Abstract
BACKGROUND
Reducing congenital syphilis has been the focus of Brazilian health programs for decades, yet the cases continue to increase. Although health interventions have targeted HIV screening and treatment, syphilis management continues to be challenging. Syphilis during pregnancy may enhance the HIV maternal seroconversion risk. The potential factors fueling the syphilis epidemic were evaluated in south Brazil, an area of high HIV or syphilis endemicity.
OBJECTIVE
We hypothesized that ineffective treatment because of a lack of partner treatment, late presentation to care, and reinfection of previously treated mothers were potential drivers of syphilis mother-to-child transmission.
STUDY DESIGN
Data on women diagnosed with syphilis during pregnancy between January 1, 2008 and December 31, 2018 were obtained from a large urban hospital in Porto Alegre, Brazil. The patients were stratified into effective vs ineffective treatment groups according to the World Health Organization guidelines. Crude and adjusted risk ratios for the prediction of congenital syphilis and adverse fetal or neonatal outcomes were computed using Poisson regression.
RESULTS
Nearly 56,000 pregnant women delivered over the 11-year period; 1541 (2.8%) had confirmed syphilis during pregnancy, with 934 (61%) receiving ineffective syphilis treatment because of late presentation and diagnosis, delayed treatment initiation, and loss to follow-up with no treatment recorded. Ineffective treatment was associated with maternal education, prenatal care, timing of syphilis diagnosis, venereal diseases research laboratory titers, and maternal HIV coinfection. On multivariate regression analysis, ineffective treatment (adjusted risk ratio, 4.52; 95% confidence interval, 2.35–8.69), absence of prenatal care (adjusted risk ratio, 9.31; 95% confidence interval, 3.77–23.0), syphilis diagnosis at delivery (adjusted risk ratio, 3.08; 95% confidence interval, 2.07–4.58), and maternal nontreponemal titers ≥1:64 (1.09–1.93) were associated with an increased risk of fetal loss. Ineffective treatment (adjusted risk ratio, 1.71; 95% confidence interval, 1.59–1.84), year of diagnosis 2014 to 2016 (adjusted risk ratio, 1.07; 95% confidence interval, 1.02–1.13), absence of prenatal care (adjusted risk ratio, 1.44; 95% confidence interval, 1.17–1.76), and maternal nontreponemal titers >1:4 were associated with an increased risk of congenital syphilis. Although partner treatment reduced the congenital syphilis risk (adjusted risk ratio, 0.60; 95% confidence interval, 0.55–0.66), only 31.8% of partners received treatment. Maternal HIV coinfection was not associated with an increased risk of fetal loss, low birthweight, preterm birth, congenital syphilis, or symptomatic neonatal infection.
CONCLUSION
Public health initiatives promoting effective syphilis treatment in pregnancy, increased access to high-quality prenatal care, and partner treatment should be considered to reduce congenital syphilis.
Key words: Brazil, HIV, ineffective treatment, mother-to-child transmission, partner treatment, pregnancy, prenatal care, public health, syphilis
AJOG Global Reports at a Glance.
Why was this study conducted?
To identify the parameters associated with the mother-to-child transmission (MTCT) of syphilis in pregnant women at a large medical network in Porto Alegre, Brazil.
Key findings
61% of women diagnosed with maternal syphilis between 2008 and 2018 received ineffective syphilis treatment. Ineffective treatment (adjusted risk ratio [ARR], 1.71; 95% confidence interval [CI], 1.59–1.84) and absence of prenatal care (ARR, 1.44; 95% CI, 1.17–1.76) were associated with an increased risk of congenital syphilis. Partner treatment reduced the risk of congenital syphilis (ARR, 0.60; 95% CI, 0.55–0.66).
What does this add to what is known?
A significant proportion of pregnant mothers with syphilis do not receive effective treatment, placing them at an increased risk of syphilis MTCT in the future.
Introduction
Attempts to control the mother-to-child transmission (MTCT) syphilis epidemic in Brazil has been fraught with challenges. The rates of maternal syphilis increased 5-fold in the country in the past decade despite clear testing guidelines in place and treatment availability.1 The incidence of congenital syphilis in 10 Brazilian states surpassed the national rate in 2019 at 8.2 per 1000 live births.1, 2, 3 Porto Alegre, the capital of the state of Rio Grande do Sul, stands out as a high-prevalence region for syphilis and HIV.1 In our previous work, we found an increase in cumulative maternal syphilis diagnoses in Brazil from 2010 to 20184; 8704 cases of maternal syphilis were identified in 2010 compared with 46,340 cases in 2018.4 Furthermore, yearly increases in syphilis among pregnant women occurred despite high rates of engagement in prenatal care, whereas 8.7% of maternal syphilis cases diagnosed from 2010 to 2018 in Brazil were not treated appropriately with penicillin.4
The growing syphilis epidemic in Brazil poses a threat to the control of the spread of HIV infection. Members of high-risk populations with syphilis exposure demonstrated a 2-fold increase in HIV incidence than those without syphilis.5 Although the care of persons living with HIV has been an area of enhanced focus in Brazil, aims to successfully reduce syphilis have not gained the same traction.6 The discrepancy between syphilis monitoring and HIV monitoring has also been observed in the prenatal care of pregnant women. Healthcare professionals in São Paulo, Brazil reported that the standard routines for screening and treating HIV-infected pregnant women and infants are better-established and more utilized than those for patients infected with syphilis.7 Further, patient follow-up was significantly higher for pregnant women with HIV than for those with syphilis.7 Women diagnosed with syphilis during pregnancy represent a subset of the population that is vulnerable to HIV seroconversion in the future.8,9
Current Brazilian Ministry of Health guidelines for syphilis management during pregnancy recommend routine screening at the initiation of prenatal care, week 28, and delivery.10,11 Complete maternal syphilis treatment is defined as penicillin therapy more than 30 days before delivery.11 The treatment is highly effective at reducing MTCT of syphilis, and safety to the fetus is well-established.2 Maternal syphilis can lead to fetal death, preterm birth, low birthweight infants, and higher risks of maternal HIV seroconversion and HIV transmission to the infant. It remains unclear why the maternal and congenital syphilis epidemic persists in Brazil when there are testing guidelines in place and accessible treatment.12
We hypothesized that ineffective treatment because of a lack of partner treatment, late presentation to care, and reinfection of previously treated mothers were potential drivers of syphilis MTCT transmission.
Materials and Methods
Study population and data sources
This was a retrospective cohort study of women diagnosed with syphilis during pregnancy. All the participants reached a pregnancy endpoint (delivery or miscarriage) at the Conceição Hospital in Porto Alegre, Brazil, between January 1, 2008 and December 31, 2018. The Conceição Hospital is part of the Grupo Hospitalar Conceição—a public tertiary medical care network including 4 hospitals and a group of ambulatory clinics in Brazil—in the same city. Anonymous syphilis pregnancy surveillance data reported to the Brazilian “Sistema de Informação de Agravos de Notificação” (SINAN) by the Conceição Hospital Network was evaluated.
Ethics
We received institutional board review (IRB) approval (IRB protocol 14.124) from the Conceição Hospital in Porto Alegre, Brazil. Obtaining written informed consent was waived because this was a secondary data analysis of deidentified data.
Selection criteria
Maternal syphilis was diagnosed by positive nontreponemal venereal diseases research laboratory (VDRL) results followed by confirmation with an antitreponemal assay such as treponemal pallidum particle agglutination assay or enzyme-linked immunosorbent assay, both routinely used in Brazil. Women with a positive VDRL result during pregnancy and unknown treponemal confirmatory test results were included in the analysis if the titers were >1:4. Titers <1:8 were not considered diagnostic for syphilis if the confirmatory test result was unknown13,14; titers <1:8 have been associated with serologic cure.15,16 False positive VDRL results can present as low titers such as 1:1, 1:2, or even 1:4 during pregnancy or in patients with autoimmune diseases.17
Exposure and outcomes
The patients were stratified into syphilis-positive pregnant women treated effectively and syphilis-positive pregnant women treated ineffectively. World Health Organization (WHO) guidelines including the following were used for establishing effective treatment: (1) adequate penicillin treatment provided >30 days before delivery, (2) demonstration of lower syphilis titers after treatment, and (3) use of 2.4 million units of 1-time intramuscular benzathine penicillin G (BPG) (for primary, secondary, or early latent stage disease) or weekly for 3 consecutive weeks (for late or unknown stage disease). Penicillin desensitization is recommended even in the event of penicillin allergy.2
The primary outcome was congenital syphilis infection, whereas the secondary outcomes were clinical findings consistent with congenital syphilis in exposed newborns and adverse fetal and neonatal outcomes, including low infant birthweight (≤2500 g), preterm birth (<37 weeks), and fetal loss. Infected newborns were categorized as symptomatic if they displayed any of the following characteristics identified by the Centers for Disease Control and Prevention: deformed bones, severe anemia (low blood count), enlarged liver and spleen, jaundice, brain and nerve problems (blindness or deafness), meningitis, or skin rashes.18 We examined the adverse outcome differences in pregnant women with partners that were treated vs partners that had unknown or no treatment. Our evaluation of the predictors of congenital syphilis is outlined in the supplemental appendix.
Data management and statistical analysis
Data were abstracted from the Grupo Hospitalar Conceição SINAN reporting database, which was originally abstracted from medical records for SINAN reporting purposes. The exclusion criteria are noted in the supplemental appendix.
The continuous baseline characteristics were reported as median values and interquartile range (IQR) and were compared with the Welch t test. The categorical variables were reported as a frequency. The relative risk and corresponding 95% confidence intervals (CIs) were generated for potential risk parameters for women who received effective and ineffective syphilis treatment. We conducted an adjusted multivariate Poisson regression for each dichotomous outcome using treatment effectiveness as the main regressor and did a backward removal of covariates found to have a P value <.20 in the crude regression stage of the analysis. Using the Baron and Kenny test, we identified treatment effectiveness and prenatal care as interaction variables. Statistical analysis was performed using Stata statistical software (version 16; StataCorp LLC, College Station, TX), and all statistical significance tests relied on a 2-sided α <0.05.
Results
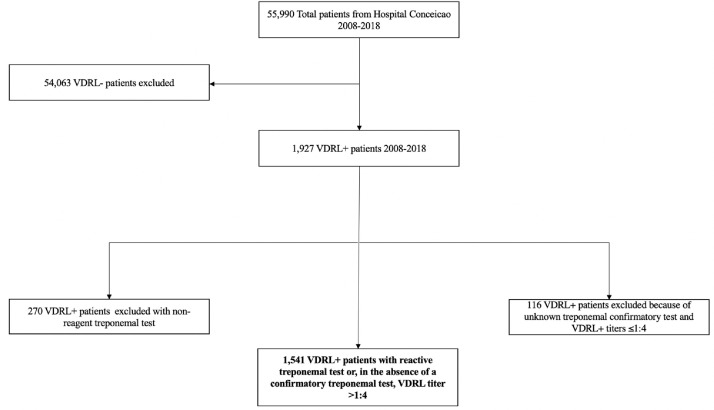
Over 11 years, 55,990 pregnant women delivered at the Conceição Hospital, of which 96.6% had a negative VDRL titer (Figure 1). Among 1927 participants with a positive VDRL result, 270 (14%) had negative treponemal test results. 116 (6%) participants with no confirmatory treponemal test results available and VDRL titers <1:8 were excluded from further analysis. The remaining study population consisted of 1541 pregnancies with both positive VDRL and treponemal antibody assay results (n=1446) and pregnancies with a positive VDRL titer of >1:4 without a confirmatory treponemal test result (n=95) (Figure 1).
Figure 1.
Pregnant participant selection flowchart
VDRL, venereal diseases research laboratory.
Swayze. Ineffective treatment and syphilis mother-to-child transmission. Am J Obstet Gynecol Glob Rep 2022.
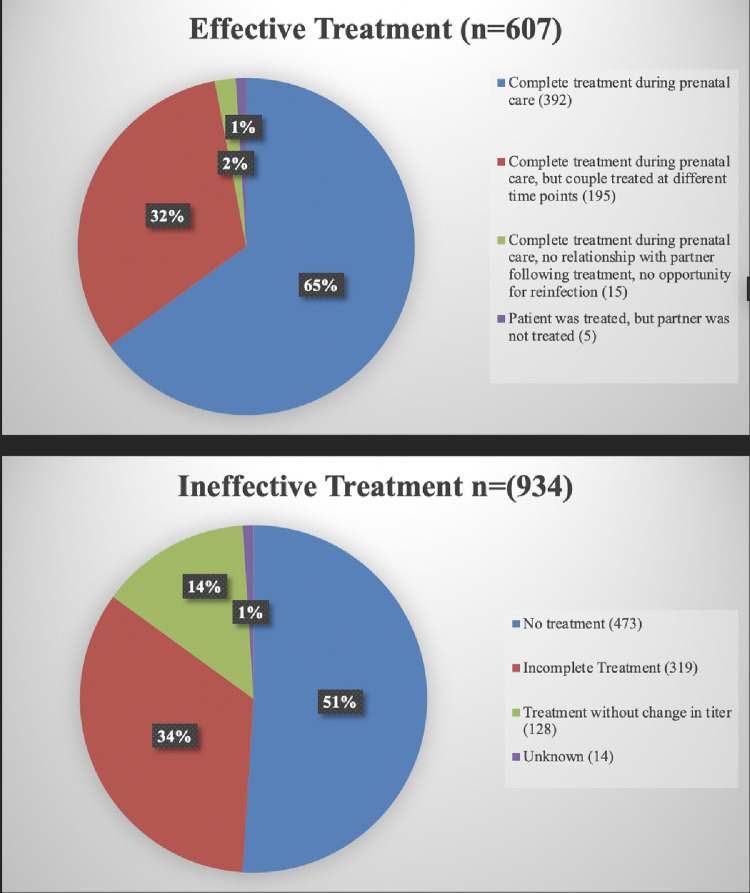
Among 1541 pregnant women diagnosed with maternal syphilis between 2008 and 2018 at Hospital Conceição, 934 (61%) received ineffective syphilis treatment (Figure 2). Total 792 (85%) women in the ineffective syphilis treatment category were either not treated while pregnant or had treatment initiated within 30 days of delivery because of a late diagnosis. An additional 128 (14%) women were treated, but VDRL titers did not decline or increased post treatment. Less than 1% of the women had a syphilis diagnosis during previous pregnancies but no evidence of treatment in the current pregnancy. For 1% of the cohort, there was no record of syphilis treatment.
Figure 2.
Breakdown of ineffective and effective treatment cohorts by maternal treatment status
VDRL, venereal diseases research laboratory.
Swayze. Ineffective treatment and syphilis mother-to-child transmission. Am J Obstet Gynecol Glob Rep 2022.
Table 1 shows the demographics and pregnancy characteristics of the study population stratified by effective vs ineffective treatment. The median age of the study population was 24 (IQR, 20–29), and no significant differences were found between race distributions in the 2 groups. Most of the study population (62.5%) self-identified as White, followed by 25.1% as Black and 12.1% as Mixed, Indigenous, Asian, or other. The educational level differed between the groups; 52.2% of women with ineffective treatment did not have secondary education compared with 39.9% of women with effective treatment (P<.01). A higher frequency of prenatal care (at least 1 visit) was observed in the women who received effective syphilis treatment (97.2% vs 69.1%, P<.01). Only 54.4% of partners received treatment in the effective treatment cohort; it was significantly higher than the 17.1% of partners treated in the ineffective treatment group (P<.01). A greater percentage of women with ineffective treatment were diagnosed at delivery and had elevated VDRL titers than those with effective treatment (P<.01). A higher proportion of women had HIV coinfection in the ineffective treatment group as opposed to the effectively treated population (13.1% vs 5.9%, respectively, P<.01). The distribution of treatment groups also differed by year of diagnosis (P<.01): 6.9% of women received effective treatment and 17.2% did not between 2008 and 2010, compared with 35.6% of women who received effective treatment and 19.3% who did not between 2017 and 2018.
Table 1.
Baseline demographic and pregnancy characteristics of women diagnosed with maternal syphilis in Porto Alegre, Brazil, 2008 to 2018
| Demographic and pregnancy characteristics | Effective treatment | Ineffective treatment | P value |
|---|---|---|---|
| N=1541 | N (%) | N (%) | |
| Group total | 607 (39) | 934 (61) | |
| Age median (IQR) | 24.0 (20.0–28.0) | 24.0 (20.0–30) | .09 |
| Age | |||
| <20 | 121 (19.9) | 186 (19.9) | .03 |
| 20–29 | 367 (60.5) | 512 (54.8) | |
| ≥30 | 119 (19.6) | 236 (25.3) | |
| Self-identified race | |||
| White | 378 (62.3) | 585 (62.6) | .34 |
| Black | 155 (25.5) | 232 (24.8) | |
| Mixed, Indigenous, Asian, Other | 74 (12.2) | 112 (12.0) | |
| Unknown | 0 (0) | 5 (0.5) | |
| Education | |||
| Primary | 242 (39.9) | 488 (52.2) | <.01 |
| Secondary | 220 (36.2) | 283 (30.3) | |
| High school or higher | 142 (23.4) | 157 (16.8) | |
| Unknown | 3 (0.5) | 6 (0.6) | |
| Year of diagnosis | |||
| 2008–2010 | 42 (6.9) | 161 (17.2) | <.01 |
| 2011–2013 | 114 (18.8) | 259 (27.7) | |
| 2014–2016 | 235 (38.7) | 334 (35.8) | |
| 2017–2018 | 216 (35.6) | 180 (19.3) | |
| Number of gestations | |||
| 1 Gestation | 218 (35.9) | 240 (25.7) | <.01 |
| 2–4 Gestations | 319 (52.6) | 514 (55.0) | |
| ≥5 Gestations | 70 (11.5) | 180 (19.3) | |
| Prenatal care | |||
| Received care | 590 (97.2) | 645 (69.1) | <.01 |
| Did not receive care | 17 (2.8) | 281 (30.1) | |
| Unknown | 0 (0) | 8 (0.9) | |
| Partner treatment | |||
| Received treatment | 330 (54.4) | 160 (17.1) | <.01 |
| Did not receive treatment | 239 (39.4) | 649 (69.5) | |
| Unknown | 38 (6.3) | 125 (13.4) | |
| Timing of syphilis Diagnosis | |||
| Prenatal care | 564 (92.9) | 479 (51.3) | <.01 |
| During delivery | 37 (6.1) | 440 (47.1) | |
| After delivery | 1 (0.2) | 2 (0.2) | |
| Unknown | 5 (0.8) | 13 (1.4) | |
| Syphilis titers | |||
| <1:8 | 446 (73.5) | 390 (41.8) | <.01 |
| 1:8–1:32 | 150 (24.7) | 387 (41.5) | |
| ≥1:64 | 11 (1.8) | 154 (16.5) | |
| Unknown | 0 (0.0) | 3 (0.2) | |
| Maternal HIV status | |||
| HIV+ | 36 (5.9) | 122 (13.1) | <.01 |
| HIV− | 570 (93.9) | 811 (86.8) | |
| HIV unknown | 1 (0.2) | 1 (0.1) |
IQR, interquartile range.
Swayze. Ineffective treatment and syphilis mother-to-child transmission. Am J Obstet Gynecol Glob Rep 2022.
Table 2 evaluates the adverse outcomes among the effective and ineffective treatment groups. Of note, 165 (72.4%) of the fetal losses reported for the ineffective treatment group were attributed to women who received no penicillin treatment before admission for miscarriage. These were generally women who presented to the hospital because of an ongoing miscarriage and were found to be VDRL positive on admission. Overall, 98.1% of the women with ineffective treatment transmitted congenital syphilis, compared with 49.8% of women with effective treatment. Significantly higher rates of fetal loss, congenital syphilis diagnoses, low birthweight, and preterm deliveries were reported in the group of women with ineffective treatment.
Table 2.
Adverse maternal and fetal outcomes in women diagnosed with syphilis during pregnancy in Porto Alegre, Brazil by maternal syphilis treatment status
| Adverse maternal and fetal outcomes | Effective treatment | Ineffective treatment | P value |
|---|---|---|---|
| N=1541 | N (%) | N (%) | |
| Group total | 607 (39) | 934 (61) | <.01 |
| Fetal birth outcome | |||
| Fetal loss at any time during pregnancy | 18 (3.0) | 228 (24.4) | <.01 |
| Live fetus | 589 (97.0) | 706 (75.6) | |
| Congenital syphilis | |||
| Yes | 302 (49.8) | 916 (98.1) | <.01 |
| No | 305 (50.2) | 18 (1.9) | |
| Symptomatic newborn | |||
| Yes | 31 (5.1) | 59 (6.3) | .55 |
| No | 566 (93.3) | 854 (91.4) | |
| Unknown | 10 (1.6) | 21 (2.3) | |
| Fetal birthweight | |||
| ≤2500 g | 67 (11.3) | 205 (26.0) | <.01 |
| >2500 g | 528 (88.7) | 582 (74.0) | |
| Not included abortions | 12 | 147 | |
| Term of birth | |||
| Preterm birth <37 wk | 57 (9.6) | 194 (24.6) | <.01 |
| Term ≥37 wk | 538 (90.4) | 590 (75.0) | |
| Unknown | 0 (0) | 3 (0.4) | |
| Not included abortions | 12 | 147 |
Swayze. Ineffective treatment and syphilis mother-to-child transmission. Am J Obstet Gynecol Glob Rep 2022.
Table 3 explores the same adverse outcomes in women that had treated partners vs women with partners that had no or unknown treatment status. Overall, only 31.8% of women reported treated partners. 47.8% of women with treated partners transmitted congenital syphilis compared with 93.6% of women with partners that had no or unknown treatment (P<.01). Women with treated partners were significantly less likely to experience any adverse fetal or neonatal outcomes than those who had partners with no or unknown treatment (P<.01).
Table 3.
Adverse maternal and fetal outcomes in women diagnosed with syphilis during pregnancy in Porto Alegre, Brazil by partner syphilis treatment status
| Adverse maternal and fetal outcomes | Partner treatment | No/Unknown Partner Treatment | P value |
|---|---|---|---|
| N=1541 | N (%) | N (%) | |
| Group total | 490 (31.8) | 1051 (68.2) | |
| Fetal birth outcome | |||
| Fetal loss at any time during pregnancy | 21 (4.3) | 225 (21.4) | <.01 |
| Live fetus | 469 (95.7) | 826 (78.6) | |
| Congenital syphilis | |||
| Yes | 234 (47.8) | 984 (93.6) | <.01 |
| No | 256 (52.2) | 67 (6.4) | |
| Symptomatic newborn | |||
| Yes | 13 (2.7) | 77 (7.4) | <.01 |
| No | 469 (96.5) | 951 (91.1) | |
| Unknown | 4 (0.8) | 16 (1.5) | |
| Fetal birthweight | |||
| ≤2500 g | 51 (10.7) | 221 (24.4) | <.01 |
| >2500 g | 424 (89.3) | 686 (75.6) | |
| Not included abortions | 15 | 144 | |
| Term of birth | |||
| Preterm birth <37 wk | 51 (10.7) | 200 (22.0) | <.01 |
| Term ≥37 wk | 424 (89.3) | 704 (77.7) | |
| Unknown | 0 (0) | 3 (0.3) | |
| Not included abortions | 15 | 144 |
Swayze. Ineffective treatment and syphilis mother-to-child transmission. Am J Obstet Gynecol Glob Rep 2022.
The predictors of adverse outcomes in women with syphilis in Brazil over an 11-year span are shown in Supplemental Table 1 (unadjusted multivariate analysis) and Table 4, which shows the adjusted multivariate analysis of predictors of fetal death, low birthweight, preterm birth, congenital syphilis, and symptomatic newborns. Ineffective treatment (adjusted risk ratio [ARR], 4.52; 95% CI, 2.35–8.69), absence of prenatal care (ARR, 9.31; 95% CI, 3.77–23.0), syphilis diagnosis at delivery (ARR, 3.08; 95% CI, 2.07–4.58), and VDRL titers ≥1:64 (ARR, 1.45; 95% CI, 1.09–1.93) were predictors of fetal loss at any time during pregnancy. Women with ineffective syphilis treatment (ARR, 1.42; 95% CI, 1.05–1.92) and higher syphilis titers ≥1:64 (ARR, 2.92; 95% CI, 2.21–3.87) were at an increased risk of delivering a low birthweight infant. In contrast, women with higher education were at a reduced risk of having a low birthweight infant (ARR, 0.70; 95% CI, 0.51–0.96). Ineffective syphilis treatment (ARR, 1.70; 95% CI, 1.22–2.38) and syphilis titers ≥1:64 (ARR, 3.13; 95% CI, 2.36–4.15) were predictors of preterm birth.
Table 4.
Adjusteda multivariate analysis of predictors of adverse maternal and fetal outcomes in pregnant women with syphilis in Porto Alegre, Brazil, 2008 to 2018
| Predictors of adverse maternal and fetal outcomes | Fetal loss at any time during pregnancy (N=246) | Low birthweight (N=272) | Preterm birth (N=251) | Congenital syphilis (N=1,218) | Symptomatic newborn (N=90) |
|---|---|---|---|---|---|
| ARR (95% confidence interval) | |||||
| Syphilis treatment | |||||
| Effective | ref | ref | ref | ref | ref |
| Ineffective | 4.52 (2.35–8.69) | 1.42 (1.05–1.92) | 1.70 (1.22–2.38) | 1.71 (1.59–1.84) | 0.91 (0.55–1.53) |
| Age | |||||
| <20 | ref | ref | ref | ref | ref |
| 20–29 | 0.92 (0.71–1.20) | 0.97 (0.73–1.29) | 0.77 (0.60–1.00) | 1.08 (1.02–1.15) | 0.93 (0.54–1.60) |
| ≥30 | 0.94 (0.70–1.27) | 1.22 (0.85–1.75) | 1.07 (0.80–1.44) | 1.12 (1.04–1.21) | 0.55 (0.25–1.19) |
| Self-identified race | |||||
| White | ref | ref | ref | ref | ref |
| Black | 1.11 (0.88–1.40) | ||||
| Mixed, Indigenous, Asian, Other | 1.12 (0.81–1.53) | ||||
| Education | |||||
| Primary | ref | ref | ref | ref | ref |
| Secondary | 0.70 (0.51–0.96) | 1.06 (1.00–1.12) | 1.09 (0.58–2.04) | ||
| High school or higher | 0.78 (0.55–1.10) | 1.02 (0.96–1.09) | 1.79 (1.01–3.18) | ||
| Year of diagnosis | |||||
| 2008–2010 | ref | ref | ref | ref | ref |
| 2011–2013 | 0.96 (0.70–1.32) | 0.83 (0.60–1.15) | 0.97 (0.92–1.02) | 1.06 (0.49–2.27) | |
| 2014–2016 | 1.05 (0.77 –1.44) | 0.86 (0.63–1.17) | 1.07 (1.02–1.13) | 1.30 (0.62–2.74) | |
| 2017–2018 | 1.50 (1.01–2.24) | 1.06 (0.76–1.49) | 0.86 (0.79–0.93) | 2.57 (1.14–5.79) | |
| Number of gestations | |||||
| 1 gestation | ref | ref | ref | ref | ref |
| 2–4 gestations | 0.98 (0.76–1.27) | 0.93 (0.88–0.98) | 0.80 (0.49–1.31) | ||
| ≥5 gestations | 1.00 (0.69–1.44) | 0.89 (0.83–0.95) | 1.38 (0.68–2.81) | ||
| Prenatal care | |||||
| Yes | ref | ref | ref | ref | ref |
| No | 9.31 (3.77–23.0) | 2.30 (0.82–6.41) | 2.65 (0.59–12.0) | 1.44 (1.17–1.76) | |
| Partner treatment | |||||
| No | ref | ref | ref | ref | ref |
| Yes | 0.85 (0.54–1.36) | 0.76 (0.55–1.04) | 0.91 (0.66–1.26) | 0.60 (0.55–0.65) | 0.48 (0.27–0.86) |
| Time of syphilis diagnosis | |||||
| Prenatal care | ref | ref | ref | ref | ref |
| During delivery | 3.08 (2.07–4.58) | 1.06 (0.79–1.42) | 1.09 (0.32–3.73) | 0.93 (0.88–0.97) | 1.43 (0.90–2.26) |
| Syphilis titers | |||||
| <1:8 | ref | ref | ref | ref | ref |
| 1:8–1:32 | 1.26 (0.99–1.60) | 1.30 (1.00–1.70) | 1.25 (0.95–1.64) | 1.17 (1.12–1.22) | 1.27 (0.81–1.97) |
| ≥1:64 | 1.45 (1.09–1.93) | 2.92 (2.21–3.87) | 3.13 (2.36–4.15) | 1.11 (1.06–1.16) | 2.04 (1.24–3.37) |
| Maternal HIV | |||||
| No | ref | ref | ref | ref | ref |
| Yes | 0.91 (0.67–1.22) | 0.93 (0.67–1.29) | 0.99 (0.94–1.05) | ||
| Interaction variable | |||||
| No prenatal care and ineffective treatment | 0.18 (0.07–0.43) | 0.65 (0.3–1.81) | 0.47 (0.10–2.20) | 0.65 (0.53–0.80) | 0.54 (0.12–2.41) |
ARR, adjusted risk ratio; ref, reference group.
Covariates were established for each outcome using predictors that yielded a P value of <.20 in the crude analysis shown in Supplemental Table 1.
Swayze. Ineffective treatment and syphilis mother-to-child transmission. Am J Obstet Gynecol Glob Rep 2022.
Women with ineffective syphilis treatment had an increased risk of transmitting congenital syphilis (ARR, 1.71; 95% CI, 1.59–1.84) than effectively treated women. Women older than 20 (ARR, 1.08; 95% CI, 1.02–1.15), those diagnosed between 2014 and 2016 (ARR, 1.07; 95% CI, 1.02–1.13), those without prenatal care (ARR, 1.44; 95% CI, 1.17–1.76), and those with syphilis titers >1:4 (ARR, 1.17; 95% CI, 1.12–1.22) were at an increased risk of delivering a baby with congenital syphilis. Alternatively, women with treated partners (ARR, 0.60; 95% CI, 0.55–0.65) and women diagnosed between 2017 and 2018 (ARR, 0.86; 95% CI, 0.79–0.93) had a reduced risk of MTCT syphilis. Higher education (ARR, 1.79; 95% CI, 1.01–3.18), diagnosis between 2017 and 2018 (ARR, 2.57; 95% CI, 1.14–5.79), and titers ≥1:64 (ARR, 2.04; 95% CI, 1.24–3.37) were associated with higher chances of having a symptomatic newborn. Partner treatment (ARR, 0.48; 95% CI, 0.27–0.86) led to reduced risk of a symptomatic newborn.
One hundred fifty eight (10.3%) women with a syphilis diagnosis had a concurrent diagnosis of HIV. One hundred twenty two (13.1%) women with HIV and syphilis were more likely to have ineffective penicillin treatment (which includes 77% of the women with HIV, P<.01). However, maternal HIV coinfection was not associated with increased risk of fetal loss, low birthweight, preterm birth, congenital syphilis, or symptomatic neonatal infection (Table 3).
Comment
Principal findings
Despite strict adherence to WHO guidelines at this hospital in southern Brazil, only 39% of the 1541 pregnant women diagnosed with syphilis between 2008 and 2018 in our analysis received effective penicillin treatment. Even more concerning is that 51% of women in the ineffective treatment group had no treatment at all. The cause for the vast undertreatment of this population is multifactorial. The absence of prenatal care and lack of follow-up visits puts patients at risk for a missed syphilis diagnosis or inadequate clearance of a previous infection. In women who miscarried, a syphilis diagnosis was generally made concurrently with the miscarriage, often times during the patient's first encounter with the medical system.
Results
Multiple prenatal care visits are essential in retesting for infections throughout pregnancy. Some barriers to prenatal care are lower socioeconomic status, greater travel distances, low maternal schooling, and negative attitudes toward pregnancy.19, 20, 21 Patient follow-up depends both on patient attendance and the effective tracking of patients in the hospital system. It is not unusual for patients to deliver at different locations from where they received prenatal care.22 Without a smooth transition of care between the ambulatory and delivery teams, the patients may not receive effective treatment. One-thirds of women were placed in the ineffective treatment cohort as a result of incomplete treatment less than 30 days before delivery. Almost half of the patients with ineffective treatment were diagnosed at the time of delivery, suggesting that the main reason why patients were treated ineffectively is because a syphilis diagnosis was made late in pregnancy.
Clinical implications
Although effective treatment was shown to reduce disease transmission, half of effectively treated women still transmitted syphilis. This frequency was higher than expected for the patients who were managed according to the appropriate guidelines and demonstrated VDRL titer decline. We hypothesize that the lack of partner treatment is contributing to these high transmission rates. We also found that women without partner treatment were more likely to have syphilis MTCT. Despite treatment according to the standard of care, pregnant women are at a high risk of reinfection from untreated partners.1,23 Inadequate partner treatment stems from both institutional and social barriers. Cuba, the first country worldwide to successfully eliminate MTCT of HIV and syphilis, prioritized partner screening and treatment in their public health initiatives.2 In areas with no standardized partner treatment guidelines, the onus is placed on the women to both notify and counsel their partners to receive treatment.
Failure to disclose diagnoses is an aspect of the untreated partner problem fueling the syphilis epidemic. Andrade and colleagues showed that women with an extramarital encounter or those who had experienced previous domestic violence were more fearful of sharing new diagnoses with their partners.24 Professional support for navigating such conversations is essential for creating a safe environment for partner notification.25 Partner reinfection is also the product of risky sexual behaviors such as refusal to engage in regular condom use.26, 27, 28 Regardless of global efforts to address the syphilis epidemic, we found that pregnant women were at increased risk of syphilis MTCT between 2014 and 2016 than between 2008 and 2010. The penicillin shortage of 2014 may explain this increase in diagnoses.3,29 Increased reports of effective treatment during this time period may be attributed to the prioritization of treatment of pregnant women outlined in the Brazilian Ministry of Health initiative.30
Ineffective syphilis treatment coincided with the absence of prenatal care and a diagnosis of syphilis at delivery. Dual screening for HIV and syphilis has been found to be more cost effective than individual rapid tests.31 Considering that low and middle income countries have been more resistant to aggressively test for both infections because of cost concerns, the money saved from dual testing may be an incentive for adjusting future public health strategies.32 Our study demonstrated that women with HIV coinfection were more likely to receive ineffective treatment. A cross-sectional study of pregnant women receiving prenatal care in Tanzania showed that women screened earlier during the course of prenatal care presented at delivery with syphilis and HIV seroconversion as a result of reinfection.9 Standardized HIV and syphilis testing throughout pregnancy in women diagnosed with syphilis during pregnancy may reduce maternal HIV seroconversion.
Research implications
Treatment effectiveness had no significant impact on whether newborns had symptomatic syphilis. Symptomatic illness at birth is a rare phenomenon.33 Women with higher levels of education were at an increased risk of having symptomatic newborns. Owing to the low frequency of symptomatic newborns in our study, further studies are warranted to determine whether this is a true phenomenon. One possible explanation is that women with higher education have more severe first-time infections. The predictive relationship between higher VDRL titers ≥1:64 and symptomatic newborn syphilis was also shown in our study. Higher-titer syphilis infections are known to be associated with adverse outcomes such as symptomatic disease in the newborn.29
Strengths and limitations
Our study further delineates the profile of patients at risk for ineffective syphilis treatment at a large urban hospital in southern Brazil over an 11-year period, allowing us to identify future interventions. A study limitation was that the surveillance system only equated 1 visit to prenatal care, making it difficult to understand how different levels of prenatal care affect syphilis MTCT. Similarly, we did not have specific information regarding the time elapsed between treatment and the control of VDRL titers, making it difficult to discern incorrect or ineffective treatment from reinfection process. No longitudinal data were available for the evaluation of patient and partner contact tracing, and there were no records of maternal treatment during postnatal visits. Without long-term partner follow-up, we could neither identify whether partners were treated adequately nor fully quantify a patient's potential for reinfection from their partner.
Conclusions
Despite efforts to curb the syphilis epidemic, the rates of MTCT and associated adverse outcomes are on the rise in Brazil. A significant proportion of pregnant mothers with syphilis do not receive effective treatment, placing them at an increased risk of syphilis MTCT and HIV seroconversion in the future. New initiatives emphasizing effective syphilis treatment in both pregnant women and their partners may be pivotal in reducing congenital syphilis and future maternal HIV seroconversion.
Footnotes
The authors report no conflict of interest.
M.C.C. was supported by the University of California Los Angeles (UCLA) Postdoctoral Fellowship Training Program in Global HIV Prevention Research (T32MH080634), E.J.S. was supported by the UCLA South American Program in HIV Prevention Research Program (R25 MH087222). K.N., M.M., I.R., B.S., and R.L. are supported by the APT-CTU U01 grant. (U01 AI069424).
Cite this article as: Swayze E, Cambou MC, Melo M, et al. Ineffective penicillin treatment and absence of partner treatment may drive the congenital syphilis epidemic in Brazil. Am J Obstet Gynecol Glob Rep 2022;2:100050.
Supplementary material associated with this article can be found in the online version at doi:10.1016/j.xagr.2022.100050.
Appendix. Supplementary materials
References
- 1.Portal do Governo Brasileiro. Boletim Sífilis 2020. 2020. Available at: http://www.aids.gov.br/pt-br/pub/2020/boletim-sifilis-2020. Accessed January 25 2020.
- 2.World Health Organization. WHO validation for the elimination of mother-to-child transmission of HIV and/or syphilis. 2019. Available at:https://www.who.int/reproductivehealth/congenital-syphilis/WHO-validation-EMTCT/en/. Accessed March 18, 2021.
- 3.Projeto nascer série F. Comunicação e educação em saúde. Projeto nascer. Minist Saúde Secretaria Executiva Programa Nac DST Aids. 2003. Available at: http://bvsms.saude.gov.br/bvs/publicacoes/projeto_nascer.pdf. Accessed March 18, 2021.
- 4.Swayze EJ, Nielsen-Saines K, Segura ER, et al. Failure to recognize low non-treponemal titer syphilis infections in pregnancy may lead to widespread under-treatment. Int J Infect Dis. 2021;104:27–33. doi: 10.1016/j.ijid.2020.12.076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wu MY, Gong HZ, Hu KR, Zheng HY, Wan X, Li J. Effect of syphilis infection on HIV acquisition: a systematic review and meta-analysis. Sex Transm Infect. 2021;97:525–533. doi: 10.1136/sextrans-2020-054706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Abara WE, Hess KL, Neblett Fanfair R, Bernstein KT, Paz-Bailey G. Syphilis trends among men who have sex with men in the United States and western Europe: a systematic review of trend studies published between 2004 and 2015. PLoS One. 2016;11 doi: 10.1371/journal.pone.0159309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ramos VM, Figueiredo EN, Succi RC. Barriers to control syphilis and HIV vertical transmission in the health care system in the city of São Paulo. Rev Bras Epidemiol. 2014;17:887–898. doi: 10.1590/1809-4503201400040008. [DOI] [PubMed] [Google Scholar]
- 8.Melku M, Kebede A, Addis Z. Magnitude of HIV and syphilis seroprevalence among pregnant women in Gondar, Northwest Ethiopia: a cross-sectional study. HIV Aids (Auckl) 2015;7:175–182. doi: 10.2147/HIV.S81481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lawi JD, Mirambo MM, Magoma M, et al. Sero-conversion rate of Syphilis and HIV among pregnant women attending antenatal clinic in Tanzania: a need for re-screening at delivery. BMC Pregnancy Childbirth. 2015;15:3. doi: 10.1186/s12884-015-0434-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Protocolo clínico e Diretrizes Terapêuticas para prevenção da transmissão vertical de HIV, sífilis e hepatites virais 2019. 2021. Available at:http://www.aids.gov.br/pt-br/pub/2015/protocolo-clinico-e-diretrizes-terapeuticas-para-prevencao-da-transmissao-vertical-de-hiv. Accessed March 18, 2021.
- 11.Tsai S, Sun MY, Kuller JA, Rhee EHJ, Dotters-Katz S. Syphilis in pregnancy. Obstet Gynecol Surv. 2019;74:557–564. doi: 10.1097/OGX.0000000000000713. [DOI] [PubMed] [Google Scholar]
- 12.Korenromp EL, Rowley J, Alonso M, et al. Correction: global burden of maternal and congenital syphilis and associated adverse birth outcomes-estimates for 2016 and progress since 2012. PLoS One. 2019;14 doi: 10.1371/journal.pone.0211720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Yeganeh N, Watts HD, Camarca M, et al. Syphilis in HIV-infected mothers and infants: results from the NICHD/HPTN 040 study. Pediatr Infect Dis J. 2015;34:e52–e57. doi: 10.1097/INF.0000000000000578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Wendel GD, Jr, Sheffield JS, Hollier LM, Hill JB, Ramsey PS, Sánchez PJ. Treatment of syphilis in pregnancy and prevention of congenital syphilis. Clin Infect Dis. 2002;35(Suppl2):S200–S209. doi: 10.1086/342108. [DOI] [PubMed] [Google Scholar]
- 15.Tong ML, Lin LR, Liu GL, et al. Factors associated with serological cure and the serofast state of HIV-negative patients with primary, secondary, latent, and tertiary syphilis. PLoS One. 2013;8:e70102. doi: 10.1371/journal.pone.0070102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Luo Z, Ding Y, Yuan J, et al. Predictors of serological cure after penicillin therapy in HIV-negative patients with early syphilis in Shenzhen, China. PLoS One. 2021;16 doi: 10.1371/journal.pone.0245812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Nayak S, Acharjya B. VDRL test and its interpretation. Indian J Dermatol. 2012;57:3–8. doi: 10.4103/0019-5154.92666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Centers for Disease Control and Prevention. Screening recommendations: clinician timeline for screening syphilis, HIV, HBV, HCV, Chlamydia, and gonorrhea. 2019. Available at:https://www.cdc.gov/nchhstp/pregnancy/screening/clinician-timeline.html. Accessed March 18, 2021.
- 19.Bernardes AC, da Silva RA, Coimbra LC, et al. Inadequate prenatal care utilization and associated factors in São Luís, Brazil. BMC Pregnancy Childbirth. 2014;14:266. doi: 10.1186/1471-2393-14-266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Wehby GL, Murray JC, Castilla EE, Lopez-Camelo JS, Ohsfeldt RL. Prenatal care effectiveness and utilization in Brazil. Health Policy Plan. 2009;24:175–188. doi: 10.1093/heapol/czp005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Bassani DG, Surkan PJ, Olinto MT. Inadequate use of prenatal services among Brazilian women: the role of maternal characteristics. Int Perspect Sex Reprod Health. 2009;35:15–20. doi: 10.1363/ifpp.35.015.09. [DOI] [PubMed] [Google Scholar]
- 22.Institute of Medicine Brown SS . National Academies Press; Washington, DC: 1988. (US) committee to study outreach for prenatal care. Prenatal care: reaching mothers, reaching infants. ed. [PubMed] [Google Scholar]
- 23.Parkes-Ratanshi R, Mbazira Kimeze J, Nakku-Joloba E, et al. Low male partner attendance after syphilis screening in pregnant women leads to worse birth outcomes: the Syphilis Treatment of Partners (STOP) randomised control trial. Sex Health. 2020;17:214–222. doi: 10.1071/SH19092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Andrade RF, Araújo MA, Vieira LJ, Reis CB, Miranda AE. Intimate partner violence after the diagnosis of sexually transmitted diseases. Rev Saude Publica. 2015;49:3. doi: 10.1590/S0034-8910.2015049005424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Rocha AFB, Araújo MAL, Miranda AE, de Leon RGP, da Silva Júnior GB, Vasconcelos LDPG. Management of sexual partners of pregnant women with syphilis in northeastern Brazil - a qualitative study. BMC Health Serv Res. 2019;19:65. doi: 10.1186/s12913-019-3910-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Guerriero I, Ayres JR, Hearst N. Masculinity and vulnerability to HIV among heterosexual men in São Paulo, Brazil. Rev saúde publ. 2002;36:50–60. [PubMed] [Google Scholar]
- 27.Yeganeh N, Varella I, Santos BR, et al. Risk-taking behavior for HIV acquisition during pregnancy in Porto Alegre. Brazil. Infect Dis Obstet Gynecol. 2012;2012 doi: 10.1155/2012/490686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Yeganeh N, Dillavou C, Simon M, et al. Audio computer-assisted survey instrument versus face-to-face interviews: optimal method for detecting high-risk behaviour in pregnant women and their sexual partners in the south of Brazil. Int J STD AIDS. 2013;24:279–285. doi: 10.1177/0956462412472814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Liu H, Chen N, Yu J, et al. Syphilis-attributable adverse pregnancy outcomes in China: a retrospective cohort analysis of 1187 pregnant women with different syphilis treatment. BMC Infect Dis. 2019;19:292. doi: 10.1186/s12879-019-3896-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Nurse-Findlay S, Taylor MM, Savage M, et al. Shortages of benzathine penicillin for prevention of mother-to-child transmission of syphilis: an evaluation from multi-country surveys and stakeholder interviews. PLoS Med. 2017;14 doi: 10.1371/journal.pmed.1002473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Gliddon HD, Peeling RW, Kamb ML, Toskin I, Wi TE, Taylor MM. A systematic review and meta-analysis of studies evaluating the performance and operational characteristics of dual point-of-care tests for HIV and syphilis. Sex Transm Infect. 2017;93(Suppl4):S3–15. doi: 10.1136/sextrans-2016-053069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Adawiyah RA, Saweri OPM, Boettiger DC, et al. The costs of scaling up HIV and syphilis testing in low- and middle-income countries: a systematic review. Health Policy Plan. 2021;36:939–954. doi: 10.1093/heapol/czab030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Yeganeh N, Watts DH, Xu J, et al. Infectious morbidity, mortality and nutrition in HIV-exposed, uninfected, formula-fed infants: results from the HPTN 040/PACTG 1043 trial. Pediatr Infect Dis J. 2018;37:1271–1278. doi: 10.1097/INF.0000000000002082. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.