Abstract
Objective
To summarize the characteristics of patients calling the 120 emergency number for pre-hospital first aid in Keyouqian Banner, Hinggan League.
Methods
The clinical data of adult patients with pre-hospital first aid from 2016 to 2018 were retrospectively analyzed.
Results
There were 2711 cases with pre-hospital first aid. Males significantly outnumbered females. Young and middle-aged patients comprised 81.5%. Patients were mainly Han and Mongolians. Most injuries and illnesses occurred at home and on the road. The time to arrival of medical services was 30.34 ± 28.29 minutes. The proportion of pre-hospital first aid for trauma was the highest, followed by diseases concerning the cardiovascular and neurological systems. The proportion of patients with improved medical conditions after onsite first aid was 43.3%, the proportion with unchanged conditions was 51.7%, and the total mortality rate was 3.9%.
Conclusion
The disease spectrum, ethnic distribution, age at onset, and pre-hospital first aid capabilities for outpatients were analyzed. These results may facilitate the establishment of a pre-hospital first aid system for the local prevention and control of acute and critical illnesses, increase the success rate of the region’s pre-hospital first aid services, and improve the prognosis.
Keywords: Keyouqian Banner, Inner Mongolia, pre-hospital first aid, emergency medical service, epidemiological analysis
Introduction
Pre-hospital first aid refers to the medical process of providing timely and effective on-site first aid in the early stage of acute and critical patients to prevent re-injury, and quickly and safely escorting patients to emergency department of the hospital for treatment. It’s purpose is to gain time and conditions for in-hospital first aid and to reduce the mortality and disability rate of acute and critical patients.1,2 However, geographical and natural environments, living habits, and socioeconomic development levels vary between regions, resulting in differences in disease spectrum, ethnic distribution, age of onset, and pre-hospital first aid capabilities for patients with pre-hospital first aid.3–6With the improvement of people’s health awareness and first aid awareness, pre-hospital first aid work has been paid more and more attention by the society. Previous studies have shown that regular analysis of pre-hospital first aid disease spectrum is helpful to adjust and optimize the local first aid resources and staffing, improve the pre-hospital emergency medical system and improve the emergency response capability.7 Keyouqian Banner, Hinggan League is considered representative of the minority farming and pastoral areas of eastern Inner Mongolia. This study retrospectively analyzed adult patients in this area with pre-hospital first aid to improve the configuration of pre-hospital first aid personnel and equipment, provide data support for strengthening the skills training for first aid personnel, promote health education, and construct a pre-hospital first aid system involving the whole society.
Materials and Methods
Clinical Data
All cases provided with pre-hospital first aid as a result of calling the 120 emergency number from January 2016 to December 2018 and admitted to the emergency department of our hospital were qualified for enrollment. The data were collected from the databases of the pre-hospital medical emergency command platform and the Emergency Department of Keyouqian Banner People’s Hospital. Patients with invalid calls or incomplete information were excluded. Finally, 2711 patients were enrolled and pre-hospital first aid provided were classified according to the emergency medicine specialty settings and the disease classification standards in the conventional internal medicine and surgical departments in the comprehensive hospital.8–10 The consent was received from all participants, and the Declaration of Helsinki were followed. This study was approved by the ethics committee of Keyouqianqi people’s Hospital.
Study Methods
The characteristics of patients were retrospectively analyzed, including gender, age, ethnicity, location of injury or illness, time between the 120 call and the arrival of the medical staff at the scene, vital signs on arrival, state of consciousness, reason for the medical service, onsite treatment measures, electrocardiogram (ECG) examination, diagnosis, outcome of the pre-hospital condition, and the effect of first aid.
Existing Baseline Pre-Hospital Personnel Training Level and Ambulance Equipment
The local pre-hospital first aid tasks are undertaken by medical staff in the Emergency Department of Keyouqian Banner People’s Hospital, which are required to obtain basic life support technology, advanced life support technology, use of first aid equipment, common first aid technology, laws, regulations and policies, doctor-patient communication skills, medical epidemic prevention and control measures, mental health and adjustment, etc. Vehicle-mounted ambulance equipment includes defibrillator monitors, transporters ventilator, automatic cardiopulmonary resuscitation machine, syringe pump, portable electrocardiograph, portable electrocardiograph, electric suction device, micro medical oxygen cylinder, special first aid kit for manual diagnosis, shovel type and automatic loading stretcher.
Criteria of Abnormal Vital Signs
The objective criteria used to mention abnormal vital signs are based on the “Expert Consensus on Emergency Pre-examination and Triage”. The objective vital signs evaluation indicators are as follows: heart rate greater than 100 beats/min or less than 55 beats/triage; systolic blood pressure greater than 180mmHg or less than 90mmHg; SpO2 less than 94%; respiratory rate greater than 20 times/min or less than 12 times/min.
The Emergency Medical Service in Mongolia
The pre-hospital medical emergency service system of the Inner Mongolia Autonomous Region requires all leagues and cities to set up pre-hospital medical emergency command centers (stations) based on the actual conditions and characteristics of their jurisdictions. In urban areas, an urban pre-hospital medical emergency network with the League City Emergency Command Center is built, with hospitals above the second level of the jurisdiction as the support. In rural and pastoral areas, a banner-level emergency command center/Qianxian-level hospital/town health center emergency network is established. The service radius in urban areas is no more than 5 kilometers, and that in rural and pastoral areas is 10 to 20 kilometers. Each league city allocates one ambulance for every 30,000 people. Pre-hospital emergency medical staff include pre-hospital emergency doctors, nurses and ambulance drivers. There is a unified pre-hospital emergency call number. According to national requirements, all leagues and cities uniformly use “120” as the pre-hospital emergency medical emergency call number to achieve one emergency in the entire region. It is required that 95% of the “120” calls for help are answered within 10 seconds, 95% of the vehicles are dispatched within 3 minutes, and 98% of the critical and critical on-site medical monitoring or rescue measures are implemented. For the unified dispatch of pre-hospital medical emergencies, the emergency command centers of all leagues and cities should establish an information platform for pre-hospital medical emergency command and dispatch, and follow the principles of nearest, urgent, and specialist to realize unified acceptance of emergency calls and unified dispatch of vehicle personnel. Relying on the emergency command centers (stations) established by medical institutions with a high comprehensive level at the banner and county level, a pre-hospital medical emergency command and dispatch system should be established according to the actual situation scheduling, improving scheduling efficiency.
Data Collection
Data collection was jointly completed by investigators in the Aerospace Center Hospital, Emergency Department of Keyouqian Banner People’s Hospital, and Emergency Department of Keyouqian Banner People’s Hospital.
Statistical Methods
The SPSS 24.0 software was adopted for statistical analysis. Data were expressed as means ± standard deviations. The descriptive research method was adopted to analyze gender composition, ethnic distribution, disease classification, and age distribution in patients provided with pre-hospital first aid, together with the pre-hospital first aid procedures, the outcome of pre-hospital first aid, etc.
Results
General Characteristics
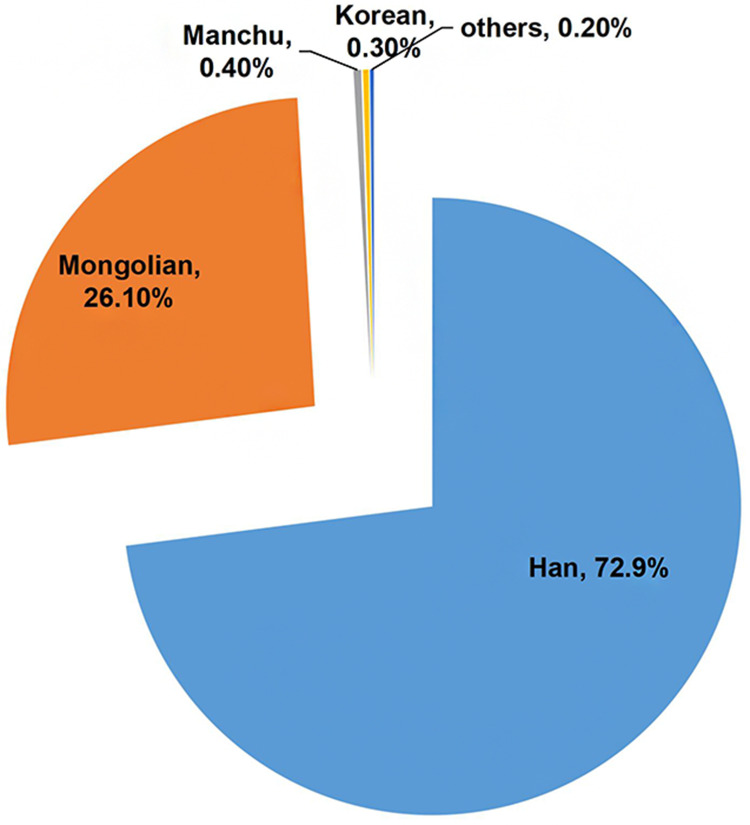
Of the 2711 patients, 1613 were male (57.7%) and 1098 were female (39.3%), with a male to female ratio of 1.47:1. There were 885 cases (32.8%) of young patients (18–40 years old), 1312 cases (48.7%) of middle-aged patients (41–65 years old), and 498 cases (18.5%) of elderly patients (≥65 years old). The ethnic distribution was 1\795 patients of Han (72.9%), 642 patients of Mongolian (26.1%), 11 patients of Manchu (0.4%), 8 patients of Korean (0.3%), and 6 patients of other ethnicities (0.2%) (Figure 1). The injuries and illnesses mainly occurred at home and on the road, with 982 cases (36.5%) and 1\164 cases (43.2%) respectively, and 565 cases (20.3%) in other locations. The time to arrival of medical services was 30.34 ± 28.29 minutes, and the time exceeded 30 minutes in 34.6% of cases. The vital signs in patients upon the arrival of medical services were 1261 cases with abnormal vital signs (45.1%), 161 cases with shock (5.9%), 482 cases with disturbance of consciousness (17.8%), and 97 cases with cardiac arrest (3.6%, 43 of them underwent on-site CPR). A total of 10 cases (0.4%) died after unsuccessful onsite first aid or died during the transfer to the hospital.
Figure 1.
The ethnic distribution of patients with provided with pre-hospital first aid as a result of calling the 120 emergency from 2016 to 2018 in the Keyouqian Banner People’s Hospital, Hinggan League.
Disease Composition
The disease category of adult patients comprised 1394 cases (51.3%) with internal medicine diseases and 1317 cases (48.7%) with surgical diseases. Among them, the main outpatient diseases concerning internal medicine comprised 499 cases (35.8%) with cardiovascular diseases, 433 cases (31.1%) with neurological diseases, 124 cases (8.9%) with respiratory diseases, 68 cases (4.9%) with intoxication, 46 cases (3.3%) with drunkenness, and 222 cases (15.9%) with other internal medicine diseases. The main outpatient surgical diseases comprised 752 cases (57.2%) with traffic accidents, 506 cases (38.5%) with other traumas, and 54 cases (4.1%) with other surgical diseases.
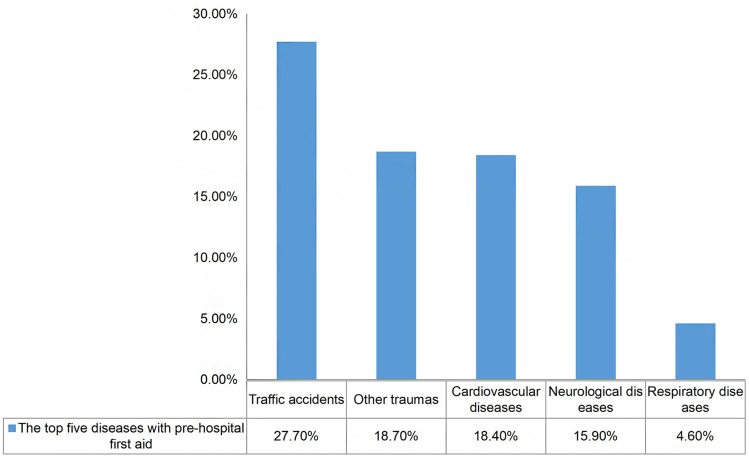
The top five diseases comprised 752 cases (27.7%) with traffic accidents, 506 cases (18.7%) with other trauma, 499 cases (18.4%) with cardiovascular diseases, 433 cases (15.9%) with neurological diseases, and 124 cases (4.6%) with respiratory diseases (Figure 2).
Figure 2.
The composition of the top five diseases in patients provided with pre-hospital first aid as a result of calling the 120 emergency from 2016 to 2018 in the Keyouqian Banner People’s Hospital, Hinggan League.
Age Distribution of the Top Five Diseases
Of the top five diseases in adult patients included in this study, traffic accidents and other traumas were the most common among young patients aged 18–44 years old, cardiovascular diseases and neurological diseases were the most common in middle-aged patients of 45–59 years old, and respiratory diseases were the most common in elderly patients aged 75–89 years (Table 1).
Table 1.
The Age Distribution of the Top Five Diseases in Adult Patients Provided with 120 Pre-Hospital First Aid from 2016 to 2018 in the Keyouqian Banner People’s Hospital, Hinggan League
| Disease Category | Sort | Age Group (n, %) | ||||
|---|---|---|---|---|---|---|
| 18~44 | 45~59 | 60~74 | 75~89 | ≥90 | ||
| Traffic Accident injury | 1 | 341(47.6) | 280(39.1) | 83(11.6) | 13(1.8) | – |
| Other Traumatic injury | 2 | 269(56.4) | 145(30.4) | 49(10.3) | 14(2.9) | – |
| Cardiovascular Disease | 3 | 136(27.8) | 147(30.1) | 142(29.0) | 59(12.1) | 5(1.0) |
| Neurological Disease | 4 | 86(20.1) | 155(36.7) | 128(30.3) | 50(11.8) | 3(0.7) |
| Respiratory Disease | 5 | 14(11.6) | 25(20.7) | 37(30.6) | 43(35.5) | 2(1.7) |
Pre-Hospital First Aid Procedures
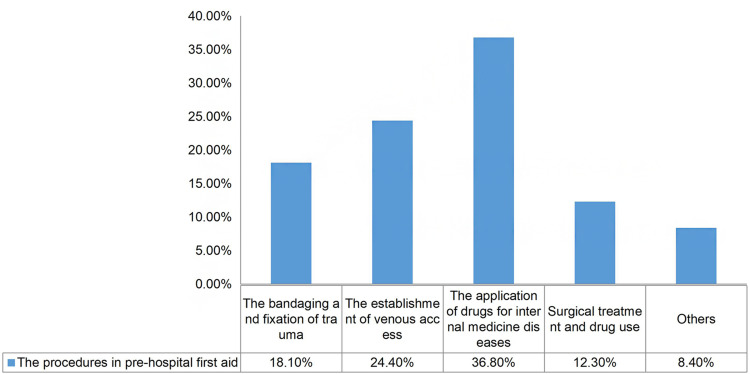
A total of 2322 cases (86.8%) received onsite procedures. Among them, the top three onsite first aid treatment measures were the application of drugs for internal medicine diseases, the establishment of venous access, and the bandaging and fixation of trauma (as illustrated in Figure 3). The onsite ECG examination showed that 887 cases (32.8%) were normal and 575 cases (21.2%) were abnormal. Additionally, 1244 cases (46.0%) did not have an ECG examination.
Figure 3.
The procedures in pre-hospital first aid.
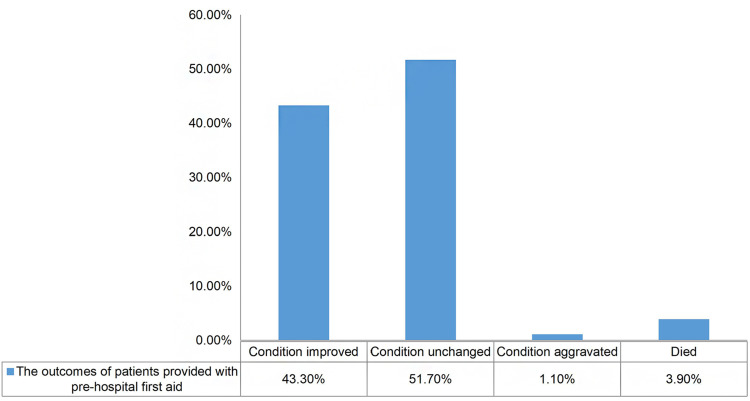
Outcomes
There were 1163 cases whose condition improved after onsite management, 1389 cases remained unchanged, 26 cases were aggravated, 97 cases had died before arrival of the medical services, and 10 cases died after onsite rescue or during the transfer to the hospital, with a mortality rate of 3.9% (Figure 4). The outcomes of medical service were as follows: 115 cases (4.3%) refused the treatment, 103 cases (3.8%) refused to come to the hospital, 593 cases (22.6%) were transferred to other hospitals, and 2003 cases (73.6%) were transferred to the emergency department of the present hospital.
Figure 4.
The outcomes of patients provided with pre-hospital first aid.
Discussion
Due to the differences in the local natural environment, living habits, and socioeconomic development levels,11 the disease spectrum, ethnic distribution, age of onset, and pre-hospital first aid capabilities in patients provided with pre-hospital first aid are quite different. Acknowledging the distributions of gender, age, ethnicity, and disease composition can improve the configuration of pre-hospital emergency personnel and equipment in other agricultural and pastoral areas in Inner Mongolia.
In patients provided with pre-hospital first aid in the region, the proportion of males was relatively high, the proportion of young and middle-aged patients was high, and injuries and illnesses mostly occurred on the road, accounting for 43.2% of locations. The reason could be correlated with the fact that trauma caused by traffic accidents, together with other traumas, were the two most observed among the disease spectrum of pre-hospital first aid in the present area, and males were at higher risk of traffic and work accidents during their life.12,13 Han and Mongolian patients accounted for a relatively large proportion, in line with the ethnic distribution of the population in the region.
The Keyouqian Banner People’s Hospital is the largest comprehensive hospital in the local area. Its first aid service covers the agricultural area, the agricultural and pastoral area, and the pastoral area according to distance. The pastoral area is a typical Mongolian population residential area. The arrival time of medical services for pre-hospital first aid was over 30 minutes in 34.6% of cases, with the longest travel time being approximately 6 hours. The long transfer times, together with difficulties during onsite rescues, significantly reduce the success rate in critically diseased patients.1,5,14 It also increases the pressure on the pre-hospital first aid medical staff.
Traffic accident injuries, other traumas, cardiovascular diseases, neurological diseases, and respiratory diseases accounted for the top five. Among these, traffic accidents and other traumas accounted for 27.7% and 18.7%, respectively, which was consistent with the disease compositions of trauma-based pre-hospital first aid reported by other emergency centers.1,5,6,15 This may be linked not only to the increase in the number of local motor vehicles and the development of construction but also to regional traffic conditions and poor road safety knowledge among the population, leading to problems such as speeding, drunk driving/riding, or driving/riding wearing no protective equipment. From the perspective of age distribution, injuries caused by traffic accidents and other traumas were the most common type among young patients aged 18 to 44 years old, indicating this was a high-risk group for accidental injuries. This age group was the highest proportion of the population overall in industrial production and in transportation usage. As age increased, the proportion of patients with trauma decreased, which may be correlated with factors such as changes in the maturity of people of different age groups, together with changes in work and lifestyles.15–17
Most patients with cardiovascular and cerebrovascular diseases were those in the middle-aged group of 45 to 59 years old, which differed from the age distribution concerning the disease spectrum in pre-hospital first aid reported by emergency centers in other regions.1,5,10,15 These results suggested that the occurrence of cardiovascular and cerebrovascular diseases in the present area was common in the younger population, and the incidence may be higher than that in other areas. This may be correlated with the high prevalence of hypertension and hyperlipidemia caused by the local alpine geographical environment, high salt intake, a diet rich in beef and mutton, and excessive drinking habits.5,18 Currently, the high incidence of cerebrovascular diseases in the local middle-aged population is already a serious problem, restricting the development of local society. Patients with mild cardiovascular and cerebrovascular diseases can experience a decline in the quality of life or loss of work and labor capacity, and even death in severe cases. These diseases also pose serious challenges to families and society.
Government departments should strengthen the primary and secondary prevention of common cardiovascular and cerebrovascular diseases (such as coronary heart disease and stroke), together with dietary intervention, smoking cessation, alcohol restriction, and control of blood pressure, blood glucose, and blood lipids.5,6,15 First aid knowledge, popularization, and education should be provided for patients with cardiovascular and cerebrovascular diseases and their families. This would improve the awareness of disease prevention among farmers and herdsmen at high risk and reduce the incidence of cardiovascular and cerebrovascular diseases.
The top three onsite first aid treatment measures were the application of drugs for internal medicine disease, the establishment of venous access, and trauma bandaging and fixation. These were in line with the first aid measures required by the top five diseases in the local adult patients undergoing pre-hospital first aid. In particular, the establishment of venous access and the completion of onsite ECG examination, which ranked second in the treatment measures, reflected the standardized first aid measures and professionalism of the pre-hospital medical staff in the Keyouqian Banner Hospital. Given the characteristics of pre-hospital first aid measures, while management for those with trauma was adequate, attention should be paid to the internal medicine diseases, especially when it comes to the emergency treatment of cardiovascular diseases, and the preparation of drugs and materials. Among patients in the present study, those with aggravated conditions accounted for 1.1%, and deaths after onsite rescue and during transportation accounted for 0.4%. These may have been caused by the critical condition of patients, the treatment conditions, the treatment competencies of the pre-hospital medical staff, the large first aid area radius, and the long transfer time, etc.5,14,15
To improve the survival of adult patients provided with pre-hospital first aid, emergency medical staff should be trained in multidisciplinary first aid knowledge. Emergency centers should optimize the deployment of pre-hospital first aid network units, shorten the radius of the emergency response area, and reduce the time of patient transportation.
Conclusion
This study provided epidemiological reference for patients in the farming and pastoral areas inhabited by ethnic minorities in eastern Inner Mongolia. These results may be used to improve traffic safety, and legal education, increase safety precautions, enhance disease prevention awareness and health promotion in agricultural and pastoral areas, to establish early intervention to reduce the incidence of disease and disease-related adverse consequences, and to improve the knowledge and training of pre-hospital first aid medical staff and thus the reduce mortality rate.
Disclosure
The authors declare that there is no conflict of interest.
References
- 1.Jia L, Xing DG, Chen F, Zhang Y. Current situation, problems and suggestions on local legislation of pre-hospital emergency care in China. Med Philos. 2021;42(6):61–65. [Google Scholar]
- 2.Scott J, Fidler G, Monk D, et al. Exploring the potential for social prescribing in pre hospital emergency and urgent care: a qualitative study. Health Soc Care Community. 2021;29(3):654–663. doi: 10.1111/hsc.13337 [DOI] [PubMed] [Google Scholar]
- 3.Boonmee C, Arimura M, Asada T. Facility location optimization model for emergency humanitarian logistics. Int J Disaster Risk Reduct. 2017;24:485–498. doi: 10.1016/j.ijdrr.2017.01.017 [DOI] [Google Scholar]
- 4.Bélanger V, Ruiz A, Soriano P. Recent optimization models and trends in location, relocation, and dispatching of emergency medical vehicles. Eur J Oper Res. 2019;272(1):1–23. doi: 10.1016/j.ejor.2018.02.055 [DOI] [Google Scholar]
- 5.Schehadat MS, Scherer G, Groneberg DA, et al. Outpatient care in acute and prehospital emergency medicine by emergency medical and patient transport service over a 10-year period: a retrospective study based on dispatch data from a German emergency medical dispatch centre (OFF-RESCUE). BMC Emerg Med. 2021;21(1):1–10. doi: 10.1186/s12873-021-00424-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Metelmann C, Metelmann B, Kohnen D, et al. Evaluation of a rural emergency medical service project in Germany: protocol for a multimethod and multiperspective longitudinal analysis. JMIR Res Protoc. 2020;9(2):e14358. doi: 10.2196/14358 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Xu L, Tang F, Wang Y, et al. Research progress of pre-hospital emergency during 2000–2020: a bibliometric analysis. Am J Transl Res. 2021;13(3):1109. [PMC free article] [PubMed] [Google Scholar]
- 8.Ge JB, Xu YJ. Internal Medicine. 8th ed. Beijing: People’s Medical Publishing House; 2013. [Google Scholar]
- 9.Chen XP, Wang JP. Surgery. 8th ed. Beijing: People’s Medical Publishing House; 2013. [Google Scholar]
- 10.Hung KKC, Cheung CSK, Rainer TH, et al. EMS systems in China. Resuscitation. 2009;80(7):732–735. doi: 10.1016/j.resuscitation.2009.04.016 [DOI] [PubMed] [Google Scholar]
- 11.Li XH. The difficult problem of implementing grassland sustainable development strategy – a case study of KEYOUQIAN banner, Xing’an League, Inner Mongolia. North Eco. 2005;2005(12X):5–7. [Google Scholar]
- 12.Brown J, Sajankila N, Claridge JA. Prehospital assessment of trauma. Surgical Clin. 2017;97(5):961–983. doi: 10.1016/j.suc.2017.06.007 [DOI] [PubMed] [Google Scholar]
- 13.Gauss T, Ageron FX, Devaud ML, et al. Association of prehospital time to in-hospital trauma mortality in a physician-staffed emergency medicine system. JAMA Surg. 2019;154(12):1117–1124. doi: 10.1001/jamasurg.2019.3475 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Mell HK, Mumma SN, Hiestand B, et al. Emergency medical services response times in rural, suburban, and urban areas. JAMA Surg. 2017;152(10):983–984. doi: 10.1001/jamasurg.2017.2230 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Li ZH, Yu HL. Epidemiological study on 120 pre hospital emergency adult patients in Beijing in 2010. Pract J Cardiac Cerebral Pneumal Vascular Dis. 2013;21(11):43–44. [Google Scholar]
- 16.Gu XM, Yao SB, He Z, et al. Meta-analysis of the success rate of heartbeat recovery in patients with prehospital cardiac arrest in the past 40 years in China. Military Med Res. 2020;7(1):1–18. doi: 10.1186/s40779-020-00263-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lo SM, Yu YM, Lee LYL, et al. Overview of the Shenzhen emergency medical service call pattern. World J Emerg Med. 2012;3(4):251. doi: 10.5847/wjem.j.issn.1920-8642.2012.04.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Berdowski J, Berg RA, Tijssen JGP, et al. Global incidences of out-of-hospital cardiac arrest and survival rates: systematic review of 67 prospective studies. Resuscitation. 2010;81(11):1479–1487. doi: 10.1016/j.resuscitation.2010.08.006 [DOI] [PubMed] [Google Scholar]