Purpose of review
Cancer screening disruption due to COVID-19 may have a significant impact on patients, healthcare practitioners, and healthcare systems. In this present review, we aim to offer a comprehensive view of the effect of the COVID-19 pandemic on cancer screening programs worldwide.
Recent findings
The present review comprised 33 publications. During the COVID-19 pandemic, the rates of cancer screening investigations were drastically reduced worldwide. Screening rates plummeted for all types of cancer, all ages, and racial/ethnic groups. Reductions in screening percentages were higher in several underserved racial groups. Cancer screening was suspended for at least 30 days in 13 countries.
Summary
Screenings for all types of cancer fell sharply. In the chain of cancer management, delays in any step are liable to change the outcome of the next step. Further long-term research will be needed to fully comprehend the impact of the pandemic on cancer services and patient outcomes.
Keywords: cancer, coronavirus disease 2019, screening
INTRODUCTION
Cancer is one of the most deadly and feared diseases in the world [1,2]. In 2020, there were 19.3 million new cases and 10 million cancer-related deaths worldwide [1]. This figure is estimated to reach 11 million by 2030 [3]. Cancer is frightening because the treatment process is painful and its effects reduce the patients’ quality of life significantly [2]. Cancer is a multifactorial disease. Several genetic and nongenetic factors create a predisposition for malignancy [4].
Screening investigations constitute an effective preventive measure to reduce the incidence of cancer and resulting mortality rates [5]. Although prevention and screening are integral to personal and population health [6], the cancer healthcare system is undergoing significant changes as a result of the COVID-19 epidemic [7]. COVID-19-related disruptions have impacted nearly every aspect of cancer control and prevention, including screening programs [8], postponed elective operations, disassembled therapy regimens [9], and furloughed healthcare providers [10]. Any interruption of secondary prevention programs delays the diagnosis and treatment of cancer in addition to facilitating advanced disease, increasing mortality rates and total years of life lost [11,12]. The Centers for Disease Control and Prevention classifies cancer and multiple noncancer conditions as high-risk diseases in the COVID-19 emergency [12]. The full impact of the pandemic is still unknown. Further research will be needed to fully comprehend its impact on cancer services and outcomes [10]. The purpose of the present systematic review of published reports was to determine the impact of COVID-19 on cancer screening programs. A simple systematic search of peer-reviewed literature published from April 2021 to April 2022 in standard databases (PubMed/MEDLINE, Scopus, and Web of Science) was performed using the following keywords ‘Cancer,’ ‘Cancer Screening,’ ‘Cancer Screening Tests,’ ‘Cancer Screening Program,’ ‘COVID 19,’ ‘Coronavirus Disease-19,’ ‘Coronavirus Pandemic,’ ‘Coronavirus Pandemic,’ ‘COVID 19 Pandemic.’ Boolean (AND, OR) operators and the MeSH terms were used for better selection of records. All types of observational studies conducted throughout the world, published in English, were included. Studies were excluded if they did not address specific findings on the effect of the coronavirus on cancer screening. Patients diagnosed with cancer before the pandemic were also excluded. Studies were selected first by title and then by abstract (L.A. and A.M.M.); their eligibility was confirmed (L.A. and I.A.) by a review of the full text. If there was disagreement between two persons, the articles were checked by a nominated third person (H.S.). All retrieved articles were entered into a database on Endnote X7. Details of all articles and results related to cancer screening were extracted and reported.
Box 1.
no caption available
INCLUDED PAPERS
We identified 481 eligible studies, of which 33 met the inclusion criteria. Six of the reviewed reports were cross-sectional studies. Ten and three studies were cohort and population-based prospective studies, respectively. The remaining reports were surveys, mixed-methods studies, prospective national investigations, descriptive studies, time series analyses, and studies of unknown design. The impact of COVID-19 on cancer screening and laboratory test samples is summarized in Table 1.
Table 1.
Impact of COVID-19 on cancer screening and pathology samples
| First author | Country | Screening type | Main results |
| Ahmed et al.[13] | Pakistan | CA19-9, PSA | Highest percentage decline was seen for PSA (−51.8%) and CA19-9 (−19%) |
| Al-Kuwari et al.[14] | Qatar | Colon and breast cancer | The breast cancer screening program dropped by 100% Colorectal cancer screening services during the COVID-19 pandemic dropped by 100% from April to July 2020 |
| Brugel et al.[15] | France | Colon and breast cancer | Colon and breast cancer screening tests fell by 86–100%, respectively All activities linked to sampling, histopathological (−48%), and biomolecular analyses (−69%) were drastically reduced |
| Chen et al.[16▪] | United States | Breast, colorectal, prostate cancers | Screening for all three cancer types dropped sharply in 2020 compared with 2019: breast (−90.8%), colorectal (−79.3%), and prostate cancer (−63.4%) |
| Dabkeviciene et al.[17] | Lithuanian | Radiology and endoscopy | Reductions in diagnostic radiology (−16%) and endoscopy (−29%) procedures |
| de Pelsemaeker et al.[18] | Belgium | Histological and cytological samples, immunohistochemistry, and molecular tests | The total number of samples received by the laboratory were reduced by 35%, which equaled a reduction of 40–45% in comparison with the 3 previous years |
| DeGroff et al.[19▪] | United States | Mammograms, Pap tests, and/or HPV tests | Total number of NBCCEDP-funded breast and cervical cancer screening tests declined by 87 and 84%, respectively, during April 2020 compared with the previous 5-year averages for that month |
| Dennis et al.[20] | United States | Mammograms, Pap tests, and sigmoidoscopy/colonoscopy | Screening percentages for 2020 were reduced from those for 2014–2019, including several underserved racial groups |
| Dos Santos et al.[21▪] | Brazil | Cervical cancer screening and mammography | More than 70% were not screened for cervical cancer More than 80% were not screened for breast cancer |
| Fisher-Borne et al.[22▪] | United States | Mammography, Pap smear, HPV, colonoscopy, and FIT | Reductions in cancer screening investigations due to COVID-19 were 77% for breast cancer, 90% for cervical cancer, and 50% for colorectal cancer |
| Laing et al.[23▪] | Canada | Pap smear or HPV, FOBT and FIT, sigmoidoscopy and colonoscopy | The mean percentage of patients appropriately screened for cervical cancer decreased by 7.5%, and those screened for colorectal cancer decreased by 8.1% |
| Marcondes et al.[24] | United States | Breast, cervical, lung, and colon cancer | Expected screening rates plummeted for all cancer screening types and all racial/ethnic groups during the COVID-19 surge |
| McBain et al.[25] | United States | Mammography and colonoscopy | Before 13 March 2020, the median weekly rate of screening mammography was 87.8 women per 10 000 beneficiaries, which declined to 6.9 in April – a 96% decline. By the end of July, this figure had rebounded to 88.2 screenings per 10 000 beneficiaries Over the same period, colonoscopy screenings declined from 15.1 per 10 000 beneficiaries to 0.9, a 95% difference, and rebounded to 12.6 per 10 000 beneficiaries by the end of July |
| Neamtiu et al.[26▪▪] | 34 European countries | Breast, cervical, and colorectal cancer | An interruption or slowdown of organized population-based cancer screening (breast, cervical, colorectal) was reported in nearly 90% of the areas |
| Selvaraja et al.[27] | India | Radiology | 91.9% (57/62) of the respondents reported that COVID-19 affected cancer screening programs at their institution/hospital |
| Vázquez Rosas et al.[28] | United States | Pap smear test, mammography, and fecal occult blood test | A significant reduction in cancer screening tests was registered (PAP smear test studies between –46 and –100%, mammography between –32 and –100%, and fecal occult blood test –73%) |
| Vigliar et al.[29] | Italy | Cytological sample | The overall cytological sample workload decreased by 41.6% in comparison with 2019. In particular, the workload declined significantly for each sample type: Pap smears –33.3%, urine –42.8%, serous fluids –14.4%, thyroid –54.5%, breast –43%, lymph node –27.3%, and salivary gland –61% |
| Villain et al.[30▪▪] | 17 low- and middle-income countries | Breast, cervical, prostate, lung, gastric, liver, oral, and colorectal cancers | Screening was suspended for at least 30 days in 13 countries The majority of the countries reported the status of their breast (16/18; 88.9%) and/or cervical (16/18; 88.9%) cancer screening programs |
| Walker et al.[11] | Canada | Breast, cervical, colorectal, and lung cancers | −41% fewer screening tests in 2020 than in 2019, and the volumes for most programs remained more than 20% below historical levels by the end of 2020 −72.9% fewer screens delivered in 2020 relative to 2019, after which volumes began to recover |
| Wilson et al.[31] | United Kingdom | Cervical and colorectal cancer | 74% of the surveyed respondents intended to attend their cervical screening and 84% intended to complete home-based CRC screening when next invited 30 and 19% of the cervical and CRC screening candidates, respectively, said they were less likely to attend a cancer screening appointment now than before the pandemic |
| Zattra et al.[32] | United States | CT imaging | Cancer screening CTs decreased by 81.7% CT volumes for cancer screening and for the initial workup did not recover to pre-COVID-19 levels in the COVID peak and postpeak period (−11.7% from baseline; −20% from baseline) The outpatient setting was particularly affected and revealed a decline of 14% from baseline for cancer screening CTs |
| Amram et al.[33] | United States | Colonoscopy and Pap test | 12.7% of patients underwent colonoscopies compared with 7.4% patients, (39.8% decrease) 10.7% of women were given Pap tests compared with 9.6% of women (7.4% reduction) |
| Carroll et al.[34] | United States | Breast, cervical, colorectal, leukemia, lung and bronchus, and prostate cancers | A clear decrease in weekly screenings and diagnoses across all cancers, particularly for regularly screened cancers The trend for leukemia screening did not differ over time, given the relative infrequency of its screening and the lack of standardized screening methods for the general population |
| Joung et al.[35▪] | United States | Mammography, breast MRI, low-dose CT scan, colorectal colonoscopy, flexible sigmoidoscopy, CT colonography, stool-based tests, barium enema, HPV test, Pap test | The majority of the facilities reported monthly screening deficits [colorectal cancer 80.6% (n = 104/129), cervical cancer 69.0% (n = 20/29), breast cancer 55.3% (n = 241/436), lung cancer 44.6% (n = 98/220)] |
| Jidkova et al.[36] | Belgium | Double read mammogram, FIT, and PAP smear | The invitation coverage for colorectal and cervical cancer screening programs remained unaffected The invitation coverage for the breast cancer screening program fell from 97.5% (2019) to 88.7% (2020), but the backlog of invitations was largely resolved in the first 6 months of 2021 The number of Pap smears during this period was just a half of those taken during the same period in 2019 (n = 20 217 vs. 45 667) |
| Kidwai et al.[37] | United States | Low-dose CT, mammography, and colonoscopy | Decline in routine cancer screening: a reduction in low-dose CTs by 49%, mammograms by 12% and colonoscopies by 55% |
| Kim et al.[38] | United States | Colon cancer, breast cancer, cervical cancer | Compared with prepandemic rates, the completion of all health screenings declined during the stay-at-home period: mammograms (OR 0.34; 95% CI 0.31–0.37), cervical cancer (OR 0.83; 95% CI 0.76–0.91), colorectal cancer (OR 0.25; 95% CI 0.23–0.28) |
| Le Bihan Benjamin et al.[39] | France | Digestive tract endoscopies, mammogram, bronchial and ENT fibroscopies, prostate biopsies, HPV test and cytopathology | In 2020, the number of mammograms decreased by 10% and digestive endoscopies by 19% Similar data were registered for bronchial and ENT fibroscopies as well as prostate biopsies An overall increase in colorectal screening and decrease in cervical screening (HPV test and cytopathology) were observed |
| Ribeiro et al.[40] | Brazil | Cytopathology and mammogram | In 2020 (pandemic period), cervical cytology tests fell by −44.6% and mammograms by −42.6% compared with the corresponding data for 2019 (prepandemic period) |
| Decker et al.[41] | Canada | Mammogram, Pap tests, FOBTs | By December 2020, there was no significant difference between the predicted and expected numbers of screening mammograms (ratio = 0.95, 95% CI 0.80–1.10) By January 2021, there was no significant difference between predicted and expected numbers of Pap tests (ratio = 0.93, 95% CI 0.81–1.06) In April 2020, there was an 83 and 81% decrease in the number of Pap tests and FOBTs, respectively The estimated cumulative deficit (backlog) from April 2020 to August 2021 was 17 370 screening mammograms, 22 086 Pap tests, and 5253 screening program FOBTs |
| Schoenborn et al.[42▪] | United States | Breast, colorectal, and prostate cancer | Overall, 293 (44.6%) participants were either screened (16.3%) or would opt for screening (28.3%) during the pandemic, whereas 120 (20.8%) participants either postponed (13.2%) or would delay screening (7.7%) |
| Shen et al.[43] | Taiwan | Cervical, breast, colorectal and oral cancers | The average percentage change declined from 15 to 40% for cervical, breast, and colorectal cancer screening, with a nearly 50% decline in oral cancer screening |
| Wenger et al.[44] | United States | Mammography, colonoscopy | Of the 41% of respondents with scheduled cancer screenings, 20% canceled or postponed the investigation The nearly 20% cancellation rate of retrospective cancer screening was stable across survey waves Persons with more numerous medical conditions were more likely to cancel or postpone cancer screening (OR 1.20, 95% CI 1.15, 1.24) |
CA19-9, cancer antigen 19–9; CI, confidence interval; CRC, colorectal cancer; CT, computed tomography; ENT, ear, nose, throat; FIT, fecal immunochemical test; FOBT, fecal occult blood test; HPV, human papillomavirus; NBCCEDP: National Breast and Cervical Cancer Early Detection Program; OR, odds ratio; PAP, papanicolaou; PSA, prostate-specific antigen.
COVID-19 AND CANCER SCREENING PROGRAM
Expected screening rates plummeted worldwide for all cancer screening types during the COVID-19 pandemic. In the United States, an interruption or a slowdown of cancer screening (breast, cervical, and colorectal) was reported in nearly 90% of the areas; 59% of centers stopped cancer screening completely [22▪]. In Canada, a population-based study by Walker et al. revealed 951 000 (−41%) fewer cancer screening tests (breast, cervical, colorectal, and lung cancer) in 2020 than in 2019, while the volumes for most programs remained more than 20% below historical levels by the end of 2020 [11]. However, a study by Fedewa et al.[45] in the United States indicated that the lung cancer screening (LCS) rate remained unchanged in 25 states and significantly increased by at least 20% in 19 states.
In studies conducted in Canada, the United States, Brazil, France, Qatar, Taiwan, and Belgium, COVID-19 had a dramatic impact on mammography and/or MRI of the breast (−10 to −100%) [11,14,15,16▪,19▪,21▪,22▪,25,28,30▪▪,34–37,40,43,44,46]. A significant drop in cancer screening computed tomography imaging in the United States (−49 to −81.7%) [32,37] and diagnostic radiology rates (−16%) was observed in Switzerland [17]. Reductions in cancer screening were reported for cervical cancer (−7.5 to −90%) in Canada, the United States, Brazil, France, Taiwan, Belgium, and 17 selected low- and middle-income countries (LMICs) [19▪,21▪–23▪,30▪▪,33,35▪,36,38–40,43,46]. A significant drop in digestive endoscopies (−19 to −29%) was reported in Lithuania and France [17,39]. Reductions in colon cancer screening (−8.1 to −95%) were registered in Canada, the United States, France, Belgium, Qatar, and 17 selected LMICs [14,15,16▪,23▪,25,30▪▪,33,35▪,36–39,43,44]. LCS rates fell in Canada, the United States, Ireland, and 17 selected LMICs (−21 to −44.6%) [11,24,30▪▪]. A significant reduction in prostate cancer screening rates (−63.4%) was reported in the United States [16▪], and oral cancer in Taiwan (−50%) [43]. Cancer screening rates were impacted according to the prevalence of COVID-19 in the respective countries, poorly controlled COVID-19 infection rates, or the preparedness of the healthcare systems in dealing with crises such as the pandemic. In France, all activities linked to sampling, histopathological (−48%), and biomolecular analyses (−69%) were drastically reduced during the COVID-19 pandemic [15]. In Italy, Vigliar et al.[29] reported a 41.6% reduction in the overall cytological sample workload compared with 2019. In particular, the workload declined significantly for each sample type: Pap tests, and/or HPV tests (–7.5–100%) in Italy and the United States [28,29,33]. The reductions in Italy were as follows: urine –42.8%; serous fluids –14.4%; breast –43%; lymph node –27.3%; and salivary gland –61% [29]. In Pakistan, Ahmed et al.[47] registered a significant drop in prostate-specific antigen (−51.8%) and cancer antigen 19–9 (−19%). A study in Canada revealed a significant reduction in fecal occult blood test by −73% [46]. According to de Pelsemaeker et al.[18], the total numbers of samples received by laboratories were reduced by 40–45% compared with the preceding three years in Belgium. A study performed by the International Agency for Research on Cancer to document the impact of the COVID-19 pandemic on the cancer screening continuum in LMICs revealed that cancer screening was suspended for at least 30 days in 13 countries [30▪▪] (Table 1).
In some studies, conducted in the United States and Ireland, screening rates for all cancer screening types, ages, and racial/ethnic groups plummeted during the COVID-19 pandemic [24,48]. However, one study in the United States showed that screening percentages in 2020 were lower than those for 2014–2019, including those in several underserved racial groups Decreases in mammography, colonoscopy, and sigmoidoscopy were higher among American Indian/Alaskan Natives, Hispanics, and multiracial participants. Decreases in Pap tests were highest among Hispanics, Whites, Asians, and African-Americans/Blacks [20]. In Canada, individuals in the oldest age groups and in low-income neighborhoods were significantly more likely to experience diagnostic delays following an abnormal breast, cervical, or colorectal cancer screening test during the pandemic, and individuals with a high probability of living on a First Nation reserve were significantly more likely to experience diagnostic delays after an abnormal fecal test [11].
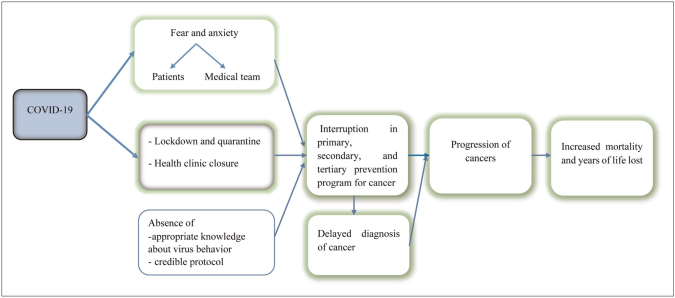
In general, interruptions in cancer screening programs have been attributed to the patients’ fear of infection, stay-at-home orders, changing hospital policies in the redeployment of staff towards critical care for the management of COVID-19 patients, triage of patients with COVID-19 infection, and the cessation of cancer screening in hospitals [49,50].
It should be noted that, in the chain of cancer management, delays in any step may alter the outcome of the next step. A reduction in the number of screening tests could result in missing the diagnosis of cancer or its recurrence (Fig. 1). Studies from various countries show that interruptions in cancer screening led to reductions in the numbers of diagnosed cancer cases, ranging from 6% in Denmark to 52% in the United States [48,51,52]. Delays in diagnosis result in a more advanced stage of disease at presentation [10], cancer in advanced stages that require more complex care, a lower likelihood of response to therapy and cure of the disease, higher costs [10,49], and poorer survival outcomes [49].
FIGURE 1.
Schematic view of the COVID-19 pandemic and comprehensive cancer prevention programs.
Based on estimations across studies, late diagnosis and advanced cancer diagnosis will lead to excess cancer mortality in 2022–2030 compared with the prepandemic period. Most deaths are anticipated before 2025 [53]. In the same vein, a study in the United Kingdom reported that there is likely to be a 20% increase in cancer-related deaths over the next 12 months because of the effect of the pandemic on healthcare systems [12].
Lessons learned in cancer care through the COVID-19 pandemic
Travel restrictions, lockdowns imposed by governments and the general fear of visiting hospitals during the acute rise in COVID-19 cases might have interfered with the screening and diagnosis of cancer patients. Furthermore, during COVID-19 pandemic, healthcare systems worldwide have struggled to maintain routine services which led to the reduction of the utilization of cancer services. In fact, medical staff, supplies, and medical activities all shifted in favor of responding to the emergency. This led to the neglect of basic, regular and essential health services. LMICs, where medical resources are inadequate and healthcare facilities scarce, may be prone to an additional risk of delayed cancer diagnoses. The consequences could be more severe for LMICs due to already low cancer screening rates as compared with developed countries. Since reductions in screening percentages were higher in several underserved racial groups, further evaluation will be needed to identify populations for whom access to cancer screening and diagnostic care has been disproportionately impacted, and quantify the impact of these service disruptions on cancer incidence, stages, and mortality rates. Coordination among partners throughout the health sector is vital to maximize resources and resume services, making health services more resilient. Important considerations including the use of mobile health systems to reach patients who are unable to access care, and the adoption of resource-based standards should be considered. Accordingly, policy-makers should consider the establishment of a flexible outreach system in the community for future pandemics. Furthermore, several years of follow-up is needed to determine whether the pandemic will translate into clinically meaningful changes in cancer incidence and stage at diagnosis, and poorer disease outcomes (e.g., mortality, survival, and quality of life). Further research will be needed to determine the most effective techniques for suspending, resuming, and maintaining cancer screening programs, as well as preparing for future interruptions, in a variety of healthcare systems.
CONCLUSION
In the COVID-19 pandemic, healthcare services were redirected away from other diseases and conditions to accommodate patients with COVID-19. Screenings for all types of cancer fell sharply. In the chain of cancer management, delays in each step are liable to alter the outcome of the next step. A late diagnosis may result in lower survival probability, fewer treatment options, more intensive treatment, and worse prognosis. The full impact is still unknown. As people throughout the world start to live with COVID-19 on a long-term basis, further research will be needed to fully comprehend the impact of the pandemic on cancer services and outcomes.
Acknowledgements
None.
Financial support and sponsorship
None.
Conflicts of interest
There are no conflicts of interest.
REFERENCES AND RECOMMENDED READING
Papers of particular interest, published within the annual period of review, have been highlighted as:
▪ of special interest
▪▪ of outstanding interest
REFERENCES
- 1.Sung H, Ferlay J, Siegel RL, et al. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin 2021; 71:209–249. [DOI] [PubMed] [Google Scholar]
- 2.Park K, Kim Y, Yang HK, Min HS. The fear of cancer from the standpoint of oneself, the opposite sex and the fear of side effects of cancer treatment. Cancer Res Treat 2020; 52:993–1001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Benson JR, Jatoi I. The global breast cancer burden. Future Oncol (London, England) 2012; 8:697–702. [DOI] [PubMed] [Google Scholar]
- 4.De Silva S, Tennekoon KH, Karunanayake EH. Overview of the genetic basis toward early detection of breast cancer. Breast Cancer Targets Ther 2019; 11:71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Loomans-Kropp HA, Umar A. Cancer prevention and screening: the next step in the era of precision medicine. NPJ Precision Oncol 2019; 3:3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Cancino RS, Su Z, Mesa R, et al. The impact of COVID-19 on cancer screening: challenges and opportunities. JMIR Cancer 2020; 6:e21697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ali JK, Riches JC. The impact of the COVID-19 pandemic on oncology care and clinical trials. Cancers 2021; 13:5924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Waterhouse DM, Harvey RD, Hurley P, et al. Early impact of COVID-19 on the conduct of oncology clinical trials and long-term opportunities for transformation: findings from an American Society of Clinical Oncology Survey. JCO Oncol Pract 2020; 16:417–421. [DOI] [PubMed] [Google Scholar]
- 9.Alkatout I, Karimi-Zarchi M, Allahqoli L. Gynecological cancers and the global COVID-19 pandemic. J Turkish German Gynecol Assoc 2020; 21:272–278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Alkatout I, Biebl M, Momenimovahed Z, et al. Has COVID-19 affected cancer screening programs? A systematic review. Front Oncol 2021; 11:675038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Walker MJ, Meggetto O, Gao J, et al. Measuring the impact of the COVID-19 pandemic on organized cancer screening and diagnostic follow-up care in Ontario, Canada: a provincial, population-based study. Prev Med 2021; 151:106586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lai AG, Pasea L, Banerjee A, et al. Estimating excess mortality in people with cancer and multimorbidity in the COVID-19 emergency. MedRxiv 2020. [Google Scholar]
- 13.Alfaro K, Mendoza L, Faron M, et al. Is COVID-19 impacting cancer screening in Pakistan? An observational study of cancer screening test requests during the pandemic. Microbiol Spectr 2021; 71:102934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Al-Kuwari MG, Abdulmalik MA, Al-Mudahka HR, et al. The impact of COVID-19 pandemic on the preventive services in Qatar. J Public Health Res 2021; 10:1910. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Brugel M, Carlier C, Essner C, et al. Dramatic changes in oncology care pathways during the COVID-19 pandemic: The French ONCOCARE-COV Study. BMC Cancer 2021; 26:e338–e341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16▪.Chen RC, Haynes K, Du S, et al. Association of cancer screening deficit in the United States with the COVID-19 pandemic. JAMA Oncol 2021; 7:878–884. [DOI] [PMC free article] [PubMed] [Google Scholar]; The cohort study showed screening deficit of 9.4 million associated with the COVID-19 pandemic for the US population. Screening declines differed by geographic region and socioeconomic status index, and use of telehealth was associated with higher screening rates.
- 17.Dabkeviciene D, Vincerzevskiene I, Urbonas V, et al. The impact of the COVID-19 pandemic on cancer patient's management—Lithuanian cancer center experience. Healthcare (Switzerland) 2021; 9:1522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.de Pelsemaeker MC, Guiot Y, Vanderveken J, et al. The impact of the COVID-19 pandemic and the associated Belgian Governmental Measures on Cancer Screening, Surgical Pathology and Cytopathology. Pathobiology 2021; 88:46–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19▪.DeGroff A, Miller J, Sharma K, et al. COVID-19 impact on screening test volume through the National Breast and Cervical Cancer early detection program, January–June 2020, in the United States. Prev Med 2021; 151:106559. [DOI] [PMC free article] [PubMed] [Google Scholar]; Results of this study showed a significant decline in screening tests during COVID-19 pandemic for both cancers with decreases evident across geography, ethnic and racial group, and rurality.
- 20.Dennis LK. Reduction in standard cancer screening in 2020 throughout the U.S. Cancers 2021; 13:5918. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21▪.Dos Santos L, Stevanato KP, Roszkowski I, et al. Impact of the covid-19 pandemic on women's health in Brazil. J Multidisciplinary Healthcare 2021; 14:3205–3211. [DOI] [PMC free article] [PubMed] [Google Scholar]; The cross-sectional study showed a significant decrease in women's access to the healthcare system during this pandemic. This article highlights that it is too soon to determine the real impact of the COVID-19 Pandemic on Women's health; most consequences would come in the middle and long term.
- 22▪.Fisher-Borne M, Isher-Witt J, Comstock S, Perkins RB. Understanding COVID-19 impact on cervical, breast, and colorectal cancer screening among federally qualified healthcare centers participating in “Back on track with screening” quality improvement projects. Prev Med 2021; 151:106681. [DOI] [PMC free article] [PubMed] [Google Scholar]; In this study, the telehealth and self-sampling in maintaining cancer screening services during the pandemic is important, but the impact of these strategies may be limited by continued pandemic-related disruptions and the inability to do most screenings at home.
- 23▪.Laing S, Johnston S. Estimated impact of COVID-19 on preventive care service delivery: an observational cohort study. BMC Health Serv Res 2021; 21:1107. [DOI] [PMC free article] [PubMed] [Google Scholar]; In this observational study, the mean percentage of patients appropriately screened for cancer decreased. Even, virtual care and reopening measures could not restore the provision of preventive care services. Therefore, additional, system-wide primary care and laboratory capacity will be needed to restore pre-COVID-19 screening rates.
- 24.Marcondes FO, Cheng D, Warner ET, et al. The trajectory of racial/ethnic disparities in the use of cancer screening before and during the COVID-19 pandemic: a large U.S. academic center analysis. Prev Med 2021; 151:106640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.McBain RK, Cantor JH, Jena AB, et al. Decline and rebound in routine cancer screening rates during the COVID-19 pandemic. J Gen Intern Med 2021; 36:1829–1831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26▪▪.Neamtiu L, Martos C, Giusti F, et al. Impact of the first wave of the COVID-19 pandemic on cancer registration and cancer care: a European survey. Eur J Public Health 2022; 32:311–315. [DOI] [PMC free article] [PubMed] [Google Scholar]; The article describes the effect of the COVID-19 pandemic on cancer program in Europe. This article highlights the cancer programs were disrupted, due to changes in the work modalities for the personnel, as well as to the difficulties in accessing sources and/or receiving the notifications. In some regions, staff was allocated to different activities related to controlling the pandemic.
- 27.Selvaraja VK, Gudipudib DK. Impact of the COVID-19 pandemic on work routine, practice and mental state of radiation oncologists in India: an online survey. Respirology (Carlton, VIC) 2021; 15:1165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Vázquez Rosas T, Cazap E. Social distancing and economic crisis during COVID-19 pandemic reduced cancer control in Latin America and will result in increased late-stage diagnoses and expense. JCO Glob Oncol 2021; 7:694–703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Vigliar E, Cepurnaite R, Iaccarino A, et al. Cytopathology practice during the COVID-19 postlockdown: an Italian experience. Cancer Cytopathol 2021; 129:548–554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30▪▪.Villain P, Carvalho AL, Lucas E, et al. Cross-sectional survey of the impact of the COVID-19 pandemic on cancer screening programs in selected low- and middle-income countries: study from the IARC COVID-19 impact study group. Int J Cancer 2021; 149:97–107. [DOI] [PMC free article] [PubMed] [Google Scholar]; In this study, 17 low- and middle-income countries (LMICs) countries participated. This article highlights cancer screening was suspended in 13 countries, while diagnostic-services for screen-positives were suspended in nine countries. Although many of the LMICs were deficient in following the ‘best practices’ to minimize service disruptions, at least some of them made significant efforts to improve screening participation, treatment compliance and program organization. Innovative strategies adopted by the programs to keep services on-track should be mutually shared.
- 31.Wilson R, Quinn-Scoggins H, Moriarty Y, et al. Intentions to participate in cervical and colorectal cancer screening during the COVID-19 pandemic: a mixed-methods study. Prev Med 2021; 153:106826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Zattra O, Fraga A, Lu N, et al. Trends in cancer imaging by indication, care setting, and hospital type during the COVID-19 pandemic and recovery at four hospitals in Massachusetts. Cancer Med 2021; 10:6327–6335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Amram O, Amiri S, Robison J, et al. COVID-19 and inequities in colorectal and cervical cancer screening and diagnosis in Washington State. Cancer Med 2022; doi: 10.1002/cam4.4655. [Online ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Carroll R, Duea SR, Prentice CR. Implications for health system resilience: quantifying the impact of the COVID-19-related stay at home orders on cancer screenings and diagnoses in southeastern North Carolina, USA. Prev Med 2022; 158:107010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35▪.Joung RH, Nelson H, Mullett TW, et al. A national quality improvement study identifying and addressing cancer screening deficits due to the COVID-19 pandemic. Cancer 2022; 128:2119–2125. [DOI] [PMC free article] [PubMed] [Google Scholar]; In this prospective study, the majority of facilities reported screening deficits, but geographic differences were not observed.
- 36.Jidkova S, Hoeck S, Kellen E, et al. Flemish population-based cancer screening programs: impact of COVID-19 related shutdown on short-term key performance indicators. BMC Cancer 2022; 22:183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Kidwai N. Routine cancer screening delays due to pandemic at veteran affairs. J Nat Med Assoc 2022; 114:12–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Kim E, Kojima N, Vangala S, et al. Impact of COVID-19 on primary care quality measures in an academic integrated health system. J Gen Intern Med 2022; 37:1161–1168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Le Bihan Benjamin C, Simonnet JA, Rocchi M, et al. Monitoring the impact of COVID-19 in France on cancer care: a differentiated impact. Sci Rep 2022; 12:4207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Ribeiro CM. Short-term effects of the COVID-19 pandemic on cancer screening, diagnosis and treatment procedures in Brazil: a descriptive study, 2019–2020. Int J Environ Res Public Health 2022; 31:e2021405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Sakai CM, Sakai P, Nahas S, et al. Evaluating the impact of the COVID-19 pandemic on cancer screening in a central Canadian province. J Med Screen 2022; 155:106961. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42▪.Schoenborn NL, Boyd CM, Pollack CE. Impact of the COVID-19 pandemic on cancer screening attitudes, intentions, and behaviors in older adults. J Am Geriatr Soc 2022; 70:67–69. [DOI] [PMC free article] [PubMed] [Google Scholar]; The cross-sectional study by univariable models highlights that age, predicted 10-year mortality risk, race, education, health literacy, local COVID-19 case rate, or concern about COVID-19 were not significantly associated with choosing ‘screen’ versus ‘delay.’
- 43.Shen CT, Hsieh HM, Chang YL, et al. Different impacts of cancer types on cancer screening during COVID-19 pandemic in Taiwan. J Formos Med Assoc 2022; doi: 10.1016/j.jfma.2022.02.006. [Online ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Wenger NS, Stanton AL, Baxter-King R, et al. The impact of COVID-19 on routine medical care and cancer screening. J Gen Intern Med 2022; 37:1450–1456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Fedewa SA, Bandi P, Smith RA, et al. Lung cancer screening rates during the COVID-19 pandemic. Chest 2022; 161:586–589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Decker KM, Feely A, Bucher O, et al. Evaluating the impact of the COVID-19 pandemic on cancer screening in a central Canadian province. Prev Med 2022; 155:106961. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Ahmed DS, Abbas Abid DM, Niaz Ali MN, et al. Is COVID-19 impacting cancer screening in Pakistan? An observational study of cancer screening test requests during the pandemic. Ann Med Surg 2021; 71:102934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Hamilton AC, Donnelly DW, Loughrey MB, et al. Inequalities in the decline and recovery of pathological cancer diagnoses during the first six months of the COVID-19 pandemic: a population-based study. Br J Cancer 2021; 125:798–805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Patt D, Gordan L, Diaz M, et al. Impact of COVID-19 on cancer care: how the pandemic is delaying cancer diagnosis and treatment for American seniors. JCO Clin Cancer Inform 2020; 4:1059–1071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Hajek A. Determinants of postponed cancer screening during the COVID-19 pandemic: evidence from the nationally representative COVID-19 snapshot monitoring in Germany (COSMO). Ther Adv Gastroenterol 2021; 14:3003–3011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Skovlund CW, Friis S, Christensen J, et al. Drop in cancer diagnosis during the COVID-19 pandemic in Denmark: assessment of impact during. Acta Oncol 2020; 2022:1–4. [DOI] [PubMed] [Google Scholar]
- 52.Kaufman HW, Chen Z, Niles J, Fesko Y. Changes in the number of US patients with newly identified cancer before and during the coronavirus disease 2019 (COVID-19) pandemic. JAMA Network Open 2020; 3:e2017267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Ward ZJ, Walbaum M, Walbaum B, et al. Estimating the impact of the COVID-19 pandemic on diagnosis and survival of five cancers in Chile from 2020 to 2030: a simulation-based analysis. Lancet Oncol 2021; 22:1427–1437. [DOI] [PMC free article] [PubMed] [Google Scholar]