Abstract
Anosmia and parosmia refer to the loss or dysfunction of smell, respectively. Dysgeusia refers to taste disturbance. The coronavirus disease 2019 (COVID-19) pandemic and the subsequent phenomenon of Long COVID syndrome have been associated with an increased incidence of anosmia and dysgeusia. Smell and taste disturbances associated with COVID-19 are usually self-limiting but can persist for longer periods in some cases. Imbalances of the autonomic nervous system, especially dysregulation of the sympathetic system, are implicated in the persistence of anosmia and dysgeusia post-COVID-19 infection. Stellate ganglion block (SGB) can diminish the increased sympathetic activity and potentially resolve anosmia and dysgeusia occurring due to Long COVID. The authors report the successful resolution of persistent anosmia and dysgeusia due to Long COVID in a female patient after she underwent SGB.
Keywords: dysautonomia, dysgeusia, anosmia, long-covid, covid-19
Introduction
Anosmia and parosmia are defined as the loss or dysfunction of smell, respectively. Dysgeusia refers to taste disturbance. There is an increased prevalence of anomia/parosmia in patients who have clinically recovered from coronavirus disease 2019 (COVID-19) infection. According to the current literature, the incidence rate of olfactory dysfunction in COVID-19 patients varies from 33.9 to 68%, with a female predominance [1]. Anosmia and dysgeusia could be self-limiting over a two- or three-week period post-COVID-19 infection but can persist for longer. Despite a high recovery rate, multiple studies have reported that up to 7% of the patients still experience smell and taste disturbances more than 12 months after the onset [2,3]. Anosmia and dysgeusia might coexist with other symptoms such as fatigue, orthostatic hypotension, shortness of breath, insomnia, anxiety, and depression. These constellations of symptoms may persist chronically and are termed "Long COVID", or formally, post-acute sequelae of SARS-CoV-2 (PASC) infection [3]. The incidence of PASC is 30% in symptomatic and 5% in asymptomatic patients with COVID-19 infection [4]. Compared to influenza, COVID-19 is reported to be associated with a higher prevalence of anosmia (53% vs. 17%) [5]. PASC patients with or without hospitalization have often reported anosmia and dysgeusia as one of the predominant and persisting symptoms [4].
Smell and taste disturbances associated with COVID-19 infection have generated a lot of interesting etiological hypotheses. One such theory implicates autonomic dysregulation or dysautonomia as the underlying mechanism behind anosmia [6]. In the case of Long COVID, dysautonomia could be induced by the autonomic nervous system's (ANS) response or maladaptation to pro-inflammatory cytokines leading to excessive sympathetic nervous system activity [4,6,7]. Sympathetic innervation of the head and neck consists of the cervical and upper thoracic sympathetic chain [8]. It is postulated that unrestrained cervical sympathetic activity in the head and neck region can be blocked by injecting local anesthetics in the stellate ganglion, restoring the homeostasis of the regional ANS [9]. The stellate ganglion block (SGB) has been used clinically for medical conditions associated with increased sympathetic nervous system activity [10-12]. In this report, the authors discuss the resolution of persistent anosmia after performing SGB in a patient who had completely recovered from COVID-19 infection, implicating dysautonomia in the pathophysiology of PASC.
This article was previously posted to the QEIOS preprint server on June 11, 2022.
Case presentation
A 48-year-old female patient, who consented to the publishing of this case report, presented to our clinic four months after recovering from a COVID-19 infection. The patient did not have any significant comorbidities. She reported that she had developed fevers ranging from 99 to 102 °F, non-productive cough, and nasal congestion. The reverse transcriptase polymerase chain reaction test (RT-PCR) performed on the patient’s nasal swab, at a drive-through laboratory, had revealed a positive COVID-19 infection.
The patient was placed on antiviral therapy (a combination of nirmatrelvir and ritonavir tablets known as Paxlovid) for five days, followed by a complete resolution of symptoms. She reported that she had first noticed the loss of smell and taste three to four days into the acute phase of COVID-19 and attributed it to nasal congestion and high fevers. The patient also reported fatigue, light-headedness, and loss of smell and taste. She reported that all her symptoms had resolved within one month, except for issues with taste and smell. She reported a complete loss of sense of smell and altered taste sensation to various types of foods. The patient further reported that she had tried various nasal decongestants and mucolytic agents. She frequently did nasal irrigation with saline. The patient had also failed olfactory threshold tests. No conductive loss of sense of smell was identified, such as nasal obstruction due to rhinosinusitis or allergic rhinitis. The patient also underwent gustatory tests with taste strips and was able to identify only salty and bitter tastes. At six months post-COVID-19 infection, she continued to have anosmia and difficulty tasting sweet and sour foods.
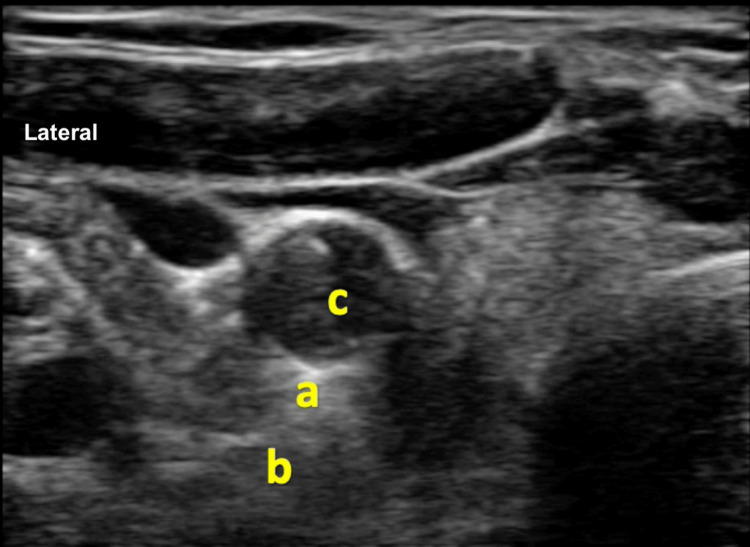
Anosmia and dysgeusia were affecting her quality of life, and she was getting annoyed due to a lack of therapeutic options. She had been finally referred to our clinic by her otolaryngologist for undergoing SGB. The patient was counseled that the authors would perform SGB based on anecdotal examples in the current literature. The patient underwent a right-sided SGB under ultrasonographic guidance, with 4 ml of 0.25% bupivacaine (Figure 1).
Figure 1. Ultrasonographic image of the right side of the neck depicting stellate ganglion.
a: stellate ganglion above the longus colli muscle. Site for deposition of local anesthetic solution. b: longus colli muscle. c: right carotid artery
The patient reported a partial return of her sense of smell within 24 hours. She then underwent the left-sided SGB after 72 hours and reported a complete resolution of anosmia 24 hours after the second SGB. She reported that her altered taste sensation resolved a few days after the last block.
Discussion
Anosmia/parosmia as a part of COVID-19 infection could be due to neurological virulence and associated cytopathic effects [13,14]. Regarding patients reporting resolution of anosmia post-SGB, an argument could be made that they might have undergone structural recovery and only need to reset the tone of the ANS to experience functional recovery. Furthermore, a dramatic resolution of anosmia after SGB favors dysautonomia rather than cytopathic or structural damage due to COVID-19 as the underlying etiology.
Dysautonomia is also reported with other viral illnesses (hepatitis C, HIV, Epstein-Barr virus) and other pathologies such as alcoholism, diabetes, and Parkinson's. Dysautonomia is associated with fatigue, anosmia, heart rate variability, bowel and bladder dysfunction, and orthostatic hypotension [6]. Multiple theories have been proposed to explain the persistence of dysautonomia post-COVID-19 infection [15]. Current literature implicates the complex interaction between the angiotensin-converting enzyme 2 (ACE2) receptor and COVID-19 as the underlying mechanism behind dysautonomia and subsequent anosmia. ACE2 enzyme converts angiotensin II (Ang II) to angiotensin (1-7) [16]. Ang inhibits inflammation [17]. ACE2, expressed in membrane-bound and soluble forms, is the receptor for the spike portion of the SARS-CoV-2 virus. A link between ACE2 and the spike portion of SARS-CoV-2 facilitates the viral entry into the cells while inhibiting the activity of the ACE2 enzyme. A subsequent decrease in the activity of ACE2 potentiates inflammation by perpetuating the feed-forward loop mediated by the ATII molecule [18]. Furthermore, auto-antibodies, such as anti-interferon, anti-nuclear, and anti-phospholipids, are ubiquitously detected in patients with PASC. Antibodies to ACE2 enzyme can also perpetuate inflammation and dysautonomia by reducing the activity of both membrane-bound and soluble ACE2 [19-21]. ACE2-viral interaction theory also explains an increased incidence of anosmia in patients of European descent with an increased expression of ACE2 compared to Asians [22]. The expression of ACE2 also increases with age, explaining the less severe prognosis of COVID-19 infection in young adults and children [23]. The female gender, with overexpression of ACE2 as compared to males, has an increased propensity for olfactory issues due to COVID-19 infection [24].
Irrespective of etiology, sequelae of COVID-19 neurotropism and tissue injury entail chronic sympathetic hyperresponsiveness, vasomotor dysfunction, persistent chronic inflammation, and aberrant neuroplasticity manifesting clinically as dysautonomia. Impaired cerebral blood flow (CBF) is a common observation reported in subjects with dysautonomia [6,7,25]. Various reports have established that CBF impairment parallels dysautonomia's clinical severity in patients with PASC [26]. SGB improves CBF under normotensive conditions [27]. The increase in CBF leading to improved perfusion of cortical areas associated with the sense of smell or the peripheral receptors in the facial region might be responsible for the immediate resolution of anosmia seen with SGB. However, the exact mechanism behind the dramatic resolution of anosmia post-SGB is still unknown.
Conclusions
The mechanistic factors related to the dramatic improvement of anosmia due to SGB are still debatable; however, SGB may be an effective treatment option for patients with olfactory and taste issues associated with PASC. At this point, the evidence for using SGB to alleviate anosmia and dysgeusia associated with Long COVID is anecdotal and limited to a few case reports. Collaborative multi-institutional research might be required to gather more evidence to support using SGB as a treatment modality for anosmia and dysgeusia due to Long COVID.
The content published in Cureus is the result of clinical experience and/or research by independent individuals or organizations. Cureus is not responsible for the scientific accuracy or reliability of data or conclusions published herein. All content published within Cureus is intended only for educational, research and reference purposes. Additionally, articles published within Cureus should not be deemed a suitable substitute for the advice of a qualified health care professional. Do not disregard or avoid professional medical advice due to content published within Cureus.
The authors have declared that no competing interests exist.
Human Ethics
Consent was obtained or waived by all participants in this study
References
- 1.COVID-19 and anosmia: a review based on up-to-date knowledge. Meng X, Deng Y, Dai Z, Meng Z. Am J Otolaryngol. 2020;41:102581. doi: 10.1016/j.amjoto.2020.102581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.COVID-19 related olfactory dysfunction. Karamali K, Elliott M, Hopkins C. Curr Opin Otolaryngol Head Neck Surg. 2022;30:19–25. doi: 10.1097/MOO.0000000000000783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.The temporal course of COVID-19 anosmia and relation to other clinical symptoms. Altundag A, Saatci O, Sanli DE, et al. Eur Arch Otorhinolaryngol. 2021;278:1891–1897. doi: 10.1007/s00405-020-06496-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Dysautonomia and implications for anosmia in long COVID-19 disease. Vallée A. J Clin Med. 2021;10:1–5. doi: 10.3390/jcm10235514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Clinical features of COVID-19 and influenza: a comparative study on Nord Franche-Comte cluster. Zayet S, Kadiane-Oussou NJ, Lepiller Q, et al. Microbes Infect. 2020;22:481–488. doi: 10.1016/j.micinf.2020.05.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Dysautonomia: an overlooked neurological manifestation in a critically ill COVID-19 patient. Eshak N, Abdelnabi M, Ball S, Elgwairi E, Creed K, Test V, Nugent K. Am J Med Sci. 2020;360:427–429. doi: 10.1016/j.amjms.2020.07.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.COVID-19 is getting on our nerves: sympathetic neural activity and haemodynamics in young adults recovering from SARS-CoV-2. Stute NL, Stickford JL, Province VM, Augenreich MA, Ratchford SM, Stickford AS. J Physiol. 2021;599:4269–4285. doi: 10.1113/JP281888. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Morphological spectra of adult human stellate ganglia: implications for thoracic sympathetic denervation. Kwon OJ, Pendekanti S, Fox JN, et al. Anat Rec (Hoboken) 2018;301:1244–1250. doi: 10.1002/ar.23797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Stellate ganglion block reduces symptoms of Long COVID: a case series. Liu LD, Duricka DL. J Neuroimmunol. 2022;362:577784. doi: 10.1016/j.jneuroim.2021.577784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Stellate ganglion block used to treat symptoms associated with combat-related post-traumatic stress disorder: a case series of 166 patients. Mulvaney SW, Lynch JH, Hickey MJ, Rahman-Rawlins T, Schroeder M, Kane S, Lipov E. Mil Med. 2014;179:1133–1140. doi: 10.7205/MILMED-D-14-00151. [DOI] [PubMed] [Google Scholar]
- 11.Effective use of percutaneous stellate ganglion blockade in patients with electrical storm. Tian Y, Wittwer ED, Kapa S, et al. Circ Arrhythm Electrophysiol. 2019;12:0. doi: 10.1161/CIRCEP.118.007118. [DOI] [PubMed] [Google Scholar]
- 12.Comparison of the effects of stellate ganglion block and paroxetine on hot flashes and sleep disturbance in breast cancer survivors. Rahimzadeh P, Imani F, Nafissi N, Ebrahimi B, Faiz SH. Cancer Manag Res. 2018;10:4831–4837. doi: 10.2147/CMAR.S173511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Olfactory epithelium histopathological findings in long-term coronavirus disease 2019 related anosmia. Vaira LA, Hopkins C, Sandison A, et al. J Laryngol Otol. 2020;134:1123–1127. doi: 10.1017/S0022215120002455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Non-neuronal expression of SARS-CoV-2 entry genes in the olfactory system suggests mechanisms underlying COVID-19-associated anosmia. Brann DH, Tsukahara T, Weinreb C, et al. Sci Adv. 2020;6:1–5. doi: 10.1126/sciadv.abc5801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Clinical characterization of dysautonomia in long COVID-19 patients. Barizien N, Le Guen M, Russel S, Touche P, Huang F, Vallée A. Sci Rep. 2021;11:14042. doi: 10.1038/s41598-021-93546-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.The cellular basis of loss of smell in 2019-nCoV-infected individuals. Gupta K, Mohanty SK, Mittal A, et al. Brief Bioinform. 2021;22:873–881. doi: 10.1093/bib/bbaa168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Proinflammatory actions of angiotensins. Ruiz-Ortega M, Lorenzo O, Suzuki Y, Rupérez M, Egido J. Curr Opin Nephrol Hypertens. 2001;10:321–329. doi: 10.1097/00041552-200105000-00005. [DOI] [PubMed] [Google Scholar]
- 18.Impact of I/D polymorphism of angiotensin-converting enzyme 1 (ACE1) gene on the severity of COVID-19 patients. Verma S, Abbas M, Verma S, et al. Infect Genet Evol. 2021;91:104801. doi: 10.1016/j.meegid.2021.104801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.High levels of anti-SSA/Ro antibodies in COVID-19 patients with severe respiratory failure: a case-based review: high levels of anti-SSA/Ro antibodies in COVID-19. Fujii H, Tsuji T, Yuba T, et al. Clin Rheumatol. 2020;39:3171–3175. doi: 10.1007/s10067-020-05359-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Profile of natural anticoagulant, coagulant factor and anti-phospholipid antibody in critically ill COVID-19 patients. Zhang Y, Cao W, Jiang W, et al. J Thromb Thrombolysis. 2020;50:580–586. doi: 10.1007/s11239-020-02182-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Diverse functional autoantibodies in patients with COVID-19. Wang EY, Mao T, Klein J, et al. Nature. 2021;595:283–288. doi: 10.1038/s41586-021-03631-y. [DOI] [PubMed] [Google Scholar]
- 22.COVID-19: possible reasons for the increased prevalence of olfactory and gustatory dysfunction observed in European studies. Gourtsoyannis Y. Clin Infect Dis. 2020;71:0. [Google Scholar]
- 23.Age-dependent sensory impairment in COVID-19 infection and its correlation with ACE2 expression. Somekh I, Yakub Hanna H, Heller E, Bibi H, Somekh E. Pediatr Infect Dis J. 2020;39:0–2. doi: 10.1097/INF.0000000000002817. [DOI] [PubMed] [Google Scholar]
- 24.Olfactory and gustatory dysfunctions as a clinical presentation of mild-to-moderate forms of the coronavirus disease (COVID-19): a multicenter European study. Lechien JR, Chiesa-Estomba CM, De Siati DR, et al. Eur Arch Otorhinolaryngol. 2020;277:2251–2261. doi: 10.1007/s00405-020-05965-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Autonomic dysfunction in 'long COVID': rationale, physiology and management strategies. Dani M, Dirksen A, Taraborrelli P, Torocastro M, Panagopoulos D, Sutton R, Lim PB. Clin Med (Lond) 2021;21:0–7. doi: 10.7861/clinmed.2020-0896. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Cerebral blood flow remains reduced after tilt testing in myalgic encephalomyelitis/chronic fatigue syndrome patients. van Campen CL, Rowe PC, Visser FC. Clin Neurophysiol Pract. 2021;6:245–255. doi: 10.1016/j.cnp.2021.09.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Sympathetic regulation of cerebral blood flow in humans: a review. ter Laan M, van Dijk JM, Elting JW, Staal MJ, Absalom AR. Br J Anaesth. 2013;111:361–367. doi: 10.1093/bja/aet122. [DOI] [PubMed] [Google Scholar]