Abstract
Objectives
Ensuring access to care for all patients—especially those with life-threatening and chronic conditions—during a pandemic is a challenge for all healthcare systems. During the COVID-19 pandemic, many countries faced excess mortality partly attributed to disruptions in essential healthcare services provision. This study aims to estimate the utilization of public primary care and hospital services during the COVID-19 epidemic in Greece and its potential association with excess non-COVID-19 mortality in the country.
Study design
This is an observational study.
Methods
A retrospective analysis of national secondary utilization and mortality data from multiple official sources, covering the first nine months of the COVID-19 epidemic in Greece (February 26th to November 30th, 2020), was carried out.
Results
Utilization rates of all public healthcare services during the first nine months of the epidemic dropped significantly compared to the average utilization rates of the 2017–19 control period; hospital admissions, hospital surgical procedures, and primary care visits dropped by 17.3% (95% CI: 6.6%–28.0%), 23.1% (95% CI: 7.3%–38.9%), and 24.8% (95% CI: 13.3%–36.3%) respectively. This underutilization of essential public services—mainly due to supply restrictions such as suspension of outpatient care and cancelation of elective surgeries—is most probably related to the 3778 excess non-COVID-19 deaths (representing 62% of all-cause excess deaths) that have been reported during the first 9 months of the epidemic in the country.
Conclusions
Greece's healthcare system, deeply wounded by the 2008–18 recession and austerity, was ill-resourced to cope with the challenges of the COVID-19 epidemic. Early and prolonged lockdowns have kept COVID-19 infections and deaths at relatively low levels. However, this “success” seems to have been accomplished at the expense of non-COVID-19 patients. It is important to acknowledge the “hidden epidemic” of unmet non-COVID-19 needs and increased non-COVID-19 deaths in the country and urgently strengthen public healthcare services to address it.
Keywords: COVID-19, Essential health services, Health services utilization, Excess mortality, Excess non-COVID-19 deaths
Introduction
The COVID-19 pandemic poses enormous challenges on health systems around the world, testing their preparedness in controlling the spread of the epidemic and managing its social and health consequences in a constantly changing environment. As far as healthcare services are concerned, this “dynamic preparedness” challenge entails their ability to manage COVID-19 morbidity effectively while ensuring unobstructed access to essential health services for all non-COVID-19 patients.1
Keeping the appropriate balance among restrictive measures for controlling the epidemic, shifting and scaling up healthcare resources for treating COVID-19 patients, and sustaining essential healthcare services for all other patients are complex tasks. During the pandemic, most countries have been reporting serious disruptions in the delivery of services and low utilization rates of even essential healthcare services,2 such as emergency department attendances and all-medical hospital admissions.3 , 4
These sharp declines in healthcare services utilization have been interpreted in various ways. Some researchers suggest that such declines may reflect the lower incidence of certain diseases during the pandemic, such as respiratory infections and cardiovascular events due to reduced air pollution and behavioral changes (more exercise, home-prepared meals) related to stay-at-home orders, and fewer injuries from work and traffic accidents related to social isolation measures such as lockdowns.4 Others suggest that the observed declines in services utilization can be explained as the result of supply restrictions (e.g. cancelation of elective care, repurposing of essential services like intensive care units (ICU) to COVID-19 ones, and redeployment of health workers to COVID-19 clinics) and increased barriers to access (e.g. patients not presenting to outpatient care due to fear of infection, explicit instructions for patients to avoid face-to-face clinical care, patients' difficulties in traveling to healthcare facilities using public transport, and financial barriers that hinder access to care). These problems may lead to delayed or inadequate treatment of conditions that might result in excess non-COVID-19 mortality.1, 2, 3, 4
COVID-19 epidemic and public health and healthcare response in Greece
The COVID-19 epidemic in Greece started on February 26, 2020, with imported cases initially from Italy and later from Israel. The early introduction of social distancing measures in early March and the timely introduction of a general stay-at-home order (lockdown) quickly resulted in the control of the first epidemic wave of COVID-19, keeping infected, hospitalized cases and related deaths at relatively low levels compared to other EU countries.5 After 42 days of lockdown, restrictive measures were gradually withdrawn starting with the lifting of the stay-at-home order on May 4, 2020, and the full restoration of cross-country mobility (opening for travel and tourism) on July 1, 2020. The second epidemic wave in Greece started in early August and slowly escalated to an exponential increase in ICU cases and COVID-19 related deaths all through November and early December. In response to this second severe epidemic wave, public health authorities introduced a second nationwide lockdown on November 7, 2020.
The Greek healthcare system was heavily impacted by the 2008–2018 recession and the neoliberal Economic Adjustment Programme that the country implemented as part of its loan agreement with the “Troika”, a coalition of the International Monetary Fund, European Commission, and European Central Bank.6 Being ill-prepared and poorly resourced, the Greek public healthcare system responded to the ongoing epidemic crisis by ceasing most of its regular activities and redirecting available resources to COVID-19 treatment in order to avoid being overwhelmed by the sudden increase in the demand for care.5 During the first epidemic wave on March 11, 2020, 10 days before the first lockdown, elective surgeries and outpatient departments in public hospitals treating patients with chronic diseases were suspended, surgical departments and ICUs were repurposed for treating COVID-19 patients, primary care centers downsized their clinical activities due to the lack of guidelines and personal protective equipment, and primary healthcare workers were redeployed to NHS hospitals.5 These supply restrictions for non-COVID-19 patients were partly counterbalanced by the introduction of telemedicine and e-prescription services in early April and publicly reimbursed referrals of non-COVID-19 hospitalized patients from public hospitals to private clinics. Disruptions in public clinical services were restored eventually in June. During the second epidemic wave, on October 9, 27 days before the second general lockdown, the above supply restrictions were gradually reintroduced.
Utilization of public healthcare services and excess mortality in Greece
From January to November 2020, Greece experienced 74 days of lockdown and almost 120 days of full or partial suspension of public elective care services.
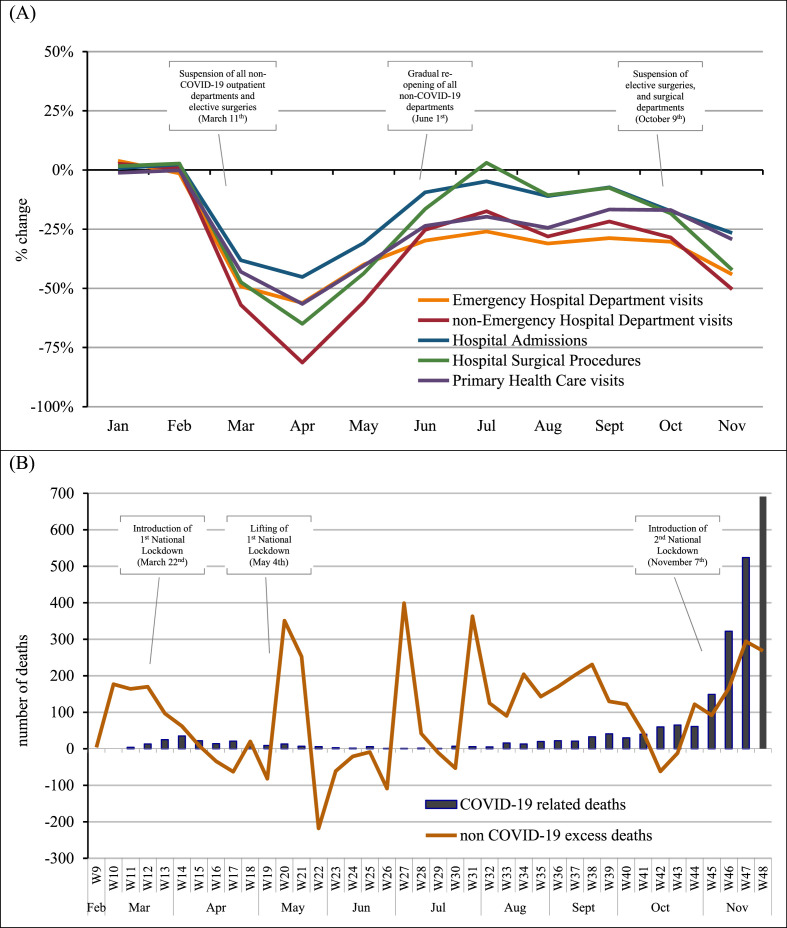
During these 9 months, according to nationwide aggregated data from the Greek Ministry of Health, utilization of essential public hospital services reduced significantly compared to the average respective period of 2017–19. All-medical admissions in public hospitals dropped by 17.3% (95% CI: 6.6%–28.0%), visits to emergency and non-emergency public hospital departments declined by 30.4% (95% CI: 18.2%–42.7%) and 33.3% (95% CI: 16.0%–50.5%) respectively, while 23.1% (95% CI: 7.3%–38.9%) fewer surgical procedures were carried out in public hospitals compared to the control period (Fig. 1 A, Supplementary Table S1).
Fig. 1.
(A) Public healthcare services utilization in Greece (Jan 1–Nov 30, 2020), compared to the average respective time period of 2017–19 (B) Excess deaths in Greece (ISO weeks 9–48; Feb 22–Nov 29, 2020), compared to the average respective time period of 2015–2019. Notes and Sources: (A) Authors' calculations are based on monthly aggregated data from all public hospitals and public primary care centers in Greece, as reported by the Greek Ministry of Health. Data were grouped by the type of facility (hospital vs primary care) and the type of service (emergency or non-emergency hospital visits, hospital admissions and surgical procedures, and total primary care visits), and utilization rates were calculated for each month from January until November 2020. The control period covers the average monthly utilization rates during the period 2017–19. (B) Authors' calculations are based on weekly data of all-cause deaths as reported by the Hellenic Statistical Authority and daily data of COVID-19 deaths as reported by the National Public Health Organisation in Greece. Excess non-COVID-19 deaths were calculated by extracting COVID-19 deaths from total all-cause excess deaths. The control period covers the average weekly all-cause deaths during the period 2015–19.
It is estimated that approximately 3.9 million outpatient visits, 253 thousand admissions, and 108 thousand surgical procedures have been missed in Greek public hospitals during the pandemic, compared to the expected ones based on the pre-COVID-19 trends (Supplementary Table S1).
These significant declines in hospital services utilization were not counterbalanced by the increased use of primary care services; visits to public primary care centers dropped by 24.8% (95% CI: 13.3%–36.3%) between January and November 2020 compared to the control period (Fig. 1A, Supplementary Table S1).
The most significant declines in public health services utilization (e.g. up to 81% reduction for non-emergency visits and 65% decline for surgeries) took place between March–May and October–November 2020, periods that coincide with the cessation of elective services in public hospitals and the introduction of social isolation measures (Fig. 1A).
In Greece, according to weekly official data from the Hellenic Statistical Authority, 6100 more deaths have been reported during the period February 26 to November 29, 2020, compared to the expected deaths based on the average respective period of 2015–2019 (Fig. 1B, Supplementary Table S2). In other words, the observed all-cause deaths during the first two epidemic waves in the country increased by 6.8% compared to the expected ones.
Of these excess deaths, 62% (3779 deaths) are not directly related to COVID-19 infection. The majority of non-COVID-19 excess deaths (61.0%; 2305 deaths) occurred between May 6 and October 6 (ISO weeks 19–41 in Fig. 1B).
Discussion
Excess mortality has been reported in several countries during the pandemic. For example, during the first epidemic wave, Italy and England were reporting excess deaths, 20% and 25% of which respectively could not be directly attributed to COVID-19 infection.7 , 8 Excess non-COVID-19 deaths typically can either be related to underreporting of COVID-19 deaths (especially if observed during COVID-19 resurgences) and/or inadequate management of non-COVID-19 diseases.
In Greece, excess non-COVID-19 deaths represent the majority (62%) of excess mortality reported during the first nine months of the epidemic in the country. Most of these excess non-COVID-19 deaths took place during summer and autumn—between the two epidemic waves in the country—when levels of SARS-CoV-2 spread in the community were very low, suggesting that they cannot be attributed to the under-certification of COVID-19 deaths.
In contrast, the sharp nationwide declines in the utilization of essential public hospital and primary care services reported in this study suggest that excess non-COVID-19 deaths in Greece are most probably related to the inadequate treatment of chronic or life-threatening conditions. Earlier studies from Greece, using small samples, have reported serious disruptions in the provision of critical care, in line with this hypothesis. For example, studies from Greek public hospitals and specific public hospital departments have reported significant drops in cardiac surgical procedures9 and significant drops in emergency department visits for patients with critical conditions such as cancer, confirmed or suspected hemorrhage, and acute cardiovascular events.10
Future research (when data on causes of mortality become available) will shed more light on the origin of the observed excess mortality in Greece. However, this early evidence suggests that the majority of excess deaths in the country are most probably associated with the underutilization of public healthcare services during the epidemic mainly due to supply restrictions and accessibility barriers.
Greece's health response to the COVID-19 epidemic has often been presented as a “success story”. However, these early findings demonstrate how an ill-resourced health system, after years of austerity, can lose balance while coping with a public health threat, sacrificing access to essential health services for chronic patients that mostly depend on them in order to cope with the epidemic. Acknowledging this “hidden epidemic” of unmet non-COVID-19 healthcare needs and consequent excess deaths is of vital importance and urgency. Strengthening public hospital services provision and scaling up primary healthcare are necessary prerequisites for ensuring safe and unobstructed access to care for all patients, including those with non-COVID-19 related conditions.
Author statements
Ethical approval
No ethical approval is required for this type of study. All data used are anonymized, aggregated data, publicly available.
Funding
The authors received no funding for this research.
Competing interests
All authors (EK, FT, and AB) have no competing interests to declare.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.puhe.2021.06.025.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- 1.Jakab M., Nathan N., Pastorino G., Evetovits T., Garner S., Langins M., et al. Managing health systems on a seesaw: balancing the delivery of essential health services whilst responding to COVID-19. Eurohealth. 2020;26:63–67. [Google Scholar]
- 2.World Health Organisation . World Health Organization; Geneva: 2020. Pulse survey on continuity of essential health services during the COVID-19 pandemic. Interim report. [Google Scholar]
- 3.Hartnett K., Kite-Powell A., DeVies J., Coletta M., Boehmer T., Adjemian J., et al. Impact of the Covid-19 pandemic on emergency department visits - United States, January 1, 2019 - may 30, 2020. CDCP MMWR. 2020;69:1–6. doi: 10.15585/mmwr.mm6923e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Birkmeyer J.D., Barnato A., Birkmeyer N., Bessler R., Skinner J. The impact of the COVID-19 pandemic on hospital admissions in the United States. Health Aff. 2020;39:2010–2017. doi: 10.1377/hlthaff.2020.00980. http://www.healthaffairs.org/doi/10.1377/hlthaff.2020.00980 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kondilis E., Pantoularis I., Makridou E., Rotulo A., Seretis S., Benos A. Centre for Research and Education in Public Health, Health Policy and Primary Health Care; Thessaloniki: 2020. Critical assessment of preparedness and policy responses to SARS-CoV2 pandemic: international and Greek experience. CEHP Report 2020.2. [Google Scholar]
- 6.Kondilis E., Giannakopoulos S., Gavana M., Ierodiakonou I., Waitzkin H., Benos A. Economic crisis, restrictive policies, and the population's health and health care: the Greek case. Am J Publ Health. 2013;103:973–979. doi: 10.2105/AJPH.2012.301126. https://ajph.aphapublications.org/doi/10.2105/AJPH.2012.301126 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Alicandro G., Remuzzi G., La Vecchia C. Italy's first wave of the COVID-19 pandemic has ended: no excess mortality in May, 2020. Lancet. 2020;396:e27–e28. doi: 10.1016/S0140-6736(20)31865-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kontopantelis E., Mamas M.A., Deanfield J., Asaria M., Doran T. Excess mortality in England and Wales during the first wave of the COVID-19 pandemic. J Epidemiol Community Health. 2021;75:213–223. doi: 10.1136/jech-2020-214764. https://jech.bmj.com/lookup/doi/10.1136/jech-2020-214764 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lazaros G., Oikonomou E., Theofilis P., Theodoropoulou A., Triantafyllou K., Charitos C., et al. The impact of COVID-19 pandemic on adult cardiac surgery procedures. Hellenic J Cardiol. 2020 Jul 15:S1109–S9666. doi: 10.1016/j.hjc.2020.07.001. https://linkinghub.elsevier.com/retrieve/pii/S1109966620301615 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kastritis E., Tsitsimpis K., Anninos E., Stamatelopoulos K., Kanakakis I., Lampropoulos C., et al. Significant reduction in the visits to the emergency room department during the COVID-19 pandemic in a tertiary hospital in Greece. Medicine. 2020;99 doi: 10.1097/MD.0000000000023845. https://journals.lww.com/10.1097/MD.0000000000023845 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.