Abstract
Background:
Given Canada’s geographically dispersed population, initial trauma care may occur at rural sites that may not manage patients with trauma frequently; thus, telementoring can play a life-saving role. In this article, we describe a rural trauma telementoring pilot program in British Columbia and report the results of an evaluation of its strengths and weaknesses.
Methods:
Trauma surgeons from a quaternary trauma centre in Vancouver helped facilitate 3 in situ trauma simulation sessions at a rural BC hospital between fall 2019 and summer 2020. The sessions involved 4 physician participants (a trauma surgeon telementor, a family physician with additional expertise in emergency medicine acting as trauma team leader, a family physician with additional expertise in anesthesia and a family physician with Enhanced Surgical Skills), an emergency department nurse, 2 operating room/trauma team nurses, and laboratory and radiology technicians. The sessions involved simulated damage-control procedures and lasted about 2 hours. The participants completed surveys assessing comfort and confidence regarding aspects of trauma care and use of the telehealth unit before and after each session, and the facilitators assessed team dynamics using the Modified Non-Technical Skills for Trauma (T-NOTECHS) tool. Focus groups were held to gather qualitative data, and costs were tracked.
Results:
The average presimulation confidence survey score was 19.6/30, and the average postsimulation score was 24.0/30. The mean score improved significantly after both the first and second sessions (p = 0.01 and p = 0.004, respectively). Across the 3 sessions, the average T-NOTECHS score improved significantly, from 18.5/25 to 21.5/25 (p = 0.02). Qualitative analysis identified 3 dominant themes: telementoring increased provider confidence, telementoring increased order to the resuscitation procedure and the technical aspects of telementorship. The telementoring program was well received by all participants.
Conclusion:
A significant improvement was seen across simulations in physician confidence and trauma team dynamics with telementorship support. Telementoring in trauma may provide a way to lessen the difference between rural and urban patient outcomes within Canada’s geographically dispersed population, although further work investigating the impact of its use in real-life patients, as well as barriers to its implementation, is required.
Abstract
Contexte:
La population canadienne étant dispersée géographiquement, les soins initiaux en traumatologie sont parfois prodigués dans des sites ruraux qui ne prennent pas couramment en charge les traumas; dans ces circonstances, le mentorat en ligne peut sauver des vies. Dans cet article, nous décrivons un programme pilote de mentorat en ligne de Colombie-Britannique axé sur la traumatologie rurale et évaluons ses forces et ses faiblesses.
Méthodes:
Des chirurgiens en traumatologie d’un centre quaternaire spécialisé en traumatologie de Vancouver ont animé 3 séances de simulation in situ en traumatologie dans un hôpital rural de Colombie-Britannique, qui ont eu lieu entre l’automne 2019 et l’été 2020. Quatre médecins participants (mentor chirurgien en traumatologie présent en ligne, médecin de famille ayant une expertise additionnelle en médecine d’urgence jouant le rôle de chef d’équipe de traumatologie, médecin de famille ayant une expertise additionnelle en anesthésie et médecin de famille détenant un certificat de compétences avancées en chirurgie), 1 infirmière d’urgence, 2 infirmières de salle d’opération ou de l’équipe de traumatologie et des techniciens de laboratoire et en radiologie se sont joints aux séances, qui prenaient la forme d’interventions simulées de stabilisation d’une durée approximative de 2 heures. Les participants ont répondu à des questionnaires évaluant leur degré d’aisance et de confiance en lien avec divers aspects des soins en traumatologie et l’utilisation de l’unité de télésanté avant et après chaque séance, et les animateurs ont évalué la dynamique d’équipe à l’aide de l’outil modifié d’évaluation des compétences non techniques en traumatologie (T-NOTECHS). Des groupes de discussion ont été formés pour recueillir des données qualitatives, et un suivi des coûts a été effectué.
Résultats:
Les participants ont obtenu un score moyen au questionnaire évaluant la confiance de 19,6/30 avant la simulation, et de 24,0/30 après la simulation. Une amélioration significative du score moyen a été constatée après la première et la deuxième séance (p = 0,01 et p = 0,004, respectivement). De la première à la troisième séance, le score moyen à l’évaluation T-NOTECHS a aussi connu une amélioration significative, passant de 18,5/25 à 21,5/25 (p = 0,02). L’analyse qualitative a permis de mettre en évidence 3 thèmes dominants : amélioration grâce au mentorat en ligne de la confiance des fournisseurs de soins; amélioration par le mentorat en ligne de la rigueur de la procédure de réanimation; aspects techniques du mentorat en ligne. Tous les participants avaient une bonne opinion du programme.
Conclusion:
Avec le soutien du mentorat en ligne, la confiance des médecins et la dynamique des équipes de traumatologie ont connu une amélioration significative au fil des simulations. Au Canada, où la population est dispersée, le mentorat en ligne en traumatologie pourrait être un bon moyen de réduire les écarts dans les issues de santé entre les populations rurales et urbaines. Il faudra toutefois étudier davantage les effets de l’intervention en contexte réel et les obstacles à la mise en oeuvre.
Traumatic injuries are Canada’s third-leading cause of death but result in more potential years of life lost than the first- and second-leading causes of death combined.1 Given this burden, and within the context of Canada’s geographically dispersed population, trauma systems are crucial in order to provide optimal patient care.2 Despite robust systems in many provinces, the outcomes of rural patients remain worse than those of their urban counterparts.3–6 Reasons for this include underlying injury patterns and patient characteristics, transportation times, and local health care resources and traumatology expertise.7,8 The last factor is modifiable and is where novel information technologies stand to play a growing role. Telementoring is 1 such technology, allowing for the provision of real-time guidance by a physically distant expert. Although trauma systems are made to allow expedient transfer of injured patients to quaternary trauma centres, transport of patients is not always possible owing to road closures, weather conditions or the time-sensitivity of a particular injury; thus, telementoring can play a life-saving role.9–11 In addition to directly affecting patient care, telementoring has also been shown to be an effective educational tool.12
With this in mind, trauma surgeons at a quaternary trauma centre (Vancouver General Hospital, Vancouver, BC) partnered with physicians at a rural centre (Queen Victoria Hospital, Revelstoke, BC) and codeveloped a trauma telementorship program, meant in part as a method of professional development for the rural participants. In this article, we describe the program, and report the results of an evaluation of its strengths and weaknesses.
Methods
We performed a parallel mixed-methods evaluation of the rural trauma telementoring pilot project using a combination of quantitative questionnaires and assessments, and qualitative focus group interviews. Institutional ethics board approval was obtained (H19–01440).
Setting
The trauma centre is 1 of 2 adult level 1 trauma centres in BC, with 700 acute inpatient beds. The rural centre is a regional hospital serving a population of about 15 000, with 15 acute inpatient beds; the main referral hospital is more than 200 km away. The rural centre has access to basic laboratory and radiologic tests, but no computed tomography scanner. Importantly, several family practitioners at the rural centre have additional expertise in emergency medicine, anesthesia or surgery (FP-ESS) (“ESS” stands for Enhanced Surgical Skills, as these family doctors have undergone a year of general surgical training and are able to perform a variety of basic procedures).
Although the rural centre is outside the catchment of the level 1 trauma centre, a relationship was formed when 1 of the FP-ESS physicians spent several weeks on the trauma service conducting a pilot “mini-fellowship” that included junior and senior resident responsibilities, as well as live tissue and cadaver laboratories, and participation in the Definitive Surgical Trauma Care Course. The rural centre’s usual referral site was involved in the planning phase of both the fellowship and ongoing telementored simulation sessions.
Participants and simulation
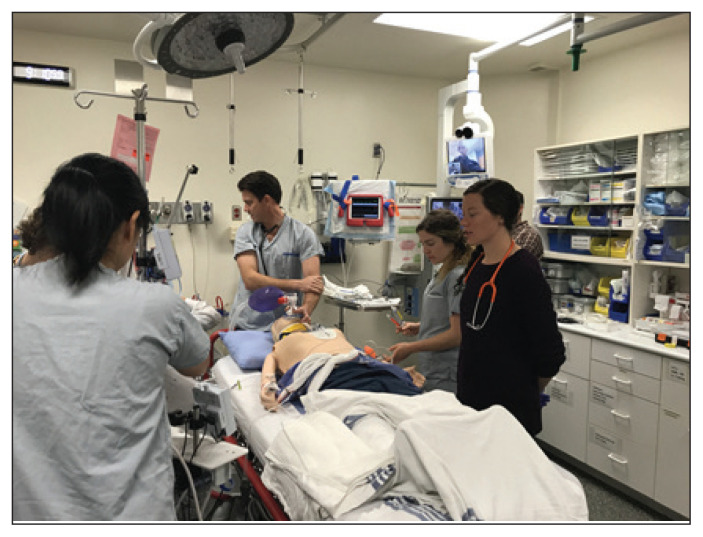
A trauma surgeon (P.D.) from the quaternary trauma centre facilitated 3 in situ trauma simulations at the rural hospital over the course of 1 year (fall 2019 to summer 2020), with local assistance by the second author (V.H.). Each simulation required telementoring of both resuscitation and performance of a damage-control procedure in an injured patient by a trauma surgeon. Both the simulated telementor and the rural trauma team were blinded to the simulation scenarios ahead of time (Figure 1). The simulation scenarios were novel scenarios that were written specifically to highlight situations in which care was beyond the normal scope of practice of the rural centre. Two of the 3 scenarios required moving the simulated resuscitation from the emergency bay to the operating room.
Fig. 1.
Telementoring simulation.
Simulation sessions involved 4 physician participants: a trauma surgeon telementor, a family physician with additional expertise in emergency medicine acting as trauma team leader, a family physician with additional expertise in anesthesia and an FP-ESS. These participants differed for each simulation session. In addition, 1 emergency department nurse, 2 operating room/trauma team nurses, and laboratory and radiology technicians participated in each session. Each session lasted about 2 hours, including post-session debriefing.
We used the Vantage remote presence system (InTouch Health), which consists of several high-definition cameras, microphones and video monitors on a moveable platform and is connected to a secure virtual private network connection. Both the trauma surgeon facilitator and simulated telementor at the trauma centre used their computer or smartphone for audiovisual display via the InTouch Health software, and received an orientation to this application in advance.
Study measures and evaluation
We used confidence surveys with 5-point Likert-type scales to assess physicians’ and nurses’ comfort and confidence regarding aspects of care of patients with trauma and use of the telehealth unit. There were 6 questions, for a total possible score of 30. The surveys were completed before and after the telementoring simulation sessions. An example of the survey used for the rural participants can be found in Appendix 1 (available at www.canjsurg.ca/lookup/doi/10.1503/cjs.015020/tab-related-content). The survey completed by the telementors used the same scale but contained only 2 items (“Ability to utilize the telehealth equipment to communicate effectively with the local trauma team” and “Ability to facilitate, via telementorship, a life-saving trauma intervention”), for a total possible score of 10. To support ongoing quality improvement, the postsession surveys for both groups had an additional question that asked participants for their overall rating of the session’s utility. The facilitators and observing physicians used the Modified Non-Technical Skills for Trauma Assessment tool (T-NOTECHS)13 to assess the trauma team dynamics of the multidisciplinary trauma resuscitation team (Appendix 1). The total possible score was 25.
Postsimulation debrief sessions with semistructured group interviews also acted as focus groups and were facilitated by the senior author (P.D.). The interview questions were as follows:
What was your gut reaction to the simulation, in 1 or 2 words?
Could 1 person (typically the trauma team leader/emergency physician) summarize the principal findings and interventions?
What did the team do well?
What could the team have improved on?
How did you feel about the telementoring process?
-
Anything else to add? Any questions for us?
All those involved in each simulation, including physicians and registered nurses, participated in the focus groups.
The sessions were audio recorded and transcribed professionally.
Data analysis
Two authors (G.H. and P.D.) read and coded the transcriptions independently. Dominant themes relating to the telementorship experience were ultimately identified and agreed on, then validated by participants. We used the COREQ checklist with regard to the design, analysis and reporting of the qualitative results.14 Time and financial costs were tracked.
We compared mean results within and across telementoring sessions using the Student t test and one-way analysis of variance, respectively. A p value < 0.05 was considered statistically significant. Statistical analysis was carried out with SPSS Statistics version 20 (IBM Corp.).
Results
Confidence surveys
The average presimulation confidence survey score was 19.6/30, and the average postsimulation score was 24.0/30. Rural participants ranked improved confidence across most domains in all 3 simulation sessions, although statistical significance was reached only in sessions 1 and 2 (Table 1). Only 3 participants returned surveys from simulation session 3. The largest improvement was in comfort using the telementoring equipment, although consistent improvement across all domains of trauma care was seen.
Table 1.
Confidence survey results for rural participants
| Simulation session; participant* | Score† | Mean Δ (p value) | |
|---|---|---|---|
| Before session | After session | ||
| Session 1 | |||
| Overall (mean) | 20.3 | 23.5 | +3.2 (0.01) |
| Family practitioner with additional expertise in emergency medicine | 19 | 26 | |
| FP-ESS | 21 | 26 | |
| Family practitioner with additional expertise in anesthesia | 19 | 22 | |
| Operating room nurse 1 | 18 | 21 | |
| Operating room nurse 2 | 21 | 22 | |
| Session 2 | |||
| Overall (mean) | 19.2 | 24.6 | +5.4 (0.004) |
| Family practitioner with additional expertise in emergency medicine | 12 | 16 | |
| FP-ESS | 22 | 26 | |
| Family practitioner with additional expertise in anesthesia | 20 | 23 | |
| Operating room nurse 1 | 21 | 30 | |
| Operating room nurse 2 | 21 | 28 | |
| Session 3 | 24 | ||
| Overall (mean) | 19.3 | 24.0 | +4.6 (0.09) |
| Family practitioner with additional expertise in emergency medicine | 15 | 22 | |
| FP-ESS | 27 | 27 | |
| Family practitioner with additional expertise in anesthesia | 16 | 23 | |
FP-ESS = family practitioner with Certificate of Added Competence in Enhanced Surgical Skills.
The emergency department nurse did not complete the surveys.
Total possible score 30.
The trauma surgeon telementor involved in simulation session 2 reported a presimulation score of 6/10 and a postsimulation score of 9/10. The telementor involved in simulation 3 reported a presimulation score of 7/10 and a postsimulation of 8/10. The telementor involved in simulation 1 did not return their surveys. All telementors rated the helpfulness of the simulation session as 4/4.
Nontechnical skills
Two to 4 physicians were in positions of facilitation or observation during each simulation and were able to provide T-NOTECHS teamwork scores. Across the 3 sessions, the average T-NOTECHS score improved significantly, from 18.5 to 21.5 (t(3) = 4.243, p = 0.2) (Table 2).
Table 2.
Results of Modified Non-Technical Skills for Trauma Assessment tool
| Facilitator/observer | Simulation session; score* | Mean Δ (p value) | ||
|---|---|---|---|---|
| Session 1 | Session 2 | Session 3 | ||
| Overall (mean) | 18.5 | 21.0 | 21.5 | +3.0 (0.02) |
| 1 | 18 | 22 | 24 | |
| 2 | 18 | 20 | 21 | |
| 3 | 19 | — | 20 | |
| 4 | 19 | — | 21 | |
Total possible score 25.
Qualitative analysis
Three dominant themes emerged from the approximately 110 minutes of transcribed data: increased provider confidence, increased calm and order, and the technical aspects of telementorship.
Multiple team members across sessions described how the telementor was able to impart confidence. This confidence boost was seen both directly, with the telementor helping the rural trauma team make big decisions more decisively, and indirectly, with participants saying that simply knowing they had expert telementored support available was enough to improve their confidence in dealing with trauma. One of the rural physicians described how “when we are running traumas once a month, or even once every 2 months… knowing that we are able to receive telementoring support improves our confidence a great deal.” Another stated that “it’s great to have feedback just to confirm the steps before you do something.”
Rural team members reported increased calm and order because of the telementor’s presence. The emergency department nurse described how, once the telementor link was established, the team was able to reorganize from a resuscitation that was previously felt to be “a little bit chaotic.” One of the physicians said that it “felt calming… like a weight was lifted… when [the telementor was] beamed into the room.”
Regarding the technical aspects of the telehealth equipment, there were features of the technology that were much appreciated. One of the trauma surgeon telementors agreed that the technology was user-friendly and that he “could have been anywhere,” alluding to the fact that he participated via his smartphone. However, some issues were noted with the telehealth unit. The audio was at times difficult to hear within the setting of an active trauma resuscitation, with 1 rural physician saying that they were “disappointed that this unit doesn’t talk louder, because it can’t speak over a busy trauma bay.” This participant went on to suggest amplifying the volume via a Bluetooth speaker. Another rural physician expressed concern that the telehealth unit was “a bit unwieldy” and suggested that “a smaller unit might be better.”
Cost
The cost of the telementoring unit and 3 years of support came close to $200 000. Each simulation session cost roughly $3000, which included equipment and physician compensation. All costs were subsidized by a provincial rural initiative stipend.
Discussion
The rural trauma telementoring pilot program was well received by all participants, and a significant improvement was seen across simulations in physician confidence and trauma team dynamics with telementorship. Whether this can translate to improvement of real-life patient outcomes is yet to be seen.
Although outside the scope of this limited report, the physicians at Queen Victoria Hospital made use of real-time telementoring on 1 occasion, and the technology was used with minimal delay or disruption to their resuscitation efforts. The case was that of a young patient involved in a single-vehicle motor vehicle collision who had an isolated traumatic brain injury. All appropriate care had been provided and transfer had been initiated at the time of the call, but validation of the decisions made was described as “very helpful” (V.H.).
Given the recent proliferation of available technologies for videoconferencing and the medical community’s growing comfort with their use during the COVID-19 pandemic, it is likely that communication equipment and applications will not commonly be the rate-limiting step in expanding this practice.15 Two factors that will likely determine the success of robust and sustainable telementoring support are bandwidth (which is susceptible to environmental conditions and disasters) and interpersonal relationships and trust between mentors and mentees. Training via telementored simulation, as described in the present report, could prove to be an important means to develop and maintain the latter. In the real-life scenario described above, health care providers at both sites (V.H., P.D.) felt that any barriers to the use of the telementoring system were lowered by the established working relationship between the 2 centres. In this regard, word-of-mouth among physicians at Queen Victoria Hospital and other rural centres have led to these other remote sites’ expressing interest in establishing similar telementoring programs. At the time of writing, initial discussions were being held at the provincial level to create a centralized trauma telementoring service. Telementored simulations are being considered both during rollout and for regular maintenance of skills.
Our next steps include accruing data, including real-life patient data, as this program continues, and potentially evaluating longevity and learning transfer of beliefs and skills acquired during the simulation sessions. Further proceduralization of real-time trauma telementoring would also be worthwhile and could help address issues such as establishing a back-up form of communication in case of a failed connection, and integrating regularly occurring resuscitation summaries to help ensure the telementor is kept abreast of off-camera actions.
Ultimately, we would like to see all remote hospitals throughout the province have access to telementoring for trauma. Whether they are partnered with their usual level 1 or 2 referral centres to make use of telementorship for ongoing professional development and real-time patient care, or there is a central provincial “trauma hotline,” or a combination of the two, remains to be seen.
Limitations
Our research design has substantial limitations. An overarching issue is that the pilot project was small in scope, with relatively few participants and no real-life patient data. Given that the same physicians were not necessarily involved from session to session, we are limited in making claims about the trends seen. Furthermore, pre–post surveys are not the most robust tool to measure the true impact of an intervention. Challenges also exist with regard to expansion of the telementoring project as it stands now, not the least of which is a high financial cost. In our case, this cost was heavily subsidized by a rural initiative fund.
Conclusion
In this pilot project, a significant improvement was seen across simulations in rural physician confidence and trauma team dynamics with telementorship support. Telementoring in trauma may provide a way to lessen the difference between rural and urban patient outcomes within Canada’s geographically dispersed population, although further work investigating the impact of its use in real-life patients, as well as barriers to its implementation, is required.
Supplementary Material
Footnotes
Funding: The Rural Surgical Obstetrical Networks initiative of the Rural Coordination Centre of BC provided sessional funding to engage participants at the rural study hospital in the educational trauma simulations.
Competing interests: None declared.
Contributors: G. Hintz and P. Dawe designed the study. V. Haines acquired the data, which G. Hintz and P. Dawe analyzed. G. Hintz wrote the manuscript, which V. Haines and P. Dawe critically revised. All authors gave final approval of the article to be published.
References
- 1.Rogers FB, Shackford SR, Hoyt DB, et al. Trauma deaths in a mature urban vs rural trauma system. A comparison. Arch Surg 1997; 132:376–81, discussion 381–2. [DOI] [PubMed] [Google Scholar]
- 2.Injury prevention & control. Ten leading causes of death and injury – unintentional injury [chart]. Atlanta: Centers for Disease Control and Prevention; 2003. Available: http://www.cdc.gov/injury/wisqars/LeadingCauses_images.html (accessed 2020 Apr. 27). [Google Scholar]
- 3.Kmet L, Macarthur C. Urban–rural differences in motor vehicle crash fatality and hospitalization rates among children and youths. Accid Anal Prev 2006;38:122–7. [DOI] [PubMed] [Google Scholar]
- 4.Boland M, Staines A, Fitzpatrick P, et al. Urban–rural variation in mortality and hospital admission rates for unintentional injury in Ireland. Inj Prev 2005;11:38–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Fatovich DM, Jacobs IG. The relationship between remoteness and trauma deaths in Western Australia. J Trauma 2009;67:910–4. [DOI] [PubMed] [Google Scholar]
- 6.Simons RK. Rural accidental injury and death: The neglected disease of modern trauma systems? J Trauma Acute Care Surg 2018;84: 972–7. [DOI] [PubMed] [Google Scholar]
- 7.Coben JH. National Highway Traffic Safety Administration (NHTSA): contrasting rural and urban fatal crashes 1994–2003. Ann Emerg Med 2006;47:574–5. [DOI] [PubMed] [Google Scholar]
- 8.Prabhakaran K, Lombardo G, Latifi R. Telemedicine for trauma and emergency management: an overview. Curr Trauma Rep 2016;2:115–23. [Google Scholar]
- 9.Latifi R, Hadeed GJ, Rhee P, et al. Initial experiences and outcomes of telepresence in the management of trauma and emergency surgical patients. Am J Surg 2009;198:905–10. [DOI] [PubMed] [Google Scholar]
- 10.Lapointe L, Lavallee-Bourget MH, Pichard-Jolicoeur A, et al. Impact of telemedicine on diagnosis, clinical management and outcomes in rural trauma patients: a rapid review. Can J Rural Med 2020; 25:31–40. [DOI] [PubMed] [Google Scholar]
- 11.Doarn CR, Latifi R. Telementoring and teleproctoring in trauma and emergency care. Curr Trauma Rep 2016;2:138–43. [Google Scholar]
- 12.Augestad KM, Han H, Paige J, et al. Educational implications for surgical telementoring: a current review with recommendations for future practice, policy, and research. Surg Endosc 2017;31:3836–46. [DOI] [PubMed] [Google Scholar]
- 13.Steinemann S, Berg B, DiTullio A, et al. Assessing teamwork in the trauma bay: introduction of a modified “NOTECHS” scale for trauma. Am J Surg 2012;203:69–75. [DOI] [PubMed] [Google Scholar]
- 14.Tong A, Sainsbury P, Craig J. Consolidated criteria for reporting qualitative research (COREQ): a 32-item checklist for interviews and focus groups. Int J Qual Health Care 2007;19:349–57. [DOI] [PubMed] [Google Scholar]
- 15.Ting DSW, Carin L, Dzau V. Digital technology and COVID-19. Nat Med 2020;26:459–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.