Abstract
Background
To understand the impact of the COVID-19 pandemic on mortality, this study investigates overall, sex- and age-specific excess all-cause mortality in 20 countries, during 2020.
Methods
Total, sex- and age-specific weekly all-cause mortality for 2015–2020 was collected from national vital statistics databases. Excess mortality for 2020 was calculated by comparing weekly 2020 observed mortality against expected mortality, estimated from historical data (2015–2019) accounting for seasonality, long- and short-term trends. Crude and age-standardized rates were analysed for total and sex-specific mortality.
Results
Austria, Brazil, Cyprus, England and Wales, France, Georgia, Israel, Italy, Northern Ireland, Peru, Scotland, Slovenia, Sweden, and the USA displayed substantial excess age-standardized mortality of varying duration during 2020, while Australia, Denmark, Estonia, Mauritius, Norway, and Ukraine did not. In sex-specific analyses, excess mortality was higher in males than females, except for Slovenia (higher in females) and Cyprus (similar in both sexes). Lastly, for most countries substantial excess mortality was only detectable (Austria, Cyprus, Israel, and Slovenia) or was higher (Brazil, England and Wales, France, Georgia, Italy, Northern Ireland, Sweden, Peru and the USA) in the oldest age group investigated. Peru demonstrated substantial excess mortality even in the <45 age group.
Conclusions
This study highlights that excess all-cause mortality during 2020 is context dependent, with specific countries, sex- and age-groups being most affected. As the pandemic continues, tracking excess mortality is important to accurately estimate the true toll of COVID-19, while at the same time investigating the effects of changing contexts, different variants, testing, quarantine, and vaccination strategies.
Keywords: COVID-19, SARS-CoV-2, all-cause mortality, excess mortality, pandemic, global impact, infection control
Key Messages.
This study highlights that, among the investigated countries, the excess mortality burden during the COVID-19 pandemic disproportionally affected specific countries such as Peru, the USA, Slovenia, England and Wales, Brazil, Italy, Northern Ireland and Georgia.
In sex-specific analyses, excess all-cause mortality was higher in males than in females for all countries, except for Slovenia where excess mortality was higher in females and for Cyprus where excess mortality was similar in both sexes.
For most countries substantial excess mortality was only detectable or was higher in the oldest age group investigated; Peru showed substantial excess mortality even in younger age groups.
Further understanding of the determinants of excess mortality is warranted, in order to strengthen health resilience in the countries and population groups impacted the most.
Introduction
Two years following the first report of cases of a ‘viral pneumonia’ of unknown cause in Wuhan, China, the true toll of the COVID-19 pandemic remains largely underestimated and its determinants are only partially understood.
Nationally published COVID-19 mortality estimates might underestimate or overestimate the actual mortality burden attributed to the pandemic1 due to reasons including i) limited testing, which precluded deaths from being categorized as COVID-19 deaths;2,3 ii) deaths attributed as COVID-19 deaths on the basis of someone testing positive, which led to over-counting in some jurisdictions; iii) a delay in the processing of death certificates, which created a lag in data;4,5 and iv) the burden to the healthcare systems and delays in health seeking behaviour due to COVID-19-related anxiety, which exacerbated deaths due to other non-COVID related causes. As an example, an indirect effect of the COVID-19 pandemic was the subversion of emergency room and hospital functioning to cope with the surge of COVID-positive patients, which may have resulted in lack of proper management of other potentially life-threatening conditions.6
Still, in certain contexts, undercounting mortality related to COVID-19 could have been rapidly overturned as tests were more readily available and made mandatory for all hospital admissions, increasing the likelihood to misclassify unrelated deaths as COVID-19 deaths, leading to likely overestimation of the true COVID-19 related mortality. As a result, differences in testing and definitions make the reported number of COVID-19 deaths not comparable across populations.7
One way to address the aforementioned methodological challenges and obtain more accurate estimates of the toll of the pandemic is to estimate the excess all-cause mortality experienced by countries, by comparing the observed to the expected number of deaths during a specified time window. The expected number of deaths can be predicted using historical data and time series analyses correcting for seasonality and other secular trends.7
To date, most studies investigating excess mortality focused on single countries or world regions during the first months of the pandemic and have mostly relied on publicly available data which are often provisional depending on the frequency of updates and the time window between the study period and data extraction.4,8–17 Furthermore, despite differential incidence rates and comorbidities leading to increased probability to adverse outcomes and deaths between age and sex groups, very few studies on more than one country investigated sex and age-specific excess mortality for the whole of 2020.18,19
In an attempt to better understand the impact of the COVID-19 pandemic on mortality, an international consortium, namely the COVID-19 MORtality (C-MOR) Consortium, consisting of over 50 institutions across 52 countries and six continents was formed.7 The consortium sought to include countries worldwide without restriction and focused all analyses on data from national primary sources. The present study investigates overall, sex and age-specific excess all-cause mortality in 20 countries, during the whole of 2020.
Methods
Data acquisition
Mortality data, collected and provided by partners from 20 countries participating in the international consortium were used in this investigation (including Australia, Austria, Brazil, Cyprus, Denmark, Estonia, France, Georgia, Israel, Italy, Mauritius, Norway, Peru, Slovenia, Sweden, countries of the United Kingdom (UK; England and Wales, Scotland and Northern Ireland), Ukraine and the United States of America (USA)). Total, sex and age-specific weekly all-cause mortality for 2015–2020 was collected from national vital statistics databases, made either publicly available or with restricted access. All countries of the consortium were asked to provide data without a pre-requisite for the civil registration and/or vital statistics system(s) of the country to be of high quality and without a requirement for information to be available in specific age groups. However, collection of weekly mortality estimates was imperative to allow for a more detailed investigation into the timing of excess mortality for each country during 2020. A picture of excess mortality with sufficient granularity provides a more accurate representation of the experience of countries and is of paramount importance for the investigation of drivers and determinants of the excess mortality, such as timing of pandemic waves, seasonality, and government control measures. Depending on the country, all-cause mortality was reported by either ISO week, starting on Monday; Epi week, starting on Sunday; or other national counting week system.
The national primary data sources used in this study and endorsed by the national partners were cross-checked against publicly available data for countries for which information was available. Any minor inconsistencies observed can be explained by retrospective addition of cases and/or delays in reporting of deaths. In addition, internal consistency and quality checks were performed on the data prior to analysis. Data were collected during June and July 2021, several months after the end of the study period, to account for reporting delays (ranging from a few days to a few weeks)4,5 and to allow enough time for data consolidation by reporting authorities toward better data quality.20 The national data source and time unit used per country, as well as data availability exceptions for specific population groups, are summarized in Supplementary Table S1 (available as Supplementary data at IJE online).
Statistical analysis
Total and sex-specific excess mortality for 2020 was calculated by comparing weekly 2020 crude mortality rate (CMR) and age-standardized (ASMR) mortality rate (per 100 000 population) against a baseline mortality (expected weekly mortality rate in 2020) estimated based on historical data (2015–2019) accounting for seasonality, and long- and short-term trends.21–23 For age-specific excess mortality, only non-standardized mortality rates were used.
For the calculation of mortality rates, total, age and sex-specific mid-year population estimates for the participating countries were obtained from the World bank,24 except for the UK nations for which sub-level data from the Office for National Statistics25 was used, and for Cyprus for which Eurostat data26 was used to include only the population in the Republic of Cyprus government-controlled area.
CMRs were calculated for total population and sex-specific groups using Equation (1) and age-specific mortality rates were calculated using Equation (2) (Supplementary Methods, available as Supplementary data at IJE online). Weekly ASMRs were calculated as a weighted average of the age specific mortality rates provided by each country using the WHO World Standard Population 2000–202527 (Equation (3), Supplementary Methods). Because several countries did not report weekly mortality by consistent 5-year or more granular age groups, the method and formula proposed by Klimkin et al. (2021)28 was used for the age standardisation. The aggregate age groups created for each country, based on the provided age-specific all-cause mortality data, are shown in Supplementary Table S2 (available as Supplementary data at IJE online). This method is not as robust as standardisation using detailed 5-year age groups. However, its results have been shown to only slightly deviate in a downward shift from the ASMR obtained using 5-year age groups, with very close (within 5%) agreement in years closer to 2020.28 ASMRs could not be estimated for Scotland due to the lack of age-specific all-cause mortality data (Supplementary Table S1, available as Supplementary data at IJE online).
Expected weekly mortality rate for 2020 was modelled using Poisson regression assuming a quasi-Poisson distribution to account for over-dispersion in the weekly mortality rates as described elsewhere.7 The residual variation was corrected for skewness by applying a 2/3 power transformation before the computation of the expected 95% confidence intervals.21 Standard deviation of the residuals was derived from the expected interval [i.e. (upper expected 95% confidence interval—expected number of deaths)/1.96]. The same model was applied to each country, for total population as well as for sex-specific and age-specific population groups, separately. Age groups <65 vs. 65+ years and/or <70 vs. 70+ years (depending on available data) were compared, to ensure a sufficient number of deaths in each age group for model robustness. For the countries that showed excess mortality in the younger age group (<65 or <70 years), the analysis was additionally performed for two age subgroups, namely <45 years and 45–64 years, or <50 and 50–69 years.
The regression models were built on complete weeks and any truncated weeks were excluded. Expected mortality rates were estimated for the corresponding complete weeks only. Truncated weeks are usually a result of the different death counts observed around Christmas and New Year,29 and these included week 53 (applicable for Australia, Austria, Cyprus, England and Wales, Estonia, France, Georgia, Mauritius, Northern Ireland, Norway, Peru, Scotland, Slovenia, Sweden, and Ukraine), week 52 for England and Wales and Scotland, weeks 51–52 for Northern Ireland, and week 1 for Mauritius. For all countries, observed and expected weekly mortality rates for 2020 were each summed up to week 52, except for England and Wales and Scotland (up to week 51), N. Ireland (up to week 50), and Mauritius (weeks 2–52).
Then, the cumulative expected 2020 mortality rate was subtracted from the cumulative observed 2020 mortality rate to obtain an estimate of excess mortality for the whole of 2020. The statistical significance of excess mortality rate was determined using the 95% confidence intervals estimated by the model.
The weekly results of the observed versus expected mortality rates are displayed graphically using z-scores [(number of observed deaths—expected mortality)/standard deviation of the residuals]. Z-scores ranging between -2 and +2 are considered ‘normal’, while a z-score >4 is considered a substantial increase.30,31
All analyses were performed in R Statistical Software, version 4.0.5 (The R Foundation for Statistical Computing, Vienna, Austria).
Results
Quality of vital registrations between countries varied, with 17 countries (85.0%) having very high or high, one country (Peru) having medium, and two countries (Georgia and Ukraine) having low quality civil registration and vital statistics systems32 (Supplementary Table S1). Therefore, presented results need to be interpreted with analogous caution.
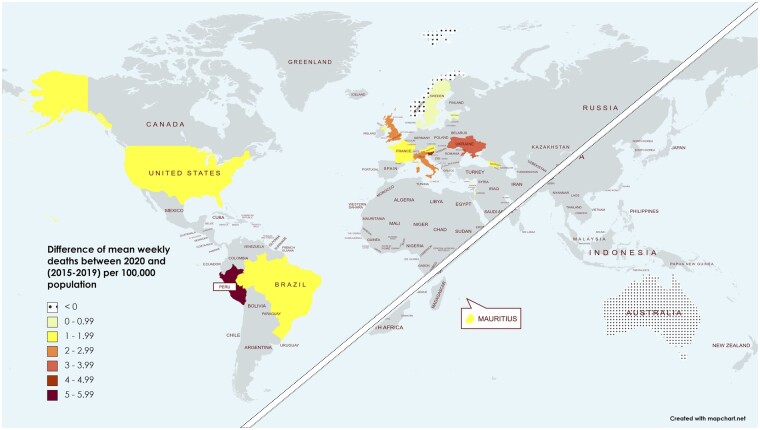
The average weekly mortality rate per 100 000 varied widely between years and between countries (Supplementary Table S3, available as Supplementary data at IJE online). Figure 1 displays the difference in weekly mean of all-cause deaths between years 2015–2019 and year 2020 for each country, per 100 000 population (raw data in Supplementary Table S3). All participating countries, except Australia and Norway, experienced a higher weekly mean of all-cause mortality rate in 2020 than during the previous five years.
Figure 1.
Difference in weekly mean of observed mortality rates between 2020 and 2015–19
Weekly comparisons—total population and by sex
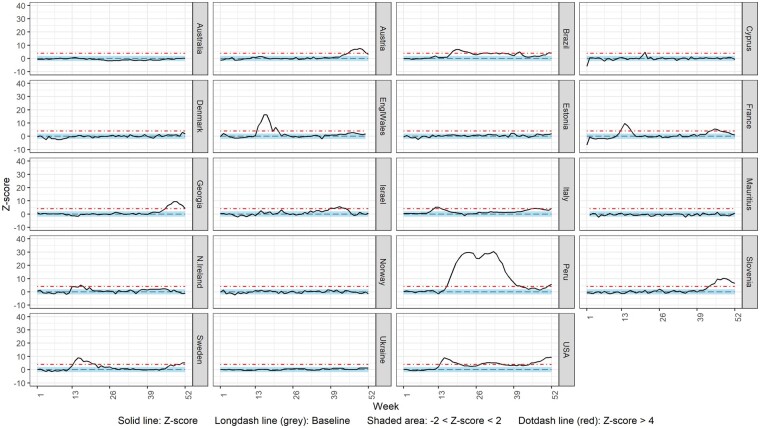
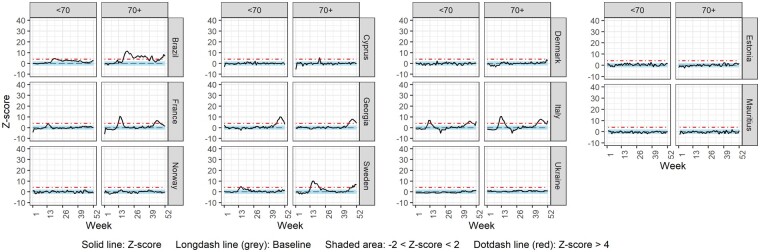
Figure 2 shows the weekly ASMR z-score over time from Week 1 2020 to Week 52 2020 for the total population for each country with the exception of Scotland, for which ASMR could not be estimated. Of the 19 included countries, Austria (Weeks 45–51), Brazil (Weeks 18–24, 29–30, 32–33, 35, 41 and 51–52), Cyprus (Week 21), England and Wales (Weeks 14–18, 20), France (Weeks 13–16 and 44–47), Georgia (Weeks 46–52), Israel (Weeks 39–44), Italy (Weeks 12–14, 45–47 and 52), Northern Ireland (Weeks 13 and 16), Peru (Weeks 16–41 and 51–52), Slovenia (Weeks 43–52), Sweden (Weeks 14–21, 49 and 51–52) and the USA (Weeks 14–20, 28–34, and 45–52) displayed substantial (>4 z-scores) excess mortality in 2020. In contrast, Australia, Denmark, Estonia, Mauritius, Norway and Ukraine did not display substantial excess mortality for any week during 2020. Similar results were obtained when analysing CMRs; CMR analysis for Scotland highlighted substantial excess mortality in Weeks 14–20 (Supplementary Figure S1, available as Supplementary data at IJE online).
Figure 2.
Weekly z-score of age-standardized all-cause mortality rate for total population
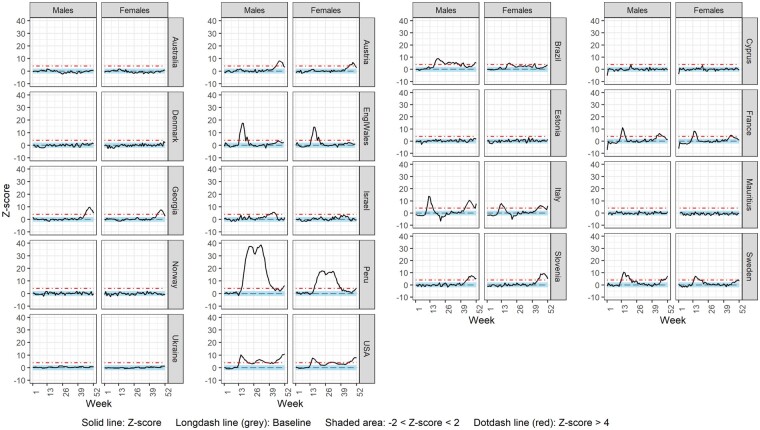
Sex-specific weekly ASMR z-scores over 2020 are shown for each country in Figure 3, except for Northern Ireland and Scotland for which sex-specific all-cause mortality and ASMR were not available, respectively (Supplementary Table S1). For most countries displaying substantial excess mortality, this was higher in males compared with females (Austria, Brazil, England and Wales, France, Georgia, Israel, Italy, Peru, Sweden and the USA) for the majority of weeks. Only Slovenia experienced higher excess mortality in females compared with males. In Cyprus, there were no notable differences in excess mortality between sexes. Similar trends were observed using CMRs, with the exception of the USA for which CMRs were higher in females than in males; CMR analysis for Scotland showed higher excess mortality in males than in females (Supplementary Figure S2, available as Supplementary data at IJE online).
Figure 3.
Weekly z-score of age-standardized all-cause mortality rate by sex
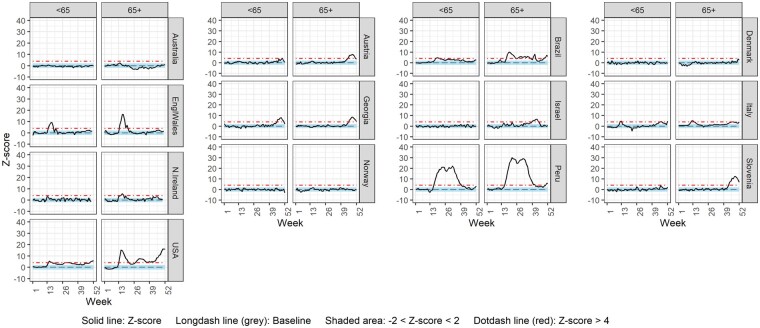
Weekly comparisons—by age group
Figures 4 and 5 display weekly mortality rate z-score over time for ages <65 vs 65+ and ages <70 vs 70+ years, respectively. Countries were included in each figure, or in both, according to the age breakdown of the data provided. Scotland was not included due to lack of age-specific all-cause mortality data (Supplementary Table S1). In Austria, Cyprus, Israel and Slovenia, substantial excess mortality was only observed in the oldest age group, whereas for Brazil, England and Wales, France, Georgia, Italy, Northern Ireland, Sweden, Peru and the USA, substantial excess mortality was observed in both age groups but was more pronounced in the oldest one (65+ and/or 70+ years). For Estonia, even though excess mortality was not substantial for either age group, it was more pronounced in the <70 age group than in the 70+ age group.
Figure 4.
Weekly z-score of all-cause mortality rate for age groups <65 and 65+
Figure 5.
Weekly z-score of all-cause mortality rate for age groups <70 and 70+
Supplementary Figure S3 (available as Supplementary data at IJE online), displays the observed z-scores against those expected by more detailed age breakdowns for the countries observing excess mortality in the younger age groups. If substantial excess mortality was observed in the <65 years age group, this was further divided into <45 and 45–64 years (Supplementary Figure S3a), and the <70 years age group was further broken down to <50 and 50–69 years (Supplementary Figure S3b). For the USA, the available age groups were <15 and 15–64 years (Supplementary Figure S3c, available as Supplementary data at IJE online). Most countries observed substantial excess mortality only in the older of the two age groups. In contrast, Peru demonstrated substantial excess mortality also in the <45 years old age group.
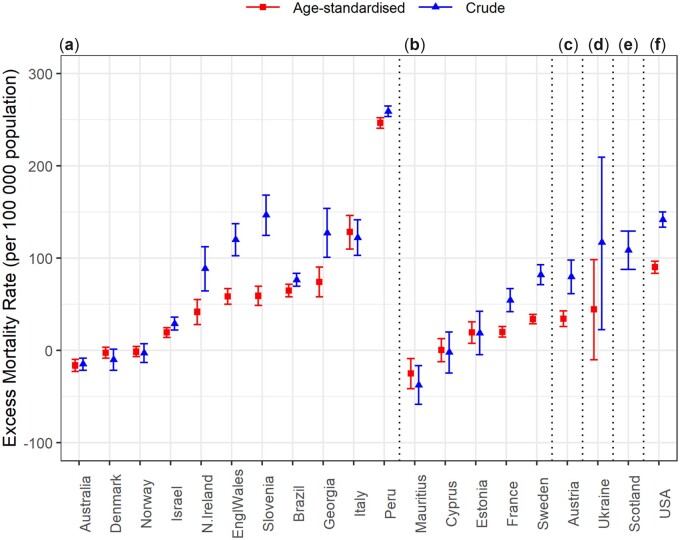
Excess mortality in 2020
Figure 6 and Supplementary Table S4 (available as Supplementary data at IJE online) display the cumulative expected and observed all-cause mortality rates for the whole year (2020), using CMRs and ASMRs. The following countries demonstrated statistically significant excess cumulative ASMRs during 2020: Austria, Brazil, France, England and Wales, Estonia, Georgia, Italy, Israel, Northern Ireland, Peru, Slovenia, Sweden and the USA. Scotland also demonstrated excess CMR in 2020. On the other hand, Australia and Mauritius demonstrated statistically significant decreases in yearly all-cause mortality rate. Cyprus, Denmark, Norway and Ukraine, observed no statistically significant differences in all-cause mortality. Similar results were obtained with CMR, except for Estonia, where the increase in CMR is not significant, and for Ukraine, where the increase in CMR is significant in contrast to the increase in ASMR.
Figure 6.
Cumulative excess crude and age-standardized mortality rate, for 2020. Plot letters correspond to the age groups in which countries have provided data and therefore the age groups used for age standardization: (a) age groups <15, 15–44, 45–64, 65+; (b) age groups <19, 20–49, 50–69, 70+; (c) age groups <19, 20–49, 50–64, 65+; (d) age groups <15, 15–64, 65+; (e) age groups <19, 20–54, 55–69, 70+ (Supplementary Table S3, available as Supplementary data at IJE online)
Supplementary Tables S5 and S6 (available as Supplementary data at IJE online) report the yearly cumulative mortality rate differences (observed-expected) by sex using CMRs and ASMRs, respectively. Sex-specific differences in all-cause ASMR for the whole year were only observed for Norway and Ukraine (significant increase only in males), and for Mauritius (statistically significant decrease only in females). Supplementary Table S7 (available as Supplementary data at IJE online) demonstrates the cumulative CMR differences (observed-expected) by age group. Age-specific differences in all-cause mortality for the whole year were observed in France, Israel and Slovenia (significant increase only in the older age group: 65+ or 70+), in Estonia (significant increase only in the younger age group: <70) and in Ukraine (significant decrease in the younger age group and significant increase in the older age group: 70+).
Discussion
This study evaluated total, sex-specific and age-specific excess all-cause mortality in 20 countries during the year 2020.
The majority of investigated countries (Austria, Brazil, Cyprus, England and Wales, France, Georgia, Israel, Italy, Northern Ireland, Peru, Scotland, Slovenia, Sweden and the USA) displayed significant excess mortality during at least 1 week of 2020. The duration of the significant excess mortality varied widely, between 1 and 2 weeks in Cyprus and Northern Ireland, 6 to 8 weeks in Austria, England and Wales, Georgia, Israel, Italy and Scotland, nine to 11 weeks in France, Slovenia, and Sweden, 15 weeks in Brazil, 28 weeks in Peru and 37 weeks in the USA. Conversely, Australia, Denmark, Estonia, Mauritius, Norway and Ukraine did not observe significant excess all-cause mortality, compared with what was expected, for any week in 2020. These results are largely in agreement with results published elsewhere, despite the use of varying methodologies and data sources,19,33–37 thus reinforcing our findings.
More specifically, Schöley et al. (2021), comparing varying methodologies using data from the Short Term Mortality Fluctuations (STMF) database, also identified Slovenia as having a high excess of all-cause deaths, Denmark and Norway with very little and Austria and Sweden in the middle ranks of excess all-cause mortality.37 Using the same data, Islam et al. (2021) also identified the USA, Italy and England and Wales as being the most affected countries in terms of excess deaths, and Slovenia, the USA, countries of the UK and Italy as most affected in terms of ASMRs. Karlinsky and Kobak (2021) used data from the World Mortality Dataset until the end of 2020 or the first half of 2021, and also evidenced Peru, Brazil, the USA, Italy and countries of the UK to be most affected and Australia to be the least affected in terms of excess absolute death numbers.38 Nepomuceno et al. (2021) identified Italy, the USA, Slovenia and countries of the UK as the most heavily affected in terms of CMRs and ASMRs, using an array of different methodologies.39 Last, in their investigation of Latin American countries, Lima et al. (2021) also identified Peru and Brazil as having experienced high excess all-cause mortality.40
As expected, the countries with prolonged substantial excess mortality in the weekly comparison also demonstrated statistically significant cumulative excess ASMR when comparing the sum of observed weekly mortality rates with the sum of expected weekly mortality rates for 2020, with the exception of Estonia. Despite having zero weeks with substantial (z-score >4) excess mortality, the statistically significant, but small in magnitude, excess yearly mortality observed by Estonia could be explained by the relatively stable mortality pattern of the country, which made even small increases in mortality show up as statistically significant.
The observed pattern of weekly excess mortality in the investigated countries indicates that some countries experienced substantial excess mortality during the first half of the year but not later (Cyprus, England and Wales, Northern Ireland and Scotland), whereas others did so during the last trimester of 2020 but not earlier (Austria, Georgia, Israel and Slovenia). For some countries, two distinct peaks in excess mortality were observed suggesting two pandemic mortality waves (France, Italy and Sweden), whereas for the most affected countries substantial excess mortality was prolonged throughout the year (Brazil, Peru and the USA). Similar peaks in excess mortality for the participating countries were observed elsewhere.19,33–36 Variation in the timing, strictness and duration of governmental control measures could explain the excess mortality patterns in the participating countries,7 along with other indicators shown to influence excess mortality such as health privatization, health expenditure, numbers of doctors and hospital beds, share of population covered by health insurance and test-and-trace capacity.41
In sex-specific weekly analyses, excess ASMR was more pronounced in males than in females, with the exception of Slovenia (higher in females) and of Cyprus (similar in both sexes). In the yearly cumulative comparison, increases or decreases in all-cause mortality were similar between sexes except for Norway (statistically significant increase only in males), for Mauritius (statistically significant decrease only in females) and for Ukraine (statistically significant increase in males and decrease in females). The male predominance in excess mortality observed in most countries, even following standardization, was previously shown19,42,43 and is expected, since male sex was identified as a risk factor for death by a global COVID-19 meta-analysis.44 In fact, all-cause male mortality has been historically higher compared with female all-cause mortality.45 Biological factors, such as a stronger immune response, and behavioural risk factors, such as smoking and other lifestyle habits, are some of the reasons why men are at a greater risk for death as a consequence of COVID-19 or of other common causes of death.46 In Slovenia the excess mortality in females is probably explained by the observed higher case fatality ratio for COVID-19 among females than males.47 Taken together, these results support the need for sex-specific investigations in excess mortality to better assess and understand the determinants of the true toll of the COVID-19 pandemic.
Interestingly, in total and sex-specific analyses, similar results were obtained when analysing CMR instead of ASMRs, except for Estonia, where the increase in cumulative 2020 CMR is not significant, and of Ukraine, where the increase in CMR is significant in contrast to the increase in ASMR. Another exception is sex-specific excess mortality in the USA, for which CMR was higher in females than in males, whereas ASMR was higher in males than in females. These results suggest that the age pattern of mortality was different across time within countries and also between the sexes, supporting the use of ASMRs where possible.30
With respect to weekly age-specific analyses, for most countries excess mortality was only evident (Austria, Cyprus, Israel and Slovenia) or was higher (Brazil, England and Wales, France, Georgia, Italy, Northern Ireland, Sweden, Peru and the USA) in the oldest age group investigated (65+ or 70+). This finding is expected since, in the absence of vaccination, age is one of the strongest predictors of all-cause and COVID-19 mortality48 and globally, the age dependency of COVID-19 (the factor by which the risk of COVID-19 mortality increases if age is increased by 10 years) is strongly associated with all-cause mortality.49 Interestingly, for Peru, excess cumulative mortality for the whole of 2020 was substantially high also in the age group <45. This result is supported by other studies showing that countries in the Americas have suffered the most potential years of life lost due to COVID-19.42 Demographic, socioeconomic, racial and pre-pandemic health status factors, such as comorbidity prevalence, can explain the increased risk of death from both COVID-19 and other causes in younger age groups in this country.16,50–52
The comparison of the sum of observed deaths with the sum of expected deaths for the whole year (2020) yielded mostly similar results, with some surprising findings. In Estonia the significant increase in yearly deaths was only observed in the younger age group (<70). This result can be explained by an increased prevalence of comorbidities in the Estonian population aged under 70 years53 and by strict control measures taken, which directly or indirectly protected the most vulnerable age groups during 2020.54
Strengths and limitations
To our knowledge, this is one of few studies investigating total, sex-specific and age-specific excess mortality for a diverse group of countries, relying on national data sources for mortality estimates. It complements other studies that quantify the impacts of the COVID-19 pandemic through life expectancy losses.18,40 In addition, it is the first peer-reviewed publication of excess mortality results for Mauritius and Georgia. Of the 20 countries included in the analysis, 17 (85.0%) were evaluated as having very high- or high-quality civil registration and vital statistics systems; only two (Georgia and Ukraine) and one (Peru) countries were evaluated as having low- and medium-quality systems, respectively).32 Focusing on death registrations, all countries included in this investigation had a coverage of 90% and above, except for Peru (50–74%).55 In addition, the model used for the estimation of excess mortality is one that has been shown to produce estimates with the least bias compared with other methods.37,39 Furthermore, this investigation allowed for any delays in data reporting, ensuring a more accurate representation of the mortality experience of countries during 2020. Of note, as the analysis was carried out using data from 2020, results were not influenced by the effects of vaccination (scarcely available in any country before the end of 2020; highest population percentages fully vaccinated on 31 December 2020 were 0.6% and 0.01% for the UK and the USA, respectively48) nor by newer virus variants. Therefore, the results serve as a useful comparator against which to investigate the effects of vaccinations and impact of new variants which defined the pandemic trajectory in subsequent years. However, our study also has some limitations such as the lack of data that would allow estimation of the direct and indirect contributions of COVID-19 to excess all-cause mortality. In addition, participating countries did not use consistent age groups to calculate age-specific all-cause mortality. Age-standardized results are thus not fully comparable between countries. Therefore, the magnitude of excess mortality for 2020 should not be used as a measure of comparison of impact between countries; rather as an indicator of the COVID-19 impact on all-cause mortality in each country. Last, even though the high quality of registration systems in the majority of the countries included in our investigation reinforces the validity of our results, it is important to acknowledge that for countries where the health system was overwhelmed with hospitalizations and mortality during 2020, quality could be compromised to a degree not amenable to allowing sufficient time to capture any delays in data reporting.
Conclusion
Our findings on excess mortality during 2020 show the asymmetrical impacts of the pandemic, highlighting countries where the impact was more extensive or more limited. Overall, males carried a heavier burden, with the exception of Slovenia where females displayed a higher excess mortality than males. In most countries, excess mortality was substantial and a public health concern in the oldest age groups, with some notable exceptions, namely Peru where excess mortality was high also in younger age groups, and Estonia where excess mortality for the whole year was higher in the 50–69 group compared with the 70+ group.
These results, which show that excess mortality during the first year of the pandemic was context-specific, prompt further investigation into the determinants of excess mortality in countries and in specific sex and age groups, which will further suggest steps to strengthen health resilience for those most affected. Furthermore as the pandemic continues, tracking excess mortality is of paramount importance in order to accurately estimate the true toll of COVID-19, at the same time investigating the effects that different variants, vaccination strategies and further public health interventions had in the studied countries.
Ethics approval
Ethical approval to conduct the study was obtained from the Cyprus National Bioethics Committee (16/6/2020, ΕΕΒΚ/ΕΠ/2020/01.127).
Supplementary Material
Contributor Information
Christiana A Demetriou, Department of Primary Care and Population Health, University of Nicosia Medical School, Nicosia, Cyprus.
Souzana Achilleos, Department of Primary Care and Population Health, University of Nicosia Medical School, Nicosia, Cyprus.
Annalisa Quattrocchi, Department of Primary Care and Population Health, University of Nicosia Medical School, Nicosia, Cyprus.
John Gabel, University of Nicosia Medical School, Nicosia, Cyprus.
Elena Critselis, Department of Primary Care and Population Health, University of Nicosia Medical School, Nicosia, Cyprus.
Constantina Constantinou, Department of Basic and Clinical Sciences, University of Nicosia Medical School, Nicosia, Cyprus.
Nicoletta Nicolaou, Department of Basic and Clinical Sciences, University of Nicosia Medical School, Nicosia, Cyprus.
Giuseppe Ambrosio, Department of Medicine, University of Perugia School of Medicine, Perugia, Italy.
Catherine M Bennett, Institute for Health Transformation, Deakin University, Burwood, Australia.
Nolwenn Le Meur, University of Rennes, EHESP, CNRS, Inserm, Arènes—UMR 6051, RSMS—U 1309, Rennes, France.
Julia A Critchley, Population Health Research Institute, St George’s, University of London, London, UK.
Laust Hvas Mortensen, Department of Methods and Analysis, Statistics Denmark, Copenhagen Oe, Denmark.
Jose Manuel Rodriguez-Llanes, European Commission Joint Research Centre, Ispra, VA, Italy.
Mario Chong, Departamento de Ingeniería, Universidad del Pacífico, Lima, Peru.
Gleb Denissov, Estonian Causes of Death Registry, National institute for Health Development, Tallinn, Estonia.
Petra Klepac, Department of Communicable Diseases, National Institute of Public Health, Ljubljana, Slovenia.
Lucy P Goldsmith, Institute for Infection and Immunity, and Population Health Research Institute, St George's, University of London, London, UK.
Antonio José Leal Costa, Institute of Studies in Collective Health (IESC), Federal University of Rio de Janeiro, Rio de Janeiro, Brazil.
Terje P Hagen, Department of Health Management and Health Economics, Institute of Health and Society, University of Oslo, Oslo, Norway.
Marie Chan Sun, Department of Medicine, Faculty of Medicine and Health Sciences, University of Mauritius, Réduit, Mauritius.
Qian Huang, Department of Geography, Center for Rural and Primary Healthcare, University of South Carolina, Columbia, SC, USA.
Nataliia Pidmurniak, Department of Medicine, Bogomolets National Medical University, Kyiv, Ukraine.
Inbar Zucker, School of Public Health, Ministry of Health, Ramat Gan, Israel.
Joseph Cuthbertson, Disaster Resilience Initiative, Monash University, Clayton,VIC, Australia.
Bo Burström, Department of Global Public Health, Karolinska Institutet, Stockholm, Sweden.
Manuel Barron, Department of Economics, Universidad del Pacifico Av Sanchez Cerro, Lima, Peru.
Ivan Eržen, School of Public Health, National Institute of Public Health, Medical Faculty, University of Ljubljana, Ljubljana, Slovenia.
Fabrizio Stracci, Public Health Section, Department of Medicine and Surgery, University of Perugia, Piazza Lucio Severi, Perugia, Italy.
Wilson Calmon, Institute of Mathematics and Statistics, Fluminense Federal University, Niteroi, Brazil.
Cyndy Martial, Department of Demography, Statistics Mauritius, LIC Centre, Port Louis, Mauritius.
Olesia Verstiuk, University of Nicosia Medical School, Nicosia, Cyprus.
Zalman Kaufman, Israeli Center of Disease Control, Ministry of Health, Ramat Gan, Israel.
Wenjing Tao, Department of Global Public Health, Karolinska Institutet, Stockholm, Sweden; Department of Molecular Medicine and SURGERY, Karolinska Institutet, Stockholm, Sweden.
Maia Kereselidze, National Center for Disease Control and Public Health, Tbilisi, Georgia.
Nino Chikhladze, Faculty of Medicine, Ivane Javakhishvili Tbilisi State University, Tbilisi, Georgia.
Claudia Zimmermann, Department of Epidemiology, Center for Public Health, Medical University of Vienna, Vienna, Austria.
Eva Schernhammer, Department of Epidemiology, Center for Public Health, Medical University of Vienna, Vienna, Austria.
Antonis Polemitis, University of Nicosia, Nicosia, Cyprus.
Andreas Charalambous, University of Nicosia Medical School, Nicosia, Cyprus.
Data availability
The data underlying this study, beyond what is available in the article and in its online Supplementary material, can be shared to facilitate methodologically sound proposals after signing a data access agreement. Proposals and data requests should be directed to [demetriou.chri@unic.ac.cy].
Supplementary data
Supplementary data are available at IJE online.
Author contributions
Authors C.A.D., S.A., A.Q., E.C., C.C., G.A., J.M.R.L., C.M.B., L.H.M., N.L.M. and J.A.C. contributed to: (i) the concep and design of the study, or acquisition of data, or analysis and interpretation of data; (ii) the drafting of the article or revising it critically for important intellectual content: and (iii) the final approval of the version to be submitted. Authors J.G., N.N., M.C., G.D., P.K., L.P.G., A.J.L.C., T.P.H., M.C.S., Q.H., N.P., I.Z., J.C., B.B., M.B., I.E., F.S., W.C., C.M., O.V., Z.K., W.T., M.K., N.C., A.P. and A.C. contributed to: (i) the concept and design of the study, or acquisition of data, or analysis and interpretation of data; and (ii) the final approval of the version to be submitted.
Funding
This work was supported by the University of Nicosia Medical School (internal funding). The funding source did not have any involvement in study design; the collection, analysis and interpretation of data; in the writing of the report; or in the decision to submit the paper for publication.
Conflict of interest
None declared.
References
- 1. Morgan D, Ino J, Paolantonio GD, Murtin F.. Excess Mortality: Measuring the Direct and Indirect Impact of COVID-19. 2020. https://www.oecd-ilibrary.org/content/paper/c5dc0c50-en (22 November 2021, date last accessed)
- 2. Arons MM, Hatfield KM, Reddy SC. et al. ; Public Health–Seattle and King County and CDC COVID-19 Investigation Team. Presymptomatic SARS-CoV-2 infections and transmission in a skilled nursing facility. N Engl J Med 2020;382:2081–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Li R, Pei S, Chen B. et al. Substantial undocumented infection facilitates the rapid dissemination of novel coronavirus (SARS-CoV-2). Science 2020;368:489–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Felix-Cardoso J, Vasconcelos H, Rodrigues P, Cruz-Correia R, Excess mortality during COVID-19 in five European countries and a critique of mortality analysis data. medRxiv 2 May 2020. doi: 10.1101/2020.04.28.20083147. Preprint: not peer-reviewed. [DOI]
- 5. Quast T, Andel R, Gregory S, Storch EA.. Years of life lost associated with COVID-19 deaths in the United States. J Public Health (Oxf) 2020;42:717–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Sofi F, Dinu M, Reboldi G. et al. Worldwide differences of hospitalization for ST-segment elevation myocardial infarction during COVID-19: a systematic review and meta-analysis. Int J Cardiol 2022;347:89–96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Achilleos S, Quattrocchi A, Gabel J. et al. Excess all-cause mortality and COVID-19-related mortality: a temporal analysis in 22 countries, from January until August 2020. Int J Epidemiol 2022;51:35–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Alicandro G, Remuzzi G, Vecchia CL.. Italy’s first wave of the COVID-19 pandemic has ended: no excess mortality in May, 2020. Lancet 2020;396:e27–e28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Blangiardo M, Cameletti M, Pirani M, Corsetti G, Battaglini M, Baio G.. Estimating weekly excess mortality at sub-national level in Italy during the COVID-19 pandemic. PLoS One 2020;15:e0240286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Brown PE, Greenwald ZR, Salinas LE. et al. Mortality from COVID in Colombia and Peru: Analyses of Mortality Data and Statistical Forecasts. medRxiv 16 November 2020. doi: 10.1101/2020.08.24.20181016. Preprint: not peer-reviewed. [DOI]
- 11. Chan EYS, Cheng D, Martin J.. Impact of COVID-19 on excess mortality, life expectancy, and years of life lost in the United States. PLoS One 2021;16:e0256835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Fouillet A, Pontais I, Caserio-Schönemann C.. Excess all-cause mortality during the first wave of the COVID-19 epidemic in France, March to May 2020. Euro Surveill 2020;25:2001485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Freitas ARR, Medeiros N. D, Frutuoso LCV. et al. Tracking excess deaths associated with the COVID-19 epidemic as an epidemiological surveillance strategy: preliminary results of the evaluation of six Brazilian capitals. Rev Soc Bras Med Trop 2020;53:e20200558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Michelozzi P, Donato FD, Scortichini M. et al. Temporal dynamics in total excess mortality and COVID-19 deaths in Italian cities. BMC Public Health 2020;20:1238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Modig K, Ahlbom A, Ebeling M.. Excess mortality from COVID-19. Weekly excess death rates by age and sex for Sweden and its most affected region. Eur J Public Health 2021;31:17–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Santos AD, Souza BD, Carvalho CD. et al. Excess deaths from all causes and by COVID-19 in Brazil in 2020. Rev Saude Publica 2021;55:71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Stang A, Standl F, Kowall B. et al. Excess mortality due to COVID-19 in Germany. J Infect 2020;81:797–801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Aburto JM, Schöley J, Kashnitsky I. et al. Quantifying impacts of the COVID-19 pandemic through life expectancy losses: a population-level study of 29 countries. Int J Epidemiol 2022;51:63–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Islam N, Shkolnikov VM, Acosta RJ. et al. Excess deaths associated with covid-19 pandemic in 2020: age and sex disaggregated time series analysis in 29 high income countries. BMJ 2021;373:n1137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Inserm-CépiDc. Covid-19. 2020. https://opendata.idf.inserm.fr/cepidc/covid-19/ (15 June 2022, date last accessed)
- 21. Farrington CP, Andrews NJ, Beale AD, Catchpole MA.. A statistical algorithm for the early detection of outbreaks of infectious disease. J R Stat Soc Ser A (Stat Soc) 1996;159:547–63. [Google Scholar]
- 22. Serfling RE. Methods for current statistical analysis of excess pneumonia-influenza deaths. Public Health Rep 1963;78:494–506. [PMC free article] [PubMed] [Google Scholar]
- 23. Nielsen J, Krause TG, Mølbak K.. Influenza-associated mortality determined from all-cause mortality, Denmark 2010/11-2016/17: The FluMOMO model. Influenza Other Respir Viruses 2018;12:591–604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. World Bank. Population, Total | Data. 2021. https://data.worldbank.org/indicator/SP.POP.TOTL (20 November 2021, date last accessed).
- 25. Office for National Statistics UK. National Life Tables: UK: Office for National Statistics. 2020. https://www.ons.gov.uk/peoplepopulationandcommunity/birthsdeathsandmarriages/lifeexpectancies/datasets/nationallifetablesunitedkingdomreferencetables (9 February 2021, date last accessed)
- 26. European Commission. Eurostat: Population on 1 January. 2021. http://ec.europa.eu/eurostat/web/population-demography-migration-projections/population-data/main-tables (25 January 2021, date last accessed).
- 27. Ahmad OB, Boschi-Pinto C, Gomez-Auli A. et al. Age Standardisation of Rates: A New WHO Standard. 2001.. https://www.scienceopen.com/document?vid=3c53ea70-1068-4276-b466-be49082fbf15 (11 July 2022, date last accessed).
- 28. Klimkin I, Shkolnikov VM, Jdanov DA, Calculation of Week-Specific Age-Standardised Death Rates from STMF Data on Mortality by Broad Age Intervals..Rostock, Germany: Max Planck Institute for Demographic Research, 2021. 10.4054/MPIDR-WP-2021-004 (5 May 2022, date last accessed). [DOI] [Google Scholar]
- 29. Kontis V, Bennett JE, Rashid T. et al. Magnitude, demographics and dynamics of the effect of the first wave of the COVID-19 pandemic on all-cause mortality in 21 industrialized countries. Nat Med 2020;26:1919–28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Vestergaard LS, Nielsen J, Richter L. et al. Excess all-cause mortality during the COVID-19 pandemic in Europe – preliminary pooled estimates from the EuroMOMO network, March to April 2020. Euro Surveill 2020;25:2001214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Nielsen J, Vestergaard LS, Richter L. et al. European all-cause excess and influenza-attributable mortality in the 2017/18 season: should the burden of influenza B be reconsidered? Clin Microbiol Infect 2019;25:1266–76. [DOI] [PubMed] [Google Scholar]
- 32. Mikkelsen L, Phillips DE, AbouZahr C. et al. A global assessment of civil registration and vital statistics systems: monitoring data quality and progress. Lancet 2015;386:1395–406. [DOI] [PubMed] [Google Scholar]
- 33. The Economist. Tracking covid-19 excess deaths across countries. 2021. https://www.economist.com/graphic-detail/coronavirus-excess-deaths-tracker (2 December 2021, date last accessed).
- 34. Centres for Disease Control and Prevention, National Center for Health Statistics. Excess Deaths Associated with COVID-19. 2021. https://www.cdc.gov/nchs/nvss/vsrr/covid19/excess_deaths.htm (2 December 2021, date last accessed).
- 35. EUROMOMO. Graphs and Maps: Z-Scores by Country. https://euromomo.eu/dev-404-page/ (2 December 2021, date last accessed).
- 36. Our World in Data. Excess Mortality: Raw Number of Deaths From All Causes Compared With Projection Based on Previous Years. 2021. https://ourworldindata.org/grapher/excess-mortality-raw-death-count (2 December 2021, date last accessed)
- 37. Schöley J. Robustness and bias of European excess death estimates in 2020 under varying model specifications. medRxiv 9 June 2021. doi: 10.1101/2021.06.04.21258353v1. Preprint: not peer-reviewed. [DOI]
- 38. Karlinsky A, Kobak D.. Tracking excess mortality across countries during the COVID-19 pandemic with the World Mortality Dataset. Elife 2021;10:e69336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Nepomuceno MR, Klimkin I, Jdanov DA, Alustiza-Galarza A, Shkolnikov VM.. Sensitivity analysis of excess mortality due to the COVID-19 pandemic. Popul Dev Rev 2022;48:279–302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Lima EEC, Vilela EA, Peralta A. et al. Investigating regional excess mortality during 2020 COVID-19 pandemic in selected Latin American countries. Genus 2021;77:30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Kapitsinis N. The underlying factors of excess mortality in 2020: a cross-country analysis of pre-pandemic healthcare conditions and strategies to cope with Covid-19. BMC Health Serv Res 2021;21:1197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Ugarte MP, Achilleos S, Quattrocchi A. et al. ; C-MOR consortium. Premature mortality attributable to COVID-19: potential years of life lost in 17 countries around the world, January–August 2020. BMC Public Health 2022;22:54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Arolas HI, Acosta E, Casasnovas GL. et al. Global years of life lost to COVID-19. 2020. https://ideas.repec.org/p/osf/socarx/gveaj.html (20 November 2020, date last accessed).
- 44. Peckham H, Gruijter NM, de Raine C. et al. Male sex identified by global COVID-19 meta-analysis as a risk factor for death and ITU admission. Nat Commun 2020;11:6317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Nielsen J, Nørgaard SK, Lanzieri G, Vestergaard LS, Moelbak K.. Sex-differences in COVID-19 associated excess mortality is not exceptional for the COVID-19 pandemic. Sci Rep 2021;11:20815. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Bwire GM. Coronavirus: why men are more vulnerable to covid-19 than women? SN Compr Clin Med 2020;2:874–76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Global Health 50/50. The Sex, Gender and COVID-19 Project. 2021. https://globalhealth5050.org/the-sex-gender-and-covid-19-project/ (3 December 2021, date last accessed)
- 48. Ritchie H, Mathieu E, Rodés-Guirao L. et al. Statistics and Research: Mortality Risk of COVID-19. 2020. https://ourworldindata.org/excess-mortality-covid (2 December 2021, date last accessed).
- 49. Bauer P, Brugger J, König F, Posch M.. An international comparison of age and sex dependency of COVID-19 deaths in 2020: a descriptive analysis. Sci Rep 2021;11:19143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Polyakova M, Udalova V, Kocks G, Genadek K, Finlay K, Finkelstein A.. Racial Disparities in Excess All-Cause Mortality During the Early COVID-19 Pandemic Varied Substantially Across States. Washington, DC: Social, Economic, and Housing Statistics Division, US Census Bureau, 2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Stokes AC, Lundberg DJ, Elo IT, Hempstead K, Bor J, Preston SH.. COVID-19 and excess mortality in the United States: a county-level analysis. PLoS Med 2021;18:e1003571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Institute for Health Metrics and Evaluation (IHME). GBD Compare: Country Profiles. 2021. https://www.healthdata.org/results/country-profiles (9 February 2022, date last accessed).
- 53. Jürisson M, Pisarev H, Uusküla A. et al. Physical-mental health comorbidity: a population-based cross-sectional study. PLoS One 2021;16:e0260464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Hale T, Atav T, Hallas L. et al. Oxford COVID-19 Government Response Tracker. 2020. https://qap.ecdc.europa.eu/public/extensions/COVID-19/COVID-19.html#global-overview-tab (9 February 2022, date last accessed).
- 55. Global Health Observatory, World Health Organization. Coverage of Death Registration (%). 2021. https://www.who.int/data/gho/indicator-metadata-registry/imr-details/coverage-of-death-registration-(-) (9 May 2022, date last accessed).
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data underlying this study, beyond what is available in the article and in its online Supplementary material, can be shared to facilitate methodologically sound proposals after signing a data access agreement. Proposals and data requests should be directed to [demetriou.chri@unic.ac.cy].