Purpose of review
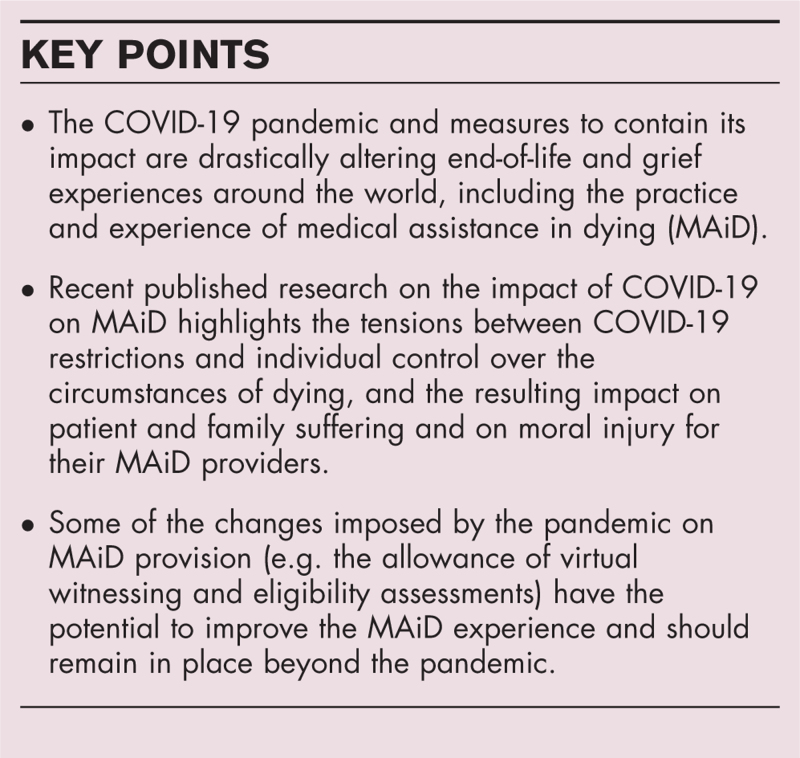
The COVID-19 pandemic and measures to contain its impact are drastically altering end-of-life and grief experiences around the world, including the practice and experience of medical assistance in dying (MAiD).
Recent findings
Recent published literature on the impact of COVID-19 on MAiD can be described under the following categories: studies investigating the impact of COVID-19 on MAiD from the healthcare providers’ perspective; studies investigating the impact of COVID-19 on MAiD from the patient/family perspective; and opinion papers that review the impact of COVID-19 on MAiD from a legal–ethical perspective. Most of these studies were either conducted in Canada or included mostly Canadian participants.
Summary
Recent published research on the impact of COVID-19 on MAiD highlights the tensions between COVID-19 restrictions and individual control over the circumstances of dying, and the resulting impact on patient and family suffering and on moral injury for their MAiD providers. These reports may help inform risk mitigation strategies for the current pandemic and future similar public health crises that acknowledge the value of humane, family-centered care at the end of life.
Keywords: assisted death, coronavirus disease 2019, medical assistance in dying
INTRODUCTION
The coronavirus disease 2019 (COVID-19) pandemic and measures to contain its impact are drastically altering end-of-life and grief experiences around the world. Death has been brought to the forefront: the pandemic is challenging our notions of ‘a good death’ [1] and may be associated with ‘a pandemic of complicated grief’ [2]. Within hospitals, a patient-centered and family-centred care approach [3] at the end-of-life has been hampered by strict visitor policies in healthcare institutions, delayed admissions [4,5] and, in some regions, by the sheer volume of COVID-19 patients that overwhelmed the healthcare system [6]. These transformations, as well as increased social isolation and restrictions on mourning rituals, may have a significant negative impact on quality of death and bereavement outcomes.
The pandemic also imposed constraints on the practice of medical assistance in dying (MAiD), a practice that is becoming more common worldwide. In Canada, where assisted death became legal in 2016, MAiD is a term that refers to both the direct administration of a lethal substance (i.e. injection of a drug) or providing/prescribing a lethal substance that the eligible patient administers themselves. In other countries, other terms, such as voluntary euthanasia and medically assisted suicide, may be used to describe this practice, and how MAiD is interpreted and implemented varies in each jurisdiction where it is legal.
The purpose of this review is to summarize what is currently known and understood about the impact of COVID-19 on MAiD. The findings of this review will assist healthcare providers and policymakers as we manage the current ongoing COVID-19 pandemic and plan for future pandemics.
Box 1.
no caption available
MATERIALS AND METHODS
A comprehensive list of search terms (e.g. physician-assisted death, voluntary euthanasia, physician-assisted suicide, legal-assisted dying or euthanasia, and MAiD) was used to search for MAiD-related literature published in the past 2 years. Then, in order to identify literature that has addressed the impact of COVID-19 on MAiD, we reviewed each relevant publication to identify if it included search terms, such as COVID-19 or pandemic in their title, abstract or list of key words, and/or if it reported on data that was collected, at least partially, after 11 March 2020 (when COVID-19 was declared a global pandemic by WHO). Any published or unpublished literature (whether peer-reviewed or other) was considered. All article types were included (e.g. reviews, editorials/commentary, original research, program development) as well as grey literature in the form of government reports and research institute publications. Only literature written in English was reviewed. We searched electronic databases including: PubMed and PsychINFO. We also searched researchgate.net (accessed on 14 June 2022) and Google Scholar (accessed on 14 June 2022) as well as government websites in jurisdictions where legal MAiD is available. Once a publication was deemed relevant, we also searched the reference list of the publication as well as publications in which it was cited. We summarized all relevant publications using descriptive analysis, and we present these findings in a narrative format.
RESULTS
Recent published literature on the impact of COVID-19 on MAiD can be described under the following categories: studies investigating the impact of COVID-19 on MAiD from the healthcare providers’ perspective [7,8,9▪,10,11,12▪▪]; studies investigating the impact of COVID-19 on MAiD from the patient/family perspective [13]; and literature that reviews the impact of COVID-19 on MAiD from a legal–ethical perspective [14,15]. All publications, except two [11,15], were situated in Canada. The over-representation of the Canadian context in the literature is likely as MAiD was only recently legalized in Canada and is currently receiving much research attention. Ongoing studies in Canada on the implementation of MAiD were able to pivot quickly to respond to questions brought on by the pandemic. All studies collected data during the earlier phases of the COVID-19 pandemic, with most reporting on data collected up until July 2020 [7,8,9▪,10] and only two including data collected in 2021 [11,13].
The impact of coronavirus disease 2019 on medical assistance in dying from the healthcare providers’ perspective
Four studies involved surveys or qualitative interviews with MAiD providers and reported on the impact of COVID-19 on MAiD from their perspective. All of these studies were either conducted in Canada [7,8,9▪,10] or included mostly Canadian participants [11,12▪▪].
The largest study was conducted by Stewart et al.[7]. In this study, 131 MAiD providers from across Canada completed a survey asking them to rank a list of stressors and protective factors in practicing MAiD. The survey was electronically distributed during the first wave of COVID-19 (from June to July 2020), and, therefore, the researchers added a survey item about ‘Difficulties of assessing/providing MAiD during COVID-19’, along with an option for adding open-ended comments on this item. Although only 28 (21.5%) participants scored this item as a moderate or severe stressor, 50 (39.6%) respondents provided comments on the impact of the pandemic on MAiD practice during COVID-19. These comments were categorized into stressors related to: impediments to referrals for MAiD; challenges because of use of personal protective equipment (PPE); a sense of greater urgency and increased suffering of patients who were assessed for MAiD during COVID-19; challenges with hospital/institutional COVID-19 policies; limitations of virtual assessments; documentation challenges; and the sense that restriction of the number of people that can be present for MAiD is inhumane.
In another survey-based study, conducted by Oliver et al.[11,12▪▪], 89 respondents who were involved in MAiD provision completed an online survey about the impact of the pandemic on MAiD services during the first wave of COVID-19 (from July to August 2020). Most of the participants (55%) were from Canada, and others were from 10 other jurisdictions in which MAiD is legal. The study also included qualitative interviews from August 2020 to January 2021 with a subsample of 18 participants, but it is unclear in which jurisdictions they were located. Oliver et al.'s [11,12▪▪] analysis uncovers how MAiD providers responded and adapted to the disruptions created by the pandemic by employing flexibility and ‘calculated rule-breaking’ (e.g. in regards to witnessing requirements or public health restrictions on the number of people present for MAiD assessment or procedure). Importantly, this study describes how some challenges and concerns differed among jurisdictions because of different MAiD eligibility criteria or procedural safeguards or based on how recently MAiD became legal in different jurisdictions. Thus, virtual assessments were more challenging in jurisdictions where it was not clear that telehealth approaches were legal, or where providers had no previous experience in this modality. In addition, concerns about managing future increased demand for MAiD were greater in jurisdictions where eligibility for MAiD does not require a demonstration of a reasonably foreseeable natural death or in jurisdictions where MAiD was not yet a long-established service.
In a smaller, qualitative study, 16 healthcare providers from across Canada who were involved in MAiD were interviewed about their experience during the first wave of COVID-19 (from April to June, 2020). Four qualitative themes were extracted from these interviews: participants perceived the pandemic to be associated with increased suffering of patients requesting MAiD because of patients being unable to spend time with their families because of institutional visitor restriction policies and travel restrictions, MAiD procedures being cancelled or rescheduled, and the inability to access palliative or hospice care; participants perceived the pandemic to be associated with decreased rapport and closeness with patients because of the need to conduct MAiD assessments virtually or wear PPE during the MAiD procedure; participants reported anxiety about putting themselves at risk of being infected or spreading COVID-19 when providing MAiD; and participants reported on the importance of making exceptions to visitor restriction and social distancing rules when providing MAiD [9▪]. In a secondary analysis of these interviews, Tremblay-Huet et al.[8] expanded on this fourth theme and described how deviating from public health rules in the context of MAiD (e.g. allowing family members to be present or disregarding social distancing) was deemed necessary by participants because of the ‘exceptionality’ and the ‘emotionality’ of the procedure.
Lastly, Wiebe et al.[10] in a study focusing on forced or chosen transfers of patients from one location to another for MAiD, conducted 13 interviews with MAiD providers across Canada from April to May 2020 in order to understand how the pandemic impacted MAiD-related transfers. The study reported that the pandemic decreased the choices of a location for MAiD and made the already challenging logistics involved in chosen transfers for MAiD more difficult.
The impact of coronavirus disease 2019 on medical assistance in dying from the patient/family perspective
Much of the research literature on MAiD has focused on the healthcare provider perspective of the MAiD experience, often excluding the perspectives of patients, and especially the perspective of their informal caregivers [16]. Thus, it is not surprising that only one study to date [13] has investigated the impact of COVID-19 on MAiD from the patient and family members’ perspectives.
In this qualitative study, interviews with seven patients who requested MAiD and 23 family caregivers of patients who requested MAiD were completed between April 2020 and May 2021. MAiD was completed for all participants in hospital in a large urban city in Canada. The analysis generated four themes with respect to the impact of COVID-19 and its containment measures on the MAiD experience: MAiD decision-making was perceived to be accelerated for patients, especially when the timeline and continued evolution of the public health threat were perceived to extend beyond the patient's life expectancy; visitor restrictions compromised family understanding of the patient's illness progression and proximity to end-of-life and challenged patients’ ability to convey their decision around MAiD to their families; visitor restrictions and PPE protocols in hospitals disrupted the MAiD day experience; and lastly, participants expressed appreciation for rule flexibility and for healthcare providers who approved exemptions of hospital restrictions nearing and during MAiD day.
In addition to the above study, it is possible to infer limited information about the impact of COVID-19 on MAiD from the patient perspective by comparing between metrics available from the 2019 [17] and 2020 [18] MAiD annual reports published by Health Canada. Specifically, these reports include a list of descriptions, provided by individuals requesting MAiD, of the nature of their intolerable suffering. A review of these lists reveals that the description of suffering as ‘a loss of ability to engage in meaningful life activities’ increased from 82.1 to 84.9% between 2019 and 2020. Similarly, the description of suffering as ‘isolation or loneliness’ increased from 13.7 to 18.6%.
The impact of coronavirus disease 2019 on medical assistance in dying from a legal–ethical perspective
Adding to the already rich discourse on the ethical and legal considerations in the regulation of MAiD, two opinion papers explored the impact of COVID-19 on the ethical debate over MAiD. The first, by Khawaja and Khawaja [14], discusses the concern that a potential decline in mental health and limited access to social support and healthcare resources, brought about by the pandemic, would cause more individuals, especially older ones, to choose to pursue a MAiD option prematurely. The second, by Salinas Mengual [15], discusses the concern that, in the face of a crisis, such as COVID-19, the legality of MAiD may encourage the selective distribution of healthcare resources that favors the young over the old. These pieces emphasize how COVID-19 has increased tensions between individual patient care and treatment decision-making, supported by ethical principles of individual autonomy, and the good and functioning of the wider system and community.
DISCUSSION
As one of the largest and most devastating public health crises in the past century, the COVID-19 pandemic and related public health measures worldwide have drastically altered dying and grieving experiences, including the experience of MAiD. Recent published research on the impact of COVID-19 on MAiD from the perspectives of healthcare providers, patients and family members [7,8,9▪,10,11,12▪▪,13] highlight the tensions between COVID-19 restrictions and individual control over the circumstances of dying, and the resulting impact on patient and family suffering and on moral injury for their MAiD providers. These findings may help inform risk mitigation strategies for the current ongoing pandemic and future similar public health crises, emphasizing that in risk–benefit analyses, the value of humane, family-centered care and the importance of a good death be considered.
Preliminary reports from Canada and Oregon demonstrate an increase in the number of individuals receiving MAiD in 2020 [18,19]. However, it is unclear if this is related to the concern raised by Khawaja and Khawaja [14] and Salinas Mengual [15] that the pandemic is causing a ‘slippery slope’ scenario where individuals, and especially the elderly, are pushed towards the option of MAiD or if this trend is because of other reasons. Indeed, available reports in Canada demonstrate that the number of Canadians receiving MAiD has increased annually since its introduction in 2016 [18,20] and so it is possible that the increase observed in 2020 is unrelated to the pandemic. It is also possible that this increase is because of the fact that the pandemic enabled improvement in access to MAiD, and especially in access to MAiD in a home-based setting [20].
As Winston Churchill famously said, ‘Never let a good crisis go to waste’. Some of the changes imposed by the pandemic have the potential to improve the MAiD experience and should remain in place beyond the pandemic. These changes include the allowance of virtual witnessing and eligibility assessments, and the provision of MAiD in a home-based setting. In addition, the respondents in these studies remind us that there may be tensions between controlling infection and allowing for humane and patient/family-centred deaths. Those of us who work in this field must continue to advocate for those who are ill and vulnerable in the face of healthcare and public pressures that are often disproportionately focused on disease prevention of disease and cure.
CONCLUSION
Recent published research on the impact of COVID-19 on MAiD highlights the tensions between COVID-19 restrictions and individual control over the circumstances of dying, and the resulting impact on patient and family suffering and on moral injury for their MAiD providers. These reports may help inform risk mitigation strategies for the current pandemic and future similar public health crises that acknowledge the value of humane, family-centered care at the end of life.
Acknowledgements
None.
Financial support and sponsorship
None.
Conflicts of interest
There are no conflicts of interest.
REFERENCES AND RECOMMENDED READING
Papers of particular interest, published within the annual period of review, have been highlighted as:
▪ of special interest
▪▪ of outstanding interest
REFERENCES
- 1.Carr D, Boerner K, Moorman S. Bereavement in the time of coronavirus: unprecedented challenges demand novel interventions. J Aging Soc Policy 2020; 32:425–431. [DOI] [PubMed] [Google Scholar]
- 2.The coming pandemic. Psychology Today. 23 June 2020. [cited 16 June 2022]. Available at: https://www.psychologytoday.com/ca/blog/good-mourning/202006/the-coming-pandemic. [Google Scholar]
- 3.Wilson-Stronks A, Schyve P, Cordero CL, Youdelman M. Project Staff. Jointcommission.org. [cited 16 June 2022]. Available at: https://www.jointcommission.org/-/media/tjc/documents/resources/patient-safety-topics/health-equity/aroadmapforhospitalsfinalversion727pdf.pdf?db=web&hash=AC3AC4BED1D973713C2CA6B2E5ACD01B. [Google Scholar]
- 4.Agarwal M, Udare A, Alabousi A, et al. Impact of the COVID-19 pandemic on emergency CT head utilization in Ontario-an observational study of tertiary academic hospitals. Emerg Radiol 2020; 27:791–797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hannon B, Mak E, Al Awamer A, et al. Palliative care provision at a tertiary cancer center during a global pandemic. Support Care Cancer 2021; 29:2501–2507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Archer SL. Providing care for the 99.9% during the COVID-19 pandemic: how ethics, equity, epidemiology, and cost per QALY inform healthcare policy. Healthc Manage Forum 2020; 33:239–242. [DOI] [PubMed] [Google Scholar]
- 7.Stewart DE, Viens P, Muralidharan O, et al. E-survey of stressors and protective factors in practicing medical assistance in dying. J Palliat Med 2021; 24:1489–1496. [DOI] [PubMed] [Google Scholar]
- 8.Tremblay-Huet S, McMorrow T, Wiebe E, et al. The impact of the COVID-19 pandemic on medical assistance in dying in Canada and the relationship of public health laws to private understandings of the legal order. J Law Biosci 2020; 7:lsaa087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9▪.Wiebe E, Kelly M, McMorrow T, et al. How the experience of medical assistance in dying changed during the COVID-19 pandemic in Canada: a qualitative study of providers. CMAJ Open 2021; 9:E400–E405. [DOI] [PMC free article] [PubMed] [Google Scholar]; An important study detailing the impact of COVID-19 on MAiD providers.
- 10.Wiebe E, Sum B, Kelly M, Hennawy M. Forced and chosen transfers for medical assistance in dying (MAiD) before and during the COVID 19 pandemic: a mixed methods study. Death Stud 2021; 1–7. [DOI] [PubMed] [Google Scholar]
- 11.Oliver P, Wilson M, McLaren C, Jonquiere R. Providing legal assisted dying and euthanasia services in a global pandemic: lessons for ensuring service continuity. OMEGA-Journal of Death and Dying 2022; 00302228221089120. [DOI] [PubMed] [Google Scholar]
- 12▪▪.Oliver P, Jonquiere R, Wilson M, McLaren C. Providing legal assisted dying and euthanasia services in a global pandemic: provider experiences and lessons for the future. Wfrtds.org. 2022 [cited 16 June 2022]. Available at: https://wfrtds.org/wp-content/uploads/2021/02/Report-PAM-Survey-FINAL-.pdf. [Google Scholar]; The only study to date that explored the impact of COVID-19 on MAiD providers outside of Canada.
- 13.Tong E, Nissim R, Thangarasa T, et al. Medical assistance in dying (MAiD) and COVID-19: the impact of the pandemic on the experience of patients and their family caregivers. Soc Sci Med. [in press]. [Google Scholar]
- 14.Khawaja M, Khawaja A. The ethics of dying: deciphering pandemic-resultant pressures that influence elderly patients’ medical assistance in dying (MAiD) decisions. Int J Environ Res Public Health 2021; 18:8819. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Salinas Mengual J. Relationship between COVID-19, euthanasia and old age: a study from a legal-ethical perspective. J Relig Health 2021; 60:2250–2284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Goldberg R, Nissim R, An E, Hales S. Impact of medical assistance in dying (MAiD) on family caregivers. BMJ Support Palliat Care 2021; 11:107–114. [DOI] [PubMed] [Google Scholar]
- 17.Canada H. Canada.ca. [cited 16 June 2022]. Available at: https://www.canada.ca/content/dam/hc-sc/documents/services/medical-assistance-dying-annual-report-2019/maid-annual-report-eng.pdf. [Google Scholar]
- 18.Canada H. Canada.ca. [cited 16 June 2022]. Available at: https://www.canada.ca/content/dam/hc-sc/documents/services/medical-assistance-dying/annual-report-2020/annual-report-2020-eng.pdf. [Google Scholar]
- 19.Oregon.gov. [cited 16 June 2022]. Available at: https://www.oregon.gov/oha/PH/PROVIDERPARTNERRESOURCES/EVALUATIONRESEARCH/DEATHWITHDIGNITYACT/Documents/year23.pdf. [Google Scholar]
- 20.Munn E, Marshall EG. Uptake in the practice of medical assistance in dying (MAiD) and involvement by physician speciality over time in Nova Scotia, Canada. Dalhous Med J 2022; 48: [Google Scholar]