Purpose:
Following COVID-19 infection a rising count of rhino-orbito-cerebral mucormycosis is observed, requiring orbital exenteration, a disabling lifetime affecting surgery. One of the potential interventions for globe salvage in these patients is retrobulbar injections of amphotericin B. This study was conducted to review protocols, outcomes, and side effects of retrobulbar injection of amphotericin B in patients with COVID-19 associated rhino-orbito-cerebral mucormycosis (CAM).
Methods:
The PubMed, Scopus, Web of Science, and Embase databases were searched using a comprehensive string of relevant keywords. All English studies with the confirmed diagnosis of CAM infection were included. We excluded all studies in which retrobulbar injection of amphotericin B was not implemented in any of the patients or there was a lack of clarified and detailed data about this procedure among participants.
Results:
A total of 647 cases had a history of retrobulbar injection(s) of amphotericin B in 13 reviewed studies with 3,132 subjects of CAM. The most common protocol was the retrobulbar injection of 1 ml of 3.5 mg/ml liposomal amphotericin B for 3 doses daily or on alternate days. We discerned that the globe salvage rate was 95.0% in eyes with a history of retrobulbar injection(s). The total rate of orbital exenteration was 14.9%, regardless of the history of retrobulbar injection of the drug. Other outcomes of this intervention were vision salvage and reduced major ophthalmic complaints, including pain, swelling, chemosis, ptosis, and ophthalmoplegia. The side effects of this intervention were not serious, and most of them were transient. They included swelling at the injection site, restriction of ocular motilities, exacerbation of orbital inflammation, and even intensification of visual impairment in a few cases.
Conclusions:
Retrobulbar injection of amphotericin B should be considered a nearly safe and protective intervention against orbital exenteration in patients with CAM. It may also be effective in saving vision. Since the effectiveness of orbital exenteration in the survival of patients is not ascertained, retrobulbar injections can be considered an alternative intervention.
Retrobulbar injection of amphotericin B is a nearly safe procedure which can lead to eye globe salvage and reducing the rate of orbital exenteration in patients with COVID-19 associated orbital mucormycosis.
The coronavirus disease 2019 (COVID-19, caused by the novel SARS-CoV-2) pandemic has created distinctive challenges for healthcare systems, including secondary infections, which are more common in admitted to the hospital and severely ill patients with COVID-19. Recently, rhino-orbito-cerebral mucormycosis (ROCM) has impacted a sizeable population in several countries. The majority of the cases were diagnosed several days to a few weeks after admission for COVID-19.1–4 Mucormycosis is a form of Zygomycosis caused by Mucorales species of the phylum Zygomycota,5 causing a highly angioinvasive disease and leading to vascular thrombosis and tissue necrosis with high morbidity and mortality.6,7 ROCM is the most common clinical manifestation of mucormycosis, with a very invasive infection having a mortality rate between 25% and 80%.8–10 Diabetes mellitus, especially with poor glycemic control, and systemic administration of corticosteroids are the major contributing factors in developing the disease.6–10 The major known risk factors for COVID-19 associated ROCM (CAM) are immune system dysfunctions, administration of systemic steroids, altered glucose homeostasis, and mechanical ventilation performed in severe cases.11–13
One of the significant mucormycosis morbidities is the orbital involvement which may need substantial orbital debridement surgeries, including orbital exenteration in patients with a life-threatening disease. However, according to previously published studies, the role of orbital exenteration in the survival rate is controversial.14–17 In addition, this procedure has lifelong disabling effects. Recently, the impact of direct delivery of antifungal agents to the involved orbital cavity has been highlighted as a possible intervention for globe salvage in patients with orbital mucormycosis.18,19 In this systematic review, the outcomes of retrobulbar injection of amphotericin B in patients with CAM were assessed to help clinicians, especially ophthalmologists, make a better plan for disease management.
METHODS
The guidelines provided by the Preferred Reporting Items for Systematic Reviews and Meta-Analyses statement were followed in this systematic review.20
Search Strategy
We used a comprehensive search string of keywords, provided in File, Supplemental Digital Content 1, available at http://links.lww.com/IOP/A339, to look for relevant studies until the end of March 2022 published on the PubMed, Web of Science, Embase, and Scopus databases. Moreover, we looked for any remaining relevant studies based on the reference lists of the included studies.
Eligibility Criteria
Study Type
Original peer-reviewed English studies, including cross-sectional and cohort studies, case reports, and case series, were considered for inclusion. Therefore, letters to the editors, editorials, meeting abstracts, and review studies were excluded. Furthermore, we defined our criteria for eligibility based on the PICO (i.e., population, intervention, comparator, and outcome) framework.21
Population
Only those with the confirmed diagnosis of the CAM infection (both COVID-19 and mucormycosis) were of interest. However, the clinical status and the timing of disease in these individuals, their age, sex, prior history of mucormycosis, recent or daily medications, including diabetes mellitus (or even the presence of diabetic ketoacidosis), hypertension, renal or hepatic diseases were not subject to limitations.
Intervention
We only included studies in which at least 1 affected individual received a local retrobulbar injection(s) of amphotericin B in any dosage or form (i.e., liposomal or deoxycholate). However, whether they also received the medication via the systemic route or not was not considered a limit.
Comparator
Whether the included studies compared the globe salvage rates of retrobulbar amphotericin B with orbital exenteration in the CAM-suffering individuals was not a subject of limitations. However, to better assess the mentioned rates, the outcome of other appropriate interventions in the studies was also of high interest.
Outcome
The primary outcome of our interest was whether the globe could be salvaged in the mentioned individuals. Moreover, the reductions in ophthalmic-related complaints were noted. In addition, the secondary outcome was the frequency of experienced drug-related adverse events following the retrobulbar injection of amphotericin B.
Exclusion Criteria
We excluded all studies in which retrobulbar injection of amphotericin B was not implemented in any of the patients or there was a lack of clarified and detailed data about this procedure among participants. Also, patients without systemic antifungal treatments were excluded from the study, regardless of history of retrobulbar injection of the drug. Retrobulbar injection of the drug is off labeled and routinely considered as an adjuvant treatment. Nevertheless, it is administered alongside systemic antifungal treatment and surgical debridement of the involved sites to enhance the outcome of the disease.18,19 Furthermore, patients without a confirmed new-onset or previous diagnosis of COVID-19 or fungal infections other than mucormycosis were excluded. Furthermore, non-English studies and commentaries, conferences, letters to the editors, editorials, and reviews were excluded.
Study Selection
Via the 20th version of Endnote,22, the identified records were scanned for existing duplicates, removed by its automated tool, and then manually double-checked. The remaining records were then uploaded to Rayyan’s systematic review web app through which the screening rounds were performed.23 Two authors then independently assessed each record’s relevancy based on its title and abstract. The full texts of those deemed relevant were then evaluated independently by 2 other authors to see whether they were eligible. Moreover, the senior author resolved any conflicts in the mentioned process.
Quality Assessment
We opted to evaluate the methodological quality of the included studies by the tools provided by the Joanna Briggs Institute, consisting of checklists for cohort, cross-sectional, case reports, and case series studies, having 12, 8, 8, and 10 items for investigation, respectively.24
Data Management
Two authors independently extracted the data for the following items from the included studies, including the study’s bibliographic characteristics and design, the number of patients, patient characteristics and comorbidities, the time from COVID-19 to mucormycosis diagnosis, presence or absence of intracranial involvement, ophthalmic presentations of the disease, administration of systemic corticosteroids for the management of COVID-19, the antifungal drug(s) that was used, the characteristics of retrobulbar injections of antifungal drugs (including indications, protocols, outcomes, and side effects), any adjunct surgery performed for mucormycosis including paranasal sinuses debridement and orbital exenteration (with its outcome), and reported patient outcome (alive, or deceased). These data were then qualitatively synthesized primarily based on the effectiveness and clinical outcomes of the retrobulbar amphotericin B injection in CAM.
RESULTS
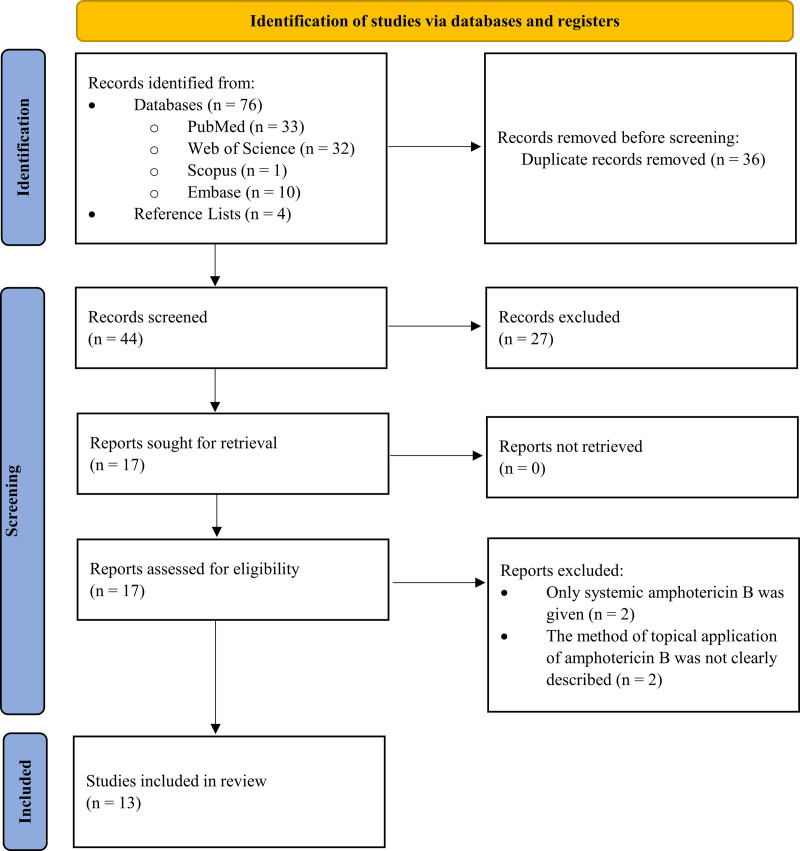
We identified 76 records from our database search, 36 of which were duplicates and therefore removed. Out of the 40 remaining studies, 27 were also irrelevant, leading to the evaluation of 13 full text studies of which 9 were included. In addition, 4 studies were included from the reference lists of the included studies, which meant that 13 studies (including 6 retrospective or prospective longitudinal, 1 cross-sectional, 2 case series, and 4 case reports studies) were included in our qualitative synthesis (Fig.).
FIG.
The systematic review flow diagram.
The ages of presentation of CAM were between 11 and 75 years. Two thousand two hundred fourteen of 3,132 (70.7%) of the patients were male. In all the cases, the diagnosis of COVID-19 was based on a reverse transcriptase-polymerase chain reaction test on nasopharyngeal/oropharyngeal swabs, and mucormycosis was confirmed by histopathology or culture. In 18.6% of the individuals, signs of intracranial involvement were detected. Moreover, among those with CAM, diabetes mellitus was the most common comorbid condition (2,381/3,048, 78.1%), while the use of systemic corticosteroids related to COVID-19 treatment was the most common risk factor (2,256/2,588, 87.2%). For treatment, amphotericin B was the most common antifungal drug used solely or in combined regimens (2,980/3,132, 95.1%), followed by paranasal sinuses surgeries and debridement (1,785/2,642, 67.6%). Furthermore, the mortality rate was 11.8% (364/3,072).
The most common presenting ophthalmic signs were periorbital swelling (62.6%), visual loss (60.5%), ptosis (53.2%), ophthalmoplegia (51.8%), and proptosis (39.6%). Moreover, other common findings were periocular hypoesthesia, pain, and chemosis.
The most commonly undertaken ophthalmic interventions were retrobulbar injection of amphotericin B (647/2,645, 24.5%) and orbital exenteration (390/2,619, 14.9%). Although the protocols for retrobulbar injections varied among the reviewed studies, the more common form of the drug injected was in the form of liposomal with a dosage of 1 ml of 3.5 mg/ml solution.25–31 Moreover, the frequency of injections was between 1 and 9 doses with intervals between 1 and 10 days. In 1 study, the drug was delivered in the orbital cavity for 5 days by insertion of an intravenous cannula.32 In another study, combined intravitreal and retrobulbar injections were done in patients with endophthalmitis.27 Although the outcomes of protocols for retrobulbar injections among the reviewed studies cannot be compared with each other by statistical analysis due to inadequate data, but these studies revealed that the effectiveness of the injections in reducing signs of orbital disease is higher among cases with minimal orbital involvement, and that advanced cases needed more injections exhibiting poorer responses to the injections.25–27
Globe salvage rate was 95.0% (494/520) following retrobulbar injections of the drug. The total rate of orbital exenteration was 14.9% (390/2,619), regardless of the history of retrobulbar injection of the drug. In addition, following orbital exenteration, the survival rate was 79.0% (143/181) (Table 1). However, due to the lack of sufficient data, a meta-analysis of the outcomes of ophthalmic interventions was not possible among the different groups of patients.
TABLE 1.
Characteristics of retrobulbar injection of amphotericin B and orbital exenteration with their outcomes
| Author/type of the study | Region | Number of cases | Retrobulbar Injection of amphotericin B | Protocol of retrobulbar amphotericin B injections | Globe salvage following retrobulbar injections, N (%) | Total orbital exenteration, N (%) | Survival following orbital exenteration | ||
|---|---|---|---|---|---|---|---|---|---|
| Form | Dosage | Frequency and intervals, N (%) | |||||||
| Sen et al.,35 retrospective observational study | India | 2,826 | 511/2,332 (21.9) | Liposomal or dexoycholate | Not mentioned. | Mean: 2 doses (range: 1–9) | 377/381 (99.0) | 339/2,327 (14.6) | 128/164 (78.0) |
| Ramamurthy et al.,25 prospective study | India | 75 (82 eyes) | 82 (100) | Liposomal | 1 ml/3.5 mg | 3 doses: 64 (78.0), 5 doses: 15 (18.3), <3 doses: 3 (3.7); on alternate days |
70/82 (85.4) | 12/82 (14.6) | Not mentioned. |
| Choksi et al.,26 retrospective case-control study | India | 73 | 18 (24.7) | Liposomal | 1 ml/3.5 mg | 1 dose: 7 (38.9), 2 doses: 4 (22.2), 3 doses: 4 (22.2), 2–3 doses with variable intervals: 3 (17); on alternate days |
15/18 (83.3) | 5/52 (9.6) | 3/5 (60.0) |
| Arora et al.,28 cross-sectional study | India | 60 | 6 (10) | Liposomal | 1 ml/3.5 mg | 3 doses: 6 (100), daily | 6/6 (100) | 2/60 (3.3) | 2/2 (100) |
| Dave et al.,30 retrospective interventional study | India | 58 | 1 (1.7) | Liposomal | 1 ml/3.5 mg | 5 doses, daily | Yes | 22/60 (36.7) | Not mentioned. |
| Nair et al.,54 retrospective study | India | 13 | 5 (38.5) | Liposomal | Not mentioned. | 2 doses: 2 (40), 3 doses: 3 (60) |
4/5 (80.0) | 8/13 (61.5) | 8/8 (100) |
| Bayram et al.,27 prospective observational study | Turkey | 11 | 11 (100) | Liposomal | 1 ml/3.5 mg | 2.2 ± 0.6 doses: 5 (45.5), 2.3 ± 0.5 doses: 6 (54.5); interval: 2–8 days (intravitreal injections in 6 cases) | 11/11 (100) | 0/11 (0) | – |
| Singh et al.,33 case series | India | 6 | 3 (50.0) | Liposomal | 1 ml/3.5 mg | 1 dose: 1 (16.7), 4 doses: 1 (16.7), 5 doses: 1 (16.7); interval: 2–10 days |
3/3 (100) | 0/3 (0) | – |
| Jhunjhunwala et al.,55 case series | India | 4 | 4 (100) | Not mentioned. | Not mentioned in details. | 2 doses: 2 (40), 3 doses: 3 (60) |
4/4 (100) | 0/4 (0) | – |
| Murthy et al.,32 case report | India | 2 | 2 (100) | Deoxycholate | 2 ml/10 mg | 5 doses: 2 (100); daily | 2/2 (100) | 0/2 (0) | – |
| Diwakar et al.,29 case report | India | 2 | 2 (100) | Liposomal | 1 ml/3.5 mg | Multiple doses: 2 (100); on alternate days | 0/2 (0) | 2/2 (100) | 2/2 (100) |
| Mekonnen et al,31 case report | USA | 1 | Yes | Liposomal | 1 ml/3.5 mg | 3 doses, daily | Yes* | No* | - |
| Singh et al.,34 case report | India | 1 | Yes | Liposomal | 1 ml/3.5 mg | 3 doses, daily | Yes | No | – |
| Total | 3,132 | 647/2,645 (24.4) | Frequency: 1–9 doses; intervals: 1–10 days | 494/520 (95.0) | 390/2,619 (14.9) | 143/181 (79.0) | |||
The patient was intubated and ICU admitted, and orbital exenteration was not possible.
The specific indications (except for trying to save the globe) for retrobulbar injections included moderate to severe visual loss, cranial neuropathy, signs of orbital apex involvement in MRI, and progression of the disease in patients who were not a candidate for orbital exenteration. In addition, the injection may reduce the load of orbital disease and thus postpone future surgeries.25,28–31,33,34 The outcomes of retrobulbar injections (except for globe salvage) were a preserved or enhanced ocular state through a reduction in ophthalmic signs including visual impairment, pain, swelling, ptosis, proptosis, and extraocular motility restriction.25,26,33–35 Occurrence of side effects was rare and, in some, transient. These adversities included aggravation of orbital inflammation, visual impairment, swelling, chemosis, ptosis, and extraocular motility restriction (Table 2).25,26,34 Choksi et al.26 showed that the most commons adverse effects after the injections were exacerbation of eyelid swelling and chemosis (in 44% and 33% of the injected eyes, respectively). They found that all adverse effects occurred in cases with repeated injections. Similarly, Singh et al.34 reported an initial increase in the periorbital swelling after 3 injections in their patient. Most of the adverse effects were transient and were managed successfully in the reviewed studies. Ramamurthy et al.25 found deterioration of orbital inflammation signs (including chemosis and conjunctival congestion) was the most common post-injections adverse effect (in 23.2% of the injected eyes), which was transient. They reported swelling at the site of injection (in 4.9% of the injected eyes) due to local inflammatory reaction to the drug, which was treated with local antibiotics and anesthetics. They observed aggravation of vision and ocular motility limitations following 3 injections just in 2.4% of the injected eyes. It could possibly be due to disease progression, rather than to drug toxicity.
TABLE 2.
Indications, other outcomes, and side effects of retrobulbar injection of amphotericin B
| Author/ Type of the study | Region | Number of cases with retrobulbar injections | Indications | Other Outcomes (except globe salvage), N (%) | Side Effects, N (%) |
|---|---|---|---|---|---|
| Sen et al.,35 retrospective observational study | India | 511 | They are not mentioned. | Vision salvage: 126/330 (38) | They are not mentioned. |
| Ramamurthy et al.,25 prospective study | India | 82 | • Orbital disease in COVID-19-positive patients and who were oxygen dependent. • Reducing the disease load for the patients who candidate for huge orbital surgeries. |
• Retained/improved vision: 52 (63.4) • Pain relief: 59 (71.9) • Reduced swelling/eyelid edema: 48 (58.5) • Improvement of drooping: 17 (20.7) • Reduced chemosis: 11 (13.4) • Reduced proptosis: 5 (6.1) • Reduced ptosis: 10 (12.0) • Improved ocular motility: 14 (17.1) |
• Transient swelling at the site of injection: 4 (4.9) • Worsening of vision: 2 (2.4) • Worsening of ocular motility restriction: 2 (2.4) • Transient orbital inflammation with an increase in chemosis and conjunctival congestion: 19 (23.2) (Seen in patients with repeated injections) |
| Choksi et al.,26 retrospective case-control study | India | 18 | They are not mentioned. | • Stable ophthalmic condition: 8 (44) • Improved ophthalmic signs: 2 (11) • 5 (28) patients died, compared with 12 of 29 (41) who did not receive retrobulbar amphotericin (P = 0.63). |
Worsening of: • Eyelid edema: 8 (44) • Chemosis: 6 (33) • Extraocular movement restriction: 4 (22) • Ptosis: 2 (11) (All them were seen in patients with repeated injections) |
| Arora et al.,28 cross-sectional study | India | 6 | Stage 3 ROCM with diffuse or apical enhancement on contrast-enhanced MRI. | They are not mentioned. | They are not mentioned. |
| Dave et al.,30 retrospective interventional study | India | 1 | Localized orbital apex involvement with contrast uptake in MRI. | They are not mentioned. | They are not mentioned. |
| Singh et al.,33 case series | India | 6 | • Visual loss • Localized orbital apex involvement with contrast uptake in MRI |
• Improved vision: 1 (16.7) • Reduced ptosis: 2 (33.4) |
They are not mentioned. |
| Diwakar et al.,29 case report | India | 2 | To halt orbital disease progression in 2 pediatric patients with cerebral involvement. | They are not mentioned. | They are not mentioned. |
| Mekonnen et al.,31 case report | USA | 1 | To halt orbital disease progression in an intubated and ICU-admitted patient (without the possibility of orbital exenteration). | They are not mentioned. | They are not mentioned. |
| Singh et al.,34 case report | India | 1 | • Moderate to severe visual loss • Subtle localized orbital enhancement (on MRI) with cranial neuropathy • Moderate to diffuse orbital enhancement or apical enhancement of orbit on contrast MRI • Loss of enhancement of surgically accessible orbital area (not involving apex) |
• Improved vision • Reduced ptosis • Reduced proptosis • Reduced ophthalmoplegia |
Transient periorbital swelling. |
DISCUSSION
In hospitalized and severely ill patients with COVID-19, secondary infections, including ROCM, are more common. The main contributing factors for this deadly disease in the COVID-19 era are pre-existing diabetes mellitus and consumption of intravenous corticosteroids, which are commonly administrated in COVID-19 to reduce lung injury and respiratory failure.11–13 Diabetes was the most common comorbidity factor in the study, similar to previous reviews among patients with CAM.36 In this study, the pooled prevalence of diabetes mellitus was 78.1%, similar to what has been reported previously (66.4–85.8%).1,37–42 Here, systemic corticosteroids given as the COVID-19 treatment was the most common predisposing factor (87.3%). Moreover, previous reviews reported their prevalence within a range of 76.3% to 94.3%.1,39–42
The present review revealed that the pooled prevalence of intracranial involvement in patients with CAM was 18.6%. In previous systematic reviews, this rate varied between 22.2% and 48.2%.1,40–42
The overall mortality rate among CAM patients was 11.8%, which is lower than previous reviews (25.6–33.6%).1,37,39–42 The lower rate of mortality in our study can be explained by the lower percentage of patients with intracranial involvement compared with the previous reviews and, therefore, as the mortality rate of mucormycosis is known to be highly dependent on the involved site, meaning that a disseminated infection is the most fatal.43
In a study by Bhattacharyya et al.39 the most commonly reviewed ophthalmic signs of the disease were ptosis, eyelid edema, proptosis, ophthalmoplegia, and vision loss, respectively. Although the order of these signs was somewhat different in our study, these signs were the same.
The most common management of patients with CAM is administering intravenous amphotericin B, solely or in combination with other antifungal medications, followed by surgical debridement of involved paranasal sinuses.44 In this study, most of the patients (95.2%) received intravenous liposomal (more common) or deoxycholate amphotericin B (solely or in combined regimens) with paranasal sinuses debridement surgery (67.5%).
Ophthalmic interventions for patients with CAM include direct administration of an antifungal drug to the orbital cavity and extensive tissue debridement in specific cases.45 The most common route for direct drug delivery to the orbital cavity is retrobulbar injection. Administration of amphotericin B via retrobulbar injection is recommended to improve signs of orbital involvement and subsequent complications. Retrobulbar injection of amphotericin B is recommended in patients with signs of optic nerve compression, including a progressive decrease in visual acuity and positive relative afferent pupillary defect. In addition, this route of drug administration is recommended when other symptoms and signs of orbital involvement, including pain, proptosis, globe firmness, limitation of extraocular motility or conjunctival chemosis, and ocular surface exposure continue despite complete systemic medical and surgical interventions.18,19,46 This route of drug delivery is reported to be effective in improving cerebritis in patients with intracranial involvement.47 Orbital MRI with contrast is useful to evaluate patients needing retrobulbar injections. By this imaging technique, the extension of the infection and the presence of the devascularized tissue can be assessed. Tissues with enhancement are compatible with infectious sites and benefit from retrobulbar administration of the drug, but devascularized tissues have no contrast enhancement and benefit from debridement rather than antifungal treatment.48–50 In this review, the most common indication for retrobulbar injections was globe salvage and decreased rate of orbital exenteration. In our reviewed studies, the specific indications for retrobulbar injection of the drug were visual loss, signs of orbital apex involvement, and progression of the disease despite appropriate systemic medical and surgical treatments.25,28–31,33,34 Similar indications were elucidated by Hirabayashi et al.19 In addition, we found that this route of the drug administration should be considered in earlier stages, especially in cases that are not good candidates for extensive surgical interventions (i.e., pediatrics and admitted patients to an intensive care unit, ICU).29,31 In the COVID-19 era, many cases are admitted to the ICU and, therefore, are not candidates with favorable outcomes following surgical interventions (including paranasal sinuses and orbital debridements). Therefore, this route of administration is a relatively superior choice for the mentioned individuals.
The recommended dose of retrobulbar injection is 3.3 to 3.5 mg/1 ml of liposomal (preferred) amphotericin B. Moreover, even though there is no protocol for the frequency of the drug injections, some reports recommend at least 3 continuous injections for 3 days.19 In this study, we found that practically different drug forms (liposomal or deoxycholate) were injected with different frequencies and intervals. Moreover, the most common protocol was the retrobulbar injection of 1 ml of 3.5 mg/ml liposomal amphotericin B for 3 doses daily or on alternate days.
Reports showed that an on-time decision for administering the antifungal is essential in achieving acceptable results.18,19 as we found the globe salvage rate to be 95.0% in eyes with a history of retrobulbar amphotericin B injection. In addition, this route of administration led to vision salvage and reduced major ophthalmic complaints, including pain, swelling, chemosis, ptosis, and ophthalmoplegia.
However, this intervention can also cause adverse effects. The retrobulbar injection is a risky intervention that may cause globe perforation by the syringe needle, retrobulbar hemorrhage, and even an inadvertent drug administration to the brain stem. Therefore, the procedure must be done sterile and by expert clinicians. In addition, amphotericin B, especially in deoxycholate form, has neurotoxic effects and potentially can cause optic neuropathy, so setting the correct dose is necessary.19,51 There are few reports about transient and self-limited side effects of the drug after retrobulbar injections, including orbital compartment syndrome, the flare-up of orbital inflammation, and deteriorating orbital symptoms and signs, especially after the first injection with the deoxycholate form.52,53 In this review, we found some side effects, including swelling at the injection site, restriction of ocular motilities, exacerbation of orbital inflammation, and even aggravation of visual impairment. However, even though these side effects were more common in those with repeated injections, these complications were not severe, and most of them were transient.
Kamat et al.40 showed that the prevalence of orbital exenteration in patients with CAM was 11.1%. Similarly, we found that the total rate of orbital exenteration was 14.9%, regardless of the retrobulbar injection history. However, we also found that this procedure was merely done in 5.0% of eyes with retrobulbar injection. This difference can be interpreted as the potential protective effect of retrobulbar injections against orbital exenteration, but it requires further studies with larger samples which allow for statistical analysis. Previous reports showed that retrobulbar injection of amphotericin B might prevent disease progression and orbital exenteration.19,47 In a study by Ashraf et al.,18 the investigators showed that the application of retrobulbar injection of amphotericin B for fungal rhino-orbital sinusitis might decrease the need for orbital exenteration without a significant increase in mortality rate. Choksi et al.26 revealed that retrobulbar injections decrease the rate of orbital exenteration but cannot reduce the risk of mortality among patients with CAM.
In addition, we confirmed that in patients with orbital exenteration, the survival rate was 79.0%. In a study by Sen et al.,35 in patients with CAM, the investigators showed a significant decrease in mortality of patients with orbital exenteration compared with others without this procedure (22% vs. 33%, P = 0.008). In contrast, Choksi et al.,26 found that orbital exenteration could not increase the survival in CAM.
Existing studies about outcomes of amphotericin B retrobulbar injection in patients with CAM were few and some of these studies had insufficient data. Therefore, we did not perform a statistical analysis, this being the most significant limitation in assessing our findings and hypotheses. In addition, this study might be biased, as only studies performing retrobulbar injection of amphotericin B were considered, some being case reports or case series.
CONCLUSIONS
Retrobulbar injection of amphotericin B is a low invasive and almost safe treatment with satisfactory outcomes, especially aimed at globe salvage in CAM with orbital involvement. But, further studies on a large sample size will help expand our knowledge about the efficacy of retrobulbar injection of amphotericin B in salvaging or restoration of vision, in treating patients with intracranial involvement, and in reducing mortality in patients with CAM.
Supplementary Material
Footnotes
The authors have no financial or conflicts of interest to disclose.
Supplemental digital content is available for this article. Direct URL citations appear in the printed text and are provided in the HTML and PDF versions of this article on the journal’s website (www.op-rs.com).
REFERENCES
- 1.Singh AK, Singh R, Joshi SR, et al. Mucormycosis in COVID-19: a systematic review of cases reported worldwide and in India. Diabetes Metab Syndr. 2021;15:102146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Pakdel F, Ahmadikia K, Salehi M, et al. Mucormycosis in patients with COVID-19: a cross-sectional descriptive multicentre study from Iran. Mycoses. 2021;64:1238–1252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Raiesi O, Hashemi SJ, Mohammadi Ardehali M, et al. Molecular identification and clinical features of fungal rhinosinusitis: a 3-year experience with 108 patients. Microb Pathog. 2021;158:105018. [DOI] [PubMed] [Google Scholar]
- 4.Hoenigl M, Seidel D, Carvalho A, et al. The emergence of COVID-19 associated mucormycosis: a review of cases from 18 countries. The Lancet Microbe. 2022;3:e543-e552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Greene J, Pak J, Tucci V, et al. Mucormycosis in immunochallenged patients. J Emergencies, Trauma Shock. 2008;1:106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Jeong W, Keighley C, Wolfe R, et al. The epidemiology and clinical manifestations of mucormycosis: a systematic review and meta-analysis of case reports. Clin Microbiol Infect. 2019;25:26–34. [DOI] [PubMed] [Google Scholar]
- 7.Prakash H, Ghosh AK, Rudramurthy SM, et al. A prospective multicenter study on mucormycosis in India: epidemiology, diagnosis, and treatment. Med Mycol. 2019;57:395–402. [DOI] [PubMed] [Google Scholar]
- 8.Nithyanandam S, Jacob MS, Battu RR, et al. Rhino-orbito-cerebral mucormycosis. A retrospective analysis of clinical features and treatment outcomes. Indian J Ophthalmol. 2003;51:231–236. [PubMed] [Google Scholar]
- 9.Vaughan C, Bartolo A, Vallabh N, et al. A meta-analysis of survival factors in rhino-orbital-cerebral mucormycosis-has anything changed in the past 20 years? Clin Otolaryngol. 2018;43:1454–1464. [DOI] [PubMed] [Google Scholar]
- 10.Yohai RA, Bullock JD, Aziz AA, et al. Survival factors in rhino-orbital-cerebral mucormycosis. Surv Ophthalmol. 1994;39:3–22. [DOI] [PubMed] [Google Scholar]
- 11.Banerjee M, Pal R, Bhadada SK. Intercepting the deadly trinity of mucormycosis, diabetes and COVID-19 in India. Postgrad Med J. 2022;98:e108–e109. [DOI] [PubMed] [Google Scholar]
- 12.John TM, Jacob CN, Kontoyiannis DP. When uncontrolled diabetes mellitus and severe COVID-19 converge: the perfect storm for mucormycosis. J Fungi (Basel). 2021;7:298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Sarda R, Swain S, Ray A, et al. COVID-19-associated mucormycosis: an epidemic within a pandemic. QJM. 2021;114:355–356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Prado-Calleros HM, Fajardo-Dolci G, Plowes-Hernández O, et al. [Rhino-Orbital Mucormycosis. Cohort study of its treatment according disease extent and reversion of its pathophysiology]. Gac Med Mex. 2016;152:770–782. [PubMed] [Google Scholar]
- 15.Palejwala SK, Zangeneh TT, Goldstein SA, et al. An aggressive multidisciplinary approach reduces mortality in rhinocerebral mucormycosis. Surg Neurol Int. 2016;7:61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hargrove RN, Wesley RE, Klippenstein KA, et al. Indications for orbital exenteration in mucormycosis. Ophthalmic Plast Reconstr Surg. 2006;22:286–291. [DOI] [PubMed] [Google Scholar]
- 17.Shah K, Dave V, Bradoo R, et al. Orbital exenteration in rhino-orbito-cerebral mucormycosis: a prospective analytical study with scoring system. Indian J Otolaryngol Head Neck Surg. 2019;71:259–265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ashraf DC, Idowu OO, Hirabayashi KE, et al. Outcomes of a modified treatment ladder algorithm using retrobulbar amphotericin b for invasive fungal rhino-orbital sinusitis. Am J Ophthalmol. 2022;237:299–309. [DOI] [PubMed] [Google Scholar]
- 19.Hirabayashi KE, Kalin-Hajdu E, Brodie FL, et al. Retrobulbar injection of amphotericin B for orbital mucormycosis. Ophthalmic Plast Reconstr Surg. 2017;33:e94–e97. [DOI] [PubMed] [Google Scholar]
- 20.Page MJ, McKenzie JE, Bossuyt PM, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372:n71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Higgins JPT, Thomas J, Chandler J, et al. Cochrane Handbook for Systematic Reviews of Interventions. 6.3. Cochrane; 2022. www.training.cochrane.org/handbook [Google Scholar]
- 22.The EndNote Team. EndNote 20. Philadelphia, PA: Clarivate Analytics, 2013. [Google Scholar]
- 23.Ouzzani M, Hammady H, Fedorowicz Z, et al. Rayyan-a web and mobile app for systematic reviews. Syst Rev. 2016;5:210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.JBI’s critical appraisal tools assist in assessing the trustworthiness, relevance and results of published papers. Institute JB. 2017. Available at: https://jbi.global/critical-appraisal-tools. Accessed April 20, 2022.
- 25.Ramamurthy LB, Bhandari R, Kanakpur S, et al. Outcome of transcutaneous retrobulbar injection of liposomal amphotericin B in post-COVID-19 rhino-orbito-cerebral mucormycosis: our experience. Indian J Ophthalmol. 2022;70:1019–1024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Choksi T, Agrawal A, Date P, et al. Cumulative mortality and factors associated with outcomes of mucormycosis after COVID-19 at a multispecialty tertiary care center in India. JAMA Ophthalmol. 2022;140:66–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Bayram N, Ozsaygili C, Sav H, et al. Susceptibility of severe COVID-19 patients to rhino-orbital mucormycosis fungal infection in different clinical manifestations. Jpn J Ophthalmol. 2021;65:515–525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Arora R, Goel R, Khanam S, et al. Rhino-orbito-cerebral-mucormycosis during the COVID-19 second wave in 2021 - a preliminary report from a single hospital. Clin Ophthalmol. 2021;15:3505–3514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Diwakar J, Samaddar A, Konar SK, et al. First report of COVID-19-associated rhino-orbito-cerebral mucormycosis in pediatric patients with type 1 diabetes mellitus. J Mycol Med. 2021;31:101203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Dave TV, Gopinathan Nair A, Hegde R, et al. Clinical presentations, management and outcomes of rhino-orbital-cerebral mucormycosis (ROCM) following COVID-19: a multi-centric study. Ophthalmic Plast Reconstr Surg. 2021;37:488–495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Mekonnen ZK, Ashraf DC, Jankowski T, et al. Acute invasive rhino-orbital mucormycosis in a patient with COVID-19-associated acute respiratory distress syndrome. Ophthalmic Plast Reconstr Surg. 2021;37:e40–e80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Murthy R, Bagchi A, Gote Y, et al. Retrobulbar injection of amphotericin B using intravenous cannula for post-COVID-19 rhino-orbital mucormycosis. Indian J Ophthalmol. 2022;70:302–305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Singh SP, Rana J, Singh VK, et al. Rhino-orbital mucormycosis: our experiences with clinical features and management in a tertiary care center. Rom J Ophthalmol. 2021;65:339–353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Singh P, Gupta A, Sanepalli SR, et al. Transcutaneous retrobulbar amphotericin-B (TRAMB) injection in orbital mucormycosis. BMJ Case Rep. 2022;15:e246307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Sen M, Honavar SG, Bansal R, et al. ; members of the Collaborative OPAI-IJO Study on Mucormycosis in COVID-19 (COSMIC) Study Group. Epidemiology, clinical profile, management, and outcome of COVID-19-associated rhino-orbital-cerebral mucormycosis in 2826 patients in India—collaborative OPAI-IJO study on mucormycosis in COVID-19 (COSMIC), report 1. Indian J Ophthalmol. 2021;69:1670–1692. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Yasmin F, Najeeb H, Naeem A, et al. COVID-19 associated mucormycosis: a systematic review from diagnostic challenges to management. Diseases. 2021;9:65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.SeyedAlinaghi S, Karimi A, Barzegary A, et al. Mucormycosis infection in patients with COVID-19: a systematic review. Heal Sci Reports. 2022;5:e529. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 38.Bhattacharyya A, Sarma P, Sharma DJ, et al. Rhino-orbital-cerebral-mucormycosis in COVID-19: a systematic review. Indian J Pharmacol. 2021;53:317–327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Bhattacharyya A, Sarma P, Kaur H, et al. COVID-19-associated rhino-orbital-cerebral mucormycosis: a systematic review, meta-analysis, and meta-regression analysis. Indian J Pharmacol. 2021;53:499–510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Kamat M, Datar U, Byakodi S, et al. COVID-19-associated mucormycosis of head-and-neck region: a systematic review. J Clin Transl Res. 2022;8:31–42. [PMC free article] [PubMed] [Google Scholar]
- 41.Hussain S, Riad A, Singh A, et al. Global prevalence of COVID-19-associated mucormycosis (CAM): living systematic review and meta-analysis. J Fungi (Basel). 2021;7:985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Pal R, Singh B, Bhadada SK, et al. COVID-19-associated mucormycosis: an updated systematic review of literature. Mycoses. 2021;64:1452–1459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Spellberg B, Edwards J, Jr, Ibrahim A. Novel perspectives on mucormycosis: pathophysiology, presentation, and management. Clin Microbiol Rev. 2005;18:556–569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Cornely OA, Arikan-Akdagli S, Dannaoui E, et al. ; European Society of Clinical Microbiology and Infectious Diseases Fungal Infection Study Group; European Confederation of Medical Mycology. ESCMID and ECMM joint clinical guidelines for the diagnosis and management of mucormycosis 2013. Clin Microbiol Infect. 2014;20(Suppl 3):5–26. [DOI] [PubMed] [Google Scholar]
- 45.Karadeniz Uğurlu Ş, Selim S, Kopar A, et al. Rhino-orbital mucormycosis: clinical findings and treatment outcomes of four cases. Turk J Ophthalmol. 2015;45:169–174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Colon-Acevedo B, Kumar J, Richard MJ, et al. The role of adjunctive therapies in the management of invasive Sino-Orbital infection. Ophthalmic Plast Reconstr Surg. 2015;31:401–405. [DOI] [PubMed] [Google Scholar]
- 47.Safi M, Ang MJ, Patel P, et al. Rhino-orbital-cerebral mucormycosis (ROCM) and associated cerebritis treated with adjuvant retrobulbar amphotericin B. Am J Ophthalmol Case Rep. 2020;19:100771. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Gorovoy IR, Kazanjian M, Kersten RC, et al. Fungal rhinosinusitis and imaging modalities. Saudi J Ophthalmol. 2012;26:419–426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Horger M, Hebart H, Schimmel H, et al. Disseminated mucormycosis in haematological patients: CT and MRI findings with pathological correlation. Br J Radiol. 2006;79:e88–e95. [DOI] [PubMed] [Google Scholar]
- 50.Kim JH, Kang BC, Lee JH, et al. The prognostic value of gadolinium-enhanced magnetic resonance imaging in acute invasive fungal rhinosinusitis. J Infect. 2015;70:88–95. [DOI] [PubMed] [Google Scholar]
- 51.Harmsen S, McLaren AC, Pauken C, et al. Amphotericin B is cytotoxic at locally delivered concentrations. Clin Orthop Relat Res. 2011;469:3016–3021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Brodie FL, Kalin-Hajdu E, Kuo DS, et al. Orbital compartment syndrome following retrobulbar injection of amphotericin B for invasive fungal disease. Am J Ophthalmol Case Rep. 2016;1:8–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Hamill RJ. Amphotericin B formulations: a comparative review of efficacy and toxicity. Drugs. 2013;73:919–934. [DOI] [PubMed] [Google Scholar]
- 54.Nair AG, Adulkar NG, D’Cunha L, et al. Rhino-orbital mucormycosis following COVID-19 in previously non-diabetic, immunocompetent patients. Orbit. 2021;40:499–504. [DOI] [PubMed] [Google Scholar]
- 55.Jhunjhunwala A, Kumar R. To study the clinical course of rhino orbital mucormycosis in post COVID-19 patients: A case series. IP Int J Ocul Oncol Oculoplasty. 2021;7:328–332. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.