health outcomes in later life through what Geronimus (1992) has termed ‘weathering’, i.e., the gradual decline of health for people from minoritised ethnic groups who experience enduring social and economic disadvantage (Forde et al., 2019; Gee et al., 2019; Geronimus, 1992). The experiences of cumulative social and economic disadvantage for people from minoritised ethnic groups, for example in employment, earnings, housing, and neighbourhoods, are underpinned and shaped by structural and institutional racism (Nazroo et al., 2020). The accumulation of disadvantage has long-term effects on poorer health outcomes (Bécares et al., 2009; Darlington et al., 2015; Gee et al., 2012, 2019; Hudson et al., 2013; Nazroo, 2003; Williams, 1999). Previous studies in the UK have demonstrated that health outcomes worsen as people age, and that ethnic inequalities in health are exacerbated in older ages (Evandrou et al., 2016; Nazroo, 2006; Stopforth et al., 2022). Hence, accounting for both age and life stage is important in analyses of the effects of racism and socio-economic disadvantage on health outcomes.
The workings of racism over time, by age, and via key mechanisms like socio-economic inequalities, are less well-documented. Examining these mechanisms is crucial to inform research and policy to address ethnic inequalities. In this paper, we use nationally representative, large-scale, longitudinal observational data from Understanding Society, the UK Household Longitudinal Study, to examine the direct effect of experiences of racism and racial discrimination on physical and mental health, and their indirect effects via socio-economic circumstances. We use data covering a 10 year period (wave 1 2009/2011 to wave 9 2017/2019) to analyse these effects. In addition, to understand processes of accumulation and weathering we take the additional step of investigating the effects of racism and discrimination on health by age, allowing us to explore the importance of life stage. This work is innovative, because we simultaneously measure the cross-sectional and longitudinal effects of racism on health. By combining the interpretation of the two sets of analyses by chronological time and by age group, we can begin to approximate a life course analysis. Doing so enables us to incorporate a consideration of the accumulation of disadvantage through structural disadvantage and experiences of racism. We return to the issue of data infrastructure and representativeness of data in the discussion.
2. Data and methods
We analyse data from Understanding Society, the UK Household Longitudinal Study (University of Essex & Institute for Social and Economic Research, 2020). Understanding Society is a longitudinal household panel survey which began in 2009, collecting data on individuals within approximately 40,000 households. It has a complex survey design with multiple sample components, including a general population sample and an ethnic minority boost (EMB) sample, with British Household Panel Survey respondents joining from wave 2, and an immigrant and ethnic minority boost (IEMB) sample added from wave 6. Fieldwork for each wave is collected over a 24-month period. Understanding Society covers a wide range of topics; core questionnaire modules are asked in every wave, and some rotating questionnaire modules are asked at regular intervals. Questions about experiences of racism and racial harassment are asked of a subset of respondents, which comprise members of the EMB and IEMB samples, and a proportion of the general population sample. The racism and harassment questions are asked in alternate waves from wave 1, and therefore we use waves 1, 3, 5, 7, and 9 in this study, covering the period 2009 to 2019.
2.1. Health
The outcome measures are mental and physical health functioning scores. Both measures are derived from the 12-Item Short Form Health Survey (SF-12); the Mental Component Summary (MCS) and the Physical Component Summary (PCS). The MCS is a measure of non-specific psychological distress, while the PCS is a measure of physical wellbeing. The health functioning scores are derived using an algorithm and range from 0 to 100 with a mean of 50 and standard deviation of 10. Scores closer to 0 represent lower functioning health, and scores closer to 100 represent higher functioning health (see Ware et al., 2001).
2.2. Experiences of racism and racial harassment
Respondents are asked about their experiences of four types of harassment and abuse in public in the past twelve months: have you been insulted, called names, threatened or shouted at; have you been physically attacked; have you felt unsafe; and have you avoided going to or being in public places. The questions are asked using a two-stage approach. First, respondents are asked about each experience separately for a series of public places: at school, at college or university, at work, on public transport, at or near a bus or train station, in shopping centres, in cinemas or cafes, at a pub, disco or club, in car parks, outside on the street or a park, at home, or other places. Respondents can select all that apply. In the second stage, respondents are then asked the reason why they experienced harassment or abuse, with options covering: sex, age, ethnicity, sexual orientation, health or disability, nationality, religion, language or accent, dress or appearance, other reason, or none of these reasons. Following Wallace et al. (2016) and Nandi et al. (2016), we derive our measures of racism and racial harassment based on respondents reporting that they had been harassed or abused due to their ethnicity, nationality, or religion. Given low numbers of participants reporting physical attacks, and following Wallace et al. (2016), we combine verbal abuse and physical attacks into one measure and include this composite measure of racial abuse in the latent measure of racism.
2.3. Income
We use income as a measure of socio-economic position. We use net household income, rather than personal or gross income, to more accurately reflect the economic resources available to individuals. We use an equivalised measure that takes account of household size using the Organisation for Economic Co-operation and Development (OECD) scale (see chapter 3 in Office for National Statistics, 2015). We then standardise the measure to have a mean of 0 and standard deviation of 1.
2.4. Analytical strategy
The central analytical focus of this paper is to examine the intricate and complex ways by which racism impacts on health over time. Fundamentally, we seek to better understand the direct effects of interpersonal racism on health, and the indirect effects of racism on health via socio-economic inequality, i.e. reduced income. We undertake the analyses separately for the mental health and physical health scores.
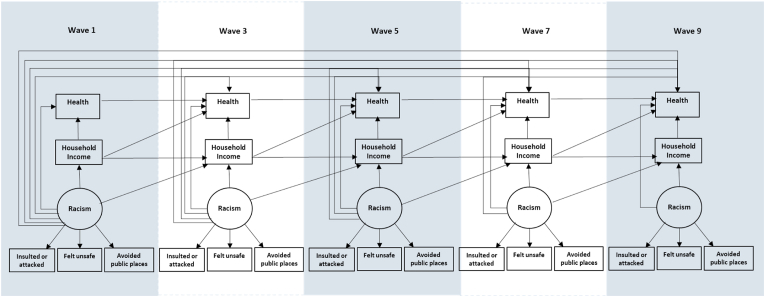
In the first stage of the analyses, we estimate longitudinal structural equation models using all available waves. Estimating structural equation models requires a balance between theory and parsimony (see Hooper et al., 2008). The measurement model estimates a latent measure of experienced racism. The structural model includes the latent measure of experienced racism and manifest measures of household income and health over time. We also include age and gender as covariates in the model. Fig. 1 presents the conceptual diagram of the model. We include paths between the latent measure of experienced racism in each wave with health in all subsequent waves to capture the long-term direct effects of racism on health. We include paths between racism and income in each wave and the next adjacent wave. We also include estimates of the covariances between the latent measures of racism in all waves.
Fig. 1.
Conceptual diagram of the structural equation models.
We present the results as the decomposition of total, direct, and indirect effects to examine the effects of racism, income, and health over time (full model outputs can be found in the online appendix). To calculate the total, direct, and indirect effects of the explanatory variable of interest, the coefficients are traced back from the main outcome to the explanatory variable (see Wright, 1960). In the following models, the direct effects of racism on health are represented by the connecting paths between these variables. The indirect effects are calculated as the product of all non-direct paths between racism and health, i.e., the product of the coefficients between racism and income, and income and health, over time. The total effect is calculated as the sum of the direct effects and indirect effects between the explanatory variable of interest and the main outcome variable.
Our analyses focus on the effects of experiences of racism on health, which we do not theorise to differ by ethnicity. The analytical sample comprises participants from all minoritised ethnic groups (i.e. the White British group were not included in the analysis), who responded to the questions on racism in the adult interview, and who were part of the Understanding Society samples eligible for the survey from wave 1 (i.e., in the general population sample or the EMB sample). The total eligible sample of respondents was n = 4444. A third of the sample contributed to all five waves. There were 580 people who responded to wave 9 only. We re-estimated the models without these respondents, but as the results were unchanged, we retain them in the sample.
In the next stage of the analyses, we further investigate how the effects of racism differ by age. Our analyses are intended to better understand the effects of racism on health at different points across the life course. We divide the analytical sample into ten-year age groups based on their age at wave 9 of the survey: the under 30s, 30-39 year-olds, 40-49 year-olds, 50-59 year-olds, and over 60s. We then estimate multi-group structural equation models to allow a comparison of effects by categories of age. Due to the computational and statistical power required for a multi-group structural equation model with increased parameters to be estimated, the models do not converge when using all waves. We therefore restrict the sample to respondents present in waves 7 and 9 only, which allows the inclusion of respondents from the IEMB refresher sample who were also asked the questions on harassment and abuse. The total analytical sample is n = 5190. We undertook sensitivity analyses around the inclusion of the IEMB sample and the results are consistent with using waves 7 and 9 for the EMB sample only. We use Wald tests to formally test for group invariance of parameters by age.
Missing data were accounted for using the full information maximum likelihood method in the structural equation models. We assess model fit using conventional fit statistics for structural equation models, including chi-square (ratio of chi-square to degrees of freedom ≤3), root mean square error approximation (<0.06), comparative fit index (≥0.95), and Tucker-Lewis index (≥0.95) (see Iacobucci, 2010; Schreiber et al., 2006). All models were estimated using Stata version 16 (StataCorp, 2019). The goodness-of-fit statistics are presented alongside each model. The models were adjusted for complex survey design and weighted using the appropriate longitudinal weights.
3. Results
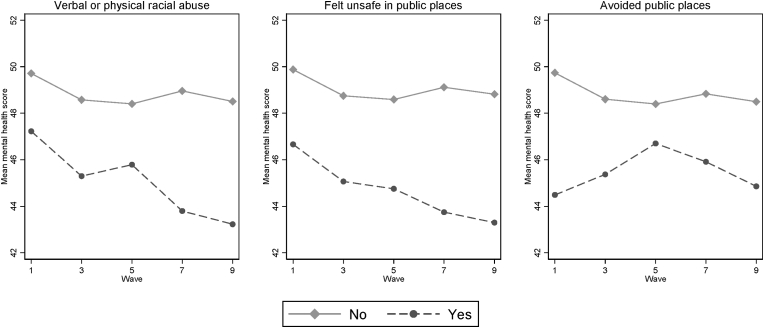
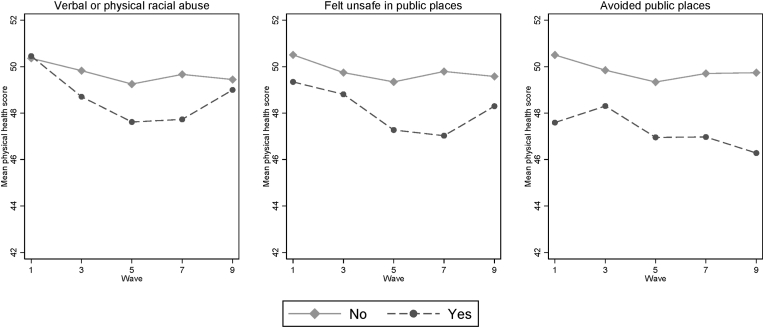
The descriptive statistics for the sample are presented in Table 1. The mean age in wave 9 is 43 years (standard deviation 17). The mean mental and physical health scores are broadly consistent over the five waves. Fig. 2, Fig. 3 present the mean health scores by experiences of racism and racial harassment. Mean mental health scores are worse for people who were exposed to verbal or physical abuse, or who felt unsafe in public places due to their ethnicity, nationality, or religion, and these differences increase over time (Fig. 2). Clear differences in mean physical health scores are also observed by experiences of racism and racial harassment, particularly between waves 1 and 7 (Fig. 3).
Table 1.
Descriptive statistics.
| All waves |
Waves 7 and 9 |
|
|---|---|---|
| Mean (standard deviation) | Mean (standard deviation) | |
| Mental health score | ||
| Wave 1 | 49.5 (10.3) | – |
| Wave 3 | 48.4 (10.0) | – |
| Wave 5 | 48.3 (10.4) | – |
| Wave 7 | 48.6 (10.4) | 48.5 (10.4) |
| Wave 9 | 48.1 (10.7) | 48.2 (10.6) |
| Physical health score | ||
| Wave 1 | 50.4 (10.3) | – |
| Wave 3 | 49.7 (9.9) | – |
| Wave 5 | 49.2 (10.3) | – |
| Wave 7 | 49.5 (10.4) | 49.6 (10.2) |
| Wave 9 | 49.4 (10.5) | 49.3 (10.4) |
|
Frequencya(%) |
Frequency (%) |
|
| Ethnicity | ||
| Irish | 109 (2.5) | 122 (2.4) |
| Gypsy/Irish Traveller | 4 (0.1) | 2 (0.0) |
| White other | 502 (11.3) | 731 (14.1) |
| White & Black Caribbean | 145 (3.3) | 151 (2.9) |
| White & Black African | 46 (1.0) | 50 (1.0) |
| White & Asian | 95 (2.1) | 93 (1.8) |
| Mixed other | 70 (1.6) | 74 (1.4) |
| Indian | 845 (19.0) | 1056 (20.4) |
| Pakistani | 765 (17.2) | 876 (16.9) |
| Bangladeshi | 538 (12.1) | 482 (9.3) |
| Chinese | 93 (2.1) | 95 (1.8) |
| Asian other | 246 (5.5) | 242 (4.7) |
| Black Caribbean | 374 (8.4) | 451 (8.7) |
| Black African | 461 (10.4) | 562 (10.8) |
| Black other | 27 (0.6) | 27 (0.5) |
| Arab | 50 (1.1) | 90 (1.7) |
| Other ethnic group | 74 (1.7) | 86 (1.7) |
| Total | 4444 (100) | 5190 (100) |
Total frequency in wave 9; frequencies vary between waves.
The analyses undertaken using all available waves comprise the EMB sample and the comparison sample, for people enumerated from wave 1 of Understanding Society. The analyses undertaken using waves 7 and 9 only comprise the EMB sample, the comparison sample, and the refresher IEMB sample, introduced from wave 6.
Fig. 2.
Mean SF-12 mental health component scores by experiences of racism over time.
Fig. 3.
Mean SF-12 physical health component scores by experiences of racism over time.
3.1. Racism and health over time
Table 2 presents the decomposition of effects for racism and income on mental health score. The total effects of racism tend to be strongest on mental health scores reported in the same wave (coefficients range from −0.06 to −0.18). The decomposition of the total effects demonstrate that the majority of the effect of racism on mental health measured at the same wave is direct, with negligible indirect effects through income. The direct effects of racism on mental health in subsequent waves are small, inconsistent and not statistically significant. However, in most waves racism has strong indirect effects on mental health in the subsequent wave. For example, there are strong indirect effects of racism in wave 7 on mental health in wave 9 (coefficient −0.09, standard error 0.02, p < 0.001). The indirect effects of racism on health between two waves are the product of all paths between racism and income, and income and health, and therefore represent the longer term effects of racism operating through lower income and poorer mental health over time.
Table 2.
Decomposition of the direct and indirect effects of racism on mental health (standardised coefficients).
| Direct effects |
Indirect effects |
Total effects |
||||
|---|---|---|---|---|---|---|
| Std. Coef | Std. Error | Std. Coef | Std. Error | Std. Coef | Std. Error | |
| Effects of racism wave 1 on | ||||||
| Income wave 1 | −0.05 | (0.06) | – | – | −0.05 | (0.06) |
| Income wave 3 | −0.06 | (0.06) | −0.03 | (0.04) | −0.09 | (0.08) |
| Income wave 5 | – | – | −0.06 | (0.05) | −0.06 | (0.05) |
| Income wave 7 | – | – | −0.04 | (0.04) | −0.04 | (0.04) |
| Income wave 9 | – | – | −0.03 | (0.02) | −0.03 | (0.02) |
| Mental health wave 1 | −0.08 | (0.05) | −0.00 | (0.00) | −0.08 | (0.05) |
| Mental health wave 3 | 0.00 | (0.10) | −0.05 | (0.02) | −0.04 | (0.10) |
| Mental health wave 5 | −0.04 | (0.08) | −0.02 | (0.05) | −0.06 | (0.08) |
| Mental health wave 7 | 0.08 | (0.05) | −0.03 | (0.04) | 0.05 | (0.06) |
| Mental health wave 9 | 0.02 | (0.06) | 0.03 | (0.03) | 0.04 | (0.07) |
| Effects of racism wave 3 on | ||||||
| Income wave 3 | 0.02 | (0.05) | – | – | 0.02 | (0.05) |
| Income wave 5 | −0.02 | (0.05) | 0.02 | (0.03) | −0.00 | (0.07) |
| Income wave 7 | – | – | −0.00 | (0.05) | −0.00 | (0.05) |
| Income wave 9 | – | – | −0.00 | (0.03) | −0.00 | (0.03) |
| Mental health wave 3 | −0.14* | (0.07) | 0.00 | (0.01) | −0.14 | (0.07) |
| Mental health wave 5 | −0.08 | (0.06) | −0.07 | (0.04) | −0.15* | (0.07) |
| Mental health wave 7 | −0.08 | (0.05) | −0.07* | (0.03) | −0.15** | (0.05) |
| Mental health wave 9 | −0.09 | (0.06) | −0.07** | (0.02) | −0.17** | (0.07) |
| Effects of racism wave 5 on | ||||||
| Income wave 5 | −0.04 | (0.03) | – | – | −0.04 | (0.03) |
| Income wave 7 | −0.05 | (0.03) | −0.03 | (0.02) | −0.08* | (0.04) |
| Income wave 9 | – | – | −0.05* | (0.02) | −0.05* | (0.02) |
| Mental health wave 5 | −0.06 | (0.05) | 0.00 | (0.00) | −0.06 | (0.05) |
| Mental health wave 7 | 0.02 | (0.04) | −0.03 | (0.02) | −0.01 | (0.04) |
| Mental health wave 9 | −0.03 | (0.04) | −0.00 | (0.02) | −0.04 | (0.05) |
| Effects of racism wave 7 on | ||||||
| Income wave 7 | −0.03 | (0.03) | – | – | −0.03 | (0.03) |
| Income wave 9 | −0.05** | (0.02) | −0.02 | (0.02) | −0.06* | (0.02) |
| Mental health wave 7 | −0.18*** | (0.05) | −0.00 | (0.00) | −0.18*** | (0.05) |
| Mental health wave 9 | 0.06 | (0.03) | −0.09*** | (0.02) | −0.03 | (0.03) |
| Effects of racism wave 9 on | ||||||
| Income wave 9 | 0.01 | (0.02) | – | – | 0.01 | (0.02) |
| Mental health wave 9 | −0.09** | (0.03) | 0.00 | (0.00) | −0.09** | (0.03) |
| Effects of income wave 1 on | ||||||
| Mental health wave 1 | 0.04 | (0.03) | – | – | 0.04 | (0.03) |
| Mental health wave 3 | −0.01 | (0.05) | 0.08* | (0.04) | 0.07 | (0.04) |
| Mental health wave 5 | – | – | 0.02 | (0.03) | 0.02 | (0.03) |
| Mental health wave 7 | – | – | 0.02 | (0.02) | 0.02 | (0.02) |
| Mental health wave 9 | – | – | 0.00 | (0.01) | 0.00 | (0.01) |
| Effects of income wave 3 on | ||||||
| Mental health wave 3 | 0.10 | (0.05) | – | – | 0.10 | (0.05) |
| Mental health wave 5 | −0.02 | (0.04) | 0.04 | (0.04) | 0.02 | (0.04) |
| Mental health wave 7 | – | – | 0.02 | (0.02) | 0.02 | (0.02) |
| Mental health wave 9 | – | – | 0.00 | (0.02) | 0.00 | (0.02) |
| Effects of income wave 5 on | ||||||
| Mental health wave 5 | −0.02 | (0.04) | – | – | −0.02 | (0.04) |
| Mental health wave 7 | 0.00 | (0.04) | 0.01 | (0.03) | 0.01 | (0.03) |
| Mental health wave 9 | – | – | −0.01 | (0.02) | −0.01 | (0.02) |
| Effects of income wave 7 on | ||||||
| Mental health wave 7 | 0.03 | (0.04) | – | – | 0.03 | (0.04) |
| Mental health wave 9 | −0.05* | (0.03) | 0.05* | (0.03) | −0.00 | (0.03) |
| Effects of income wave 9 on | ||||||
| Mental health wave 9 | 0.06* | (0.02) | – | – | 0.06* | (0.02) |
Chi square (d.f.) 1607.8 (264)***RMSEA 0.034 (0.032–0.035) CFI 0.91TLI 0.88.
Source: Understanding Society waves 1, 3, 5, 7, and 9, n = 4444. Adjusted for complex survey design. Model also adjusts for age and gender. *p < 0.05 **p < 0.01 ***p < 0.001.
The direct effects of racism on income are similar in magnitude whether income is reported at the same time as racism, or in the subsequent wave (coefficients range from −0.06 to 0.02). Indirect effects of racism on income in subsequent waves, operating through successive income levels, are similar in magnitude, and therefore fairly consistent, across waves. The total effects of income on mental health scores are relatively strong (but not significant) for income in waves 1 and 3 on mental health in wave 3, and modest and significant for income in wave 9 on mental health score in wave 9; all other effects of income on mental health scores are lower and tend not to be significant in the model.
Table 3 presents the decomposition of effects for racism, income, and physical health. As with mental health, there are significantly strong direct effects of racism on physical health outcomes when reported in the same wave, and significant, slightly weaker indirect effects of racism on physical health reported in the subsequent wave. The total effects of racism on physical health are stronger in waves 5, 7, and 9 (coefficients ranging from −0.06 to −0.18). The effects of racism on income are entirely consistent with the results from the mental health model, which is to be expected as this pathway is unchanged. The effects of income on physical health are strong and persist over time. The effects are strongest in the earlier waves, with the total effects of income in wave 1 very strong, positive, and significant on physical health outcomes in all waves (coefficients decreasing steadily from 0.15 to 0.07). Greater income is strongly associated with better physical health in all waves.
Table 3.
Decomposition of the direct and indirect effects of racism on physical health (standardised coefficients).
| Direct effects |
Indirect effects |
Total effects |
||||
|---|---|---|---|---|---|---|
| Std. Coef | Std. Error | Std. Coef | Std. Error | Std. Coef | Std. Error | |
| Effects of racism wave 1 on | ||||||
| Income wave 1 | −0.05 | (0.07) | – | – | −0.05 | (0.07) |
| Income wave 3 | −0.05 | (0.06) | −0.03 | (0.04) | −0.08 | (0.08) |
| Income wave 5 | – | – | −0.05 | (0.05) | −0.05 | (0.05) |
| Income wave 7 | – | – | −0.04 | (0.04) | −0.04 | (0.04) |
| Income wave 9 | – | – | −0.02 | (0.02) | −0.02 | (0.02) |
| Physical health wave 1 | 0.04 | (0.04) | −0.01 | (0.01) | 0.03 | (0.04) |
| Physical health wave 3 | −0.03 | (0.07) | 0.01 | (0.02) | −0.02 | (0.07) |
| Physical health wave 5 | 0.09 | (0.07) | −0.02 | (0.04) | 0.08 | (0.06) |
| Physical health wave 7 | 0.00 | (0.06) | 0.04 | (0.04) | 0.05 | (0.05) |
| Physical health wave 9 | 0.03 | (0.06) | 0.03 | (0.03) | 0.06 | (0.06) |
| Effects of racism wave 3 on | ||||||
| Income wave 3 | 0.01 | (0.05) | – | – | 0.01 | (0.05) |
| Income wave 5 | −0.01 | (0.05) | 0.01 | (0.03) | −0.00 | (0.07) |
| Income wave 7 | – | – | −0.00 | (0.05) | −0.00 | (0.05) |
| Income wave 9 | – | – | −0.00 | (0.03) | −0.00 | (0.03) |
| Physical health wave 3 | −0.05 | (0.05) | −0.00 | (0.00) | −0.05 | (0.05) |
| Physical health wave 5 | 0.04 | (0.05) | −0.03 | (0.02) | 0.01 | (0.05) |
| Physical health wave 7 | −0.02 | (0.05) | 0.01 | (0.03) | −0.01 | (0.05) |
| Physical health wave 9 | −0.07 | (0.06) | −0.00 | (0.03) | −0.08 | (0.06) |
| Effects of racism wave 5 on | ||||||
| Income wave 5 | −0.04 | (0.03) | – | – | −0.04 | (0.03) |
| Income wave 7 | −0.06 | (0.04) | −0.03 | (0.03) | −0.09* | (0.04) |
| Income wave 9 | – | – | −0.06* | (0.03) | −0.06* | (0.03) |
| Physical health wave 5 | −0.18** | (0.06) | −0.00 | (0.00) | −0.18** | (0.06) |
| Physical health wave 7 | 0.07 | (0.06) | −0.11** | (0.04) | −0.05 | (0.05) |
| Physical health wave 9 | −0.06 | (0.07) | −0.03 | (0.03) | −0.09 | (0.07) |
| Effects of racism wave 7 on | ||||||
| Income wave 7 | −0.02 | (0.03) | – | – | −0.02 | (0.03) |
| Income wave 9 | −0.05** | (0.02) | −0.01 | (0.02) | −0.06* | (0.02) |
| Physical health wave 7 | −0.11** | (0.03) | −0.00 | (0.00) | −0.11** | (0.03) |
| Physical health wave 9 | 0.03 | (0.04) | −0.07** | (0.02) | −0.04 | (0.04) |
| Effects of racism wave 9 on | ||||||
| Income wave 9 | 0.01 | (0.02) | – | – | 0.01 | (0.02) |
| Physical health wave 9 | −0.06 | (0.04) | 0.00 | (0.00) | −0.06 | (0.04) |
| Effects of income wave 1 on | ||||||
| Physical health wave 1 | 0.15*** | (0.03) | – | – | 0.15*** | (0.03) |
| Physical health wave 3 | 0.08* | (0.03) | 0.07** | (0.03) | 0.14*** | (0.03) |
| Physical health wave 5 | – | – | 0.13*** | (0.02) | 0.13*** | (0.02) |
| Physical health wave 7 | – | – | 0.09*** | (0.02) | 0.09*** | (0.02) |
| Physical health wave 9 | – | – | 0.07*** | (0.01) | 0.07*** | (0.01) |
| Effects of income wave 3 on | ||||||
| Physical health wave 3 | −0.01 | (0.03) | – | – | −0.01 | (0.03) |
| Physical health wave 5 | 0.07* | (0.03) | 0.02 | (0.03) | 0.09** | (0.03) |
| Physical health wave 7 | – | – | 0.08*** | (0.02) | 0.08*** | (0.02) |
| Physical health wave 9 | – | – | 0.07*** | (0.01) | 0.07** | (0.01) |
| Effects of income wave 5 on | ||||||
| Physical health wave 5 | 0.03 | (0.03) | – | – | 0.03 | (0.03) |
| Physical health wave 7 | 0.01 | (0.03) | 0.06 | (0.03) | 0.06 | (0.03) |
| Physical health wave 9 | – | – | 0.07** | (0.02) | 0.07** | (0.02) |
| Effects of income wave 7 on | ||||||
| Physical health wave 7 | 0.06 | (0.03) | – | – | 0.06 | (0.03) |
| Physical health wave 9 | 0.03* | (0.02) | 0.04 | (0.02) | 0.08** | (0.02) |
| Effects of income wave 9 on | ||||||
| Physical health wave 9 | 0.02 | (0.02) | – | – | 0.02 | (0.02) |
Chi square (d.f.) 1797.19 (264)***RMSEA 0.036 (0.035–0.038) CFI 0.91 TLI 0.88.
Source: Understanding Society waves 1, 3, 5, 7, and 9, n = 4444. Adjusted for complex survey design. Model also adjusts for age and gender. *p < 0.05 **p < 0.01 ***p < 0.001.
3.2. Racism and health by age group
Table 4 presents the results of the multi-group structural equation model of mental health by age group. There are significant, negative covariances between age and racism for 50–59 year olds and the over 60s. This suggests that older people are less likely to report racism. Nonetheless, the patterns of effects of racism on mental health are very similar across age groups, and the formal test of group invariance (i.e. whether estimates differ across age groups) is not significant for racism and mental health. The total effects of racism on mental health in both waves are strong and negative for all age groups; the strongest effects are racism in wave 7 on health for the under 30s (coefficients −0.24 in wave 7 and -0.15 in wave 9), 30–39 year olds (coefficients −0.33 in wave 7 and -0.12 in wave 9), and 50–59 year olds (coefficients −0.24 in wave 7 and -0.20 in wave 9). For all age groups, there are strong direct effects of racism on mental health where reported in the same wave, and strong indirect effects of racism on mental health where reported in the subsequent wave.
Table 4.
Decomposition of the direct and indirect effects of racism on mental health by age group (standardised coefficients).
| Direct effects |
Indirect effects |
Total effects |
||||
|---|---|---|---|---|---|---|
| Std. Coef | Std. Error | Std. Coef | Std. Error | Std. Coef | Std. Error | |
| Under 30s | ||||||
| Effects of racism wave 7 on | ||||||
| Income wave 7 | −0.09 | (0.07) | – | – | −0.09 | (0.07) |
| Income wave 9 | −0.05 | (0.06) | −0.06 | (0.05) | −0.11 | (0.06) |
| Mental health wave 7 | −0.25* | (0.09) | 0.00 | (0.01) | −0.24* | (0.09) |
| Mental health wave 9 | −0.03 | (0.08) | −0.13* | (0.05) | −0.15 | (0.07) |
| Effects of racism wave 9 on | ||||||
| Income wave 9 | 0.05 | (0.06) | – | – | 0.05 | (0.06) |
| Mental health wave 9 | 0.00 | (0.08) | 0.00 | (0.01) | 0.00 | (0.07) |
| Effects of income wave 7 on | ||||||
| Mental health wave 7 | −0.03 | (0.04) | – | – | −0.03 | (0.04) |
| Mental health wave 9 | −0.06 | (0.07) | 0.02 | (0.06) | −0.03 | (0.06) |
| Effects of income wave 9 on | ||||||
| Mental health wave 9 |
0.05 |
(0.08) |
– |
– |
0.05 |
(0.08) |
| 30–39 year olds | ||||||
| Effects of racism wave 7 on | ||||||
| Income wave 7 | −0.13** | (0.04) | – | – | −0.13** | (0.04) |
| Income wave 9 | −0.07* | (0.03) | −0.08** | (0.03) | −0.15** | (0.04) |
| Mental health wave 7 | −0.33*** | (0.07) | −0.00 | (0.01) | −0.33*** | (0.07) |
| Mental health wave 9 | 0.04 | (0.06) | −0.16** | (0.04) | −0.12* | (0.05) |
| Effects of racism wave 9 on | ||||||
| Income wave 9 | 0.03 | (0.04) | – | – | 0.03 | (0.04) |
| Mental health wave 9 | −0.12 | (0.06) | 0.00 | (0.00) | −0.12 | (0.06) |
| Effects of income wave 7 on | ||||||
| Mental health wave 7 | 0.03 | (0.06) | – | – | 0.03 | (0.06) |
| Mental health wave 9 | −0.02 | (0.05) | 0.04 | (0.04) | 0.02 | (0.05) |
| Effects of income wave 9 on | ||||||
| Mental health wave 9 |
0.04 |
(0.05) |
– |
– |
0.04 |
(0.05) |
| 40–49 year olds | ||||||
| Effects of racism wave 7 on | ||||||
| Income wave 7 | −0.04 | (0.12) | – | – | −0.04 | (0.12) |
| Income wave 9 | −0.01 | (0.06) | −0.02 | (0.06) | −0.03 | (0.06) |
| Mental health wave 7 | −0.14* | (0.06) | −0.00 | (0.01) | −0.14* | (0.05) |
| Mental health wave 9 | 0.08* | (0.04) | −0.07* | (0.03) | 0.01 | (0.04) |
| Effects of racism wave 9 on | ||||||
| Income wave 9 | −0.07 | (0.04) | – | – | −0.07 | (0.04) |
| Mental health wave 9 | −0.14** | (0.04) | −0.00 | (0.00) | −0.14** | (0.04) |
| Effects of income wave 7 on | ||||||
| Mental health wave 7 | 0.05 | (0.08) | – | – | 0.05 | (0.08) |
| Mental health wave 9 | −0.00 | (0.08) | 0.04 | (0.04) | 0.04 | (0.07) |
| Effects of income wave 9 on | ||||||
| Mental health wave 9 |
0.03 |
(0.04) |
– |
– |
0.03 |
(0.04) |
| 50–59 year olds | ||||||
| Effects of racism wave 7 on | ||||||
| Income wave 7 | −0.16* | (0.08) | – | – | −0.16* | (0.08) |
| Income wave 9 | −0.06 | (0.05) | −0.10* | (0.05) | −0.16* | (0.05) |
| Mental health wave 7 | −0.21** | (0.09) | −0.03 | (0.01) | −0.24** | (0.10) |
| Mental health wave 9 | −0.05 | (0.11) | −0.15** | (0.05) | −0.20 | (0.10) |
| Effects of racism wave 9 on | ||||||
| Income wave 9 | 0.01 | (0.09) | – | – | 0.01 | (0.09) |
| Mental health wave 9 | −0.10 | (0.11) | 0.00 | (0.02) | −0.09 | (0.11) |
| Effects of income wave 7 on | ||||||
| Mental health wave 7 | 0.16* | (0.07) | – | – | 0.16* | (0.07) |
| Mental health wave 9 | −0.07 | (0.07) | 0.21** | (0.07) | 0.14* | (0.06) |
| Effects of income wave 9 on | ||||||
| Mental health wave 9 |
0.19** |
(0.06) |
– |
– |
0.19** |
(0.06) |
| Over 60s | ||||||
| Effects of racism wave 7 on | ||||||
| Income wave 7 | −0.04 | (0.04) | – | – | −0.04 | (0.04) |
| Income wave 9 | −0.03 | (0.03) | −0.02 | (0.03) | −0.05 | (0.04) |
| Mental health wave 7 | −0.12 | (0.10) | −0.00 | (0.00) | −0.13 | (0.10) |
| Mental health wave 9 | −0.02 | (0.07) | −0.06 | (0.05) | −0.08 | (0.10) |
| Effects of racism wave 9 on | ||||||
| Income wave 9 | 0.00 | (0.02) | – | – | 0.00 | (0.02) |
| Mental health wave 9 | −0.12 | (0.06) | 0.00 | (0.00) | −0.12 | (0.06) |
| Effects of income wave 7 on | ||||||
| Mental health wave 7 | 0.07* | (0.03) | – | – | 0.07* | (0.03) |
| Mental health wave 9 | −0.13** | (0.05) | 0.13*** | (0.04) | −0.00 | (0.04) |
| Effects of income wave 9 on | ||||||
| Mental health wave 9 | 0.14** | (0.04) | – | – | 0.14** | (0.04) |
Chi square (d.f.) 537.948 (227)***RMSEA 0.036 (0.032–0.040) CFI 0.96 TLI 0.94.
Source: Understanding Society waves 7 and 9, n = 5190 across 5 groups. Adjusted for complex survey design. Model also adjusts for age and gender. *p < 0.05 **p < 0.01 ***p < 0.001.
The effects of racism on income are also strongest for the under 30s, 30–39 year olds, and 50–59 year olds in wave 7. The total effects of income on mental health are strong and significant for the two oldest age groups: the 50–59 year olds (coefficients 0.16 in wave 7 and 0.19 in wave 9) and the over 60s (coefficients 0.07 in wave 7 and 0.14 in wave 9). The total effects are largely driven by strong direct effects when income and mental health are reported in the same wave.
Table 5 presents the results of the multi-group structural equation model of physical health by age group. The formal test of group invariance (i.e. whether estimates differ across age groups) is significant for racism and physical health. The model output would suggest that this is the difference between the under 30s and all other age groups. For the under 30s, the total effects of racism in wave 7 are negligible on physical health in wave 7, positive on physical health in wave 9, and the effects of racism in wave 9 are very strong and negative on physical health in wave 9. For all age groups over 30, there are strong, negative total effects of racism in wave 7 on physical health in waves 7 and 9. These effects are strongest for the 40–49 year olds (coefficients −0.26 in wave 7 and -0.27 in wave 9) and 50–59 year olds (coefficients −0.25 in wave 7 and -0.15 in wave 9). The effects of racism in wave 9 on physical health in wave 9 are stronger for the two oldest age groups compared with the 30–39 and 40–49 year olds. For all age groups over the age of 30, there are strong direct effects of racism on physical health where reported in the same wave, and strong indirect effects of racism on physical health where reported in the subsequent wave. These effects are significant for the 30–39, 40–49, and 50–59 age groups, but they are not significant for the over 60s.
Table 5.
Decomposition of the direct and indirect effects of racism on physical health by age group (standardised coefficients).
| Direct effects |
Indirect effects |
Total effects |
||||
|---|---|---|---|---|---|---|
| Std. Coef | Std. Error | Std. Coef | Std. Error | Std. Coef | Std. Error | |
| Under 30s | ||||||
| Effects of racism wave 7 on | ||||||
| Income wave 7 | −0.08 | (0.07) | – | – | −0.08 | (0.07) |
| Income wave 9 | −0.04 | (0.06) | −0.06 | (0.05) | −0.09 | (0.06) |
| Physical health wave 7 | −0.00 | (0.08) | −0.01 | (0.01) | −0.02 | (0.08) |
| Physical health wave 9 | 0.20 | (0.11) | −0.01 | (0.04) | 0.19 | (0.10) |
| Effects of racism wave 9 on | ||||||
| Income wave 9 | 0.04 | (0.06) | – | – | 0.04 | (0.06) |
| Physical health wave 9 | −0.29* | (0.11) | 0.00 | (0.01) | −0.29* | (0.11) |
| Effects of income wave 7 on | ||||||
| Physical health wave 7 | 0.17** | (0.04) | – | – | 0.17** | (0.04) |
| Physical health wave 9 | −0.04 | (0.07) | 0.14* | (0.06) | 0.10** | (0.05) |
| Effects of income wave 9 on | ||||||
| Physical health wave 9 |
0.09 |
(0.09) |
– |
– |
0.09 |
(0.09) |
| 30–39 year olds | ||||||
| Effects of racism wave 7 on | ||||||
| Income wave 7 | −0.13** | (0.04) | – | – | −0.13** | (0.04) |
| Income wave 9 | −0.07* | (0.03) | −0.08** | (0.03) | −0.15** | (0.04) |
| Physical health w7 | −0.12* | (0.06) | −0.00 | (0.01) | −0.13* | (0.05) |
| Physical health w9 | −0.09 | (0.06) | −0.08** | (0.03) | −0.17* | (0.08) |
| Effects of racism wave 9 on | ||||||
| Income wave 9 | 0.03 | (0.04) | – | – | 0.03 | (0.04) |
| Physical health wave 9 | −0.02 | (0.06) | 0.00 | (0.00) | −0.02 | (0.06) |
| Effects of income wave 7 on | ||||||
| Physical health wave 7 | 0.03 | (0.04) | – | – | 0.03 | (0.04) |
| Physical health wave 9 | 0.05 | (0.04) | 0.04 | (0.03) | 0.09 | (0.05) |
| Effects of income wave 9 on | ||||||
| Physical health wave 9 |
0.04 |
(0.04) |
– |
– |
0.04 |
(0.04) |
| 40–49 year olds | ||||||
| Effects of racism wave 7 on | ||||||
| Income wave 7 | −0.04 | (0.12) | – | – | −0.04 | (0.12) |
| Income wave 9 | −0.02 | (0.06) | −0.02 | (0.07) | −0.04 | (0.06) |
| Physical health wave 7 | −0.25** | (0.08) | −0.00 | (0.01) | −0.26** | (0.08) |
| Physical health wave 9 | −0.12 | (0.06) | −0.16** | (0.05) | −0.27** | (0.09) |
| Effects of racism wave 9 on | ||||||
| Income wave 9 | −0.07 | (0.04) | – | – | −0.07 | (0.04) |
| Physical health wave 9 | 0.01 | (0.05) | −0.00 | (0.00) | 0.01 | (0.04) |
| Effects of income wave 7 on | ||||||
| Physical health wave 7 | 0.11 | (0.06) | – | – | 0.11 | (0.06) |
| Physical health wave 9 | 0.02 | (0.06) | 0.10 | (0.04) | 0.12 | (0.05) |
| Effects of income wave 9 on | ||||||
| Physical health wave 9 |
0.06 |
(0.04) |
– |
– |
0.06 |
(0.04) |
| 50–59 year olds | ||||||
| Effects of racism wave 7 on | ||||||
| Income wave 7 | −0.16* | (0.08) | – | – | −0.16* | (0.08) |
| Income wave 9 | −0.05 | (0.05) | −0.10* | (0.05) | −0.15** | (0.05) |
| Physical health wave 7 | −0.22 | (0.12) | −0.03 | (0.02) | −0.25 | (0.11) |
| Physical health wave 9 | 0.04 | (0.11) | −0.19 | (0.08) | −0.15 | (0.09) |
| Effects of racism wave 9 on | ||||||
| Income wave 9 | 0.01 | (0.09) | – | – | 0.01 | (0.09) |
| Physical health wave 9 | −0.07 | (0.09) | 0.00 | (0.00) | −0.07 | (0.09) |
| Effects of income wave 7 on | ||||||
| Physical health wave 7 | 0.18** | (0.06) | – | – | 0.18** | (0.06) |
| Physical health wave 9 | 0.06 | (0.05) | 0.14* | (0.06) | 0.20** | (0.06) |
| Effects of income wave 9 on | ||||||
| Physical health wave 9 |
0.02 |
(0.05) |
– |
– |
0.02 |
(0.05) |
| Over 60s | ||||||
| Effects of racism wave 7 on | ||||||
| Income wave 7 | −0.04 | (0.04) | – | – | −0.04 | (0.04) |
| Income wave 9 | −0.03 | (0.02) | −0.02 | (0.03) | −0.05 | (0.04) |
| Physical health wave 7 | −0.10 | (0.06) | −0.00 | (0.00) | −0.11 | (0.06) |
| Physical health wave 9 | −0.00 | (0.07) | −0.07 | (0.04) | −0.07 | (0.08) |
| Effects of racism wave 9 on | ||||||
| Income wave 9 | 0.00 | (0.02) | – | – | 0.00 | (0.02) |
| Physical health wave 9 | −0.05 | (0.04) | −0.00 | (0.00) | −0.05 | (0.04) |
| Effects of income wave 7 on | ||||||
| Physical health wave 7 | 0.10** | (0.03) | – | – | 0.10** | (0.03) |
| Physical health wave 9 | 0.08** | (0.03) | 0.02 | (0.04) | 0.10** | (0.03) |
| Effects of income wave 9 on | ||||||
| Physical health wave 9 | −0.07 | (0.04) | – | – | −0.07 | (0.04) |
Chi square (d.f.) 614.08 (227)***RMSEA 0.041 (0.037–0.044) CFI 0.95 TLI 0.93.
Source: Understanding Society waves 7 and 9, n = 5190 across 5 groups. Adjusted for complex survey design. Model also adjusts for age and gender. *p < 0.05 **p < 0.01 ***p < 0.001.
The effects of racism on income are also strongest for the under 30s, 30–39 year olds, and 50–59 year olds in wave 7. The total effects of income in wave 7 on physical health in waves 7 and 9 are strong and significant for the under 30s (coefficients 0.17 in wave 7 and 0.10 in wave 9), 50–59 year olds (coefficients 0.18 in wave 7 and 0.20 in wave 9), and the over 60s (coefficients 0.10 in both waves). The effects are of a similar magnitude, but not significant, for the 40–49 year olds (coefficients 0.11 and 0.12), and much weaker for the 30–39 year olds (coefficients 0.03 and 0.09). The total effects of income in wave 9 on physical health in wave tend to be smaller than the effects of income in wave 7.
4. Discussion
The central aims of this paper were to better understand the workings of racism over time, whether this differs by age, and how racism indirectly impacts on health via its impact on socio-economic inequalities. We estimated longitudinal structural equation models and decomposed the total, direct, and indirect effects of racism on health over a ten-year period, and by ten-year age groups. The results clearly indicate that exposure to racism severely and negatively impacts the health of people from minoritised ethnic groups in the UK. Our findings make an important contribution to the existing literature as we demonstrate the persistence of these effects over time and across age groups. In particular, by investigating the effects of racism on health by age, our approach allows us to understand processes of accumulation and the importance of life stage. Repeated exposure to racism leads to an accumulation of disadvantage and poorer health outcomes over the life course.
When racism is reported at the same time as health, there are strong direct and negative effects. The indirect effects (i.e., operating through income) when measured at the same time as health are negligible. When racism is reported before health, there are strong indirect effects operating through income and prior health over time. This clearly demonstrates the enduring effect of racism which operates both directly at the time of experiencing racism, as well as indirectly, operating through lower income and poorer health over time. For mental health, these effects are consistent across waves, and for physical health these effects are stronger in more recently collected data. The effects of racism on mental health are not significantly different by age group, suggesting that the effects of racism are consistent over the life course. The effects of racism on physical health are significantly different by age group, with the models suggesting slightly different patterns of effects for the under 30s compared with all other age groups. This complements previous literature which has demonstrated that ethnic inequalities in physical health outcomes greatly and progressively increase after the age of 30 (Nazroo, 2006; Stopforth et al., 2022).
The effects of experienced interpersonal racism on health persist, but are slightly weaker in the oldest age group (the over 60s). When estimating the multi-group models by age, there are significant, negative covariances between age and racism for the two oldest age groups, suggesting that older people are less likely to report racism. Under-reporting of racism and discrimination for older people has been demonstrated in previous empirical work (Bécares et al., 2009; Breheny et al., 2021). There are a number of potential explanations for this, for example, a desensitisation to racism as a result of sustained experiences of racism and discrimination over the life course. People from older age groups may also become less exposed to racism and racial discrimination as they withdraw from the workplace. Older people may also be more likely to experience racism vicariously through children and grandchildren, and this is not captured by the measures we used. By contrast, the effects of income on mental and physical health are greater for the older age groups. This suggests that the effects of previous discrimination and racism may operate more strongly on the health of older people from minoritised ethnic groups. Life course accumulation of disadvantage, as a result of lower paid, more insecure employment situations, may result in this greater effect on health in later life.
In previous studies of racism and health, measures of racism only capture direct experiences of interpersonal racial discrimination (Bécares et al., 2015b). This is the case in the present study. We cannot address all levels or domains of racial discrimination and harassment using the available data. Further, the measures of racism and discrimination relate to experiences within the past 12 months and therefore we cannot assess the effects of racism occurring earlier in people's lives. Due to the rotating questionnaire module, we can only observe experiences of racism every two years. Racism further has negative effects on the health of people who experience it vicariously (Bécares et al., 2015a; Gee et al., 2012), which cannot be captured using these measures. Self-reported measures of experiences of racism may not capture the full effects, as the pervasiveness of racism within society means that individuals may not perceive or report racism (Paradies, 2006). However, not reporting racism does not remove the negative health impact caused by the experience. We expect that our results therefore will underestimate the full range of racial discrimination faced by people from minoritised ethnic groups and will not account for the impact of earlier experiences on health outcomes over the life course.
We cannot adequately study life course effects of racism on health with current data available within the UK. Existing life course surveys, such as the earlier British birth cohorts, or longer-running surveys, such as the British Household Panel Survey, do not have suitable sample sizes of ethnic minority people, or suitable measures of racial discrimination in their questionnaires. Understanding Society helps to fill this data gap by asking detailed questions about racial discrimination to a subset of respondents, and by incorporating ethnic minority boost samples within the original survey design, but at the time of analysis this was limited to ten waves of data with five observations on experiences of harassment and abuse. We have navigated this obstacle by examining the effects of racism on health for all ages over a ten-year period, and by separately examining the effects of racism on health by ten-year age groups for the latest two waves of data, when sample sizes were large enough. Although longitudinal data were not available for some respondents, this does not detract from the main message of the paper about the strength of direct and indirect effects both within and across waves. We are further limited by the considerably smaller sample sizes of older ethnic minority people in Understanding Society. In this analysis, half of the over 60s group were aged 68 or younger, and only a quarter of the group were over the age of 75. This is a systemic problem in all social surveys and administrative data and one that continues to contribute to the marginalisation of older ethnic minority people in the UK (Bécares et al., 2020). Future data collection needs to better represent older ethnic minority people and adequately capture historical experiences of racism and discrimination, to enable more robust understandings of the effects of racism on health outcomes over the entire life course.
Racism and racial discrimination experienced by people from minoritised ethnic groups has a strong association with poorer health outcomes (Paradies, 2006; Paradies et al., 2015; Williams et al., 2019; Williams & Mohammed, 2013). It is well-established that socio-economic inequalities lead to poorer mental and physical health (Bartley et al., 2004; Maheswaran et al., 2015; Scambler, 2012). Indeed, ethnic inequalities in socio-economic circumstances are directly related to ethnic inequalities in health (Nazroo, 2001). However, policy and academic debates around ethnic inequalities focus almost entirely on socio-economic factors, and largely ignore the underlying processes of structural, institutional and interpersonal racism (see Nazroo & Bécares, 2021; Torres, 2020). Findings from this study not only cement the evidence on the harm of racial discrimination on health over time, but also bring to light the central role of racism in reduced socio-economic positions for people from minoritised ethnic groups.
Ethics statement
This study is a secondary data analysis of Understanding Society. The University of Essex Ethics Committee has approved all data collection on Understanding Society main study and innovation panel waves.
Funding
This work was supported by the Nuffield Foundation (LB, award WEL/43881), but the views expressed are those of the authors and not necessarily those of the Foundation. Laia Bécares, James Nazroo, and Dharmi Kapadia also received funding from the ESRC (ES/W000849/1).
CRediT author statement
Sarah Stopforth: Methodology, Software, Data curation, Formal analysis, Writing - original draft, Writing – review & editing. Dharmi Kapadia: Conceptualization, Writing – review & editing. James Nazroo: Conceptualization, Writing – review & editing. Laia Bécares: Conceptualization, Writing – review & editing, Visualization, Supervision, Project administration.
Declaration of interest
None.
Acknowledgements
We gratefully acknowledge the participants of Understanding Society, the UK Household Longitudinal Study. This work was supported by the Nuffield Foundation (LB, award WEL/43881), but the views expressed are those of the authors and not necessarily those of the Foundation. Laia Bécares, James Nazroo, and Dharmi Kapadia also received funding from the ESRC (ES/W000849/1).
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.ssmph.2022.101217.
Contributor Information
Sarah Stopforth, Email: sarah.stopforth@kcl.ac.uk.
Dharmi Kapadia, Email: dharmi.kapadia@manchester.ac.uk.
James Nazroo, Email: james.nazroo@manchester.ac.uk.
Laia Bécares, Email: laia.becares@kcl.ac.uk.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
Data availability
The authors do not have permission to share data.
References
- Bartley M., Sacker A., Clarke P. Employment status, employment conditions, and limiting illness: Prospective evidence from the British household panel survey 1991-2001. Journal of Epidemiology & Community Health. 2004;58:501–506. doi: 10.1136/jech.2003.009878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bécares L., Kapadia D., Nazroo J. Neglect of older ethnic minority people in UK research and policy. BMJ. 2020;368:m212. doi: 10.1136/bmj.m212. [DOI] [PubMed] [Google Scholar]
- Bécares L., Nazroo J., Kelly Y. A longitudinal examination of maternal, family, and area-level experiences of racism on children's socioemotional development: Patterns and possible explanations. Social Science & Medicine. 2015;142:128–135. doi: 10.1016/j.socscimed.2015.08.025. [DOI] [PubMed] [Google Scholar]
- Bécares L., Nazroo J., Kelly Y. A longitudinal examination of maternal, family, and area-level experiences of racism on children's socioemotional development: Patterns and possible explanations. Social Science & Medicine. 2015;142:128–135. doi: 10.1016/j.socscimed.2015.08.025. [DOI] [PubMed] [Google Scholar]
- Bécares L., Stafford M., Nazroo J. Fear of racism, employment and expected organizational racism: Their association with health. The European Journal of Public Health. 2009;19:504–510. doi: 10.1093/eurpub/ckp071. [DOI] [PubMed] [Google Scholar]
- Bécares L., Zhang N. Perceived interpersonal discrimination and older women's mental health: Accumulation across domains, attributions, and time. American Journal of Epidemiology. 2018;187:924–932. doi: 10.1093/aje/kwx326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Breheny M., Stevenson B., Bécares L., Abelson J., Rafferty J., Cormack D. Tabulating experiences of racism and racial discrimination across the life course. Stigma and health (Washington, D.C.) 2021;6:43–52. [Google Scholar]
- Brynin M., Longhi S. Joseph Rowntree Foundation; London: 2015. The effect of occupation on poverty among ethnic minority groups. [Google Scholar]
- Clark K., Shankley W. In: Ethnicity, race and inequality in the UK: State of the nation. Byrne B., Alexander C., Khan O., Nazroo J., Shankley W., editors. Policy Press; Bristol: 2020. Ethnic minorities in the labour market in Britain. [Google Scholar]
- Darlington F., Norman P., Ballas D., Exeter D.J. Exploring ethnic inequalities in health: Evidence from the health survey for england, 1998-2011. Diversity and Equality in Health and Care. 2015;12:54–65. [Google Scholar]
- Dolezsar C.M., McGrath J.J., Herzig A.J.M., Miller S.B. Perceived racial discrimination and hypertension: A comprehensive systematic review. Health Psychology. 2014;33:20–34. doi: 10.1037/a0033718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Evandrou M., Falkingham J., Feng Z., Vlachantoni A. Ethnic inequalities in limiting health and self-reported health in later life revisited. Journal of Epidemiology & Community Health. 2016;70:653–662. doi: 10.1136/jech-2015-206074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Finney N., Harries B. Vol. 23. Race Equality Foundation; London: 2013. Understanding ethnic inequalities in housing: Analysis of the 2011 Census. (Better housing briefing). [Google Scholar]
- Forde A.T., Crookes D.M., Suglia S.F., Demmer R.T. The weathering hypothesis as an explanation for racial disparities in health: A systematic review. Annals of Epidemiology. 2019;33:1–18. doi: 10.1016/j.annepidem.2019.02.011. e13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gee G.C., Hing A., Mohammed S., Tabor D.C., Williams D.R. Racism and the life course: Taking time seriously. American Journal of Public Health. 2019;109:S43–S47. doi: 10.2105/AJPH.2018.304766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gee G.C., Walsemann K.M., Brondolo E. A life course perspective on how racism may Be related to health inequities. American Journal of Public Health. 2012;102:967–974. doi: 10.2105/AJPH.2012.300666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Geronimus A.T. The weathering hypothesis and the health of african-American women and infants: Evidence and speculations. Ethnicity & Disease. 1992;2:207–221. [PubMed] [Google Scholar]
- Harris R., Tobias M., Jeffreys M., Waldegrave K., Karlsen S., Nazroo J. Effects of self-reported racial discrimination and deprivation on māori health and inequalities in New Zealand: Cross-sectional study. The Lancet. 2006;367:2005–2009. doi: 10.1016/S0140-6736(06)68890-9. [DOI] [PubMed] [Google Scholar]
- Hooper D., Coughlan J., Mullen M. Structural equation modelling: Guidelines for determining model fit. Electronic Journal of Business Research Methods. 2008;6:53–60. [Google Scholar]
- Hudson D.L., Puterman E., Bibbins-Domingo K., Matthews K.A., Adler N.E. Race, life course socioeconomic position, racial discrimination, depressive symptoms and self-rated health. Social Science & Medicine. 2013;97:7–14. doi: 10.1016/j.socscimed.2013.07.031. [DOI] [PubMed] [Google Scholar]
- Iacobucci D. Structural equations modeling: Fit Indices, sample size, and advanced topics. Journal of Consumer Psychology. 2010;20:90–98. [Google Scholar]
- Jivraj S., Khan O. In: Ethnic identity and inequalities in Britain: The dynamics of diversity. Jivraj S., Simpson L., editors. Policy Press; Bristol: 2015. How likely are people from minority ethnic groups to live in deprived neighbourhoods? pp. 199–213. [Google Scholar]
- Jones C.P. Levels of racism: A theoretic framework and a gardener's tale. American Journal of Public Health. 2000;90:1212–1215. doi: 10.2105/ajph.90.8.1212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kapadia D., Nazroo J., Clark K. In: Ethnic identity and inequalities in Britain: The dynamics of diversity. Jivraj S., Simpson L., editors. Policy Press; Bristol: 2015. Have ethnic inequalities in the labour market persisted? pp. 161–179. [Google Scholar]
- Karlsen S., Nazroo J.Y. Agency and structure: The impact of ethnic identity and racism on the health of ethnic minority people. Sociology of Health & Illness. 2002;24:1–20. [Google Scholar]
- Karlsen S., Nazroo J.Y. Relation between racial discrimination, social class, and health among ethnic minority groups. American Journal of Public Health. 2002;92:624–631. doi: 10.2105/ajph.92.4.624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Karlsen S., Nazroo J.Y. Fear of racism and health. Journal of Epidemiology & Community Health. 2004;58:1017–1018. doi: 10.1136/jech.2004.020479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Karlsen S., Nazroo J.Y., McKenzie K., Bhui K., Weich S. Racism, psychosis and common mental disorder among ethnic minority groups in England. Psychological Medicine. 2005;35:1795–1803. doi: 10.1017/S0033291705005830. [DOI] [PubMed] [Google Scholar]
- Lewis T.T., Williams D.R., Tamene M., Clark C.R. Self-reported experiences of discrimination and cardiovascular disease. Current cardiovascular risk reports. 2014;8 doi: 10.1007/s12170-013-0365-2. 365-365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maheswaran H., Kupek E., Petrou S. Self-reported health and socio-economic inequalities in England, 1996-2009: Repeated national cross-sectional study. Social Science & Medicine. 2015;136–137:135–146. doi: 10.1016/j.socscimed.2015.05.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nandi A., Luthra R., Benzeval M. ISER Working Paper Series: Institute for Social and Economic Research, University of Essex; 2016. Ethnic and racial harassment and mental health : Identifying sources of resilience. [Google Scholar]
- Nazroo J.Y. Policy Studies Institute; London, England: 2001. Ethnicity, class and health. [Google Scholar]
- Nazroo J.Y. The structuring of ethnic inequalities in health: Economic position, racial discrimination, and racism. American Journal of Public Health. 2003;93:277–284. doi: 10.2105/ajph.93.2.277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nazroo J. In: The futures of old age. Vincent J.A., Phillipson C., Downs M., editors. Sage; 2006. Ethnicity and old age; pp. 65–76. [Google Scholar]
- Nazroo J., Bécares L. Evidence for ethnic inequalities in mortality related to COVID-19 infections: Findings from an ecological analysis of england. BMJ Open. 2020;10 doi: 10.1136/bmjopen-2020-041750. e041750-e041750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nazroo J., Bécares L. Ethnic inequalities in COVID-19 mortality: A consequence of persistent racism. London: Runnymede trust and centre of dynamics on ethnicity. 2021. https://www.runnymedetrust.org/uploads/Runnymede%20CoDE%20COVID%20briefing%20v3.pdf Available at.
- Nazroo J.Y., Bhui K.S., Rhodes J. Where next for understanding race/ethnic inequalities in severe mental illness? Structural, interpersonal and institutional racism. Sociology of Health & Illness. 2020;42:262–276. doi: 10.1111/1467-9566.13001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Office for National Statistics . Office for National Statistics; London: 2015. Family spending in the UK: Calendar year 2014.https://www.ons.gov.uk/peoplepopulationandcommunity/personalandhouseholdfinances/incomeandwealth/compendium/familyspending/2015 available at. [Google Scholar]
- Paradies Y. A systematic review of empirical research on self-reported racism and health. International Journal of Epidemiology. 2006;35:888–901. doi: 10.1093/ije/dyl056. [DOI] [PubMed] [Google Scholar]
- Paradies Y., Ben J., Denson N., Elias A., Priest N., Pieterse A., et al. Racism as a determinant of health: A systematic review and meta-analysis. PLoS One. 2015;10 doi: 10.1371/journal.pone.0138511. e0138511-e0138511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pascoe E.A., Smart Richman L. Perceived discrimination and health: A meta-analytic review. Psychological Bulletin. 2009;135:531–554. doi: 10.1037/a0016059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scambler G. Health inequalities. Sociology of Health & Illness. 2012;34:130–146. doi: 10.1111/j.1467-9566.2011.01387.x. [DOI] [PubMed] [Google Scholar]
- Schmitt M.T., Branscombe N.R., Postmes T., Garcia A. The consequences of perceived discrimination for psychological well-being: A meta-analytic review. Psychological Bulletin. 2014;140:921–948. doi: 10.1037/a0035754. [DOI] [PubMed] [Google Scholar]
- Schreiber J.B., Nora A., Stage F.K., Barlow E.A., King J. Reporting structural equation modeling and confirmatory factor Analysis results: A review. The Journal of Educational Research. 2006;99:323–338. [Google Scholar]
- Shankley W., Finney N. In: Ethnicity, race and inequality in the UK: State of the nation. Byrne B., Alexander C., Khan O., Nazroo J., Shankley W., editors. Policy Press; Bristol: 2020. Ethnic minorities and housing in Britain. [Google Scholar]
- StataCorp . StataCorp LLC; College Station, TX: 2019. Stata statistical software: Release 16. [Google Scholar]
- Stopforth S., Bécares L., Kapadia D., Nazroo J. In: The routledge handbook of contemporary inequalities and the life course. Nico M., Pollock G., editors. Routledge; Oxon: 2022. A life course approach to understanding ethnic health inequalities in later life: An example using the United Kingdom as national context; pp. 383–393. [Google Scholar]
- Torres S. Racialization without racism in scholarship on old age. Swiss Journal of Sociology. 2020;46:331–349. [Google Scholar]
- University of Essex, Institute for Social and Economic Research . 12th ed. UK Data Service; 2020. Understanding society: Waves 1-9, 2009-2018 and harmonised BHPS: Waves 1-18, 1991-2009. [data collection] [Google Scholar]
- Wallace S., Nazroo J., Bécares L. Cumulative effect of racial discrimination on the mental health of ethnic minorities in the United Kingdom. American Journal of Public Health. 2016;106:1294–1300. doi: 10.2105/AJPH.2016.303121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ware J.E., Kosinski M., Turner-Bowker D.M., Gandek B. QualityMetric Incorporated; Lincoln, RI: 2001. How to score version 2 of the SF-12 health survey (with a supplement documenting version 1) [Google Scholar]
- Williams D.R. Race, socioeconomic status, and health. The added effects of racism and discrimination. Annals of the New York Academy of Sciences. 1999;896:173–188. doi: 10.1111/j.1749-6632.1999.tb08114.x. [DOI] [PubMed] [Google Scholar]
- Williams D.R., Lawrence J.A., Davis B.A. Racism and health: Evidence and needed research. Annual Review of Public Health. 2019;40:105–125. doi: 10.1146/annurev-publhealth-040218-043750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams D.R., Mohammed S.A. Racism and health I: Pathways and scientific evidence. American Behavioral Scientist. 2013;57:1–19. doi: 10.1177/0002764213487340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams D.R., Neighbors H. Racism, discrimination and hypertension: Evidence and needed research. Ethnicity & Disease. 2001;11:800–816. [PubMed] [Google Scholar]
- Wright S. Path coefficients and path regressions: Alternative or complementary concepts? Biometrics. 1960;16:189–202. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The authors do not have permission to share data.