Abstract
BACKGROUND AND PURPOSE:
Because stroke therapy has changed with the introduction of endovascular stroke treatment as a standard approach, studies on intrahospital causes of death from stroke are no longer up-to-date. The purpose of this observational study was to present the causes of death during hospitalization of patients with ischemic stroke who received endovascular stroke treatment, with the focus on a differentiation of curative and secondary palliative treatment.
MATERIALS AND METHODS:
We studied a total cohort of 1342 patients who received endovascular stroke treatment in a tertiary stroke center (Aachen, Germany) between 2010 and 2020 and analyzed the causes of death in all 326 consecutive deceased patients. We distinguished between curative treatment and a secondary palliative approach and analyzed causes of death and treatment numbers across the years.
RESULTS:
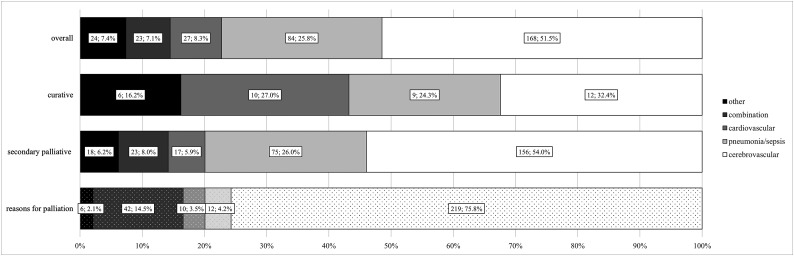
In the entire cohort of 326 deceased patients, the most common cause of death was of a cerebrovascular nature (51.5%), followed by pneumonia and sepsis (25.8%) and cardiovascular causes (8.3%). Neurovascular causes constituted 75.8% of reasons for palliation. In the group with a secondary palliative approach, causes of death were neurovascular in 54.0% of patients and pneumonia and sepsis in 26.0% of patients.
CONCLUSIONS:
Cerebrovascular causes in patients with stroke play a major role in the intrahospital causes of death and reasons for palliation. Considering the large proportion of secondarily palliative–treated patients, reasons for palliation should be considered instead of causes of death to avoid concealment by, for example, life-terminating measures.
Stroke is ranked by the World Health Organizaton as the second leading cause of death worldwide in 2019 and forms the third most common cause of death in Germany.1,2 Feigin et al3 confirmed the increasing burden of stroke on patients globally, but especially in low-income and middle-income countries. Depending on the type of stroke and the therapy administered, the mortality in untreated patients can be as high as 80%.4
It has been shown that there is an increased risk of death in the acute phase after stroke and a long-term risk of poststroke death that is twice as high as in the healthy population.5-7 Before endovascular stroke treatment was established, various studies showed that the most common cause of death in the first 7 days was due to cerebrovascular issues, and most deaths within the first 30 days can be attributed to the initial infarction.8,9 The profile of the causes of death after ischemic stroke is reported to change with time: In the first 5 years after stroke, cardiovascular causes of death were shown to be most prominent, whereas nonvascular events accounted for most causes of death during the poststroke period of 5–10 years.10 Equally large but more recent studies are rare: D’Alton et al11 reported pneumonia as the most common cause of death in patients with both hemorrhagic and ischemic stroke; in contrast Aked et al12 reported a majority of cerebrovascular causes of death after 3 years, followed by cardiovascular deaths.
However, the standards in the treatment of patients with ischemic stroke have changed across the years, and there are few records with more recent and larger data sets that would allow an analysis of changes in causes of death resulting from the increasing use of endovascular stroke treatment. In patients with emergent, large-vessel-occlusion stroke, thrombectomy results in a better functional outcome and shows no increased mortality rates compared with intravenous thrombolysis or standard therapy only.13-15 Hence, it is equally conceivable that causes of death vary depending on treatment type: while thrombolytic therapies carry a risk of intracranial bleeding, endovascular stroke treatment is additionally associated with technical complications such as vascular dissection, vasospasm, embolus formation, bleeding, and device failure.16-18 The objective of this study was to determine intrahospital causes of death in patients receiving endovascular stroke treatment in a tertiary stroke center during 10 years.
MATERIALS AND METHODS
This study is based on a prospective registry of consecutive patients with acute ischemic stroke admitted to a tertiary stroke center of the University Hospital RWTH Aachen (Aachen, Germany). The study was approved by our local ethics committee. A need for written consent for this analysis was waived by this committee.
Our university hospital is a tertiary stroke center that serves an area of approximately 1 million inhabitants. In our regional stroke network of 4 hospitals, only 2 hospitals provide endovascular stroke therapy, with our university hospital being the only hospital that provides endovascular stroke therapy 24 hours a day and 7 days a week. Most patients eligible for endovascular stroke therapy are either directly admitted to our institution or transferred. Our standard is to continue treatment in our hospital and not to transfer patients back to their referring hospital.
We included all consecutive patients with acute ischemic stroke submitted to endovascular stroke treatment (including mechanical thrombectomy and/or intra-arterial thrombolysis, in combination or not with intravenous thrombolysis) between January 2010 and September 2020. The applied diagnostic methods and indicators for therapeutic measures used have already been described in a previous publication.19
We collected the following variables from the prospective registry and from the patients’ clinical records when needed: demographic information, comorbidities, initial NIHSS score, ASPECTS, large-vessel occlusion site, established concept of treatment after endovascular stroke treatment, poststroke mRS, length of stay, intrahospital mortality, and causes of intrahospital death. Missing data were marked as “missing/unknown,” whenever retrospective analysis did not allow completion of data. The concept of treatment and causes of intrahospital death were retrieved from the patient’s clinical records and independently reviewed by 2 senior neurologists. Disagreements were settled in a consensus reading. We specifically focused on the spectrum of causes of death during approximately 1 decade rather than analyzing risk factors leading to death in endovascularly treated patients with stroke. We assessed baseline clinical characteristics and treatment modalities.
The established concept of clinical treatment after endovascular stroke treatment was classified into the following categories: curative care (maximal therapy during hospital stay) and secondary palliative care (palliative care decided by the treating physicians together with the patient or with the patient’s legal representatives or care partners, taking into consideration the patient’s will and expected outcome). The decision to establish a secondary palliative care concept in our institution is multidisciplinary and is always documented in the patient’s clinical record. Palliative care was performed in-hospital and based on generally accepted recommendations; patients were not transferred to external facilities for secondary palliative care.20
Causes of death were classified into the following categories: cerebrovascular, pneumonia and/or sepsis, cardiovascular, other (eg, renal failure), and a combination of multiple causes. This classification was based on previous studies and adapted to the intrahospital setting of our study.11 For the secondary palliative care group, reasons for palliation were collected and the same categories were used.
Statistics
We analyzed the baseline data of the overall collective of endovascularly treated patients with stroke and compared the baseline characteristics of curative and secondary palliative care groups using χ2 tests or Mann-Whitney U tests as appropriate. All values are indicated as frequencies or as median with interquartile range (IQR) due to the nonparametric nature of our data. We characterized causes of death in the overall study population but also separately for the curative care group and the secondary palliative group. Additionally, we characterized reasons for establishing a secondary palliative care concept. To assess changes across time, we analyzed the causes of death and reasons for secondary palliative care during the years of the study using trend analyses for proportions. Likewise, changes of continuous baseline variables across the study period were tested using the Cuzick nonparametric test. The Wilcoxon signed-rank test was used to compare the reasons for palliation with the actual causes of death in the secondary palliative group. We also compared the extreme ends of our observation period, namely patients in 2010–2011, when we established thrombectomy as a standard of care in our department, and patients in 2019, a more recent time period.
Statistical analyses were performed with SPSS Statistics 26 (IBM) and Stata Statistical Software, Release 16.1 (StataCorp). Statistical significance was set at an α value <.05.
RESULTS
During the study period, 2846 patients with acute ischemic stroke underwent acute reperfusion treatment, of whom 1342 received endovascular treatment and were included in our study. Among the latter, 597 patients (44.5%) received isolated mechanical thrombectomy, 722 patients (53.8%) received mechanical thrombectomy in combination with IV thrombolysis, and 23 patients (1.7%) received isolated intra-arterial thrombolysis. The distribution of treatment modalities was similar among patients who died in the curative care group and in the secondary palliative care group (P = .840).
The median age of all patients was 75 years (IQR, 64–82 years); 667 patients (49.7%) were women (median NIHSS score, 16; IQR, 10–20). We focused our analysis on all 326 patients (24.3%) who died during hospitalization in our institution. Among patients who died in the hospital, a curative care concept had been pursued in 37 patients (11.3%) and a secondary palliative care concept had been established in 289 patients (88.7%). Baseline characteristics of the study population are presented in the Table. Patients who died under curative care were significantly younger (median age, 72 versus 80 years; P < .001) than patients for whom secondary palliative care was established and had a shorter median length of stay (3 versus 5 days, P = .005). A detailed analysis of the time period from stroke onset to death is found in the Online Supplemental Data. In summary, cerebrovascular causes were the earliest to cause death (median of 4 days), followed by cardiovascular, other, and a combination of causes (median of 7 days each), and pneumonia and sepsis (median of 11 days). The median onset to death was significantly shorter in the curative group compared with the secondary palliative group when the cause of death was cerebrovascular (2.5 days versus 4 days, P = .016) or cardiovascular (2 days versus 8 days, P = .027).
Baseline data
| Characteristic | Deceased Patients (n = 326) |
||||
|---|---|---|---|---|---|
| Overall Collective (n = 1342)All Treatment Groups | Overall (n = 326) | Secondary Palliative (n = 289) | Curative (n = 37) | P Valuea | |
| Age (median) (IQR) (yr) | 75 (64–82) | 80 (71–86) | 80 (72–87) | 72 (62–82) | .001b |
| Female sex (No.) | 667 (49.7%) | 163 (50.0%) | 147 (50.9%) | 16 (43.2%) | .383 |
| Hypertension (No.) (n = 2 missing) | 1067 (79.5%) | 260 (79.8%) | 232 (80.3%) | 28 (75.7%) | .427 |
| Cardiovascular disease (No.) (n = 4 missing) | 657 (49%) | 167 (51.2%) | 146 (50.5%) | 21 (56.8%) | .367 |
| Diabetes mellitus (No.) (n = 3 missing) | 342 (25.5%) | 97 (29.8%) | 78 (27%) | 19 (51.4%) | .809 |
| Obesity (No.) (n = 4 missing) | 374 (27.9%) | 78 (23.9%) | 69 (23.9%) | 9 (24.3%) | .360 |
| Atrial fibrillation (No.) (n = 3 missing) | 640 (47.7%) | 168 (51.5%) | 153 (52.9%) | 15 (40.5%) | .304 |
| Prior stroke (No.) (n = 2 missing) | 255 (19%) | 79 (24.2%) | 72 (24.9%) | 7 (18.9%) | .919 |
| NIHSS score (median) (IQR) | 16 (10–20) | 18 (15–21) | 18 (15–21) | 20 (16–23) | .381 |
| mRS at discharge (median) (IQR) | 4 (2–5) | Noncalculable | Noncalculable | Noncalculable | NA |
| Length of stay (median) (IQR) (day) | 12 (6–22) | 5 (3–12) | 5 (3–13) | 3 (1–8) | .005b |
Note:—NA indicates noncalculable.
Comparison of secondary palliative and curative groups.
Statistically significant.
The Figure shows the causes of death and reasons for establishing a secondary palliative care concept. The most common cause of death in the entire cohort as well as in the curative and the secondary palliative care groups was cerebrovascular. However, the groups differed regarding the subsequent causes of death: In the entire cohort, most patients (51.5%; 168/326) died from cerebrovascular causes, with pneumonia and sepsis (25.8%; 84/326) being the second most frequent cause of death, whereas cardiovascular reasons (8.3%; 27/326) were less common. In the curative group, cerebrovascular deaths (32.4%; 12/37) were also the most common cause, with cardiovascular events (27.0%; 10/37) being the second most frequent cause of death, closely followed by pneumonia and sepsis (24.3%; 9/37). In the secondary palliative group, cerebrovascular deaths (54.0%; 156/289) were also the most common cause, with pneumonia and sepsis (26.0%; 75/289) being the second most frequent cause of death, whereas cardiovascular reasons (5.9%; 17/289) were markedly less frequent. The most common combination cause of death was pneumonia and sepsis and cardiovascular diseases (57%; 13/23). This was followed by the combination of cerebrovascular causes and pneumonia and sepsis (22%; 5/23). The most common combination cause of palliation was pneumonia and sepsis and cardiovascular causes (26%; 11/42), followed by pneumonia and sepsis and other causes of palliation (19%; 8/42). Causes of death differed significantly (P = .011) between the curative and secondary palliative groups. In contrast, cerebrovascular causes (75.4%; 218/289) were the main reason to pursue secondary palliative care in most patients, with a combination of causes (14.5%; 42/289) being the second most frequent reason for secondary palliative care. The reason for palliation could not be specified with sufficient certainty in 1 patient.
FIGURE.
Causes of death in the overall, curative, and secondary palliative groups as well as reasons for palliation (absolute numbers and percentage). The exact reason for palliation was not determinable with sufficient certainty in 1 case.
A comparison of reasons for palliation and causes of death in the secondary palliative group showed no significant alteration (P = .169).
Trends across the Study Period
An analysis of treatment numbers during 2010–2019 shows an increase in endovascular stroke treatment, ranging from 27 (31.0%) cases in 2010 to a maximum of 210 (61.4%) cases in 2019, with isolated mechanical thrombectomy being the most frequent approach after 2016. During the study period, the median age of patients undergoing endovascular treatment increased significantly (P < .001) and the median NIHSS score decreased significantly in the entire cohort (P < .001) and in the secondary palliative group (P < .001). No time trend was observed for in-hospital mortality for patients who underwent endovascular treatment during the study period (P = .384). However, there was a higher proportion of patients receiving palliative care (P = .045) and a lower proportion of curative care deaths (P < .001) across time. Our trend analysis also revealed that the proportion of cardiovascular deaths among patients who died decreased across the study period (P = .026) and that specifically in the curative group, the proportion of cerebrovascular deaths (P = .003) and cardiovascular deaths (P = .002) also decreased. Detailed information on the trend analyses and comparison of 2010–2011 versus 2019 is found in the Online Supplemental Data.
DISCUSSION
An initial objective of our study was to identify the intrahospital causes of death in endovascularly treated patients with stroke. Our analysis shows that in patients in whom a curative approach was pursued throughout, cerebrovascular causes and cardiovascular causes, and pneumonia and sepsis were the 3 main causes of death (sorted in order). This finding is in accordance with previous studies that demonstrated that cerebrovascular causes constitute most causes of death a short time after stroke.7-10,12 This is also in accordance with previous studies that demonstrated the importance of pneumonia as a main cause of death after stroke, which usually occurs due to prolonged ventilation times or dysphagia.9,11,21 Some authors report that pneumonia may play a particular role in patients with intracranial hemorrhage, who are reported to be likely to have dysphagia and subsequent pneumonia.22,23 The high proportion of cardiovascular deaths in the curative group is rather surprising, considering that previous data revealed an increase of cardiovascular deaths only in the first months poststroke.6,7,24 Acknowledging that cardiovascular reasons are less likely in our overall cohort and in our secondary palliative group, a possible explanation for the excess of cardiovascular causes of death in the curative group may be that patients who had previously died from large-vessel stroke now survive their stroke due to endovascular treatment but might die from their concomitant cardiovascular diseases. This finding is supported by our observation that in our curative cohort, cardiovascular disease was the earliest cause of death. However, our cohort is too small to draw definite conclusions. Also, previous studies were based on data from before endovascular stroke treatment was established and mainly focused on long-term analyses of causes of death and are, therefore, difficult to compare with our study that focuses on intrahospital deaths after endovascular stroke treatment.
Curative versus Secondary Palliative Care
A novel finding of our analysis is that a differentiation must be made between patients receiving secondary palliative therapy and those treated with curative intent throughout because their causes of death differed considerably. Cerebrovascular causes, cardiovascular causes, and pneumonia and sepsis are the 3 main causes of death (sorted in order) in our patients, but these results must be interpreted with great caution because our results show that the reasons for death and palliation differed, albeit not significantly. Our analysis showed that because of the therapeutic switch, the causes of death of patients receiving secondary palliative care could not be equated to those of the curative group. It was interesting to compare the reasons for switching to the palliative approach with the actual causes of death. In line with the palliative concept, minimized therapeutic intervention results in a high number of pulmonary, cardiovascular, and other causes of death. At the same time, the most common reason for palliation appears to be neurovascular. Supporting data can be found in the literature indicating that withdrawal of life-sustaining treatment is the most common cause of death in ventilated patients in the intensive care unit and is primarily associated with a severe neurologic condition.25,26 On the basis of these findings, further analyses regarding case fatality and causes of death should pay attention to the large proportion of patients receiving palliative care. In accordance with Singh et al,27 the quality of acute hospital care should not depend solely on the mortality rate, given the varying frequency of palliative concepts used.
Trends across the Study Period
Given a shift toward isolated mechanical thrombectomy across time as well as an increasing median age of patients and a decreasing median NIHSS score on admission, a change in causes of death with time would not have been surprising, especially with regard to the inclusion of elderly patients who are more likely to be treated with a palliative approach.28 In fact, there was a higher proportion of patients receiving palliative care across time in our cohort. Even though the overall mortality did not change with time, there was a trend toward a lower proportion of cardiovascular deaths across time. Additionally, we found a time trend for decreasing cardiovascular and cerebrovascular deaths in the curative group. Higher rates of palliation on the one hand and lower rates of cardiovascular and cerebrovascular deaths in the curative group on the other hand may be explained by the inclusion of a wider spectrum of patients across time, with older patients on the one hand and patients with less severe stroke on the other receiving endovascular stroke therapy. This trend may also be explained by imbalances in the distribution of comorbidities, vascular risk factors, and frailty status, which were not the focus of this analysis. Because subsequent increases of other causes of death do not appear to have had a significant impact in the curative group, a note of caution is due here because the number of patients in each group across the years was very small, especially within the curative cohort.
Limitations
The monocentric approach of our study can be seen as both an advantage and a disadvantage. Systematic bias occurs due to internal standards for inclusion of patients and implementation of therapies, such as general anesthesia for thrombectomies. On the other hand, this bias can be seen as an advantage because the same conditions and criteria apply to the therapy of all patients. Selection and attrition biases are expected to be negligible because most patients eligible for endovascular stroke therapy are admitted to our institution by the regional emergency service or transferring hospitals and only 1 patient was transferred back to their referring hospital immediately after stroke therapy due to capacity reasons. Nonetheless, even though we included a very wide spectrum of patients, the small sample size within the individual groups (especially in our trend analyses) requires a cautious interpretation of our results. Also, causes of death could not be determined in a blinded fashion because the treating clinicians and the reviewing neurologists needed to be aware of the clinical course of patients for their assessment. To develop a full picture of intrahospital mortality, causes of death, and changes due to increased use of endovascular therapy, additional studies will be needed that include additional treatment groups (eg, intravenous thrombolysis) or data of different stroke units.
CONCLUSIONS
The most common intrahospital causes of death in patients with acute stroke who received endovascular therapy are cerebrovascular causes, cardiovascular causes followed by pneumonia and sepsis. One of the most striking findings to emerge from this study is that a large proportion of deceased patients with stroke were treated secondarily with a palliative approach; here, the causes of death should be considered with caution because the reasons for palliation and causes of death differ, albeit not significantly. The reasons for palliation are less vulnerable to bias by life-terminating measures and should be considered when analyzing causes of death.
ABBREVIATION:
- IQR
interquartile range
Footnotes
Disclosure forms provided by the authors are available with the full text and PDF of this article at www.ajnr.org.
References
- 1.World Health Organizaton. Global Health Estimates: Life expectancy and leading causes of death and disability. https://www.who.int/data/gho/data/themes/mortality-and-global-health-estimates. Accessed June 28, 2021
- 2.World Health Organizaton. Global health estimates: Leading causes of death—Cause-specific mortality, 2000–2019. https://www.who.int/data/gho/data/themes/mortality-and-global-health-estimates. Accessed June 28, 2021
- 3.Feigin VL, Forouzanfar MH, Krishnamurthi R, et al. Global and regional burden of stroke during 1990–2010: findings from the Global Burden of Disease Study 2010. Lancet 2014;383:245–54 10.1016/S0140-6736(13)61953-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Huttner HB, Schwab S. Malignant middle cerebral artery infarction: clinical characteristics, treatment strategies, and future perspectives. Lancet Neurol 2009;8:949–58 10.1016/S1474-4422(09)70224-8 [DOI] [PubMed] [Google Scholar]
- 5.Brønnum-Hansen H, Davidsen M, Thorvaldsen P; Danish MONICA Study Group. Long-term survival and causes of death after stroke. Stroke 2001;32:2131–36 10.1161/hs0901.094253 [DOI] [PubMed] [Google Scholar]
- 6.Hankey GJ, Jamrozik K, Broadhurst RJ, et al. Five-year survival after first-ever stroke and related prognostic factors in the Perth Community Stroke Study. Stroke 2000;31:2080–86 10.1161/01.STR.31.9.2080 [DOI] [PubMed] [Google Scholar]
- 7.Loor HI, Groenier KH, Limburg M, et al. Risks and causes of death in a community-based stroke population: 1 month and 3 years after stroke. Neuroepidemiology 1999;18:75–84 10.1159/000069410 [DOI] [PubMed] [Google Scholar]
- 8.Kiyohara Y, Kubo M, Kato I, et al. Ten-year prognosis of stroke and risk factors for death in a Japanese community. Stroke 2003;34:2343–47 10.1161/01.STR.0000091845.14833.43 [DOI] [PubMed] [Google Scholar]
- 9.Vernino S, Brown RD, Sejvar JJ, et al. Cause-specific mortality after first cerebral infarction. Stroke 2003;34:1828–32 10.1161/01.STR.0000080534.98416.A0 [DOI] [PubMed] [Google Scholar]
- 10.Hardie K, Hankey GJ, Jamrozik K, et al. Ten-year survival after first-ever stroke in the Perth Community Stroke Study. Stroke 2003;34:1842–46 10.1161/01.STR.0000082382.42061.EE [DOI] [PubMed] [Google Scholar]
- 11.D'Alton M, Coughlan T, Cogan N, et al. Patterns of mortality in modern stroke care. Ir Med J 2018;111:750 [PubMed] [Google Scholar]
- 12.Aked J, Delavaran H, Lindgren AG. Survival, causes of death and recurrence up to 3 years after stroke: a population-based study. Eur J Neurol 2021;28:4060–68 10.1111/ene.15041 [DOI] [PubMed] [Google Scholar]
- 13.Nogueira RG, Jadhav AP, Haussen DC, et al. Thrombectomy 6 to 24 hours after stroke with a mismatch between deficit and infarct. N Engl J Med 2018;378:11–21 10.1056/NEJMoa1706442 [DOI] [PubMed] [Google Scholar]
- 14.Goyal M, Menon BK, van Zwam WH, et al. Endovascular thrombectomy after large-vessel ischaemic stroke: a meta-analysis of individual patient data from five randomised trials. Lancet 2016;387:1723–31 10.1016/S0140-6736(16)00163-X [DOI] [PubMed] [Google Scholar]
- 15.Bhatia R, Hill MD, Shobha N, et al. Low rates of acute recanalization with intravenous recombinant tissue plasminogen activator in ischemic stroke: real-world experience and a call for action. Stroke 2010;41:2254–58 10.1161/STROKEAHA.110.592535 [DOI] [PubMed] [Google Scholar]
- 16.Emberson J, Lees KR, Lyden P, et al. Effect of treatment delay, age, and stroke severity on the effects of intravenous thrombolysis with alteplase for acute ischaemic stroke: a meta-analysis of individual patient data from randomised trials. Lancet 2014;384:1929–35 10.1016/S0140-6736(14)60584-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Elakkad A, Drocton G, Hui F. Endovascular stroke interventions: procedural complications and management. Semin Intervent Radiol 2020;37:199–200 10.1055/s-0040-1709206 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Balami JS, White PM, McMeekin PJ, et al. Complications of endovascular treatment for acute ischemic stroke: prevention and management. Int J Stroke 2018;13:348–61 10.1177/1747493017743051 [DOI] [PubMed] [Google Scholar]
- 19.Nikoubashman O, Dekeyzer S, Riabikin A, et al. True first-pass effect. Stroke 2019;50:2140–46 10.1161/STROKEAHA.119.025148 [DOI] [PubMed] [Google Scholar]
- 20.Woerdehoff D, Bredbach GB, Frohnhofen H, et al. Palliativversorgung bei Schlaganfall. NeuroGeriatrie 2014;11:69–73 [Google Scholar]
- 21.Nikoubashman O, Schurmann K, Probst T, et al. Clinical impact of ventilation duration in patients with stroke undergoing interventional treatment under general anesthesia: the shorter the better? AJNR Am J Neuroradiol 2016;37:1074–79 10.3174/ajnr.A4680 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Liljehult J, Christensen T, Christensen KB. Early prediction of one-year mortality in ischemic and haemorrhagic stroke. J Stroke Cerebrovasc Dis 2020;29:104667 10.1016/j.jstrokecerebrovasdis.2020.104667 [DOI] [PubMed] [Google Scholar]
- 23.Joundi RA, Martino R, Saposnik G, et al. Dysphagia screening after intracerebral hemorrhage. Int J Stroke 2018;13:503–10 10.1177/1747493017729265 [DOI] [PubMed] [Google Scholar]
- 24.Olsen TS. Stroke recurrence and prognosis after stroke. Handb Clin Neurol 2009;92:407–21 10.1016/S0072-9752(08)01921-0 [DOI] [PubMed] [Google Scholar]
- 25.Diringer MN, Edwards DF, Aiyagari V, et al. Factors associated with withdrawal of mechanical ventilation in a neurology/neurosurgery intensive care unit. Crit Care Med 2001;29:1792–97 10.1097/00003246-200109000-00023 [DOI] [PubMed] [Google Scholar]
- 26.Verkade MA, Epker JL, Nieuwenhoff MD, et al. Withdrawal of life-sustaining treatment in a mixed intensive care unit: most common in patients with catastropic brain injury. Neurocrit Care 2012;16:130–35 10.1007/s12028-011-9567-y [DOI] [PubMed] [Google Scholar]
- 27.Singh T, Peters SR, Tirschwell DL, et al. Palliative care for hospitalized patients with stroke: results from the 2010 to 2012 National Inpatient Sample. Stroke 2017;48:2534–40 10.1161/STROKEAHA.117.016893 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Parry-Jones AR, Paley L, Bray BD, et al. ; on behalf of the SSNAP Collaborative Group. Care-limiting decisions in acute stroke and association with survival: analyses of UK national quality register data. Int J Stroke 2016;11:321–31 10.1177/1747493015620806 [DOI] [PubMed] [Google Scholar]