Abstract
Our goal was to examine inequality in healthcare utilization and the factors that contribute to inequality between China's floating and native populations. Based on the China Labor-force Dynamics Surveys from 2014 to 2018, which used three rounds of data, we utilized a panel probit model that included fixed effects for time and province to estimate the probability of healthcare utilization for floating and native populations. In addition, we calculated the degree of inequality in healthcare utilization by using the method of mobility-related inequality and a decomposition approach was used to explain the contribution of each factor to the inequality. The floating population utilized healthcare at a lower rate, with a 10.5% probability of visiting a hospital and a 20.9% probability of receiving hospitalized treatment. The concentration index of mobility-related inequality in healthcare utilization shows a negative coefficient of −0.137 for hospital visits and −0.356 for hospitalized treatment. Contribution decomposition shows that self-assessed health, job category and household registration account for the largest contribution to the inequality in hospital visits, contributing −0.038, 0.021 and −0.017, respectively. Age, household registration and insurance account for the largest contribution to the inequality in hospitalized treatment, contributing −0.053, 0.024 and −0.023, respectively. The floating population was less likely to use health services and faced an inequality in treatment compared with the native population.
Keywords: concentration index, floating population, healthcare utilization, inequality, pro-native population
Introduction
The World Health Organization's Global Action Plan outlines the goals for human rights for everyone and equity in human rights means that everyone has a chance to receive essential healthcare services as needed. Its primary goal is to achieve universal health coverage (UHC) through the full and equal admission of immigrants to healthcare systems.1,2 A wide range of global literature indicates that there is a connection between immigration, health and disease and that immigration affects the epidemiology of diseases globally and especially in recipient countries.3 However, when accessing essential healthcare services, immigrants face many barriers, including differences in language, culture, irregular immigration identities and exclusionary healthcare policies and public services.4 Studies in Europe have demonstrated that immigrant populations are less likely than native populations to use healthcare services.4 Immigrants are usually one of the most vulnerable groups around the world in terms of the use of healthcare; they should have equal access to local national healthcare systems, but do not receive these rights.
In 2018 there were 241 million internal migrants in China, which accounted for 17.27% of China's total population.5 Internal migrants (floating population) are defined as those who live outside of the city where they are registered; they also constitute the majority of China's rural-to-urban migrant population. China's household registration system (also known as hukou) is a legacy of the dualistic economy that was established in the 1950s. It serves as an effective measure to restrict movement from rural to urban regions or from one place to another. In China, many social welfare programs and public policies are implemented for eligible native residents based on the long-established hukou system.6,7 The result is that local healthcare benefits and social welfare are only available to native populations with a registered hukou, but not to the floating population.8 Following China's rapid urbanization over the past 30 y, the hukou no longer restricts mobility but still affects migrants’ lives in other ways, such as limiting access to social welfare and healthcare services,9 which prevents the implementation of UHC in China. Because of their hukou restrictions and lower socio-economic status, these floating populations usually have limited access to healthcare services, resulting in growing barriers to healthcare utilization among the different groups of residents.10,11
Equity should be an essential part of UHC.12 But despite these noble intentions, recent literature indicates that UHC may be implemented in low- and middle-income countries by addressing inequalities in the quality of healthcare provided, as there is a pro-rich phenomenon in the use of higher-level services despite the fact that there is a greater need for these services among poorer groups.13 The Chinese government has introduced a series of interventions and policies that seek to achieve all goals by 2030. Although they have committed a large budget to national healthcare and the public healthcare sector, there is little evidence that the current healthcare system will allow for an equitable use of healthcare services among populations with different household registration characteristics. Literature has mainly focused on the demographics of the floating and native populations, but little information is provided about the inequality in healthcare utilization based on different mobility statuses.10,11 Therefore it is important to assess the degree of inequality in healthcare utilization and explore which groups are vulnerable to lower degrees of healthcare utilization in China.
Attention towards inequality in access to healthcare services has grown steadily in recent years. Most studies exploring inequality in healthcare utilization have focused on income-related inequality and the factors that contribute to this inequality.14–18 By using the income-related inequality concentration index (CI), previous studies that assessed equity in essential healthcare services have consistently identified a pro-rich distribution in healthcare utilization.18–20 These methods of measuring inequalities are based on income-related inequalities in healthcare utilization, but income is not an absolute factor in determining the probability that an individual will utilize healthcare, and there is no direct relationship between individual income and mobility. Therefore we utilized longitudinal household survey data to examine inequality in the use of healthcare services based on individual mobility status. To our knowledge, this is the first time that mobility-related inequality has been used to evaluate inequality in healthcare utilization. In addition, this method does not have a specialized analysis for the contribution to mobility-related inequality. Therefore, based on mobility-related inequality in healthcare utilization, we use decomposition to break down the factors that contribute to inequality in healthcare utilization between floating and native populations.
Determining the degree of inequality in healthcare utilization can serve as a useful tool for promoting the development of healthcare policies. The goal of the present study is to assess mobility-related inequality and to identify the factors of mobility-related inequality that contribute to inequality in healthcare utilization. First, we use the panel probit model to assess differences in healthcare utilization between the floating and native populations. This allows us to examine whether the nature and extent of inequality is different for different types of floating populations, which allows us to create a more complete picture of inequality in healthcare provision. Second, by using mobility-related inequality in our analyses of inequality, we can assess how mobility-related inequality impacts healthcare utilization between groups of people with different mobility statuses. This allows us to observe the degree of inequality in healthcare utilization and to explore which groups are more likely to use healthcare among the floating and native populations. Finally, we break down the mobility-related inequality estimates to explain the extent of inequality in healthcare utilization, finding that most of these differences can be attributed to population characteristics.
Methods
Data
The data used in the present study were taken from the China Labor-force Dynamic Survey (CLDS), which is a nationally representative longitudinal survey. The CLDS project is an ongoing prospective study involving 29 provinces in China, which was first started in 2012 and is updated every 2 y. It was designed using a multistage cluster and stratified probability proportional to size sampling strategy conducted by Sun Yat-sen University. The CLDS covers population, economy, society, psychology, health and other areas, which allows it to provide substantial scientific and objective social science data for multidisciplinary studies. In the present study, three rounds of follow-up surveys were completed in 2014, 2016 and 2018. A total of 60 811 participants with 53 452 floating samples and 7359 native samples were recruited within Chinese territory during these three rounds of survey data.
Methodology
Since Adam et al.21 used income-related inequality to measure socio-economic inequality in healthcare utilization, it has become the most commonly used method for measuring inequality in healthcare service utilization. A useful feature of the CI is measuring the factors that contribute to the inequality index in healthcare utilization.22 A concentration curve (CC) is introduced to observe the distributed bias of healthcare utilization; points that fall below the line of equality indicate that there is a higher concentration of healthcare utilization among the wealthy.23 In the present context, one important point of measuring the CI and using a decomposition approach is that results will not be linear because the dependent variable in demand models of healthcare utilization is predicted by a non-linear function based on individual characteristics. The empirical models of healthcare utilization are based on truncated and generalized negative binomial regression and/or probit models, which are essentially non-linear.18
We used the Wagstaff et al.14 approach to quantify mobility-related inequality in healthcare utilization based on income-related inequality with pool data. In these calculating systems, previous calculations use income as a continuous variable to rank individual grade. Thus we use the probit model's estimated coefficients to predict individual mobility status as a continuous variable for the respondents with a correcting method. For weighted data, the CI can be calculated using the covariance between the fractional rank of the individual sorted by mobility status and healthcare utilization as24
 |
(1) |
where COVw is the weighted covariance, n is the sample size, yi is the binary variable of whether the ith person had used a health service in the previous 2 weeks, μ is the (weighted) mean healthcare utilization and wi is the sampling weight of each individual i (with the sum of wi equal to N). Ri is the relative fractional rank (based on weights) of the ith individual, which indicates the weighted cumulative proportion of the population up to the midpoint of each individual weight.16,18 In this study, the CI is the inequality index for the use of health services, with a range from −1 to 1. Native populations are more likely to use health services when the CI is significantly <0, while a CI >0 indicates that healthcare utilization is biased towards floating populations.16,18
Decomposition of inequality
Drawing on the literature of labour economics and income inequality, Wagstaff et al.22 introduced this decomposing approach to explain income-related inequality in healthcare utilization. Subsequently, Doorslaer et al.18 expanded this approach to separate the degree to which different factors contribute to inequality in the use of health services. The CI of healthcare utilization can be separated into the contribution of individual factors and unexplained factors, in which each contribution is the product of the elasticity of the use of the healthcare variable associated with that factor and the degree of unequal distribution of that factor across the mobility status.18 Therefore the decomposition analysis is different from the traditional regression approach in that it allows explaining of inequality based on contributing factors rather than on the variation of related variables.
We conducted a decomposition analysis based on Doorslaer et al.’s18 approach to assess the extent to which various factors contribute to inequality in the use of healthcare services, using the linear approximation of a probit model, which is expressed as
 |
(2) |
where y is whether the participant uses healthcare services, the xk variables include the determinants of demand for healthcare utilization, ε is a disturbance term, αm is the intercept and βk is the marginal effects dy/dxi of each factor evaluated at sample means. One could think of this equation as a simplified form of a need for health services equation where all the xk variables are exogenous determinants. Given the relationship between yi and xki in equation (2), the CI can be written as
 |
(3) |
In equation (3), βk denotes the coefficient of independent variables,  is the elasticity of healthcare utilization with respect to independent variables and CIk is the concentration index of the independent variables with respect to mobility status. Finally, GCε is the generalized CI of the residual. In the decomposition of equation (3), the product of the elasticity of each factor multiplied by its CIk gives us the contribution of that factor to inequality and the products of
is the elasticity of healthcare utilization with respect to independent variables and CIk is the concentration index of the independent variables with respect to mobility status. Finally, GCε is the generalized CI of the residual. In the decomposition of equation (3), the product of the elasticity of each factor multiplied by its CIk gives us the contribution of that factor to inequality and the products of  are the contribution of a factor x to the actual inequality index in healthcare utilization. CIk was estimated for each of the factors, along with absolute and percentage contributions to the inequality in healthcare utilization. A positive contribution indicates that the given variable contributes towards a pro-floating population distribution of healthcare utilization, but a negative contribution indicates a pro-native population distribution of healthcare utilization.
are the contribution of a factor x to the actual inequality index in healthcare utilization. CIk was estimated for each of the factors, along with absolute and percentage contributions to the inequality in healthcare utilization. A positive contribution indicates that the given variable contributes towards a pro-floating population distribution of healthcare utilization, but a negative contribution indicates a pro-native population distribution of healthcare utilization.
Healthcare utilization
In the present study, healthcare utilization was based on whether the participants used healthcare services. Therefore we asked the subjects whether they had suffered from any illnesses in the 2 weeks prior to the survey; this item was used to determine the need for healthcare services. In addition, we asked the subjects who had experienced illnesses whether they visited a doctor; this item was used to determine the healthcare utilization of hospital visits. In addition, we used actual hospitalization as the robustness test for healthcare utilization. Among the subgroups of participants who were diagnosed as needing hospitalization, the robustness proxy for healthcare utilization was measured by whether the participant was diagnosed by a doctor for hospitalization in the year prior to the survey and whether they had received hospitalization treatment. In short, healthcare utilization was measured based on the indicators of whether participants experiencing illness during the past 2 weeks had visited a hospital and/or whether they had received hospitalization treatment. We only selected participants who needed healthcare services for the study of healthcare utilization and excluded the selection bias of the healthy immigrant effect by deleting the sample that had not suffered from any illnesses or had not been diagnosed as needing hospitalization.11,25
Mobility status
In the survey, individuals were classified as being part of the floating population if they chose the answer ‘your household registration is in another subdistrict/town/county than your current place of residence’. Mobility status was defined as a binary variable (1=yes) in the original data.
In the calculation of CI, individual mobility status must be a continuous variable to allow for the sorting of fractional rank. Therefore we used the panel probit model to apply the fixed effects of time and province to individual characteristics, allowing us to predict individual mobility status as a continuous variable for the respondent. A predicted mobility status with a continuous outcome can be used in the calculation of mobility-related inequality, which is similar to the calculation of income-related inequality.
Independent variables
The independent variables used to depict individual characteristics in this study included mobility, age, gender, marital status, income, education level, job category, household registration (hukou), self-assessed health, drinking, smoking, physical activity and health insurance. These variables were collected via in-home interviews and general information questionnaires. The sample's education level was divided into five levels (none, primary school, middle school, high school and university). Job category was divided into a binary indicator of agricultural jobs and non-agricultural jobs. Self-assessed health was ranked from 1 to 5, with 1 being the worst and 5 being the best. Given that health insurance has an important effect on the amount of healthcare subsidies that individuals receive when accepting healthcare, we define a dummy variable of 1 if the individual has health insurance. Other control variables are quantified by binary dummy variables.
Analysis
Related data were analysed using Stata 15 (StataCorp, College Station, TX, USA) to determine the inequality between the floating and native populations in healthcare utilization. First, we conducted a series of descriptive analyses regarding the rate of illness and healthcare utilization. We also depicted the differences in people's personal characteristics between floating and native populations. Comparisons of the differences in characteristics across mobility status were made by using t tests for continuous variables and χ2 tests for categorical variables. Second, we used panel probit regression models to examine the association of the probability of individual healthcare utilization with mobility status (yes=1), controlling their demographic characteristics, and including time and province fixed effects. Furthermore, on the basis of the results demonstrated above, we depicted the CC of mobility-related inequality in healthcare utilization and then calculated the CI of healthcare utilization (where mobility is a continuous variable fitted with individual characteristics) based on the method of inequality with pool data,16,18,21 thus exploring whether current healthcare utilization is pro-floating or pro-native populations. Finally, we decomposed the factors that contribute to the CI in healthcare utilization, finding the reasons that lead to inequality.
Results
From the eligible cohort, we obtained 58 602 samples in the three rounds of surveys. Floating and native populations showed significant differences in individual characteristics (Table 1). The floating population tended to be younger, male, unmarried, employed in non-agricultural work, rural residents and drinkers. In addition, the floating population reported higher levels of income, education, smoking, self-assessed health and physical activity compared with the native population. However, members of the floating group were less likely to have insurance than members of the native group, which may be the main reason for the inequality in healthcare utilization.26
Table 1.
Descriptive statistics of variables (N=58 602)
| Native population | Floating population | p-Value | |||||
|---|---|---|---|---|---|---|---|
| Variables | Mean | SD | n | Mean | SD | n | |
| Age | 45.68 | 14.55 | 53 216 | 39.21 | 13.20 | 7298 | 0.000 |
| Gender (male=1) | 0.520 | 0.500 | 53 451 | 0.547 | 0.498 | 7359 | 0.000 |
| Marriage (yes=1) | 0.816 | 0.387 | 53 452 | 0.780 | 0.415 | 7359 | 0.000 |
| Agricultural job (yes=1) | 0.332 | 0.471 | 53 452 | 0.0467 | 0.211 | 7359 | 0.000 |
| Registration (rural resident=1) | 0.207 | 0.405 | 53 344 | 0.344 | 0.475 | 7239 | 0.000 |
| Education | 2.885 | 1.173 | 53 318 | 3.465 | 1.122 | 7325 | 0.000 |
| Insurance (yes=1) | 0.887 | 0.317 | 53 215 | 0.797 | 0.403 | 7217 | 0.000 |
| Self-assessed health | 3.615 | 1.010 | 53 417 | 3.821 | 0.901 | 7333 | 0.000 |
| Smoking (yes=1) | 0.270 | 0.444 | 53 413 | 0.241 | 0.428 | 7333 | 0.000 |
| Drinking (yes=1) | 0.188 | 0.390 | 53 411 | 0.190 | 0.392 | 7332 | 0.000 |
| Physical activity (yes=1) | 0.267 | 0.443 | 53 411 | 0.352 | 0.478 | 7331 | 0.000 |
| Income (yuan) | 27 181 | 33 214 | 35 652 | 45 947 | 43 219 | 5 097 | 0.000 |
SD: standard deviation.
Table 2 compares floating and native populations in terms of the mean statistics of needed treatment for all the samples and actual health service treatment based on subgroups that needed treatment. According to Table 2, the native population reported a higher number of hospital visits and hospitalization treatments than the floating population by 5.46 and 1.83, respectively. These difference in healthcare utilization provide further analysis for the inequality in healthcare between different floating groups.
Table 2.
Comparison of the percentage of participants using healthcare among the floating and native populations
| Variables | Native population | Floating population | ||||
|---|---|---|---|---|---|---|
| Mean | SD | n | Mean | SD | n | |
| Illness in total samples (%) | 9.62 | 29.48 | 53 408 | 8.87 | 28.43 | 7331 |
| Hospital visits in illness subgroups (%) | 63.31 | 48.20 | 5140 | 57.85 | 49.42 | 650 |
| Total people who needed hospitalization (%) | 8.59 | 28.02 | 53 407 | 5.70 | 23.19 | 7331 |
| Hospitalization treatment in subgroups that needed hospitalization (%) | 83.93 | 36.73 | 4588 | 82.10 | 38.38 | 419 |
SD: standard deviation.
In Table 3 we use the panel probit model to analyse the probability of illness and healthcare utilization between different floating populations with three rounds of data, controlling their demographic characteristics and with the fixed effects of time and province. Both the estimated coefficients of hospital visits and hospitalization treatment on the variable of mobility status show a negative statistical significance. In other words, there is a lower probability of healthcare utilization in the floating population than in the native population. The floating population suffered from an inequality in treatment in both hospital visits and hospitalization treatment, which demonstrated the high degree of inequality in healthcare utilization compared with the native population. It is worth noting that job category, insurance and self-assessed health show a statistical significance on the variables of both hospital visits and hospitalization treatment. These results conform with expectations, given that people with insurance can obtain a certain ratio of reimbursement in medical institutions where they received treatment.11 In addition, an individual's gender, marital status, registration location, physical activity and whether they are a smoker has a significant impact on hospital visits, and individual age and income have a significant positive impact on the use of hospitalization treatment.
Table 3.
Comparing the probability of illness and healthcare utilization among the floating and native populations
| Variables | Hospital visits, mean (SE) | Hospitalization treatment, mean (SE) |
|---|---|---|
| Migrant (yes=1) | −0.102* (0.060) | −0.219** (0.102) |
| Age | 0.001 (0.002) | 0.007*** (0.003) |
| Gender (female=1) | 0.114** (0.050) | −0.040(0.076) |
| Marriage (yes=1) | 0.138** (0.055) | 0.133 (0.087) |
| Agricultural job (yes=1) | −0.114** (0.049) | −0.136* (0.073) |
| Registration (rural resident=1) | −0.175*** (0.059) | 0.048 (0.088) |
| Education | 0.002 (0.022) | 0.047 (0.033) |
| Insurance (yes=1) | 0.124** (0.063) | 0.229** (0.100) |
| Self-assessed health | −0.084*** (0.020) | 0.127*** (0.030) |
| Smoking (yes=1) | −0.111** (0.055) | −0.096 (0.081) |
| Drinking (yes=1) | −0.032 (0.054) | −0.087 (0.080) |
| Physical activity (yes=1) | 0.074* (0.043) | 0.007 (0.065) |
| Income (yes=1) | 0.007 (0.005) | −0.013* (0.007) |
| Control time | ✓ | ✓ |
| Control province | ✓ | ✓ |
| Constant | 0.639*** (0.233) | −0.440 (0.351) |
| Observations | 5728 | 4971 |
SE: standard error. *p<0.1, **p<0.05, ***p<0.01.
Most of individuals’ demographic characteristics have a significant impact on healthcare utilization. These variables may be the main factors that cause inequality in healthcare utilization between different floating populations. Therefore we further depict the CC and CI related to mobility status.
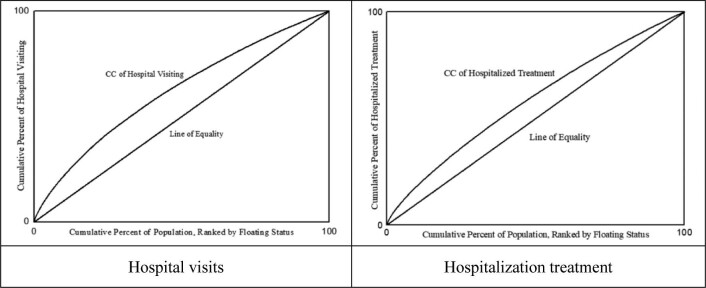
Table 4 shows the CI for healthcare utilization. The CI was negative for both hospital visits and hospitalization treatments, i.e. native populations are more likely to utilize healthcare. The results of these negative CIs in healthcare utilization are similar to the coefficients of mobility in Table 3, which further demonstrates the inequality of healthcare utilization in floating populations. In addition, Figure 1, which is the CC of two commonly used measures of healthcare utilization, shows that inequality in hospital visits is biased towards native populations, as the CC of hospital visits is above the line of equality, and a similar explanation applies to hospitalization treatment.
Table 4.
Mobility-related inequality estimates of healthcare utilization
| Item | Hospital visiting | Hospitalization treatment |
|---|---|---|
| CI | -0.137 | −0.356 |
Figure 1.
The concentration curve of healthcare utilization.
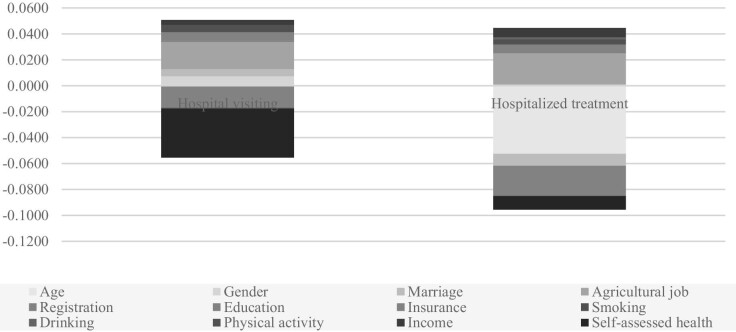
Although the CI and CC are an attractive way to exhibit inequality in healthcare utilization as it relates to mobility status, they do not quantify the factors of inequality. Therefore we further break down the gap in the inequality between the different groups into the characteristics of individuals.
Table 5 and Figure 2 reveal how personal characteristics contribute to the explained inequality in the probability of healthcare utilization. According to the results for hospital visits and hospitalization treatment, personal characteristics play a key role in explaining the gap in healthcare utilization between floating and native populations. For hospital visits, self-assessed health, job category and household registration are all important variables that contribute to inequality in healthcare utilization. Self-assessed health contributes the most to decreasing the gap in healthcare utilization inequality, because good self-assessed health shows a higher health status and a lower use of healthcare services compared with the native population. Job category contributes the most to increasing the gap in healthcare utilization inequality, because those who work in agriculture show a negative healthcare utilization and a lower proportion of mobility compared with the native population. However, household registration plays the largest role in decreasing inequality in healthcare utilization, because rural registration shows a negative healthcare utilization rate and a higher proportion of mobility compared with the native population. The sum total contribution of individual characteristics is 0.0047 in decreasing the inequality of hospital visits. In addition, gender, marital status, education, insurance, physical activity and income increase the gap of inequality in hospital visits, while age, smoking and drinking show an opposite effect on the inequality in hospital visits. For hospitalization treatment, job category contributes the most to increasing inequality, but age and insurance contribute the most to decreasing inequality. The sum total contribution of individual characteristics is 0.051 in decreasing the inequality of hospitalized utilization. However, unexplained factors associated with mobility status play an important role in explaining inequality in the probability of hospital visits and hospitalization treatment. In short, inequality in healthcare utilization among different mobility states is not only due to the direct effects of factors that influence health, including age, job category, household registration and insurance, but also because of the indirect effects of these factors caused by mobility status. All these results indicate that mobility plays a significant role in healthcare utilization.
Table 5.
Decomposing individual characteristics of mobility status in the inequality of healthcare utilization
| Hospital visiting | Hospitalization treatment | |||||
|---|---|---|---|---|---|---|
| Variables | CIk | Elasticity | Contributions to overall CI | CIk | Elasticity | Contributions to overall CI |
| Age | −0.0034 | 0.0766 | −0.0003 | −0.1151 | 0.4565 | −0.0525 |
| Gender | 0.0706 | 0.1040 | 0.0073 | −0.0323 | −0.0297 | 0.0010 |
| Marriage | 0.0302 | 0.1817 | 0.0055 | −0.0684 | 0.1341 | −0.0092 |
| Agricultural job | −0.3500 | −0.0600 | 0.0210 | −0.4331 | −0.0556 | 0.0241 |
| Registration | 0.3490 | −0.0477 | −0.0166 | 0.3466 | 0.0073 | 0.0025 |
| Education | 0.1467 | 0.0053 | 0.0008 | 0.0301 | 0.1385 | 0.0042 |
| Insurance | 0.0356 | 0.1880 | 0.0067 | −0.0872 | 0.2663 | −0.0232 |
| Smoking | 0.0012 | −0.0455 | −0.0001 | −0.1270 | −0.0309 | 0.0039 |
| Drinking | 0.0581 | −0.0094 | −0.0005 | −0.0730 | −0.0188 | 0.0014 |
| Physical activity | 0.1750 | 0.0332 | 0.0058 | 0.1226 | 0.0017 | 0.0002 |
| Income | 0.0658 | 0.0556 | 0.0037 | −0.0825 | −0.0896 | 0.0074 |
| Self-assessed health | 0.1008 | −0.3771 | −0.0380 | −0.0262 | 0.4077 | −0.0107 |
| Total | – | – | −0.0047 | – | – | −0.0510 |
Figure 2.
Contribution of factors of mobility difference in the inequality of healthcare utilization.
Discussion
Literature about the utilization of healthcare services frequently indicates that the floating population faces barriers in accessing healthcare services,4,10,11,20,26 but it does not identify the degree of inequality that is directly related to mobility. The present study uses the methods of the panel probit model and mobility-related inequality index to show that the floating population faces inequality when it comes to hospital visits and hospitalization treatment. The CI in healthcare utilization based on the method of mobility-related inequality shows a significant bias towards the native population, which is seen in the results of individual healthcare utilization, as compared with previous pro-rich distributions based on the method of income-related inequality.27,28 In the present work, we sought to further assess the extent to which mobility-related inequality can be attributed to individual characteristics by decomposing the factors that contribute to inequality in healthcare utilization. There are few studies that utilize an inequality index between China's floating and native populations to examine inequalities in healthcare utilization.10,11 Based on this special perspective, the present study offers an accurate measure of the utilization of healthcare services among different floating groups and accurately quantifies the degree of inequality in healthcare utilization.
Our results found that the native population reports a 10.2% higher probability of hospital visits and a 21.9% higher probability of hospitalization treatment compared with the floating population, adjusting for individual characteristics, and with the fixed effects of time and province, thus there is inequality in the utilization of healthcare services. These phenomena can be explained by the individual characteristics between the floating and native populations. Floating groups report a lower age, prevalence of insurance and smoking and higher education levels and percentages of rural residents, as the significant results in hospital visits show in Table 3. Generally, the healthier the people were and the less they smoked, the less likely they were to use healthcare services. In China, people without insurance have relatively lower incentive to seek hospitalization treatment even if they have been diagnosed with illness, because they cannot receive medical reimbursements without insurance.29 Furthermore, the healthier the people are, the more likely they are to have higher incomes and better knowledge and awareness of health. A previous study also demonstrated that high levels of education can regulate the use of health services by improving health status.30 In our study, we found that the floating population contained a higher percentage of rural inhabitants than the native population. Government policies provide a higher rate of insurance coverage for urban populations (88.75%) compared with rural populations (83.60%). In addition, China's society has traditionally been divided between less-educated and poorer rural residents and well-educated and richer urban residents, which can explain the lower rate of healthcare utilization among rural populations.31 In the past few decades, China has made great progress in achieving equality of insurance coverage and health services across and within registration systems.29
Most previous studies into inequality in healthcare utilization between floating and native populations have focused on urban–rural comparisons11,32 and/or income-related inequality with a CI.4,26 These studies have found that the floating population reports high barriers to healthcare utilization because of household registration, job category, insurance and lifestyle.4,11 For the floating population, previous studies that used the method of income-related inequality showed a pro-rich bias in the utilization of healthcare services but did not directly measure mobility-related inequality. Jiménez-Rubio and Hernández-Quevedo26 attempted to use the Oaxaca–Blinder decomposition method to explore inequality in the use of healthcare services between native and immigrant populations in Spain and found that some factors associated with immigrant status determine, to a significant extent, disparities in the use of healthcare services. In the present study, based on the method of mobility-related inequality, our results show a pro-native population bias with a negative CI in the utilization of healthcare services, which directly indicates a pro-native rather than a pro-rich phenomenon. Further decomposition of the contributing factors corroborates the existence of barriers to healthcare utilization based on mobility status. For hospital visits, differences in individual characteristics explain, to a great extent, the inequality for floating populations compared with native populations. These individual characteristics of the floating population mainly reported the factors of being young, male, unmarried, in non-agricultural work, high education and income, better physical activity and low insurance coverage as factors that contributed to the gap in increasing inequality in hospital visits, while rural registration, high self-assessed health and a higher prevalence of smokers and drinkers contributed to decreasing inequality in the utilization of hospital visits. In short, individual characteristics can fully explain the contributing factors in the gap of healthcare utilization by 0.0047 in hospital visits and by 0.051 in hospitalization treatment. The size of these contributory coefficients is relatively small compared with that of unexplained factors, which is quite similar to Jiménez-Rubio and Hernández-Quevedo26 and Saito et al.’s33 results. There are some unexplained factors associated with mobility status that play an important role in interpreting inequality in hospital visits and hospitalization treatment.26
In the present study, age, self-assessed health, job category, registration system and insurance play the most important roles in inequality in healthcare utilization. Mobility is significantly determined by individual characteristics, so the inequality in healthcare utilization that mobility directly contributes is also closely related to individual characteristics. In China, rural populations are some of the most vulnerable groups due to lower income and education levels. Because of the restrictions of China's household registration system, they are often engaged in agriculture and/or manual labour and face large obstacles in accessing local insurance. These factors lead to unequal treatment in healthcare utilization. In addition, the Chinese government provides reimbursement for using healthcare services at designated local facilities.34 Some studies have reported a lower use of healthcare services35 or poor quality of healthcare services relating to health behaviour among China's floating population.36,37 It is typically reported that the high cost of health services, lack of insurance and health awareness, financial difficulties and problems in navigating local healthcare systems are the main barriers to health services among China's floating population.36,38 In addition, more severe inequality in the floating population might be associated with a poorer socio-economic status and living conditions.39
To ensure healthcare for all people, in recent decades China has focused on the provision of convenient and affordable healthcare services across rural and urban areas and established a health insurance system that provides essential health insurance. In 2009, China introduced the policy of off-site medical billing, which aims to help provide the floating population with access to equal medical services in inflow regions.40 In addition, with the progress of urbanization and reform of the household registration system, an increasing number of rural-to-urban migrants could become urban residents, which helps floating populations to receive equal medical services. Therefore, some interventions should promote deep integration between the floating and native populations. It is necessary to improve the satisfaction with healthcare services and job demands of floating populations and improve the equalization system of healthcare services and the accessibility of medical resources for China's floating populations, especially for patients living in rural districts, so as to reduce the gap of inequality in healthcare utilization between the floating and native populations.
The present research has several strengths compared with other studies. First, the methods and data are novel and comprehensive, utilizing three rounds of longitudinal survey data, which provides a high degree of analytical reliability. Second, using the sample of confirmed patients for the study can more accurately identify the probability of healthcare utilization. In the present samples, most of the participants were healthy individuals who did not need hospital visits and/or hospitalization treatment; only participants who suffered from illnesses and/or who were diagnosed by a doctor for hospitalization were used to measure the probability of healthcare utilization. Third, our study measures mobility-related inequality in healthcare utilization compared with previous studies of income-related inequality and discovered a pro-native population bias. Both our estimated coefficient and mobility-related CI show that the floating population faces a low probability and inequality in healthcare utilization. Finally, we used the method of mobility-related inequality to describe the extent of inequality in healthcare utilization and decomposed the contributing factors to the inequality. The decomposing approach shows that age, self-assessed health, job category, registered system and insurance play the most important roles in the contribution to inequality in healthcare utilization. Our main research area in the present study was regarding how to measure the probability of the utilization of healthcare services and explore its influencing factors to reduce inequality in healthcare utilization among the floating population.
There are several limitations to this study. First, since the paper used the CLDS, information on the proxy variable of using healthcare services only considers hospital visits and hospitalization treatment. Other indicators of using healthcare services such as general practitioner visits, specialist visits and emergency room visits were not considered in the present study; this is not enough information when considering the measurement of healthcare utilization. Second, the present study only addressed healthcare utilization after migration, leaving out many important factors that affect what patterns of access to health services existed in the original regions of floating populations. There could be reverse causality between healthcare utilization and migration decision making.
Conclusions
The floating population faced a low probability of and inequality in healthcare utilization when they had diseases and there is a pro-native population phenomenon when it comes to hospital visits and hospitalization treatment. According to the primary barriers of healthcare utilization in the floating population, a variety of individual characteristics, household registration and insurance integrating the strengths of society and government should be implemented to improve healthcare utilization in the future.
Acknowledgements
Thanks to the Center for Large-scale Data Systems Research for providing CLDS data. Thanks to all the subjects involved in the experiment, who agreed to use of the data and the publishing of relevant data and reports.
Contributor Information
Daisheng Tang, School of Economics and Management, Beijing Jiaotong University, Haidian, Beijing, China.
Tao Bu, School of Economics and Management, Beijing Jiaotong University, Haidian, Beijing, China.
Yahong Liu, School of Economics and Management, Beijing Jiaotong University, Haidian, Beijing, China.
Authors’ contributions
All authors contributed to this work. DT and TB worked on the study design and method. TB was responsible for manuscript design, data analysis and writing the manuscript. DT supervised the analysis. YL provided interpretive input and language correction. All authors critically reviewed and approved the final manuscript.
Funding
This work was supported by a grant-in-aid for the Fundamental Research Funds for the Central Universities (2020YJS060).
Competing interests
None declared.
Ethical approval
This study was reviewed and approved by the institutional review board of Beijing Jiaotong University of School of Economics and Management.
Data availability
The datasets used and/or analysed during the current study are available from the corresponding author upon request.
References
- 1. Gostin LO. WHO global action plan to promote the health of refugees and migrants. Milbank Q. 2019;97(3):631–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Pant S, Eder B, Vračar A. WHO's global action plan to promote the health of refugees and migrants. BMJ. 2019:366:I4806. [DOI] [PubMed] [Google Scholar]
- 3. Gushulak BD, Macpherson DW. The basic principles of migration health: population mobility and gaps in disease prevalence. Emerg Themes Epidemiol. 2006;3:3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Graetz V, Rechel B, Groot Wet al. . Utilization of health care services by migrants in Europe—a systematic literature review. Br Med Bull. 2017;121(1):5–18. [DOI] [PubMed] [Google Scholar]
- 5. National Bureau of Statistics of China . Migrants population dynamic monitoring survey data in 2018. Beijing: National Bureau of Statistics of China; 2018. [Google Scholar]
- 6. Hu X, Cook S, Salazar MA. Internal migration and health in China. Lancet. 2008;372(9651):1717–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Mou J, Griffiths SM, Fong Het al. . Health of China's rural–urban migrants and their families: a review of literature from 2000 to 2012. Br Med Bull. 2013;106(1):19–43. [DOI] [PubMed] [Google Scholar]
- 8. Démurger S, Li S, Yang J. Earnings differentials between the public and private sectors in China: exploring changes for urban local residents in the 2000s. China Econ Rev. 2012;23(1):138–53. [Google Scholar]
- 9. Jan C, Zhou X, Stafford RS. Improving the health and well-being of children of migrant workers. Bull World Health Org. 2017;95(12):850–2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Zhang J, Lin S, Liang Det al. . Public health services utilization and its determinants among internal migrants in China: evidence from a nationally representative survey. Int J Environ Res Public Health. 2017;14(9):1002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Ma S, Zhou X, Jiang Met al. . Comparison of access to health services among urban-to-urban and rural-to-urban older migrants, and urban and rural older permanent residents in Zhejiang Province, China: a cross-sectional survey. BMC Geriatr. 2018;18(1):174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Carrin G, Xu K, Evans DB. Exploring the features of universal coverage. Bull World Health Org. 2008;86(11):818. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Rodney AM, Hill PS. Achieving equity within universal health coverage: a narrative review of progress and resources for measuring success. Int J Equity Health. 2014;13:72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Wagstaff A, van Doorslaer E, Paci P. On the measurement of horizontal inequality in the delivery of health care. J Health Econ. 1991;10(2):169–205. [DOI] [PubMed] [Google Scholar]
- 15. van Doorslaer E, Wagstaff A, Bleichrodt Het al. . Income-related inequalities in health: some international comparisons. J Health Econ. 1997;16(1):93–112. [DOI] [PubMed] [Google Scholar]
- 16. Kakwani N, Wagstaff A, van Doorslaer E. Socioeconomic inequalities in health: measurement, computation, and statistical inference. J Econometrics. 1997;77(1):87–103. [Google Scholar]
- 17. Gerdtham UG. Equity in health care utilization: further tests based on hurdle models and Swedish micro data. Health Econ. 1997;6(3):303–19. [DOI] [PubMed] [Google Scholar]
- 18. van Doorslaer E, Koolman X, Jones AM. Explaining income-related inequalities in doctor utilisation in Europe. Health Econ. 2004;13(7):629–47. [DOI] [PubMed] [Google Scholar]
- 19. Bago d'Uva T, Jones AM, van Doorslaer E. Measurement of horizontal inequality in health care utilisation using European panel data. J Health Econ. 2009;28(2):280–9. [DOI] [PubMed] [Google Scholar]
- 20. Vallejo-Torres L, Morris S. Income-related inequality in healthcare utilisation among individuals with cardiovascular disease in England—accounting for vertical inequality. Health Econ. 2013;22(5):533–53. [DOI] [PubMed] [Google Scholar]
- 21. Wagstaff A, van Doorslaer E, Paci P. Equity in the finance and delivery of health care: some tentative cross-country comparisons. Oxford Rev Econ Policy. 1989;5(1):89–112. [Google Scholar]
- 22. Wagstaff A, van Doorslaer E, Watanabe N. On decomposing the causes of health sector inequalities with an application to malnutrition inequalities in Vietnam. J Econometrics. 2003;112(1):207–23. [Google Scholar]
- 23. O'Donnell O, van Doorslaer E, Wagstaff Aet al. . Analyzing health equity using household survey data: a guide to techniques and their implementation. Washington, DC: World Bank; 2008. [Google Scholar]
- 24. Lerman RI, Yitzhaki S. Improving the accuracy of estimates of Gini coefficients. J Econometrics. 1989;42(1):43–7. [Google Scholar]
- 25. Noymer A, Lee R. Immigrant health around the world: evidence from the World Values Survey. J Immigr Minor Health. 2013;15(3):614–23. [DOI] [PubMed] [Google Scholar]
- 26. Jiménez-Rubio D, Hernández-Quevedo C. Inequalities in the use of health services between immigrants and the native population in Spain: what is driving the differences? Eur J Health Econ. 2011;12(1):17–28. [DOI] [PubMed] [Google Scholar]
- 27. Leung GM, Tin KYK, O'Donnell O. Redistribution or horizontal equity in Hong Kong's mixed public-private health system: a policy conundrum. Health Econ. 2009;18(1):37–54. [DOI] [PubMed] [Google Scholar]
- 28. Elwell-Sutton TM, Jiang CQ, Zhang WSet al. . Inequality and inequality in access to health care and treatment for chronic conditions in China: the Guangzhou Biobank Cohort Study. Health Policy Plan. 2013;28(5):467–79. [DOI] [PubMed] [Google Scholar]
- 29. Meng Q, Xu L, Zhang Yet al. . Trends in access to health services and financial protection in China between 2003 and 2011: a cross-sectional study. Lancet. 2012;379(9818):805–14. [DOI] [PubMed] [Google Scholar]
- 30. Zajacova A, Lawrence EM. The relationship between education and health: reducing disparities through a contextual approach. Annu Rev Public Health. 2018;39:273–89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Liang Z, Ma Z. China's floating population: new evidence from the 2000 census. Popul Dev Rev. 2004;30(3):467–88. [Google Scholar]
- 32. Solé-Auró A, Guillén M, Crimmins EM. Health care usage among immigrants and native-born elderly populations in eleven European countries: results from SHARE. Eur J Health Econ. 2012;13(6):741–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Saito E, Gilmour S, Yoneoka Det al. . Inequality and inequality in healthcare utilization in urban Nepal: a cross-sectional observational study. Health Policy Plan. 2016;31(7):817–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Jakovljevic M, Timofeyev Y, Ekkert NVet al. . The impact of health expenditures on public health in BRICS nations. J Sport Health Sci. 2019;8(6):516–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Shaokang Z, Zhenwei S, Blas E. Economic transition and maternal health care for internal migrants in Shanghai, China. Health Policy Plan. 2002;17(Suppl):47–55. [DOI] [PubMed] [Google Scholar]
- 36. Cowan AJ, Allen C, Barac Aet al. . Global burden of multiple myeloma: a systematic analysis for the Global Burden of Disease Study 2016. JAMA Oncol. 2018;4(9):1221–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Jakovljevic MB, Milovanovic O. Growing burden of non-communicable diseases in the emerging health markets: the case of BRICS. Front Public Health. 2015;3:65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Cheng L, Liu H, Zhang Yet al. . The impact of health insurance on health outcomes and spending of the elderly: evidence from China's New Cooperative Medical Scheme. Health Econ. 2015;24(6):672–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Jakovljevic MM. Comparison of historical medical spending patterns among the BRICS and G7. J Med Econ. 2016;19(1):70–6. [DOI] [PubMed] [Google Scholar]
- 40. Zhu K, Zhang L, Yuan Set al. . Health financing and integration of urban and rural residents’ basic medical insurance systems in China. Int J Equity Health. 2017;16(1):194. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets used and/or analysed during the current study are available from the corresponding author upon request.