Abstract
Background
Improving mobility outcomes after hip fracture is key to recovery. Possible strategies include gait training, exercise and muscle stimulation. This is an update of a Cochrane Review last published in 2011.
Objectives
To evaluate the effects (benefits and harms) of interventions aimed at improving mobility and physical functioning after hip fracture surgery in adults.
Search methods
We searched the Cochrane Bone, Joint and Muscle Trauma Group Specialised Register, the Cochrane Central Register of Controlled Trials, MEDLINE, Embase, CINAHL, trial registers and reference lists, to March 2021.
Selection criteria
All randomised or quasi‐randomised trials assessing mobility strategies after hip fracture surgery. Eligible strategies aimed to improve mobility and included care programmes, exercise (gait, balance and functional training, resistance/strength training, endurance, flexibility, three‐dimensional (3D) exercise and general physical activity) or muscle stimulation. Intervention was compared with usual care (in‐hospital) or with usual care, no intervention, sham exercise or social visit (post‐hospital).
Data collection and analysis
Members of the review author team independently selected trials for inclusion, assessed risk of bias and extracted data. We used standard methodological procedures expected by Cochrane. We used the assessment time point closest to four months for in‐hospital studies, and the time point closest to the end of the intervention for post‐hospital studies. Critical outcomes were mobility, walking speed, functioning, health‐related quality of life, mortality, adverse effects and return to living at pre‐fracture residence.
Main results
We included 40 randomised controlled trials (RCTs) with 4059 participants from 17 countries. On average, participants were 80 years old and 80% were women. The median number of study participants was 81 and all trials had unclear or high risk of bias for one or more domains. Most trials excluded people with cognitive impairment (70%), immobility and/or medical conditions affecting mobility (72%).
In‐hospital setting, mobility strategy versus control
Eighteen trials (1433 participants) compared mobility strategies with control (usual care) in hospitals. Overall, such strategies may lead to a moderate, clinically‐meaningful increase in mobility (standardised mean difference (SMD) 0.53, 95% confidence interval (CI) 0.10 to 0.96; 7 studies, 507 participants; low‐certainty evidence) and a small, clinically meaningful improvement in walking speed (CI crosses zero so does not rule out a lack of effect (SMD 0.16, 95% CI ‐0.05 to 0.37; 6 studies, 360 participants; moderate‐certainty evidence). Mobility strategies may make little or no difference to short‐term (risk ratio (RR) 1.06, 95% CI 0.48 to 2.30; 6 studies, 489 participants; low‐certainty evidence) or long‐term mortality (RR 1.22, 95% CI 0.48 to 3.12; 2 studies, 133 participants; low‐certainty evidence), adverse events measured by hospital re‐admission (RR 0.70, 95% CI 0.44 to 1.11; 4 studies, 322 participants; low‐certainty evidence), or return to pre‐fracture residence (RR 1.07, 95% CI 0.73 to 1.56; 2 studies, 240 participants; low‐certainty evidence). We are uncertain whether mobility strategies improve functioning or health‐related quality of life as the certainty of evidence was very low.
Gait, balance and functional training probably causes a moderate improvement in mobility (SMD 0.57, 95% CI 0.07 to 1.06; 6 studies, 463 participants; moderate‐certainty evidence). There was little or no difference in effects on mobility for resistance training. No studies of other types of exercise or electrical stimulation reported mobility outcomes.
Post‐hospital setting, mobility strategy versus control
Twenty‐two trials (2626 participants) compared mobility strategies with control (usual care, no intervention, sham exercise or social visit) in the post‐hospital setting. Mobility strategies lead to a small, clinically meaningful increase in mobility (SMD 0.32, 95% CI 0.11 to 0.54; 7 studies, 761 participants; high‐certainty evidence) and a small, clinically meaningful improvement in walking speed compared to control (SMD 0.16, 95% CI 0.04 to 0.29; 14 studies, 1067 participants; high‐certainty evidence). Mobility strategies lead to a small, non‐clinically meaningful increase in functioning (SMD 0.23, 95% CI 0.10 to 0.36; 9 studies, 936 participants; high‐certainty evidence), and probably lead to a slight increase in quality of life that may not be clinically meaningful (SMD 0.14, 95% CI ‐0.00 to 0.29; 10 studies, 785 participants; moderate‐certainty evidence). Mobility strategies probably make little or no difference to short‐term mortality (RR 1.01, 95% CI 0.49 to 2.06; 8 studies, 737 participants; moderate‐certainty evidence). Mobility strategies may make little or no difference to long‐term mortality (RR 0.73, 95% CI 0.39 to 1.37; 4 studies, 588 participants; low‐certainty evidence) or adverse events measured by hospital re‐admission (95% CI includes a large reduction and large increase, RR 0.86, 95% CI 0.52 to 1.42; 2 studies, 206 participants; low‐certainty evidence).
Training involving gait, balance and functional exercise leads to a small, clinically meaningful increase in mobility (SMD 0.20, 95% CI 0.05 to 0.36; 5 studies, 621 participants; high‐certainty evidence), while training classified as being primarily resistance or strength exercise may lead to a clinically meaningful increase in mobility measured using distance walked in six minutes (mean difference (MD) 55.65, 95% CI 28.58 to 82.72; 3 studies, 198 participants; low‐certainty evidence). Training involving multiple intervention components probably leads to a substantial, clinically meaningful increase in mobility (SMD 0.94, 95% CI 0.53 to 1.34; 2 studies, 104 participants; moderate‐certainty evidence). We are uncertain of the effect of aerobic training on mobility (very low‐certainty evidence). No studies of other types of exercise or electrical stimulation reported mobility outcomes.
Authors' conclusions
Interventions targeting improvement in mobility after hip fracture may cause clinically meaningful improvement in mobility and walking speed in hospital and post‐hospital settings, compared with conventional care. Interventions that include training of gait, balance and functional tasks are particularly effective. There was little or no between‐group difference in the number of adverse events reported. Future trials should include long‐term follow‐up and economic outcomes, determine the relative impact of different types of exercise and establish effectiveness in emerging economies.
Plain language summary
Do mobility strategies improve and restore mobility after hip fracture surgery in adults?
Key messages
Mobility is the ability to move about, including standing up and walking. Mobility strategies are treatments that aim to help people move better.
Mobility treatment undertaken in hospital may moderately improve people's mobility four months after their hip was fractured. The effect of mobility treatment on other main outcomes was unclear. Mobility treatment undertaken after discharge from hospital after a fractured hip improves mobility, probably increases walking speed, improves functioning slightly and reduces falls.
Future studies should focus on which types of treatments work best and whether the treatments work in poorer countries.
What can people do to improve their mobility after a hip fracture?
A key aim of care after surgery for hip fracture is to get people safely back on their feet, moving and walking again. Initially, people may be asked to rest in bed and restrict weight bearing. Then various strategies to improve mobility, including walking retraining, exercise programmes and electrical stimulation, are used during hospital stay and often after discharge from hospital.
What did we want to find out?
We wanted to find out:
‐ whether mobility treatments delivered in the hospital or after discharge from hospital help people move around better;
‐ what type of treatments help people move well after hip fracture.
We also wanted to know if mobility treatments can cause unwanted effects.
What did we do?
We searched for studies that compared:
‐ mobility training against no mobility training; or
‐ different methods and times of mobility treatments.
We compared and summarised their results, and rated our confidence in the evidence, based on factors such as study methods and sizes.
What did we find?
We found 40 studies that involved 4059 people with hip fracture, most of whom were over 65 years old, with an average age of 80. The smallest study involved 26 people and the largest involved 336 people. The studies were conducted in 17 countries. Many of the studies had weak methods. Twenty‐seven studies received funding, mostly from government and research funding organisations.
Main results
Eighteen studies evaluated mobility strategies that started in the hospital within a week after hip fracture surgery. Mobility treatment undertaken in hospital may moderately increase people's mobility four months after their fracture and probably increases walking speed to a small but meaningful degree. Mobility treatment probably makes little or no difference to re‐admission to hospital, return to living at home, or death. We are not certain if mobility treatment affects physical functioning (the ability to move around and function in one’s environment) or well‐being.
Twenty‐two trials evaluated longer‐duration mobility strategies that started after discharge from hospital and were undertaken in homes, retirement villages and outpatient clinics. In these settings, mobility treatment increases mobility to a small but meaningful degree, meaningfully increases walking speed, and leads to a small but non‐meaningful increase in functioning. Compared to no treatment, social visits or usual care, mobility treatment probably slightly improves people's well‐being but not to a meaningful level. Mobility treatment probably makes little or no difference to re‐admission to hospital or death.
The types of treatment that appear effective in improving people’s mobility are exercises in additional to standard physiotherapy. Both in the hospital and after discharge from hospital, the helpful exercises target balance, walking and functional tasks. After discharge from hospital, extra strength or endurance training may also improve mobility. The effect of electrical stimulation was not clear.
Overall, the review found that both in hospital and after discharge, there is enough evidence to say that treatment targeting mobility is probably better than no extra treatment in helping people get people safely back on their feet, moving and walking again after hip fracture surgery.
What are the limitations of the evidence?
We have low to moderate confidence in the results of the studies in hospitals. Our confidence was lowered because: some of the studies did not report all their results; they used different ways of delivering treatments; and many of the studies were small.
We are more confident in the results of the studies conducted after discharge from hospital, including the finding that mobility training improves movement and walking. We are less confident in the results for unwanted effects, because of the low number of unwanted effects reported.
How up to date is this evidence?
This review updates our previous review. The evidence is up to date to March 2021.
Summary of findings
Summary of findings 1. Summary of findings: in‐hospital studies.
| Mobility strategies compared with control (e.g. usual care) after hip fracture surgery in the in‐hospital setting | ||||||
|
Patient or population: adults following hip fracture surgery Settings: in‐hospital Intervention: mobility strategiesa Comparison: usual in‐hospital careb | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | No of participants (studies) | Certainty of the evidence (GRADE) | Comments | |
| Assumed risk | Corresponding risk | |||||
| Controlc | Intervention | |||||
|
Mobilityd ‐ overall analysis Using different mobility scales: MILA (range 0 to 36), EMS (range 0 to 20), BBS (range 0 to 56), PPME (range 0 to 12), Koval (range 1 to 7). Higher values indicate better mobility (except MILA and Koval, where scale was inverted for consistency with other measures). Follow‐up: range 5 days to 4 months |
In the control group, the mean scores for the outcomes were: MILA = 19.2; EMS = 16.3 to 17; BBS = 26; PPME = 6.8 to 9.1; Koval = 4. | SMD 0.53 higher (0.10 higher to 0.96 higher) |
SMD 0.53 (0.10 to 0.96) | 507 (7) | ⊕⊕⊝⊝ Lowe | Re‐expressing the results using the 12‐point PPME, the intervention group scored 1.46 points higher (95% CI 0.28 to 2.64). MID for the PPME is typically 1.13 to 2.15 (de Morton 2008). Based on Cohen’s effect sizesf, mobility strategies may cause a moderate increase in mobility compared with control (SMD 0.53). Types of intervention in included trials: gait, balance and functional exercise: 6 studies; resistance exercise: 1 study |
|
Walking speedg ‐ overall analysis Measured using metres/second (m/s) and metres/minute (m/min). A higher score indicates faster walking. Follow‐up: range 2 weeks to 4 months |
The mean walking speed score in the control group ranged from 0.19 m/s to 0.72 m/s, and was 24.4 m/min. | SMD 0.16 higher (0.05 lower to 0.37 higher) | SMD 0.16 (‐0.05 to 0.37) | 360 (6) | ⊕⊕⊕⊝ Moderateh |
Overall, there is moderate‐certainty evidence of a small increase in walking (based on Cohen's effect sizes) compared with control (SMD 0.16); however, the confidence interval includes both slower and faster walking. Re‐expressing the results using gait speed (m/s) showed an increase of 0.04 m/s in the intervention group (MD 0.04, 95% CI ‐0.01 to 0.08). Small meaningful change for gait speed is 0.04 m/s to 0.06 m/s (Perera 2006). Types of intervention in included trials: gait, balance and functional exercise: 5 studies; electrical stimulation: 1 study |
|
Functioningi ‐ overall analysis Using different scales: mBI (range 0 to 20), BI (range 0 to 100), FIM (range 18 to 126), NEADL (range 0 to 66). A higher score indicates better functioning. Follow‐up: range 3 weeks to 4 months |
In the control group, the mean scores for the outcomes were: mBI: 18; BI: 95; FIM: 69 to 81; NEADL 33.4 | SMD 0.75 higher (0.24 higher to 1.26 higher) | SMD 0.75 (0.24 to 1.26) |
379 (7) | ⊕⊝⊝⊝ Verylowj | We are uncertain whether mobility strategies improve functioning as the certainty of the evidence is very low. Re‐expressing the results using the BI, the intervention group scored 4.4 points higher (95% CI 1.4 to 7.38). MID for the BI (post‐ hip surgery) is typically 9.8 (Unnanuntana 2018). Types of intervention in included trials: gait, balance and functional exercise: 5 studies; resistance exercise: 1 study. |
|
HRQoL Using EQ‐5D (range 0 to 1) and HOOS (range 0 to 100). A higher score indicates better quality of life. Follow‐up: range 10 weeks to 6 months |
In the control group, the mean scores for the outcomes were: EQ‐5D (range 0.54 to 0.62), HOOS 50.37 | SMD 0.26 higher (0.07 lower to 0.85 higher) | SMD 0.39 (‐0.07, 0.85) |
314 (4) | ⊕⊝⊝⊝
Verylowk |
We are uncertain whether mobility strategies improve HRQoL as the certainty of the evidence is very low. We calculated SMD for 3 trials with EQ‐5D and 1 trial with HOOS. Re‐expressing the results using the EQ‐5D (0 to 1 scale), there was an increase in quality of life of 0.03 in the intervention group (95% CI ‐0.02 to 0.22). MID for the EQ‐5D is typically 0.074 (Walters 2005). Types of intervention in included trials: gait, balance and functional exercise: 4 studies. |
|
Mortality Follow‐up: short‐term range 10 days to 6 months; long‐term = 12 months |
Short term: 45 per 1000 |
Short term: 48 per 1000 (22 to 104) |
Short term: RR 1.06 (0.48 to 2.30) |
Short term: 489 (6) |
⊕⊕⊝⊝ Lowm | It is unclear whether mobility strategies reduce mortality as the certainty of evidence is low and the 95% CI includes both a reduction and an increase in the risk of mortality, in both the short term and the long term. Types of intervention in included trials: gait, balance and functional exercise: 4 studies; resistance exercise: 3 studies; electrical stimulation: 1 study. |
| Long term: 116 per 1000l |
Long term: 142 per 1000 (56 to 362) | Long term: RR 1.22 (0.48 to 3.12) |
Long term: 133 (2) |
⊕⊕⊝⊝ Lowm | ||
|
Adverse event: number of people who were re‐admitted Follow‐up: range 5 days to 4 months |
229 per 1000k | 160 (36 to 254) | RR 0.70 (0.44 to 1.11) | 322 (4) | ⊕⊕⊝⊝ Lown | It is unclear whether mobility strategies reduce re‐admission compared with usual care, as the CI includes both a reduction and an increase in the risk of re‐admission. Types of intervention in included trials: gait, balance and functional exercise: 3 studies; resistance exercise: 1 study |
|
Number of people who returned to living at pre‐fracture residence Follow‐up: range 10 days to 4 months |
705 per 1000k | 754 per 1000 (452 to 1099) | RR 1.07 (0.73 to 1.56) | 240 (2) | ⊕⊕⊝⊝
Lowo |
It is unclear whether mobility strategies increase the odds of returning to living at the pre‐fracture residence: there is low‐certainty evidence and the CI includes both a reduction and an increase in the risk of re‐admission. Types of intervention in included trials: gait, balance and functional exercise: 1 study; resistance exercise: 1 study. |
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). BBS: Berg Balance Scale; BI: Barthel Index; CI: confidence interval; EMS: Elderly Mobility Scale; EQ‐5D: EuroQoL‐5 dimension questionnaire; FIM: Functional Independence Measure; HRQoL: health‐related quality of life; HOOS: Hip Disability and Osteoarthritis Outcome Score; HRQoL: health‐related quality of life; Koval: Koval Walking Ability Score; mBI: modified Barthel Index; MD: mean difference; MID: minimal important difference; MILA: Modified Iowa Level of Assistance; NEADL: Nottingham Extended Activities of Daily Living; PPME: Physical Performance and Mobility Examination; RR: risk ratio; SMD: standardised mean difference | ||||||
| GRADE Working Group grades of evidence High certainty: we are very confident that the true effect lies close to that of the estimate of the effect. Moderate certainty: we are moderately confident in the effect estimate; the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. Low certainty: our confidence in the effect estimate is limited; the true effect may be substantially different from the estimate of the effect. Very low certainty: we have very little confidence in the effect estimate; the true effect is likely to be substantially different from the estimate of effect. | ||||||
aMobility strategies may include exercises, physical training and muscle stimulation, used at various stages in rehabilitation, which aim to improve walking and minimise functional impairments. bA control intervention may be: usual orthopaedic, medical care or allied health care. cThe all‐studies population risk was based on the number of events and the number of participants in the control groups of studies included in this review reporting this outcome. dMobility, measuring the ability of a person to move. Scales may measure a number of aspects of mobility (e.g. sit to stand, walking, turning, stairs).eDowngraded by one level due to risk of bias (removing studies with high risk of bias in one or more items had a marked impact on results, with the confidence intervals (CIs) crossing zero). Downgraded one level for imprecision, with wide CI. Not downgraded for inconsistency; the substantial heterogeneity (I2 = 84%) is explained by inclusion of Monticone 2018 and the large between‐group difference in the volume and intensity of functional exercise undertaken, compared with other studies. Removing Monticone 2018 reduced I2 to 44%, and it changed the effect size from SMD 0.53 (95% CI 0.10 to 0.96) to SMD 0.29 (95% CI 0.03 to 0.55). fCohen's effect size 0.2 is described as small, 0.5 as medium/moderate effect, 0.8 as large effect (Sawilowsky 2009). gWalking speed, measured using distance/time. hNot downgraded due to risk of bias (as removing studies with high risk of bias in one or more items had no impact on results, with similar point estimate and CIs). Downgraded due to imprecision, with CI crossing zero. iFunctioning, using functioning scales. jDowngraded by one level due to risk of bias (removing studies with high risk of bias in one or more items had a marked impact on results), downgraded one level due to substantial heterogeneity (I2 = 81%), and downgraded one level due to imprecision (n = 315). kDowngraded by one level due to risk of bias (removing the studies with high risk of bias in one or more items had a marked impact on results), one level for imprecision (small number of trials and participants, wide CI) and one level due to substantial heterogeneity (I2 = 71%). lOur illustrative risks for dichotomous outcomes were based on the proportion calculated from the number of people who experienced the event divided by the number of people in the group, for the control group in those trials included in the analysis for that outcome. mWe downgraded both the short‐term and long‐term analyses by one level due to risk of bias (removing studies with high risk of bias in one or more items had a marked impact on results) and one level for imprecision (few events and wide CI). nDowngraded one level for imprecision (few events and wide CI) and one level because a large number of studies included in the review did not contribute to this adverse event outcome. oDowngraded one level for imprecision (few events and wide CI) and one level because a large number of studies included in the review did not contribute to the outcome.
Summary of findings 2. Summary of findings: different types of intervention on mobility outcome, in‐hospital.
| Different types of mobility strategies compared with control after hip fracture surgery, on mobility, in the in‐hospital setting | |||||||
|
Patient or population: adults following hip fracture surgery Settings: in‐hospital Comparison: usual in‐hospital carea Outcome: mobility, measured using mobility scales, 6‐Minute Walk Test and Timed Up and Go testb | |||||||
| Intervention type (according to ProFaNE)c | Mobility outcome | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | No of participants (studies) | Certainty of the evidence (GRADE) | Comments | |
| Assumed risk | Corresponding risk | ||||||
| Control | Intervention | ||||||
| Gait, balance and functional training Follow‐up: range 5 days to 4 months |
Mobility scales, using different mobility scales: MILA (range 0 to 36), EMS (range 0 to 20), BBS (range 0 to 56), PPME (range 0 to 12), Koval (range 1 to 7). Higher values indicate better mobility (except MILA and Koval, where scale was inverted for consistency with other outcomes). | In the control group, the mean scores for the outcomes were: MILA = 19.2; EMS = 16.3; BBS = 26; PPME = 6.8 to 9.1; Koval = 4. | SMD 0.57 higher (0.07 higher to 1.06 higher). | SMD 0.57 (0.07 to 1.06) |
463 (6) | ⊕⊕⊕⊝ Moderated | Interventions classified as gait, balance and functional training probably cause a moderatee increase in mobility compared with control (SMD 0.57). Re‐expressing the results using the 12‐point PPME, the intervention group scored 1.56 points higher (95% CI 0.02 to 2.92). MID for the PPME is typically 1.13 to 2.15 (de Morton 2008). |
| Resistance/strength training Follow‐up: range 10 days to 4 months |
Mobility scales, using EMS (range 0 to 20). Higher values indicate better mobility | The meanf score on the EMS in the control group was 17. | MD 1 point higher on the EMS (0.81 lower to 2.81 higher). | MD 1.0 (‐0.81 to 2.81) | 44 (1) | ⊕⊕⊝⊝ Lowg | It is unclear whether resistance/strength training interventions increase mobility as the certainty of evidence is low and the 95% CI includes both a reduction and an increase in mobility. |
| TUG (lower score = faster) | The mean TUG time in the control group was 25.4 seconds. | MD 1.5 second faster TUG time (6.4 seconds faster to 3.4 seconds slower) | MD ‐1.5 (‐6.4 to 3.4) | 74 (1) | ⊕⊕⊝⊝ Lowh | It is unclear whether resistance/strength training interventions improve TUG as the certainty of evidence is low and the 95% CI includes both a reduction and an increase in score. | |
| Flexibility | 0 | 0 studies contained a mobility strategy categorised as primarily being flexibility. | |||||
| 3D (Tai Chi, dance) | 0 | 0 studies contained a mobility strategy categorised as primarily being 3D. | |||||
| General physical activity | 0 | 0 studies contained a mobility strategy categorised as primarily being general physical activity. | |||||
| Endurance | 0 | 0 studies contained a mobility strategy categorised as primarily being endurance training. | |||||
| Multiple types of exercise | 0 | 0 studies contained a mobility strategy categorised as containing multiple types of exercise. | |||||
| Electrical stimulation | 0 | 0 studies contained a mobility strategy categorised as primarily being electrical stimulation. | |||||
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). BBS: Berg Balance Scale; CI: confidence interval; EMS: Elderly Mobility Scale; Koval: Koval Walking Ability Score; MD: mean difference; MID: minimally important difference; MILA: Modified Iowa Level of Assistance; PPME: Physical Performance and Mobility Examination; SMD: standardised mean difference; TUG: Timed Up and Go test | |||||||
| GRADE Working Group grades of evidence High certainty: we are very confident that the true effect lies close to that of the estimate of the effect. Moderate certainty: we are moderately confident in the effect estimate; the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. Low certainty: our confidence in the effect estimate is limited; the true effect may be substantially different from the estimate of the effect. Very low certainty: we have very little confidence in the effect estimate; the true effect is likely to be substantially different from the estimate of effect. | |||||||
aA control intervention may be: usual orthopaedic, medical care or allied health care. bMobility, measuring the ability of a person to move. Scales may measure a number of aspects of mobility (e.g. sit to stand, walking, turning, stairs). A higher score indicates better mobility. cMobility strategies involve postoperative care programmes such as immediate or delayed weight bearing after surgery, and any other mobilisation strategies, such as exercises, physical training and muscle stimulation, used at various stages in rehabilitation, which aim to improve walking and minimise functional impairments. We categorised the exercise and physical training strategies using the Prevention of Falls Network Europe (ProFaNE) guidelines, see Appendix 1. These categories are gait, balance and functional training; strength/resistance training; flexibility; 3D (Tai Chi, dance); general physical activity; endurance; multiple types of exercise; other. Electrical stimulation is an additional intervention type. dDowngraded one level for inconsistency (unexplained heterogeneity, I2 = 84%). eCohen's effect size 0.2 is described as small, 0.5 as medium/moderate effect, 0.8 as large effect (Sawilowsky 2009). fMean was estimated from median for the single study. gDowngraded one level for risk of bias and one level for imprecision. hDowngraded one level for risk of bias and one level for imprecision.
Summary of findings 3. Summary of findings: post‐hospital studies.
| Mobility strategies compared with control (e.g. usual care) after hip fracture surgery in the post‐hospital setting | ||||||
|
Patient or population: adults following hip fracture surgery Settings: post‐hospital Intervention: mobility strategiesa Comparison: non‐provision controlb | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | No of participants (studies) | Certainty of the evidence (GRADE) | Comments | |
| Assumed risk | Corresponding risk | |||||
| Controlc | Intervention | |||||
|
Mobilityd ‐ overall analysis Using different mobility scales: mPPT (range 0 to 36), POMA (range 0 to 30), SPPB (range 0 to 12), PPME (range 0 to 12). A higher score indicates better mobility. Follow‐up: range 2 months to 12 months |
In the control group, the mean scores for the outcomes were: mPPT (23.3), POMA (20.7), SPPB (range 6 to 7.72), PPME (10.1) | SMD 0.32 higher (0.11 higher to 0.54 higher) | SMD 0.32 (0.11 to 0.54) |
761 (7) | ⊕⊕⊕⊕ Highe | Overall, there is a small (based on Cohen's effect sizesf) increase in mobility compared with control (SMD 0.32). Re‐expressing the results using the 12‐point SPPB, the intervention group scored 0.89 points higher (95% CI 0.30 to 1.50). Small meaningful change for SPPB: 0.27 to 0.55 points; substantial meaningful change: 0.99 to 1.34 points (Perera 2006). Types of intervention in included trials: gait, balance and functional exercise: 5 studies; multiple types: 2 studies. |
|
Walking speedg ‐ overall analysis Measured using metres/second (m/s) and metres/minute (m/min). A higher score indicates faster walking. Follow‐up: range 1 month to 12 months |
The mean walking speed score in the control group ranged from 0.44 m/s to 0.97 m/s, and 20 m/min to 59.4 m/min. | SMD 0.16 higher (0.04 higher to 0.29 higher) | SMD 0.16 (0.04 to 0.29) | 1067 (14) | ⊕⊕⊕⊕
Highh |
There is a small increase in walking speed compared with control (SMD 0.16). Re‐expressing the results using gait speed (m/sec), there was an increase in gait speed of 0.05 m/s in the intervention group (MD 0.05, 95% CI 0.01 to 0.09). Small meaningful change for walking speed is 0.04 to 0.06 m/s (Perera 2006). Types of intervention in included trials: gait, balance and functional exercise: 7 studies; resistance exercise: 3 studies; endurance exercise: 1 study; multiple types: 3 studies. |
|
Functioningi ‐ overall analysis Using different functioning scales: FSQ (range 0 to 36), BI (range 0 to 100), AM‐PAC daily activity (range 9 to 101), COPM (range 0 to 20), LEFS (range 0 to 80), NEADL (range 0 to 66). A higher score indicates better functioning. Follow‐up: range 3 months to 12 months |
In the control group, the mean scores for the outcomes were: FSQ (24.8), BI (94.5), AM‐PAC (58.6), COPM (6.54), LEFS (28.8), NEADL (range 14.2 to 43.2). | SMD 0.23 higher (0.10 higher to 0.36 higher) | SMD 0.23 (0.10 to 0.36) | 936 (9) | ⊕⊕⊕⊕ Highj | Overall, there is a small increase in functioning compared with control (SMD 0.23). Re‐expressing the results using the BI, the intervention group scored 1.4 points higher (95% CI 0.6 to 2.1). MID for the BI (post‐hip surgery) is typically 9.8 (Unnanuntana 2018). Types of intervention in included trials: gait, balance and functional exercise: 4 studies; resistance exercise: 2 studies; multiple types: 2 studies; other: 1 study |
|
HRQoL using EQ‐ 5D (range 0 to 1), SF‐36 (range 0 to 100), SF‐12 (range 0 to 100), and WHOQOL‐BREF (range 0 to 130). A higher score indicates better quality of life. Follow‐up: range 3 months to 6 months |
In the control group, the mean scores for the outcomes were: EQ‐5D (range 0.6 to 0.75), SF‐36 (range 48 to 63), SF‐12 (45.5), WHOQOL‐BREF (13.2). | SMD 0.14 higher (0.00 lower to 0.29 higher) | SMD 0.14 (0.00 to 0.29) | 785 (10) | ⊕⊕⊕⊝
Moderatek |
SMD was calculated for 5 trials with EQ‐5D, 3 trials with SF‐36, 1 trial with SF‐12, 1 trial with WHOQOL‐BREF. Re‐expressing the results using the EQ‐5D (0 to 1 scale), there was an increase in quality of life of 0.01 in the intervention group (95% CI ‐0.007 to 0.08). MID for the EQ‐5D is typically 0.074 (Walters 2005). Re‐expressing the results using the SF‐36 (0 to 100 scale), there was an increase in quality of life of 3 points in the intervention group (95% CI ‐0.6 to 5.7). MID for SF‐36 typically 3 to 5 (Walters 2003). Mobility strategies probably make little important difference to patient‐reported health‐related quality of life compared with control. Types of intervention in included trials: gait, balance and functional exercise: 4 studies; resistance exercise: 3 studies; endurance exercise: 1 study; multiple types: 1 study; other: 1 study |
|
Mortality Follow‐up: range 3 months to 12 months |
Short term: 35 per 1000l | Short term: 35 per 1000 (14 to 72) | Short term: RR 1.01 (0.49 to 2.06) |
Short term: 737 (8) |
⊕⊕⊕⊝ Moderatem | Overall, there is moderate‐certainty evidence that mobility strategies probably make little or no difference to mortality compared to control in the short term. It is unclear whether mobility strategies reduce mortality in the long term as the certainty of evidence is low and the 95% CI includes both a reduction in the risk of mortality and an increase in the risk of mortality. Types of intervention in included trials: gait, balance and functional exercise: 3 studies; resistance exercise: 3 studies; multiple types: 5 studies. |
| Long term: 71 per 1000l | Long term: 52 per 1000 (28 to 97) |
Long term: RR 0.73 (0.39 to 1.37) | Long term: 588 (4) |
⊕⊕⊝⊝ Lown | ||
|
Adverse event: number of people who were re‐admitted Follow‐up: range 1 month to 12 months |
231 per 1000l | 199 (120 to 328) | RR 0.86 (0.52 to 1.42) | 206 (2) | ⊕⊕⊝⊝ Lowo | The evidence is of low certainty: the intervention may decrease the number of re‐admissions by 14%; however, the 95% CI includes the possibility of both a 48% reduction and a 42% increase. Types of intervention in included trials: multiple types: 1 study; other: 1 study. |
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). AM‐PAC: Activity Measure for Post Acute Care; BI: Barthel Index; CI: confidence interval; COPM: Canadian Occupational Performance Measure; EQ5D: EuroQoL‐5Dl; FSQ: Functional StaRR: risk ratio; HRQoL: Health‐Related Quality of Life; LEFS: Lower Extremity Functional Scale; MID: minimal important difference; MD: mean difference; mPPT: modified Physical Performance Test; tus Questionnaire; NEADL: Nottingham Extended Activities of Daily Living; PME: Physical Performance and Mobility Examination; POMA: Performance Oriented Mobility Assessment; PWHOQOL BREF: World Health Organization Quality of LIfe short version; SMD: standardised mean difference; SF12: Short Form‐12 SF36: Short Form‐36; SPPB: Short Physical Performance Battery. | ||||||
| GRADE Working Group grades of evidence High certainty: we are very confident that the true effect lies close to that of the estimate of the effect. Moderate certainty: we are moderately confident in the effect estimate; the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. Low certainty: our confidence in the effect estimate is limited; the true effect may be substantially different from the estimate of the effect. Very low certainty: we have very little confidence in the effect estimate; the true effect is likely to be substantially different from the estimate of effect. | ||||||
a Postoperative care programmes such as exercises, physical training and muscle stimulation, used at various stages in rehabilitation, which aim to improve walking and minimise functional impairments. bA non‐provision control is defined as no intervention, usual care, sham exercise (the exercise was intended to be a control, or appeared to be of insufficient intensity and progression to have beneficial effects on mobility) or a social visit. cThe all‐studies population risk was based on the number of events and the number of participants in the control group. dMobility, measuring the ability of a person to move. Scales may measure a number of aspects of mobility (e.g. sit to stand, walking, turning, stairs). eNot downgraded for risk of bias, as point estimate increased from 0.32 to 0.38 and CI remained close to zero (95% CI from (0.11 to 0.54) to (‐0.04 to 0.79)) upon removal of the trials at a high risk of bias in one or more items. fCohen's effect size 0.2 is described as small, 0.5 as medium/moderate effect, 0.8 as large effect (Sawilowsky 2009). gWalking speed, measured using distance/time. hNot downgraded for risk of bias, as point estimate reduced from 0.16 to 0.14 and CI remained close to zero (95% CI from (0.04 to 0.29) to (‐0.08 to 0.36) upon removal of the trials at a high risk of bias in one or more items. iFunctioning, using functioning scales. jNot downgraded for risk of bias, as point estimate increased and CI remained above zero upon removal of the trials at a high risk of bias in one or more domains. kDowngraded one level for risk of bias (removing studies with high risk of bias in one or more domains had a marked impact on results). lOur illustrative risks for dichotomous outcomes were based on the proportion calculated from the number of people who experienced the event divided by the number of people in the group, for the control group in those trials included in the analysis for that outcome. mNot downgraded for risk of bias, as results were essentially unchanged with removal of the trials at a high risk of bias in one or more domains. Downgraded by one level due to imprecision (few events and wide CI). nDowngraded one level for risk of bias (removing studies with high risk of bias in one or more domains had an important impact on results) and one level for imprecision (few events and wide CI). oWe downgraded one level for risk of bias, as both trials were at a high risk of bias in one or more domains. Downgraded one level for imprecision (few events and wide CI).
Summary of findings 4. Summary of findings: different types of intervention on mobility outcome, post‐hospital.
| Different types of mobility strategies compared with control after hip fracture surgery, on mobility, in the post‐hospital setting | |||||||
|
Patient or population: adults following hip fracture surgery Settings: post‐hospital Comparison: non‐provision controla Outcome: mobilityb | |||||||
| Intervention type (according to ProFaNE)c | Mobility outcome | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | No of participants (studies) | Certainty of the evidence (GRADE) | Comments | |
| Assumed risk | Corresponding risk | ||||||
| Control | Intervention | ||||||
| Gait, balance and functional training Follow‐up: range 2 months to 12 months |
Mobility scales, using different scales: SPPB (range 0 to 12), PPME (range 0 to 12). A higher score indicates better mobility. | In the control group, the mean scores for the outcomes were: SPPB (range 6 to 7.72), PPME (10.1). | SMD 0.20 higher (0.05 higher to 0.36 higher) | SMD 0.20 (95% CI 0.05 to 0.36) |
621 (5) | ⊕⊕⊕⊕ Highd | Interventions classified as gait, balance and functional training cause a smalle increase in mobility compared with control. Re‐expressing the results using the 12‐point SPPB, the intervention group scored 0.55 points higher (95% CI 0.14 to 1.0). Small meaningful change for SPPB: 0.27 to 0.55 points; substantial meaningful change: 0.99 to 1.34 points (Perera 2006). |
| TUG (lower score = faster) | The mean TUG time in the control group was 30.22 seconds. |
MD 7.57 seconds faster (19.25 seconds faster to 4.11 seconds slower) | MD ‐7.57 (‐19.25 to 4.11) |
128 (1) | ⊕⊝⊝⊝ Very lowf | Gait, balance and functional training may increase TUG speed by 7.57 seconds; however, the 95% confidence interval includes both a reduction and increase in TUG. | |
| 6 Minute Walk Test | 0 | ||||||
| Resistance/strength training Follow‐up: range 10 weeks to 3 months |
Mobility scales | 0 | |||||
| TUG | The mean TUG time in the control group was 20 seconds. | MD 6 seconds faster (12.95 seconds faster to 0.95 seconds slower) | MD ‐6.00 (‐12.95, 0.95) | 96 (1) | ⊕⊕⊝⊝ Lowg | Resistance/strength training may increase TUG speed by 6 seconds; however, the 95% confidence interval includes both a reduction and increase in TUG. | |
| 6MWT | The mean 6MWT distance in the control group was 243 m. | MD 56 metres further (29 metres further to 83 metres further) | MD 55.65 (28.58 to 82.72) | 198 (3) | ⊕⊕⊝⊝ Lowh | Resistance/strength training may increase 6MWT by 53 metres. MID for the 6MWT (adults with pathology) is typically 14.0 to 30.5m (Bohannon 2017). |
|
| Flexibility | All | 0 | 0 studies contained a mobility strategy categorised as primarily being flexibility. | ||||
| 3D (Tai Chi, dance) | All | 0 | 0 studies contained a mobility strategy categorised as primarily being 3D. | ||||
| General physical activity | All | 0 | 0 studies contained a mobility strategy categorised as primarily being general physical activity. | ||||
| Endurance Follow‐up: 3 months |
Mobility scales | 0 | |||||
| TUG | 0 | ||||||
| 6MWT | The mean 6MWT distance in the control group was 266 m. | MD 12.7 metres further (72 metres less to 97 metres further). | MD 12.70 (‐72.12, 97.52) | 21 (1) | ⊕⊝⊝⊝ Very lowi | We are uncertain whether endurance training improves mobility as the certainty of the evidence is very low. | |
| Multiple primary types of exercise Follow‐up: range 2 months to 6 months |
Mobility scales, using different mobility scales: mPPT (range 0 to 36), POMA (range 0 to 30). | In the control group, the mean scores for the outcomes were: mPPT (23.3), POMA (range 20.7). | SMD 0.94 higher (0.53 higher to 1.34 higher) | SMD 0.94 (0.53 to 1.34) | 104 (2) | ⊕⊕⊕⊝ Moderatej | Interventions that contain multiple types of exercise probably leads to a moderate increase in mobility. Re‐expressing the results using the 12‐point SPPB, the intervention group scored 2.6 points higher (95% CI 1.47 to 3.71). Substantial meaningful change for SPPB: 0.99 to 1.34 points (Perera 2006). |
| TUG | 0 | ||||||
| 6MWT | The mean 6MWT distance in the control group was 233.1 m. | MD 9 metres further (15 metres less to 33 metres further) | 9.30 (‐14.62 to 33.22) | 187 (1) | ⊕⊕⊝⊝ Lowk | Interventions containing strength training and endurance training may increase 6MWT by 9 metres. MID for the 6MWT (adults with pathology) is typically 14.0 to 30.5m (Bohannon 2017). |
|
| Electrical stimulation | 0 | 0 studies contained a mobility strategy categorised as primarily being electrical stimulation | |||||
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). 6MWT: 6‐Minute Walk Test; CI: confidence interval; MID: minimal important difference; mPPT: modified Physical Performance Test; POMA: Performance Oriented Mobility Assessment; PPME: Physical Performance and Mobility Examination; SMD: standardised mean difference; SPPB: Short Physical Performance Battery; TUG: Timed Up and Go test. | |||||||
| GRADE Working Group grades of evidence High certainty: we are very confident that the true effect lies close to that of the estimate of the effect. Moderate certainty: we are moderately confident in the effect estimate; the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. Low certainty: our confidence in the effect estimate is limited; the true effect may be substantially different from the estimate of the effect. Very low certainty: we have very little confidence in the effect estimate; the true effect is likely to be substantially different from the estimate of effect. | |||||||
aA non‐provision control is defined as no intervention, usual care, sham exercise (the exercise was intended to be a control, or appeared to be of insufficient intensity and progression to have beneficial effects on mobility) or a social visit. bMobility, measuring the ability of a person to move. Scales may measure a number of aspects of mobility (e.g. sit to stand, walking, turning, stairs). A higher score indicates better mobility. cMobility strategies involve postoperative care programmes such as immediate or delayed weight bearing after surgery, and any other mobilisation strategies, such as exercises, physical training and muscle stimulation, used at various stages in rehabilitation, which aim to improve walking and minimise functional impairments. We categorised the exercise and physical training strategies using the Prevention of Falls Network Europe (ProFaNE) guidelines, see Appendix 1. These categories are gait, balance and functional training; strength/resistance training; flexibility; 3D (Tai Chi, dance); general physical activity; endurance; multiple types of exercise; other. Electrical stimulation is an additional intervention type. dNot downgraded for risk of bias (removing studies with high risk of bias in one or more domains had no important impact on results). eCohen's effect size 0.2 is described as small, 0.5 as medium/moderate effect, 0.8 as large effect (Sawilowsky 2009). fDowngraded one level for risk of bias and two levels for imprecision. gDowngraded two levels for imprecision. hDowngraded one level for risk of bias (all studies had high risk of bias for at least one item) and one level for imprecision. iDowngraded one level for risk of bias (removing studies with high risk of bias in one or more domains had an important impact on results) and two levels for imprecision). jDowngraded for imprecision. kDowngraded one level for risk of bias and one level for imprecision.
Background
Description of the condition
Hip fractures, which are fractures of the proximal femur, can be subdivided into intracapsular fractures (those occurring proximal to the attachment of the hip joint capsule to the femur) and extracapsular (those occurring distal to the hip joint capsule). The majority of hip fractures occur in older people with an average age of around 80 years. Females predominate over males by about four to one and the injury is usually the result of a simple fall. This reflects the loss of skeletal strength from osteoporosis. As well as osteoporosis, people experiencing a hip fracture frequently have other medical and physical problems associated with ageing, including impaired mobility and frailty.
Currently, in high‐income nations the majority of hip fractures are treated surgically, which enables earlier mobilisation of the patient and avoids some of the complications of prolonged recumbency and immobilisation. Surgery entails either internal fixation, where the fracture is fixed using various implants and thereby retaining the femoral head, or by replacing the femoral head with a prosthesis.
Although surgery is generally successful, few people recover fully from their hip fracture (Dyer 2016).
Between 5% and 10% of people die within one month of their hip fracture. About one‐third of people will have died by one year after fracture, compared with an expected annual mortality of about 10% in this age group (Roche 2005). Most survivors fail to regain their former levels of mobility and activity, many become more dependent, and 10% to 60% of survivors are unable to return to their previous residence (Magaziner 2000; Royal College of Physicians 2019).
Description of the intervention
A variety of postoperative care programmes following surgery for hip fracture have been employed. In the early stages, these include bed rest and restricted weight bearing. Mobilisation is a major component of postoperative care and rehabilitation. Various mobilisation strategies are in use. These aim to get people out of bed, back on their feet, weight bearing, moving and walking. Other strategies for mobilisation relate to the nature of the physiotherapy or exercise regimens used. These include mobilisation interventions, such as exercise and electrical stimulation of muscles, which aim to minimise impairments (such as reduced strength) and improve the physical performance of walking. Exercise programmes may include one or more types of exercise. The Prevention of Falls Network Europe (ProFaNE) developed a taxonomy that classifies exercise type as: i) balance, gait and functional (task) training; ii) strength/resistance training (including power); iii) flexibility; iv) three‐dimensional (3D) exercise (e.g. Tai Chi, dance, Qigong); v) general physical activity; vi) endurance; and vii) other kinds of exercises (Lamb 2011; Appendix 1). This taxonomy captures how multiple types of exercise can be delivered within an exercise programme.
This review, an update of Handoll 2011, focuses on mobilisation strategies. Thus, this review does not include trials testing interventions, including multi‐component interventions, that aim to enhance outcomes other than mobility. Separate Cochrane Reviews consider other aspects of rehabilitation after hip fracture, including single therapy programmes specifically designed to improve physical and psychosocial functioning (Crotty 2010), multidisciplinary care programmes (Handoll 2009), nutritional supplementation (Avenell 2016), fall prevention (Cameron 2018; Sherrington 2019), and models of care including enhanced rehabilitation strategies designed specifically for people with dementia (Smith 2020).
How the intervention might work
The timing and extent of weight bearing form part of any mobilisation strategy after hip fracture surgery. Other components of mobilisation strategies generally involve various forms of exercise regimens; again, the extent and timing of these will vary. Their aim is to improve people's walking ability and associated functioning. The possibility of a refracture and other complications usually affects the decisions as to when to allow restricted or full weight bearing on the injured hip and the subsequent pace and stages of physical rehabilitation. In particular, following internal fixation of a hip fracture, individuals are at risk of several complications of fracture healing. For example, the implant may fail to hold the fracture or 'cut‐out' of the bone (penetration of the implant from the proximal femur either into the hip joint or external to the femur), causing pain and impaired mobility. This may require revision surgery to re‐fix the fracture, or replace the femoral head with an arthroplasty. Other complications of fracture healing that may occur are non‐union of the fracture (that is, failure of the fracture to heal) and avascular necrosis of the femoral head (also termed segmental collapse or aseptic necrosis).
Different considerations feature in the later stages of rehabilitation, which occur after discharge from hospital and in a community or residential care setting. Mobilisation strategies across the continuum aim to improve the individual's walking ability and associated functioning. However, compared with the in‐hospital setting, there may be a greater emphasis on independent and confident ambulation post‐hospital, with the correct use of ambulatory aids, as well as specific interventions such as muscle strengthening (voluntary and via electrical stimulation) and balance training exercises, that aim to minimise or correct impairments; for example, various impairments may manifest as a limp during walking.
Why it is important to do this review
In 2018, a group of leading professional medical organisations published a global call to action to improve the care of people with fragility fractures (Dreinhofer 2018). This broad‐based and international collaboration identified an urgent need to improve acute and post‐acute care following fragility fracture, plus secondary prevention to prevent further fractures (Dreinhofer 2018). Worldwide, an estimated 1.26 million hip fractures occurred in adults in 1990, with predictions of numbers rising to 6.26 million by the year 2050 (Curtis 2017). The age‐standardised rates of hip fracture are advancing differently among countries (some countries report decreased rates, some increased and some stable (Veronese 2018)). However, given the increasing number of older people worldwide, the total numbers of hip fracture cases and their economic consequences are likely to rise substantially (Sànchez‐Riera 2017). These developments, together with the generally unfavourable outcome in survivors (many of whom become more dependent and move into residential care), mean that the burden on society from hip fractures is immense and increasing.
Mobility is the ability for a person to move within environments, from their home, to their community and beyond (Webber 2010). Improving mobility outcomes is key to relieving the burden on individuals, their carers and society. The previous version of this review noted the insufficiency of the evidence to inform practice, but it also identified ongoing trials that potentially could help address this gap (Handoll 2011). This update continues the systematic review of the evidence on mobilisation strategies for these fractures.
Objectives
To evaluate the effects (benefits and harms) of interventions aimed at improving mobility and physical functioning after hip fracture surgery in adults.
Methods
Criteria for considering studies for this review
Types of studies
We included all randomised controlled trials (including cluster‐randomised controlled trials) comparing different postoperative mobilisation strategies or programmes after surgery to repair an acute hip fracture. We considered for inclusion quasi‐randomised trials (for example, allocation by alternation or date of birth) and trials in which the treatment allocation was inadequately concealed. We included published and unpublished reports; however, we included trials reported only in conference abstracts only if sufficient data were available from correspondence with study authors or from the final report of the trial.
Types of participants
We included trials involving skeletally mature individuals treated for a hip fracture. We included studies in which interventions were commenced for most participants within one year of fracture.
We included trials involving adults who had undergone hip fracture surgery, irrespective of the type of fracture of the proximal femur (e.g. intracapsular or extracapsular), or type of surgery (e.g. internal fixation, hemiarthroplasty, total hip replacement). We did not define specific age limits, but we anticipated that most participants would be aged 65 years and over. Although it may not be specified in all trials, we anticipated the majority of participants would have had a fragility fracture; that is, a low‐energy trauma fracture, such as a fall from a standing height. We included mixed population trials, specifically those also including participants who had elective hip replacement or other lower‐limb fractures, provided the majority were hip fracture patients.
Types of interventions
We included trials of postoperative care programmes, such as immediate or delayed weight bearing after surgery, and any other mobilisation strategies, such as exercises, physical training and electrical stimulation, used at various stages in rehabilitation, which aim to improve walking ability and minimise functional impairments. We excluded trials testing interventions that did not aim specifically to improve mobility, and those testing care programmes, management strategies and other multi‐component interventions that were not solely aimed at mobilisation. All trials testing mobilisation strategies with nutrition as a co‐intervention have been included in updates since 2011 (Handoll 2011).
From 2019, we categorised exercise and physical training strategies using the Prevention of Falls Network Europe (ProFaNE) guidelines (see Appendix 1). These categories are gait, balance and functional training; strength/resistance training; flexibility; 3D (Tai Chi, dance); general physical activity; endurance; other kinds of exercises. We categorised strategies as 'multiple types of exercise' when two or more of the ProFaNE categories were major components of the intervention.
We grouped trials according to the basic stage in the rehabilitation process when the trial intervention(s) commenced: either in‐hospital (where preoperative, operative and postoperative acute and subacute care is undertaken) or post‐hospital (following discharge from in‐hospital care after hip fracture surgery: outpatients, residential care units, nursing homes and community health care centres, as well as an individual’s own home, where rehabilitation is undertaken).
Comparisons
We included trials where the intervention was compared with a control group that received no intervention, usual care, sham exercise (the exercise appeared to be of insufficient intensity and progression to have beneficial effects on mobility) or a social visit. We acknowledge that usual care differs greatly between locations and has changed over time. We also included trials comparing two or more interventions if a) the difference between the intervention and control groups was a mobilisation strategy, or b) if two types of intervention programmes were compared, including the comparison of increased intensity versus standard intensity of intervention, within the same setting and same type of intervention.
In the in‐hospital setting, we considered the following main comparisons for people after surgery for a hip fracture.
Provision of any specific mobilisation strategy or programme and non‐provision, where the non‐provision control is defined as usual orthopaedic, medical care or allied health care.
-
Different mobilisation strategies or programmes such as:
early (e.g. day of or day following surgery) versus late mobilisation, within the same setting and type of exercise;
programmes of different intensity, within the same setting and type of exercise;
programmes with different components; for example, different types of exercise (weight‐bearing versus non‐weight‐bearing exercises).
In studies conducted entirely in the post‐hospital (outpatient and community) setting, we considered the following main comparisons for people after surgery for a hip fracture who had been discharged from in‐hospital care.
Provision of any specific mobilisation strategy or programme and non‐provision, where the non‐provision control is defined as no intervention, usual care, sham exercise (where the exercise was intended to be a control, or appeared to be of insufficient intensity and progression to have beneficial effects on mobility) or a social visit.
-
Different mobilisation strategies or programmes for people such as:
programmes of different intensity, within the same setting and type of exercise;
programmes with different components; for example, different types of exercise (aerobic versus resistance).
Types of outcome measures
While the outcomes we sought remained largely unchanged from the previous version (see Handoll 2011), we restructured the types of outcome measures into three categories, according to the Grading of Recommendations Assessment, Development, and Evaluation (GRADE) system guidance: a) the seven 'critical' or main outcomes for presentation, where appropriate, in summary of findings tables; b) other 'important' outcomes; and c) economic and resource outcomes. We made these changes to align with updates to related Cochrane Reviews in hip fracture (we elaborate on the changes in Differences between protocol and review). The outcomes also align with the core outcome set for hip fracture trials (Haywood 2014; Smith 2019).
As noted above, the main focus of the interventions tested in this review is to safely restore or, better still, enhance mobility and physical functioning. Such interventions and outcome assessment can apply to the whole rehabilitation period. We describe the outcomes in more detail in Appendix 2.
The main outcomes include one time point from each study. For in‐hospital studies with outcomes measured at multiple time points, we focused on an interim outcome at approximately four months. It has been established that quality of life and poor outcome (defined as death or deterioration in residential status) are likely to be consistent at four months and 12 months (Griffin 2015). Where an outcome was not measured at four months, we used the nearest outcome to four months. For post‐hospital studies, we used the time point closest to the end of the intervention period.
Main or 'critical' outcomes
We selected the following main or 'critical' outcomes for presentation in summary of findings tables and other summary sections of the review.
For each outcome, we planned pooled analysis of one outcome measure per study. For studies with outcomes measured at multiple time points, we used the outcome measured at the time point closest to four months (in‐hospital studies) or the time point closest to the end of the intervention period (outpatient and community studies), unless specified below. We did not include outcomes collected at different time points for a single trial.
Mobility. The order of priority was broad mobility measures (i.e. scales seeking to measure a number of aspects of mobility, such as the Short Physical Performance Battery, Timed Up and Go test, Elderly Mobility Scale, Parker Mobility Score), followed by endurance walking measures over a longer distance (e.g. 6‐Minute Walk Test). We prioritised continuous outcomes over dichotomous ones, and objective measures over self‐reported measures.
Walking speed. Using observed gait measures, the order of priority was 10‐Metre Walk Test then 6‐Metre Walk Test. We gave preference to fast walk and used usual speed walk if no fast walk was reported.
Functioning. We used measures of functioning, prioritising continuous outcomes over dichotomous ones, and objective measures over self‐reported measures.
Health‐related quality of life measures (e.g. 36‐item Short Form Health Survey (SF‐36), EQ‐5D). We prioritised the more commonly measured SF‐36 and EQ‐5D. We prioritised the time point closest to four months; however, we considered how mortality was reported and the availability of death‐adjusted estimates (Parsons 2018).
Mortality (all cause): short term (around four months, but we also accepted at‐discharge data) and long term (around 12 months).
-
Adverse effects. We prioritised the number of events; however, if these data were unavailable, we reported the number of people experiencing one or more of the following, at final follow‐up:
re‐admission
re‐operation (unplanned return to operating theatre)
surgical complications of fixation within the follow‐up period of the study
avascular necrosis
non‐union of the fracture (the definition of non‐union is that used within each individual study, and this outcome includes early re‐displacement of the fracture)
other complications (e.g. thromboembolic complications (deep vein thrombosis or pulmonary embolism))
falls (rate of falls or number of people who fell).
pain (persistent hip or lower‐limb pain at the final follow‐up assessment): verbal rating or visual analogue score (VAS).
Return to living at pre‐fracture residence (home), for in‐hospital studies. Timing between four and 12 months.
Other important outcomes
The following list summarises other important outcomes presented in this review. These outcomes include individual categories of the mobility measures (walking (aid and subjective measures), balance, sit to stand).
-
Mobility: walking
use of walking aids / need for assistance
self‐reported measures (e.g. difficulty walking 400 metres)
-
Mobility: balance while standing, reaching and stepping
observed balance measures (e.g. functional reach, step test, timed tandem stance)
self‐reported balance measures
-
Mobility: sit to stand
observed sit to stand measures (e.g. timed sit to stand)
Muscle strength (of the affected leg; priority for quadriceps strength)
Activities of daily living (e.g. Barthel Index, Functional Independence Measure)
Patient‐reported measures of lower‐limb or hip function (e.g. Hip Rating Questionnaire, Harris Hip Score, Oxford Hip Score, Merle D’Aubigne Hip Score)
-
Participant satisfaction
acceptability of interventions
adherence
Economic and resource outcomes
We summarised any economic analyses reported by the included trials. We reviewed each trial report for costs and resource data that would enable economic evaluation. The resources considered depended on the context and stage of rehabilitation; these included:
length of hospital stay (in days);
number of physiotherapy sessions;
number of outpatient attendances; and
need for special care.
Search methods for identification of studies
Electronic searches
We searched the Cochrane Bone, Joint and Muscle Trauma Group Specialised Register (10 March 2021), the Cochrane Central Register of Controlled Trials (CENTRAL) (10 March 2021, Issue 3), MEDLINE (Ovid MEDLINE 1946 to 9 March 2021), Embase (Ovid 1974 to 10 March 2021 Week 09), Cumulative Index to Nursing and Allied Health Literature (CINAHL) (EBSCO 1982 to 10 March 2021) and the Physiotherapy Evidence Database (PEDro) (2010 to 10 March 2021). For this update, we limited the search results for MEDLINE, Embase and CINAHL from 2010 onwards. No language or publication restrictions were applied.
In MEDLINE, we combined the subject‐specific terms with the sensitivity‐maximising version of the Cochrane Highly Sensitive Search Strategy for identifying randomised trials (Lefebvre 2019) (Appendix 3). Search strategies for CENTRAL, EMBASE, and CINAHL can also be found in Appendix 3.
We also searched the World Health Organization (WHO) International Clinical Trials Registry Platform Search Portal (ICTRP) (10 March 2021) and ClinicalTrials.gov (10 March 2021) to identify ongoing and recently completed trials (Appendix 3).
Searching other resources
We checked reference lists of articles and contacted study authors.
Data collection and analysis
Selection of studies
For this update, SD, NF or WK conducted initial scrutiny of electronic database downloads. SD, NF, JD and WK independently performed study selection from lists of potentially eligible trials provided by the Trials Search Co‐ordinator of the Cochrane Bone, Joint and Muscle Trauma Group; and subsequently from full reports where doubts remained. Trial selection was by consensus and discussion with CS as necessary.
Data extraction and management
At least two review authors independently extracted trial information and data, using a pre‐piloted data extraction form. We resolved differences through discussion. Review authors were not blinded to study authors and sources. Review authors did not assess their own trials.
We recorded the following items using a standardised data extraction form.
General information: study author’s name and year; study ID; citation of paper; trial registration, period of study (dates) and specified primary outcomes.
-
Trial details: trial design; sample size; location; setting.
-
Setting was described as:
In‐patient settings where preoperative, operative and postoperative acute and subacute care is undertaken.
Post‐hospital settings, including residential care units, nursing homes and community health care centres, hospital outpatient clinics, as well as an individual’s own home, where rehabilitation is undertaken.
-
Inclusion and exclusion criteria (noting whether there was exclusion for cognitive impairment, dementia or delirium); comparability of groups; length of follow‐up; stratification; and funding source.
Risk of bias assessment and justification for judgements: sequence generation; allocation concealment; blinding (participants, personnel), blinding (outcome assessors); incomplete outcome data; and selective outcome reporting.
Characteristics of participants: age; gender; pre‐fracture mobility (prior use of walking aids versus not); other conditions/illnesses; type of fracture (intracapsular versus extracapsular fractures); mental status, treatment received; the number randomised, analysed and lost to follow‐up; and dropouts in each arm (with reasons).
Interventions: experimental and control interventions; details of intervention programme (stage of rehabilitation, content, duration, frequency, intensity and individual‐ or group‐based delivery, level of supervision, instructor:participant ratio); timing of intervention; uptake of intervention (acceptance of intervention), whether studies assessed adherence (compliance) with interventions and associated data (e.g. number of sessions attended); and additional co‐interventions (such as motivational strategies, additional information or support given to participants); expertise of personnel delivering intervention (expert health provider (e.g. therapist) versus personnel not specified as an expert, their role, timing).
Details of review outcomes (Types of outcome measures) to include time of measurement and type of measurement tool (including direction of scales where appropriate).
We assessed five aspects of trial design and reporting that would help us judge the applicability of the trial findings. The five aspects were: definition of the study population; description of the interventions; description of outcome measures; length of follow‐up; and assessment of compliance/adherence with interventions.
Assessment of risk of bias in included studies
At least two review authors independently assessed risk of bias in newly included studies, without masking of the source and authorship. At least one review author assessed risk of bias for trials that had been assessed in previous versions of the review. We piloted the assessment form on two trials. We resolved all differences through discussion. We used the tool outlined in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011). This tool incorporates the following domains:
sequence generation (selection bias);
allocation concealment (selection bias);
blinding of participants and personnel (performance bias);
blinding of outcome assessors (detection bias);
incomplete outcome data (attrition bias);
selective reporting (reporting bias);
other risks of bias.
During assessment of detection bias and attrition bias, we considered three different types of outcomes separately: i) observer‐reported outcomes involving some judgement (mobility, walking speed, functional outcomes, activities of daily living and strength); ii) observer‐reported outcomes not involving judgement (death, re‐admission, re‐operation, surgical complications, return to living at home); iii) participant/proxy‐reported outcomes (health‐related quality of life, pain, falls, patient‐reported questionnaires, satisfaction).
When considering blinding (detection bias) for staff‐reported (in‐hospital studies) and self‐reported (in‐hospital and post‐hospital studies) outcomes of health‐related quality of life, pain, falls, patient‐reported questionnaires and satisfaction, we recognised that some risk of bias is inherent. However, it can be minimised by blinding of research staff and statisticians involved in data collection and analysis, and we made an assessment on the basis of these factors. If data collection and analysis were not performed by blinded research staff, we considered the risk of bias to be high. If data collection and analysis were performed by blinded research staff, we considered the risk of bias to be unclear.
For 'other bias', we assessed four additional sources of bias: bias resulting from imbalances in key baseline characteristics (e.g. pre‐injury mobility, mental test score, type of surgery); performance bias such as that resulting from lack of comparability in the experience of care providers; bias relating to the recall of falls due to unreliable methods of ascertainment; and bias relating to cluster‐randomised trials. For trials using cluster‐randomisation, we considered additional risk of bias relating to recruitment, baseline imbalance, loss of clusters, incorrect analysis and comparability with individually‐randomised trials, as described in Chapter 23 of the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2021b).
Measures of treatment effect
We calculated risk ratios or rate ratios (for falls) and 95% confidence intervals (CI) for dichotomous outcomes; standardised mean differences (SMD) and 95% confidence intervals for continuous outcomes where different scales were pooled; and mean differences and 95% confidence intervals for continuous outcomes where a single scale was pooled. We present final values rather than change scores for continuous outcomes.
To facilitate interpretation of the mobility and functioning outcomes, where investigators measured outcomes using different instruments, we expressed SMD in the units of one of the measurement instruments used by the included studies. Using the approach suggested by Schünemann 2022, we calculated the absolute difference in means by multiplying the SMD by an estimate of the standard deviation (SD) associated with the most familiar instrument. We obtained this SD by calculating a weighted pre‐intervention average across all intervention groups of all studies that used the selected instrument. We compared the summary effect, re‐expressed in the original units of that particular instrument, with the minimal important difference, when this was available. During analysis of mobility outcome according to the different types of exercise interventions, we re‐expressed SMD in the units of one of the measurement instruments only when the between‐group difference was statistically significant.
Unit of analysis issues
We included one cluster‐randomised trial (Pol 2019). The study authors adjusted for clustering in the analysis. No trials reported the inclusion of people with bilateral hip fractures.
All participants in Sylliaas 2012 were previously in the intervention arm of an earlier study included in this review (Sylliaas 2011). As a result, we did not include data from Sylliaas 2012 in the analyses of intervention effect.
Dealing with missing data
We contacted trial authors to request missing data. Where possible, we performed intention‐to‐treat analyses to include all people randomised. However, we used actual denominators of participants contributing data to the relevant outcome assessments where dropouts were identified. We were alert to the potential mislabelling or non‐identification of standard errors and standard deviations. Unless we could derive missing standard deviations from confidence intervals or standard errors, we did not assume values in order to present these in the analyses.
Assessment of heterogeneity
Where study interventions were considered sufficiently similar to be combined in meta‐analyses, we assessed heterogeneity of treatment effects by visual inspection of forest plots along with consideration of the Chi² test (with a significance level at P < 0.10) and the I² statistic for statistical heterogeneity, in conjunction with likely causes of clinical heterogeneity. We based our interpretation of the I² results on that suggested by Higgins 2011: 0% to 40% might not be important; 30% to 60% may represent moderate heterogeneity; 50% to 90% may represent substantial heterogeneity; and 75% to 100% may represent considerable heterogeneity.
Assessment of reporting biases
There were insufficient trials and data for the assessment of reporting biases. Our search of clinical trial registers has the potential to reduce the impact of publication bias, especially in the future. For individual trials, we checked all publications and trial registration details where available to assess completeness and consistency in outcome reporting. For outcomes that included more than 10 data points, we constructed and visually inspected funnel plots.
Data synthesis
During pooling, we initially pooled the results of comparable groups of trials using a fixed‐effect model and 95% confidence intervals. Where there was substantial heterogeneity between the results of individual trials, and/or when considered appropriate, we viewed and presented the results of pooling studies using a random‐effects model instead of those from the fixed‐effect model. Where scales within a meta‐analysis were contrary (i.e. a higher score indicating better performance versus a higher score indicating worse performance), we multiplied by ‐1 to invert scales for consistency with other trial outcomes (Sambunkak 2017).
Included studies measured the mobility outcome using a range of instruments, not all of which could be combined in meta‐analysis. We undertook separate meta‐analyses for the mobility scales (continuous outcome), the Timed Up and Go test (measured in seconds), and the 6‐Minute Walk Test (measured in metres).
Some studies reported data for the same outcome using more than one measurement tool. To avoid a unit of analysis error, we used data from only one tool. However, because we were concerned that we would lose information, we also presented analyses for the mobility outcome with the results separated according to the types of measurement tool; this allowed a study to contribute to multiple outcome measures.
In the summary of findings tables, we presented adverse events in terms of hospital re‐admissions. Pooling of the different types of adverse events was not appropriate as some outcomes were subsets of others, some were too dissimilar and the denominators of reported results were often unclear.
Our interpretations of continuous outcomes were based upon guiding rules for interpreting SMDs (‘Cohen’s effect sizes’ (Cohen 1998)), or expressed in the units of a specific measurement instrument where appropriate.
Subgroup analysis and investigation of heterogeneity
Where appropriate and depending on whether sufficient studies were available, we planned the following subgroup analyses.
Trials excluding participants with cognitive impairment, dementia or delirium versus trials not excluding participants based upon cognition
Secondary and social care, with intervention delivered in home and community, versus intervention delivered in outpatient clinics, for post‐hospital interventions
Expertise (expert health provider (e.g. therapist) versus personnel not specified as an expert), for post‐hospital interventions
In‐hospital ward versus rehabilitation ward
Mean age ≤ 80 years versus mean age > 80 years.
We undertook subgroup analyses for each outcome, where there were ten or more studies in the analysis.
We investigated whether the results of subgroups were significantly different by inspecting the overlap of CIs and performing the test for subgroup differences available in Review Manager 5.4 (Review Manager 2020).
We performed subgroup analysis of secondary and social care (interventions delivered in the home and community) versus outpatient care (interventions delivered in the outpatient setting) in the post‐hospital setting.
Our prespecified subgroup analysis by expert versus non‐expert delivery of intervention was not possible. We assumed all interventions were delivered by experts in the in‐hospital setting. The three post‐hospital studies that did not have experts deliver the intervention did not contribute to the main outcomes, so these subgroup analyses could not be conducted.
Sensitivity analysis
We conducted our prespecified sensitivity analyses for the mobility outcome, measured using mobility scales. The sensitivity analyses included assessing the effect of excluding trials at high or unclear risk of bias associated with a lack of allocation concealment; trials at high risk of bias on any domain; trials reported only in conference abstracts; trials that included mixed populations; trials that did not clearly focus on or predominantly include the target population of people with a fragility fracture resulting from low‐energy trauma; and in‐hospital trials that measured outcomes at the end of the in‐hospital phase (the usual time point used in analyses was that closest to four months). We undertook post hoc sensitivity analysis to examine the impact on the results of the use of fixed‐effect rather than random‐effects models for data pooling for the mobility outcome.
Summary of findings and assessment of the certainty of the evidence
We used the GRADE approach to assess the certainty of evidence related to all critical outcomes listed in the Types of outcome measures (Schünemann 2017). We assessed the certainty of the evidence as ‘high’, ‘moderate’, ‘low’ or ‘very low’ depending on the presence and extent of five factors: risk of bias; inconsistency of effect; indirectness; imprecision; and publication bias.
Risk of bias. We downgraded by one level due to risk of bias when either all studies had high risk of bias in one or more domains or removing studies with high risk of bias in one or more domains had a marked impact on results. We did not downgrade for risk of bias where removing studies with high risk of bias in one or more domains changed the point estimate to a stronger effect with or without narrower confidence intervals (CI). We did not consider risk of bias domains that were not related to the outcome of interest (e.g. domains related to falls when evaluating GRADE for mortality).
Inconsistency. We downgraded for inconsistency where there was significant heterogeneity (I2 exceeded 60%) that could not be explained.
Indirectness. We downgraded for indirectness where trials examined a limited version of the main review question with regard to population, intervention, comparison or outcomes.
Imprecision. We downgraded for imprecision when there were fewer than 400 participants for continuous outcomes, fewer than 300 events for dichotomous outcomes, the CI was wide or the CI crossed zero and estimates of clinically important effect.
Publication bias. For outcomes that included more than 10 data points, we constructed and visually inspected funnel plots.
We prepared summary of finding tables featuring the 'critical' outcomes for the intervention versus control comparison, for the in‐hospital setting and post‐hospital setting. For adverse events, we reported re‐admission to hospital. We also prepared summary of finding tables featuring the mobility outcome for the intervention versus control comparison, for different types of exercise and electrical stimulation, for the in‐hospital setting and post‐hospital setting. We used standardised qualitative statements to describe the different combinations of effect size and the certainty of evidence (Cochrane Norway 2017). Our illustrative risks for dichotomous outcomes were based on the proportion calculated from the number of people who experienced the event divided by the number of people in the group, for those trials included in the analysis for that outcome.
In addition, we also applied GRADE to the mobility outcome when analysed according to the different types of exercise interventions, and we prepared bespoke summary of findings tables to summarise the effect sizes and describe the certainty of this evidence. We applied GRADE to other important outcomes in all comparison groups when the between‐group difference in treatment effect was statistically significant.
Results
Description of studies
Results of the search
For this update (January 2010 to March 2021), we screened a total of 3424 records from the following databases: the Cochrane Bone, Joint and Muscle Trauma Group Specialised Register (10); CENTRAL (561), MEDLINE (401), Embase (1190), CINAHL (252), PEDro (125), the WHO International Clinical Trials Registry Platform (361) and ClinicalTrials.gov (524). We also found 35 potentially eligible studies from other sources.
We identified a total of 62 new studies (127 reports) potentially eligible for inclusion, and obtained full reports of these, where possible. After full‐text review, we included 21 new studies (see Characteristics of included studies), excluded 18 (Excluded studies), and classified 21 as ongoing studies (Ongoing studies). Two studies await classification (Studies awaiting classification). A flow diagram summarising the study selection process is shown in Figure 1.
1.
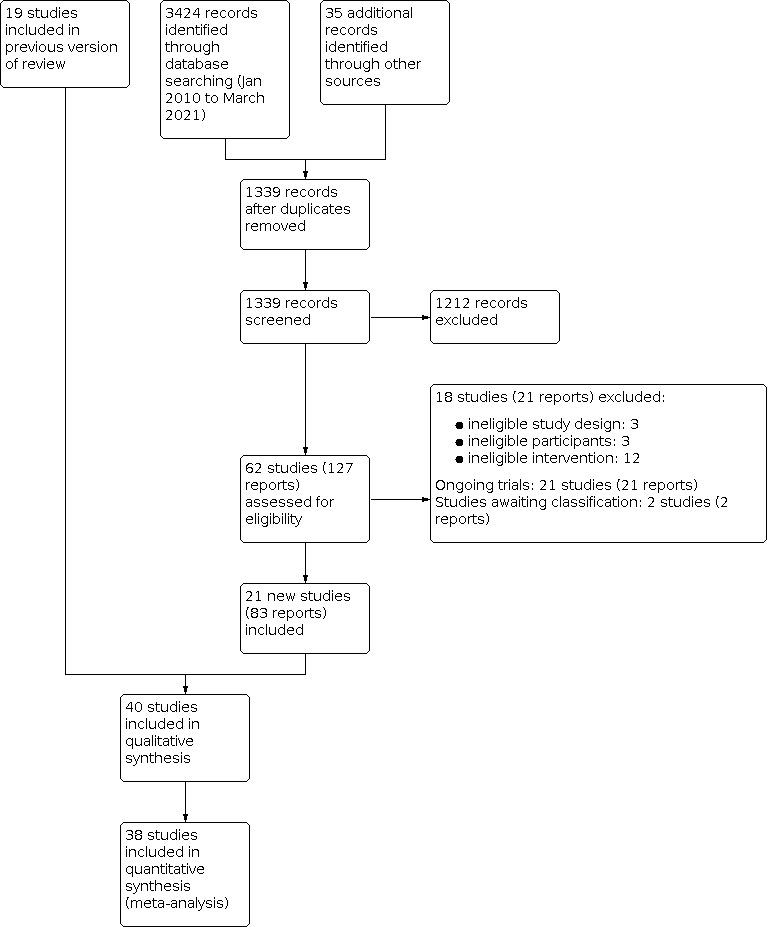
Study flow diagram
Overall, there are now 40 included studies, 18 excluded studies, two studies awaiting classification and 21 ongoing trials.
The results from the previous searches (up to April 2010) are shown in Appendix 4. Three ongoing studies from Handoll 2011 have been included in this update (Kronborg 2017, previously Kristensen 2009, NCT00848913; Latham 2014, previously Jette 2008, NCT00592813; Salpakoski 2015, previously Sipila 2011, ISRCTN53680197). The 22 excluded studies in Handoll 2011 are not reported in the update.
Included studies
This review now includes 40 trials with 4059 participants. Details are provided in the Characteristics of included studies and are summarised briefly below. Due to the size of the review, we have not inserted links to all study references in the following description, but full details can be viewed in Appendix 5. We have summarised characteristics of the included studies in Table 5 and Table 6.
1. Key characteristics of participants and intervention approach.
| Study ID | Age (mean) | % women | Gait speed in control group at follow‐up (m/s) | Duration of intervention (weeks) | Type of intervention (ProFaNE) | Intervention delivered by expert health provider | Exclusion criterion based on impaired cognition |
| Baker 1991 | 84 | 100% | 0.43 | Not specified | Balance, gait & functional | Yes | No |
| Binder 2004 | 80 | 74% | 0.99 | 24 | Balance, gait & functional; resistance | Yes | Yes |
| Bischoff‐Ferrari 2010 | 84 | 79% | NR | 52 | Balance, gait & functional | Yes | Yes |
| Braid 2008 | 81 | 92% | NR | 6 | Electrical stimulation | Yes | Yes |
| Gorodetskyi 2007 | 71 | 67% | NR | 1.5 | Electrical stimulation | Yes | No |
| Graham 1968 | NR | NR | NR | Early WB v late WB | Balance, gait & functional | Unclear | No |
| Hauer 2002 | 81 | 100% | 0.44 | 12 | Balance, gait & functional; resistance | Unclear | Yes |
| Karumo 1977 | 73 | 75% | NR | 4.7 | Balance, gait & functional | Yes | No |
| Kimmel 2016 | 81 | 64% | NR | 1 | Balance, gait & functional | Yes | No |
| Kronborg 2017 | 80 | 77% | NR | 10 days (or discharge, if discharged prior) | Resistance | Yes | Yes |
| Lamb 2002 | 84 | 100% | 0.43 | 6 | Electrical stimulation | No | Yes |
| Langford 2015 | 83 | 63% | 0.83 | 16 | Other (telephone support and coaching) | Yes | Yes |
| Latham 2014 | 78 | 69% | NR | 24 | Balance, gait & functional | Yes | Yes |
| Lauridsen 2002 | 80 | 100% | NR | 2 | Balance, gait & functional | Yes | No |
| Magaziner 2019 | 81 | 77% | 0.74 | 16 | Resistance; endurance | Yes | No |
| Mangione 2005 | 79 | 73% | 0.65 | 12 | Resistance; endurance | Yes | Yes |
| Mangione 2010 | 81 | 81% | 0.91 | 10 | Resistance | Yes | Yes |
| Miller 2006 | 84 | 77% | 0.5 | 12 | Resistance | Yes | Yes |
| Mitchell 2001 | 80 | 84% | 0.42 | 6 | Balance, gait & functional; resistance | Unclear | Yes |
| Monticone 2018 | 77 | 71% | NR | 3 | Balance, gait & functional | Yes | Yes |
| Moseley 2009 | 84 | 81% | 0.6 | 16 | Balance, gait & functional | Yes | Yes |
| Oh 2020 | 79 | 68% | NR | 2 | Balance, gait & functional | Yes | Yesa |
| Ohoka 2015 | 90 | 100% | 0.35 | 12 | Balance, gait & functional | Yes | No |
| Oldmeadow 2006 | 79 | 68% | NR | 1 | Balance, gait & functional | Yes | No |
| Orwig 2011 | 82 | 100% | NR | 52 | Resistance; endurance; other (self‐efficacy‐based motivational component) | No | Yes |
| Pol 2019 | 80 | 89% | NR | 12 | Other (cognitive behavioural therapy (CBT), CBT plus sensory monitoring) | Yes | No |
| Resnick 2007 | 81 | 100% | NR | 52 | Resistance; endurance; other (motivational interventions) | No | Yes |
| Salpakoski 2015 | 80 | 78% | 0.97 | 52 | Balance, gait & functional | Yes | Yes |
| Sherrington 1997 | 79 | 79% | 0.5 | 4 | Balance, gait & functional | Yes | Yes |
| Sherrington 2003 | 81 | 68% | 0.19 | 2 | Balance, gait & functional | Yes | Yes |
|
Sherrington 2004 (WB group; NWB group) |
79 | 80% | 0.55; 0.62 | 16 | Balance, gait & functional; other (specific group of muscle contractions in supine) | Yes | Yes |
| Sherrington 2020 | 78 | 76% | 0.83 | 52 | Balance, gait & functional | Yes | Yes |
| Stasi 2019 | 78 | 75% | NR | 12 | Resistance | Yes | No |
| Suwanpasu 2014 | 75 | 66% | NR | 6 | Other (physical activity enhancing program, based on Resnick's self‐efficacy model) | No | No |
| Sylliaas 2011 | 82 | 83% | 0.51 | 12 | Resistance | Yes | Yes |
| Sylliaas 2012 | 82 | 81% | 0.8 | 12 | Resistance | Yes | Yes |
| Taraldsen 2019 | 83 | 77% | 0.62 | 10 | Balance, gait & functional | Yes | No |
| Tsauo 2005 | 73 | 80% | 0.33 | 12 | Balance, gait & functional | Yes | Yes |
| Van Ooijen 2016 | 83 | 73% | 0.72 | 6 | Balance, gait & functional | Yes | Yes |
| Williams 2016 | 79 | 75% | 0.8 | 12 | Balance, gait & functional; other (workbook and goal setting diary) | Yes | Yes |
NR: not reported; NWB: non‐weight bearing; WB: weight bearing aParticipants with severe cognitive dysfunction (obey command ≤ 1 step ) were excluded. At baseline, 21/38 participants had cognitive dysfunction, defined using Mini‐Mental State Examination score adjusted with age and education level.
2. Study design, length of follow‐up, setting and trial size.
| Study ID | Setting | Length of follow‐up (months) | No. randomised | No. analysed | % lost to follow‐up |
| Baker 1991 | Inpatient | Until discharge from hospital | 40 | 40 | 0% |
| Binder 2004 | Post‐hospital | 6 | 90 | 80 | 11% |
| Bischoff‐Ferrari 2010 | Post‐hospital | 12 | 173 | 128 | 26% |
| Braid 2008 | Inpatienta | 3.5 | 26 | 18 | 31% |
| Gorodetskyi 2007 | Inpatient | 10 days | 60 | 60 | 0% |
| Graham 1968 | Inpatient | 12 | 273 | 212 | 22% |
| Hauer 2002 | Post‐hospital | 6 | 28 | 24 | 14% |
| Karumo 1977 | Inpatient | 3 | 100 | 87 | 13% |
| Kimmel 2016 | Inpatient | 6 | 92 | 92 | 0% |
| Kronborg 2017 | Inpatient | 10 days | 90 | 74 | 18% |
| Lamb 2002 | Inpatienta | 3 | 27 | 24 | 11% |
| Langford 2015 | Post‐hospitalb | 4 months | 30 | 26 | 13% |
| Latham 2014 | Post‐hospital | 9 | 232 | 195 | 16% |
| Lauridsen 2002 | Inpatient | Until discharge from hospital | 88 | 60 | 32% |
| Magaziner 2019 | Post‐hospital | 4 | 201 | 187 | 7% |
| Mangione 2005c | Post‐hospital | 3 | 41 | 33 | 20% |
| Mangione 2010 | Post‐hospital | 12 | 26 | 26 | 0% |
| Miller 2006c | Inpatienta | 3 | 63 | 63 | 0% |
| Mitchell 2001 | Inpatient | 4 | 80 | 44 | 45% |
| Monticone 2018 | Inpatienta | 12 (3 weeks used in analysis) | 52 | 52 | 0% |
| Moseley 2009 | Inpatienta | 4 | 160 | 150 | 6% |
| Oh 2020 | Inpatient | 6 | 45 | 41 | 16% |
| Ohoka 2015 | Inpatient | 3 | 27 | 18 | 33% |
| Oldmeadow 2006 | Inpatient | 0.25 | 60 | 60 | 0% |
| Orwig 2011 | Post‐hospital | 12 | 180 | 180 | 0% |
| Pol 2019c,d | Post‐hospital | 4 | 240 | 151 | 37% |
| Resnick 2007c | Post‐hospital | 12 | 155 | 113 | 27% |
| Salpakoski 2015 | Post‐hospital | 12 | 81 | 75 | 7% |
| Sherrington 1997 | Post‐hospital | 1 | 44 | 40 | 9% |
| Sherrington 2003 | Inpatient | 0.5 | 80 | 77 | 4% |
| Sherrington 2004c | Post‐hospital | 4 | 120 | 105 | 13% |
| Sherrington 2020 | Post‐hospital | 12 | 336 | 159 | 53% |
| Stasi 2019 | Post‐hospitalb | 3 | 100 | 96 | 4% |
| Suwanpasu 2014 | Post‐hospital | 1.5 | 46 | 46 | 0% |
| Sylliaas 2011 | Post‐hospital | 3 | 150 | 150 | 0% |
| Sylliaas 2012 | Post‐hospital | 3 | 95 | 90 | 5% |
| Taraldsen 2019 | Post‐hospital | 2 | 143 | 123 | 14% |
| Tsauo 2005 | Post‐hospital | 3 | 54 | 25 | 54% |
| Van Ooijen 2016c | Inpatient | 13 (4 weeks used in analysis) | 70 | 51 | 27% |
| Williams 2016 | Post‐hospital | 3 | 61 | 24 | 61% |
aIntervention delivered in hospital and after discharge. Majority of intervention delivered in inpatient setting bIntervention started as inpatient. Majority of intervention delivered in post‐hospital setting cThree study arms dCluster‐randomised trial
Thirty‐nine included trials were published as full reports in journals; one trial was published as an abstract with additional information provided by study authors (Ohoka 2015). The publication dates range from 1968 (Graham 1968) to 2020 (Oh 2020; Sherrington 2020). Two studies did not contribute any outcomes to this review: Suwanpasu 2014 included no outcomes of interest, while participants in Sylliaas 2012 were a subset of those in Sylliaas 2011.
We included 21 new trials, with a total of 2470 participants, in this update. Six were in‐hospital trials (Kimmel 2016; Kronborg 2017; Monticone 2018; Oh 2020; Ohoka 2015; Van Ooijen 2016), 14 were community rehabilitation trials (Bischoff‐Ferrari 2010; Langford 2015; Latham 2014; Magaziner 2019; Mangione 2010; Orwig 2011; Pol 2019; Salpakoski 2015; Sherrington 2020; Stasi 2019; Sylliaas 2011; Sylliaas 2012; Taraldsen 2019; Williams 2016), and one trial did not explicitly report how the intervention was delivered (Suwanpasu 2014).
Twenty‐seven of the included studies received funding, primarily from governmental, university and professional research funding bodies. The Van Ooijen 2016 trial was funded by the company, affiliated with two authors, that manufactured and patented the treadmills used in the intervention.
Design
Thirty‐eight trials were randomised controlled trials, although two of these provided no details of their method of randomisation (Graham 1968; Tsauo 2005), and thus the use of quasi‐randomised methods for sequence generation cannot be ruled out. Baker 1991 was a quasi‐randomised trial using alternation for treatment allocation. Bischoff‐Ferrari 2010 was a 2x2 factorial design but we included only two trial arms in this review. Pol 2019 was a three‐arm, stepped‐wedge cluster‐randomised trial. Thirty‐three trials had two comparison groups; four trials had three comparison groups (Mangione 2005; Sherrington 2004; Pol 2019; Van Ooijen 2016); and two trials had four comparison groups (Miller 2006; Resnick 2007). Of the latter two studies, we included only three groups from each study in the review.
In Table 7, we show our assessment of five aspects of trial design and reporting, to facilitate judgement of the applicability of the trial findings. The majority of studies (37/40) defined the study population; most studies (33/40) described the interventions (seven studies did not adequately describe the intervention dosage or usual care); and most (36/40) described outcome measures. Length of follow‐up exceeded six months in 16/40 trials, with trials in the in‐hospital setting generally having shorter follow‐up than those conducted after discharge. Compliance or adherence to interventions was reported in less than half (16/40) of included trails.
3. Assessment of items relating to applicability of trial findings.
| Clearly defined study population? | Interventions sufficiently described? | Main outcomes sufficiently described? | Appropriate timing of outcome measurement? (Yes ≥ 6 months) | Assessment of compliance with interventions | |
| Baker 1991 | Yes | Partial: frequency and intensity of gait retraining not described | Yes | No: only followed up until discharge: mean stay in rehabilitation hospital for intervention group was 54 days. | No: although mention of treadmill participants aiming to exceed previous performance on the treadmill |
| Binder 2004 | Yes | Yes | Yes | Partial: although 6 months follow‐up, it was only until the end of the intervention. | Yes: in both groups |
| Bischoff‐Ferrari 2010 | Yes | Yes | Yes | Yes | Yes |
| Braid 2008 | Yes | Partial: usual post‐discharge physiotherapy not described | Yes | Partial: 14 weeks. Intervention ended after 6 weeks. | Partial: compliance and tolerance to electrical stimulation only reported for intervention group |
| Gorodetskyi 2007 | Yes | Yes | Yes (although limited) | No: 10 days marking end of treatment. | Yes: it is stated that intervention was received by all participants |
| Graham 1968 | Partial: inadequate description; excluded post‐randomisation if unsuitable to walk at 2 weeks | Partial: little description of rehabilitation | Partial: no record of mobility outcomes | Yes: 1 year | No |
| Hauer 2002 | Yes | Yes | Partial: however, clarification on some outcome measures was obtained via contact with trial author | Yes: 6 months (3 months after the end of the intervention). Two year follow‐up results reported for whole study population | Yes: in both groups |
| Karumo 1977 | Partial: no mention of exclusion criteria. Though the inclusion criteria were a displaced femoral neck fracture, the implants used for some participants (9 Jewett nails, 1 Rush nail, 1 Kuntscher nail) suggest that some extracapsular fractures were included. | Yes | Partial: incomplete descriptions | No: 9 weeks only for function (3 months for mortality) | No |
| Kimmel 2016 | Yes | Yes | Yes | No: length of follow‐up is Day 5 or discharge if discharged before Day 5 | No |
| Kronborg 2017 | Yes | Yes | Yes | No: 10 days or discharge if sooner | Yes: in both groups |
| Lamb 2002 | Yes | Yes | Yes | Partial: 13 weeks from surgery. | Yes: “All of the women used their stimulators for more than 75% of the cumulative time requested” |
| Langford 2015 | Yes | Yes | Yes | Partial | No |
| Latham 2014 | Yes | Yes | Yes | Partial: 9 months | Yes: compliance with interventions assessed: "adherence was 98%” |
| Lauridsen 2002 | Yes | Yes | Yes | No: primary outcome = length of training period; otherwise until discharge | Yes: in terms of the interventions (although not the components) |
| Magaziner 2019 | Yes | Yes | Yes | Partial: 40 weeks | Yes |
| Mangione 2005 | Yes | Yes | Yes | No: 12 weeks for the two intervention groups but 8 weeks only for the control group. | Partial: only compliance of the intervention groups recorded |
| Mangione 2010 | Yes | Yes | Yes | Partial: majority followed up for 16 weeks | Yes |
| Miller 2006 | Yes | Yes | Yes | Partial: 12 weeks only for mobility outcomes. One year follow‐up data for mortality, re‐admissions and admission to higher level of care | Partial: only compliance of the intervention groups recorded |
| Mitchell 2001 | Yes | Yes | Yes | Partial: 16 weeks follow‐up. Intervention ended at 6 weeks | Partial: only compliance with intervention recorded |
| Monticone 2018 | Yes | Partial: dosage about open kinetic chain exercises in the control group not described | Yes | Partial | Yes: “Physiotherapists’ systematic checking of the exercise administration manual revealed excellent compliance rates in both groups". |
| Moseley 2009 | Yes | Yes | Yes | Partial: 16 weeks follow‐up. | Yes: “Participants completed exercise diaries which were analysed to ascertain adherence to the programmes.” Care provider visits also documented |
| Oh 2020 | Yes | Yes | Yes | Partial: 6 months follow‐up (5 months after the end of intervention) | No |
| Ohoka 2015 | Yes | No: standard physical therapy not described. Intensity of treadmill training not described | Yes | Partial: average of approximately 6 months | No |
| Oldmeadow 2006 | Yes | Yes | Yes | No: only until acute hospital discharge. Mobility outcomes at 7 days | Yes: time to first walk recorded in both groups |
| Orwig 2011 | Yes | Yes | Yes | Yes. Outcomes were assessed at 2, 6, and 12 months after hip fracture | Yes. Hours spent exercising quantified |
| Pol 2019 | Yes | Yes | Yes | Partial | Yes |
| Resnick 2007 | Yes | Yes | Yes | No: although follow‐up was 12 months from fracture, this coincided with the end of treatment | Partial: no data for usual care group |
| Salpakoski 2015 | Yes | Partial: control standard care did not have specific dosage for the exercise “5‐7 exercises for the lower limbs” | Yes | Partial | Partial: only compliance in intervention group reported but reported “None of the participants were followed for compliance” in control |
| Sherrington 1997 | Yes | Partial: "Usual care" not described | Yes | No: final assessment at 1 month (27 to 43 days) | Partial: only the intervention group completed diaries and were asked about the specific exercises. However, all participants were asked about general exercise. |
| Sherrington 2003 | Yes | Yes | Yes | No: 2 weeks follow‐up only | Partial: some data available but not regarding weight bearing |
| Sherrington 2004 | Yes | Yes | Yes | Partial: 4 months follow‐up only | Partial: compliance data collected for the two exercise groups but not for the control group. |
| Sherrington 2020 | Yes | Yes | Yes | Yes: 12 months | Partial: compliance data collected for intervention group via diaries |
| Stasi 2019 | Yes | Yes | No | Partial: 6 months | No |
| Suwanpasu 2014 | No | No | Unclear | No: 6 weeks after discharge | No |
| Sylliaas 2011 | Yes | Yes | Yes | No: intervention is only 12 weeks following an observation period of 12 weeks | No: not assessed |
| Sylliaas 2012 | Yes | Yes | Yes | Partial: although is 36 weeks after fracture, trial 1 starts 12 weeks after fracture, final follow‐up is 24 weeks after start of 2011 intervention | No: not assessed |
| Taraldsen 2019 | Yes | Yes | Yes | Yes: T3 = 48 to 56 weeks | Yes |
| Tsauo 2005 | Yes | Yes | Yes | Yes: 6 months' follow‐up. | No. However, 4 participants in the intervention group were excluded because of poor compliance. |
| Van Ooijen 2016 | Yes | Yes | Yes | Partial: 12 months' follow‐up for some but not all outcomes | No, included in protocol bot not reported |
| Williams 2016 | Yes | Yes | Yes | No: 3 months | No |
Sample sizes
The 40 included trials involved a total of 4059 participants. The median number of participants randomised per trial was 81 (interquartile range (IQR) 49 to 147). Study size ranged from 26 participants (Braid 2008; Mangione 2010) to 336 participants (Sherrington 2020).
Setting
The trials were conducted in 17 different countries: Australia (9 trials); Canada (1); Denmark (2); Finland (2); Germany (1); Greece (1); Italy (1); Japan (1); the Netherlands (2); Norway (3); Russia (1); South Korea (1); Switzerland (1); Taiwan (1); Thailand (1); UK (5); and USA (7). See Appendix 5.
Eighteen trials examined primarily in‐hospital rehabilitation; that is, settings where preoperative, operative and postoperative acute and subacute care is undertaken. Of these trials, 16 were single‐centre and two were multi‐centre trials; seven trials were in orthopaedic wards, 10 in rehabilitation wards and one ward type was unclear.
Nineteen trials were classified in the review as post‐hospital studies. Rehabilitation was undertaken predominantly in individuals' own homes; some trials had options for intervention in community health care centres; one trial had a rehabilitation component in skilled nursing facilities before discharge home (Pol 2019); and no studies were conducted in a social care setting. Three trials, also classified as post‐hospital studies, were in the outpatient setting with an additional home‐based component (Binder 2004; Sylliaas 2011; Sylliaas 2012).
Details of the timing of trial recruitment provided for included trials show Graham 1968 had the earliest start date (1961) and Pol 2019 the most recent start date (2016).
Participants
Overall, 80% of included participants were women, with the majority of participants in each trial being women (63% to 100% of trial population). Seven trials only included women (Baker 1991; Hauer 2002; Lamb 2002; Lauridsen 2002; Ohoka 2015; Orwig 2011; Resnick 2007). The average participant age in the included trials was 80 years. The mean ages of trial participants ranged from 71 years (Gorodetskyi 2007) to 90 years (Ohoka 2015), and was 80 or above in 24 trials. Thirty‐four trials set lower age limits, ranging from 50 years (Karumo 1977) to 90 years (Ohoka 2015). Twenty‐eight trials, including 19 of the 22 post‐hospital trials and nine of the 18 in‐hospital trials, specifically excluded people with various extents of cognitive impairment, judged according to various criteria and assessment instruments. Explicit exclusion criteria relating to previous and/or current immobility and/or medical conditions affecting mobility were stated in all trials except Bischoff‐Ferrari 2010, Gorodetskyi 2007, Langford 2015, Mangione 2010, Monticone 2018, Ohoka 2015, Pol 2019, Suwanpasu 2014, Sylliaas 2012, Tsauo 2005 and Williams 2016. The majority of included trials did not select on type of hip fracture, except for Gorodetskyi 2007, which specified trochanteric fractures, Graham 1968 (displaced intracapsular fractures), Karumo 1977 (femoral neck fractures), Kimmel 2016 (isolated subcapital or intertrochanteric hip fractures), Monticone 2018 (extracapsular hip fractures), Salpakoski 2015 (femoral neck or pertrochanteric fractures), Stasi 2019 (femoral neck fractures), Suwanpasu 2014 (femoral neck, intertrochanteric or subtrochanteric fractures), Sylliaas 2011 and Sylliaas 2012 (femoral neck or trochanteric fractures) and Taraldsen 2019 (intracapsular or extracapsular fractures). While not stated explicitly in some trials, it is very likely that all trial participants had surgery for a hip fracture except for three participants in Hauer 2002 who had elective hip surgery, and 12 participants in Miller 2006 who were treated for another lower limb fracture. For Sherrington 2020, data were obtained for 194 participants treated for hip fracture, exclusive of the 142 participants with pelvic or other lower limb fractures.
Interventions
Differences in duration, type and composition of the intervention are shown in Table 5 and Appendix 5.
In‐hospital rehabilitation
In the in‐hospital setting, 16 trials with 1100 participants compared the effect of different types of mobility training with a control intervention such as usual care, very gentle exercise or 'sham exercise'. Two trials (333 participants) compared the effect of different timing of mobility training (Graham 1968; Oldmeadow 2006).
The intervention was delivered by an expert health professional in all in‐hospital studies.
In‐hospital rehabilitation: comparing intervention to control, grouped by different types of intervention
Gait, balance and functional exercises
Two‐week programme of weight‐bearing exercise versus non‐weight‐bearing exercise: Sherrington 2003 (80 participants, Australia)
Weight‐bearing exercise twice daily for 60 minutes per day for 16 weeks versus usual care (mainly non‐weight‐bearing exercise for 30 minutes per day): Moseley 2009 (160 participants, Australia)
Treadmill gait retraining programme versus conventional gait retraining: Baker 1991 (40 participants, Australia)
Body‐weight supported treadmill training (10 minutes, four times per week) plus standard physiotherapy (40 minutes per day, six times per week) versus standard physiotherapy (40 minutes per day, six times per week): Ohoka 2015 (27 participants, Japan)
Body‐weight supported treadmill training (20 minutes/day for 10 consecutive work days) plus standard physiotherapy (30 minutes per day for 10 consecutive work days) versus standard physiotherapy (30 minutes per day for 10 consecutive work days): Oh 2020 (45 participants, Korea)
Six weeks C‐Mill gait adaptability treadmill training or conventional treadmill training (two study arms pooled for analysis) versus usual physiotherapy: Van Ooijen 2016 (70 participants, the Netherlands)
Two additional physiotherapy sessions/day, seven days/week versus usual care of one session/day. Additional sessions focused on function and gait: Kimmel 2016 (92 participants, Australia)
Three‐week programme of 90 minutes of balance task‐specific exercise in standing, transfers, gait and stairs training versus control (90 minutes open kinetic chain exercises in the supine position): Monticone 2018 (52 participants, Italy)
Twice daily physiotherapy versus standard regimen of once daily physiotherapy: Karumo 1977 (100 participants, Finland)
Intensive physiotherapy comprising six hours of physiotherapy per week versus standard physiotherapy of 15 to 30 minutes each weekday: Lauridsen 2002 (88 participants, Denmark)
Resistance exercises
Quadriceps muscle strengthening regimen for six weeks versus conventional physiotherapy alone: Mitchell 2001 (80 participants, UK)
Twelve‐week programme of resistance training versus resistance training for 12 weeks plus nutritional supplementation for six weeks versus attention control starting seven days post injury: Miller 2006 (75 participants; 63 with hip fracture, Australia)
Additional daily progressive knee‐extension strength training with three sets of 10 repetitions at 10 repetition maximum (RM), versus routine physiotherapy only (12 lower limb exercises and basic mobility): Kronborg 2017 (90 participants, Denmark)
Electrical stimulation of the quadriceps
Six‐week programme of electrical stimulation of the quadriceps muscle (18‐minute sessions) versus no electrical stimulation: Braid 2008 (26 participants, UK)
Six‐week programme of electrical stimulation of the quadriceps for three hours daily versus placebo stimulation: Lamb 2002 (27 participants, UK)
Ten‐day programme of electrical stimulation for 20 to 30 minutes at three sites close to surgical incision versus placebo stimulation: Gorodetskyi 2007 (60 participants, Russia)
In‐hospital rehabilitation: comparing different timing of intervention
Early assisted ambulation (within 48 hours) versus delayed assisted ambulation after surgery (fixation or hemiarthroplasty): Oldmeadow 2006 (60 participants, Australia)
Weight bearing at two weeks versus 12 weeks after internal fixation of a displaced intracapsular fracture: Graham 1968 (273 participants, UK)
Post‐hospital rehabilitation
In the post‐hospital setting, all 22 trials compared the effect of mobility training with no intervention, usual care, sham exercise or a social visit. Four of these trials each had two intervention groups and one control group, resulting in a total of 26 intervention arms (Mangione 2005; Pol 2019; Resnick 2007; Sherrington 2004). The two intervention arms in Mangione 2005 and Sherrington 2004 were sufficiently different to compare the different types of exercise programmes; for these two studies we compared each intervention arm with the control arm, and also compared the two different types of exercise programmes. The two intervention arms in Pol 2019 and Resnick 2007 were similar and therefore were combined for the analysis of intervention arm versus control arm.
The interventions tested by the 22 trials in the post‐hospital category all started after hospital discharge, except for three trials that commenced in the in‐hospital setting but delivered the majority of the intervention in the community (Bischoff‐Ferrari 2010; Langford 2015; Stasi 2019). The stage of rehabilitation at planned commencement varied: namely, recent discharge from in‐hospital treatment or rehabilitation (Hauer 2002; Orwig 2011; Pol 2019; Salpakoski 2015; Suwanpasu 2014; Tsauo 2005; Williams 2016); at completion of standard physical therapy (Binder 2004; Latham 2014; Magaziner 2019; Mangione 2005; Mangione 2010; Resnick 2007; Sherrington 2020); and later home‐based exercises (Sherrington 1997; Sherrington 2004; Sylliaas 2011; Sylliaas 2012; Taraldsen 2019).
The intervention was delivered by an expert health professional in 19 of the 22 post‐hospital studies, by a non‐expert (trained assistant) in one (Lamb 2002), and in two trials, it was unclear (Graham 1968; Hauer 2002).
We grouped the intervention arms by their primary exercise modality into six categories (Appendix 6) using the ProFaNE taxonomy (Appendix 1).
Most intervention arms (n = 9; 35%) included gait, balance and functional exercises as the primary intervention (ProFaNE taxonomy gait/balance/co‐ordination/functional task training).
Strength/resistance training was the primary component of six (23%) intervention arms.
Endurance training alone was the primary component of one (5%) intervention arm.
Multiple categories of the ProFaNE taxonomy were the primary intervention in five (19%) intervention arms (resistance training plus endurance training in three intervention arms; balance and functional exercise plus resistance training in two arms)
No studies included flexibility exercise, 3D exercise or general physical activity training as a primary intervention component.
We categorised the mobility strategy interventions in four trials as 'other': coaching based on cognitive behavioural therapy (two arms in Pol 2019); additional post‐discharge physiotherapy telephone support and coaching (Langford 2015); specific group of muscle contractions in the supine position (one intervention arm of Sherrington 2004); and a physical activity enhancing program, based on Resnick's self‐efficacy model (outlined in Resnick 2009) (Suwanpasu 2014).
Post‐hospital rehabilitation: comparing intervention to control, grouped by different types of intervention
Gait, balance and functional exercises
Additional 30 minutes of physiotherapy during acute care (total 60 minutes) plus additional 30 minutes per day unsupervised home programme for 12 months versus standard physiotherapy (30 minutes per day during acute care with no home programme): Bischoff‐Ferrari 2010 (173 participants, Switzerland)
Six months of training with monthly telephone calls using cognitive behavioural strategies, functional tasks using a Thera‐band programme based on INVEST (Bean 2004) and Sherrington 1997 programmes, versus attention control (nutrition education): Latham 2014 (232 participants, USA)
Home‐based, year‐long programme including progressive home exercise programme (strength training plus stretching three times per week, balance and walking exercises two to three times per week) and physical activity counselling, versus control (standard care, including written home exercise programme), after discharge from hospital: Salpakoski 2015 (81 participants, Finland)
One month of home‐based, weight‐bearing exercises started seven months after hip fracture versus usual care (no specific instructions): Sherrington 1997 (44 participants, Australia)
Four months of home‐based, weight‐bearing exercises or home‐based, non‐weight‐bearing exercises (performed in the supine position) versus no specific instructions started 22 weeks after hip fracture: Sherrington 2004 (120 participants, Australia)
Ten home visits plus phone calls over 12 months to deliver an individualised physiotherapist‐prescribed home programme of weight‐bearing balance and strength exercises plus fall prevention advice, versus usual care: Sherrington 2020 (194 participants with hip fracture, Australia)
Ten weeks of two exercise sessions per week with physiotherapists at home, targeting balance and gait with individually‐tailored, weight‐bearing exercises, all entailing change in base of support, versus usual care: Taraldsen 2019 (143 participants, Norway)
Three months, delivered in eight visits, of home‐based individualised physical therapy versus unsupervised home exercise on discharge from an acute ward: Tsauo 2005 (54 participants, Taiwan)
Six home‐based physiotherapy sessions over three months, delivered by a physiotherapist or technical instructor in home or outpatient clinic, plus novel information workbook and goal‐setting diary, in addition to usual rehabilitation services, versus usual care (usual rehabilitation services, of variable content): Williams 2016 (61 participants, Wales)
Resistance exercises
Twelve weeks of supervised, home‐based moderate‐ to high‐intensity resistance training versus education control group after completion of usual physical therapy: Mangione 2005 (41 participants, USA)
Ten weeks of progressive resistance leg strengthening exercises versus control (TENS causing no muscle contraction): Mangione 2010 (26 participants, USA)
Twelve‐week hip abductor strength training programme, three times per week with physiotherapist, from week 3 after discharge. Home‐based sessions, 40 to 55 minutes, progressing to three sets of 15 repetitions, with resistance added, versus control group receiving lesser intensity of hip abductor strengthening (approximately 10 minutes less per session, strengthening commenced two weeks later, resistance added later): Stasi 2019 (100 participants, Greece)
Three months of progressive resistance training twice weekly in outpatient setting as well as once a week at home, plus treadmill warm‐up and walking versus usual care (no specific instructions): Sylliaas 2011 (150 participants, Norway)
Six months of prolonged resistance training (three months of Sylliaas 2011 plus additional three months) plus treadmill warm‐up and walking versus usual care (no specific instructions): Sylliaas 2012 (95 participants, Norway)
Endurance exercise
Twelve weeks of supervised aerobic exercise training versus education control group after completion of usual physical therapy: Mangione 2005 (41 participants, USA)
Multiple categories
Six months of supervised intensive outpatient physical therapy and exercise training versus low‐intensity home exercise after completion of standard therapy: Binder 2004 (90 participants, USA)
Twelve weeks of intensive physical training versus placebo motor activity starting about four to five weeks after surgery upon discharge from in‐hospital rehabilitation: Hauer 2002 (28 participants; three had elective hip surgery, Germany)
Sixteen weeks of two to three times per week physiotherapist home visits to implement and progress: i) lower limb strength training programme using portable progressive resistance device, ii) endurance training (outdoor ambulation, indoor walking or other upright activity) aiming for 20 minutes at 50% of heart rate reserve. Compared with active control of seated active range‐of‐motion exercises and sensory‐level TENS: Magaziner 2019 (210 participants, USA)
Twelve months of home‐based exercise with a self‐efficacy based motivational component including aerobic exercise using Stairstep and stretching versus usual care: Orwig 2011 (180 participants, USA)
Twelve‐month programme of trainer‐led exercise sessions with or without motivational interventions (two arms pooled for this analysis) versus usual care (no intervention) after completion of standard rehabilitation: Resnick 2007 (155 participants, USA)
Other
Twelve months of additional telephone support and coaching: up to five post‐discharge telephone calls from physiotherapist: Langford 2015 (30 participants, Canada)
Four weeks of weekly coaching based on cognitive behavioural therapy, with a focus on increasing daily activity and practising exercises where indicated, plus a second intervention arm also wearing a physical activity monitor, versus usual care (physiotherapy and occupational therapy) in skilled nursing facilities for short‐term rehabilitation: Pol 2019 (240 participants, the Netherlands)
Face‐to‐face contact and five telephone calls for seven weeks post‐surgery, to implement a physical activity‐enhancing programme, based on Resnick's self‐efficacy model (Resnick 2009), versus standard care control (physical activity for hip fracture booklet): Suwanpasu 2014 (46 participants, Thailand)
Post‐hospital rehabilitation: comparing two different types of intervention
Twelve weeks of supervised, home‐based moderate‐ to high‐intensity resistance training versus aerobic exercise training after completion of usual physical therapy: Mangione 2005 (41 participants, USA)
Four months of home‐based, weight‐bearing exercises versus home‐based, non‐weight‐bearing exercises (performed in the supine position) started 22 weeks after hip fracture: Sherrington 2004 (120 participants, Australia)
Excluded studies
We excluded 18 studies during this update. We give brief details and reasons for exclusion of these studies in Characteristics of excluded studies. The primary reasons for exclusion related to study design (three trials), study participants (three trials) and study intervention (12 trials). For studies excluded in the previous version of this review, see Handoll 2011.
Ongoing studies
Details of the 21 ongoing trials are provided in the Characteristics of ongoing studies. Almost all studies are set in the in‐hospital rehabilitation or community settings, with exercise being the dominant intervention and robotic‐assisted balance training being evaluated in three trials.
Studies awaiting classification
Two trials await classification.
Che 2020 randomised 78 participants with 'old' femoral neck fractures. The intervention group received early rehabilitation training and the control group underwent routine rehabilitation. A conference abstract has been published. We have requested by email further details on the time post fracture, intervention, outcome measures and results.
Wu XY 2019 randomised 100 participants undergoing cementless total hip arthroplasty for femoral neck fracture. Weight‐bearing exercise was commenced early in the intervention group, versus at three weeks in the control group. We await translation of this study to English.
Risk of bias in included studies
We summarise our risk of bias judgements for 13 domains for the individual trials in Figure 2 and Figure 3. Details are described in the risk of bias tables in Characteristics of included studies. Blank spaces in the risk of bias summary figure indicate that we made no judgement for the domain because it was not applicable to the individual study (for example, because the study did not measure these outcomes).
2.

Risk of bias summary: review authors' judgements about each risk of bias domain for each included study
Note: a 'Yes' (+) judgement means that review authors considered there was a low risk of bias associated with the item, whereas a 'No' (‐) means that there was a high risk of bias. Assessments that resulted in an 'Unclear' (?) verdict often reflected a lack of information upon which to judge the domain. However, lack of information on blinding for mobility outcomes was always taken to imply that there was no blinding and rated as a 'No'; similarly for unblinded staff/self‐reported outcomes (health‐related quality of life, pain, falls, patient‐reported questionnaires and satisfaction), lack of information on blinding of researchers was rated as 'No', data collated by blinded researchers was rated 'Unclear'. An empty square (no judgement) indicates the domain was not applicable to that study.
3.

Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies
Allocation
We judged 21 trials (51%) to be at low risk of selection bias resulting from adequate sequence generation and allocation concealment; three additional trials took adequate measures to safeguard allocation concealment only. Conversely, Sherrington 1997, by using an open list, failed to conceal allocation and we judged this study to be at high risk of selection bias. Baker 1991, a quasi‐randomised trial using alternation, was at high risk of selection bias.
Blinding
Performance bias
The majority of studies (38 studies, 95%) did not blind participants or therapists (which in many cases is not feasible for these interventions), leading us to rate their risk of performance bias as unclear. A low risk of performance bias was judged likely for Lamb 2002, which used placebo stimulation. We considered one study to be at high risk of bias: the treating physiotherapist referred participants for outcome assessment once they considered the study objectives had been obtained (Lauridsen 2002).
Detection bias
Twenty‐seven trials had a low risk of detection bias for observer‐reported outcomes involving some judgement (mobility, walking speed, functional outcomes, activities of daily living and strength) due to assessor blinding of these measurable outcomes. Magaziner 2019 reported blinding, yet assessors were unblinded for three participants; the majority of trials did not report instances of unblinding. No blinding was reported in 12 trials, resulting in high risk of bias.
We judged 17 trials to be at a low risk of detection bias for observer‐reported outcomes not involving judgement (death, re‐admission, re‐operation, surgical complications, return to living at home), as they clearly described the methods for measurement of the outcome. We considered 16 trials to have an unclear risk of bias due to lack of blinding of assessors, inadequate description of how outcomes were measured, or both. Risk of bias was high in one trial where there was no blinding for discharge arrangements (return to living at home) (Oldmeadow 2006), an outcome which is potentially susceptible to bias.
We judged none of the trials to be at low risk of detection bias for participant/proxy‐reported outcomes (health‐related quality of life, pain, falls, patient‐reported questionnaires, satisfaction). We assessed 16 trials to be at unclear risk of bias, and four trials at high risk, for these outcomes. We assessed risk of detection bias for fall outcomes as unclear in the two trials that did not specify whether there was blinding (Bischoff‐Ferrari 2010; Ohoka 2015), and in the five trials that specified that assessors recording and entering fall data were blinded, yet participants reporting falls were not blinded (Langford 2015; Moseley 2009; Orwig 2011; Sherrington 2020; Van Ooijen 2016). The risk of bias was high in Taraldsen 2019, with falls reported in retrospect by participants and staff who were aware of group allocation.
Incomplete outcome data
We judged 13 trials to be at low risk of bias from the incompleteness of data on observer‐reported outcomes involving some judgement (mobility, walking speed, functional outcomes, activities of daily living and strength). We assessed 16 trials to be at high risk of bias for various reasons, including large losses to follow‐up, imbalances in loss to follow‐up between groups, incomplete data and post‐randomisation exclusions. For 11 trials, the impact of post‐randomisation exclusions and differential loss to follow‐up led to an unclear risk of bias rating. For observer‐reported outcomes not involving judgement (death, re‐admission, re‐operation, surgical complications, return to living at home), we considered 16 trials to be at low risk of bias, 11 at high risk of bias and 10 as unclear. For participant/proxy‐reported outcomes (health‐related quality of life, pain, falls, patient‐reported questionnaires, satisfaction), we considered six trials to be at low risk of bias, 10 at high risk of bias and five as unclear.
Selective reporting
The lack of prospective trial registration and protocols hindered the appraisal of the risk of bias from selective reporting. We considered six trials (Baker 1991; Graham 1968; Karumo 1977; Kronborg 2017; Oldmeadow 2006; Orwig 2011), which also featured incomplete reporting of trial results, to be at high risk of selective reporting bias. We considered 13 trials to be at low risk of bias and 21 as unclear.
Other potential sources of bias
Baseline characteristics
We judged five trials to be at high risk of bias in the estimate of the intervention effect due to major imbalances in baseline characteristics. This judgement resulted primarily from a lack of information on baseline characteristics in Graham 1968 and Karumo 1977; and from baseline imbalances in Mangione 2005 (the control group was more depressed and started the study seven weeks earlier than the two intervention groups), Kimmel 2016 (there were disproportionately more females and fewer carers in the home in the intervention group), and Sherrington 1997 (disproportionately more males in the intervention group).
Care programmes
We judged the risk of performance bias from important differences between intervention and control groups in care programmes other than the trial interventions or differences in the experience of care providers as low in 22 trials and unclear in eight trials (usually based on inadequate information). We assessed the risk of performance bias from between‐group differences in care programmes as high in 10 trials: Graham 1968 provided no information on care programmes; the extreme variation (28 to 200 days) in the timing of the first intervention visit from the trainer to the participants in Resnick 2007 may have affected trial findings; additional treadmill training was not the only difference between groups in Ohoka 2015, as the time in standard therapy was greater in the intervention group. In multiple post‐hospital trials, the lack of control for the effect of social interaction in the intervention group may have impacted upon the intervention effect (Bischoff‐Ferrari 2010; Orwig 2011; Sherrington 2020; Suwanpasu 2014; Sylliaas 2011; Sylliaas 2012; Taraldsen 2019).
Ascertainment bias for measurement of falls
Four of the eight trials that measured falls had low risk of bias for the method of ascertaining falls, while the risk of bias was unclear in four trials (Moseley 2009; Ohoka 2015; Orwig 2011; Taraldsen 2019).
Cluster‐randomised controlled trials
We judged the only cluster‐randomised trial, Pol 2019, to be at low risk of bias due to clustering. Although recruitment did not occur prior to randomisation, baseline characteristics were reported as well balanced, adjustment was made for confounders at baseline and for missing values, no clusters were lost, clustering was adjusted for, and the results are comparable with other trials.
Effects of interventions
See: Table 1; Table 2; Table 3; Table 4
In this section, we report outcomes separately for in‐hospital studies and post‐hospital studies. For in‐hospital studies, we distinguish two comparisons: studies which compared a mobilisation strategy with usual care (labelled as Comparison 1); and studies that compared different timings of an intervention in‐hospital (labelled as Comparison 2). For post‐hospital studies, we also distinguish two comparisons: studies which compared a mobilisation strategy with usual care (labelled as Comparison 3); and studies that compared one type of intervention with another type in the post‐hospital setting (labelled as Comparison 4).
For each outcome described below, we report the overall pooled effects of all mobilisation strategies. We summarise the findings and illustrate the absolute impact of interventions for critical outcomes in two summary of findings tables for the overall 'mobilisation strategy versus usual care' comparison in the in‐hospital setting (Table 1), and the overall 'mobilisation strategy versus control' comparison in the post‐hospital setting (Table 3).
We also report the effects on mobility according to each exercise category of the ProFaNE taxonomy (Appendix 1; Appendix 6), as well as the results of exercise interventions that included multiple categories or electrical stimulation. We summarise the findings for the mobility outcome and illustrate the absolute impact of each type of exercise category versus usual care in the in‐hospital setting, and versus control in the post‐hospital setting, in bespoke summary of findings tables (Table 2; Table 4).
We did not present summary of findings tables for the studies that compared different timings of an intervention in‐hospital or the studies that compared one type of intervention with another type in the post‐hospital setting.
Two post‐hospital studies did not contribute any outcomes to the review (Suwanpasu 2014; Sylliaas 2012).
Comparison 1. In‐hospital rehabilitation studies: mobilisation strategy versus usual care: critical outcomes
Note the mobilisation strategy interventions are compared with non‐provision of any specific mobilisation strategy, where the non‐provision control is defined as usual orthopaedic, medical care or allied health care.
Effect of mobilisation strategy versus usual care on mobility
Pooled analysis showed mobility strategies may improve mobility (measured using mobility scales) at the time point closest to four months (standardised mean difference (SMD) 0.53, 95% confidence interval (CI) 0.10 to 0.96; P = 0.02, I2 = 81%; 7 studies, 507 participants; low‐certainty evidence, downgraded due to risk of bias and imprecision; Analysis 1.1). The substantial heterogeneity in this analysis is explained by inclusion of Monticone 2018 and the large between‐group difference in the volume and intensity of functional exercise undertaken, compared with other studies. Removing Monticone 2018 reduced I2 to 44%, and it changed the effect size from SMD 0.53 (95% CI 0.10 to 0.96) to SMD 0.29 (95% CI 0.03 to 0.55).
1.1. Analysis.

Comparison 1: In‐hospital rehabilitation: mobilisation strategy versus usual care, critical outcomes, Outcome 1: Mobility (measured using mobility scales): combined data for all strategy types
Re‐expressing the results using the 12‐point Physical Performance and Mobility Examination (PPME), the intervention group scored 1.46 points higher (95% CI 0.28 to 2.64). The minimal important difference (MID) for the PPME is typically 1.13 to 2.15 (de Morton 2008).
Pooled analyses of dichotomous outcomes showed low‐certainty evidence that the intervention group may have less failure to regain pre‐fracture mobility, compared with controls (RR 0.48, 95% CI 0.27 to 0.85; P = 0.01, I2 = 0%; 2 studies, 64 participants; low certainty evidence, downgraded for risk of bias and imprecision; Analysis 1.2). There may be a beneficial effect of mobility strategies on self‐reported mobility as measured using the Western Ontario and McMaster Universities Osteoarthritis Index, physical function subscale (range 0 to 100, with lower score showing better function) (MD 25.40, 95% CI 28.72 to 22.08; 1 study, 52 participants; low‐certainty evidence, downgraded for risk of bias and imprecision; Analysis 1.3).
1.2. Analysis.

Comparison 1: In‐hospital rehabilitation: mobilisation strategy versus usual care, critical outcomes, Outcome 2: Mobility (failure to regain pre‐facture mobility): combined data for all strategy types
1.3. Analysis.

Comparison 1: In‐hospital rehabilitation: mobilisation strategy versus usual care, critical outcomes, Outcome 3: Mobility (measured using self‐reported outcomes): combined data for all strategy types
Types of intervention
Gait, balance or functional training
Trials where exercise interventions were classified as primarily gait, balance or functional task training using the ProFaNE taxonomy probably lead to a moderate improvement in mobility (measured using mobility scales) (SMD 0.57, 95% CI 0.07 to 1.06; P = 0.02, I2 = 84%; 6 studies, 463 participants; moderate‐certainty evidence; Analysis 1.4). Re‐expressing the results using the 12‐point PPME, the intervention group scored 1.56 points higher (95% CI 0.02 to 2.92). The MID for the PPME is typically 1.13 to 2.15 (de Morton 2008).
1.4. Analysis.

Comparison 1: In‐hospital rehabilitation: mobilisation strategy versus usual care, critical outcomes, Outcome 4: Mobility (measured using mobility scales): gait, balance and function
Resistance/strength training
Exercises classified as primarily resistance/strength training may make little or no difference to mobility as the certainty of evidence is low and the 95% CI included both a reduction and an increase in mobility (measured using mobility scales) (mean difference (MD) 1.0, 95% CI ‐0.81 to 2.81; P = 0.28; 1 study, 44 participants; low‐certainty evidence; Analysis 1.5). Similarly, resistance/strength training interventions may make little or no difference to mobility as measured by the Timed Up and Go test (TUG), as the certainty of evidence is low and the 95% CI includes both a reduction and an increase in score (MD ‐1.5, 95% CI ‐6.4 to 3.4; 1 study, 74 participants; low‐certainty evidence; Analysis 1.6).
1.5. Analysis.

Comparison 1: In‐hospital rehabilitation: mobilisation strategy versus usual care, critical outcomes, Outcome 5: Mobility (measured using mobility scales): resistance/strength training
1.6. Analysis.

Comparison 1: In‐hospital rehabilitation: mobilisation strategy versus usual care, critical outcomes, Outcome 6: Mobility (measured in seconds using TUG): resistance/strength training
No studies contained interventions classified primarily as flexibility, 3D, general physical activity, endurance, multiple intervention types or electrical stimulation.
We reported the outcomes separately for each of eight different mobility measurement tools in Analysis 1.7.
1.7. Analysis.

Comparison 1: In‐hospital rehabilitation: mobilisation strategy versus usual care, critical outcomes, Outcome 7: Mobility (measured using mobility scales) reporting individual outcome measures
Effect of mobilisation strategy versus usual care on walking speed
Pooled analysis provided moderate‐certainty evidence that mobilisation strategies probably improve walking speed compared to control; however, the 95% confidence interval includes the possibility of both increased and reduced walking speed (SMD 0.16, 95% CI ‐0.05 to 0.37; P = 0.13, I2 = 0%; 6 studies, 360 participants; moderate‐certainty evidence, downgraded for imprecision; Analysis 1.8). Re‐expressing the results using gait speed (metres/second, or m/s), showed an increase of 0.04 m/s in the intervention group (MD 0.04, 95% CI ‐0.01 to 0.08), which is considered a small meaningful change for gait speed (Perera 2006); however, the CI included both an increase and reduction in gait speed.
1.8. Analysis.

Comparison 1: In‐hospital rehabilitation: mobilisation strategy versus usual care, critical outcomes, Outcome 8: Walking speed (measured as metres/time): combined data for all strategy types
Types of intervention
Gait, balance or functional training
Trials where exercise interventions were classified as primarily gait, balance or functional task training using the ProFaNE taxonomy probably lead to a small improvement in walking speed; however, the 95% CI included both increased and decreased walking speed (SMD 0.15, 95% CI ‐0.07 to 0.36; P = 0.19, I2 = 0%; 5 studies, 336 participants; Analysis 1.9).
1.9. Analysis.

Comparison 1: In‐hospital rehabilitation: mobilisation strategy versus usual care, critical outcomes, Outcome 9: Walking speed (measured as metres/time): gait, balance and function
Electrical stimulation
Electrical stimulation increased walking speed in one small study; however, the 95% CI included both increased and decreased walking speed (MD 0.11, 95% CI ‐0.12 to 0.34; P = 0.35; 1 study, 24 participants; Analysis 1.10).
1.10. Analysis.

Comparison 1: In‐hospital rehabilitation: mobilisation strategy versus usual care, critical outcomes, Outcome 10: Walking speed (measured as metres/time): electrical stimulation
No studies contained interventions classified as primarily resistance/strength, flexibility, 3D, general physical activity, endurance training or multiple intervention types.
Effect of mobilisation strategy versus usual care on functioning
We are uncertain whether mobility strategies improve functioning compared with control as the certainty of the evidence was very low (SMD 0.75, 95% CI 0.24 to 1.26; P = 0.04, I2 = 79%; 7 studies, 379 participants; very low‐certainty evidence, downgraded due to risk of bias, substantial heterogeneity and imprecision; Analysis 1.11). Re‐expressing the results using the Barthel Index, the intervention group scored 4.4 points higher (95% CI 1.4 to 7.38). The MID for the Barthel Index (post hip surgery) is typically 9.8 (Unnanuntana 2018).
1.11. Analysis.

Comparison 1: In‐hospital rehabilitation: mobilisation strategy versus usual care, critical outcomes, Outcome 11: Functioning (measured using functioning scales): combined data for all strategy types
Types of intervention
Gait, balance or functional training
The effect of exercise interventions classified as primarily gait, balance or functional task training on functioning is unclear as the certainty of the evidence is very low (SMD 0.56, 95% CI ‐0.00 to 1.13; I2 = 79%; 5 studies, 312 participants; very low‐certainty evidence, downgraded for risk of bias, imprecision and inconsistency; Analysis 1.12).
1.12. Analysis.

Comparison 1: In‐hospital rehabilitation: mobilisation strategy versus usual care, critical outcomes, Outcome 12: Functioning (measured using functioning scales): gait, balance and function
Resistance/strength training
It is unclear whether exercise interventions classified as primarily resistance/strength training increase functioning, as the certainty of evidence was very low (MD 1.00, 95% CI 0.56 to 1.44; 1 study, 44 participants; very low‐certainty evidence, downgraded for risk of bias and two levels for imprecision; Analysis 1.13).
1.13. Analysis.

Comparison 1: In‐hospital rehabilitation: mobilisation strategy versus usual care, critical outcomes, Outcome 13: Functioning (measured using functioning scales): resistance/strength training
Electrical stimulation
A single study showed electrical stimulation may increase functioning (MD 3.0, 95% CI 1.0 to 5.00; 1 study, 23 participants; low‐certainty evidence, downgraded two levels for imprecision; Analysis 1.14).
1.14. Analysis.

Comparison 1: In‐hospital rehabilitation: mobilisation strategy versus usual care, critical outcomes, Outcome 14: Functioning (measured using functioning scales): electrical stimulation
No studies contained interventions classified as primarily flexibility, 3D, general physical activity or endurance.
Effect of mobilisation strategy versus usual care on health‐related quality of life
We were able to pool data from four of the five trials that assessed health‐related quality of life in‐hospital. Based on pooled SMD results from the four trials, we are uncertain whether mobility strategies improve health‐related quality of life as the certainty of the evidence was very low (SMD 0.39, 95% CI ‐0.07 to 0.85; P = 0.01, I2 = 71%; 4 studies, 314 participants; very low‐certainty evidence downgraded due to risk of bias, imprecision and heterogeneity; Analysis 1.15). The trial that could not be included in the meta‐analysis reported no significant difference between groups (Miller 2006; outcomes were reported as median and the denominator was not confirmed).
1.15. Analysis.

Comparison 1: In‐hospital rehabilitation: mobilisation strategy versus usual care, critical outcomes, Outcome 15: Health‐related quality of life (measured using HRQoL scales): gait, balance and function
Transformation of this result to the EQ‐5D score (0 to 1 scale), showed the mean difference (0.03, 95% CI ‐0.02 to 0.22) was smaller than the MID for the EQ‐5D, which is typically 0.074 (Walters 2005).
The time point for measurement ranged from 10 weeks (Kimmel 2016) to six months (Van Ooijen 2016).
Effect of mobilisation strategy versus usual care on mortality
Death was reported in eight trials with separate data for the intervention and control groups; six trials reported deaths in the short term and two in the long term (12 months). No deaths were clearly associated with trial participation.
Short‐term mortality (around 4 months or at discharge)
In the short term, mobility strategies may make little or no difference to the number of people who die compared with usual care; the certainty of the evidence is low and the 95% CI includes the possibility of both reduced and increased death with mobility strategy intervention (RR 1.06, 95% CI 0.48 to 2.30; P = 0.89, I2 = 0%; 6 studies, 489 participants; low‐certainty evidence, downgraded two levels due to risk of bias (removing studies with high risk of bias in one or more domains had a marked impact on results) and imprecision (few events and wide CI); Analysis 1.16).
1.16. Analysis.

Comparison 1: In‐hospital rehabilitation: mobilisation strategy versus usual care, critical outcomes, Outcome 16: Mortality, short term: combined data for all strategy types
Types of intervention
Gait, balance or functional training
There was no clear evidence of an effect of exercise interventions classified as primarily gait, balance or functional task training using the ProFaNE taxonomy (RR 1.43, 95% CI 0.44 to 4.66; I2 = 0%; 3 studies, 293 participants; Analysis 1.17).
1.17. Analysis.

Comparison 1: In‐hospital rehabilitation: mobilisation strategy versus usual care, critical outcomes, Outcome 17: Mortality, short term: gait, balance and function
Resistance/strength training
There was no clear evidence of an effect of exercise interventions classified as resistance/strength training (RR 0.83, 95% CI 0.26 to 2.62; I2 = 6%; 2 studies, 170 participants; Analysis 1.18).
1.18. Analysis.

Comparison 1: In‐hospital rehabilitation: mobilisation strategy versus usual care, critical outcomes, Outcome 18: Mortality, short term: resistance/strength training
Electrical stimulation
There was no clear evidence of an effect of exercise interventions classified as electrical stimulation (RR 0.73, 95% CI 0.05 to 10.49; 1 study, 26 participants; Analysis 1.19).
1.19. Analysis.

Comparison 1: In‐hospital rehabilitation: mobilisation strategy versus usual care, critical outcomes, Outcome 19: Mortality, short term: electrical stimulation
No studies contained interventions classified as primarily flexibility, 3D, general physical activity or endurance.
Long‐term mortality (around 12 months)
In the long term, mobility strategies may make little or no difference to the number of people who die compared with usual care (RR 1.22, 95% CI 0.48 to 3.12; P = 0.67, I2 = 0%; 2 studies, 133 participants; low‐certainty evidence, downgraded two levels due to risk of bias and imprecision; Analysis 1.20).
1.20. Analysis.

Comparison 1: In‐hospital rehabilitation: mobilisation strategy versus usual care, critical outcomes, Outcome 20: Mortality, long term: combined data for all strategy types
Types of intervention
Gait, balance or functional training
There was no evidence of an effect on long‐term mortality of exercise interventions classified as primarily gait, balance or functional task training using the ProFaNE taxonomy (RR 1.47, 95% CI 0.16 to 13.35; 1 study, 70 participants; Analysis 1.21).
1.21. Analysis.

Comparison 1: In‐hospital rehabilitation: mobilisation strategy versus usual care, critical outcomes, Outcome 21: Mortality, long term: gait, balance and function
Resistance/strength training
There was no evidence of an effect of exercise interventions classified as primarily resistance/strength training (RR 1.16, 95% CI 0.41 to 3.26; 1 study, 63 participants; Analysis 1.22).
1.22. Analysis.

Comparison 1: In‐hospital rehabilitation: mobilisation strategy versus usual care, critical outcomes, Outcome 22: Mortality, long term: resistance/strength training
No studies contained interventions classified as primarily flexibility, 3D, general physical activity, endurance or electrical stimulation.
Effect of mobilisation strategy versus usual care on adverse events
Mobility strategies may make little or no difference to re‐admission compared with usual care: there is low‐certainty evidence and the CI includes both a reduction and an increase in re‐admission (RR 0.70, 95% CI 0.44 to 1.11; P = 0.13, I2 = 33%; 4 studies, 322 participants; low‐certainty evidence, downgraded for imprecision and risk of bias; Analysis 1.23).
1.23. Analysis.

Comparison 1: In‐hospital rehabilitation: mobilisation strategy versus usual care, critical outcomes, Outcome 23: Adverse events (measured using dichotomous outcomes): combined data for all strategy types
Mobility strategies may make little or no difference to re‐operation (RR 0.32, 95% CI 0.01 to 7.57; P = 0.48; 1 study, 80 participants; Analysis 1.23), number of people who reported pain versus no pain (RR 1.12, 95% CI 0.80 to 1.57; P = 0.53, I2 = 0%; 3 studies, 245 participants; Analysis 1.23), number of people who experienced one or more falls (RR 0.67, 95% CI 0.32 to 1.38; P = 0.28; 1 study, 50 participants; Analysis 1.23), rate of falls (rate ratio 0.85, 95% CI 0.64 to 1.12; P = 0.25; 3 studies, 214 participants; Analysis 1.24) or other orthopaedic complications (RR 1.50, 95% CI 0.45 to 4.95; 1 study, 88 participants; Analysis 1.23). The effect of mobility strategies on surgical complications could not be estimated, with a single small study reporting no complications (Analysis 1.23). The effect of mobility strategies on pain as measured by continuous measures was markedly different in the two studies that measured it, with less pain in the intervention group in Monticone 2018 but little to no difference in Lamb 2002. We did not combine these studies as I2 = 98% (Analysis 1.25).
1.24. Analysis.

Comparison 1: In‐hospital rehabilitation: mobilisation strategy versus usual care, critical outcomes, Outcome 24: Adverse events (measured using rate of falls): all studies were gait, balance and function
1.25. Analysis.

Comparison 1: In‐hospital rehabilitation: mobilisation strategy versus usual care, critical outcomes, Outcome 25: Adverse events (measured using continuous measures of pain): combined data for all strategy types
Effect of mobilisation strategy versus usual care on number of people who returned to living at pre‐fracture residence
Mobility strategies may make little or no difference to the proportion of people who return to living at their pre‐fracture residence compared with usual care in the two studies that could be combined (RR 1.07, 95% CI 0.73 to 1.56; I2 = 19%; 2 studies, 240 participants; low‐certainty evidence, downgraded due to imprecision and indirectness; Analysis 1.26), or in a third study (RR 0.57, 95% CI 0.23 to 1.41; 1 study, 86 participants; Analysis 1.27).
1.26. Analysis.

Comparison 1: In‐hospital rehabilitation: mobilisation strategy versus usual care, critical outcomes, Outcome 26: Return to living at pre‐fracture residence: combined data for all strategy types
1.27. Analysis.

Comparison 1: In‐hospital rehabilitation: mobilisation strategy versus usual care, critical outcomes, Outcome 27: Return to living at pre‐fracture residence: additional study not included in main analysis
Types of intervention
Gait, balance or functional training
There was no evidence of an effect of exercise interventions classified primarily as gait, balance or functional task training using the ProFaNE taxonomy (RR 1.23, 95% CI 0.79 to 1.91; 1 study, 150 participants; Analysis 1.28).
1.28. Analysis.

Comparison 1: In‐hospital rehabilitation: mobilisation strategy versus usual care, critical outcomes, Outcome 28: Return to living at pre‐fracture residence: gait, balance and function
Resistance/strength training
There was no evidence of an effect of exercise interventions classified primarily as resistance/strength training (RR 0.75, 95% CI 0.35 to 1.60; 1 study, 90 participants; Analysis 1.29).
1.29. Analysis.

Comparison 1: In‐hospital rehabilitation: mobilisation strategy versus usual care, critical outcomes, Outcome 29: Return to living at pre‐fracture residence: resistance/strength training
Comparison 1. In‐hospital rehabilitation studies: mobilisation strategy versus usual care: other important outcomes
Effect of mobilisation strategy versus usual care on mobility: walking (aids and self‐reported outcomes)
Two studies evaluated the effect of mobility strategies on ability to walk unaided or with walking aids; pooled results showed no strong evidence of effect (RR 0.91, 95% CI 0.74 to 1.11; I2 = 0%; 2 studies, 230 participants; Analysis 2.1).
2.1. Analysis.

Comparison 2: In‐hospital rehabilitation: mobilisation strategy versus usual care, other important outcomes, Outcome 1: Walking, use of walking aid/need for assistance
No studies measured self‐reported walking outcomes.
Effect of mobilisation strategy versus usual care on mobility: balance
Pooled analysis of two studies that reported measures of balance (reach) indicated that mobility strategies may improve balance (reach) compared with control (SMD 0.37, 95% CI 0.01 to 0.73; P = 0.05, I2 = 0%; 2 studies, 121 participants; low‐certainty evidence, downgraded for risk of bias and imprecision; Analysis 2.2) and may improve score on the Berg Balance Scale (MD 9.37, 95% CI 2.70 to 16.04; P = 0.006; 1 study, 41 participants; low‐certainty evidence, downgraded two points for imprecision; Analysis 2.3). There was no evidence of a treatment effect in studies measuring the ability to tandem stand (RR 0.80, 95% CI 0.28 to 2.27; 1 study, 24 participants; Analysis 2.4), take repeated steps (MD 1.40, 95% CI ‐0.23 to 3.03; 1 study, 150 participants; Analysis 2.5) or in the pooling of two studies using subjective measures of balance (RR 0.96, 95% CI 0.71 to 1.29; I2 = 64%; 2 studies, 226 participants; random effects; Analysis 2.6).
2.2. Analysis.

Comparison 2: In‐hospital rehabilitation: mobilisation strategy versus usual care, other important outcomes, Outcome 2: Balance (measured using functional reach test, cm)
2.3. Analysis.

Comparison 2: In‐hospital rehabilitation: mobilisation strategy versus usual care, other important outcomes, Outcome 3: Balance (measured using balance scale)
2.4. Analysis.

Comparison 2: In‐hospital rehabilitation: mobilisation strategy versus usual care, other important outcomes, Outcome 4: Balance (measured using ability to tandem stand)
2.5. Analysis.

Comparison 2: In‐hospital rehabilitation: mobilisation strategy versus usual care, other important outcomes, Outcome 5: Balance (measured using step test; number of steps)
2.6. Analysis.

Comparison 2: In‐hospital rehabilitation: mobilisation strategy versus usual care, other important outcomes, Outcome 6: Balance (measured using self‐reported outcomes)
Effect of mobilisation strategy versus usual care on mobility: sit to stand
Pooled analysis of two studies indicated that mobilisation strategies probably improve sit to stand ability compared with control (MD 0.04, 95% CI 0.01 to 0.07; P = 0.005, I2 = 0%; 2 studies, 227 participants; moderate‐certainty evidence; Analysis 2.7).
2.7. Analysis.

Comparison 2: In‐hospital rehabilitation: mobilisation strategy versus usual care, other important outcomes, Outcome 7: Sit to stand (measured as number of stand ups/second)
Effect of mobilisation strategy versus usual care on muscle strength
Mobility strategies may make little or no difference to lower‐limb strength compared with control, as the 95% confidence interval includes the possibility of both increased and reduced strength (SMD 0.11, 95% CI ‐0.07 to 0.28; P = 0.24, I2 = 38%; 8 studies, 498 participants; low‐certainty evidence; Analysis 2.8).
2.8. Analysis.

Comparison 2: In‐hospital rehabilitation: mobilisation strategy versus usual care, other important outcomes, Outcome 8: Strength
Effect of mobilisation strategy versus usual care on activities of daily living
We are uncertain whether mobility strategies improve activities of daily living compared with control as the certainty of the evidence was very low (SMD 0.87, 95% CI 0.35 to 1.38; P = 0.001, I2 = 66%; 5 studies, 306 participants; very low‐certainty evidence; Analysis 2.9). We downgraded this result due to risk of bias, substantial heterogeneity and imprecision.
2.9. Analysis.

Comparison 2: In‐hospital rehabilitation: mobilisation strategy versus usual care, other important outcomes, Outcome 9: Activities of daily living (measured using ADL scales)
Effect of mobilisation strategy versus usual care on self‐reported measures of lower‐limb or hip function
No in‐hospital studies reported patient‐reported measures of lower‐limb or hip function.
Effect of mobilisation strategy versus usual care on participant satisfaction
Acceptability of interventions
No in‐hospital trials measured satisfaction.
Adherence
Six of the 18 in‐hospital studies measured and reported adherence (Appendix 7). Measures used to quantify adherence were varied; the majority of studies summarised the number of intervention sessions completed (n = 2), proportion of prescribed sessions attended (n = 1), proportion of participants who completed all sessions (n = 1) or quantified the amount of exercise performed (n = 2).
Resource outcomes
Available data on resource use is reported in Appendix 8. Length of hospital stay (in days) was reported in intervention and control groups in nine in‐hospital trials. Mean length of stay ranged from 17 days in the intervention versus 11 days in the control group (Oldmeadow 2006) to 92 days intervention versus 98 days in the control group (Ohoka 2015). Four trials reported data appropriate for pooling; pooled analysis provided no clear evidence that mobility strategies reduce the length of hospital stay compared with control, with the 95% confidence interval including the possibility of both increased and reduced length of stay (MD ‐0.83, 95% CI ‐3.94 to 2.28; I2 = 45%; 4 studies, 335 participants; Analysis 2.10). The number of physiotherapy sessions was reported in four in‐hospital trials (range of mean of 6 sessions to mean of 17 sessions). Moseley 2009 reported less community service use in the intervention group (RR 0.75, 95% CI 0.56 to 1.03; P = 0.09; 1 study, 98 participants; Analysis 2.11).
2.10. Analysis.

Comparison 2: In‐hospital rehabilitation: mobilisation strategy versus usual care, other important outcomes, Outcome 10: Resource use (measured by length of hospital stay)
2.11. Analysis.

Comparison 2: In‐hospital rehabilitation: mobilisation strategy versus usual care, other important outcomes, Outcome 11: Resource use (measured by use of community services)
Comparison 2. In‐hospital studies: comparing different timings of mobility intervention: critical and other important outcomes
Two trials compared the effect of different timings of mobility training (Oldmeadow 2006; Graham 1968). There are no data for the following critical outcomes: mobility, gait speed, functioning or health‐related quality of life. The two studies were insufficiently similar to be combined in meta‐analysis.
Effect of early versus delayed rehabilitation on mortality
There may be little or no impact on mortality when weight bearing commences at two weeks compared with 12 weeks post‐surgery (RR 0.74, 95% CI 0.43 to 1.29; 1 study, 273 participants; low‐certainty evidence, downgraded for risk of bias and imprecision; Analysis 3.1).
3.1. Analysis.

Comparison 3: In‐hospital rehabilitation: comparing different intervention strategies, critical outcomes, Outcome 1: Weight‐bearing at 2 wks v weight‐bearing at 12 weeks (mortality)
We are uncertain of the impact of commencing ambulation less than 48 hours compared with more than 48 hours postoperatively, as the certainty of evidence is very low (RR 3.20, 95% CI 0.14 to 75.55; 1 study, 60 participants; very low‐certainty evidence, downgraded for risk of bias and two levels for imprecision; Analysis 3.2).
3.2. Analysis.

Comparison 3: In‐hospital rehabilitation: comparing different intervention strategies, critical outcomes, Outcome 2: Early assisted ambulation (< 48 hrs) v delayed assisted ambulation (mortality)
Effect of early versus delayed rehabilitation on adverse events
No studies evaluated the effect of different timings of intervention on hospital re‐admission.
We are uncertain of the impact of commencing weight bearing at two weeks compared with 12 weeks post‐surgery for the adverse events of avascular necrosis (RR 0.69, 95% CI 0.33 to 1.42; 1 study, 112 participants), infection (RR 0.65, 95% CI 0.11 to 3.81; 1 study, 270 participants) or non‐union (RR 1.06, 95% CI 0.56 to 2.03; 1 study, 212 participants), as there is very low‐certainty evidence, downgraded one level for risk of bias and two levels for imprecision (see Analysis 3.3).
3.3. Analysis.

Comparison 3: In‐hospital rehabilitation: comparing different intervention strategies, critical outcomes, Outcome 3: Weight‐bearing at 2 wks v weight‐bearing at 12 weeks (adverse events)
Effect of early versus delayed rehabilitation on number of people who returned to living at pre‐fracture residence
There may be little or no impact of commencing ambulation less than 48 hours compared with more than 48 hours postoperatively on the outcome of return to living at home (RR 0.86, 95% CI 0.72 to 1.02; P = 0.09; 1 study, 60 participants; low‐certainty evidence, downgraded for risk of bias and imprecision; Analysis 3.4).
3.4. Analysis.

Comparison 3: In‐hospital rehabilitation: comparing different intervention strategies, critical outcomes, Outcome 4: Early assisted ambulation (< 48 hrs) v delayed assisted ambulation (return to living at home)
Effect of early versus delayed rehabilitation on mobility: need for assistance with transfers
There may be little or no impact of commencing ambulation less than 48 hours compared with more than 48 hours postoperatively on the need for assistance with transfers at one week follow‐up (RR 0.51, 95% CI 0.29 to 0.89; P = 0.02; 1 study, 60 participants; low‐certainty evidence, downgraded for risk of bias and imprecision; Analysis 3.5).
3.5. Analysis.

Comparison 3: In‐hospital rehabilitation: comparing different intervention strategies, critical outcomes, Outcome 5: Early assisted ambulation (< 48 hrs) v delayed assisted ambulation (walking aid/assistance)
In‐hospital studies: sensitivity analyses
For the mobility outcome (mobility scales) we carried out six sensitivity analyses to explore the stability of the results. For each of these analyses, the impact on the pooled mobility strategy versus control mobility outcome is summarised in Appendix 9.
Sensitivity analyses revealed little difference in the results when we excluded trials at high or unclear risk of bias associated with a lack of allocation concealment, removed trials with high risk of bias on any domains, removed trials that were reported only in conference abstracts, removed in‐hospital trials that measured outcomes at the end of the in‐hospital phase (the usual time point was that closest to four months), or using fixed‐effect (rather than random‐effects) meta‐analysis for the mobility outcome. There were no trials that focused on a population different from our target population (i.e. people with a fragility fracture resulting from low‐energy trauma), and no trials with mixed populations.
Funnel plots
We did not construct any funnel plots as all outcomes had fewer than 10 data points.
Comparison 3. Post‐hospital rehabilitation studies: mobilisation strategy versus usual care: critical outcomes
In these studies, the provision of any specific mobilisation strategy or programme was compared with non‐provision, where the non‐provision control was defined as no intervention, usual care, sham exercise (where the exercise was intended to be a control, or appeared to be of insufficient intensity and progression to have beneficial effects on mobility) or a social visit.
Effect of mobilisation strategy versus usual care on mobility
Pooled analysis provided evidence that mobilisation strategies increase mobility, measured using mobility scales, compared with control (SMD 0.32, 95% CI 0.11 to 0.54; P = 0.003, I2 = 48%; 7 studies, 761 participants; high‐certainty evidence; Analysis 4.1). Re‐expressing the results using the 12‐point Short Physical Performance Battery (SPPB), the intervention group scored 0.89 points higher (95% CI 0.30 to 1.50), which exceeds small meaningful change for SPPB (0.27 to 0.55 points) and is smaller than substantial meaningful change (0.99 to 1.34 points) (Perera 2006).
4.1. Analysis.

Comparison 4: Post‐hospital rehabilitation: mobilisation strategy versus control, critical outcomes, Outcome 1: Mobility (measured using mobility scales): combined data for all strategy types
Mobility strategies may make little or no difference to mobility as measured by TUG, as the certainty of evidence is low and the 95% CI includes both a reduction and an increase in score (MD ‐1.98, 95% CI ‐5.59 to 1.63; I2 = 15%; 4 studies, 375 participants; low‐certainty evidence; Analysis 4.2). Mobility training probably increases mobility, measured by the 6‐Minute Walk Test (6MWT), compared with control (MD 28.66, 95% CI 10.88 to 46.44; I2 = 37%; 5 studies, 396 participants; moderate‐certainty evidence; Analysis 4.3).
4.2. Analysis.

Comparison 4: Post‐hospital rehabilitation: mobilisation strategy versus control, critical outcomes, Outcome 2: Mobility (measured using Timed Up and Go, seconds): combined data for all strategy types
4.3. Analysis.

Comparison 4: Post‐hospital rehabilitation: mobilisation strategy versus control, critical outcomes, Outcome 3: Mobility (measured using 6‐Minute Walk Test, metres): combined data for all strategy types
Types of intervention
Gait, balance or functional training
Trials where exercise interventions were classified as primarily gait, balance or functional task training using the ProFaNE taxonomy lead to a moderate improvement in mobility (measured using mobility scales) (SMD 0.20, 95% CI 0.05 to 0.36; I2 = 0%; 5 studies, 621 participants; high‐certainty evidence; Analysis 4.4). Re‐expressing the results using the 12‐point SPPB, the intervention group scored 0.55 points higher (95% CI 0.14 to 1.0), which is a small meaningful change on this outcome measure (Perera 2006). The effect on mobility measured using TUG is not clear as the certainty of evidence is very low (MD ‐7.57, 95% CI ‐19.25 to 4.11; 1 study, 128 participants; very low‐certainty evidence; Analysis 4.5).
4.4. Analysis.

Comparison 4: Post‐hospital rehabilitation: mobilisation strategy versus control, critical outcomes, Outcome 4: Mobility (measured using mobility scales): gait, balance and function
4.5. Analysis.

Comparison 4: Post‐hospital rehabilitation: mobilisation strategy versus control, critical outcomes, Outcome 5: Mobility (measured using Timed Up and Go, seconds): gait, balance and function
No studies of gait, balance or functional task training measured mobility using the 6MWT.
Resistance/strength training
Trials where exercise interventions were classified as primarily resistance/strength training may make little or no difference to mobility (measured using TUG) as the certainty of evidence is low and the 95% CI included both a reduction and an increase in mobility (MD ‐6.00, 95% CI ‐12.95 to 0.95; 1 study, 96 participants; low‐certainty evidence; Analysis 4.6). Resistance/strength training may increase mobility as measured using the 6MWT (MD 55.65, 95% CI 28.58 to 82.72; I2 = 0%; 3 studies, 198 participants; low‐certainty evidence; Analysis 4.7). The minimal important difference (MID) for the 6MWT (adults with pathology) is typically 14.0 m to 30.5 m (Bohannon 2017).
4.6. Analysis.

Comparison 4: Post‐hospital rehabilitation: mobilisation strategy versus control, critical outcomes, Outcome 6: Mobility (measured using Timed Up and Go, seconds): resistance/strength training
4.7. Analysis.

Comparison 4: Post‐hospital rehabilitation: mobilisation strategy versus control, critical outcomes, Outcome 7: Mobility (measured using 6‐Minute Walk Test, metres): resistance/strength training
No studies of resistance/strength training measured mobility using mobility scales.
Endurance training
The effect of exercises classified as being primarily endurance training on mobility measured using the 6MWT is not clear as the certainty of evidence is very low (MD 12.70, 95% CI ‐72.12 to 97.52; 1 study, 21 participants; very low‐certainty evidence; Analysis 4.8).
4.8. Analysis.

Comparison 4: Post‐hospital rehabilitation: mobilisation strategy versus control, critical outcomes, Outcome 8: Mobility (measured using 6‐Minute Walk Test, metres): endurance training
Multiple types of exercise
Interventions containing multiple primary types of exercise probably lead to a moderate increase in mobility (mobility scales) (SMD 0.94, 95% CI 0.53 to 1.34; I2 = 6%; 2 studies, 104 participants; moderate‐certainty evidence; Analysis 4.9). Both studies included gait, balance or functional training plus resistance/strength training ProFaNE categories (Binder 2004; Hauer 2002). Re‐expressing the results using the 12‐point SPPB, the intervention group scored 2.6 points higher (95% CI 1.47 to 3.71), with substantial meaningful change for SPPB being 0.99 to 1.34 points (Perera 2006). A study including multiple types of interventions, classified in ProFaNE as strength training and endurance training, may have little or no effect on mobility (6MWT) (MD 9.30, 95% CI ‐14.62 to 33.22; 1 study, 187 participants; low‐certainty evidence; Analysis 4.10). The mean 6MWT distance in the intervention group was 9 m further (95% CI 15 m less to 33 m further) than in the control group, with a MID of 14.0 m to 30.5 m (Bohannon 2017).
4.9. Analysis.

Comparison 4: Post‐hospital rehabilitation: mobilisation strategy versus control, critical outcomes, Outcome 9: Mobility (measured using mobility scales): multiple component
4.10. Analysis.

Comparison 4: Post‐hospital rehabilitation: mobilisation strategy versus control, critical outcomes, Outcome 10: Mobility (measured using 6‐Minute Walk Test, metres): multiple component
No studies containing multiple primary types of exercise measured mobility using TUG.
Other
Two interventions were classified as 'other', according to the ProFaNE taxonomy. Non‐weight‐bearing exercise had no clear effect on mobility (mobility scales) compared with control (MD 0.40, 95% CI ‐0.37 to 1.17; 1 study, 72 participants; Analysis 4.11); nor did cognitive behavioural therapy with or without a sensor to monitor physical activity (MD 0.58, 95% CI ‐3.96 to 5.11; 1 study, 151 participants; Analysis 4.12).
4.11. Analysis.

Comparison 4: Post‐hospital rehabilitation: mobilisation strategy versus control, critical outcomes, Outcome 11: Mobility (measured using mobility scales): other type of exercise (non‐weight bearing exercise)
4.12. Analysis.

Comparison 4: Post‐hospital rehabilitation: mobilisation strategy versus control, critical outcomes, Outcome 12: Mobility (measured using Timed Up and Go, seconds): other type of exercise OT +/‐ sensor)
No studies contained interventions classified primarily as flexibility, 3D, general physical activity or electrical stimulation.
We reported the outcomes separately for each of eight different mobility measurement tools in Analysis 4.13.
4.13. Analysis.

Comparison 4: Post‐hospital rehabilitation: mobilisation strategy versus control, critical outcomes, Outcome 13: Mobility (measured using mobility scales) reporting individual outcome measures
Three studies reported self‐reported mobility outcomes. There was no strong evidence of an intervention effect on the continuously scored Activity Measure for Post Acute Care (range 9 to 101, higher score indicates better function) (MD 1.46, 95% CI ‐0.62 to 3.53; I2 = 0%; 2 studies, 355 participants; Analysis 4.14). The intervention group may be more likely to be able to climb a flight of stairs compared with the control group (RR 0.45, 95% CI 0.29 to 0.72; I2 = 0%; 2 studies, 148 participants; low‐certainty evidence; Analysis 4.15).
4.14. Analysis.

Comparison 4: Post‐hospital rehabilitation: mobilisation strategy versus control, critical outcomes, Outcome 14: Mobility (measured using self‐report, continuous scales): combined data for all strategy types
4.15. Analysis.

Comparison 4: Post‐hospital rehabilitation: mobilisation strategy versus control, critical outcomes, Outcome 15: Mobility (measured using self‐reported, dichotomous outcome): combined data for all strategy types
Effect of mobilisation strategy versus usual care on walking speed
Pooled analysis provided high‐certainty evidence that mobilisation strategies improve walking speed compared to control (SMD 0.16, 95% CI 0.04 to 0.29; I2 = 1%; 14 studies, 1067 participants; high‐certainty evidence; Analysis 4.16). Re‐expressing the results using gait speed (m/sec), there was an increase in gait speed of 0.05 m/sec in the intervention group (MD 0.05, 95% CI 0.01 to 0.09). A small meaningful change for gait speed is 0.04 to 0.06 m/sec (Perera 2006).
4.16. Analysis.

Comparison 4: Post‐hospital rehabilitation: mobilisation strategy versus control, critical outcomes, Outcome 16: Walking speed: combined data for all strategy types
Types of intervention
Gait, balance or functional training
Trials where exercise interventions were classified as primarily gait, balance or functional task training using the ProFaNE taxonomy have no clear effect on gait speed; the 95% CI includes both a reduction and increase in gait speed (SMD 0.08, 95% CI ‐0.09 to 0.25; I2 = 0%; 7 studies, 511 participants; Analysis 4.17).
4.17. Analysis.

Comparison 4: Post‐hospital rehabilitation: mobilisation strategy versus control, critical outcomes, Outcome 17: Walking speed: gait, balance and function
Resistance/strength training
The impact of trials classified primarily as resistance/strength training on gait speed is unclear; the 95% CI includes both a reduction and increase in gait speed (SMD 0.29, 95% CI ‐0.01 to 0.58; I2 = 0%; 3 studies, 197 participants; Analysis 4.18).
4.18. Analysis.

Comparison 4: Post‐hospital rehabilitation: mobilisation strategy versus control, critical outcomes, Outcome 18: Walking speed: resistance/strength training
Endurance
In the single study with an intervention arm classified primarily as endurance training, the 95% CI included both a reduction and increase in gait speed (MD 0.14, 95% CI ‐0.06 to 0.34; 1 study, 22 participants; Analysis 4.19).
4.19. Analysis.

Comparison 4: Post‐hospital rehabilitation: mobilisation strategy versus control, critical outcomes, Outcome 19: Walking speed: endurance
Multiple types of intervention
It is unclear whether training involving multiple ProFaNE categories increases walking speed as the certainty of evidence is very low (SMD 0.53, 95% CI ‐0.13 to 1.18; I2 = 81%; 3 studies, 285 participants; very low‐certainty evidence, downgraded for risk of bias, inconsistency and imprecision; Analysis 4.20).
4.20. Analysis.

Comparison 4: Post‐hospital rehabilitation: mobilisation strategy versus control, critical outcomes, Outcome 20: Walking speed: multiple component
Other
Two Interventions were classified as 'other' according to the ProFaNE taxonomy. Post‐discharge telephone support and coaching had no clear effect on walking speed compared with control (MD 0.00, 95% CI ‐0.20 to 0.20; 1 study, 26 participants; Analysis 4.21), nor did non‐weightbearing exercise (MD 0.06, 95% CI ‐0.19 to 0.31; 1 study; 72 participants; Analysis 4.22).
4.21. Analysis.

Comparison 4: Post‐hospital rehabilitation: mobilisation strategy versus control, critical outcomes, Outcome 21: Walking speed: other (post‐discharge physio telephone support and coaching)
4.22. Analysis.

Comparison 4: Post‐hospital rehabilitation: mobilisation strategy versus control, critical outcomes, Outcome 22: Walking speed: other (non‐weight bearing)
No studies contained interventions classified primarily as flexibility, 3D, general physical activity or electrical stimulation.
Subgroup analyses
Subgroup analysis by trials excluding participants with cognitive impairment at baseline found no evidence of a difference in the effect of mobility strategies on walking speed outcome between trials where participants were specifically excluded if they had impaired cognition (SMD 0.19, 95% CI 0.04 to 0.34; 12 studies, 762 participants) and with trials that did not have impaired cognition as an exclusion criterion (SMD 0.07, 95% CI ‐0.16 to 0.29; 2 studies, 304 participants. Test for subgroup differences: Chi² = 0.79, degrees of freedom (df) = 1, P = 0.37, I² = 0%; Analysis 4.23).
4.23. Analysis.

Comparison 4: Post‐hospital rehabilitation: mobilisation strategy versus control, critical outcomes, Outcome 23: Walking speed subgrouped by studies with cognitive impairment included v studies with cognitive impairment not included, combined data for all strategy types
Subgroup analysis found no evidence of a difference in the effect of mobility strategies on walking speed outcome between trials where interventions were delivered in the outpatient setting (SMD 0.35, 95% CI 0.08 to 0.62; I2 = 24%; 2 studies, 229 participants) and trials where interventions were delivered in the secondary and social care setting (SMD 0.11, 95% CI ‐0.02 to 0.25; I2 = 0%; 14 studies, 838 participants. Test for subgroup differences: Chi² = 2.34, df = 1, P = 0.13, I² = 57.3%; Analysis 4.24). Note that no trials were conducted in a social care setting.
4.24. Analysis.

Comparison 4: Post‐hospital rehabilitation: mobilisation strategy versus control, critical outcomes, Outcome 24: Walking speed: subgrouped by outpatient v secondary and social care setting
Subgroup analysis by age found no evidence of a difference in the effect of mobility strategies on walking speed outcome between trials where mean age was 80 years or less (SMD 0.12, 95% CI ‐0.05 to 0.30; I2 = 0%; 10 studies, 536 participants) and trials where mean age was above 80 years (SMD 0.18, 95% CI 0.01 to 0.36; I2 = 48%; 6 studies, 530 participants. Test for subgroup differences: Chi² = 0.23, df = 1, P = 0.63, I² = 0%; Analysis 4.25).
4.25. Analysis.

Comparison 4: Post‐hospital rehabilitation: mobilisation strategy versus control, critical outcomes, Outcome 25: Walking speed subgrouped by mean age ≤ 80 years v > 80 years, combined data for all strategies
Effect of mobilisation strategy versus usual care on functioning
Whilst there is high‐certainty evidence indicating mobility strategies increase function, this improvement is unlikely to be clinically important (SMD 0.23, 95% CI 0.10 to 0.36; I2 = 0%; 9 studies, 936 participants; high‐certainty evidence; Analysis 4.26). Re‐expressing the results using the Barthel Index, the intervention group scored 1.4 points higher (95% CI 0.6 to 2.1). The MID for the Barthel Index (post‐hip surgery) is typically 9.8 (Unnanuntana 2018).
4.26. Analysis.

Comparison 4: Post‐hospital rehabilitation: mobilisation strategy versus control, critical outcomes, Outcome 26: Functioning (measured using functioning scales): combined data for all strategy types
Intervention types
Gait, balance or functional training
The impact of gait, balance or functional task training on functioning is unclear as the 95% CI includes both increased and reduced functioning (SMD 0.17, 95% CI ‐0.02 to 0.36; I2 = 0%; 4 studies, 432 participants; Analysis 4.27).
4.27. Analysis.

Comparison 4: Post‐hospital rehabilitation: mobilisation strategy versus control, critical outcomes, Outcome 27: Functioning (measured using functioning scales): gait, balance and function
Resistance/strength training
Exercises classified as primarily resistance or strength training may increase functioning (SMD 0.29, 95% CI 0.03 to 0.55; I2 = 0%; 2 studies, 246 participants; low‐certainty evidence; Analysis 4.28)
4.28. Analysis.

Comparison 4: Post‐hospital rehabilitation: mobilisation strategy versus control, critical outcomes, Outcome 28: Functioning (measured using functioning scales): resistance/strength training
Multiple types of intervention
The impact of training involving multiple ProFaNE components is unclear for the functioning outcome (SMD 0.34, 95% CI ‐0.04 to 0.72; I2 = 0%; 2 studies, 107 participants; Analysis 4.29).
4.29. Analysis.

Comparison 4: Post‐hospital rehabilitation: mobilisation strategy versus control, critical outcomes, Outcome 29: Functioning (measured using functioning scales): multiple components
Other
In a trial comparing cognitive behavioural therapy with or without physical activity monitor with control, the effect of intervention on functioning is unclear as the 95% CI includes both increased and reduced functioning (MD 0.34, 95% CI ‐0.13 to 0.81, I2 = 0%; 2 studies, 151 participants; Analysis 4.30).
4.30. Analysis.

Comparison 4: Post‐hospital rehabilitation: mobilisation strategy versus control, critical outcomes, Outcome 30: Functioning (measured using functioning scales): other: OT +/‐ sensor
No studies contained interventions classified primarily as flexibility, 3D, general physical activity or electrical stimulation.
Effect of mobilisation strategy versus usual care on health‐related quality of life
Mobility strategies probably lead to a slight increase in health‐related quality of life that may not be clinically meaningful (SMD 0.14, 95% CI ‐0.00 to 0.29; I2 = 29%; 10 studies, 785 participants; moderate‐certainty evidence; Analysis 4.31). Re‐expressing the results using the EQ‐5D (0 to 1 scale), there was an increase in quality of life of 0.01 in the intervention group (95% CI ‐0.007 to 0.08). The MID for the EQ‐5D is typically 0.074 (Walters 2005). Re‐expressing the results using the SF‐36 (0 to 100 scale), there was an increase in quality of life of 3 points in the intervention group (95% CI ‐0.6 to 5.7). The MID for SF‐36 is typically 3 to 5 (Walters 2003). Thus, the respective means were smaller than the MIDs for both scales, although the 95% CI for the SF‐36 included the MID.
4.31. Analysis.

Comparison 4: Post‐hospital rehabilitation: mobilisation strategy versus control, critical outcomes, Outcome 31: Health‐related quality of life (measured using HRQoL scales): combined data for all strategy types
Intervention types
Gait, balance or functional training
The impact of gait, balance or functional task training on functioning is unclear as the 95% CI includes both increased and reduced functioning (SMD 0.08, 95% CI ‐0.37 to 0.53; I2 = 0%; 4 studies, 316 participants; Analysis 4.32).
4.32. Analysis.

Comparison 4: Post‐hospital rehabilitation: mobilisation strategy versus control, critical outcomes, Outcome 32: Health‐related quality of life (measured using HRQoL scales): gait, balance and function
Resistance/strength training
Exercises classified as primarily resistance or strength training may make little or no difference to functioning as the 95% CI includes both increased and reduced functioning (SMD 0.15, 95% CI ‐0.14 to 0.45; I2 = 0%; 3 studies, 197 participants; low‐certainty evidence; Analysis 4.33)
4.33. Analysis.

Comparison 4: Post‐hospital rehabilitation: mobilisation strategy versus control, critical outcomes, Outcome 33: Health‐related quality of life (measured using HRQoL scales): resistance/strength training
Endurance training
The impact of exercises classified as primarily endurance training is unclear (MD 9.50, 95% CI ‐8.56 to 27.56; I2 = 0%; 1 study, 22 participants; Analysis 4.34).
4.34. Analysis.

Comparison 4: Post‐hospital rehabilitation: mobilisation strategy versus control, critical outcomes, Outcome 34: Health‐related quality of life (measured using HRQoL scales): endurance
Multiple types of intervention
Training involving multiple ProFaNE components may improve health‐related quality of life, as measured using the SF‐36 Physical Function subscale (MD 11.00, 95% CI 0.42 to 21.58; 1 study, 83 participants; Analysis 4.35).
4.35. Analysis.

Comparison 4: Post‐hospital rehabilitation: mobilisation strategy versus control, critical outcomes, Outcome 35: Health‐related quality of life (measured using HRQoL scales): multiple components
No studies contained interventions classified primarily as flexibility, 3D, general physical activity or electrical stimulation.
Subgroup analyses
Subgroup analysis by trials excluding participants with cognitive impairment at baseline found no evidence of a difference in the effect of mobility strategies on health‐related quality of life outcome between trials where participants were specifically excluded if they had impaired cognition (SMD 0.17, 95% CI 0.01 to 0.33; I2 = 33%; 11 studies, 665 participants) compared with trials that did not have impaired cognition as an exclusion criterion (SMD 0.00, 95% CI ‐0.36 to 0.36; I2 = 0%; 1 study, 120 participants. Test for subgroup differences: Chi² = 0.73, df = 1 (P = 0.39), I² = 0; Analysis 4.36).
4.36. Analysis.

Comparison 4: Post‐hospital rehabilitation: mobilisation strategy versus control, critical outcomes, Outcome 36: Health‐related quality of life subgrouped by studies with cognitive impairment included v studies with cognitive impairment not included, combined data for all strategy types
Subgroup analysis found no evidence of a difference in the effect of mobility strategies on health‐related quality of life outcome between trials where interventions were delivered in the outpatient setting (SMD 0.18, 95% CI ‐0.09 to 0.45; I2 = 56%; 2 studies, 233 participants) and trials where interventions were delivered in the secondary and social care setting (SMD 0.13, 95% CI ‐0.04 to 0.30; I2 = 32%; 10 studies, 552 participants), where strength was increased in both settings. (Test for subgroup differences: Chi² = 0.09, df = 1 (P = 0.76), I² = 0%; Analysis 4.37).
4.37. Analysis.

Comparison 4: Post‐hospital rehabilitation: mobilisation strategy versus control, critical outcomes, Outcome 37: Health‐related quality of life subgrouped by outpatient v secondary and social care setting
Subgroup analysis by age found no evidence of a difference in the effect of mobility strategies on health‐related quality of life outcome between trials where mean age was 80 years or less (SMD 0.25, 95% CI ‐0.05 to 0.55; I2 = 66%; 5 studies, 184 participants) and trials where mean age was above 80 years (SMD 0.11, 95% CI ‐0.05 to 0.27; I2 = 0%; 7 studies, 601 participants. Test for subgroup differences: Chi² = 0.64, df = 1 (P = 0.43), I² = 0%, Analysis 4.38).
4.38. Analysis.

Comparison 4: Post‐hospital rehabilitation: mobilisation strategy versus control, critical outcomes, Outcome 38: Health‐related quality of life subgrouped by mean age ≤ 80 years v > 80 years, combined data for all strategy
Effect of mobilisation strategy versus usual care on mortality
Death was reported in 12 studies with separate data for the intervention and control groups; eight studies reported short‐term mortality and four reported long‐term (12 months) mortality.
Short‐term mortality (around 4 months or at discharge)
In the short term, mobility strategies probably have no impact on the number of people who die compared with usual care; the certainty of the evidence is moderate and the 95% CI includes the possibility of both reduced and increased death with a mobility strategy intervention (RR 1.01, 95% CI 0.49 to 2.06; P = 0.99, I2 = 0%; 7 studies, 737 participants; moderate‐certainty evidence, downgraded due to imprecision (few events and wide CI); Analysis 4.39).
4.39. Analysis.

Comparison 4: Post‐hospital rehabilitation: mobilisation strategy versus control, critical outcomes, Outcome 39: Mortality, short term: combined data for all strategy types
Types of intervention
Gait, balance or functional training
There was no clear evidence of an effect of exercise interventions classified as primarily gait, balance or functional task training using the ProFaNE taxonomy (RR 1.12, 95% CI 0.46 to 2.72; I2 = 0%; 3 studies, 264 participants; Analysis 4.40).
4.40. Analysis.

Comparison 4: Post‐hospital rehabilitation: mobilisation strategy versus control, critical outcomes, Outcome 40: Mortality, short term: gait, balance and function
Resistance/strength training
There was no clear evidence of an effect of exercise interventions classified as primarily resistance/strength training (RR 1.40, 95% CI 0.19 to 10.03; I2 = 0%; 2 studies, 123 participants; Analysis 4.41).
4.41. Analysis.

Comparison 4: Post‐hospital rehabilitation: mobilisation strategy versus control, critical outcomes, Outcome 41: Mortality, short term: resistance/strength training
Multiple types of intervention
The impact of training involving multiple ProFaNE components is unclear as the 95% CI includes both reduced and increased mortality (RR 0.61, 95% CI 0.08 to 4.55; I2 = 0%; 2 studies, 290 participants; Analysis 4.42).
4.42. Analysis.

Comparison 4: Post‐hospital rehabilitation: mobilisation strategy versus control, critical outcomes, Outcome 42: Mortality, short term: multiple components
Other
In a trial comparing non‐weight bearing exercise with control, the effect of intervention on mortality is unclear as the 95% CI includes both increased and reduced mortality (RR 0.50, 95% CI 0.03 to 7.59; 1 study, 60 participants; Analysis 4.43).
4.43. Analysis.

Comparison 4: Post‐hospital rehabilitation: mobilisation strategy versus control, critical outcomes, Outcome 43: Mortality, short term: other: non‐weight bearing
No studies contained interventions classified primarily as flexibility, 3D, general physical activity, endurance or electrical stimulation.
Long‐term mortality (around 12 months)
In the long term, it is unclear whether mobility strategies impact the number of people who die compared with usual care (RR 0.73, 95% CI 0.39 to 1.37; P = 0.33, I2 = 0%; 4 studies, 588 participants; low‐certainty evidence, downgraded two levels due to risk of bias (removing studies with high risk of bias in one or more domains had a marked impact on results) and imprecision (few events and wide CI); Analysis 4.44).
4.44. Analysis.

Comparison 4: Post‐hospital rehabilitation: mobilisation strategy versus control, critical outcomes, Outcome 44: Mortality, long term: combined data for all strategy types
Types of intervention
Gait, balance or functional training
There was no clear evidence of an effect of exercise interventions classified as primarily gait, balance or functional task training using the ProFaNE taxonomy on long‐term mortality (RR 0.75, 95% CI 0.34 to 1.67; I2 = 0%; 2 studies, 254 participants; Analysis 4.45).
4.45. Analysis.

Comparison 4: Post‐hospital rehabilitation: mobilisation strategy versus control, critical outcomes, Outcome 45: Mortality, long term: gait, balance and function
Multiple types of intervention
The impact of training involving multiple ProFaNE components is unclear as the 95% CI includes both reduced and increased mortality (RR 0.70, 95% CI 0.25 to 1.96; I2 = 0%; 2 studies, 334 participants; Analysis 4.46).
4.46. Analysis.

Comparison 4: Post‐hospital rehabilitation: mobilisation strategy versus control, critical outcomes, Outcome 46: Mortality, long term: multiple components
Effect of mobilisation strategy versus usual care on adverse events
We prespecified re‐admission to hospital as the critical adverse event to be reported in the summary of findings table (Table 3). There is no clear evidence of the effect of mobility strategies on re‐admissions: mobilisation strategies may decrease the number of re‐admissions; however, the 95% confidence interval includes the possibility of both a large reduction and large increase. We downgraded the evidence by one level for risk of bias, as both trials were at a high risk of bias in one or more domains, and one level for imprecision due to very few events and wide CIs (RR 0.86, 95% CI 0.52 to 1.42; I2 = 0%; 2 studies, 206 participants; low‐certainty evidence; Analysis 4.47). A single study that reported re‐admission rate and could not be pooled had a similar result (RR 1.00, 95% CI 0.62 to 1.60; 1 study, 173 participants; Analysis 4.48).
4.47. Analysis.

Comparison 4: Post‐hospital rehabilitation: mobilisation strategy versus control, critical outcomes, Outcome 47: Adverse events (measured using dichotomous outcomes): combined data for all strategy types
4.48. Analysis.

Comparison 4: Post‐hospital rehabilitation: mobilisation strategy versus control, critical outcomes, Outcome 48: Adverse events (measured using re‐admission rate: combined for all strategy types
There was no strong evidence of an effect of mobility strategies on the adverse outcomes of re‐operation (RR 0.46, 95% CI 0.20 to 1.08; 1 study, 173 participants; Analysis 4.47), or surgical complications (RR 0.92, 95% CI 0.06 to 13.18; 1 study, 25 participants; Analysis 4.47).
Pooled analysis provided evidence that mobilisation strategies probably reduce the number of falls by 21% compared with control (rate ratio 0.79, 95% CI 0.63 to 0.99; I2 = 0%; 3 studies, 397 participants; moderate‐certainty evidence, downgraded one level for risk of bias; Analysis 4.49). Exercise interventions classified as primarily gait, balance or functional task training using the ProFaNE taxonomy reduced falls (rate ratio 0.78, 95% CI 0.62 to 0.99; I2 = 0%; 2 studies, 367 participants; Analysis 4.50); however, there was no evidence of an effect of additional phone support and coaching (rate ratio 1.00, 95% CI 0.14 to 7.10; 1 study, 26 participants; Analysis 4.51).
4.49. Analysis.

Comparison 4: Post‐hospital rehabilitation: mobilisation strategy versus control, critical outcomes, Outcome 49: Adverse events (measured using rate of falls): combined for all strategy types
4.50. Analysis.

Comparison 4: Post‐hospital rehabilitation: mobilisation strategy versus control, critical outcomes, Outcome 50: Adverse events (measured using rate of falls): gait, balance and function
4.51. Analysis.

Comparison 4: Post‐hospital rehabilitation: mobilisation strategy versus control, critical outcomes, Outcome 51: Adverse events (measured using rate of falls): other (additional phone support and coaching)
There was no strong evidence of an effect of mobility strategies on the number of people experiencing one or more falls (risk ratio 1.03, 95% CI 0.85 to 1.25; 4 studies, 527 participants; Analysis 4.52).
4.52. Analysis.

Comparison 4: Post‐hospital rehabilitation: mobilisation strategy versus control, critical outcomes, Outcome 52: Adverse events (measured as number of people who experienced 1 or more falls)
There was no evidence of an effect of mobility strategies on pain in the three studies that used a continuous pain score (SMD ‐0.04, 95% CI ‐0.29 to 0.22; I2 = 0%; 3 studies, 242 participants; Analysis 4.53), or one study using a dichotomous score to determine the impact on pain of weight‐bearing (OR 1.40, 95% CI 0.48 to 4.10; 71 participants) and non‐weight‐bearing exercise (OR 0.82, 95% CI 0.26 to 2.55; 73 participants) compared with control (Sherrington 2004).
4.53. Analysis.

Comparison 4: Post‐hospital rehabilitation: mobilisation strategy versus control, critical outcomes, Outcome 53: Adverse events (measured using continuous measure of pain)
Comparison 3. Post‐hospital rehabilitation studies: mobilisation strategy versus usual care: other important outcomes
Effect of mobilisation strategy versus usual care on mobility: walking (aids and self‐reported outcomes)
Pooled analysis provided no evidence that mobilisation strategies affect walking‐aid use compared with control (RR 0.46, 95% CI 0.16 to 1.31; I2 = 94%; 4 studies, 314 participants; low‐certainty evidence; Analysis 5.1).
5.1. Analysis.

Comparison 5: Post‐hospital rehabilitation: mobilisation strategy versus control, other important outcomes, Outcome 1: Walking (measured as use of walking aid/need for assistance)
Pooled analysis of two studies provided no evidence that mobilisation strategies improved subjective walking measures (number of people who said they had difficulty or inability to walk specified distances) compared to control (RR 0.55, 95% CI 0.28 to 1.06; I2 = 0%; 2 studies, 182 participants; Analysis 5.2).
5.2. Analysis.

Comparison 5: Post‐hospital rehabilitation: mobilisation strategy versus control, other important outcomes, Outcome 2: Walking (measured using self‐reported outcomes)
Effect of mobilisation strategy versus usual care on mobility: balance
Pooled analysis provided no clear evidence that mobility training improves balance compared with control when balance is measured using reach (MD 1.30, 95% CI ‐1.70 to 4.31; I2 = 34%; 2 studies, 144 participants; Analysis 5.3), timed standing in various positions (SMD 0.24, 95% CI ‐0.37 to 0.86; I2 = 79%; 2 studies, 234 participants; Analysis 5.4) or balance scales (SMD 0.28, 95% CI ‐0.52 to 1.08; I2 = 71%; 2 studies, 212 participants; Analysis 5.5). For self‐reported measures of balance, pooled analysis provided contradictory evidence for the effect of mobility training on balance compared with control, although the level of evidence was low to very low. For continuous outcomes, the intervention group reported more unsteadiness (MD ‐0.66, 95% CI ‐1.19 to ‐0.13; I2 = 0%; 1 study, 24 participants; very low‐certainty evidence; Analysis 5.6), and for dichotomous outcomes, the intervention group may report less unsteadiness (RR 0.82, 95% CI 0.69, 0.98; I2 = 0%; 2 studies, 148 participants; low‐certainty evidence; Analysis 5.7).
5.3. Analysis.

Comparison 5: Post‐hospital rehabilitation: mobilisation strategy versus control, other important outcomes, Outcome 3: Balance (measured using functional reach test, cm)
5.4. Analysis.

Comparison 5: Post‐hospital rehabilitation: mobilisation strategy versus control, other important outcomes, Outcome 4: Balance (measured using timed standing in various positions)
5.5. Analysis.

Comparison 5: Post‐hospital rehabilitation: mobilisation strategy versus control, other important outcomes, Outcome 5: Balance (measured using balance scale)
5.6. Analysis.

Comparison 5: Post‐hospital rehabilitation: mobilisation strategy versus control, other important outcomes, Outcome 6: Balance (measured using continuous self‐reported meaure)
5.7. Analysis.

Comparison 5: Post‐hospital rehabilitation: mobilisation strategy versus control, other important outcomes, Outcome 7: Balance (measured using dichotomous self‐reported measure)
Effect of mobilisation strategy versus usual care on mobility: sit to stand
Pooled analysis provided evidence that mobilisation strategies may improve sit to stand mobility compared with control (MD ‐6.49, 95% CI ‐12.23 to ‐0.75; I2 = 91%; 5 studies, 457 participants; low‐certainty evidence, downgraded one level as all studies had high risk of bias in at least one domain and one level for inconsistency; Analysis 5.8)
5.8. Analysis.

Comparison 5: Post‐hospital rehabilitation: mobilisation strategy versus control, other important outcomes, Outcome 8: Sit to stand (measured as number of stand ups/second)
Effect of mobilisation strategy versus usual care on muscle strength
Pooled analysis found that mobilisation strategies increase lower‐limb strength compared with control (SMD 0.30, 95% CI 0.18 to 0.42; I2 = 34%; 14 studies, 1121 participants; high‐certainty evidence; Analysis 5.9).
5.9. Analysis.

Comparison 5: Post‐hospital rehabilitation: mobilisation strategy versus control, other important outcomes, Outcome 9: Strength
Subgroup analyses
Subgroup analysis by trials excluding participants with cognitive impairment at baseline found evidence of a significantly greater effect of mobility strategies on strength outcome in trials where participants were specifically excluded if they had impaired cognition (SMD 0.37, 95% CI 0.23 to 0.50; I2 = 23%; 14 studies, 891 participants) compared with trials that did not have impaired cognition as an exclusion criterion (SMD 0.07, 95% CI ‐0.19 to 0.33; I2 = 51%; 2 studies, 230 participants. Test for subgroup differences: Chi² = 3.86, df = 1, P = 0.05, I² = 74.1%; Analysis 5.10).
5.10. Analysis.

Comparison 5: Post‐hospital rehabilitation: mobilisation strategy versus control, other important outcomes, Outcome 10: Strength subgrouped by studies with cognitive impairment included v studies with cognitive impairment not included, combined data for all strategy types
Subgroup analysis found no evidence of a difference in the effect of mobility strategies on strength outcome between trials where interventions were delivered in the outpatient setting (SMD 0.67, 95% CI 0.39 to 0.95; I2 = 0%; 2 studies, 227 participants) and trials where interventions were delivered in the secondary and social care setting (SMD 0.39, 95% CI 0.25 to 0.52; I2 = 15%; 12 studies, 890 participants); however, both stages of rehabilitation resulted in increased strength. (Test for subgroup differences: Chi² = 3.15, df = 1, P = 0.08, I² = 68.2%; Analysis 5.11.)
5.11. Analysis.

Comparison 5: Post‐hospital rehabilitation: mobilisation strategy versus control, other important outcomes, Outcome 11: Strength subgrouped by stage of rehabilitation
Subgroup analysis by age found no evidence of a difference in the effect of mobility strategies on strength outcome between trials where mean age was 80 years or less (SMD 0.35, 95% CI 0.16 to 0.54; I2 = 48%; 8 studies, 464 participants) and trials where mean age was above 80 years (SMD 0.27, 95% CI 0.11 to 0.43; I2 = 70%; 6 studies, 657 participants); however, both stages of rehabilitation resulted in increased strength. (Test for subgroup differences: Chi² = 0.39, df = 1, P = 0.53, I² = 0%; Analysis 5.12).
5.12. Analysis.

Comparison 5: Post‐hospital rehabilitation: mobilisation strategy versus control, other important outcomes, Outcome 12: Strength subgrouped by mean age ≤ 80 years v > 80 years, combined data for all strategies
Effect of mobilisation strategy versus usual care on activities of daily living
There is no evidence that mobility strategies improve activities of daily living (SMD ‐0.01, 95% CI ‐0.26 to 0.23; I2 = 55%; 6 studies, 683 participants; Analysis 5.13).
5.13. Analysis.

Comparison 5: Post‐hospital rehabilitation: mobilisation strategy versus control, other important outcomes, Outcome 13: Activities of daily living (measured using ADL scales)
Effect of mobilisation strategy versus usual care on self‐reported measures of lower‐limb or hip function
It is unclear whether mobility strategies improve lower‐limb or hip function (SMD 0.78, 95% CI ‐20 to 1.77; I2 = 74%; 2 studies, 106 participants; Analysis 5.14). This was measured using the Hip Rating Questionnaire (Binder 2004) and Harris Hip Score (Tsauo 2005).
5.14. Analysis.

Comparison 5: Post‐hospital rehabilitation: mobilisation strategy versus control, other important outcomes, Outcome 14: Self‐reported measures of lower limb/hip function
Effect of mobilisation strategy versus usual care on participant satisfaction
Acceptability of interventions
No trials in the post‐hospital setting measured acceptability of interventions.
Adherence
Of the 22 post‐hospital studies, 14 measured and reported adherence (Appendix 7). Measures used to quantify adherence were varied; the majority of studies summarised the number of intervention sessions completed (n = 5), proportion of prescribed sessions attended (n = 1), proportion of participants who completed a specified number of sessions/week (n = 3), proportion of participants who completed all sessions (n = 1) or quantified the amount of exercise performed (n =4).
Resource outcomes
Resources use is reported in Appendix 8. The number of physiotherapy sessions was reported in six post‐hospital trials (range = mean of 2 sessions to mean of 36 sessions). No studies reported the number of outpatient attendances or need for special care. Langford 2015 reported the total telephone intervention time delivered for the intervention group, over 5 calls, was 151 minutes (range 42 to 286 minutes).
Comparison 4. Post‐hospital studies: comparing different mobility strategy interventions: critical and other important outcomes
Endurance training versus resistance training
One study compared endurance training versus resistance training (Mangione 2005).
Effect of endurance training versus resistance training on mobility
There was no evidence of a difference in effect on mobility measured using the 6‐Minute Walk Test (MD ‐42.20, 95% CI ‐131.07 to 46.67; 1 study, 23 participants; Analysis 6.1).
6.1. Analysis.

Comparison 6: Post‐hospital rehabilitation: comparing different intervention strategies, critical outcomes, Outcome 1: Resistance/strength training v endurance training (mobility measured using 6‐Minute Walk Test
Effect of endurance training versus resistance training on walking speed
There was no evidence of a difference in effect on walking speed (MD ‐0.08, 95% CI ‐0.30 to 0.14; 1 study, 23 participants; Analysis 6.2).
6.2. Analysis.

Comparison 6: Post‐hospital rehabilitation: comparing different intervention strategies, critical outcomes, Outcome 2: Resistance/strength training v endurance training (walking speed)
Effect of endurance training versus resistance training on health‐related quality of life
There was no evidence of a difference in effect on health‐related quality of life (MD 0.20, 95% CI ‐18.36 to 18.76; 1 study, 23 participants; Analysis 6.3).
6.3. Analysis.

Comparison 6: Post‐hospital rehabilitation: comparing different intervention strategies, critical outcomes, Outcome 3: Resistance/strength training v endurance training (health‐related quality of life)
Effect of endurance training versus resistance training on strength
There was no evidence of a difference in effect on strength (MD ‐7.50, 95% CI ‐24.08 to 9.08; 1 study, 23 participants; Analysis 6.4).
6.4. Analysis.

Comparison 6: Post‐hospital rehabilitation: comparing different intervention strategies, critical outcomes, Outcome 4: Resistance/strength training v endurance training (strength)
Weight‐bearing versus non‐weight‐bearing exercise
One study compared weight‐bearing exercise (classified as primarily gait, balance, co‐ordination or functional task training using the ProFaNE taxonomy) and non‐weight‐bearing exercise (classified as other) (Sherrington 2004).
Effect of weight‐bearing exercise versus non‐weight‐bearing exercise on mobility
There was no evidence of a difference in effect on mobility measured using a mobility scale (MD ‐0.20, 95% CI ‐1.13 to 0.73; 1 study, 69 participants; Analysis 6.5).
6.5. Analysis.

Comparison 6: Post‐hospital rehabilitation: comparing different intervention strategies, critical outcomes, Outcome 5: Gait, balance and function v other (muscle contraction in supine) (mobility measured using mobility scale)
Effect of weight‐bearing exercise versus non‐weight‐bearing exercise on walking speed
There was no evidence of a difference in effect on walking speed (MD ‐0.70, 95% CI ‐5.40 to 4.00; 1 study, 69 participants; Analysis 6.6).
6.6. Analysis.

Comparison 6: Post‐hospital rehabilitation: comparing different intervention strategies, critical outcomes, Outcome 6: Gait, balance and function v other (muscle contraction in supine) (walking speed)
Effect of weight‐bearing exercise versus non‐weight‐bearing exercise on mortality
There was no evidence of a difference in effect on short‐term mortality (RR 3.00, 95% CI 0.33 to 27.63; 1 study, 80 participants; Analysis 6.7).
6.7. Analysis.

Comparison 6: Post‐hospital rehabilitation: comparing different intervention strategies, critical outcomes, Outcome 7: Gait, balance and function v other (muscle contraction in supine) (mortality)
Effect of weight‐bearing exercise versus non‐weight‐bearing exercise on adverse events
There was no evidence of a difference in effect on pain from fracture (RR 1.51, 95% CI 0.65 to 3.53; 1 study, 72 participants; Analysis 6.8), pain during exercise (RR 2.11, 95% CI 0.80 to 5.57; 1 study, 72 participants; Analysis 6.8) or number of people who fell (RR 1.06, 95% CI 0.53 to 2.12; 1 study, 72 participants; Analysis 6.9).
6.8. Analysis.

Comparison 6: Post‐hospital rehabilitation: comparing different intervention strategies, critical outcomes, Outcome 8: Gait, balance and function v other (muscle contraction in supine) (Adverse events: pain)
6.9. Analysis.

Comparison 6: Post‐hospital rehabilitation: comparing different intervention strategies, critical outcomes, Outcome 9: Gait, balance and function v other (muscle contraction in supine) (Adverse events: number of people who fell)
Effect of weight‐bearing exercise versus non‐weight‐bearing exercise on balance
The weight‐bearing group may have better objective balance at four months compared with the control group (MD 4.90, 95% CI 0.87 to 8.93; 1 study, 68 participants; low‐certainty evidence, downgraded for risk of bias and imprecision; Analysis 6.10); however, there was no between‐group difference for self‐reported balance (RR 1.02, 95% CI 0.77 to 1.34; 1 study, 72 participants; Analysis 6.11).
6.10. Analysis.

Comparison 6: Post‐hospital rehabilitation: comparing different intervention strategies, critical outcomes, Outcome 10: Gait, balance and function v other (muscle contraction in supine) (Balance, observed)
6.11. Analysis.

Comparison 6: Post‐hospital rehabilitation: comparing different intervention strategies, critical outcomes, Outcome 11: Gait, balance and function v other (muscle contraction in supine) (Balance, self‐reported)
Effect of weight‐bearing exercise versus non‐weight‐bearing exercise on strength
There was no evidence of a difference in effect on strength (MD 27.30, 95% CI ‐3.41 to 58.01; 1 study, 66 participants; Analysis 6.12).
6.12. Analysis.

Comparison 6: Post‐hospital rehabilitation: comparing different intervention strategies, critical outcomes, Outcome 12: Gait, balance and function v other (muscle contraction in supine) (strength)
Post‐hospital studies: sensitivity analyses
For the mobility outcome (broad mobility measures), we carried out five sensitivity analyses to explore the stability of the results. For each of these analyses, the impact on the pooled mobility strategy versus control mobility outcome is summarised in Appendix 9.
Sensitivity analyses revealed little difference in the results when we excluded trials at high or unclear risk of bias associated with a lack of allocation concealment, removed trials with high risk of bias on any domains, removed trials that did not clearly focus on people with a fragility fracture resulting from low‐energy trauma, removed trials with mixed populations, or used fixed‐effect (rather than random‐effects) meta‐analysis for the mobility outcome. There were no trials reported only in conference abstracts.
Funnel plots
The funnel plots in Figure 4, Figure 5 and Figure 6 do show some asymmetry. However, we did not consider the asymmetry sufficient to downgrade the level of evidence.
4.

Funnel plot of comparison 4: post‐hospital rehabilitation: mobilisation strategy versus control, critical outcomes. Outcome 4.16: walking speed: combined data for all strategy types
5.

Funnel plot of comparison 4: post‐hospital rehabilitation: mobilisation strategy versus control, critical outcomes. Outcome 4.31: health‐related quality of life (measured using HRQoL scales): combined data for all strategy types
6.

Funnel plot of comparison 5: post‐hospital rehabilitation: mobilisation strategy versus control, other important outcomes. Outcome: 5.9 strength
Economic outcomes
Of the 40 included studies, we identified two that had reported economic data (Appendix 10). Taraldsen 2019 reported costs of intervention and health services from the broad healthcare perspective, plus cost‐effectiveness analysis results. The probability that a home‐based exercise programme delivered for four months was cost‐effective was below 39% for any incremental cost‐effectiveness ratio (ICER) ceiling ratio below EUR 150,000 per quality‐adjusted life‐year (QALY) gained. Williams 2016 reported costs from a public sector perspective, considering the cost of health services, social services and medications. Cost‐effectiveness analysis was not conducted as there was no between‐group difference in QALYs.
Adherence
Across both in‐hospital and post‐hospital settings, 20 studies measured and reported adherence (Appendix 7). Measures used to quantify adherence were varied. The majority of studies summarised the number of intervention sessions completed (n = 7). Other studies: measured the proportion of prescribed sessions attended (n = 3); measured the proportion of participants who completed a specified number of sessions/week (n = 4); measured the proportion of participants who completed all sessions (n = 2); or quantified the amount of exercise performed (n = 4). The median proportion of intervention group participants that met the study's prespecified definition of adherence was 83% (IQR 70 to 93) (10 studies).
Discussion
Summary of main results
Our review covers mobilisation strategies implemented during rehabilitation after hip fracture surgery. The evidence from randomised and quasi‐randomised trials now comprises that from 40 trials. In some trials, methodological flaws undermined the validity of their findings. The trials involved a total of 4059 participants, most of whom were female and aged over 65 years. Of these, 18 trials (1433 participants) contributed to the evidence for the ‘mobility strategy versus control comparison’ for at least one of the main outcomes in the in‐hospital setting. Twenty trials (2485 participants) contributed evidence for the ‘mobility strategy versus control comparison’ for at least one of the main outcomes in the post‐hospital setting. Two trials (141 participants) in the post‐hospital setting did not contribute to the main outcomes.
Our interpretations of continuous outcomes, presented in Table 1, Table 2, Table 3 and Table 4 are based upon guiding rules for interpreting SMDs (‘Cohen’s effect sizes’) and expressed in the units of a specific measurement instrument where appropriate. Our illustrative risks for dichotomous outcomes presented in Table 1 and Table 3 are based on proportions calculated from the number of people who experienced the event divided by the number of people in the group, for those trials included in the analysis for that outcome.
We classified the exercise interventions using the ProFaNE classification system. As described in Appendix 6, of the 46 comparisons conducted in 40 studies, 23 compared interventions classified as primarily gait, balance and functional training, with usual care. Resistance training was evaluated in eight studies, endurance training in one study, multiple categories in seven studies (usually gait, balance and functional training combined with resistance training), and three comparisons were categorised as 'other'. In addition, three studies primarily involved electrical stimulation.
In‐hospital setting, mobility strategy versus control
Mobility strategy versus control
Mobility strategies may cause a moderate, meaningful improvement in mobility; however, we assessed the certainty of the evidence as low. Overall, there is moderate‐certainty evidence of a small, meaningful improvement in walking speed compared with control; however, the confidence interval includes both slower walking and faster walking. Any difference in the effect of in‐hospital mobility strategies on mobility and walking may be due to mobility measures being more sensitive to smaller changes in mobility than walking outcomes (particularly the use of an aid or assistance).
Mobility strategies may make little or no difference to short‐term or long‐term mortality (low‐certainty evidence), re‐admission (low‐certainty evidence) or return to living at the pre‐fracture residence (low‐certainty evidence). We are uncertain whether mobility strategies improve functioning or health‐related quality of life as we assessed the certainty of the evidence as very low. Mobility strategies may make little or no difference to the adverse events of re‐operation, pain or falls.
Regarding non‐critical outcomes, mobility strategies may make little or no difference to the ability to walk unaided or with walking aids. Mobility strategies may increase balance (measured using reach and balance scales, low‐certainty evidence) and probably improve sit to stand ability (moderate‐certainty evidence). There is also low‐certainty evidence that mobility strategies may increase strength; however, the 95% confidence interval includes the possibility of both increased and reduced strength.
Resource use was reported to varying degrees in 18 studies. It was most often reported in terms of length of hospital stay and number of physiotherapy sessions. Four studies with 335 participants were available for pooling of data, with the mobility strategies making little or no difference to length of hospital stay.
Types of interventions
When we explored the effect of different types of mobility strategies on the mobility outcome, interventions that include training of gait, balance and functional tasks were effective in increasing mobility. The effects of resistance training were unclear. No studies evaluated the effect of other forms of exercise or electrical stimulation on the critical outcome of mobility. Electrical stimulation may improve function in the in‐hospital setting.
Other comparisons
One study found early assisted ambulation commencing within 48 hours postoperatively may reduce the need for assistance with transfers at one week follow‐up, compared with assisted ambulation starting after 48 hours post‐surgery (low‐certainty evidence). The impact of early versus delayed rehabilitation on mortality and adverse events is unclear as the certainty of evidence is very low, and there may be little or no impact on return to living at home (low certainty evidence).
Subgroup analyses
There were insufficient studies to conduct subgroup analyses.
Post‐hospital setting, mobility strategy versus control
Mobility strategy versus control
There is high‐certainty evidence that mobility strategies lead to a small, clinically‐meaningful increase in mobility compared with control (usual care, no intervention, sham exercise or social visit) in the post‐hospital setting. Mobility strategies make small, clinically meaningful improvements in walking speed compared to control (high‐certainty evidence), lead to a small, non‐clinically meaningful improvement in functioning (high‐certainty evidence) and probably lead to a slight increase in health‐related quality of life that may not be meaningful (moderate‐certainty evidence).
Mobility strategies probably make little or no difference to short‐term mortality compared with control (moderate‐certainty evidence). Mobility strategies may make little or no difference to the adverse outcomes of long‐term mortality or re‐admission (low‐certainty evidence). It is unclear whether mobilisation strategies affect re‐operation, pain or the number of people who fall, due to low‐ and very low‐certainty of evidence. There is moderate‐certainty evidence, however, that number of falls were probably reduced by 21% compared with control.
Regarding non‐critical outcomes, mobility strategies may improve sit to stand ability (low‐certainty evidence), and increase muscle strength (high‐certainty evidence). There may be little or no effect on the need for a walking aid or objective measures of balance.
Resource use was difficult to establish. The number of physiotherapy sessions conducted varied greatly between studies and there was little reporting of other resource use.
Types of interventions
Interventions that include training comprising gait, balance and functional tasks were effective in increasing mobility in the post‐hospital setting (high‐certainty evidence).
There was low‐certainty evidence that resistance training may also increase mobility (measured in distance) and functioning in the post‐hospital setting.
Interventions containing multiple categories of exercise from the ProFaNE taxonomy (resistance or endurance training in addition to gait, balance and functional training), probably improve mobility post‐hospital (moderate‐certainty evidence).
The effect of endurance training interventions is unclear as we assessed the certainty of evidence as very low for many of the outcomes.
No studies evaluated the effect of other forms of exercise or electrical stimulation on the critical outcome of mobility.
Subgroup analyses
There were sufficient studies to conduct subgroup analyses for three outcomes: walking speed, health‐related quality of life and strength. There was probably little or no difference in the effect of mobility strategies on gait speed, health‐related quality of life and strength in trials where the intervention was delivered in an outpatient setting versus secondary and social care setting or delivered in trials with a mean participant age of 80 years or less versus more than 80 years. Subgroup analysis found a larger effect of mobility strategies on strength outcomes in trials where participants were excluded if they had impaired cognition compared with trials where participants were not excluded; however, this subgroup effect was not evident for gait speed and health‐related quality of life outcomes.
Economic data
Only two of the 40 studies in this review reported economic data, with the single cost‐effectiveness analysis of home exercise targeting gait and balance finding no evidence of the intervention being cost‐effective from the comparison of incremental costs and QALYs eight months after randomisation (Taraldsen 2019).
Overall completeness and applicability of evidence
Trial design and participants
We have provided additional details on the study populations and interventions in Table 5, Table 6, Appendix 5 and Appendix 6.
The participants were post‐hip fracture, primarily women (80%) and of a range of ages. Participant characteristics varied markedly due to the methods of recruitment and inclusion and exclusion criteria.
The majority of trials excluded older people who were cognitively impaired (70%) or had a history of immobility, medical conditions affecting mobility or both (72%). The results of this review may therefore not be applicable to these high‐risk groups. The majority of trials were relatively small (median = 81 participants), with a mean age of 80 (ranging from a mean age of 71 to a maximum mean age of 90 years).
In the 18 in‐hospital trials, six reported follow‐up at discharge, 12 reported follow‐up beyond discharge, including two that reported outcomes at 12 months. In the 22 post‐hospital trials, nine reported follow‐up at one to three months, six reported follow‐up at four to six months, one at nine months and six reported 12‐month follow‐up. Trials were undertaken over a period of 58 years from 1961 to 2019.
Setting
We included a further 21 RCTs of interventions for improving mobility after hip fracture surgery in this review update compared with Handoll 2011. The trials were conducted in 17 countries using a variety of healthcare models: differences in healthcare provision and policies, including the type of surgery and the extent of support post‐hospital discharge, may impact the effectiveness of some interventions. There is a lack of trials undertaken in low‐income countries, residential aged care settings and social care settings.
Interventions
We classified the exercise interventions using the ProFaNE classification system. While this classification system is well described (Lamb 2011, Appendix 1), there is a degree of subjectivity when classifying the interventions in the presence of brief descriptions in trial reports. The duration of the intervention in the in‐hospital trials ranged from two to 16 weeks. In the post‐hospital studies, the duration of the intervention ranged from one month to one year, with 50% of trials delivering their intervention for three to four months, and 27% of trials delivering the intervention for 12 months.
The pooling of many studies into such categories does not readily inform decisions about which interventions to choose in practice. We suggest that practitioners examine the details of the intervention and comparator in individual trials that are effective, taking into account any risk of bias, to help inform which particular interventions within an effective category may be applicable in their setting.
It would be useful if we were able to provide more information on individual aspects of intervention programmes, including their intensity. Unfortunately, this is not possible given variation in reporting and the likely variability of these factors within trials. Future trials could explore optional intensity of therapies, as both under‐ and over‐treatment could involve risks for those with complex chronic conditions.
Comparisons
Some difficultly may arise in interpreting results from these analyses as outcomes are pooled as comparisons against conventional care (for in‐hospital studies) or against conventional care, sham or no exercise (in post‐hospital studies). As the studies have been conducted in many different nations, over an extended period of time (1961 to 2020), conventional care will vary considerably over time, and therefore applicability to a particular, current, local context may be difficult to determine. In some trials, which interventions make up the control group (particularly where it is conventional care) is not clearly reported.
We suggest that readers examine the details of trials as described in Table 5, Table 6, Appendix 5 and Appendix 6 to determine which trials in particular are the most applicable to their local context, in terms of setting and conventional care approaches.
Outcomes
We sought data for the critical outcomes using mobility measures (analysed as mobility scales, outcomes measured in seconds and outcomes measured in distance), walking speed, functioning, health‐related quality of life, mortality, number of people who experienced five specified adverse events (with re‐admission shown on the summary of findings table), and return to living at the pre‐fracture residence (in‐hospital studies). However, few studies provided health‐related quality of life, adverse event or return to residence data.
We sought minimal clinically important differences for the critical outcomes. We re‐expressed mobility, measured using mobility scales, using the 12‐point Physical Performance and Mobility Examination (PPME) in the in‐hospital setting. The mean point estimate of effect (1.46 points) exceeded the minimal important difference for PPME, which is typically 1.13 to 2.15 (de Morton 2008). Likewise in the post‐hospital setting, where we re‐expressed the mobility result using the 12‐point Short Physical Performance Battery, the mean point estimate of the effect of the intervention (0.89 points) exceeded the small meaningful change (0.27 to 0.55 points) but was less than the substantial meaningful change of 0.99 to 1.34 points reported by Perera 2006.
Mobility training interventions increased walking speed in excess of the minimal important difference in both the in‐hospital (0.05 metres/second (m/s)) and post‐hospital (0.05 m/s) settings, with small meaningful change for gait speed being 0.04 to 0.06 m/s (Perera 2006). The minimal important difference for functioning was not reached in the in‐hospital or post‐hospital analyses, when the results were re‐expressed using the Barthel Index. Minimal important difference (post‐hip surgery) is typically 9.8 points (Unnanuntana 2018).
The mean minimal important difference for quality of life has been reported as 0.074 on the EQ‐5D (Walters 2005), or as 3 to 5 on the SF‐36 (Walters 2003). Mobility interventions delivered post‐hospital had a mean point estimate of effect below these values, when converted to these quality of life scales (reported converted values in‐hospital EQ‐5D = 0.03; post‐hospital EQ‐5D = 0.01; SF‐36 = 3).
We prespecified that, in addition to the main outcomes, we would also report mobility in terms of walking aids, subjective mobility, balance and sit to stand. We also reported muscle strength, activities of daily living, lower‐limb or hip function and participant satisfaction outcomes.
For in‐hospital trials in this review, we selected the outcome closest to four months post‐intervention for analysis. In some cases, this decision excluded data at different time points, and for other trials, the data included are actually for a shorter or longer intervention time. This may reduce the applicability of the 4‐month time point to practice and does mean that information from some trials on shorter and longer time periods has not been used within this review. For post‐hospital trials, we selected the outcome at the end of the intervention period.
Other considerations relating to applicability
Table 7 shows our assessments for each trial of five aspects of relevance to ascertaining external validity: definition of the study population, description of the interventions, definition of primary outcome measures, length of follow‐up, assessment of compliance.
In some studies there were incomplete descriptions of study inclusion (three trials), interventions (eight trials) or outcomes (five trials), limiting the ability to determine the applicability or details of results of these trials. We considered the timing of outcome measurement as suboptimal in 31 trials, and especially in those where participants were followed up to either hospital discharge or only until the end of the intervention. Some assessment of compliance with allocated interventions or control interventions was reported in sixteen trials, but ten other trials which reported compliance only did so for the active intervention group(s).
Certainty of the evidence
This review provides very low‐ to high‐certainty evidence of the effectiveness of interventions for improving mobility after hip fracture surgery in adults.
We have summarised the GRADE certainty of evidence in four summary of findings tables:
Table 1 (mobility strategy versus control in the in‐hospital setting);
Table 2 (different types of interventions on mobility outcome, in hospital);
Table 3 (mobility strategy versus control in the post‐hospital setting);
Table 4 (different types of interventions on mobility outcome, post‐hospital).
The certainty of the evidence for different outcomes across settings ranged from very low to high. We downgraded the level of evidence by one level for risk of bias if the results changed upon removal of the trials with a high risk of bias on one or more domains. We did not downgrade for risk of bias where removing studies with high risk of bias in one or more domains changed the point estimate to a stronger effect with narrower confidence intervals, or to a similar effect with wider confidence intervals. We downgraded one level for inconsistency if heterogeneity exceeded 60%, but not where this was explained by subgroup or sensitivity analyses. We downgraded by one or two levels for imprecision in the presence of wide confidence intervals, or where there were too few participants or events. We downgraded the level of evidence one level for return to pre‐fracture residence as a large number of trials did not contribute to the outcome.The funnel plots in Figure 4, Figure 5 and Figure 6 do show some asymmetry; however, we did not consider the asymmetry sufficient to downgrade the level of evidence.
Sensitivity analyses indicate the results for the mobility outcome are stable to risks of bias associated with allocation concealment and participant selection. In several instances, exclusion of studies at high risk of bias increased the effect estimates, providing stronger support for conclusions of effectiveness. During the GRADE assessment, we downgraded the certainty of evidence based on sensitivity analysis for risk of bias (removal of trials with one or more domains at high risk of bias) for three outcomes in both the in‐hospital and post‐hospital analyses (mobility, functioning and health‐related quality of life).
This review’s analyses of critical outcomes display minimal to substantial heterogeneity with P < 0.05 for the Chi2 test and I2 values up to 81%. We believe this likely represents between‐study differences in the nature of programmes (e.g. adherence, dose, intensity) and target populations, which was not explained by our subgroup analyses and necessitates further investigation. Considering the stability of results, we do not believe this undermines the meta‐analyses we have undertaken.
One consideration in interpreting the certainty of the evidence is that the evaluation of rehabilitation interventions is difficult to do well. These are generally complex interventions with considerable variation in practice, including the often adaptive nature of rehabilitation, where treatment is varied according to the perceived needs and progress of individual patients. Some aspects of trial methodology, notably concealment of allocation, are possible but others, such as blinding, are more of a challenge for these trials. In particular, blinding of participants is not possible in trials of many physical interventions such as exercise. Blinding of outcome assessors is possible for tests of mobility but not for self‐reported outcomes where the participant is effectively the outcome assessor. Thus, we have based judgements on whether risk was minimised in the different types of outcomes.
Potential biases in the review process
We designed this review to minimise the risk of potential biases. We used multiple databases to conduct a comprehensive search of the published literature and searched clinical trial registries for completed studies not previously identified. Two review authors independently undertook screening, data extraction and risk of bias assessments in duplicate. We acknowledge some relevant trials may have been missed despite this thorough search strategy, especially if they were published only in conference proceedings or in languages other than English.
While we consider that we have included and excluded trials appropriately, the variety and complexity of trial interventions encountered in the eligible trials made it difficult to apply our criteria in some instances. Indeed, we sometimes progressed to the point of data extraction with trials that we subsequently realised were not suitable. These have required us to reconsider and clarify our inclusion criteria, such as setting a limit on the time for starting the intervention at one year post‐fracture. We have also excluded trials that tested multifactorial interventions or primarily focused on elective hip surgery. The reason for excluding the first category is that it is not possible to separate out the effects of the mobilisation component of multifactorial interventions. Although the aim of these trials is to restore or augment function, we have kept our focus on mobilisation and mobility. These latter outcomes remain key objectives for people after hip fracture surgery. The exclusion of trials focusing on elective hip replacement surgery reflects that these populations are likely to differ in important ways to the generally older and frailer populations sustaining a hip fracture.
The previous version of this review deemed meta‐analysis inappropriate because of the differences in the included trials in terms of trial participants, settings, interventions or a combination of these (Handoll 2011). With the addition of 21 trials in the current update, the categorisation into two established intervention stages (in‐hospital and post‐hospital), and modification of the outcome measures (in response to a commissioning brief generated in relation to the Cochrane Programme Grant on the management of hip fracture), we judged it appropriate to pool data in meta‐analyses in this update. As the presentation of different interventions separately is useful for clinicians, we have also presented the effects of different interventions separately in addition to the overall results.
The variation in the broad mobility and function outcome measures used by different trials necessitated the use of standardised mean differences to meta‐analyse these outcomes, which can be difficult to interpret. We consider that the pooling of data for different measures of mobility and functioning is of value from the more general perspective of informing health funders and managers on the likely effectiveness of the interventions. The consistently‐measured walking outcomes did, however, enable comparison, with accepted cutoffs for clinically meaningful changes in gait speed.
Lastly, one of the authors (Catherine Sherrington) was the lead investigator of four trials included in the review (Sherrington 1997; Sherrington 2003; Sherrington 2004; Sherrington 2020), and a co‐investigator on Moseley 2009. Processing of these trials was carried out by other review authors to avoid conflict of interest.
Agreements and disagreements with other studies or reviews
Our review of the importance of interventions for improving mobility after hip fracture surgery in adults extends the findings of Handoll 2011 by pooling results from multiple studies and by categorising exercise intervention programmes to determine the primary exercise component for each included trial (Appendix 1).
Multiple systematic reviews have assessed the effect of interventions on mobility outcomes following hip fracture. These reviews identified the same trials included in this review, in addition to a number of non‐randomised controlled trials. McDonough 2021 provided a comprehensive overview of relevant systematic reviews in their recently published clinical practice guidelines, 'Physical therapy management of older adults with hip fracture' (McDonough 2021).
A 2016 meta‐analysis of 13 trials evaluating the effect of structured exercise on mobility after hip fracture found small improvements in mobility after hip fracture (Diong 2016).
Beckmann 2020 conducted a systematic review and meta‐analysis including nine RCTs of exercise interventions started within the first three months after hip fracture. Findings were generally consistent with this review; the authors found high‐ to moderate‐certainty evidence that the intervention improved physical function, despite high heterogeneity (I2 = 92%). Eight of the included trials were also included in this review (Binder 2004; Hauer 2002; Kimmel 2016; Kronborg 2017; Monticone 2018; Moseley 2009; Sherrington 2003; Van Ooijen 2016); one of the trials (Mendelsohn 2008) was excluded from this review as it was an upper‐body exercise programme focused on cardiovascular fitness rather than being a mobilisation strategy. Two of the included trials were categorised as post‐hospital interventions in this review (Binder 2004; Hauer 2002).
Kuijlaars 2019 and Chen 2019 conducted systematic reviews and meta‐analyses of home‐based exercise interventions following hip fracture. Kuijlaars 2019 included six trials conducted in older people, all of which were included in this review as post‐hospital interventions (Latham 2014; Mangione 2005; Mangione 2010; Orwig 2011; Salpakoski 2015; Sherrington 1997), and found limited evidence for improvements in performance‐based activities of daily living, and over the long term for fast gait speed. Chen 2019 included eleven trials; seven were included in this review (Binder 2004; Latham 2014; Mangione 2005; Mangione 2010; Sherrington 1997; Sherrington 2004; Tsauo 2005), four were excluded (one due to hip fracture on average three years prior to the trial (Edgren 2012), one as it was a trial of early discharge (Crotty 2002) and two had multi‐component interventions (Tinetti 1999; Zidén 2008). They found that the effect on physical function was not significant, although there was a significant improvement in leg strength and the 6‐Minute Walk Test.
Lee and colleagues conducted two systematic reviews and meta‐analyses of randomised controlled trials of the effects of exercise interventions in improving outcomes following hip fracture surgery (Lee 2017; Lee 2019). Lee 2017 examined the effects of lower‐limb progressive resistance exercise and included eight RCTs. The authors reported a significant improvement in mobility, activities of daily living, balance and lower‐limb strength or power with the intervention. Four included trials were also included in this review (Mangione 2005; Mangione 2010; Sylliaas 2011; Sylliaas 2012). We excluded Sylliaas 2012 from our meta‐analysis as it included a subgroup of participants from an earlier trial (Sylliaas 2011). Four other trials were excluded from this review: two as the participants sustained their hip fracture on average more than one year prior to the trial (Edgren 2012: mean of 3 years; Portegijs 2008: mean of 4.4 years), and two trials as they examined multifactorial interventions in which the effects of the mobilisation strategy could not be distinguished from the other intervention components (Peterson 2004a; Singh 2012).
Lee 2019 included eight RCTs of balance training and concluded that the intervention significantly improves overall physical functioning, balance, gait, lower‐limb strength, activities of daily living and health‐related quality of life. Seven of these trials were also included in this review (Binder 2004; Hauer 2002; Latham 2014; Moseley 2009; Monticone 2018; Sherrington 1997; Sherrington 2004). We excluded Peterson 2004a from this review as it examined a multifactorial intervention; this trial was included in both the progressive resistance and balance meta‐analysis by Lee and colleagues. Wu J 2019 included nine RCTs of balance training with similar results.
The fall‐prevention impact of mobility strategies in the post‐hospital population is consistent with the results of a previous Cochrane Review in community‐dwelling older people (Sherrington 2019).
Authors' conclusions
Implications for practice.
In the in‐hospital setting, interventions targeting improvement in mobility after hip fracture surgery in adults may improve mobility (low‐certainty evidence), and probably improve walking (moderate‐certainty evidence) compared with conventional care, respectively (Table 1). The effects of mobility strategies are less certain for other main outcomes, mainly reflecting the low number of studies and participants. There is low‐certainty evidence that mobility strategies may make little or no difference to mortality, re‐admission and return to living at the pre‐fracture residence. We are uncertain whether mobility strategies improve functioning or health‐related quality of life as the certainty of the evidence is very low.
In the post‐hospital setting, the evidence for the use of additional mobility strategies to improve outcomes after discharge following hip fracture surgery has greater certainty than for the in‐hospital setting. There is high‐certainty evidence that mobility strategies lead to a meaningful increase in mobility compared to control (usual care, no intervention, sham exercise or social visit). Mobility strategies also lead to a small improvement in functioning, which is not meaningful (high‐certainty evidence), and mobility strategies probably cause meaningful improvement in walking speed (moderate‐certainty evidence). The effects of mobility strategies are less clear for other main outcomes, mainly reflecting under‐reporting of these outcomes in the included trials. Mobilisation strategies probably make no difference to short‐term mortality, may make little or no difference to adverse outcomes of long‐term mortality or re‐admission, and probably lead to a slight, non‐meaningful increase in health‐related quality of life.
Pooled data examining the effect of the intervention versus control do not capture the details of the certainty of evidence for all the plausible individual comparisons. We attempted to address this by exploring the effects of different intervention types. In the included in‐hospital and post‐hospital trials, interventions that included gait, balance and functional tasks had moderate‐ and high‐certainty evidence for effectiveness at increasing mobility. In the post‐hospital setting, mobility may also be increased by resistance or endurance training in addition to gait, balance and functional training. Readers may wish to examine further details of the intervention and control arms of individual trials presented in Table 5 and the Description of studies.
Implications for research.
The presence of ongoing trials points to the importance of maintaining this review, but further primary research in the form of sufficiently‐powered, preferably multicentre, high‐quality randomised controlled trials is also required to inform practice. Such research should focus on interventions that are likely to have a beneficial overall, long‐term impact; thus, trials should have long‐term (one year or more) and comprehensive follow‐up, including the collection of validated and patient‐orientated outcome measures, and economic outcomes. Given the investment required for such trials, priority questions and areas need to be identified. We consider that this endeavour should be open to general debate, but some clues can be gained from this review and the following considerations.
This review already gives some indication of the variety of questions that clinicians consider important and have, we assume, successfully justified to ethics committees and, often, to funders. With some exceptions, such as Graham 1968, the control arm of which is not relevant to current practice, the questions evaluated incompletely by these trials remain pertinent. Some can be considered as pilot studies and after appropriate adjustments, such as to the study design, power and perhaps to the interventions, a potentially more informative trial will emerge.
Further research is needed to determine the relative impact of different types of exercise programmes. These studies must be very large to be adequately powered to detect differences in effects between interventions.
Further work is required to establish the effectiveness of rehabilitation after hip fracture in emerging economies, and in Asia where hip fractures are increasing most rapidly (Gullberg 1997).
It is debatable whether future research priorities should be on the evaluation of multi‐faceted or multi‐component interventions (excluded from this review when not solely aimed at mobilisation) with mobilisation components, rather than mobilisation interventions or programmes by themselves. This is particularly relevant to rehabilitation after discharge from hospital, which is an increasingly important area. Lessons from the literature on fall prevention (Cameron 2018; Sherrington 2019) and strength training (Liu 2009) in older people may be applicable here as well as generally to rehabilitation after hip fracture surgery. We consider, however, that it is still useful to investigate mobilisation strategies in themselves, particularly as these will form a substantive part of any rehabilitation intervention for this patient group.
Some consideration of these trials' results must be given to the differences in the physical and mental capacities of people with hip fracture. Different interventions may be suitable for different subgroups of hip fracture patients: for instance, the more frail versus more physically able. Thus, trials could also investigate whether differing responses to interventions occur among different subgroups of hip fracture patients. Of course such investigations should take into account methodological concerns about excessive subgroup analyses in clinical trials and prespecify subgroups and use appropriate statistical techniques (Sun 2010).
Validated patient‐orientated outcome measures are needed, to measure what is important for individual patients. Development of a standard portfolio of validated and patient‐orientated outcome measures for trials would facilitate meta‐analysis of the results of future trials.
What's new
| Date | Event | Description |
|---|---|---|
| 8 May 2021 | New citation required and conclusions have changed | 1. Authorship of the review has changed. 2. The conclusions of the review were revised to give a more appropriate emphasis to optimal strategies. |
| 8 May 2021 | New search has been performed | For this update, the main changes are: 1. Search update to March 2021. 2. Twenty‐one trials, including a total of 2470 participants, were newly included in this update. Six were in‐hospital trials and 15 were post‐hospital rehabilitation trials. 3. Study selection resulted in the exclusion of 18 trials, the placement of 21 trials in ongoing studies and two trials in studies awaiting classification. 4. Restructured list of outcomes. 5. Categorised exercise and physical training interventions using the ProFaNE classification. 6. Assessed four additional sources of bias. 7. Added four new subgroup analyses. 8. Enhanced descriptions of study populations and interventions. 9. Adopted new review format and updated Background, Discussion and Conclusion. |
History
Protocol first published: Issue 3, 1999 Review first published: Issue 3, 2000
| Date | Event | Description |
|---|---|---|
| 24 July 2008 | Amended | Converted to new review format. |
| 31 October 2006 | New citation required and conclusions have changed | The main changes for the fourth update of this review, published Issue 1, 2007, were as follows.
1. Date of search for trials was extended to January 2006.
2. Three studies were newly included (Binder 2004; Tsauo 2005; Mangione 2005), one of which was previously waiting assessment (Mangione 2005, formerly Mangione 2001) and one was previously an ongoing study (Binder 2004, formerly Binder 2001). All three trials took place after hospital discharge.
3. A study which was previously ongoing (Crotty 2003) has become Miller 2006 and is awaiting assessment.
4. One study (Braid 2001) previously listed as ongoing is now excluded.
5. Two newly identified studies were excluded (Licciardone 2004; Shyu 2005).
6. Adjustments were made to text and tables to conform to revised methodology and the Cochrane Style Guide.
7. The conclusions of the review were revised to accommodate the new studies.
8. Authorship of the review has changed. For details of previous updates, please see 'Notes'. |
Notes
This review is an expansion of the scope of the review described in the title of the protocol 'Early weight bearing and mobilisation after internal fixation of intracapsular proximal femoral fractures in adults'.
The main changes for the first update of this review, published Issue 2, 2002, were:
date of search for trials was extended to February 2002;
one new study (Mitchell 2001) of quadriceps muscle training was included;
of the other seven newly identified studies, one was excluded, two were placed in 'Ongoing studies' and four were placed in 'Studies awaiting assessment';
there was no substantive change to the conclusions of the review.
The main changes for the second update of this review, published Issue 1, 2003, were:
date of search for trials was extended to October 2002;
one new study (Lauridsen 2002) evaluating intensive physiotherapy was included;
two newly identified studies were excluded (Barber 2002; Hauer 2002);
additional details/results were added from the full publication of Lamb 2002, formerly Lamb 1998;
availability of the full publication of Kuisma 2002, formerly Johnstone 1999, resulted in its exclusion;
the identification of 3 more ongoing trials (Cameron 2004; Crotty 2003; Sherrington 2002);
there was no substantive change to the conclusions of the review.
The main changes for the third update of this review, published Issue 4, 2004, were:
expansion of the scope of the review to cover interventions aimed at initiating and enhancing mobilisation throughout the whole rehabilitation process;
types of outcome measures and the order of presentation of the trials were revised upon reconsideration of the new scope of the review;
date of search for trials was extended to May 2004;
four studies were newly included. One (Sherrington 1993) applied to the early postoperative period; the other three (Hauer 2002; Sherrington 2004; Sherrington 1997) took place after hospital discharge;
four newly identified studies were excluded (Crotty 2002; Hesse 2003; Lehmann 1961; Tinetti 1999);
two previously ongoing studies are now excluded (Allegrante 2001; Maltby 2000) as is one trial previously awaiting assessment (Johnston 1995);
one trial (Binder 2001) previously awaiting assessment is now listed as an ongoing study;
one newly identified study (Mangione 2001) awaits assessment;
various changes were made to comply with the Cochrane Style Guide;
the conclusions of the review were revised to accommodate the new scope of the review.
The main changes for the fourth update of this review, published Issue 1, 2007, were:
date of search for trials was extended to January 2006.
three studies were newly included (Binder 2004; Tsauo 2005; Mangione 2005), one of which was previously waiting assessment (Mangione 2005, formerly Mangione 2001) and one was previously an ongoing study (Binder 2004, formerly Binder 2001). All three trials took place after hospital discharge;
a study which was previously ongoing (Crotty 2003) has become Miller 2006 and is awaiting assessment;
one study (Braid 2001) previously listed as ongoing is now excluded.
The main changes for the fifth update of this review, published Issue 3, 2011, were:
updated title to reflect better the scope of the review;
trials testing interventions started after the generally perceived recovery of around one year are now excluded;
trials testing mobilisation strategies with nutrition as a co‐intervention are included;
types of outcomes were restructured, with the categorisation of primary and secondary outcomes;
risk of bias was assessed using the Cochrane risk of bias tool, replacing assessment of 10 aspects of methodological quality.
Acknowledgements
For the current (sixth) update, we thank Helen Handoll, lead author on previous versions of this review, for the expert guidance in the methods section of this update. We thank Liz Bickerdike, Sharon Lewis and Joanne Elliott for their comments and help at editorial review, and Maria Clarke for her help with the literature searches. We thank Christine McDonough and Mattia Morri (external referees) and Janet Wale (consumer reviewer) for their helpful feedback.
The Acknowledgements for previous versions of this review can be found in Appendix 11.
This project was funded and supported by the National Institute for Health Research (NIHR). The views and opinions expressed herein are those of the review authors and do not necessarily reflect those of the Systematic Reviews Programme, the NIHR, the National Health Service or the Department of Health.
Editorial and peer‐reviewer contributions
Cochrane Bone, Joint and Muscle Trauma (BJMT) Group supported the authors in the development of this review.
The following people conducted the editorial process for this article:
Sign‐off Editor (final editorial decision): Xavier Griffin, Co‐ordinating Editor, Cochrane BJMT Group
Editor (advised on methodology and review content, edited the article): Sharon Lewis, Deputy Co‐ordinating Editor, Cochrane BJMT Group
Methodological Editor (advised on methodology and review content): Liz Bickerdike, Cochrane Acute and Emergency Care Network Associate Editor
Managing Editor (selected peer reviewers, collated peer‐reviewer comments, provided editorial guidance to authors, edited the article): Joanne Elliott, Managing Editor, Cochrane BJMT Group
Information Specialist (developed search strategy, advised on search methods): Maria Clarke, Information Specialist, Cochrane BJMT Group
Copy Editor (copy‐editing and production): Faith Armitage, Copy Edit Support
Peer‐reviewers (provided comments and recommended an editorial decision): Christine McDonough, Mattia Morri (clinical reviewers) and Janet Wale (consumer reviewer)
Appendices
Appendix 1. Categorisation of interventions using ProFaNE
| Exercise category | ProFaNE description | How we applied the category criteria in this reviewa,b |
| Gait, balance and functional training | Gait training involves specific correction of walking technique (e.g. posture, stride length and cadence) and changes of pace, level and direction. Balance training involves the efficient transfer of bodyweight from one part of the body to another or challenges specific aspects of the balance systems (e.g. vestibular systems). Balance retraining activities range from the re‐education of basic functional movement patterns to a wide variety of dynamic activities that target more sophisticated aspects of balance. Functional training uses functional activities as the training stimulus, and is based on the theoretical concept of task specificity. All gait, balance and functional training should be based on an assessment of the participant’s abilities prior to starting the programme; tailoring of the intervention to the individuals abilities; and progression of the exercise programme as ability improves. | Selected as exercise category if the intervention met the baseline assessment, tailoring and progression criteria. Selected as primary category for interventions where most exercises were conducted standing and where the intervention focus and most time spent was on exercise in this category. We classed programmes that included treadmill walking as this category, if the treadmill training involved specific correction of walking technique. |
| Strength/resistance (including power) | The term ’resistance training’ covers all types of weight training i.e. contracting the muscles against a resistance to ‘overload’ and bring about a training effect in the muscular system. The resistance is an external force, which can be one’s own body placed in an unusual relationship to gravity (e.g. prone back extension) or an external resistance (e.g. free weight). All strength/resistance training should be based on an assessment of the participant’s abilities prior to starting the programme; tailoring the intervention to the individual’s abilities; and progression of the exercise programme as ability improves. | Selected as exercise category if the intervention met the baseline assessment, tailoring and progression criteria. Selected as primary category for interventions where additional resistance was used or where it was clear that overload was sufficient without external resistance and where the intervention focus and most time spent was on exercise in this category. Electrical stimulation as a single intervention was not included in this category. |
| Flexibility | Flexibility training is the planned process by which stretching exercises are practised and progressed to restore or maintain the optimal range of movement (ROM) available to a joint or joints. The ranges of motion used by flexibility programmes may vary from restoration/maintenance of the entire physiological range of motion, or alternatively, maintenance of range that is essential to mobility or other functions. | Selected as exercise category if the intervention met the progression of stretching criterion. Selected as primary category for interventions where flexibility training was a stated aim of the intervention and where the intervention focus and most time spent was on exercise in this category. |
| 3D | 3D training involves constant movement in a controlled, fluid, repetitive way through all three spatial planes or dimensions (forward and back, side to side, and up and down) . Tai Chi and Qi Gong incorporate specific weight transferences and require upright posture and subtle changes of head position and gaze direction. Dance involves a wide range of dynamic movement qualities, speeds and patterns. | Selected as exercise category if the intervention involved Tai Chi or dance. Selected as primary category for interventions where the intervention focus and most time spent was on exercise in this category. |
| General physical activity | Physical activity is any bodily movement produced by skeletal muscle contraction resulting in a substantial increase in energy expenditure. Physical activity has both occupational, transportation and recreational components and includes pursuits like golf, tennis and swimming. It also includes other active pastimes such as gardening, cutting wood and carpentry. Physical activity can provide progressive health benefits and is a catalyst for improving health attitudes, health habits and lifestyle. Increasing habitual physical activity should be with specific recommendations as to duration, frequency and intensity if a physical or mental health improvement is indicated. | Selected as exercise category if the intervention included unstructured physical activity. We classed programmes that included un‐structured walking as this category. Selected as primary category for interventions where the intervention focus and most time spent was on exercise in this category. |
| Endurance | Endurance training is aimed at cardiovascular conditioning and is aerobic in nature and simultaneously increases the heart rate and the return of blood to the heart. | Selected as exercise category if the intervention focused on structured aerobic training. We classed programmes that included treadmill walking as this category if the treadmill training did not involve specific correction of walking technique. Selected as primary category for interventions where the intervention focus and most time spent was on exercise in this category. |
| Other | Other kinds of exercises not described | Selected as exercise category if the intervention did not meet the other categories listed and where the intervention focus and most time spent was on exercise in this category. |
aInterventions were allocated a secondary category if some but not all criteria were met by the intervention or where the category was not the primary focus of the intervention, or both. bThese criteria were used in Sherrington 2019.
Appendix 2. Outcome measures
| Outcome | Aspects measured | Examples of measurement instruments |
| GRADE critical outcomes | ||
| Mobility | Mobility scales, seeking to measure multiple aspects of mobility, e.g. standing up, walking and stair climbing | Short Physical Performance Battery, Physical Performance and Mobility Examination, Elderly Mobility Scale, Parker Mobility Score |
| Timed tasks incorporating multiple aspects of mobility, e.g. standing up, walking and stair climbing, measured in seconds | Timed Up and Go test | |
| Timed tasks incorporating multiple aspects of mobility, e.g. standing up, walking and stair climbing, endurance, measured in minutes | 6‐Minute Walk Test | |
| Dichotomous outcomes | ||
| Self‐report outcomes | ||
| Walking speed | Timed walk | Timed 4‐Metre Walk Test, timed 6‐Metre Walk Test |
| Functioning | Functioning scales | Canadian Occupational Performance Measure, Nottingham Extended Activities of Daily Living scale |
| Health‐related quality of life | SF‐36, EQ‐5D | |
| Mortality | Early (< 4 months) and late (> 4 months) | |
| Adverse events | i) Re‐admission | |
| ii) Re‐operation | Unplanned return to operating theatre | |
| iii) Surgical complications | Non‐union, avascular necrosis, thromboembolic complications | |
| iii) Falls | Number of falls, number of people who experienced one or more falls | |
| ii) Pain | Persistent hip or lower‐limb pain at the final follow‐up assessment. Verbal rating or visual analogue score (VAS) | |
| Return to living at home versus residence in aged care facility (in‐hospital studies only) | ||
| GRADE important outcomes | ||
| Mobility: walking | Use of walking aid/need for assistance | |
| Self‐reported outcomes | Self‐reported difficulty walking a specified distance, e.g. 400 m | |
| Mobility: balance while standing, reaching and stepping | Balance while reaching | Functional Reach |
| Balance while stepping | Number of steps in specified time | |
| Balance while standing with different foot positions | Timed tandem stance, timed single leg stand | |
| Balance scales | Berg Balance Scale | |
| Balance using self‐report | ||
| Mobility: sit to stand | Timed sit to stand | Time to sit to stand 5 times |
| Muscle strength | One measure of affected leg from each study, with priority for quadriceps | |
| Activities of daily living | Activities of daily living scales | Barthel Index, Functional Independence Measure |
| Lower‐limb/hip function | Validated patient‐reported measures of lower‐limb or hip function | Hip Rating Questionnaire, Harris Hip Score, Oxford Hip Score, Merle D’Aubigne Hip Score |
| Patient satisfaction | i) Acceptability of interventions | |
| ii) Adherence | Porportion of intervention sessions completed, estimate of adherence, proportion of repetitions completed | |
| Resource outcomes | ||
| Resources | i) Length of hospital stay | Number of days |
| ii) Number of physiotherapy sessions | Number of sessions | |
| iii) Number of outpatient attendances | Number of attendances | |
| iv) Need for special care | ||
| Economic outcomes | ||
| Cost‐effectiveness | Summarise cost‐analyses reported by the included trials | |
Appendix 3. Search strategies
We carried out the CENTRAL, MEDLINE, Embase and CINAHL searches in four stages: the first search was run from January 2010 to March 2016; top‐up searches were run from March 2016 to April 2019, April 2019 to March 2020 and March 2020 to March 2021.
CENTRAL (CRS Online): 2016 Issue 3
Search 1
#1 MESH DESCRIPTOR Hip Fractures EXPLODE ALL TREES (962) #2 (((hip* or ((femur* or femoral*) adj3 (neck or proximal))) adj4 fracture*)):TI,AB,KY (2219) #3 #1 OR #2 (2219) #4 MESH DESCRIPTOR Physical Therapy Modalities EXPLODE ALL TREES (16078) #5 MESH DESCRIPTOR Exercise EXPLODE ALL TREES (15526) #6 MESH DESCRIPTOR Exercise Therapy EXPLODE ALL TREES (7925) #7 MESH DESCRIPTOR Rehabilitation (242) #8 MESH DESCRIPTOR Early ambulation (284) #9 MESH DESCRIPTOR Gait (1312) #10 MESH DESCRIPTOR Electric Stimulation Therapy (1416) #11 MESH DESCRIPTOR Electric Stimulation (1591) #12 ((quadriceps or muscle or strength or gait or resistance) adj3 (training or retraining)):TI,AB,KY (6501) #13 ((electric* adj3 stimulat*) or neurostimulat*):TI,AB,KY (6083) #14 (physiotherapy or physical therapy):TI,AB,KY (7354) #15 exercis*:TI,AB,KY (46629) #16 ((early or delayed) adj3 (weight bearing or mobili* or ambulation)):TI,AB,KY (847) #17 #4 OR #5 OR #6 OR #7 OR #8 OR #9 OR #10 OR #11 OR #12 OR #13 OR #14 OR #15 OR #16 (63888) #18 #3 AND #17 (222)
Search 2 (top‐up search)
CENTRAL (CRS web): 2019 Issue 4
1. MESH DESCRIPTOR Hip Fractures EXPLODE ALL AND CENTRAL:TARGET (1127) 2. (((hip* or ((femur* or femoral*) NEAR3 (neck or proximal))) NEAR4 fracture*)): AB,EH,KW,KY,MC,MH,TI,TO (3964) 3. #1 OR #2 (4122) 4. MESH DESCRIPTOR Physical Therapy Modalities EXPLODE ALL AND CENTRAL:TARGET (20266) 5. MESH DESCRIPTOR Exercise EXPLODE ALL AND CENTRAL:TARGET (17932) 6. MESH DESCRIPTOR Exercise Therapy EXPLODE ALL AND CENTRAL:TARGET (10351) 7. MESH DESCRIPTOR Rehabilitation AND CENTRAL:TARGET (351) 8. MESH DESCRIPTOR Early ambulation AND CENTRAL:TARGET (320) 9. MESH DESCRIPTOR Gait AND CENTRAL:TARGET (1604) 10. MESH DESCRIPTOR Electric Stimulation Therapy AND CENTRAL:TARGET (1673) 11. MESH DESCRIPTOR Electric Stimulation AND CENTRAL:TARGET (1730) 12. ((quadriceps or muscle or strength or gait or resistance) NEAR3 (training or retraining)): AB,EH,KW,KY,MC,MH,TI,TO (14344) 13. ((electric* NEAR3 stimulat*) or neurostimulat*): AB,EH,KW,KY,MC,MH,TI,TO (10112) 14. (physiotherapy or physical therapy): AB,EH,KW,KY,MC,MH,TI,TO (15315) 15. exercis*: AB,EH,KW,KY,MC,MH,TI,TO (85690) 16. ((early or delayed) NEAR3 (weight bearing or mobili* or ambulation)): AB,EH,KW,KY,MC,MH,TI,TO (1675) 17. #4 OR #5 OR #6 OR #7 OR #8 OR #9 OR #10 OR #11 OR #12 OR #13 OR #14 OR #15 OR #16 (113638) 18. #3 AND #17 (450) 19. 01/03/2016_TO_24/04/2019:CRSCREATED AND CENTRAL:TARGET (603040) 20. #18 AND #19 (204)
Search 3 (top‐up search)
19. 24/04/2019_TO_05/03/2020:CRSCREATED AND CENTRAL:TARGET (145491) 20. #18 AND #19 (71)
Search 4 (top‐up search)
#19 05/03/2020_TO_10/03/2021:CRSCREATED AND CENTRAL:TARGET (133254) #20 #19 AND #18 (64)
MEDLINE (Ovid Online): January 2010 to August 2015
Search 1
1 exp Hip Fractures/ (19441) 2 ((hip* or ((femur* or femoral*) adj3 (neck or proximal))) adj4 fracture*).tw. (21065) 3 1 or 2 (27438) 4 exp Physical Therapy Modalities/ (120513) 5 exp Exercise/ or exp Exercise Therapy/ (161044) 6 Rehabilitation/ (17077) 7 Early ambulation/ (2303) 8 Gait/ (20289) 9 Electric Stimulation Therapy/ or Electric Stimulation/ (125489) 10 ((quadriceps or muscle or strength or gait or resistance) adj3 (training or retraining)).tw. (12984) 11 ((electric* adj3 stimulat*) or neurostimulat*).tw. (57491) 12 (physiotherapy or physical therapy).tw. (24887) 13 exercis*.tw. (221705) 14 ((early or delayed) adj3 (weight bearing or mobili$ or ambulation)).tw. (5632) 15 or/4‐14 (553864) 16 Randomized controlled trial.pt. (409861) 17 Controlled clinical trial.pt. (90286) 18 randomized.ab. (339312) 19 placebo.ab. (167495) 20 Drug therapy.fs. (1829870) 21 random*.mp. (1011865) 22 trial.ab. (350855) 23 groups.ab. (1527871) 24 or/16‐23 (3890400) 25 exp Animals/ not Humans/ (4203554) 26 24 not 25 (3339996) 27 3 and 15 and 26 (518) 28 (2010* or 2011* or 2012* or 2013* or 2014* or 2015* or 2016*).ed,dc. (6857104) 29 27 and 28 (205)
*Lines 16 to 26 = sensitivity‐maximizing version of the Cochrane Highly Sensitive Search Strategy for identifying randomised trials (Lefebvre 2019)
Search 2 (top‐up search)
28 (201603* 201604* or 201605* or 201606* or 201607* or 201608* or 201609* or 201610* or 201611* or 201612*or 2017* or 2018* or 2019*).ed,dt. (1899444) 29 27 and 28 (81)
Search 3 (top‐up search)
28 (2019* or 2020*).ed,dt. (2244671) 29 27 and 28 (67)
Search 4 (top‐up search)
28 (202003* 202004* or 202005* or 202006* or 202007* or 202008* or 202009* or 202010* or 202011* or 202012*or 2021*).ed,dt. (1336861) 29 27 and 28 (48)
Embase (Ovid Online): January 2010 to March 2016
Search 1
1 exp Hip Fracture/ (34032) 2 ((hip* or ((femur* or femoral*) adj3 (neck or proximal))) adj4 fracture*).tw. (28031) 3 1 or 2 (41024) 4 exp Physiotherapy/ (66069) 5 exp Exercise/ (249304) 6 Rehabilitation/ or Functional training/ (67321) 7 Mobilization/ (24026) 8 exp Walking/ (77732) 9 exp Electrostimulation/ or exp Electrostimulation therapy/ (263228) 10 Training/ (70576) 11 exp Kinesiotherapy/ (56409) 12 ((quadriceps or muscle or strength or gait or resistance) adj3 (training or retraining)).tw. (16906) 13 ((electric* adj3 stimulat*) or neurostimulat*).tw. (68981) 14 (physiotherapy or physical therapy).tw. (39437) 15 exercis*.tw. (290568) 16 ((early or delayed) adj3 (weight bearing or mobili$ or ambulation)).tw. (7775) 17 or/4‐16 (914632) 18 3 and 17 (4198) 19 Randomized Controlled Trial/ (397452) 20 Controlled Clinical Study/ (392474) 21 random*.ti,ab. (1063967) 22 Randomization/ (69625) 23 Intermethod Comparison/ (205888) 24 placebo.ti,ab. (232796) 25 (compare or compared or comparison).ti. (411612) 26 ((evaluated or evaluate or evaluating or assessed or assess) and (compare or compared or comparing or comparison)).ab. (1361741) 27 (open adj label).ti,ab. (49085) 28 ((double or single or doubly or singly) adj (blind or blinded or blindly)).ti,ab. (181525) 29 Double Blind Procedure/ (129282) 30 parallel group*1.ti,ab. (17820) 31 (crossover or cross over).ti,ab. (79505) 32 ((assign* or match or matched or allocation) adj5 (alternate or group*1 or intervention*1 or patient*1 or subject*1 or participant*1)).ti,ab. (229497) 33 (assigned or allocated).ti,ab. (271897) 34 (controlled adj7 (study or design or trial)).ti,ab. (236666) 35 (volunteer or volunteers).ti,ab. (196942) 36 Human Experiment/ (349917) 37 trial.ti. (200279) 38 or/19‐37 (3546573) 39 (exp Animal/ or animal.hw. or Nonhuman/) not (exp Human/ or Human cell/ or (human or humans).ti.) (5806202) 40 38 not 39 (3076799) 41 18 and 40 (933) 42 (2010* or 2011* or 2012* or 2013* or 2014* or 2015* or 2016*).em,dd. (9402642) 43 41 and 42 (514)
*Lines 19 to 38 = RCT search filter developed to identify eligible EMBASE records for the Cochrane Library. Further details can be found here.
Search 2 (top‐up search)
42 (2016* or 2017* or 2018* or 2019*).dc,yr. (5538640) 43 41 and 42 (356)
Search 3 (top‐up search)
42 (2019* or 2020*).dc,yr. (2440275) 43 41 and 42 (126)
Search 3 (top‐up search)
42 (2020* or 2021*).dc,yr. (2706903) 43 41 and 42 (194)
CINAHL (Ebsco): January 2010 to March 2016
Search 1
S1 (MH "Hip Fractures+") (6,478) S2 TX ((hip* or ((femur* or femoral*) n3 (neck or proximal))) n4 fracture*) (9,089) S3 S1 OR S2 (9,089) S4 (MH "Physical Therapy+") (96,969) S5 (MH "Exercise+") (72,644) S6 (MH "Rehabilitation") OR (MH "Early Ambulation") OR (MH "Home Rehabilitation+") (16,623) S7 (MH "Electric Stimulation+") (12,434) S8 (MH "Muscle Strengthening+") (14,874) S9 TX (quadriceps or muscle or strength or gait or resistance) n3 (training or retraining) (9,289) S10 TX (electric* n3 stimulat*) or neurostimulat* (12,873) S11 TX physiotherapy or physical therapy (169,978) S12 TX exercis* (133,264) S13 TX (early or delayed) n3 (weight bearing or mobili* or ambulation) (1,628) S14 S4 OR S5 OR S6 OR S7 OR S8 OR S9 OR S10 OR S11 OR S12 OR S13 (321,976) S15 S3 AND S14 (1,641) S16 PT Clinical Trial (79,299) S17 (MH "Clinical Trials+") (196,724) S18 TI clinical trial* OR AB clinical trial* (51,838) S19 TI ( (single blind* or double blind*) ) OR AB ( (single blind* or double blind*) ) (23,865) S20 TI random* OR AB random* (168,561) S21 S16 OR S17 OR S18 OR S19 OR S20 (304,815) S22 S15 AND S21 (268) S23 EM 2010 OR EM 2011 OR EM 2012 OR EM 2013 OR EM 2014 OR EM 2015 OR EM 2016 (2,226,972) S24 S22 AND S23 (143)
Search 2 (top‐up search)
S23 EM 2016 OR EM 2017 OR EM 2018 OR EM 2019 (1,213,382) S24 (S22 AND S23) (60)
Search 3 (top‐up search)
S23 EM 2019 OR EM 2020 (413,148) S24 (S22 AND S23) (21)
Search 3 (top‐up search)
S23 EM 2020 OR EM 2021 (426,935) S24 S22 AND S23 (28)
PEDro (January 2010 to April 2019)
Advanced search
Abstract & Title: fracture* Body Part: thigh or hip Method: clinical trial New records added since: 01/01/2010
Total = 125
WHO International Clinical Trials Registry Platform Search Portal
1. hip* AND fracture* AND exercis* OR hip* AND fracture*AND rehab* OR hip* AND fracture* AND ambulation OR hip* AND fracture* AND electr* OR hip* AND fracture* AND physiotherap* OR hip* AND fracture* AND physical therapy OR hip* AND fracture* AND train* OR hip* AND fracture* AND strength* OR hip* AND fracture* AND gait OR hip* AND fracture* AND resistance OR hip* AND fracture* AND mobil* OR hip* AND fracture* AND weight bearing (175)
2. femur AND fracture* AND exercis* OR femur AND fracture*AND rehab* OR femur AND fracture* AND ambulation OR femur AND fracture* AND electr* OR femur AND fracture* AND physiotherap* OR femur AND fracture* AND physical therapy OR femur AND fracture* AND train* OR femur AND fracture* AND strength* OR femur AND fracture* AND gait OR femur AND fracture* AND resistance OR femur AND fracture* AND mobil* OR femur AND fracture* AND weight bearing (92)
3. femoral AND fracture* AND exercis* OR femoral AND fracture*AND rehab* OR femoral AND fracture* AND ambulation OR femoral AND fracture* AND electr* OR femoral AND fracture* AND physiotherap* OR femoral AND fracture* AND physical therapy OR femoral AND fracture* AND train* OR femoral AND fracture* AND strength* OR femoral AND fracture* AND gait OR femoral AND fracture* AND resistance OR femoral AND fracture* AND mobil* OR femoral AND fracture* AND weight bearing (94)
ClinicalTrials.gov
Fracture AND (hip OR femur OR femoral) AND (exercise OR rehabilitation OR ambulation OR electrical OR electrostimulation OR physiotherapy OR physical therapy OR training OR strength OR gait OR resistance OR mobilisation OR mobility OR weight bearing) (524)
Appendix 4. Search results reported in the previous version of the review (Handoll 2011)
On extension of the search for trials (the full search was completed in March 2010, but some ongoing trials were identified subsequently), 21 new studies were identified. Of these, two were included (Gorodetskyi 2007; Oldmeadow 2006), nine were excluded (Carmeli 2006; Di Lorenzo 2007; Franczuk 2005a; Franczuk 2005b; Giangregorio 2005; Mendelsohn 2008; Ohsawa 2007; Olivetti 2007; Portegijs 2008; Stenvall 2007), seven were placed in ongoing trials (INTERACTIVE; Jette; Kristensen; NCT01129219; MASTER; NCT01174589; ProMo), and two await assessment (Mangione; Orwig). New reports resulted in the inclusion of four more trials (Braid 2008: formerly excluded study Braid 2001; Miller 2006 formerly awaiting assessment; Moseley 2009 former ongoing study Cameron 2004; Resnick 2007 former ongoing study Resnick 2002). Further reports, which were often retrospective trial registration entries, were identified also for studies that were categorised as either included or excluded in the previous version of this review (Handoll 2007)
In all, 19 trials are now included, seven trials are listed as ongoing, 22 trials are excluded and two are in the Studies awaiting classification.
Appendix 5. Included studies
Appendix 6. Categories of exercise (ProFaNE), and use of electrical stimulation, in interventions in included trials
| Study ID | Gait, balance & functional training | Strength/resistance training | Flexibility | 3D (Tai Chi, dance etc.) | General physical activity | Endurance | Other | Electrical stimulation |
| In‐hospital | ||||||||
| Baker 1991 | Primary | |||||||
| Braid 2008 | Primary | |||||||
| Gorodetskyi 2007 | Primary | |||||||
| Graham 1968 early weight bearing (2 weeks) | Primary | |||||||
| Graham 1968 late weight bearing (12 weeks) | Primary | |||||||
| Karumo 1977 | Primary | |||||||
| Kimmel 2016 | Primary | |||||||
| Kronborg 2017 | Primary | |||||||
| Lamb 2002 | Primary | |||||||
| Lauridsen 2002 | Primary | |||||||
| Miller 2006 resistance training | Primary | |||||||
| Miller 2006 resistance training and nutrition | Primary | |||||||
| Mitchell 2001 | Primarya | Primary | ||||||
| Monticone 2018 | Primary | |||||||
| Moseley 2009 | Primary | |||||||
| Oh 2020 | Primary | |||||||
| Ohoka 2015 | Primary | |||||||
| Oldmeadow 2006 early assisted ambulation (< 48 hours) | Primary | |||||||
| Oldmeadow 2006 delayed assisted ambulation (> 48 hours) | Primary | |||||||
| Sherrington 2003 | Primary | |||||||
| Van Ooijen 2016 | Primary | |||||||
| Post‐hospital | ||||||||
| Binder 2004 | Primary | Primary | Secondary | Secondary | ||||
| Bischoff‐Ferrari 2010 | Primary | |||||||
| Hauer 2002 | Primary | Primary | ||||||
| Langford 2015 | Additional post‐discharge physio telephone support and coaching | |||||||
| Latham 2014 | Primary | Secondary | ||||||
| Magaziner 2019 | Primary | Primary | ||||||
| Mangione 2005 resistance | Primary | |||||||
| Mangione 2005 endurance | Primary | |||||||
| Mangione 2010 | Primary | |||||||
| Orwig 2011 | Primary | Primary | Self‐efficacy‐based motivational component | |||||
| Pol 2019 | Coaching based on cognitive behavioural therapy | |||||||
| Resnick 2007 exercise group | Primary | Primary | ||||||
| Resnick 2007 exercise plus education/motivation aspect | Primary | Primary | Motivational interventions, including education and goal setting | |||||
| Salpakoski 2015 | Primary | |||||||
| Sherrington 1997 | Primary | |||||||
| Sherrington 2004 weight bearing exercise | Primary | |||||||
| Sherrington 2004 non‐weight bearing exercise | Specific group of muscle contractions in supine | |||||||
| Sherrington 2020 | Primary | |||||||
| Stasi 2019 | Primary | |||||||
| Suwanpasu 2014 | Physical activity‐enhancing programme, based on Resnick's self‐efficacy model (Resnick 2009) | |||||||
| Sylliaas 2011 | Primary | |||||||
| Sylliaas 2012 | Primary | |||||||
| Taraldsen 2019 | Primary | |||||||
| Tsauo 2005 | Primary | Secondary | ||||||
| Williams 2016 | Primary | Workbook and goal‐setting diary | ||||||
aBoth intervention and control groups received identical gait, balance and functional training. This study was considered as resistance training in analyses, as this was the between‐group difference.
Appendix 7. Adherence
| Study ID | Adherence was measured | Adherence data were reported | Measurement of adherence | Reported adherence results |
| Baker 1991 | No | No | ‐ | ‐ |
| Binder 2004 | Yes | Yes | Adherence to exercise programme, measured as the percentage of 72 sessions performed | Intervention group: mean (SD) attendance (/72 sessions) = 87% (24%); mean (SD) number of exercise session per week 2.3 (0.2) Control group: control participants who completed exercise log data (n = 32, 74%). Of these, the percentage of the 72 sessions performed was mean (SD) 131% (62%) (NB: participants in control were advised to perform at least 3 times per week but not prohibited from performing more exercises and the mean compliance reported in control group indicated some participants performed more than 3 times per week) |
| Bischoff‐Ferrari 2010 | Yes | Yes | Adherence to exercise programme | Intervention group: 69% of participants reached 12‐month visit or telephone call and performed the home programme at least once a week |
| Braid 2008 | No | No | ‐ | ‐ |
| Gorodetskyi 2007 | No | No | ‐ | ‐ |
| Graham 1968 | No | No | ‐ | ‐ |
| Hauer 2002 | Yes | Yes | Adherence to exercise programme | Intervention group: mean (SD) [range] adherence to exercise = 93.1% (13.5%) [55% to 100%] Control group: mean (SD) [range] adherence to placebo activities = 96.7 % (6.1%) [83% to 100%] |
| Karumo 1977 | No | No | ‐ | ‐ |
| Kimmel 2016 | No | No | ‐ | ‐ |
| Kronborg 2017 | Yes | Yes | Adherence to exercise programme | Intervention group: 80% of participants completed all strength training sessions |
| Lamb 2002 | No | No | ‐ | ‐ |
| Langford 2015 | Yes | No | ‐ | ‐ |
| Latham 2014 | Yes | Yes | Attendance | Intervention group: attendance across 26 weeks = 70% |
| Lauridsen 2002 | Yes | Yes | Adherence to exercise programme | Intervention group: average hours of training = 6.4 hours; average number of days of training = 14 days; average number of hours per day = 0.5 hours. Prescribed physical therapy: 6 hours + non‐supervised training for other 4 days Control group: average hours of training = 4 hours; average number of days of training = 17 days; average number of hours per day = 0.2 hours Prescribed physical therapy: approximately 2 hours (NB: did not clearly state if there is non‐supervised training) |
| Magaziner 2019 | Yes | Yes | Adherence to exercise programme | Intervention group: 72.4% participants completed ≥ 80% expected intervention visits; mean (SD) percentage of expected intervention visits completed per participant = 78.3% (27.6%) Control group: 81% participants completed ≥ 80% expected intervention visits; mean (SD) percentage of expected intervention visits completed per participant = 87.0% (14.3%) |
| Mangione 2005 | Yes | Yes | Attendance | Mean attendance in exercise training = 98% |
| Mangione 2010 | Yes | Yes | Attendance | Intervention group: attendance = 99% (number of sessions completed divided by possible number of sessions = 237/240 sessions). Control group attendance = 99% (178/180 sessions) |
| Miller 2006 | Yes | Yes | Attendance | Adherence to the 12 weeks of resistance training = 86% |
| Mitchell 2001 | Yes | Yes | Adherence to exercise programme | Intervention group: median (range) number of training sessions completed at the six‐week assessment = 11 (10 to 12) |
| Monticone 2018 | Yes | No | ‐ | ‐ |
| Moseley 2009 | Yes | Yes | Adherence to exercise programme | Higher dose weight‐bearing exercise group: median (interquartile range (IQR)) total exercise time during the in‐hospital phase = 543 (463) minutes (min); median (IQR) number of times visited by physiotherapist during the community phase = 8 (4); median (IQR) reported walking time: 517 min (1125)). Lower dose weight‐bearing exercise group: median (IQR) total exercise time during the in‐hospital phase = 363 (318) min; median (IQR) number of times visited by physiotherapist during the community phase = 4 (1) |
| Oh 2020 | No | No | ‐ | ‐ |
| Ohoka 2015 | No | No | ‐ | ‐ |
| Oldmeadow 2006 | No | No | ‐ | ‐ |
| Orwig 2011 | Yes | Yes | Adherence to exercise programme | Intervention group: mean number of visits = 36.2 |
| Pol 2019 | Yes | Yes | Attendance of the 20 scheduled exercise sessions | Intervention group: 49 of the 70 participants completed the exercise programmes Median number of sessions: 20 Median number of exercises per visits: 5 |
| Resnick 2007 | Yes | Yes | Adherence to exercise programme | Combined two exercise groups: mean (SD) exercise time in hours per week at 12 month = 3.22 (3.87) Control group: mean (SD) exercise time in hours per week at 12 month = 0.92 (1.45) NB. Prescribed duration of training was not clear |
| Salpakoski 2015 | Yes | Yes | Adherence to exercise programme | Interevention group: proportion of classes attended (amount of performed exercises over expected number of exercises) during the first 6 months, strengthening = 61%, stretching = 53%, balance = 65%, functional exercises = 69%. All but 1 participant attended the first face‐to‐face physical activity counselling session. Responded to phone contact: first contact = 90%, second contact = 88%, third contact = 83%. Control group: did not follow for compliance with the home exercises |
| Sherrington 1997 | Yes | Yes | Adherence to exercise programme | Mean (SD) [range] number of days of exercise determined from the exercise diaries = 24.7 (3.8) [18 to 30] Prescribed number of days of exercise: 30 days Mean (SD) [range] number of repetitions completed = 737 (664) [154 to 2450]. Median (IQR) number of repetitions = 480 (405 to 692) |
| Sherrington 2003 | No | No | ‐ | ‐ |
| Sherrington 2004 | No | No | ‐ | ‐ |
| Sherrington 2020 | No | No | ‐ | ‐ |
| Stasi 2019 | No | No | ‐ | ‐ |
| Suwanpasu 2014 | No | No | ‐ | ‐ |
| Sylliaas 2011 | No | No | ‐ | ‐ |
| Sylliaas 2012 | No | No | ‐ | ‐ |
| Taraldsen 2019 | Yes | Yes | Attendance to occupational therapy sessions | Inpatient period: median (IQR) of in‐hospital number of sessions: 4 (2 to 5) for usual care, 4 (2 to 6) for cognitive behavioural therapy (CBT)‐based occupational therapy, 2.5 (1 to 5) for CBT‐based occupational therapy with sensor monitoring At home: 2 (0 to 4) for CBT‐based occupational therapy and 4 (2 to 4) for CBT‐based occupational therapy with sensor monitoring Duration of session (minutes): 41 (0 to 60) for CBT‐based occupational therapy, 45 (38.5 to 60) for CBT‐based occupational therapy with sensor monitoring |
| Tsauo 2005 | No | No | ‐ | ‐ |
| Van Ooijen 2016 | Yes | Yes | Attendance | Adaptability treadmill training group: median (minimum to maximum) number of training sessions on treadmill: 11 (8 to 15); number of sessions of usual therapy = 13 (7 to 18). Conventional treadmill training group: median (minimum to maximum) number of training sessions on treadmill:12 (7 to 14); number of sessions of usual therapy = 12 (7 to 15). Usual physical therapy: median (minimum to maximum) number of sessions = 27 (16 to 31) |
| Williams 2016 | Yes | Yes | Adherence to exercise programme | Number of participants who received 6 sessions = 13; average number of sessions delivered to the intervention participants = 5 |
Appendix 8. Studies reporting resource use in intervention and control groups
| Study ID (source if not primary reference) | Length of stay, intervention/control, mean (SD), n | Number of physiotherapy sessions, intervention/control, mean (SD), n | Number of outpatient attendances, intervention/control, mean (SD), n | Need for special care, intervention/control, mean (SD), n | Community service use, intervention/control, n (%) | Other, intervention/control, mean (SD), n |
| Binder 2004 | ‐ | Physical therapy group: 2.3 (0.2), n = 44 | ‐ | ‐ | ||
| Bischoff‐Ferrari 2010 | ‐ | No. of physiotherapy sessions during acute care Standard group: 7.6 (95% CI 6.3 to 8.9), n = 86 Extended physiotherapy (PT): 7.2 (95% CI 6.4 to 8.0), n = 87 Total minutes of physiotherapy as an inpatient Standard: 176 (95% CI 144 to 208), n = 86 Extended PT: 292 (95% CI 259 to 326), n = 87 Total duration of physiotherapy post‐hospital = unclear |
‐ | ‐ | ||
| Karumo 1977 | Routine physical therapy group: 35.0 (21.6), n = 49 Intensive physical therapy group: 32.2 (21.7), n = 38 |
‐ | ‐ | ‐ | ||
| Kimmel 2016 | Median (IQR) Control: 35.0 (19.0 to 49.8), n = 46 Intervention: 24.4 (16.4 to 31.6), n = 46 |
‐ | ‐ | ‐ | ||
| Kronborg 2017 | ‐ | Physiotherapy with strength training: 6.0 (1.9), n = 43 Physiotherapy: 5.6 (1.7), n = 44 Total training time per day (min) Physiotherapy with strength training: 20.6 (5.8), n = 43 Physiotherapy: 23.5 (4.3), n = 44 |
‐ | ‐ | ||
| Langford 2015 | ‐ | ‐ | ‐ | ‐ | Total telephone intervention time over 5 calls: 151 minutes (range 42 to 286 minutes), n = 11 | |
| Lauridsen 2002 | Median (range) Intervention: 32 (5 to 126), n = 44 Control: 34 (8 to 145), n = 44 |
Median (range) of training period (days) Intervention: 14 (1 to 42), n = 44 Control: 17 (3 to 58), n = 44 Median (range) total hours spent in training Intervention: Intervention: 6.4 (1.3 to 21.3), n = 44 Control: 4.0 (0.3 to 12.5), n = 44 |
‐ | ‐ | ||
| Mangione 2010 | ‐ | Total no. of sessions planned for all participants Leg strengthening group: 240 (total for 14 participants) Control: 180 (total for 12 participants) Total no. of sessions completed for all participants Leg strengthening group: 237 (total for 14 participants), i.e. mean 17 sessions each Control: 178 (total for 12 participants), i.e. mean 15 sessions each |
‐ | ‐ | ||
| Miller 2006 | Median (95% CI) Exercise group: 23.0 (16.0 to 32.0), n = 25 Nutrition and exercise: 27.5 (13.0 to 31.0), n = 24 Control: 24.0 (17.0 to 30.0), n = 26 |
‐ | ‐ | |||
| Mitchell 2001 | Median (IQR) Quadriceps training: 39 (27 to 50), n = 20 Control: 40 (28 to 57), n = 24 |
‐ | ‐ | ‐ | ||
| Moseley 2009 | Days from fracture to rehabilitation admission (days) Median (IQR) High dose weight‐bearing exercise group: 14 (9 to 21), n = 80 Low dose limited weight‐bearing exercise group: 12 (9 to 19), n = 80 |
Median (IQR) Exercise time with a physiotherapist or assistant (mins) High dose weight‐bearing exercise group: 543 (463), n = 80 Low dose limited weight‐bearing exercise group: 363 (318), n = 80 Median (IQR) no. of sessions during community phase: High dose weight‐bearing exercise group: 8 (4), n = 73 Low dose limited weight‐bearing exercise group: 4 (1), n = 77 |
‐ | ‐ | User of community services (n (%) High dose weight‐bearing exercise group: 25 (56%) Low dose limited weight‐bearing exercise group: 39 (74%) |
|
| Ohoka 2015 | Weight bearing group: 92, n = 9 Non‐weight bearing group: 98, n = 9a |
‐ | ‐ | ‐ | ||
| Oldmeadow 2006 | Early ambulation group: 16.6 (range 4 to 136), n = 29 Delayed ambulation: 11.4 (range: 5 to 24), n = 31 |
‐ | ‐ | ‐ | ||
| Orwig 2011 | ‐ | No. of visits to exercise: 36.2, n = 91a Planned no. of trainers' visits: 56 Actual no. of trainers' visits: 42a |
‐ | ‐ | ||
| Pol 2019 | Number of sessions delivered, median (IQR): Other therapy (OT) + sensor: 4 (2 to 4) OT: 2 (0 to 4) Duration of sessions at home (min) (median (IQR): OT + sensor: 45 (38.5 to 60) OT: 41 (0 to 60) |
|||||
| Sherrington 2003 | Length of stay in the inpatient rehabilitation ward Non‐weight bearing exercise group: 25.2 (12.1), n = 37 Weight bearing exercise group 24.1 (12.4), n = 40 Overall length of stay Non‐weight bearing exercise group: 38.5 (16.3), n = 37 Weight bearing exercise group: 36.2 (13.6), n = 40 |
‐ | ‐ | ‐ | ||
| Van Ooijen 2016 | ‐ | Planned no. of sessions: 30 Median (minimum to maximum) no. of sessions on the treadmill: Adaptability treadmill: 11 (8 to 15), n = 24 Conventional treadmill: 12 (7 to 14), n = 23 Median (minimum to maximum) no. of physical therapy sessions Adaptability treadmill: 13 (7 to 18), n = 24 Conventional treadmill 12 (7 to 15), n = 23 Usual physical therapy: 27 (16 to 31), n = 23 |
‐ | ‐ | ||
| Williams 2016 | Inpatient orthopaedic trauma ward Intervention group: 15.2, n = 25 Control: 10.5, n = 24a Rehabilitation ward Intervention group: 12.1, n = 25 Control: 18.8, n = 24a |
‐ | ‐ | ‐ |
NB: data were expressed as mean (standard deviation (SD)) unless otherwise specified aSD not reported
Appendix 9. Sensitivity analyses: exploring the impact on results (mobility: broad mobility measures)
| Sensitivity analysis | Pooled impact of mobility strategies on mobility outcome (SMD, 95% CI) |
| In‐hospital trials | |
| Primary analysis, all trials, random‐effects meta‐analysis | SMD 0.53, 95% CI 0.10 to 0.96; participants = 507; studies = 7; I2 = 81% |
| Sensitivity analysis 1, removing trials with unclear or high risk of bias on allocation concealment | SMD 0.58, 95% CI 0.05 to 1.10; participants = 415; studies = 6; I2 = 84% |
| Sensitivity analysis 2, removing trials with high risk of bias on any items | SMD 0.57, 95% CI ‐0.46 to 1.61; participants = 191; studies = 2; I2 = 87% |
| Sensitivity analysis 3, removing trials reported only in conference abstracts | No studies removed |
| Sensitivity analysis 4, removing trials that did not clearly focus on or predominantly include the target population of people with a fragility fracture resulting from low‐energy trauma | No studies removed |
| Sensitivity analysis 5, removing trials that included mixed populations | No studies removed |
| Sensitivity analysis 6, removing in‐hospital trials that measured outcomes at the end of the in‐hospital phase (the usual time point was that closest to four months). | SMD 0.39, 95% CI 0.01 to 0.78; participants = 327; studies = 4; I2 = 62% |
| Sensitivity analysis 7, all trials, fixed‐effects meta‐analysis | SMD 0.38, 95% CI 0.20 to 0.56; participants = 507; studies = 7; I2 = 81% |
| Post‐hospital trials | |
| Primary analysis, all trials, random‐effects meta‐analysis | SMD 0.32, 95% CI 0.11 to 0.54; participants = 761; studies = 7; I2 = 48% |
| Sensitivity analysis 1, removing trials with unclear or high risk of bias on allocation concealment | SMD 0.22, 95% CI ‐0.01 to 0.46; participants = 486; studies = 5; I2 = 22% |
| Sensitivity analysis 2, removing trials with high risk of bias on any items | SMD 0.38, 95% CI ‐0.04 to 0.79; participants = 350; studies = 3; I2 = 70% |
| Sensitivity analysis 3, removing trials reported only in conference abstracts | No studies removed |
| Sensitivity analysis 4, removing trials that did not clearly focus on or predominantly include the target population of people with a fragility fracture resulting from low‐energy trauma | SMD 0.36, 95% CI 0.10 to 0.62; participants = 602; studies = 6; I2 = 53% |
| Sensitivity analysis 5, removing trials that included mixed populations | SMD 0.36, 95% CI 0.10 to 0.62; participants = 602; studies = 6; I2 = 53% |
| Sensitivity analysis 6, all trials, fixed‐effects meta‐analysis | SMD 0.33, 95% CI 0.17 to 0.50; participants = 602; studies = 6; I2 = 53% |
Appendix 10. Studies reporting cost‐effectiveness, cost‐utility or costs (intervention and/or healthcare resource use)
| Study ID (source if not primary reference), sample, type of evaluation | Intervention(s) and comparator (N in analysis) | Perspective(s), type of currency, price year, time horizon | Cost items measured | Mean (SD) intervention cost per person | Healthcare service costs | Incremental cost per quality‐adjusted life‐year (QALY) gained |
Taraldsen 2019
|
1. Received two home‐based exercise sessions two times a week for 10 weeks four months following hip fracture 2. Usual care |
|
Cost including physiotherapy, primary care costs (home‐based services, nursing home, general practitioners) and hospital services | Mean (SD) total health and care cost per patient EUR 26,219 (25,468) for intervention group and EUR 25,976 (28,631) for control group |
Mean QALY difference: ‐0.009 (95% CI ‐0.061 to 0.038) Mean cost difference: 65.7 EUR (95% CI: ‐8740.4 to 9076.8), 51% of the replicates gave higher cost for the intervention group |
|
Williams 2016 (Williams 2017)
|
1. Usual care plus enhanced rehabilitation package, including six additional home‐based physiotherapy sessions delivered by a physiotherapist or technical instructor, novel information workbook and goal‐setting diary. 2. Usual care |
|
Health (primary and secondary healthcare services) and social care service use (including social worker, psychologist, home care worker, care attendant, nursing home, rehabilitation, charity services), and medication use | Intervention group: mean GBP 231 | GBP 149,243 for intervention group; GBP 105,243 for control group (includes intervention cost) |
Cost‐effectiveness analysis not conducted due to no between‐group difference in QALY. |
Appendix 11. Acknowledgements for previous versions of review
| Acknowledgements |
| We thank the following individuals for their comments and help at editorial review of the first version of the review: Prof William Gillespie, Prof Harley Gray (external referee: review only), Mr Peter Herbison (review only), Prof James Hutchison (external referee: protocol only), Prof Rajan Madhok, Ms Leeann Morton, Prof Gordon Murray (protocol only), Mr Anthony Pohl (external referee: review only) and Prof Marc Swiontkowski. We also thank Ms Hilda Bastian for her help with the Synopsis.
For the first and second updates, we thank Mrs Lesley Gillespie for her help with the search strategy and trial retrieval, and Ms Leeann Morton and Prof William Gillespie for their help at editorial review.
We thank Dr Yvonne Dynan for her contribution to the first two versions of the review and Ms Pernille Jensen for checking over a study report in Danish.
Dr Helen Handoll's work on the first two versions of the review was supported by the Chief Scientist Office, Department of Health, The Scottish Office, UK.
For the third update, we thank Mrs Lesley Gillespie for her help with the search strategy, trial retrieval and final editorial checks, Ms Judy Sherrington for proof reading, Prof William Gillespie, Mr Peter Herbison, Dr Janet Wale and Dr Meghan Donaldson (external referee) for their feedback and help at editorial review. We would like to acknowledge the important contributions of Dr Martyn Parker as author of the first four versions of this review. Dr Parker, who initiated and designed the first version of this review and contributed greatly to the first three updates, resigned authorship due to his many other commitments. For the fourth update, we thank Mrs Lesley Gillespie for her help with trial retrieval, Ms Lindsey Shaw and Dr Joanne Elliott for final editorial checks, and Prof William Gillespie, Dr Vicki Livingstone, Dr Janet Wale and Dr Meghan Donaldson (external referee) for their feedback and help at editorial review. For the fifth update, we thank Dr Joanne Elliott for help with the literature searches, Mrs Monika Browning for her help with assessing the eligibility of two Polish trials, and Mrs Nicola Fairhall for her advice on electrostimulation. |
Data and analyses
Comparison 1. In‐hospital rehabilitation: mobilisation strategy versus usual care, critical outcomes.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1.1 Mobility (measured using mobility scales): combined data for all strategy types | 7 | 507 | Std. Mean Difference (IV, Random, 95% CI) | 0.53 [0.10, 0.96] |
| 1.2 Mobility (failure to regain pre‐facture mobility): combined data for all strategy types | 2 | 64 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.48 [0.27, 0.85] |
| 1.3 Mobility (measured using self‐reported outcomes): combined data for all strategy types | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 1.4 Mobility (measured using mobility scales): gait, balance and function | 6 | 463 | Std. Mean Difference (IV, Random, 95% CI) | 0.57 [0.07, 1.06] |
| 1.5 Mobility (measured using mobility scales): resistance/strength training | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 1.6 Mobility (measured in seconds using TUG): resistance/strength training | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 1.7 Mobility (measured using mobility scales) reporting individual outcome measures | 8 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 1.7.1 Elderly Mobility Scale | 2 | 95 | Mean Difference (IV, Random, 95% CI) | 0.49 [‐0.81, 1.79] |
| 1.7.2 Physical Performance and Mobility Examination Score | 2 | 227 | Mean Difference (IV, Random, 95% CI) | 0.34 [‐0.31, 0.99] |
| 1.7.3 Berg Balance Scale | 2 | 93 | Mean Difference (IV, Random, 95% CI) | 12.39 [8.79, 15.98] |
| 1.7.4 Modified Iowa Level of Assistance | 1 | 92 | Mean Difference (IV, Random, 95% CI) | 2.70 [‐0.94, 6.34] |
| 1.7.5 Timed Up and Go | 3 | 158 | Mean Difference (IV, Random, 95% CI) | 4.03 [‐6.17, 14.23] |
| 1.7.6 Performance Oriented Mobility Assessment | 1 | 51 | Mean Difference (IV, Random, 95% CI) | 0.90 [‐1.14, 2.94] |
| 1.7.7 Koval Walking Ability score | 1 | 41 | Mean Difference (IV, Random, 95% CI) | 1.53 [0.72, 2.34] |
| 1.7.8 Western Ontario and McMaster Universities OA Index (self‐reported) | 1 | 52 | Mean Difference (IV, Random, 95% CI) | ‐25.40 [‐28.72, ‐22.08] |
| 1.8 Walking speed (measured as metres/time): combined data for all strategy types | 6 | 360 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.16 [‐0.05, 0.37] |
| 1.9 Walking speed (measured as metres/time): gait, balance and function | 5 | 336 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.15 [‐0.07, 0.36] |
| 1.10 Walking speed (measured as metres/time): electrical stimulation | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 1.11 Functioning (measured using functioning scales): combined data for all strategy types | 7 | 379 | Std. Mean Difference (IV, Random, 95% CI) | 0.75 [0.24, 1.26] |
| 1.12 Functioning (measured using functioning scales): gait, balance and function | 5 | 312 | Std. Mean Difference (IV, Random, 95% CI) | 0.56 [‐0.00, 1.13] |
| 1.13 Functioning (measured using functioning scales): resistance/strength training | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 1.14 Functioning (measured using functioning scales): electrical stimulation | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 1.15 Health‐related quality of life (measured using HRQoL scales): gait, balance and function | 4 | 314 | Std. Mean Difference (IV, Random, 95% CI) | 0.39 [‐0.07, 0.85] |
| 1.16 Mortality, short term: combined data for all strategy types | 6 | 489 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.06 [0.48, 2.30] |
| 1.17 Mortality, short term: gait, balance and function | 3 | 293 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.43 [0.44, 4.66] |
| 1.18 Mortality, short term: resistance/strength training | 2 | 170 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.83 [0.26, 2.62] |
| 1.19 Mortality, short term: electrical stimulation | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 1.20 Mortality, long term: combined data for all strategy types | 2 | 133 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.22 [0.48, 3.12] |
| 1.21 Mortality, long term: gait, balance and function | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 1.22 Mortality, long term: resistance/strength training | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 1.23 Adverse events (measured using dichotomous outcomes): combined data for all strategy types | 7 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 1.23.1 Re‐admission | 4 | 322 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.70 [0.44, 1.11] |
| 1.23.2 Re‐operation | 1 | 80 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.32 [0.01, 7.57] |
| 1.23.3 Surgical complications | 1 | 18 | Risk Ratio (M‐H, Fixed, 95% CI) | Not estimable |
| 1.23.4 Pain | 3 | 245 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.12 [0.80, 1.57] |
| 1.23.5 Falls (number of people who experienced one or more falls) | 1 | 50 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.67 [0.32, 1.38] |
| 1.23.6 Other: orthopaedic complication (as reason for withdrawal from study) | 1 | 88 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.50 [0.45, 4.95] |
| 1.24 Adverse events (measured using rate of falls): all studies were gait, balance and function | 3 | Rate Ratio (IV, Fixed, 95% CI) | 0.85 [0.64, 1.12] | |
| 1.25 Adverse events (measured using continuous measures of pain): combined data for all strategy types | 2 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 1.26 Return to living at pre‐fracture residence: combined data for all strategy types | 2 | 240 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.07 [0.73, 1.56] |
| 1.27 Return to living at pre‐fracture residence: additional study not included in main analysis | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 1.28 Return to living at pre‐fracture residence: gait, balance and function | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 1.29 Return to living at pre‐fracture residence: resistance/strength training | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected |
Comparison 2. In‐hospital rehabilitation: mobilisation strategy versus usual care, other important outcomes.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 2.1 Walking, use of walking aid/need for assistance | 2 | 230 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.91 [0.74, 1.11] |
| 2.2 Balance (measured using functional reach test, cm) | 2 | 121 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.37 [0.01, 0.73] |
| 2.3 Balance (measured using balance scale) | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 2.4 Balance (measured using ability to tandem stand) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 2.5 Balance (measured using step test; number of steps) | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 2.6 Balance (measured using self‐reported outcomes) | 2 | 226 | Risk Ratio (M‐H, Random, 95% CI) | 0.96 [0.71, 1.29] |
| 2.7 Sit to stand (measured as number of stand ups/second) | 2 | 227 | Mean Difference (IV, Fixed, 95% CI) | 0.04 [0.01, 0.07] |
| 2.8 Strength | 8 | 498 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.11 [‐0.07, 0.28] |
| 2.9 Activities of daily living (measured using ADL scales) | 5 | 206 | Std. Mean Difference (IV, Random, 95% CI) | 0.87 [0.35, 1.38] |
| 2.10 Resource use (measured by length of hospital stay) | 4 | 335 | Mean Difference (IV, Fixed, 95% CI) | ‐0.83 [‐3.94, 2.28] |
| 2.11 Resource use (measured by use of community services) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected |
Comparison 3. In‐hospital rehabilitation: comparing different intervention strategies, critical outcomes.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 3.1 Weight‐bearing at 2 wks v weight‐bearing at 12 weeks (mortality) | 1 | 273 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.74 [0.43, 1.29] |
| 3.2 Early assisted ambulation (< 48 hrs) v delayed assisted ambulation (mortality) | 1 | 60 | Risk Ratio (M‐H, Fixed, 95% CI) | 3.20 [0.14, 75.55] |
| 3.3 Weight‐bearing at 2 wks v weight‐bearing at 12 weeks (adverse events) | 1 | 594 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.86 [0.54, 1.37] |
| 3.3.1 Avascular necrosis | 1 | 112 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.69 [0.33, 1.42] |
| 3.3.2 Infection | 1 | 270 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.65 [0.11, 3.81] |
| 3.3.3 Non‐union | 1 | 212 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.06 [0.56, 2.03] |
| 3.4 Early assisted ambulation (< 48 hrs) v delayed assisted ambulation (return to living at home) | 1 | 60 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.86 [0.72, 1.02] |
| 3.5 Early assisted ambulation (< 48 hrs) v delayed assisted ambulation (walking aid/assistance) | 1 | 60 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.51 [0.29, 0.89] |
Comparison 4. Post‐hospital rehabilitation: mobilisation strategy versus control, critical outcomes.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 4.1 Mobility (measured using mobility scales): combined data for all strategy types | 7 | 761 | Std. Mean Difference (IV, Random, 95% CI) | 0.32 [0.11, 0.54] |
| 4.2 Mobility (measured using Timed Up and Go, seconds): combined data for all strategy types | 3 | 375 | Mean Difference (IV, Fixed, 95% CI) | ‐1.98 [‐5.59, 1.63] |
| 4.3 Mobility (measured using 6‐Minute Walk Test, metres): combined data for all strategy types | 4 | 396 | Mean Difference (IV, Fixed, 95% CI) | 28.66 [10.88, 46.44] |
| 4.4 Mobility (measured using mobility scales): gait, balance and function | 5 | 621 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.20 [0.05, 0.36] |
| 4.5 Mobility (measured using Timed Up and Go, seconds): gait, balance and function | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 4.6 Mobility (measured using Timed Up and Go, seconds): resistance/strength training | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 4.7 Mobility (measured using 6‐Minute Walk Test, metres): resistance/strength training | 3 | 198 | Mean Difference (IV, Fixed, 95% CI) | 55.65 [28.58, 82.72] |
| 4.8 Mobility (measured using 6‐Minute Walk Test, metres): endurance training | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 4.9 Mobility (measured using mobility scales): multiple component | 2 | 104 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.94 [0.53, 1.34] |
| 4.10 Mobility (measured using 6‐Minute Walk Test, metres): multiple component | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 4.11 Mobility (measured using mobility scales): other type of exercise (non‐weight bearing exercise) | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 4.12 Mobility (measured using Timed Up and Go, seconds): other type of exercise OT +/‐ sensor) | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 4.13 Mobility (measured using mobility scales) reporting individual outcome measures | 14 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 4.13.1 Modified Physical Performance Test | 1 | 80 | Mean Difference (IV, Random, 95% CI) | 5.70 [2.74, 8.66] |
| 4.13.2 Physical Performance and Mobility Examination Score | 1 | 105 | Mean Difference (IV, Random, 95% CI) | 0.32 [‐0.42, 1.05] |
| 4.13.3 Short Physical Performance Battery | 4 | 552 | Mean Difference (IV, Random, 95% CI) | 0.68 [0.15, 1.21] |
| 4.13.4 Performance Oriented Mobility Assessment | 1 | 24 | Mean Difference (IV, Random, 95% CI) | 4.90 [2.11, 7.69] |
| 4.13.5 Timed Up and Go | 3 | 366 | Mean Difference (IV, Random, 95% CI) | 1.69 [‐2.74, 6.12] |
| 4.13.6 6 Minute Walk Test | 4 | 396 | Mean Difference (IV, Random, 95% CI) | 33.98 [7.08, 60.89] |
| 4.14 Mobility (measured using self‐report, continuous scales): combined data for all strategy types | 2 | 355 | Mean Difference (IV, Fixed, 95% CI) | 1.46 [‐0.62, 3.53] |
| 4.15 Mobility (measured using self‐reported, dichotomous outcome): combined data for all strategy types | 1 | 108 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.45 [0.29, 0.72] |
| 4.16 Walking speed: combined data for all strategy types | 14 | 1067 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.16 [0.04, 0.29] |
| 4.17 Walking speed: gait, balance and function | 7 | 511 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.08 [‐0.09, 0.25] |
| 4.18 Walking speed: resistance/strength training | 3 | 197 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.29 [‐0.01, 0.58] |
| 4.19 Walking speed: endurance | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 4.20 Walking speed: multiple component | 3 | 285 | Std. Mean Difference (IV, Random, 95% CI) | 0.53 [‐0.13, 1.18] |
| 4.21 Walking speed: other (post‐discharge physio telephone support and coaching) | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 4.22 Walking speed: other (non‐weight bearing) | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 4.23 Walking speed subgrouped by studies with cognitive impairment included v studies with cognitive impairment not included, combined data for all strategy types | 14 | Std. Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 4.23.1 People with cognitive impairment included | 2 | 304 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.07 [‐0.16, 0.29] |
| 4.23.2 People with cognitive impairment excluded | 12 | 762 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.19 [0.04, 0.34] |
| 4.24 Walking speed: subgrouped by outpatient v secondary and social care setting | 14 | Std. Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 4.24.1 Outpatient | 2 | 229 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.35 [0.08, 0.62] |
| 4.24.2 Secondary and social care | 12 | 838 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.11 [‐0.02, 0.25] |
| 4.25 Walking speed subgrouped by mean age ≤ 80 years v > 80 years, combined data for all strategies | 14 | Std. Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 4.25.1 Mean age in study 80 years or less | 8 | 536 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.12 [‐0.05, 0.30] |
| 4.25.2 Mean age in study > 80 years | 6 | 530 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.18 [0.01, 0.36] |
| 4.26 Functioning (measured using functioning scales): combined data for all strategy types | 9 | 936 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.23 [0.10, 0.36] |
| 4.27 Functioning (measured using functioning scales): gait, balance and function | 4 | 432 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.17 [‐0.02, 0.36] |
| 4.28 Functioning (measured using functioning scales): resistance/strength training | 2 | 246 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.29 [0.03, 0.55] |
| 4.29 Functioning (measured using functioning scales): multiple components | 2 | 107 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.34 [‐0.04, 0.72] |
| 4.30 Functioning (measured using functioning scales): other: OT +/‐ sensor | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 4.31 Health‐related quality of life (measured using HRQoL scales): combined data for all strategy types | 10 | 785 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.14 [‐0.00, 0.29] |
| 4.32 Health‐related quality of life (measured using HRQoL scales): gait, balance and function | 4 | 316 | Std. Mean Difference (IV, Random, 95% CI) | 0.08 [‐0.37, 0.53] |
| 4.33 Health‐related quality of life (measured using HRQoL scales): resistance/strength training | 3 | 197 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.15 [‐0.14, 0.45] |
| 4.34 Health‐related quality of life (measured using HRQoL scales): endurance | 1 | 22 | Mean Difference (IV, Random, 95% CI) | 9.50 [‐8.56, 27.56] |
| 4.35 Health‐related quality of life (measured using HRQoL scales): multiple components | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 4.36 Health‐related quality of life subgrouped by studies with cognitive impairment included v studies with cognitive impairment not included, combined data for all strategy types | 10 | Std. Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 4.36.1 People with cognitive impairment included | 1 | 120 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.00 [‐0.36, 0.36] |
| 4.36.2 People with cognitive impairment excluded | 9 | 665 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.17 [0.01, 0.33] |
| 4.37 Health‐related quality of life subgrouped by outpatient v secondary and social care setting | 10 | Std. Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 4.37.1 Outpatient | 2 | 233 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.18 [‐0.09, 0.45] |
| 4.37.2 Secondary and social care | 8 | 552 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.13 [‐0.04, 0.30] |
| 4.38 Health‐related quality of life subgrouped by mean age ≤ 80 years v > 80 years, combined data for all strategy | 10 | Std. Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 4.38.1 Mean age in study 80 years or less | 4 | 184 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.25 [‐0.05, 0.55] |
| 4.38.2 Mean age in study > 80 years | 6 | 601 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.11 [‐0.05, 0.27] |
| 4.39 Mortality, short term: combined data for all strategy types | 7 | 737 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.01 [0.49, 2.06] |
| 4.40 Mortality, short term: gait, balance and function | 3 | 264 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.12 [0.46, 2.72] |
| 4.41 Mortality, short term: resistance/strength training | 2 | 123 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.40 [0.19, 10.03] |
| 4.42 Mortality, short term: multiple components | 2 | 290 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.61 [0.08, 4.55] |
| 4.43 Mortality, short term: other: non‐weight bearing | 1 | 60 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.50 [0.03, 7.59] |
| 4.44 Mortality, long term: combined data for all strategy types | 4 | 588 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.73 [0.39, 1.37] |
| 4.45 Mortality, long term: gait, balance and function | 2 | 254 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.75 [0.34, 1.67] |
| 4.46 Mortality, long term: multiple components | 2 | 334 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.70 [0.25, 1.96] |
| 4.47 Adverse events (measured using dichotomous outcomes): combined data for all strategy types | 4 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 4.47.1 Re‐admission | 2 | 206 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.86 [0.52, 1.42] |
| 4.47.2 Re‐operation | 1 | 173 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.46 [0.20, 1.08] |
| 4.47.3 Surgical complications | 1 | 25 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.92 [0.06, 13.18] |
| 4.48 Adverse events (measured using re‐admission rate: combined for all strategy types | 1 | Rate Ratio (IV, Fixed, 95% CI) | Totals not selected | |
| 4.49 Adverse events (measured using rate of falls): combined for all strategy types | 3 | Rate Ratio (IV, Fixed, 95% CI) | 0.79 [0.63, 0.99] | |
| 4.50 Adverse events (measured using rate of falls): gait, balance and function | 2 | Rate Ratio (IV, Fixed, 95% CI) | 0.78 [0.62, 0.99] | |
| 4.51 Adverse events (measured using rate of falls): other (additional phone support and coaching) | 1 | Rate Ratio (IV, Fixed, 95% CI) | Totals not selected | |
| 4.52 Adverse events (measured as number of people who experienced 1 or more falls) | 4 | Risk Ratio (IV, Fixed, 95% CI) | 1.03 [0.85, 1.25] | |
| 4.53 Adverse events (measured using continuous measure of pain) | 3 | 242 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.04 [‐0.29, 0.22] |
Comparison 5. Post‐hospital rehabilitation: mobilisation strategy versus control, other important outcomes.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 5.1 Walking (measured as use of walking aid/need for assistance) | 4 | 314 | Risk Ratio (M‐H, Random, 95% CI) | 0.46 [0.16, 1.31] |
| 5.2 Walking (measured using self‐reported outcomes) | 2 | 182 | Risk Ratio (M‐H, Random, 95% CI) | 0.55 [0.28, 1.06] |
| 5.3 Balance (measured using functional reach test, cm) | 2 | 144 | Mean Difference (IV, Fixed, 95% CI) | 1.30 [‐1.70, 4.31] |
| 5.4 Balance (measured using timed standing in various positions) | 2 | 234 | Std. Mean Difference (IV, Random, 95% CI) | 0.24 [‐0.37, 0.86] |
| 5.5 Balance (measured using balance scale) | 2 | 212 | Std. Mean Difference (IV, Random, 95% CI) | 0.28 [‐0.52, 1.08] |
| 5.6 Balance (measured using continuous self‐reported meaure) | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 5.7 Balance (measured using dichotomous self‐reported measure) | 2 | 148 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.82 [0.69, 0.98] |
| 5.8 Sit to stand (measured as number of stand ups/second) | 5 | 457 | Mean Difference (IV, Random, 95% CI) | ‐6.49 [‐12.23, ‐0.75] |
| 5.9 Strength | 14 | 1121 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.30 [0.18, 0.42] |
| 5.10 Strength subgrouped by studies with cognitive impairment included v studies with cognitive impairment not included, combined data for all strategy types | 14 | Std. Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 5.10.1 People with cognitive impairment included | 2 | 230 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.07 [‐0.19, 0.33] |
| 5.10.2 People with cognitive impairment excluded | 12 | 891 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.37 [0.23, 0.50] |
| 5.11 Strength subgrouped by stage of rehabilitation | 12 | Std. Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 5.11.1 Outpatient | 2 | 227 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.67 [0.39, 0.95] |
| 5.11.2 Secondary and social care | 12 | 890 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.39 [0.25, 0.52] |
| 5.12 Strength subgrouped by mean age ≤ 80 years v > 80 years, combined data for all strategies | 14 | Std. Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 5.12.1 Mean age in study 80 years or less | 8 | 464 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.35 [0.16, 0.54] |
| 5.12.2 Mean age in study > 80 years | 6 | 657 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.27 [0.11, 0.43] |
| 5.13 Activities of daily living (measured using ADL scales) | 6 | 683 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.01 [‐0.26, 0.23] |
| 5.14 Self‐reported measures of lower limb/hip function | 2 | 106 | Std. Mean Difference (IV, Random, 95% CI) | 0.78 [‐0.20, 1.77] |
Comparison 6. Post‐hospital rehabilitation: comparing different intervention strategies, critical outcomes.
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Baker 1991.
| Study characteristics | ||
| Methods | Quasi‐randomised trial: by alternation; participants were allocated "sight unseen" | |
| Participants | Caulfield Hospital, Victoria, Australia Period of study: started 12 May 1985 40 participants Inclusion: women with a hip fracture Exclusion: rheumatoid arthritis, active cardiac disease, neurological condition that would influence gait pattern Age: mean 83.5 years (range 69 to 97 years) % male: none Number lost to follow‐up: probably none, although 1 died. | |
| Interventions | Early postoperative rehabilitation
1. Treadmill gait retraining programme. Use of Repco treadmill with velocity and distance controls. Adjustable side rails for partial weight‐bearing stage.
versus
2. Conventional gait retraining involving use of ambulatory aid (walking frame) Both groups had participated in the same muscle strengthening programme beforehand. Other aspects of physical therapy was reported to be similar. |
|
| Outcomes | Length of follow‐up: until discharge from rehabilitation hospital Mobility level at discharge (3 levels: house bound; limited outdoor activity; outdoor activity unlimited by symptoms) Walking velocity Knee extensor strength Return to living at home Length of hospital stay Mortality (in hospital) |
|
| Notes | A subgroup of 6 'matched pairs' were studied in greater detail for gait analysis, strength and length of stay. These matched pairs are not included in this review. Funding: none declared Conflict of interest: nil |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Quasi‐randomised trial involving alternation: "the first patient was allocated to the treadmill group, the second to the control group, and so on". |
| Allocation concealment (selection bias) | High risk | Predictable sequence even though researcher apparently "allocated patient 'sight unseen'" |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | No mention of blinding of therapists conducting the intervention and the participants. Impact of non‐blinding is unclear. |
| Blinding of outcome assessment (detection bias) Observer‐reported outcomes, some judgement | High risk | There was no mention of blinding. |
| Blinding of outcome assessment (detection bias) Observer‐reported outcomes, no judgement | Low risk | Not blinded; however, the assessment of the outcome is unlikely to be influenced by knowledge of group allocation |
| Incomplete outcome data (attrition bias) Observer‐reported outcomes, some judgement | High risk | Measure of mobility assessment was crude. Gait analysis was reported for 6 matched pairs: this decision was not explained fully. |
| Incomplete outcome data (attrition bias) Death, re‐admission, re‐operation, surgical complications, return to living at home | High risk | The group allocations for the only death and the 5 other participants requiring nursing home or special accommodation were not given. |
| Selective reporting (reporting bias) | High risk | The reason for reporting gait analysis outcomes for 6 matched pairs was not provided. |
| Free from baseline imbalance bias? | Unclear risk | Insufficient information |
| Free from performance bias due to non‐trial interventions? | Low risk | Explicit mention of comparability |
Binder 2004.
| Study characteristics | ||
| Methods | Randomised trial: use of a computer‐generated algorithm and block design, stratified by type of surgery (hemiarthroplasty or internal fixation) | |
| Participants | Community‐dwellers, St Louis, Missouri, USA Period of study: August 1998 to May 2003 90 participants Inclusion: physically frail people (modified Physical Performance Test score of 12 to 28 and ADL difficulty) aged 65 years or over with a surgically‐repaired proximal femoral fracture in the previous 16 weeks who had completed standard physical therapy. Informed consent Exclusion: pathological fracture, contralateral hip fracture, dementia or cognitive impairment, inability to walk 50 feet, visual or hearing impairments interfering with participation, other major medical conditions (cardiopulmonary or neuromuscular disease), taking medication for osteoporosis, on hormone replacement therapy, terminally ill Age: mean 80 years (range not given) % male: 26 Number lost to follow‐up: 5 (2 due to personal reasons, 2 due to medical problems, 1 died) | |
| Interventions | Started after end of standard physical therapy.
1. Six months of supervised exercise carried out 3 times weekly. For the first 3 months, small group (2 to 5 participants) progressive exercise for flexibility, balance, co‐ordination, movement speed, strength and endurance led by a physical therapist. After the first 3 months, progressive resistance training was added (progressed by end of 1 month to 3 sets of 8 to 12 repetitions at 85% to 100% of initial 1 RM voluntary strength.
versus
2. Low‐intensity, non‐progressive home exercise programme carried out 3 times weekly after a 1‐hour training session, plus monthly group sessions and weekly 10‐minute telephone calls. Additional interventions for both groups: monitoring and instruction by dietitian if indicated, and vitamin D if indicated at baseline. All received calcium and multi‐vitamin tablets. |
|
| Outcomes | Length of follow‐up: 6 months Physical Performance Test score (modified) Functional Status Questionnaire score Instrumental Activities of Daily Living score Basic Activities of Daily Living score Use of assistive gait devices Knee extension strength Fast walking speed Single limb stance time Berg Balance Scale SF‐36 (health, physical function, social subscales) Hip Rating Questionnaire Adherence Adverse events and subsequent fractures Mortality |
|
| Notes |
Host 2007 reported data only from intervention group participants (31/46 participants) who had completed at least 30 sessions in each of the two 3‐month exercise phases. Measured adherence Funding: National Institute of Aging grant R01 G15795, the Washington University General Clinical Research Center grant 5‐M01 RR00036, the Washington University Clinical Nutrition Research Center grant P30 DK56341, and the Barnes Jewish Hospital Foundation. Conflict of interest: nil |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "Random assignment ... was performed on completion of the baseline assessments within strata, defined as the types of surgical repair procedure (hemiarthroplasty vs open reduction internal fixation), using a computer generated algorithm and block design." |
| Allocation concealment (selection bias) | Unclear risk | No clear indication of allocation concealment |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Therapists conducting the intervention and participants were not blinded to the group assignment. Impact of non‐blinding is unclear |
| Blinding of outcome assessment (detection bias) Observer‐reported outcomes, some judgement | Low risk | There was blinding of outcome assessors: "the research staff who conducted the assessments were not involved in exercise training and were blinded to group assignment". |
| Blinding of outcome assessment (detection bias) Observer‐reported outcomes, no judgement | Unclear risk | Binding relating to attribution of study related/unrelated causes of medical problems or fractures is uncertain. |
| Blinding of outcome assessment (detection bias) Participant/proxy‐reported outcomes | Unclear risk | There was blinding of outcome assessors: "the research staff who conducted the assessments were not involved in exercise training and were blinded to group assignment". |
| Incomplete outcome data (attrition bias) Observer‐reported outcomes, some judgement | Unclear risk | Five of the 90 participants were lost to follow‐up at 6 months. The last observation for these 5 participants was carried forward and an intention‐to‐treat analysis was conducted with data for the whole trial population. |
| Incomplete outcome data (attrition bias) Death, re‐admission, re‐operation, surgical complications, return to living at home | Low risk | Mortality follow‐up adequate |
| Incomplete outcome data (attrition bias) Participant/proxy‐reported outcomes | Unclear risk | Five of the 90 participants were lost to follow‐up at 6 months. The last observation for these 5 participants was carried forward and an intention‐to‐treat analysis was conducted with data for the whole trial population. |
| Selective reporting (reporting bias) | Low risk | Pre‐trial completion information shows consistent primary outcome |
| Free from baseline imbalance bias? | Low risk | Comprehensive breakdown of characteristics without significant differences |
| Free from performance bias due to non‐trial interventions? | Low risk | Measures taken to counteract differences in social contact in the control group by weekly phone calls |
Bischoff‐Ferrari 2010.
| Study characteristics | ||
| Methods | Randomised trial: 2x2 factorial design | |
| Participants | Triemli City Hospital, Switzerland
Period of study: January 2005 to December 2007
173 participants
Inclusion: aged 65 years or over with a surgically‐repaired hip fracture, MMSE ≥ 15, able to walk 3 m, German speaking, creatinine clearance of more than 15 mL/min (to convert to millilitres per second, multiply by 0.0167)
Exclusion: prior fracture of same hip, metastatic cancer or chemotherapy in the last year, severe visual or hearing impairment, kidney stone in the past 5 years, hypercalcaemia, primary hyperparathyroidism or sarcoidosis Age: mean 84 years (range 65 to 99) % male: 21 Number lost to follow‐up: 22. Analysed as ITT |
|
| Interventions | Extended physiotherapy plus high/low dose cholecalciferol 1. Extended physiotherapy plus 800 IU/d cholecalciferol. Supervised 60 min during acute care (additional 30 min home programme instruction each day during acute care) plus unsupervised home programme over 12 months. Advised to maintain usual diet and avoid additional calcium and cholecalciferol supplements. 2. Standard physiotherapy (supervised 30 min/day during acute care plus no home programme) plus 2000 IU/d cholecalciferol 3. Extended physiotherapy plus 2000 IU/d cholecalciferol. 4. Control. Standard physiotherapy (supervised 30 min/day during acute care plus no home program) plus 800 IU/d cholecalciferol. Advised to maintain usual diet and avoid additional calcium and cholecalciferol supplements. Only the comparison of standard versus extended physiotherapy eligible for inclusion in this review. |
|
| Outcomes | Length of follow‐up: 24 weeks Mortality Knee extensor Timed Up & Go EQ‐5D‐3L Adverse effects: re‐fracture rate, re‐admission, admission to institution, falls, mild hypercalcaemia, nephrolithiasis Adherence (total days and minutes of physiotherapy) |
|
| Notes | Measured adherence Funding: this study was supported by Swiss National Foundations (NFP‐53), Vontobel Foundation, Baugarten Foundation and Swiss National Foundations professorship grant PP00B‐ 114864. Conflict of interest: nil |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐based randomisation |
| Allocation concealment (selection bias) | Unclear risk | Not clearly reported |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Therapists conducting the intervention and participants were not blinded to the group assignment. Impact of non‐blinding is unclear |
| Blinding of outcome assessment (detection bias) Observer‐reported outcomes, some judgement | Low risk | Outcome assessors blinded |
| Blinding of outcome assessment (detection bias) Observer‐reported outcomes, no judgement | Low risk | Outcome assessors blinded. All admission records were reviewed by 3 blinded co‐investigators to determine the main cause of re‐admission. |
| Blinding of outcome assessment (detection bias) Participant/proxy‐reported outcomes | Unclear risk | Outcome assessors blinded for health‐related quality of life. Blinding of personnel collecting fall data and answering hotline telephones was not specified. |
| Incomplete outcome data (attrition bias) Observer‐reported outcomes, some judgement | High risk | Large degree of loss to follow‐up. Although analysed as ITT, the high degree of attrition incurs a high risk of bias. |
| Incomplete outcome data (attrition bias) Death, re‐admission, re‐operation, surgical complications, return to living at home | High risk | Large loss to follow‐up |
| Incomplete outcome data (attrition bias) Participant/proxy‐reported outcomes | High risk | Large loss to follow‐up |
| Selective reporting (reporting bias) | Unclear risk | Mobility outcomes not clearly stated in study registration |
| Free from baseline imbalance bias? | Low risk | Groups balanced at baseline |
| Free from performance bias due to non‐trial interventions? | High risk | Extended physiotherapy had home visits which may have a confounding effect due to the social interaction |
| Method of ascertaining falls | Low risk | Falls recorded via monthly telephone calls and a patient diary. Also, a telephone hotline to report falls at any time |
Braid 2008.
| Study characteristics | ||
| Methods | Randomised controlled trial | |
| Participants | Two rehabilitation units at two hospitals (Glasgow Royal Infirmary and Hairmyres Hospital), UK Period of study: November 1999 to November 2000 26 participants Inclusion: people aged ≥ 65 years with hip fracture treated surgically (all internal fixation) up to 21 days previously, written informed consent Exclusion: terminal disease, abbreviated mental score < 7/10, previous inability to walk, profoundly deaf, cardiac pacemaker, unstable medical conditions (e.g. pneumonia, heart failure) Age: mean 81 years (range not stated) % male: 8% Number lost to follow‐up: 3 refusals + 2 deaths; also 2 telephone follow‐up only | |
| Interventions | Postoperative rehabilitation 1. Supplementary electrical stimulation (ES) of quadriceps for 6 weeks: 5 days / week for inpatients; twice a week upon discharge. ES consisted of 7 seconds of stimulation of quadriceps followed by 23 seconds of relaxation for 36 repetitions; each session lasted 18 minutes. Delivery by physiotherapist assistant. Usual physiotherapy. versus 2. Usual physiotherapy only. Inpatient physiotherapy consisted of supervised strengthening and range of motion exercises, balance training, work on transfers and progressive gait re‐education. Expert physiotherapist established optimum electrical stimulation post‐baseline measurement but prior to randomisation (tolerance levels not provided for control group participants). Intervention started in hospital, baseline measurements at median 10 to 11 days post‐surgery, and continued at home after hospital discharge. |
|
| Outcomes | Length of follow‐up: 14 weeks Elderly Mobility Scale Leg extension power Barthel Index Nottingham Health Profile (gait speed, emotional reactions, energy, pain, physical mobility, sleep, social isolation) Mortality |
|
| Notes | Two other outcomes (Timed Up and Go test, isometric quadriceps strength) described in trial registration / abstracts but not in full report Funding: Royal Infirmary Reserch Endowments Fund Conflict of interest: nil |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "Randomisation was by computer‐generated random numbers" |
| Allocation concealment (selection bias) | Low risk | "[With] individual patient codes held in opaque sealed envelopes by an administrator independent from the study.” |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Therapists conducting the intervention and participants were not blinded to the group assignment. Impact of non‐blinding is unclear |
| Blinding of outcome assessment (detection bias) Observer‐reported outcomes, some judgement | Low risk | “Measurements were made at baseline, at 6 weeks (the end of intervention) and 14 weeks by a single blinded assessor.” |
| Blinding of outcome assessment (detection bias) Observer‐reported outcomes, no judgement | Low risk | Only mortality was reported. “Measurements were made at baseline, at 6 weeks (the end of intervention) and 14 weeks by a single blinded assessor.” Assessment of mortality is not likely to be influenced by knowledge of group allocation. |
| Incomplete outcome data (attrition bias) Observer‐reported outcomes, some judgement | Unclear risk | Although participant flow data provided, loss to follow‐up was proportionality greater in the intervention group. |
| Incomplete outcome data (attrition bias) Death, re‐admission, re‐operation, surgical complications, return to living at home | Low risk | Only mortality reported |
| Selective reporting (reporting bias) | Unclear risk | Consistent reporting of primary outcomes, but 'Timed Up and Go test' and isometric muscle data indicated in abstract and trial registration form are missing |
| Free from baseline imbalance bias? | Unclear risk | "There was a non‐significant trend for the control group to have a greater unfractured leg extensor power and higher Barthel scores at study entry." Proportionally fewer intervention group participants had independent mobility at baseline (27% versus 55%). |
| Free from performance bias due to non‐trial interventions? | Unclear risk | Although participants in both groups received standard physiotherapy while inpatients, it is not clear whether post‐discharge provision was similar. |
Gorodetskyi 2007.
| Study characteristics | ||
| Methods | Randomised controlled trial | |
| Participants | Moscow City Hospital NO71, Moscow, Russia Period of study: February to November 2005 60 participants Inclusion: people aged between 60 and 75 years who had undergone stabilisation (dynamic hip screw or external fixation) of an A2 femoral trochanteric fracture. Informed consent Exclusion: limitations that might interfere with electrical stimulation including insulin pumps, pacemakers and neurostimulation implants; history of epilepsy or seizure; bilateral fractures; pathological fractures (excluding osteoporosis) Age: mean 71 years (range 63 to 75) % male: 33% Number lost to follow‐up: 0 | |
| Interventions | Postoperative rehabilitation. Electrical stimulation or placebo (sham device) included in the standard rehabilitation started within 24 hours of surgery. Treatments and physiotherapy were carried out each morning and took 20 to 30 minutes to complete. Non‐steroidal anti‐inflammatory drug (ketorolac tromethamine) prescribed as needed. 1. Electrical stimulation (ES) for 10 days: use of a hand‐held, non‐invasive, interactive neurostimulation device (InterX 5000; Neuro Resource Group, Plano, Texas). (Device generates high peak amplitude averaging 17 volts on the skin with a low current of about 6 milliamperes (mA), and damped biphasic electrical impulses which are delivered to the tissue via a pair of concentric electrodes placed in direct contact with the target area. Device adjusts biphasic stimulus in accordance to the impedance of the underlying tissue by varying voltage to maintain constant peak current. Device applied for 20 to 30 minutes with electrodes at 3 sites close to surgical incision. Also corresponding areas on contralateral side. After adjustment for impedance, intensity increased to produce "comfortable sensation for patient"). versus 2. Sham device; same timing. All the participants received standard interdisciplinary postoperative care including routine assessment and daily care by an orthopaedic surgeon supported by a physiotherapist and nurse. |
|
| Outcomes | Length of follow‐up: 10 days (end of treatment) Pain score (VAS: 0 to 10: worst) 'Pain inventory': effects of pain on walking ability, sleep, mood and enjoyment of life (1: no interference; 10: absolute interference) Analgaesic consumption Surgeon's evaluation of participant's progress at 10 days in terms of improvement: none, minimal, average, substantial, full recovery |
|
| Notes | All participants were functionally independent before start of study.
Authors refer to reduced life expectancy in Russia. Funding / conflict of interest: "The author or one or more of the authors have received or will receive benefits for personal or professional use from a commercial party related directly or indirectly to the subject of this article. In addition, benefits have been or will be directed to a research fund, foundation, educational institution, or other nonprofit organisation with which one or more of the authors are associated". |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Insufficient information. "Fixed randomisation scheme with sealed envelopes" |
| Allocation concealment (selection bias) | Unclear risk | "Fixed randomisation scheme with sealed envelopes" |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | "The therapist who administered treatment was aware of the assignment of the patient to an active or sham device. However, all the assessing surgeons, patients and research personnel involved in determining and recording outcome measurements were blinded to this information. The sham device had an identical appearance and application to the active device with lights, buzzing and beeps, but did not produce interactive neurostimulation." Patient blinding may not be possible if they are familiar with neurostimulation. |
| Blinding of outcome assessment (detection bias) Observer‐reported outcomes, some judgement | Low risk | All the assessing surgeons, patients and research personnel involved in determining and recording outcome measurements were blinded to this information (active v sham device). |
| Blinding of outcome assessment (detection bias) Observer‐reported outcomes, no judgement | Low risk | Assessment of the outcome is not likely to be influenced by knowledge of group allocation. |
| Incomplete outcome data (attrition bias) Observer‐reported outcomes, some judgement | Low risk | No loss to follow‐up |
| Incomplete outcome data (attrition bias) Death, re‐admission, re‐operation, surgical complications, return to living at home | Unclear risk | Not reported |
| Selective reporting (reporting bias) | Unclear risk | Possible but no trial protocol or trial registration available |
| Free from baseline imbalance bias? | Low risk | Intervention groups appeared well matched. |
| Free from performance bias due to non‐trial interventions? | Low risk | Same rehabilitation provided to all |
Graham 1968.
| Study characteristics | ||
| Methods | Randomised trial: method not stated; stratified by age of participant | |
| Participants | Western Infirmary, Glasgow, UK Period of study: February 1961 to August 1966 273 participants (but possible that 604 participants were randomised) Inclusion: people with a displaced intracapsular proximal femoral fracture (Garden type III or IV) treated by closed reduction and internal fixation with a sliding nail plate. Exclusion (post randomisation): any reason (pulmonary or cardiac complications, deep venous thrombosis, general feebleness, re‐displacement of the fracture) at 2 weeks that the individual was not considered fit enough to walk at this time. Age: not stated (within 56 to 95 for the 175 participants followed up for 3 years) % male: not known Number lost to follow‐up: disregarding post‐randomisation exclusions, 13 with incomplete follow‐up and 43 died at 1 year. | |
| Interventions | Early postoperative rehabilitation. Operative treatment consisted of closed fracture reduction and internal fixation with a sliding nail plate. For the first 2 weeks postop, patients sat out of bed but were not permitted to stand or walk. 1. Early weight bearing at 2 weeks after surgery: unguarded walking versus 2. Delayed weight bearing until 12 weeks after surgery | |
| Outcomes | Length of follow‐up: 1 year for all, 3 years for subgroup Mortality Non‐union of the fracture (failure) Avascular necrosis (segmental collapse) Infection of the hip |
|
| Notes | An interim report for 124 trial participants at 3 months was available in 1964 (Abrami 1964), with a second report in 1968 (Graham 1968) which presented results for 273 participants at 1 year and results at 3 years for the 175 participants who had been followed up by then. Data from Abrami 1964 are not presented in the review. Funding: none declared Conflict of interest: none declared |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | According to earliest report: "After operation, but according to the sequence of their admission to hospital, patients in comparable five‐year age groups were randomly allocated to either the early or the late weight‐bearing groups" (Abrami 1964). But as reported by Graham 1968: "After admission to hospital each patient was allocated, by random selection, to an early or late weight‐bearing group within each decade from fifty‐six to ninety‐five years'. It was emphasised in the report that it was not alternation. |
| Allocation concealment (selection bias) | Unclear risk | No information |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | No mention of blinding. Impact of non‐blinding is unclear |
| Blinding of outcome assessment (detection bias) Observer‐reported outcomes, some judgement | High risk | No mention of blinding, nor of measures taken to safeguard knowledge of allocation at follow‐up data collection |
| Blinding of outcome assessment (detection bias) Observer‐reported outcomes, no judgement | Unclear risk | No mention of blinding; however, assessment of the outcome is unlikely to be influenced by knowledge of group allocation |
| Incomplete outcome data (attrition bias) Observer‐reported outcomes, some judgement | High risk | Outcomes were not reported. Even so, there was incomplete long‐term follow‐up (only 175 of the 273 included participants ‐ after post‐randomisation exclusions) ‐ see next item. |
| Incomplete outcome data (attrition bias) Death, re‐admission, re‐operation, surgical complications, return to living at home | High risk | Trial recruitment and randomisation were at hospital admission (604 admitted), but only those 273 patients who were judged as being suitable ‐ in that they could be expected to walk at the 2‐week clinical assessment ‐ were included in the analyses. The number of participants excluded at 2 weeks was not reported. Included participants were analysed in the group they were allocated at randomisation. |
| Selective reporting (reporting bias) | High risk | No indication of a protocol. Interim results generally reported. Differences between papers in account of trial (e.g. stratification) |
| Free from baseline imbalance bias? | High risk | Baseline data not given for randomised groups, nor for followed‐up participants, with the exception of gender and age group. All intracapsular fractures treated with same implant |
| Free from performance bias due to non‐trial interventions? | High risk | No information |
Hauer 2002.
| Study characteristics | ||
| Methods | Randomised controlled trial using a protected random number system; stratified by hip‐ or lower‐extremity fracture surgery and non‐hip‐ or lower‐extremity fracture patients (see Notes) | |
| Participants | Heidelberg, Germany Period of study: not stated, but trial may have started around 1997 28 female participants Inclusion: females aged ≥ 75 years (25 with a fall‐related hip fracture and 3 with elective hip surgery) who had experienced a recent injurious fall. Written informed consent and permission from orthopaedic surgeon Exclusion: acute neurological impairment, severe cardiovascular disease, unstable chronic or terminal illness, major depression, severe cognitive impairment, severe musculoskeletal impairment Age: mean 81 years (range not stated) % male: none Number lost to follow‐up: 4 (3 didn't start exercises and 1 dropped out) | |
| Interventions | Started immediately upon hospital discharge.
1. 12‐week regimen of intensive physical training (lower extremity progressive resistance training, progressive functional and balance training). All exercise sessions took place in training groups (4 to 6 participants) supervised by a therapeutic recreation specialist. Each session: 1.5 hours of resistance training (with recovery breaks) and 45 minutes of balance/functional training. Intensity of strength training adjusted to 70% to 90% of individual maximal workload. Basic functions such as walking, stepping or balancing were trained progressively with increasing complexity.
versus
2. Placebo motor activity: 1‐hour sessions of activities such as flexibility exercise, callisthenics, ball games and memory tasks while seated. Both regimens, taking place 3 times a week, started on average 4 to 5 weeks after surgery upon discharge from inpatient rehabilitation. Both groups received identical additional physiotherapy (mainly massage, stretching and application of heat or ice) twice weekly for 25 minutes: strength and balance training was excluded from these sessions. |
|
| Outcomes | Length of follow‐up: 6 months (12 weeks + 3 months) Walking velocity and cadence Independent weight bearing Performance‐orientated motor assessment Box step Functional Reach Timed Up and Go test Chair and stair rises Activities of daily living; sports and household activities Muscle strength: leg‐press, leg‐extensor, leg flexor, ankle‐plantar flexion, hand grip strength (non‐trained muscle group) Loss of independence Subjective fear of falling Subjective walking steadiness Emotional state: depression, morale and handicap scales Adherence |
|
| Notes | Measured adherence This trial was excluded from versions of this review up to Issue 3, 2004 because the intervention began after the early postoperative period covered by this review, which then focused on early postoperative rehabilitation. Trial actually included 57 people who had experienced an injurious fall. One report of the trial gave the results for the subgroup of 28 participants who had hip surgery. Of these, 25 had surgery for a fall‐related hip fracture and 3 had elective hip surgery. The patient characteristics of the latter 3 women were confirmed as being essentially similar to those of the 25 women with hip fracture. A 2‐year follow‐up of the trial is available but only for the whole trial population. Further information, including method of randomisation, received from lead trialist on 05 March 2004 and 24 June 2004 Funding: grant from Ministerium fur Wissenschaft, Forschung und Kunst Baden‐Wuerttemberg and the University of Heidelberg Conflict of interest: none declared |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "Randomization was performed .... using a protected random number system" |
| Allocation concealment (selection bias) | Low risk | "Randomization was performed by an external person who did not participate in the study using a protected random number system" |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Care providers providing the intervention and the participants were not blinded to the group assignment. Impact of non‐blinding is unclear |
| Blinding of outcome assessment (detection bias) Observer‐reported outcomes, some judgement | Low risk | "Main outcome variables were documented by a person blinded to the patients' group assignment." |
| Blinding of outcome assessment (detection bias) Participant/proxy‐reported outcomes | Unclear risk | "Main outcome variables were documented by a person blinded to the patients' group assignment." |
| Incomplete outcome data (attrition bias) Observer‐reported outcomes, some judgement | High risk | Efforts had been made to collect outcome data for the 4 dropouts, 3 of whom did not start the exercises and 1 who discontinued their exercises. However, these data were not available. |
| Incomplete outcome data (attrition bias) Death, re‐admission, re‐operation, surgical complications, return to living at home | Unclear risk | While all participants were accounted for, there were incomplete data on complications (although: 'minor') and long‐term follow‐up. |
| Incomplete outcome data (attrition bias) Participant/proxy‐reported outcomes | High risk | Efforts had been made to collect outcome data for the 4 dropouts, 3 of whom did not start the exercises and 1 who discontinued their exercises. However, these data were not available. |
| Selective reporting (reporting bias) | Unclear risk | Unclear. However, the 3 main reports of the trial were consistent in the reported outcomes and the author provided clarification on some of the outcome measures used. |
| Free from baseline imbalance bias? | Low risk | Baseline characteristics were similar in the 2 groups. |
| Free from performance bias due to non‐trial interventions? | Low risk | There was no cause for concern. |
Karumo 1977.
| Study characteristics | ||
| Methods | Randomised trial: use of random numbers | |
| Participants | University Central Hospital, Helsinki, Finland Period of study: May 1973 to October 1974 100 participants Inclusion: people aged > 50 years with femoral neck fracture treated surgically (internal fixation or prosthesis), capable of independent 'getting about' before fracture Exclusion: none given Age: mean 73 years (range not stated; all over 50 years) % male: 25% Number lost to follow‐up: 13 (excluded from 9‐week follow‐up because of inadequate follow‐up), 4 (excluded from 3‐month mortality data) | |
| Interventions | Early postoperative rehabilitation, started first postoperative day onwards
1. Intensive (performed twice daily) physiotherapy regimen
versus
2. Same regimen performed once daily (conventional care) Routine physiotherapy was on average 30 minutes per day. For the intensive group, the physiotherapy time was doubled. Both groups were under supervision of the study physiotherapist. Regimen was continued for 14 days. From first postoperative day, training in walking on crutches; training in sitting in chair; flexion‐extension movements of knee, hip and ankle. Most participants were allowed full weight bearing from the beginning. (For those with internal fixation, crutch use for up to 2 to 3 months.) From second postoperative week, training in walking up and down stairs. |
|
| Outcomes | Length of follow‐up: 9 weeks (for strength) Walking ability Ability to move and sit up in bed on first postoperative day Abductor muscle strength at 9 weeks Residence at 9 weeks Mortality "Mechanical" postoperative complications Medical complications, including thromboembolism and postoperative infection Length of hospital stay |
|
| Notes | Of the 100 people recruited for the trial, 13 had inadequate follow‐up and the results of these participants are not presented. Most of the results for the trial were presented split according to whether the participant had a prosthesis or internal fixation, rather than by the trial interventions. A thesis (1978, University of Helsinki) was located by Lesley Gillespie (10 June 2004). Requests for a copy met with no success. Funding: none declared Conflict of interest: none declared |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "Using random numbers the patients selected for the study were divided before the operation into two physiotherapy groups." |
| Allocation concealment (selection bias) | Unclear risk | No report |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | No mention of blinding. Impact of non‐blinding is unclear |
| Blinding of outcome assessment (detection bias) Observer‐reported outcomes, some judgement | High risk | No mention of blinding |
| Blinding of outcome assessment (detection bias) Observer‐reported outcomes, no judgement | Unclear risk | No mention of blinding; however, assessment of the outcome is unlikely to be influenced by knowledge of group allocation. |
| Incomplete outcome data (attrition bias) Observer‐reported outcomes, some judgement | High risk | Results for 13 participants with inadequate follow‐up were not presented. |
| Incomplete outcome data (attrition bias) Death, re‐admission, re‐operation, surgical complications, return to living at home | High risk | Results for 13 participants with inadequate follow‐up were not presented. |
| Selective reporting (reporting bias) | High risk | Mobility data split by treatment group were not presented. |
| Free from baseline imbalance bias? | High risk | There was a lack of information on baseline characteristics and comparability; data were not provided for 13 participants with inadequate follow‐up. The report referred to a non‐significantly greater number of participants in the routine physiotherapy group being treated with Jewett nails. |
| Free from performance bias due to non‐trial interventions? | Low risk | Appears so; the same physiotherapist provided both interventions. |
Kimmel 2016.
| Study characteristics | ||
| Methods | Randomised controlled trial. Randomly assigned by computer program | |
| Participants | The Alfred Hospital, a level 1 trauma centre, Melbourne, Australia Period of study: March 2014 to January 2015 92 participants Inclusion: at least 65 years old, admitted with an isolated subcapital or intertrochanteric hip fracture, treated by internal fixation or hemiarthroplasty Exclusion: subtrochanteric or pathological fracture; postoperative orders for non‐weight bearing on the operated hip; unable to move independently or needed a gait aid prior to admission; admitted from nursing home Age: mean (SD) = 81.3 (8.2) % male: 36 Number lost to follow‐up: 13 (died = 1, unable to contact via telephone at 6 months = 12) | |
| Interventions | 1. Intervention group: usual care* in the morning plus 2 additional daily sessions, 7 days per week. One session (delivered by allied health assistant) practised the achievements of the morning session. One session (delivered by physiotherapist) aimed to improve the functional advances achieved during the earlier physiotherapy session; e.g. increased independence, progression of gait aid (e.g. from frame to crutches) and increasing the distance walked. 2. Control: usual care* in the morning *Usual care: participants in both groups received daily physiotherapy according to usual practice in the trauma centre, 7 days per week. Treatment was individualised and involved bed‐based limb exercises (e.g. strength exercises, such as knee extension, and active hip exercises) and gait re‐training. The goal was early, independent transfer and mobility, with the objective of discharge directly home or to fast stream rehabilitation. |
|
| Outcomes | Length of follow‐up: Mobility and Modified Iowa Level of Assistance outcomes = Day 5 postop (or discharge, if discharged before Day 5); QOL 6 months. Modified Iowa Level of Assistance score (hip‐fracture‐specific outcome, with 6 domains, including bed and chair transfer, ambulation, ascending/descending 1 step, and gait aid used, 0 (independent in all activities without a gait aid) to 36 (unable to attempt any of the activities). Day 5 or day of discharge (if earlier) Timed Up and Go test Day 5 or day of discharge (if earlier) Length of stay (acute, inpatient rehabilitation, combined) Inpatient complication Re‐admission SF‐12, EQ‐5D (6 months) Discharge destination Death |
|
| Notes | Resource use collected: physiotherapy hours of service, acute / rehab / combined hospital length of stay Funding: Victorian Department of Health (Workforce Innovation and Allied Health) Conflict of interest: nil |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Participants were randomly assigned by computer program" |
| Allocation concealment (selection bias) | Unclear risk | Allocation concealment not specified. Insufficient information to permit judgement |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Therapists conducting the intervention and participants were not blinded to the group assignment. Impact of non‐blinding is unclear. The usual care physiotherapist was blinded to allocated group. |
| Blinding of outcome assessment (detection bias) Observer‐reported outcomes, some judgement | Low risk | Blinding specified for Modified Iowa Level of Assistance, Timed Up and Go test. |
| Blinding of outcome assessment (detection bias) Observer‐reported outcomes, no judgement | Low risk | Blinding not specified, but likely as data were collected from Victorian Orthopaedic Trauma Outcomes Registry, for SF‐12, EQ‐5D and Glasgow Outcome Scale. Blinding not specified for length of stay, inpatient complications, re‐admissions. Outcome measurement is unlikely to be influenced by lack of blinding. |
| Blinding of outcome assessment (detection bias) Participant/proxy‐reported outcomes | Unclear risk | Health‐related quality of life data derived from data in the Victorian Orthopaedic Trauma Outcomes Registry. Can assume this was collected by personnel blinded to the study. |
| Incomplete outcome data (attrition bias) Observer‐reported outcomes, some judgement | Unclear risk | Timed Up and Go test performed only for people who could walk, so only 40/92 (42%) of participants contributed to this measure. All participants contributed to other measures at 5 days postop. |
| Incomplete outcome data (attrition bias) Death, re‐admission, re‐operation, surgical complications, return to living at home | Low risk | 13/92 (14%) lost to follow‐up at 6 months |
| Incomplete outcome data (attrition bias) Participant/proxy‐reported outcomes | Low risk | 15% lost to follow‐up at 6 months for health‐related quality of life |
| Selective reporting (reporting bias) | Low risk | All outcomes specified in trial registry and methods section were reported in the results |
| Free from baseline imbalance bias? | High risk | There were statistically significant between‐group differences in anaesthetic type (general versus spinal), proportion of men, and having a carer at home. |
| Free from performance bias due to non‐trial interventions? | Low risk | Care and experience of care providers was consistent across groups |
Kronborg 2017.
| Study characteristics | ||
| Methods | Randomised trial (randomisation was stratified for fracture type (trochanteric/femoral neck)) | |
| Participants | Acute orthopaedic ward at a university hospital, Copenhagen, Denmark Period of study: October 2013 to May 2015 90 participants Inclusion: home‐dwelling, primary hip fracture surgery, aged 65 years or older, able to speak and understand the Danish language, independent pre‐fracture indoor walking ability equal to a New Mobility Score ≥ 2 Exclusion: multiple fractures, weight‐bearing restrictions, people unwilling to participate in appropriate rehabilitation or unable to co‐operate in tests, terminal illness, and treatment with total hip arthroplasty or parallel pins Age: mean (SD) 79.6 (7.56) % male: 23 Number lost to follow‐up: 10 (restrictions after X‐ray n = 1, re‐fracture n = 1, discharge without notice n = 2, declined assessment n = 1, death n = 2, transferred n = 2, incomplete follow‐up test of fractured limb n = 1) | |
| Interventions | 1. Intervention: routine physiotherapy* plus additional daily individual progressive knee‐extension strength training with 3 sets of 10 repetitions performed with an intensity of 10 repetition maximum (10 RM), defined as ±2 RM of the fractured limb using ankle weight cuffs. 2. Control: routine physiotherapy* *Routine physiotherapy: basic mobility and exercise therapy primarily aimed at lower extremities following a guideline with 12 specific lower limb exercises, progressed individually and conducted daily on weekdays with 1 to 2 contacts per day (weekends included postoperative day 1 to 3 only). Repetitions and intensity were not standardised. Also basic mobility activities, balance and stair climbing aimed at regaining physical function corresponding with levels of pre‐fracture habitual activity, and progression of walking aids. |
|
| Outcomes | Change in maximal isometric knee‐extension strength (N·m/kg) in the fractured limb in percentage of non‐fractured limb (Maximal Voluntary Torque per kilo body mass) from inclusion to postoperative day 10 or discharge (follow‐up), using belt‐fixed handheld dynamometer Timed Up and Go test, measured as early as possible after surgery when participant could walk independently with rollator and at follow‐up using a rollator as a standardised walking aid Independent mobility at discharge (scored using Cumulated Ambulation Score) Length of admission (postoperative day of discharge) Discharge destination Pain. Hip‐fracture‐related pain at rest and during outcome assessment, evaluated by Verbal Ranking Scale (score 0 to 4) using the highest pain level reported from each session Death |
|
| Notes | The stratification on fracture type was violated in the last 10 included participants due to slow inclusion of participants with a femoral neck fracture, allowing more participants with trochanteric fractures (n = 52) to enter the study compared to femoral neck fractures (n = 38). Measured gait speed and independent mobility, but no data presented. Measured adherence Funding: grants from The IMK Foundation (LK), The Research Foundation of the Capital Region (MTK), The Research Foundation of the Danish Physical Therapy Conflict of interest: none declared |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "[Randomly] allocated to two different postoperative in‐hospital rehabilitation interventions by a neutral person (blinded to outcomes and patient characteristics) via a computer‐generated list" |
| Allocation concealment (selection bias) | Low risk | "[Notes] placed in sealed envelopes and marked with participant numbers only" |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Therapists conducting the intervention and participants were not blinded to the group assignment. Impact of non‐blinding is unclear |
| Blinding of outcome assessment (detection bias) Observer‐reported outcomes, some judgement | Low risk | Outcome assessor was blinded to group assignment. |
| Blinding of outcome assessment (detection bias) Observer‐reported outcomes, no judgement | Unclear risk | Method of assessing death was unclear. |
| Incomplete outcome data (attrition bias) Observer‐reported outcomes, some judgement | Unclear risk | Timed Up and Go test and timed 10 m walk were performed only for people who could walk;unclear what percentage of participants contributed to these measures |
| Incomplete outcome data (attrition bias) Death, re‐admission, re‐operation, surgical complications, return to living at home | Low risk | 10/90 (11%) lost to follow‐up |
| Selective reporting (reporting bias) | High risk | Protocol appended to paper. Thigh and lower leg circumference is an outcome in protocol, but not reported. Protocol states Timed Up and Go test, 10‐Metre Walk Test, New Mobility Score, and isometric strength would be assessed at 16 weeks, but these were not reported in results paper. Data not presented for 10m walk time, but between‐group difference is reported. |
| Free from baseline imbalance bias? | Low risk | No imbalance noted |
| Free from performance bias due to non‐trial interventions? | Low risk | Care and experience of care providers appears consistent across groups |
Lamb 2002.
| Study characteristics | ||
| Methods | Randomised trial: use of sequentially‐numbered, sealed, opaque envelopes; stratified by pre‐injury mobility | |
| Participants | John Radcliffe Nuffield Orthopaedic Hospital, Oxford, UK Period of study: not stated, earliest report located 1998 27 female participants Inclusion: women aged ≥ 75 years who had surgical fixation (not total hip replacement) of a hip fracture, living in own home or a relative's home or in sheltered housing before their injury. Written informed consent Exclusion: history of stroke or Parkinson's disease, clinical depression or acute mental illness, cognitive impairment: 6 or lower on the Hodkinson Mental Test Score. Other fracture, respiratory or cardiac failure sufficient to prevent walking 50 feet (15.25 m), systolic blood pressure > 200 mmHg or diastolic blood pressure > 100 mmHg, surgical complications, pathological fracture. At medication assessment at day 6: on hypnotics, sedatives, muscle relaxant or medications likely to affect muscular function during postoperative period. Age: mean 84 years (range: not stated) % male: none Number lost to follow‐up: 3 excluded. One had myasthenia gravis (confirmed independently as not related to trial), one a severe chest infection and the third participant withdrew consent after a few days. | |
| Interventions | Early postoperative rehabilitation, started at 7 days after surgery.
1. Patterned neuromuscular (electrical) stimulation of the quadriceps muscle for 3 hours a day for 6 weeks. Stimulus intensity was the minimum required for visible muscle contraction. Each stimulus delivered 0.3 micro coulomb of charge.
versus
2. Placebo stimulation for same time period. Interventions started in hospital 1 week after surgery and continued at participants' homes after hospital discharge at 10 to 14 days. A trained assistant, who was independent of the study, showed the participants how to apply the stimulator. |
|
| Outcomes | Length of follow‐up: 12 weeks after randomisation (13 weeks after surgery) Recovery of mobility Walking velocity Leg extensor power Compliance Pain (1: no pain to 6: severe pain) Side effects (none) |
|
| Notes | Patterned neuromuscular (electrical) stimulation is "a variable frequency stimulus (mean frequency 8.9 Hz) derived from the discharge of a fatiguing motor unit of the quadriceps". The stimulator was designed for home use, being portable and independent of an electric supply. Difficulties found by the participants in changing the batteries meant that weekly visits were required by study personnel. Funding: Research into Ageing and the PPP Healthcare Charitable Trust. Conflict of interest: nil |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | “Randomization lists were prepared in advance of the study with a random number table.” |
| Allocation concealment (selection bias) | Low risk | “Assignments were placed in sealed, numbered, opaque envelopes that were opened in a strict sequence after eligibility had been established and consent obtained.” |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Good attempt made to blind participants with placebo stimulation. |
| Blinding of outcome assessment (detection bias) Observer‐reported outcomes, some judgement | Low risk | “The investigator responsible for measuring outcomes and all participants were blind to the treatment assignment." |
| Blinding of outcome assessment (detection bias) Observer‐reported outcomes, no judgement | Low risk | Only complications reported, blinding indicated, and assessment of this outcome is unlikely to be influenced by knowledge of group allocation. |
| Incomplete outcome data (attrition bias) Observer‐reported outcomes, some judgement | Unclear risk | No data, including group allocation, presented for the 3 people who did not complete the study |
| Incomplete outcome data (attrition bias) Death, re‐admission, re‐operation, surgical complications, return to living at home | Unclear risk | Only complications reported |
| Selective reporting (reporting bias) | Unclear risk | Probably, but no trial protocol or trial registration available |
| Free from baseline imbalance bias? | Unclear risk | Incomplete report of baseline data as those for the 3 post‐randomisation exclusions were not available. No major differences in the available data for those followed up. |
| Free from performance bias due to non‐trial interventions? | Low risk | No obvious differences. Both arms included similar usual care. |
Langford 2015.
| Study characteristics | ||
| Methods | Randomised trial | |
| Participants | Acute orthopedic unit in metro Vancouver teaching hospital, Vancouver, BC, Canada Period of study: November 2013 to September 2014 30 participants Inclusion: community‐dwelling adults with a recent fall‐related hip fracture ≥ 60 years of age, recruited following surgical repair. English speaking Exclusion: fracture related to metastatic disease or bisphosphonate use, did not return home in the community after hospital discharge, medical contraindications restricting activity and exercise, hearing or speech impairments precluding telephonic communication, or physician‐diagnosed dementia. Age: mean 82.5 years (range 61 to 97) % male: 37% Number lost to follow‐up: 4 (postoperative complications n = 3, moved to residential care n = 1) |
|
| Interventions | Additional post‐discharge physiotherapist telephone support and coaching 1. Telephone support and coaching: usual care plus 1‐hour in‐hospital individualised education session using the hip fracture recovery manual and 4 educational videos (FReSH Start), plus up to 5 phone calls in the first 4 months post‐fracture from research physiotherapist (average 151 minutes of phone time). Phone calls focused on goal setting regarding recovery goals, mobility goals, adherence to exercise programme and community reintegration. 2. Usual care: usual care plus 1‐hour in‐hospital individualised education session using the hip fracture recovery manual and 4 educational videos (FReSH Start). Usual care included follow‐up physician and surgeon visits, and usual rehabilitation and home care as appropriate. |
|
| Outcomes | Length of follow‐up: 4 months Mobility (observed): 4‐Metre Walk Test Mobility (self‐reported): use of mobility aid Quality of life (EQ‐5D‐5L) Strength: grip Strength Adverse events: falls (risk and number), re‐admissions (30‐day) Pain |
|
| Notes | Funding: nil Conflict of interest: nil |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Web‐based randomisation service. Stratified randomisation by sex and age group |
| Allocation concealment (selection bias) | Low risk | An independent statistician from an off‐site consulting firm generated the allocation sequence. |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Therapists conducting the intervention and the participants were not blinded to the group assignment. Impact of non‐blinding is unclear |
| Blinding of outcome assessment (detection bias) Observer‐reported outcomes, some judgement | High risk | Participants, the research physiotherapist and study co‐ordinator were aware of treatment allocation. Outcome assessment completed by research physiotherapist |
| Blinding of outcome assessment (detection bias) Observer‐reported outcomes, no judgement | Unclear risk | Participants, the research physiotherapist and study co‐ordinator were aware of treatment allocation. Outcome assessment completed by research physiotherapist. Unclear how this affected objective outcomes |
| Blinding of outcome assessment (detection bias) Participant/proxy‐reported outcomes | High risk | Health‐related quality of life: participants, the research physiotherapist and study co‐ordinator were aware of treatment allocation. Outcome assessment completed by research physiotherapist. Risk of bias for health‐related quality of life = high Falls: ascertained by the same method in both groups, self‐reported by participant. Blinded assessors monitored monthly via telephone. Risk of bias for falls = unclear |
| Incomplete outcome data (attrition bias) Observer‐reported outcomes, some judgement | High risk | 27% of intervention group participants were lost to follow‐up (3 postop complications, 1 residential care admission). No control group participants were lost to follow‐up. The disproportionate loss in intervention and control groups may affect the outcome and it is possible those lost due to complications had different mobility. |
| Incomplete outcome data (attrition bias) Death, re‐admission, re‐operation, surgical complications, return to living at home | High risk | 27% of intervention group participants were lost to follow‐up (3 postop complications, 1 residential care admission). No control group participants were lost to follow‐up. The disproportionate loss in intervention and control groups may affect the outcome and it is possible those lost due to complications would have been more likely to be re‐admitted. |
| Incomplete outcome data (attrition bias) Participant/proxy‐reported outcomes | High risk | 27% of intervention group participants were lost to follow‐up (3 postop complications, 1 residential care admission). No control group participants were lost to follow‐up. Those excluded due to complications more likely to have reduced quality of life and greater risk of falls. |
| Selective reporting (reporting bias) | Low risk | Outcomes not reported in published manuscript were provided by author. |
| Free from baseline imbalance bias? | Low risk | No significant differences at baseline; additional outcomes provided by author. |
| Free from performance bias due to non‐trial interventions? | Unclear risk | Incomplete assurance of comparability of other care provided to the 2 groups. |
| Method of ascertaining falls | Low risk | Monitored falls via prospective self‐reported daily falls diary and monthly telephone calls by a research assistant blinded to group allocation. |
Latham 2014.
| Study characteristics | ||
| Methods | Randomised trial | |
| Participants | Greater Boston, Massachusetts, USA Period of study: September 2008 to October 2012 232 participants enrolled Inclusion: primary diagnosis of hip fracture, > 60 years, discharged from rehabilitation ≤ 20 months of baseline assessment, can understand and communicate in English, able to safely and independently move from sitting to standing ± mobility device, have a functional limitation (defined as a limitation in at least 1 of the tasks listed in the Short Form‐36 physical function scale) Exclusion: significant cognitive deficits (i.e. a Mini Mental State Examination score of < 20), severe depression (i.e. a score of ≥ 10 on the short form of the Geriatric Depression Scale), a terminal illness (survival expected to be < 1 year), significant pulmonary or cardiovascular contraindications or preexisting conditions that precluded participation in an exercise programme, legally blind, currently receiving rehabilitation therapy, lived outside of the study’s catchment area in New England, had a bilateral hip fracture, hip fracture was the result of a malignancy, it had been more than 24 months since the hip fracture at enrolment in the study, or had a rapidly progressive neurological disease. Age: mean 78.0 (SD 9.9) years % male: 31% Number lost to follow‐up: 53 |
|
| Interventions | 6‐month programme 1. Home exercise intervention: exercise intervention 3 times per week for 6 months. Training by physical therapist with monthly telephone calls. Cognitive and behavioural strategies used. Participants given DVD of programme and DVD player if necessary. Programme: simple functional tasks based on Strong for Life programme using Thera‐Bands for resistance. Standing exercises with steps and weighted vests. Based on Increased Velocity Exercise Specific to Task (INVEST), Sherrington and Lord programmes. 2. Attention control: same frequency of contact as intervention group but with registered dieticians. Nutrition education for cardiovascular health based on the Dietary Guidelines for Americans. Single home visit of 1 hour, followed by a series of telephone calls of approximately 30 minutes’ duration, and mailings. |
|
| Outcomes | Length of follow‐up: 6 months (at end of intervention), 9 months (3 months post‐intervention) Mobility (observed): Short Physical Performance Battery Mobility (self‐reported): Activity Measure‐Post Acute Care (AM‐PAC) mobility Function: AM‐PAC daily activity Balance (observed): Berg Balance Scale Strength: knee extension force Other outcomes not included in review: self‐efficacy, modified falls self‐efficacy, outcomes expectations for exercise scale |
|
| Notes | Measured adherence Funding: National Institute of Nursing Research. Thera‐Band products were donated by Thera‐Band. Conflict of Interest: nil |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computerised central randomisation scheme generated by the study biostatistician |
| Allocation concealment (selection bias) | Unclear risk | Inadequate information to support judgement |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Therapists conducting the intervention and participants were not blinded to the group assignment. Impact of non‐blinding is unclear |
| Blinding of outcome assessment (detection bias) Observer‐reported outcomes, some judgement | Low risk | Function assessed by blinded assessors |
| Blinding of outcome assessment (detection bias) Participant/proxy‐reported outcomes | Unclear risk | Blinded assessors |
| Incomplete outcome data (attrition bias) Observer‐reported outcomes, some judgement | Low risk | Losses and reasons balanced between groups. 21.7% loss from intervention group versus 24.1% loss from control group, but reasons balanced and accounted for in multiple ways in analysis |
| Incomplete outcome data (attrition bias) Death, re‐admission, re‐operation, surgical complications, return to living at home | Low risk | Losses and reasons balanced between groups. 21.7% loss from intervention group versus 24.1% loss from control group, but reasons balanced and accounted for in multiple ways in analysis |
| Incomplete outcome data (attrition bias) Participant/proxy‐reported outcomes | Low risk | Losses and reasons balanced between groups. 21.7% loss from intervention group versus 24.1% loss from control group, but reasons balanced and accounted for in multiple ways in analysis |
| Selective reporting (reporting bias) | Low risk | Outcomes reported as per trial registration |
| Free from baseline imbalance bias? | Low risk | Groups balanced at baseline |
| Free from performance bias due to non‐trial interventions? | Low risk | No obvious other differences between groups. |
Lauridsen 2002.
| Study characteristics | ||
| Methods | Randomised trial: use of consecutively‐drawn, numbered, sealed, opaque envelopes | |
| Participants | Rehabilitation Unit, Hvidovre Hospital, Copenhagen, Denmark Period of study: not stated 88 participants Inclusion: women aged 60 to 89 years transferred to a rehabilitation unit within 3 weeks after surgical treatment (osteosynthesis or partial hip replacement) of an "uncomplicated" hip fracture, full mobility prior to fracture, full weight bearing allowed, no concomitant disabling disorders, informed consent Exclusion: women who fell ill during the trial with symptoms that hindered training for more than 2 days; women discharged before attaining the planned functional capacity. (These appear to be post‐randomisation exclusion criteria.) Age: median 80 years (range 61 to 89 years) % male: none Number lost to follow‐up: none (37 dropouts still accounted for in analyses) | |
| Interventions | Early postoperative rehabilitation
1. Participants were offered 6 hours per week of intensive physiotherapy, comprising 2 hours on Monday, Wednesday and Friday
versus
2. Standard physiotherapy of 15 to 30 minutes per weekday Qualitative content of the 2 programmes were identical: bench exercises, gait, balance, co‐ordination, stair climbing and, in some cases, hydrotherapy. Training was stopped when the planned functional capacity was attained unaided (walk 50 or more metres without resting in 2 minutes or less, using walking stick or quadruped if necessary; climb 1 flight of stairs; manage sit‐to‐stand transfer; move in and out of bed; manage bathing, dressing and lavatory visits) or when participants withdrew from study. |
|
| Outcomes | Length of follow‐up: until discharge from hospital Use of walking aids Orthopaedic complication Length of hospital stay Duration of training and length of training period Dropouts from training |
|
| Notes | Details of the method of randomisation provided on contact with lead trialist, but no other information gained. The current account of the trial is based on the report in the Danish Medical Bulletin. A colleague, Pernille Jensen, based in Denmark, checked through the paper written in Danish (in Ugeskr Laeger) and confirmed that, with the exception of a few small details, the English paper was a straight translation. Participants in the intervention arm spent significantly more total hours training and significantly more hours per day training than those in the control arm. Measured adherence Funding: none declared Conflict of interest: none declared |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "Patients were randomised" |
| Allocation concealment (selection bias) | Low risk | Letter from authors to Martyn Parker (06 August 2002): "numbered sealed opaque envelopes drawn consecutively" |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | "A blinded evaluation was performed by an external observer when the treating physiotherapist considered that the objective [attainment of functional capacity] had been obtained." However, this was after a non‐blinded person had assessed achievement of functional goals. |
| Blinding of outcome assessment (detection bias) Observer‐reported outcomes, some judgement | High risk | "A blinded evaluation was performed by an external observer when the treating physiotherapist considered that the objective [attainment of functional capacity] had been obtained." However, this was after a non‐blinded person had assessed achievement of functional goals. |
| Blinding of outcome assessment (detection bias) Observer‐reported outcomes, no judgement | Unclear risk | Blinding not specified. Unclear how assessment of adverse effects is influenced by potential knowledge of group allocation |
| Incomplete outcome data (attrition bias) Observer‐reported outcomes, some judgement | Low risk | Data provided for all participants for intention‐to‐treat analysis as well as per‐protocol analysis |
| Incomplete outcome data (attrition bias) Death, re‐admission, re‐operation, surgical complications, return to living at home | Low risk | Data provided for all participants for intention‐to‐treat analysis as well as per‐protocol analysis |
| Selective reporting (reporting bias) | Unclear risk | Possible but no confirmation |
| Free from baseline imbalance bias? | Low risk | Baseline comparability evident |
| Free from performance bias due to non‐trial interventions? | Unclear risk | Incomplete assurance of comparability of other care provided to the 2 groups |
Magaziner 2019.
| Study characteristics | ||
| Methods | Parallel, 2‐group, randomised clinical trial | |
| Participants | Conducted at 3 clinical centres in the USA: Arcadia University, University of Connecticut Health Center, and University of Maryland, Baltimore Period of study: September 2013 to October 2017 210 participants Inclusion: minimal trauma, closed, non‐pathologic hip fracture with surgical repair; age 60 years and older; community‐dwelling at time of fracture and randomisation; ambulating without human assistance 2 months before the fracture; and walking less than 300 m during the 6‐Minute Walk Test at the time of randomisation Exclusion: medical contraindications for exercise, low potential to benefit from the intervention, and practical impediments to participation Age: mean (SD) 80.75 (8.4) % male: 23 Number lost to follow‐up: 13 | |
| Interventions | For both treatment groups, physical therapists provided 60‐minute in‐home intervention visits on non‐consecutive days for 16 weeks. The first 75 participants = 3 visits per week during the first 8 weeks and 2 visits per week during the remaining 8 weeks (40 assigned visits). Participants randomised after the protocol change = 2 visits per week (32 assigned visits). Participants in both groups received 2000 IU of vitamin D3, 600 mg of calcium and a multivitamin daily for 40 weeks. A registered dietician provided nutritional counselling at baseline. Additional dietician consults were provided by telephone if participants lost 2% or more of weight over 4 weeks. 1. Intervention: strength training using portable progressive resistance device, 3 sets of 8 repetitions at 8 RM or body weight, per leg, for 4 muscle groups (leg press, hip abduction, hip extension and heel raises). Intensity reassessed every 2 weeks. Endurance training (outdoor ambulation, indoor walking or other upright activity), aiming for 20 minutes at 50% of heart rate reserve. 2. Active control: "These activities were selected because they are common physical therapy interventions but were not expected to have an effect on walking ability". Seated active range‐of‐motion exercises (neck, trunk, upper and lower limbs), progressed from 3 to 20 repetitions per exercise, target volume > 20 minutes. Sensory‐level TENS unit application to lower extremity muscle groups, frequency = 80 pulses/second, pulse duration = 50 microseconds, and amplitude to produce a minimally detectable tingling sensation to each muscle complex for 7 minutes. Target volume = 21 minutes per session. |
|
| Outcomes | 16 weeks: 6‐Minute Walk Test Short Physical Performance Battery Balance subscale of Short Physical Performance Battery, and 2 additional single leg stands (eyes open and eyes closed) as used in the National Health and Aging Trends Study (NHATS) Quadriceps Muscle Strength Modified Physical Performance Test Gait speed (fast walking, 50 feet) |
|
| Notes | ClinicalTrials.gov Identifier: NCT01783704 Protocol modified during study: reduced target sample size from 300 to 210, expanded eligibility criteria, removed 1 outcome time point (40 weeks), reduced intervention intensity from 3 days/week to 2 days/week Measured adherence Funding: Dr Beamer reported receiving grants from the NIA/NIH and Veterans Affairs. Dr Binder reported receiving grants from Astellas Pharma and an interview stipend from Pfizer. Dr Miller reported being a full‐time employee of Novartis Institutes for Biomedical Research. Ms McBride reported receiving grants from the University of Maryland School of Medicine. Dr Craik reported receiving grants from the NIH and personal fees from the University of Maryland School of Medicine, as well as serving on the external advisory board of the Pepper Center at the University of Maryland School of Medicine. No other disclosures were reported. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "The random allocation sequence...was implemented using a secure web‐based system. Treatments were assigned according to separate randomization schedules for each clinical site, in randomly ordered blocks of randomly selected sizes of 2, 4, 6, or 8, with equal numbers of participants assigned to each treatment within each block". |
| Allocation concealment (selection bias) | Low risk | Randomisation "implemented using a secure web‐based system" |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Therapists conducting the intervention and participants were not blinded to the group assignment. Impact of non‐blinding is unclear |
| Blinding of outcome assessment (detection bias) Observer‐reported outcomes, some judgement | Unclear risk | Quote: "Assessors who measured outcomes were blinded to treatment group; participants were instructed not to discuss group assignments with assessors". 3 cases of unblinding of assessment staff were reported, all in the training group. |
| Blinding of outcome assessment (detection bias) Observer‐reported outcomes, no judgement | Low risk | Unclear if assessors were blinded for phone calls: quote: "Information on reportable adverse events, including serious or unexpected adverse events or injury that occurred under supervision by study staff, was obtained by telephone interview every 4 weeks". Bias unlikely for mortality |
| Incomplete outcome data (attrition bias) Observer‐reported outcomes, some judgement | Low risk | Less than 20% loss to follow‐up |
| Incomplete outcome data (attrition bias) Death, re‐admission, re‐operation, surgical complications, return to living at home | Unclear risk | Less than 20% loss to follow‐up |
| Selective reporting (reporting bias) | Low risk | Authors specify certain outcomes are not reported in this paper, including cost‐effectiveness, quality of life (Short Form‐36 not reported), and activities of daily living (Pepper Assessment Tool for Disability) |
| Free from baseline imbalance bias? | Low risk | Groups balanced at baseline |
| Free from performance bias due to non‐trial interventions? | Low risk | For both treatment groups, physical therapists provided 60‐minute in‐home intervention visits on non‐consecutive days for 16 weeks. At study initiation, physical therapists were randomly assigned to treatment groups. |
Mangione 2005.
| Study characteristics | ||
| Methods | Randomised trial: use of a list of computer‐generated random numbers | |
| Participants | Community‐dwellers in the vicinity of Arcadia University, USA Period of study: not stated 41 participants Inclusion: people aged 65 years or over living at home after successful hip fracture surgery (partial or total hip replacement or internal fixation) who were willing to go to Arcadia University for assessment, discharged from other physical therapy, informed consent Exclusion: medical contraindications (unstable angina; uncompensated heart failure; on renal dialysis) to resistance or aerobic exercise, stoke with hemiplegia, Parkinson's disease, life expectancy less than 6 months, Mini Mental State Exam score < 20, living in nursing home Age (of 33 completers): mean 79 years (range 64 to 89 years) % male (of 33 completers): 27 Number lost to follow‐up: 8 (1 unable to perform prescribed exercises, 2 withdrew consent, 1 diagnosis of progressive neuromuscular disorder, 4 hospitalisations of whom 2 died) | |
| Interventions | The two intervention groups (1 and 2) received high‐intensity home‐based exercise supervised by a physical therapist in 20 visits over 12 weeks: twice‐weekly for 8 weeks and once‐weekly for 4 weeks. Each session lasted 30 to 40 minutes. 1. Resistance training group did 3 sets of 8 repetitions at 8 RM intensity using a portable resistance exercise machine for hip extensors, hip abductors, knee extensors and plantar flexors versus 2. An aerobic training group did activities that increased the heart rate to 65% to 75% of age‐predicted maximum for 20 continuous minutes (walking, stair climbing or ROM exercises) versus 3. Control group: bi‐weekly mailings on a variety of non‐exercise topics. Participants asked not to begin any new exercise programmes until the study was completed. They were told that they were eligible to receive either of the exercise interventions at the end of the study. | |
| Outcomes | Length of follow‐up: 12 weeks; but only 8 weeks for the control group. 6‐Minute Walk Test distance Maximum voluntary isometric force of the lower extremity Fast gait speed SF‐36 physical function Mortality |
|
| Notes | Measured adherence Funding: Foundation for Physical Therapy Research Grant Conflict of interest: none declared |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "..assignment to a group was determined by referring to a list of computer‐generated random numbers" |
| Allocation concealment (selection bias) | Unclear risk | Unclear if allocation concealed |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Therapists conducting the intervention and participants were not blinded to the group assignment. Impact of non‐blinding is unclear |
| Blinding of outcome assessment (detection bias) Observer‐reported outcomes, some judgement | Low risk | "The physical therapist examiner was masked to group assignment and performed all testing at baseline and after treatment. Different physical therapists provided the interventions and were masked to outcome testing results." There is no indication on whether the participants were told not to inform the assessor of their group allocation. |
| Blinding of outcome assessment (detection bias) Observer‐reported outcomes, no judgement | Low risk | Outcomes are clearly reported and unlikely to be affected by lack of blinding. |
| Blinding of outcome assessment (detection bias) Participant/proxy‐reported outcomes | Unclear risk | "The physical therapist examiner was masked to group assignment and performed all testing at baseline and after treatment. Different physical therapists provided the interventions and were masked to outcome testing results." |
| Incomplete outcome data (attrition bias) Observer‐reported outcomes, some judgement | High risk | Participant flow diagram provided but differential loss to follow‐up (6 from the resistance training group of 8 overall) |
| Incomplete outcome data (attrition bias) Death, re‐admission, re‐operation, surgical complications, return to living at home | Low risk | Participant flow diagram provided |
| Incomplete outcome data (attrition bias) Participant/proxy‐reported outcomes | Unclear risk | Participant flow diagram provided but differential loss to follow‐up (6 from the resistance training group of 8 overall) |
| Selective reporting (reporting bias) | Unclear risk | No protocol available. However, the 2 conference abstracts point to consistency in reporting. |
| Free from baseline imbalance bias? | High risk | Baseline data provided for only 33 of 41 participants. There were some between‐group differences, which may have been clinically significant. In particular, participants in the control group were more depressed and the time from surgery to the start of the study was around 7 weeks more in the 2 exercise groups compared with the control group (19.4 versus 19.7 versus 12.6 weeks). |
| Free from performance bias due to non‐trial interventions? | Unclear risk | Variation in delivery by the 6 physiotherapists may have occurred. |
Mangione 2010.
| Study characteristics | ||
| Methods | Randomised controlled trial | |
| Participants | Community‐dwellers in the Bucks and Montgomery county area (Pennsylvania), USA. Period of study: June 2003 to January 2006 26 participants Inclusion: community‐dwelling before fracture, successful fixation of a hip fracture within previous 6 months, aged ≥ 64 years, physician referral, discharged from physical therapy Exclusion: medical history of unstable angina pectoris or uncompensated congestive heart failure, ongoing chemotherapy or renal dialysis, history of stroke with residual hemiplegia, Parkinson’s disease, absence of sensation in the lower extremities due to sensory neuropathy, life expectancy < 6 months, MMSE < 20, walking speed < 0.3 m/s or > 1.0 m/s. Age: mean 80.7 years (SD 5.95) % male: 19 Number lost to follow‐up at 10 weeks = 5, at 12 months after fracture = 10 |
|
| Interventions | 10‐week programmes delivered by licensed physical therapist. 1. Progressive resistance exercise: leg strengthening exercises, strengthening exercises for the hip extensors and abductors, knee extensors, and ankle plantar flexors bilaterally because of the role of these muscles in gait and transfers. 2x weekly for 20 weeks, total of 20 sessions of 30 to 40 minutes. Intensity: 8 repetition maximum (RM), volume: 3 sets of 8 RM. 2. Control: TENS ("Attentional control group"), at or above the sensory threshold but below the motor threshold, with no visible muscle contraction. Intensity not progressed. Bilateral gluteal muscles (hip extensors and abductors), knee extensors, and ankle plantar flexors were stimulated for 7 minutes for a total of 21 minutes each session. Guided imagery also. |
|
| Outcomes | Length of follow‐up: 10 weeks (end of intervention, used in analysis); study also reported outcomes 26 weeks after randomisation (12 months after fracture) 6‐Minute Walk Test HRQoL: SF‐36 physical function Fast gait speed Strength (lower extremity torque) Modified Physical Performance Score |
|
| Notes | Measured adherence Adverse events not systematically assessed "By having a physical therapist administer the placebo TENS and imagery each treatment session, it was possible to control for attention and motivation...". Funding: National Institutes of Health, National Institute of Child Health and Human Development, National Institute on Aging Grant 1 R03 HD041944‐01A1 Conflict of interest: nil |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Insufficient information for judgement. Quote: "using an unrestricted randomization method" |
| Allocation concealment (selection bias) | Low risk | Quote: "opaque sealed envelopes" |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Participants possibly blinded due to placebo transcutaneous electrical nerve stimulation (TENS). Therapists not blinded; effect of non‐blinding unclear |
| Blinding of outcome assessment (detection bias) Observer‐reported outcomes, some judgement | Low risk | Assessors were blinded to group allocation. |
| Blinding of outcome assessment (detection bias) Observer‐reported outcomes, no judgement | Unclear risk | Method of assessing complications is unclear; however, it does not appear to be blinded. |
| Blinding of outcome assessment (detection bias) Participant/proxy‐reported outcomes | Unclear risk | Assessors were blinded to group allocation. |
| Incomplete outcome data (attrition bias) Observer‐reported outcomes, some judgement | High risk | Less than 20% (19%) lost to follow‐up at 10 weeks; however, 31% lost to follow‐up at 26 weeks |
| Incomplete outcome data (attrition bias) Death, re‐admission, re‐operation, surgical complications, return to living at home | Unclear risk | Method of assessing complications is unclear |
| Incomplete outcome data (attrition bias) Participant/proxy‐reported outcomes | High risk | Less than 20% (19%) lost to follow‐up at 10 weeks; however, 31% lost to follow‐up at 26 weeks |
| Selective reporting (reporting bias) | Unclear risk | No trial registry or protocol paper; outcomes in methods section are reported in the results |
| Free from baseline imbalance bias? | Low risk | Groups comparable at baseline |
| Free from performance bias due to non‐trial interventions? | Low risk | Quote: “Licensed physical therapists conducted treatment sessions for both groups”. TENS used as an active control |
Miller 2006.
| Study characteristics | ||
| Methods | Randomised controlled trial | |
| Participants | Orthopaedic wards of Flinders Medical Centre, Adelaide, Australia Period of study: recruitment September 2000 to October 2002 63 hip fracture patients (out of a total of 75 participants with fall‐related lower limb fracture) Inclusion: age 70 years or over, fall‐related lower limb fracture, resident in Southern Adelaide, malnourished ( < 25thpercentile for mid‐arm circumference for older Australians), written consent by patient or next of kin. Exclusion: unable to understand instructions for positioning of upper arm, could not full weight bear on side of injury > 7 days post admission, not independently mobile pre‐fracture, medically unstable > 7 days post admission, cancer, chronic renal failure, unstable angina, diabetes. Age (of 75): mean 83.5 years % male (of 75): 23 Number lost to follow‐up: 5 (3 dead at 12 weeks and 2 withdrew) | |
| Interventions | Early postoperative rehabilitation. Intervention started from 7 days after fracture.
1. Resistance training supervised by a physiotherapist 3 times per week, 20 to 30 minutes per session, for 12 weeks. To ensure standardisation, the trial physiotherapists were instructed to deliver only the structured programme of therapy to participants. Programme incorporated progressive resistance training of the hip extensors and abductors (supine), knee extensors (supine or sitting) and ankle dorsi‐ and plantar‐flexors (supine or sitting). Training was increased as soon as 2 sets of 8 repetitions of the exercise could be completed in good form, judged by physiotherapist.
versus
2. Resistance training plus nutrition: Fortisip (Nutricia Australia Pty Ltd) oral protein and energy supplement (1.5 kcal/mL, 16% protein, 35% fat, 49% carbohydrate) to provide 45% of estimated energy intakes. (Individually prescribed and delivered.) Four doses of equal volume given by nurses from drug trolley, continued after hospital discharge at twice per day or more. Once weekly visits on weeks 7 to 12.
versus
3. Attention control. Usual care and general nutrition and exercise advice. Tri‐weekly visits on weeks 1 to 6, once weekly on weeks 7 to 12. Discussions during these visits were limited to general information (e.g. benefits of regular exercise and nutrient‐dense meals). All participants were encouraged to continue prescribed treatments. All participants received usual clinical care (including general nutrition and exercise advice, usual dietetic and physiotherapy care, transfer to residential care, rehabilitation facility or directly home). |
|
| Outcomes | Length of follow‐up: 12 weeks (mobility outcomes); 12 months (mortality and re‐admissions) Gait speed Quadriceps strength Quality of life (SF‐12 physical component score and mental component score) Hospital re‐admission Mortality (reported for hip fracture patients at 12 months. Three‐month time point not used as data reported for non‐hip fracture patients) Length of hospital stay (acute, rehabilitation, total) | |
| Notes | Measured adherence Trial population also included 25 other participants (23 with hip fracture) who were allocated to the nutrition‐only intervention group. Data from this group are not included in this review. Of the 14 participants with other lower limb fractures: 6 were pelvic and 8 were of the femur, tibia or fibula. Further information on trial, including mortality data for hip fracture patients, provided to Alison Avenell by Maria Crotty for the nutrition supplementation review (Avenell 2010). Started in acute orthopaedic ward and continued after discharge home. Median length of stay (acute and rehab) = 24 days. Funding: NHMRC Public Health Postgraduate Research Scholarship, Flinders University‐Industry Collaborative Research Grant and Nutricia Australia Pty Ltd. Conflict of interest: none declared |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "Participants were randomized by using a stratified (admission accommodation: community or residential care), block randomization method (blocks of 12) following baseline assessment.” From summary data provided 25 July 2003: "computer generated table of random numbers" |
| Allocation concealment (selection bias) | Low risk | "The Pharmacy department maintained a computer generated allocation sequence in sealed opaque envelopes." |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Care providers and patients not blinded. Impact of non‐blinding unclear |
| Blinding of outcome assessment (detection bias) Observer‐reported outcomes, some judgement | Low risk | "Research staff blinded to treatment allocation performed outcome assessments (weight, quadriceps strength, gait speed, quality of life) 12 weeks after commencement of trial interventions." |
| Blinding of outcome assessment (detection bias) Observer‐reported outcomes, no judgement | Unclear risk | Unclear whether research staff were blinded for these outcomes; however, mortality outcomes not likely to be influenced by knowledge of group allocation, uncertain for adverse events |
| Incomplete outcome data (attrition bias) Observer‐reported outcomes, some judgement | High risk | Denominators for gait analysis, quadriceps strength etc. not provided |
| Incomplete outcome data (attrition bias) Death, re‐admission, re‐operation, surgical complications, return to living at home | Unclear risk | Participant flow diagram provided (for 12 weeks), but inconsistent data provided at 1 year in a summary provided by trialists |
| Selective reporting (reporting bias) | Unclear risk | Protocol not available |
| Free from baseline imbalance bias? | Unclear risk | “No significant differences were identified across the four treatment groups.” However, twice as many cognitively‐impaired participants (17) in attention control group compared with combined intervention group (8); 12 in exercise group. |
| Free from performance bias due to non‐trial interventions? | Unclear risk | No information. More attention control group participants (11) were referred for dietetic intervention, as part of usual care, compared with exercise (6) and nutrition and exercise (5) groups. |
Mitchell 2001.
| Study characteristics | ||
| Methods | Randomised controlled trial | |
| Participants | Geriatric Orthopaedic Unit (Lightburn Hospital) connected with Glasgow Royal Infirmary, UK Period of study: February 1997 to August 1998 80 participants Inclusion: people aged ≥ 65 years with hip fracture treated surgically, written informed consent Exclusion: abbreviated mental score < 6/10, previously unable to walk, medically unstable Age: mean 80 years (range not stated) % male: 16% Number lost to follow‐up: 16 (refused or unavailable); also, 7 died and 13 with new comorbidity precluding assessment were not included in final analyses. | |
| Interventions | Early postoperative rehabilitation 1. Twice weekly quadriceps strengthening exercises in both legs for 6 weeks whilst a hospital inpatient on a rehabilitation ward. Sessions involved 6 sets of 12 repetitions of knee extension (both legs), progressing from 50% of participant's 1 RM (weeks 1 and 2), 70% (weeks 3 and 4) and up to 80% (weeks 5 and 6). Participant’s 1 RM (maximum load an individual can lift through full range of knee extension) established initially and at 3 and 5 weeks. Plus usual care. versus 2. Usual care only. Consisted of conventional physiotherapy for approximately 20 minutes per day, 5 days a week. Initial bed exercises, progressing to bed and chair transfers, gait re‐education and balance training, to practice of functional activities in gym including use of parallel bars. Participants transferred to a rehabilitation unit at about 15 days (median 15 versus 16 days) after surgery for a hip fracture. | |
| Outcomes | Length of follow‐up: 6 weeks and 16 weeks (16 weeks used in analysis) Elderly mobility scale Leg extension power Walking velocity Barthel Index 'Get up and go' test Functional reach Length of hospital stay Mortality |
|
| Notes | Measured adherence Funding: none declared Conflict of interest: nil |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "Randomisation was performed using computer‐generated random numbers" |
| Allocation concealment (selection bias) | Low risk | "[Group] allocation for each study patient concealed in a sealed envelope and held by a third party who was not otherwise involved in the study" |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Therapists conducting the intervention and participants were not blinded to the group assignment. Impact of non‐blinding is unclear |
| Blinding of outcome assessment (detection bias) Observer‐reported outcomes, some judgement | High risk | “Recordings were made by a single research assistant who was not blinded to study group allocation.” While “an independent blinded assessor performed repeat measurements of leg extensor in a convenience sample of 18” participants at 6 weeks plus 2 days gave reassuring results, this was not considered an adequate protection against bias. |
| Blinding of outcome assessment (detection bias) Observer‐reported outcomes, no judgement | Low risk | Blinding unclear; however, mortality outcome is usually unlikely to be influenced by knowledge of group allocation. |
| Incomplete outcome data (attrition bias) Observer‐reported outcomes, some judgement | High risk | Bias could have occurred given the high loss to follow‐up at 16 weeks (intervention: 50% versus control: 40%). |
| Incomplete outcome data (attrition bias) Death, re‐admission, re‐operation, surgical complications, return to living at home | High risk | Bias could have occurred given the high loss to follow‐up at 16 weeks (intervention: 50% versus control: 40%). |
| Selective reporting (reporting bias) | Low risk | Comprehensive report of outcome including consistent primary outcome |
| Free from baseline imbalance bias? | Low risk | In all key characteristics |
| Free from performance bias due to non‐trial interventions? | Low risk | Care other than the trial interventions appears comparable in the 2 groups. |
Monticone 2018.
| Study characteristics | ||
| Methods | Randomised controlled trial | |
| Participants | Scientific Institute of Lissone of the Clinical and Scientific Institutes Maugeri Period of study: July 2012 to December 2015 52 participants Inclusion: internal fixation due to extracapsular hip fractures, such as trochanteric, subtrochanteric, pertrochanteric, intertrochanteric, basal and lateral femoral fractures, 7 to 10 days before admission to rehabilitation unit; good understanding of Italian, age > 70 years Exclusion: previous hip and lower limb surgery, systemic illness, cognitive impairment (Mini Mental State Examination < 24), recent myocardial infarctions, cerebrovascular events, chronic lung or renal diseases Age: mean (SD) 77.45 (7.0) % male: 29 Number lost to follow‐up: 3 weeks = 2, 12 months = 5 | |
| Interventions | 1. Intervention: individual sessions, 90‐minute sessions, 5 times a week for 3 weeks, in‐hospital programme. Balance task‐specific exercises while standing (open and closed eyes, aiming for symmetrical leg loading, proprioceptive pillows under feet, shrinking the support base, or maintaining the tandem position). Walking on a rectilinear trajectory while changing speed and direction, or while performing motor‐cognitive tasks. Additional exercises included moving from a sitting to a standing position, ascending/descending stairs and climbing obstacles. versus 2. Control: individual sessions, 90‐minute sessions, 5 times a week for 3 weeks, in‐hospital programme. Open kinetic chain exercises in the supine position aimed at improving range of hip motion, increasing hip and lower limb muscle strength, and maintaining the length and elasticity of thigh tissues. Both groups: gait training with crutches, ergonomic advice Intervention and control delivered by 1 physiatrist and 2 physiotherapists (i.e. 2 physiatrists and 4 physiotherapists total) |
|
| Outcomes | Assessments after randomisation, 3 weeks (used in analysis) and 12 months Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) (3 subscales: physical function (primary outcome), pain and stiffness). Subscales scored 0 (best) to 100 (worst health status). Italian version Pain intensity: 0 to 10 rating scale Italian Berg Balance Scale Functional Independence Measure Short Form‐36 (subscales reported in paper) Global Perceived Effect Scale at end of treatment |
|
| Notes | Funding: nil Conflict of interest: nil |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "The principal investigator randomized the subjects to one of the two treatment programmes using a list of blinded treatment codes, generated in MATLAB" |
| Allocation concealment (selection bias) | Low risk | "An automatic assignment system made in MATLAB to conceal the allocation" |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Therapists were not blinded. Attempts were made to blind participants. Quote: "The physiatrists, the physiotherapists and the patients were not blinded. To partially limit expectation bias and to reduce problems of crossover, patients were not made aware of the study’s hypothesis and were told that the trial was intended to compare two common approaches to hip fractures postsurgical rehabilitation, whose efficacy had not yet been established". |
| Blinding of outcome assessment (detection bias) Observer‐reported outcomes, some judgement | High risk | Blinding of the secretarial staff collecting data was not specified. Effect of any non‐blinding is unknown; however, baseline assessment was conducted after randomisation, which increases risk of bias. Quote: "The principal investigator obtaining and assessing the data and the biostatistician making the analyses were both blinded to the treatment allocation". However, the paper states it was secretarial staff that collected the data. |
| Blinding of outcome assessment (detection bias) Observer‐reported outcomes, no judgement | Unclear risk | "Using a specific form, the patients were asked to report any serious and/or distressing symptoms they experienced during the study that required further treatment". Blinding of the secretarial staff collecting data was not specified. Effect of apparent non‐blinding on adverse event outcomes is unclear |
| Incomplete outcome data (attrition bias) Observer‐reported outcomes, some judgement | Low risk | Less than 20% of outcome data missing (8% missing, with 2/26 lost to follow‐up in intervention group and 3/26 in control group) |
| Incomplete outcome data (attrition bias) Death, re‐admission, re‐operation, surgical complications, return to living at home | Low risk | Less than 20% of outcome data missing (8% missing, with 2/26 lost to follow‐up in intervention group and 3/26 in control group) |
| Selective reporting (reporting bias) | Low risk | All outcomes in trial registration and methods section are reported |
| Free from baseline imbalance bias? | Low risk | No indication of baseline imbalance bias |
| Free from performance bias due to non‐trial interventions? | Low risk | Intervention and control delivered by equally experienced physiatrists and physiotherapists |
Moseley 2009.
| Study characteristics | ||
| Methods | Randomised controlled trial | |
| Participants | Inpatient rehabilitation units of 3 teaching hospitals, Sydney, Australia Period of study: March 2002 to May 2005 160 participants Inclusion: people with surgical fixation for hip fracture admitted to the inpatient rehabilitation unit from the acute orthopaedic ward. Approval to weight bear or partial weight bear; able to tolerate the exercise programmes; able to take 4‐plus steps with a forearm support frame and the assistance of 1 person; no medical contraindications that would limit ability to exercise; living at home or low‐care residential facility prior to the hip fracture, with the plan to return to this accommodation at discharge. People with cognitive impairment were included if a carer who was able to supervise the exercise programme was available. Exclusion: high‐functioning patients discharged directly to home and low‐functioning patients discharged to a residential aged care facility from the acute orthopaedic ward. Patients with > 4 adjusted errors on the Short Portable Mental Status Questionnaire if no carer was available. Age: mean 84 years (range: not stated) % male: 19 Number lost to follow‐up: 10 (3 withdrew consent; 7 died) | |
| Interventions | Postoperative rehabilitation, started after admission to inpatient rehabilitation unit. Continued at home post discharge.
1. Weight‐bearing exercise twice daily for a total of 60 minutes per day for 16 weeks. Five weight‐bearing exercises were prescribed in addition to walking on a treadmill with partial body weight support using a harness (for inpatients) or a walking programme (after hospital discharge). The 5 weight‐bearing exercises used for both legs included stepping in different directions, standing up and sitting down, tapping the foot and stepping onto and off a block. Hand support could be used if necessary. The exercises were progressed by reducing support from the hands, increasing block height, decreasing chair height and increasing the number of repetitions. This commenced as an inpatient programme, followed by home visits and a structured home exercise programme after inpatient discharge. The home exercise programme incorporated the 5 weight‐bearing exercises used in the inpatient phase, plus a walking programme. The frequency of home visits gradually decreased.
versus
2. Usual care (mainly non‐weight bearing exercise): participants undertook 5 exercises in sitting or lying position plus a small amount of walking using parallel bars or walking aids for a total of 30 minutes each day for 4 weeks. The exercises were progressed by increasing the repetitions and resistance. (This type of exercise programme is commonly prescribed after hip fracture). This commenced as an inpatient programme, followed by weekly home visits and a structured home exercise programme incorporating the same exercises. After 4 weeks, participants were provided with a tailored programme of limited weight‐bearing exercises for 12 weeks and encouraged to continue exercising; no further physiotherapy home visits were undertaken. "All participants received usual post‐operative mobilisation programme usually provided by other health professionals (e.g. occupational therapists) and any gait aids were progressed as per usual protocols. No other physiotherapy treatments were administered during the trial." |
|
| Outcomes | Follow‐up: 16 weeks Walking ability: able to walk unaided or with sticks Gait: walking velocity Strength: knee extension Balance: step test, sway and functional reach, lateral stability, coordinated stability test, choice stepping reaction time Physical Performance and Mobility Examination Sit‐to‐stand time Barthel Index Quality of life: EuroQol‐5D Pain (7‐point ordinal scale) Subjectively‐assessed outcomes (use of 5‐point Likert scales): current mobility, strength and balance Falls Accommodation in the community Use of community services Length of hospital stay Hospital re‐admission Mortality (stated as unrelated to trial protocol) Subjectively‐reported negative effects |
|
| Notes | Measured adherence Funding: National Health and Medical Research Council of Australia Conflict of interest: nil |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "Participants were randomly allocated.... Randomisation was stratified for recruitment site and pre‐fracture Barthel Index (i.e. ≥80/100 or <80/100). The allocation sequence was generated from computer software..." |
| Allocation concealment (selection bias) | Low risk | "The allocation sequence was .... concealed using consecutively numbered, sealed and opaque envelopes." |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Therapists conducting the intervention and participants were not blinded to the group assignment. Impact of non‐blinding is unclear. |
| Blinding of outcome assessment (detection bias) Observer‐reported outcomes, some judgement | Low risk | "Measurements were made by assessors who were blinded to group allocation." |
| Blinding of outcome assessment (detection bias) Observer‐reported outcomes, no judgement | Low risk | The assessment of mortality and re‐admission outcomes are usually unlikely to be influenced by knowledge of group allocation. |
| Blinding of outcome assessment (detection bias) Participant/proxy‐reported outcomes | Unclear risk | Health‐related quality of life: blinded assessors Falls recorded by participants on falls calendar and assessors blinded. Impact of unblinded participant reporting of falls unclear |
| Incomplete outcome data (attrition bias) Observer‐reported outcomes, some judgement | Unclear risk | Participant flow provided and full accounting of loss to follow‐up but differential loss to follow‐up (7 versus 3) could have made some difference |
| Incomplete outcome data (attrition bias) Death, re‐admission, re‐operation, surgical complications, return to living at home | Unclear risk | Participant flow provided but aside from death, these outcomes not reported for whole groups |
| Incomplete outcome data (attrition bias) Participant/proxy‐reported outcomes | Unclear risk | Participant flow provided and full accounting of loss to follow‐up but differential loss to follow‐up (7 versus 3) could have made some difference |
| Selective reporting (reporting bias) | Low risk | Trial registration and consistently well‐reported trial |
| Free from baseline imbalance bias? | Low risk | "There were no clinically important differences between the groups." Also evident from the presented data |
| Free from performance bias due to non‐trial interventions? | Unclear risk | Possible; the trialists speculate that one reason for the general lack of differences between the two groups was that the therapists, who were not blinded to group allocation, may have modified the programme for participants in the control group. |
| Method of ascertaining falls | Unclear risk | Falls were obtained using a falls calendar collected at 4‐week and 16‐week assessments and via a postal survey at 10 weeks. |
Oh 2020.
| Study characteristics | ||
| Methods | Randomised controlled trial | |
| Participants | Department of Rehabilitation Medicine at a university hospital, South Korea
Period of study: September 2017 to April 2019
45 participants
Inclusion: men and women aged 65 to 90 years old who underwent surgery for femoral neck (intertrochanteric or subtrochanteric) fracture and had sarcopenia (diagnosed as low muscle mass combined with low muscle strength (handgrip strength) and/or low physical performance) Exclusion: (i) hip surgery for infection, arthritis, implant loosening, or avascular necrosis; (ii) femoral shaft fracture, acetabular fracture, isolated fracture of the greater or lesser tuberosity, or periprosthetic fracture; (iii) pathologic fracture; (iv) combined multiple fracture; (v) revision surgery; and (vi) severe cognitive dysfunction (obey command ≤ 1 step). Refusal to participate in a clinical trial Age: mean 79 years (range: not stated) % male: 32 Number lost to follow‐up: 7 (2 withdrew consent; 3 lost to follow‐up; 2 died) |
|
| Interventions | Control: standardised rehabilitation treatment, 30 minutes/day each of 10 consecutive working days. Physiotherapist delivered passive hip and knee mobilisation, strengthening of the hip abductor and extensor muscles, transfer and gait training on the floor and stairs during every session. Plus 20 minutes of lower limb exercises in supine position. Intervention: standardised rehabilitation treatment as above, identical to control group. Plus antigravity treadmill (AGT) for 20 minutes/day for each of 10 consecutive working days. Days 1 to 5 AGT was applied with 50% to 60% of body weight administered at a rate of 1.5 miles per hour. Days 6 to 10 AGT was applied with 70% to 80% of body weight administered at a rate of 1.5 to 1.8 miles per hour. |
|
| Outcomes | Baseline, 3 weeks, 3 months, 6 months Koval walking ability score Functional ambulatory category Berg Balance Scale EuroQol‐5D Korean version of the modified Barthel Index Hand grip strength |
|
| Notes | Funding: nil Conflict of interest: nil |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated randomisation lists generated by statistician not involved in the intervention |
| Allocation concealment (selection bias) | Low risk | Sealed, opaque envelopes |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Therapists who provided the rehabilitation programme and the participants were not blinded to group. The effect on bias is unclear. |
| Blinding of outcome assessment (detection bias) Observer‐reported outcomes, some judgement | Low risk | Researchers conducting outcome measurements were blinded to group. |
| Blinding of outcome assessment (detection bias) Observer‐reported outcomes, no judgement | Low risk | Unclear whether researchers ascertaining mortality were blinded. Assessment of mortality outcome is usually unlikely to be influenced by knowledge of group allocation. |
| Blinding of outcome assessment (detection bias) Participant/proxy‐reported outcomes | Unclear risk | Researchers conducting outcome measurements were blinded to group. |
| Incomplete outcome data (attrition bias) Observer‐reported outcomes, some judgement | Unclear risk | 16% loss to follow‐up |
| Incomplete outcome data (attrition bias) Death, re‐admission, re‐operation, surgical complications, return to living at home | Unclear risk | 16% loss to follow‐up |
| Incomplete outcome data (attrition bias) Participant/proxy‐reported outcomes | Unclear risk | 16% loss to follow‐up |
| Selective reporting (reporting bias) | Unclear risk | Trial registered prospectively; however, not translated from Korean for assessment at time of publication. May change to 'low risk' after assessment of trial registration |
| Free from baseline imbalance bias? | Unclear risk | Difference in type of surgery between groups (intervention group had 9 hemiarthroplasty, 9 open reduction and internal fixation (ORIF), 1 total hip joint replacement; control group had 17 hemiarthroplasty, 2 ORIF). Potential effect of this on outcome is unclear |
| Free from performance bias due to non‐trial interventions? | Low risk | Time in training and staff involved were the same in both groups |
Ohoka 2015.
| Study characteristics | ||
| Methods | Randomised controlled trial | |
| Participants | Matterhorn Rehabilitation Hospital, Kure, Japan Period of study: not reported 27 participants Inclusion: proximal femoral fracture, surgical management, 90 years of age or older Exclusion: conservative treatment Age: mean 90.2 years (range: 90 to 93, SD 1.4) % male: 0 Number lost to follow‐up: 14 (7 withdrew, 2 excluded, 5 lost to final follow‐up) |
|
| Interventions | Additional exercise: treadmill training in addition to standard physiotherapy 1. Body weight‐supported treadmill training for 10 minutes, 4 times per week in addition to standard physical therapy 4 times a week versus 2. Usual care. No body weight‐supported treadmill training. Standard physical therapy 6 times a week for 40 minutes a day |
|
| Outcomes | Follow‐up: at discharge (mean (SD) length of stay in intervention group = 84 (8.6) days, control 77.8 (5.5) days. Therefore, used 81 days (12 weeks) for follow‐up. Gait speed: 10m walking time Strength: isometric knee extension Functional Independence Measure Length of stay Adverse events: surgical complications, re‐admission, persistent pain, falls |
|
| Notes | Published as conference abstract only. Author provided additional study details by email correspondence. Funding: none declared Conflict of interest: none declared |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Reported as 'simple randomisation' in correspondence with author |
| Allocation concealment (selection bias) | Low risk | Author correspondence: ‘central randomisation’ |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Therapists conducting the intervention and participants were not blinded to the group assignment. Impact of non‐blinding is unclear |
| Blinding of outcome assessment (detection bias) Observer‐reported outcomes, some judgement | Low risk | Author reported 'single blind test' |
| Blinding of outcome assessment (detection bias) Observer‐reported outcomes, no judgement | Low risk | Author reported 'single blind test'. Unclear whether researchers ascertaining surgical complications and re‐admission were blinded. Assessment of these outcomes is usually unlikely to be influenced by knowledge of group allocation. |
| Blinding of outcome assessment (detection bias) Participant/proxy‐reported outcomes | Unclear risk | Insufficient information for assessment |
| Incomplete outcome data (attrition bias) Observer‐reported outcomes, some judgement | High risk | Large loss to follow‐up (52%) |
| Incomplete outcome data (attrition bias) Death, re‐admission, re‐operation, surgical complications, return to living at home | High risk | Large loss to follow‐up (52%) |
| Incomplete outcome data (attrition bias) Participant/proxy‐reported outcomes | High risk | Large loss to follow‐up (52%) |
| Selective reporting (reporting bias) | Unclear risk | No trial registration or protocol identified |
| Free from baseline imbalance bias? | Unclear risk | Not clearly reported (baseline mobility not available) |
| Free from performance bias due to non‐trial interventions? | High risk | Time spent in training sessions appears to be different between groups |
| Method of ascertaining falls | Unclear risk | Not reported |
Oldmeadow 2006.
| Study characteristics | ||
| Methods | Randomised controlled trial | |
| Participants | Acute trauma ward, the Alfred Hospital, Melbourne, Australia Period of study: March 2004 to December 2004 60 participants Inclusion: people admitted for surgical fixation of a hip fracture (20 had hemiarthroplasty), written informed consent from patient or carer Exclusion: pathological fracture, postoperative orders for non‐weight bearing on operated hip, admission from nursing home, non‐ambulant pre‐morbidity Age: mean 79 years (range 53 to 95 years) % male: 32% Number lost to follow‐up: none. Separate data provided for 10 failed early ambulators but also for whole early ambulation group | |
| Interventions | Early postoperative rehabilitation. Participants received routine, standard postoperative medical and nursing clinical care. All participants were transferred to sit out of bed as early as possible after surgery (range 13 to 120 hours).
1. Early assisted ambulation started within 48 hours (postoperative day 1 or 2).
versus
2. Delayed assisted ambulation until after 48 hours (postoperative day 3 or 4). The same physiotherapy ambulation re‐education programme, implemented for all participants, was implemented once daily over 7 days. Programme included walking re‐education, bed exercise and chest physiotherapy as indicated. The 2 physiotherapists providing treatments received instruction regarding the ambulation protocol to ensure standardisation. |
|
| Outcomes | Length of follow‐up: until discharge (1 week after surgery for functional outcomes) Iowa Level of Assistance Scale (0 = independent; 1 = standby supervision; 2 = minimal assistance; 3 = moderate assistance; 4 = maximal assistance; 5 = failure) for transfers, ambulation and negotiation of 1 step Walking distance, poor functional mobility (assistance required for transfers, negotiating 1 step), time to first walk Discharge location Length of hospital stay Mortality (in hospital) |
|
| Notes | Mean time to surgery was 57 hours (6 to 264 hours)
Trial authors noted that clinical practice was to prescribe bedrest in the presence of cardiovascular challenge. Funding: none declared Conflict of interest: none declared |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "Patients were randomly allocated, using a computer‐generated program, into one of two time to first ambulation intervals..." |
| Allocation concealment (selection bias) | Unclear risk | No mention of methods for safeguarding prior allocation concealment |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Therapists conducting the intervention and participants were not blinded to the group assignment. Impact of non‐blinding is unclear |
| Blinding of outcome assessment (detection bias) Observer‐reported outcomes, some judgement | Low risk | "A blinded assessor carried out the testing." |
| Blinding of outcome assessment (detection bias) Observer‐reported outcomes, no judgement | High risk | No blinding for discharge arrangements (return to living at home), an outcome which is potentially susceptible to bias |
| Incomplete outcome data (attrition bias) Observer‐reported outcomes, some judgement | Unclear risk | Standard deviations not provided and incomplete results for level of assistance scale. While separate data were reported for the 10 failed early ambulators, results were reported for the whole early ambulation group. |
| Incomplete outcome data (attrition bias) Death, re‐admission, re‐operation, surgical complications, return to living at home | High risk | Very short follow‐up with no post‐discharge data |
| Selective reporting (reporting bias) | High risk | Trial registration was retrospective |
| Free from baseline imbalance bias? | Low risk | Baseline comparability evident |
| Free from performance bias due to non‐trial interventions? | Low risk | "The two physiotherapists who provided the treatments received instruction regarding the ambulation protocol to ensure standardisation." |
Orwig 2011.
| Study characteristics | ||
| Methods | Randomised controlled trial | |
| Participants | Community‐dwelling women attending 1 of 3 Baltimore‐area hospitals, USA Period of study: November 1998 through September 2004 180 participants Inclusion: Community‐dwelling women, ≥ 65 years age, screened within 15 days of the fracture, completing at least 80% of the baseline survey, admitted within 72 hours of a non‐pathological hip fracture receiving surgical repair, walking without human assistance prior to the fracture, cognitively intact (i.e. score ≥ 20 on the Folstein Mini Mental State Examination) and received orthopedic surgeon clearance Exclusion: pathologic fracture; cardiovascular, neurologic, and respiratory diseases that could interfere with exercising independently at home; diseases of the bone (e.g. Paget disease, osteomalacia); metastatic cancer; cirrhosis; end‐stage renal disease; hardware in the contralateral hip; and conditions that increase risk of falling while exercising independently Age: mean (SD) 82.4 (7) years % male: 0% Number lost to follow‐up: 49 did not have 12‐month follow‐up |
|
| Interventions | 1. Home exercise. Exercise sessions and a self‐efficacy‐based motivational component. Aerobic exercise using a Stairstep (progressed time and ankle weights), upper and lower limb strengthening programme (progressed with resistance and intensity, aiming for 3 sets of 10 reps), and stretching exercises (20‐ to 30‐minute warm‐up and cool‐down periods). Total of 56 exercise sessions over 12 months, frequency reduced over time, supplemented with telephone calls to remind participants to exercise and address any questions or concerns. Participants were expected to perform aerobic activity at least 3 days/week and strength training 2 days/week for 30 minutes. 2. Usual care. Plus information on bone health and management of osteoporosis. |
|
| Outcomes | Length of follow‐up: 12 months Mortality Discharge to community Adverse events: re‐admission Adverse events: persistent pain Adverse events: falls Adverse events: treatment‐related *Additional outcomes displayed graphically not extracted Adverse events: surgical complication Other outcomes: discharge to nursing home |
|
| Notes | Measured adherence Funding: this research was supported by the National Institute on Aging, Bethesda, Maryland (grants R37 AG09901, R01 AG18668, R01 AG17082, T32 AG00262), and the Claude D. Pepper Older Americans Independence Center (grants P60 AG12583 and P30 AG028747). Conflict of interest: not reported |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote "PC‐PLAN software37 was used to randomize participants within blocks of 2 or 10" |
| Allocation concealment (selection bias) | Unclear risk | Allocation method not reported |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Participants and therapists not blinded to group allocation and the effect of this non‐blinding not clear |
| Blinding of outcome assessment (detection bias) Observer‐reported outcomes, some judgement | Low risk | Study staff conducting assessments were blind to group assignment. Participants obviously not blinded in presence of self‐report outcomes (SF‐36) |
| Blinding of outcome assessment (detection bias) Observer‐reported outcomes, no judgement | Low risk | Study staff conducting assessments were blind to group assignment. Assessment of mortality outcome is usually unlikely to be influenced by knowledge of group allocation. |
| Blinding of outcome assessment (detection bias) Participant/proxy‐reported outcomes | Unclear risk | Falls ascertained by the same method in both groups. Study staff conducting assessments were blind to group assignment. Impact of unblinded participant reporting of falls unclear |
| Incomplete outcome data (attrition bias) Observer‐reported outcomes, some judgement | High risk | 69% and 77% completed all 3 follow‐up visits. |
| Incomplete outcome data (attrition bias) Death, re‐admission, re‐operation, surgical complications, return to living at home | High risk | 69% and 77% completed all 3 follow‐up visits. |
| Incomplete outcome data (attrition bias) Participant/proxy‐reported outcomes | High risk | 69% and 77% completed all 3 follow‐up visits. |
| Selective reporting (reporting bias) | High risk | Self‐efficacy reported as primary outcome but not included in trial report. Secondary outcomes not reported: dietary intake, time to weight bearing (possibly not enough space in publication, time to exercising reported) |
| Free from baseline imbalance bias? | Low risk | Groups balanced at baseline |
| Free from performance bias due to non‐trial interventions? | High risk | Home visits may have had a social effect with these community‐dwelling elderly women; some who had cognitive impairment (Mini Mental State Examination 21 to 25) were included in the trial. |
| Method of ascertaining falls | Unclear risk | Insufficent data available to make judgement. 'Monthly telephone calls were made to participants to ascertain falls'. |
Pol 2019.
| Study characteristics | ||
| Methods | Three‐arm stepped‐wedge cluster‐randomised trial | |
| Participants | Skilled nursing facilities, the Netherlands Period of study: 1 April 2016 to 1 December 2017 240 participants Inclusion: people > 65 years old with traumatic hip fracture admitted to a skilled nursing facility with an indication of short‐term rehabilitation, living alone and having an MMSE score of 15 or higher Exclusion: terminally ill, were waiting for permanent placement in a nursing home, or did not give informed consent Age: mean 84 % of male: 20 Number lost to follow‐up: 89 |
|
| Interventions | 1. Usual care: usual discharge planning, usual physiotherapy (focusing on mobility, muscle strength, balance, transfer and walking), usual occupational therapy (focusing on performance of daily functioning and safety at home) 2. Cognitive behavioural therapy (CBT): usual care, plus 4 weeks of weekly coaching based on CBT, including 5 steps: i) Educate on the importance of physical activity and daily exercise; ii) Ascertain the amount of movement and physical activity during the day and give feedback; iii) Define realistic goals for the performance of daily activities; iv) Agree on an activity plan with the patient and, if needed, practice exercises and activities safely; v) Evaluate progress. 3. CBT plus sensory monitoring: usual care, plus 4 weeks of CBT (above), plus 4 weeks of: ‐ wearing of the physical activity monitor (PAM)‐sensor, sensor monitoring, daily instructions how to wear the PAM ‐ weekly coaching based on CBT, including use of the PAM to: i) Ascertain objectively the amount of movement and number of activities during the day and give feedback; ii) Use as a starting point for discussion about the daily patterns and activities that are important to practice; iii) Make new plans for activities; and iv) Evaluate the progress. |
|
| Outcomes | Timepont used = after the intervention stopped, at approximately 4 months after the start of rehabilitation Canadian Occupational Performance Measure (performance score) Timed Up and Go test Modified Katz ADL score Fall Efficacy Scale International EuroQol 5D Service use: number of sessions/duration/content |
|
| Notes | This intervention was different to others in this review, yet met the inclusion criteria for a mobility strategy. The study authors adjusted for clustering in their analyses. Funding: Dutch grant Fonds Nuts Ohra (1401‐057). MP was supported by the Netherlands Organisation for Scientific Research (NWO) (023.003.059). Conflict of interest: nil |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Generated using STATA software |
| Allocation concealment (selection bias) | High risk | Quote: "After admission to the nursing home, the nursing home physicians will identify potential patients on the basis of the inclusion criteria.” Physicians likely to be aware of allocation of wards as well as participant characteristics, and admission occurred after allocation of wards. Recruitment period 12 months. If participants admitted after allocation of ward, allocation concealment not possible |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Participants and therapists not blinded to group allocation and the effect of this non‐blinding not clear |
| Blinding of outcome assessment (detection bias) Observer‐reported outcomes, some judgement | Low risk | Assessors blinded to intervention group (although authors acknowledge potential for unblinding) |
| Blinding of outcome assessment (detection bias) Participant/proxy‐reported outcomes | Unclear risk | Assessors blinded to intervention group (although authors acknowledge potential for unblinding). |
| Incomplete outcome data (attrition bias) Observer‐reported outcomes, some judgement | High risk | Large loss to follow‐up (37% at 4 months, 46% at 6 months). (Statistical modelling with imputation performed for 6‐month analysis) |
| Incomplete outcome data (attrition bias) Participant/proxy‐reported outcomes | High risk | Large loss to follow‐up (37% at 4 months, 46% at 6 months). (Statistical modelling with imputation performed for 6‐month analysis) |
| Selective reporting (reporting bias) | Unclear risk | Protocol states Canadian Occupational Performance Measure (COPM)‐physical and COPM‐social are both primary outcomes and will be reported combined. The results paper reports COPM‐p as the primary outcome and COPM‐s as the secondary outcome. |
| Free from baseline imbalance bias? | Low risk | No important baseline imbalance |
| Free from performance bias due to non‐trial interventions? | Low risk | No important issues |
| Cluster‐randomised trials | Low risk | Although recruitment did not occur prior to randomisation, baseline characteristics were reported as well‐balanced, adjustment was made for confounders at baseline and for missing values, no clusters were lost, clustering was adjusted for, and the results are comparable with other trials. |
Resnick 2007.
| Study characteristics | ||
| Methods | Randomised trial using computer program. Allocation by independent project co‐ordinator | |
| Participants | Community‐dwellers and independent ambulators (at time of fracture) who had completed Medicare‐funded rehabilitation recruited from 9 hospitals in the greater Baltimore area, USA Period of study: August 2000 to September 2005 (last follow‐up) 155 participants (see Notes) Inclusion: female, aged 65 years or over with a non‐pathological fracture which had occurred within 72 hours of hospital admission, who had surgical repair of their hip fracture. Community‐dwellers and independent walkers before fracture. Free of medical problems that would potentially put them at risk of falls when exercising alone at home alone (e.g. neuromuscular conditions). Score of 20 or higher on the Folstein Mini Mental State Examination. Informed consent. Exclusion: angina, myocardial infarction, stroke, heart condition, pulmonary oedema, Paget's disease, uncontrolled diabetes, Parkinson's disease, multiple sclerosis, cancer, severe blindness, seizures, gastrointestinal haemorrhage (many criteria were limited to the previous 6 months). See trial registration document for full list (clinicaltrials.gov/ct2/show/NCT00389844). Age: mean 81 years % male: 0 (all female) Number lost to follow‐up: 42 (25 withdrew, 10 impractical/other, 7 died) | |
| Interventions | Planned to initiate the intervention as soon as Medicare‐covered rehabilitation services were completed (generally around 1 month); but start dictated by participants. 1. Exercise‐only component. Exercise sessions with an exercise trainer. Sessions incorporated aerobic exercise using a 'Stairstep' (a 4‐inch stair step with handles on either side for support and balance) for 3 days a week, strengthening exercises for main muscle groups relevant to hip fracture recovery for 2 days a week (11 exercises with Thera‐Band and/or ankle wrist cuff weights up to 3 sets of 10 then weight increased), and stretching exercises (these were part of the warm‐up and cool‐down periods). Time and repetitions individually prescribed. (No encouragement given.) versus 2. The full 'Exercise Plus' programme, which includes the above together with the Plus component (motivational interventions: addition of education about the benefits of exercise from the same exercise trainer using a booklet, verbal encouragement through goal setting and positive reinforcement, medications/heat/ice (for pain), cueing with posters describing the exercises, a 'Goal Form' and a calendar of daily exercise activities. versus 3. Routine care In both treatment groups (1 and 2), visits from the trainer were initially twice a week and then decreased to once a month in the final 4 months of the programme, with weekly telephone calls for those exposed to the 'Plus' (motivation) component of the intervention during the weeks when no visit was scheduled. All visits lasted 1 hour. The maximum number of anticipated visits was 38. |
|
| Outcomes | Length of follow‐up: 12 months from injury Mortality | |
| Notes | Extensive account of rationale published in 2002. Trial funded by the National Institute on Aging and National Institutes of Health. 209 were randomised into 4 groups. The 'Plus' or motivation‐only group (54 participants) is not considered in this review (see Crotty 2010). One participant in the exercise‐only group was excluded because they did not receive surgery. Measured adherence Funding: National Institute on Aging grants R37 AG09901, R01‐AG18668, R01 AG17082; Claude D. Pepper Older Americans Independence Center P60‐AG12583; Thera‐Band Academy for contribution of Thera‐Band1 resistive bands. Conflict of interest: none declared |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "Randomization was performed using a freeware computer program. Patient assignment was blocked by hospital to assure equal probabilities within each hospital being assigned to each of the four study groups. Patients were assigned to groups at random with forced balancing of treatment groups within hospital." |
| Allocation concealment (selection bias) | Low risk | "The resulting randomization scheme was given to the project coordinator and patients assigned as they became available at the indicated hospital. The study nurses involved with recruitment and data collection were blind to randomization." |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | "Study participants were not informed of what specific arm of the intervention they were randomized to (i.e. exercise only, plus only, or exercise plus)." Safeguards were not described. Therapists were not blinded to group allocation. |
| Blinding of outcome assessment (detection bias) Observer‐reported outcomes, some judgement | Low risk | "The study nurses involved with recruitment and data collection were blind to randomization". |
| Blinding of outcome assessment (detection bias) Observer‐reported outcomes, no judgement | Low risk | "The study nurses involved with recruitment and data collection were blind to randomization". Assessment of these outcome is usually unlikely to be influenced by knowledge of group allocation. |
| Incomplete outcome data (attrition bias) Observer‐reported outcomes, some judgement | Unclear risk | While participant flow diagram was provided, more participants (10) in the exercise‐only group refused study follow‐up compared with 2 in the usual care group. |
| Incomplete outcome data (attrition bias) Death, re‐admission, re‐operation, surgical complications, return to living at home | Low risk | Participant flow diagram provided. |
| Selective reporting (reporting bias) | Unclear risk | Retrospective trial registration. Insufficient information but no report of overall health status and muscle strength (as stipulated beforehand) |
| Free from baseline imbalance bias? | Low risk | No obvious imbalance (all female) |
| Free from performance bias due to non‐trial interventions? | High risk | Time from fracture to first intervention visit from trainer ranged from 28 to 200 days. Participants indicated when they were willing to have their first visit. |
Salpakoski 2015.
| Study characteristics | ||
| Methods | Randomised controlled trial | |
| Participants | Community‐dwellers, following discharge from Central Finland Central Hospital Period of study: not stated 81 participants randomised Inclusion: age > 60 years; ambulatory and community‐dwelling; operated for femoral neck or pertrochanteric fracture (International Classification of Diseases code S72.0 or S72.1); living in the city of Jyväskylä or in 9 neighbouring municipalities. Exclusion: living in an institution or confined to bed at the time of the fracture; suffering from severe memory problems (Mini Mental State Examination < 18); alcoholism, severe cardiovascular, pulmonary or progressive (i.e. neoplasm) disease, para‐ or tetraplegic or severe depression (Beck Depression Inventory > 29) Age: mean 80, SD 7.09 % male: 22 Number lost to follow‐up: 4 (control: 2 dropouts; intervention: 1 dropout, 1 died) | |
| Interventions | 1. Intervention: 1 year. Promoting mobility after hip fracture (ProMo): standard care and a home‐based, year‐long programme including evaluation/modification of environmental hazards, guidance for safe walking, pain management, progressive home exercise programme and physical activity counselling. Exercise programme = lower‐limb strengthening exercises for the lower limbs (progressed, resistance bands), balance training in standing position, walking exercises and stretching, 30 minutes; strengthening and stretching = 3x/week, balance and walking exercises = 2 to 3x/week. Physical activity counselling = 2 x 30‐minute face‐to‐face sessions and 3 phone contacts, with personal physical activity plan. 2. Control: standard care, included written home exercise programme with 5 to 7 exercises for lower limbs |
|
| Outcomes | Follow‐up: 12 months Short Physical Performance Battery Berg Balance Scale Timed 10 m walk Perceived difficulties in negotiating stairs. “Are you able to negotiate 1 flight of stairs (5 stairs)?” 5‐item response Difficulty walking 500 m Leg extension power (Nottingham Leg Extensor Power Rig) SF‐36 (HRQoL) (email correspondence: outcomes not available at time of writing) Mortality Independent activities of daily living, sum score |
|
| Notes | Measured adherence Funding: nil Conflict of interest: nil |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "A computer‐generated group allocation list was generated by a statistician not involved in the recruitment or data collection. Randomization by sex and by surgical procedure (internal fixation vs arthroplasty) was performed in blocks of 10". |
| Allocation concealment (selection bias) | Low risk | "The study group assignments were enclosed in sealed envelopes" |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Participants and therapists not blind to group allocation but impact of non‐blinding unclear |
| Blinding of outcome assessment (detection bias) Observer‐reported outcomes, some judgement | Low risk | The researchers who collected the outcome measures were blinded to group allocation. |
| Blinding of outcome assessment (detection bias) Observer‐reported outcomes, no judgement | Unclear risk | Unclear how death and complications were recorded |
| Incomplete outcome data (attrition bias) Observer‐reported outcomes, some judgement | Low risk | Less than 20% of outcome data missing |
| Incomplete outcome data (attrition bias) Death, re‐admission, re‐operation, surgical complications, return to living at home | Low risk | Less than 20% of outcome data missing |
| Selective reporting (reporting bias) | Low risk | Reporting of outcomes as primary and secondary differs in protocol paper (Sipila 2011) and main results paper (Salpakoski 2015). In addition, some components of the primary outcome mobility‐related disability noted in protocol paper (difficulty walking outdoors, 500 m and 2 km) were not reported in results paper. Emailed author 15 July 2019 to ask if the outcomes were analysed. Email received with comprehensive results provided. |
| Free from baseline imbalance bias? | Low risk | No imbalance in baseline characteristics |
| Free from performance bias due to non‐trial interventions? | Low risk | No evidence that therapists delivering care to each group were different |
Sherrington 1997.
| Study characteristics | ||
| Methods | Randomised trial: use of random numbers, balanced within blocks of 10 participants, to generate open list | |
| Participants | South Western Sydney, Australia Period of study: December 1994 to December 1995 44 participants Inclusion: people aged 60 years or over with a fall‐related hip fracture who had lived in the community beforehand. Discharged from 1 of 4 acute hospitals to home or residential care within 9 months of their fracture. Contactable and consenting Exclusion: severe cognitive impairment or too ill or immobile to participate as judged by carers Age (of 42): mean 78.5 years (range 64 to 94 years) % male: 21 Number lost to follow‐up: 2 (withdrew consent); also 2 excluded at initial assessment. Also mentions: "One further person in the control group was not able to complete all the physical aspects of the assessment because of pain from a fall, later diagnosed as a further fracture." | |
| Interventions | All participants had a preliminary interview and physical assessment lasting about 1 hour. This took place on average 7 months (5 to 9 months) after their injury.
1. Home‐based, weight‐bearing exercises for 1 month. Individuals in the intervention group were provided with stepping block(s) made of old telephone directories wrapped up with tape and shown the exercises by a physiotherapist. They were advised on how many stepping blocks and repetitions to do at least once daily at the start (these ranged from 5 to 50) and told to increase the repetitions gradually. A photograph was taken to help remind the participant of the correct method and they were checked at 1 week (4 to 16 days). Participants also kept a diary.
versus
2. Control (no specific instructions: usual care) Each telephone directory was 5 cm thick: approximately one‐third of a standard house step. |
|
| Outcomes | Length of follow‐up: 1 month (range 27 to 43 days) Quadriceps strength Sway and balance Functional reach Walking velocity Subjectively‐assessed balance |
|
| Notes | Measured adherence This trial was excluded in the versions of the review up to Issue 3, 2004 because participants were recruited 7 months after a hip fracture; this was previously outside the time period covered by this review, which then focused on early postoperative rehabilitation. Additional information obtained from Cathie Sherrington 09 Febrary 2004 and 24 March 2004 Funding: nil Conflict of interest: nil |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "[Randomly] allocated in order of contact using a random number method within groups of ten subjects." |
| Allocation concealment (selection bias) | High risk | Trial investigator reported that "it was not concealed ‐ just a list of subject numbers and group allocation generated by a random number table; subjects were assigned to subject numbers in the order that contact was made with them." |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Therapists conducting the intervention and participants were not blinded to the group assignment. Impact of non‐blinding is unclear. |
| Blinding of outcome assessment (detection bias) Observer‐reported outcomes, some judgement | High risk | Not blinded |
| Blinding of outcome assessment (detection bias) Observer‐reported outcomes, no judgement | Unclear risk | The few results are unlikely to be affected. |
| Blinding of outcome assessment (detection bias) Participant/proxy‐reported outcomes | High risk | Not blinded |
| Incomplete outcome data (attrition bias) Observer‐reported outcomes, some judgement | Unclear risk | The post‐randomisation exclusion of 2 participants meant that intention‐to‐treat analysis was not done. |
| Incomplete outcome data (attrition bias) Death, re‐admission, re‐operation, surgical complications, return to living at home | Low risk | Few data but complete data provided on contact with trial investigator. |
| Incomplete outcome data (attrition bias) Participant/proxy‐reported outcomes | Unclear risk | The post‐randomisation exclusion of 2 participants meant that intention‐to‐treat analysis was not done. |
| Selective reporting (reporting bias) | Unclear risk | Bias unlikely but protocol not available. |
| Free from baseline imbalance bias? | High risk | Statistically significantly more males in intervention group (8 versus 1). Males generally have poorer prognosis post hip fracture but also may have different baseline strength and attitude to exercises. |
| Free from performance bias due to non‐trial interventions? | Unclear risk | There was a lack of information on care‐programme comparability. |
Sherrington 2003.
| Study characteristics | ||
| Methods | Randomised trial: use of random numbers, balanced within blocks of 6 participants. | |
| Participants | Inpatient rehabilitation wards at Bankstown‐Lidcombe Hospital, Sydney, Australia Period of study: January 1997 to December 1999 80 participants Inclusion: people aged 60 years or over with a fall‐related hip fracture who were admitted to rehabilitation wards after surgery; written consent Exclusion: unable to complete assessment and participate in exercise programme due to a) cognitive impairment (assessed by observation), b) major medical conditions, or c) complications from fracture (if directed to be non‐weight bearing or touch‐weight bearing due to problems with fracture fixation). Age: mean 81 years (range 64 to 98 years) % male: 32 Number lost to follow‐up: 3 (1 withdrew consent; 2 with actual or suspected problems with fracture fixation precluding their further participation) | |
| Interventions | Early postoperative rehabilitation. Baseline assessment at mean 18.3 days from fracture. The programme commenced while the participant was on the rehabilitation ward and was carried out each weekday in the rehabilitation gymnasium. Participants (21) were advised to continue the programme at home if discharged before the final assessment.
1. Two‐week programmes of weight‐bearing (weight‐bearing position with support as required) exercise prescribed by a physiotherapist. Exercises were sit‐to‐stand, lateral step‐up, forward step‐up‐and‐over, forward foot taps, and a stepping grid. Exercises initially conducted with support of a walking frame or adjustable‐height tables. Exercises progressed by increasing the number of repetitions, lessening the hand support, increasing the height of blocks, decreasing height of surface from which the participants was standing up, etc.
versus
2. Non‐weight‐bearing (performed in the supine position) exercise prescribed by a physiotherapist. Exercises were hip abduction, hip flexion, hip/knee flexion/extension, end of range knee extension, ankle dorsiflexion/plantarflexion. Exercises were progressed by increasing the number of repetitions undertaken. For both groups, the treating physiotherapist chose several initial exercises, then added extra exercises in keeping with the participant's capability. Number of repetitions was established on the basis of the participant's initial performance (ranged from 5 to 30 for a single exercise). Participants were encouraged to take prescribed pain relief before exercising. All participants also received usual physiotherapy intervention involving practice of walking and assessment of tasks needed for discharge (bed mobility, sit‐to‐stand and stair climbing), and usual care from other health professionals (nursing staff, social workers, etc). |
|
| Outcomes | Length of follow‐up: 2 weeks Walking ability: use of supports Gait: walking velocity, step length, force plate weight‐bearing Strength: hip abduction and flexion and knee extension Balance: functional reach, step test and sway Functional performance measures Sit‐to‐stand x5 Compliance and assessment of exercises Subjectively‐assessed (use of ordinal scales): risk of falling, balance, pain, sleep quality, health Fracture fixation problems Length of hospital stay |
|
| Notes | This trial, previously listed in Ongoing studies under Sherrington 2002, was performed as part of Cathie Sherrington's PhD work. Additional information provided 15 January 2004 by Cathie Sherrington included further details of method of randomisation and data for self‐assessed outcomes. Funding: National Health and Medical Research Council; Health Research Foundation Sydney South West; Arthritis Foundation of Australia. Conflict of interest: none declared |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "Patients were randomised into one of two exercise groups using a random number table and randomisation in blocks of six." |
| Allocation concealment (selection bias) | Low risk | "Subjects were assigned into groups using a concealed randomisation method". Clarification of method by personal communication: "This method involved a list of group allocation by subject number on which group allocation for each subject was concealed by a separate piece of opaque paper. Once the subject had agreed to participate in the trial, one piece of paper was removed to reveal the group allocation for the subject in question without revealing the allocation for subsequent subjects." |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Therapists conducting the intervention and participants were not blinded to the group assignment. Impact of non‐blinding is unclear. |
| Blinding of outcome assessment (detection bias) Observer‐reported outcomes, some judgement | High risk | Assessor was not blinded to group allocation. |
| Blinding of outcome assessment (detection bias) Observer‐reported outcomes, no judgement | Unclear risk | Unlikely to be affected by the lack of blinding |
| Incomplete outcome data (attrition bias) Observer‐reported outcomes, some judgement | Unclear risk | Intention‐to‐treat analysis was done and a participant flow diagram provided. However, the denominators for various outcomes were quite varied. |
| Incomplete outcome data (attrition bias) Death, re‐admission, re‐operation, surgical complications, return to living at home | Unclear risk | Very short follow‐up. |
| Selective reporting (reporting bias) | Unclear risk | Bias unlikely but protocol not available |
| Free from baseline imbalance bias? | Low risk | Baseline comparability evident |
| Free from performance bias due to non‐trial interventions? | Low risk | Care other than interventions under test comparable in both groups |
Sherrington 2004.
| Study characteristics | ||
| Methods | Randomised trial: use of random numbers, balanced within blocks of 6 participants. Use of sealed opaque numbered envelopes | |
| Participants | Community‐dwellers and residents of aged‐care facilities discharged from 6 hospitals in Sydney, Australia Period of study: April 1998 to June 2000 120 participants Inclusion: people who had completed usual care after a fall‐related hip fracture; consent Exclusion: unable to complete assessment and participate in exercise programme due to a) severe cognitive impairment, b) medical conditions, or c) complications from fracture resulting in delayed healing and associated weight‐bearing restrictions. Age: mean 79 years (range 57 to 95 years) % male: 20 Number lost to follow‐up: 12 (7 withdrew consent ‐ refused assessment; 5 died) | |
| Interventions | All participants had a preliminary assessment which took place, on average, 22 weeks after their injury.
1. Home‐based, weight‐bearing exercises (weight‐bearing position with support as required). Exercises were sit‐to‐stand, lateral step‐up, forward step‐up‐and‐over, forward foot taps, and a stepping grid. Exercises initially conducted with tables, chairs or walking aids used for support. Exercises progressed by increasing the number of repetitions, lessening the hand support, increasing the height of blocks, decreasing height of surface from which the participant was standing up, etc.
versus
2. Home‐based, non‐weight‐bearing exercises (performed in the supine position) prescribed by a physiotherapist. Exercises were hip abduction, hip flexion, hip/knee flexion/extension, end of range knee extension, ankle dorsiflexion/plantarflexion. Exercises were progressed by increasing the number of repetitions undertaken.
versus
3. Control (no specific instructions) For both exercise groups, the prescribing physiotherapist chose several initial exercises and number of repetitions in keeping with the participant's capability. Individuals in the weight‐bearing group were provided with stepping block(s). Participants were advised on progression. Line drawings of the exercises were provided and they were checked at 1 week. Further assessment and prescription at 1 and 4 months. Participants also asked to keep a record of their exercises. Exercises were prescribed for 4 months minimum. Advice for exercises etc. given to each participant as deemed appropriate by the physiotherapist conducting final assessment at 4 months. |
|
| Outcomes | Length of follow‐up: 4 months Walking ability/mobility Gait: walking velocity, step length Strength: hip abduction and flexion and knee extension Balance: step test, sway and functional reach Functional performance measures: timed sit‐to‐stand, supine‐to‐sit and Physical Performance and Mobility Examination Mortality Subjectively‐assessed: risk of falling, balance, pain, sleep quality, health Compliance and assessment of exercises (intervention groups only) Falls |
|
| Notes | Trial was performed as part of Cathie Sherrington's PhD work Additional information, including binary data for mobility and subjective outcomes, received 09 February 2004. Funding: Health Research Foundation Sydney South West, Arthritis Foundation of Australia, and National Health and Medical Research Council Partnership in Injury Grant. Conflict of interest: nil |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "The randomization schedule was produced with a random number table, with subjects being randomized to groups in blocks of 6." |
| Allocation concealment (selection bias) | Low risk | "..subjects were allocated to groups using assignments sealed in opaque envelopes." Clarification of method by personal communication: "Group allocation enclosed in sealed opaque envelopes which were numbered by subject number which was allocated when the consent form was signed." |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Therapists conducting the intervention and participants were not blinded to the group assignment. Impact of non‐blinding is unclear |
| Blinding of outcome assessment (detection bias) Observer‐reported outcomes, some judgement | High risk | Assessors were not blinded. However, there was training with the aim of standardisation between the 3 testers. |
| Blinding of outcome assessment (detection bias) Observer‐reported outcomes, no judgement | Unclear risk | Not blinded. Unlikely to be affected by the lack of blinding. |
| Blinding of outcome assessment (detection bias) Participant/proxy‐reported outcomes | High risk | Assessors were not blinded |
| Incomplete outcome data (attrition bias) Observer‐reported outcomes, some judgement | Low risk | Intention‐to‐treat analysis was done and a participant flow diagram provided. Though percentages were presented in the trial report, full data were provided by contact with the lead trialist. |
| Incomplete outcome data (attrition bias) Death, re‐admission, re‐operation, surgical complications, return to living at home | Low risk | Intention‐to‐treat analysis was done and a participant flow diagram provided |
| Incomplete outcome data (attrition bias) Participant/proxy‐reported outcomes | Low risk | Intention‐to‐treat analysis was done and a participant flow diagram provided. Though percentages were presented in the trial report, full data were provided by contact with the lead trialist. |
| Selective reporting (reporting bias) | Unclear risk | Bias unlikely but protocol not available. |
| Free from baseline imbalance bias? | Low risk | Visual inspection of the table of baseline characteristics was consistent with the claim in the report of there being no clinically important or statistically significant differences between the 3 study groups at the initial assessment. |
| Free from performance bias due to non‐trial interventions? | Low risk | A systematic approach was taken. |
Sherrington 2020.
| Study characteristics | ||
| Methods | Randomised controlled trial, New South Wales (NSW), Australia | |
| Participants | Community‐dwellers recruited after discharge from 11 hospitals and from community advertising in NSW, Australia Period of study: April 2010 to December 2015. 336 participants (194 with hip fracture, 31 with pelvic fracture, 111 with other fracture) Inclusion: community‐dwellers aged 60+ years within 2 years of lower‐limb or pelvic fracture Exclusion: resided in a high‐care residential facility (nursing home); cognitive impairment (a Folstein Mini Mental State Examination score of < 24); had insufficient English language to understand study procedures; unable to walk more than ten metres despite assistance from a walking aid and/or another person; medical condition precluding exercise; currently receiving a treatment programme from a rehabilitation facility. Age: mean 77.7 (8.7) % male: 24 Number lost to follow‐up: 52 | |
| Interventions | 1. Intervention: individualised physiotherapist‐prescribed home programme of weight‐bearing balance and strength exercises, fall prevention advice based on Stepping On programme. 10 home visits (more frequent in first 3 months) and 5 phone calls to implement, review and progress programme. Exercise programme prescribed for 20 to 30 minutes, 3x/week. 2. Control: usual care |
|
| Outcomes | 12 months Short Physical Performance Battery (score, plus individual components analysed: gait speed, balance, sit to stand x5) Balance (sum of feet together, semi tandem and tandem stance times) Falls Acute Measure for Post Acute Care Pain Mortality Quality of life |
|
| Notes | Inclusion criteria for study was recent lower‐limb or pelvic fracture. Only data from 194 participants with hip fracture were included in this review. Total n in study = 336. Funding: Australian National Health and Medical Research Council Conflict of interest: Lord: Physiological Profile Assessment instrument is commercially available in Australia; Australian National Health and Medical Research Council funding for salary |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Randomization order was determined using a computer generated random number schedule with randomly permuted block sizes of 2–6". |
| Allocation concealment (selection bias) | Low risk | Quote: "Allocation was concealed by using central randomization performed by an investigator not involved in assessments or recruitment and the treatment allocation tables were inaccessible to recruitment staff". |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Therapists conducting the intervention and participants were not blinded to the group assignment. Impact of non‐blinding is unclear |
| Blinding of outcome assessment (detection bias) Observer‐reported outcomes, some judgement | Low risk | Quote: "Study staff who conducted interviews and assessments, received calendars and questionnaires, made phone calls and entered data were unaware of group allocation". "Participants were instructed not to inform the assessors of their intervention status, and all exercise equipment was removed prior to the final assessment". |
| Blinding of outcome assessment (detection bias) Observer‐reported outcomes, no judgement | Low risk | Quote: "Study staff who conducted interviews and assessments, received calendars and questionnaires, made phone calls and entered data were unaware of group allocation". |
| Blinding of outcome assessment (detection bias) Participant/proxy‐reported outcomes | Unclear risk | Health‐realated quality of life: blinded assessors. Falls ascertained by the same method in both groups. Participants reporting falls were not blind to group. Blinded assessors recorded and confirmed falls with participants. Impact of unblinded participant reporting of falls unclear |
| Incomplete outcome data (attrition bias) Observer‐reported outcomes, some judgement | Low risk | Less than 20% of data lost to follow‐up |
| Incomplete outcome data (attrition bias) Death, re‐admission, re‐operation, surgical complications, return to living at home | Low risk | Less than 20% of data lost to follow‐up |
| Incomplete outcome data (attrition bias) Participant/proxy‐reported outcomes | Low risk | Less than 20% of data lost to follow‐up |
| Selective reporting (reporting bias) | Low risk | Outcomes in trial registry either reported or draft paper states they will be reported in subsequent paper (EuroQol‐5D, Short Form‐12) |
| Free from baseline imbalance bias? | Low risk | No notable difference between groups. |
| Free from performance bias due to non‐trial interventions? | High risk | Pragmatic trial, yet social contact in intervention arm likely to confound any effect |
| Method of ascertaining falls | Low risk | Monthly falls calendar. Participants who did not return calendars or who reported a fall were telephoned by blinded research assistants |
Stasi 2019.
| Study characteristics | ||
| Methods | Randomised controlled trial. Stratified by gender and age | |
| Participants | Inpatient orthopaedic ward of KAT General Hospital of Attica, Athens, Greece (for 1 week), then participants' homes Period of study: recruitment April 2012 to May 2016 100 participants Inclusion: diagnosis of displaced femoral neck fracture (Garden's classification III or ΙV), aged between 70 and 84 years, with community‐dwelling status before hip fracture, not having undergone previous orthopaedic surgery on the fractured or the contralateral hip, body mass index between 19 and 35 kg/m2, able to walk outdoors for 2 neighbourhood blocks before fracture Exclusion: nil Age: mean (SD) 77.5 (4.2) % male: 25 Number lost to follow‐up: 4 | |
| Interventions | 1. Intervention: Weeks 1 to 3, intervention the same in both groups. From week 4, addition of intensive exercise programme to control programme, emphasising hip abductor strengthening of affected limb. Hip abductor strength training in standing and side‐lying positions, resistance progressed with cuff weights and loop elastic bands, 2 sets of 10 reps, progressing to 3 sets of 15 reps. Home sessions initially 40 minutes, increasing to approx. 55 minutes. 2. Control: 'Standard Physiotherapy', a 12‐week standard physiotherapy programme, initiated on the 2nd postoperative day, continuing for 1 week in hospital and 11 weeks at home. Physiotherapist delivered individualised programme daily in hospital and 3x/week at home, with participants instructed to do programme independently on other days. Programme included progressive functional movements, range of motion, gait training, strengthening (progressing to loop elastic bands). Home sessions initially 30 minutes, increasing to maximum of 45 minutes. Difference between groups: intervention group had approx. 10 minutes extra per physio session. Isotonic hip abductor strengthening commenced week 4 (intervention group), 6 (control group). Resistance added earlier in intervention group. At end of 12‐week intervention, both groups encouraged to continue exercise programme 3x/week for 3 months. |
|
| Outcomes | 12 weeks and 24 weeks. Hip abductor strength, dynamometer Timed Up and Go test Lower Extremity Functional Scale‐Greek version Falls Use of walking aid |
|
| Notes | Trial registered ISRCTN30713542 The study states results are reported as mean (SD). During analysis, we noted the study was an outlier for all outcomes. If we assumed standard error was reported instead of standard deviation, then converted standard error to standard deviation, the results were consistent with other studies. We used the converted data in the review’s analyses. In this study the difference in intervention between groups occurs at home. Funding: nil Conflict of interest: nil |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Randomization..was performed by an independent clinician according to the randomization list". "Sex and age were used as stratification factors in the randomization process. The sex ratio was 3/1 (3 females to 1 male). The age ratio was 1/1/1 (three age sub‐groups), equally spaced using block size 4. The study’s randomization list was formed on the basis of these principles." |
| Allocation concealment (selection bias) | Unclear risk | Not specified |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | No mention of blinding of therapists and participants; impact of this on results is unclear |
| Blinding of outcome assessment (detection bias) Observer‐reported outcomes, some judgement | Low risk | Quote: "All assessments were carried out by the same examiner, who was not involved in any way with the rehabilitation program and was blinded with respect to the group assignment". |
| Blinding of outcome assessment (detection bias) Observer‐reported outcomes, no judgement | Low risk | Unlikely to be affected by bias |
| Incomplete outcome data (attrition bias) Observer‐reported outcomes, some judgement | Low risk | Less than 20% of data lost to follow‐up |
| Incomplete outcome data (attrition bias) Death, re‐admission, re‐operation, surgical complications, return to living at home | Low risk | Less than 20% of data lost to follow‐up |
| Selective reporting (reporting bias) | Low risk | All outcome measures listed in trial registration are reported |
| Free from baseline imbalance bias? | Low risk | Appears balanced for reported outcomes. Note baseline values not presented for physical measures |
| Free from performance bias due to non‐trial interventions? | Low risk | Both groups received physiotherapy intervention 3x/week at home |
Suwanpasu 2014.
| Study characteristics | ||
| Methods | Randomised controlled trial | |
| Participants | King Chulalongkorn Memorial Hospital, Bangkok, Thailand Period of study: January 2012 to February 2013 46 participants Inclusion: 60 to 93 years of age, diagnosed with femoral neck fracture, intertrochanteric fracture or subtrochanteric fracture Exclusion: nil Age: mean (SD) 75.2 (8.4) % male: 34 Number lost to follow‐up: | |
| Interventions | 1. Intervention: physical activity‐enhancing programme, based on Resnick's self‐efficacy model (Resnick 2009). Four phases of physical training and efficacy‐based intervention, covering 5 sessions. Phases: assessment, preparation, practicing and evaluation. Face‐to‐face contact and 5 telephone calls during 7 weeks post‐surgery. 2. Control: standard care (physical activity for hip fracture booklet) |
|
| Outcomes | 6 weeks after discharge International Physical Activity Questionnaire |
|
| Notes | Contributed no outcomes to this review Funding: Thai Red Cross Society and King Chulalongkorn Memorial Hospital Conflict of interest: nil |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "We used a simple block randomization technique with a coin flip to assign subjects" |
| Allocation concealment (selection bias) | Unclear risk | Allocation concealment not specified |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Therapists conducting the intervention and participants were not blinded to the group assignment. Impact of non‐blinding is unclear |
| Blinding of outcome assessment (detection bias) Observer‐reported outcomes, some judgement | High risk | Blinding not specified; outcome was self‐reported |
| Incomplete outcome data (attrition bias) Observer‐reported outcomes, some judgement | Low risk | Less than 20% of data missing |
| Selective reporting (reporting bias) | Unclear risk | No protocol or trial registry. Only 1 outcome reported in methods and results |
| Free from baseline imbalance bias? | Unclear risk | Trend toward intervention group being older and having greater physical activity at baseline (between group difference, P = 0.06 for both). Few functional or health characteristics at baseline reported (mental test and physical activity only) |
| Free from performance bias due to non‐trial interventions? | High risk | Social contact in intervention arm likely to confound any effect. An appropriate comparator would have been social home visits but no physical intervention. |
Sylliaas 2011.
| Study characteristics | ||
| Methods | Randomised controlled trial | |
| Participants | Outpatient clinic, recruited from Ullevål University Hospital or Diakonhjemmet Hospital in Oslo, Norway. Period of study: June 2007 and June 2009 150 participants Inclusion: femoral neck fracture or a trochanteric fracture; 12 weeks after the operation: (i) age 65 years or older; (ii) living at home; (iii) able to undergo physical therapy for the hip fracture; and (iv) scoring 23 or more (out of 30) on the Mini Mental State Examination Age: mean (SD) 82.4 (5.7) % male: 17 Number lost to follow‐up: 12 |
|
| Interventions | 1. Intervention: 3 to 6 months after fracture: physiotherapist‐led programme, exercise class 2x/week and home programme at least once/week. 45‐ to 60‐minute exercise session, 15‐minute warm‐up on cycle or treadmill; 4 exercises (standing knee flexion, lunge, sitting knee extension and leg extension, with 3 sets of 15 reps at 70% of 1 RM, increasing to 8 to 10 reps at 80% of 1 RM at 3 weeks. Encouraged to walk approx. 30 minutes/day. 2. Control: participants were asked to maintain their current lifestyle. No restrictions were placed on their exercise activities. |
|
| Outcomes | 12 weeks: 6‐Minute Walk Test Berg Balance Scale Sit to stand x10 Timed Up and Go test Gait speed Maximum step height Nottingham Extended Activities of Daily Living scale Short Form‐12 mental and physical domains |
|
| Notes | Funding: Eastern Regional Health Authority Conflict of interest: nil |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote "patients were assigned randomly by a computer‐generated list" |
| Allocation concealment (selection bias) | Low risk | Quote "using lots in sealed opaque envelopes" |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Therapists conducting the intervention and participants were not blinded to the group assignment. Impact of non‐blinding is unclear |
| Blinding of outcome assessment (detection bias) Observer‐reported outcomes, some judgement | Low risk | Assessor blinded to group allocation |
| Blinding of outcome assessment (detection bias) Participant/proxy‐reported outcomes | Unclear risk | Assessor blinded to group allocation |
| Incomplete outcome data (attrition bias) Observer‐reported outcomes, some judgement | Low risk | Adequate follow‐up and ITT analysis. Less than 20% of data missing |
| Incomplete outcome data (attrition bias) Death, re‐admission, re‐operation, surgical complications, return to living at home | Low risk | Adequate follow‐up and ITT analysis. Less than 20% of data missing |
| Incomplete outcome data (attrition bias) Participant/proxy‐reported outcomes | Low risk | Adequate follow‐up and ITT analysis. Less than 20% of data missing |
| Selective reporting (reporting bias) | Unclear risk | No trial protocol identified |
| Free from baseline imbalance bias? | Low risk | Groups balanced at baseline |
| Free from performance bias due to non‐trial interventions? | High risk | Social contact in intervention arm likely to confound any effect. An appropriate comparator would have been social home visits but no physical intervention. |
Sylliaas 2012.
| Study characteristics | ||
| Methods | Randomised controlled trial | |
| Participants | Recruited from Ullevål University Hospital or Diakonhjemmet Hospital in Oslo, Norway. Period of study: unclear 95 participants Inclusion: in the intervention arm in previous trial (Sylliaas 2011; 12‐week intervention from 12 to 24 weeks post fracture); age at least 65 years; living at home; assessed as able to undergo physical therapy for the hip fracture by the responsible orthopaedic surgeon; scoring 23 or more (out of 30) on the Mini Mental State Examination. Exclusion: admitted from nursing homes, metastatic cancer or had sustained the hip fracture as part of a multi‐trauma, in an institution 3 months after the fracture, absent from 3‐month follow‐up for Sylliaas 2011 study. Age: mean (SD) 82.3 (5.8) % male: 19 Number lost to follow‐up: 5 |
|
| Interventions | 1. Intervention: 6 to 9 months after fracture: physiotherapist led programme, exercise class 1x/week and home programme at least once/week. Exercise class: 15‐minute warm‐up on cycle or treadmill. 45‐ to 60‐minute exercise session; 4 exercises (standing knee flexion, lunge, sitting knee extension and leg extension, with 3 sets of 10 reps at 80% of 1 RM, progressed every 3 weeks. Home programme: standing knee flexion and lunge exercises, resistance added via weight belts. Walk approx. 30 minutes/day. 2. Control: participants were asked to maintain their current lifestyle. No restrictions were placed on their exercise activities. |
|
| Outcomes | 12 weeks: Timed Up and Go test Berg Balance Scale Sit to stand x10 Gait speed 6‐min walk test Nottingham Extended Activities of Daily Living scale SF‐12 mental and physical domains Maximum step height |
|
| Notes | All participants were recruited from those who completed a preceding 3‐month progressive strength‐training programme twice a week, in the intervention arm of Sylliaas 2011. Due to the resulting unit of analysis issues, we did not include data from this study in the meta‐analysis. Funding: Eastern Regional Health Authority funded the study Conflict of interest: nil |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "a new randomisation of the participants in the intervention arm was carried out". Assume this was the same method of randomisation as used in preceding trial (Sylliaas 2011), where "patients were assigned randomly by a computer‐generated list" |
| Allocation concealment (selection bias) | Low risk | Assume this was the same method of randomisation as used in preceding trial (Sylliaas 2011), "using lots in sealed opaque envelopes" |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Therapists conducting the intervention and participants were not blinded to the group assignment. Impact of non‐blinding is unclear |
| Blinding of outcome assessment (detection bias) Observer‐reported outcomes, some judgement | Low risk | Assessor blinded to group allocation |
| Incomplete outcome data (attrition bias) Observer‐reported outcomes, some judgement | Low risk | Adequate follow‐up and ITT analysis |
| Selective reporting (reporting bias) | Unclear risk | No trial protocol identified |
| Free from baseline imbalance bias? | Low risk | Groups balanced at baseline |
| Free from performance bias due to non‐trial interventions? | High risk | Social contact in intervention arm likely to confound any effect. An appropriate comparator would have been social home visits but no physical intervention. |
Taraldsen 2019.
| Study characteristics | ||
| Methods | Randomised controlled trial | |
| Participants | Hospital in central Norway Period of study: February 2011 to March 2014 143 participants Inclusion: community‐dwelling in Trondheim municipality prior to the fracture, 70 years or older, diagnosed and operated for intracapsular or extracapsular hip fractures and identified by experienced physiotherapists by use of hospital admission lists. Exclusion: pathological fracture, less than 3 months' life expectancy, inability to walk 10 m (with or without walking aids) before the fracture, or participating in conflicting research project; at 4 months, participants were also excluded after a medical examination if they had contraindications for training (unstable medical conditions) or were bedridden Age: mean (SD) 83.4 (6.1) % of male: 31 Number lost to follow‐up: 20 |
|
| Interventions | Additional home‐based exercise programme delivered 4 months following hip fracture in additional to usual rehabilitation and health care services 1. Received 2 exercise sessions a week for 10 weeks from physiotherapists at home. The programme targeted balance and gait and consisted of 5 individually‐tailored, weight‐bearing exercises, all entailing change in base of support: walking, stepping in a grid pattern, stepping up on a box, sit‐to‐stand, and lunge. Each exercise was described at 5 levels with increasing challenge. 2. Usual care |
|
| Outcomes | End of intervention = 2 months. Outcomes also at 8 months. Short Physical Performance Battery Gait speed Barthel Index Nottingham Extended Independent ADL EuroQol 5D‐3L Need for walking aid / assistance Number of people who fell Cost‐effectiveness |
|
| Notes | Funding: Norwegian Women’s Health Association and the Norwegian Extra Foundation for Health and Rehabilitation through the EXTRA funds, the Norwegian Fund for Postgraduate Training in Physiotherapy, and the Liaison Committee between the Central Norway Regional Health Authority (RHA), Trondheim Municipality, and the Norwegian University of Science and Technology (NTNU). Conflict of interest: nil |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "The randomization was performed using a web‐based computerized randomization service... A stratified block randomization technique was used to ensure balanced group concerning intra‐capsular versus extra‐capsular fractures and pre‐fracture use of walking aid (rollator indoor or not)." |
| Allocation concealment (selection bias) | Low risk | Randomisation performed off‐site using a web‐based computerised randomisation service |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Therapists conducting the intervention and participants were not blinded to the group assignment. Impact of non‐blinding is unclear |
| Blinding of outcome assessment (detection bias) Observer‐reported outcomes, some judgement | Low risk | "Assessors and personnel performing statistical analyses were blinded to participants’ group allocation." Participants were instructed not to provide information that could reveal group allocation to the researchers and assessors, and this information was repeated prior to each assessment. |
| Blinding of outcome assessment (detection bias) Observer‐reported outcomes, no judgement | Unclear risk | Method of ascertainment of death unclear |
| Blinding of outcome assessment (detection bias) Participant/proxy‐reported outcomes | Unclear risk | Health‐related quality of life: blinded assessors Falls reported in retrospect by participants and staff who were aware of group allocation; therefore, high risk of bias for falls |
| Incomplete outcome data (attrition bias) Observer‐reported outcomes, some judgement | Low risk | Less than 20% of data lost to follow‐up |
| Incomplete outcome data (attrition bias) Death, re‐admission, re‐operation, surgical complications, return to living at home | Low risk | Less than 20% of data lost to follow‐up |
| Incomplete outcome data (attrition bias) Participant/proxy‐reported outcomes | Low risk | Less than 20% of data lost to follow‐up |
| Selective reporting (reporting bias) | Unclear risk | TUG and strength are in protocol but were not measured on frailer participants "due to burden on the participants." Therefore, these measures were not reported in the results. This seems an adequate explanation and the majority of prespecified outcomes were measured. |
| Free from baseline imbalance bias? | Unclear risk | Intervention group more likely to live alone; mobility measures were balanced |
| Free from performance bias due to non‐trial interventions? | High risk | No control for social interaction effect, with 2x weekly physio visits in home and a high proportion of participants living alone |
| Method of ascertaining falls | Unclear risk | Number of new falls during the 12‐month follow‐up period was registered based on retrospective report |
Tsauo 2005.
| Study characteristics | ||
| Methods | Randomised: method not specified | |
| Participants | People recently discharged from an acute orthopaedic unit, National Taiwan University Hospital, Taiwan Period of study: October 2000 to September 2001 54 participants Inclusion: people recently discharged from hospital after surgery for a hip fracture; agreement to participate from participant and surgeon; written informed consent Exclusion: individual or family rejected further treatment or follow‐up; did not have transport or were not in hospital neighbourhood; were unable to co‐operate due to cognitive problems; or had ongoing medical litigation Age (of 25 completers): mean 73 years (range not given) % male (of 25 completers): 20 Number lost to follow‐up: 29 (25 lost and 4 excluded due to low compliance) | |
| Interventions | Commenced after hospital discharge (mean 11 days)
1. Home‐based individualised physical therapy programme delivered in 8 visits over 3 months and involving strengthening exercises, range‐of‐motion exercises, balance training, functional training (such as sit‐to‐stand, ambulation and stair‐climbing training), practice of transfer techniques, adjustment of walking aids and adaptation and modification of the home environment. 5 exercises were taught at each visit, initially in 3 sets of 10 repetitions a day for each item, progressed at the visits.
versus
2. Practice of an exercise programme given at the bedside before discharge All participants had bedside physiotherapy during their hospital stay. |
|
| Outcomes | Length of follow‐up: 6 months Strength Harris Hip Score Walking speed Quality of life: assessed 4 domains of the WHOQOL‐BREF (physical health, psychosocial, social relationship, environment) Adverse events: wound infection |
|
| Notes | Article notes that most people in Taiwan do not receive physiotherapy after they leave hospital because there is no insurance payout for such services. Funding: supported by the National Science Council (grant nos. NSC‐89‐2320‐B‐002‐051‐ M5, NSC‐90‐2320‐B‐002‐012‐M56). Conflict of interest: none |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "Patients were randomized". The method of randomisation was not described. |
| Allocation concealment (selection bias) | Unclear risk | "Patients were randomized". No methods for concealing allocation were described. |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Therapists conducting the intervention and participants were not blinded to the group assignment. Impact of non‐blinding is unclear |
| Blinding of outcome assessment (detection bias) Observer‐reported outcomes, some judgement | High risk | No blinding was reported. |
| Blinding of outcome assessment (detection bias) Observer‐reported outcomes, no judgement | Unclear risk | No blinding was reported; unknown risk of bias. |
| Blinding of outcome assessment (detection bias) Participant/proxy‐reported outcomes | High risk | No blinding was reported. |
| Incomplete outcome data (attrition bias) Observer‐reported outcomes, some judgement | High risk | Baseline 3‐month and 6‐month follow‐up data were only available for 25 of the 54 trial participants and an intention‐to‐treat analysis was not carried out. 4 poor compliers with the intervention were excluded. |
| Incomplete outcome data (attrition bias) Death, re‐admission, re‐operation, surgical complications, return to living at home | High risk | Baseline 3‐month and 6‐month follow‐up data were only available for 25 of the 54 trial participants and an intention‐to‐treat analysis was not carried out. 4 poor compliers with the intervention were excluded. |
| Incomplete outcome data (attrition bias) Participant/proxy‐reported outcomes | High risk | Baseline 3‐month and 6‐month follow‐up data were only available for 25 of the 54 trial participants and an intention‐to‐treat analysis was not carried out. 4 poor compliers with the intervention were excluded. |
| Selective reporting (reporting bias) | Unclear risk | The outcomes recorded appeared to be reported. |
| Free from baseline imbalance bias? | Unclear risk | Baseline data were only available for 25 of the 54 trial participants. For these 25 participants, only diabetes differed significantly between the 2 groups. The authors reported that the number and characteristics of the 25 participants (4 others were excluded for low compliance) lost to follow‐up were similar between the two groups. |
| Free from performance bias due to non‐trial interventions? | Low risk | There appeared to be care programme comparability before discharge and identical follow‐up assessment procedures. |
Van Ooijen 2016.
| Study characteristics | ||
| Methods | Randomised controlled trial | |
| Participants | A ‘residential and rehabilitation center’ in Zorggroep Solis in Deventer, the Netherlands. This is where most people recovering from a hip fracture are referred to when they need additional temporary care before returning to their homes. Period of study: January 2012 and December 2015. 70 participants Number lost to follow‐up: 36 Inclusion: admission to Zorggroep Solis with a hip fracture related to falling, ≥ 65 years of age, Functional Ambulation Category score 2 or higher, expected duration of admission at Zorggroep Solis ≥ 6 weeks, ability to understand and execute simple instructions Exclusion: not allowed to bear weight on the affected leg; moderate or severe cognitive impairments as indicated with a score below 18 on the MMSE; severe non‐corrected visual impairments limiting the correct perception of the direct environment; contraindication to physical activity; activity tolerance below 40 minutes with rest intervals Age: mean (SD) 83.4 (6.7) years % male: 14 Number lost to follow‐up: at 3 months = 19, at 6 months = 36 |
|
| Interventions | Three‐arm trial. Interventions delivered by physical therapist. 1 therapist to 2 participants, with the participants taking turns to train. Provided verbal instructions or occasional physical assistance when necessary. 1. Control: usual physiotherapy = conventional physical therapy, including exercises of leg strength in sitting or standing, balance (e.g. stance), transfers (e.g. bed to chair, chair to toilet, chair to chair, sit to stand and vice versa), overground walking (e.g. parallel bars, inside, outside, obstacles) and activities of daily living. These training sessions followed locally‐implemented guidelines regarding the treatment of hip fractures and aimed to facilitate the participant’s return to home.
2. Conventional treadmill. 15 sessions = conventional physiotherapy, 15 sessions = treadmill (TM) walking. TM walking used no body‐weight support other than the handrail. Walking at a speed that was reported as comfortable. Focus was initially on the quality and safety aspects of walking and gradually shifted towards walking faster and longer.
3. Adaptability treadmill: 15 sessions = conventional physiotherapy, 15 sessions = adaptability treadmill (TM) training. TM walking used no body‐weight support other than the handrail. Walking at a speed that was reported as comfortable. Focus on practicing walking adjustments in response to the visual context projected on the C‐Mill, e.g. visually‐guided stepping to targets, obstacle avoidance, speed variation. Walking adaptability games consisting of interactive stepping targets and obstacles.
|
|
| Outcomes | Immediately after 6‐week intervention, 4 weeks after intervention finished (10 weeks after randomisation), 52 weeks after intervention period (58 weeks after randomisation). 10 weeks after randomisation used in this analysis. Elderly Mobility Scale Performance Oriented Mobility Assessment Timed Up and Go test (inadequate data to be included in analysis) Walking speed Falls Nottingham Extended Activities of Daily Living Index Hip Disability and Osteoarthritis Score ‐ Quality of Life Mortality |
|
| Notes | Measured adherence Funding: none noted Conflict of interest: MR and PJB are inventors of rehabilitation treadmills that include visual context for foot placement. Vrije Universiteit Amsterdam granted this idea exclusively to ForceLink (Culemborg, the Netherlands, now part of Motekforce Link, Amsterdam, the Netherlands), an industrial partner of Vrije Universiteit Amsterdam. ForceLink is manufacturer of the C‐Mill and assignee of a patent for rehabilitation treadmills with visual context for foot placement, with MR and PJB listed as inventors. Vrije Universiteit Amsterdam received patent revenues, and transferred part of these revenues to spend them freely for their research endeavours. Vrije Universiteit Amsterdam used these revenues to finance a research project on the effectiveness of C‐Mill training. The present study is part of that research project. MR and PJB did not receive reimbursements, fees, funding or salary from ForceLink, nor do they benefit personally from patent revenues. ForceLink had no influence on the interpretation of the results, the final conclusions and their publication. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated block randomisation |
| Allocation concealment (selection bias) | Low risk | Quote: "Allocation concealment by opaque sequentially numbered envelopes" |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Subjects and therapists not blinded; effect of non‐blinding is unclear |
| Blinding of outcome assessment (detection bias) Observer‐reported outcomes, some judgement | Low risk | Assessors blinded |
| Blinding of outcome assessment (detection bias) Observer‐reported outcomes, no judgement | Low risk | Only relevant outcome death. Objective outcome and assessors blinded: risk of bias considered low |
| Blinding of outcome assessment (detection bias) Participant/proxy‐reported outcomes | Unclear risk | Health‐related quality of life: assessors blinded Falls ascertained by the same method in both groups. Participants reporting falls were not blind to group. Blinded assessors recorded and confirmed falls with participants. Unclear impact of lack of participant blinding |
| Incomplete outcome data (attrition bias) Observer‐reported outcomes, some judgement | High risk | > 20% loss to follow‐up |
| Incomplete outcome data (attrition bias) Death, re‐admission, re‐operation, surgical complications, return to living at home | High risk | Large loss to follow‐up, although ITT analysis conducted for deaths |
| Incomplete outcome data (attrition bias) Participant/proxy‐reported outcomes | High risk | 35% had no falls follow‐up. |
| Selective reporting (reporting bias) | Low risk | Outcomes reported as per trial registration and published protocol |
| Free from baseline imbalance bias? | Low risk | Groups comparable at baseline |
| Free from performance bias due to non‐trial interventions? | Low risk | Groups use similarly qualified therapists and contract hours for delivery of intervention |
| Method of ascertaining falls | Low risk | Monthly falls calendar. Participants who did not return calendars or provided incomplete information were telephoned by blinded assessors. |
Williams 2016.
| Study characteristics | ||
| Methods | Randomised controlled trial. Stratified by hospital and gender | |
| Participants | 3 main acute hospitals of Betsi Cadwaladr University Health Board (BCUHB) in North Wales (Wrexham Maelor, Ysbyty Glan Clwyd and Ysbyty Gwynedd) Period of study: June 2014 to June 2016 61 participants randomised (62 recruited) Inclusion: age 65 years or older; recent proximal hip fracture; surgical repair by replacement arthroplasty or internal fixation; living in their own home prior to hip fracture; capacity to give informed consent, as assessed by the clinical team in the acute hospital; people with postoperative delirium were approached if this was resolved prior to discharge from the acute hospital; living and receiving rehabilitation from the National Health Service in the area covered by BCUHB Exclusion: living in residential or nursing homes prior to hip fracture; not able to understand Welsh or English Age: mean (SD) 79.4 (7.6); range 66 to 99 % male: 25 Number lost to follow‐up: 13/62 | |
| Interventions | 1. Intervention: usual care plus enhanced rehabilitation package, including 6 additional home‐based physiotherapy sessions delivered by a physiotherapist or technical instructor, novel information workbook and goal‐setting diary 2. Control: usual care |
|
| Outcomes | 3 months: Walking speed Barthel Activities of Daily Living Nottingham Extended Activities of Daily Living scale Eight‐foot Get Up and Go test Sit to Stand Pain EuroQol‐5D Mortality |
|
| Notes | Measured adherence ‐ "Stratification by hospital was necessary as each hospital has differing usual care pathways and, due to the geography of the area, different therapy teams delivered the intervention in different areas". ‐ Timed Up and Go test and gait speed were only measured in people with unaided gait. Therefore they had very poor follow‐up (n = 24 of the 60 randomised, compared with n = 59 for primary outcome, the Barthel Index). ‐ The 3‐month follow‐up of TUG and gait speed were performed on average 3 weeks later in the control group than in the intervention group. Funding: National Institute for Health Research’s Health Technology Assessment Programme Conflict of interest: CS reports being a member of the NIHR HSDR board. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "The randomisation was performed by dynamic allocation to ensure that good balance in the allocation ratio of 1: 1 was maintained, both within each stratification variable and across the trial. Participants were stratified by (1) hospital and (2) gender". |
| Allocation concealment (selection bias) | Low risk | "Randomisation was achieved by secure web access to the remote randomisation centre at the North Wales Organisation for Randomised Trials in Health (NWORTH) at Bangor University. This system was set up, maintained and monitored independently of the trial statistician and other trial staff". |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Participants and intervention staff not blind to group allocation. Effect of non‐blinding unclear |
| Blinding of outcome assessment (detection bias) Observer‐reported outcomes, some judgement | Low risk | Blinded assessors |
| Blinding of outcome assessment (detection bias) Observer‐reported outcomes, no judgement | Unclear risk | Adverse events were reported to researchers; however, blinding is not clear. Method of detecting death is unclear. |
| Incomplete outcome data (attrition bias) Observer‐reported outcomes, some judgement | High risk | More than 20% did not complete 3‐month follow‐up for physical function tests. |
| Incomplete outcome data (attrition bias) Death, re‐admission, re‐operation, surgical complications, return to living at home | Unclear risk | 20% withdrawals or loss to follow‐up; proportion followed up for death unclear |
| Incomplete outcome data (attrition bias) Participant/proxy‐reported outcomes | High risk | More than 20% did not complete 3‐month follow‐up for pain outcome. |
| Selective reporting (reporting bias) | Low risk | All outcomes in trial registration are reported in results section |
| Free from baseline imbalance bias? | Unclear risk | "The proportions in the two groups were similar according to gender, living status, type of property, type of fracture, type of surgery and admitting hospital. The mean age of the intervention group was 2.9 years older than the control group. After the hospital admission, there was a small discrepancy between those discharged directly to their place of usual residence (34% in the intervention group; 53% in the control group), and those sent to a community hospital for rehabilitation (52% in the intervention group; 22% in the control group). The baseline scores of the outcome measures and physical function tests were similar between the 2 groups (table 3). However, the Nottingham Extended Activities of Daily Living score was 2.4 points higher in the control group". |
| Free from performance bias due to non‐trial interventions? | Unclear risk | Pragmatic, usual care varied as per protocol |
ADL: activities of daily living; AGT: antigravity treadmill; CBT: cognitive behavioural therapy; EQ‐5D(‐3L): EuroQol Quality of Life Questionnaire Five‐Dimensional Classification (3 levels); ES: electrical stimulation; HRQoL: health‐related quality of life; ITT: intention to treat; IU: international units; MMSE: Mini Mental State Examination; N·m/kg: newton‐metre/kilogram; PAM: physical activity monitor; RM: repetition maximum; ROM: range of motion; SD: standard deviation; SF‐12/SF‐36: 12‐Item/36‐Item Short Form Health Survey; TENS: transcutaneous electrical nerve stimulation; TUG: Timed Up and Go test; VAS: visual analogue scale; WHOQOL‐BREF: World Health Organization abbreviated Quality of Life scale
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Adunsky 2011 | Intervention not solely aimed at mobilisation |
| Aftab 2020 | The intervention group received multifactorial multidisciplinary rehabilitation program |
| Beckman 2021 | Pseudo‐randomised |
| Berggren 2019 | Intervention not solely aimed at mobilisation |
| Corna 2021 | Intervention was conventional rehabilitation plus individualised, progressive aerobic exercise training with an arm crank ergometer for 30 minutes/day, 5 days/week for 3 weeks. Aerobic training was conducted on a commercial motorised arm crank ergometer. The difference between the intervention and control groups is not a mobilisation strategy. |
| Dallimore 2015 | Proportion of participants receiving intervention after a hip fracture is unknown |
| Invernizzi 2019 | Both groups undertook exercise. Difference between groups was amino acids |
| Kalron 2018 | Hip fracture and total hip joint replacement. Outcomes not reported for hip fracture only |
| Karlsson 2016 | Intervention included multiple components delivered by a multidisciplinary team |
| Kim 2020 | Outcomes focused on strength and muscle activity; did not measure mobility |
| Lahtinen 2017 | Compared interventions containing multiple components and compared two models of care |
| Laiz 2017 | Primarily a vitamin D trial. Intervention participants also received instruction on exercises and a leaflet. This trial was excluded as the intervention did not target mobility. Compliance for vitamin D recorded but no mention of exercise compliance. The outcomes were limited to survival and complications (with no mobility focus). |
| Lehrl 2012 | Participants underwent total hip arthroplasty; proportion with hip fracture unknown. Intervention was a video game with cognitive tasks, aiming to improve mental activation |
| Pfeiffer 2020 | The intervention primarily focused on reducing falls and fear of falling; the intervention was largely cognitive and employed behavioural strategies that did not meet the intervention criteria for this review. |
| Scheffers‐Barnhoorn 2019 | Both the intervention and control groups received multidisciplinary geriatric rehabilitation including regular exercise training, with the between‐group difference in intervention being a cognitive‐behavioural strategy rather than a mobility‐training strategy. |
| Taraldsen 2015 | Intervention was a care programme, rather than a mobility strategy |
| Wang 2020 | The intervention was a model of care, with medical and therapy involvement, rather than a mobility strategy. |
| Wu 2010 | Participants had acetabular not hip (proximal femur) fractures |
Characteristics of studies awaiting classification [ordered by study ID]
Che 2020.
| Methods | Randomised controlled trial |
| Participants | 78 people with old femoral neck fractures who underwent surgery in hospital between 2 September 2017 and 25 August 2019 |
| Interventions | The control group underwent routine rehabilitation training, and the observation group performed early rehabilitation training. |
| Outcomes | Harris Hip Score, length of stay, pain, complications |
| Notes | A conference abstract has been published. We have emailed authors to request further details on the time post fracture, intervention, outcome measures and results. |
Wu XY 2019.
| Methods | Randomised controlled trial |
| Participants | 100 people undergoing cementless total hip arthroplasty for femoral neck fractures at Department of Orthopedics, Tianjin Hospital from March 2016 to April 2017 |
| Interventions | "The trial group received early weight‐bearing exercise with the concept of enhanced recovery after surgery, and control group was given weight‐bearing exercise at 3 weeks with the traditional rehabilitation concept." |
| Outcomes | Visual analogue scale score, hip range of motion, Harris Hip Score, Short Form‐36, postoperative complications |
| Notes | Awaiting translation to English |
Characteristics of ongoing studies [ordered by study ID]
ACTRN12617001345370.
| Study name | Recumbent bike riding for people with fractured neck of femur: a feasibility trial |
| Methods | Randomised controlled trial. Blinded outcomes assessor and investigators |
| Participants | People aged 18 years or above. Have had surgical correction of a fractured neck of femur. Be unable to walk 15 m with assistance at enrolment (within 4 days of surgery). Aim: 60 participants |
| Interventions | 1. Routine care plus bike training 2. Routine care |
| Outcomes | Trial feasibility; participant recruitment and retention, completion of outcome measures, documentation of any trial protocol deviations or variations, and feedback from trial staff about any issues encountered in the delivery of the protocol. Intervention feasibility Intervention safety Trial feasibility Modified Iowa Level of Assistance Scale Discharge destination Gait speed Acute length of stay Quality of life Subacute length of stay |
| Starting date | Study start date: November 2017 |
| Contact information | A/Prof Catherine Said Physiotherapy Department Austin Health Studley Rd Heidelberg, 3084 Victoria Australia +61 3 9496 3697 cathy.said@austin.org.au |
| Notes |
ACTRN12618000903280.
| Study name | The feasibility of prescribing a walking program to improve physical functioning of people living in the community after hip fracture: a phase II randomised controlled trial |
| Methods | Randomised controlled trial; blinded outcomes assessor |
| Participants | Aged 60 years or above; community‐dwelling and receiving services from the Community Rehabilitation Program at Eastern Health; had a hip fracture (S72.0–S72.2 according to the International Classification of Diseases 10th revision, ICD‐10) which was managed surgically; are able to walk independently with or without a gait aid; can communicate with conversational English. Aim: 42 participants |
| Interventions | 1. Intervention: usual care plus prescription of total 100 minutes of walking per week, of at least moderate intensity (at level 3 determined by the Rate of Perceived Exertion Scale from 0 to 10), in bouts of at least 10 minutes, for 12 weeks 2. Control: usual care without any additional prescription of physical activity |
| Outcomes | Follow‐up: 12 weeks post‐intervention Primary outcome: feasibility Secondary outcomes
|
| Starting date | Study start date: July 2018 Estimated completion date: NR |
| Contact information | Prof Nicholas Taylor Eastern Health ‐ La Trobe University +61 3 9091 8874 n.taylor@latrobe.edu.au |
| Notes |
Heiberg 2017.
| Study name | Recovery of physical functioning, activity level, and quality of life after hip fracture in the fragile elderly |
| Methods | Randomised controlled trial; blinded outcome assessors |
| Participants | People with an acute low‐energy hip fracture (intracapsular, trochanteric or subtrochanteric) and treated surgically, ≥ 65 years of age, living in their own homes prior to the fracture, and able to give informed consent. Aim: 160 participants |
| Interventions | 1. Functional training group 2. Usual care |
| Outcomes | Follow‐up: 12 months after surgery Primary outcome measure: change in the performance‐based Short Physical Performance Battery Secondary outcome measures
|
| Starting date | Study start date: May 2016 Estimated completion date: December 2018 |
| Contact information | Kristi E Heiberg, PhD 004790980258 kristi.elisabeth.heiberg@vestreviken.no Arnljot Tveit, PhD arnljot.tveit@vestreviken.no |
| Notes |
ISRCTN32476360.
| Study name | Effects of transcutaneous electrical nerve stimulation on acute postoperative pain intensity, ambulation and mobility after hip fracture: a double‐blinded, randomised trial |
| Methods | Randomised trial. Double‐blinded |
| Participants | People aged over 50 years of age, with stable extracapsular proximal hip fraction (intertrochanteric or subtrochanteric); partial or full weight bearing instructions; ability to ambulate independently for at least 10 m with or without an assistive device prior to the fracture; ability to follow instructions; Mini Mental State Examination test score = 20 Aim: 80 participants |
| Interventions | 1. Active transcutaneous electrical nerve stimulation (TENS) with a biphasic symmetric waveform at a continuous frequency of 100 Hz and phase duration of 200 µseconds 2. Sham TENS |
| Outcomes | Follow‐up: 5 days Pain level at rest, at night and during ambulation Ambulation status measures Physical performance tests |
| Starting date | Start date: December 2014 Estimated completion date: December 2015 |
| Contact information | Michal Elboim Balfour 9 Nahariya 224216 Israel |
| Notes |
jRCTs052190018.
| Study name | A pilot study of training using the Balance Exercise Assist Robot for the patients after the proximal femoral fractures surgery at the convalescent rehabilitation ward |
| Methods | Randomised controlled trial; open‐label |
| Participants | People aged 65 years to 95 years; more than one week after surgery; able to stand for more than 90 seconds; able to walk more than 10 m with supervision; able to stand still on the Balance Exercise Assist Robot; height: 140 cm to 190 cm; weight: 35 kg to 100 kg Aim: 30 participants |
| Interventions | 1. Conventional therapy (100 minutes per day) plus robotic training group using the balance exercise assist robot (80 minutes per day) for 21 days 2. Conventional therapy (100 minutes per day) plus conventional balance training (80 minutes per day) for 21 days |
| Outcomes | Follow‐up: not reported Primary outcome: Functional Reach Test Secondary outcomes
|
| Starting date | Study start date: April 2019 |
| Contact information | Mikihiro Fujioka Kyoto Takeda Hospital 11, Nishishichijo, Minamikinutacho, Shimogyo‐ku +81‐75‐321‐7001 Kyoto, Japan |
| Notes |
jRCTs052190022.
| Study name | A preliminary study of training using the Balance Exercise Assist Robot for the patients after the proximal femoral fractures surgery at the community‐based integrated care ward |
| Methods | Randomised controlled trial; open‐label |
| Participants | Aged 65 years to 90 years; one week after surgery; able to walk more than 10 m with supervision; able to stand still on the Balance Exercise Assist Robot; height: 140 cm to 190 cm, weight: 35 kg to 100 kg |
| Interventions | 1. Conventional therapy (80 minutes per day) plus robotic training group using the balance exercise assist robot (40 minutes per day) for 13 days 2. Conventional therapy (80 minutes per day) plus conventional balance training (40 minutes per day) for 13 days |
| Outcomes | Primary Outcome: Functional Reach Test Secondary outcomes
|
| Starting date | Study start date: April 2019 Estimated completion date: not reported |
| Contact information | Seiji Tokugawa Ayabe City Hospital +81‐773‐43‐0123 ortho.toku@zeus.eonet.ne.jp Tomoyoshi Obata Ayabe City Hospital obata.t@ayabe‐hsp.or.jp |
| Notes |
KCT0004122.
| Study name | A randomised feasibility study of inpatient rehabilitation using advanced techniques in older people with fragility hip fracture |
| Methods | Randomised controlled trial; blinded outcomes assessor |
| Participants | Aged 65 or above; diagnosed with femoral neck, intertrochanteric fracture; hip operative methods include bipolar artificial joint replacement, total hip arthroplasty, open reduction Aim: 20 participants |
| Interventions | 1. Intervention: comprehensive rehabilitation using advanced rehabilitation equipment comprised of 30‐minute weightless treadmill walking exercise, strength and balance exercise with pneumatic or non‐pneumatic exercise equipment; twice a day for total 60 minutes per day 2. Control: 30‐minute aerobic exercise using general treadmill; twice a day for total 60 minutes per day Treatment duration for both groups: 2 weeks |
| Outcomes | Follow‐up: 3 months post‐surgery Primary outcome: efficacy using Koval Secondary outcomes
|
| Starting date | Study start date: July 2019 Estimated completion date: Apri 2021 |
| Contact information | Bo Ryun Kim Jeju National University Hospital +82‐64‐717‐2711 |
| Notes |
Lima 2016.
| Study name | Effectiveness of a physical exercise intervention program in improving functional mobility in older adults after hip fracture in later stage rehabilitation: a randomized clinical trial |
| Methods | Randomised controlled trial; blinded outcome assessor |
| Participants | After the first hip fragility fracture following a fall from standing height or while turning; surgically treated in the later stage of rehabilitation phase (6 months up to 2 years after the fracture). Aim: 82 participants |
| Interventions | 1. Home‐based physical exercise 2. Usual care |
| Outcomes | Follow‐up: 12 months Primary outcome measure: lower extremity function (Short Physical Performance Battery) Secondary outcome measures
|
| Starting date | Study start date: November 2014 Estimated completion date: December 2019 |
| Contact information | Monica R Perracini, PhD monica.perracini@unicid.edu.br Camila A Lima camilabrown@hotmail.com |
| Notes |
NCT01129219.
| Study name | Observation and progressive strength training after hip fracture |
| Methods | Randomised trial in 2:1 ratio at 12 weeks after fracture. Blinded outcomes assessor |
| Participants | Hip fracture patients. Enrolled 150 participants |
| Interventions | Started at 12 weeks post‐fracture. Participants randomised in a 2:1 manner to: 1. Intervention: progressive strength training, for 12 weeks. After 12 weeks, randomisation to further intervention or not. 2. Control. |
| Outcomes | Follow‐up: 24 weeks Primary outcome: Berg Balance Scale Secondary outcome: strength via Sit to Stand test |
| Starting date | Start date: June 2007 Estimated completion date: December 2010 |
| Contact information | Mette Martinsen Oslo University Hospital Oslo Norway |
| Notes |
NCT01174589.
| Study name | Training of patients with hip fracture |
| Methods | Randomised trial. Blinded outcomes assessor |
| Participants | Aged 60 years or over; hip fracture patients who are full weight bearing on the affected leg; living in own home with an independent walking ability; within 2 weeks after discharge from hospital Aim: 120 participants |
| Interventions | 1. 12 weeks of physical training consisting of muscle strength training of both legs, balance and coordination exercises 2 times a week 2. 6 weeks of physical training (as above) |
| Outcomes | Follow‐up: 24 weeks after baseline testing Changes in knee‐extension strength Changes in the Timed Up and Go test |
| Starting date | Start date: March 2010 Estimated completion date: June 2013 |
| Contact information | Jan Overgaard Maribo Health Center Maribo, Denmark, 4930 email: jover@lolland.dk |
| Notes |
NCT02305433.
| Study name | Effects of long‐term intensive home‐based physiotherapy on older people with an operated hip fracture or frailty (RCT) |
| Methods | Randomised controlled trial |
| Participants | Age 65 and over for frail persons and age 60 and over for hip fracture patients; home‐dwelling but an increased risk for disabilities or for institutional care; ability to walk inside own home with or without mobility aids; ability to communicate in Finnish; in case of hip fracture: the first operated hip fracture; in case of frailty: signs of frailty assessed by modified Fried's frailty criteria 421 participants |
| Interventions | 1. Physiotherapy (physical exercise) 2. Usual care |
| Outcomes | Follow‐up: 12 months Primary outcome measure: duration of time living at home Secondary outcome measures
|
| Starting date | Study start date: December 2014 Estimated completion date: December 2019 |
| Contact information | Markku T Hupli, MD, PhD South Karelia, Social and Health Care District |
| Notes |
NCT02407444.
| Study name | A comparison of two physiotherapy treatment protocols, with and without cycling training, in elderly patients with hip fractures at their subacute stage following surgery |
| Methods | Randomised trial; blinded outcome assessor |
| Participants | People aged 65 years to 95 years. Proximal hip fracture with full or partial weight bearing indication. Surgical fixation (nailing or total hip replacement or hemiarthroplasty). Pre‐morbid function: walking independently or under supervision with or without assistance aid. Cognitive function: Mini Mental State Examination score above 21. Aim: 60 participants |
| Interventions | 1. Physiotherapy treatment and leg cycling 2. Physiotherapy treatment and music listening |
| Outcomes | Follow‐up: end of intervention at third week Functional Independence Measure Static balance test and weight‐bearing distribution while standing Muscle strength Pain intensity |
| Starting date | Study start date: July 2015 Completion date: December 2018 |
| Contact information | Avital Hershkovitz, MD, PhD 97 2522342123 avitalhe@clalit.org.il Hila Dahan, BPT 972542458459 dahan.hila@gmail.com "Beit‐ Rivka" geriatric rehabilitation hospital Petach tiqva, Israel |
| Notes |
NCT02815254.
| Study name | The effect of exercise in elderly hip fracture patients: a clinical randomised trial |
| Methods | Randomised trial; blinded outcome assessor |
| Participants | People aged 65 years or older. Fractura colli femoris, pertrochanter or subtrochanter. Discharged from hospital within 3 weeks since surgery. Need of minimum two weeks of rehabilitation. Life expectancy of more than one month. Able to walk at least 3 metres with walking aid. Willingness to participate. Able to follow instructions. Aim: 130 participants |
| Interventions | 1. Low‐intensity functional exercise 2. High‐intensity functional exercise |
| Outcomes | Follow‐up: 3 years Short Physical Performance Battery |
| Starting date | Start date: November 2015 Completion date: October 2018 |
| Contact information | Astrid Bergland Braseth rehabilitation centre Røyken, Norway, 3440 +47 45272760 astrid.bergland@hioa.no |
| Notes |
NCT02938923.
| Study name | Combining testosterone therapy and exercise to improve function post hip fracture |
| Methods | Multicenter, randomised, placebo‐controlled trial. Blinded participants, care providers, investigators and outcomes assessors |
| Participants | Community‐dwelling or in assisted living prior to the hip fracture event. Female 65 years and older. Surgical repair of a non‐pathologic fracture of the proximal femur (including: intracapsular, intertrochanteric and subtrochanteric fractures) with a surgical repair date that is within 6 to 14 weeks at screening, and within 16 weeks at randomisation. Functional impairment at the time of screening, defined as a modified Physical Performance Score (mPPT) of 12 to 28. Serum total testosterone level < 40 ng/dL. Aim: 300 participants |
| Interventions | 1. Exercise plus testosterone gel 2. Exercise plus placebo gel 3. Enhanced usual care |
| Outcomes | Follow‐up: 6 months Change in 6‐Minute Walk Test distance Change in total lean body mass Change in appendicular lean body mass Change in 1 repetition maximum (1 RM) leg press strength Change in Total Modified Physical Performance Test score Change in Short Physical Performance Battery score Change in Older Adult Resources and Services Activities of Daily Living Questionnaire ADL Total Score Change in Functional Status Questionnaire Total Score Change in Hip Rating Questionnaire Total Score Change in Patient‐Reported Outcomes Measurement Information System Global Health score Change in bone mineral density of the non‐fractured proximal femur |
| Starting date | Study start date: September 2017 Estimated completion date: May 2022 |
| Contact information | Ellen F Binder, MD Professor of Medicine, Washington University School of Medicine 314‐286‐2707 ebinder@wustl.edu Kelly M Monroe, MSW 314‐273‐1160 monroek@wustl.edu |
| Notes | RM: repetition maximum |
NCT03030092.
| Study name | Maximal strength training following hip fracture surgery: impact on muscle mass, balance, walking efficiency and bone density |
| Methods | Randomised trial |
| Participants | People aged over 65 with hip fracture surgery Aim: 40 participants |
| Interventions | 1. Maximal strength training 2. Standard care |
| Outcomes | Follow‐up: 8 weeks Walking efficiency Muscle mass Bone density Balance |
| Starting date | Study start date: January 2017 Completion date: July 2018 |
| Contact information | Molde University College |
| Notes |
NCT04095338.
| Study name | Assistive robotic in the elderly: innovative models in the rehabilitation of the elderly with hip fractures through technological innovation |
| Methods | Randomised controlled trial; blinded outcomes assessor |
| Participants | Aged 65 or above; traumatic event within 60 days; Functional Ambulation Category score ≤ 2; Ranking scale score ≤ 3; Romberg test: negative; capacity to consent Aim: 195 participants |
| Interventions | 1. Experiment (virtual reality game): each session includes 30 minutes of traditional physical rehabilitation plus 20 minutes of virtual robotic training that simulates floor walking and stair climbing 2. Robotic treadmill: each session includes 30 minutes of traditional physical rehabilitation plus 20 minutes of robotic training on a treadmill 3. Control: 50 minutes of traditional physical rehabilitation per session All groups: 2 sessions per week for 5 weeks |
| Outcomes | Follow‐up: 24 months post‐intervention Primary outcome: difference in fall risk using the Tinetti Performance‐Oriented Mobility Assessment Secondary outcomes
|
| Starting date | Study start date: November 2019 Estimated completion date: September 2022 |
| Contact information | Roberta Bevilacqua INRCA Research Hospital Ancona, Italy, 60131 00390718004767 r.bevilacqua@inrca.it |
| Notes |
NCT04108793.
| Study name | Effectiveness of home‐based rehabilitation program in minimizing disability and secondary falls after a hip fracture: a randomized controlled trial |
| Methods | Randomised controlled trial; open‐label |
| Participants | Aged 60 or above; diagnosis of proximal femoral fracture; surgical procedure was bipolar hemiarthroplasty / total hip replacement and postoperative ambulatory status weight bearing as tolerated; able to walk independently with or without a walking frame prior to the fracture; history of fall Aim: 224 participants |
| Interventions | 1. Intervention: extended home‐based rehabilitation programme including progressive balance and lower limb strengthening exercises, twice a week for 12 weeks 2. Control: usual postoperative rehabilitation |
| Outcomes | Follow‐up: 2 years Primary outcome: occurrence of secondary fall Secondary outcome: physical mobility and mobility‐related disability |
| Starting date | Study start date: October 2019 Estimated completion date: October 2021 |
| Contact information | Dr. Shahryar Noordin Associate Professor and orthopedic surgeon Aga Khan University +92 34864384 ext 4384 shahryar.noordin@aku.edu |
| Notes |
NCT04207788.
| Study name | HIP fracture REhabilitation Programme for elderly with hip fracture (HIP‐REP) |
| Methods | Randomised controlled trial; blinded participants, care provider, investigator and outcomes assessor |
| Participants | Aged 65 years or older; recent proximal hip fracture (International Classification of Diseases codes S72.0 medial femur fracture, S72.1, pertrochanteric femur fracture, S72.2 subtrochanteric femur fracture); living at home prior to hip fracture in Herlev, Gentofte, Furesoe, Rudersdal or Lyngby‐Taarbæk municipalities; ability to give informed consent Aim: 108 participants |
| Interventions | 1. Usual care plus 5 add‐on individual activity‐focused interventions specific to the needs of elderly people with hip fracture 2. Usual care |
| Outcomes | Follow‐up: 6 months after baseline testing Primary outcome: Assessment of Motor and Process Skills Secondary outcomes:
|
| Starting date | Study start date: January 2020 Estimated completion date: August 2021 |
| Contact information | Carsten Bogh Juh Herlev and Gentofte Hospital carsten.bogh.juhl@regionh.dk |
| Notes |
NCT04228068.
| Study name | A home‐based rehabilitation program for patients with hip fracture: a pilot randomized trial |
| Methods | Randomised controlled trial; blinded outcome assessors |
| Participants | Hip fracture patients who are 65 years or older and being discharged to home or retirement home Aim: 40 participants |
| Interventions | 1. Seven home visits in total over the first 12 weeks after returning home; 2 visits by the physiotherapist to assess, tailor the program and coach the participants in carrying out the exercises at home; the physiotherapy assistant to facilitate and progress the exercise program as prescribed by the physiotherapist every other week 2. Usual care |
| Outcomes | Follow‐up: 12 weeks post‐discharge to home Lower Extremity Functional Scale Short Physical Performance Battery |
| Starting date | Start date: March 2018 Estimated completion date: October 2020 |
| Contact information | Mohammad Auais Providence Care Hospital Kingston, Ontario, Canada, K7M 3N6 mara@queensu.ca [mailto:mara%40queensu.ca?subject=NCT04228068, REH‐721‐18, The Stronger at Home Study] |
| Notes |
NTR6794.
| Study name | COMplex Fracture Orthopedic Rehabilitation (COMFORT): real‐time visual biofeedback on weight bearing versus standard training methods in the treatment of proximal femur fractures in elderly: a randomised controlled trial |
| Methods | Randomised controlled trial; single‐blind |
| Participants | Age ≥ 60 years; participants rehabilitate from a proximal femur fracture following low‐energy trauma; prescribed unrestricted weight bearing after (surgical) treatment of their fracture; expected clinical rehabilitation duration of ≥ 2 weeks; bodyweight ≤ 120 kg Aim: 186 participants |
| Interventions | 1. Real‐time, visual feedback about weight bearing during 30 m walk 2. Control: active |
| Outcomes | Primary outcome measures
Secondary outcomes
|
| Starting date | Study start date: March 2017 Completion date: August 2018 |
| Contact information | M. Raaben M.Raaben‐2@umcutrecht.nl Department of Surgery, UMC Utrecht, Suite G04.228 Heidelberglaan 100 3584 CX Utrecht The Netherlands |
| Notes |
UMIN000036379.
| Study name | Randomized controlled trial with parallel design on the effects of maximum voluntary velocity training in patients after femoral neck fracture surgery |
| Methods | Randomised controlled trial; double‐blind |
| Participants | Aged 65 or above; femoral neck or trochanteric fracture treated surgically; reside in home; independent pre‐fracture and the ability to walk indoors; New Mobility Score (NMS) of 2 or more Aim: 26 participants |
| Interventions | 1. Evidence‐based standardised rehabilitation programme plus high‐velocity knee extension and hip abduction exercises 2 weeks after surgery 2. Evidence‐based standardised rehabilitation programme plus low‐velocity knee extension and hip abduction exercises 2 weeks after surgery |
| Outcomes | Follow‐up: not reported Primary outcome: knee extension maximum angular velocity of fracture side Secondary outcomes
|
| Starting date | Study start date: March 2019 Estimated completion date: March 2020 |
| Contact information | Yuuki Shimada Department of Rehabilitation, Nakazuyagi Hospital 088‐625‐3535 y_kato0928@yahoo.co.jp |
| Notes |
Differences between protocol and review
Summary of major changes in the current update (2022)
We updated the review methodology according to current Cochrane guidance: this included risk of bias assessment, GRADE assessment of the certainty of the evidence, and production of summary of findings tables.
Other key differences are as follows.
In Objectives, we combined two objectives into one: to evaluate the effects (benefits and harms) of interventions aimed at improving mobility and physical functioning after hip fracture surgery in adults.
In Types of studies, we clarified that we would not include trials reported only in conference abstracts and where sufficient data were not available from correspondence with study authors or from the final report of the trial.
We expanded our account in Types of participants to clarify that we included trials where participants had undergone hip fracture surgery, irrespective of the type of hip fracture or surgery. We also described our expected population and clarified that we would include certain mixed population trials provided the majority of trial participants had hip fracture.
In Types of interventions, we clarified that we included trials testing early versus late mobilisation (in the in‐hospital setting), different intensities of mobilisation interventions, as well as different types of exercise programmes.
In Types of interventions, we indicated that we would now categorise exercise and physical training interventions using the ProFaNE classification. This is in addition to other intervention types (electrical stimulation, postoperative care programmes such as immediate or delayed weight bearing after surgery), which aim to improve walking ability and minimise functional impairments. We also specified our main comparisons and clarified that these included comparisons of different intensities of the same type of intervention.
We restructured Types of outcome measures, with the categorisation of main or 'critical' outcomes for presentation in summary of findings tables, other important outcomes and economic outcomes. All outcomes previously listed in Handoll 2011 still feature. We gave a greater priority to outcomes at four months for in‐hospital trials.
We listed the types of information, including details of intervention and co‐interventions, that we sought from reports of included studies in Data extraction and management.
In Assessment of risk of bias in included studies, we assessed four additional sources of bias: bias resulting from imbalances in key baseline characteristics (e.g. pre‐injury mobility, mental test score, type of surgery); performance bias such as that resulting from lack of comparability in the experience of care providers; bias relating to the recall of falls due to unreliable methods of ascertaining occurrence of falls; and detection bias for staff‐reported (in‐hospital studies) and self‐reported (post‐hospital studies) outcomes such as falls, where some risk of bias is inherent but can be minimised by blinding of research staff and statisticians involved in data collection and analysis. In order to evaluate bias effectively at the outcome level, we re‐considered our approach to assessing performance bias, detection bias and attrition bias. For performance bias, we made judgements for all outcomes in a single domain. For detection bias and attrition bias, we separated these into three separate domains according to whether outcomes were reported by an observer (in which personal judgement was likely or not likely) or reported by a participant or proxy.
We prespecified the following additional subgroup analyses in Subgroup analysis and investigation of heterogeneity: intervention delivered by expert health provider versus delivered by personnel not specified as an expert (for post‐hospital studies); trials excluding participants with cognitive impairment, dementia or delirium versus not excluding them; outpatient setting versus secondary and social care (for post‐hospital studies); in‐hospital ward versus rehabilitation ward; mean age of 80 years or less versus mean age over 80 years. We removed the following prespecified subgroup analysis, following direction from Cochrane: different types of interventions.
Whilst undertaking the review, we did not perform a subgroup analysis prespecified in Subgroup analysis and investigation of heterogeneity. We did not perform the prespecified subgroup analysis by expert versus non‐expert delivery of intervention, as it was not possible (we assumed all interventions were delivered by experts in the in‐hospital setting, and the three post‐hospital studies that did not have experts deliver the intervention did not contribute to the main outcomes).
In Sensitivity analysis, we prespecified additional sensitivity analyses with regard to publication status, risk of bias, study population and in‐hospital trials that measured outcomes at the end of the in‐hospital phase (the usual time point closest to four months). We undertook post hoc sensitivity analysis according to effects model (fixed‐effect versus random‐effects).
We assessed the certainty of the evidence using GRADE, and we prepared two summary of findings tables for the main comparison groups. We also developed two bespoke summary of findings tables in order to summarise the effects for the mobility outcome according to the different categories of exercise interventions.
In outcomes, we reported the main outcome (mobility) as an overall outcome, with one outcome from each study, prioritising objective measures over self‐report measures, broad mobility measures over (in order of priority) walking, balance and sit‐to‐stand measures. Because some studies reported multiple clinically useful measures of mobility and we were concerned that we would lose information, we also reported the objective measures separately for the broad mobility outcome, with a study able to contribute to multiple outcomes.
For this update, we specified that we compare "Provision of any specific mobilisation strategy or programme and non‐provision, where the non‐provision control is defined as no intervention, usual care, sham exercise (the exercise was intended to be a control, or appeared to be of insufficient intensity and progression to have beneficial effects on mobility) or a social visit." In the in‐hospital setting, standard physiotherapy is therefore considered a control intervention. In previous versions of the review, Karumo 1977 was analysed under 'intensive versus usual physiotherapy' and Lauridsen 2002 had been considered a study of intensive versus standard physiotherapy. From this version of the review, we consider the interventions of these two studies versus control.
We reported adherence to the intervention.
Where mean and standard deviation were not reported and appropriate data were available, we calculated mean and standard deviation from the median IQR/1.35 in accordance with Higgins 2021a.
The author team has changed since Handoll 2011. H Handoll is no longer an author. N Fairhall, S Dyer and J Diong became authors, and W Kowk became an author after work on this review commenced.
Most of these changes to protocol, which were made partly in response to a commissioning brief generated in relation to the Cochrane Programme Grant on the management of hip fracture, were established in April 2019 prior to the date of the final search.
Summary of major changes up to the update in 2011
The key differences made in the 2011 update were as follows (Handoll 2011).
Title was revised to reflect better the scope of the review.
Trials testing interventions that, in the majority of participants, started after approximately one year were excluded.
Trials testing mobilisation strategies with nutrition as a co‐intervention were included.
Types of outcomes were restructured, with the categorisation of primary and secondary outcomes.
Risk of bias was assessed using the Cochrane risk of bias tool (RoB1), which replaced the assessment of 10 aspects of methodological quality.
The original review was confined to the topic of early weight bearing and mobilisation after internal fixation of intracapsular proximal femoral fractures in adults (Parker 1999). This was then expanded to include interventions that had been used in the mobilisation of all hip fracture patients after surgery and started in the first phase of rehabilitation, generally whilst the patient was in hospital (Handoll 2003). The third update extended the scope further to include mobilisation strategies applied in the later stages of rehabilitation, generally in the community (Handoll 2004).
Contributions of authors
All authors have contributed to the production of this review.
NF was involved in screening, data extraction, data analysis and co‐led the writing of the review. SD was involved in screening, data extraction, data analysis, contributed to writing the review and commented on drafts of the review. JM was involved in screening, contributed to writing the review and commented on drafts of the review. JD contributed to writing the review and commented on drafts of the review. WK was involved in screening, data extraction and contributed to writing the review. CS was involved in screening, data extraction, data analysis, co‐led the writing of the review and acted as guarantor of the review.
The contribution statements for all previous versions of the review up to 2011 are presented in Handoll 2011.
Sources of support
Internal sources
-
N/A, Other
N/A
-
Nil, Other
Nil
External sources
-
National Health and Medical Research Council, Fellowship, Australia
Fellowship funding
Declarations of interest
NF: none SD: none JM: none JD: none WK: none CS: as Catherine Sherrington is an active investigator in several randomised trials in this area, assessment of eligibility of these trials and quality assessment of the four included trials was done independently by two other review authors. Independent data extraction and entry into Review Manager software, presentation and interpretation of these trials were also performed.
New search for studies and content updated (conclusions changed)
References
References to studies included in this review
Baker 1991 {published data only}
- Baker PA, Evans OM, Lee C. Treadmill gait retraining following fractured neck-of-femur. Archives of Physical Medicine and Rehabilitation 1991;72(9):649-52. [PubMed] [Google Scholar]
Binder 2004 {published data only}
- Binder EF, Brown M, Sinacore DR, Steger-May K, Yarasheski KE, Schechtman KB. Effects of extended outpatient rehabilitation after hip fracture: a randomized controlled trial. Journal of the American Medical Association 2004;292(7):837-46. [DOI] [PubMed] [Google Scholar]
- Binder EF, Sinacore DR, Schechtman KB, Brown M. Effects of intensive exercise after hip fracture: results from a randomised, controlled trial [Abstract]. Journal of the American Geriatrics Society 2003;51(Suppl 4):S232. [Google Scholar]
- Host HH, Sinacore DR, Bohnert KL, Steger-May K, Brown M, Binder EF. Training-induced strength and functional adaptations after hip fracture. Physical Therapy 2007;87(3):292-303. [DOI] [PubMed] [Google Scholar]
- NCT00006194. Effects of exercise on markers of inflammation in skeletal muscle in elderly hip fracture patients. clinicaltrials.gov/ct2/show/NCT00006194 (first received 8 September 2000).
Bischoff‐Ferrari 2010 {published data only}
- Bischoff-Ferrari, H. Functioning and quality of life outcomes [personal communication]. Email to: N Fairhall 5 October 2019.
- Bischoff-Ferrari H, Dawson-Hughes B, Orav E, Willett W, Egli A, Maetzel A, et al. The economic consequences of hip fractures: impact of home exercise and high-dose vitamin D. Journal of Bone and Mineral Research 2010;25(Suppl 1):[no pagination]. [Google Scholar]
- Bischoff-Ferrari HA, Dawson-Hughes B, Platz A, Orav EJ, Stahelin HB, Willett WC, et al. Effect of high-dosage cholecalciferol and extended physiotherapy on complications after hip fracture: a randomized controlled trial. Archives of Internal Medicine 2010;170(9):813-20. [DOI] [PubMed] [Google Scholar]
- Renerts K, Fischer K, Dawson-Hughes B, Orav EJ, Freystaetter G, Simmen HP, et al. Effects of a simple home exercise program and vitamin D supplementation on health-related quality of life after a hip fracture: a randomized controlled trial. Quality of Life Research 2019;28:1377-86. [DOI] [PubMed] [Google Scholar]
- Stemmle J, Marzel A, Chocano-Bedoya PO, Orav EJ, Dawson-Hughes B, Freystaetter G, et al. Effect of 800 IU versus 2000 IU Vitamin D3 with or without a simple home exercise program on functional recovery after hip fracture: a randomized controlled trial. Journal of the American Medical Directors Association 2019;20(5):530-6. [DOI] [PubMed] [Google Scholar]
Braid 2008 {published and unpublished data}
- Braid V, Barber M, Mitchell SL, Martin BJ, Granat M, Stott DJ. Randomised controlled trial of electrical stimulation of the quadriceps after proximal femoral fracture. Aging Clinical and Experimental Research 2008;20(1):62-6. [DOI] [PubMed] [Google Scholar]
- Braid V, Barber M, Mitchell SL, Martin BJ, Grant SJ, Granat M, et al. Proximal femoral fracture: a randomised controlled trial of electrical stimulation [abstract]. In: Extending the boundaries. Congress and Exhibition of the Chartered Society of Physiotherapy. Proceedings Book; 2001 Oct 19-21; Birmingham (UK). London (UK): The Chartered Society of Physiotherapy, 2001:15.
- Braid V, Barber M, Mitchell SL, Martin BJ, Grant SJ, Granat M, et al. Proximal femoral fracture rehabilitation: a randomised controlled trial of electrical stimulation of the quadriceps [abstract]. Age and Ageing 2002;28 Suppl 1:28. [Google Scholar]
- Braid V. [personal communication]. 3 March 2004.
- Mitchell S. A randomised, controlled trial of electrical stimulation of the quadriceps in patients rehabilitating after a proximal femoral fracture. In: National Research Register, Issue 2, 2001. Oxford: Update Software.
Gorodetskyi 2007 {published data only}
- Gorodetskyi IG, Gorodnichenko AI, Tursin PS, Reshetnyak VK, Uskov ON. Non-invasive interactive neurostimulation in the post-operative recovery of patients with a trochanteric fracture of the femur: a randomised, controlled trial. Journal of Bone and Joint Surgery - British Volume 2007;89(11):1488-94. [DOI] [PubMed] [Google Scholar]
Graham 1968 {published data only}
- Abrami G, Stevens J. Early weight bearing after internal fixation of transcervical fracture of the femur. Preliminary report of a clinical trial. Journal of Bone and Joint Surgery. British Volume 1964;46(2):204-5. [PubMed] [Google Scholar]
- Graham J. Early or delayed weight-bearing after internal fixation of transcervical fracture of the femur. A clinical trial. Journal of Bone and Joint Surgery. British Volume 1968;50(3):562-9. [PubMed] [Google Scholar]
Hauer 2002 {published and unpublished data}
- Hauer K, Pfisterer M, Schuler M, Bartsch P, Oster P. Two years later: a prospective long-term follow-up of a training intervention in geriatric patients with a history of severe falls. Archives of Physical Medicine and Rehabilitation 2003;84(10):1426-32. [DOI] [PubMed] [Google Scholar]
- Hauer K, Rost B, Rutschle K, Opitz H, Specht N, Bartsch P, et al. Exercise training for rehabilitation and secondary prevention of falls in geriatric patients with a history of injurious falls. Journal of the American Geriatrics Society 2001;49(1):10-20. [DOI] [PubMed] [Google Scholar]
- Hauer K, Specht N, Schuler M, Bartsch P, Oster P. Intensive physical training in geriatric patients after severe falls and hip surgery. Age and Ageing 2002;31(1):49-57. [DOI] [PubMed] [Google Scholar]
- Hauer K. [personal communication]. 5 March 2004.
- Oster P, Hauer K, Specht N, Rost B, Baertsch P, Schlierft G. Muscle strength and coordination training for prevention of falls in elderly patients [Kraft- and Koordinationstraining zur Sturzpravention in Alter]. Zeitschrift Fur Gerontologie Und Geriatrie 1997;30:289-92. [PubMed] [Google Scholar]
Karumo 1977 {published data only}
- Karumo I. A Randomized Trial of Postoperative Physiotherapy After Meniscectomy and Fractures of the Femoral Neck and Shaft [Thesis]. Helsinki, Finland: University of Helsinki, 1978. [Google Scholar]
- Karumo I. Recovery and rehabilitation of elderly subjects with femoral neck fractures. Annales Chirurgiae et Gynaecologiae 1977;66(3):170-6. [PubMed] [Google Scholar]
Kimmel 2016 {published data only}
- Kimmel LA, Liew SM, Sayer JM, Holland, AE. HIPS4HIPS (high intensity physiotherapy for hip fractures in the acute hospital setting): a randomised controlled trial. Medical Journal of Australia 2016;205(2):73-8. [DOI] [PubMed] [Google Scholar]
Kronborg 2017 {published data only}
- Kronborg L, Bandholm T, Palm H, Kehlet H, Kristensen MT. Effectiveness of acute in-hospital physiotherapy with knee-extension strength training in reducing strength deficits in patients with a hip fracture: a randomised controlled trial. PLOS One 2017;12(6):e0179867. [DOI] [PMC free article] [PubMed] [Google Scholar]
- NCT00848913. Strength training after hip fracture surgery. clinicaltrials.gov/ct2/show/NCT00848913?term=NCT00848913 (first received 20 February 2009).
Lamb 2002 {published data only}
- Lamb SE, Grimley Evans J, Morse RE, Trundle H. A randomised placebo controlled and double blind study of neuromuscular stimulation to improve mobility in the first three months after surgical fixation for proximal femoral fracture [abstract]. Journal of Bone and Joint Surgery. British Volume 1998;80(Suppl II):172. [Google Scholar]
- Lamb SE, Oldham JA, Morse RE, Evans JG. Neuromuscular stimulation of the quadriceps muscle after hip fracture: a randomized controlled trial. Archives of Physical Medicine and Rehabilitation 2002;83(8):1087-92. [DOI] [PubMed] [Google Scholar]
Langford 2015 {published and unpublished data}
- Langford D. Pain outcome [personal communication]. Email to: S Dyer 3 May 2016.
- Langford DP, Fleig L, Brown KC, Cho NJ, Frost M, Ledoyen M, et al. Back to the future - feasibility of recruitment and retention to patient education and telephone follow-up after hip fracture: a pilot randomized controlled trial. Patient Preference and Adherence 2015;9:1343-51. [DOI] [PMC free article] [PubMed] [Google Scholar]
Latham 2014 {published data only}
- Chang FH, Latham NK, Ni P, Jette AM. Does self-efficacy mediate functional change in older adults participating in an exercise program after hip fracture? A randomized controlled trial. Archives of Physical Medicine and Rehabilitation 2015;96(6):1014-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Latham NK, Harris BA, Bean JF, Heeren T, Goodyear C, Zawacki S, et al. Effect of a home-based exercise program on functional recovery following rehabilitation after hip fracture: a randomized clinical trial. Journal of the American Medical Association 2014;311(7):700-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- NCT00592813. Efficacy of a post-rehabilitation exercise intervention. clinicaltrials.gov/ct2/show/NCT00592813 (first received 14 January 2008).
Lauridsen 2002 {published data only}
- Lauridsen UB, la Cour BB, Gottschalck L, Svensson BH. Intensive physical therapy after hip fracture. Danish Medical Bulletin 2002;49(1):70-2. [PubMed] [Google Scholar]
- Lauridsen UB, la Cour BB, Gottschalck L, Svensson BH. Intensive physical therapy after trochanteric femoral fracture. A randomized clinical trial [Intensiv fysisk traening efter hoftenaer femurfraktur. En randomiseret klinisk undersogelse]. Ugeskrift for Laeger 2002;164(8):1040-4. [PubMed] [Google Scholar]
- Parker MJ. [personal communication]. 6 August 2002.
Magaziner 2019 {published data only}
- Magaziner J, Mangione KK, Orwig D, Baumgarten M, Magder L, Terrin M, et al. Effect of a multicomponent home-based physical therapy intervention on ambulation after hip fracture in older adults - the CAP randomized clinical trial. Journal of the American Medical Association 2019;322(10):946-56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Magaziner J. Measurement of fall outcome [personal communication]. Email to S Dyer November 2019.
Mangione 2005 {published data only}
- Mangione KK, Craik RL, Tomlinson SS, Palombaro KM. Can elderly patients who have had a hip fracture perform moderate- to high-intensity exercise at home. Physical Therapy 2005;85(8):727-39. [PubMed] [Google Scholar]
- Mangione KK, Craik RL, Tomlinson SS, Palombaro KM. The effects of aggressive home exercise in patients post hip fracture. In: 56th Annual Scientific Meeting of the Gerontological Society of America; 2003 Nov 21-25; San Diego, California. 2003.
- Mangione KK, Tomlinson S, Craik RL. Physical therapist interventions to optimize physical performance in patients after hip fracture. Journal of Geriatric Physical Therapy 2001;24(3):17. [Google Scholar]
Mangione 2010 {published data only}
- Mangione KK, Craik RL, Palombaro KM, Tomlinson SS, Hofmann MT. Home-based leg-strengthening exercise improves function 1 year after hip fracture: a randomized controlled study. Journal of the American Geriatrics Society 2010;58(10):1911-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- NCT00997776. Effect of leg strengthening exercise after hip fracture. clinicaltrials.gov/ct2/show/NCT00997776 (first received 19 October 2009).
Miller 2006 {published and unpublished data}
- Crotty M. [personal communication]. 20 February 2009.
- Crotty M. [personal communication]. 25 July 2003.
- Miller MD, Crotty M, Whitehead C, Bannerman E, Daniels LA. Nutritional supplementation and resistance training in nutritionally at risk older adults following lower limb fracture: a randomized controlled trial. Clinical Rehabilitation 2006;20(4):311-23. [DOI] [PubMed] [Google Scholar]
Mitchell 2001 {published and unpublished data}
- Martin BJ. Randomised, controlled trial of additional quadriceps strength training in patients rehabilitating after a proximal femoral fracture. In: National Research Register, Issue 2, 2001. Oxford: Update Software.
- Mitchell SL, Stott DJ, Martin BJ, Grant SJ. Randomised controlled trial of quadriceps training after proximal femoral fracture. Clinical Rehabilitation 2001;15(3):282-90. [DOI] [PubMed] [Google Scholar]
- Mitchell SL, Stott DJ, Martin BJ, Grant SJ. Randomised controlled trial of quadriceps training after proximal femoral fracture [abstract]. Age and Ageing 1999;28(Suppl 2):81. [DOI] [PubMed] [Google Scholar]
Monticone 2018 {published data only}
- Monticone M, Ambrosini E, Brunati R, Capone A, Pagliari G, Secci C, et al. How balance task-specific training contributes to improving physical function in older subjects undergoing rehabilitation following hip fracture: a randomized controlled trial. Clinical Rehabilitation 2018;32(3):340-51. [DOI] [PubMed] [Google Scholar]
Moseley 2009 {published and unpublished data}
- ACTRN12605000649617. Enhancing mobility after hip fracture. www.anzctr.org.au/ACTRN12605000649617.aspx (first received 09 September 2005).
- Cameron IC. [personal communication]. 1 March 2002.
- Moseley AM, Sherrington C, Lord SR, Barraclough E, St George RJ, Cameron ID. Mobility training after hip fracture: a randomised controlled trial. Age and Ageing 2009;38(1):74-80. [DOI] [PubMed] [Google Scholar]
Oh 2020 {published data only}
- Oh MK, Yoo JI, Byun H, Chun SW, Lim SK, Jang YJ, et al. Efficacy of combined antigravity treadmill and conventional rehabilitation after hip fracture in patients with sarcopenia. Journals of Gerontology: Series A 2020;75(10):e173-e181. [DOI: 10.1093/gerona/glaa158] [DOI] [PubMed] [Google Scholar]
Ohoka 2015 {published and unpublished data}
- Ohoka, T. Outcomes [personal communication]. Email to: S Dyer 8 May 2017.
- Ohoka T, Urabe Y, Shirakawa T. Therapeutic exercises for proximal femoral fracture of super-aged patients: effect of walking assistance using body weight-supported treadmill training (BWSTT). Physiotherapy 2015;101(1):e1124-5. [0031-9406] [Google Scholar]
Oldmeadow 2006 {published data only}
- NCT00224367. Does early ambulation after hip fracture surgery accelerate recovery? clinicaltrials.gov/ct2/show/record/NCT00224367 (first received 23 September 2005).
- Oldmeadow LB, Edwards ER, Kimmel LA, Kipen E, Robertson VJ, Bailey MJ. No rest for the wounded: early ambulation after hip surgery accelerates recovery. ANZ Journal of Surgery 2006;76(7):607-11. [DOI] [PubMed] [Google Scholar]
Orwig 2011 {published data only}
- Orwig DL, Hochberg M, Yu-Yahiro J, Resnick B, Hawkes WG, Shardell M, et al. Delivery and outcomes of a yearlong home exercise program after hip fracture: a randomized controlled trial. Archives of Internal Medicine 2011;171(4):323-31. [DOI] [PMC free article] [PubMed] [Google Scholar]
Pol 2019 {published data only}
- Pol MC, Ter Riet G, Van Hartingsveldt M, Kröse B, Rooij SE, Buurman BM. Effectiveness of sensor monitoring in an occupational therapy rehabilitation program for older individuals after hip fracture, the SO-HIP trial: study protocol of a three-arm stepped wedge cluster randomized trial. BMC Health Services Research 2017;17(1):3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pol MC, Ter Riet G, Van Hartingsveldt M, Krose B, Buurman BM. Effectiveness of sensor monitoring in a rehabilitation programme for older patients after hip fracture: a three-arm stepped wedge randomised trial. Age and Ageing 2019;48(5):648-55. [DOI] [PubMed] [Google Scholar]
Resnick 2007 {published and unpublished data}
- NCT00389844. BHS5 - Testing the effectiveness of the exercise plus program (Hip5) [Testing the effectiveness of the exercise plus program on efficacy expectations, exercise behavior & activity of older adults following a hip fracture]. clinicaltrials.gov/ct2/show/NCT00389844 (first received 19 October 2006).
- Resnick B, D'Adamo C, Shardell M, Orwig D, Hawkes W, Hebel JR. Adherence to an exercise intervention among older women post hip fracture. Journal of Clinical Sport Psychology 2008;2(1):41-56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Resnick B, Magaziner J, Orwig, D, Zimmerman S. Evaluating the components of the Exercise Plus Program: rationale, theory and implementation. Health Education Research 2002;17(5):648-58. [DOI] [PubMed] [Google Scholar]
- Resnick B, Orwig D, D'Adamo C, Yu-Yahiro J, Hawkes W, Shardell M, et al. Factors that influence exercise activity among women post hip fracture participating in the Exercise Plus Program. Clinical Interventions In Aging 2007;2(3):413-27. [PMC free article] [PubMed] [Google Scholar]
- Resnick B, Orwig D, Hawkes W, Shardell M, Golden J, Werner M, et al. The relationship between psychosocial state and exercise behavior of older women 2 months after hip fracture. Rehabilitation Nursing 2007;32(4):139-49. [DOI] [PubMed] [Google Scholar]
- Resnick B, Orwig D, Yu-Yahiro J, Hawkes W, Shardell M, Hebel JR, et al. Testing the effectiveness of the exercise plus program in older women post-hip fracture. Annals of Behavioral Medicine 2007;34(1):67-76. [DOI] [PubMed] [Google Scholar]
- Resnick B. [personal communication]. 9 February 2004.
- Resnick B. Testing the Exercise Plus Program following hip fracture. www1.od.nih.gov/behaviorchange/projects/maryland.htm (accessed 10 January 2004).
- Yu-Yahiro JA, Resnick B, Orwig D, Hicks G, Magaziner J. Design and implementation of a home-based exercise program post-hip fracture: the Baltimore hip studies experience. Physical Medicine and Rehabilitation 2009;1(4):308-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
Salpakoski 2015 {published and unpublished data}
- Edgren J, Salpakoski A, Sihvonen SE, Portegijs E, Kallinen M, Arkela M, et al. Effects of a home-based physical rehabilitation program on physical disability after hip fracture: a randomized controlled trial. Journal of the American Medical Directors Association 2015;16(4):350.e1-7. [DOI] [PubMed] [Google Scholar]
- Salpakoski, A. Mobility and strength outcomes [personal communication]. Email to: N Fairhall 12 August 2019.
- Salpakoski A, Tormakangas T, Edgren J, Kallinen M, Sihvonen SE, Pesola M, et al. Effects of a multicomponent home-based physical rehabilitation program on mobility recovery after hip fracture: a randomized controlled trial. Journal of the American Medical Directors Association 2014;15(5):361-8. [DOI] [PubMed] [Google Scholar]
- Sipilä S, Salpakoski A, Edgren J, Heinonen A, Kauppinen MA, Arkela-Kautiainen M, et al. Promoting mobility after hip fracture (ProMo): study protocol and selected baseline results of a year-long randomized controlled trial among community-dwelling older people. BMC Musculoskeletal Disorders 2011;12:277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Turunen K, Salpakoski A, Edgren J, Törmäkangas T, Arkela M, Kallinen M, et al. Physical activity after a hip fracture: effect of a multicomponent home-based rehabilitation program—a secondary analysis of a randomized controlled trial. Archives of Physical Medicine and Rehabilitation 2017;98(5):981-8. [DOI] [PubMed] [Google Scholar]
Sherrington 1997 {published and unpublished data}
- Sherrington C, Lord SR. Home exercise to improve strength and walking velocity after hip fracture: a randomised controlled trial. Archives of Physical Medicine and Rehabilitation 1997;78(2):208-12. [DOI] [PubMed] [Google Scholar]
- Sherrington C. [personal communication]. 15 January 2004.
- Sherrington C. [personal communication]. 24 March 2004.
Sherrington 2003 {published and unpublished data}
- Sherrington C, Lord SR, Herbert RD. A randomised trial of weight-bearing versus non-weight-bearing exercise for improving physical ability in inpatients after hip fracture. Australian Journal of Physiotherapy 2003;49(1):15-22. [DOI] [PubMed] [Google Scholar]
- Sherrington C, Lord SR, Herbert RD. The effects of exercise on physical ability following fall-related hip fracture: two randomised controlled trials. In: Proceedings of the Australian Physiotherapy Association 7th International Physiotherapy Congress; 2002 May 25-28; Sydney, Australia. 2002.
- Sherrington C. [personal communication]. 15 January 2004.
Sherrington 2004 {published and unpublished data}
- Sherrington C, Lord SR, Herbert RD. A randomised controlled trial of weight-bearing versus non-weight-bearing exercise for improving physical ability after hip fracture and completion of usual care [Abstract]. In: XVIth Conference of the International Society for Postural and Gait Research; 2003 March 23-27; Sydney, Australia. www.powmri.unsw.edu.au/ispg2003/ (accessed 24 July 03).
- Sherrington C, Lord SR, Herbert RD. A randomized controlled trial of weight-bearing versus non-weight-bearing exercise for improving physical ability after usual care for hip fracture. Archives of Physical Medicine and Rehabilitation 2004;85(5):710-6. [DOI] [PubMed] [Google Scholar]
- Sherrington C, Lord SR, Herbert RD. The effects of exercise on physical ability following fall-related hip fracture: two randomised controlled trials. In: Proceedings of the Australian Physiotherapy Association 7th International Physiotherapy Congress; 2002 May 25-28; Sydney, Australia. 2002.
- Sherrington C. [personal communication]. 9 February 2004.
Sherrington 2020 {published and unpublished data}
- Sherrington C, Fairhall N, Kirkham C, Clemson L, Tiedemann A, Vogler C, et al. Exercise and fall prevention self-management to reduce mobility-related disability and falls after fall-related lower limb or pelvic fracture in older people: the RESTORE (Recovery Exercises and STepping On afteR fracturE) randomized controlled trial. Journal of General Internal Medicine 2020;35:2907–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sherrington C. Outcomes in study participants with hip fracture. Personal communication with N Fairhall February 2020.
Stasi 2019 {published data only}
- Stasi S, Papathanasiou G, Chronopoulos E, Dontas IA, Baltopoulos IP, Papaioannou NA. The effect of intensive abductor strengthening on postoperative muscle efficiency and functional ability of hip-fractured patients: a randomized controlled trial. Indian Journal of Orthopaedics 2019;53(3):407–19. [DOI] [PMC free article] [PubMed] [Google Scholar]
Suwanpasu 2014 {published data only}
- Suwanpasua S, Aungsurochb Y, Jitapanyab C. Post-surgical physical activity enhancing program for elderly patients after hip fracture: a randomized controlled trial. Asian Biomedicine 2014;8(4):525-32. [Google Scholar]
Sylliaas 2011 {published data only}
- Sylliaas H, Brovold T, Wyller TB, Bergland A. Progressive strength training in older patients after hip fracture: a randomised controlled trial. Age and Ageing 2011;40(2):221-7. [DOI] [PubMed] [Google Scholar]
Sylliaas 2012 {published data only}
- Sylliaas H, Brovold T, Wyller TB, Bergland A. Prolonged strength training in older patients after hip fracture: a randomised controlled trial. Age and Ageing 2012;41(2):206-12. [DOI] [PubMed] [Google Scholar]
Taraldsen 2019 {published data only}
- Taraldsen K, Thingstad P, Dohl O, Follestad T, Helbostad JL, Lamb SE, et al. Short and long-term clinical effectiveness and cost-effectiveness of a late-phase community-based balance and gait exercise program following hip fracture. The EVA-Hip Randomised Controlled Trial. PLoS One 2019;14(11):e0224971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taraldsen K. Faller outcome data [personal communication]. Email to: N Fairhall 22 June 2020.
Tsauo 2005 {published data only}
- Tsauo J-Y, Leu W-S, Chen Y-T, Yang R-S. Effects on function and quality of life of postoperative home-based physical therapy for patients with hip fracture. Archives of Physical Medicine and Rehabilitation 2005;86(10):1953-7. [DOI] [PubMed] [Google Scholar]
Van Ooijen 2016 {published data only}
- Van Ooijen MW, Roerdink M, Timmermans C, Trekop M, Arendse S, Nijenhuis E, et al. Feasibility of C-mill gait-adaptability training in older adults after fall-related hip fracture: user's perspective and training content. European Geriatric Medicine 2014;5:S169. [Google Scholar]
- Van Ooijen MW, Roerdink M, Trekop M, Janssen TW, Beek PJ. The efficacy of treadmill training with and without projected visual context for improving walking ability and reducing fall incidence and fear of falling in older adults with fall-related hip fracture: a randomized controlled trial. BMC Geriatrics 2016;16(1):215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van Ooijen MW, Roerdink M, Trekop M, Visschedijk J, Janssen TW, Beek PJ. Functional gait rehabilitation in elderly people following a fall-related hip fracture using a treadmill with visual context: design of a randomized controlled trial. BMC Geriatrics 2013;13:34. [DOI] [PMC free article] [PubMed] [Google Scholar]
Williams 2016 {published data only}
- Williams NH, Roberts JL, Din NU, Totton N, Charles JM, Hawkes CA, et al. Fracture in the Elderly Multidisciplinary Rehabilitation (FEMuR): a phase II randomised feasibility study of a multidisciplinary rehabilitation package following hip fracture. BMJ Open 2016;6:e012422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams NH, Roberts JL, Ud Din N, Charles JM, Totton N, Williams M, et al. Developing a multidisciplinary rehabilitation package following hip fracture and testing in a randomized feasibility study: fracture in the Elderly Multidisciplinary Rehabilitation (FEMuR). Health Technology Assessment 2017;21(44):1-527. [DOI] [PMC free article] [PubMed] [Google Scholar]
References to studies excluded from this review
Adunsky 2011 {published data only}
- Adunsky A, Chandler J, Heyden N, Lutkiewicz J, Scott BB, Berd Y, et al. MK-0677 (ibutamoren mesylate) for the treatment of patients recovering from hip fracture: a multicenter, randomized, placebo-controlled phase IIb study. Archives of Gerontology and Geriatrics 2011;53(2):183-9. [DOI] [PubMed] [Google Scholar]
Aftab 2020 {published data only}
- Aftab A, Awan WA, Habibullah S, Lim JY. Effects of fragility fracture integrated rehabilitation management on mobility, activity of daily living and cognitive functioning in elderly with hip fracture. Pakistan Journal of Medical Sciences 2020;36(5):965-70. [DOI: 10.12669/pjms.36.5.2412] [DOI] [PMC free article] [PubMed] [Google Scholar]
Beckman 2021 {published data only}
- Beckmann M, Bruun-Olsen V, Pripp AH, Bergland A, Smith T, Heiberg KE. Effect of an additional health-professional-led exercise programme on clinical health outcomes after hip fracture. Physiotherapy Research International 2021;26(2):e1896. [DOI: 10.1002/pri.1896] [DOI] [PubMed] [Google Scholar]
Berggren 2019 {published data only}
- Berggren M, Karlsson Å, Lindelöf N, Englund U, Olofsson B, Nordström P, et al. Effects of geriatric interdisciplinary home rehabilitation on complications and readmissions after hip fracture: a randomized controlled trial. Clinical Rehabilitation 2019;33(1):64-73. [DOI] [PMC free article] [PubMed] [Google Scholar]
Corna 2021 {unpublished data only}
- Corna S, Arcolin I, Giardini M, Bellotti L, Godi M. Addition of aerobic training to conventional rehabilitation after hip fracture: a randomized, controlled, pilot feasibility study [with consumer summary]. Clinical Rehabilitation 2021;35(4):568-77. [DOI] [PubMed] [Google Scholar]
- NCT04025866. The addition of aerobic training to conventional rehabilitation after proximal femur fracture: a randomized controlled trial. clinicaltrials.gov/ct2/show/NCT04025866 (first received 19 July 2019).
Dallimore 2015 {published data only}
- Dallimore KM. Personal communication. Email to: S Dyer 19 May 2017.
- Dallimore RK, Asinas-Tan M, Chan D, Hussain S, Willett C, Zainuldin R. A randomised double-blinded clinical study on the efficacy of multimedia presentation using an iPad for patient education of postoperative hip surgery patients in a public hospital in Singapore. Annals of the Academy of Medicine Singapore: Singapore Health and Biomedical Congress (SHBC); 2015 October 2-3 2015;44(10):S58. [DOI] [PMC free article] [PubMed] [Google Scholar]
Invernizzi 2019 {published data only}
- Invernizzi M, Sire A, D'Andrea F, Carrera D, Reno F, Migliaccio S, et al. Effects of essential amino acid supplementation and rehabilitation on functioning in hip fracture patients: a pilot randomized controlled trial. Aging Clinical and Experimental Research 2019;31(10):1517-24. [DOI] [PubMed] [Google Scholar]
Kalron 2018 {published data only}
- Kalron A, Tawil H, Peleg-Shani S, Vatine JJ. Effect of telerehabilitation on mobility in people after hip surgery: a pilot feasibility study. International Journal of Rehabilitation Research 2018;41(3):244-50. [DOI] [PubMed] [Google Scholar]
Karlsson 2016 {published data only}
- Karlsson Å, Berggren M, Gustafson Y, Olofsson B, Lindelöf N, Stenvall M. Effects of geriatric interdisciplinary home rehabilitation on walking ability and length of hospital stay after hip fracture: a randomized controlled trial. Journal of the American Medical Directors Association 2016;17(5):464 e9-e15. [DOI] [PubMed] [Google Scholar]
- Karlsson A, Lindelof N, Olofsson B, Berggren M, Gustafson Y, Nordstrom P, et al. Effects of geriatric interdisciplinary home rehabilitation on independence in activities of daily living in older people with hip fracture: a randomized controlled trial. Archives of Physical Medicine and Rehabilitation 2020;101:571-8. [DOI] [PubMed] [Google Scholar]
Kim 2020 {published data only}
- Kim P, Lee H, Choi W, Jung S. Effect of 4 weeks of anti-gravity treadmill training on isokinetic muscle strength and muscle activity in adults patients with a femoral fracture: a randomized controlled trial. International Journal of Environmental Research and Public Health 2020;17(22):1-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Lahtinen 2017 {published data only}
- Lahtinen A, Leppilahti J, Vähänikkilä H, Harmainen S, Koistinen P, Rissanen P, et al. Costs after hip fracture in independently living patients: a randomised comparison of three rehabilitation modalities. Clinical Rehabilitation 2017;31(5):672-85. [DOI] [PubMed] [Google Scholar]
Laiz 2017 {published data only}
- Laiz A, Malouf J, Marin A, Longobardi V, Caso J, Farrerons J, et al. Impact of 3-monthly vitamin D supplementation plus exercise on survival after surgery for osteoporotic hip fracture in adult patients over 50 years: a pragmatic randomized, partially blinded, controlled trial. Journal of Nutrition, Health & Aging 2017;21(4):413-20. [DOI] [PubMed] [Google Scholar]
Lehrl 2012 {published data only}
- Lehrl S, Gusinde J, Schulz-Drost S, Rein A, Schlechtweg PM, Jacob H, et al. Advancement of physical process by mental activation: a prospective controlled study. Journal of Rehabilitation Research and Development 2012;49(8):1221-8. [DOI] [PubMed] [Google Scholar]
Pfeiffer 2020 {published data only}
- Pfeiffer K, Kampe K, Klenk J, Rapp K, Kohler M, Albrecht D, et al. Effects of an intervention to reduce fear of falling and increase physical activity during hip and pelvic fracture rehabilitation. Age and Ageing 2020;49(5):771–8. [DOI] [PubMed] [Google Scholar]
Scheffers‐Barnhoorn 2019 {published data only}
- Scheffers-Barnhoorn MN, Van Eijk M, Van Haastregt JC, Schols JM, Van Balen R, Van Geloven N, et al. Effects of the FIT-HIP intervention for fear of falling after hip fracture: a cluster-randomized controlled trial in geriatric rehabilitation. Journal of the American Medical Directors Association 2019;20(7):857-65. [DOI] [PubMed] [Google Scholar]
Taraldsen 2015 {published data only}
- Taraldsen K, Granat MH, Helbostad JL. Quantification of outdoor mobility by use of accelerometer-measured physical behaviour. BioMed Research International 2015;2015:910259. [DOI] [PMC free article] [PubMed] [Google Scholar]
Wang 2020 {published data only}
- Wang K, Fan J, Li X, Yang S, Ren D, He C. Long-term intensive family rehabilitation training for postoperative functional recovery in elderly hip fracture patients. Chinese Journal of Tissue Engineering Research 2020;24(14):2158-63. [Google Scholar]
Wu 2010 {published data only}
- Wu XB, Zhang Q, Song LX, Zhang YZ. Effect of early rehabilitation on the hip joint function in patients with comminuted posterior wall fractures of the acetabulum after internal fixation. Journal of Clinical Rehabilitative Tissue Engineering Research 2010;14(4):732-5. [Google Scholar]
References to studies awaiting assessment
Che 2020 {unpublished data only}
- Che X, Zhang X, Li H, Xu P, Zhao D. Therapeutic effect of early rehabilitation training on the recovery of limb function in elderly patients with femoral neck fracture [Abstract]. Basic and Clinical Pharmacology and Toxicology 2020;127 (Suppl 3):300. [Google Scholar]
Wu XY 2019 {published data only}
- Wu WY, Xu WG. Evaluation of the effect of early total weight-bearing training after cementless total hip arthroplasty. Chinese Journal of Tissue Engineering Research 2019;23(18):2827-32. [Google Scholar]
References to ongoing studies
ACTRN12617001345370 {unpublished data only}
- ACTRN12617001345370. Recumbent bike riding for people with fractured neck of femur: a feasibility trial. www.anzctr.org.au/Trial/Registration/TrialReview.aspx?id=373575 (first received 1 September 2017).
ACTRN12618000903280 {unpublished data only}
- ACTRN12618000903280. The feasibility of prescribing a walking program to improve physical functioning of people living in the community after hip fracture [The feasibility of prescribing a walking program to improve physical functioning of people living in the community after hip fracture: a phase II randomised controlled trial]. anzctr.org.au/Trial/Registration/TrialReview.aspx?ACTRN=12618000903280 (first received 25 May 2018).
Heiberg 2017 {unpublished data only}
- Heiberg KE, Bruun-Olsen V, Bergland A. The effects of habitual functional training on physical functioning in patients after hip fracture: the protocol of the HIPFRAC study. BMC Geriatrics 2017;17(1):23. [DOI] [PMC free article] [PubMed] [Google Scholar]
ISRCTN32476360 {unpublished data only}32476360
- ISRCTN32476360. Effects of transcutaneous electrical nerve stimulation on acute postoperative pain intensity, ambulation and mobility after hip fracture: a double-blinded, randomized trial. www.isrctn.com/ISRCTN32476360 (first received 05 July 2018). [DOI: 10.1186/ISRCTN32476360] [DOI]
jRCTs052190018 {unpublished data only}
- jRCTs052190018. A pilot study of training using the Balance Exercise Assist Robot for the patients after the proximal femoral fractures surgery at the convalescent rehabilitation ward. rctportal.niph.go.jp/en/detail?trial_id=jRCTs052190018 (first received, unknown. date registered 17 May 2019).
jRCTs052190022 {unpublished data only}
- jRCTs052190022. A preliminary study of training using the Balance Exercise Assist Robot for the patients after the proximal femoral fractures surgery at the community-based integrated care ward. rctportal.niph.go.jp/en/detail?trial_id=jRCTs052190022 (first received, unknown. date registered 27 May 2019.
KCT0004122 {unpublished data only}
- KCT0004122. A randomized feasibility study of inpatient rehabilitation using advanced techniques in older people with fragility hip fracture. cris.nih.go.kr/cris/search/detailSearch.do?seq=14311&search_page=L&search_lang=E&lang=E (first received: unknown; approved 17 June 2019).
Lima 2016 {unpublished data only}
- Lima CA, Sherrington C, Guaraldo A, Moraes SA, Varanda RD, Melo J, et al. Effectiveness of a physical exercise intervention program in improving functional mobility in older adults after hip fracture in later stage rehabilitation: protocol of a randomized clinical trial (REATIVE Study). BMC Geriatrics 2016;16(1):198. [DOI] [PMC free article] [PubMed] [Google Scholar]
NCT01129219 {unpublished data only}
- NCT01129219. Observation and progressive strength training after hip fracture. clinicaltrials.gov/ct2/show/NCT01129219 (first received 24 May 2010).
NCT01174589 {unpublished data only}
- NCT01174589. Training of patients with hip fracture. clinicaltrials.gov/show/NCT01174589 (first received 3 August 2010).
NCT02305433 {unpublished data only}
- NCT02305433. Effects of long-term intensive home-based physiotherapy on older people with an operated hip fracture or frailty (RCT) (HIPFRA) [Effects of long-term intensive home-based physiotherapy on older people with an operated hip fracture or frailty (RCT)]. clinicaltrials.gov/ct2/show/NCT02305433 (first received 2 December 2014).
NCT02407444 {unpublished data only}
- NCT02407444. Treatment efficacy of leg cycling as part of physiotherapy treatment in elderly patients with hip fracture [A comparison of two physiotherapy treatment protocols, with and without cycling training, in elderly patients with hip fractures at their subacute stage following surgery]. clinicaltrials.gov/ct2/show/NCT02407444 (first received 3 April 2015).
NCT02815254 {unpublished data only}
- ANCT02815254. The effect of exercise in elderly hip fracture patients: a clinical randomised trial. clinicaltrials.gov/ct2/show/NCT02815254 (first received 28 June 2016).
NCT02938923 {unpublished data only}
- NCT02938923. Starting a testosterone and exercise program after hip injury (STEP-HI) [Combining testosterone therapy and exercise to improve function post hip fracture]. clinicaltrials.gov/ct2/show/NCT02938923 (first received 19 October 2016).
NCT03030092 {unpublished data only}
- NCT03030092. Maximal strength training following hip fracture surgery: impact on muscle mass, balance, walking efficiency and bone density. clinicaltrials.gov/ct2/show/NCT03030092 (first received 24 January 2017).
NCT04095338 {unpublished data only}
- NCT04095338. Assistive robotic in the elderly: innovative models in the rehabilitation of the elderly with hip fractures through technological innovation. clinicaltrials.gov/ct2/show/NCT04095338 (first received 19 September 2019).
NCT04108793 {unpublished data only}
- NCT04108793. Effectiveness of home-based rehabilitation program in minimizing disability and secondary falls after a hip fracture: a randomized controlled trial. clinicaltrials.gov/ct2/show/NCT04108793 (first received 30 September 2019).
NCT04207788 {unpublished data only}
- NCT04207788. HIP fracture rehabilitation programme (HIP-REP) [HIp fracture rehabilitation programme for elderly with hip fracture]. clinicaltrials.gov/ct2/show/NCT04207788 (first received 23 December 2019).
NCT04228068 {unpublished data only}
- NCT04228068. The stronger at home study [A home-based rehabilitation program for patients with hip fracture: a pilot randomized trial]. clinicaltrials.gov/ct2/show/NCT04228068 (first received 14 January 2020).
NTR6794 {unpublished data only}
- NTR6794. Rehabilitation after hip fractures in elderly [COMplex Fracture Orthopedic Rehabilitation (COMFORT) - Real-time visual biofeedback on weight bearing versus standard training methods in the treatment of proximal femur fractures in elderly: a randomized controlled trial]. www.trialregister.nl/trial/6609 (date first received: unclear; date registered 20 October 2017).
UMIN000036379 {unpublished data only}
- UMIN000036379. Randomized controlled trial with parallel design on the effects of maximum voluntary velocity training in patients after femoral neck fracture surgery. upload.umin.ac.jp/cgi-open-bin/ctr_e/ctr_view.cgi?recptno=R000041346 (first received 02 April 2019).
Additional references
Abrami 1964
- Abrami G, Stevens J. Early weight bearing after internal fixation of transcervical fracture of the femur. Preliminary report of a clinical trial. Journal of Bone and Joint Surgery. British Volume 1964;46(2):204-5. [PubMed] [Google Scholar]
Avenell 2010
- Avenell A, Handoll HH. Nutritional supplementation for hip fracture aftercare in older people. Cochrane Database of Systematic Reviews 2010, Issue 1. Art. No: CD001880. [DOI: 10.1002/14651858.CD001880.pub5] [DOI] [PubMed] [Google Scholar]
Avenell 2016
- Avenell A, Smith TO, Curtain JP, Mak JC, Myint PK. Nutritional supplementation for hip fracture aftercare in older people. Cochrane Database of Systematic Reviews 2016, Issue 11. Art. No: CD001880. [DOI: 10.1002/14651858.CD001880.pub6] [DOI] [PMC free article] [PubMed] [Google Scholar]
Bean 2004
- Bean JF, Herman S, Kiely DK, Frey IC, Leveille SG, Fielding RA, et al. Increased velocity exercise specific to task (InVEST) training: a pilot study exploring effects on leg power, balance, and mobility in community-dwelling older women. Journal of the American Geriatrics Society 2004;52(5):799-804. [DOI] [PubMed] [Google Scholar]
Beckmann 2020
- Beckmann M, Bruun-Olsen V, Pripp AH, Bergland A, Smith T, Heiberg KE. Effect of exercise interventions in the early phase to improve physical function after hip fracture – a systematic review and meta-analysis. Physiotherapy 2020;108:90-97. [DOI] [PubMed] [Google Scholar]
Bohannon 2017
- Bohannon RW, Crouch R. Minimal clinically important difference for change in 6-minute walk test distance of adults with pathology: a systematic review. Journal of Evaluation in Clinical Practice 2017;23(2):377-81. [DOI: 10.1111/jep.12629] [DOI] [PubMed] [Google Scholar]
Cameron 2018
- Cameron ID, Dyer SM, Panagoda CE, Murray GR, Hill KD, Cumming RG, et al. Interventions for preventing falls in older people in care facilities and hospitals. Cochrane Database of Systematic Reviews 2018, Issue 9. Art. No: CD005465. [DOI: 10.1002/14651858.CD005465.pub4] [DOI] [PMC free article] [PubMed] [Google Scholar]
Chen 2019
- Chen B, Hu N, Tan J‐H. Efficacy of home‐based exercise programme on physical function after hip fracture: a systematic review and meta‐analysis of randomised controlled trials. International Wound Journal 2019;17(1):45-54. [DOI] [PMC free article] [PubMed] [Google Scholar]
Cochrane Norway 2017
- Cochrane Norway. How to write a plain language summary of a Cochrane intervention review. www.cochrane.no/sites/cochrane.no/files/public/uploads/ checklist for cochrane pls 28th feb 2017 0.pdf (accessed 15 November 2018).
Cohen 1998
- Cohen J. Statistical Power Analysis in the Behavioral Sciences. 2nd edition. Hillsdale (NJ): Lawrence Erlbaum Associates, Inc, 1998. [Google Scholar]
Crotty 2010
- Crotty M, Unroe K, Cameron ID, Miller M, Ramirez G, Couzner L. Rehabilitation interventions for improving physical and psychosocial functioning after hip fracture in older people. Cochrane Database of Systematic Reviews 2010, Issue 1. Art. No: CD007624. [DOI: 10.1002/14651858.CD007624.pub3] [DOI] [PubMed] [Google Scholar]
Curtis 2017
- Curtis EM, Moon RJ, Harvey NC, Cooper C. The impact of fragility fracture and approaches to osteoporosis risk assessment worldwide. Bone 2017;104:29-38. [DOI] [PMC free article] [PubMed] [Google Scholar]
de Morton 2008
- Morton NA, Berlowitz DJ, Keating JL. A systematic review of mobility instruments and their measurement properties for older acute medical patients. Health Quality of Life Outcomes 2008;6(44):[15 p.]. [DOI: 10.1186/1477-7525-6-44] [DOI] [PMC free article] [PubMed] [Google Scholar]
Diong 2016
- Diong J, Allen N, Sherrington C. Structured exercise improves mobility after hip fracture: a meta-analysis with meta-regression. British Journal of Sports Medicine 2016;50:346-55. [DOI] [PubMed] [Google Scholar]
Dreinhofer 2018
- Dreinhöfer KE, Mitchell PJ, Bégué T, Cooper C, Costa ML, Falaschi P, et al. A global call to action to improve the care of people with fragility fractures. Injury 2018;49(8):1393-97. [DOI: 10.1016/j.injury.2018.06.032] [DOI] [PubMed] [Google Scholar]
Dyer 2016
- Dyer S, Crotty M, Fairhall N, Magaziner J, Beaupre LA, Cameron ID, et al. A critical review of the long-term disability outcomes following hip fracture. BMC Geriatrics 2016;16(1):158. [DOI] [PMC free article] [PubMed] [Google Scholar]
Edgren 2012
- Edgren J, Rantanen T, Heinonen A, Portegijs E, Alén M, Kiviranta I, et al. Effects of progressive resistance training on physical disability among older community-dwelling people with history of hip fracture. Aging Clinical and Experimental Research 2012;24(2):171-5. [DOI] [PubMed] [Google Scholar]
Griffin 2015
- Griffin XL, Parsons N, Achten J, Fernandez M, Costa ML. Recovery of health-related quality of life in a United Kingdom hip fracture population. The Warwick Hip Trauma Evaluation--a prospective cohort study. Bone and Joint Journal 2015;97-B(3):372-82. [DOI] [PubMed] [Google Scholar]
Gullberg 1997
- Gullberg B, Johnell O, Kanis JA. World-wide projections for hip fracture. Osteoporosis International 1997;7:407-13. [DOI] [PubMed] [Google Scholar]
Handoll 2009
- Handoll HH, Cameron ID, Mak JC, Finnegan TP. Multidisciplinary rehabilitation for older people with hip fractures. Cochrane Database of Systematic Reviews 2009, Issue 4. Art. No: CD007125. [DOI: 10.1002/14651858.CD007125.pub2] [DOI] [PubMed] [Google Scholar]
Haywood 2014
- Haywood KL, Griffin XL, Achten J, Costa ML. Developing a core outcome set for hip fracture trials. Bone and Joint Journal 2014;26(8):1016-23. [DOI] [PubMed] [Google Scholar]
Higgins 2011
- Higgins JP, Green S (editors). Cochrane Handbook for Systematic Reviews of Interventions. Version 5.1.0 (updated March 2011). The Cochrane Collaboration, 2011. Available from www.handbook.cochrane.org.
Higgins 2021a
- Higgins JP, Li T, Deeks JJ (editors). Chapter 6: Choosing effect measures and computing estimates of effect. In: Higgins JP, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, et al (editors). Cochrane Handbook for Systematic Reviews of Interventions version 6.2 (updated February 2021). Cochrane, 2021. Available from www.training.cochrane.org/handbook.
Higgins 2021b
- Higgins JP, Eldridge S, Li T. Chapter 23: Including variants on randomized trials. In: Higgins JP, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, et al (editors). Cochrane Handbook for Systematic Reviews of Interventions version 6.2 (updated February 2021). Cochrane, 2021. Available from www.training.cochrane.org/handbook.
Host 2007
- Host HH, Sinacore DR, Bohnert KL, Steger-May K, Brown M, Binder EF. Training-induced strength and functional adaptations after hip fracture. Physical Therapy 2007;87(3):292-303. [DOI] [PubMed] [Google Scholar]
Kuijlaars 2019
- Kuijlaars IA, Sweerts L, Nijhuis-van der Sanden MW, Van Balen R, Staal JB, Van Meeteren NL. Effectiveness of supervised home-based exercise therapy compared to a control intervention on functions, activities, and participation in older patients after hip fracture: a systematic review and meta-analysis. Archives Physical Medicine Rehabilitation 2019;100(1):101-14.e6. [DOI] [PubMed] [Google Scholar]
Lamb 2011
- Lamb SE, Becker C, Gillespie LD, Smith JL, Finnegan S, Potter R, et al. Reporting of complex interventions in clinical trials: development of a taxonomy to classify and describe fall-prevention interventions. Trials 2011;12(125):[8 p.]. [DOI: 10.1186/1745-6215-12-125] [DOI] [PMC free article] [PubMed] [Google Scholar]
Lee 2017
- Lee SY, Yoon B-H, Beom J, Ha Y-C, Lim J-Y. Effect of lower-limb progressive resistance exercise after hip fracture surgery: a systematic review and meta-analysis of randomized controlled studies. Journal of the American Medical Directors Association 2017;18(12):1096.e26-1096.e19. [DOI] [PubMed] [Google Scholar]
Lee 2019
- Lee SY, Jung SH, Lee S-U, Ha Y-C, Lim J-Y. Effect of balance training after hip fracture surgery: a systematic review and meta-analysis of randomized controlled studies. Journals of Gerontology. Series A, Biological Sciences and Medical Sciences 2019;74(10):1679-85. [DOI] [PubMed] [Google Scholar]
Lefebvre 2019
- Lefebvre C, Glanville J, Briscoe S, Littlewood A, Marshall C, Metzendorf MI. Chapter 4: Searching for and selecting studies. In: Higgins JP, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, et al (editors). Cochrane Handbook for Systematic Reviews of Interventions version 6.0 (updated July 2019). Cochrane, 2019. Available from www.training.cochrane.org/handbook.
Liu 2009
- Liu CJ, Latham NK. Progressive resistance strength training for improving physical function in older adults. Cochrane Database of Systematic Reviews 2009, Issue 3. Art. No: CD002759. [DOI: 10.1002/14651858.CD002759.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Magaziner 2000
- Magaziner J, Hawkes W, Hebel JR, Zimmerman SI, Fox KM, Dolan M. Recovery from hip fracture in eight areas of function. Journals of Gerontology Series A-Biological Sciences & Medical Sciences 2000;55(9):498-507. [DOI] [PubMed] [Google Scholar]
McDonough 2021
- McDonough CM, Harris-Hayes M, Kristensen MT, Overgaard JA, Herring TB, Kenny AM, et al. Physical therapy management of older adults with hip fracture. Journal of Orthopaedic Sports Physical Therapy 2021;51(2):CPG1-CPG81. [DOI: 10.2519/jospt.2021.0301] [DOI] [PubMed] [Google Scholar]
Parsons 2018
- Parsons N, Griffin XL, Achten J, Chesser TJ, Lamb SE, Costa ML. Modelling and estimation of health-related quality of life after hip fracture. A re-analysis of data from a prospective cohort study. Bone and Joint Research 2018;7(1):1-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
Perera 2006
- Perera S, Mody SH, Woodman RC, Studenski SA. Meaningful change and responsiveness in common physical performance measures in older adults. Journal of the American Geriatrics Society 2006;54(5):743-9. [DOI] [PubMed] [Google Scholar]
Peterson 2004a
- Peterson MG, Ganz SB, Allegrante JP, Cornell CN. High-intensity exercise training following hip fracture. Topics in Geriatric Rehabilitation 2004;20(4):273-84. [Google Scholar]
Resnick 2009
- Resnick B. Self-efficacy. In: SJ Peterson, TS Bredow, editors(s). Middle Range Theories: Application to Nursing Research. 2nd edition. Philadelphia (PA): Lippincott William & Wilkins, 2009. [Google Scholar]
Review Manager 2020 [Computer program]
- Review Manager 5 (RevMan 5). Version 5.4. Copenhagen: Nordic Cochrane Centre, The Cochrane Collaboration, 2020. Available at revman.cochrane.org.
Roche 2005
- Roche JJ, Wenn RT, Sahota O, Moran CG. Effect of comorbidities and postoperative complications on mortality after hip fracture in elderly people: prospective observational cohort study. BMJ 2005;331(7529):1374-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
Royal College of Physicians 2019
- Royal College of Physicians. National Hip Fracture Database annual report 2019. London: RCP, 2019.
Sambunkak 2017
- Sambunjak D, Cumpston M, Watts C. Module 6: Analysing the data. In: Cochrane interactive learning: conducting an intervention review. Cochrane, 2017. Available at training.cochrane.org/interactivelearning/module-6-analysing-data (accessed 17 August 2019).
Sànchez‐Riera 2017
- Sànchez-Riera L, Wilson N. Fragility fractures and their impact on older people. Best Practice & Research. Clinical Rheumatology 2017;31(2):169–91. [DOI] [PubMed] [Google Scholar]
Sawilowsky 2009
- Sawilowsky S. New effect size rules of thumb. Journal of Modern Applied Statistical Methods 2009;8(2):467–74. [Google Scholar]
Schünemann 2017
- Schünemann HJ, Oxman AD, Higgins JP, Vist GE, Glasziou P, Akl E, et al, on behalf of the Cochrane GRADEing Methods Group (formerly Applicability and Recommendations Methods Group) and the Cochrane Statistical Methods Group. Chapter 11: Completing ‘Summary of findings’ tables and grading the confidence in or quality of the evidence. In: Higgins JP, Churchill R, Chandler J, Cumpston MS (editors), Cochrane Handbook for Systematic Reviews of Interventions version 5.2.0 (updated June 2017). Cochrane, 2017. Available from www.training.cochrane.org/handbook.
Schünemann 2022
- Schünemann HJ, Vist GE, Higgins JP, Santesso N, Deeks JJ, Glasziou P, et al. Chapter 15: Interpreting results and drawing conclusions. In: Higgins JP, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, et al (editors). Cochrane Handbook for Systematic Reviews of Interventions version 6.3 (updated February 2022). Cochrane, 2022. Available from handbook.cochrane.org.
Sherrington 2019
- Sherrington C, Fairhall NJ, Wallbank GK, Tiedemann A, Michaleff ZA, Howard K, et al. Exercise for preventing falls in older people living in the community. Cochrane Database of Systematic Reviews 2019, Issue 1. Art. No: CD012424. [DOI: 10.1002/14651858.CD012424.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Singh 2012
- Singh NA, Quine S, Clemson LM, Williams EJ, Williamson DA, Stavrinos TM, et al. Effects of high-intensity progressive resistance training and targeted multidisciplinary treatment of frailty on mortality and nursing home admissions after hip fracture: a randomized controlled trial. Journal of the American Medical Directors Association 2012;13(1):24-30. [DOI] [PubMed] [Google Scholar]
Smith 2019
- Smith TO, Collier T, Sheehan KJ, Sherrington C. The uptake of the hip fracture core outcome set: analysis of 20 years of hip fracture trials. Age and Ageing 2019;48(4):595-8. [DOI] [PubMed] [Google Scholar]
Smith 2020
- Smith TO, Gilbert AW, Sreekanta A, Sahota O, Griffin XL, Cross JL, et al. Enhanced rehabilitation and care models for adults with dementia following hip fracture surgery. Cochrane Database of Systematic Reviews 2020, Issue 2. Art. No: CD010569. [DOI: 10.1002/14651858.CD010569.pub3] [DOI] [PMC free article] [PubMed] [Google Scholar]
Sun 2010
- Sun X. Is a subgroup effect believable? Updating criteria to evaluate the credibility of subgroup analyses. British Medical Journal 2010;340:c117. [DOI] [PubMed] [Google Scholar]
Unnanuntana 2018
- Unnanuntana A, Jarusriwanna A, Nepal S. Validity and responsiveness of Barthel index for measuring functional recovery after hemiarthroplasty for femoral neck fracture. Archives of Orthopaedic Trauma Surgery 2018;138(12):1671-7. [DOI: 10.1007/s00402-018-3020-z] [DOI] [PubMed] [Google Scholar]
Veronese 2018
- Veronese N, Maggai S. Epidemiology and social costs of hip fracture. Injury 2018;49(8):1458-60. [DOI] [PubMed] [Google Scholar]
Walters 2003
- Walters SJ, Brazier JE. What is the relationship between the minimally important difference and health state utility values? The case of the SF-6D. Health and Quality of Life Outcomes 2003;1(4):[8 p.]. [DOI: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Walters 2005
- Walters SJ, Brazier JE. Comparison of the minimally important difference for two health state utility measures: EQ-5D and SF-6D. Quality of Life Research 2005;14(6):1523–32. [DOI] [PubMed] [Google Scholar]
Webber 2010
- SC Webber, MM Porter, VH Menec. Mobility in older adults: a comprehensive framework. Gerontologist 2010;50(4):443–50. [DOI: 10.1093/geront/gnq013] [DOI] [PubMed] [Google Scholar]
Wu J 2019
- Wu J, Mao L, Wu J. Efficacy of balance training for hip fracture patients: a meta-analysis of randomized controlled trials. Journal of Orthopaedic Surgery and Research 2019;14(1):83. [DOI] [PMC free article] [PubMed] [Google Scholar]
Zidén 2008
- Zidén L, Frandin K, Kreuter M. Home rehabilitation after hip fracture. A randomized controlled study on balance confidence, physical function and everyday activities. Clinical Rehabilitation 2008;22(12):1019-33. [DOI] [PubMed] [Google Scholar]
References to other published versions of this review
Handoll 2003
- Handoll HH, Parker MJ, Sherrington C. Mobilisation strategies after hip fracture surgery in adults. Cochrane Database of Systematic Reviews 2003, Issue 1. Art. No: CD001704. [DOI: 10.1002/14651858.CD001704] [DOI] [PubMed] [Google Scholar]
Handoll 2004
- Handoll HH, Sherrington C, Parker MJ. Mobilisation strategies after hip fracture surgery in adults. Cochrane Database of Systematic Reviews 2004, Issue 4. Art. No: CD001704. [DOI: 10.1002/14651858.CD001704.pub2] [DOI] [PubMed] [Google Scholar]
Handoll 2007
- Handoll HH, Sherrington C. Mobilisation strategies after hip fracture surgery in adults. Cochrane Database of Systematic Reviews 2007, Issue 1. Art. No: CD001704. [DOI: 10.1002/14651858.CD001704.pub3] [DOI] [PubMed] [Google Scholar]
Handoll 2011
- Handoll HH, Sherrington C, Mak JC. Interventions for improving mobility after hip fracture surgery in adults. Cochrane Database of Systematic Reviews 2011, Issue 3. Art. No: CD001704. [DOI: 10.1002/14651858.CD001704.pub4] [DOI] [PubMed] [Google Scholar]
Parker 1999
- Parker MJ. Early weight bearing and mobilisation after internal fixation of intracapsular proximal femoral fractures in adults. Cochrane Database of Systematic Reviews 1999, Issue 3. Art. No: CD001704. [DOI: 10.1002/14651858.CD001704] [DOI] [Google Scholar]


